- 1Tokyo Bay Rehabilitation Hospital, Narashino, Japan
- 2Graduate School of Human Sciences, Waseda University, Tokorozawa, Japan
- 3Faculty of Rehabilitation, School of Health Sciences, Fujita Health University, Toyoake, Japan
- 4Department of Rehabilitation Medicine I, Fujita Health University School of Medicine, Toyoake, Japan
- 5Faculty of Human Sciences, Waseda University, Tokorozawa, Japan
- 6Graduate School of Comprehensive Human Science, University of Tsukuba, Tokyo, Japan
Background: Motivation is essential for patients with subacute stroke undergoing intensive rehabilitation. Although it is known that motivation induces behavioral changes toward rehabilitation, detailed description has been lacking. Motivation can be intrinsic or extrinsic; however, it is unclear which type of factors mainly motivates patients' daily rehabilitation.
Purpose: This study aimed to examine the factors influencing patients' motivation and to explore the behavioral changes induced by motivation, especially age-related differences.
Method: Twenty participants (mean age 65.8 years [standard deviation 13.7]) who had a subacute stroke and underwent rehabilitation at a convalescent hospital were recruited using convenience sampling. Semi-structured interviews were conducted by an occupational therapist with an interview topic guide regarding factors influencing motivation and how it affects behavioral change. Interviews were recorded, transcribed to text, and analyzed by three occupational therapists using thematic analysis. The participants were divided into two groups: aged patients (aged ≥ 65 years) and middle-aged patients (aged < 65 years), and data were analyzed according to the groups. This study was conducted according to the consolidated criteria for reporting qualitative research.
Results: Seven core categories were identified as factors influencing patients' motivation: patients' goals, experiences of success and failure, physical condition and cognitive function, resilience, influence of rehabilitation professionals, relationships between patients, and patients' supporters. The first four and last three core categories were further classified as personal and social-relationship factors, respectively. The categories related to intrinsic motivation such as enjoyment of rehabilitation itself were not derived. In both age-groups, motivation affected the frequency of self-training and activity in daily lives. In some aged patients, however, high motivation restrained their self-training to conserve their physical strength for rehabilitation by professionals. Some aged patients do not express their high motivation through their facial expressions and conversations compared to middle-aged patients; therefore, motivation is not always observable in aged patients.
Conclusions: Interventions tailored to extrinsic factors are important for maintaining patients' motivation. Observational evaluation may lead to mislabeling of their motivation, especially for aged patients. Rehabilitation professionals should use validated evaluation scales or patients' narratives to assess patients' motivation.
Introduction
Stroke patients undergoing rehabilitation are required to be active participants in their treatment, and motivation is an essential factor for active participation. Self-determination theory (SDT) is a commonly known motivational theory (1, 2) and is applied in rehabilitation fields (3, 4). Conventionally, motivation is divided into extrinsic motivation and intrinsic motivation. Extrinsic motivation involves doing something because it leads to a separable consequence; that is, the goal is separate from the activity itself. In contrast, intrinsic motivation involves doing something because it is interesting and enjoyable in itself (1, 2). According to this classification, rewards such as functional improvement and praise from medical staff and family members can be categorized as extrinsic motivation, and enjoyment of rehabilitation itself can be considered intrinsic motivation. In previous studies, motivation for rehabilitation was reported to be affected by extrinsic factors such as environmental factors (5–7), individual beliefs (6–10), and support from medical staff and family (7, 10–13). Since the majority of stroke patients in the convalescent phase attend rehabilitation to return to their before-stroke-onset lives, a form of extrinsic motivation, we do not expect that intrinsic motivation is a major part of their commitments. Especially subacute stroke patients who are in convalescent phase are considered to be more affected by extrinsic motivation than chronic patients, and since their physical functions are relatively more changeable than that of chronic stroke patients, it is easier for them to earn rewards, i.e., functional recovery. Thus, we hypothesize that subacute stroke patients undergo rehabilitation based mostly on extrinsic factors such as functional improvement.
Motivation can induce behavioral changes. In rehabilitation, motivation is suggested as a predictor of functional outcomes (14). The motivation for rehabilitation is reported to influence physical activity (8, 15) and participation in training (16, 17). Thus, motivation can be expressed as physical activity and attitude toward rehabilitation. Therefore, medical staff tend to label the patients' motivation based on the activity in their daily lives, their attitude, and compliance with rehabilitation (7). However, a previous qualitative study pointed out a mismatch between motivation and activity and warned that observational evaluation of patients' motivation by medical staff may sometimes lead to mislabeling (7). Stroke patients in convalescent rehabilitation hospitals are required to pursue intensive rehabilitation training. Since the physical strength and capacity of aged patients tend to be less than that of younger patients (18), they may not have enough capacity to actively engage in physical activities or express a positive attitude toward rehabilitation. If medical staff label patients' motivation according to daily activity or attitude, those patients are mislabeled as being unmotivated. To correctly evaluate these patients, a detailed description of behavioral change, especially, age-related differences in their behavior, is required.
The purpose of this study is as follows: first, we clarified the factors influencing patients' motivation for rehabilitation in the convalescent rehabilitation hospital. In particular, this study aimed to examine which type of factors, extrinsic or intrinsic, mainly motivates patients' daily rehabilitation. Second, we hypothesized that the behavioral changes influenced by motivation may differ in aged patients and middle-aged patients; thus, we analyzed the behavioral changes among different age-groups.
Although several evaluation scales of motivation for rehabilitation have been reported (19–22), no validated evaluation scale for rehabilitation explicitly contains items related to intrinsic motivation. Furthermore, questionnaires cannot provide detailed descriptions about the patients' behavioral changes in daily life. Thus, we adopted a qualitative method. Qualitative methods are appropriate for investigating topics that are poorly understood (23). Semi-structured interviews are based around open-ended questions that define the area to be explored; then, the interviewer and interviewee pursue an idea in more detail (23). In order to investigate the factors influencing motivation and patients' behavioral changes in detail, it is necessary to understand patients' narrative. Therefore, we employed semi-structured interviews to elucidate participants' motivation for rehabilitation. We also adopted thematic analysis, since it provides a more detailed and nuanced account of themes within the data (24, 25).
Materials and Methods
This study was conducted according to the consolidated criteria for reporting qualitative research [COREQ; (26)]. The study protocol was approved by the Ethics Committee of Tokyo Bay Rehabilitation Hospital (No. 144) and the Ethics Committee of Waseda University (No. 2019-059). All participants provided written and verbal informed consent before participating in this study.
Sample
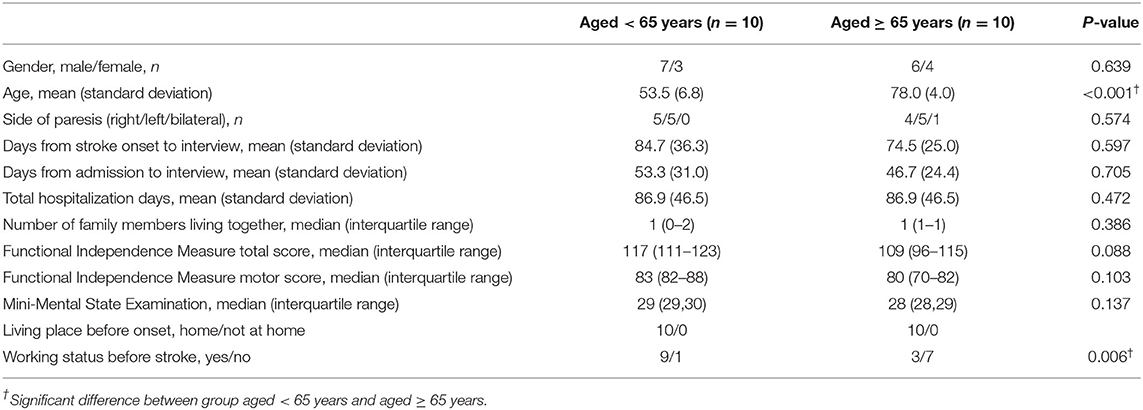
Participants were recruited from those who were admitted to the Tokyo Bay Rehabilitation Hospital in Japan, which had three convalescent rehabilitation wards with 160 beds. The inclusion criteria were as follows: a Mini-Mental State Examination score of 24 or more and having had their first-ever hemiparetic stroke in the subacute phase (27). Patients who were diagnosed by their doctors as having aphasia, depression, or cognitive impairments, and therefore would have difficulty participating in the study, were excluded. Twenty-two Japanese patients who met the inclusion criteria were recruited through convenience sampling; of these, 20 agreed to participate (10 aged < 65 years). All participants were assessed with the Functional Independence Measure (FIM) (28) by trained nurses to evaluate their functional status. Sample characteristics are presented in Table 1.
Study Setting
This study was conducted at convalescent rehabilitation wards called Kaifukuki Rehabilitation Wards (KRWs). KRW is the system for subacute rehabilitation in Japan and is covered by governmental medical insurance. In KRW, patients undergo one-on-one rehabilitation with therapists up to 3 h every day. A typical schedule was 1 h in the morning and 1 or 2 h in the afternoon. Patients engage in self-training out of rehabilitation sessions if indicated. The content of the self-training is usually supervised by the therapist or doctor in charge. The participants can usually adjust the frequency and the intensity of self-training based on their own conditions and schedules. Interviews were conducted only once during the hospitalization and did not interrupt the participants' schedule of rehabilitation, meals, bathing, self-training, family visits, and meetings with doctors. It was mainly conducted in the afternoon between rehabilitation sessions and dinner. Interviews took place in the rehabilitation room or in the patient's room, where the content of the interview could not be overheard by others.
Interviews
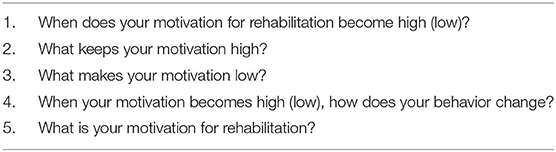
The interviewers were three occupational therapists (TY, MK, and SK) at the hospital with a mean clinical experience of 6.7 ± 1.5 years. They had no personal relationships with the interviewees. All the interview contents were recorded using an IC recorder with pre-obtained permission from the interviewees. The interview topic guide (Table 2) was developed based on discussions between the three occupational therapists (TY, MK, and SK) and a rehabilitation doctor (YO) with more than 20 years of clinical experience. All interviews were performed according to the interview topic guide. The term “motivation” in the study was defined as “the impetus to initiate, sustain, orientate, enliven, and move forward a goal-oriented action,” which was taken from the Japanese psychological dictionary (29). The definition was explained to participants prior to the interview to share a common understanding of the term. In addition, explanations for each question were prepared and shared among the interviewers; the meaning of the question was explained using these shared understandings prior to each question being asked and if the participant asked the interviewer about the meaning of the question. The interview was conducted by the occupational therapist who was not in charge of the patents' rehabilitation. Considering the psychological burden of the participants, the participants were told that the interview could be stopped immediately if a psychological burden arose during the interview.
Analyses
Recorded interview data were transcribed to text format and analyzed using thematic analysis (24, 25). The transcripts were read thoroughly to acquire meanings from the words of each sample. Close readings of transcripts generated sentences as the record units. Record units of each interview were categorized into codes by their meanings. The codes were then categorized into subcategories. These subcategories were then categorized into categories, which were further categorized into core categories. An occupational therapist (TY) made record units and codes, and three occupational therapists (TY, MK, and SK) made subcategories, categories, and core categories through repeated discussion until a consensus was reached. The personally identifiable data were not included in data analysis to preserve anonymity. These procedures were conducted separately for samples of participants aged < 65 and ≥ 65 years to consider age-group differences, since lifestyles may differ between these age-groups. Comparisons of the characteristics including demographic variables and FIM scores were performed between aged and middle-aged groups with Mann–Whitney U-test and chi-square test depending on the types of variables. Statistical analyses were performed with IBM SPSS Statistics 27 (IBM Corp., Armonk, NY). P < 0.05 were considered statistically significant.
Results
Comparisons of Sample Characteristics Between Age-Groups
No significant differences were found in characteristics between age-groups, except for age and working status before onset (Table 1). Total FIM score ranged from 96 to 115 and 111 to 123 in aged and middle-aged groups, respectively. The participants in both age-groups had relatively high functional status.
Codes and Categories
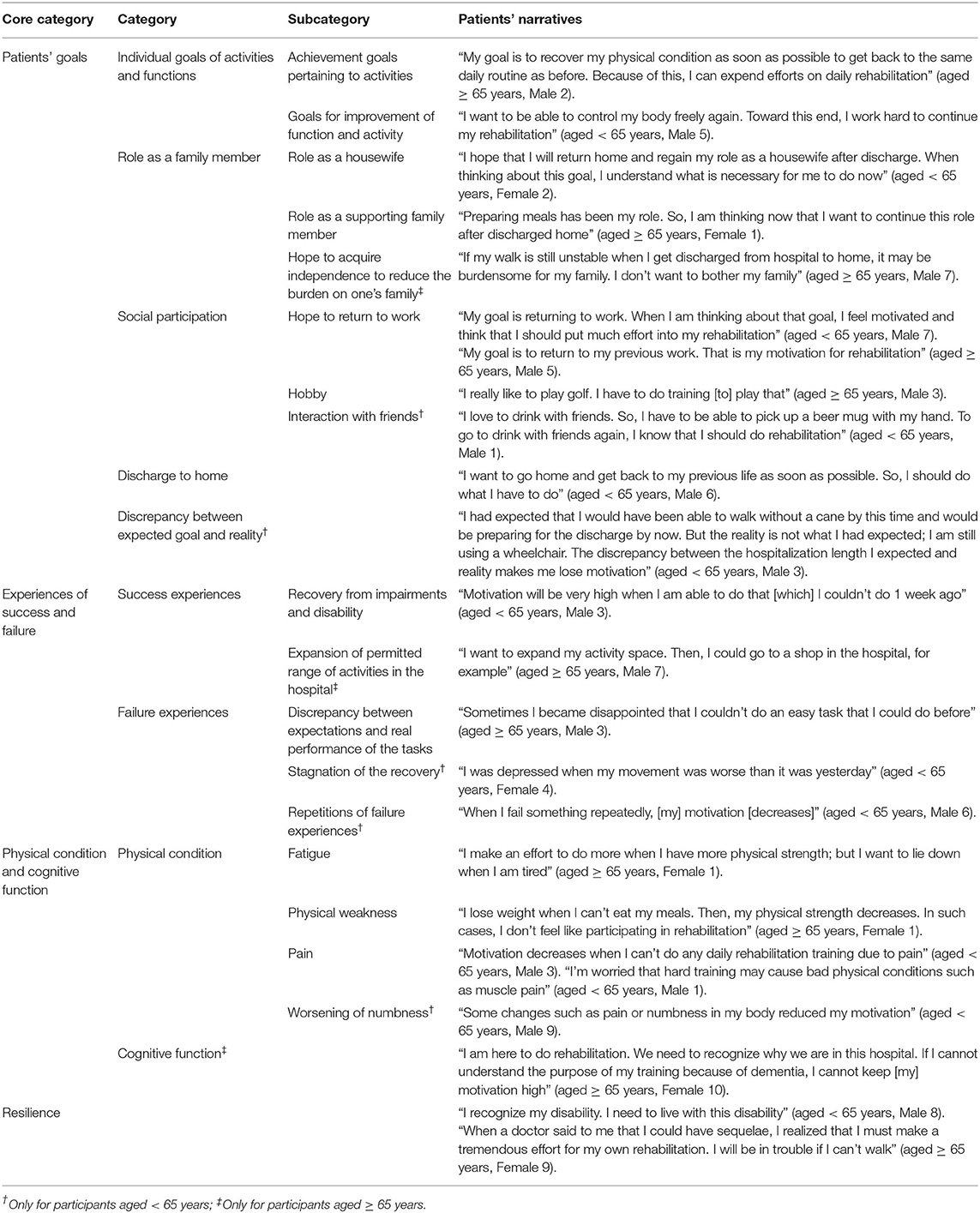
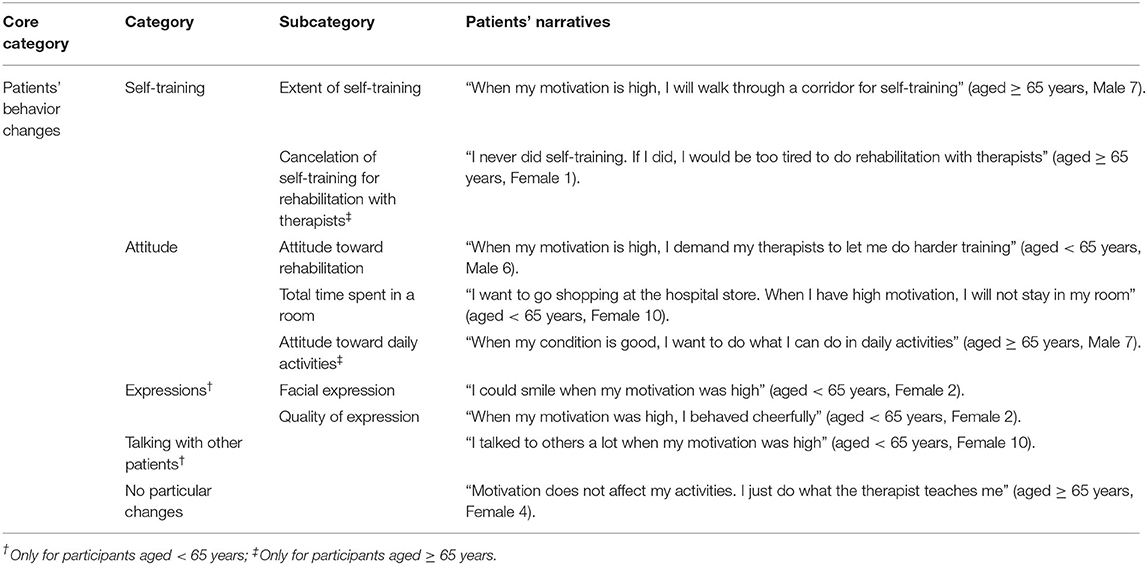
The average interview time for participants aged ≥ 65 was 19 min 46 s (SD ±193 s), while time for participants aged < 65 was 17 min 17 s (SD ±238 s). From interviews with participants aged < 65 years, 462 record units, 191 codes, 37 subcategories, 21 categories, and eight core categories were derived. From interviews with participants aged ≥ 65 years, 490 record units, 176 codes, 36 subcategories, 19 categories, and eight core categories were derived (Tables 3–5). Although some differences between the two age-groups were found in some categories and subcategories, the same eight core categories were derived for both age-groups. Among these eight core categories, seven included factors influencing motivation for rehabilitation and one category concerned the effects of motivation on patients' behaviors (Tables 3–5).
Factors Influencing Motivation for Rehabilitation
The seven core categories for influencing factors of motivation for rehabilitation were patients' goals, experiences of success and failure, physical condition and cognitive function, resilience, influence of rehabilitation professionals, relationships between patients, and patients' supporters. The former four core categories were classified as personal factors (Table 3), and the latter three core categories were classified as social relationship factors (Table 4).
Personal Factors
Patients' Goals
Regardless of age-group, participants mentioned that their rehabilitation goal regarding individual goals of activities and functions, role as a family member, social participation such as work and hobby, and discharge to home influenced their motivation. In addition, one participant (aged < 65 years) mentioned the discrepancy between expected goal and reality. A participant (aged ≥ 65 years) noted that acquiring independence to reduce the burden on his family was a key motivation. A participant (aged < 65 years) mentioned being motivated to interact with friends, which was included in the “social participation” category.
Experiences of Success and Failure
Recovery from impairments and disabilities was reported as experiences of successes. A participant (aged ≥ 65 years) reported that the ability to have an expanded range of activities at the hospital was a motivator. The discrepancy between movement that participants expected and real task performance was reported as a failure, which decreased patients' motivation. Some participants (aged < 65 years) mentioned that recovery stagnation and repeated failures decreased their motivation.
Physical Condition and Cognitive Function
Participants in both age-groups commented that physical conditions including fatigue, physical weakness, and pain influenced their motivation. Some participants (aged ≥ 65 years) reported that it was vital that they have cognitive function to understand the purpose of rehabilitation, and some participants (aged < 65 years) reported that worsening numbness influenced their motivation.
Resilience
“Resilience” refers to the ability to adjust and adapt to varied situations and overcome challenges after adversity, although no universal definition exists (30). Participants in both age-groups reported that high resiliency played a key role in maintaining their motivation.
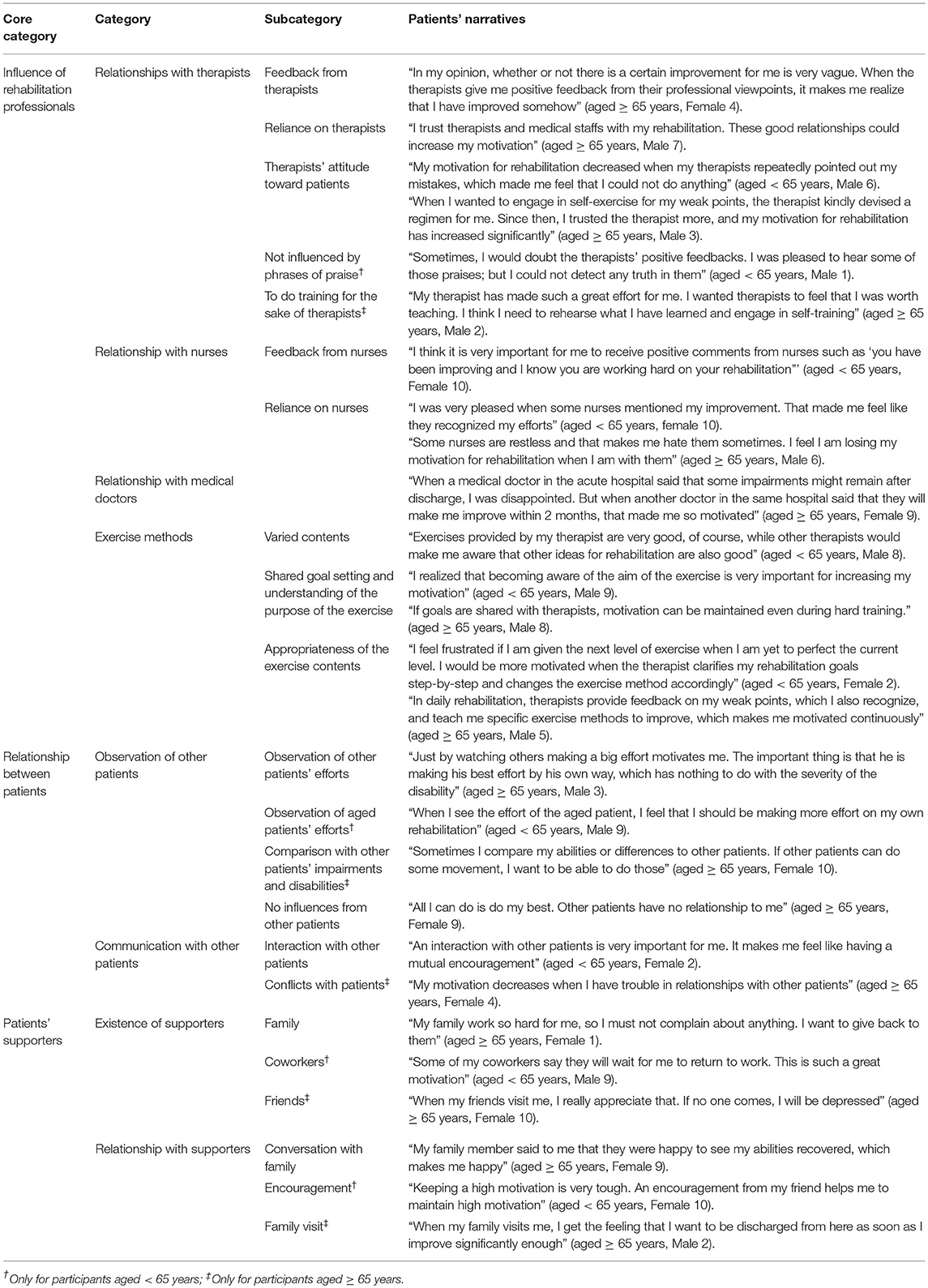
Social Relationship Factors
Influence of Rehabilitation Professionals
Relationships with professionals on the rehabilitation team—including therapists, nurses, and medical doctors—as well as exercise methods were classified into this core category.
Regardless of participants' age, they mentioned that professional positive feedback from therapists and nurses, reliance on therapists and nurses, and therapists' positive attitudes toward patients were motivating factors. Some participants (aged < 65 years) did not feel influenced by therapists' words, regardless of what they said; and some participants (aged ≥ 65 years) seemed to be motivated by their own beliefs—that they wanted to improve their body functions for the sake of their therapists. For some participants, doctors' explanations about medical conditions and prognosis also influenced their motivation. The explanation by a medical doctor that a patient could have sequelae and the percentage of improvement was lower than patient's expected reduced patients' motivation.
The variation and appropriateness of the exercises, sharing the goal setting, and understanding the purpose of the exercise positively influenced patients' motivation. Some advices and viewpoints for rehabilitation not only from the therapist in charge but also from other therapists could positively influence patients' motivation. Furthermore, some participants commented that motivation was positively influenced by the appropriateness of exercise contents, including adjusting the difficulty of the exercises, setting a goal through shared decision-making step-by-step, and changing the exercise regimen appropriately.
Relationships Between Patients
Observations of other patients' efforts influenced some participants' motivation, regardless of the severity of other patients' disabilities. Motivation was greatly enhanced by observing other patients completing their training; however, some participants were not influenced by other patients. Some participants (aged < 65 years) reported that observing aged patients' efforts was influential, while some participants (aged ≥ 65 years) reported that comparing their abilities to those of other patients had a positive influence on their motivation. Motivation increased when mutual encouragement was obtained. Some participants (aged ≥ 65 years) reported that motivation decreased owing to the frustrations from the conflicts with other patients.
Patients' Supporters
Existence of supporters and their relationships devised this core category. Regardless of age-group, participants reported that having a family and the conversations with them influenced their motivation. Regarding the existence of supporters, participants in both age-groups commented about their coworkers and friends. One participant (aged < 65 years) talked about getting encouragement from her supporters, and some participants (aged ≥ 65 years) reported the influence of family visits.
Patients' Behavioral Change
The interviews revealed that patients' motivation had an effect on their behaviors in the hospital, although some participants reported that motivation had no influence on their behaviors (Table 5). Some participants reported on self-training and active participation for daily activities. Some other participants (aged ≥ 65 years) reported that they did not do self-training that made them tired when their motivation for rehabilitation was high because they wanted to display better performance during rehabilitation with therapists. For some participants (aged < 65 years), the frequency of communication with other patients and changes in facial expressions were also reported.
Discussion
This study investigated the factors influencing subacute stoke patients' motivation for rehabilitation and the behavioral changes induced by motivation at a convalescent rehabilitation hospital. The strength of the study was that it comprehensively elucidated the factors influencing patients' motivation for rehabilitation with the qualified study methodology according to COREQ. In addition, this study revealed that behavioral changes due to motivation differ depending on patients' age. Seven factors influencing motivation were identified, all of which were categorized as extrinsic motivation. No factor included a purely intrinsic description such as enjoyment of rehabilitation itself. Regarding behavioral change, we found that high motivation does not always enhance activity in aged stroke patients.
As for the core categories influencing patients' motivation, four personal factors (patients' goals, experiences of success and failure, physical condition and cognitive function, and resilience) and three social relationship factors (influence of rehabilitation professionals, relationship between patients, and patients' supporters) were derived. While all these core categories are classified as extrinsic motivation, a category such as joy for rehabilitation itself (intrinsic motivation) was not derived from patients' narratives. The same core categories were derived from both aged and middle-aged patients. Therefore, these core categories will affect the majority of stroke patients' motivation for rehabilitation. Previous studies have shown that the motivation for rehabilitation in patients who have had strokes or various other diseases is influenced by individual traits (8, 9) and social environmental and social relationship factors (5–7, 10–13). However, these studies have not discussed the existence of intrinsic motivation for rehabilitation. Our results indicated that motivation for rehabilitation is mainly based on extrinsic, rather than intrinsic, motivation, at least for subacute stroke patients in convalescent rehabilitation hospitals.
The results indicate that, unlike sports or studies where internal motivation is vital, it is relatively effective to intervene with extrinsic motivation (1, 2), rather than intrinsic motivation, in the rehabilitation fields. Some of the personal and social relationship factors elucidated in this study are modifiable in rehabilitation practice, such as patients' goal setting and relationships with medical staff. Our results will be useful to help optimize rehabilitation practice and planning.
If the goal is set too high, the rewards the patients receive, such as functional improvement, will be less than what they expected. Such reward prediction errors could reduce patients' motivation to reach their goals (31). To maintain stroke patients' motivation, it is important to set appropriate goals and provide a variety of training content that can be tailored according to the patient's situation, such as age.
Previous studies pointed out the importance of relationships with others. For example, overprotection from medical staff and family makes patients incapable (9, 32), while appropriate information from rehabilitation professionals helps maintain patients' motivation (9). Our results are consistent with these studies and demonstrate the importance of social relationships, such as communication with medical staff, other patients, and family for maintaining the motivation for rehabilitation.
A previous qualitative study targeting medical professionals reported that motivation is affected by both physical and human environments, such as a well-maintained room and group treatment sessions (7). In our study, however, only human environmental factors such as medical staff, other patients, and supporters were derived, not physical environmental factors. The participants of this study were all patients who were admitted to the convalescent rehabilitation hospital for the first time and were not able to compare it with other environments, which could be the reason physical environmental factors were not derived.
Although no differences in the core categories were found based on patients' age-groups, some differences appeared in subcategories. In the middle-aged patients, factors associated with improvement in physical function were derived, such as stagnation of recovery, repetitions of failure experiences, and discrepancy between expectations and reality. In contrast, among the aged patients, the subcategory associated with self-care was derived, such as hoping to acquire independence to reduce the burden on their family. Younger participants with disability may have higher expectations of what they can achieve compared to individuals in other age-groups (33). During inpatient rehabilitation, aged patients' main goals were regaining independence in self-care activities and going home (34). In other words, factors related to physical function and its disability may affect motivation among middle-aged patients, while factors related to independent self-care and its disability may affect motivation among aged patients.
Regarding the behavioral changes induced by motivation, the frequency of self-training, attitude toward rehabilitation, and total time spent in a room were derived regardless of the patient's age. The majority of stroke patients in the hospital engage in self-training, rehabilitation, and activities of daily living more actively when they are highly motivated. Some aged patients, however, intentionally did not participate in self-training when their motivation was high to conserve their physical strength. Some of them wanted to show better performance during rehabilitation with therapists, to live up to their expectations. Meanwhile, the category related to expression and frequency of communication with other patients was derived in only middle-aged patients. Therefore, motivation is not likely to be expressed as an observable behavior such as emotional expression and self-training in some aged patients. Medical professionals tend to label patients' motivation based on observable activities such as demeanor and their compliance with rehabilitation (7). Our results indicate that if medical staff evaluate patients' motivation only from observational assessment, it may lead to mislabeling of motivation, especially in aged patients. Medical staff members need to understand that the differences in behavioral change are related to age. To assess patients' motivation for rehabilitation, it is desirable to evaluate their narrative or to use a validated evaluation scale for assessing patients' motivation.
There are several limitations in the study. Firstly, the sample size was relatively small, and the participants were enrolled with convenience sampling in a single institution. All the participants were Japanese and had relatively high functional level as measured with FIM. Since motivation may be influenced by the functional level as well as social factors, the generalizability of results obtained in this study should be done with caution. To examine the validity, a further study with a larger sample and participants with various functional levels using random sampling from multiple facilities in many countries should be conducted. Secondly, this study also involves the methodological limitations of qualitative studies. Although the study was conducted according to COREQ, the labeling could be different for another analyst. Some of the subcategories could be classified into multiple core categories. For example, hobby is classified as a subcategory in the category “social participation” but also could be allocated to the category “Individual goals of activities and functions.” Thus, interpretation of classification needs to be considered given the analysts' characteristics. Lastly, we cannot eliminate the possible existence of intrinsic motivation because we did not ask the direct/specific questions about the existence of intrinsic motivation, e.g., whether the participants enjoy rehabilitation itself. Although it is difficult to prove the non-existence of intrinsic motivation, more in-depth interview research will help clarify this point.
The motivation of patients with subacute stroke in convalescent rehabilitation hospitals was mainly influenced by factors related to extrinsic motivation. The patients' goals, experiences of success and failure, physical condition and cognitive function, resilience, relationships with rehabilitation professionals, and family and supporters were derived as the core categories. It is important that rehabilitation professionals consider these factors when helping patients stay motivated. Regarding behavioral changes induced by motivation, some aged patients do not show motivation via activities observable by rehabilitation professionals. For accurate evaluation of patients' motivation, rehabilitation professionals should use not only observation but also validated evaluation scales or patients' narratives. The findings of this study can help facilitate rehabilitation professionals' understanding of patients' motivation, encourage motivation, and develop optimal treatment plans.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics Statement
The protocol of this study was reviewed and approved by Ethic Committee of Tokyo Bay Rehabilitation Hospital and Ethic Committee of Waseda University. The patients provided their written informed consent to participate in this study.
Author Contributions
TY, YO, and JY contributed to the conception, design, and methodology of this study. TY, YO, MK, SK, and JY performed the formal analysis. YO, RO, and JY supervised this study. TY wrote the first draft of the manuscript. TY, YO, RO, and JY reviewed and edited the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Funding
This study was supported by JSPS KAKENHI Grant-in-Aid for Young Scientists (Start-up) (Grant no. 20K23271), and Grants-in-Aid for Scientific Research (KAKENHI) on Innovative Areas (Hyper-Adaptability, 20H05482) from the Ministry of Education, Culture, Sports, Science and Technology (MEXT), Japan.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank all participants in Tokyo Bay Rehabilitation Hospital. We gratefully acknowledge the cooperation of Tokyo Bay Rehabilitation Hospital and Waseda University.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fresc.2021.664758/full#supplementary-material
References
1. Deci EL, Ryan RM. Motivation, personality, and development within embedded social contexts: an overview of self-determination theory. In: Ryan RM, editor. The Oxford Handbook of Human Motivation. Oxford: Oxford University Press (2012). p. 84–108. doi: 10.1093/oxfordhb/9780195399820.013.0006
2. Ryan R, Deci E. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. (2000) 55:68–78. doi: 10.1037/0003-066X.55.1.68
3. Kusec A, Velikonja D, DeMatteo C, Harris JE. Motivation in rehabilitation and acquired brain injury: can theory help us understand it? Disabil Rehabil. (2019) 41:2343–9. doi: 10.1080/09638288.2018.1467504
4. Siegert RJ, Taylor WJ. Theoretical aspects of goal-setting and motivation in rehabilitation. Disabil Rehabil. (2004) 26:1–8. doi: 10.1080/09638280410001644932
5. Holmqvist LW, Koch LV. Environmental factors in stroke rehabilitation. BMJ. (2001) 322:1501–2. doi: 10.1136/bmj.322.7301.1501
6. Maclean N, Pound P. A critical review of the concept of patient motivation in the literature on physical rehabilitation. Soc Sci Med. (2000) 50:495–506. doi: 10.1016/s0277-9536(99)00334-2
7. Maclean N, Pound P, Wolfe C, Rudd A. The concept of patient motivation: a qualitative analysis of stroke professionals' attitudes. Stroke. (2002) 33:444–8. doi: 10.1161/hs0202.102367
8. Morris JH, Oliver T, Kroll T, Joice S, Williams B. Physical activity participation in community dwelling stroke survivors: synergy and dissonance between motivation and capability. A qualitative study. Physiotherapy. (2017) 103:311–21. doi: 10.1016/j.physio.2016.05.001
9. Maclean N, Pound P, Wolfe C, Rudd A. Qualitative analysis of stroke patients' motivation for rehabilitation. BMJ. (2000) 321:1051–4. doi: 10.1136/bmj.321.7268.1051
10. Poltawski L, Boddy K, Forster A, Goodwin VA, Pavey AC, Dean S. Motivators for uptake and maintenance of exercise: perceptions of long-term stroke survivors and implications for design of exercise programmes. Disabil Rehabil. (2015) 37:795–801. doi: 10.3109/09638288.2014.946154
11. Luker J, Lynch E, Bernhardsson S, Bennett L, Bernhardt J. Stroke survivors' experiences of physical rehabilitation: a systematic review of qualitative studies. Arch Phys Med Rehabil. (2015) 96:1698–708.e10. doi: 10.1016/j.apmr.2015.03.017
12. Eng XW, Brauer SG, Kuys SS, Lord M, Hayward KS. Factors affecting the ability of the stroke survivor to drive their own recovery outside of therapy during inpatient stroke rehabilitation. Stroke Res Treat. (2014) 2014:626538. doi: 10.1155/2014/626538
13. Resnick B, Michael K, Shaughnessy M, Kopunek S, Nahm ES, Macko RF. Motivators for treadmill exercise after stroke. Top Stroke Rehabil. (2008) 15:494–502. doi: 10.1310/tsr1505-494
14. Wang YH, Yang YR, Pan PJ, Wang RY. Modeling factors predictive of functional improvement following acute stroke. J Chin Med Assoc. (2014) 77:469–76. doi: 10.1016/j.jcma.2014.03.006
15. Tornbom K, Sunnerhagen KS, Danielsson A. Perceptions of physical activity and walking in an early stage after stroke or acquired brain injury. PLoS ONE. (2017) 12:e0173463. doi: 10.1371/journal.pone.0173463
16. Signal N, McPherson K, Lewis G, Kayes N, Saywell N, Mudge S, et al. What influences acceptability and engagement with a high intensity exercise programme for people with stroke? A qualitative descriptive study. Neurorehabilitation. (2016) 39:507–17. doi: 10.3233/NRE-161382
17. Damush TM, Plue L, Bakas T, Schmid A, Williams LS. Barriers and facilitators to exercise among stroke survivors. Rehabil Nurs. (2007) 32:253–60. doi: 10.1002/j.2048-7940.2007.tb00183.x
18. Lord SR, Delbaere K, Sturnieks DL. Aging. Handb Clin Neurol. (2018) 159:157–71. doi: 10.1016/B978-0-444-63916-5.00010-0
19. Chervinsky AB, Ommaya AK, deJonge M, Spector J, Schwab K, Salazar AM. Motivation for traumatic brain injury rehabilitation questionnaire (MOT-Q): reliability, factor analysis, and relationship to MMPI-2 variables. Arch Clin Neuropsychol. (1998) 13:433–46. doi: 10.1093/arclin/13.5.433
20. Boosman H, van Heugten CM, Winkens I, Smeets SM, Visser-Meily JM. Further validation of the motivation for traumatic brain injury rehabilitation questionnaire (MOT-Q) in patients with acquired brain injury. Neuropsychol Rehabil. (2016) 26:87–102. doi: 10.1080/09602011.2014.1001409
21. Oddy M, Cattran C, Wood R. The development of a measure of motivational changes following acquired brain injury. J Clin Exp Neuropsychol. (2008) 30:568–75. doi: 10.1080/13803390701555598
22. White G, Cordato D, O'Rourke F, Mendis R, Ghia D, Chan D. Validation of the stroke rehabilitation motivation scale: a pilot study. Asian J Gerontol Geriatr. (2012) 7:80–7.
23. Britten N, Jones R, Murphy E, Stacy R. Qualitative research methods in general practice and primary care. Fam Pract. (1995) 12:104–14. doi: 10.1093/fampra/12.1.104
24. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. (2006) 3:77–101. doi: 10.1191/1478088706qp063oa
25. Clarke V, Braun V. Teaching thematic analysis: overcoming challenges and developing strategies for effective learning. Psychologist. (2013) 26:120–3.
26. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health C. (2007) 19:349–57. doi: 10.1093/intqhc/mzm042
27. Bernhardt J, Hayward KS, Kwakkel G, Ward NS, Wolf SL, Borschmann K, et al. Agreed definitions and a shared vision for new standards in stroke recovery research: the Stroke Recovery and Rehabilitation Roundtable taskforce. Int J Stroke. (2017) 12:444–50. doi: 10.1177/1747493017711816
28. Keith RA, Granger CV, Hamilton BB, Sherwin FS. The functional independence measure: a new tool for rehabilitation. Adv Clin Rehabil. (1987) 1:6–18.
30. Aburn G, Gott M, Hoare K. What is resilience? An integrative review of the empirical literature. J Adv Nurs. (2016) 72:980–1000. doi: 10.1111/jan.12888
31. Kim SI. Neuroscientific model of motivational process. Front Psychol. (2013) 4:98. doi: 10.3389/fpsyg.2013.00098
32. Thompson SC, Sobolew-Shubin A, Graham MA, Janigian AS. Psychosocial adjustment following a stroke. Soc Sci Med. (1989) 28:239–47.
33. Evans SA, Airey MC, Chell SM, Connelly JB, Rigby AS, Tennant A. Disability in young adults following major trauma: 5 year follow up of survivors. BMC Public Health. (2003) 3:1. doi: 10.1186/1471-2458-3-8
Keywords: motivation, stroke, rehabilitation, qualitative study, age
Citation: Yoshida T, Otaka Y, Osu R, Kumagai M, Kitamura S and Yaeda J (2021) Motivation for Rehabilitation in Patients With Subacute Stroke: A Qualitative Study. Front. Rehabilit. Sci. 2:664758. doi: 10.3389/fresc.2021.664758
Received: 06 February 2021; Accepted: 26 April 2021;
Published: 07 June 2021.
Edited by:
Winand H. Dittrich, FOM University of Applied Sciences for Economics and Management, GermanyReviewed by:
Ingmar Matthes Schenk, Rehaklinik Bellikon, SwitzerlandElena Vasilchenko, FSBI Novokuznetsk Scientific and Practical Centre for Medical and Social Expertise and Rehabilitation of Disabled Persons, Russia
Copyright © 2021 Yoshida, Otaka, Osu, Kumagai, Kitamura and Yaeda. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yohei Otaka, b3Rha2ExMTlAbWFjLmNvbQ==
 Taiki Yoshida
Taiki Yoshida Yohei Otaka
Yohei Otaka Rieko Osu
Rieko Osu Masashi Kumagai
Masashi Kumagai Shin Kitamura
Shin Kitamura Jun Yaeda6
Jun Yaeda6