- 1Rehabilitation Sciences Institute, Temerty Faculty of Medicine, University of Toronto, Toronto, ON, Canada
- 2Toronto Rehabilitation Institute, KITE Research Institute, University Health Network, Toronto, ON, Canada
- 3Department of Medicine, Geras Centre for Aging Research, McMaster University, Hamilton, ON, Canada
- 4Department of Occupational Science and Occupational Therapy, Temerty Faculty of Medicine, University of Toronto, Toronto, ON, Canada
- 5Department of Physical Therapy, Temerty Faculty of Medicine, University of Toronto, Toronto, ON, Canada
- 6Psychology Department, Northumbria University, Newcastle upon Tyne, United Kingdom
Background: Concerns about falling (e.g., low balance confidence) increase fall risk in older populations with balance impairments. Exercise can improve physical limitations associated with falls (e.g., poor balance), which are more prevalent in people with Mild Cognitive Impairment (MCI) and dementia. This scoping review aimed to understand exercise interventions targeting concerns about falling in people with MCI and dementia.
Methods: Using Arksey and O'Malley's five-stage scoping review framework, 968 search combinations were run across six electronic databases from inception to September 15, 2023. Articles were available in English full text, featured original peer-reviewed research with an intervention study design, targeted people with MCI or dementia with the exercise intervention, and included concerns about falling as an outcome measure.
Results: Of the 2,111 articles screened, 27 met the inclusion criteria. Only one article looked at concerns about falling as a primary outcome; in the remaining studies, concerns about falling were a secondary outcome. Multi-modal interventions (i.e., containing more than one type of exercise) were most common, with balance and strength as the most frequently employed exercise types. Secondary results are presented on (i) intervention details, (ii) outcomes and measures for concerns about falling, (iii) participant accommodations, and (iv) components of effective interventions for concerns about falling.
Conclusions: There is a lack of focus on concerns about falling experienced by people with MCI and dementia. Although concerns about falling were not the primary outcome of most papers, the results highlight the potential of exercise interventions to help address concerns about falling and other fall risk factors (e.g., balance, cognition) in people with MCI and dementia.
1 Introduction
Falls are a significant public health problem and the second leading cause of unintentional injury deaths worldwide (World Health Organization, 2021). Globally, an estimated 684,000 people die of falls each year, with the most significant proportion of fallers being older adults aged 60 years and above (World Health Organization, 2021). For people living with mild cognitive impairment (MCI) and dementia, most of whom are older adults (Sachdev et al., 2014), falls are two to eight times more likely to occur than in older adults without dementia (Meuleners et al., 2016), making cognitive impairment an independent risk factor for falling (Hsu et al., 2012).
In addition to cognition, the risk of falls in MCI and dementia is also linked to physical factors, such as balance impairments (Mazoteras Muñoz et al., 2010). For example, a study of people with subjective cognitive impairment, MCI, and Alzheimer's disease found balance impairments in all groups, with the impairment levels increasing with the severity of cognitive impairment (Tangen et al., 2014). Concerns about falling (e.g., fear of falling) are defined as “a persistent feeling related to one's risk of falling during daily activities” (Neuroscience Research Australia, 2020). These concerns are widely known to increase the occurrence of falls in older adults without cognitive impairment (Asai et al., 2022). Among older adults without cognitive impairment, concerns about falling have been associated with factors such as activity avoidance, poor perceived health, and history of multiple falls (Zijlstra et al., 2007). Fear of falling (a specific concern about falling) has also been associated with lower muscle strength and worse balance performance among community-residing older adults (Deshpande et al., 2009). Further to this, concerns about falling have been associated with cognitive impairment (Uemura et al., 2014) and can also increase fall risk in people with MCI and dementia (Borges et al., 2014).
Exercise interventions for people with MCI and dementia have primarily focused on physical outcomes, particularly considering the challenges individuals with MCI and dementia experience with recall and abstract thinking required during traditional concerns about falling assessments (Delbaere et al., 2013). To mitigate this challenge, the Iconographical Falls Efficacy Scale was developed using pictorial cues to assess individuals' concerns about falling during daily activities (Delbaere et al., 2011). This visual augmentation can be helpful for individuals with cognitive impairment, as it provides a more concrete and accessible way to express their confidence in physical activities related to falls (Delbaere et al., 2013).
A systematic review and meta-analysis of 43 clinical trials demonstrated that 2–3 h per week of supervised, multi-modal physical exercise (i.e., using more than one exercise type) improved strength, balance, mobility, and endurance in people with MCI and dementia (Lam F. M. et al., 2018). However, evidence regarding the impact of improving physical outcomes on fall prevention and risk management in people with MCI and dementia is less consistent (Burton et al., 2015; Li et al., 2021; Booth et al., 2015). Exercise could be a way to address concerns about falling in people with MCI and dementia. However, our understanding of how physical exercise interventions for fall risk may influence concerns about falling in people with MCI or dementia is limited.
This scoping review aimed to understand exercise interventions targeting concerns about falling in people with MCI and dementia. The secondary aims of this review were to explore how interventions were delivered (e.g., in-person, group-based, clinic-based), the constructs and assessment tools used to measure concerns about falling, any accommodations made for participants with MCI and dementia, and the components of effective interventions addressing concerns about falling.
2 Methods
2.1 Design
We utilized a scoping review methodology to map the current landscape of exercise interventions to target concerns about falling in people living with MCI and dementia. A five-stage scoping review framework (Arksey and O'Malley, 2005) involved (i) identifying the research question(s), (ii) study selection, (iii) screening and selecting relevant publications, (iv) charting the data, and (v) collating, summarizing, and reporting the results. In addition to (Arksey and O'Malley, 2005), we also followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for scoping reviews (PRISMA-ScR) checklist (Tricco et al., 2018) to ensure rigor in review conduct and reporting.
2.1.1 Identifying the research questions
The primary research question for this scoping review was: “Are there any exercise interventions targeting concerns about falling in people with MCI and dementia?”
Secondary review questions included the following:
1. “How were the interventions delivered (e.g., in-person) and in what setting and format?”
2. “What constructs and assessment tools were used to examine concerns about falling before and after the interventions?”
3. “What accommodations were made to support people with MCI and dementia to participate in the interventions, if any?”
4. “What were components of effective interventions for addressing concerns about falling?”
2.1.2 Study selection
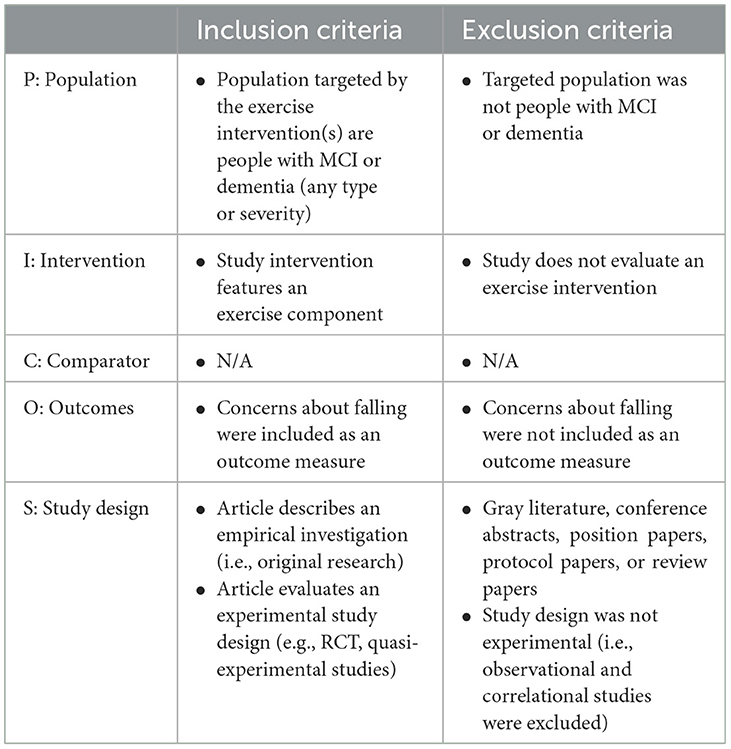
To identify relevant studies, 968 search combinations were systematically applied across six electronic databases accessible through an institutional library. The search strategy was developed using a modified version of the Population, Intervention, Comparator, Outcome, and Study design (PICOS) model (da Costa Santos et al., 2007) (see Table 1). The searched databases included MEDLINE (Ovid), Embase (Ovid), CINAHL (EBSCO), Ageline (EBSCO), AMED (Ovid), and PsycINFO (Ovid).
Each term listed under its respective column was combined within and across. Where possible, search terms were expanded to include as many synonyms as possible to ensure all word variations were captured. The search was undertaken on September 15, 2023. Hand searches of retrieved articles (e.g., checking reference lists of relevant articles) were completed to generate additional results, where possible.
Once the final search strategy was confirmed with an institutional librarian, the formal searches were run across the databases. Search results from the databases were de-duplicated to remove matching publications before the title and abstract screening. All retrieved articles were tracked through database searching and hand-searching, and the number of duplicates removed was tracked using review management software.
2.1.3 Screening and selecting relevant publications
Next, each article was screened against the review's inclusion and exclusion criteria, based on an adapted version of the PICOS model (da Costa Santos et al., 2007) (see Table 2). Articles were published within any timeframe. Only studies written in English were chosen as the authors can only read and understand English. The purpose of a scoping review is to map the breadth of literature on a given topic (Arksey and O'Malley, 2005). Therefore, feasibility studies were included if they met the criteria of an exercise intervention with concerns about falling as a primary or secondary outcome.
First, two reviewers independently screened all database hits at the title and abstract levels. Both reviewers had similar experiences and had previously published scoping reviews. Reasons for excluding articles at the title and abstract stages were determined by comparing the articles against the inclusion and exclusion criteria. Discrepancies identified were resolved through discussion between the two reviewers, with the option of bringing in a third reviewer if consensus was not achieved. If a reviewer was unsure whether an article met the eligibility criteria based on the title and abstract, the article was included in the full-text screening process to ensure that potentially relevant literature was not overlooked.
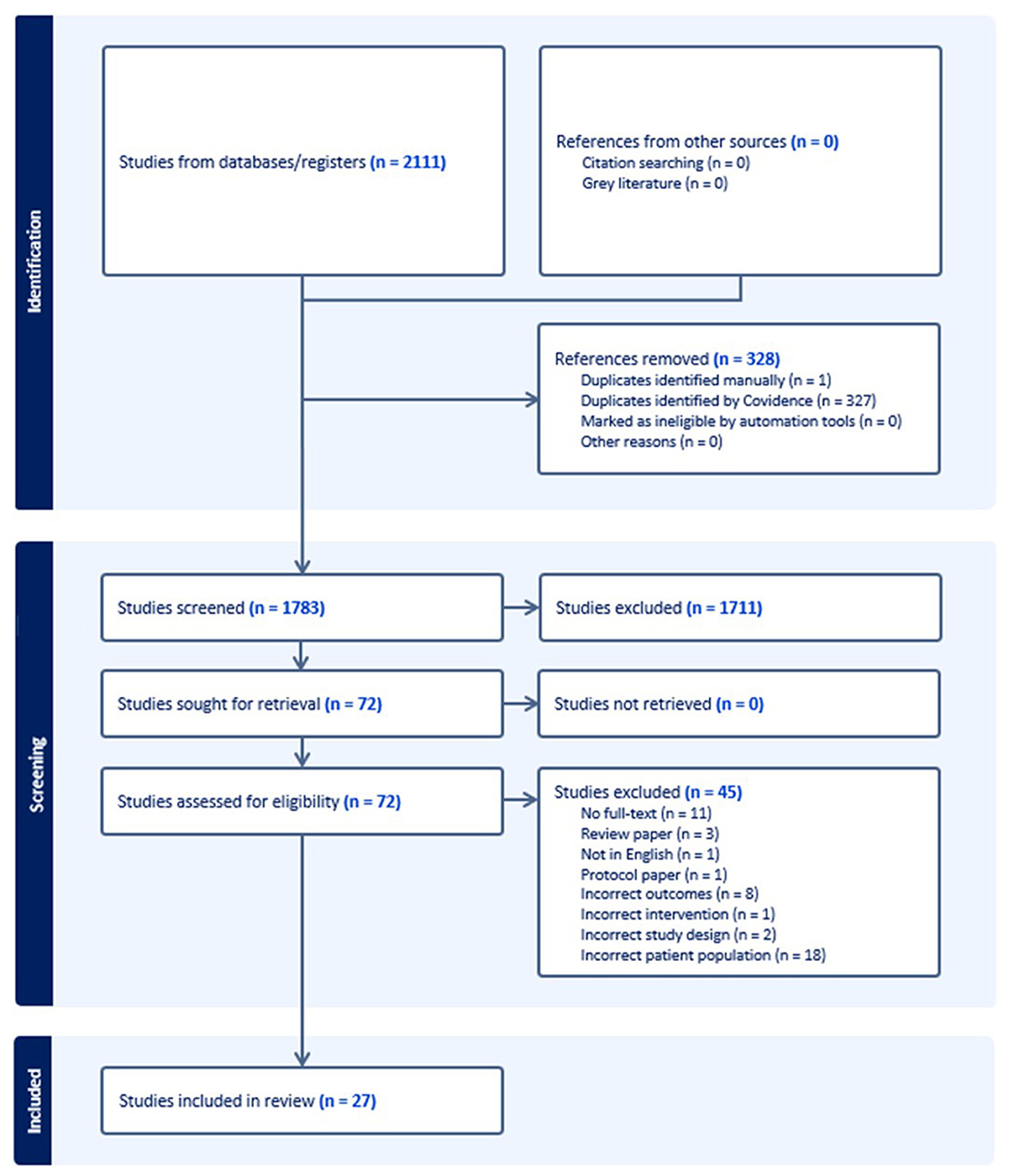
Next, the two reviewers independently reviewed full-text articles which passed title and abstract screening and collaborated to discuss their decision regarding each article and the reason behind their decision. If the reviewers disagreed, a discussion was held until consensus was achieved. Reasons for excluding articles at the full-text level were tracked using review management software. The final breakdown of studies reviewed, excluded, and included in the scoping review is presented in Figure 1 using the PRISMA diagram (Tricco et al., 2018; Peters et al., 2020).
2.1.4 Charting the data
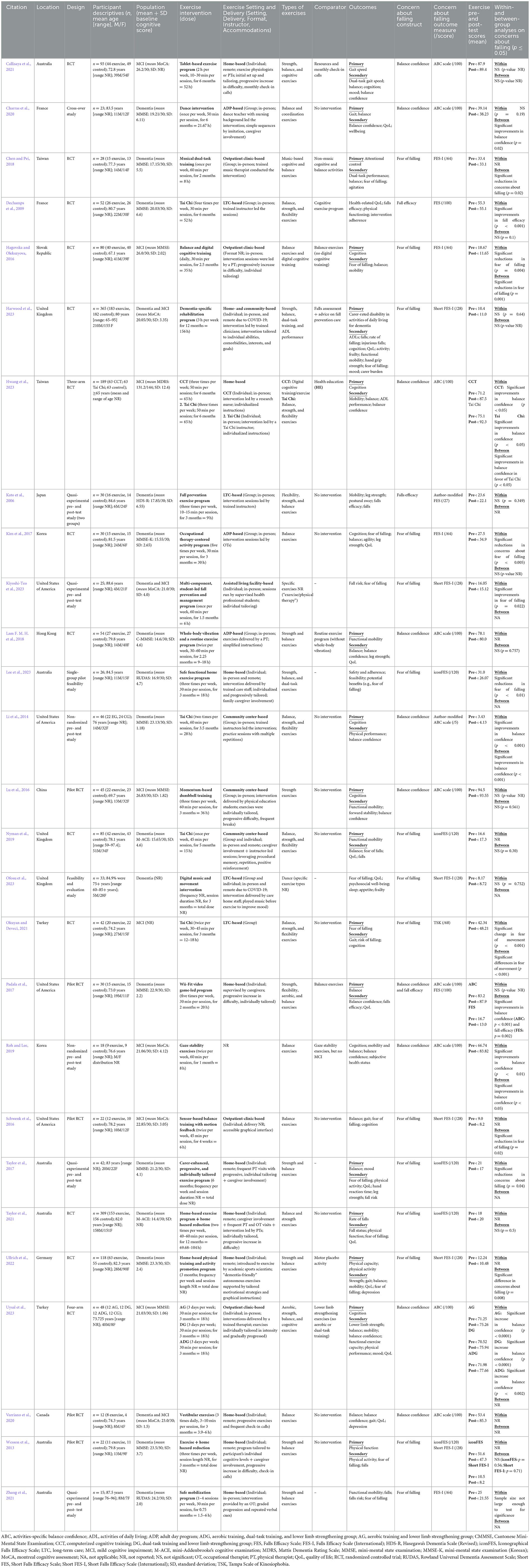
Data from the 27 included studies after full-text exclusion were charted according to publication details, study design, demographics, population targeted (i.e., MCI and/or dementia), exercise intervention employed, specific exercise types used, intervention dose, outcome measure(s) used, primary outcomes, efficacy of the interventions, delivery details (e.g., therapist-led, home-based), and accommodations for participants with cognitive impairment (e.g., cueing, practice). Data extracted from each article were synthesized to answer the research questions.
Data from the included articles were extracted by the first author using a spreadsheet and verified by the second author. Given that this review was scoping rather than systematic, a quality appraisal and risk of bias assessment of the included literature were not undertaken. Scoping reviews are meant to systematically map the breadth of the literature on a given topic rather than assess the existing literature's quality (Arksey and O'Malley, 2005; Joanna Briggs Institute, 2021; Levac et al., 2010). As such, articles were also not graded according to the strength of the evidence.
2.1.5 Collating, summarizing, and reporting the results
The full-text screening results were collated, summarized, and reported by extracting data from the studies and organizing details into a table (see Table 3). Results from the 27 studies were categorized as follows: (i) exercise types, (ii) intervention details, (iii) outcome measures used to examine concerns about falling, (iv) participant accommodations, and (v) components of effective interventions.
3 Results
3.1 Descriptive summary
A total of 27 studies were identified that used exercise interventions to help address concerns about falling in people with MCI and dementia (see Table 3). The year of publication spanned 2006 (Kato et al., 2006) to 2023 (Harwood et al., 2023; Hwang et al., 2023; Kiyoshi-Teo et al., 2023; Lee et al., 2023; Ofosu et al., 2023; Uysal et al., 2023), with 1,882 study participants reported (range: 12–365 participants; mean age: 72.9 years; 40.6% female). Only three studies (Harwood et al., 2023; Nyman et al., 2019; Zhang et al., 2021) reported the age range of their participants, so overall age range was not reported. The research occurred in a total of 13 locations (Table 3), with the most common location being Australia (n = 6) (Lee et al., 2023; Zhang et al., 2021; Callisaya et al., 2021; Taylor et al., 2017, 2021; Wesson et al., 2013), followed by the United States (n = 4) (Li et al., 2021; Kiyoshi-Teo et al., 2023; Padala et al., 2017; Schwenk et al., 2016), and the United Kingdom (n = 3) (Harwood et al., 2023; Ofosu et al., 2023; Nyman et al., 2019). Only one study was conducted in Canada (Varriano et al., 2020), where the authors of this review are located. The studies showed substantial heterogeneity in exercise program frequency and duration. For example, the duration of the study interventions ranged from 4 weeks (Roh and Lee, 2019) to 12 months (Taylor et al., 2021), and the frequency of the exercise sessions ranged from once per week (Kiyoshi-Teo et al., 2023; Nyman et al., 2019; Charras et al., 2020; Chen and Pei, 2018) to daily (Hagovska and Olekszyova, 2016). A total of 707.8 h of exercise was performed across the interventions, with a mean total of 30.8 h per study (range: 3.75–156 h).
Of the 27 studies, most (n = 16; 59.3%) focused on dementia (Kato et al., 2006; Lee et al., 2023; Ofosu et al., 2023; Nyman et al., 2019; Zhang et al., 2021; Taylor et al., 2017, 2021; Wesson et al., 2013; Padala et al., 2017; Charras et al., 2020; Chen and Pei, 2018; Dechamps et al., 2009; Kim et al., 2017; Lam F. M. H. et al., 2018; Li et al., 2014; Ullrich et al., 2022), eight studies (29.6%) examined people with MCI (Hwang et al., 2023; Uysal et al., 2023; Callisaya et al., 2021; Schwenk et al., 2016; Roh and Lee, 2019; Hagovska and Olekszyova, 2016; Lu et al., 2016; Okuyan and Deveci, 2021), and three studies (Harwood et al., 2023; Kiyoshi-Teo et al., 2023; Varriano et al., 2020) researched both populations. Of the studies focusing on people with dementia, participants were in the early (n = 7; 46.7%) (Zhang et al., 2021; Taylor et al., 2017; Wesson et al., 2013; Padala et al., 2017; Dechamps et al., 2009; Li et al., 2014; Ullrich et al., 2022) or moderate stages of the disease (n = 8; 53.3%) (Kato et al., 2006; Lee et al., 2023; Nyman et al., 2019; Taylor et al., 2021; Charras et al., 2020; Chen and Pei, 2018; Kim et al., 2017; Lam F. M. H. et al., 2018), as indicated by their scores on baseline cognitive assessments. None of the studies featured participants with more severe dementia. One study looking at people with dementia (Ofosu et al., 2023), plus one study examining people with MCI (Okuyan and Deveci, 2021), did not report participants' baseline cognitive scores. Most studies did not report the range of cognitive scores; therefore, only mean and standard deviation were included in Table 3.
To understand the degree of concerns about falling among the participants, we took the reported scores from the included articles and interpreted them based on the established cut-off scores for each measure (e.g., ABC scale score of 81 or higher indicates high balance confidence). Regarding concerns about falling, only five of 27 studies (18.5%) (Kato et al., 2006; Kiyoshi-Teo et al., 2023; Charras et al., 2020; Chen and Pei, 2018; Kim et al., 2017) included participants with high concerns about falling at baseline. The remaining 22 studies (81.5%) recruited participants with low/no (n = 12; 44.4%) (Hwang et al., 2023; Lee et al., 2023; Ofosu et al., 2023; Nyman et al., 2019; Callisaya et al., 2021; Taylor et al., 2017, 2021; Padala et al., 2017; Hagovska and Olekszyova, 2016; Dechamps et al., 2009; Lam F. M. H. et al., 2018; Lu et al., 2016) or moderate (n = 10; 37.0%) (Harwood et al., 2023; Uysal et al., 2023; Zhang et al., 2021; Wesson et al., 2013; Schwenk et al., 2016; Varriano et al., 2020; Roh and Lee, 2019; Li et al., 2014; Okuyan and Deveci, 2021; Ullrich et al., 2022) baseline concerns about falling. Twenty studies (74.1%) featured a type of randomized controlled trial (n = 19) (Kato et al., 2006; Harwood et al., 2023; Hwang et al., 2023; Uysal et al., 2023; Nyman et al., 2019; Callisaya et al., 2021; Taylor et al., 2021; Wesson et al., 2013; Padala et al., 2017; Schwenk et al., 2016; Varriano et al., 2020; Chen and Pei, 2018; Hagovska and Olekszyova, 2016; Dechamps et al., 2009; Kim et al., 2017; Lam F. M. H. et al., 2018; Lu et al., 2016; Okuyan and Deveci, 2021; Ullrich et al., 2022) or crossover design (n = 1) (Charras et al., 2020) with exercise and control or usual care arms. The remaining studies (n = 7) consisted of three quasi-experimental (i.e., one arm) pre- and post-test studies (Kiyoshi-Teo et al., 2023; Zhang et al., 2021; Taylor et al., 2017), two non-randomized (i.e., two arm) pre- and post-test studies (Roh and Lee, 2019; Li et al., 2014), and two pilot feasibility studies (Lee et al., 2023; Ofosu et al., 2023).
3.2 Detailed findings
3.2.1 Types of exercises
Eighteen of the 27 included studies (66.7%) were multi-modal (Kato et al., 2006; Harwood et al., 2023; Hwang et al., 2023; Lee et al., 2023; Uysal et al., 2023; Nyman et al., 2019; Zhang et al., 2021; Callisaya et al., 2021; Taylor et al., 2017, 2021; Wesson et al., 2013; Padala et al., 2017; Charras et al., 2020; Dechamps et al., 2009; Lam F. M. H. et al., 2018; Li et al., 2014; Okuyan and Deveci, 2021; Ullrich et al., 2022). Balance was the most used type of exercise, included in all but three articles (i.e., n = 24; 88.9%; see Table 2) (Kiyoshi-Teo et al., 2023; Ofosu et al., 2023; Lu et al., 2016), two of which did not state the specific types of exercises included in the interventions (Kiyoshi-Teo et al., 2023; Ofosu et al., 2023). Examples of balance exercises included performing specific stances (e.g., one-legged stance, tandem stance) and stepping activities (e.g., side-stepping, step-ups onto a block). Second after balance were strength exercises, used in 18 (66.7%) studies (Kato et al., 2006; Harwood et al., 2023; Hwang et al., 2023; Lee et al., 2023; Uysal et al., 2023; Nyman et al., 2019; Zhang et al., 2021; Callisaya et al., 2021; Taylor et al., 2017, 2021; Wesson et al., 2013; Padala et al., 2017; Dechamps et al., 2009; Lam F. M. H. et al., 2018; Li et al., 2014; Lu et al., 2016; Okuyan and Deveci, 2021; Ullrich et al., 2022), often partnered with balance. In addition to balance and strength, other modalities included flexibility (Kato et al., 2006; Hwang et al., 2023; Nyman et al., 2019; Padala et al., 2017; Dechamps et al., 2009; Li et al., 2014; Okuyan and Deveci, 2021), aerobic fitness (Uysal et al., 2023; Padala et al., 2017), and coordination (Charras et al., 2020). Five studies (18.5%) implemented Tai Chi-based exercise (Hwang et al., 2023; Nyman et al., 2019; Dechamps et al., 2009; Li et al., 2014; Okuyan and Deveci, 2021), simultaneously targeting balance, strength, and flexibility.
3.2.2 Intervention details
Of the 27 included articles, the exercise interventions occurred in a variety of settings serving older adults with MCI and dementia (see Table 3). Personal homes were the most common location for the exercise interventions (n = 11; 40.7%) (Harwood et al., 2023; Hwang et al., 2023; Lee et al., 2023; Zhang et al., 2021; Callisaya et al., 2021; Taylor et al., 2017, 2021; Wesson et al., 2013; Padala et al., 2017; Varriano et al., 2020; Ullrich et al., 2022), followed by community-based settings such as private rehabilitation clinics (n = 4) (Uysal et al., 2023; Schwenk et al., 2016; Chen and Pei, 2018; Hagovska and Olekszyova, 2016), community centers (n = 3) (Nyman et al., 2019; Li et al., 2014; Lu et al., 2016), and adult day programs (n = 3) (Charras et al., 2020; Kim et al., 2017; Lam F. M. H. et al., 2018). The remaining studies occurred in institutional settings such as long-term care (n = 4) (Kato et al., 2006; Ofosu et al., 2023; Dechamps et al., 2009; Okuyan and Deveci, 2021) and one assisted-living facility (Kiyoshi-Teo et al., 2023). One study did not report information about the intervention setting (Roh and Lee, 2019).
Over half of the studies (14/27; 51.9%) delivered the interventions individually (Harwood et al., 2023; Hwang et al., 2023; Kiyoshi-Teo et al., 2023; Lee et al., 2023; Uysal et al., 2023; Zhang et al., 2021; Callisaya et al., 2021; Taylor et al., 2017, 2021; Wesson et al., 2013; Padala et al., 2017; Schwenk et al., 2016; Varriano et al., 2020; Ullrich et al., 2022). A further third (n = 9; 33.3%) were delivered in a group (Kato et al., 2006; Charras et al., 2020; Chen and Pei, 2018; Dechamps et al., 2009; Kim et al., 2017; Lam F. M. H. et al., 2018; Li et al., 2014; Lu et al., 2016; Okuyan and Deveci, 2021). The remaining studies offered both group and individual formats (Ofosu et al., 2023; Nyman et al., 2019), or the format was not reported (Roh and Lee, 2019; Hagovska and Olekszyova, 2016). Individual-based intervention studies tended to be delivered in participants' homes, while group-based interventions tended to take place in long-term care, adult day programs, outpatient rehabilitation clinics, and community centers.
Twelve of the 27 (44.4%) interventions occurred in-person (Kato et al., 2006; Hwang et al., 2023; Kiyoshi-Teo et al., 2023; Uysal et al., 2023; Charras et al., 2020; Chen and Pei, 2018; Hagovska and Olekszyova, 2016; Dechamps et al., 2009; Kim et al., 2017; Lam F. M. H. et al., 2018; Li et al., 2014; Lu et al., 2016), six (22.2%) were delivered remotely (Callisaya et al., 2021; Taylor et al., 2017, 2021; Wesson et al., 2013; Varriano et al., 2020; Ullrich et al., 2022), and four used both in-person and remote approaches. Two studies that used both in-person and remote delivery did so due to challenges associated with the COVID-19 pandemic (Harwood et al., 2023; Ofosu et al., 2023). One-quarter of the studies (n = 7) used technology (e.g., touchscreen tablets, music devices, sensor-based exercise platforms, commercial exercise gaming consoles) to deliver the exercise interventions (Ofosu et al., 2023; Callisaya et al., 2021; Padala et al., 2017; Schwenk et al., 2016; Hagovska and Olekszyova, 2016; Lam F. M. H. et al., 2018; Lu et al., 2016). Delivery details of the intervention were not mentioned in four studies (Padala et al., 2017; Schwenk et al., 2016; Roh and Lee, 2019; Okuyan and Deveci, 2021).
3.2.3 Outcome measures
Only one study examined participants' concerns about falling as the primary or first-listed outcome (Okuyan and Deveci, 2021). In the remaining 26 studies, concerns about falling were a secondary outcome (see Table 3). Of the 27 articles, all (100%) examined concerns about falling using self-report, quantitative outcome measures. Six different scales were used in total across the 27 studies, including the ABC scale, which was used the most in just over one-third of studies (n = 10; 37%) (Hwang et al., 2023; Uysal et al., 2023; Callisaya et al., 2021; Padala et al., 2017; Varriano et al., 2020; Roh and Lee, 2019; Charras et al., 2020; Lam F. M. H. et al., 2018; Li et al., 2014; Lu et al., 2016), followed by the Short FES-I in six studies (22.2%) (Harwood et al., 2023; Kiyoshi-Teo et al., 2023; Ofosu et al., 2023; Wesson et al., 2013; Schwenk et al., 2016; Ullrich et al., 2022). Other measures used to examine concerns about falling in this population included the FES-I (n = 4) (Zhang et al., 2021; Chen and Pei, 2018; Hagovska and Olekszyova, 2016; Kim et al., 2017), iconFES (n = 4) (Lee et al., 2023; Nyman et al., 2019; Taylor et al., 2017, 2021), original FES (n = 3) (Kato et al., 2006; Padala et al., 2017; Dechamps et al., 2009), and the TSK (n = 1) (Okuyan and Deveci, 2021).
The most measured construct related to concerns about falling was fear of falling, identified in half of the studies (n = 14; 51.9%) (Harwood et al., 2023; Kiyoshi-Teo et al., 2023; Lee et al., 2023; Ofosu et al., 2023; Nyman et al., 2019; Zhang et al., 2021; Taylor et al., 2017, 2021; Wesson et al., 2013; Schwenk et al., 2016; Chen and Pei, 2018; Hagovska and Olekszyova, 2016; Kim et al., 2017; Ullrich et al., 2022). This construct was measured using several different scales. Next was balance confidence, measured in 10 studies (37.0%) (Hwang et al., 2023; Uysal et al., 2023; Callisaya et al., 2021; Padala et al., 2017; Varriano et al., 2020; Roh and Lee, 2019; Charras et al., 2020; Lam F. M. H. et al., 2018; Li et al., 2014; Lu et al., 2016), continuously assessed by the ABC scale (Powell and Myers, 1995). Fall efficacy was measured in three articles (11.1%) (Kato et al., 2006; Padala et al., 2017; Dechamps et al., 2009); one of these studies also measured balance confidence (Padala et al., 2017). Finally, the one study looking at concerns about falling as the primary outcome (Okuyan and Deveci, 2021) measured fear of movement using the TSK. No studies examined movement confidence as a construct.
3.2.4 Participant accommodations
Several of the studies reported making accommodations for the cognitive needs of the participants with MCI or dementia (see Table 3). The primary accommodation was using “support persons.” In 20 studies (74.1%), interventions were supported by clinicians (e.g., OT, PT) and other trained facilitators (e.g., kinesiology students, nurse practitioners, exercise physiologists) (Kato et al., 2006; Harwood et al., 2023; Hwang et al., 2023; Kiyoshi-Teo et al., 2023; Ofosu et al., 2023; Uysal et al., 2023; Nyman et al., 2019; Zhang et al., 2021; Callisaya et al., 2021; Taylor et al., 2017, 2021; Charras et al., 2020; Chen and Pei, 2018; Hagovska and Olekszyova, 2016; Dechamps et al., 2009; Kim et al., 2017; Lam F. M. H. et al., 2018; Li et al., 2014; Lu et al., 2016; Ullrich et al., 2022) to prescribe, deliver, progress, and/or supervise/monitor the exercise interventions. There was also some degree of family/friend caregiver involvement (n = 6; 22.2%) (Lee et al., 2023; Nyman et al., 2019; Taylor et al., 2017, 2021; Wesson et al., 2013; Padala et al., 2017) for additional support during the exercise interventions and related data collection, particularly for home-based programs (e.g., monitoring for safety or motivational purposes).
Another accommodation for participants with MCI and dementia was individual tailoring (n = 13; 48.0%) by establishing initial exercises, sets, repetitions, and durations to suit participant abilities (Harwood et al., 2023; Hwang et al., 2023; Kiyoshi-Teo et al., 2023; Lee et al., 2023; Uysal et al., 2023; Callisaya et al., 2021; Taylor et al., 2017, 2021; Wesson et al., 2013; Padala et al., 2017; Hagovska and Olekszyova, 2016; Lu et al., 2016; Ullrich et al., 2022). In addition to, or as part of individual tailoring, progressive increases in difficulty (n = 11; 40.7%) (Lee et al., 2023; Uysal et al., 2023; Zhang et al., 2021; Callisaya et al., 2021; Taylor et al., 2017, 2021; Wesson et al., 2013; Padala et al., 2017; Varriano et al., 2020; Hagovska and Olekszyova, 2016; Lu et al., 2016) of exercise components (e.g., narrowing stance, adding weights) were used as participants became increasingly able to perform the exercises initially prescribed. Additional accommodations for participants with MCI and dementia included “cognitive-friendly” instruction techniques (n = 8; 29.6%), such as mirroring, repetition, procedural memory-based pedagogies, and practice sessions (Ofosu et al., 2023; Nyman et al., 2019; Schwenk et al., 2016; Charras et al., 2020; Lam F. M. H. et al., 2018; Li et al., 2014; Lu et al., 2016; Ullrich et al., 2022). A few studies also offered check-in calls (n = 3) (Zhang et al., 2021; Callisaya et al., 2021; Varriano et al., 2020) or home visits (n = 2) (Taylor et al., 2017, 2021).
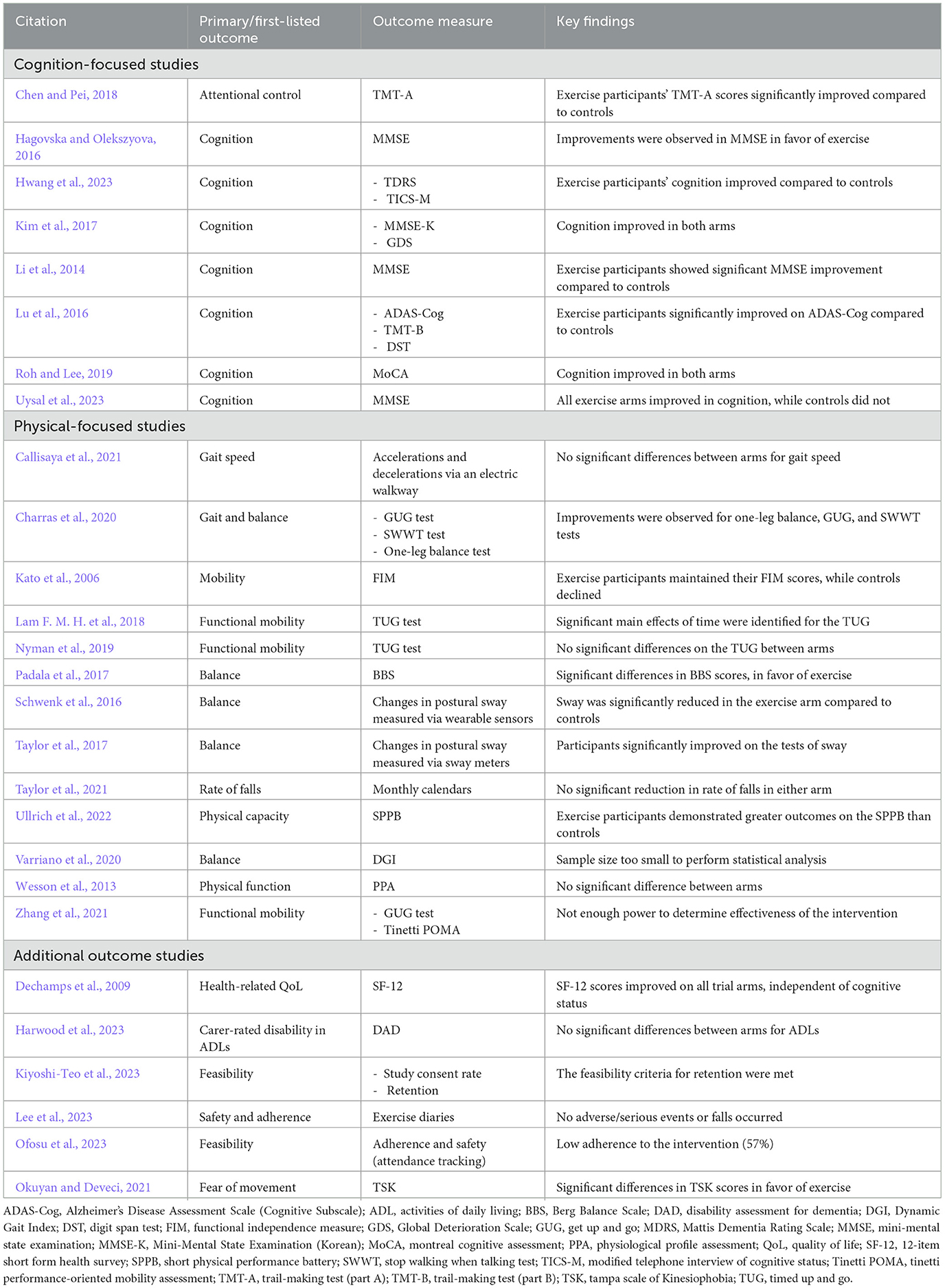
3.2.5 Components of effective interventions
The 27 studies explored 13 primary outcomes. Nineteen (70.4%) studies reported statistically significant (Kato et al., 2006; Hwang et al., 2023; Kiyoshi-Teo et al., 2023; Lee et al., 2023; Uysal et al., 2023; Taylor et al., 2017; Padala et al., 2017; Schwenk et al., 2016; Roh and Lee, 2019; Charras et al., 2020; Chen and Pei, 2018; Hagovska and Olekszyova, 2016; Dechamps et al., 2009; Kim et al., 2017; Lam F. M. H. et al., 2018; Li et al., 2014; Lu et al., 2016; Okuyan and Deveci, 2021; Ullrich et al., 2022) changes in their primary or first-listed outcome. Primary or first-listed outcomes were grouped into three categories: cognitive-focused outcomes, physical-focused outcomes, and additional outcomes (see Table 4).
The most common primary outcome among the 27 studies was cognition. Seven studies (25.9%) had a cognitive measure as their primary outcome (Hwang et al., 2023; Uysal et al., 2023; Roh and Lee, 2019; Hagovska and Olekszyova, 2016; Kim et al., 2017; Li et al., 2014; Lu et al., 2016), with one further study (Chen and Pei, 2018) focusing on an aspect of cognition (attentional control). All studies with cognition (or an aspect of it) as their primary outcome showed significant improvements at post-intervention.
Despite the prevalence of balance exercise interventions, only five studies (18.5%) looked at balance as their primary outcome (Taylor et al., 2017; Padala et al., 2017; Schwenk et al., 2016; Varriano et al., 2020; Charras et al., 2020), of which four (Taylor et al., 2017; Padala et al., 2017; Schwenk et al., 2016; Charras et al., 2020) recorded a significant change. Four studies focused on mobility as the primary or first-listed outcome (Kato et al., 2006; Nyman et al., 2019; Zhang et al., 2021; Lam F. M. H. et al., 2018), with only one demonstrating a significant effect at post-intervention (Lam F. M. H. et al., 2018). Of the two studies primarily examining gait (Callisaya et al., 2021; Charras et al., 2020), only one significantly improved (Charras et al., 2020). The one study looking at fall rate (Taylor et al., 2021) was not significant at post-intervention, while the single study investigating physical capacity [defined as “the ability to perform a physical task or action measured by self-report or objective measurement” (Kasper et al., 2017)] was (Ullrich et al., 2022).
Other primary outcomes concerned the feasibility of the exercise intervention (n = 2) (Kiyoshi-Teo et al., 2023; Ofosu et al., 2023), one of which was significant (Kiyoshi-Teo et al., 2023), followed by safety and adherence (n = 1; criteria met) (Lee et al., 2023), ADLs (n = 1; not significant) (Harwood et al., 2023), health-related QoL (n = 1; significant at post-intervention) (Dechamps et al., 2009), and fear of movement (n = 1; significant at post-intervention) (Okuyan and Deveci, 2021). Two studies (Zhang et al., 2021; Varriano et al., 2020) did not have a large enough sample to perform statistical analyses and could not examine the effectiveness of the exercise interventions on their primary outcome(s).
Of the 19 “successful” interventions (i.e., the intervention significantly impacted the primary outcome), most (n = 13; 68.4%) were conducted outside of the home setting (e.g., LTC, ADPs, outpatient clinics, community centers, etc.) (Kato et al., 2006; Kiyoshi-Teo et al., 2023; Uysal et al., 2023; Schwenk et al., 2016; Charras et al., 2020; Chen and Pei, 2018; Hagovska and Olekszyova, 2016; Dechamps et al., 2009; Kim et al., 2017; Lam F. M. H. et al., 2018; Li et al., 2014; Lu et al., 2016; Okuyan and Deveci, 2021). There was a relatively even split between group (n = 9/19; 47.4%) (Kato et al., 2006; Charras et al., 2020; Chen and Pei, 2018; Dechamps et al., 2009; Kim et al., 2017; Lam F. M. H. et al., 2018; Li et al., 2014; Lu et al., 2016; Okuyan and Deveci, 2021) and individual (n = 8/19; 42.1%) interventions (Hwang et al., 2023; Kiyoshi-Teo et al., 2023; Lee et al., 2023; Uysal et al., 2023; Taylor et al., 2017; Padala et al., 2017; Schwenk et al., 2016; Ullrich et al., 2022), with two studies (Roh and Lee, 2019; Hagovska and Olekszyova, 2016) not reporting this information. Many successful interventions (n = 13/19; 68.4%) were conducted in-person (Kato et al., 2006; Hwang et al., 2023; Kiyoshi-Teo et al., 2023; Lee et al., 2023; Uysal et al., 2023; Charras et al., 2020; Chen and Pei, 2018; Hagovska and Olekszyova, 2016; Dechamps et al., 2009; Kim et al., 2017; Lam F. M. H. et al., 2018; Li et al., 2014; Lu et al., 2016) vs. remotely (n = 4/19; 21.1%) (Lee et al., 2023; Taylor et al., 2017; Padala et al., 2017; Ullrich et al., 2022). All but two successful studies (Roh and Lee, 2019; Okuyan and Deveci, 2021) (i.e., n = 17/19; 89.5%) included at least one form of participant accommodations (e.g., trained instructors, tailored instructions, progressive increase in difficulty, etc.). Of note, in all five studies where participants had a high fear of falling (Kato et al., 2006; Kiyoshi-Teo et al., 2023; Charras et al., 2020; Chen and Pei, 2018; Kim et al., 2017), the exercise interventions significantly impacted their primary or first-listed outcome. These outcomes included mobility (Kato et al., 2006), feasibility (Kiyoshi-Teo et al., 2023), gait and balance (Charras et al., 2020), and cognition (Chen and Pei, 2018; Kim et al., 2017). The intervention dose, including the frequency (i.e., number of sessions per week) and duration (i.e., number of months), did not appear to impact whether the intervention was successful at addressing the primary outcome. For example, of the 19 successful studies, intervention frequency ranged from once weekly (Kiyoshi-Teo et al., 2023; Charras et al., 2020; Chen and Pei, 2018) to daily (Hagovska and Olekszyova, 2016), while the intervention duration ranged from 4 weeks (1 month) (Schwenk et al., 2016; Roh and Lee, 2019) to 24 weeks (6 months) (Hwang et al., 2023; Taylor et al., 2017; Charras et al., 2020; Dechamps et al., 2009). Interestingly, both studies with interventions lasting 1 year (Harwood et al., 2023; Taylor et al., 2021) did not significantly impact their primary outcomes. Additionally, when reviewing level of cognition (i.e., MCI or dementia) in greater detail, it was found that interventions appeared to elicit greater benefit for individuals living with MCI, with only one study (Callisaya et al., 2021) of the eight focusing solely on MCI (Hwang et al., 2023; Uysal et al., 2023; Callisaya et al., 2021; Schwenk et al., 2016; Roh and Lee, 2019; Hagovska and Olekszyova, 2016; Lu et al., 2016; Okuyan and Deveci, 2021) not producing significant impacts (i.e., 7/8 = 87.5%). Finally, but importantly, of the 19 interventions to successfully impact their primary outcome, all but three studies (Kato et al., 2006; Lam F. M. H. et al., 2018; Lu et al., 2016) (n = 16/19; 84.2%) also had a significant within- or between-group effect on concerns about falling.
4 Discussion
This scoping review mapped exercise interventions to help address concerns about falling in people with MCI and dementia. Of the 27 studies identified, only one (Okuyan and Deveci, 2021) had concerns about falling as the primary outcome. The other 26 included concerns about falling as secondary outcomes. Among the 27 studies, only five included participants who had high concerns about falling, limiting our understanding of the potential of exercise interventions to impact people with MCI and dementia with the most concerns. Therefore, interpreting the potential of the significant studies should consider the degree of concerns about falling (i.e., none, low, medium, or high) among study participants.
Two-thirds of the studies included people living with dementia and one-third with MCI (three included both). Based on reported cognitive scores, the participants were mainly at the mild to moderate stage of dementia. As such, they may have been able to self-report their concerns about falling more accurately, given that insight decreases with the increasing severity of cognitive impairment (McDaniel et al., 1995; Zanetti et al., 1999). The iconFES (30 items and scored out of 120 points), used in only four included studies (Delbaere et al., 2011), includes pictures to assess fear of falling. However, although designed with people with cognitive impairment in mind (Delbaere et al., 2013), the clinical cut-off scores for the iconFES are rather broad, with ≤ 40 indicating low concern about falling, 41–58 indicating moderate concerns about falling, and ≥59 indicating high concerns about falling (Delbaere et al., 2013, 2011). More research is needed to use this tool clinically and, more specifically, to evaluate the effectiveness of exercise interventions in this population.
Eight of the 27 studies had cognition as the primary outcome, all reporting significant improvements from the exercise interventions. Furthermore, four studies reported a significant improvement in balance, supporting the potential of exercise interventions to tackle the two main fall risk factors in dementia (Hsu et al., 2012; Mazoteras Muñoz et al., 2010). Regarding concerns about falling, 16 studies that reported successful interventions also reported a significant within- or between-group effect on concerns about falling (Hwang et al., 2023; Kiyoshi-Teo et al., 2023; Lee et al., 2023; Uysal et al., 2023; Taylor et al., 2017; Padala et al., 2017; Schwenk et al., 2016; Roh and Lee, 2019; Charras et al., 2020; Chen and Pei, 2018; Hagovska and Olekszyova, 2016; Dechamps et al., 2009; Kim et al., 2017; Li et al., 2014; Okuyan and Deveci, 2021; Ullrich et al., 2022). Multimodal interventions (i.e., more than one exercise type) were the most successful.
Multiple studies implemented MCI- and dementia-friendly accommodations. These included support persons, repeated instructions, mirroring, procedural cues, plus elements commonly seen in rehabilitation programs, such as individual tailoring and progressive increases in difficulty. The success of these accommodated interventions (17/19; 89.5%) challenges the negative perceptions of people living with progressive cognitive impairment to benefit from rehabilitation interventions. The findings also coincide with the development of resources for exercise providers to offer sessions to people living with dementia, such as the “Dementia Inclusive Choices for Exercise” (DICE) toolkit (Middleton et al., 2023). The DICE toolkit includes individual tailoring and progressive increases in difficulty, as well as dementia-friendly instruction techniques (e.g., pacing speech, breaking exercises into steps, offering modifications of exercises) to support exercise providers. These findings demonstrate that people with MCI and dementia can participate in exercise interventions, especially when accommodations are put in place.
The review highlights the current lack of focus on concerns about falling as a primary outcome for exercise targeting people with MCI and dementia. There are a few potential reasons why there is a lack of primary focus on exercise to help address concerns about falling in people with MCI and dementia. Several studies recruited people with MCI and dementia who had little to no concerns about falling at baseline, which may have impacted the degree to which participants could improve because of the intervention. For example, participants with MCI in Callisaya et al. (2021) scored a mean of 87.9/100 on the baseline ABC, with higher scores on the ABC indicating higher balance confidence. With scores indicating a high or moderate level of functioning/confidence, researchers may be “missing the true target” regarding who they recruit for exercise interventions. This is important to note given that concerns about falling are associated with fall risk factors among older adults without cognitive impairment, such as poor perceived health and a history of multiple falls (Zijlstra et al., 2007), plus lower muscle strength and worse balance (Deshpande et al., 2009). Future research should explore these associations further with people who have cognitive impairment, as this may help drive more targeted interventions for falls, which people with cognitive impairment are more likely to experience (Meuleners et al., 2016).
This study has some limitations. It is acknowledged that terms encompassing concerns about falling (e.g., balance confidence, fear of falling, etc.) are unique constructs that are defined, measured, and interpreted differently (Adamczewska and Nyman, 2018; Soh et al., 2021). However, this review combined all these terms in the outcome column of the search strategy. This decision could be considered a limitation, creating heterogeneity, or further perpetuating generic mixing of specific terminology. However, combining all terms in one outcome category allowed the review to map the breadth of literature on all constructs related to concerns about falling, which aligns with the objectives of a scoping review (Arksey and O'Malley, 2005). During the review process, the decision was made to exclude any literature not featuring full-text, original, empirical research articles. This excluded gray literature (although none was identified), 11 conference abstracts, one protocol paper, and three review papers. Additionally, there is no “gold-standard” mechanism to measure concerns about falling; this outcome is assessed using self-report measures, as evident by the studies included in this review. With self-report measures assessing concerns about falling and other constructs (e.g., health service use), there is a risk of recall bias or reporting errors when working with people living with cognitive impairment, such as MCI and dementia (Callahan et al., 2015; Frank et al., 2011). To address this, we recommend that future studies use self-report measures suitable for people living with cognitive impairment by offering visual (i.e., picture) cues and prompts, such as the iconFES (Delbaere et al., 2013, 2011). Further, concerns about falling, which are measured through self-report scales, introduce the possibility of social desirability bias, whereby participants modify their responses to be viewed more favorably by others (e.g., researchers) (Delbaere et al., 2010). To mitigate this effect, it is proposed to implement more anonymous, self-administered measurement methods for assessing concerns about falling. Finally, only studies written in English were included in this review, meaning that studies meeting the inclusion criteria but from other languages were excluded.
Despite the limitations identified above, it is anticipated that the conclusions of this review will stimulate future impactful research in this area. For example, there is a clear need for more large-scale, in-depth experiments evaluating exercise interventions involving people living with MCI and dementia, where concerns about falling are the primary outcome. Further, this scoping review confirms the need for a future systematic review on this topic area, where the formal effectiveness of exercise interventions for people living with MCI and dementia on concerns about falling, fall risk factors (e.g., balance), and falls are examined in greater detail. For future studies, it is recommended that researchers use consistent terminology and mechanisms of intervention measurement (e.g., specific scales). For example, in line with the findings of this review regarding the applicability of accommodations for people living with MCI and dementia, it is recommended that researchers adopt the use of the iconFES (Delbaere et al., 2013) with this population given the included visual prompts that generate more reliable responses and reduce the cognitive demands on participants.
5 Conclusions
This is the first scoping review to map the literature using exercise interventions to target concerns about falling in people with MCI and dementia. This scoping review highlights that concerns about falling can be improved with exercise interventions in older adults with MCI and dementia. Although concerns about falling were not the primary outcome of most papers, the results also highlight the potential of exercise interventions to target other fall risk factors (e.g., balance) in people with MCI and dementia.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
ED: Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Writing – original draft. PH: Conceptualization, Data curation, Formal analysis, Methodology, Writing – review & editing. RW: Conceptualization, Methodology, Writing – review & editing. KP: Conceptualization, Methodology, Writing – review & editing. AA: Conceptualization, Methodology, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This scoping review was funded by a doctoral award from the Alzheimer Society of Canada (#21-20) and a graduate award in technology and aging from AGE-WELL (#AW-HQP2020-04). These funds were awarded to Erica Dove as part of her doctoral dissertation.
Acknowledgments
The authors would like to thank Julia Martyniuk, Liaison and Education Librarian, for their help in developing the search strategy. The authors of this paper would also like to thank the three peer reviewers for improving the comprehensiveness and rigor of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Adamczewska, N., and Nyman, S. R. (2018). A new approach to fear of falls from connections with the posttraumatic stress disorder literature. Gerontol. Geriatr. Med. 4:2333721418796238. doi: 10.1177/2333721418796238
Arksey, H., and O'Malley, L. (2005). Scoping studies: towards a methodological framework. Int. J. Soc. Res. Methodol. 8, 19–32. doi: 10.1080/1364557032000119616
Asai, T., Oshima, K., Fukumoto, Y., Yonezawa, Y., Matsuo, A., Misu, S., et al. (2022). The association between fear of falling and occurrence of falls: a one-year cohort study. BMC Geriatr. 22:393. doi: 10.1186/s12877-022-03018-2
Booth, V., Logan, P., Harwood, R., and Hood, V. (2015). Falls prevention interventions in older adults with cognitive impairment: a systematic review of reviews. Int. J. Ther. Rehabil. 22, 289–296. doi: 10.12968/ijtr.2015.22.6.289
Borges, S., Radanovic, M., and Forlenza, O. (2014). Fear of falling and falls in older adults with mild cognitive impairment and Alzheimer's disease. Neuropsychol. Dev. Cogn. B Aging Neuropsychol. Cogn. 22, 1–10. doi: 10.1080/13825585.2014.933770
Burton, E., Cavalheri, V., Adams, R., Browne, C. O., Bovery-Spencer, P., Fenton, A. M., et al. (2015). Effectiveness of exercise programs to reduce falls in older people with dementia living in the community: a systematic review and meta-analysis. Clin. Interv. Aging. 10, 421–344. doi: 10.2147/CIA.S71691
Callahan, C. M., Tu, W., Stump, T. E., Clark, D. O., Unroe, K. T., Hendrie, H. C., et al. (2015). Errors in self-reports of health services use: impact on Alzheimer disease clinical trial designs. Alzheimer Dis. Assoc. Disord. 29, 75–81. doi: 10.1097/WAD.0000000000000048
Callisaya, M. L., Vaidya, A., Srikanth, V., Jayakody, O., Farrow, M., and Delbaere, K. (2021). A novel cognitive-motor exercise program delivered via a tablet to improve mobility in older people with cognitive impairment - standingtall cognition and mobility. Exp. Gerontol. 152:111434. doi: 10.1016/j.exger.2021.111434
Charras, K., Mabire, J.-B., Bouaziz, N., Deschamps, P., Froget, B., de Malherbe, A., et al. (2020). Dance intervention for people with dementia: lessons learned from a small-sample crossover explorative study. Arts Psychother. 70:101676. doi: 10.1016/j.aip.2020.101676
Chen, Y.-L., and Pei, Y.-C. (2018). Musical dual-task training in patients with mild-to-moderate dementia: a randomized controlled trial. Neuropsychiatr. Dis. Treat. 14, 1381–1393. doi: 10.2147/NDT.S159174
da Costa Santos, C. M., de Mattos Pimenta, C. A., and Nobre, M. R. (2007). The PICO strategy for the research question construction and evidence search. Rev. Lat. Am. Enfermagem. 15, 508–511. doi: 10.1590/S0104-11692007000300023
Dechamps, A., Onifade, C., Decamps, A., and Bourdel-Marchasson, I. (2009). Health-related quality of life in frail institutionalized elderly: effects of a cognition-action intervention and Tai Chi. J. Aging Phys. Act. 17, 236–248. doi: 10.1123/japa.17.2.236
Delbaere, K., Close, J. C., Brodaty, H., Sachdev, P., and Lord, S. R. (2010). Determinants of disparities between perceived and physiological risk of falling among elderly people: cohort study. BMJ 341:c4165. doi: 10.1136/bmj.c4165
Delbaere, K., Close, J. C. T., Taylor, M., Wesson, J., and Lord, S. R. (2013). Validation of the iconographical falls efficacy scale in cognitively impaired older people. J. Gerontol. A. 68, 1098–1102. doi: 10.1093/gerona/glt007
Delbaere, K., Smith, S. T., and Lord, S. R. (2011). Development and initial validation of the iconographical falls efficacy scale. J. Gerontol. A Biol. Sci. Med. Sci. 66, 674–680. doi: 10.1093/gerona/glr019
Deshpande, N., Metter, E. J., Lauretani, F., Bandinelli, S., and Ferrucci, L. (2009). Interpreting fear of falling in the elderly: what do we need to consider? J. Geriatr. Phys. Ther. 32, 91–96. doi: 10.1519/00139143-200932030-00002
Frank, L., Lenderking, W. R., Howard, K., and Cantillon, M. (2011). Patient self-report for evaluating mild cognitive impairment and prodromal Alzheimer's disease. Alzheimers. Res. Ther. 3:35. doi: 10.1186/alzrt97
Hagovska, M., and Olekszyova, Z. (2016). Impact of the combination of cognitive and balance training on gait, fear and risk of falling and quality of life in seniors with mild cognitive impairment. Geriatr. Gerontol. Int. 16, 1043–1050. doi: 10.1111/ggi.12593
Harwood, R. H., Goldberg, S. E., Brand, A., van Der Wardt, V., Booth, V., Di Lorito, C, et al. (2023). Promoting activity, independence, and stability in early dementia and mild cognitive impairment (PrAISED): randomised controlled trial. BMJ. 382:e074787. doi: 10.1136/bmj-2023-074787
Hsu, C. L., Nagamatsu, L. S., Davis, J. C., and Liu-Ambrose, T. (2012). Examining the relationship between specific cognitive processes and falls risk in older adults: a systematic review. Osteoporos. Int. 23, 2409–2424. doi: 10.1007/s00198-012-1992-z
Hwang, H.-F., Tseng, K.-C., Chen, S.-J., Yu, W.-Y., Chen, C.-Y., Lin, M.-R., et al. (2023). Effects of home-based computerized cognitive training and tai chi exercise on cognitive functions in older adults with mild cognitive impairment. Aging Ment. Health. 27, 2170–2178. doi: 10.1080/13607863.2023.2225430
Joanna Briggs Institute (2021). Resources. Available at: https://jbi.global/scoping-review-network/resources (accessed August 19, 2022).
Kasper, J. D., Chan, K. S., and Freedman, V. A. (2017). Measuring physical capacity. J. Aging Health. 29, 289–309. doi: 10.1177/0898264316635566
Kato, M., Izumi, K., Hiramatsu, T., and Shogenji, M. (2006). Development of an exercise program for fall prevention for elderly persons in a long-term care facility. Jpn. J. Nurs. Sci. 3, 107–117. doi: 10.1111/j.1742-7924.2006.00057.x
Kim, K.-U., Kim, S.-H., and Oh, H.-W. (2017). The effects of occupation-centered activity program on fall-related factors and quality of life in patients with dementia. J. Phys. Ther. Sci. 29, 1188–1191. doi: 10.1589/jpts.29.1188
Kiyoshi-Teo, H., McKinley-Yoder, C., Ochoa-Cosler, O., Lemon, E., Stoyles, S., Tadesse, R., et al. (2023). Feasibility study of student-led fall prevention care management: reducing fall risks in assisted living facilities. Gerontol. Geriatr. Educ. 44, 59–74. doi: 10.1080/02701960.2021.1969387
Lam, F. M., Huang, M. Z., Liao, L. R., Chung, R. C., Kwok, T. C., Pang, M. Y., et al. (2018). Physical exercise improves strength, balance, mobility, and endurance in people with cognitive impairment and dementia: a systematic review. J. Physiother. 64, 4–15. doi: 10.1016/j.jphys.2017.12.001
Lam, F. M. H., Liao, L. R., Kwok, T. C. Y., and Pang, M. Y. C. (2018). Effects of adding whole-body vibration to routine day activity program on physical functioning in elderly with mild or moderate dementia: a randomized controlled trial. Int. J. Geriatr. Psychiatry 33, 21–30. doi: 10.1002/gps.4662
Lee, D.-C. A., Haines, T. P., Callisaya, M. L., and Hill, K. D. (2023). A scalable program for improving physical activity in older people with dementia including culturally and linguistically diverse (CALD) groups who receive home support: a feasibility study. Int. J. Environ. Res. Public Health 20, 1–18. doi: 10.3390/ijerph20043662
Levac, D., Colquhoun, H., and O'Brien, K. K. (2010). Scoping studies: advancing the methodology. Implement. Sci. 5:69. doi: 10.1186/1748-5908-5-69
Li, F., Harmer, P., Eckstrom, E., Ainsworth, B. E., Fitzgerald, K., Voit, J., et al. (2021). Efficacy of exercise-based interventions in preventing falls among community-dwelling older persons with cognitive impairment: is there enough evidence? An updated systematic review and meta-analysis. Age Ageing 50, 1557–1568. doi: 10.1093/ageing/afab110
Li, F., Harmer, P., Liu, Y., and Chou, L.-S. (2014). Tai Ji Quan and global cognitive function in older adults with cognitive impairment: a pilot study. Arch. Gerontol. Geriatr. 58, 434–439. doi: 10.1016/j.archger.2013.12.003
Lu, J., Sun, M., Liang, L., Feng, Y., Pan, X., Liu, Y., et al. (2016). Effects of momentum-based dumbbell training on cognitive function in older adults with mild cognitive impairment: a pilot randomized controlled trial. Clin. Interv. Aging. 11, 9–16. doi: 10.2147/CIA.S96042
Mazoteras Muñoz, V., Abellan van Kan, G., Cantet, C., Cortes, F., Ousset, P. J., Rolland, Y., et al. (2010). Gait and balance impairments in Alzheimer disease patients. Alzheimer Dis. Assoc. Disord. 24, 79–84. doi: 10.1097/WAD.0b013e3181c78a20
McDaniel, K. D., Edland, S. D., and Heyman, A. (1995). Relationship between level of insight and severity of dementia in Alzheimer disease. CERAD clinical investigators. consortium to establish a registry for Alzheimer's Disease. Alzheimer Dis. Assoc. Disord. 9, 101–104. doi: 10.1097/00002093-199509020-00007
Meuleners, L. B., Fraser, M. L., Bulsara, M. K., Chow, K., and Ng, J. Q. (2016). Risk factors for recurrent injurious falls that require hospitalization for older adults with dementia: a population based study. BMC Neurol. 16:188. doi: 10.1186/s12883-016-0711-3
Middleton, L. E., Pelletier, C. A., Koch, M., Norman, R., Dupuis, S., Astell, A., et al. (2023). The dementia-inclusive choices in exercise project: using participatory action research to improve physical activity supports for persons with dementia. Dementia 22, 1651–1676. doi: 10.1177/14713012231197144
Neuroscience Research Australia (2020). Concern about falling. Available at: https://www.standingtall.org.au/assets/Uploads/FactCentral/Fact-Sheet-6-Fear-of-Falling-June-2020.pdf (accessed March 17, 2024).
Nyman, S., Bibi, I., Barrado-Martin, Y., Ingram, W., Sanders, J., Thomas, P., et al. (2019). Randomised controlled trial of the effect of Tai chi on postural balance of people with dementia. Age Ageing 48, 2017–2029. doi: 10.1093/ageing/afz164.89
Ofosu, E. F., De Nys, L., Connelly, J., Ryde, G. C., and Whittaker, A. C. (2023). A realist evaluation of the feasibility of a randomised controlled trial of a digital music and movement intervention for older people living in care homes. BMC Geriatr. 23:125. doi: 10.1186/s12877-023-03794-5
Okuyan, C., and Deveci, E. (2021). The effectiveness of Tai Chi Chuan on fear of movement, prevention of falls, physical activity, and cognitive status in older adults with mild cognitive impairment: a randomized controlled trial. Perspect. Psychiatr. Care 57, 1273–1281. doi: 10.1111/ppc.12684
Padala, K. P., Padala, P. R., Lensing, S. Y., Dennis, R. A., Bopp, M. M., Roberson, P. K., et al. (2017). Home-based exercise program improves balance and fear of falling in community-dwelling older adults with mild Alzheimer's disease: a pilot study. J. Alzheimers Dis. 59, 565–574. doi: 10.3233/JAD-170120
Peters, M. D., Marnie, C., Tricco, A. C., Pollock, D., Munn, Z., Alexander, L., et al. (2020). Updated methodological guidance for the conduct of scoping reviews. JBI Evid. Synthesis 18, 2119–2126. doi: 10.11124/JBIES-20-00167
Powell, L. E., and Myers, A. M. (1995). The activities-specific balance confidence (ABC) Scale. J. Gerontol. A Biol. Sci. Med. Sci. 50a, M28–M34. doi: 10.1093/gerona/50A.1.M28
Roh, M., and Lee, E. (2019). Effects of gaze stability exercises on cognitive function, dynamic postural ability, balance confidence, and subjective health status in old people with mild cognitive impairment. J. Exerc. Rehabil. 15, 270–274. doi: 10.12965/jer.1938026.013
Sachdev, P. S., Blacker, D., Blazer, D. G., Ganguli, M., Jeste, D. V., Paulsen, J. S., et al. (2014). Classifying neurocognitive disorders: the DSM-5 approach. Nat. Rev. Neurol. 10, 634–642. doi: 10.1038/nrneurol.2014.181
Schwenk, M., Sabbagh, M., Lin, I., Morgan, P., Grewal, G. S., Mohler, J., et al. (2016). Sensor-based balance training with motion feedback in people with mild cognitive impairment. J. Rehabil. Res. Dev. 53, 945–958. doi: 10.1682/JRRD.2015.05.0089
Soh, S. L., Tan, C. W., Thomas, J. I., Tan, G., Xu, T., Ng, Y. L., et al. (2021). Falls efficacy: extending the understanding of self-efficacy in older adults towards managing falls. J. Frailty Sarcopenia Falls 6, 131–138. doi: 10.22540/JFSF-06-131
Tangen, G. G., Engedal, K., Bergland, A., Moger, T. A., and Mengshoel, A. M. (2014). Relationships between balance and cognition in patients with subjective cognitive impairment, mild cognitive impairment, and Alzheimer disease. Phys. Ther. 94, 1123–1134. doi: 10.2522/ptj.20130298
Taylor, M. E., Lord, S. R., Brodaty, H., Kurrle, S. E., Hamilton, S., Ramsay, E., et al. (2017). A home-based, carer-enhanced exercise program improves balance and falls efficacy in community-dwelling older people with dementia. Int. Psychogeriatr. 29, 81–91. doi: 10.1017/S1041610216001629
Taylor, M. E., Wesson, J., Sherrington, C., Hill, K. D., Kurrle, S., Lord, S. R., et al. (2021). Tailored exercise and home hazard reduction program for fall prevention in older people with cognitive impairment: the i-FOCIS randomized controlled trial. J. Gerontol. A Biol. Sci. Med. Sci. 76, 655–665. doi: 10.1093/gerona/glaa241
Tricco, A. C., Lillie, E., Zarin, W., O'Brien, K. K., Colquhoun, H., Levac, D., et al. (2018). PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann. Intern. Med. 169, 467–473. doi: 10.7326/M18-0850
Uemura, K., Shimada, H., Makizako, H., Doi, T., Tsutsumimoto, K., Yoshida, D., et al. (2014). Effects of mild and global cognitive impairment on the prevalence of fear of falling in community-dwelling older adults. Maturitas 78, 62–66. doi: 10.1016/j.maturitas.2014.02.018
Ullrich, P., Werner, C., Schonstein, A., Bongartz, M., Eckert, T., Beurskens, R., et al. (2022). Effects of a home-based physical training and activity promotion program in community-dwelling older persons with cognitive impairment after discharge from rehabilitation: a randomized controlled trial. J. Gerontol. A Biol. Sci. Med. Sci. 77, 2435–2444. doi: 10.1093/gerona/glac005
Uysal, I., Basar, S., Aysel, S., Kalafat, D., and Buyuksunnetci, A. O. (2023). Aerobic exercise and dual-task training combination is the best combination for improving cognitive status, mobility and physical performance in older adults with mild cognitive impairment. Aging Clin. Exp. Res. 35, 271–281. doi: 10.1007/s40520-022-02321-7
Varriano, B., Misquitta, K., Multani, N., Anor, C., Sulway, S., Dillon, W., et al. (2020). Vestibular exercises as a fall prevention strategy in patients with cognitive impairment. Can. J. Neurol. Sci. 47, 126–130. doi: 10.1017/cjn.2019.309
Wesson, J., Clemson, L., Brodaty, H., Lord, S., Taylor, M., Gitlin, L., et al. (2013). A feasibility study and pilot randomised trial of a tailored prevention program to reduce falls in older people with mild dementia. BMC Geriatr. 13:89. doi: 10.1186/1471-2318-13-89
World Health Organization (2021). Falls. Available at: https://www.who.int/news-room/fact-sheets/detail/falls (accessed August 19, 2022).
Zanetti, O., Vallotti, B., Frisoni, G. B., Geroldi, C., Bianchetti, A., Pasqualetti, P., et al. (1999). Insight in dementia: when does it occur? Evidence for a nonlinear relationship between insight and cognitive status. J. Gerontol. B 54B, P100–P106. doi: 10.1093/geronb/54B.2.P100
Zhang, W., Low, L. F., Gwynn, J. D., Beveridge, A. H., Harper, E., Mills, N., et al. (2021). A Safe mobilisation program to improve functional mobility and reduce fall risks in cognitively impaired older adults with higher level gait disorders: a pilot study. Dement. Geriatr. Cogn. Disord. 50, 364–371. doi: 10.1159/000519055
Zijlstra, G. A., van Haastregt, J. C., van Eijk, J. T., van Rossum, E., Stalenhoef, P. A., Kempen, G. I., et al. (2007). Prevalence and correlates of fear of falling, and associated avoidance of activity in the general population of community-living older people. Age Ageing 36, 304–309. doi: 10.1093/ageing/afm021
Keywords: cognitive impairment, older adults, fall prevention, balance confidence, exercise
Citation: Dove E, Hewston P, Wang RH, Patterson KK and Astell AJ (2024) Concerns about falling in people with Mild Cognitive Impairment and dementia: a scoping review of exercise interventions. Front. Dement. 3:1456125. doi: 10.3389/frdem.2024.1456125
Received: 28 June 2024; Accepted: 01 November 2024;
Published: 20 November 2024.
Edited by:
Ying Li, Jishou University, ChinaReviewed by:
Lenis Chen-Edinboro, University of North Carolina Wilmington, United StatesLambert Zixin Li, Stanford University, United States
Chen Li, Shanghai University of Engineering Sciences, China
Copyright © 2024 Dove, Hewston, Wang, Patterson and Astell. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Erica Dove, ZXJpY2EuZG92ZUBtYWlsLnV0b3JvbnRvLmNh
†ORCID: Erica Dove orcid.org/0000-0002-4016-5630
Patricia Hewston orcid.org/0000-0003-3787-7941
Rosalie H. Wang orcid.org/0000-0001-7777-9989
Kara K. Patterson orcid.org/0000-0001-8200-6403
Arlene J. Astell orcid.org/0000-0002-6822-9472
 Erica Dove
Erica Dove Patricia Hewston3†
Patricia Hewston3† Kara K. Patterson
Kara K. Patterson