- 1School of Health Sciences, Örebro University, Örebro, Sweden
- 2Center for Adult Rehabilitation, Faculty of Medicine and Health, Örebro University, Örebro, Sweden
Persons with neurological diseases often have some degree of cognitive impairment. They are in need of assistive technology for cognition (ATC) to compensate for cognitive impairments that affect their daily functioning. Goal setting in relation to cognitive deficits using ATC are common in clinical practice, and therapists often set several rehabilitation goals together with a patient. However, these rehabilitation goals are usually phrased differently, which limit the comparison of ATC and rehabilitation goals. It is thus valuable to link the goals to some standardized terminologies, such as the International Classification of Functioning, Disability and Health (ICF). Furthermore, goal achievement is seldom used to evaluate long-term effects of ATC in persons with neurological diseases and limited attention has been paid to the factors that predict goal achievement in using the ATC as cognitive support in persons with neurological diseases. The aim of the project is 3-fold. Firstly, we will use the ICF to link rehabilitation goals regarding the use of ATC in adults with neurological diseases. Secondly, we will evaluate effects of the ATC using goal achievement over a 5-year period. Thirdly, we will explore the variables that predict goal achievement in relation to the effects of ATC.
Introduction
Neurological diseases are diseases of the central and peripheral nervous systems that negatively affect cognition, independence, and daily functioning. They are one of the leading causes of disability and unfortunately, advances in prevention and management of major neurological disorders are not sufficiently effective to encounter global burden of neurological diseases (1). Persons with neurological diseases often have some degree of cognitive impairment, which include attention deficits, visual perception deficits, sensory processing deficits, slow processing speeds, short-/long- term memory difficulties, and executive dysfunctioning (2, 3). They are often in need of assistive technology for cognition (ATC) to compensate for cognitive impairments that affect their daily functioning.
ATC are technologies designed to compensate for cognitive impairments as we mentioned earlier. Most of the ATC available in the commercial market are designed for the areas of time/day orientation, organization of daily activities and management of daily routine. Common examples of ATC are visual and audio reminders to perform a given task at a particular time, electronic clocks that visualize the time in different colors or modes (analog or digital), electronic calendars that visualize days and weeks and electronic planners that visualize activities during the day and week (4, 5). The goals of ATC are to compensate for cognitive impairments, increase independence and reduce the need for personal assistance (6, 7). ATC can thus be seen as cognitive support for “someone” (a person with cognitive impairment) doing something (an activity) somewhere (in a particular environment) (4). A number of reviews have reported the benefits of ATC in adults with neurological diseases (5–8). The main findings were that ATC effectively provides support for cognitive functions relating to attention, calculation, emotion, experience of self, higher level cognitive functions (planning and time management) and memory. Smartphones, personal digital assistants (PDAs), etc. with e.g., calendars and reminder alarms can improve prospective memory (8).
However, it is a complex interaction among the person with neurological disease, the activities that she or he wants to engage in, the environment or context in which the activity occurs, and the ATC that is available to support the activity. The International Classification of Functioning, Disability and Health (ICF) (9) describes human functioning and disability in relation to contextual factors; and has the potential to accommodate this complex interaction. The ICF organizes human functioning into two parts. Part 1 has two components: body functions and body structure, activity and participation. Part 2 also has two components: environmental factors and contextual factors. Each component consists of a number of categories with clear definitions. The ICF team and experts in neurological conditions have developed two ICF core sets for neurological conditions, one for the acute phase and the other for the post-acute rehabilitation phase (10, 11), however, these two core sets may not be fully applicable for patients with neurological diseases in the community rehabilitation phase. During the community rehabilitation phase, the conditions of patients with neurological diseases are relatively stable; some of the patients may have the opportunity to return to work part-time or establish a better daily routine, and most importantly, they would like to be as independent as possible.
During the community rehabilitation phase, patients with neurological diseases need cognitive support (ATC) to be able to perform different activities, alone or with others in different environments. Often, goal setting in this rehabilitation phase is important because it motivates both the patient and the rehabilitation team to work toward the same goal (12). Goal setting in relation to cognitive deficits using ATC are common in clinical practice and therapists often set several rehabilitation goals together with a patient. However, these rehabilitation goals are usually phrased differently, which limits the comparisons of rehabilitation goals in relation to the ATC. Particularly at the level of participation, goals are very much dependent on the person's daily habits and occupation. It is thus valuable to link the goals to some standardized terminologies, such as the ICF. Linking rehabilitation goals to the ICF will provide a comprehensive overview of the goals in relation to the use of ATC as cognitive support and help to identify the aspects that are lacking in rehabilitation service for persons with neurological diseases. One question is whether the ATC available in the market only support certain cognitive functions or a broad range of cognitive functions. Linking the rehabilitation goals to the ICF will provide us a good answer to this question.
However, although goal setting in relation to the prescription of ATC is a common clinical practice, effects of ATC in relation to goal achievement are seldom investigated in persons with neurological diseases. Measuring goal achievement in relation to the effects of ATC is to measure the extent to which patient's individual goals are achieved after the prescription of ATC. Particularly, there is a lack of literature that reports goal achievement in relation to the use of ATC to support different levels of participation, such as cognitive support for returning to work, or cognitive support for social functioning. Furthermore, despite the potential benefits of ATC reported in numerous studies, there are very few longitudinal studies that report the long-term effects of ATC in persons with neurological diseases. Long-term effects are crucial for different reasons. First, a long-term follow-up evaluation will provide a better picture whether the technology has been fully integrated into the user's everyday life. Second, learning and using ATC often requires a substantial degree of cognitive function, especially for those with moderate cognitive impairments. A long-term follow up will show the learning progress of ATC users. Third, development of ATC is advancing rapidly, and new ATC are released every year. Long-term follow up of the usability of ATC will show a better view of any improvement in human-machine interface. Fourth, the aim of ATC is to increase independence of the patients and reduce the burden on caregivers. However, environmental factors, such as caregivers that are close to the person, can be either barriers or facilitators in the use of ATC (13). It is important to identify the factors that would predict goal achievement in using the ATC as cognitive support in persons with neurological diseases. Conclusions that will be drawn from a long-term follow up of ATC will influence our services, prescription, policymaking, and the expenditure of public funds.
Thus, the aim of the study is 3-fold. Firstly, we will use the ICF to link rehabilitation goals regarding the use of ATC in adults with neurological diseases. Secondly, we will evaluate effects of the ATC using goal achievement over a 5-year period. Thirdly, we will explore the factors that predict goal achievement in relation to the effects of ATC.
Method
Study Design
A longitudinal prospective study will be used to answer the aim. The study is a 5-year project and data will be collected at different time points during a 5-year period.
Participants
Inclusion criteria are (i) patients who have a neurological disease, (ii) patients who have a need for at least one ATC, and (iii) age 18 or over. We will exclude patients with neurological diseases who have other non-neurological diseases.
Ethics
The study has received ethical approval from Swedish Ethical Review Authority. The number is Dnr 2021–01337.
Recruitment
We will recruit patients with different neurological diseases via Adult Rehabilitation Center, Region Örebro County, Sweden. Power analysis based on multiple regression model suggests a total of 100 participants will be enough for data analysis. With a consideration of 40% dropout over the 5-year period, we plan to include 140 participants.
Information about the study will be sent to the homes of potential participants. The patients and their families will have the opportunity to ask questions about the study and how data will be extracted from their records. The patients will be assured that their refusal of participation will not affect the health care service they will continue to receive from the rehabilitation center. Once a patient has consented to take part in the study, a research assistant will start data collection from the patient's records.
Data Collection and Instruments
We will extract data before, during and after the prescription of the ATC. The following data will be extracted:
1. Number of diagnoses and symptoms: the number of health conditions will be measured by summing the number of neurological diagnoses (according to the ICD-10 SE) and the number of neurological symptoms. For example, a patient can have two neurological diagnoses, such as stroke and epilepsy.
2. Demographic data: We will collect data on age, sex (0 = male, 1 = female), marital status (0 = single, 1 = married, 2 = divorced, 3 = widow), years of education, living arrangement (0 = living alone, 1 = not living alone), availability of caregiver (0 = no caregiver, 1 = have caregiver).
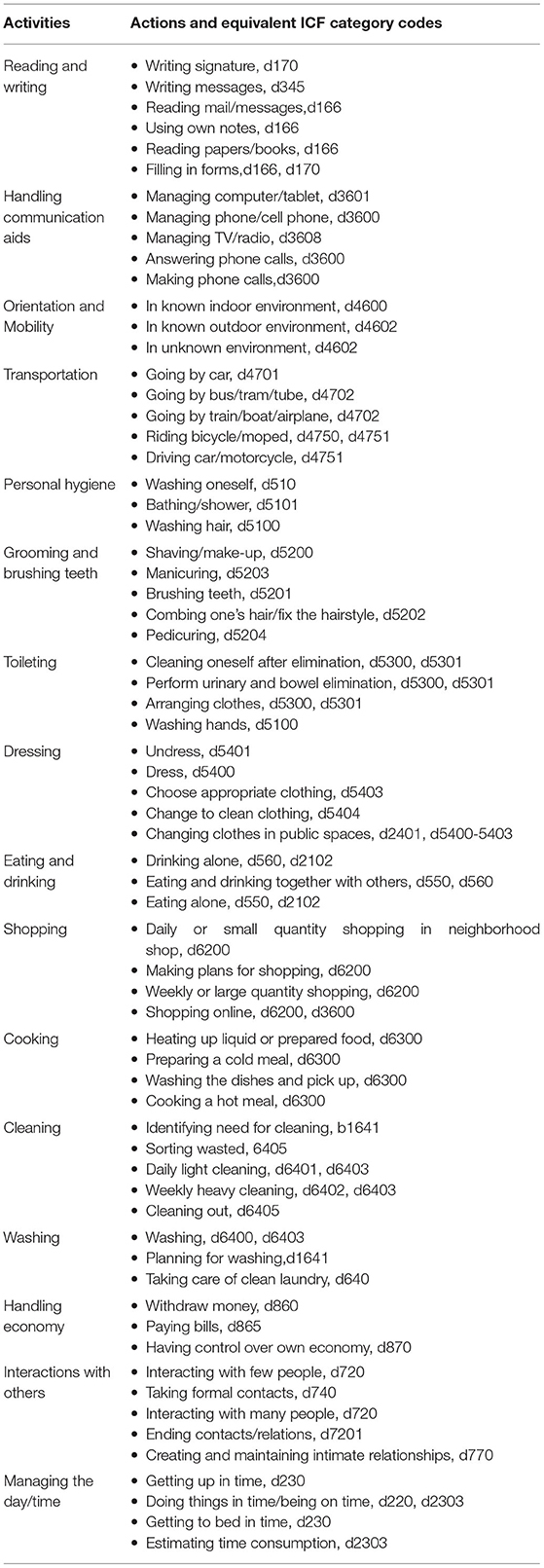
3. Performance in everyday activities: We will collect results of the performance in everyday activities using the ADL Taxonomy (14). It is an instrument that consists of 16 activities with three to six actions in each activity and it is routinely used by occupational therapists at the center. As for this study, the result of performance will be summed by the number of successful performances of each action (0 = cannot, 1 = can). The actions in the ADL Taxonomy are already mapped by its developers to the following equivalent ICF categories (Table 1) (14).
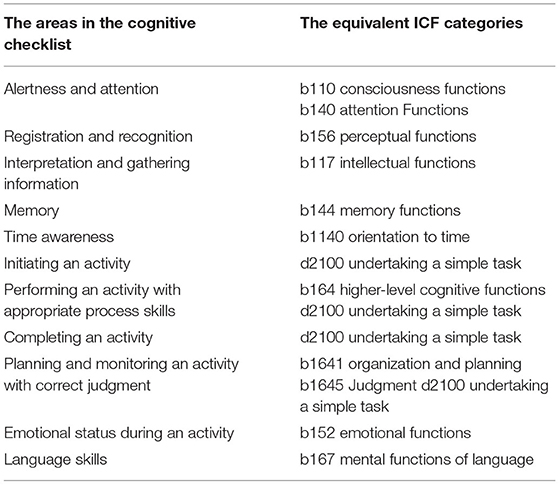
4. Assessment of cognitive functions during everyday activities: the Cognitive Checklist is a checklist that assesses 11 cognitive areas in one of the everyday activities in the ADL-Taxonomy (15). It is routinely used by occupational therapists at the center to assess cognitive functions in an everyday activity performed by patients. The results of the assessment will be summed by the number of successful areas (0 = cannot, 1 = can). The checklist assesses 11 cognitive areas and we have mapped the areas to the equivalent ICF categories (Table 2).
5. Choice of ATC: We will collect data on the ATC that will be chosen. The ATC will be primarily classified using the ICF cognitive functions (9) and according to Gillespie (16):
• Attention Functions (b140)
• Calculation Functions (b172)
• Emotional Functions (b152)
• Higher-level Cognitive Functions (b164)
• Memory Functions (b144)
Other ICF cognitive functions will be used to classify the ATC if none of the above ICF cognitive functions are appropriate. We will also classify the ATC using ICF categories in the environmental factor, e1151 Assistive products and technology for personal use in daily living.
6. Goal achievement using Goal Attainment Scale (GAS) (17): The GAS is an instrument that is intended to evaluate the effect of an intervention by assessing changes in a person's rehabilitation goals. The scale has five levels:
• −2: no change or current status
• −1: less than expected
• 0: expected
• +1: more than expected
• +2: much more than expected
A patient and their therapist will formulate a rehabilitation goal regarding the use of the ATC. This rehabilitation goal will then be used to develop a 5-step GAS. This 5-step GAS will be used to assess changes in reaching the goal in relation to the use of ATC. The GAS score will be evaluated by the therapist and the patient together. When the goal is reached within 5 years, that is, when the patient's goal has reached 0 or above, a new rehabilitation goal will be set.
Data Management
Every participant will be given a unique number in an unidentified database. The database will be stored in a research computer that will be locked with a secure password, and only the research team will have the password to access the database.
Data Analysis
Linking the Data to the ICF
To answer the first fold of the aim “linking rehabilitation goals regarding the use of ATC to the ICF”, we have developed a preliminary set of ICF categories for persons with neurological diseases in community rehabilitation. We began the development with examining and combining the two ICF core sets for neurological conditions (10, 11), one for the acute phase and the other for the postacute rehabilitation phase and selected the ICF categories that are relevant for persons with neurological diseases in community rehabilitation.
Based on a previous evaluation of rehabilitation goals from the center in this project (unpublished work), we have selected the following ICF categories that are relevant to community rehabilitation. The process of updating this preliminary set of ICF categories will continue throughout the course of the project (Table 3).
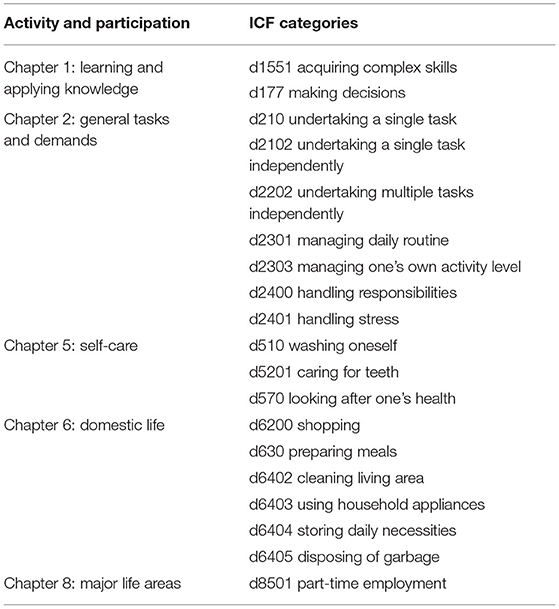
Table 3. A preliminary set of ICF categories for rehabilitation goals in community rehabilitation for persons with neurological diseases.
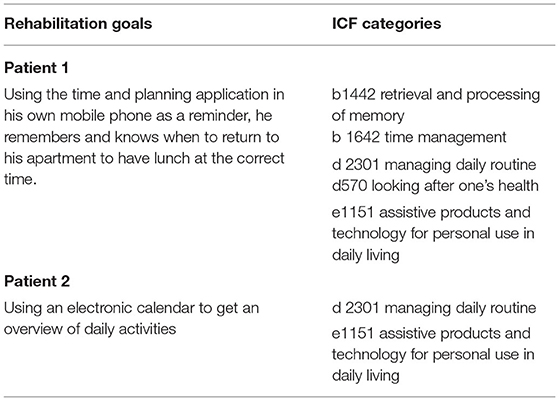
We will link the rehabilitation goals to the ICF categories according to the linking rules suggested by Cieza et al. (18, 19). The first author and the second author will start with the extraction of meaningful concepts from the goals and the other data. According to the refinement of the linking rules, Cieza et al. (18) suggest that one should ask the question of what the piece of data is about, taking all relevant contextual information into account. Two examples of rehabilitation goals are presented in Table 4. Patient 1 has a diagnosis of ischemic stroke, and patient 2 has a diagnosis of mild brain injury after a traffic accident. We have linked their rehabilitation goals to the corresponding ICF categories.
Statistical Analysis
The changes in GAS scores will be used to evaluate the effects of ATC in supporting daily functioning. All patients in the study will have at least one rehabilitation goal in relation to the use of ATC as cognitive support over a 5-year period. Each goal will be rated on a 5-point GAS (between −2 and +2), with the degree of attainment capture for each scale level. The overall GAS will be calculated as described in Turner-Stokes (17). The GAS scores will be incorporated into a single aggregated T-score by applying the formula:
Where Wi is the weight assigned to a particular goal (if equal weight, Wi = 1), Xi=the numerical value achieved (between −2 and +2). The formula will be used to calculate the baseline GAS score and the final GAS score. The difference between the baseline and the final GAS score will be used to indicate effects of the ATC.
Multiple regression analyses will be performed at six different time points to explore the variables that predict goal achievement of the patients. The time points are: 6 months after receiving the ATC, 1 year, 2 years, 3 years, 4 years, 5 years. First, using a standard multiple regression, the following variables were entered in the model: GAS score (between baseline score and final score), number of diagnoses, number of neurological symptoms, living condition, ADL-taxonomy score, Cognitive checklist score and part-time job. The best predictor variable for goal achievement will then identified. Second, hierarchical multiple regression will be performed to assess the ability of this best predictor to predict goal achievement after controlling for the influence of the other variables.
Conclusion
It is a complex interaction between the person with neurological disease, the activity in which she or he wants to engage in, the environment or context in which the activity occurs, and the ATC available to support the activity. The ICF is a common framework for all health professionals for the coding of functioning. Linking the rehabilitation goals to the ICF categories will provide a comprehensive overview of the goals in relation to the use of cognitive assistive technology and helps to identify the aspects that are lacking in rehabilitation service for persons with neurological diseases. Goal achievement is seldom used to evaluate long-term effects of ATC in persons with neurological diseases and limited attention has been paid to the factors that predict goal achievement in using the ATC as cognitive support in persons with neurological diseases.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Swedish Ethical Review Authority. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
HL led on the writing of this manuscript and NB read and approved the final version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We want to thank occupational therapist Anna-Lena Johansson for her suggestions of ICF categories in the Table 3.
References
1. Feigin VL, Vos T, Nichols E, Owolabi MO, Carroll WM, Dichgans M, et al. The global burden of neurological disorders: translating evidence into policy. Lancet Neurol. (2020) 19:255–65. doi: 10.1016/S1474-4422(19)30411-9
2. Morley J. An overview of cognitive impairment. Clin Geriatr Med. (2018) 34. doi: 10.1016/j.cger.2018.08.013
3. Petersen RC, Caracciolo B, Brayne C, Gauthier S, Jelic V, Fratiglioni L. Mild cognitive impairment: a concept in evolution. J Intern Med. (2014) 275:214–28. doi: 10.1111/joim.12190
4. O'Neill B, Gillespie A, Manly T, Dewar B-K, Kopelman M, Kapur N, et al. Assistive Technology for Cognition. London: Psychology Press (2014). doi: 10.4324/9781315779102
5. Leopold A, Lourie A, Petras H, Elias E. The use of assistive technology for cognition to support the performance of daily activities for individuals with cognitive disabilities due to traumatic brain injury: the current state of the research. Neuro Rehabilitation. (2015) 37:359–78. doi: 10.3233/NRE-151267
6. Gagnon-Roy M, Bourget A, Stocco S, Courchesne A-CL, Kuhne N, Provencher V. Assistive technology addressing safety issues in dementia: a scoping review. Am J Occup Ther. (2017) 71:7105190020p1-p10. doi: 10.5014/ajot.2017.025817
7. Repetto C, Paolillo MP, Tuena C, Bellinzona F, Riva G. Innovative technology-based interventions in aphasia rehabilitation: a systematic review. Aphasiology. (2021) 35:1623–46. doi: 10.1080/02687038.2020.1819957
8. Brandt Å, Jensen MP, Søberg MS, Andersen SD, Sund T. Information and communication technology-based assistive technology to compensate for impaired cognition in everyday life: a systematic review. Disabil rehabilitation Assist Technol. (2020) 15:810–24. doi: 10.1080/17483107.2020.1765032
9. World Health Organisation. International Classification of Functioning, Disability and Health (ICF). Geneva, Switzerland: World Health Organisation (2001).
10. Stier-Jarmer M, Grill E, Ewert T, Bartholomeyczik S, Finger M, Mokrusch T, et al. ICF Core Set for patients with neurological conditions in early post-acute rehabilitation facilities. Disabil Rehabil. (2005) 27:389–95. doi: 10.1080/09638280400014022
11. Ewert T, Grill E, Bartholomeyczik S, Finger M, Mokrusch T, Kostanjsek N, et al. ICF Core set for patients with neurological conditions in the acute hospital. Disabil Rehabil. (2005) 27:367–73. doi: 10.1080/09638280400014014
12. Levack WM, Taylor K, Siegert RJ, Dean SG, McPherson KM, Weatherall M. Is goal planning in rehabilitation effective? A systematic review. Clin Rehabil. (2006) 20:739–55. doi: 10.1177/0269215506070791
13. Boot FH, Owuor J, Dinsmore J, MacLachlan M. Access to assistive technology for people with intellectual disabilities: a systematic review to identify barriers and facilitators. J Intellect Disabil Res. (2018) 62:900–21. doi: 10.1111/jir.12532
14. Lidström-Holmqvist K, Törnquist K, Sonn U, Hjört K, Lena H. The ADL taxonomy - an assessment of occupational performance. 4 ed: The Swedish Association of Occupational Therapists (2017).
15. Andersson A-K, Blomstrand I, Dahm L, Gustafsson S, Göthlin H, Lund Å, et al. The Cognitive Checklist for everyday activities. In: Regionförbundet Örebro. (2012) 1–11.
16. Gillespie A, Best C, O'Neill B. Cognitive function and assistive technology for cognition: a systematic review. J Int Neuropsychol Soc. (2012) 18:1–19. doi: 10.1017/S1355617711001548
17. Turner-Stokes L. Goal attainment scaling (GAS) in rehabilitation: a practical guide. Clin Rehabil. (2009) 23:362–70. doi: 10.1177/0269215508101742
18. Cieza A, Fayed N, Bickenbach J, Prodinger B. Refinements of the ICF linking rules to strengthen their potential for establishing comparability of health information. Disabil Rehabil. (2019) 41:574–83. doi: 10.3109/09638288.2016.1145258
Keywords: assistive technology for cognition, neurological disease, goal, community rehabilitation, longitudinal effect
Citation: Lindner H and Buer N (2022) A Study Protocol for Persons With Neurological Diseases: Linking Rehabilitation Goals to the International Classification of Functioning, Disability and Health With a Focus on Assistive Technology for Cognition and Its Effects. Front. Rehabilit. Sci. 3:864804. doi: 10.3389/fresc.2022.864804
Received: 28 January 2022; Accepted: 01 April 2022;
Published: 10 May 2022.
Edited by:
Tsan-Hon Liou, Taipei Medical University, TaiwanReviewed by:
Wu Ting-fang, National Taiwan Normal University, TaiwanWen-Chou Chi, Chung Shan Medical University, Taiwan
Copyright © 2022 Lindner and Buer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Helen Lindner, helen.lindner@oru.se
 Helen Lindner
Helen Lindner