
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Rehabil. Sci., 16 August 2021
Sec. Human Functioning Sciences
Volume 2 - 2021 | https://doi.org/10.3389/fresc.2021.709682
This article is part of the Research TopicICF-Based Assessment and Documentation of Functioning and DisabilityView all 10 articles
Background: The International Classification of Functioning, Disability and Health (ICF) classification is a biopsychosocial frame of reference that contributes to a holistic understanding of the functioning of a client and the factors involved. Personal factors (PFs) are not currently classified in the ICF due to large societal and cultural diversity and lack of clarity in the scope of such factors.
Aims: To ascertain which factors in the ICF classification have been defined as PFs in different studies and what conclusions have been drawn on their role in the ICF classification.
Methods: The study was a scoping review. A systematic search for articles published in 2010–2020 was performed on the Cinahl, Pubmed, ScienceDirect, and Sport Discus databases. The PFs specified in the articles were classified according to the seven categories proposed by Geyh et al. socio-demographic factors; position in the immediate social and physical context; personal history and biography; feelings; thoughts and beliefs; motives; and general patterns of experience and behavior.
Results: The search yielded 1,988 studies, of which 226 met the inclusion criteria. The studies had addressed a wide variety of PFs that were linked to all seven categories defined by Geyh et al. Some studies had also defined PFs that were linkable to other components of the ICF or that did not describe functioning. Approximately 22% (51) of the studies discussed the role of PFs in rehabilitation.
Conclusions: The range of PFs in the ICF classification addressed in the reviewed studies is wide. PFs play an important role in rehabilitation. However, according to the reviewed studies, a more precise coding of PFs is not yet warranted.
Over the past 20 years, the International Classification of Functioning, Disability, and Health (ICF) has become a generally accepted biopsychosocial framework for rehabilitation (1). Through the provision of uniform concepts and a commonly shared frame of reference, the ICF classification has changed the practices and the statistics used to assess functioning and disability (2). However, the utilization of the ICF still needs to be further developed in the Nordic countries (3). In the ongoing rehabilitation reform led by the Finnish Ministry of Social Affairs and Health, the ICF classification is seen as a framework for establishing uniform practices in the assessment and documentation of functioning (4).
Enabling sufficient functioning is a complex process, as it comprises multiple interacting components that must be tailored to individual needs and situations (5). The Nordic countries appear to have a common conceptual understanding of client-centered practice (6), which is supported by applying the bio-psycho-social framework of the ICF in the complex processes of rehabilitation (7).
The ICF contains a broad range of categories for describing body functions and structures and activities and participation. In addition, environmental factors, which is one component of the contextual factors, can be defined as a barrier or a facilitator for functioning. However, the other component of contextual factors, personal factors (PFs), which are defined as the background information about the life and lifestyle of an individual, have not been classified (1). PFs include the resources, means of coping, education, and behavioral patterns of an individual. Identifying these functioning-related factors helps to understand how one's clients are, how they think, how they evaluate and understand their own situation, what they hope for, and how they cope in their daily lives. PFs and their interpretation influence the choice of rehabilitation services and measures, as well as other forms of support (8). Hence, the key question is how to identify and take into account the diverse PFs that affect the functioning of an individual in the same way as other factors included in the ICF classification.
It has been suggested that full utilization of the ICF classification is hindered by the fact that PFs are not categorized in the same way as their other components (9). Given the absence of a formal categorization of PFs in the ICF, studies have used various other categorizations. For example, in their review, Muller & Geyh (10) compared the background and content of eight different classifications. These classifications included, in varying degrees, the following 12 areas: socio-demographic factors, behavioral and lifestyle factors, cognitive psychological factors, social relationships, experiences and biography, coping, emotional factors, satisfaction, other health conditions, biological/physiological factors, personality, and motives/motivation. On the other hand, the use of a more precise classification of PFs has also been criticized. Leonardi et al. (11) suggested that PFs such as gender, age, or education may have implications for the disability of a person and are therefore important in understanding functioning. However, they did not favor a more precise classification of PFs, as this could lead to “blaming” clients for their functional limitations. Simeonsson et al. (12) proposed that before constructing a taxonomy of codes for PFs, one should critically assess the need for PFs as a separate component in the ICF classification. These conflicting views suggest that there is a need to systematically examine how PFs are defined and manifested in rehabilitation studies.
The role of PFs in the ICF classification is also linked to the ongoing discussion on the need for a full reconsideration of the ICF classification framework. An alternative ICF model in which medical health status is incorporated in PFs has been proposed (13). Moreover, Mitra and Shakespeare (14) proposed a visual scheme of the model in which environmental and personal factors are located at the top of the model, thereby emphasizing their importance. They also highlighted the importance of well-being, quality of life, and individual experience of agency when re-designing the ICF model. The need to review the ICF model is also shared by Sykes et al. (15), who suggested that any such process should be based on research evidence and, importantly, include people with disabilities. This ongoing discussion on if, and if so how, PFs should be included in the ICF indicates a need to systematically identify, analyze, and summarize how PFs have, to date, been studied in the field of rehabilitation.
In 2011, Geyh et al. (16) presented an overview of conceptualizations of the PFs component of the ICF. The review comprises 79 articles in which more than 200 concepts in total were labeled as PFs. Examples of the most significant of these include self-efficacy, attitudes, expectations, motivation, personality traits, and life goals. PFs were described in the articles as affecting disability and health and as having a significant role in the assessment of functioning and rehabilitation and in research and social security settings. The authors concluded that the PFs need to be standardized (16). In 2019, Geyh et al. (8) presented a classification of PFs. In this scoping review, we systematically collected research articles published after Geyh et al.'s work in (2011) (16) and applied the classification by Geyh et al. (8) in our analysis.
In 2017, the Finnish Rehabilitation Reform Committee submitted proposals for reforming Finland's rehabilitation services. Based on those proposals, the rehabilitation services reform was planned to take place between 2020 and 2022 as part of both a wider national reform program and as separate legislative projects. One important development area concerns the use of the ICF framework in organizing and producing rehabilitation services that meet the individual needs of the clients (4). The present review contributes to this reform work and aims, in particular, to provide a basis for determining the role of PFs in harmonizing monitoring systems and indicators of functioning. This review assembles research data and views on the need for the assessment of PFs and the possible need for a more precise classification as part of a comprehensive assessment of functioning. Our purpose was twofold: first, to summarize the PFs that have been investigated in research articles, irrespective of the study design, and second, to describe the reflections of the authors on the issue of PFs.
This study followed the scoping review methodological framework (17, 18). This method was appropriate, given the present objective of mapping the evidence on PFs. Literature searches were conducted by an expert information specialist in consultation with the research team. The search was undertaken in the following electronic databases: Cinahl, PubMed, ScienceDirect, and Sport Discus, and all potentially relevant studies published from 2010 to 2020 were extracted. The search terms were as follows: (ICF[Title/Abstract] OR “International Classification of Functioning”[Title/Abstract]) AND (personal[Title/Abstract] OR context*[Title/Abstract]). All study designs were eligible, whether qualitative, quantitative, or mixed methods. Methodology or guideline reports were also searched.
Throughout the selection process, the eligibility of studies was determined by applying established criteria: an article was included for the assessment of relevancy if it addressed one or more PFs in the context of ICF and excluded if it made no mention of PFs. Data selection was performed independently by two researchers. In addition, all members of the research team participated in the consensus discussions, in which the data selection protocol and choices were refined based on the inclusion and exclusion criteria. In the first step, the titles and abstracts were screened by two researchers.
The relevance of the full-text articles in relation to the research questions was then determined using the classification by Goodman et al. (19) (Table 1). Two researchers screened whether the article addressed one or more of the factors defined in the article as an ICF PF. Thereafter, articles were rated for relevance on a scale of one to six (1 = low relevance; 6 = high relevance). After the relevance ratings, only articles rated 5 and 6 were included in the further analysis.
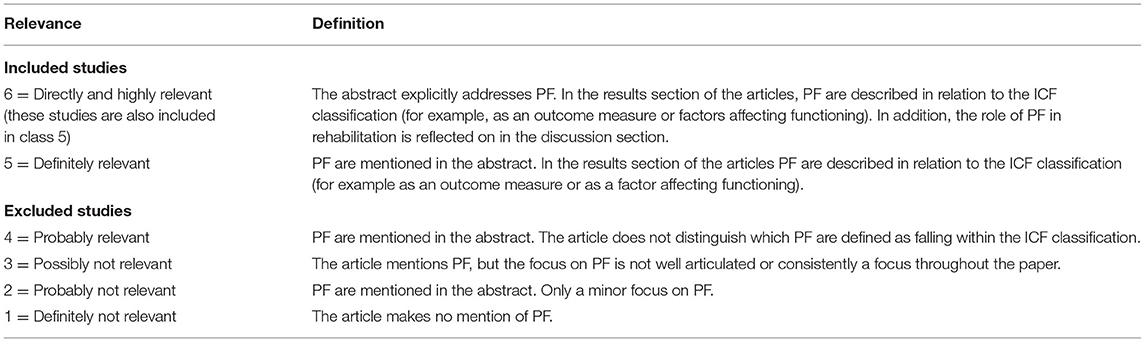
Table 1. Relevance scale of the publication, adapted from Goodman et al. (19).
Data extraction and analysis were conducted in two separate phases. The first phase of the data analysis included studies that reached level 5. Data on PFs were extracted, categorized according to the classification by Geyh et al. (8), and entered into a chart. The relevant descriptive characteristics of the studies (e.g., frequencies of methods used and study populations) were gathered and analyzed (see Tables 2, 3).
In the second phase, all the studies at level 5 that reached level 6 were extracted (see Table 1), and subjected to qualitative thematic analysis. All these studies included reflections on the role of PFs in rehabilitation. These reflections were subjected to a qualitative thematic analysis. The thematic analysis was implemented using a mind-mapping process in which the researchers analyzed qualitative themes identified in the reflections. Team members met frequently to compare mind maps and further consider their interpretations of the thematic categories and produce a thematic map of the findings. Thematic analysis was used to broaden knowledge on the role of PFs in rehabilitation research.
A total of 226 definitely relevant (level 5) research articles were included in the analysis. Of these, 51 articles were classified as direct and highly relevant (level 6), as the authors had reflected in the discussion section on the role of PFs in rehabilitation (Figure 1).
The research designs of the included articles ranged from quantitative, qualitative, and mixed methods to conceptual/theoretical (Table 2). The target groups of the articles were also heterogeneous, comprising different client groups and professionals (Table 3).
The 226 articles addressed a wide variety of PFs. The PFs mentioned in articles, along with references to the articles in question, and factors included in the ICF as part of a component other than PFs or that do not describe functioning, are presented in Supplementary Table 1. The factors were linked to all seven of the categories defined by Geyh et al. (8). Of these articles, 154 articles (68%) addressed PFs that were linked to General patterns of experience and behavior (category 7). PFs related to Socio-demographic factors, most commonly gender and education (category 1) were addressed in 145 articles (64%), and factors related to Thoughts and beliefs (category 5), such as self-expectations and interest in various issues, in 106 articles (47%). PFs were also linked to the other four categories. PFs linked to Motives (category 6) were addressed the least, in only 25 articles (11%). Moreover, almost half of the studies (46%) dealt with PFs other than those listed in the classification of Geyh et al. (8). These included other diseases, quality of life, severity of injury, and compliance with treatment (Supplementary Table 1).
Factors included in the ICF as part of a component other than PFs or that do not describe functioning were mentioned as PFs in 71 articles (31%). For example, personality or personality traits related to ICF body functions (b126 temperament and personality functions) were defined as a PF in 17 articles, pain (b280–289) in 10 articles, and body mass index (b150 weight management functions) in 10 articles. Similarly, support from family, friends, or others was defined as a PF in 9 articles, although they are listed under environmental factors in the ICF (e3 support and interpersonal relationships). Factors that do not describe functioning but which were defined as PFs included lack of time, the ability of the therapist to communicate, and preparation for therapy.
The thematic analysis (of 51 articles) highlighted three themes on the role of PFs in rehabilitation: a person- and client-centered rehabilitation process, commitment to rehabilitation, and the need for classifying PFs (Figure 2). Each theme comprised different sub-themes.
In sum, the PFs reflected on in this group of articles largely concerned person- and client-centered care (20–39). PFs support a bio-psycho-social point of view of rehabilitation (40) and allow a comprehensive observation of functioning (8). In general, PFs were argued to be meaningful in person- and client-centered care (29). Professionals should permit the individual to drive the process (35). The role of PFs was reflected on in the different phases of rehabilitation. For example, the age and gender of a person seem to be especially important factors in rehabilitation planning (21, 23, 41–43). In addition, the classification of PFs helps in identifying the individually perceived needs of the clients and the planning of individual care (i.e., medication) (44). It also helps professionals to plan and select rehabilitation interventions for clients (45) and enables them to see the effects of these interventions (31). PFs seem to be more relevant to physical activity and training than environmental factors (38). A PF may act as a significant enabler or deterrent in determining the social, medical, or rehabilitative benefits sought (46). Consideration of PFs can have an impact on multiple outcomes, including quality of life (24, 32, 47), functioning and participation in society (32), and social integration (48).
Several articles discussed PFs around the theme “commitment to rehabilitation.” In particular, the role of PFs in motivating rehabilitation was addressed in many articles. Hawkins et al. (25) argued that PFs should be taken into account when planning rehabilitation as they are relevant to motivation. It was also argued that PFs can promote or hinder the motivation of a person (30), device uptake (49), return to work (50) and realistic goal setting in rehabilitation (27). Giving consideration to personal interests generates resources and prevents frustration with rehabilitation, and thus promotes the commitment of a client (51). Positive coping strategies, self-efficacy, and an optimistic attitude toward rehabilitation are important factors in its success (33, 52, 53). They also allow us to understand and take note of the experience of illness and satisfaction by the clients with their activities (54). Willingness and an optimistic attitude toward rehabilitation are thus meaningful factors (30). The confidence of a person in his/her own abilities and capacities is also important in promoting commitment to the rehabilitation process (51). PFs can also help in identifying the challenges that rehabilitation presents to individuals (31).
The need for a classification of PFs was considered in the articles from different perspectives. Generally, it was stated that professionals should recognize the benefits of having a classification of PFs (47, 55), notably in the context of rehabilitation (56). For example, a classification would help interprofessional teams to achieve a consensus on care and rehabilitation (33). Furthermore, a classification would facilitate a comprehensive and systematic examination, description, and documentation of problems and resources of a client and how these impact on functioning (55, 57) and would also save time (46). Making assessments and decisions based on the use of non-standardized individual factors involves high risks (46). The systematic gathering of data can assist in planning and implementing more precisely targeted interventions and in monitoring rehabilitation outcomes (31). A standardized classification could also help professionals to develop common concepts and documentation (12, 58). It was also argued that non-standardized use presents a risk in rehabilitation (8). Without the inclusion of PFs, the model of functioning remains narrow and reduces the status of an individual to one of illness and disability bereft of autonomy, subjectivity, and humanity, and thus ignores the whole life context of the individual. Without PFs, the ICF is an unhumanized model (8, 12, 40).
This scoping review summarized the literature on research that included discussion of ICF PFs to better understand what PFs are and to analyze their role in rehabilitation. As in the previous review by Geyh et al. (16), the studies included in this review were heterogeneous in their research settings, target groups, and targeted stage of the rehabilitation process. Mentions of PFs were extracted from all the eligible studies and, excepting those that were clearly not PFs, grouped into seven categories according to Geyh et al. (8). PFs were most often linked to personal experiences or habits, sociodemographic factors, and personal thoughts and beliefs. The qualitative analysis of the importance and meaningfulness of PF in rehabilitation yielded three themes: a person- and client-centered rehabilitation process, commitment to rehabilitation, and the need for classifying PFs. Armed with these findings from recent research studies, we entered the debate on the role of PFs in rehabilitation, their importance in understanding functioning and disability, and their ethical use (11, 15).
Overall, the studies revealed a wide range of different types of PFs. While the included studies used heterogeneous methods and focused on different target groups, they all considered PFs to be important factors in assessing functioning and in planning and implementing rehabilitation. While all the included studies (n = 226) included an analysis of PFs, they were not always the central aim. In fact, only a quarter of the included studies (n = 51) focused on PFs to the extent of explicitly drawing conclusions about them, and only 14 studies called for the classification of PFs.
Martinuzzi et al. (59) argued for the importance of adding PFs described by clients to those that are already described in classifications. The same PFs were mentioned in different types of research studies, thereby indicating how essential they are for understanding situations from the perspective of a client. Surprisingly, however, the PFs named in many studies were clearly not PFs and could be linked to some of the existing ICF components. A possible explanation for this is that the ICF is still not thoroughly understood with respect to which factors belong to which components. Alternatively, the short descriptions given about the PFs in the ICF may not be clear enough for users. These results are in line with those of Martinuzzi et al. (59), who emphasized the need to understand the whole ICF model, including the relations between its components, when assessing PFs. However, it can be also argued that the ICF itself is ambiguous. In particular, factors such as personality or motivation, that can be linked to the ICF b1 mental functions category and linked to the ICF as PFs in the studies included in this review, showed that these constructs merit consideration when further developing the ICF.
Our thematic analysis showed that PFs play an essential role in rehabilitation. Three different themes on their role emerged. The first theme concerned their role in supporting a person- and client-centered rehabilitation process. Assessment of PFs is essential when planning rehabilitation and when documenting information on functioning. Asking and understanding about PFs can foster core components of person- and client centered rehabilitation such as respect for values, beliefs, experience, and contexts, and inclusion of family as defined by the client (60). It has also been argued that person-centered care could have a positive effect on rehabilitation outcomes, although it has not yet been fully implemented in rehabilitation settings (61). The rehabilitation process combines two theoretical frameworks: treatment theory, which provides tools on how a change in a particular factor can be brought about, and enablement theory, which acknowledges that functioning is complex and determined by multiple factors, and which seeks to model these complex interrelationships (62). To apply enablement theory in the rehabilitation process, it is essential to understand individual variation in PFs. Our results show that PFs contribute essential information that should be linked with information on functioning in the rehabilitation process of a person. However, in clinical practice professionals mostly document them in the history of a client in a narrative form. Using unified terminology could enhance documentation quality, but this does not necessarily mean that all PFs should be contained in a single classification.
The second theme highlighted the importance of PFs for the commitment of a person in various rehabilitation programs and in different phases of rehabilitation. Motivation is clearly a personal matter, and it has been noticed to be an important predictor of adherence to, for example, exercise interventions (63) In addition, it is important to take into account that different clients consider different things important, as this affects commitment. Similarly, the need, highlighted by Lee et al. (64), to recognize the experience of purposefulness by a client influences rehabilitation outcomes. Professionals can learn how to support empowerment and strengths of a person by considering how various PFs might facilitate or hinder the commitment of a person. These findings support previous studies that have suggested reorganizing the ICF model to emphasize PFs (13, 14). Notably, we found no mention of the concern that a classification of PF within the ICF could lead to “blaming” the person for their functional limitations (11) in any of the studies. Instead, PFs were invariably used to support clients in their rehabilitation process.
The third theme concerned the importance of classifying PFs for the benefit of professionals. Studies supporting this idea identified the need to develop the ICF classification and its core lists to include PFs. This would create a comprehensive and systematic tool to facilitate communication, increase consensus, and save time. Another question concerned whether a minimum generic list of essential PFs could be developed for use in clinical practice with all clients. Clinically, the ICF can be used to organize and code the assessment data on functioning and environmental factors. As the PFs of the client can have a strong influence not only on health and functioning but also on the rehabilitation process, professionals would benefit from reliable tools to help in the assessment and guide the discussion. Such a tool could be, for example, a minimum list of potentially important PFs. In client-centered practice, the professional should, together with the client, consider which factors are important and relevant for that client and use this knowledge to discuss how best to help the client go forward in the rehabilitation process (65). Future research should evaluate whether this would enhance core elements of client-centered rehabilitation, such as communication and partnership (66). It seems that in the absence of a generally accepted classification, several differing classifications have arisen (10, 67). Based on this scoping review, the classification proposed by Geyh et al. (8) covers a lot of important PFs of relevance for client-centered rehabilitation. However, a large number of PFs were not included in the Geyh et al.'s (8) classification. This must be borne in mind when applying the classification in clinical practice. Since the completion of the present analysis, Grotkamp et al. (68) published a classification that includes PFs more broadly related to, for example, life situation and physical functioning compared with Geyh's classification. It would therefore be useful to apply them as complementary classifications when assessing functioning in relation to PFs in clinical practice.
This review did not seek an answer to the question of whether to classify PFs or not. All the included studies stated that they are important, while a few proposed classifying them. However, a complete taxonomy or classification of all possible PFs may not be necessary as some of them are already included in other classifications or instruments. Many information structures in health and social care include PFs, particularly factors in categories 1 and 2 of the classification by Geyh et al. (8), such as gender, age, occupation, or education. In Finland, the National Code Server has defined some common information components to unify documentation of the same type of data using the same structures. These components include PFs related to life habits (category 7), such as motion, nutrition, sleep/rest, as well as smoking and alcohol use habits (69). Rehabilitation professionals also use instruments that focus on PFs and structurally assess PFs based on the subjective experience of clients. For example, the Occupational Performance History Interview (OPHI-II), a method that collects unique data on a person's functional history during working age (70) can be subsumed under personal history (category 3). PFs regarding health, feelings, and mood of the self (category 4) and attitudes, expectations, and motives (categories 5 and 6) of the self can either be discussed freely with the client or incorporated in a structured interview, using, for example, the Readiness for Return to Work Questionnaire (71) or the relevant part of the Model of Human Occupation Screening Tool (MOHOST), which assesses the own will and motivation of the client (72). Future research should explore precisely what instruments or other methods of PF are available and whether they are comprehensive enough to describe and document the wide variety of PFs.
All the public health care institutions of the Nordic countries subscribe to a democratic value system, in which all citizens have equal rights to individualized and person-centered health care services (73). In many countries, the professional use of PFs is guided by legislation and other principles. For example, the UN Convention on the Rights of Persons with Disabilities (74) stipulates that all disabled people should be treated equally. The new EU legislation takes this one step further and considers a client's personal data, such as functioning or PFs, as sensitive data (75). In the EU, at least, this gives clients better protection and control over their personal information and how this information is used in rehabilitation processes. Moreover, health care professionals are under a duty to base their decisions and actions on ethical principles. These include empathy, honesty, and confidentiality. Finnish physical therapists, for example, should adhere to the basic ethical principles of doing good, avoiding bad actions, and respecting client autonomy and justice (76).
A key strength of this study was the implementation of a rigorous and systematic methodological approach. Furthermore, by addressing the importance of PFs in rehabilitation research and practice, this study may be of value in the future development and use of the ICF classification.
This scoping review synthesized the key characteristics attributed to PFs in the rehabilitation literature. Due to the broad focus of the study, we may have failed to identify all the relevant studies. However, consultation with an information specialist throughout the search process reduced the likelihood of this limitation. To enhance the trustworthiness of the data, the team members cross-checked and verified the search results in pairs. Owing to the scoping review method (77), the methodological quality or risk for bias of the included articles was not evaluated. Moreover, this study does not produce a critically appraised answer to the question of whether PFs should be classified. The broad aim of the review generated a large number of references. More specific inclusion and exclusion criteria might have enabled a more precise focus on the role of PFs in rehabilitation.
A substantial number of studies concluded that PFs have an important role and a specific meaning in rehabilitation processes. PFs foreground the principle of person- and client-centeredness in such processes. Furthermore, when PFs are well understood and taken into account in assessing the functioning of a client, the professional will have a better understanding of how to strengthen the commitment of a client. Professionals would also benefit from a classification of PFs to facilitate systematic documentation and save time. Future research should define what tools to use and what factors to include in a list of the minimum PFs needed to guide rehabilitation processes. In the meantime, it is recommended to use the ICF framework as an instrument for the structuring of information and concepts related to functioning, even if PFs have not been further defined at the level of categories. The classification developed by Geyh et al. (8) and/or that by Grotkamp et al. (68) can serve as checklists when mapping, together with the client, which PFs promote or hinder activity and participation, and how important different factors are to the client.
MK, AK, SS, HA, EX, and TH: Conceptualization. MK, HA, and AK: Theoretical framework and literature review. MK: Project administration. MK, AK, SS, EX, TH, and HA: Analysis and writing and editing. All authors have read and agreed to the published version of the manuscript.
The soping review is funded by Social Insurance Institution of Finland. Open access publication fees and revising the English language of the manuscript of the article are funded by South-Eastern Finland University of Applied Sciences.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The handling Editor declared a past co-authorship with one of the authors HA.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We sincerely thank information specialist Tapio Salmela for literature searches. We would also like to thank Michael Freeman for revising the English language of this article.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fresc.2021.709682/full#supplementary-material
1. World Health Organization. The International Classification of Functioning, Disability and Health (ICF). Geneva: WHO (2001).
2. Madden RH, Bundy A. The ICF has made a difference to functioning and disability measurement and statistics. Disabil Rehabil. (2019) 41:1450–62. doi: 10.1080/09638288.2018.1431812
3. Maribo T, Petersen KS, Handberg C, Melchiorsen H, Momsen AM, Nielsen CV, et al. Systematic Literature Review on ICF From 2001 to 2013 in the Nordic Countries Focusing on Clinical and Rehabilitation Context. J Clin Med Res. (2016) 8:1–9. doi: 10.14740/jocmr2400w
4. Ministry of Social Affairs and Health. Rehabilitation Reform. Action Plan for Reforming Rehabilitation Services 2020–2022. Helsinki: Ministry of Social Affairs and Health (2020).
5. Campbell NC, Murray E, Darbyshire J, Emery J, Farmer A, Griffiths F, et al. Designing and evaluating complex interventions to improve health care. BMJ. (2007) 334:455–9. doi: 10.1136/bmj.39108.379965.BE
6. Karstensen JK, Kristensen HK. Client-centred practice in Scandinavian contexts: a critical discourse analysis. Scand J Occup Ther. (2021) 28:46–62. doi: 10.1080/11038128.2020.1769183
7. Alford VM, Ewen S, Webb GR, McGinley J, Brookes A, Remedios LJ. The use of the international classification of functioning, disability and health to understand the health and functioning experiences of people with chronic conditions from the person perspective: a systematic review. Disabil Rehabil. (2015) 37:655–66. doi: 10.3109/09638288.2014.935875
8. Geyh S, Schwegler U, Peter C, Müller R. Representing and organizing information to describe the lived experience of health from a personal factors perspective in the light of the international classification of functioning, disability and health (ICF): a discussion paper. Disabil Rehabil. (2019) 41:1727–38. doi: 10.1080/09638288.2018.1445302
9. Nguyen T, Stewart D, Rosenbaum P, Baptiste S, Kraus de. Camargo O, Gorter JW. Using the ICF in transition research and practice? Lessons from a scoping review. Res Dev Disabil. (2018) 72:225–39. doi: 10.1016/j.ridd.2017.11.003
10. Müller R, Geyh S. Lessons learned from different approaches towards classifying personal factors. Disabil Rehabil. (2015) 37:430–8. doi: 10.3109/09638288.2014.923527
11. Leonardi M, Sykes CR, Madden RC., ten Napel H, Hollenweger J, Snyman S, et al. Do we really need to open a classification box on personal factors in ICF? Disabil Rehabil. (2016) 38:1327–8. doi: 10.3109/09638288.2015.1089604
12. Simeonsson RJ, Lollar D, Björck-Åkesson E, Granlund M, Brown SC, Zhuoying Q, et al. ICF and ICF-CY lessons learned: Pandora's box of personal factors. Disabil Rehabil. (2014) 36:2187–94. doi: 10.3109/09638288.2014.892638
13. Heerkens YF, de Weerd M, Huber M, de Brouwer CPM, van der Veen S, Perenboom RJM, et al. Reconsideration of the scheme of the international classification of functioning, disability and health: incentives from the Netherlands for a global debate. Disabil Rehabil. (2018) 40:603–11. doi: 10.1080/09638288.2016.1277404
14. Mitra S, Shakespeare T. Remodeling the ICF. Disabil Health J. (2019) 12:337–9. doi: 10.1016/j.dhjo.2019.01.008
15. Sykes CR, Maribo T, Stallinga HA, Heerkens Y. Remodeling of the ICF: a commentary. Disabil Health J. (2021) 14:100978. doi: 10.1016/j.dhjo.2020.100978
16. Geyh S, Peter C, Müüller R, Bickenbach JE, Kostanjsek N, ÜÜstüün BT, et al. The personal factors of the international classification of functioning, disability and health in the literature - a systematic review and content analysis. Disabil Rehabil. (2011) 33:1089–102. doi: 10.3109/09638288.2010.523104
17. Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Meth. (2005) 8:19–32. doi: 10.1080/1364557032000119616
18. Tricco AC, Lillie E, Zarin W, O'Brien K, Colquhoun H, Kastner M, et al. A scoping review on the conduct and reporting of scoping reviews. BMC Med Res Methodol. (2016) 9:15–4. doi: 10.1186/s12874-016-0116-4
19. Goodman V, Wardrope B, Myers S, Cohen S, McCorquodale L, Kinsella EA. Mindfulness and human occupation: a scoping review. Scand J Occup Ther. (2019) 26:157–70. doi: 10.1080/11038128.2018.1483422
20. Abeysekara P, Turchi R, O'Neil M. Obesity and children with special healthcare needs: special considerations for a special population. Curr Opin Pediatr. (2014) 26:508–15. doi: 10.1097/MOP.0000000000000124
21. Baert I, Vanlandewijck Y, Feys H, Vanhees L, Beyens H, Daly D. Determinants of cardiorespiratory fitness at 3, 6 and 12 months poststroke. Disabil Rehabil. (2012) 34:1835–42. doi: 10.3109/09638288.2012.665130
22. Amano T, Morrow-Howell N, Park S. Patterns of social engagement among older adults with mild cognitive impairment. J Gerontol B Psychol Sci Soc Sci. (2020) 75:1361–71. doi: 10.1093/geronb/gbz051
23. Andelic N, Stevens LF, Sigurdardottir S, Arango-Lasprilla JC, Roe C. Associations between disability and employment 1 year after traumatic brain injury in a working age population. Brain Inj. (2012) 26:261–9. doi: 10.3109/02699052.2012.654589
24. Andresen EM, Fried-Oken M, Peters B, Patrick DL. Initial constructs for patient-centered outcome measures to evaluate brain–computer interfaces. Disabil Rehabil Assist Technol. (2016) 11:548–57. doi: 10.3109/17483107.2015.1027298
25. Hawkins BL, McGuire FA, Britt TW, Linder SM. Identifying contextual influences of community reintegration among injured servicemembers. J Rehabil Res Dev. (2015) 52:235–46. doi: 10.1682/JRRD.2014.08.0195
26. Kang TW, Cynn HS. Progressive intervention strategy for the gait of sub-acute stroke patient using the international classification of functioning, disability, and health tool. NeuroRehabilitation. (2017) 40:473–81. doi: 10.3233/NRE-171434
27. Nam HS, Kim KD, Shin HI. ICF based comprehensive evaluation for post-acute spinal cord injury. Ann Rehabil Med. (2012) 36:804–14. doi: 10.5535/arm.2012.36.6.804
28. Martins AC. Using the international classification of functioning, disability and health (ICF) to address facilitators and barriers to participation at work. Work. (2015) 50:585–93. doi: 10.3233/WOR-141965
29. Escorpizo R, Davis K, Stumbo T. Mapping of a standard documentation template to the ICF core sets for arthritis and low back pain. Physiother Res Int. (2010) 15:222–31. doi: 10.1002/pri.466
30. Earde PT, Praipruk A, Rodpradit P, Seanjumla P. Facilitators and barriers to performing activities and participation in children with cerebral palsy: caregivers' perspective. Pediatr Phys Ther. (2018) 30:27–32. doi: 10.1097/PEP.0000000000000459
31. Segev D, Schiff M. Integrating israeli defense force (IDF) veterans with disabilities into the workforce: characteristics and predictors. Isr J Health Policy Res. (2019) 8:86. doi: 10.1186/s13584-019-0352-2
32. Scott-Roberts S, Purcell C. Understanding the functional mobility of adults with developmental coordination disorder (DCD) through the international classification of functioning (ICF). Curr Dev Disord Rep. (2018) 5:26–33. doi: 10.1007/s40474-018-0128-3
33. Jobst A, Kirchberger I, Cieza A, Stucki G, Stucki A. Content validity of the comprehensive ICF core set for chronic obstructive pulmonary diseases: an international delphi survey. Open Respir Med J. (2013) 7:33–45. doi: 10.2174/1874306401307010033
34. Glocker C, Kirchberger I, Gläßel A, Fincziczki A, Stucki G, Cieza A. Content validity of the comprehensive international classification of functioning, disability and health (ICF) core set for low back pain from the perspective of physicians: a Delphi survey. Chronic Illn. (2013) 91:57–72. doi: 10.1177/1742395312451280
35. Dwyer KJ, Mulligan H. Community reintegration following spinal cord injury: insights for health professionals in community rehabilitation services in New Zealand. Nz J Physiother. (2015) 43:75–85. doi: 10.15619/NZJP/43.3.02
36. Worrall LE, Hudson K, Khan A, Ryan B, Simmons-Mackie N. Determinants of living well with aphasia in the first year poststroke: a prospective cohort study. Arch Phys Med Rehabil. (2017) 98:235–40. doi: 10.1016/j.apmr.2016.06.020
37. Amsters D, Schuurs S, Pershouse K, Power B, Harestad Y, Kendall M, et al. Factors which facilitate or impede interpersonal interactions and relationships after spinal cord injury: a scoping review with suggestions for rehabilitation. Rehabil Res Pract. (2016) 9373786:1–13. doi: 10.1155/2016/9373786
38. Saebu M, Sørensen M. Factors associated with physical activity among young adults with a disability. Scand J Med Sci Sports. (2011) 21:730–8. doi: 10.1111/j.1600-0838.2010.01097.x
39. Blake HL, McLeod S. Speech-language pathologists' support for multilingual speakers' English intelligibility and participation informed by the ICF. J Commun Disord. (2019) 77:56–70. doi: 10.1016/j.jcomdis.2018.12.003
40. Huber JG, Sillick J, Skarakis-Doyle E. Personal perception and personal factors: incorporating health-related quality of life into the international classification of functioning, disability and health. Disabil Rehabil. (2010) 32:1955–65. doi: 10.3109/09638281003797414
41. Batten H, Lamont R, Kuys S, McPhail S, Mandrusiak A. What are the barriers and enablers that people with a lower limb amputation experience when walking in the community? Disabil Rehabil. (2020) 42:3481–7. doi: 10.1080/09638288.2019.1597177
42. Hancock AB. An ICF perspective on voice-related quality of life of american transgender women. J Voice. (2017) 31:115.e1–115.e8. doi: 10.1016/j.jvoice.2016.03.013
43. Rauch A, Fekete C, Cieza A, Geyh S, Meyer T. Participation in physical activity in persons with spinal cord injury: a comprehensive perspective and insights into gender differences. Disabil Health J. (2013) 6:165–76. doi: 10.1016/j.dhjo.2013.01.006
44. Bornbaum CC, Doyle PC, Skarakis-Doyle E, Theurer JA. A critical exploration of the international classification of functioning, disability, and health (ICF) framework from the perspective of oncology: recommendations for revision. J Multidiscip Healthc. (2013) 6:75–86. doi: 10.2147/JMDH.S40020
45. Geidl W, Semrau J, Pfeifer K. Health behaviour change theories: contributions to an ICF-based behavioural exercise therapy for individuals with chronic diseases. Disabil Rehabil. (2014) 36:2091–100. doi: 10.3109/09638288.2014.891056
46. Seger W, Grotkamp S, Cibis W. Personal factors and their relevance for the assessment and allocation of benefits in social medicine and rehabilitation. Electron Physician. (2017) 912:5868–70. doi: 10.19082/5868
47. Awad H, Alghadir A. Validation of the comprehensive international classification of functioning, disability and health core set for diabetes mellitus: physical therapists' perspectives. Am J Phys Med Rehabil. (2013) 92:968–79. doi: 10.1097/PHM.0b013e31829b4a6d
48. Ditchman N, Sheehan L, Rafajko S, Haak C, Kazukauskas K. Predictors of social integration for individuals with brain injury: an application of the ICF model. Brain Inj. (2016) 30:1581–9. doi: 10.1080/02699052.2016.1199900
49. Perfect E, Hoskin E, Noyek S, Davies TC. A systematic review investigating outcome measures and uptake barriers when children and youth with complex disabilities use eye gaze assistive technology. Dev Neurorehabil. (2020) 23:145–59. doi: 10.1080/17518423.2019.1600066
50. Culler KH, Wang YC, Byers K, Trierweiler R. Barriers and facilitators of return to work for individuals with strokes: perspectives of the stroke survivor, vocational specialist, and employer. Top Stroke Rehabil. (2011) 18:325–40. doi: 10.1310/tsr1804-325
51. Sivan M, Gallagher J, Holt R, Weightman A, Levesley M, Bhakta B. Investigating the international classification of functioning, disability, and health (ICF) framework to capture user needs in the concept stage of rehabilitation technology development. Assist Technol. (2014) 26:164–73. doi: 10.1080/10400435.2014.903315
52. Becker S, Kirchberger I, Cieza A, Berghaus A, Harréus U, Reichel O, et al. Content validation of the comprehensive ICF core set for head and neck cancer (HNC): the perspective of psychologists. Psycho Oncol. (2010) 19:594–605. doi: 10.1002/pon.1608
53. Kirchberger I, Sinnott A, Charlifue S, Kovindha A, Lüthi H, Campbell R, et al. Functioning and disability in spinal cord injury from the consumer perspective: an international qualitative study using focus groups and the ICF. Spinal Cord. (2010) 48:603–13. doi: 10.1038/sc.2009.184
54. Arnadottir SA, Gunnarsdottir ED, Stenlund H, Lundin-Olsson L. Determinants of self-rated health in old age: a population-based, cross-sectional study using the international classification of functioning. BMC Public Health. (2011) 11:670. doi: 10.1186/1471-2458-11-670
55. Glässel A, Kirchberger I, Kollerits B, Amann E, Cieza A. Content Validity of the extended ICF core set for stroke: an international delphi survey of physical therapists. Phys Ther. (2011) 91:1211–22. doi: 10.2522/ptj.20100262
56. Bossmann T, Kirchberger I, Glaessel A, Stucki G, Cieza A. Validation of the comprehensive ICF core set for osteoarthritis: the perspective of physical therapists. Physiotherapy. (2011) 97:3–16. doi: 10.1016/j.physio.2009.11.011
57. Koehler B, Kirchberger I, Glaessel A, Kool J, Stucki G, Cieza A. Validation of the international classification of functioning, disability and health comprehensive core set for osteoporosis: the perspective of physical therapists. J Geriatr Phys Ther. (2011) 34:117–30. doi: 10.1519/JPT.0b013e31820aa990
58. Ng L, Khan F. Identification of personal factors in motor neurone disease: a pilot study. Rehabil Res Pract. (2011) 2011:871237. doi: 10.1155/2011/871237
59. Martinuzzi A, Mea VD, Ten Napel H. Personal factors in ICF: responding to the challenge. Newsl WHO-FIC. (2018) 16:3–4. Available online at: https://www.whofic.nl/sites/default/files/2018-10/WHO-FIC%20newsletter%202018-1_0.pdf (accessed July 29, 2021).
60. Mroz TM, Pitonyak JS, Fogelberg D, Leland NE. Client centeredness and health reform: key issues for occupational therapy. Am J Occup Ther. (2015) 69:6905090010p1–8. doi: 10.5014/ajot.2015.695001
61. Yun D, Choi J. Person-centered rehabilitation care and outcomes: a systematic literature review. Int J Nurs Stud. (2019) 93:74–83. doi: 10.1016/j.ijnurstu.2019.02.012
62. Whyte J. Contributions of treatment theory and enablement theory to rehabilitation research and practice. Arch Phys Med Rehabil. (2014) 95:S17–23.e2. doi: 10.1016/j.apmr.2013.02.029
63. Ormel HL, van der Schoot GGF, Sluiter WJ, Jalving M, Gietema JA, Walenkamp AME. Predictors of adherence to exercise interventions during and after cancer treatment: a systematic review. Psychooncology. (2018) 27:713–24. doi: 10.1002/pon.4612
64. Lee JY, Ready EA, Davis EN, Doyle PC. Purposefulness as a critical factor in functioning, disability and health. Clin Rehabil. (2017) 31:1005–18. doi: 10.1177/0269215516672274
65. Sumsion T, Law M. A review of evidence on the conceptual elements informing client-centred practice. Can J Occup Ther. (2006) 73:153–62. doi: 10.1177/000841740607300303
66. Constand MK, MacDermid JC, Dal Bello-Haas V, Law M. Scoping review of patient-centered care approaches in healthcare. BMC Health Serv Res. (2014) 14:271. doi: 10.1186/1472-6963-14-271
67. Grotkamp S, Cibis W, Nüchtern E, Baldus A, Behrens J, Bucher PO, et al. Personal factors of the ICF. Gesundheitswesen. (2012) 74:449–58. doi: 10.1055/s-0032-1314823
68. Grotkamp S, Cibis W, Brüggemann S, Coenen M, Gmünder H, Keller K, et al. Personal factors classification revisited: A proposal in the light of the biopsychosocial model of the World Health Organization (WHO). Aust J Rehab Couns. (2020) 26:73–91. doi: 10.1017/jrc.2020.14
69. Finnish institute for health and welfare. Terveydenhuollon tietokomponentit (2020). Available online at: https://thl.fi/fi/web/tiedonhallinta-sosiaali-ja-terveysalalla/maaraykset-ja-maarittelyt/maarittelyt-terveydenhuollolle/terveydenhuollon-tietokomponentit- (accessed March 16, 2021).
70. Kielhofner G, Henry AD. Development and investigation of the occupational performance history interview. Am J Occup Ther. (1988) 42:489–98. doi: 10.5014/ajot.42.8.489
71. Franche RL, Corbière M, Lee H, Breslin FC, Hepburn CG. The readiness for return-to-work (RRTW) scale: development and validation of a self-report staging scale in lost-time claimants with musculoskeletal disorders. J Occup Rehabil. (2007) 17:450–72. doi: 10.1007/s10926-007-9097-9
72. Kielhofner G, Fan C, Morley M, Garnham M, Heasman D, Forsyth K, et al. A psychometric study of the model of human occupation screening tool (MOHOST). Hong Kong J Occup Ther. (2010) 20:63–70. doi: 10.1016/S1569-18611170005-5
73. Kristensen HK. Occupational science in a Nordic environment. J Occup Sci. (2019) 26:193–9. doi: 10.1080/14427591.2019.1572530
74. United Nations. Convention on the Rights of Persons with Disabilities (CRPD). (2006). Available online at: https://www.un.org/development/desa/disabilities/convention-on-the-rights-of-persons-with-disabilities.html (accessed May 8, 2021).
75. European Parliament and the Council of the European Union. General Data Protection Regulation. (2016). Available online at: https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32016R0679 (accessed May 8, 2021).
76. Finnish Association of Physiotherapists. Ethical guidelines for physiotherapists. (2014). Available online at: https://www.suomenfysioterapeutit.fi/wp-content/uploads/2018/01/Ethical_Guidelines_2014.pdf (accessed May 8, 2021).
Keywords: international classification of functioning disability and health, client-centeredness, person-centeredness, personal factors, rehabilitation, scoping review
Citation: Karhula M, Saukkonen S, Xiong E, Kinnunen A, Heiskanen T and Anttila H (2021) ICF Personal Factors Strengthen Commitment to Person-Centered Rehabilitation – A Scoping Review. Front. Rehabilit. Sci. 2:709682. doi: 10.3389/fresc.2021.709682
Received: 14 May 2021; Accepted: 15 July 2021;
Published: 16 August 2021.
Edited by:
Thomas Maribo, Aarhus University, DenmarkReviewed by:
Juana Gómez-Benito, University of Barcelona, SpainCopyright © 2021 Karhula, Saukkonen, Xiong, Kinnunen, Heiskanen and Anttila. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maarit Karhula, bWFhcml0Lmthcmh1bGFAeGFtay5maQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.