- 1Department of Child and Adolescent Psychiatry, Carl von Ossietzky Universität Oldenburg, Oldenburg, Germany
- 2Department of Child and Adolescent Psychiatry, Faculty of Medicine, Technische Universität Dresden, Dresden, Germany
- 3Fachbereich Psychologie, Klinische Psychologie und Psychotherapie, Phillips Universität Marburg, Marburg, Germany
Introduction: Experiencing traumatic events (TEs), especially interpersonal TEs, is related to an increased risk of developing post-traumatic stress disorder (PTSD). Both TEs and PTSD are associated with a higher risk of substance use and problems in emotion regulation. Little is known about the associations between specific types of TEs, problems with general self-regulation (including cognitive and behavioral components) and substance use severity in adolescents. Knowledge on these associations could provide important approaches for prevention and therapy for adolescents with a history of trauma.
Methods: This study investigated associations between different types of TEs and PTSD, self-regulation and substance use severity. Moreover, participants were categorized into three groups according to their trauma status: (I) no history of TEs (noTEs), (II) history of TEs but no PTSD diagnosis (TEs), and (III) history of TEs and PTSD diagnosis (PTSD). Differences between the three groups were analyzed in terms of self-regulation and substance use severity. Our sample consisted of N = 89 adolescents aged 12 to 18 years in a child and adolescent psychiatric outpatient clinic in Germany. Substance use severity was only assessed in a smaller subsample (n = 37). Data were obtained from standardized diagnostic procedures and included information on types of TEs and PTSD diagnosis according to ICD-10, problems in self-regulation assessed with the Child Behavior Checklist (CBCL)/ Youth Self Report (YSR) Dysregulation Profile (DP), and substance use severity measured with the Drug Use Disorders Identification Test (DUDIT).
Results: We found that interpersonal TEs were significantly associated with higher rates of PTSD diagnosis compared to non-interpersonal TEs. We found no significant associations between different types of TEs and both problems in self-regulation and substance use severity. Moreover, our findings do not indicate differences in both self-regulation and substance use severity between trauma statuses (noTEs, TEs, PTSD).
Discussion: Future studies should consider other characteristics of TEs such as timing and duration when investigating associations with self-regulation. Longitudinal studies are needed to investigate developmental pathways, as a better understanding of the role of characteristics of TEs and self-regulation in the development of PTSD and substance use problems would provide opportunities for prevention and therapy for trauma-exposed patients.
1 Introduction
Throughout the lifespan, adolescence represents the period of highest risk for experiencing traumatic events (TEs) (1), with a correlation between a greater number of exposures to TEs over time and an increased likelihood of developing post-traumatic stress disorder (PTSD) (2). PTSD is defined as a specific reaction that may occur after the exposure to one or more TEs typically characterized by their “threatening or catastrophic nature”. It is manifested by the symptoms of re-experiencing in the form of flashbacks or nightmares, avoidance of trauma-associated stimuli and of heightened arousal (3).
Previous studies indicate a number of risk factors that influence the risk of developing PTSD following exposure to TEs. Certain sociodemographic risk factors such as female gender (4) or younger age in children (5) are associated with increased risk. Further findings suggest that both the quantity and severity of TEs may be a reliable predictor of the development of PTSD (6–8). TEs can be divided into interpersonal (“man-made” trauma, e.g., physical or sexual assault) and non-interpersonal (e.g., natural disasters, car accidents) types (9, 10). Different types of TEs have been demonstrated to influence the likelihood of developing PTSD. Research in adults indicates that interpersonal TEs are linked to a higher risk of developing PTSD compared to non-interpersonal TEs (11, 12). In particular, TEs related to violence, war (13, 14) and sexual assault are correlated with a higher risk of developing PTSD (7, 15). These associations have been investigated less frequently in adolescents. One study of children and adolescents aged 8–17 years aligns with findings from adult studies indicating that interpersonal TEs are associated with a higher risk of developing PTSD, while this is not the case for non-interpersonal TEs (16). In contrast, another study found no association between exposure to violence and the risk of PTSD in adolescents (17).
Both the experience of TEs and a PTSD have been found to be related to substance use (18, 19) and problems in emotion regulation (20, 21). Emotion regulation is a facet of self-regulation, a multidimensional construct that encompasses emotional, cognitive and behavioral regulation. It involves behaviors aimed at achieving goals or adapting to a context and is characterized by activation or inhibition (22–25). Self-regulation is thought to play a pivotal role in the development of psychiatric disorders across the lifespan (26–29).
The AAA-profile of the Child Behavior Checklist (CBCL) (30) comprises the scales anxiety/depression, attention problems and aggressive behavior and was initially regarded as a measure of juvenile bipolar disorder. Nowadays, it is thought to be a composite measure of emotional, cognitive and behavioral dysregulation (31) and is thus referred to as the Dysregulation Profile (DP). It can also be assessed using the corresponding self-report form of the CBCL, the Youth Self Report (YSR) (32, 33). Higher DP scores in YSR and CBCL indicate higher (emotional, cognitive and behavioral) dysregulation and thus more severe problems with self-regulation. Leibenluft, Charney (34) corroborated these findings and proposed the existence of a broad phenotype of severe mood and behavioral dysregulation characterized, for example, by increased reactivity and hyperarousal. They hypothesized that many individuals with at least one psychiatric diagnosis meet the criteria for this phenotype. Emotion dysregulation has been the subject of numerous studies investigating associations with TEs and PTSD. It has been shown to be influenced by the type of trauma, with higher emotional dysregulation being associated with interpersonal TEs compared to non-interpersonal TEs (35–37) and being a risk factor for the development of PTSD (36, 37). Moreover, emotion dysregulation appears to mediate the relationship between TEs and PTSD symptoms (37, 38). However, research on the relationship between self-regulation, encompassing cognitive and behavioral components, and both TEs and PTSD is lacking, although knowledge on these associations may provide further avenues for early prevention, for identifying high-risk groups prone to develop severe psychiatric problems such as PTSD, and for optimizing treatment of PTSD.
TEs and PTSD have also been linked to substance use disorder (SUD) in both adolescents and adults (18, 19). Basting, Medenblik (39) demonstrated in a sample of adults that a higher number of adverse childhood experiences is associated with the highest risk for posttraumatic stress symptoms and substance use problems. Several studies also indicate that adverse childhood experiences are associated with illicit substance use in adolescence (40, 41). Longitudinal studies confirm these results and indicate that adverse childhood experiences increase the risk for substance use in adolescence (42, 43). Some studies with adult samples have reported stronger associations between interpersonal TEs and later substance use (12, 44). One possible explanation for this could be that interpersonal TEs are usually related to more severe PTSD symptoms compared to non-interpersonal TEs (45). This in turn could be associated with greater substance use to cope with these symptoms (46, 47). On the other hand, reviews have not consistently confirmed these findings about the relationship for both adolescents and adults (48). In addition to examining the relationships between interpersonal and non-interpersonal TEs and substance use, no studies to date have examined the relationships between specific TEs and substance use among adolescents.
Previous studies also suggest associations between dysregulation and SUD. Clark, Donnellan (49) provide evidence that dysregulation, measured as temperamental reactivity, can predict later substance use in adolescence. Holtmann, Buchmann (50) showed that higher scores on the CBCL-DP at age 8 or 11 are associated with a higher risk of substance use at age 19. The authors discuss that dysregulation could follow different developmental trajectories. For example, SUD may reflect a type of (behavioral) dysregulation in adolescence.
To the best of our knowledge, this study is the first to investigate the relationship between specific types of TEs, dysregulation and SUD severity in a sample of adolescents. In addition, for the first time in this context, we will examine the DP as a more comprehensive measure of self-regulation, encompassing emotional, behavioral, and cognitive components. We will investigate its associations with substance use severity, as well as differences in DP and substance use severity in adolescents in three groups: (i) no history of TEs (noTEs), (ii) history of TEs but no PTSD (TEs), and (iii) history of TEs and PTSD (PTSD). While previous studies have focused on emotional regulation, this study is the first to examine a broader concept of self-regulation including emotional, behavioral and cognitive self-regulation in the context of trauma and substance use. This allows us to show for the first time whether there are abnormalities in self-regulation in patients in a psychiatric outpatient clinic. In addition, the current study's findings could provide important information for the optimization of prevention and therapy, as dysregulation could be specifically addressed during interventions. Of course, longitudinal studies would be necessary in the future to analyze causal relationships, but the results of the current study could be used to generate research questions for further investigation of the relationships and to investigate the role of emotional, behavioral and cognitive dysregulation in the development of psychopathology. Our study therefore has four objectives: Firstly, we seek to explore the relationship between different types of TEs and the risk of current PTSD in a sample of adolescents in two outpatient clinics. Building upon previous research, we expect trauma types to differ in their ability to explain PTSD and assume that experiencing interpersonal TEs such as war, terrorism and sexual assault will increase the risk for a current PTSD diagnosis compared to non-interpersonal TEs. Secondly, we will examine associations between different types of TEs, PTSD and DP as a measure of emotional, cognitive and behavioral dysregulation in adolescents. Previous findings on emotion dysregulation suggest the possibility of a stronger relationship between interpersonal TEs and dysregulation compared to non-interpersonal TEs. Moreover, we hypothesize that DP will be increased after TEs and in individuals diagnosed with PTSD compared to the noTEs group. Thirdly, we will investigate associations between TEs and substance use severity in adolescents. We assume that the association will be stronger for interpersonal TEs. In addition, we expect higher substance use severity in TEs and PTSD groups compared to noTEs group. Fourthly, the relationship between DP and substance use severity will be analyzed. We expect a positive correlation between DP and substance use severity.
In summary, a deeper understanding on the associations between TEs, PTSD, DP and substance use can provide important implication for prevention and therapy for children and adolescents, especially for those with a history of TEs.
2 Methods
2.1 Procedure
Data collection was embedded into the standard diagnostic procedure during admission to the Outpatient Clinic for Adolescent Substance Abuse and the Outpatient Clinic for Child and Adolescent Trauma, University Hospital C. G. Carus Dresden, Germany. After comprehensive verbal and written information, both the participants and their legal guardians gave their written informed consent for the anonymized diagnostic data to be used for research. All procedures were approved by the Institutional Review Board of the University Hospital C. G. Carus Dresden (EK 66022018). Patients did not receive reimbursements for participation in analyzed assessments.
2.2 Participants
Between November 2017 and January 2023, N = 740 patients contacted the outpatient clinics. N = 569 patients and their legal guardians agreed to the diagnostic data being used for research. We excluded patients who did not return CBCL and/or YSR questionnaires (N = 251), patients who were younger than 12 years of age (N = 80) as this study focuses on adolescents, patients with missing information on their age or gender (N = 4), patients with missing data on whether or not they had a history of TEs (N = 136), and patients with missing data on whether or not they had a PTSD diagnosis (N = 9) resulting in a final sample of N = 89 adolescents. Patients were 12.7–18.0 years old (M = 15.66, SD = 1.38). The sample consisted of N = 33 males (37.1%) and N = 56 females (62.9%). Participants were divided into three groups according to their trauma status: no history of TEs (noTEs), a history of TEs but no PTSD (TEs), and PTSD (PTSD).
2.3 Measures
2.3.1 PTSD diagnosis
Diagnoses were made in the outpatient clinics according to ICD-10 criteria. The diagnoses relied on the combination of information from (1) multiple individual meetings between clinic staff, adolescents, and their caregivers, (2) the German version of the UCLA Child/Adolescent PTSD Reaction Index for DSM-5 (51) and (3) the Diagnostic Interview for psychiatric disorders in children and adolescents [Diagnostisches Interview bei psychischen Störungen im Kindes- und Jugendalter; J-DIPS] (52, 53).
2.3.2 Dysregulation profile
A DP can be determined using the Youth Self Report (YSR/11–18) (54) and the Child Behaviour Checklist (CBCL/4–18) (30). The YSR, a self-report form for adolescents aged 11–18, and the corresponding caregiver report form, the CBCL/4–18, consist of 120 items which are answered on a 3-point-scale (0 = not applicable, 1 = sometimes, 2 = frequently). The DP is obtained by summing the t-values of the scales anxiety/depression, attention problems and aggressive behavior, which are assumed to reflect measures of emotional, cognitive and behavioral dysregulation, respectively (55, 56). This three-factor structure of the CBCL-DP was confirmed and validated in previous studies (57). It is therefore assumed that the DP reflects an overall measurement of dysregulation (55, 56). YSR/11–17 and CBCL/4–18 were handed out to patients and parents at the first consultation appointment. If both parents completed the CBCL/4–18, the mean of the two scores was calculated.
2.3.3 Substance use severity
The Drug Use Disorders Identification Test (DUDIT) is a self-report screening questionnaire consisting of 11 items to assess problems related to illegal drug use (58). Items 1–9 are rated on a 5-point Likert scale and items 10 and 11 are rated on a 3-point Likert scale. A total score with a maximum of 44 can be calculated by summing all item scores (58). The questionnaire was developed to assess problematic use of illegal drugs and initially evaluated in a Swedish adult sample (58). It is available free of charge in several languages from the European Monitoring Centre for Drugs and Drug Addiction (59) and has proven to be a useful and reliable diagnostic tool for assessing drug use in adolescents (60).
2.3.4 Control variables
Information on the age and gender of the adolescents was collected using a standardized generic questionnaire at the first consultation in the outpatient clinics.
2.3.5 Types of traumatic events
The types of TEs were determined using information assessed by clinical staff during the diagnostic process and/or information from the UCLA Child/Adolescent PTSD Reaction Index for DSM-5 (61). The information on traumatic events (TEs) was categorized according to the types of TEs assessed in the UCLA Child/Adolescent PTSD Reaction Index for DSM-5 (Steinberg et al., 2004). These types of TEs are: natural disaster; serious accident; war terrorism; domestic violence; a family member experiencing physical assault; physical assault, shots or threats of serious injury; witnessing physical attacks, shootings or the death of others; saw dead body; sexual assault; violent death or serious injury of a loved one; painful or threatening medical treatment; child neglect; others. These were divided into “interpersonal” or “non-interpersonal” TEs, and the following are assumed to be interpersonal TEs: war terrorism; domestic violence; family member experiencing physical assault; physical assault, shots or threats of serious injury; witnessing physical attacks, shootings or the death of other; sexual assault; violent death or serious injury of a loved one; child neglect.
2.4 Statistical analysis
All analyses were conducted using IBM SPSS Statistics, version 29.0. To investigate the differences in the likelihood of a PTSD diagnosis between adolescents with and without interpersonal TEs, we performed a chi square test with the groups TEs and PTSD as well as no interpersonal TEs and at least 1 interpersonal TE. To examine how different types of TEs were related to the likelihood of a PTSD diagnosis, we conducted a binary logistic regression. The types of TEs were included as dichotomous variables (yes/no) indicating whether the event was experienced or not.
T-tests were conducted to test for differences in YSR-DP and CBCL-DP between patients with and without a history of interpersonal trauma. Both measures are used because previous studies indicate differences between self-reports and parental reports of psychopathology and recommend using both to obtain more valid information (62). Due to the violation of normal distributions, a non-parametric Mann–Whitney U test was also performed. To further investigate how different types of TEs are associated with YSR-DP and CBCL-DP linear regressions were conducted with the different types of TEs as independent variables and YSR-DP and CBCL-DP as dependent variables. To investigate whether there are differences in YSR-DP and CBCL-DP depending on trauma status, a Multivariate analysis of variances (MANCOVA) was performed with trauma status (noTE/TE/PTSD) as a group factor, age and gender as control variables and YSR-DP and CBCL-DP as dependent variables.
T-tests were conducted to examine differences in the DUDIT score between patients with and without a history of interpersonal trauma. To further investigate how the different types of TEs were related to the DUDIT score, we performed a linear regression with the different types of TEs as independent variables and the DUDIT score as the dependent variable. To investigate the differences in DUDIT score depending on trauma status, a one-way ANOVA was conducted with trauma status (noTE/TE/PTSD) as the group factor and DUDIT score as the dependent variable.
Due to missing data in DUDIT questionnaires, the sample size is smaller for analyses that include the DUDIT as an outcome measure. No adjustment for multiple testing was made in any of the analyses, as these analyses were intended to be explorative and hypothesis-generating to guide future work in this area. An alpha value of 0.05 was used as the threshold for statistical significance. The effect sizes were classified according to Cohen (63) into small effects (|η2| ≥ .01), medium effects (|η2| ≥ .06), and large effects (|η2| ≥ .14).
3 Results
3.1 Traumatic events and PTSD
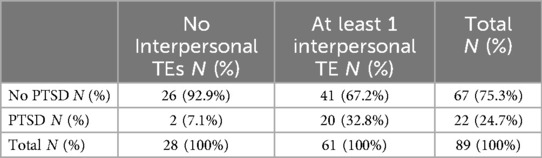
A chi-square test investigating the association between interpersonal TEs and PTSD diagnosis indicates that adolescents with interpersonal TEs show higher rates of PTSD [χ²(1) = 6.78, p = .009, φ = 0.276] (see Table 1).
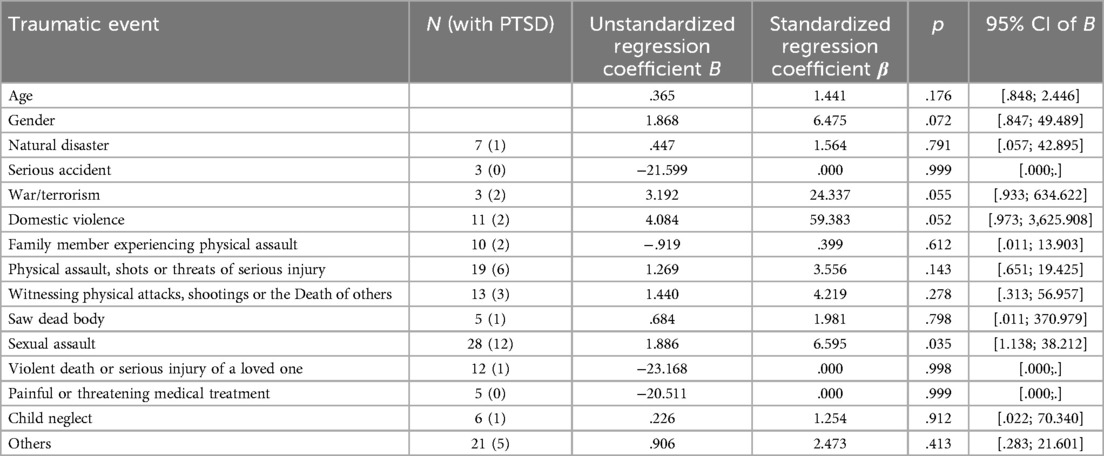
The binomial logistic regression model was statistically significant, χ²(15) = 30.71, p = .010, resulting in a medium amount of explained variance (Backhaus et al., 2003), as shown by Nagelkerke's R² = .466. The overall percentage of accuracy in classification was 83.8% with a sensitivity of 57.1% and a specificity of 93.2%. The variable sexual assault contributed significantly to the risk of PTSD (p = .035, OR = 6.595, 95% CI [21.138, 38.212]. All model coefficients and odds can be found in Table 2.
3.2 Traumatic events, PTSD and dysregulation profile
3.2.1 Associations between types of traumatic events and dysregulation profile
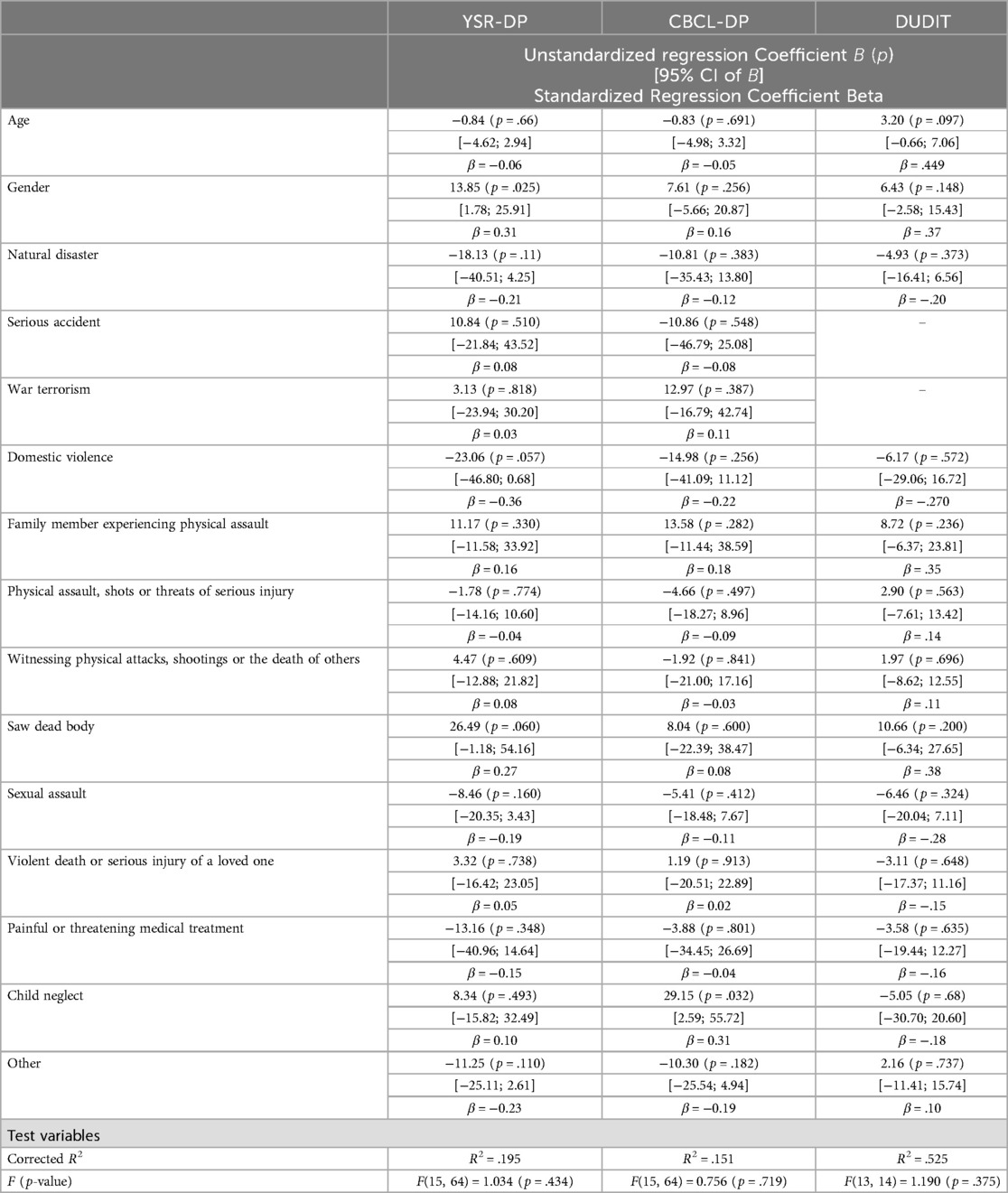
T-tests to test for differences in YSR-DP and CBCL-DP between patients with and without a history of interpersonal TEs obtained no significant differences between groups for YSR-DP [t(87) = 1.33, p = .187; U = 689.50, p = .146] and for CBCL-DP [t(87) = −0.409, p = .683].
Linear regressions were conducted to test whether there were significant associations between age, gender, and types of TEs and both YSR-DP and CBCL-DP. All model coefficients can be found in Table 3. The types of TEs were not able to explain YSR-DP [F(15, 64) = 1.034, p = .434] and CBCL-DP [F(15, 64) = 0.756, p = .719].
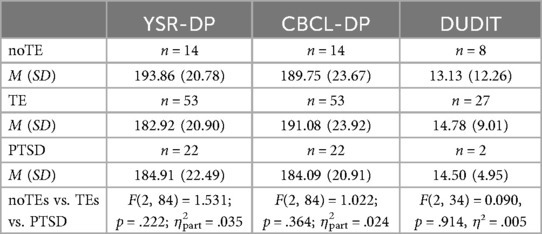
3.2.2 Group differences between noTEs, TEs and PTSD in dysregulation profile
A MANCOVA to investigate whether there are differences in DP depending on trauma status revealed no significant differences between groups [F(4, 168) = 1.543, p = .192, η²part = .035, Wilk's Λ = .930] (see also Table 4).
3.3 Traumatic events, PTSD and substance use severity
3.3.1 Associations between types of traumatic events and substance use severity
T-tests investigating differences in DUDIT score between patients with (N = 23, MDUDIT = 15.00, SD = 9.43) and without a history of interpersonal TEs (N = 14, MDUDIT = 13.43, SD = 9.71) revealed no significant difference in DUDIT score between groups [t(35) = −.762, p = .630].
A linear regression testing for significant associations between types of TEs and DUDIT score showed that types of TEs were not able to explain DUDIT scores [F(13, 14) = 1.190, p = .375]. All model coefficients can be found in Table 3.
3.3.2 Group differences between noTEs, TEs and PTSD in substance use severity
A one-way ANOVA to investigate differences in DUDIT score depending on trauma status did not reveal any statistically significant difference between groups [F(2, 34) = 0.090, p = .914, η² = .005] (see also Table 4).
3.4 Dysregulation and substance use severity
The Pearson correlation revealed no significant correlations between DUDIT score and YSR-DP (r = .275, p = .099) and between DUDIT score and CBCL-DP (r = .128, p = .451).
4 Discussion
In this study, we investigated a sample of adolescents in two German child psychiatric outpatient clinics. Our first aim was to examine relationships between different types of TEs and PTSD diagnoses. Secondly, we aimed to investigate the relationship between different types of TEs and DP and differences in DP according to trauma status (noTEs, TEs, PTSD). Third, we wanted to examine the relationship between types of TEs and substance use severity as well as differences between the three groups (noTEs, TEs, PTSD) in terms of substance use severity. Fourth, we aimed to investigate the association between DP and substance use severity. Our findings suggest that adolescents who have experienced interpersonal TEs exhibit higher rates of PTSD compared to adolescents who have not experienced interpersonal TEs. In particular, the experience of sexual assault contributed significantly to the explanation of PTSD. We found no associations between the different types of TEs and both DP and substance use severity and no differences between the three groups (noTEs, TEs, PTSD) in terms of DP and substance use severity. Moreover, substance use severity did not correlate significantly with both YSR-DP and CBCL-DP.
In line with previous findings, this study showed a stronger association between interpersonal TEs and PTSD compared to non-interpersonal TEs (9, 11, 12). In particular, the experience of sexual assault increased the risk of PTSD in our study. These results should be further investigated in longitudinal studies as they could provide important information for specific preventive measures against the development of PTSD for those affected by this type of TEs. In this study we found no association between the different types of TEs and both self- and parent-reported DP. In addition, no differences in DP were found between the three groups (noTEs, TEs, PTSD) in this study. As we know from previous research, the association between TEs and PTSD is affected by several factors (64, 65). For example, a current meta-analysis investigated peritraumatic risk factors for PTSD in children and adolescents (64). The authors reported that subjective threat during the trauma appears to increase the likelihood of developing PTSD in children and adolescents, although this factor alone cannot explain it. Nevertheless, these results suggest that, in addition to objective variables such as psychiatric diagnoses, the subjective experience of TEs appears to be related to posttraumatic consequences and could therefore also be associated with DP (64).
Several previous studies have linked emotion regulation to PTSD symptom severity (66), whereas we only compared DP between groups with and without PTSD diagnosis. It could also be that PTSD diagnoses are not generally characterized by higher DP scores, but that the severity of PTSD symptoms correlates with DP. In this context, it should also be noted that arousal or irritability are also part of the diagnostic criteria of PTSD (3). In our study, it is not possible to distinguish between dysregulation as a personality trait, dysregulation as a reaction following TEs and potential risk factor for developing PTSD and dysregulation as a PTSD symptom.
Furthermore, it has been observed that dysregulation is associated with psychopathology in general (67, 68). For example, Dölitzsch et al. (69), investigated children and adolescents aged 10–18 years in residential care. They compared those with T-scores ≥67 on the AAA-scales of YSR/CBCL with those below this cutoff and found that patients with a YSR-DP T-score ≥67 on the AAA-scales had more different psychiatric diagnoses than patients with a lower YSR-DP. These results suggest that the number of psychiatric diagnoses appears to be related to DP and should therefore be considered in future studies investigating relationships between TEs, PTSD and DP.
Due to the cross-sectional design of our study, we were not able to investigate causal relationships and developmental trajectories of DP and the development of PTSD. As Deutz et al. (70) show, YSR-DP and CBCL-DP seem to follow a non-linear developmental trajectory that appears to be relatively stable from 4 to 17 years, with a peak in adolescence. These findings suggest that early development and TEs in early childhood may have a greater impact on dysregulation, whereas the experience of TEs later in life may play a subordinate role. Therefore, it would be interesting for future research to consider not only the type of TEs but also the timing of TEs when investigating associations with dysregulation. Of course, additional factors that contribute to dysregulation independently of the TEs should also be included in the investigations.
Due to the design of our study, we were only able to investigate cross-sectional associations. Future studies should focus on longitudinal investigations to investigate causal relationships between dysregulation, TEs and PTSD as well as possible factors influencing the associations. These investigations would be an important step towards a better understanding of the developmental pathways of dysregulation and PTSD and would provide important approaches for prevention and intervention options for children and adolescents with a history of TEs.
We found no significant differences in substance use severity between adolescents with and without a history of interpersonal TEs. In accordance with previous studies, our results reveal that patients with a history of interpersonal trauma had, on average, higher mean substance use severity than patients without a history of interpersonal trauma (12, 44).
Besides, we found no significant associations between the different types of TEs and substance use severity. One explanation is that, in addition to the type of TEs, other factors could also mediate the relationship between TEs and substance use severity. Khoury et al. (71), investigated associations between physical, sexual and emotional abuse in childhood and the use of alcohol, cocaine, opiates, cannabis and tobacco in adulthood. They reported associations between certain types of TEs and the use of different substances. Because our sample was too small to conduct analyses for different subsamples of substances, we were not able to investigate these associations.
Previous research also suggests that the association between TEs and substance use severity is mediated by trauma-related factors such as posttraumatic stress symptoms (19, 72). As posited by the self-medication hypothesis, substance use serves as a coping mechanism for managing symptoms of PTSD (46, 47). Therefore, the use of certain substances appears to differ depending on trauma-related symptoms and the specific effects of the different substances (47, 73). For example, Dworkin et al. (74) reported an association between hyperarousal symptoms and cocaine use disorder, while others did not find this relationship (75, 76). Even less is known about these associations in adolescents. One study that examined associations between trauma symptom clusters and MDMA use found a relationship between avoidance symptoms and use of MDMA (77).
Overall, further research is needed to gain a better understanding of the association between types of TEs and substance use severity and potential mediating factors. A recent review suggests that early risks such as child maltreatment increase the risks for earlier and more severe substance use in adolescence and for later SUD (78), which emphasizes the importance of considering these associations in therapeutic approaches for at-risk adolescents.
In our study, we also found no significant differences in substance use severity between the three groups (noTEs, TEs, PTSD). It should be noted that only n = 2 adolescents were included in the PTSD group. However, the mean substance use severity scores were higher for the TEs and the PTSD groups compared to the noTEs group, although the differences were not significant. These findings are consistent with previous studies (18), although surprisingly the mean substance use severity was higher in the TEs group than in the PTSD group. Due to the small sample sizes results should be interpreted with caution.
Our results reveal no correlation between substance use severity and self-and parent-reported DP (79, 80). These results are in contrast to former research findings (49). It might be possible, that substance use is rather associated with emotion regulation than with general self-regulation in adolescents. In addition, previous studies indicate that the relationship between emotional dysregulation and substance use varies depending on the substance consumed (81). Characteristics such as substances used, but also frequency or amount could be taken into account in future studies.
Cooper et al. (82) made one of the first attempts to investigate the relationship between the three variables TEs, dysregulation and SUD in a sample of adolescents. Childhood maltreatment, substance use and emotional, behavioral and cognitive dysregulation were assessed at the age of 10–12 years and again 1, 2 and 3 years later. The results showed positive associations between the extent of childhood maltreatment and emotional and behavioral dysregulation as well as between emotional and behavioral dysregulation and substance use. Further, emotional and behavioral dysregulation mediated the association between childhood maltreatment and substance use. Although the findings of Cooper et al. (82) suggest a mediating role of dysregulation in the association between TEs and substance use, the assumption of linear relationships between predictor (TEs), mediator (dysregulation) and criterion (substance use) could not be confirmed in our study, so we were unable to investigate these associations in our sample. However, further investigations on this association would be important as they may provide important insights into the apparently complex developmental pathways and interactions of dysregulation and substance use severity in adolescents with a history of trauma.
As the present study is an exploratory study, no adjustment for multiple testing was applied. The results must therefore be interpreted cautiously. Additionally, the subsamples in the various analyses are limited and the analyses on substance use severity were only conducted with a smaller subsample due to the lack of DUDIT questionnaires. Since we used cross-sectional data, no conclusions about causal relationships can be drawn. Prospective longitudinal studies are needed to investigate causal relationships and developmental pathways of PTSD, dysregulation and substance use severity in adolescents with a history of TEs.
Altogether, our results suggest that interpersonal TEs are associated with a higher risk of PTSD, whereas we found no association between TEs and both DP and substance use severity in a sample of adolescents with trauma history in an outpatient clinic. Our findings underscore the significance of early interventions aimed at adolescents who have encountered interpersonal TEs. Longitudinal investigations are essential for elucidating causal relationships and developmental trajectories, while also considering comorbidities and attributes of traumatic events, including number, timing and duration. Furthermore, dysregulation should not only be investigated as a consequence or correlate of PTSD and substance use, but also as a risk factor, that develops as a function of various factors and could influence the development of psychopathology, especially after TEs. Longitudinal studies and comparisons between clinical and non-clinical samples could improve the understanding of the role of self-regulation in the development of psychiatric disorders. A deeper comprehension of these associations could provide valuable perspectives for prevention and therapeutic interventions for individuals who have been exposed to trauma.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by University Hospital C. G. Carus Dresden. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
Author contributions
ER: Conceptualization, Data curation, Formal Analysis, Writing – original draft, Writing – review & editing, Investigation. LB: Conceptualization, Writing – original draft, Writing – review & editing, Data curation, Investigation. VR: Supervision, Writing – original draft, Writing – review & editing, Project administration, Resources. YG: Writing – original draft, Writing – review & editing, Conceptualization, Funding acquisition, Project administration, Resources, Supervision.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The Sächsische Aufbaubank -Förderbank-, (grant 100362999 to YG) and Roland Ernst Stiftung für Gesundheitswesen (grant “DELTA-JU 6/21” to YG), funded this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Breslau N. The epidemiology of trauma, PTSD, and other posttrauma disorders. Trauma Violence Abuse. (2009) 10(3):198–210. doi: 10.1177/1524838009334448
2. Suliman S, Mkabile SG, Fincham DS, Ahmed R, Stein DJ, Seedat S. Cumulative effect of multiple trauma on symptoms of posttraumatic stress disorder, anxiety, and depression in adolescents. Compr Psychiatry. (2009) 50(2):121–7. doi: 10.1016/j.comppsych.2008.06.006
3. World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization (1992).
4. Hiscox LV, Hiller R, Fraser A, Rabie S, Stewart J, Seedat S, et al. Sex differences in post-traumatic stress disorder in a high adversity cohort of South African adolescents: an examination of depressive symptoms, age, and trauma type as explanatory factors. Eur J Psychotraumatol. (2021) 12(1):1978669. doi: 10.1080/20008198.2021.1978669
5. Schreier H, Ladakakos C, Morabito D, Chapman L, Knudson MM. Posttraumatic stress symptoms in children after mild to moderate pediatric trauma: a longitudinal examination of symptom prevalence, correlates, and parent-child symptom reporting. J Trauma. (2005) 58(2):353–63. doi: 10.1097/01.TA.0000152537.15672.B7
6. Wilker S, Pfeiffer A, Kolassa S, Koslowski D, Elbert T, Kolassa IT. How to quantify exposure to traumatic stress? Reliability and predictive validity of measures for cumulative trauma exposure in a post-conflict population. Eur J Psychotraumatol. (2015) 6:28306. doi: 10.3402/ejpt.v6.28306
7. Gnanadesikan M, Novins DK, Beals J. The relationship of gender and trauma characteristics to posttraumatic stress disorder in a community sample of traumatized northern plains American Indian adolescents and young adults. J Clin Psychiatry. (2005) 66(9):1176–83. doi: 10.4088/JCP.v66n0914
8. Scott ST. Multiple traumatic experiences and the development of posttraumatic stress disorder. J Interpers Violence. (2007) 22(7):932–8. doi: 10.1177/0886260507301226
9. Forbes D, Lockwood E, Phelps A, Wade D, Creamer M, Bryant RA, et al. Trauma at the hands of another: distinguishing PTSD patterns following intimate and nonintimate interpersonal and noninterpersonal trauma in a nationally representative sample. J Clin Psychiatry. (2014) 75(2):147–53. doi: 10.4088/JCP.13m08374
10. Berenz EC, Cho SB, Overstreet C, Kendler K, Amstadter AB, Dick DM. Longitudinal investigation of interpersonal trauma exposure and alcohol use trajectories. Addict Behav. (2016) 53:67–73. doi: 10.1016/j.addbeh.2015.09.014
11. Ferry F, Bunting B, Murphy S, O’Neill S, Stein D, Koenen K. Traumatic events and their relative PTSD burden in northern Ireland: a consideration of the impact of the ‘Troubles’. Soc Psychiatry Psychiatr Epidemiol. (2014) 49(3):435–46. doi: 10.1007/s00127-013-0757-0
12. Dell'Aquila A, Berle D. Predictors of alcohol and substance use among people with post-traumatic stress disorder (PTSD): findings from the NESARC-III study. Soc Psychiatry Psychiatr Epidemiol. (2023) 58(10):1509–22. doi: 10.1007/s00127-023-02472-6
13. Conrad D, Wilker S, Pfeiffer A, Lingenfelder B, Ebalu T, Lanzinger H, et al. Does trauma event type matter in the assessment of traumatic load? Eur J Psychotraumatol. (2017) 8(1):1344079. doi: 10.1080/20008198.2017.1344079
14. Holbrook TL, Hoyt DB, Stein MB, Sieber WJ. Perceived threat to life predicts posttraumatic stress disorder after major trauma: risk factors and functional outcome. J Trauma. (2001) 51(2):287–92; discussion 92–3. doi: 10.1097/00005373-200108000-00010
15. Perrin M, Vandeleur CL, Castelao E, Rothen S, Glaus J, Vollenweider P, et al. Determinants of the development of post-traumatic stress disorder, in the general population. Soc Psychiatry Psychiatr Epidemiol. (2014) 49(3):447–57. doi: 10.1007/s00127-013-0762-3
16. Luthra R, Abramovitz R, Greenberg R, Schoor A, Newcorn J, Schmeidler J, et al. Relationship between type of trauma exposure and posttraumatic stress disorder among urban children and adolescents. J Interpers Violence. (2009) 24(11):1919–27. doi: 10.1177/0886260508325494
17. Milan S, Zona K, Acker J, Turcios-Cotto V. Prospective risk factors for adolescent PTSD: sources of differential exposure and differential vulnerability. J Abnorm Child Psychol. (2013) 41(2):339–53. doi: 10.1007/s10802-012-9677-9
18. Schiff M, Fang L. Adolescents’ exposure to disasters and substance use. Curr Psychiatry Rep. (2016) 18(6):57. doi: 10.1007/s11920-016-0693-2
19. Basedow LA, Kuitunen-Paul S, Roessner V, Golub Y. Traumatic events and substance use disorders in adolescents. Front Psychiatry. (2020) 11:559. doi: 10.3389/fpsyt.2020.00559
20. Villalta L, Smith P, Hickin N, Stringaris A. Emotion regulation difficulties in traumatized youth: a meta-analysis and conceptual review. Eur Child Adolesc Psychiatry. (2018) 27(4):527–44. doi: 10.1007/s00787-018-1105-4
21. Lackner CL, Santesso DL, Dywan J, O’Leary DD, Wade TJ, Segalowitz SJ. Adverse childhood experiences are associated with self-regulation and the magnitude of the error-related negativity difference. Biol Psychol. (2018) 132:244–51. doi: 10.1016/j.biopsycho.2018.01.006
22. McClelland MM, Ponitz CC, Messersmith EE, Tominey S. Self-Regulation. The Handbook of Life-Span Development. Hoboken, New Jersey: John Wiley & Sons, Inc. (2010).
23. Gagne JR, Liew J, Nwadinobi OK. How does the broader construct of self-regulation relate to emotion regulation in young children? Dev Rev. (2021) 60:100965. doi: 10.1016/j.dr.2021.100965
24. Bridgett DJ, Burt NM, Edwards ES, Deater-Deckard K. Intergenerational transmission of self-regulation: a multidisciplinary review and integrative conceptual framework. Psychol Bull. (2015) 141(3):602–54. doi: 10.1037/a0038662
25. Nigg JT. Annual research review: on the relations among self-regulation, self-control, executive functioning, effortful control, cognitive control, impulsivity, risk-taking, and inhibition for developmental psychopathology. J Child Psychol Psychiatry. (2017) 58(4):361–83. doi: 10.1111/jcpp.12675
26. Eisenberg N, Valiente C, Spinrad TL, Liew J, Zhou Q, Losoya SH, et al. Longitudinal relations of children’s effortful control, impulsivity, and negative emotionality to their externalizing, internalizing, and co-occurring behavior problems. Dev Psychol. (2009) 45(4):988–1008. doi: 10.1037/a0016213
27. Wakschlag LS, Choi SW, Carter AS, Hullsiek H, Burns J, McCarthy K, et al. Defining the developmental parameters of temper loss in early childhood: implications for developmental psychopathology. J Child Psychol Psychiatry. (2012) 53(11):1099–108. doi: 10.1111/j.1469-7610.2012.02595.x
28. Zucker RA, Heitzeg MM, Nigg JT. Parsing the undercontrol/disinhibition pathway to substance use disorders: a multilevel developmental problem. Child Dev Perspect. (2011) 5(4):248–55. doi: 10.1111/j.1750-8606.2011.00172.x
29. Fineberg NA, Chamberlain SR, Goudriaan AE, Stein DJ, Vanderschuren LJ, Gillan CM, et al. New developments in human neurocognition: clinical, genetic, and brain imaging correlates of impulsivity and compulsivity. CNS Spectr. (2014) 19(1):69–89. doi: 10.1017/S1092852913000801
30. Arbeitsgruppe Deutsche Child Behavior Checklist. Elternfragebogen über das Verhalten von Kindern und Jugendlichen; Deutsche Bearbeitung der Child Behavior Checklist (CBCL/4-18). Cologne: Einführung und Anleitung zur Handauswertung (1998). p. 2.
31. Althoff RR, Rettew DC, Faraone SV, Boomsma DI, Hudziak JJ. Latent class analysis shows strong heritability of the child behavior checklist-juvenile bipolar phenotype. Biol Psychiatry. (2006) 60(9):903–11. doi: 10.1016/j.biopsych.2006.02.025
32. Achenbach TM. Manual for ASEBA School-age Forms & Profiles. Burlington, NJ: University of Vermont, Research Center for Children, Youth & Families (2001).
33. Deutz MH, Geeraerts SB, van Baar AL, Deković M, Prinzie P. The dysregulation profile in middle childhood and adolescence across reporters: factor structure, measurement invariance, and links with self-harm and suicidal ideation. Eur Child Adolesc Psychiatry. (2016) 25(4):431–42. doi: 10.1007/s00787-015-0745-x
34. Leibenluft E, Charney DS, Towbin KE, Bhangoo RK, Pine DS. Defining clinical phenotypes of juvenile mania. Am J Psychiatry. (2003) 160(3):430–7. doi: 10.1176/appi.ajp.160.3.430
35. Berfield JB, Goncharenko S, Forkus SR, Contractor AA, Weiss NH. The differential relation of trauma types with negative and positive emotion dysregulation. Anxiety Stress Coping. (2022) 35(4):425–39. doi: 10.1080/10615806.2021.1964072
36. Contractor AA, Weiss NH, Natesan P, Elhai JD. Clusters of trauma types as measured by the life events checklist for DSM-5. Int J Stress Manag. (2020) 27(4):380–93. doi: 10.1037/str0000179
37. Raudales AM, Short NA, Schmidt NB. Emotion dysregulation mediates the relationship between trauma type and PTSD symptoms in a diverse trauma-exposed clinical sample. Pers Individ Dif. (2019) 139:28–33. doi: 10.1016/j.paid.2018.10.033
38. Barlow MR, Goldsmith Turow RE, Gerhart J. Trauma appraisals, emotion regulation difficulties, and self-compassion predict posttraumatic stress symptoms following childhood abuse. Child Abuse Negl. (2017) 65:37–47. doi: 10.1016/j.chiabu.2017.01.006
39. Basting EJ, Medenblik AM, Eberwein JD, Garner AR, Shorey RC, Stuart GL. Adverse childhood experiences, posttraumatic stress disorder symptoms, and compulsive behaviors among adults in substance use treatment: a latent class analysis. J Trauma Stress. (2024). doi: 10.1002/jts.23079
40. Pakdaman S, Unger JB, Forster M, Rogers CJ, Sussman SY, Benjamin SM. Childhood trauma and prescription drug misuse in a college population. Subst Use Misuse. (2021) 56(1):140–4. doi: 10.1080/10826084.2020.1846056
41. Forster M, Grigsby TJ, Rogers CJ, Benjamin SM. The relationship between family-based adverse childhood experiences and substance use behaviors among a diverse sample of college students. Addict Behav. (2018) 76:298–304. doi: 10.1016/j.addbeh.2017.08.037
42. Patel H, Tapert SF, Brown SA, Norman SB, Pelham WE III. Do traumatic events and substance use co-occur during adolescence? Testing three causal etiologic hypotheses. J Child Psychol Psychiatry. (2024) 65(10):1388–97. doi: 10.1111/jcpp.13985
43. Mongan D, Millar SR, Brennan MM, Doyle A, Galvin B, McCarthy N. Associations and mediating factors between adverse childhood experiences and substance use behaviours in early adulthood: a population-based longitudinal study. Addict Behav. (2024) 161:108194. doi: 10.1016/j.addbeh.2024.108194
44. Cisler JM, Begle AM, Amstadter AB, Resnick HS, Danielson CK, Saunders BE, et al. Exposure to interpersonal violence and risk for PTSD, depression, delinquency, and binge drinking among adolescents: data from the NSA-R. J Trauma Stress. (2012) 25(1):33–40. doi: 10.1002/jts.21672
45. Forbes D, Fletcher S, Parslow R, Phelps A, O'Donnell M, Bryant RA, et al. Trauma at the hands of another: longitudinal study of differences in the posttraumatic stress disorder symptom profile following interpersonal compared with noninterpersonal trauma. J Clin Psychiatry. (2012) 73(3):372–6. doi: 10.4088/JCP.10m06640
46. Hawn SE, Cusack SE, Amstadter AB. A systematic review of the self-medication hypothesis in the context of posttraumatic stress disorder and comorbid problematic alcohol use. J Trauma Stress. (2020) 33(5):699–708. doi: 10.1002/jts.22521
47. Basedow LA, Wiedmann MF, Roessner V, Golub Y, Kuitunen-Paul S. Coping motives mediate the relationship between PTSD and MDMA use in adolescents with substance use disorders. Addict Sci Clin Pract. (2022) 17(1):46. doi: 10.1186/s13722-022-00329-y
48. Konkolÿ Thege B, Horwood L, Slater L, Tan MC, Hodgins DC, Wild TC. Relationship between interpersonal trauma exposure and addictive behaviors: a systematic review. BMC Psychiatry. (2017) 17(1):164. doi: 10.1186/s12888-017-1323-1
49. Clark DA, Donnellan MB, Robins RW, Conger RD. Early adolescent temperament, parental monitoring, and substance use in Mexican-origin adolescents. J Adolesc. (2015) 41:121–30. doi: 10.1016/j.adolescence.2015.02.010
50. Holtmann M, Buchmann AF, Esser G, Schmidt MH, Banaschewski T, Laucht M. The child behavior checklist-dysregulation profile predicts substance use, suicidality, and functional impairment: a longitudinal analysis. J Child Psychol Psychiatry. (2011) 52(2):139–47. doi: 10.1111/j.1469-7610.2010.02309.x
51. Ruf M, Schauer M, Elbert T. UPID: UCLA PTSD Index for DSM IV (Child Version, Revision 1, Deutsche Fassung). Göttingen: Hogrefe (2011).
52. Margraf J, Cwik JC, Pflug V, Schneider S. Strukturierte klinische interviews zur erfassung psychischer störungen über die lebensspanne: gütekriterien und weiterentwicklungen der DIPS-verfahren. [Structured clinical interviews for mental disorders across the life span: psychometric quality and further developments of the DIPS open access interviews.]. Z Klin Psychol Psychother. (2017) 46(3):176–86. doi: 10.1026/1616-3443/a000430
53. Schneider S, Pflug V, In-Albon T, Margraf J. Kinder-DIPS Open Access: Diagnostisches Interview bei Psychischen Störungen im Kindes- und Jugendalter. Bochum: Forschungs- und Behandlungszentrum für psychische Gesundheit, Ruhr-Universität Bochum (2017).
54. Arbeitsgruppe Deutsche Child Behavior Checklist. Fragebogen für Jugendliche; Deutsche Bearbeitung der Youth Self-Report Form der Child Behavior Checklist (YSR). Cologne: Einführung und Anleitung zur Handauswertung (1998). p. 2.
55. Althoff RR, Ayer LA, Rettew DC, Hudziak JJ. Assessment of dysregulated children using the child behavior checklist: a receiver operating characteristic curve analysis. Psychol Assess. (2010) 22(3):609–17. doi: 10.1037/a0019699
56. Ayer L, Althoff R, Ivanova M, Rettew D, Waxler E, Sulman J, et al. Child behavior checklist juvenile bipolar disorder (CBCL-JBD) and CBCL posttraumatic stress problems (CBCL-PTSP) scales are measures of a single dysregulatory syndrome. J Child Psychol Psychiatry. (2009) 50(10):1291–300. doi: 10.1111/j.1469-7610.2009.02089.x
57. Geeraerts SB, Deutz MH, Deković M, Bunte T, Schoemaker K, Espy KA, et al. The child behavior checklist dysregulation profile in preschool children: a broad dysregulation syndrome. J Am Acad Child Adolesc Psychiatry. (2015) 54(7):595–602.e2. doi: 10.1016/j.jaac.2015.04.012
58. Berman AH, Bergman H, Palmstierna T, Schlyter F. Evaluation of the drug use disorders identification test (DUDIT) in criminal justice and detoxification settings and in a Swedish population sample. Eur Addict Res. (2005) 11(1):22–31. doi: 10.1159/000081413
59. EMCDDA. Drug Use Disorders Identification Test (DUDIT). Available online at: https://www.emcdda.europa.eu/drugs-library/drug-use-disorders-identification-test-dudit_en (accessed September 22, 2023).
60. Basedow LA, Kuitunen-Paul S, Eichler A, Roessner V, Golub Y. Diagnostic accuracy of the drug use disorder identification test and its short form, the DUDIT-C, in German adolescent psychiatric patients. Front Psychol. (2021) 12:678819. doi: 10.3389/fpsyg.2021.678819
61. Steinberg AM, Brymer MJ, Decker KB, Pynoos RS. The university of California at Los Angeles post-traumatic stress disorder reaction Index. Curr Psychiatry Rep. (2004) 6(2):96–100. doi: 10.1007/s11920-004-0048-2
62. Kuitunen-Paul S, Eichler A, Wiedmann M, Basedow LA, Roessner V, Golub Y. Comparing self-report and parental report of psychopathologies in adolescents with substance use disorders. Eur Child Adolesc Psychiatry. (2023) 32(2):331–42. doi: 10.1007/s00787-021-01865-9
63. Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Mahwah, NJ: Erlbaum (1988).
64. Memarzia J, Walker J, Meiser-Stedman R. Psychological peritraumatic risk factors for post-traumatic stress disorder in children and adolescents: a meta-analytic review. J Affect Disord. (2021) 282:1036–47. doi: 10.1016/j.jad.2021.01.016
65. Trickey D, Siddaway AP, Meiser-Stedman R, Serpell L, Field AP. A meta-analysis of risk factors for post-traumatic stress disorder in children and adolescents. Clin Psychol Rev. (2012) 32(2):122–38. doi: 10.1016/j.cpr.2011.12.001
66. Ehring T, Quack D. Emotion regulation difficulties in trauma survivors: the role of trauma type and PTSD symptom severity. Behav Ther. (2010) 41(4):587–98. doi: 10.1016/j.beth.2010.04.004
67. Bradley B, DeFife JA, Guarnaccia C, Phifer J, Fani N, Ressler KJ, et al. Emotion dysregulation and negative affect: association with psychiatric symptoms. J Clin Psychiatry. (2011) 72(5):685–91. doi: 10.4088/JCP.10m06409blu
68. McLaughlin KA, Hatzenbuehler ML, Mennin DS, Nolen-Hoeksema S. Emotion dysregulation and adolescent psychopathology: a prospective study. Behav Res Ther. (2011) 49(9):544–54. doi: 10.1016/j.brat.2011.06.003
69. Dölitzsch C, Kölch M, Fegert JM, Schmeck K, Schmid M. Ability of the child behavior checklist-dysregulation profile and the youth self report-dysregulation profile to identify serious psychopathology and association with correlated problems in high-risk children and adolescents. J Affect Disord. (2016) 205:327–34. doi: 10.1016/j.jad.2016.08.010
70. Deutz MHF, Vossen HGM, De Haan AD, Deković M, Van Baar AL, Prinzie P. Normative development of the child behavior checklist dysregulation profile from early childhood to adolescence: associations with personality pathology. Dev Psychopathol. (2018) 30(2):437–47. doi: 10.1017/S0954579417000955
71. Khoury L, Tang YL, Bradley B, Cubells JF, Ressler KJ. Substance use, childhood traumatic experience, and posttraumatic stress disorder in an urban civilian population. Depress Anxiety. (2010) 27(12):1077–86. doi: 10.1002/da.20751
72. Park T, Thompson K, Wekerle C, Al-Hamdani M, Smith S, Hudson A, et al. Posttraumatic stress symptoms and coping motives mediate the association between childhood maltreatment and alcohol problems. J Trauma Stress. (2019) 32(6):918–26. doi: 10.1002/jts.22467
73. Basedow LA, Wiedmann MF, Kuitunen-Paul S, Roessner V, Golub Y. Attenuated psychotic symptoms, substance use and self-reported PTSD in adolescence. Eur J Psychotraumatol. (2023) 14(2):2193327. doi: 10.1080/20008066.2023.2193327
74. Dworkin ER, Wanklyn S, Stasiewicz PR, Coffey SF. PTSD Symptom presentation among people with alcohol and drug use disorders: comparisons by substance of abuse. Addict Behav. (2018) 76:188–94. doi: 10.1016/j.addbeh.2017.08.019
75. Avant E, Davis J, Cranston C. Posttraumatic stress symptom clusters, trauma history, and substance use among college students. Journal of aggression. Maltreatment & Trauma. (2011) 20:539–55. doi: 10.1080/10926771.2011.588153
76. Tull MT, Gratz KL, Aklin WM, Lejuez CW. A preliminary examination of the relationships between posttraumatic stress symptoms and crack/cocaine, heroin, and alcohol dependence. J Anxiety Disord. (2010) 24(1):55–62. doi: 10.1016/j.janxdis.2009.08.006
77. Basedow LA, Kuitunen-Paul S, Wiedmann MF, Roessner V, Golub Y. Self-reported PTSD is associated with increased use of MDMA in adolescents with substance use disorders. Eur J Psychotraumatol. (2021) 12(1):1968140. doi: 10.1080/20008198.2021.1968140
78. Kirsch DE, Lippard ETC. Early life stress and substance use disorders: the critical role of adolescent substance use. Pharmacol Biochem Behav. (2022) 215:173360. doi: 10.1016/j.pbb.2022.173360
79. Rescorla L, Ewing G, Ivanova M, Aebi M, Bilenberg N, Dieleman G, et al. Parent–adolescent cross-informant agreement in clinically referred samples: findings from seven societies. Journal of Clinical Child & Adolescent Psychology. (2017) 46:74–87. doi: 10.1080/15374416.2016.1266642
80. Rescorla L, Ginzburg S, Achenbach T, Ivanova M, Almqvist F, Begovac I, et al. Cross-Informant agreement between parent-reported and adolescent self-reported problems in 25 societies. Journal of clinical child and adolescent psychology: the official journal for the society of clinical child and adolescent psychology, American psychological association. Division. (2012) 53:42. doi: 10.1080/15374416.2012.717870
81. González-Roz A, Castaño Y, Krotter A, Salazar-Cedillo A, Gervilla E. Emotional dysregulation in relation to substance use and behavioral addictions: findings from five separate meta-analyses. Int J Clin Health Psychol. (2024) 24(3):100502. doi: 10.1016/j.ijchp.2024.100502
Keywords: adolescents, traumatic events, PTSD–posttraumatic stress disorder, dysregulation profile, substance use
Citation: Reyentanz E, Basedow LA, Roessner V and Golub Y (2024) PTSD, dysregulation profile and substance use: exploring differences in a sample of adolescents in an outpatient clinic. Front. Child Adolesc. Psychiatry 3:1421486. doi: 10.3389/frcha.2024.1421486
Received: 22 April 2024; Accepted: 25 November 2024;
Published: 19 December 2024.
Edited by:
Eva Möhler, Saarland University Hospital, GermanyReviewed by:
Mauro Ceccanti, Sapienza University of Rome, ItalyIsabelle V. Daignault, Université de Montréal, Canada
Copyright: © 2024 Reyentanz, Basedow, Roessner and Golub. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Emely Reyentanz, ZW1lbHkucmV5ZW50YW56QHVuaS1vbGRlbmJ1cmcuZGU=
 Emely Reyentanz
Emely Reyentanz Lukas A. Basedow
Lukas A. Basedow Veit Roessner2
Veit Roessner2