- 1Military Population Health Directorate, Naval Health Research Center, San Diego, CA, United States
- 2Performance and Readiness Division, Leidos, Inc., San Diego, CA, United States
Background: Adolescence is a particularly sensitive period of development for military-connected youth, given the socioemotional and physical changes that occur against the backdrop of the military career of their parent(s). Military-connected adolescents face unique stressors relative to their civilian counterparts, such as military relocations, parental absence due to deployments and trainings, and parental military-related physical and mental injury. These stressors may change family dynamics and disrupt social support networks, which can have lasting implications for adolescent health and well-being. At present, very little is known about how the current generation of military-connected adolescents are faring regarding their psychological and physical health, academic achievement, and educational or career aspirations. As part of the Biden-Harris Administration's commitment to military families, the U.S. Department of Defense pledged to address these major knowledge gaps by supporting the Study of Adolescent Resilience (SOAR). SOAR's longitudinal design provides a powerful tool for evaluating the effects of military family life on adolescent well-being into early adulthood.
Methods and design: SOAR is embedded within the larger Millennium Cohort Study, the first U.S. population-based prospective study to investigate long-term health effects of military service among active duty service members. Nearly 40,000 Millennium Cohort participants with adolescent children were invited to complete a web-based self-report survey that included items across interpersonal, socioenvironmental, and health domains, among others. Military parents provided referral information for their adolescent child and another primary parental figure, when available, to be invited to SOAR. This approach allowed survey data to be linked between these three family members (service member, spouse, and adolescent) to promote a comprehensive, family systems-based understanding of military-connected adolescent experiences and determinants of health, risk, and resilience.
Discussion: Research findings will shed light on the enduring impact of military life on adolescents and the nature of associations between military-specific experiences and psychosocial health and well-being. Further, this research will assess modifiable risk and protective factors that may elucidate differences in military-connected adolescent psychosocial development and physical health, academic achievement, and educational and military career aspirations over time.
Conclusions: Findings gleaned from this research will be used to inform existing policy and programs designed to promote adolescent resilience.
1 Introduction
There are over 1.6 million children with a parent in the U.S. military, of whom about one quarter are adolescents between the ages of 12 and 18 years (1). Adolescence is a sensitive period of development in many areas that are critical to healthy adult functioning, such as the formation of a strong identity and independent sense of self (2, 3). Adolescents’ relationships with their parents transform during adolescence, and peers become more influential as adolescents spend more time away from home (4, 5). These social changes intersect with intense biological changes, including hormonal shifts that contribute to the development of mental health problems such as depression and anxiety, with rates peaking as adolescents approach young adulthood (6). Specifically, the National Institute of Mental Health reported rates of mental health conditions among adolescents in the U.S. general population of 31.9% for general anxiety disorders (38.0% for females, 26.1% for males), 17.0% for major depressive episode (25.2% for females, 9.2% for males), 8.7% for attention-deficit/hyperactivity disorder (13.0% for males, 4.2% for females), and 5.0% for posttraumatic stress disorder (PTSD; 8.0% for females, 2.3% for males) (7–10). In addition, suicide is the second leading cause of death for adolescents, behind unintentional injury, with the age-adjusted suicide rate increasing 35.2% since 2000 from 10.4% to 13.5% suicides per 100,000, which is nearly four times higher for males (22.0 per 100,000) than females (5.5 per 100,000) (11). Data from the national 2021 Youth Risk Behavior Survey, the first since the beginning of the COVID-19 pandemic, reveal that poor mental health and suicidal thoughts and behaviors are increasing for nearly all groups of youth and that female students are faring more poorly than male students (12). Given these alarming trends before and over the course of the COVID-19 pandemic, the American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry, and the Children's Hospital Association recently joined together to declare a national state of emergency in children's mental health (13).
For military-connected adolescents, these profound physical, social, and emotional changes occur against the backdrop of the military career of their parent(s). Adolescents who grow up in military families face unique stressors compared with civilian youth, such as unexpected and frequent military relocations, changes in schools and peer groups, and disruptions in family dynamics due to parental absence (14–16). For example, Chandra and colleagues (17) found a linear association between the greater number of months a parent was deployed and adolescents' number of difficulties. Research with small, nonrepresentative samples of mostly Army-connected youth has examined youth perceptions of parental deployment and found that adolescents reported changes in their academic performance as well as an awareness of the dangers associated with deployment (18). This cognitive awareness may lead to ingrained thought patterns in youth that contribute to increased risk of anxiety and depression (19–21).
Additionally, military stressors may affect adolescents indirectly through their impact on their parents' marital relationship, the quality of the parent–adolescent relationship, and parenting behaviors. Namely, the military parent's exposure to high operational tempo and combat increases the risk for negative physical and psychological health outcomes (e.g., PTSD, depression, substance use, traumatic brain injury, sleep disturbance, physical injuries) related to deployment (22–24). Parental PTSD has been linked to increased risk for family violence, poor parenting behaviors, and disengagement with children (17, 19, 25, 26), with PTSD symptoms often increasing during the postdeployment period (27). Relatedly, the postdeployment adjustment of children is characterized by increased risk for internalizing and externalizing problems (19, 28).
Nevertheless, some military-connected adolescents seem to exhibit resilience and, in fact, may flourish relative to stress experiences. In a small study of adolescents observed during a parental deployment (18), researchers found that most adolescents took on additional household responsibilities while their parent was deployed, and older adolescents also appeared to have a better understanding of the sacrifices required for their parent's military career; this ability to process stress compared with younger adolescents may mitigate detrimental aspects of stress (29). Research has also examined protective factors such as availability of social support that may moderate the association of stress on adolescents' anxiety and stress symptoms (30). Although no known studies have specifically examined the role of health behaviors such as good sleep, nutrition, and exercise in mitigating stress in military-connected adolescents, studies of military spouses have found that these behaviors may shield against the effects of stress on psychological health (31). Other studies have found that community-level supports buffered negative outcomes, such as for adolescents living in military base housing compared with adolescents not living on base (17, 29).
Importantly, a growing body of work suggests the psychological health of the civilian parent is paramount to their child's adjustment (17, 18, 32, 33). Identifying resilience factors among military-connected youth is critical in developing effective interventions, particularly for youth who have been exposed to higher levels of military stress.
Although adolescent psychosocial functioning has been a fertile subject of research for decades, most studies have been conducted with adolescents outside of military-family contexts. Furthermore, much extant research on military-connected adolescents uses administrative data only [e.g., medical records or Department of Defense (DoD) records] or uses parent reports of youth experiences, health, and well-being as a proxy for adolescent functioning rather than utilizing self-report data from adolescents themselves. This approach may not accurately gauge youths' thoughts, feelings, and behaviors, particularly among older youth who are able to spend more time outside of the home. The conflicting reports between parents and adolescents has contributed to mixed findings regarding the impact of military operational stressors on adolescents' health and well-being, with some research showing that these youth are generally more resilient than their civilian peers (34, 35), while other research has found that military-connected youth exhibit higher rates of depression (36), substance use (37), suicidality (38), difficulties with peers (39), and lower academic performance (17, 18) than their civilian peers.
After nearly two decades of sustained warfare, military and veteran families have made considerable sacrifices in service to the U.S. In response, a report from the Joining Forces Interagency Policy Committee describes the commitment of the Biden-Harris Administration to U.S. military families (40) to address a major knowledge gap by supporting the development of a large-scale, representative study designed to uncover risk and protective factors related to psychosocial outcomes of military-connected youth. This study will enable DoD to understand critical issues facing military-connected youth and their families, provide key insights into modifiable risk and protective factors to inform military programs and services aimed at military-connected youth and their families, identify knowledge gaps pertinent to understudied populations (e.g., adolescents in minority families and single-parent households), and uncover emerging and specialized needs among families to inform tailored programs. Evaluating the long-term well-being of youth in the military community supports the goals of the Joining Forces initiative to enhance military child education and military family health and well-being.
1.1 Overview of the millennium cohort study of adolescent resilience
The Millennium Cohort Study of Adolescent Resilience (SOAR) is part of the larger Millennium Cohort Program (MCP), which includes the Millennium Cohort Study (MCS) of service members and veterans and the Millennium Cohort Family Study (Family Study) of military spouses. The MCS was launched in 2001 with the enrollment of its first panel of participants drawn from a representative random sample of service members. This prospective epidemiological study was designed to evaluate the effects of military service on the long-term health and well-being of U.S. service members (41).
With over a quarter of a million participants, the MCS is now the largest and longest running prospective DoD study and is the only study to follow active duty, Reserve, and National Guard personnel from all service branches during and after their military service (42). In addition, the Family Study was established in 2011 as a complementary effort to assess the effects of military experiences on the health and well-being of the spouses and children of service members who enrolled in the MCS that same year (43, 44). Leveraging existing MCP infrastructure supports, SOAR was established in 2022 and designed by a multidisciplinary team of investigators at the Naval Health Research Center (NHRC), with survey development guided by subject matter experts across DoD and academia. SOAR uses a multi-informant design to survey MCS participants, their children aged 11–17 years, and their other parent, if applicable, on topics related to adolescent psychosocial adjustment and physical health, academic achievement, and educational or career aspirations. SOAR survey data will be linked with MCS, and when possible, with Family Study and military administrative and medical health records. Moreover, adolescent participants will be surveyed approximately every 18 months until they reach the age of 25 (emerging adulthood stage).
1.2 Purpose and aims of SOAR
The primary objective of the study is to assess the impacts and associations of military experiences on the health and well-being of military-connected adolescents. The data collected will have implications for family readiness and delivery of military family-related services and will inform existing and future training or family-focused programs, education efforts, policy development, and clinical practice to best support military adolescents throughout their parent's military service.
SOAR has three overarching research questions:
1. What are the direct associations between military experiences, such as permanent change of station (PCS) relocations, parental separations, and parental injury, and adolescents' psychosocial adjustment and physical health, academic achievement, and educational and career aspirations?
2. What are the indirect associations between military experiences, such as PCS moves, parental separations, and parental injury, and adolescents' psychosocial adjustment and physical health, academic achievement, and educational and career aspirations through their impact on parents' marital/relationship quality, parent–adolescent relationship quality, and parenting behaviors?
3. What are the most salient, modifiable risk and protective factors that may explain differences in adolescents' psychosocial development and physical health, academic achievement, and educational and career aspirations?
2 Methods and analysis
SOAR is a longitudinal, multi-informant cohort study, including self-report data from military-connected adolescents and from their parent(s). Data from SOAR surveys will be linked to various official DoD data files, including military occupational and medical data records.
2.1 Study participants
The SOAR sampling frame was drawn from MCS participants enrolled between 2001 and 2021 (see Figure 1).
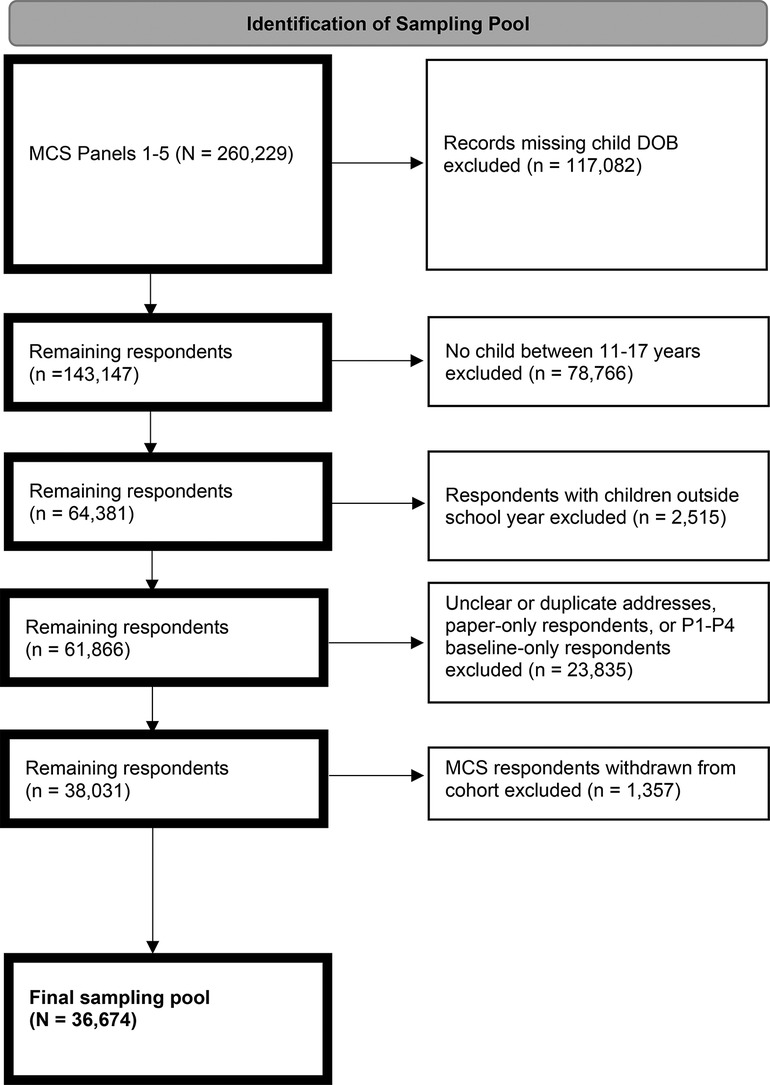
Figure 1. Flow diagram for study of adolescent resilience (SOAR) recruitment. DOB, date of birth; MCS, Millennium Cohort Study; P, panel.
Participants enrolled in MCS were recruited from a random sample of U.S. military service members on active rosters maintained by DMDC, including individuals from all service branches (i.e., Army, Marine Corps, Navy, Air Force, Space Force, and Coast Guard) and components (i.e., active duty, Reserve, and National Guard). The first panel of participants consisted of service members from a probability-based sample of the entire military population on July 1, 2001. To augment the initial panel, four additional random samples of personnel, with lengths of military service ranging from 1 to 5 years, were enrolled in 2004, 2007, 2011, and 2021, respectively. Over half of the current MCS population are no longer in active duty service. Response rates for enrollment of new panels ranged from 20% to 36%, however, investigations of potential biases in the MCS have found participants to be representative of the U.S. Armed Forces population (45). Service members and veterans enrolled in MCS with an adolescent child between the ages of 11 and 17 years during the 2022/23 academic year according to DMDC records were eligible to participate in SOAR.
Table 1 presents the sociodemographic and military characteristics of service members with adolescent children in the final SOAR study sampling pool (N = 38,031). The majority of service member participants invited to SOAR were male (75.2%), aged 25–34 years (46.9%), non-Hispanic White (69.9%), and married (81.2%). Most participants were on active duty (40.9%) and enlisted (i.e., military personnel who serve under officers; 74.4%). Further, most of the sampling frame participants were in the Army (44.7%), followed by the Air Force (30.7%), Navy (15.1%), Marine Corps (7.8%), and Coast Guard (1.9%).
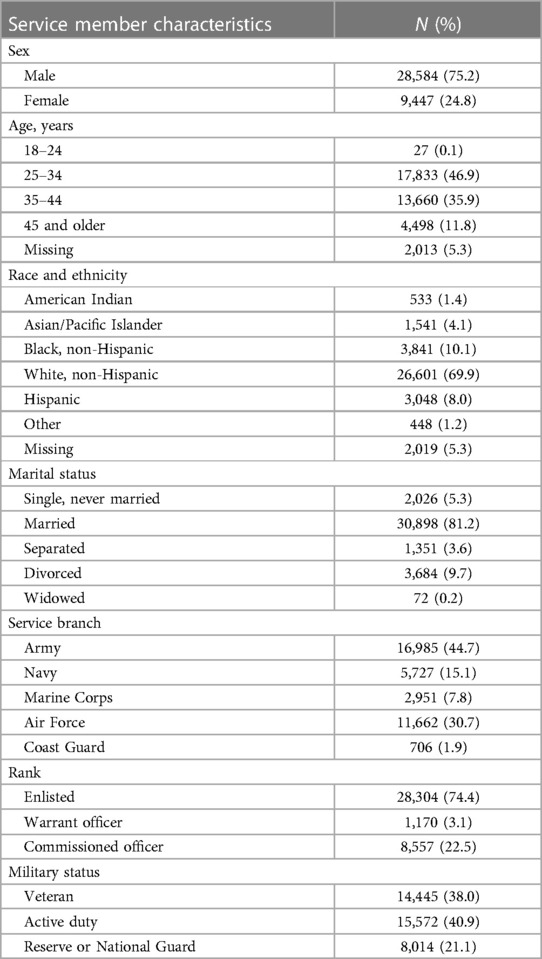
Table 1. Characteristics of service member respondents from the study of adolescent resilience (SOAR) sampling pool (N = 38,031).
2.2 Materials and equipment
MCS participants were invited to the study via email and postal mailings containing a link to the web-based survey. Once the MCS participant logged into the web survey hosted on the study website (www.millenniumcohort.com/soar), they completed consent and HIPAA forms (parent and child), and confirmed having a child aged 11–17 years. If the MCS participant indicated having more than one eligible adolescent child, one child was randomly selected via a pre-programmed algorithm as the focal child. Child questions were then answered only about this focal child. Upon completion of the survey, the MCS parent was asked to provide complete names and email addresses for the focal adolescent and the other primary parent so that they could be invited to join the study. Referred family members were each provided with a unique subject identification number and password associated with the appropriate web survey (i.e., adolescent or other primary parent) via email and postal mailings.
Given the complexity of a multi-informant design, considerable attention was paid to creating recruitment materials to enhance participation rates (Figure 2). The study name (SOAR), tag line (Rising to the Challenge), and logo (soaring eagle) were designed to evoke positive thoughts of strength and empowerment, in addition to making postal and email communication easily recognizable. The theoretical basis for designing each contact drew heavily from social exchange theory (46), as presented by Dillman et al. (47). MCS participants invited to the study were sent a postal mailing containing a tote bag and sticker with the study logo (pre-incentives), an illustrated explanation of the research highlighting the $10 Amazon gift code post-incentive for each family member, and a personalized letter from the SOAR principal investigator underscoring the importance of participation. The second postal mailing provided a sample of the survey, which highlighted questions from various sections of the adolescent and parent surveys, to legitimize the study and provide survey content without needing to log into the survey site. The third postal mailing included a postcard branded with the study logo, inspirational images, and a note from the principal investigator reiterating the benefits of participation (i.e., helping military families, monetary incentive, adolescent certificate of completion). In addition, study invitation emails were sent to parents and adolescents, and nonresponder and partial responder reminder emails were sent weekly to prompt survey completion. To encourage response from adolescents, referring parents were sent weekly emails requesting that they remind family members to complete their surveys. A “thank you” email was sent to everyone upon completion of the survey, along with a $10 Amazon gift code. Adolescents were emailed an additional $10 Amazon gift code when all referred family members completed their surveys. All correspondence provided contact information for the study team, survey login information, and the survey web address.
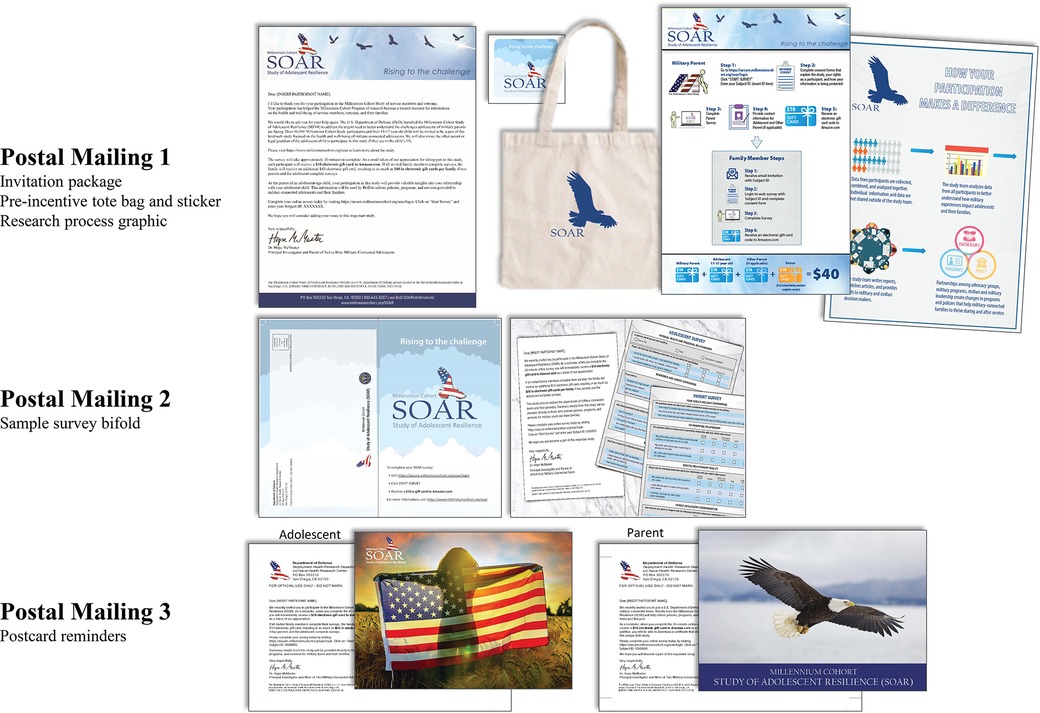
Figure 2. Study of adolescent resilience (SOAR) recruitment materials, including three separate postal mailings.
Recruitment of study participants was also facilitated by the study website, which augmented information sent in email and postal mailings. The website included details about the confidentiality of survey responses, data security, frequently asked questions, contact information, and survey approval numbers in order to alleviate any possible concerns regarding the legitimacy of the research.
2.3 Retention of participants
Between survey collections cycles, participants will be sent emails and postal mailings with study findings, press coverage, and information on how the study is being used to directly inform policies and programs for military and veteran families. These strategies have been successfully used by the MCP over the last 20 years to engage participants and to maintain current postal addresses.
2.4 Survey instruments and supplementary databases
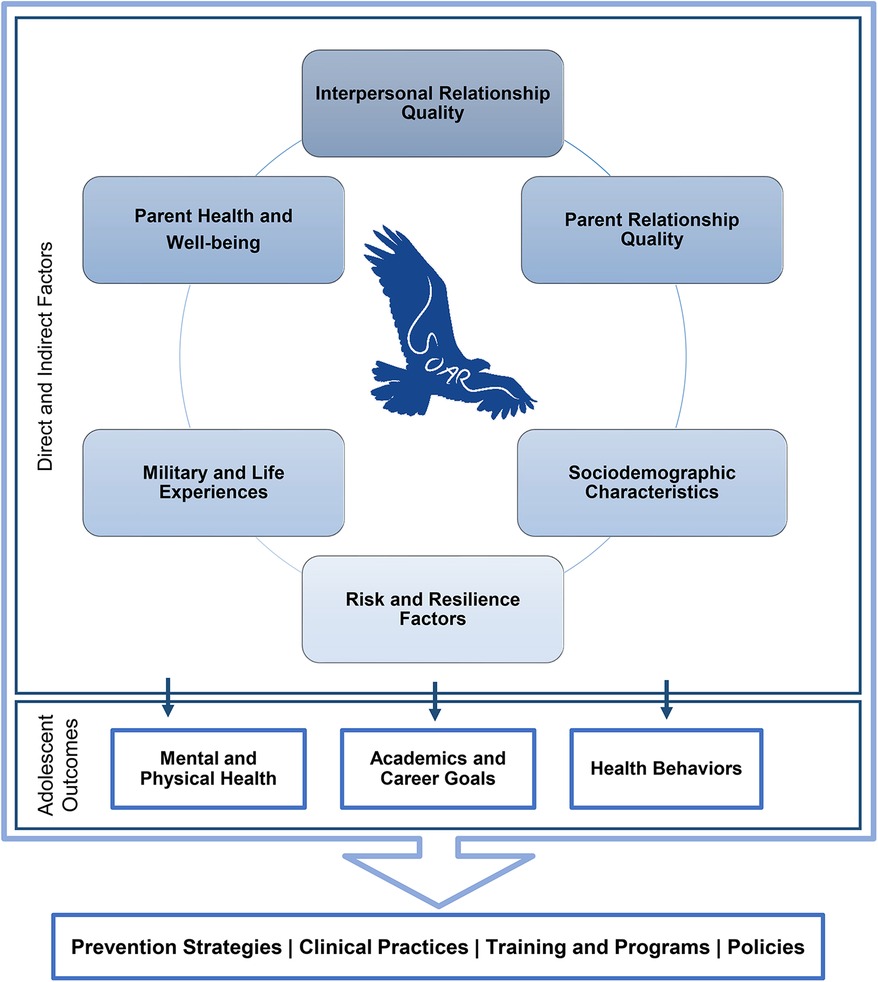
The SOAR adolescent and parent questionnaires included approximately 60 and 75 questions, respectively. Some items across both questionnaires included multiple components (i.e., item matrices, follow-up items) and skip logic. Specific questions within the survey were drawn from a conceptual model adapted from the Family Study spouse and child models (48). The SOAR model comprises six content areas theorized to link to military-connected adolescent outcomes in different capacities: (1) interpersonal relationships, (2) parent relationships, (3) parent health and well-being, (4) military and life experiences, (5) sociodemographic characteristics, and (6) risk and resilience factors (see Figure 3).
The surveys included items assessing participants' demographic characteristics and service history for military parents, and various aspects of participants' social support networks, physical and mental health, and military experiences. Adolescent and parent questionnaires were divided into eight specific domains. Each domain was composed of themes that varied depending on whether the survey was designed for an adolescent (Table 2) or for a parent.
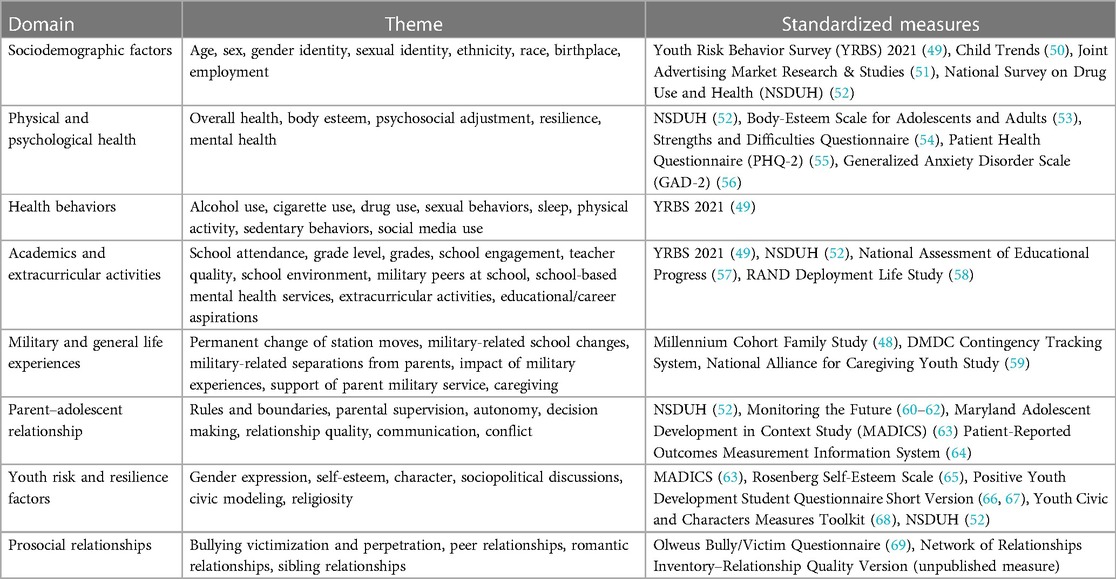
Table 2. Key domains and a selection of measures included in the study of adolescent resilience (SOAR) adolescent surveys.
Additional themes were included in the parent questionnaire (Table 3) relative to the adolescent questionnaire to reduce survey burden for adolescents and to increase the accuracy of information associated with objective questions (e.g., services used, household composition). In this way, the SOAR adolescent questionnaire was streamlined to improve usability and to conserve adolescent attentional resources.
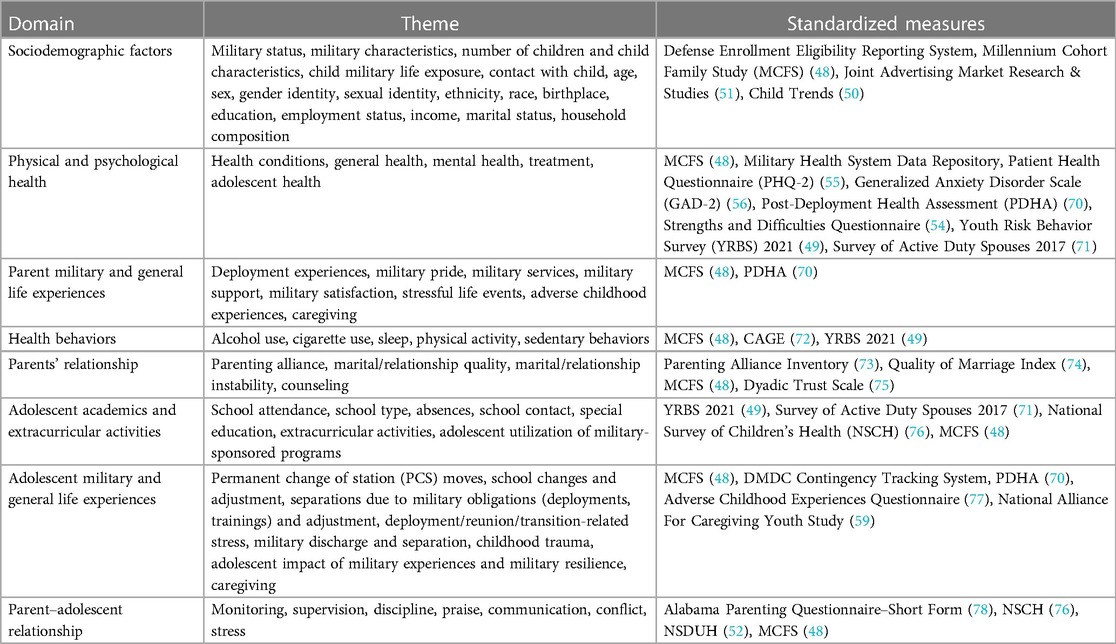
Table 3. Key domains and a selection of measures included in the study of adolescent resilience (SOAR) parent surveys.
Data on adolescent health and well-being were reported by both parents (as applicable) and by the adolescent themselves (i.e., triangulated), and they may be linked with various official DoD data files, including military and medical data records. These data include medical care services (medical diagnostic codes, vaccinations, and pharmaceutical prescriptions) provided to the service member, their spouse, and their adolescent child at military treatment facilities or through the military insurance program (TRICARE). Likewise, data on service members' deployments, occupations, injuries, environmental exposures, and other military events (e.g., disciplinary actions, promotions, and separation) can be investigated with respect to adolescent outcomes. All told, the primary data collections along with administrative data will produce a comprehensive data set to elucidate the effects of military family life on the health and psychosocial well-being of adolescents.
2.5 Analytic approach
Planned analyses involve a mix of univariate, multivariable, and multivariate statistics, including descriptive statistics to describe sample characteristics, group comparison analyses, multiple regression models, and structural equation modeling to test research questions. Multilevel (hierarchical) models will be used to estimate relationships between study constructs across levels while accounting for between, within, and bidirectional effects at the family unit level (79). Analyses will center on five primary research aims: (1) determine the unique contribution of military-specific experiences and stressors on adolescent academic and health outcomes; (2) identify the unique contribution of parental military experiences to parenting behaviors, and the impact of parental military experiences on adolescent outcomes through parenting behaviors; (3) explore group-specific differences in adolescent outcomes (i.e., unique influence of parent gender, dual-military families, other family structures); (4) determine the added effects of risk and protective factors above and beyond military exposures on adolescents' outcomes, accounting for between, within, and bidirectional effects at the family level; and (5) explore differences between adolescents who participate in vs. do not participate in military-sponsored programs (e.g., Junior Reserve Officers' Training Corps) activities. Further, data will be compared across baseline and follow-up surveys to examine changes over time in self-reported psychosocial adjustment, physical health, and academic and career outcomes. Administrative datasets will be linked with SOAR data to investigate health outcomes captured by medical records and military experiences captured by personnel data. Reports and briefings will be generated and provided to DoD stakeholders, and infographics will be posted on the SOAR and MCS websites to ensure timely dissemination of study results and to promote study engagement.
2.6 Response rates
The survey cycle remained open from November 22, 2022, to July 28, 2023, in order to facilitate answering questions related to academics and extracurricular activities that typically coincide with the school year. Figure 4 provides response rates over the survey cycle and the timing of study postal mailings.
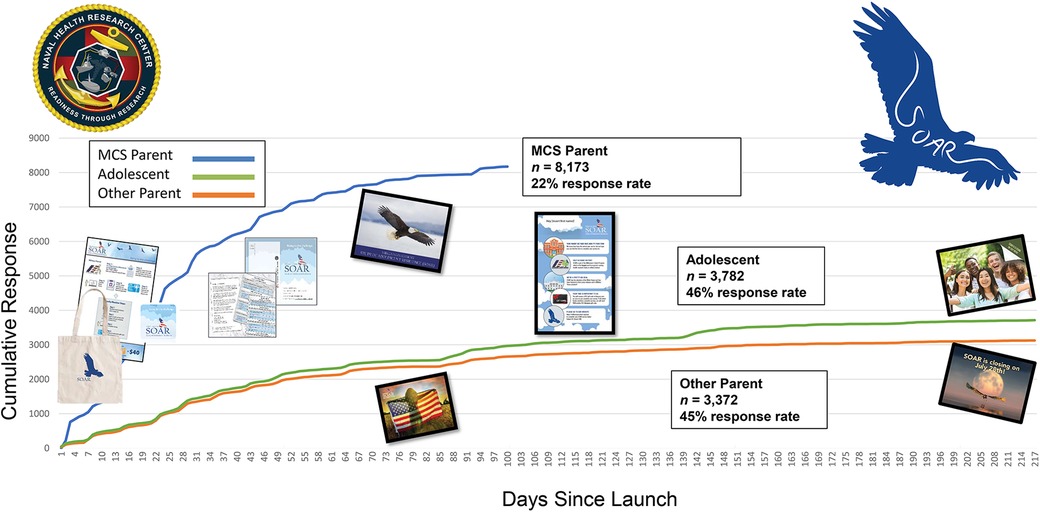
Figure 4. Study of adolescent resilience (SOAR) response rates for millennium cohort study (MCS) parent, adolescent, and other parent.
Response rates were typical of large computer-administrated surveys, with small upticks in response around pre-incentive contacts. Once approximately 8,000 military parents were recruited, all recruitment efforts were directed toward completing dyads and triads to include the military adolescent and their other parent, if applicable.
2.7 Participant characteristics
Data were collected from 14,826 participants (see Table 4 for participant characteristics). Across all participants, most identified as White and non-Hispanic. Of the 7,870 MCS parents, 69.3% identified as male, and 30.3% identified as female. Most MCS parents were cisgender (i.e., sex assigned at birth is the same as their gender identity; 98.5%), and fewer than 1% identified with a gender different from their sex assigned at birth. The majority of MCS parents identified as heterosexual (94.9%); 0.6% of MCS parents identified as gay or lesbian, 2.1% identified as bisexual, 0.4% identified with a different sexual identity, and 1.0% preferred not to answer. Most MCS parents were married at the time of their participation (80.4%). Most MCS parents were active duty (58.6%), enlisted (62.8%), and served in the U.S. Army (43.1%). In addition, 1.5% of parent participants were in dual active duty or National Guard/Reservist relationships.
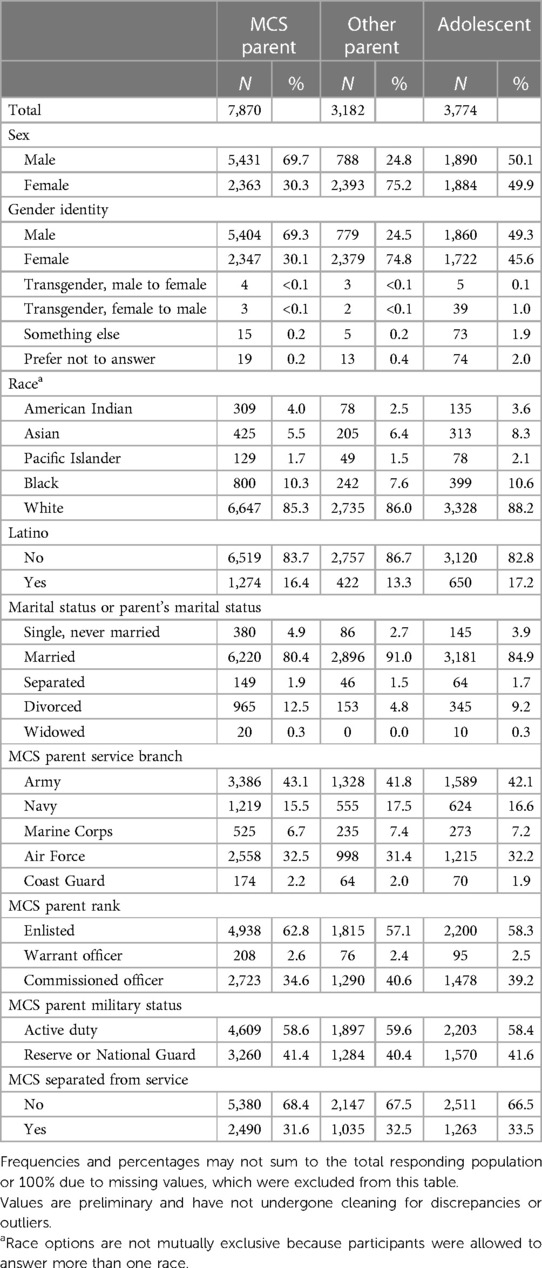
Table 4. Participant characteristics for millennium cohort study (MCS) parents, other parents, and adolescents.
About three quarters of other parents (n = 3,182) identified as female (75.2%), and 24.8% identified as male. Most other parents identified as cisgender (99.9%), and less than 1% identified with a gender different from their sex assigned at birth. The majority of other parents identified as heterosexual (94.72%), and a small proportion of other parents identified as gay or lesbian (0.5%), bisexual (2.8%), or a different sexual identity (2.8%), or indicated they preferred not to answer (1.4%). Most other parents were married at the time of study participation (91.04%). Of the 3,774 adolescents, 49.3% identified as male, 45.6% identified as female, and less than 1% identified with a gender different from their sex assigned at birth. Among adolescents, 63.34% identified as heterosexual; 22.5% identified as gay or lesbian, bisexual, a different sexual identity, or were unsure about their sexual identity; and the remaining either skipped the question or indicated that they did not understand the meaning of the question.
2.8 Anticipated impact
SOAR is the most comprehensive study of military-connected adolescents undertaken by the DoD. It is expected to provide key insights on modifiable risk and protective factors to inform military programs and services for military-connected youth and their families and to identify knowledge gaps to guide future research. SOAR's multi-informant design, combined with longitudinal follow-up of adolescents into emergent adulthood, is a powerful tool for understanding adolescent health and well-being.
3 Discussion
Adolescence is a challenging developmental period for any child, perhaps more so for those in military families. It is critical to identify the unique challenges faced by military-connected adolescents from their perspectives, and to provide them with essential supports and resources to ensure positive psychosocial health and well-being. This study is the first of its kind to address the impact of military family life on military-connected adolescents through a comprehensive data collection effort that includes longitudinal self-report data from adolescents, their parents, and administrative and medical data in concert. Research findings will improve empirical understanding of the impact of military life on adolescents and the nature of associations between military-specific experiences and psychosocial health and well-being. Further, this research will assess prominent modifiable risk and protective factors that may elucidate differences in psychosocial development and physical health, academic achievement, and educational and career aspirations.
Data from this research study will be used to address the association between parents' military exposures and their adolescent children's health and well-being. Important conditions of this association, such as the quality of parent relationships and how these relationships fluctuate over time, will reveal salient risk and protective factors that differentiate positive and negative outcomes among adolescents at different developmental stages. The capability to link SOAR survey data with prior deployment records, longitudinal MCS survey data, and parent and child medical records will provide a longer-term perspective of the impact of military risk factors on adolescent and parent current well-being. For example, medical records could be used to examine the impact of PCS moves on adolescent healthcare service utilization and DoD personnel records could be used to examine the impact of deployment frequency and length on parent-child relationships. Likewise, the inclusion of all branches, veterans, Reserve and National Guard member families, and dual-military couples in this study will allow for examination of these important yet understudied groups.
Notably, a longitudinal research approach is the only mechanism by which we can temporally assess the causal relationships between military-specific experiences and health and well-being outcomes among military-connected adolescents. This is imperative in military contexts, given the numerous transitions and acute but consistent challenges faced by military families. This approach allows for nuanced understanding of adolescent well-being across experiences like PCSs and changing schools, parent deployments and pre- and postdeployment phases, parent changes in rank or other employment factors over time, and parent injuries or separation from the military. Longitudinal data collection over a series of time points will allow for analyses measuring change over time and testing causal hypotheses and behavioral trajectories. This is particularly important during adolescence, given the vast developmental milestones that occur across time and the consequences of these changes for future adult outcomes. Ultimately, this line of research will provide a foundation for evidence-based interventions to support military-connected adolescents, thereby strengthening military families and promoting well-being and readiness among U.S. warfighters.
4 Ethics and dissemination
To ensure the welfare of study participants, regulatory approval was received from the NHRC Institutional Review Board (NHRC.2021.0018), per DoD requirements. Survey approval was received from the Office of Management and Budget (#0704-0635). Data access and data management procedures are compliant with DoD requirements for the protection and confidentiality of research participants. Findings from this study will be disseminated through national and international peer-reviewed journal publications, the Defense Technical Information Center, and academic and military conferences. Findings from this research study will be leveraged by key military family stakeholders to inform policies and programs geared toward supporting military-connected youth.
Ethics statement
The studies involving humans were approved by Naval Health Research Center Institutional Review Board (Protocol #NHRC.2021.0018). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
KT: Writing – original draft. HM: Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
This work was supported by the U.S. Navy Bureau of Medicine and Surgery under work unit no. 60002 and NHRC and MC&FP agreement no. NMR-10921.
Acknowledgments
The authors express their gratitude to members of the Millennium Cohort Program Team from the Naval Health Research Center, including Lauren Bauer, MPH; Beth Birenbaum, MPH; Sarah Carinio, BA; Mike Dorrell, BS; Alejandro Esquivel, MPH; Travis Ray, PhD; Sabrina Richardson, PhD; Rudolph Rull, PhD; Neika Sharifian, PhD; Beverly Sheppard, BS; Steven Speigle; Valerie Stander, PhD; Jennifer Walstrom; and Kelly Woodall, MPH. The authors are indebted to Dr. Jackie Pflieger for her contributions to the development of SOAR. In addition, the authors are thankful to the professionals at the Office of Military Community and Family Policy for their contributions to and continued support of SOAR. Lastly, the authors express their gratitude to SOAR participants, without whom this study would not be possible.
Conflict of interest
KT was employed by Leidos, Inc,.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
HM is an employee of the U.S. Government. This work was prepared as part of her official duties. Title 17, U.S.C. §105 provides that copyright protection under this title is not available for any work of the U.S. Government. Title 17, USC, §101 defines a U.S. Government work as work prepared by a military service member or employee of the U.S. Government as part of that person's official duties. Report No. 23-62 was supported by the U.S. Navy Bureau of Medicine and Surgery under work unit no. 60002. The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, nor the U.S. Government. The study protocol was approved by the Naval Health Research Center Institutional Review Board in compliance with all applicable federal regulations governing the protection of human subjects. Research data were derived from approved Naval Health Research Center Institutional Review Board protocol NHRC.2021.0018.
References
1. Department of Defense (DoD). 2021 Demographics profile of the military community. DoD, Office of the Deputy Assistant Secretary of Defense for Military Community and Family Policy. Available online at: https://download.militaryonesource.mil/12038/MOS/Reports/2021-demographics-report.pdf (accessed January 15, 2023).
2. Meeus W. Studies on identity development in adolescence: an overview of research and some new data. J Youth Adolesc. (1996) 25:569–98. doi: 10.1007/BF01537355
3. Steinberg L, Morris AS. Adolescent development. Annu Rev Psychol. (2001) 52(1):83–110. doi: 10.1146/annurev.psych.52.1.83
4. Laursen B, Collins WA. Parent–child communication during adolescence. In: Vangelisti AL, editors. Handbook of Family Communication. New York: Lawrence Erlbaum (2003). p. 333–48.
5. Steinberg L, Silverberg SB. The vicissitudes of autonomy in early adolescence. Child Dev. (1986) 57:841–51. doi: 10.2307/1130361
6. National Institute of Mental Health. Statistics on mental health conditions (2019). (accessed January 15, 2023).
7. National Institute of Mental Health. Statistics on anxiety disorders (2019). Available online at: https://www.nimh.nih.gov/health/statistics/any-anxiety-disorder (accessed January 15, 2023).
8. National Institute of Mental Health. Statistics on major depression. Available online at: https://www.nimh.nih.gov/health/statistics/major-depression (accessed March 30, 2023).
9. National Institute of Mental Health. Statistics on attention-deficit/hyperactivity disorder. Available online at: https://www.nimh.nih.gov/health/statistics/attention-deficit-hyperactivity-disorder-adhd (accessed March 30, 2023).
10. National Institute of Mental Health. Statistics on posttraumatic stress disorder. Available online at: https://www.nimh.nih.gov/health/statistics/post-traumatic-stress-disorder-ptsd (accessed March 30, 2023).
11. National Institute of Mental Health. Statistics on suicide. Available online at: https://www.nimh.nih.gov/health/statistics/suicide#part_2557 (accessed March 30, 2023).
12. Centers for Disease Control and Prevention. CDC report shows concerning increases in sadness and exposure to violence among teen girls and LGBQ+ youth. Available online at: https://www.cdc.gov/nchhstp/newsroom/fact-sheets/healthy-youth/sadness-and-violence-among-teen-girls-and-LGBQ-youth-factsheet.html (accessed March 30, 2023).
13. American Academy of Pediatrics. AAP-AACAP-CHA Declaration of a National Emergency in Child and Adolescent Mental Health. Available online at: https://www.aap.org/en/advocacy/child-and-adolescent-healthy-mental-development/aap-aacap-cha-declaration-of-a-national-emergency-in-child-and-adolescent-mental-health/ Last updated October 19, 2021. (accessed January 15, 2023).
14. Jelleyman T, Spencer N. Residential mobility in childhood and health outcomes: a systematic review. J Epidemiol Community Health. (2008) 62:584–92. doi: 10.1136/jech.2007.060103
15. Milburn NG, Lightfoot M. Adolescents in wartime US military families: a developmental perspective on challenges and resources. Clin Child Fam Psychol Rev. (2013) 16:266–77. doi: 10.1007/s10567-013-0144-0
16. Simpson GA, Fowler MG. Geographic mobility and children’s emotional/behavioral adjustment and school functioning. Pediatrics. (1994) 93:303–9. doi: 10.1542/peds.93.2.303
17. Chandra A, Lara-Cinisomo S, Jaycox LH, Tanielian T, Burns RM, Ruder T, et al. Children on the homefront: the experience of children from military families. Pediatrics. (2010) 125:16–25. doi: 10.1542/peds.2009-1180
18. Huebner AJ, Mancini JA. Adjustments Among Adolescents in Military Families When a Parent is Deployed. Final Report to the Military Family Research Institute and Department of Defense Quality of Life Office. Falls Church, VA: Virginia Tech, Department of Human Development (2005).
19. Lester P, Peterson K, Reeves J, Knauss L, Glover D, Mogil C, et al. The long war and parental combat deployment: effects on military children and at-home spouses. J Am Acad Child Adolesc Psychiatry. (2010) 49:310–20. doi: 10.1016/j.jaac.2010.01.003
20. Riggs SA, Riggs DS. Risk and resilience in military families experiencing deployment: the role of the family attachment network. J Fam Psychol. (2011) 25:675–87. doi: 10.1037/a0025286
21. Trickey D, Siddaway AP, Meiser-Stedman R, Serpell L, Field AP. A meta-analysis of risk factors for post-traumatic stress disorder in children and adolescents. Clin Psychol Rev. (2012) 32:122–38. doi: 10.1016/j.cpr.2011.12.001
22. Brown JM, Williams J, Bray RM, Hourani L. Postdeployment alcohol use, aggression, and post-traumatic stress disorder. Mil Med. (2012) 177:1184–90. doi: 10.7205/MILMED-D-11-00119
23. Milliken CS, Auchterlonie JL, Hoge CW. Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. JAMA. (2007) 298:2141–48. doi: 10.1001/jama.298.18.2141
24. Vasterling JJ, Proctor SP, Friedman MJ, Hoge CW, Heeren T, King LA, et al. PTSD symptom increases in Iraq-deployed soldiers: comparison with nondeployed soldiers and associations with baseline symptoms, deployment experiences, and postdeployment stress. J Trauma Stress. (2010) 23:41–51. doi: 10.1002/jts.20487
25. Gewirtz AH, Polusny MA, DeGarmo DS, Khaylis A, Erbes CR. Posttraumatic stress symptoms among national guard soldiers deployed to Iraq: associations with parenting behaviors and couple adjustment. J Consult Clin Psychol. (2010) 78:599–610. doi: 10.1037/a0020571
26. Herzog JR, Everson RB, Whitworth JD. Do secondary trauma symptoms in spouses of combat-exposed national guard soldiers mediate impacts of soldiers’ trauma exposure on their children? Child Adolesc Social Work J. (2011) 28:459–73. doi: 10.1007/s10560-011-0243-z
27. Smith BN, Shipherd JC, Schuster JL, Vogt DS, King LA, King DW. Posttraumatic stress symptomatology as a mediator of the association between military sexual trauma and post-deployment physical health in women. J Trauma Dissociation. (2011) 12:275–89. doi: 10.1080/15299732.2011.551508
28. Ruscio AM, Weathers FW, King LA, King DW. Male war-zone veterans’ perceived relationships with their children: the importance of emotional numbing. J Trauma Stress. (2002) 15:351–57. doi: 10.1023/A:1020125006371
29. Wong L, Gerras SJ. The Effects of Multiple Deployments on Army Adolescents [Monograph]. Carlisle, PA: Army War College Strategic Studies Institute (2010).
30. Cozza SJ, Chun RS, Polo JA. Military families and children during operation Iraqi freedom. Psychiatr Q. (2005) 76:371–78. doi: 10.1007/s11126-005-4973-y
31. O’Neal CW, Lucier-Greer M, Mancini JA, Ferraro AJ, Ross DB. Family relational health, psychological resources, and health behaviors: a dyadic study of military couples. Mil Med. (2016) 181:152–60. doi: 10.7205/MILMED-D-14-00740
32. Flake EM, Davis BE, Johnson PL, Middleton LS. The psychosocial effects of deployment on military children. J Dev Behav Pediatr. (2009) 30:271–8. doi: 10.1097/DBP.0b013e3181aac6e4
33. Huebner AJ, Mancini JA, Wilcox RM, Grass SR, Grass GA. Parental deployment and youth in military families: exploring uncertainty and ambiguous loss. Fam Relat. (2007) 56:112–22. doi: 10.1111/j.1741-3729.2007.00445.x
34. Cozza SJ, Lerner RM, Haskins R. Military and veteran families and children: policies and programs for health maintenance and positive development. Soc Policy Rep. (2014) 28:1–17. doi: 10.1002/j.2379-3988.2014.tb00080.x
35. Easterbrooks MA, Ginsburg K, Lerner RM. Resilience among military youth. Future Child. (2013) 23:99–120. doi: 10.1353/foc.2013.0014
36. Orthner DK, Rose R. Adjustment Among Army Children to Deployment Separations. Washington, DC: Army Research Institute for the Behavioral and Social Sciences (2005).
37. Lipari RN, Forsyth B, Bose J, Kroutil LA, Lane ME. Spouses and Children of U.S. Military Personnel: Substance Use and Mental Health Profile From the 2015 National Survey on Drug Use and Health. Rockville, MD: Substance Abuse and Mental Health Administration (2016).
38. Wickman M, Greenberg C, Boren D. The relationship of perception of invincibility, demographics, and risk behaviors in adolescents of military parents. J Pediatr Health Care. (2010) 24:25–33. doi: 10.1016/j.pedhc.2008.11.005
39. Finkel LB, Kelley ML, Ashby J. Geographic mobility, family, and maternal variables as related to the psychosocial adjustment of military children. Mil Med. (2003) 168:1019–24. doi: 10.1093/milmed/168.12.1019
40. Brosius R. Strengthening America’s military families: White House report on administration commitments to support the families of service members and veterans, their caregivers and survivors (2021). Available online at: https://www.whitehouse.gov/joiningforces/blog/2021/09/30/strengthening-americas-military-amilies-white-house-report-on-administration-commitments-to-support-the-families-of-service-members-and-veterans-their-caregivers-and-survivors/ (accessed February 05, 2023).
41. Gray GC, Chesbrough KB, Ryan MAK, Amoroso PJ, Boyko EJ, Gackstetter GD, et al. The millennium cohort study: a 21-year prospective cohort study of 140,000 military personnel. Mil Med. (2002) 167:483–88. doi: 10.1093/milmed/167.6.483
42. Belding JN, Castañeda SF, Jacobson IG, LeardMann CA, Porter B, Powell TM, et al. The millennium cohort study: the first 20 years of research dedicated to understanding the long-term health of US service members and veterans. Ann Epidemiol. (2022) 67:61–72. doi: 10.1016/j.annepidem.2021.12.002
43. Corry NH, Williams CS, Battaglia M, McMaster HS, Stander VA. Assessing and adjusting for non-response in the millennium cohort family study. BMC Med Res Methodol. (2017) 28(17):16. doi: 10.1186/s12874-017-0294-8
44. McMaster HS, LeardMann CA, Speigle S, Dillman DA. An experimental comparison of web-push vs. Paper-only survey procedures for conducting an in-depth health survey of military spouses. BMC Med Res Methodol. (2017) 17:73. doi: 10.1186/s12874-017-0337-1
45. Littman AJ, Boyko EJ, Jacobson IG, Horton J, Gackstetter GD, Smith B, et al. Assessing nonresponse bias at follow-up in a large prospective cohort of relatively young and mobile military service members. BMC Med Res Methodol. (2010) 10:1–11. doi: 10.1186/1471-2288-10-99
46. Thibaut JW, Kelley HH. The Social Psychology of Groups. New York: John Wiley & Sons, Inc. (1959).
48. Crum-Cianflone NF, Fairbank JA, Marmar CR, Schlenger W. The millennium cohort family study: a prospective evaluation of the health and well-being of military service members and their families. Int J Methods Psychiatr Res. (2014) 23:320–30. doi: 10.1002/mpr.1446
49. Centers for Disease Control and Prevention. Youth Risk Behavior Survey Questionnaire (2021). www.cdc.gov/yrbs (accessed August 26, 2020).
50. Temkin D, Belford J, McDaniel T, Stratford B, Parris D. Improving measurement of sexual orientation and gender identity among middle and high school students. Child Trends. (2017) 22:1–64. doi: 10.13140/RG.2.2.13550.20802
51. Joint Advertising Market Research & Studies. DoD Youth Poll 2019. Available online at: https://jamrs.defense.gov/Portals/20/Futures-Survey-Spring-2019_1.pdf (accessed August 26, 2020).
52. Center for Behavioral Health Statistics and Quality. 2020 National Survey on Drug Use and Health (NSDUH): Screener Specifications for Programming. Rockville, MD: Substance Abuse and Mental Health Services Administration (2019).
53. Mendelson BK, Mendelson MJ, White DR. Body-esteem scale for adolescents and adults. J Pers Assess. (2001) 76:90–106. doi: 10.1207/S15327752JPA7601_6
54. Vostanis P. Strengths and difficulties questionnaire: research and clinical applications. Curr Opin Psychiatry. (2006) 194:367–72. doi: 10.1097/01.yco.0000228755.72366.05
55. Kroenke K, Spitzer RL, Williams JB. The patient health questionnaire-2: validity of a two-item depression screener. Med Care. (2003) 41:1284–92. doi: 10.1097/01.MLR.0000093487.78664.3C
56. Kroenke K, Spitzer RL, Williams JB, Monahan PO, Löwe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. (2007) 146:317–25. doi: 10.7326/0003-4819-146-5-200703060-00004
57. National Center for Education Statistics. National Assessment of Educational Progress. Available online at: https://nces.ed.gov/nationsreportcard/ (accessed August 23, 2020).
58. Meadows SO, Tanielian TL, Karney BR. The Deployment Life Study: Longitudinal Analysis of Military Families Across the Deployment Cycle. Santa Monica, CA: RAND Corporation (2016).
59. Whiting CG, Heinz PA, Prudencio G, Wittke MR, Reinhard S, Feinberg LF, Skufca L, Stephen R, Choula R. Caregiving in the U.S. 2020. The National Alliance for Caregiving. Available online at: https://www.caregiving.org/wp-content/uploads/2021/01/full-report-caregiving-in-the-united-states-01-21.pdf (accessed November 08, 2022).
60. Johnston LD, Miech RA, O’Malley PM, Bachman JG, Schulenberg JE, Patrick ME. Monitoring the future National Survey Results on Drug Use 1975–2018: Overview, Key Findings on Adolescent Drug Use. Ann Arbor: Institute for Social Research, University of Michigan (2019).
61. Johnston LD, Miech RA, O’Malley PM, Bachman JG, Schulenberg JE, Patrick ME. Monitoring the Future National Survey Results on Drug Use 1975–2019: Overview, Key Findings on Adolescent Drug Use. Ann Arbor: Institute for Social Research, University of Michigan (2020).
62. Johnston LD, Miech RA, O’Malley PM, Bachman JG, Schulenberg JE, Patrick ME. Monitoring the Future National Survey Results on Drug Use 1975–2020: Overview, Key Findings on Adolescent Drug Use. Ann Arbor: Institute for Social Research, University of Michigan (2021).
63. MADICS: Questionnaires. Gender & Achievement Research Program (n.d.). http://garp.education.uci.edu/madics---questionnaires.html (accessed September 15, 2021).
64. Bevans KB, Riley AW, Landgraf JM, Carle AC, Teneralli RE, Fiese BH, et al. Children’s family experiences: development of the PROMIS® pediatric family relationships measures. Qual Life Res. (2017) 26:3011–23. doi: 10.1007/s11136-017-1629-y
65. Rosenberg M. Society and the Adolescent Self-Image. Princeton, NJ: Princeton University Press (1965).
66. Lerner RM, Phelps E, Lerner JV. Positive Youth Development Student Questionnaire Short Version, 2008. Available online at: https://cyfar.org/sites/default/files/Positive%20youth%20development%20student%20short%20(10%20yrs%20and%20older)_0.pdf (Accessed August 26, 2020).
67. Lerner RM, Lerner JV, Almerigi J, Theokas C, Phelps E, Gestsdottir S, et al. Positive youth development, participation in community youth development programs, and community contributions of fifth grade adolescents: findings from the first wave of the 4-H study of positive youth development. J Early Adolesc. (2005) 25:17–71. doi: 10.1177/0272431604272461
68. Syvertsen AK, Wray-Lake L, Metzger A. Youth Civic and Character Measures Toolkit. Minneapolis, MN: Search Institute (2015).
69. Olweus D. The Revised Olweus Bully/Victim Questionnaire. Mimeo, Bergen, Norway: Research Center for Health Promotion (HEMIL Center), University of Bergen (1996).
70. Denning LA, Meisnere M, Warner KE, editors. Preventing Psychological Disorders in Service Members and Their Families: An Assessment of Programs. Washington, DC: National Academies Press (2014).
71. Office of People Analytics (OPA). 2017 Survey of Active duty Spouses: Tabulations of Responses. Alexandria, VA: OPA (2018). Available online at: https://apps.dtic.mil/sti/trecms/pdf/AD1081212.pdf (Accessed March 30, 2023).
72. Ewing JA. Detecting alcoholism: the CAGE questionnaire. JAMA. (1984) 252(14):1905–7. doi: 10.1001/jama.252.14.1905
73. Abidin RR, Brunner JF. Development of a parenting alliance inventory. J Clin Child Psychol. (1995) 24:31–40. doi: 10.1207/s15374424jccp2401_4
74. Norton R. Measuring marital quality: a critical look at the dependent variable. J Marriage Fam. (1983) 1:141–51. doi: 10.2307/351302
75. Larzelere RE, Huston TL. The dyadic trust scale: toward understanding interpersonal trust in close relationships. J Marriage Fam. (1980) 1:595–604. doi: 10.2307/351903
76. Child and Adolescent Health Measurement Initiative. National Survey of Children’s Health 2019. Data Resource Center for Child and Adolescent Health. www.childhealthdata.org (Accessed September 27, 2021).
77. Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the adverse childhood experiences (ACE) study. Am J Prev Med. (1998) 14:245–58. doi: 10.1016/S0749-3797(98)00017-8
78. Elgar FJ, Waschbusch DA, Dadds MR, Sigvaldason N. Development and validation of a short form of the Alabama parenting questionnaire. J Child Fam Stud. (2007) 16:243–59. doi: 10.1007/s10826-006-9082-5
Keywords: military, youth, adolescents, psychosocial adjustment, cohort, health
Citation: Tannenbaum K and McMaster HS (2024) The Study of Adolescent Resilience (SOAR): a research protocol. Front. Child Adolesc. Psychiatry 3:1346726. doi: 10.3389/frcha.2024.1346726
Received: 8 December 2023; Accepted: 19 February 2024;
Published: 19 March 2024.
Edited by:
Niclas Schaper, University of Paderborn, GermanyReviewed by:
Jonathan M. Platt, The University of Iowa, United StatesTatiana Matheus Pinto, Mackenzie Presbyterian University, Brazil
© 2024 Tannenbaum and McMaster. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Karen Tannenbaum a2FyZW4udGFubmVuYmF1bS5jdHJAaGVhbHRoLm1pbA==
Abbreviations DoD, department of defense; HIPAA, health insurance portability and accountability act; MCP, millennium cohort program; MCS, millennium cohort study; NHRC, naval health research center; PCS, permanent change of station; PTSD, posttraumatic stress disorder; SOAR, study of adolescent resilience.
 Karen Tannenbaum
Karen Tannenbaum Hope Seib McMaster
Hope Seib McMaster