- 1Neurosciences, Rehabilitation, and Vision Strategic Clinical Network, Alberta Health Services, Edmonton, AB, Canada
- 2Division of Physical Medicine and Rehabilitation, University of Alberta, Edmonton, AB, Canada
- 3Faculty of Nursing, University of Alberta, Edmonton, AB, Canada
- 4Community Health Sciences, Cumming School of Medicine, University of Calgary, Calgary, AB, Canada
- 5Spinal Cord Injury Alberta, Edmonton, AB, Canada
Background: Spinal cord injury (SCI) results in long-term functional impairments that significantly impact participation and role in the community. Newly injured persons are often reintroduced to the community with significant deficits in knowledge, including how to access and navigate community resources and supports. This warrants a better understanding of the patient experience of in-hospital care and discharge planning to ensure individuals with SCI are best supported during transitions in care and while living in the community.
Objective: To explore the lived experience of persons with acute SCI and their perceptions of care, focusing on the initial hospital experiences to inpatient rehabilitation.
Methods: A phenomenological research study was conducted using semi-structured interviews. Eligible participants had differing etiologies of SCI (including non-traumatic and traumatic SCI), were over the age of 18 at the time of initial care, and experienced acute hospital and inpatient rehabilitation at an Alberta-based institution within the last 10 years. One-on-one interviews took place between March and June 2021 over telephone or virtual platforms (Zoom). Interview transcripts, and field notes developed the text, which underwent hermeneutic analysis to develop central themes.
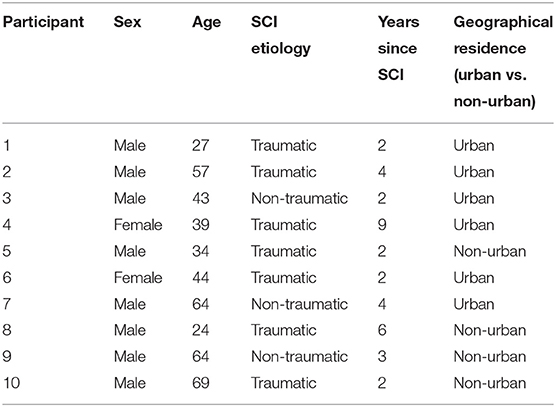
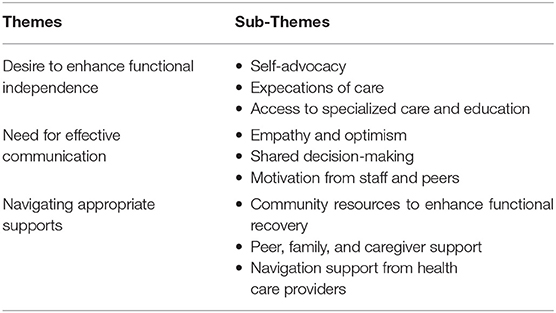
Results: The present study included 10 participants living with an SCI in Alberta, Canada. Most participants (80%) were male. Participants' age ranged from 24 to 69 years. The median years since initial SCI was 3 years. Interviews lasted 45–75 min. Seven participants identified as having a traumatic SCI injury and three identified as having a non-traumatic SCI. The interplay between empowerment and disempowerment emerged as the core theme, permeating participants' meanings and perceptions. Three main themes emerged from the interviews regarding the perceptions of the SCI patient experience. Each theme represents a perception central to their inpatient experience: desire to enhance functional independence to empower confidence and self-management; need for effective communication with healthcare providers to support recovery; and navigating appropriate care supports to enhance preparedness for discharge and returning home.
Conclusion: This study demonstrates the significant need to enhance education of person/family-centered SCI care, foster positive communication between care recipients and care providers, and facilitate better in-hospital access to appropriate navigation and wayfinding supports.
Introduction
Spinal Cord Injury (SCI) is a highly disruptive and debilitating condition that interferes with sensory, motor and autonomic function, and directly impacts physical, psychological, and social wellbeing (1, 2). SCI can arise from trauma (e.g., injuries from falls), or from non-traumatic conditions (e.g., degenerative disease) (2). Recovery from SCI is divided into three main phases of care: acute, inpatient rehabilitation, and longitudinal outpatient care (3). Acute in-hospital care consists of initial post-injury care, while inpatient rehabilitation and longitudinal care delivers post-injury care in both the inpatient and outpatient setting (3). Inpatient rehabilitation for persons with SCI focuses on enhancing physical capacity and performance of activities of daily living to prepare for discharge (4). SCI is a lifelong condition and is often associated with chronic multi-morbidity, including the development of secondary health complications such as urinary tract infections and pressure ulcers (5). SCI has also been shown to impact an individual's mental health, with evidence of increased anxiety, depression, substance abuse, and overall cognitive changes (6).
SCI results in long-term functional impairments that significantly impacts participation and role in the community, such as changes to employment, and living situation (7, 8). Persons with SCI are deemed ready for discharge from hospital after they receive appropriate education on their condition, managing and preventing secondary complications at home, and strategies to participate in activities of daily living based on their neurological level of injury (9). However, newly-injured persons are often reintroduced to the community with significant deficits in knowledge, including how to access and navigate community resources and supports (10). SCI patient education is fundamental to supporting a seamless transition from hospital to community and living with a disability (11). This emphasizes the need to focus on long-term rehabilitation goals, including community re-integration, during the acute and subacute phases of SCI care (12). It also warrants a better understanding of the patient experience of in-hospital care and discharge planning. These insights may better identify the interplay of factors that support transitions from hospital to home (13).
Most studies exploring the patient experience of SCI in-hospital care focus on inpatient rehabilitation (14–16). A meta-synthesis of qualitative evidence concerning the patient experience of rehabilitation following SCI concluded that rehabilitation care services must be informed by the experiences and perspectives of people with SCI to ensure care delivery is appropriate and effective (14). SCI patient experience literature has also addressed participation in decision-making (17–19). These studies found many barriers to collaborative decision-making, including professional paternalism as well as physical, psychological, and environmental factors (17–19). Considering the complexity of the SCI care, a clearer understanding of the lived experience of the healthcare system, specifically acute hospital care and inpatient rehabilitation, following an SCI is essential to informing the delivery of care and appropriate resources to support patient readiness for discharge and reintegration into the community.
Materials and Methods
Design
This study was phenomenological and involved semi-structured interviews. A phenomenological method was used to remain open to participants' narratives and meaning-making while investigating their lived experience, as Phenomenology aims to reveal meaning behind the subjective experiences of individuals and groups (20). The research team used a post-positivism epistemological stance, which acknowledges that the research findings are bound by context, and considers both researcher and theoretical biases in the design and interpretation of the results (21). The COREQ checklist used as a guideline to ensure accurate reporting throughout the manuscript (22).
Sampling
Purposive sampling for maximum variation helped capture diverse experiences of persons living with SCI in Alberta, Canada (i.e., males and females, persons from rural and urban communities, different levels and etiologies of SCI). This study aimed to recruit 8–15 individuals living with an SCI.
Eligibility Criteria
Study inclusion criteria included: individuals over the age of 18 at the time of initial care; and experience of acute in-hospital care and inpatient rehabilitation on neuro-trauma units for their SCI at an Alberta-based institution within the last 10 years. The time limit was set to balance a minimization of recall bias with improved feasibility in recruitment. Participants with different levels and etiology of SCI (including non-traumatic and traumatic SCI) were eligible for participation. Participants were excluded if they were unable to give informed consent by themselves or with assistance from a close relation.
Recruitment
We partnered with a community SCI agency (Spinal Cord Injury (SCI) Alberta) based in Alberta, Canada to support participant recruitment. SCI Alberta offers client support, family and peer supports, as well as community services for persons living with SCI across the province. The provincial reach and contacts associated with SCI Alberta enabled widespread engagement and advertising for recruitment to advance diversity of representation. SCI Alberta recruited eligible participants by advertising the study on their social media page or by directly contacting eligible individuals by phone to share details of the study. If recruited by social media, interested participants directly contacted the research team. For those recruited directly, SCI Alberta obtained verbal consent from interested participants to provide their name and contact information to the research team. The research team then contacted participants by email or phone to review informed consent and organize study participation.
Data Collection
A semi-structured interview guide with open-ended questions was developed based on relevant SCI patient experience literature (23–26), as well as discussions with subject matter experts, including three persons with lived experience of SCI. The interview questions covered the experience of injury and initial care, expectations of care, and other considerations of care including emotional or psychological care, support for family and care providers, role in decision making, and transitions in care. The full interview guide is available (see Supplementary File S1). Interviews were conducted one-on-one by phone or virtual platform (Zoom). Interviews took place between March and June 2021 and were performed by the lead researcher (JAK), a female post-doctoral fellow, experienced in qualitative interview analysis for health services research. The interviewer connected with all participants prior to the interview to explain the purpose of the study, review the consent form, organize the interview, and answer any questions. Fourteen individuals were contacted about the study and 10 were interested in participating. All interviews were audio-recorded, and confidentially transcribed verbatim. All participants were assigned a study ID and any potentially-identifiable details were removed from the transcripts.
Data Analysis
Two researchers independently reviewed all interview transcripts and field notes (JAK, MPG). Qualitative analysis was conducted using NVIVO-12 software (QSR International 2022). To ensure consistency of data analysis, interviews were analyzed according to Dieklemann's 7-step hermeneutic analysis to ensure research validity and credibility (27). A hermeneutic cycle was used to determine a valid and consistent understanding of the participant's experience of the phenomena, and uncover deeper meaning and emerging themes from the text (28, 29). Overall understanding of the lived experience was ensured by co-designing and reviewing the interview guide with three persons with lived experience of SCI as well as employees of SCI Alberta. Interview transcripts and field notes enabled in-depth description of data. Field notes were written to supplement the data and captured the interviewer's initial impressions and participant non-verbal cutes (when participants had their video turned on). Two transcripts were independently coded by four authors (JAK, MPG, KPM, EP) into meaning-bearing units (codes) related to the study objectives. Any disagreements on interpretation were resolved by revisiting the original interview transcripts. The codes were compared and discussed until agreement was achieved by all researchers. This subset analysis built a set of defined codes that were applied to subsequent interviews. The codes generated were refined and expanded as additional interviews were analyzed. The process of interviewing and analysis was iterative. The connections between the identified themes were examined to explore relationships or causality, and to gain a more in-depth understanding of the participant's experience. All members of the research team reviewed the draft themes and exemplar quotes prior to subsequent analysis of interpretation.
Ethical Considerations
This study was approved by the University of Alberta Research Ethics Board (Pro00105843). All participants were informed about the study and consented to participating prior to the interview.
Results
Characteristics of Study Participants
The study interviewed 10 participants living with an SCI in Alberta, Canada between March and June 2021. Interviews lasted 45–75 min. Participants were recruited until richness and data saturation were achieved, whereby additional interviews brought no additional insights to the primary research question (30), and data saturation was determined by the interviewer and confirmed by a second researcher (MPG) involved in transcript analysis. Participant demographics (age, sex, level of injury, years since SCI, and hospital facility visited) were self-reported during the interview. Characteristics of study participants are reported in Table 1. The majority of participants (80%) were male. Participants' age ranged from 24 to 69 years. The median years since initial SCI was 3 years (range 2–9 years). All participants were interviewed after discharge from hospital or inpatient rehabilitation. During their initial care experience, six participants were living in urban regions and four were living in rural regions of the province. There were seven participants that self-reported a traumatic SCI injury and three that self-reported a non-traumatic SCI. Participants discussed care experiences from two acute hospitals and two inpatient rehabilitation care sites across Alberta. There were three participants that received initial acute care outside of the province prior to admission to an Albertan inpatient rehabilitation facility. Thematic coding led to the development of a conceptual representation of the in-hospital care experiences for persons with SCI in Alberta (Figure 1, Table 2).
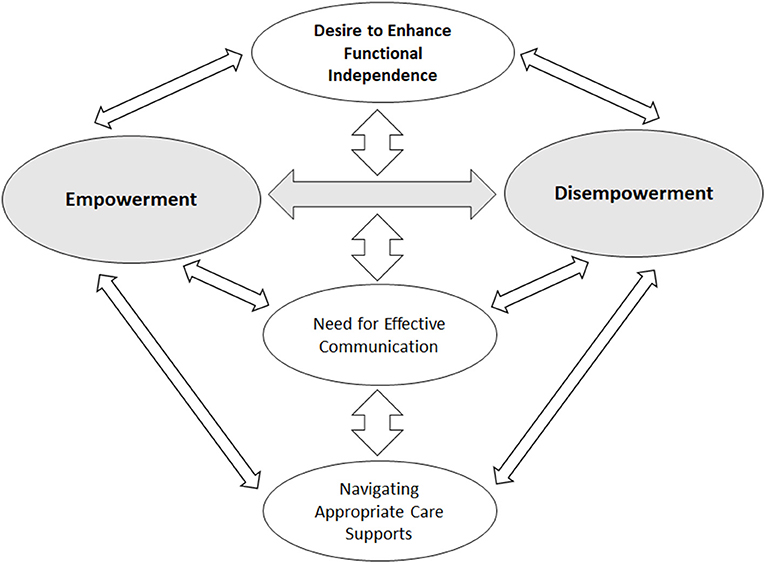
Figure 1. Thematic framework underlying the experience of persons with SCI regarding in-hospital care.
In-hospital Care Experiences of Persons With SCI
The interplay between empowerment and disempowerment emerged as the core theme, permeating participants' meanings and perceptions. Participants felt the need to be self-empowered for recovery amidst conditions that often deprived them of control over their situation. Three main themes emerged from the patient experience: (1) desire to enhance functional independence; (2) need for effective communication; (3) navigating appropriate care supports. Each theme represents a perception central to their inpatient experience across three sub-themes (Table 2).
These themes are discussed in further detail below. Additional exemplar quotes are provided in Table 3.
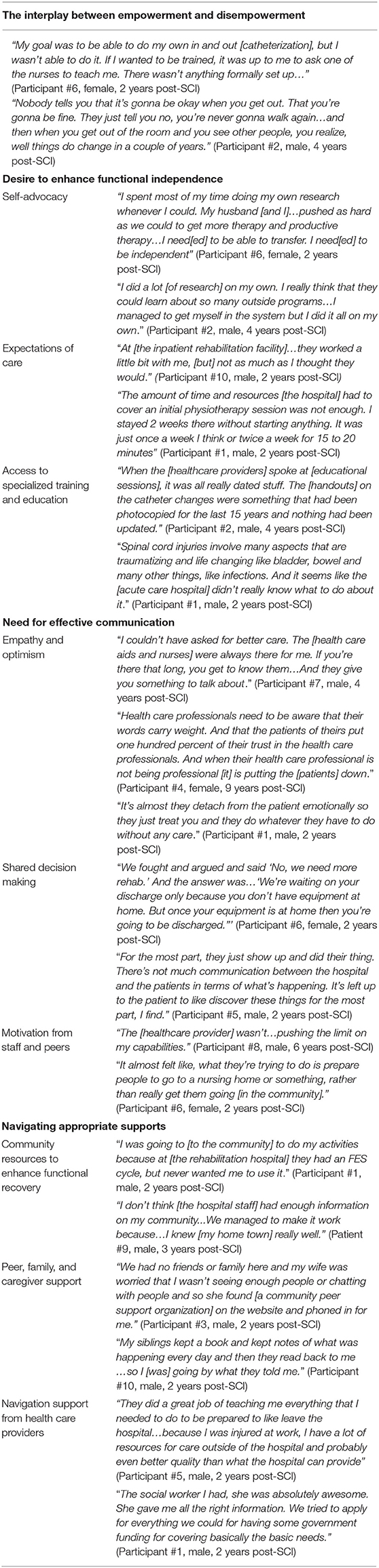
Core Theme: Interplay Between Empowerment and Disempowerment
A core theme underscoring the SCI perception of acute and inpatient rehabilitation was the interplay between generating empowerment from themselves, staff, peers, and family to enhance their functional recovery and the perceived disempowerment from the healthcare system to achieve this goal.
Disillusionment with the healthcare system, and obstacles to their rehabilitation created a tension between the need for empowerment in their rehabilitation journey, and an often disempowering milieu of care. Throughout their care experience, participants were generally motivated to enhance their overall functional independence, and gain as much knowledge as possible to best support themselves in the community following discharge. Their inherent motivation and trust in the healthcare system was often discouraged by a perceived lack of SCI education during acute hospital care and was accompanied by apparent demotivating personnel and limited personalized care plans during inpatient rehabilitation.
“There is a lot of encouragement that needs to happen [during recovery]. It's understandable that you need to help people accept their injury. But to basically shut down any kind of hope - that is the worst thing…Trying isn't going to hurt us. We're going to fall and get up as many times as it takes.” (Participant #6, female, 2 years post-SCI)
In our participants, the tension between the need to be empowered and barriers to empowerment appeared to fuel their motivation to maximize their outcomes regardless of obstacles. This was realized through active agency in discovering and utilizing diverse resources in the community, peer-groups, SCI societies and rehabilitation centers with the help of their families. Ultimately, participants discovered a path to empowerment through claiming agency of their rehabilitation and recovery.
“When I was in the [inpatient rehabilitation facility], there was nobody there to tell you about [community] programs and funding…That is really a shame because we find out about it all on our own after the fact. I believe [the health care providers] should be handing out information like that to help people realize that when you get out, there are supports for you.” (Participant #2, male, 4 years post-SCI)
Desire to Enhance Functional Independence
All participants expressed a desire to increase their knowledge of SCI and rehabilitation strategies to enhance their overall independence and preparedness for discharge. Participants were motivated to obtain the necessary skills to increase their functional capacity and independence over time. Many participants expressed a strong desire to learn care practices that better enabled them to manage their own care. Some participants felt that they had to be assertive or go out of their way to receive appropriate information and resources to support their recovery. This was especially noted during the acute, in-hopsital phase of care.
“I researched it all on my own...I was very fit before…I knew that I had to get my movement back. I have to move my body to maintain whatever muscle mass I had and I knew I had to do it right to get it back.” (Participant #4, female, 9 years post-SCI)
Unmet expectations of care was often discussed during the inpatient rehabilitation phase of care and represented a common negative experience and barrier toward participant goal attainment. Participants generally expected greater access to one-on-one physical-therapy prior to admission to inpatient rehabilitation. They felt that the care received during their stay in inpatient rehabilitation was not enough to enhance their overall functioning and preparedness for discharge.
“I was expecting when I went to the [Inpatient Rehabilitation Facility] that it was going to be full on rehabilitation. But when I got there I…was scheduled for 1 h of physiotherapy, 1 h for occupational therapy, and then…the rest of the time you're basically in your bed.” (Participant #2, male, 4 years post-SCI)
There were mixed feelings on the specialized training and types of rehabilitation programs offered in the inpatient rehabilitation setting. While some participants found benefit from the standardized rehabilitation programs, many felt that more personalized, patient-centered rehabilitation opportunities would offer greater benefits.
“Probably for a lot of people [the rehabilitation program] was helpful…but for me it was waste of time. I didn't find it helpful for me and that was very frustrating.” (Participant #7, male, 4 years post-SCI)
When describing their experiences of acute, in-hospital care, participants often cited a lack of provider competencies in specialized SCI care, knowledge of local resources and supports, as well as differing care practices between hospital units. This perceived knowledge gap reduced participant's overall confidence in their care providers, and for some, resulted in insufficient training to support self-management following discharge.
“The techniques they were teaching, like transferring yourself in and out of the wheelchair…weren't how they do them at the [other hospital]. You are receiving mixed information in the transition [from the] hospital setting to a rehabilitation hospital” (Participant #5, male, 2 years post-SCI)
Need for Effective Communication
Communication with care providers, both positive and negative, influenced participants' motivation to participate in rehabilitation and their perceived readiness for discharge. Poor communication with care providers was identified as a negative experience by most participants. Many described a general lack of empathy and optimism from acute hospital care providers when discussing their prognosis, with some citing that certain providers were discouraging or demotivating of their aspirations for rehabilitation.
“[The staff] always tried to turn down the will I had and the energy I was putting toward rehab, to the point that I had to push against their negativity.” (Participant #1, male, 2 years post-SCI)
Several participants described feeling excluded from decisions regarding their care and perceived this as a barrier to receiving appropriate care and feeling ready for discharge. Participants also described that certain healthcare providers at inpatient rehabilitation facilities were not motivating or challenging them enough to progress to their desired level of functional independence.
“They have a team of professionals that make all the decisions for you. But…you're not a part of that conversation. Everything is done for you, not with you” (Participant #4, female, 9 years post-SCI)
Many participants described building relationships with healthcare staff as a positive experience while in inpatient rehabilitation. These relationships were often described by examples of empathetic communication and encouragement from healthcare providers, which overall built trust and enhanced participant's motivation for rehabilitation and preparation for discharge.
“The people at the [Inpatient Rehabilitation Facility] said that I was one of the hardest workers that they ever had. [That] made me feel good and just kept me in the right frame of mind…to do the things that I used to be able to do...” (Participant #3, male, 2 years post-SCI)
Navigating Appropriate Care Supports
Navigating or learning about and accessing appropriate rehabilitation and recovery supports, including information on community resources and financial supports, were identified as a facilitator of positive patient experience. Many participants learned of, and visited, community facilities during their hospital stay as a means to access additional rehabilitation or related resources to support their recovery. Participants often learned of these programs by themselves, a social worker, or through family and peer support persons.
“I started going to this [community] rehabilitation center and there, I really improved my function, because they made me stand, and taught me how to [manage] my spasms” (Participant #1, male, 2 years post-SCI)
Family and caregiver support was an important source of way-finding for participants. A family member was usually present in the hospital throughout the patient care journey. The family member would often keep track of the participant's procedures and treatments. They would search for community resources and supports to help better prepare their loved one for discharge and return home.
Thankfully, since my mom was involved with health care as a career she knew what was expected and the majority of the resources…I feel like if I didn't have [a] mom with a health care background, it would have been a completely different situation. (Participant #8, male, 6 years post-SCI)
Peer support volunteers were helpful at answering participant questions, setting expectations, educating about SCI care and self-management, as well as identifying local community resources and supports throughout the patient care journey.
“[The peer support volunteer] came in once a month…She was [a] really good person to talk to if you took advantage of her knowledge… they offered a support system for questions for home care and stuff like that.” (Participant #7, male, 4 years post-SCI)
Participants noted that communication with social workers and occupational therapists was helpful for resource finding, setting up financial supports, as well as preparing for discharge and return to home.
“The social worker was great…I once [asked], ‘just come in and talk to me', because I was struggling for a while with minor depression, but they were good. They meant to get [me] back in the community, communicating with various government [agencies] and they were excellent and telling me what was there.” (Participant #9, male, 3 years post-SCI)
Discussion
This study highlights experiences of persons living with SCI during the acute hospital care and inpatient rehabilitation, from which we can derive recommendations to improve quality of care to best support persons during transitions in care and return to community. The experience of in-hospital care for persons with SCI underlines the need for empowerment to support recovery, return to home, and community re-integration. Our findings highlight a significant need to enhance education of person/family-centered SCI care; foster positive communication between care recipients and healthcare providers; and facilitate better in-hospital access to appropriate community supports. The identified themes have direct implications on aspects of community re-integration, and showcase the impact of the patient experience on this essential phase of care.
Desire to Enhance Functional Independence
This study revealed that, during their initial hospital visit, persons with SCI have significant motivation to enhance their functional capacity to become as independent as possible. Participants had a strong desire to participate in their own care planning and self-management, but often felt they had insufficient information on their condition early in their care experience and needed to advocate for their own information or resources. A previous study on 214 patients with traumatic and non-traumatic SCI reported that, at the time of discharge, only 47% of patients reported good knowledge about SCI self-care, while 22% reported poor knowledge (31). Persons living with SCI have a high risk of secondary complications over the first year of discharge (32). A study by May and colleagues found that SCI patients who experienced care at an inpatient rehabilitation facility consistently rated bladder, bowel, and skin care as topics on which they frequently sought information (33). Early and frequent in-hospital patient self-management education and symptom monitoring may enable persons with SCI to better manage their health following discharge and prevent unnecessary secondary medical complications.
Relationships with peers, family and staff influenced the participant's motivation toward rehabilitation and recovery. Participants felt frustrated by the perceived discouraging demeanor of some staff, or not feeling sufficiently challenged during structured rehabilitation programs. Conversely, building relationships over time with staff created a positive dynamic that encouraged participation in their recovery. These findings align with a qualitative meta-analysis from 2007, which identified that the SCI patient experience of rehabilitation was largely influenced by the qualities of the staff at enhancing patient self-esteem (14).
Study participants often perceived limited provider knowledge of SCI in the acute care setting as well as inconsistencies in SCI care practices between hospitals. Some participants noted significant differences in care practices related to bladder and skin care, which often left them unsure of best practices and how to manage their own care at home. The low prevalence of SCI can challenge non-specialist care providers within and outside the hospital setting on staying up-to-date on current best practices (34). Opportunities to enhance care provider knowledge could include continuing education, mentoring, updated best practice guidelines, and enhanced communication between specialist and non-specialist care providers (34).
The complexity and diversity of SCI treatment and management strategies warrants the need for multidisciplinary collaboration and coordination to ensure providers have the resources and tools to consistently support patient care. One study used a step-wise multidisciplinary team approach in the acute care setting for traumatic SCI to implement a dedicated SCI service. This service involved bi-weekly SCI sessions that included: collaboration of surgical specialists and allied health care professionals; developing and implementing SCI bundle order sets to promote standardization of care, coordination of surgical services; patient and family education; and promoting social lifestyle changes at discharge (35). These type of approaches may enhance continuity of care and standardized care practices for patients across diverse care settings. Implementing SCI standards of care provides an opportunity to re-design in-hospital SCI care provision, reduce unnecessary complications following discharge, improve the patient experience, and address health issues that lead to frequent re-hospitalization (36, 37). However, identifying optimal management strategies for SCI is challenging (38). There is limited rehabilitation research, inconsistent outcome measures, and heterogeneous populations to support SCI best practice standards (1). Furthermore SCI rehabilitation is complex, often involving multiple treatments by multiple care providers and input from the patient and their care providers. Patient participation in rehabilitation is considered a cornerstone of SCI care and is strongly encouraged to promote patient involvement in care planning and decision-making (19). Developing and implementing standardized outcome measures of SCI care that are both evidence-informed and patient-centered can enable health systems to continuously learn from patients and providers to update practice, while enabling comparisons across sites for quality improvement (39). A 2013 publication from the Institute of Medicine recommended healthcare systems adopt a continuous learning health system to support the development of standardized clinical processes and team-based care (40). Learning health systems use measurement to inform practice and practice to inform evidence and quality improvement of care (40). In Canada, the Rick Hansen Spinal Cord Injury Registry collects SCI patient data during the in-hospital phase of care as well as through community follow-up for years following injury (41). These types of registries can enable researchers to investigate the relationship between indicators of SCI inpatient care, patient outcome measures, and long-term patient outcomes to identify areas of health system improvement.
Need for Effective Communication
Poor communication with healthcare providers emerged as a significant negative experience among individuals with SCI. These negative experiences are addressed within the Canadian Patient's Bill of Rights, including receiving appropriate and timely care, being treated with dignity and respect, and receiving information relating to proposed treatment and options (42). Participants felt some providers lacked empathy toward their condition, and noted situations where they felt they were not treated appropriately; did not receive timely information about their care; and were not included in their care decision making. Many of these negative interactions were found to reduce overall trust in the providers and was perceived to hinder their ability to achieve their desired rehabilitation outcomes. This aligns with findings from a qualitative study on the meaning, process, and consequences of care during SCI rehabilitation, which found that patients who perceived care providers as non-caring felt more hindered to successfully attain their desired rehabilitation outcomes (15). In the present study, many participants expressed that some care providers, particularly during the acute care phase, were unsympathetic of their condition and generally de-motivating when discussing their prognosis and recovery trajectory.
A common theme among participants was unmet expectations of inpatient rehabilitation. This finding is similar to results by Garrino et al. who found that patients with SCI expected greater treatment and rehabilitation care and less time in a clinical or medical setting compared to an acute care hospital (43). Patient expectations can refer to many areas including general expectations about health care provision, health care provider's interpersonal and clinical skills, or receiving information about their care (44). In general, patient needs for support and information are found to be more valued than technical interventions from the patient perspective (44, 45). Our findings demonstrate that, prior to transition to inpatient rehabilitation, patients may benefit from education about what to expect during their stay in inpatient rehabilitation, as well as clear discussions on patient and provider expectations of care. This may also apply to providing appropriate education to patients to prepare for discharge, return to home, and community re-integration.
Navigating Appropriate Care Supports
Navigating care supports, including identifying and accessing government funding opportunities, as well as peer and community resources, were useful in supporting participants throughout their care journey, especially during discharge and transition to home or assisted living facility. A contributing factor to quality life following an acquired disability is making connections with others, often through participation in the community (46). A qualitative study of persons with SCI identified strong social supports as an important facilitator for participation and connection with community (46). They recommend family and close friends be involved in the SCI rehabilitation process, and be engaged in the facilitation of social and community activities as early as possible (14, 46). This finding was also observed in the present study, where most participants had a family member support their transition home and way finding of community resources and supports.
The importance of peer support workers has been recommended to model a positive future for persons that recently acquired an SCI (46–48). In the present study, several participants recommended peer-support volunteers. These volunteers provided in-hospital education and community supports for persons with SCI. Many participants appreciated peer support as providing information on community resources and modeled positive life experiences outside of the hospital. However, study participants that received SCI care during the COVID-19 pandemic noted limited or no access to in-hospital peer support due to public health restrictions. This was troublesome for participants of older age that struggled to connect with peers through virtual means on their own. Although this was not the primary aim of this study, this warrants a need for alternative strategies to provide in-hospital peer support. Advances in virtual health can provide opportunities to connect with patients in-hospital during restrictions such as COVID-19 (49). Emerging technologies have been proposed to support the facilitation of virtual peer support in rehabilitation care settings (50). This can include webinars, video phone calls, chatbots, and virtual reality programs, which could enable virtual peer support or contact with family and friends. They can also be used to deliver emotional support to enhance patient motivation (51). Peer support, whether in-person or virtual, should be embedded in patient care plans as early as acute care to best support preparedness for discharge and transition to community.
Strengths and Limitations
This study explored in-depth the experience of persons with SCI regarding in-hospital care from acute care to inpatient rehabilitation. Key strengths of the methodology include the diversity of participants, in-depth interviews, and two independent coders for all transcripts, which strengthens the rigor of our findings and supports ensure transferability. A notable limitation is the eligibility criteria for participation. Participants were eligible up to 10 years post-injury, which may result in recall bias since their initial hospital experience. Additionally, most participants were biologically male, which may limit the interpretations of the findings to the female experience. Of the ten participants, three received initial care outside of the province, which may influence their overall perceptions of care. Due to restrictions of the COVID-19 pandemic, all interviews were conducted over virtual platforms or telephone, which may reduce participant accessibility to participate, and comfort with the interviewer.
Conclusion
The experience of initial hospital care for persons with SCI is complex and has many barriers. Self-empowerment, motivation from staff, appropriate informational needs, peer and family support, and resource way finding can help better support patients to overcome these barriers and may enhance quality of life post-discharge. These findings can inform recommendations to better incorporate community supports and discharge planning to enhance rehabilitation stay and improve the transition to back to community.
Data Availability Statement
The dataset includes transcripts with identifiable patient data. Representative quotes can be found in Table 3 of the manuscript. Requests to access the datasets should be directed to amFjcXVlbGluZS5rcnlzYUBhbGJlcnRhaGVhbHRoc2VydmljZXMuY2E=.
Ethics Statement
This study involved human participants and was reviewed and approved by University of Alberta Research Ethics Board. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
JK, KP, EP, and CH led the conception and design of the study. JK performed the interviews and wrote the manuscript. MG transcribed all interviews. JK and MG extracted and analyzed transcripts for emerging themes. KP, CH, EP, and RM reviewed and edited the manuscript for clarity. All authors have contributed to the manuscript in accordance with the criteria for authorship.
Funding
JK was funded through the Alberta Paraplegic Foundation. CH is a Canadian Institutes for Health Research Principal Investigator. MG was funded through the Faculty of Nursing Studentship from the University of Alberta.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to thank all the participants that volunteered their time to participate in this study. We would also like to acknowledge Ms. Glenda Moore and Ms. Carol Kuzio of the Neurosciences, Rehabilitation and Vision Strategic Clinical Network who led the work supporting this project. We further thank the employees from SCI Alberta for their input on study design and recruitment support.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fresc.2022.904716/full#supplementary-material
References
1. Fehlings MG, Tetreault LA, Wilson JR, Kwon BK, Burns AS, Martin AR, et al. A clinical practice guideline for the management of acute spinal cord injury: introduction, rationale, and scope. Global Spine Journal. (2017) 7:84S−94S doi: 10.1177/2192568217703387
2. PRAXIS Spinal Cord Institute. A look at traumatic spinal cord injury in Canada: Rick Hansen Spinal Cord Registry (RHSCIR) J Spinal Cord Med. (2017) 40:870. doi: 10.1080/10790268.2017.1387124
3. Burns A, Marino RJ, Kalsi-Ryan S, Middleton JW, Tetreault LA, Dettori JR, et al. Type and timing of rehabilitation following acute and subacute spinal cord injury: a systematic review. Glob spine J. (2017) 7:175S−194S. doi: 10.1177/2192568217703084
4. Haisma J, Bussmann J, Stam H, Sluis T, Bergen M, Dallmeijer A, et al. Changes in physical capacity during and after inpatient rehabilitation in subjects with a spinal cord injury. Arch Phys Med Rehabil. (2006) 87:741–8. doi: 10.1016/j.apmr.2006.02.032
5. Guilcher SJT, Craven BC, Lemieux-Charles L, Casciaro T, McColl MA, Jaglal SB. Secondary health conditions and spinal cord injury: an uphill battle in the journey of care. Disabil Rehabil. (2013) 35:894–906. doi: 10.3109/09638288.2012.721048
6. Stricsek G, Ghobrial G, Wilson J, Theofanis T, Harrop JS. Complications in the Management of Patients with Spine Trauma. Neurosurg Clin N Am. (2017) 28:147–55. doi: 10.1016/j.nec.2016.08.007
7. Middleton JW, Simpson GK, De Wolf A, Quirk R, Descallar J, Cameron ID. Psychological distress, quality of life, and burden in caregivers during community reintegration after spinal cord injury. Arch Phys Med Rehabil. (2014) 95:1312–9. doi: 10.1016/j.apmr.2014.03.017
8. Lidal IB, Huynh TK, Biering-Sørensen F. Return to work following spinal cord injury: a review. Disabil Rehabil. (2007) 29:1341–75. doi: 10.1080/09638280701320839
9. Hassan Soelaylah Am Visagie S, Mji G. The achievement of community integration and productive activity outcomes by CVA survivors in the Western Cape Metro Health District. S Afr J Occup Ther. (2012) 42:11–6.
10. Boschen KA, Tonack M, Gargaro J. Long-term adjustment and community reintegration following spinal cord injury. Int J Rehabil Res. (2003) 26:157–64. doi: 10.1097/01.mrr.0000088440.78481.1f
11. Potter PJ, Wolfe DL, Burkell JA, Hayes KC. Challenges in educating individuals with SCI to reduce secondary conditions. Top Spinal Cord Inj Rehabil. (2004) 10. doi: 10.1310/WP5P-CNHM-NC6T-DL7P
12. Moreno A, Zidarov D, Raju C, Boruff J, Ahmed S. Integrating the Perspectives of Individuals With Spinal Cord Injuries, Their Family Caregivers and Healthcare Professionals from the Time of Rehabilitation Admission to Community Reintegration: Protocol for a Scoping Study on SCI Needs. Available online at: http://bmjopen.bmj.com/
13. Kroll T. Rehabilitative needs of individuals with spinal cord injury resulting from gun violence: the perspective of nursing and rehabilitation professionals. Appl Nurs Res. (2008) 21:45–9. doi: 10.1016/j.apnr.2006.06.001
14. Hammell W. Review experience of rehabilitation following spinal cord injury: a meta-synthesis of qualitative findings. Spinal Cord. (2007) 45:260–74. doi: 10.1038/sj.sc.3102034
15. Lucke K. Knowledge acquisition and decision-making: spinal cord injured individuals perceptions of caring during rehabilitation. Sci Nurs. (1997) 14:87–95.
16. May L, Day R, Warren S. Perceptions of patient education in spinal cord injury rehabilitation. Disabil Rehabil. 28:1041–9 doi: 10.1080/09638280500494744
17. Pellatt G. Patient-professional partnership in spinal cord injury rehabilitation. Br J Nurs. (2004) 13:948–53. doi: 10.12968/bjon.2004.13.16.15966
18. Scheel-Sailer A, Post MW P, Michel F, Weidmann-Hügle T, Baumann Hölzle R. Patients' views on their decision making during inpatient rehabilitation after newly acquired spinal cord injury-A qualitative interview-based study. Health Exp. (2017) 20:1133–42. doi: 10.1111/hex.12559
19. Lindberg J, Kreuter M, Taft C, Person L. Patient participation in care and rehabilitation from the perspective of patients with spinal cord injury. Spinal Cord. (2013) 51:834–7. doi: 10.1038/sc.2013.97
20. Speziale HJS, Carpenter DR. Qualitative Research in Nursing: Advancing the Humanistic Imperative. 4th ed. Philadelphia: Lippincott Williams & Wilkins. (2007).
21. Clark AM. The qualitative-quantitative debate: moving from positivism and confrontation to post-positivism and reconciliation CLARK A. J Advanced Nurs. (1998) 27. doi: 10.1046/j.1365-2648.1998.00651.x
22. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Heal Care. (2007) 19:349–57. doi: 10.1093/intqhc/mzm042
23. Trezzini B, Brach M, Post M, Gemperli A. Prevalence of and factors associated with expressed and unmet service needs reported by persons with spinal cord injury living in the community. Spinal Cord. (2019) 57:490–500. doi: 10.1038/s41393-019-0243-y
24. Mahooti F, Raheb G, Alipour F, Hatamizadeh N. Psychosocial challenges of social reintegration for people with spinal cord injury: a qualitative study. Spinal Cord. (2020) 58:1119–27. doi: 10.1038/s41393-020-0449-z
25. Ronca E, Scheel-Sailer A, Koch HG, Essig S, Brach M, Münzel N, et al. Satisfaction with access and quality of healthcare services for people with spinal cord injury living in the community. J Spinal Cord Med. (2020) 43:111–21. doi: 10.1080/10790268.2018.1486623
26. Goodridge D, Rogers M, Klassen L, Jeffery B, Knox K, Rohatinsky N, et al. Access to health and support services: perspectives of people living with a long-term traumatic spinal cord injury in rural and urban areas. Disabil Rehabil. (2015) 37:1401–10. doi: 10.3109/09638288.2014.972593
27. Diekelmann NL, Allen D, Tanner CA, National League for Nursing. Council of Baccalaureate and Higher Degree Programs. The NLN Criteria for Appraisal of Baccalaureate Programs : A Critical Hermeneutic Analysis. New York, NY: National League for Nursing (1989) p. 70.
28. Tan H, Grief M, Couns PC, Wilson A, Olver I. Ricoeur's theory of interpretation: An Instrument for Data Interpretation in Hermeneutic Phenomenology. Int J Qual Methods. (2009) 8:1–15. doi: 10.1177/160940690900800401
29. Lohne V. The battle between hoping and suffering: A conceptual model of hope within a context of spinal cord injury. Adv Nurs Sci. (2008) 31:237–48. doi: 10.1097/01.ANS.0000334287.19473.5c
30. Mack N, Woodsong C, MacQueen KM, Guest G, Namey E. Qualitative research methods: A data collector's field guide. In: Family Health International. North Carolina: FLI (2005).
31. Thietje R, Giese R, Pouw M, Kaphengst C, Hosman A, Kienast B, et al. How does knowledge about spinal cord injury-related complications develop in subjects with spinal cord injury? A descriptive analysis in 214 patients. Spinal Cord. (2011) 49:43–8. doi: 10.1038/sc.2010.96
32. Stillman MD, Barber J, Burns S, Williams S, Hoffman JM. Complications of spinal cord injury over the first year after discharge from inpatient rehabilitation. Arch Phys Med Rehabil. (2017) 98:1800–5. doi: 10.1016/j.apmr.2016.12.011
33. May DL, Day R, Warren S. v. Evaluation of patient education in spinal cord injury rehabilitation: Knowledge, problem-solving and perceived importance. Disabil Rehabil. (2009) 28:405–13. doi: 10.1080/09638280500192439
34. Milligan J, Lee J, Smith M, Donaldson L, Athanasopoulos P, Bassett-Spiers K, et al. Advancing primary and community care for persons with spinal cord injury: Key findings from a Canadian summit. J Spinal Cord Med. 43:223–33. doi: 10.1080/10790268.2018.1552643
35. Alizo G, Sciarretta JD, Gibson S, Muertos K, Holmes S, Denittis F, et al. Multidisciplinary team approach to traumatic spinal cord injuries: a single institution's quality improvement project. Eur J Trauma Emerg Surg. (2018) 44:245–50. doi: 10.1007/s00068-017-0776-8
36. DeJong G, Groah SL. Advancing SCI health care to avert rehospitalization. J Spinal Cord Med. (2015) 38:696. doi: 10.1080/10790268.2015.1101917
37. DeJong G, Tian W, Hsieh C, Junn C, Karam C, Ballard P, et al. Rehospitalization in the first year of traumatic spinal cord injury after discharge from medical rehabilitation. Arch Phys Med Rehabil. (2013) 94. doi: 10.1016/j.apmr.2012.10.037
38. Burns AS, Yee J, Flett HM, Guy K, Cournoyea N. Impact of benchmarking and clinical decision making tools on rehabilitation length of stay following spinal cord injury. Spinal Cord. (2013) 51:165–9. doi: 10.1038/sc.2012.91
39. Craven BC, Alavinia SM, Wiest MJ, Farahani F, Hitzig SL, Flett H, et al. Methods for development of structure, process and outcome indicators for prioritized spinal cord injury rehabilitation Domains: SCI-High Project. J Spinal Cord Med. (2019) 42:51–67. doi: 10.1080/10790268.2019.1647386
40. Smith M, Saunders R, Stuckhardt L, McGinnis JM, America America C on the LHCS in Medicine I of.. A Continuously Learning Health Care System. (2013) Available online at: https://www.ncbi.nlm.nih.gov/books/NBK207218/ (accessed February 23, 2022).
41. Noonan VK, Kwon BK, Soril L, Fehlings MG, Hurlbert RJ, Townson A, et al. The Rick Hansen Spinal Cord Injury Registry (RHSCIR): a national patient-registry. Spinal Cord. (2012) 50:22–7. doi: 10.1038/sc.2011.109
42. Smith M. Patient's Bill of Rights - A Comparative Overview. (2002). Available online at: https://publications.gc.ca/Collection-R/LoPBdP/BP/prb0131-e.htm (accessed December 12, 2021).
43. Garrino L, Curto N, Decorte R, Felisi N, Matta E, Gregorino S, et al. Towards personalized care for persons with spinal cord injury: a study on patients' perceptions. J Spinal Cord Med. 34:67–75. doi: 10.1179/107902610x12883422813741
44. Berhane A, Enquselassie F. Patient expectations and their satisfaction in the context of public hospitals. Patient Prefer Adherence. (2016) 10:1919. doi: 10.2147/PPA.S109982
45. Ruiz-Moral R, Pérula de Torres L, Jaramillo-Martin I. The effect of patients' met expectations on consultation outcomes. A study with family medicine residents. J Gen Intern Med. (2007) 22:86–91. doi: 10.1007/s11606-007-0113-8
46. Barclay L, McDonald R, Lentin P, Bourke-Taylor H. Facilitators and barriers to social and community participation following spinal cord injury. Aust Occup Ther J. (2016) 63:19–28. doi: 10.1111/1440-1630.12241
47. Price P, Stephenson S, Krantz L, Ward K. Beyond my front door: the occupational and social participation of adults with spinal cord injury. OTJR Occupation Participation and Health. (2010) 30:81–88. doi: 10.3928/15394492-20100521-01
48. Unger J, Singh H, Mansfield A, Hitzig SL, Lenton E, Musselman KE. The experiences of physical rehabilitation in individuals with spinal cord injuries: a qualitative thematic synthesis. Disabil Rehabil. (2019) 41:1367–83. doi: 10.1080/09638288.2018.1425745
49. Lambercy O, Lehner R, Chua K, Wee SK, Rajeswaran DK, Kuah CWK, et al. Neurorehabilitation from a distance: can intelligent technology support decentralized access to quality therapy? Front Robot AI. (2021) 0:126. doi: 10.3389/frobt.2021.612415
50. Brennan DM, Mawson S, Brownsell S. Telerehabilitation: enabling the remote delivery of healthcare, rehabilitation, and self management. Stud Health Technol Inform. (2009) 145:231–48. doi: 10.3233/978-1-60750-018-6-231
Keywords: Spinal Cord Injury (SCI), patient experience, rehabilitation, acute care, inpatient rehabilitation
Citation: Krysa JA, Gregorio MP, Pohar Manhas K, MacIsaac R, Papathanassoglou E and Ho CH (2022) Empowerment, Communication, and Navigating Care: The Experience of Persons With Spinal Cord Injury From Acute Hospitalization to Inpatient Rehabilitation. Front. Rehabilit. Sci. 3:904716. doi: 10.3389/fresc.2022.904716
Received: 25 March 2022; Accepted: 19 April 2022;
Published: 31 May 2022.
Edited by:
Christina Papadimitriou, Oakland University, United StatesCopyright © 2022 Krysa, Gregorio, Pohar Manhas, MacIsaac, Papathanassoglou and Ho. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chester H. Ho, Q2hlc3Rlci5Ib0BhbGJlcnRhaGVhbHRoc2VydmljZXMuY2E=
 Jacqueline A. Krysa
Jacqueline A. Krysa Marianne Pearl Gregorio
Marianne Pearl Gregorio Kiran Pohar Manhas1,4
Kiran Pohar Manhas1,4 Elizabeth Papathanassoglou
Elizabeth Papathanassoglou Chester H. Ho
Chester H. Ho