- 1DeafKidz International, London, United Kingdom
- 2Ear Institute, University College London, London, United Kingdom
- 3SOUND lab, Department of Clinical Neurosciences, University of Cambridge, Cambridge, United Kingdom
- 4Audiology and ENT, Queen Elizabeth Central Hospital, Blantyre, Malawi
- 5School of Chemical and Biomolecular Engineering, Georgia Institute of Technology, Atlanta, GA, United States
- 6Interdisciplinary Graduate Program in Quantitative Biosciences, Georgia Institute of Technology, Atlanta, GA, United States
- 7Department of Otolaryngology–Head and Neck Surgery, University of Colorado School of Medicine, Aurora, CO, United States
- 8UCHealth Hearing and Balance, University of Colorado Hospital, Aurora, CO, United States
- 9Virtual Hearing Lab, Collaborative Initiative Between University of Colorado School of Medicine and University of Pretoria, Aurora, CO, United States
- 10Department of Speech-Language Pathology and Audiology, University of Pretoria, Gauteng, South Africa
- 11Department of Speech and Hearing, Manipal College of Health Professions, Manipal Academy of Higher Education, Manipal, India
Introduction: Access to ear and hearing health services are limited or non-existent in low-income countries, with less than 10% of the global production of hearing aids distributed to this population. The aim of this feasibility study was to compare the outcomes of an ultra-low-cost hearing aid (LoCHAid) to programmable, refurbished hearing aids for adults with high-frequency hearing loss, in Blantyre, Malawi.
Methods: Sixteen adults with high frequency hearing loss, and no prior experience of hearing aids, took part in this study, nine were fitted with the LoCHAid and seven were fitted with refurbished, programmable hearing aids, for a one-month trial. Five standardized hearing qualities questionnaires were used to compare outcomes pre and post device fitting and between devices. Questionnaire scales were analysed using general linear models and inductive thematic analysis was used to evaluate qualitative data.
Results: Overall, there was no significant difference found between LoCHAid and refurbished hearing aids, and the two device types each showed a similar degree of improvement after fitting. Qualitative data analysis identified two key themes: Sound Quality and User experience.
Conclusion: The results from this feasibility study are encouraging, but a comprehensive, larger clinical study is needed to draw firm conclusions about the LoCHAid's performance. This study has identified key improvement indicators required to enhance sound quality and user experience of the LoCHAid.
Introduction
Access to ear and hearing health services are limited or non-existent in low-income countries (1), with less than 10% of the global production of hearing aids being distributed to this population (2). Age-Related Hearing Loss (ARHL) is one of the most prevalent chronic conditions in older adults and is estimated to affect 900 million people by 2050 (3). ARHL is managed primarily through use of hearing aids (4), but uptake varies globally (5, 6).
One of the factors contributing to variable hearing aid uptake is cost. Hearing aids can cost between $500–$3,000 in the US. The WHO guideline states that a hearing aid should be no more than 3% of the gross national product, per capita, per hearing aid (7). Therefore, according to World Bank figures, for low-income, lower-middle income, and low- and middle-income countries combined, the affordable price would be approximately $20, $68, and $135, respectively. To address the growing need for hearing health, non-governmental organisations have been developing ear and hearing care services, and providing donated hearing aids, in low resource settings for many years (8–10). One of the key challenges in this process is the lack of trained local hearing healthcare professionals and a lack of specialised resources. Also, the large-scale fitting of donated hearing aids has several ethical implications. These could include the potential lack of associated lifelong audiological follow up, reduced access to hearing aid replacements, consumables and batteries and the choice of hearing aid model/manufacturer being dictated by the donation source and dependent on availability. Therefore, ongoing engagement with local stakeholders is key for the sustainability of effective, patient centred hearing aid services (11).
Ear and hearing care in Malawi
Malawi is a landlocked country located in southeastern Africa, sharing borders with Tanzania, Mozambique, and Zambia. It has a population of around 20 million people. Audiology and hearing healthcare services are extremely limited in Malawi (12). There are only two publicly available audiology departments in the country, one in Blantyre and one in Lilongwe. Within the public hospital system, there are two Ear, Nose and Throat (ENT) Specialist doctors; 32 ENT Clinical Officers (ENT clinical officers complete a 3-year diploma in clinical medicine and receive specialist ENT training); 4 audiology technicians and one audiologist.
Hearing aids are not routinely provided by the Malawian Ministry of Health. Instead, the country relies on donated hearing aids provided by charitable organisations (13). Despite donated hearing aids being available in cities including Lilongwe and Blantyre, much of Malawi's ear and hearing care needs are underserved. Furthermore, refurbished hearing aids are pre-used devices, and this process relies on a constant flow of hearing aids and the relevant consumables and programming tools from the donation source, into Malawi. Another barrier to uptake is that digital hearing aids mainly function by using a battery which is not locally available. A retrospective study to understand the profile of patients attending the Queen Elizabeth Central Hospital Audiology department in Blantyre, Malawi found that demand for hearing healthcare services is growing in Malawi, but hearing aid uptake is low (13). Of the 2,299 patients seen over a two-year period, 61% of adults were found to have some degree of hearing loss, but only 28% were fitted with refurbished hearing aids. Some patients had access to employment health insurance to pay towards the hearing aids, but others relied on self-funding. There is need for lower cost hearing devices for Malawian ear and hearing care services to become more accessible and sustainable.
The LoCHAid- an ultra low cost hearing aid for age related hearing loss
Preliminary data from both electroacoustic testing and simulated gain measurements demonstrates that a low-cost device, LoCHAid, provides amplification in the high frequency region that is needed for individuals with mild- to moderate ARHL (14). It is a minimal component hearing aid designed to address ARHL and has been adapted since the original study to improve user experience and sound quality. The LoCHAid is a body worn, pre-set, rechargeable, hearing device. Headphones are used rather than ear moulds or tubes to couple to the patient's ear. Due to the open-source nature of the device, it could be manufactured locally and could be offered to users with minimal cost. Although the original LoCHAid study confirmed the presence of the high frequency gain necessary to address ARHL, there is a need to clinically validate this technology, particularly in contexts where it may be of most use, i.e., low resource countries. Therefore, the primary aim of this feasibility study was to compare the self-reported outcomes and user experiences of the LoCHAid to programmable, refurbished hearing aids in individuals with high-frequency hearing loss.
Method
Study design and ethical considerations
This feasibility study involved the following phases: protocol development, participant recruitment, outcome measure translation, staff training and the clinical validation of the LoCHAid. The study was carried out at Queen Elizabeth Central Hospital Audiology department (QECH), Blantyre, Malawi.
Ethical approval was obtained from the Malawian College of Medicine Research and Ethics Committee (COMREC) (P.07/20/3091). Informed consent was obtained from all participants before the intervention was received. An information sheet was given to the participants, which outlined the purposes of the study. This was also summarized verbally before written consent was obtained.
Recruitment
A purposive sampling strategy was implemented to select people over the age of 18 years with bilateral mild to moderate high frequency sensorineural hearing loss, and no experience of hearing aid use, and no reported cognitive or neurological conditions. Recruitment took place during outreach clinical activities or clinical activities within QECH Audiology. Audiology clinicians carried out diagnostic otoscopy, pure tone audiometry and tympanometry on all patients. All participants were reimbursed their travel costs and given a financial incentive to attend each research session.
Staff training
The QECH audiology team were given remote and in-person training by a practicing audiologist (first author BP). Training included how to use the LoCHAid device, hearing aid fitting, hearing aid testing, counselling, study procedures, clinical testing, follow up and data management. Staff were in regular contact with the UK audiology team throughout the project. All QECH audiology technicians involved were also trained in basic research methods to aid the data collection process. All QECH staff assisted in creating the English and Chichewa hearing aid instruction manuals for the LoCHAid and the refurbished hearing aids.
Outcome measures
The five standardized hearing qualities or hearing aid benefit measures used in this project were chosen after a joint discussion within the research team. All outcome measures captured self-reported listening experiences (rather than measuring aided speech perception performance). The outcome measures were: Glasgow Hearing aid Benefit Questionnaire part one (GHABP) (15), Speech, Spatial and Qualities of Hearing Scale (SSQ-12) (16), Listening Effort Assessment Scale (EAS) (17), Satisfaction with Amplification in Daily Life Questionnaire (SADL) (18) International Outcome Inventory: Hearing Aids (IOI-HA) (19). The SADL is a fifteen-item questionnaire, divided into 4 subscales: positive effect, service and cost, negative features and personal image. However, an item referring to hearing aid cost and an item referring to telephone use were removed as the hearing aids were issued at no cost in this study, and the LoCHAid is not suitable to use with the telephone.
As all questionnaires were originally written and validated in English and because of the lack of hearing related outcome measures available in the Malawian national language of Chichewa, the questionnaires were translated to Chichewa by a qualified Malawian translator with had previously translated for research studies (20, 21). Forward and backward translation processes were implemented (22), and the Malawian audiology team were involved to assisted to ensure accurate translation of audiology specific technical terms. When translating research questionnaires, it is important to assure congruency between words and their true meaning in the language to which the questionnaire is translated (23). The Chichewa questionnaires were trialed on a small number of normal hearing adults and necessary amendments were made to improve consistency, accuracy and context. Open questions were also designed within a topic guide to explore participants' experiences of their hearing devices. The topic guide included questions about the overall user experience, preference of usage for specific situations and barriers to continued usage.
Hearing aids
Two types of hearing device were used in this feasibility study (see Table 2): a fixed-frequency-response low cost hearing aid (LoCHAid) (14) and a refurbished, programmable hearing aid (Oticon Spirit Zest). The LoCHAid has a fixed-frequency threshold, making it less tunable to individual participants' hearing thresholds, but more suitable for health professionals who have no specialist ear and hearing care training to fit. The LoCHAid was first demonstrated by the audiology clinician before the participant listened through the device. The programmable hearing aids were donations from the charitable organisation Deaf Kidz International (DKI) and they were cleaned, checked and reset by audiology clinicians at a DKI partner organisation based in Lusaka, Zambia. All refurbished hearing aids used in this study were behind-the-ear hearing aids—coupled to the appropriate slim tubes and domes, and used standard hearing aid batteries which were provided at the hearing aid fitting. They were programmed to participants' hearing thresholds using the NAL NL1 prescription formula (24). Fine tuning adjustments were made in the consultation to ensure adequate audibility and comfort for each participant.
Participants
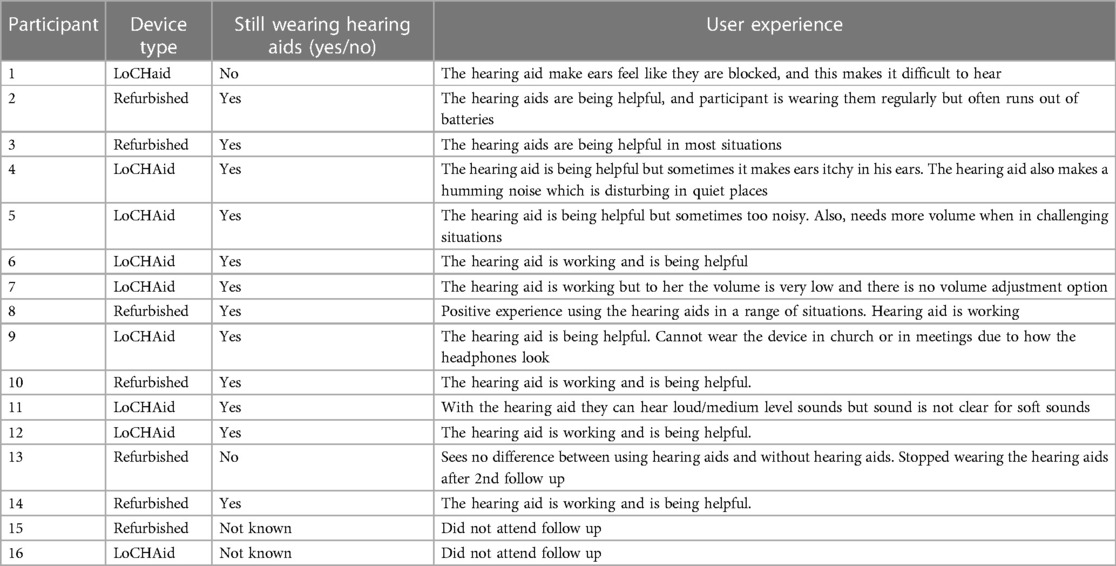
Initially, 18 participants consented to take part in the study where nine were randomized to the LoCHAid group, and nine to the refurbished hearing aid group. After hearing device fitting, 2 people from the refurbished hearing aid group withdrew from the study due to unforeseen circumstances. Therefore, sixteen participants with bilateral mild to moderate sensorineural hearing loss participated in this study. Demographics are described in Table 1. Hearing thresholds are presented in Figure 1.
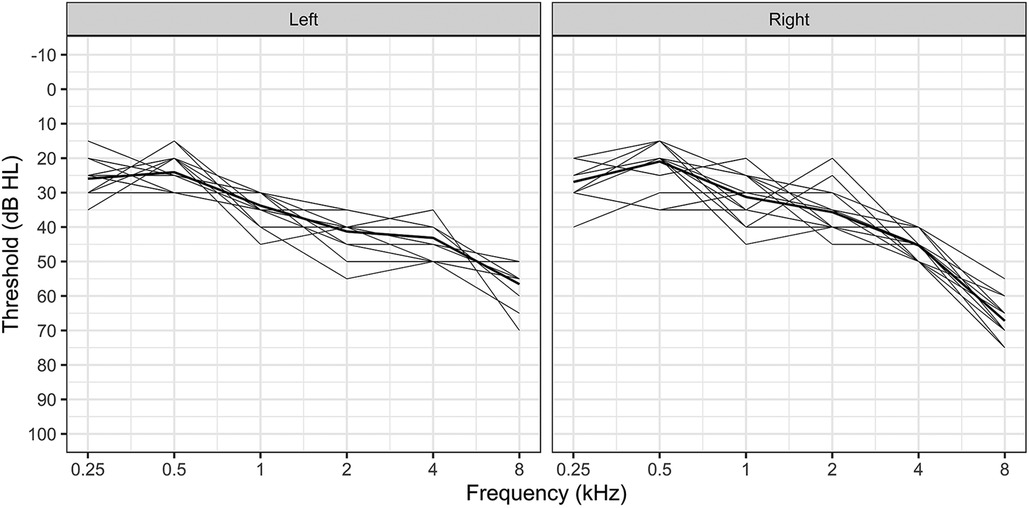
Figure 1. Hearing thresholds for all participants, presented for each ear. The bold line represents mean thresholds.
Study protocol
Each participant completed three in-person visits to the QECH Audiology department for this study.
During visit 1 participants completed a diagnostic audiological assessment, including the following 4 questionnaires:
- Demographics Questionnaire
- Glasgow Hearing aid Benefit Questionnaire part one (GHABP) (15)
- Speech, Spatial and Qualities of Hearing Scale (SSQ-12) (16)
- Listening Effort Assessment Scale (EAS) (17)
Participants were then randomly assigned to one of two groups: LoCHAid or refurbished hearing aids. The audiology clinicians carried out the hearing aid fittings using the allocated devices. Both groups were given detailed instruction booklets, specifically created for this study (written in Chichewa and English), to show them how to use the hearing aids and how to contact the audiology department. They were asked to use the hearing device as much as possible, in a variety of situations over the one-month trial. They were counseled on good communication tactics, realistic expectations, and acclimatization to the new sense of amplification, in line with typical clinical hearing aid fittings.
The follow up visit took place 4 weeks after the initial hearing aid fitting. The Chichewa versions of the following questionnaires were completed during the session:
- Glasgow hearing aid benefit questionnaire (GHABP) part two (15)
- Speech, Spatial and Qualities of Hearing Scale (SSQ-12) (16)
- Listening Effort Assessment Scale (EAS) (17)
- Satisfaction with Amplification in Daily Life Questionnaire (SADL) (18)
- International Outcome Inventory: Hearing Aids (IOI-HA) (19)
During the questionnaires, participants were asked to base their answers on their experience of hearing aid use within the one-month trial. After the follow up, participants were able to keep their trial hearing device if they wanted to. Additional open questions were asked in an interview style to explore the users' general usage and experience of the allocated hearing devices.
A second follow up was carried out 3 months after fitting to check for medium term hearing aid use. During the session, open questions were asked, and notes were transcribed by the QECH team.
Data analysis
As recommended in the literature, the SSQ12 subscales (speech, spatial, and qualities) were calculated by averaging the scores of the four items in each category together. The GHABP disability subscale was calculated by averaging across the four disability scenarios. Improvement in hearing was evaluated by comparing the extent of initial disability (recorded upon inclusion before device implementation) and the extent of residual disability (recorded at follow-up after device implementation). The SADL was analysed by using individual items and its established subscales. The listening effort assessment scale and the IOI-HA were evaluated by global score differences and with individual item comparisons, between hearing aid types.
Statistical modeling was completed using R version 4.1.1. The SSQ12, GHABP, and Listening Effort questionnaires were each completed both before and after hearing aid fitting. Linear mixed modelling for repeated measures was. We tested each subscale as a dependent variable against changes in scores over time (before vs. after hearing aid fitting), between devices (LoCHAid vs. refurbished), and for an interaction between the two to indicate whether one device changed more than another over time. We additionally included a random grouping factor for participant to control for repeated measures. Repeated measures modeling was completed using the R package lme4. Satisfaction with amplification in daily life and IOI-HA items were each addressed individually, using a general linear model, with each item tested for differences between devices. Estimated marginal means were calculated using the R package lsmeans (25). For all models, residuals were confirmed as normally distributed using QQ-plots with the Kolmogorov-Shapiro test for normality. Multicollinearity among predictors was tested by calculating the variance inflation factor and was deemed negligible.
Inductive thematic analysis (26) was carried out to analyse open text answers to questions including: “How would you describe your experience using the hearing device?”. Sub-questions included: “What situations did you like/dislike wearing your hearing device?”, “Is there anything you would like to change about your hearing device?”.
Positionality
Hearing aid fitting and follow ups were conducted in Chichewa by trained audiology technicians (authors MP, LJ and RK). BP (first author) was present in the clinic to assist the clinicians during the hearing device fitting appointments but did not make their presence known in case this influenced the flow of the appointments. BP completed the data analysis in collaboration with the Malawian audiology team to ensure contextual details were not overlooked or misinterpreted.
Results
Data from sixteen participants are presented in this study. Nine had been fitted with the LoCHAid device and seven wore bilateral refurbished hearing aids.
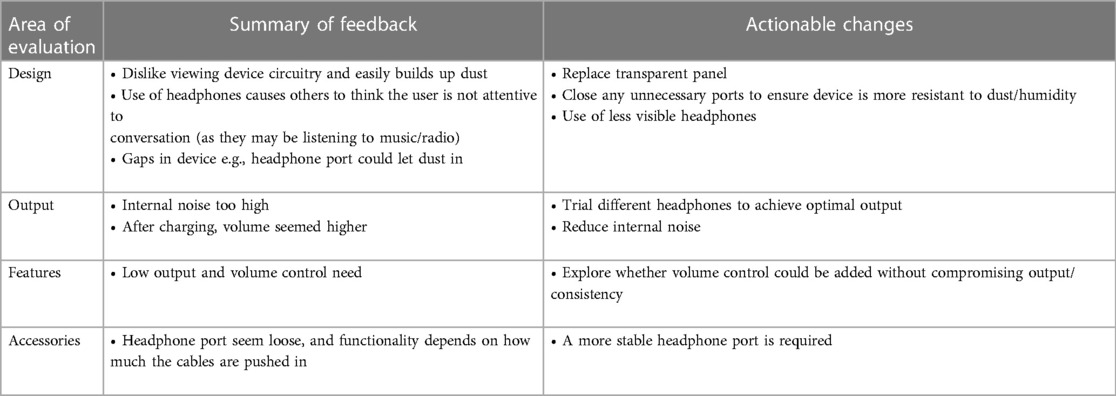
Glasgow hearing Aid benefit profile
Part one of the GHABP was completed at the first session, and part two was completed at the follow up session. Figure 2 displays the results of both parts, for both groups. Results were collapsed across the four questionnaire scenarios. The 6 dimensions of the GHABP: initial disability, initial handicap, HA use, HA benefits, residual disability, and HA satisfaction, for both devices can be seen in Figure 2. Overall, residual disability was reduced compared to the initial disability [subscale scores reduced from 2.56 (SE = 0.18) to 1.53 (SE = 0.18)]. This was a significant reduction [F(1, 13) = 5.15, p = 0.041]. However, there was no significant difference found between devices (LoCHAid vs. Refurbished), and the two device types each showed a similar degree of improvement after fitting.
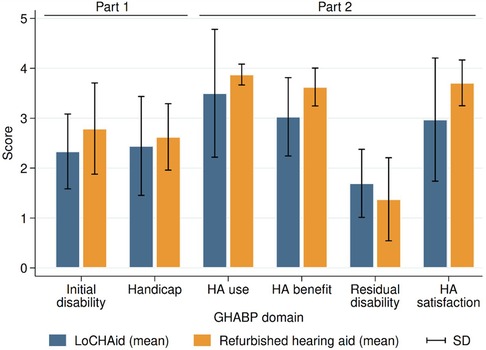
Figure 2. GHABP part one (pre fitting) and part two (post fitting) results. LoCHAid: n = 9, refurbished hearing aid: n = 7. Data collapsed across questions in each category with mean and standard deviation presented. Disability scores: 0 = no difficulty, 5 = cannot manage at all.
Speech, spatial and qualities of hearing scale (SSQ-12)
There was a significant improvement after device fitting in each of the speech [F(1, 13) = 13.24, p = 0.003], spatial [F(1, 13) = 8.45, p = 0.012] and qualities [F(1, 13) = 5.57, p = 0.035] subscales, as shown in Figure 3. However, there was no significant difference between LoCHAid vs. refurbished devices, and the degree of improvement after fitting was similar when comparing the two.
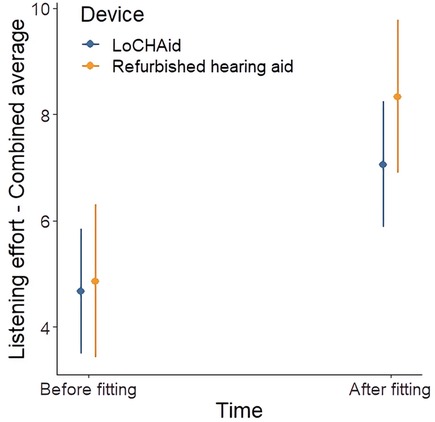
Figure 3. SSQ12 subscale scores before and after fitting for LoCHAid (n = 9) and refurbished devices (n = 7), with mean predicted scores and 95% confidence intervals shown. Category subscales 0 = not at all, 10 = perfectly. Example SSQ speech question with a score of 0 = “Not at all” and score of 10: “Perfectly”: “You are in conversation with one person in a room where there are many other people talking. Can you follow what the person you are talking to is saying?
Listening effort assessment scale (EAS)
Of the six items addressed in the EAS, five showed significant improvements over time, as outlined in Table 3. The only item which did not show a significant improvement was “How easily can you ignore other sounds when trying to listen to something”. Overall, there was no significant difference between LoCHAid vs. refurbished devices in any of the items, and the degree of improvement between time points was not significantly different between devices for any item. This same pattern was true for the global score, as shown in Table 3 and Figure 4.
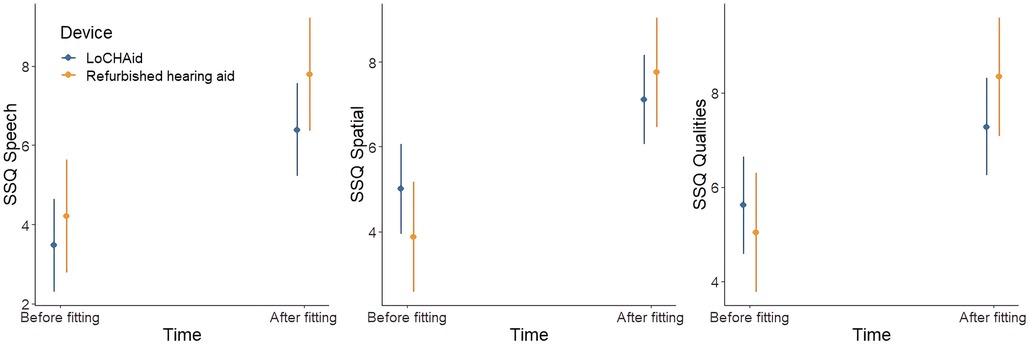
Figure 4. Listening effort assessment scale global score before and after fitting for LoCHAid and refurbished devices, with mean predicted scores and 95% confidence intervals shown. Higher score indicates less listening effort exerted.
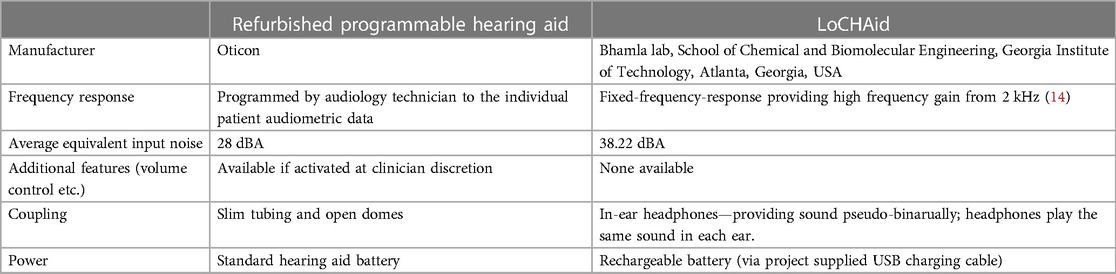
Table 2. Device characteristics and fitting parameters for LoCHAid and the refurbished programmable hearing aid.
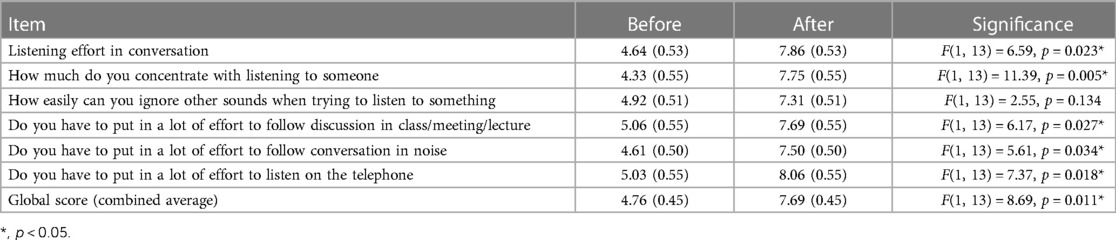
Table 3. Listening effort questionnaire items before and after hearing aid fitting, with estimated scores and standard error shown for each item (high score indicates less effort). Significant differences are shown using asterisks.
Satisfaction with amplification in daily life
Of the fifteen items in the SADL questionnaire, four indicated a significant preference toward refurbished devices relative to LoCHAid devices. These items are shown in Table 4. Overall, participants using refurbished hearing aids were significantly more likely to report improvements in the following parameters: helpful with understanding people, natural sounding, dependable, and worth the trouble, compared to those using the LoCHAid.
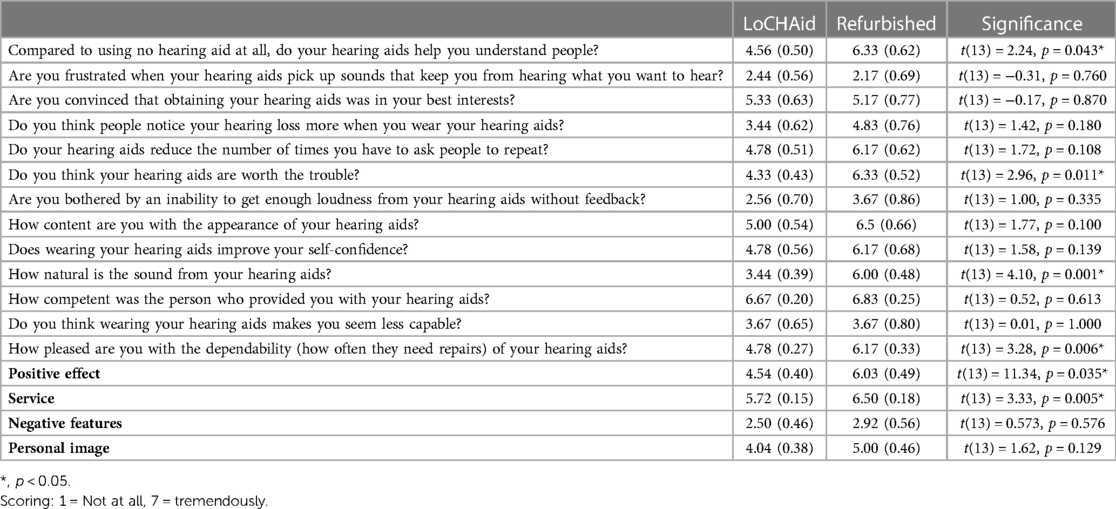
Table 4. SADL questionnaire items for each device type, with estimated scores and standard error shown for each item. Significant differences are shown using asterisks.
International outcome inventory: hearing aids (IOI-HA)
Of the seven items in the IOI-HA questionnaire, only one showed a significant difference between device types. Users of refurbished devices reported significantly less difficulty than they used to have in the situations that they considered most important for requiring a hearing aid, compared to the LoCHAid users (see Table 5).
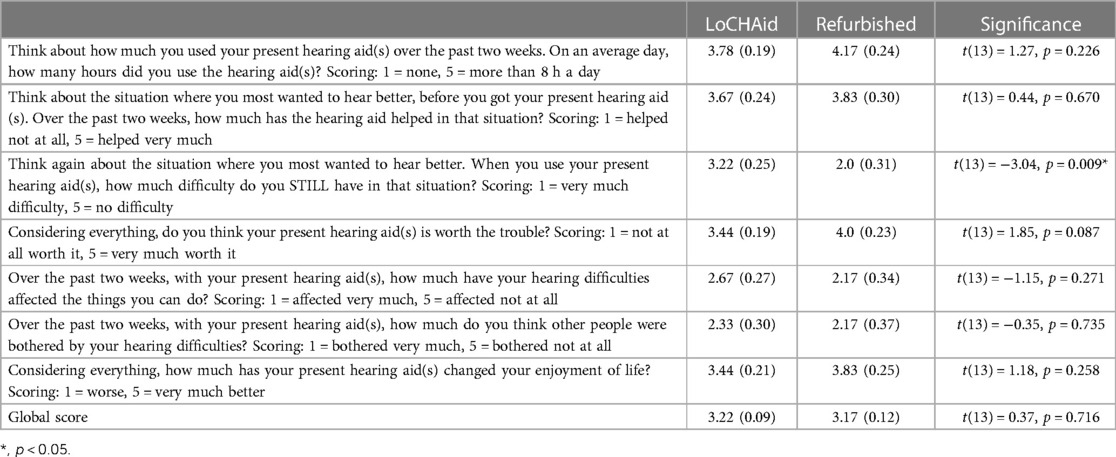
Table 5. IOI-HA questionnaire items for each device type, with estimated scores and standard error shown for each item. Significant differences are shown using asterisks.
Qualitative data
Two key themes from analysing the qualitative data obtained in the first follow up appointment are described below, with some example quotes. Table 6 summarises participant feedback from the second follow up session.
Theme 1: sound quality
Participants commented on the sound quality of the amplification and the internal noise of the hearing device. Overall, all participants reported positive experiences of the refurbished hearing aid's sound quality. However, those in the LoCHAid group reported that although the device improved their hearing ability, the internal noise from the device negatively impacted the listening experience.
“Apart from amplifying sound, the sound it also produces is a noise like when you are tuning a radio” (LoCHAid)
“Volume control would be very helpful because sometimes I needed it higher” (LoCHAid)
“I liked everything about the sound” (Refurbished)
“I can hear much better with the device and I can hear the things I couldn’t hear without it” (LoCHAid)
“I think I hear perfectly but it took some time to get used to it” (Refurbished)
“too noisy” (LoCHAid)
Theme 2: user experience
Some participants liked the appearance of the LoCHAid as it did not look like a traditional hearing aid and therefore helped them avoid unnecessary attention. However, others felt the use of headphones made it look like they were using a music device, e.g., radio, and therefore not paying attention to their surroundings. The structure of the LoCHAid was reported to be quite delicate and there were some concerns raised about the number of visible open ports which may cause the device to malfunction in humid, dusty environment. Participants also commented on overall appearance and usability of each device.
“The appearance is good, nobody knew it is hearing aid and that I have a hearing loss” (LoCHAid)
“It makes me look older” (Refurbished)
“Very easy to use” (Refurbished)
“Since it has headphones, you might wear it in places, you are not supposed to put headphones, people get disappointed in you” (LoCHAid)
“The machine has lots of open spaces where dust can get in, like where the headphones go and the on button switch” (LoCHAid)
“Needs to be more powerful or have a volume control so I can control it, also sometimes headphones come out of my ear if I am eating/chewing” (LoCHAid)
“At church people thought I was listening to my phone or the radio. People thought because I am old that I am wearing this device to listen to music and look younger. Maybe they thought I was being rude. It is a problem when it doesn’t look like something that is helping my medical condition” (LoCHAid)
“less visible headphones needed” (LoCHAid)
“The machine looks like it will break easily, what if I need a replacement or if the headphones stop working- can I use any headphones?” (LoCHAid)
“it is easy to put on and off, the colour of the headset makes it get dirty quickly. It improves my hearing, but the headphones can fall out easily. I don’t like being able to see inside the machine as I am worried it will break easily” (LoCHAid)
Discussion
This feasibility study is the first to clinically evaluate the effectiveness of the LoCHAid in a low resource setting. The results, from this Malawian population, found that the LoCHAid and the refurbished programmed hearing aids were similarly beneficial for people with high frequency hearing loss but that some improvements are required to improve the LoCHAid sound quality and user experience.
Low hearing aid uptake or hearing aid availability in Sub Saharan Africa has been noted in the literature (13, 27). Furthermore, many countries rely on hearing aid donations from non-governmental organisations (28, 29). A number of previous studies have explored the effectiveness of low cost hearing aids (30) and some research has piloted their use in low resource settings (31), as recommended in the WHO Guidelines for hearing aids and services for developing countries (2). Pienaar et al. (32) found positive patient benefit of hearing aid fitting in a South African context, even without optimal hearing aid fittings (suboptimal fitting due to financial constraints) (32). McPherson and Wong (33) used the IOI-HA to investigate the effectiveness of an affordable (approximately $125USD) pre-programmed hearing aid in Hong Kong, with most patients benefitting from the hearing aids. Qualitative interviews in the study found the main disadvantages of the device to be hearing aid design (e.g., difficult to change battery) and hearing aid related problems including feedback and internal noise. It is important to note that the LoCHAid is lower in cost than the low-cost hearing aids used in other studies (32–34).
The present study found the LoCHAid had potential to serve people with hearing loss in Malawi and broadly performed similarly to digitally programmed refurbished, donated, behind-the-ear hearing aids. Three standardized measures, SSQ-12, GHABP and EAS, were carried out before and after hearing aid fitting to explore the effectiveness of hearing aid use on various listening situations. Results from each of these outcome measures found that both devices, the LoCHAid and refurbished hearing aid, improved hearing abilities and listening effort (compared to the unaided experiences) at a similar degree. Two outcome measures reviewed overall hearing aid use and experience and were completed at the follow up appointment. Results from the SADL found that the LoCHAid was less helpful compared to the refurbished hearing aid in helping to understand people during conversation, the LoCHAid was less natural sounding and less dependable overall. Results from the IOI-HA found that users of refurbished devices reported significantly less difficulty, compared to LoCHAid, than they used to have in the situations that they considered most important for requiring a hearing aid. The poorer satisfaction of LoCHAid users could be due to the device providing sound pseudo-binaurally (through headphones playing the same sound in each ear), and the position of the body-worn microphone, affecting sound localisation and overall sound quality.
During the follow up visits, participants were asked open questions about their overall hearing aid use and experience and probing questions about how their device does or does not benefit them. This feedback was analysed to present key themes and summarized to identify some key improvement indicators required to improve the LoCHAid user experience. These improvement indicators included factors affecting the design, hearing aid output, features and accessories and are shown in Table 7. If these improvement indicators are actioned, the user experience would be improved, and this is likely to increase LoCHAid device use and device reliability.
The study had some limitations. Firstly, due to the nature of the device and its role in providing only high frequency amplification, finding the appropriate patient population for this trial was challenging. Despite running many outreach recruitment events, in neighboring villages and towns, the number with mild-moderate high frequency hearing loss, with no other otological symptoms was low. One of the reasons for this may have been because although recruitment activities were carried out in the community, the testing and hearing aid fitting was completed in a tertiary hospital setting (QECH). Other studies have found low-cost hearing aid provision to be similarly effective in community settings (34), therefore extending ear and hearing care beyond tertiary care would help reach a wider population. This project took place during the COVID-19 pandemic and was affected by many delays due to travel restrictions, procurement delays and staff shortages in Malawi. Our team were able to overcome these challenges by carrying out regular remote training sessions between our team in the UK and the Malawian audiology team. Also, we arranged for an audiology technician from another city in Malawi to work at QECH for the duration of this feasibility trial. Staffing shortages also introduced some potential for bias as the data collection activities were carried out by the same clinicians that fitted the hearing devices.
A key strength of this study was the involvement of the Malawian audiology clinicians as they were trained to recruit and consent participants, run the feasibility trial and had key involvement in the development of the outcome measures and the hearing aid instruction booklets. This experience and training would help future trials that take place at QECH.
There are currently no validated hearing aid outcome measures (speech perception tests or questionnaires) in Malawi. However, during the development phase of this study five hearing qualities/hearing aid benefit questionnaires were translated to Chichewa and validated with a small normal hearing adult population. Backwards and forwards translation was implemented by a professional English-Chichewa translation service and the audiology team at QECH cross checked all translations. Additional validation of these Chichewa questionnaires using a larger population would further confirm the consistency of the measures. Speech perception and speech in noise perception measures are used to guide and evaluate hearing aid fittings in audiology settings (35), but Chichewa measures of this kind are not currently available. A Digits in Noise test, or similar, could be used in future for this purpose, if self-reported English-competence and age were considered (36).
Conclusion and future research
The results from this feasibility study are encouraging, but a comprehensive, larger clinical study is needed to draw firm conclusions about the LoCHAid's performance. This study has identified key improvement indicators required to enhance sound quality and user experience of the LoCHAid. Once these improvements are made, further electroacoustic, speech perception and self-report testing should be completed on similar patient populations.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Malawian College of Medicine Research and Ethics Committee (COMREC) (P.07/20/3091). The patients/participants provided their written informed consent to participate in this study.
Author contributions
BP, MB, VM and WM designed the study. BP assisted data collection, completed data analysis and wrote the manuscript. MB and BS created the LoCHAid devices. MP and LJ assisted questionnaire translation, participant recruitment, data collection and data analysis. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Disability Impact Fund. B.P is funded by the National Institute of Health Research (NIHR) Programme grant for Applied Research (201608) and the Biomedical Research Centre (203312). The views expressed are those of the authors and not necessarily those of the NIHR of the Department of Health and Social Care (UK). MSB acknowledges funding support from Microsoft's AI for Accessibility program, NIH Grant R35GM142588, and the Open Philanthropy Project.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Wilson BS, Tucci DL, Merson MH, O'Donoghue GM. Global hearing health care: new findings and perspectives. Lancet. (2017) 390(10111):2503–15. doi: 10.1016/s0140-6736(17)31073-5
2. World Health Organization. Guidelines for hearing aids and services for developing countries. (2004). Available at: https://www.who.int/publications/i/item/guidelines-for-hearing-aids-and-services-for-developing-countries (Retrieved January 21, 2023).
3. World Health Organization. Deafness and hearing loss. (2021). Available at: https://www.who.int/news-room/fact-sheets/detail/deafness-and-hearing-loss
4. Van Eyken E, Van Camp G, Van Laer L. The complexity of age-related hearing impairment: contributing environmental and genetic factors. Audiol Neurootol. (2007) 12(6):345–58. doi: 10.1159/000106478
5. Bainbridge KE, Ramachandran V. Hearing aid use among older U.S. adults; the national health and nutrition examination survey, 2005–2006 and 2009–2010. Ear Hear. (2014) 35(3):289–94. doi: 10.1097/01.aud.0000441036.40169.29
6. Hartley D, Rochtchina E, Newall P, Golding M, Mitchell P. Use of hearing aids and assistive listening devices in an older Australian population. J Am Acad Audiol. (2010) 21(10):642–53. doi: 10.3766/jaaa.21.10.4
7. McPherson B. Innovative technology in hearing instruments: matching needs in the developing world. Trends Amplif. (2011) 15(4):209–14. doi: 10.1177/1084713811424887
8. Newall J, Biddulph R, Ramos H, Kwok C. Hearing aid or “band aid”? Evaluating large scale hearing aid donation programmes in the Philippines. Int J Audiol. (2019) 58(12):879–88. doi: 10.1080/14992027.2019.1666308
9. Thammaiah S, Manchaiah V, Easwar V, Krishna R, McPherson B. Community-based hearing rehabilitation: implementation and outcome evaluation. Perspectives ASHA SIG. (2017) 2(17):83–95. doi: 10.1044/persp2.SIG17.83
10. Wertz AP, Mannarelli G, Shuman AG, McKean EL. Comprehensive hearing aid intervention at a free subspecialty clinic. JAMA Otolaryngol Head Neck Surg. (2017) 143(9):876–80. doi: 10.1001/jamaoto.2017.0680
11. Kaspar A, Pifeleti S, Faumuina PA, Newton O, Driscoll C. Ethical issues for large-scale hearing aid donation programmes to the Pacific Islands: a samoan perspective. J Med Ethics. (2020) 46(10):710–2. doi: 10.1136/medethics-2020-106560
12. Mulwafu W, Fagan JJ, Mukara KB, Ibekwe TS. ENT outreach in Africa: rules of engagement. OTO Open. (2018) 2(2):2473974-18777220. doi: 10.1177/2473974-18777220
13. Parmar B, Phiri M, Caron C, Bright T, Mulwafu W. Development of a public audiology service in southern Malawi: profile of patients across two years. Int J Audiol. (2021) 60(10):789–96. doi: 10.1080/14992027.2020.1864486
14. Sinha S, Irani UD, Manchaiah V, Bhamla MS. LoCHAid: an ultra-low-cost hearing aid for age-related hearing loss. PLoS One. (2020) 15(9):e0238922. doi: 10.1371/journal.pone.0238922
15. Gatehouse S. Glasgow hearing aid benefit profile: derivation and validation of a client-centered outcome measure for hearing aid services. J Am Acad Audiol. (1999) 10(02):80–103. doi: 10.1055/s-0042-1748460
16. Noble W, Jensen NS, Naylor G, Bhullar N, Akeroyd MA. A short form of the speech, spatial and qualities of hearing scale suitable for clinical use: the SSQ12. Int J Audiol. (2013) 52(6):409–12. doi: 10.3109/14992027.2013.781278
17. Alhanbali S, Dawes P, Lloyd S, Munro KJ. Self-reported listening-related effort and fatigue in hearing-impaired adults. Ear Hear. (2017) 38(1):e39–48. doi: 10.1097/AUD.0000000000000361
18. Cox RM, Alexander GC. Measuring satisfaction with amplification in daily life: the SADL scale. Ear Hear. (1999) 20(4):306–20. doi: 10.1097/00003446-199908000-00004
19. Cox R, Hyde M, Gatehouse S, Noble W, Dillon H, Bentler R, et al. Optimal outcome measures, research priorities, and international cooperation. Ear Hear. (2000) 21(4):106S–15S. doi: 10.1097/00003446-200008001-00014
20. Manda-Taylor L, Kufankomwe M, Chatha G, Chipeta E, Mamani-Mategula E, Mwangi M, et al. Perceptions and experiences of intravenous iron treatment for anaemia in pregnancy in Malawi: a formative qualitative study. Gates Open Res. (2022) 6:66. doi: 10.12688/gatesopenres.13631.2
21. Singal N, Mbukwa-Ngwira J, Taneja-Johansson S, Lynch P, Chatha G, Umar E. Impact of COVID-19 on the education of children with disabilities in Malawi: reshaping parental engagement for the future. Int J Incl Educ. (2021):1–17. doi: 10.1080/13603116.2021.1965804
22. Hall DA, Zaragoza Domingo S, Hamdache LZ, Manchaiah V, Thammaiah S, Evans C, et al. A good practice guide for translating and adapting hearing-related questionnaires for different languages and cultures. Int J Audiol. (2018) 57(3):161–75. doi: 10.1080/14992027.2017.1393565
23. Eremenco SL, Cella D, Arnold BJ. A comprehensive method for the translation and cross-cultural validation of health status questionnaires. Eval Health Prof. (2005) 28(2):212–32. doi: 10.1177/0163278705275342
24. Byrne D, Dillon H, Ching T, Katsch R, Keidser G. NAL-NL1 procedure for fitting nonlinear hearing aids: characteristics and comparisons with other procedures. J Am Acad Audiol. (2001) 12(1):37–51. doi: 10.1055/s-0041-1741117
25. Lenth R. Least-Squares means: the R package lsmeans. J Stat Softw. (2016) 69:1–33. doi: 10.18637/jss.v069.i01
26. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. (2006) 3(2):77–101. doi: 10.1191/1478088706qp063oa
27. Hlayisi V-G, Ramma L. Rehabilitation for disabling hearing loss: evaluating the need relative to provision of hearing aids in the public health care system. Disabil Rehabil. (2019) 41(22):2704–7. doi: 10.1080/09638288.2018.1473507
28. Seelman KD, Werner R. Technology transfer of hearing aids to low and middle income countries: policy and market factors. Disabil Rehabil Assist Technol. (2014) 9(5):399–407. doi: 10.3109/17483107.2014.905641
29. Thiga E, Awori B, Abuom T. Perceptions on hearing aid use and its influence on self-esteem of learners with hearing impairment in integrated settings in Nairobi city county, Kenya. J Educ Train. (2022) 10:100. doi: 10.5296/jet.v10i1.20301
30. Parving A, Christensen B. Clinical trial of a low-cost, solar-powered hearing aid. Acta Otolaryngol. (2004) 124(4):416–20. doi: 10.1080/00016480310000638a
31. Vo QT, Pham D, Choi KJ, Nguyen UTT, Le L, Shanewise T, et al. Solar-powered hearing aids for children with impaired hearing in Vietnam: a pilot study. Paediatr Int Child Health. (2018) 38(1):40–5. doi: 10.1080/20469047.2016.1276119
32. Pienaar E, Stearn N, Swanepoel de W. Self-reported outcomes of aural rehabilitation for adult hearing aid users in a South African context. S Afr J Commun Disord. (2010) 57:4–10. doi: 10.4102/sajcd.v57i1.44
33. McPherson B, Wong ETL. Effectiveness of an affordable hearing aid with elderly persons. Disabil Rehabil. (2005) 27(11):601–9. doi: 10.1080/09638280400019682
34. Borg J, Ekman BO, Östergren PO. Is centre-based provision of hearing aids better than community-based provision? A cluster-randomized trial among adolescents in Bangladesh. Disabil Rehabil Assist Technol. (2018) 13(6):497–503. doi: 10.1080/17483107.2017.1332110
35. Parmar BJ, Rajasingam SL, Bizley JK, Vickers DA. Factors affecting the use of speech testing in adult audiology. Am J Audiol. (2022) 31(3):528–40. doi: 10.1044/2022_aja-21-00233
Keywords: audiology, low- and lower-middle-income countries, hearing, hearing device evaluation, hearing aid (HA)
Citation: Parmar B, Phiri M, Jailos L, Kachapila R, Saleb B, Mulwafu W, Manchaiah V and Bhamla MS (2023) Comparing outcomes of ultra-low-cost hearing aids to programmable, refurbished hearing aids for adults with high frequency hearing loss in Malawi: a feasibility study. Front. Rehabil. Sci. 4:1153056. doi: 10.3389/fresc.2023.1153056
Received: 28 January 2023; Accepted: 8 May 2023;
Published: 12 June 2023.
Edited by:
Muhammad Raheel Afzal, Flanders Make, BelgiumReviewed by:
Marguerite Schneider, University of Cape Town, South AfricaBradley McPherson, The University of Hong Kong, Hong Kong SAR, China
© 2023 Parmar, Phiri, Jailos, Kachapila, Saleb, Mulwafu, Manchaiah and Bhamla. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bhavisha Parmar YnA0NzJAY2FtLmFjLnVr
 Bhavisha Parmar
Bhavisha Parmar Mwanaisha Phiri4
Mwanaisha Phiri4 Regina Kachapila
Regina Kachapila Vinay Manchaiah
Vinay Manchaiah M. Saad Bhamla
M. Saad Bhamla