- 1Department of Physical Medicine and Rehabilitation, Donald and Barbara Zucker School of Medicine at Hofstra Northwell, Hempstead, NY, United States
- 2Institute of Molecular Medicine, The Feinstein Institute for Medical Research, New York, NY, United States
- 3Department of Rehabilitation Services, Northwell Health, New York, NY, United States
Objective: To investigate the incidence and severity of pressure injuries among COVID-19 patients who required acute hospitalization and subsequent acute inpatient rehabilitation (AIR).
Design: Data was collected retrospectively from medical charts of COVID-19 patients who were admitted to AIR during April 2020–April 2021.
Setting: Acute Inpatient Rehabilitation at a single hospital in the greater New York metropolitan area.
Participants: Subjects included COVID-19 patients (N = 120) who required acute hospitalization and subsequent acute inpatient rehabilitation, of whom 39 (32.5%) had pressure injuries.
Interventions: Not applicable.
Main outcome measure(s): The incidence, location, and severity of pressure injuries in COVID-19 patients, as well as demographic and clinical characteristics of the acute hospitalization.
Results: Among patients who developed pressure injuries, more patients received mechanical ventilation (59% vs. 33%, P < 0.05) and tracheostomy (67% vs. 17%, P < 0.00001). The lengths of stay were longer in both the intensive care unit (ICU) (34 vs. 15 days, P < 0.005), and in acute inpatient rehabilitation (22 vs. 17 days P < 0.05).
Conclusion: Pressure injuries were more common in COVID-19 patients who had longer lengths of stay, received mechanical ventilation or tracheostomy, during acute hospitalization. This supports the use of protocols to prioritize pressure offloading in this patient population.
Introduction
In 2019, the novel coronavirus 2 (SARS-CoV-2) started a global pandemic that remains ongoing. Early in the pandemic, New York City (NYC) and the surrounding metropolitan area experienced an exponential surge of acutely ill COVID-19 patients who required acute hospitalization (1). Patients who experience critical illness have a wide range of disabilities requiring intensive rehabilitation. COVID-19 patients incurred prolonged acute hospitalizations and ICU treatments with subsequent disability necessitating intensive inpatient rehabilitation (2). Between March 2020 and April 2020, out of the 5,700 patients admitted to a NY-based hospital system, 14% were admitted to the intensive care unit (ICU) (3). On discharge, 5.9% of the patients were discharged to a post-acute facility such as acute inpatient rehabilitation (AIR) or skilled nursing facility to address functional decline and to manage ongoing medical needs (3).
Pressure injuries are a potential complication experienced by critically ill patients due to immobility from prolonged hospitalization, direct pressure from positioning during proning and a systemic inflammatory response (4). Pressure injuries can develop through a variety of environmental or physical conditions such as age, smoking, diabetes mellitus, peripheral vascular disease, immobility, and direct pressure (5–7). Because pressure injuries are most commonly caused by immobility or prolonged direct pressure, there is a high incidence of pressure injury development in patients in the ICU (8). Patients who are bedridden have a 5-fold increased risk and patients who required the use of wheelchairs had a 4-fold increased risk of developing pressure injuries (9). Furthermore, medical device related pressure injuries account for approximately 35% of hospital-acquired pressure injuries (HAPI) (10). Mechanical ventilation accounts for 28% of all HAPIs in the critical care patient population (11). The incidence rate of ICU-acquired pressure injuries rate is highly variable and has been reported from 3% to 56% (12, 13).
The goal of this study was to characterize the incidence and severity of pressure injuries among COVID-19 patients who required acute hospitalization and subsequent acute inpatient rehabilitation in the NY metropolitan area during the first surge in 2020.
Methods
Data was collected retrospectively from medical charts of COVID-19 patients who were admitted during April 2020–April 2021 to Acute Inpatient Rehabilitation (AIR) at a single hospital in the greater New York metropolitan area. Data was collected from electronic health records (Allscripts and Sunrise) in a HIPAA compliant database in RedCap. Inclusion criteria were patients who were admitted sequentially for inpatient rehabilitation after acute hospitalization for COVID-19. Patient records were classified into groups based on the presence or absence of pressure injuries acquired during their acute care hospitalizations. Data collected included: gender, age, race, ethnicity, ICU length of stay, AIR length of stay, rates of mechanical ventilation in the ICU, rates of tracheostomy in the ICU, rates of proning in the ICU, number of pressure injuries, stages of pressure injuries, and location of pressure injuries. Statistical significance was determined using unpaired T-tests, with significance P < 0.05 using Prism GraphPAD Software. For comparison, historical data was extracted from the Uniform Data System (UDS) for 2019, prior to the COVID-19 pandemic. The numbers of patients that developed pressure injuries obtained from this period of time were from a large sample size of 1,345 patients and thus were able to provide a good estimate of pressure injury incidence pre-COVID-19.
Results
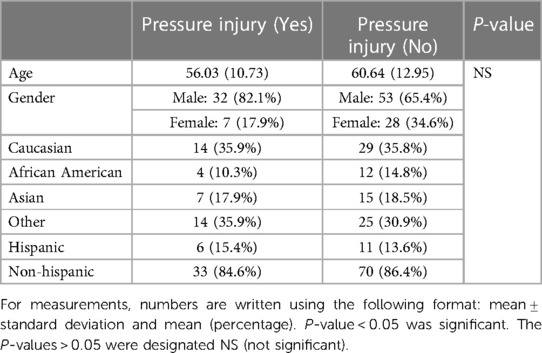
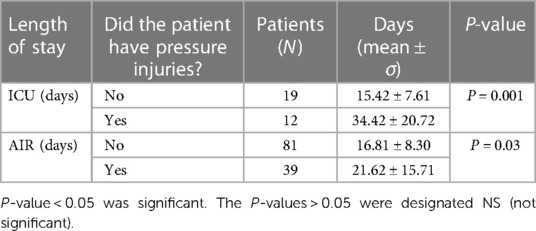
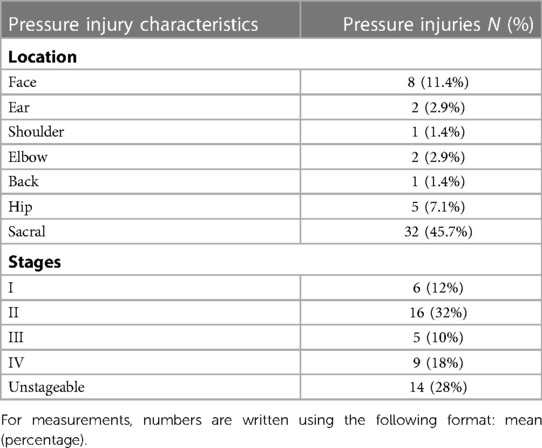
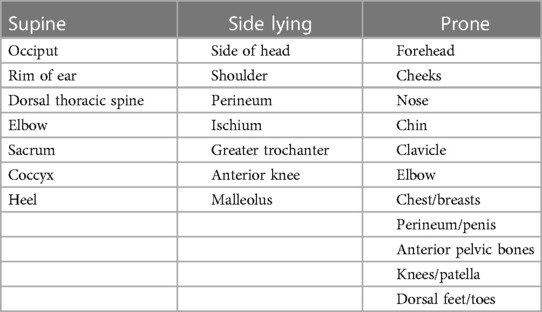
There were 120 patients who satisfied the inclusion criteria for the study, of whom 39 (32.5%) had pressure injuries. By comparison, UDS data obtained from the same facility in 2019 showed 1.7% patients admitted to AIR had pressure injuries. Clinical and demographic information is provided in Table 1. The age of patients was 56 ± 10.7 in the pressure injury group and 60.6 ± 12.9 in the non-pressure injury group. Age, race and ethnicity were comparable between the two groups. Both groups were predominantly male (Table 1). Length of stay in the ICU was longer for patients with pressure injuries (34 vs. 15 days, P < 0.005) (Table 2). Length of stay in acute inpatient rehabilitation was longer for patients with pressure injuries (22 vs. 17 days, P < 0.05) (Table 2). The number of patients who received mechanical ventilation was higher in the group that developed pressure injuries (59.0% vs. 33%, P < 0.01) (Table 3). Tracheostomy rates were higher for patients with pressure injuries (67% vs. 17%, P < 0.00001) (Table 3). Rates of proning were comparable between the groups (Table 3). Of the 70 pressure injuries with recorded location data, most (N = 60, 85.7%) had typical pressure injuries in typical locations, while a minority (N = 10, 14.3%) had atypical pressure injury locations, such as the face and ear (Table 4) (14).
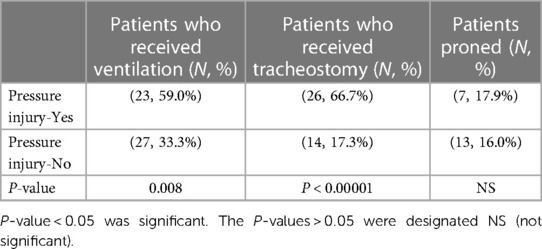
Table 3. Ventilation, tracheostomy, and proning in the ICU of COVID-19 patients ± pressure injuries.
Discussion
This study examined rates of pressure injury development in COVID-19 patients who were admitted to AIR from April 2020–April 2021. Patients who were admitted with pressure injuries were more likely to have received mechanical ventilation and tracheostomy and had significantly longer length of stay in the ICU and d acute inpatient rehabilitation. Similarly, from April 1 to May 9, 2020, Kendall et al. noted that the prevalence and severity of pressure injuries in inpatient rehabilitation hospital patients increased by 15%, compared to patients admitted before the pandemic (Jan 1–Feb 12, 2020) (15). Sianes-Gallén et al. observed that among 1987 COVID-19 patients, 136 patients (6.8%) developed dependency-related injuries (pressure injuries, moisture-related injuries, friction-related injuries, and skin tears), with 99 of them (73%) being pressure injuries (16). Rrapi et al. identified prolonged lengths of stay and high rates of endotracheal intubation as risk factors of pressure injury development in COVID-19 patients (17).
There are likely several types of risk factors promoting increased incidence and severity of pressure injuries among COVID-19 patients. Molecular mechanisms of tissue injury by SARS-CoV-2 may exacerbate the quantity and severity of the pressure injuries in COVID-10 patients, which may be due in part to the increased risk of thrombosis, microvascular injury, and hypoxemia experienced by COVID-19 patients (16, 18). In addition, SARS-CoV-2 patients are known to have higher activation of systemic inflammation as demonstrated by Zanella et al. (19). Prior to the current pandemic, risk factors that are most associated with increased pressure injury development in the ICU are age, history of diabetes mellitus, define MBP < 60–70 mmHg, mechanical ventilation, and prolonged length of stay (8, 20–22). Between March 1–April 30, 2020, 3,176 out of 11, 542 (27.5%) COVID-19 admissions to acute care hospitals in NY received mechanical ventilation (23). Prone positioning while the patient is undergoing mechanical ventilation is thought to reduce posterior alveoli atelectasis by reducing intrapulmonary shunting and improving ventilation-perfusion matching throughout the lungs (24). However, proning exerts compressive forces on the mouth and nose, increasing the risk of pressure injury to the face by 3-fold (18, 25–27). In the present study, 14.3% of the pressure injuries that had location data were on the face and ears, which are atypical locations for pressure injury development and may have resulted from proning. However, in this study, proning was not statistically significant with regards to pressure injury development, which may have resulted from the limited data available for rates of proning between the two groups of patients.
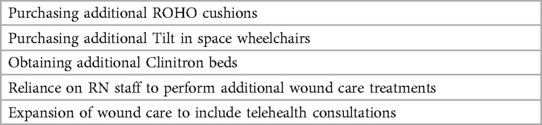
Also, during the study period, staffing shortages led to hiring of medical personnel with less advanced training, such as medical students as temporary residents, to supplement the medical workforce (28, 29). Furthermore, staffing shortages crossed multiple sectors, as U.S. nursing homes also reported shortages of nurse staff and clinical staff between 2.5% and 18.4% (30). In addition, due to isolation precautions and clinical staff shortages, rehabilitation and mobilization of patients may have been delayed (31). During the first COVID-19 surge (April 2020–2021), AIR units were forced to adapt quickly in order to provide care for a rapidly increasing number of patients. This included changes to infection control policies, space allocation for therapy and staffing modifications (32). Patients in AIR were admitted for a wide range of physical and cognitive disabilities following COVID-19 infection, such as stroke, debility from respiratory failure, vascular complications such as amputation and peripheral neuropathy (2). In this study, patients admitted to AIR with pressure injury had a statistically significant longer length of stay in both the ICU (34 vs. 15 days, P < 0.0005) and in acute rehabilitation (22 vs. 17 days, P < 0.05) when compared to the group without pressure injury. This may be due in part to the involved care needed to discharge a patient with a wound to the community, as homecare services were limited during the initial surge of COVID-19 patients. Longer lengths of stay in the ICU and AIR may contribute to delay of acute care hospitals to discharge their patients and increased healthcare costs. For example, in 2019, Padula et al. estimated that US hospital-acquired pressure injuries cost $10,708 per patient, and the U.S. had a national average of 2.5 million reported cases, potential costing $26.8 billion annually (33). The COVID-19 pandemic was an unprecedented challenge to the healthcare system as a whole in terms of resource and staff availability (36). During the initial surge of COVID-19 patients, homecare services were limited which may have contributed in part to longer lengths of stay for patients in this study. Given the significant increase in pressure injuries in COVID-19 patients admitted to AIR (32.5% vs. 1.7% of patients during the study period compared to 2019), it was necessary to purchase extra equipment, as well as to expand the wound care treatment team (physicians and nurses) who were able to provide consultations through the use of telehealth (Table 5).
Given hospital ICU surges observed across the U.S. during each wave of the pandemic, developing strategies to prevent pressure injury among patients admitted to ICUs with COVID-19 is warranted. After noting a steady increase of pressure injuries during the first surge (March to May 2020), Polancich et al. observed that prone placement was a significant risk factor for pressure injury development. Thus, they were able to implement interventional strategies, such as placing silicon adhesive dressings on pressure points on the prone patients (34, 35). One such set of recommendations adapted for the care of COVID-19 patients in the acute care setting is summarized in Tables 6, 7, so that similar pandemic surges in the future will have decreased pressure injury incidence (36–39).
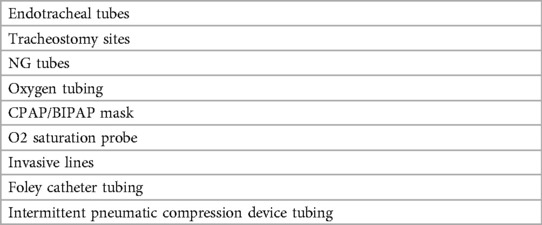
Table 7. Recommendations for off-loading of medical devices to decrease pressure injuries in critically ill patients.
This study had several limitations. First, this was a retrospective study. Second, there was a small sample size (N = 120 cases) that satisfied inclusion and exclusion criteria. Third, the comparison of COVID-19 data was to historical data (prior to the COVID-19 pandemic) and not non-COVID-19 patients treated in the same AIR during the same time period. In the future, other covariates such as preexisting comorbidities and time to healing of pressure injury can also be examined to see the effect COVID-19 may or may not have on pressure injuries. Finally, future studies can also examine whether or not having COVID-19 specifically increases the skin to be prone to pressure injury.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by Northwell Health IRB. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
WL, SM, OB contributed to conception and design of the study. WL organized the database. OB performed the statistical analysis. WL wrote the first draft of the manuscript. WL, SM, MR wrote sections of the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fresc.2023.1058982/full#supplementary-material.
Abbreviations
SARS-CoV-2, coronavirus 2; AIR, acute inpatient rehabilitation; ICU, intensive care unit; HAPI, hospital-acquired pressure injuries.
References
1. N, P, R. New York City, U.S. Epicenter, Braces For Peak. NPR. Available at: https://www.npr.org/2020/03/24/820610818/new-york-city-u-s-epicenter-braces-for-peak (Accessed January 20, 2022).
2. Maltser S, Trovato E, Fusco HN, Sison CP, Ambrose AF, Herrera J, et al. Challenges and lessons learned for acute inpatient rehabilitation of persons with COVID-19: clinical presentation, assessment, needs, and services utilization. Am J Phys Med Rehabil. (2021) 100(12):1115–23. doi: 10.1097/PHM.0000000000001887
3. Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York city area. J Am Med Assoc. (2020) 323(20):2052–9. doi: 10.1001/jama.2020.6775
4. Loehner D, Culleton C, Feinstein AM, Gunning ME, Melina M, Norberg M. COVID-19 skin manifestations versus deep-tissue pressure injuries in the acute care setting: a view from here. J Wound Ostomy Cont Nurs. (2021) 48(5):466–7. doi: 10.1097/WON.0000000000000788
5. Medical Advisory Secretariat. Management of chronic pressure ulcers: an evidence-based analysis. Ont Health Technol Assess Ser. (2009) 9(3):1–203. PMID: 23074533; PMCID: PMC3377577
6. Allman RM. Pressure ulcer prevalence, incidence, risk factors, and impact. Clin Geriatr Med. (1997) 13(3):421–36. doi: 10.1016/S0749-0690(18)30152-6
7. Qaseem A, Humphrey LL, Forciea MA, Starkey M, Denberg TD: Clinical Guidelines Committee of the American College of Physicians. Treatment of pressure ulcers: a clinical practice guideline from the American College of Physicians. Ann Intern Med. (2015) 162(5):370–9. doi: 10.7326/M14-1568
8. Lima Serrano M, González Méndez MI, Carrasco Cebollero FM, Lima Rodríguez JS. Risk factors for pressure ulcer development in intensive care units: a systematic review. Med Intensiva Engl Ed. (2017) 41(6):339–46. doi: 10.1016/j.medine.2017.04.006
9. Tervo-Heikkinen TA, Heikkilä A, Koivunen M, Kortteisto TR, Peltokoski J, Salmela S, et al. Pressure injury prevalence and incidence in acute inpatient care and related risk factors: a cross-sectional national study. Int Wound J. (2022) 19(4):919–31. doi: 10.1111/iwj.13692
10. Black JM, Cuddigan JE, Walko MA, Didier LA, Lander MJ, Kelpe MR. Medical device related pressure ulcers in hospitalized patients. Int Wound J. (2010) 7(5):358–65. doi: 10.1111/j.1742-481X.2010.00699.x
11. Cox J. Predictors of pressure ulcers in adult critical care patients. Am J Crit Care. (2011) 20(5):364–75. doi: 10.4037/ajcc2011934
12. Tescher AN, Branda ME, Byrne TJO, Naessens JM. All at-risk patients are not created equal: analysis of braden pressure ulcer risk scores to identify specific risks. J Wound Ostomy Continence Nurs. (2012) 39(3):282–91. doi: 10.1097/WON.0b013e3182435715
13. Jiricka MK, Ryan P, Carvalho MA, Bukvich J. Pressure ulcer risk factors in an ICU population. Am J Crit Care. (1995) 4(5):361–7. PMID: 7489039
14. Chaboyer WP, Thalib L, Harbeck EL, Coyer FM, Blot S, Bull CF, et al. Incidence and prevalence of pressure injuries in adult intensive care patients: a systematic review and meta-analysis. Crit Care Med. (2018) 46(11):e1074. doi: 10.1097/CCM.0000000000003366
15. Kendall JA, Haberl JK, Hartsgrove C, Murphy LF, DeLuca R, Diaz-Segarra N, et al. Surveillance for pressure injuries on admission to inpatient rehabilitation hospitals during the COVID-19 pandemic. Arch Phys Med Rehabil. (2021) 102(10):1932–8. doi: 10.1016/j.apmr.2021.06.011
16. Sianes-Gallén M, Pujol-García AM, Rus García M, Partera Luque C, Lopez Postigo M, Call Manosa S, et al. Pressure injuries during the SARS-CoV-2 pandemic: a retrospective, case-control study. J Tissue Viability. (2021) 30(4):478–83. doi: 10.1016/j.jtv.2021.07.011
17. Rrapi R, Chand S, Lo JA, Gabel CK, Song S, Holcomb Z, et al. The significance of pressure injuries and purpura in COVID-19 patients hospitalized at a large urban academic medical center: a retrospective cohort study. J Am Acad Dermatol. (2021) 85(2):462–4. doi: 10.1016/j.jaad.2021.03.051
18. Ramondetta A, Ribero S, Costi S, Dapavo P. Pression-induced facial ulcers by prone position for COVID-19 mechanical ventilation. Dermatol Ther. (2020) 33:e13748. doi: 10.1111/dth.13748
19. Zanella A, Florio G, Antonelli M, Bellani G, Berselli A, Bove T, et al. Time course of risk factors associated with mortality of 1260 critically ill patients with COVID-19 admitted to 24 Italian intensive care units. Intensive Care Med. (2021) 47(9):995–1008. doi: 10.1007/s00134-021-06495-y
20. Jiang Q, Li X, Qu X, Liu Y, Zhang L, Su C, et al. The incidence, risk factors and characteristics of pressure ulcers in hospitalized patients in China. Int J Clin Exp Pathol. (2014) 7(5):2587–94. PMID: 24966973; PMCID: PMC406992324966973
21. Tayyib N, Coyer F, Lewis P. Saudi Arabian adult intensive care unit pressure ulcer incidence and risk factors: a prospective cohort study. Int Wound J. (2016) 13(5):912–9. doi: 10.1111/iwj.12406
22. Coleman S, Gorecki C, Nelson EA, Closs SJ, Defloor T, Halfens R, et al. Patient risk factors for pressure ulcer development: systematic review. Int J Nurs Stud. (2013) 50(7):974–1003. doi: 10.1016/j.ijnurstu.2012.11.019
23. Jafari D, Gandomi A, Makhnevich A, Qiu M, Rolston D, Gottesman EP, et al. Trajectories of hypoxemia and pulmonary mechanics of COVID-19 ARDS in the NorthCARDS dataset. BMC Pulm Med. (2022) 22:51. doi: 10.1186/s12890-021-01732-y
24. Sud S, Friedrich JO, Adhikari NKJ, Taccone P, Mancebo J, Polli F, et al. Effect of prone positioning during mechanical ventilation on mortality among patients with acute respiratory distress syndrome: a systematic review and meta-analysis. Can Med Assoc J. (2014) 186(10):E381–390. doi: 10.1503/cmaj.140081
25. Challoner T, Vesel T, Dosanjh A, Kok K. The risk of pressure ulcers in a proned COVID population. Surgeon. (2021) 20(4):e144-e8. doi: 10.1016/j.surge.2021.07.001
26. Gefen A, Ousey K. Update to device-related pressure ulcers: SECURE prevention. COVID-19, face masks and skin damage. J Wound Care. (2020) 29(5):245–59. doi: 10.12968/jowc.2020.29.5.245
27. Girard R, Baboi L, Ayzac L, Richard JC, Guérin C, Proseva Trial Group. The impact of patient positioning on pressure ulcers in patients with severe ARDS: results from a multicentre randomised controlled trial on prone positioning. Intensive Care Med. (2014) 40(3):397–403. doi: 10.1007/s00134-013-3188-1
28. Rasmussen S, Sperling P, Poulsen MS, Emmersen J, Andersen S. Medical students for health-care staff shortages during the COVID-19 pandemic. Lancet Lond Engl. (2020) 395(10234):e79–80. doi: 10.1016/S0140-6736(20)30923-5
29. Martel T, Orgill DP. Medical device–related pressure injuries during the COVID-19 pandemic. J Wound Ostomy Continence Nurs. (2020) 47(5):430–4. doi: 10.1097/WON.0000000000000689
30. Xu H, Intrator O, Bowblis JR. Shortages of staff in nursing homes during the COVID-19 pandemic: what are the driving factors? J Am Med Dir Assoc. (2020) 21(10):1371–7. doi: 10.1016/j.jamda.2020.08.002
31. Deana C, Verriello L, Pauletto G, Corradi F, Forfori F, Cammarota G, et al. Insights into neurological dysfunction of critically ill COVID-19 patients. Trends Anaesth Crit Care. (2021) 36:30–8. doi: 10.1016/j.tacc.2020.09.005
32. McNeary L, Maltser S, Verduzco-Gutierrez M. Navigating coronavirus disease 2019 (COVID-19) in physiatry: a CAN report for inpatient rehabilitation facilities. PM R. (2020) 12(5):512–5. doi: 10.1002/pmrj.12369
33. Padula WV, Delarmente BA. The national cost of hospital-acquired pressure injuries in the United States. Int Wound J. (2019) 16(3):634–40. doi: 10.1111/iwj.13071
34. Polancich S, Hall AG, Miltner R, Poe T, Enogela EM, Montgomery AP, et al. Learning during crisis: the impact of COVID-19 on hospital-acquired pressure injury incidence. J Healthc Qual. (2021) 43(3):137–44. doi: 10.1097/JHQ.0000000000000301
35. Polancich S, Williamson J, Poe T, Armstrong A, Vander Noot RM. Innovations in pressure injury reporting: creating actionable data for improvement. J Healthc Qual. (2019) 41(3):180–7. doi: 10.1097/JHQ.0000000000000196
36. Gillespie BM, Walker RM, Latimer SL, Thalib L, Whitty JA, McInnes E, et al. Repositioning for pressure injury prevention in adults: an abridged cochrane systematic review and meta-analysis. Int J Nurs Stud. (2021) 120:103976. doi: 10.1016/j.ijnurstu.2021.103976
37. Lin F, Wu Z, Song B, Coyer F, Chaboyer W. The effectiveness of multicomponent pressure injury prevention programs in adult intensive care patients: a systematic review. Int J Nurs Stud. (2020) 102:103483. doi: 10.1016/j.ijnurstu.2019.103483
38. Team V, Team L, Jones A, Teede H, Weller CD. Pressure injury prevention in COVID-19 patients with acute respiratory distress syndrome. Front Med. (2021) 7:558696. doi: 10.3389/fmed.2020.558696
Keywords: COVID-19, pressure injury, rehabilitation coronavirus 2 (SARS-CoV-2), acute rehabilitation humans, quality improvement-outcomes
Citation: Lu W, Bloom O, Rathgeber M and Maltser S (2023) Pressure injury prevalence and characteristics in patients with COVID-19 admitted to acute inpatient rehabilitation unit. Front. Rehabil. Sci. 4:1058982. doi: 10.3389/fresc.2023.1058982
Received: 30 September 2022; Accepted: 1 March 2023;
Published: 3 April 2023.
Edited by:
Marta Imamura, Universidade de Sao, BrazilReviewed by:
Feilong Zhu, Beijing Normal University, ChinaLuigi Vetrugno, University of Studies G. d'Annunzio Chieti and Pescara, Italy
© 2023 Lu, Bloom, Rathgeber and Maltser. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Susan Maltser c21hbHRzZXJAbm9ydGh3ZWxsLmVkdQ==
Specialty Section: This article was submitted to Medical and Surgical Rehabilitation, a section of the journal Frontiers in Rehabilitation Sciences
 Weiying Lu
Weiying Lu Ona Bloom
Ona Bloom Melissa Rathgeber
Melissa Rathgeber Susan Maltser
Susan Maltser