- 1Capstone College of Nursing, University of Alabama, Tuscaloosa, United States
- 2Idda Moffet School of Nursing, Samford University, Birmingham, AL, United States
- 3Department of Nutrition and Kinesiology, University of Illinois at Urbana-Champaign, Champaign, IL, United States
Purpose: Physical inactivity is one of the important factors leading to chronic diseases including cardiovascular disease (CVD) in individuals with disabilities. However, not many Physical Activity (PA) interventions are available for improving the efficacy of PA and cardiovascular outcomes among community wheelchair users. Therefore, this systematic review will appraise the existing PA interventions for the community dwelling wheelchair users; we especially examined features of the PA programs that showed the improvements in PA and the CVD outcomes compared to the interventions that did not show any improvements in these outcomes among these population. The study also aimed to provide some recommendations for future research.
Materials and Methods: A comprehensive and systematic search of literature published between 2015 and 2020 using the databases Scopus, Pubmed, Embase, and Cochrane CENTRAL was conducted. This review has followed the Preferred Reporting Items for Systematic Review (PRISMA) guidelines. The quality of the evidence was assessed by Using Joanna Briggs Institute's critical appraisal tool. Studies that tested the efficacy of PA interventions for community-dwelling adult wheelchair users and published in English were involved. Two reviewers reviewed the literature and any disagreements among these reviewers were resolved by a third reviewer.
Results: Fourteen articles were selected for this review. Most of the studies reported improvements in PA. A few studies followed up the participants and majority of the studies have looked at the CVD outcomes.
Conclusion: Large-scale studies with follow-ups, and community participatory research that evaluates the effect of PA interventions on PA and CVD outcomes among wheelchair users are needed.
Introduction
In the United States, an estimated 2.7 million adults require the use of a wheelchair based on their physical disabilities (1). Cardiovascular Disease (CVD) is a major cause of morbidity and mortality in these populations (2). There is compelling evidence that wheelchair users with physical disabilities have an increased incidence of chronic diseases, including CVD, cancer, diabetes, and osteoporosis (3). Physical inactivity, unhealthy diet, and alcohol consumption are major risk factors for increased risk of chronic diseases including CVD in wheelchair users (4). The majority of hospitals and clinical facilities focus on short-term rehabilitation services to improve wheelchair user skills for mobility (5). However, after discharge from the medical facilities, the improvement in daily activity in this population remains a concern as there are limited physical rehabilitation services available for continuing the recommended physical activity (PA) in residential communities (6). Additional factors, including disease severity and adaptations, add to the burden of physical inactivity in these individuals. For example, wheelchair users with multiple sclerosis indicated reduced PA participation based on dependence on the mobility device, disease severity (7), and environmental adaptations (8). Half of the wheelchair users with chronic spinal cord injury (SCI) reported no leisure-time PA (6) due to the disease severity. This underscores a critical need to focus on PA promotion among wheelchair users to decrease the burden of CVD and improve their overall well-being and quality of life.
The center for disease control (CDC) has recommended moderate to vigorous-intensity PA and muscle strengthening exercises for individuals with disabilities (CDC, 2019). In addition to the reduce risks for chronic disease, PA is essential to regain mobility, improved walking ability, balance, fitness, proper gait, and functional-ability in individuals with disabilities (9). Therefore, these individuals should perform a PA on regular basis that involves bodily movement produced by skeletal muscle contraction resulting in more energy utilization than at resting levels (10).
Wheelchair-users living in community settings engage in insufficient amount of PA for health benefits (3). This may be explained by inaccessible and unaffordable care, low education, and environmental obstacles as critical barriers for engaging in PA (11). This has underscored the importance of designing and delivering feasible and efficacious PA programs for community-dwelling wheelchair users. To that end, we conducted a systematic review to summarize the literature related to PA programs for community-dwelling wheelchair users and understand the features of the PA interventions that improve the PA and CVD outcomes compared to the PA interventions that did not show any improvements in these outcomes for this vulnerable population. We also aimed to identifying gaps in the literature for informing future research.
Methods
Overview
Literature search strategy
We conducted a comprehensive and systematic search of literature published between 2015 and 2020 using the databases Scopus, Pubmed, Embase, and Cochrane CENTRAL. This time span was selected as most of the research on the efficacy of interventions for PA in wheelchair users was done during this time period. Articles were located using keywords: exercise, physical-activit*, pilot, yoga, sport*, martial-art, recreation, garden, sports, leisure activities, community health services, wheelchairs, wheelchair*, initiative, project, program, plan. These keywords were used as they helped to catch almost all the research studies involving any kind of physical activity interventions for our target population. A professional librarian at the University of Alabama at Birmingham helped with the Literature search. The appendix lists search strings and terms used for different databases (Appendix A).
Data extraction and analysis
Two reviewers independently vetted each abstract and full article to ensure the validity and suitability of each study for inclusion. These reviewers have received an intense training in developing systematic reviews and have published some reviews before. Any disagreements among these reviewers were resolved through discussion. If a consensus was not reached, a third party who has expertise in behavioral and physical activity interventions, and has published several reviews, independently reviewed the material and resolved disputes for the articles.
Inclusion criteria
Articles describing experimental research were included. This included single subject design, RCTs, multisite RCTs, and pre-post designs of feasibility, pilot, and efficacy studies that examined the effect of PA interventions delivered among community dwelling wheelchair users in the community settings. Database searches were limited to articles written in English and continued until December 20, 2020. Studies that looked at PA for wheelchair users outcome variable, and the population residing in community settings were included for review. Studies involving PA, including leisure time PA, exercises, gardening, sports, recreation, yoga, and martial arts, as well as robotic exoskeletons were included in the review.
Exclusion criteria
Studies involving populations below 18 years of age and not involving wheelchair users were excluded. Studies conducted in any setting other than the community settings were excluded. Studies published in any language other than English were excluded.
Quality rating
Using Joanna Briggs Institute's critical appraisal tool, the two reviewers assessed the quality of studies selected for this review (12). The tools for critical appraisal were selected based on the study design. A score of 6 was given to the quasi-experimental study and a score of 9 was given to the randomized controlled trials. Any disagreements for critical appraisal were resolved by a third-party consultation.
Results
There were 304 articles identified in our initial search. We removed four duplicate articles. After reviewing the titles and abstracts for the remaining 300 articles, 161 articles were excluded and 139 articles were selected for full text review. After full text review of 139 articles, 125 articles were excluded for the failure to meet criteria, which resulted in the inclusion of 14 articles; Figure 1 provides the flow of article inclusion for this review (PRISMA flow diagram).
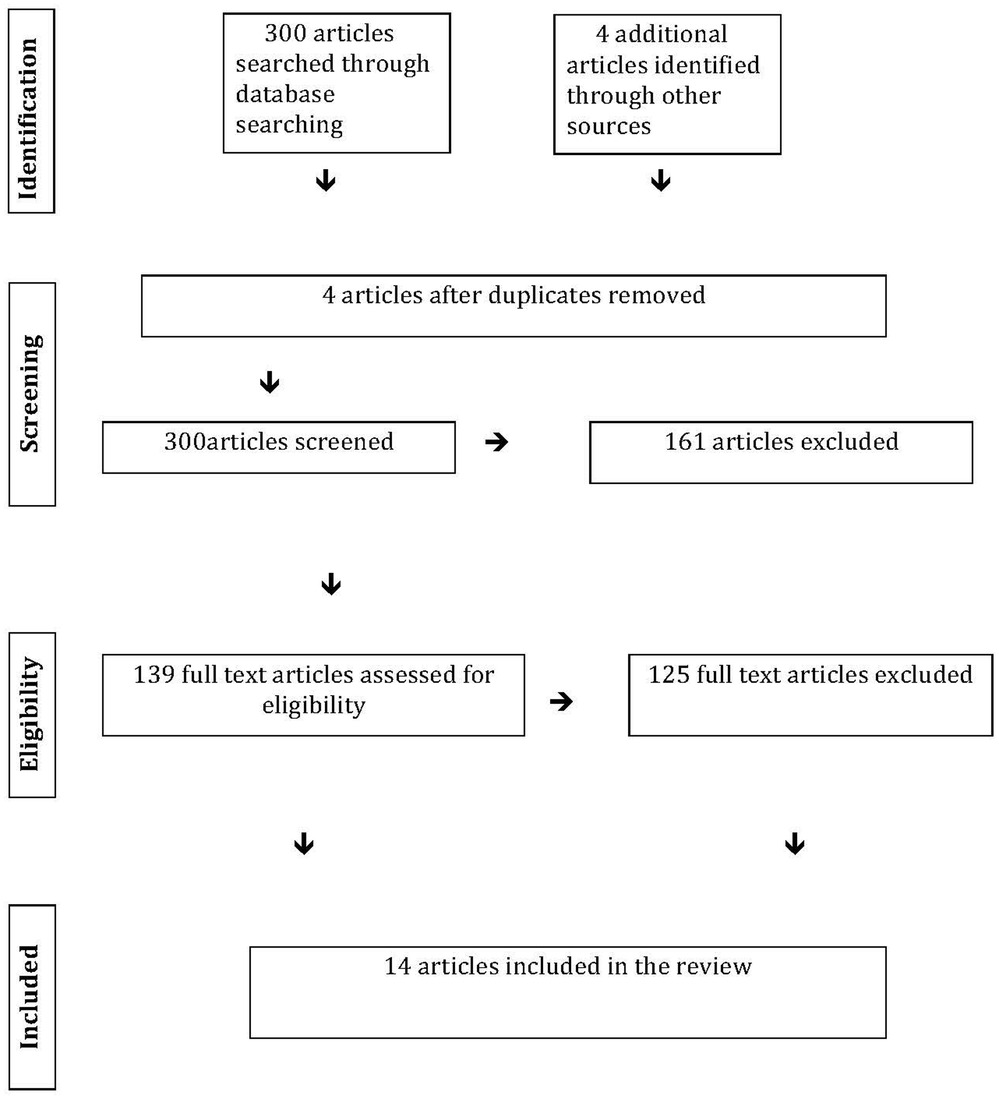
Figure 1. Show the data identification and stepwise data extraction including screening of the articles, removal of duplicates, and selection of the articles based on the inclusion and exclusion criteria.
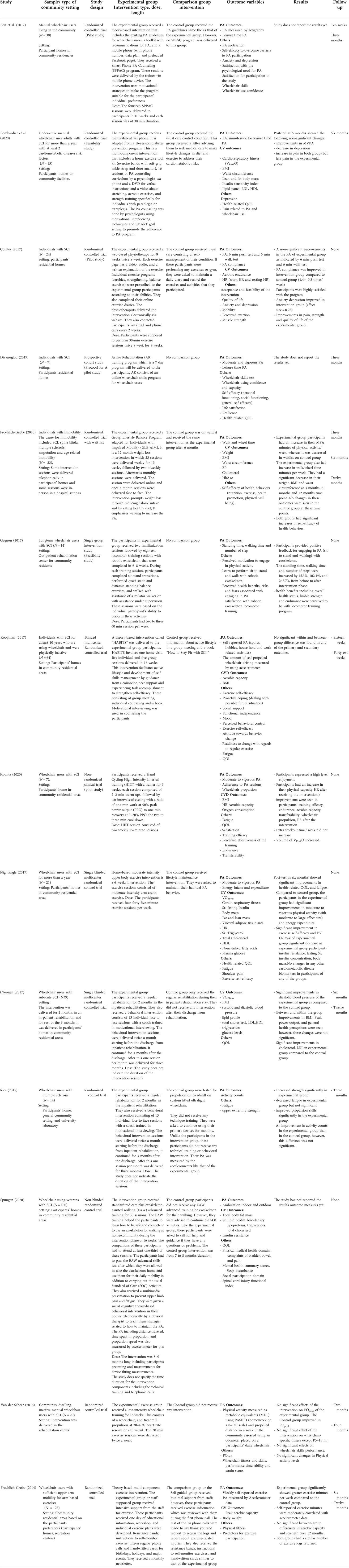
Table 1 provides the selected study characteristics. All of the studies were conducted in home/community settings. Study designs include single group intervention design (13, 14), randomized clinical trials (15–22), or multisite randomized clinical trials (23–25).
Ten studies were conducted on wheelchair users with spinal cord injuries (SCI) (13, 14, 16, 17, 20, 21, 23–26), Three studies had participants with immobility due to any disorder (15, 18, 27), one study involved persons with multiple sclerosis (19).
The duration of PA programs ranged between 6 and 12 months. The interventions included exercise interventions (16–18, 23), rehabilitation programs/physiotherapy programs (26), locomotor training programs with robotic exoskeleton (13, 20), hand cycling high intensity interval training (14), low intensity wheelchair training with treadmill propulsion (21), wheelchair and propulsions skills training (19), behavioral interventions including coaching, motivational interviewing (19, 23–25, 28).
These interventions were delivered in different modes including, face-to-face delivery, online delivery, and hybrid of both face-to-face and online sessions. Some of the interventions were delivered among participants individually, some in groups and some both involved both individual and groups sessions. The dose of the PA interventions also varied between these studies. Majority of the studies have delivered interventions weekly once or twice and the duration of a session varied between 25 (1), 30 min (6), 60 min (13). These PA programs are also varied in terms of the total time duration. The shortest intervention was 7 days long (17), and others varied from 6 weeks (24, 29) to a year long intervention (27).
Although the interventions were delivered for the community residential areas; however one of the studies had the intervention delivered in a rehabilitation center near the community residential areas, the participants were coming from their homes to attend the intervention sessions (13). Two studies delivered a component of intervention in the hospital setting and rest of the intervention was delivered in the participants homes (13, 30). All other studies have used participants' homes or community facilities to deliver the interventions in person or online.
The primary outcomes for this review is PA and CVD related outcomes. The secondary outcomes for this review were pain, aerobic endurance, cardiovascular fitness, wheelchair skills, body mass index, motivation, self-efficacy, mood, anxiety and depression, resilience, quality of life, participation and satisfaction with the intervention. Majority of the studies did not have any follow-up after cessation of the programs; three studies had one year follow up (18, 27, 30) and three studies had 3–4 month follow ups (19, 21, 26).
The PA outcomes were assessed differently in these studies, including leisure time PA, moderate to vigorous PA, minutes of walk, wheelchair propelled time and distance, standing time, self-reported PA (sports, hobbies, house hold and work related activities), PA measured as metabolic equivalents. Most of these studies reported improvements in PA (14, 16–19, 24, 27). Some of the studies further reported improvements in exercise self-efficacy (24, 27), depression and anxiety (16, 17), fatigue (19, 24), endurance (14), strength (19) quality of life (24) and the compliance with the PA intervention (17).
Nine studies have looked at the cardiovascular outcomes (1, 16–18, 20, 23, 27, 29, 30). The cardiovascular outcomes that were assessed include, heart rate, blood pressure (systolic and diastolic), body mass index, body weight, serum cholesterol, triglycerides, low-density lipoproteins, high-density lipoproteins, plasma glucose, insulin resistance assessment, cardiorespiratory fitness, Serum fasting insulin, lean and fat mass and visceral adipose tissue area.
Only three studies reported improvements in blood pressure, body mass index (27, 30), heart rate (1) and cholesterol, low density lipoproteins (30).
The studies involved in this review had high quality of methodology, however, due to the small sample size of most of these studies and the inconsistencies in PA measurement, the level of evidence for this review will be of low level.
Discussion
Community based PA programs for wheelchair users
Community-based programs for promoting PA for wheelchair users represents a prime opportunity for improving chronic diseases and other outcomes. These programs are scalable and sustainable, yet may not be as effective as supervised center-based programs. Unfortunately, there are not many community-based programs available for wheelchair users living in community settings. The studies included in this review were three multisite randomized controlled trials (RCTs) and seven RCTs, including four pilot RCTs. The majority of RCTs, including one multisite RCT (n = 6), reported an increase in PA from before to the after intervention phase; however, some RCTs (n = 4) did not report any improvements in PA among wheelchair users. The interventions in these studies differ for instance, behavioral and life style intervention, skills training, low and high intensity exercise training interventions. The interventions further differ in features including type of PA, individual vs. groups sessions, in-person vs. online delivery of intervention, length of whole intervention and duration of intervention sessions, use of technology, theory based vs. no theory-based interventions. These differences in interventions may explain the differences in efficacy of improving the PA among this population.
Lifestyle and behavioral interventions focusing on self-efficacy and adherence
Lifestyle behavioral interventions involved teaching people skills and strategies for increasing PA as part of daily life and may improve PA among wheelchair users. An increase in PA in a large magnitude (vector counts at wrist) were seen in wheelchair users with multiple sclerosis after receiving a three months behavioral intervention in addition to a wheelchair skills training. This intervention focused on enhancing self-efficacy, overcoming barriers, and identifying facilitators, in addition to the behavioral strategies of self-monitoring, goal setting, planning, optimizing outcome expectations (19). Weekly follow-ups were done telephonically with the participants to teach them about initiation and maintenance of PA. Another behavioral intervention with in-person individual sessions reported a significant improvement in PA and the cardiovascular outcomes of BMI, cholesterol, blood pressure, and low-density lipoproteins at one year follow up. However, these differences were not significant between the experimental and control groups. The intervention had a component of motivational interviewing, that might have increased the adherence to the intervention (25). Hence, the interventions that targeted on improving the PA self-efficacy seem to be promising for these populations. In additions some measures to improve the adherence of intervention must be incorporated into the PA interventions for better efficacy.
Contrary to the above studies, in a multisite RCT, a sixteen-week theory-based intervention that involved a home visit, 5 individual and 5 group counseling sessions and a book did not increase the self-reported PA of wheelchair users in the experimental group. The intervention focused on developing participants' active lifestyle and their self-management skills. There were no within or between-group differences in PA at four- and ten-months follow-ups. The control group had received information about active lifestyle by one group meeting and a book (23). Like other behavioral studies (19, 25), this intervention targeted PA self-efficacy, and behavioral control, however, the baseline self-efficacy in these participants was high, indicating that the intervention was not formulate based on the needs of this population. This could be explaining the ineffectiveness of this intervention on PA. In addition, this study included individuals with SCI for more than 20 years, the authors of this study believe that the long duration of their disabilities of this sample might have made their behavioral tendencies toward inactivity, thereby challenging for them to engage in the PA.
One recent study by Froehlich-Grobe et al. (2020) delivered a 12 month weight loss program to wheelchair users. The intervention was delivered in hybrid form, via telephone, and in-person. The intervention had a dietary and a PA component. The waitlist control group received the intervention after six months. Experimental group participants had a significant increase in minutes of walk and wheel time per week, and further had a significant weight loss after six months of starting the intervention. Both groups had a significant increase in self-efficacy of health behaviors (27).
Previously, Froehlich-Grobe et al. (2014) had delivered a theory-based multi-component exercise intervention to experimental and control groups (N = 128). The staff support group received additional intensive staff support for exercise, while the self-guided group received minimal support. The staff support group significantly increased exercise (17 min/week) compared to the self-guided group. There was no significant difference in aerobic capacity and strength over twelve month time period (18). Although staff-assisted interventions may show greater efficacy in improving PA, the time and cost related to such interventions affect their sustainability, especially in socio-ecologically deprived communities. Therefore, in order to develop sustainable programs, it is crucial to develop cost-effective interventions, and utilize previously existing resources from communities into these programs.
Community involvement is critical for community participatory research so as to use the already existing resources and develop interventions that are need based and acceptable to a community (31); therefore, it is vital to involve community dwelling wheelchair users when developing health promotion intervention for them. The knowledge about their needs, preferences, resources, barriers and facilities of a community is critical for the development of PA interventions (32). Cole et al. (2019) conducted a feasibility study in which participants' (N = 7) opinion related to the content, delivery, and self-management strategies of an evidence-based exercise intervention was assessed. Based on this information, this study developed a six months Workout on Wheels internet intervention (WoWii), which will be evaluated in the future (33). Such community-based research in which community-dwelling wheelchair users are involved in developing PA interventions is scarce. Hence, there is a critical need for such culturally sensitive PA interventions. These interventions may potentially show better acceptability, adherence, and sustainability in community settings as seen in other disciplines (34). Thereby will be more efficacious in improving wheelchair users' PA and their cardiovascular outcome.
The behavioral and lifestyle PA interventions report mixed results with regards to improvements in PA among wheelchair users. Therefore, novel lifestyle behavior programs that are tailored to the needs of these populations should be developed and tested by studies with strong methodology and larger sample sizes. The individual, interpersonal, and environmental levels factors that are found to be related to the adherence to community-based interventions (28) can be incorporated into these programs to improve consumer compliance. Studies should also examine the ecological validity and long-term sustenance of these programs in community settings. In addition, the long-term effects on cardiovascular outcomes are scarcely studied and must be focused in future research.
Wheelchair skills training programs
Wheelchair skills training programs demonstrated mixed results regarding the changes in PA of community-dwelling wheelchair users. Two RCTs delivered the wheelchair propulsion/skills training interventions to wheelchair users with SCI reported improvements in PA (14, 19). A custom-fit ultra-lightweight manual wheelchair propulsion and skills training revealed an increase in activity counts, strength and propulsion skills, and decreased fatigue of wheelchair users with multiple sclerosis (n = 14) compared to the participants in the control group. The experimental group had received theory-based behavioral intervention consisting of the moderate intensity wheelchair skills training and weekly telephonic follow-ups to teach behavioral strategies for initiation and maintenance of PA. Control group participants did not receive any training (19). In contrast, a sixteen-week low-intensity wheelchair propulsion-training program did not show any significant changes in PA levels of the experimental group participants. The participants received twice a week 30-minute sessions. Also, there were no improvements in their wheelchair propulsion and POpeak. The study indicates that low-intensity training to be insufficient to improve PA for wheelchair users with long term disabilities (21).
These studies suggest contradicting effects of wheelchair training on PA, and more studies are needed to confirm the efficacy of such interventions on PA of wheelchair users living in community settings. Van der Scheer et al. (2016) had delivered intervention to community dwelling wheelchair users in a rehabilitation setting; the barriers to access for such interventions must be focused especially in relation to availability of these resources in these underserved populations.
Exercise training programs
In a multicenter RCT, home-based moderate intensity upper body exercise intervention delivered in-person to wheelchair users with chronic SCI (n = 21) showed improvements in their PA. This behavioral intervention consisted of a PA component and a dietary component; it involved 45-minute weekly sessions for six weeks. The control group received lifestyle maintenance intervention in which they were asked to maintain their routine PA behavior. The study reported moderate (d = 0.62) to large (d = 1.37) effect sizes for improvements in PA, cardiorespiratory fitness, and exercise self-efficacy among the intervention participants. These improvements were seen after six weeks of intervention; the study did not do any follow up to see the long-term effects (24). Since the intervention was personalized to each participant's needs and delivered in the home setting, it improved exercise self-efficacy, which is reported to be a key factor in improvements in PA (35, 36). Delivering such interventions that are accessible to the community residents overcomes the barriers of the lack of transportation, time and access. These factors resulted in low attrition (11%) and increased adherence to the intervention, which might explain the large effect size of the intervention outcomes.
Recently, hand cycling high-intensity interval training intervention delivered to the wheelchair users (n = 7) showed an increase in the participants' PA. The participants received the intervention in three weekly sessions for six weeks. The participants also showed an increase in their PA heart rate (max.), training efficacy, endurance, aerobic capacity, and wheelchair propulsion skills. The study did not do any follow-ups. The intervention was tailored to each participant's pace and the study used some measure to assess and prompt the intervention adherence (14). These programs can be tested in future studies with large sample size to confirm efficacy in these populations.
Robotic exoskeleton to improve PA
An eight-week locomotor training program with EKSOTM (version 1.1) robotic exoskeleton was delivered among long-term wheelchair users (N = 14) to see its effect on their PA, motivation to engage in PA and performance capability to stand transfers. The intervention consisted of 2–3 training sessions per week in which participants completed sit to stand transitions, quasi static and standing balance exercises, and walked with assistance of a rollator walker while contact-guarded by a physical therapist. The walk with assistance of rollator walker was followed by walk with robotic exoskeleton. There was a significant increase in walking speed after the completion of intervention (P < 0.0001) (37). The participants provided positive feedback for the robotic exoskeleton and learning about walking capability and performance of sit-to-stand transfers. The participants' perceived an increase in their motivation to engage in leisure time PA adapted to their condition. In addition, participants also perceived positive effects of this program on their overall health, endurance, and upper limb strength (13).
Another RCT, still in the implementation phase, is planning to deliver exoskeleton assisted walking to experimental group participants (wheelchair users with SCI), in addition to standard care (N = 160). The control group is receiving only standard care. The study aims to see the effect of this intervention on indoor and outdoor ambulation, body fat mass, serum lipid profile, insulin resistance, social participation, and sleep disturbance (20). The results of this study are not yet reported. These studies show varied types of locomotor training with varied duration. Therefore, making it difficult to make any conclusions about the dose and duration of the locomotor training interventions. More experimental studies are needed to see the effectiveness of locomotor training with robotic exoskeleton on the PA efficacy of community-dwelling wheelchair users. Studies should be conducted to understand the duration of each type of training and the mechanisms involved in improving PA and cardiovascular health outcomes due to robotic exoskeleton training in these populations.
Technology based interventions for changing lifestyle PA
Technology offers a way to reach the increased number of populations in less time and helps eliminate the barriers (like lack of transportation and physical therapist time) that interfere with the delivery of care services. The majority of the studies included in this review (n = 6) used technology in the interventions. Use of technology (e.g., telephone calls, exercise videos delivered via web or DVD, smart phones apps.) in interventions seems to be promising for improving PA efficacy and intervention adherence among wheelchair users (16, 17, 27). Bombardier et al. (2020) adapted and delivered a multipronged diabetes prevention program to the experimental group (n = 7). This intervention used the telephone calls for delivering counseling sessions and DVDs videos for delivering aerobic exercise and strength training sessions to the experimental group. The control group participants (n = 8) received usual care involving advice to seek preventive care for cardio metabolic risk factors. Posttest at six months indicated though not significant, but there was an increase in experimental group participants' leisure-time PA (minutes of walk per week). There were significant improvements in their exercise self-efficacy and depression levels, also the likelihood of increase pain was significantly low in experimental group (P < 0.05) (16). Coulter et al. (2017) reported an improved adherence to web-based physiotherapy intervention in the experimental group participants (n = 16). The intervention was delivered for 8 weeks with two sessions per week and was tailored to each participant's individual needs. The intervention consists of strengthening, stretching, aerobic, and balance exercises as appropriate based on participants' abilities. The control group (n = 8) were advised to do the self-management for their condition. The participants in experimental group had moderate effect size (d = 0.40) improvements in their mobility and endurance. The study also reported improvements in PA compliance and depression in experimental group compared to control group (17). Thereby, increasing their PA performance in everyday life.
These pilot studies suggest that technology-based interventions yield improvements in PA and intervention adherence among wheelchair users, yet studies with large sample size and diverse sample in terms of severity of disability and wheelchair dependence should be conducted to help draw some concrete conclusions. For example, Best et al. (2017) has planned to deliver a 12-week Smart Phone Peer PA Counseling (SPPAC) program via phone to the experimental group participants, whereas the control group participants are supposed to receive PA guidelines only. The study aims to improve participants' autonomy to get engaged in leisure time PA as measured by Actigraph, PA self-efficacy and their motivation. The study is reported to be in implementation phase (15). Based on this study, Best et al. (2019) have developed a theory based Active Living Lifestyle Program (ALLWheel) for wheelchair users with SCI. This program is aimed to reach large number of individuals in their communities to improve their self-efficacy, motivation and autonomy, thereby improving their engagement in leisure time PA (38). The intervention is anticipated to have high participant adherence due to the benefits of technology use including flexibility in timing, independence in performing the intervention and lack of need for transportation and scheduling.
These studies have used simple technology (e.g., telephone, web delivery of home exercise videos, DVDs), which can be easily available in rural communities. However, so far, none of the RCTs that have technology-based interventions have been conducted on community dwelling wheelchair users. The use of technology could be useful to overcome the ecological barriers related to remote areas, and their sustenance in these health services deprived areas (39). Therefore, there is a need for studies with controlled designs to test efficacy of technology-based interventions to improve PA and cardio metabolic outcomes in rural dwelling wheelchair users. In addition, theory based and community partnership research should be emphasized to increase the sustenance of these programs.
Limitations
There is a possibility of some articles not being captured by the search strategies of this systematic review. The above findings should be interpreted carefully as there is a potential bias caused due to the limitations imposed by small sample size of the studies involved in this review. Limitations of this review also arise from the inconsistencies in PA measurement, and other confounding factors.
Conclusion
The purpose of this review is to gather knowledge about the availability of PA programs focused on improving PA and CVD outcomes among wheelchair users living in community settings. The knowledge gathered from this review illustrates that behavioral and lifestyle interventions have produced promising results in improving PA and CVD outcomes. Although the incorporation of technology that is mostly available to community-dwelling wheelchair users (telephone calls, DVDs, web-based exercise videos) has helped to overcome the facility barriers in community settings, none of the studies were community participatory research. As such, it is critical to involve community resources and partnerships for the ecological validity and sustainability of such PA programs in community settings. Most of the studies are small-scale pilot studies, and only a few have focused on the improvements in CVD outcomes in these populations. Large-scale studies with advanced methodology and long-term follow-ups are required to make any concrete conclusions and interpretations.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
Data extraction, data analysis. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Koontz AM, Ding D, Jan YK, de Groot S, Hansen A. Wheeled mobility. Biomed Res Int. (2015) 2015:138176. doi: 10.1155/2015/138176
2. Wilby ML. Physical mobility impairment and risk for cardiovascular disease. Health Equity. (2019) 3(1):527–31. doi: 10.1089/heq.2019.0065
3. CDC.gov. Disability and Health Promotion (2020) [cited 2021]. Available from: https://www.cdc.gov/ncbddd/disabilityandhealth/relatedconditions.html
4. Smith AE, Molton IR, Jensen MP. Self-reported incidence and age of onset of chronic comorbid medical conditions in adults aging with long-term physical disability. Disabil Health J. (2016) 9(3):533–8. doi: 10.1016/j.dhjo.2016.02.002
5. Emerich L, Parsons KC, Stein A. Competent care for persons with spinal cord injury and dysfunction in acute inpatient rehabilitation. Top Spinal Cord Inj Rehabil. (2012) 18(2):149–66. doi: 10.1310/sci1802-149
6. Best KL, Arbour-Nicitopoulos KP, Sweet SN. Community-based physical activity and wheelchair mobility programs for individuals with spinal cord injury in Canada: current reflections and future directions. J Spinal Cord Med. (2017) 40(6):777–82. doi: 10.1080/10790268.2017.1367363
7. Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U, et al. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. (2012) 380(9838):247–57. doi: 10.1016/S0140-6736(12)60646-1
8. Learmonth YC, Rice IM, Ostler T, Rice LA, Motl RW. Perspectives on physical activity among people with multiple sclerosis who are wheelchair users: informing the design of future interventions. Int J MS Care. (2015) 17(3):109–19. doi: 10.7224/1537-2073.2014-018
9. AHRQ.org. Can Physical Activity improve Health of Wheelchir Users 2019 [cited 2021]. Available from: https://effectivehealthcare.ahrq.gov/products/physical-activity-wheelchair/protocol
10. Westerterp KR. Physical activity and physical activity induced energy expenditure in humans: measurement, determinants, and effects. Front Physiol. (2013) 4:90. doi: 10.3389/fphys.2013.00090
11. Wakely L, Langham J, Johnston C, Rae K. Physical activity of rurally residing children with a disability: a survey of parents and carers. Disabil Health J. (2018) 11(1):31–5. doi: 10.1016/j.dhjo.2017.05.002
13. Gagnon DH, Vermette M, Duclos C, Aubertin-Leheudre M, Ahmed S, Kairy D. Satisfaction and perceptions of long-term manual wheelchair users with a spinal cord injury upon completion of a locomotor training program with an overground robotic exoskeleton. Disabil Rehabil Assist Technol. (2017) 19(2):138–45. doi: 10.1080/17483107.2017.1413145
14. Koontz AM, Garfunkel CE, Crytzer TM, Anthony SJ, Nindl BC. Feasibility, acceptability, and preliminary efficacy of a handcycling high-intensity interval training program for individuals with spinal cord injury. Spinal Cord. (2021) 59(1):34–43. doi: 10.1038/s41393-020-00548-7
15. Best KL, Routhier F, Sweet SN, Arbour-Nicitopoulos KP, Borisoff JF, Noreau L, et al. The smartphone peer physical activity counseling (SPPAC) program for manual wheelchair users: protocol of a pilot randomized controlled trial. JMIR Res Protoc. (2017) 6(4):e69. doi: 10.2196/resprot.7280
16. Bombardier CH, Dyer JR, Burns P, Crane DA, Takahashi MM, Barber J, et al. A tele-health intervention to increase physical fitness in people with spinal cord injury and cardiometabolic disease or risk factors: a pilot randomized controlled trial. Spinal Cord. (2021) 59(1):63–73. doi: 10.1038/s41393-020-0523-6
17. Coulter EH, McLean AN, Hasler JP, Allan DB, McFadyen A, Paul L. The effectiveness and satisfaction of web-based physiotherapy in people with spinal cord injury: a pilot randomised controlled trial. Spinal Cord. (2017) 55(4):383–9. doi: 10.1038/sc.2016.125
18. Froehlich-Grobe K, Lee J, Aaronson L, Nary DE, Washburn RA, Little TD. Exercise for everyone: a randomized controlled trial of project workout on wheels in promoting exercise among wheelchair users. Arch Phys Med Rehabil. (2014) 95(1):20–8. doi: 10.1016/j.apmr.2013.07.006
19. Rice IM, Rice LA, Motl RW. Promoting physical activity through a manual wheelchair propulsion intervention in persons with multiple sclerosis. Arch Phys Med Rehabil. (2015) 96(10):1850–8. doi: 10.1016/j.apmr.2015.06.011
20. Spungen AM, Bauman WA, Biswas K, Jones KM, Snodgrass AJ, Goetz LL, et al. The design of a randomized control trial of exoskeletal-assisted walking in the home and community on quality of life in persons with chronic spinal cord injury. Contemp Clin Trials. (2020) 96:106102. doi: 10.1016/j.cct.2020.106102
21. van der Scheer JW, de Groot S, Tepper M, Faber W, group A, Veeger DH, et al. Low-intensity wheelchair training in inactive people with long-term spinal cord injury: a randomized controlled trial on fitness, wheelchair skill performance and physical activity levels. J Rehabil Med. (2016) 48(1):33–42. doi: 10.2340/16501977-2037
22. Ferri-Caruana A, Millan-Gonzalez L, Garcia-Masso X, Perez-Nombela S, Pellicer-Chenoll M, Serra-Ano P. Motivation to physical exercise in manual wheelchair users with paraplegia. Top Spinal Cord Inj Rehabil. (2020) 26(1):1–10. doi: 10.1310/sci2601-01
23. Kooijmans H, Post MWM, Stam HJ, van der Woude LHV, Spijkerman DCM, Snoek GJ, et al. Effectiveness of a self-management intervention to promote an active lifestyle in persons with long-term spinal cord injury: the HABITS randomized clinical trial. Neurorehabil Neural Repair. (2017) 31(12):991–1004. doi: 10.1177/1545968317736819
24. Nightingale TE, Rouse PC, Walhin JP, Thompson D, Bilzon JLJ. Home-based exercise enhances health-related quality of life in persons with spinal cord injury: a randomized controlled trial. Arch Phys Med Rehabil. (2018) 99(10):1998–2006. doi: 10.1016/j.apmr.2018.05.008
25. Nooijen CF, Stam HJ, Sluis T, Valent L, Twisk J, van den Berg-Emons RJ. A behavioral intervention promoting physical activity in people with subacute spinal cord injury: secondary effects on health, social participation and quality of life. Clin Rehabil. (2017) 31(6):772–80. doi: 10.1177/0269215516657581
26. Divanoglou A, Tasiemski T, Jorgensen S. INTERnational project for the evaluation of “ctivE rehabilitation” (inter-PEER)—a protocol for a prospective cohort study of community peer-based training programmes for people with spinal cord injury. BMC Neurol. (2020) 20(1):14. doi: 10.1186/s12883-019-1546-5
27. Froehlich-Grobe K, Betts AC, Driver SJ, Carlton DN, Lopez AM, Lee J, et al. Group lifestyle balance adapted for individuals with impaired mobility: outcomes for 6-month RCT and combined groups at 12 months. Am J Prev Med. (2020) 59(6):805–17. doi: 10.1016/j.amepre.2020.06.023
28. Wilroy JD, Lai B, Davlyatov G, Mehta T, Thirumalai M, Rimmer JH. Correction: correlates of adherence in a home-based, self-managed exercise program tailored to wheelchair users with spinal cord injury. Spinal Cord. (2021) 59(1):92. doi: 10.1038/s41393-020-0526-3
29. Nightingale TE, Walhin JP, Thompson D, Bilzon JLJ. Impact of exercise on cardiometabolic component risks in spinal cord-injured humans. Med Sci Sports Exerc. (2017) 49(12):2469–77. doi: 10.1249/MSS.0000000000001390
30. Nooijen CF, de Groot S, Postma K, Bergen MP, Stam HJ, Bussmann JB, et al. A more active lifestyle in persons with a recent spinal cord injury benefits physical fitness and health. Spinal Cord. (2012) 50(4):320–3. doi: 10.1038/sc.2011.152
31. Henderson S, Kendall E, See L. The effectiveness of culturally appropriate interventions to manage or prevent chronic disease in culturally and linguistically diverse communities: a systematic literature review. Health Soc Care Community. (2011) 19(3):225–49. doi: 10.1111/j.1365-2524.2010.00972.x
32. Wright J, Williams R, Wilkinson JR. Development and importance of health needs assessment. Br Med J. (1998):316(7140):1310-3. doi: 10.1136/bmj.316.7140.1310
33. Cole M, Froehlich-Grobe K, Driver S, Shegog R, McLaughlin J. Website redesign of a 16-week exercise intervention for people with spinal cord injury by using participatory action research. JMIR Rehabil Assist Technol. (2019) 6(2):e13441. doi: 10.2196/13441
34. Trinh NH, Hagan PN, Flaherty K, Traeger LN, Inamori A, Brill CD, et al. Evaluating patient acceptability of a culturally focused psychiatric consultation intervention for Latino Americans with depression. J Immigr Minor Health. (2014) 16(6):1271–7. doi: 10.1007/s10903-013-9924-3
35. McAuley E, Szabo A, Gothe N, Olson EA. Self-efficacy: implications for physical activity, function, and functional limitations in older adults. Am J Lifestyle Med. (2011) 5(4). doi: 10.1177/1559827610392704
36. Chu IH, Chen YL, Wu PT, Wu WL, Guo LY. The associations between self-determined motivation, multidimensional self-efficacy, and device-measured physical activity. Int J Environ Res Public Health. (2021) 18(15). doi: 10.3390/ijerph18158002
37. Gagnon DH, Escalona MJ, Vermette M, Carvalho LP, Karelis AD, Duclos C, et al. Locomotor training using an overground robotic exoskeleton in long-term manual wheelchair users with a chronic spinal cord injury living in the community: lessons learned from a feasibility study in terms of recruitment, attendance, learnability, performance and safety. J Neuroeng Rehabil. (2018) 15(1):12. doi: 10.1186/s12984-018-0354-2
38. Best KL, Routhier F, Sweet SN, Lacroix E, Arbour-Nicitopoulos KP, Borisoff JF. Smartphone-delivered peer physical activity counseling program for individuals with spinal cord injury: protocol for development and pilot evaluation. JMIR Res Protoc. (2019) 8(3):e10798. doi: 10.2196/10798
39. RuralHealthInfo.org. Healthcare Access in Rural Communities 2020 [cited 2021]. Available from: https://www.ruralhealthinfo.org/topics/healthcare-access
Appendix A
Embase
(exercise*:ti,ab OR 'physical activit*':ti,ab OR gymnastic*:ti,ab OR calisthenic*:ti,ab OR run*:ti,ab OR jog*:ti,ab OR swim*:ti,ab OR walk*:ti,ab OR climb*:ti,ab OR 'weight lift*':ti,ab OR pilate*:ti,ab OR qigong:ti,ab OR 'qi gong':ti,ab OR danc*:ti,ab OR 'tai ji':ti,ab OR 'tai chi':ti,ab OR 'tai ji quan':ti,ab OR taiji:ti,ab OR taijiquan:ti,ab OR 'tai chi chuan':ti,ab OR yoga:ti,ab OR sport*:ti,ab OR athletic*:ti,ab OR baseball:ti,ab OR softball:ti,ab OR basketball:ti,ab OR netball:ti,ab OR bicycling:ti,ab OR cycling:ti,ab OR boxing:ti,ab OR cricket:ti,ab OR football:ti,ab OR rugb*:ti,ab OR golf*:ti,ab OR hockey*:ti,ab OR wrestl*:ti,ab OR 'martial art*':ti,ab OR 'hap di do':ti,ab OR judo:ti,ab OR karate:ti,ab OR jujitsu:ti,ab OR 'tae kwon do':ti,ab OR aikido:ti,ab OR wushu:ti,ab OR 'kung fu':ti,ab OR 'gong fu':ti,ab OR gongfu:ti,ab OR mountaineer*:ti,ab OR tennis:ti,ab OR racquetball:ti,ab OR racketball:ti,ab OR 'racket ball':ti,ab OR badminton:ti,ab OR lacrosse:ti,ab OR skating*:ti,ab OR skateboard*:ti,ab OR snowmobiling:ti,ab OR sledding:ti,ab OR skiing:ti,ab OR snowboard*:ti,ab OR soccer:ti,ab OR track:ti,ab OR volleyball:ti,ab OR surfing:ti,ab OR rowing:ti,ab OR polo:ti,ab OR kayaking:ti,ab OR canoeing:ti,ab OR boating:ti,ab OR surfboarding:ti,ab OR recreation*:ti,ab OR ballet:ti,ab OR 'hip hop':ti,ab OR jazz:ti,ab OR tap:ti,ab OR salsa:ti,ab OR fitness:ti,ab OR 'exercise'/exp OR 'sport'/exp OR 'recreation'/exp OR 'fitness'/exp OR 'physical activity'/exp) AND ('wheelchair'/exp OR wheelchair*:ab,ti OR scooter*:ab,ti)
Retrieves 123
PubMed
("Exercise"[Mesh] OR Exercise* [tiab] OR physical-activit*[Title/Abstract] OR pilate*[Title/Abstract] OR yoga[Title/Abstract] OR Sport*[Title/Abstract] OR martial-art [tiab] OR recreation*[Title/Abstract] OR garden*[Title/Abstract] OR "Sports"[Mesh] OR "Recreation"[Mesh] OR "Leisure Activities"[Mesh] OR "Community Health Services"[Mesh]) AND ("Wheelchairs"[Mesh] OR wheelchair* OR scooter*) AND (initiative*[Title] OR project*[Title] OR program*[Title] OR plan*[Title])
Retrieves 79
Scopus
TITLE-ABS-KEY (initiative* OR project* OR program* OR plan*) AND TITLE-ABS-KEY (exercise* OR physical-activit* OR sport* OR recreation* OR leisure) AND TITLE-ABS-KEY (wheelchair* OR scooter*)
Retrieves 94 results
CENTRAL
ID Search Hits
#1 MeSH descriptor: [Leisure Activities] explode all trees 18458
#2 MeSH descriptor: [Exercise] explode all trees 24606
#3 MeSH descriptor: [Community Health Services] explode all trees 13872
#4 (Exercise* OR physical-activit* OR pilate* OR yoga OR Sport* OR martial-art OR recreation* OR garden*):ti,ab,kw 128302
#5 (initiative* OR project* OR program* OR plan*):ti 48466
#6 (wheelchair* OR scooter*):ti,ab,kw 848
#7 MeSH descriptor: [Wheelchairs] explode all trees 197
#8 #1 OR #2 OR #3 OR #4145083
#9 #6 OR #7848
#10 #5 AND #8 AND #932
#11 #8 AND #9324
Keywords: wheelchair users, physical activity, cardiovascular disease, technology use, community
Citation: Andrabi MS, Mumba M, Key B and Motl R (2022) Physical activity programs for cardiovascular outcomes in community wheelchair users: A systematic review. Front. Rehabilit. Sci. 3:1007778. doi: 10.3389/fresc.2022.1007778
Received: 30 July 2022; Accepted: 28 September 2022;
Published: 4 November 2022.
Edited by:
Reuben Escorpizo, University of Vermont, United StatesReviewed by:
Zhuoying Qiu, China Rehabilitation Research Center/WHO Collaborating Center for Family International Classifications, ChinaMasauso Chirwa, University of Zambia, Zambia
© 2022 Andrabi, Mumba, Key and Motl. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mudasir Saleem Andrabi bWFuZHJhYmlAdWEuZWR1
Specialty Section: This article was submitted to Disability, Rehabilitation, and Inclusion, a section of the journal Frontiers in Rehabilitation Sciences
 Mudasir Saleem Andrabi
Mudasir Saleem Andrabi Mercy Mumba1
Mercy Mumba1 Betty Key
Betty Key