
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
METHODS article
Front. Rehabil. Sci., 13 December 2021
Sec. Translational Research in Rehabilitation
Volume 2 - 2021 | https://doi.org/10.3389/fresc.2021.764022
This article is part of the Research TopicHighlights in Translational Research in Rehabilitation 2021/22View all 5 articles
Purpose: Service providers must identify and assess older adults who have concurrent vision and hearing loss, or dual sensory impairment (DSI). An assessment tool suitable for this purpose is the interRAI Community Health Assessment (CHA) and its Deafblind Supplement. This study's goal was to explore this assessment's administration process and to generate suggestions for assessors to help them optimize data collection.
Methods: A social worker with experience working with adults who have sensory loss, who was also naïve to the interRAI CHA, administered the assessment with 200 older adults (65+) who had visual and/or hearing loss. The assessor evaluated the utility of the instrument for clinical purposes, focusing on sections relevant to identifying/characterizing adults with DSI.
Results: Suggestions include the recommendation to ask additional questions regarding the person's functional abilities. This will help assessors deepen their understanding of the person's sensory status. Recommendations are also provided regarding sensory impairments and rehabilitation, in a general sense, to help assessors administer the interRAI CHA.
Conclusions: Suggestions will help assessors to deepen their knowledge about sensory loss and comprehensively understand the assessment's questions, thereby allowing them to optimize the assessment process and increase their awareness of sensory loss in older adults.
There is an ongoing rise in the prevalence of dual sensory impairment (DSI), defined as the combination of any level of concurrent vision and hearing loss irrespective of age of onset (1). DSI interferes with a person's ability to communicate, acquire information, and perform daily activities (2). The prevalence of DSI increases with increasing age, and estimates vary among diverse sub-groups of older adults (65+), ranging from 20% in residential care or day centers (3) to 38% among centenarians (4). Most developed countries are experiencing population aging, with the most rapid increase among people aged 85+ years, who are also the most likely to experience DSI and its associated challenges (5, 6). Given the correlation between aging and sensory impairment, it is estimated that as many as one in three individuals over the age of 50 have either reduced vision, impaired hearing, or DSI (1). Once detected, rehabilitation services for sensory loss are available, such as those in Montreal, Canada, where 69% of clients receiving services for DSI are over the age of 64 (7).
As a result of population aging, the proportion of older adults who access any type of health service in developed countries is currently high and will likely increase over the coming decades. For example, in 2009–2010 in Canada, seniors made up 14% of the population, but accounted for 40% of acute hospital stays (8). The detection and evaluation of sensory impairments are of the utmost importance because several aspects of health care delivery, and communication with health professionals, depend on it. However, many first-line health care providers operate under the basic assumption that their clients can hear and see them; however, in a third of their older patients this may not always be the case (1). Therefore, it is critical to provide first-line health service providers with standardized and user-friendly assessment tools to identify individuals with DSI, assess their needs and strengths, and guide the design of rehabilitation strategies.
The interRAI Community Health Assessment (CHA) and its Deafblind Supplement (DbS) is a standardized, valid, and reliable assessment instrument for use with adults (18+), including those with DSI (9, 10). This assessment was created by interRAI (http://www.interrai.org/), a not-for-profit research network of 90 members from 35 countries, who have a mandate to develop and test assessment systems that aim to improve the quality of life and delivery of services for vulnerable populations, including older persons and those with disabilities. The interRAI instruments are based on significant input from content experts, clinicians and service providers, are used internationally, including being mandated in several regions in Canada, and are backed by studies evaluating their psychometric properties (11). The goal of the instrument is to help an assessor identify the needs and abilities of adults who reside in the community and to guide the assessor in terms of developing a service plan.
The interRAI CHA consists of roughly 150 items, and four supplemental assessments, one of which is the DbS. The responses to two items on the CHA that refer to the person's functional vision and hearing, will “trigger” whether or not the person likely has DSI and should therefore be assessed more comprehensively with the DbS. The DbS includes an additional 150 items that capture further detail about the person's vision and hearing and other issues relevant for an individual with DSI (e.g., age of onset of sensory loss, diagnoses, communication, psychosocial well-being) (9). Research shows the assessment has good internal consistency and convergent validity (12), as well as some preliminary evidence of acceptable inter-rater reliability (13). The assessment constitutes a comprehensive assessment of a person's overall health and functional abilities, as well as a more specific evaluation of domains that are relevant in individuals with DSI. A person is classified as having DSI if they report having at least minimal difficulty with near vision activities (using vision device if applicable) and with hearing (14). The assessor uses the gathered information and his/her own clinical judgement to decide how to proceed in terms of referrals (e.g., referral to programs/resources specific to persons with DSI) and implementation of a service plan.
While many age-related conditions have been investigated, few studies have examined the assessment and service needs of older persons with DSI (15, 16). After completion of the data collection for a larger protocol on sensory-cognitive aging (17, 18), the team members noticed during team discussions that the individual who had collected the data had developed a unique expertise and extensive case notes that would allow the team to develop recommendations to improve the administration of the interRAI CHA and its DbS. Based on this expertise, the aim of the present study was to develop suggestions that can help future assessors optimize data collection with the interRAI CHA and DbS. This study utilized the experience of a knowledgeable assessor, who administered the interRAI CHA and DbS to 200 older adults (61+) with sensory impairments, to qualitatively evaluate the instrument and provide recommendations that would be useful to others completing the assessment who may be less familiar with the nuances of communication and interviewing older persons with sensory challenges. This evaluation was undertaken with the needs of three groups of stakeholders in mind: 1. persons who experience significant functional limitations due to either a single or dual hearing and/or vision loss; 2. assessors new to the instrument; and 3. those who are experienced in developing and using interRAI tools. As much as any assessment tool can be useful in understanding the needs and preferences of the person, it should be recognized that an assessment should always be considered as a compliment to clinical judgement, and not a replacement, and that all assessments are inherently imperfect. This paper presents the resulting recommendations and aims to improve assessor's awareness of sensory loss in older adults and how it impacts the assessment process in order to facilitate assessors' administration of the instrument and optimize the quality of the information captured.
This study required the use of the interRAI community health (CHA) assessment form and user's manual (10).
The interRAI CHA is generally administrated with a global focus on multiple aspects of functioning (19). Sensory health only becomes the focus once the DbS has been triggered during the administration of the CHA; therefore, it has been the clinical experience of our team members that individuals who administer the CHA do not automatically consider potential administration barriers (e.g., subtle cues indicating the need for communication accommodations) that may be present before a sensory impairment has been detected or identified. The awareness of such barriers may be largely connected to the level of clinical experience of the administrator, and at present there are no clear training recommendations or administration considerations in place. Most individuals who administered the interRAI CHA therefore do not have much experience with the assessment of persons living with vision and/or hearing impairment. While conducting a series of studies on sensory-cognitive aging using the interRAI CHA (17, 18), our team realized that our assessor combined a list of rare qualities that make her unique as an administrator of the interRAI tool.
The assessor is a social worker with over 30 years of direct clinical experience in the context of sensory rehabilitation, and has developed and implemented a sensory screening program (13, 20). Her work experience and her professional interactions with sensory rehabilitation professionals allowed her to develop extensive expertise on how to interact and communicate with persons living with different levels of sensory impairment., and how to explore and assess their functional abilities and needs. She participated in a two-day education session on how to administer the assessment based on the information available in the manual produced by interRAI. This included instructions for obtaining information from secondary sources, how to enter the data into the software system and how to interpret information generated by the software (e.g., scores on the health index scales). While the social worker had no prior experience administering the interRAI assessments, she had extensive interviewing skills, clinical experience and knowledge in the field of sensory rehabilitation who, by the end of the data collection period, also may be the first person ever to have administered the interrail CHA and its DbS to 200 older adults with confirmed sensory impairments. These characteristics led the team to consider her a “deviant case,” given her exceptional skill set and professional placement. The idea to synthesize the recommendations presented here did not emerge until after data collection was complete. Therefore, she and the team were unaware of the purpose of the present study, because its idea emerged afterwards.
To be included in this study, participants had to be eligible for sensory rehabilitation services as defined by the Quebec Ministry of Health, with a visual acuity in the better eye with best correction of 20/60 (6/18) or less, or a visual field diameter of <60 degrees, or hemianopsia (loss of half of the visual field); and/or an unassisted pure tone average decibel hearing level (dB HL) in the better ear of 35 dB HL or more (21, 22). Additionally, it was required that participants had an initial evaluation by a sensory rehabilitation center at least 6 months prior to data collection, and had received sensory rehabilitation within the past 3 years. This excluded individuals who had recently undergone extensive intake/initial interviews by their respective rehabilitation centers. Study exclusion criteria included persons unable to communicate in English or French, those unable to communicate verbally, and clients who could not be reached by phone. All study procedures were reviewed and approved by the Centre de recherche interdisciplinaire en réadaptation de Montréal métropolitain (CRIR-1018-1114).
Participants were recruited through the respective programs of three Québec sensory rehabilitation establishments: (1) Lethbridge-Layton-Mackay Rehabilitation Centre (LLM); (2) Institut Nazareth et Louis-Braille (INLB); and (3) Institut Raymond-Dewar (IRD). Included within LLM are persons with visual impairment that participate in the Day Center, 60% of whom have compromised hearing (23). Some participants, who attended an INLB and IRD inter-establishment program (programme surdicécité), were registered in both of those centers. Participants were recruited by staff from each of the three rehabilitation centers. The staff provided eligible participants with information concerning the nature and voluntary participation in the study and gave them an opportunity to ask questions. Upon receipt of their verbal consent, their names were forwarded to this study's assessor (CM), who was responsible for scheduling the interview. After receiving more details about the study protocol, 21 (INLB = 10, IRD = 6, LLM = 5) of the 221 persons who had initially agreed to participate, canceled their participation in the study before data collection began, mentioning reasons related to health issues, as well as limited energy.
The final sample consisted of 200 adults aged 61 and over (61%women, 39% men) with a mean age of 81.3 years. Based on the interRAI CHA and DbS, 35% of the sample had only hearing loss (hard of hearing or HH), 29% had only visual loss (visually impaired or VI), and 37% had DSI. Among participants with VI solely, whose medical records contained visual acuity measurements (N = 120), the best eye's average distance visual acuity in logMAR was 0.9. Among participants that were solely HH, whose medical records included hearing loss measurements (N = 93), the best ear's average hearing was 59 dB HL. Additional details about the sensory and cognitive profiles of these participants has been presented elsewhere (17, 18). Please note that the process of telephone recruitment prohibited us from recruiting individuals who primarily communicated using sign language, or those whose hearing loss was too profound for verbal communication. Even though complete blindness was not an exclusion criteria, none of the recruited participants utilized braille for print access. Of the participants who were assessed with the Montreal Cognitive Assessment (MoCA; see “Measures” for a detailed description), most passed this test (56% of N = 198), indicating they were not at risk for mild cognitive impairment (24). Of the two participants that were not assessed with the MoCA, one died before the scheduled appointment and, in the other case, it was not administered because the assessor felt that the test would have caused the participant undue psychological stress.
The roughly 150 items in the interRAI CHA capture basic demographic information about the person and detailed information across 13 domains, including abilities in activities of daily living (e.g., bathing, dressing, grooming), instrumental activities of daily living (e.g., using the telephone, managing finances), cognition, social functioning, mental health, pain, hearing, and vision. Once the CHA is completed electronically, a series of health index scales can be automatically generated. For example, the Deafblind Severity Index is based on two items within the CHA which measure functional vision and hearing. The Deafblind Severity Index ranges from 0 (no impairment in either sense) to 5 (severe impairment in both senses); a score of 3+ identifies individuals with any level of DSI (12). If an individual scores three or higher on the CHA, it is recommended that the assessor complete the DbS. This supplemental assessment includes ~150 items to gather further information across 11 domains considered relevant for the assessment of individuals with DSI, including vision and hearing (e.g., age of onset of vision/hearing loss, diagnoses, visual acuity and field diameter, alerting to sounds, devices used), communication (e.g., communication modes used, ability to communicate with family members), mood and behavior, level and type of informal support from friends/family, psychosocial well-being, and orientation and mobility/O&M (e.g., ability to move about in both familiar and unfamiliar environments). Based on previously published information (12), Table 1 provides an overview of the content captured within the interRAI CHA and DbS. All of the responses to items within the interRAI CHA and DbS are closed-ended; most are scored as yes/no, others are scored on an ordinal scale (typically 0–5, but sometimes up to 8). The typical time frame for assessment is the previous 3 days; a few items ask about the past 90 days[10].
The interRAI CHA and DbS is a copyrighted tool. Further information is available in the assessment's manual [10], which is available for purchase from interRAI (http://www.interrai.org/instruments/).
The assessor secured participants' written consent and provided them with a description and basic guidelines concerning the assessment process that included the topics to be covered, the interview format, and the respondents' ability to ask clarifying questions and take breaks. Participants chose the location where the interview was conducted. Most participants (61%) chose their homes, the remaining participants preferred an office appointment at their respective rehabilitation center (LLM = 38.5%, IRD = 0.5%). At the interview, participants were asked if they understood or had questions before proceeding. To meet the participant's individualized needs, the assessor used effective communication strategies, in surroundings suitable for clear two-way communication (25).
In scoring the assessment items, the assessor considered both the participants' answers and information from participants' medical records. Study team members had access to participants' files from their respective rehabilitation centers. From the files, demographic (e.g., sex, age) and health information (e.g., vision and/or hearing diagnoses) was obtained. Assessment responses were entered into a software system, using unique identifiers to ensure confidentiality. Interviews lasted ~90 min, and were conducted in the participant's service language, either English or French. To facilitate communication, a personal amplification device (Pocket Talker®, WilliamsAV, Eden Prairie, MN, USA), was made available to participants who required an assistive listening device. Similarly, a large-print version of the consent form was available, as needed. As part of her process as a rehabilitation professional, the assessor took detailed case notes on the administration of each assessment.
To obtain additional information about participants' cognitive status, the MoCA, a 10-min cognitive screening tool for identifying individuals as risk for mild cognitive impairment, was completed. Cognitive screening of participants was included in the protocol because the data contributed to a larger overall protocol on sensory-cognitive aging (17, 18). Mild Cognitive Impairment is a clinical diagnosis characterized by cognitive decline that goes beyond normal cognitive aging and in many cases leads to dementia (24). The tasks included in the MoCA assess attention, concentration, working memory, short-term memory, visuospatial abilities, executive functions, language, and orientation to time and place [see Nasreddine et al. (24) for further detail]. The original version of the MoCA (hereafter “full” MoCA) was developed for and validated in adults without sensory impairment (24). A version for persons with VI (hereafter “blind” MoCA) was created by eliminating the first 3 items of the scale that require vision (i.e., viewing, copying and, creating drawings) and adjusting the cut-off scores accordingly. Compared to the full MoCA, the blind version has higher specificity for detecting healthy participants and lower sensitivity for detecting those with Mild Cognitive Impairment (26).
Participants who had sufficient vision, based on self-report and/or the assessor's clinical opinion, completed the full MoCA; those with VI completed the blind MoCA. The MoCA was typically administered during the interview when the interRAI CHA and DbS were completed, with the exception of 5 participants who completed the MoCA at a second session.
Given the unique professional experience of the assessor and her unusual experience of administering 200 interRAI CHA assessments to individuals with objectively confirmed sensory impairment, we explored different analytical approaches in order to frame our analyses. We were inspired by deviant case analysis (27), even though originally this approach was intended to explore whether an existing theory can explain extreme observations or whether a theory needs to be expanded (28). Here, we treat the skill set of our expert assessor as unique or extreme, given her rare combination of abilities and experiences. We therefore decided to explore her perspective on the administration of the interRAI CHA and its DbS with the goal of expanding the training guidelines for assessment administrators that have less experience and/or exposure to individuals with sensory impairments.
Based on the available detailed case notes, the assessor reflected on her experience conducting the interRAI CHA and DbS interviews with the goal of generating recommendations relevant to future assessors completing the instrument, and suggestions for edits to the instruments and manual. She then engaged in dialogue with the team members about these experiences, where by all team members brought their expertise on sensory impairment, assessment administration and the interRAI measures into the discussion. As a team, we developed the content of the tables in this manuscript, using a reflective and iterative process. Within the CHA, this process focused on the section “Communication and Vision” because two of its items are used to calculate the Deafblind Severity Index which in turn triggers the DbS. Within the DbS, we focused on three sections that included items related to vision and hearing, communication, and orientation and mobility (O&M). These domains were chosen because they provide information that is the most specific to people with DSI. Communication, either expressive or receptive, relies on hearing of speech and seeing of facial gestures and body movements and creates significant difficulty for individuals with DSI. O&M refers to strategies and devices that are designed for people with visual and/or hearing loss. As part of the synthesis and team discussion process, the assessor also consulted with other professionals in her program that work with the participants in this study with DSI, specifically a low vision optometrist, an audiologist, and an O&M specialist. These professionals provided feedback on the instrument's questions, and the assessor's suggestions to facilitate the its administration. After this process, the initial list of suggestions was finalized by the team members. Because the qualitative analysis did not reveal any suggestions that differed depending on the study participant's sex, and the lack of evidence indicating that the use of the interRAI CHA and DbS are influenced by a respondent's sex, no sex-based analyses were conducted.
Overall, the qualitative evaluation of the utility of the interRAI CHA and DbS generated suggestions that stress how vision and hearing include several abilities, all of which are worth exploring when assessing a person's visual and hearing functioning. If the assessor focuses on only one sensory ability, for instance only near vision but not at a distance, s/he will have an incomplete view of the respondent's sensory capacities or miss a sensory impairment altogether. Suggestions also chiefly highlight the fact that a person's specific sensory function can be more or less impaired depending on contextual factors that may not be present during the interview; for instance, hearing speech in a quiet vs. a noisy environment. Determining a respondent's sensory performance must include observations of the person's behavior but also the context of the observation, and will benefit from gaining information about the respondent's performance in a variety of settings. Lastly, this study brings attention to specific information on sensory impairment/rehabilitation that will aid assessors in the administration of the assessment, particularly those naïve to the field of sensory loss.
An overview of the suggestions is presented below. Then in Tables 2–5, each specific suggestion for the assessor is listed, in connection to its corresponding question in the assessment instrument. Please note that these suggestions are based on the exper assessor's own experience when administering the interRAI CHA and its deafblind supplement, or specifically address potential concerns she would anticipate with less experienced administrators that are unfamiliar with individuals living with sensory impairment.
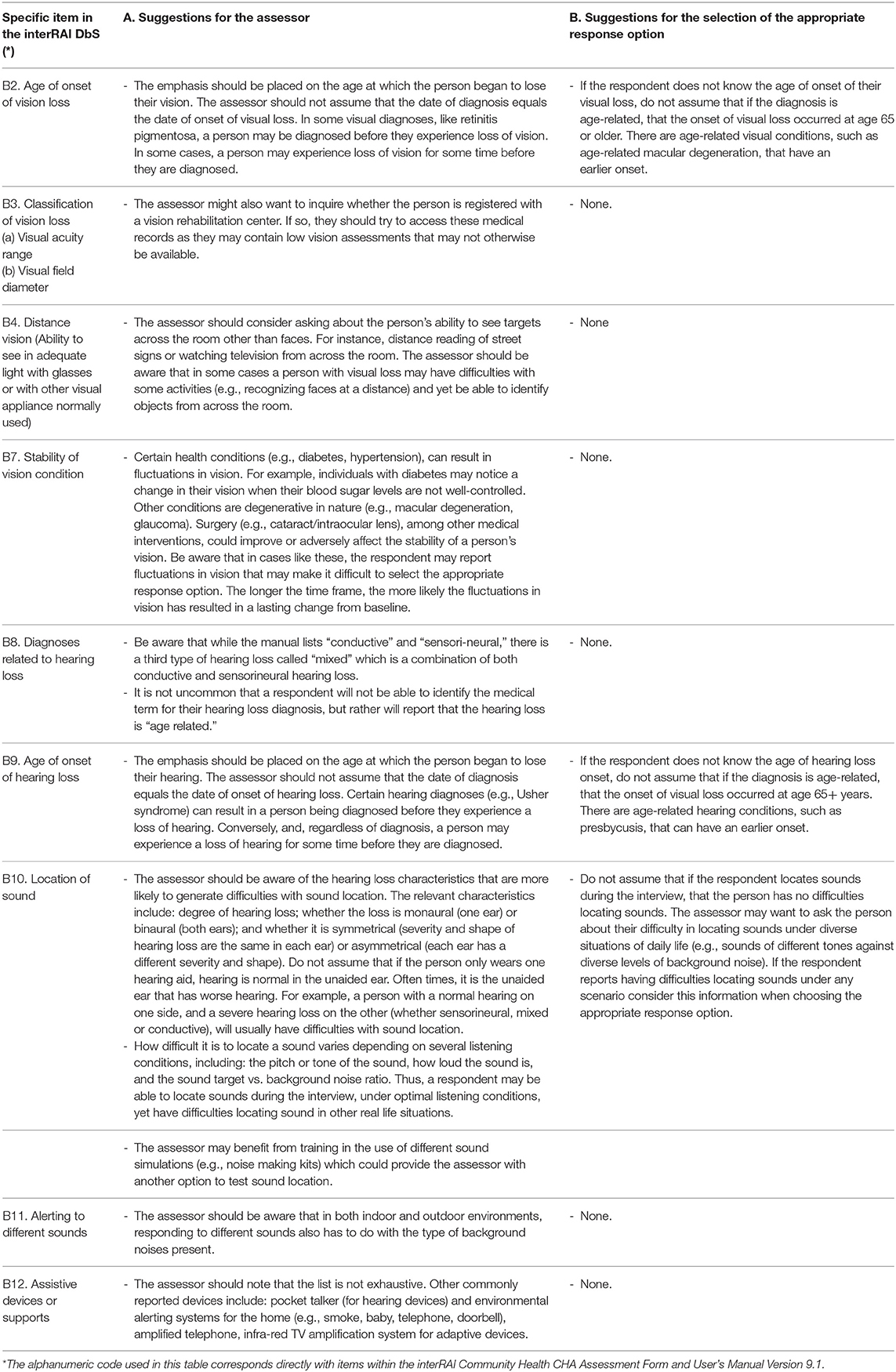
Table 3. Supplemental guidelines for completing section B (Vision and Hearing) within the Deafblind Supplement (DbS).
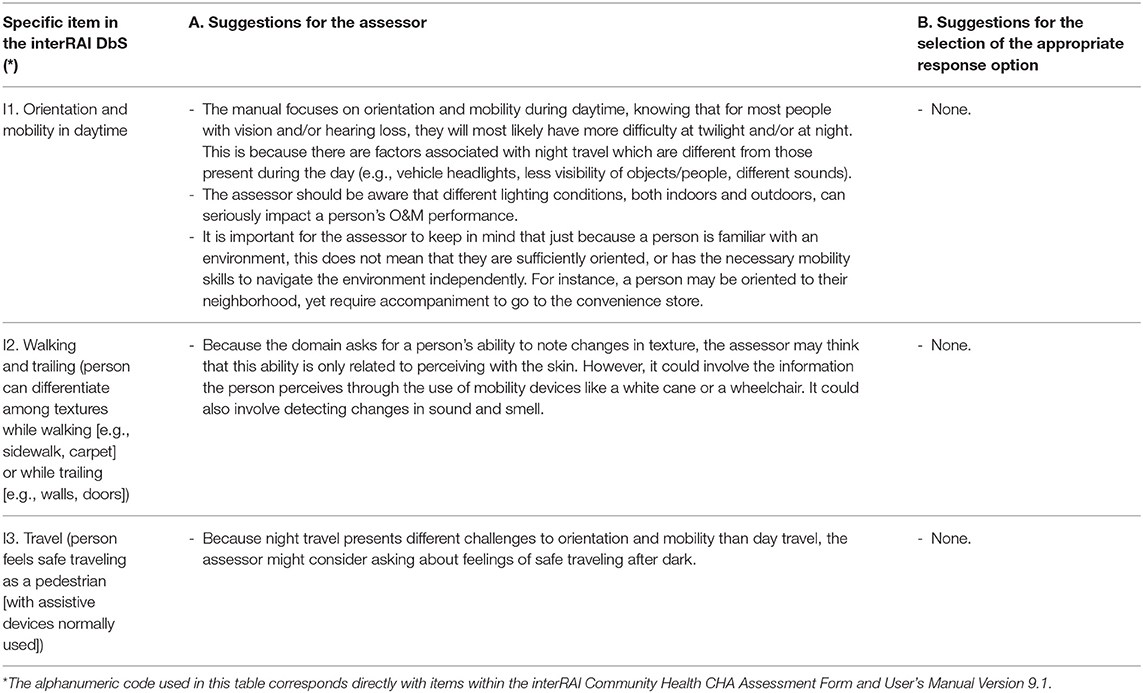
Table 5. Supplemental guidelines for completing interRAI DbS section I Orientation and Mobility (O&M).
It is recommended that assessors ask the client about multiple aspects of sensory loss which can help the assessor gain a more comprehensive understanding of the client's sensory status. More specifically, the CHA question regarding vision asks specifically about near vision. It is suggested that the assessor also inquire about the client's ability to see objects at a distance. Likewise, the CHA question for hearing focuses primarily on hearing speech. It is recommended that the assessor also ask about the client's ability to hear other sources of sound, such as processing concurrent multiple environmental sounds. The information generated from these additional questions can be added to the assessor's own clinical notes and contribute to their development of a service plan. Similarly, regarding the questions on vision and hearing within the DbS, assessors are encouraged to ask clients about additional aspects of their sensory loss. For example, the vision item on the DbS refers to the client's ability to see a face and/or object from across the room. We propose to also ask the client about other visual tasks, such as distance reading of street signs. Regarding the DbS question on hearing, we encourage the assessor to ask about the impact on the client's hearing ability of the sound's characteristics (e.g., pitch, volume), and levels of background noise.
Assessor should not assume that if the client locates sounds during the interview that the person has no difficulty locating sounds. It is advisable to explore the client's ability in locating sounds under diverse situations of daily life (e.g., sounds of different tones against diverse levels of background noise), and to consider this information when choosing the appropriate response option.
Some suggestions stress how important it is to keep in mind that the client's hearing behavior during the interview is likely an incomplete picture of their overall hearing abilities. This is particularly true if the interview is carried out under optimal hearing conditions (e.g., in a quiet office room without competing noises, with an assessor that speaks slowly and provides non-verbal cues), which might mask the hearing problem a client would have in common daily life environments. As another example, Table 3 includes information about the typical age of onset of vision and hearing conditions and cautions that the assessor not make assumptions about the age of onset since some “age-related” conditions can have an “early” onset and thus do not necessarily entail an onset in late adulthood.
All specific suggestions are presented in the tables below. Note that each table is structured in the following way: Each row corresponds to the relevant question in the interRAI CHA and DbS. Column A “Suggestions for the Assessor” provides overall considerations for the assessor with the goal of supplementing the instructions in the interRAI user's manual. For example, this includes recommendations for performing the interview, with respect to its setting and questions, with the goal of obtaining the most comprehensive response to the item. This column also presents information specific to sensory loss that will help the assessor conduct the interview. Column B “Suggestions for Coding” includes considerations for how to choose a response in instances when definitions for the response options for the particular item would benefit from further elaboration, as well as information to clarify codes when their definitions could lead to misinterpretation. These recommendations were developed with the purpose of aiding assessors in administering the instrument to a group of older adults with sensory loss. Although we believe these suggestions will help assessors to gather information in an optimal way, the recommendations are ours alone and do not replace or change in any way the instructions and guidelines outlined within the interRAI CHA and DbS manual.
To our knowledge, this is the first study that provides specific recommendations for assessors when administering the interRAI CHA and DbS, the only existing measure validated and designed for use with adults that are living with combined vison and hearing loss. Our findings are particularly relevant given the complexities of assessing older adults with DSI since the combined sensory loss can have a profound influence on the person's ability to communicate with the assessor.
The supplemental guidelines we propose, used in tandem with the wealth of information, definitions and procedural instructions contained in the interRAI CHA user's manual, we hope will assist assessors to better understand sensory impairment and its importance in the assessment process. By following the proposed suggestions, we anticipate that assessors will deepen their knowledge on vision and hearing loss; more comprehensively understand the assessment's questions and response options; and optimize the completion of the assessment.
Included in Tables 2–5 are suggestions of topics to include in the training of future interRAI CHA and DbS assessors. Beyond these specific suggestions, we think that training would benefit overall from including trainers who have had exposure to sensory impairment information and thus can teach communication and assessment strategies tailored to clients with single or combined vision and hearing loss. We recognize that this recommendation is an ideal scenario that may not be feasible given clinical autonomy, time and resources, and hope that this study's suggestions can at least help future assessors gain some additional information on sensory loss, and trigger their curiosity for learning more about these topics.
Our recommendations are supported by several study strengths. Our sample is representative of older adults who are receiving sensory loss rehabilitation services at no cost to the client in an urban environment, in that participants were recruited from all three of Montreal's sensory rehabilitation centers (7). This study's assessor had significant clinical experience with adults that have VI, HH, or DSI, yet was novel to the interRAI CHA and DbS. This allowed for a qualitative evaluation of the utility of the assessment that could detect areas where additional information about sensory loss could help future assessor's administration of the instrument, as well as difficulties a novel assessor may encounter when first using the assessment.
This study also needs to be viewed and interpreted within certain limitations. All participants were receiving rehabilitation treatment for sensory loss, and thus, to varying degrees, had successfully navigated the health system to access these services. They were also reconciled with the loss of their vision/hearing and had acquired sensory compensation strategies and aids/devices. Additionally, participating in the study required several skills, such as: communicating verbally by phone, having the stamina for answering about 300 questions followed by a cognitive test. Thus, our findings may only apply to the most highly functioning older adults with VI, HH or DSI. Also, since most participants had acquired sensory impairment, our results may not apply to older persons with more severe or congenital sensory loss. Future studies should include recruitment and communication techniques that can reach older adults with all levels of sensory loss severity, and with a larger spread across the impairment spectrum (29). While the assessor's professional experience served to facilitate the qualitative evaluation of the assessment, it may have also minimized the level of difficulty involved in use of the instrument, particularly by those who are new assessors or have no disability-specific knowledge. For instance, whereas assessors in a previous study (14) had challenges with addressing items on mood and psychological well-being, the present study's assessor, who was an experienced social worker, did not experience these type of difficulties. Lastly, this study's results are limited since they are based on the experience of a single assessor, albeit one with extensive experience working with the population studied and who had some input from other professionals knowledgeable about sensory loss. Our results therefore need to be considered as an expert's opinion whom we methodological considered to be a “deviant case” (28).
This study reports concrete recommendations aimed to optimize the administration of the interRAI CHA and DbS, the only standardized interview instrument for adults that helps first-line health care providers to identify the needs, strengths and challenges for someone with DSI. Recommendations include additional questions that assessors can ask about a respondent's functional abilities, and information on sensory impairment and rehabilitation that will deepen assessors' understanding of vision and hearing loss. Together, these recommendations will help assessors more comprehensively understand the assessment's questions and response options, thereby allowing them to optimize the assessment process. In addition, we believe that that improved administration of the interRAI CHA and its DbS will be definition lead to more appropriate intervention and care. These findings are relevant given the increasing prevalence of DSI in the world's aging population. The detection and evaluation of DSI is of utmost importance because several aspects of health care delivery, and communication with health professionals, depend on it. The approach presented in this study will increase the awareness of sensory loss in older adults and its importance in assessment by first-line service providers.
The data utilized in this project cannot be made publicly available since data protection rules in Canada preclude them from being shared at the record level. The data were collected through a data sharing agreement with interRAI, the holder of the copyright to the CHA and Deafblind Supplement, and restrictions apply to the availability of these data. Requests to access the datasets should be directed to https://www.cihi.ca/en/data-inquiry-form.
The studies involving human participants were reviewed and approved by Centre de recherche interdisciplinaire en réadaptation de Montréal métropolitain (CRIR-1018-1114). The patients/participants provided their written informed consent to participate in this study.
AU contributed to formal analysis, investigation, methodology, validation, writing-original draft, and writing-review and editing. CM contributed to data curation, formal analysis, investigation, methodology, resources, writing-original draft, and writing-review and editing. DG contributed to conceptualization, data curation, funding acquisition, investigation, project administration, resources, supervision, validation, and writing-review and editing. WW contributed to conceptualization, data curation, funding acquisition, investigation, methodology, project administration, resources, supervision, validation, and writing-review and editing. All authors agree to be accountable for the content of the work included in this study.
This study was funded by the Canadian Consortium on Neurodegeneration and Aging (CCNA; http://ccna-ccnv.ca/en). The CCNA was supported by a grant from the Canadian Institutes of Health Research (Grant no. CNA-137794) (CIHR; http://www.cihr-irsc.gc.ca/e/193.html) with funding from several partners. Funding was also provided by the Foundation of the CRIR/Centre de réadaptation Lethbridge-Layton-Mackay du CIUSSS du Centre-Ouest-de-l'Île-de-Montréal, and the Fondation En Vue of the CRIR/Institut Nazareth et Louis-Braille du CISSS de la Montérégie-Centre. WW was supported by a Junior 2 FRQS chercheur boursier career award (#281454).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The authors gratefully acknowledge the contribution of the study participants and participating organizations, CRIR/Centre de réadaptation Lethbridge-Layton-Mackay du CIUSSS du Centre-Ouest-de-l'Île-de-Montréal, CRIR/Institut Nazareth et Louis-Braille du CISSS de la Montérégie-Centre and CRIR/Institut Raymond-Dewar of the CIUSSS du Centre-Sud-de-l'Île-de-Montréal, along with Martine Gendron. We also acknowledge the contributions of Manon Pilon, Audiologist, Marie-Noëlle Labrie, O&M Specialist, and Dr. Stéfanie Parenteau, Optometrist, whose reviews of the manuscript were invaluable. Also appreciated was the attention to detail given by research assistants, Alexandre Beaulieu and Jonathan Jarry.
1. Viljanen A, Törmäkangas T, Vestergaard S, Andersen-Ranberg K. Dual sensory loss and social participation in older Europeans. Eur J Ageing. (2014) 11:155–67. doi: 10.1007/s10433-013-0291-7
2. Munroe S. Developing a National Volunteer Registry of Persons With Deafblindness in Canada: Results From the Study 1999-2001. (2001). Available online at: http://www.cdbc-csac.ca/#projects (accessed November 28, 2021).
3. Roets-Merken LM, Zuidema SU, Vernooij-Dassen MJFJ, Kempen GIJM. Screening for hearing, visual and dual sensory impairment in older adults using behavioural cues: a validation study. Int J Nurs Stud. (2014) 51:1434–40. doi: 10.1016/j.ijnurstu.2014.02.006
4. Cimarolli VR, Jopp DS. Sensory impairments and their associations with functional disability in a sample of the oldest-old. Qual. Life Res. (2014) 23:1977–84. doi: 10.1007/s11136-014-0657-0
5. Christensen K, Doblhammer G, Rau R, Vaupel JW. Ageing populations: the challenges ahead. Lancet. (2009) 374:1196–208. doi: 10.1016/S0140-6736(09)61460-4
6. Heine C, Browning C. Dual sensory loss in older adults: a systematic review. Gerontol. (2015) 55:gnv074. doi: 10.1093/geront/gnv074
7. Wittich W, Watanabe DH, Gagné JP. Sensory and demographic characteristics of deafblindness rehabilitation clients in Montreal, Canada. Ophthalmic Physiol Opt. (2012) 32:242–51. doi: 10.1111/j.1475-1313.2012.00897.x
8. Canadian Institutes for Health Information. Health Care in Canada 2011: A Focus on Seniors and Aging. Ottawa, ON: Canadian Institutes for Health Information (2011).
9. Hirdes J, Dalby D, Curtin-Telegdi N, Poss J, Stolee P, Strong G, et al. interRAI Deafblind Supplement to CHA: Guide for Use of the interRAI Deafblind Supplement Assessment Form (Canadian Version 9). Washington, DC: interRAI (2007).
10. Morris J, Berg K, Bjorkgren M, Declercq A, Finne-Soveri H, Fries B, et al. interRAI Community Health (CHA) Assessment Form and User's Manual. Version 9.1 (Canadian Edition edition). Washington, DC (2010).
11. Hirdes J, Ljunggren G, Morris JN, Frijters DHM, Finne Soveri H, Gray L, et al. Reliability of the interRAI suite of assessment instruments: a 12-country study of an integrated health information system. BMC Health Serv Res. (2008) 8:277. doi: 10.1186/1472-6963-8-277
12. Dalby DM, Hirdes J, Stolee P, Strong JG, Poss J, Tjam EY, et al. Development and psychometric properties of a standardized assessment for adults who are deaf-blind. J Vis Impair Blind. (2009) 103:7–16. doi: 10.1177/0145482X0910300103
13. Déry L, McGraw C, Wittich W. Le repérage des incapacités visuelles: un moyen de prévenir les chutes chez les aînés. In: Wanet-Defalque M-C, Overbury O, Temisjian K, editors. Actes du 13e Symposium scientifique sur l'incapacité visuelle et la réadaptation ≪ Innover pour mieux intervenir ≫. Montréal, QC: INLB et Université de Montréal (2011).
14. Guthrie DM, Pitman R, Stolee P, Strong G, Poss J, Tjam EY, et al. Reliability of standardized assessment for adults who are deafblind. J Rehabil Res Dev. (2011) 48:545–54. doi: 10.1682/JRRD.2010.09.0175
15. Schneider JM, Dunsmore M, McMahon CM, Gopinath B, Kifley A, Mitchell P, et al. (2014). Improving access to hearing services for people with low vision: Piloting a “hearing screening and education model” of intervention. Ear Hear. 35:e153–61. doi: 10.1097/AUD.0000000000000038
16. Schneider JM, McMahon CCM, Gopinath B, Kifley A, Barton R, Mitchell P, et al. Dual sensory impairment and hearing aid use among clients attending low-vision services in australia: the vision-hearing project. J Aging Health. (2014) 26:231–49. doi: 10.1177/0898264313513610
17. Urqueta Alfaro A, Guthrie DM, McGraw C, Wittich W. Older adults with dual sensory loss in rehabilitation show high functioning and may fare better than those with single sensory loss. PLoS ONE. (2020) 15:e0237152. doi: 10.1371/journal.pone.0237152
18. Urqueta Alfaro A, Guthrie DM, Phillips NA, Kathleen Pichora-Fuller M, Mick P, McGraw C, et al. Detection of vision and/or hearing loss using the interRAI Community Health Assessment aligns well with common behavioral vision/hearing measurements. PLoS ONE. (2019) 14:e0223123. doi: 10.1371/journal.pone.0223123
19. interRAI Instrument and Systems Development Committee (2006). InterRai Community Health (CHA) Assessment Form and User's Manual and Related Materials : Version 9.1.4. Boston, MA: interRAI Instrument and Systems Development Committee.
20. McGraw C, Dery L, Wittich W. Falls prevention through the Visual Impairment Detection Program. Insight: Research and Practice in Visual Impairment and Blindness. (2011) 4:74–82. Available online at: https://aerbvi.org/wp-content/uploads/2016/01/insight-04-02-complete_Spring-2011.pdf
21. Regie de l'assurance maladie du Quebec/RAMQ,. Services covered in Quebec–Hearing devices. (2006). Available online at: https://www.ramq.gouv.qc.ca/en/citizens/aid-programs/hearing-aids (accessed November 28, 2021).
22. Regie de l'assurance maladie du Quebec/RAMQ. Services covered in Quebec–Visual devices. (2006). Available online at: https://www.ramq.gouv.qc.ca/en/citizens/aid-programs/visual-aids (accessed November 28, 2021).
23. Wittich W, Murphy C, Mulrooney D. An adapted adult day centre for older adults with sensory impairment. Br J Vis Impair. (2014) 32:249–62. doi: 10.1177/0264619614540162
24. Nasreddine ZS, Phillips NA, Bedirian V, Charbonneau S, Whitehead V, Collin I, et al. (2005). The Montreal cognitive assessment, MoCA : a brief screening. J Am Geriatr Soc. 53:695–9. doi: 10.1111/j.1532-5415.2005.53221.x
25. Tye-Murray N. Foundations of Aural Rehabilitation. Children, Adults and Their Family Members. 4th ed. Stamford, CT: Cengage Learning (2015).
26. Wittich W, Phillips N, Nasreddine ZS, Chertkow H. Sensitivity and specificity of the montreal cognitive assessment modified for individuals who are visually impaired. J Vis Impair Blind. (2010) 104:360–8. doi: 10.1177/0145482X1010400606
27. Patton MQ. Designing qualitative studies. In Patton MQ, editor. Qualitative Research and Evaluation Methods, 3rd ed. Thousand Oaks, CA: Sage Publications, Inc (2002). p. 209–58.
28. Booth A, Carroll C, Ilott I, Low LL, Cooper K. Desperately seeking dissonance: identifying the disconfirming case in qualitative evidence synthesis. Qual Health Res. (2013) 23:126–41. doi: 10.1177/1049732312466295
Keywords: deafblindness, hearing loss, vision loss, low vision, hard of hearing, dual sensory impairment (DSI), screening, interRAI
Citation: Urqueta Alfaro A, McGraw C, Guthrie DM and Wittich W (2021) Optimizing Evaluation of Older Adults With Vision and/or Hearing Loss Using the interRAI Community Health Assessment and Deafblind Supplement. Front. Rehabilit. Sci. 2:764022. doi: 10.3389/fresc.2021.764022
Received: 24 August 2021; Accepted: 19 November 2021;
Published: 13 December 2021.
Edited by:
Behdin Nowrouzi-Kia, University of Toronto, CanadaReviewed by:
Amy T. Parker, Portland State University, United StatesCopyright © 2021 Urqueta Alfaro, McGraw, Guthrie and Wittich. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Walter Wittich, d2FsdGVyLndpdHRpY2hAdW1vbnRyZWFsLmNh
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.