- 1Medical Student, King George's Medical University, Lucknow, UP, India
- 2Department of Geriatric Mental Health, King George's Medical University, Lucknow, UP, India
- 3Department of Community Medicine, King George's Medical University, Lucknow, UP, India
- 4Diagnostic Radiography Technology Department, Faculty of Applied Medical Sciences, Jazan University, Jazan, Saudi Arabia
- 5School of Medical Science and Research Center, AlFalah University, Faridabad, Haryana, India
- 6Institute of Medical Sciences, University of Aberdeen, Aberdeen, United Kingdom
Background: Hypertension is a potentially modifiable risk factor for cognitive decline. Understanding the variables of hypertension related to cognitive functions will help in mitigating the risk.
Objective: The study aims to assess the characteristics of hypertension and its effect on cognitive functions in the older adults.
Methods: The study involved 95 hypertensive participants aged 60 years and above from cardiology and medicine outpatient services of a tertiary care hospital from August to October 2022. The characteristics of hypertension and cognitive functions were assessed using semi-structured proforma and Adenbrooke's Cognitive Examination (ACE-III) Hindi version respectively. Further, individual cognitive functions were compared with duration of the hypertension and hypertensive status of the participants. The chi-square test and independent t-tests were used and p value < 0.05 was considered to be significant.
Result: The mean age of the study population was 68.2 years, the cognitive functions was comparable in terms of age, sex, locality, co-morbidity, and treatment characteristic. Although a significant difference in cognitive functions was present in relation to duration and status of hypertension. Among the individual cognitive domains, a significant difference was observed in attention and fluency domains of cognitive function based on HTN status (p > 0.05) but differential effect on cognitive domains was not seen with the duration of HTN. However, there was overall decline in cognitive domains with both hypertension status and the duration of hypertension.
Conclusion: The study highlights association of status of hypertension and its characteristics with cognitive decline.
Introduction
Worldwide, hypertension is a significant risk factor for cardiovascular disease and mortality (Mills and Stefanescu, 2020). It is also a leading cause of cognitive impairment and dementia (Iadecola et al., 2019). Hypertension affects one-third of adults and two-thirds of the older adults, with higher prevalence in low- and middle-income countries (Mills et al., 2016; Ungvari et al., 2021). In India, the prevalence of HTN is 29.8%. Higher rates are seen in urban population (33.85%) compared to rural population (27.6%) (Anchala et al., 2014). According to the longitudinal aging study of India (LASI), HTN prevalence among people aged 45 and above is 45.9% in India, with only 31.7% having their blood pressure under control (Lee et al., 2022). HTN is characterized by exceeding systolic BP of 140 mmHg and diastolic BP of 90 mmHg (Muntner et al., 2020). Individuals with BP levels below this threshold are considered to have controlled HTN within the hypertensive population (Gillespie and Hurvitz, 2013).
HTN exerts a direct influence on both the vasculature and brain structure, increasing the likelihood of end-organ damage. This raises the risk of cognitive impairment and dementia (Gasecki et al., 2013). HTN has been linked to cognitive impairment through several pathophysiological mechanisms, including reduced cerebral blood flow, rarefaction of microvasculature, disruption of the blood-brain barrier (BBB), oxidative stress, and impaired neurovascular coupling. Moreover, it is worth noting that cerebral micro-hemorrhages, lacunar infarcts, and white matter (WM) injuries are frequently observed in individuals with both hypertension and dementia (Ungvari et al., 2021). Mid-life hypertension carries a lifetime risk of 20%−54% of developing dementia (McGrath et al., 2017). Previous studies have shown that the risk of vascular events and strokes doubles with uncontrolled HTN and subsequently increases the risk of dementia. Chronic uncontrolled hypertension reduces elasticity and increases vascular resistance, resulting in higher pulse pressure and increased risk for cognitive impairment due to WM lesions and transient hemorrhage (Beason-Held et al., 2007; Mitchell, 2008). HTN is a recognized risk factor for both vascular cognitive impairment and Alzheimer's Disease (AD), which often co-exist and constitute the majority of cases of dementia (Wei et al., 2018; Iadecola and Gottesman, 2019). Incidental neuroimaging and post-mortem studies on people with AD reveal vascular pathology in approximately one-third of the patients (Snowdon et al., 1997; Schneider et al., 2004).
Considering the modifiability of HTN in the early stages and understanding its characteristics, we can elucidate its role in cognition. This will further aid in understanding the mechanisms involved in developing cognitive impairment and exploring newer therapeutic targets. Although previous studies highlighted mid-life hypertension as a common risk factor for developing dementia, late-life hypertension is less studied, and the results are variable. Moreover, several studies in the past have tried to explore the impact of controlled HTN on halting the progression of cognitive decline but the evidence is inconsistent (Mishra et al., 2020). The current study aimed to explore the characteristics of HTN and its impact on cognitive functions in the older adults. It could contribute to existing knowledge and enhance clinical practice. This knowledge could guide healthcare professionals in implementing preventive measures, optimizing hypertension management, and developing interventions to preserve cognitive health in older adults with hypertension. Ultimately, this research could improve the quality of life and overall wellbeing of older adults by addressing the complex relationship between hypertension and cognitive functions.
Materials and methods
Participants
The study involved the enrolment of 95 participants with a diagnosis of hypertension and their demographics and clinical data were obtained from the Cardiology and Medicine Outpatient Department (OPD) at King George's Medical University (KGMU) in Lucknow, spanning the period of September through October 2022. The selection of participants was done using a purposive sampling technique. This cross-sectional study was conducted after obtaining approval from the Institutional Ethical Committee, with reference number XIPGTSCIB/P3. The study was conducted in accordance with the ethical standards set forth by the institutional and national committees responsible for human experimentation, as well as the Helsinki Declaration of 1975, which was subsequently revised in 2013.
Inclusion and exclusion criteria
The inclusion criteria for both participants were: (1) hypertensive patients of age 60 years or above; (2) participants with at least 5 years of formal education who can read and write. The exclusion criteria for both participants were: (1) patients with severe vision and hearing impairment; (2) patients with any known psychiatric and cognitive disorders; and (3) Severely ill and uncooperative participants.
Sample size
According to a previous study (Mekala et al., 2020), the occurrence of cognitive impairment within the North Indian population is reported to be 8.8% (Sengupta et al., 2014). The calculation of the sample size (n) is determined using the formula; n = (zα/2)2 *P(1-p)/MOE2. Given a confidence level of 95%, a proportion (p) of 0.088, a margin of error (MOE) of 0.06, and a value of zα/2 equals 1.96, the sample size (n) was determined to be 84. After accounting for a non-responsive rate of 10%, the final sample size is determined to be 92, which was rounded up to 95.
Clinical measures (hypertension and cognition)
The participants were evaluated using a semi-structured proforma for socio-demographic and clinical details. Patients were analyzed based on their current BP, HTN duration, and status (Controlled and uncontrolled HTN). The definition of controlled hypertension in hypertensive individuals is SBP <140 mm Hg and DBP <90 mm Hg (Gillespie and Hurvitz, 2013). They were asked the following questions about hypertension: “When were they first diagnosed with hypertension?” for determining the age of onset of HTN, “Are they under treatment for HTN, and if yes, how long have they been under medication?” and “Are they taking medications regularly?” The family history of patients and the history of any other medical co-morbidity were also taken. The treatment in this study refers to subjects on antihypertensive medications at any point in time after the diagnosis of HTN. The cognition of participants was evaluated using the Adenbrooke's Cognitive Examination (ACE) III Hindi version (Mekala et al., 2020). The ACE scale assesses the cognition of a person using five domains: attention, fluency, memory, language, and visuospatial. Each domain carries a different score, and a higher total score implies better cognition. Using the total ACE score, a cut-off of 71 was considered for classifying the subjects as cognitively normal, and impaired (Bajpai et al., 2020).
Data analysis
Data was collected using a semi-structured proforma and the ACE III Hindi version. This data was tabulated in Microsoft EXCEL, and statistical analysis was done on the Statistical Package for Social Sciences (SPSS), version 24, IBM, Chicago, USA. Descriptive data were represented as frequency percentage, mean, standard deviation (SD), or proportion. Probability (p) was calculated to test for statistical significance at the 5% level of significance. The association between categorical variables was tested using the Chi-Square test. However, differences between continuous variables were tested using the student t-test. A minimum 95% confidence interval or p-value <0.05 was considered statistically significant.
Results
Participant characteristics
The current cross-sectional study included a sample of 95 participants diagnosed with HTN with a mean age of 68.2 ± 3.29 years. The mean age of onset of HTN was 62.64 ± 3.69 years and the mean duration of HTN was 5.53 ± 1.86 years in the participants. No statistically significant differences in cognitive functions were observed based on gender, age, and residence areas (urban or rural) (all p > 0.80). A total of 90 subjects were on treatment; among 77 subjects with uncontrolled HTN, 4 were not on treatment. Statistically significant differences in cognitive functions were observed with the duration of HTN, Blood pressure measures (Systolic and Diastolic blood pressure), HTN status, and duration of treatment, as indicated by chi-square tests (P < 0.05). Table 1 displays the demographic and clinical characteristics associated with cognitive functions.
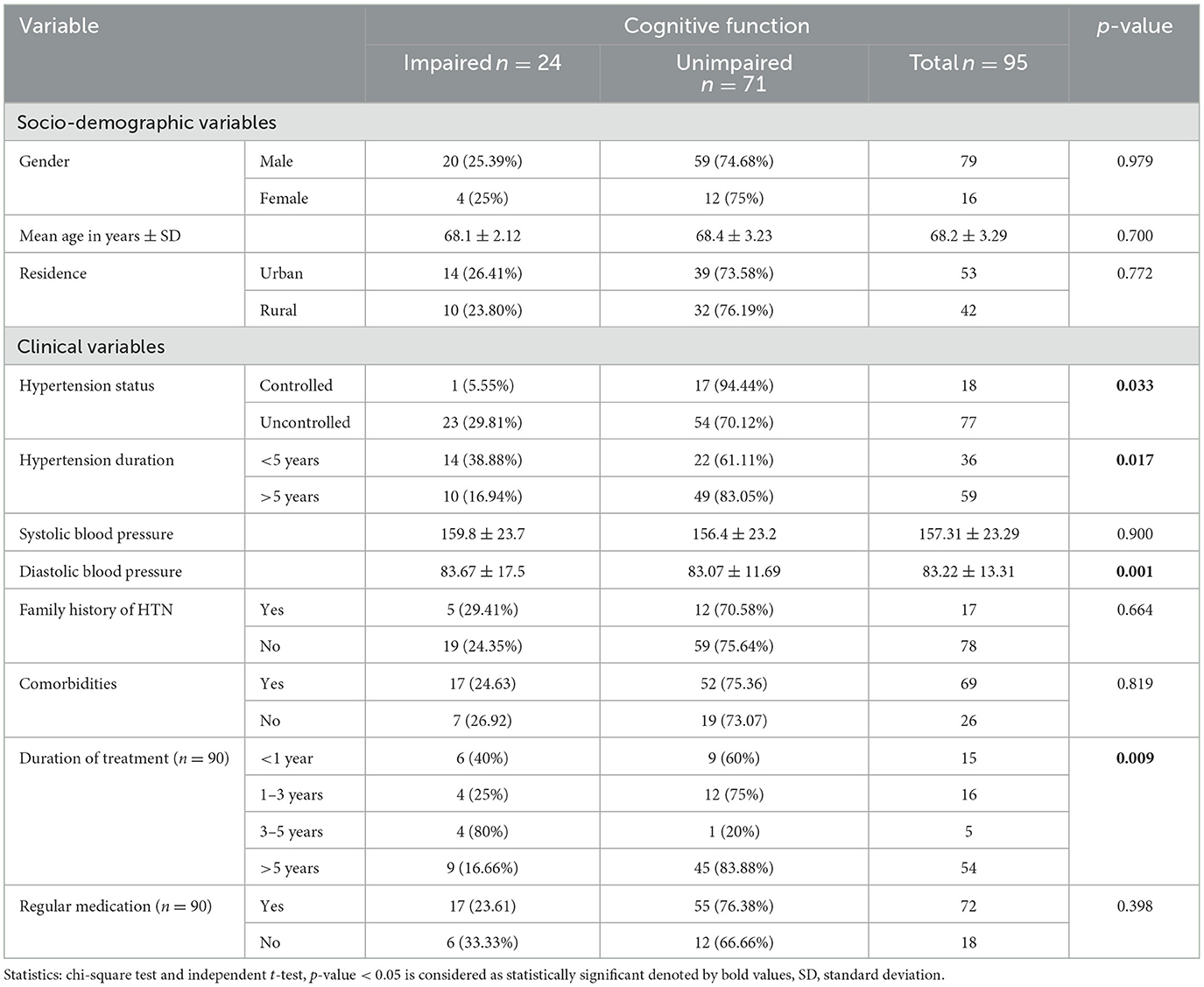
Table 1. Comparison of socio-demographic and clinical characteristics of subjects with Hypertension with and without cognitive impairment.
Comparison of cognitive functions based on the status of HTN
There was a significant difference in overall cognitive function and in domains of attention and fluency according to HTN status with p-values of 0.04, 0.01, and 0.02 respectively (Table 2).

Table 2. Comparison of cognitive subdomains of ACE score based on the status and duration of Hypertension among the study population.
Comparison of cognitive functions based on the duration of HTN
There was a significant difference in overall cognitive function score based on the duration of HTN (<5 years and >5 years) with p 0.04 (Table 2). However, individual cognitive domains did not differ based on the duration of HTN.
Discussion
HTN and cognitive impairment are the two most frequently occurring conditions in the older adults (Iadecola et al., 2019) and the current study is the first to investigate the characteristics of HTN and its impact on cognitive functions in older adults of India. Notably, 95.8% of people with cognitive impairment in this study had uncontrolled HTN. People with uncontrolled HTN had poorer cognitive functions compared to people with controlled hypertension. This is in accordance with a recent study in which hypertensive individuals with uncontrolled BP had more cognitive impairment in comparison to controlled hypertensives (de Menezes et al., 2021). Our findings also support another study reporting chronic uncontrolled HTN can lead to cognitive impairment as it increases the risk of white matter lesions by increasing vascular resistance and vessel wall stiffening and it can be inferred that the risk of cognitive impairment was higher in uncontrolled hypertensives than in controlled hypertensives (Mitchell, 2008). Moreover, people with <5 years of duration of HTN had more chances of developing cognitive impairment in comparison to hypertensives of >5 years duration (38.88% vs. 16.94%) which is not in agreement with the studies reporting midlife hypertensives are at increased risk cognitive impairment (Launer et al., 1995; Livingston et al., 2020). Moreover, a recent study reported minimal effect of late-life hypertension on cognition (Moll and Woodard, 2022). However, a few other studies have reported an association of late-life hypertension with cognitive impairment in older adults and suggested that the association between cognition and hypertension is age-dependent (Wei et al., 2018).
HTN is a modifiable risk factor for cognitive impairment and it can be presumed that it can be modified by antihypertensive treatment at early stages to reduce the risk of cognitive impairment (Wei et al., 2018). Notably, the people with regular medication for a duration of 3–5 years had more chances of developing cognitive impairment in comparison to people who were commenced on antihypertensive medications recently (<3 years) or more than 5 years ago which contradicts the findings of a meta-analysis suggesting reduced risk of incident dementia with antihypertensive use as antihypertensive use for 3–5 years had higher impairment in cognition (Ding et al., 2020). It suggests that antihypertensive use can modify the disease or reduce the risk of dementia for the initial few years and causes cognitive decline later as low and high blood pressure both can increase the risk of cognitive impairment (Ding et al., 2020) and blood pressure variability in older people increases the risk of dementia (Razay et al., 2009; Oishi et al., 2017). However, people on antihypertensive treatment with more than 5 years duration of hypertension had less chance of cognitive impairment and this supports the findings that early commencement of treatment with antihypertensive medication may be associated with better cognitive functions later in life (Mogi, 2022).
On further evaluation of individual cognitive domains with HTN status, the domains were differentially affected as the attention and fluency differ significantly in controlled and uncontrolled hypertensives. The uncontrolled hypertensives had lower scores on attention and fluency in comparison to controlled hypertensives and it seems like attention is primarily affected cognitive domain with uncontrolled hypertension as fluency is a cognitive skill directly associated with attention and working memory (Francisco et al., 2019). A deficit in attention due to uncontrolled hypertension may lead to a deficit in verbal fluency and this contradicts the earlier findings that hypertension affects cognitive processing speed and episodic and working memory but not attention (Saxby et al., 2003). However, the differential effect on specific cognitive domains was not seen with the duration of hypertension, and an overall deficit in cognitive scores was found in the people with a lesser duration of the illness in this study which is not per a previous study reporting deficit in only verbal memory with duration of hypertension (Zhou et al., 2022). Our study also contradicts the findings that midlife hypertension has a greater risk for cognitive impairment in comparison to late-life hypertension (Livingston et al., 2020).
Limitations of the study
The current study has several limitations including this study was conducted with a limited sample size, suggesting that it may be prone to overestimating the magnitude of the effect size and the sample population may not be representative of the general population as this is a hospital-based study. Further, a multi-centric study with a large sample size is required to overcome the limitations of the study. Moreover, longitudinal studies are needed to find the association between the trajectory of cognitive decline and characteristics of hypertension in subjects with hypertension.
Conclusion
This study highlighted the impact of hypertension characteristics including hypertension status (controlled and uncontrolled) and duration of hypertension with cognitive functions. Uncontrolled hypertensives had poorer cognitive functions in comparison to controlled hypertensives. Moreover, there was a differential impact of uncontrolled hypertension on cognitive domains as attention and fluency were more affected in comparison to other cognitive domains. Interestingly, those with a shorter duration of HTN had lower cognitive scores than those with a longer HTN duration.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the King George's Medical University, U.P., Intitutional Ethics Committee, Lucknow (UP), India. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
Author contributions
NP: Writing – original draft, Methodology. PC: Writing – review & editing, Formal analysis. SS: Writing – review & editing, Formal analysis. PP: Formal analysis, Writing – review & editing. NM: Writing – review & editing, Formal analysis. NQ: Writing – review & editing, Formal analysis. ST: Writing – original draft, Supervision, Conceptualization.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research did not receive any specific grant from any funding agency in the public, commercial, or not-for-profit sector. However, this research has been conducted as part of a short-term studentship scheme from the Indian Council of Medical Research (2022-09236).
Acknowledgments
The authors are very grateful to the study participants, data collectors, and supervisors.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Anchala, R., Kannuri, N. K., Pant, H., Khan, H., Franco, O. H., Di Angelantonio, E., et al. (2014). Hypertension in India: a systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J. Hypertens. 32, 1170–1177. doi: 10.1097/HJH.0000000000000146
Bajpai, S., Upadhyay, A., Sati, H., Pandey, R., Chaterjee, P., Dey, S., et al. (2020). Hindi Version of Addenbrooke's cognitive examination III: distinguishing cognitive impairment among older Indians at the lower cut-offs. Clin. Interv. Aging. 15, 329–339. doi: 10.2147/CIA.S244707
Beason-Held, L. L., Moghekar, A., Zonderman, A. B., Kraut, M. A., and Resnick, S. M. (2007). Longitudinal changes in cerebral blood flow in the older hypertensive brain. Stroke 38, 1766–1773. doi: 10.1161/STROKEAHA.106.477109
de Menezes, S. T., Giatti, L., Brant, L. C. C., Griep, R. H., Schmidt, M. I., Duncan, B. B., et al. (2021). Hypertension, prehypertension, and hypertension control: association with decline in cognitive performance in the ELSA-Brasil cohort. Hypertension 77, 672–681. doi: 10.1161/HYPERTENSIONAHA.120.16080
Ding, J., Davis-Plourde, K. L., Sedaghat, S., Tully, P. J., Wang, W., Phillips, C., et al. (2020). Antihypertensive medications and risk for incident dementia and Alzheimer's disease: a meta-analysis of individual participant data from prospective cohort studies. Lancet Neurol. 19, 61–70. doi: 10.1016/S1474-4422(19)30393-X
Francisco, H. C., Brigola, A. G., Ottaviani, A. C., dos Santos-Orlandi, A. A., de Orlandi, F. S., Fraga, F. J., et al. (2019). Relationship between cognitive processing, language and verbal fluency among elderly individuals. Dement Neuropsychol. 13, 299–304. doi: 10.1590/1980-57642018dn13-030006
Gasecki, D., Kwarciany, M., and Nyka, W. (2013). Hypertension, brain damage and cognitive decline. Curr. Hypert. Rep. 15, 547–558. doi: 10.1007/s11906-013-0398-4
Gillespie, C. D., and Hurvitz, K. A. (2013). Centers for Disease Control and Prevention (CDC). Prevalence of hypertension and controlled hypertension - United States, 2007-2010. MMWR Suppl. 62, 144–148.
Iadecola, C., Duering, M., Hachinski, V., Joutel, A., Pendlebury, S. T., Schneider, J. A., et al. (2019). Vascular cognitive impairment and dementia: JACC scientific expert panel. J. Am. Coll. Cardiol. 73, 3326–3344. doi: 10.1016/j.jacc.2019.04.034
Iadecola, C., and Gottesman, R. F. (2019). Neurovascular and cognitive dysfunction in hypertension. Circ. Res. 124, 1025–1044. doi: 10.1161/CIRCRESAHA.118.313260
Launer, L. J., Masaki, K., Petrovitch, H., Foley, D., and Havlik, R. J. (1995). The association between midlife blood pressure levels and late-life cognitive function. The Honolulu-Asia aging study. JAMA. 274, 1846–1851. doi: 10.1001/jama.1995.03530230032026
Lee, J., Wilkens, J., Meijer, E., Sekher, T. V., Bloom, D. E., Hu, P., et al. (2022). Hypertension awareness, treatment, and control and their association with healthcare access in the middle-aged and older Indian population: a nationwide cohort study. PLoS Med. 19:e1003855. doi: 10.1371/journal.pmed.1003855
Livingston, G., Huntley, J., Sommerlad, A., Ames, D., Ballard, C., Banerjee, S., et al. (2020). Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 396, 413–446. doi: 10.1016/S0140-6736(20)30367-6
McGrath, E. R., Beiser, A. S., DeCarli, C., Plourde, K. L., Vasan, R. S., Greenberg, S. M., et al. (2017). Blood pressure from mid- to late life and risk of incident dementia. Neurology 89, 2447–2454. doi: 10.1212/WNL.0000000000004741
Mekala, S., Paplikar, A., Mioshi, E., Kaul, S., Divyaraj, G., Coughlan, G., et al. (2020). Dementia diagnosis in seven languages: the Addenbrooke's Cognitive Examination-III in India. Arch. Clin. Neuropsychol. 35, 528–538. doi: 10.1093/arclin/acaa013
Mills, K. T., Bundy, J. D., Kelly, T. N., Reed, J. E., Kearney, P. M., Reynolds, K., et al. (2016). Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation 134, 441–450. doi: 10.1161/CIRCULATIONAHA.115.018912
Mills, K. T., and Stefanescu, A. (2020). The global epidemiology of hypertension. Nat. Rev. Nephrol. 16, 223–237. doi: 10.1038/s41581-019-0244-2
Mishra, N., Mohan, D., Fuad, S., Basavanagowda, D. M., Alrashid, Z. A., Kaur, A., et al. (2020). The association between hypertension and cognitive impairment, and the role of antihypertensive medications: a literature review. Cureus 12:e12035. doi: 10.7759/cureus.12035
Mitchell, G. F. (2008). Effects of central arterial aging on the structure and function of the peripheral vasculature: implications for end-organ damage. J. Appl. Physiol. 105, 1652–1660. doi: 10.1152/japplphysiol.90549.2008
Mogi, M. (2022). Hypertension management to prevent dementia. Hypert. Res. 45, 573–575. doi: 10.1038/s41440-022-00869-5
Moll, A. C., and Woodard, J. L. (2022). Hypertension and cognition are minimally associated in late life. Hypertens. Res. 45, 1622–1631. doi: 10.1038/s41440-022-00970-9
Muntner, P., Hardy, S. T., Fine, L. J., Jaeger, B. C., Wozniak, G., Levitan, E. B., et al. (2020). Trends in blood pressure control among US adults with hypertension, 1999-2000 to 2017-2018. JAMA 324, 1190–1200. doi: 10.1001/jama.2020.14545
Oishi, E., Ohara, T., Sakata, S., Fukuhara, M., Hata, J., Yoshida, D., et al. (2017). Day-to-day blood pressure variability and risk of dementia in a general Japanese elderly population: the Hisayama Study. Circulation 136, 516–525. doi: 10.1161/CIRCULATIONAHA.116.025667
Razay, G., Williams, J., King, E., and Smith, A. D. (2009). Blood pressure, dementia and Alzheimer's disease: the OPTIMA longitudinal study. Dement Geriatr. Cogn. Disor. 28, 70–74. doi: 10.1159/000230877
Saxby, B. K., Harrington, F., McKeith, I. G., and Wesnes, K. (2003). Effects of hypertension on attention, memory, and executive function in older adults. Health Psychol. 22:587. doi: 10.1037/0278-6133.22.6.587
Schneider, J. A., Wilson, R. S., Bienias, J. L., Evans, D. A., and Bennett, D. A. (2004). Cerebral infarctions and the likelihood of dementia from Alzheimer disease pathology. Neurology 62, 1148–1155. doi: 10.1212/01.WNL.0000118211.78503.F5
Sengupta, P., Benjamin, A. I., and Singh, Y. (2014). Prevalence and correlates of cognitive impairment in a north Indian elderly population. WHO South-East Asia J. Public Health 3, 135–143. doi: 10.4103/2224-3151.206729
Snowdon, D. A., Greiner, L. H., Mortimer, J. A., Riley, K. P., Greiner, P. A., Markesbery, W. R., et al. (1997). Brain infarction and the clinical expression of Alzheimer disease. The nun study. JAMA 277, 813–817. doi: 10.1001/jama.1997.03540340047031
Ungvari, Z., Toth, P., Tarantini, S., Prodan, C. I., Sorond, F., Merkely, B., et al. (2021). Hypertension-induced cognitive impairment: from pathophysiology to public health. Nat. Rev. Nephrol. 17, 639–654. doi: 10.1038/s41581-021-00430-6
Wei, J., Yin, X., Liu, Q., Tan, L., and Jia, C. (2018). Association between hypertension and cognitive function: a cross-sectional study in people over 45 years old in China. J. Clin. Hypert. 20, 1575–1583. doi: 10.1111/jch.13393
Keywords: hypertension, cognitive functions, cognition, older adults, late life
Citation: Parandiyal N, Chutia P, Sinha SS, Pandit P, Majrashi NA, Qureshi N and Tripathi SM (2024) Characteristics of hypertension and its impact on cognitive functions in older adults: a cross-sectional study. Front. Dement. 3:1486147. doi: 10.3389/frdem.2024.1486147
Received: 25 August 2024; Accepted: 05 November 2024;
Published: 26 November 2024.
Edited by:
Kristin Rene Krueger, Rush University Medical Center, United StatesReviewed by:
Celeste Annemarie De Jager Loots, Imperial College London, United KingdomCiro Gaona, Alzheimer's Foundation of Venezuela, Venezuela
Copyright © 2024 Parandiyal, Chutia, Sinha, Pandit, Majrashi, Qureshi and Tripathi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shailendra Mohan Tripathi, ZHJfc210cmlwYXRoaUByZWRpZmZtYWlsLmNvbQ==
 Nivedita Parandiyal
Nivedita Parandiyal Porimita Chutia
Porimita Chutia Shashank Saurabh Sinha
Shashank Saurabh Sinha Pratyaksha Pandit
Pratyaksha Pandit Naif Ali Majrashi
Naif Ali Majrashi Naseem Qureshi5
Naseem Qureshi5 Shailendra Mohan Tripathi
Shailendra Mohan Tripathi