- 1Department of Child and Adolescent Psychiatry, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, London, United Kingdom
- 2Centre for the Developing Brain, School of Biomedical Engineering & Imaging Sciences, King’s College London, London, United Kingdom
- 3Department of Psychological Medicine, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, London, United Kingdom
- 4Department of Neuroimaging, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, London, United Kingdom
Introduction: The COVID-19 pandemic has caused a global mental health crisis, especially for those individuals who are vulnerable to stress and anxiety due to pre-existing mental health problems. This study aimed to understand the emotional impact of the COVID-19 lockdown on children who were born very preterm (VPT, <32 weeks' gestation), as they are vulnerable to mental health difficulties and are at increased risk of developing psychiatric problems during childhood compared to their full-term-born counterparts.
Methods: The parents of 32 VPT children (mean age = 8.7) and 29 term-born controls (mean age = 8.8), who had previously taken part in a study of brain development and psychopathology following VPT birth, completed an online modified version of the Coronavirus Health and Impact Survey (CRISIS). The emotional impact of the COVID-19 lockdown on the child and the parent, measured by the CRISIS, was studied in relation to pre-existing mental health, assessed with the parent-rated Strengths and Difficulties Questionnaire (SDQ), evaluated before the CRISIS completion (mean time gap 15 months). Linear regression model comparisons were conducted to study the effects of COVID-19-related stressors on children's and parents' behavior, relationships and mental health.
Results: There were no significant group differences in pre-existing SDQ internalizing/externalizing symptoms, child's emotions or parent's emotions during the COVID-19 lockdown. However, higher pre-existing internalizing symptoms in VPT children were associated with greater lockdown-related emotional problems and worries (simple slope = 1.95, p < 0.001), whereas this was not observed in term-born children.
Conclusion: Our results suggest that VPT children with pre-existing internalizing problems may be more vulnerable to the negative impact of certain societal and familial stressors, such as social restrictions during the national COVID-19 lockdown periods. Further rigorous studies are therefore needed to assess the severity of increased risks for this particularly vulnerable group in the context of potentially stressful life changes and adjustments.
1. Introduction
Restrictions to daily life during the COVID-19 pandemic had profound effects on children's well-being, friendships and mental abilities. Closure and reduction of access to academic settings and routine medical care resulted in decreased social support to children and young people, with likely adverse consequences for their mental health (1–3). In addition, the COVID-19 pandemic was associated with socioeconomic challenges for some families, due to increasing financial pressure, income decline and job loss (4, 5). Taken together, such factors contributed to changes in family dynamics during these uncertain times, in some instances exacerbating psychological stress for all family members (6).
Whilst it is now established that the COVID-19 pandemic has caused a global secondary mental health crisis (7, 8), this appears to be especially true for those individuals who are vulnerable to stress and anxiety due to pre-existing mental health conditions (9, 10). In uncertain times and when facing stressful events, such individuals may be particularly worried about what is happening, become socially isolated and, at the extreme end, experience mental health problems (11, 12).
Here we studied the emotional impact of the COVID-19 lockdown on children who were born very preterm (VPT, <32 weeks’ gestation) as they are vulnerable to stress and anxiety (13). Furthermore, VPT children have also been found to show a more than twofold incidence of anxiety symptoms in the clinical range compared to their full-term born peers (14, 15), to experience increased emotional and behavioral symptoms in young adult life (16) and to be at increased risk of receiving a diagnosis of attention-deficit/hyperactivity disorder (ADHD) (17). VPT children also have a doubled risk of developing clinically significant anxiety compared to full-term-born children (18).
Given the pre-existing vulnerability of VPT children to mental health difficulties, we investigated the effects of COVID-19-related stressors on children's and parents' behavior, relationships and mental health. We hypothesized that VPT children would be more negatively impacted than their term-born peers by lockdown-related stressors and that their pre-existing mental health would be associated with COVID-19 related emotional problems. Understanding the impact of COVID-19 on VPT children will help us understand what type of mental health support is needed, now and in the future.
2. Methods
2.1. Participants
This longitudinal study recruited parents of very preterm and full-term children who had taken part in the Brain, Immunity and Psychopathology following very Preterm birth (BIPP) study. The BIPP study is currently ongoing, inviting consenting participants who previously took part in the “Evaluation of MR imaging to predict neurodevelopmental impairment in the preterm infant” study [ePrime; EudraCT 2009-011602-42 (19)] to complete a follow-up assessment between the ages of 8 and 10 years. Eligible participants were those who had previously taken part in a behavioral follow-up assessment at the age of 4–7 (20, 21). Infants recruited into ePrime had the following inclusion criteria: birth before 33 weeks of gestation, maternal age above 16 years, and mothers not being hospital inpatients. Exclusion criteria were major congenital malformations, contraindications to magnetic resonance imaging, parents not being able to speak English, or being subject to child protection proceedings. 511 very preterm infants delivered at 14 hospitals in the North and South-West London Perinatal Network were recruited at birth between April 2010 and July 2013 (19).
Full-term (FT) born controls matched for sex and age are also currently being studied as part of the BIPP study. Controls were recruited via three strategies: asking parents of preterm children to invite a child of the same sex and similar in age within the same academic year to participate in the study, through recruitment letters to local schools and via internal advertisements to college staff and students. Inclusion criteria are full-term birth (38–42 weeks) and birth weight >2,500 grams, the exclusion criteria are a history of neurological conditions (meningitis, head injury and cerebral infections) and contraindication for MRI. The BIPP study aims to recruit 240 VPT and 120 term-born participants by August 2024.
The parents of 134 BIPP participants (83 VPT children and 51 FT) who had already been assessed in person between October 2018 and July 2021 were contacted via email in September 2021 and asked to complete an online modified version of the Coronavirus Health and Impact Survey (CRISIS) (22). The current study included 32 questionnaires completed by a parent of a VPT child and 29 questionnaires completed by a parent of a term-born child (Figure 1).

Figure 1. Flow chart of participants inclusion. For the follow-up at 4–7 years of age, a convenience sample (N = 251) was recruited corresponding to 82% of 306 participants who were past their fourth birthday by the follow-up study end date (September 1st, 2019), and had consented to be contacted for future research.
2.2. Assessments
2.2.1. Coronavirus Health and Impact Survey (CRISIS)
The Online Surveys platform (https://www.onlinesurveys.ac.uk) was used to obtain participants' informed consent and complete the CRISIS. The survey was completed by one of the child's legal guardians (97% birth mothers, 3% birth fathers). All the other assessments had already been collected in person as part of the BIPP study prior to the CRISIS completion between October 2018 and July 2021.
The CRISIS was created to assess the mental health impact of the COVID-19 pandemic, covering key domains relevant to mental distress and resilience (22). All three versions (for adults, parents/caregivers and youth) cover six domains, including COVID-19 exposure, COVID-19-related emotions/worries, life changes, mood states, substance use and daily behaviors. Our online survey used the parent/caregiver form to assess the impact of COVID-19 on children, and the adult self-report form to assess its impact on the responding parent (V1.0, http://www.crisissurvey.org/download/). Questions were rephrased to reflect the time during the UK's government-imposed COVID-19 lockdown period, rather than focusing only on the past two weeks, as in the original version. The varying degrees of national restrictions in the United Kingdom ranged from forced “stay at home measures” to eased “2m rules” and “Rule of six”.
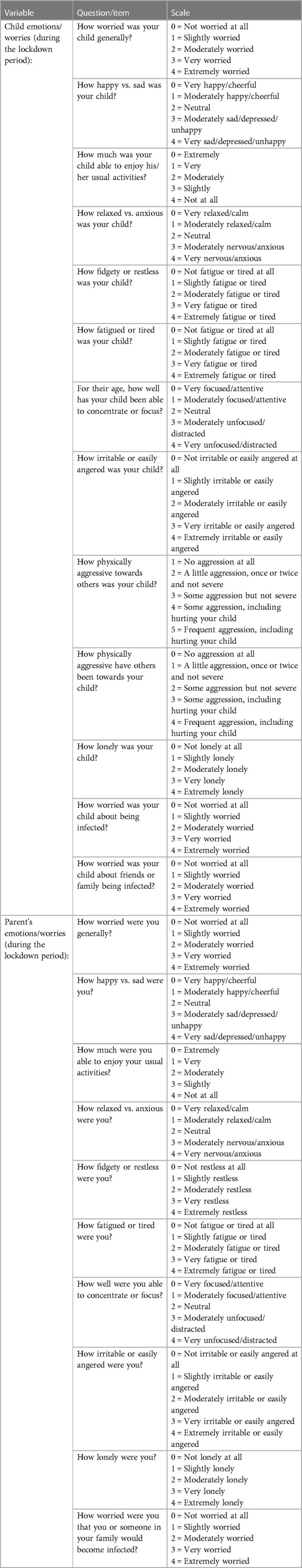
For this study, we focused only on items in the “Emotions/Worries” sections pertaining to either the child or the parent (see Table 1 and Appendix). Responses to 13 items in the Emotions/Worries section of the parent/caregiver form were coded as 0 to 4 and the sum of scores was calculated to derive a continuous “child emotions” variable. The same coding was used for 10 questions in the “Emotions/Worries” section of the adult self-report form, and the sum of scores was calculated as a continuous variable to reflect parent emotions. Internal reliability of both the child and parent emotions subscales were found to be acceptable in our sample, with Cronbach's alpha for the child emotions subscale of 0.828, 95% CI: [0.747, 0.880]; and for the parent emotions subscale of 0.735, 95% CI: [0.622, 0.804].
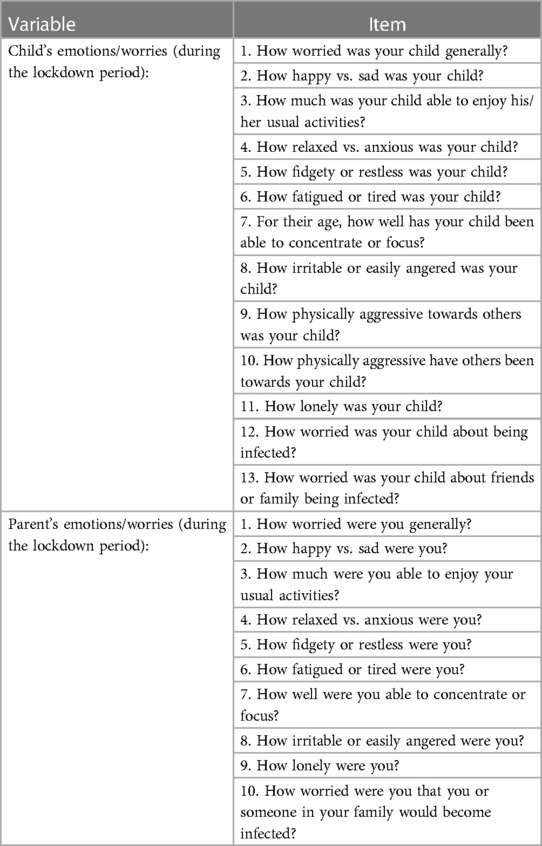
Table 1. Adapted CRISIS questions for each item included in the primary outcome variables (child's emotions and parent's emotions).
2.2.2. Strengths and difficulties questionnaire (SDQ)
Parents had previously completed the Strengths and Difficulties Questionnaire (SDQ) (23, 24) as part of the BIPP study. The SDQ is a 25-item questionnaire to assess behavioral and emotional symptoms used to evaluate mental health concerns in children and young people aged 4–17. The SDQ comprises five sub-scales of five items each: emotional symptoms; conduct problems, hyperactivity/inattention, peer relationship problems and prosocial behavior. For this study, the “Emotional Symptoms” and “Peer relationship” subscales were combined into an internalizing subscale, while the “Conduct problems” and “Hyperactivity/inattention” subscales were combined into an externalizing subscale (24).
Internalizing and externalizing subscales were considered to reflect pre-existing mental health in the children. However, given the between-participant variation in the amount of time elapsing between completion of the SDQ and the CRISIS, a time gap variable was calculated as the number of days between the SDQ assessments and CRISIS survey completion, which was used in all further analyses as a covariate of interest.
2.2.3. Wechsler intelligence scale for children, fourth edition (WISC-IV)
The Wechsler Intelligence Scale for Children, Fourth Edition (WISC-IV) (25) was also administered as part of the BIPP study. Full-scale intelligence quotient (IQ) scores were derived as a measure of children's cognitive abilities.
2.3. Statistical analysis
Statistical analyses were performed in R-4.2.1 and RStudio-1.4.1717. Independent samples t-tests were used to probe differences between the VPT and the full-term (FT) groups on continuous variables of interest. Separate linear regression models were run to test for the effects of pre-existing internalizing symptoms (or externalizing symptoms, respectively) and group (VPT vs. FT) on children's emotions during the lockdown. These regression models controlled for sex, age, time interval (between SDQ and CRISIS assessments), and parent's emotions during the lockdown.
Each model was compared to a further model including the interaction between internalizing (or externalizing, respectively) and group using likelihood ratio F-tests, to determine whether the association between pre-existing mental health symptoms and children's emotions differed between groups. In the case of a significant interaction, simple slope analyses were conducted to quantify the effect. Due to group differences in IQ, we also reran these regression analyses after inclusion of IQ as an additional covariate of no interest in all models.
3. Results
3.1. Sample characteristics
Table 2 presents the characteristics of the study sample. There were more boys than girls in the VPT group and more girls than boys in the control group, but there was no group difference in age, internalizing, or externalizing symptoms. FT children had significantly higher IQ than VPT children. There were no significant differences between participants included in this study and the overall BIPP sample at time of study in terms of SDQ internalizing symptoms, externalizing symptoms, age, or sex distribution, all ps > .05.
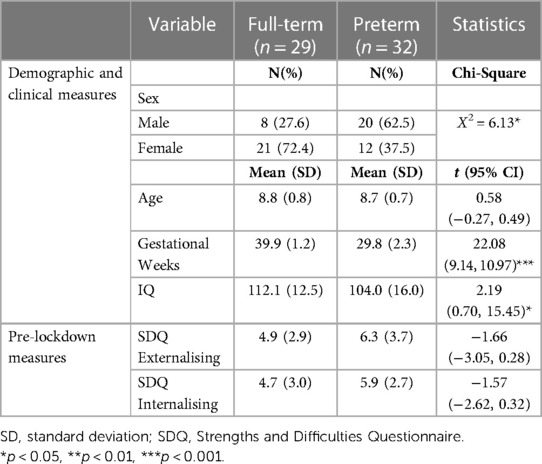
Table 2. Demographic, clinical, cognitive and pre-lockdown mental health characteristics of the study participants.
3.2. COVID-19 related child and parent emotions
In order to explore differences between groups in COVID-19 related child and parent emotions (indexed by the CRISIS), univariate linear regressions were conducted with group, sex, age and time gap as predictors. There was no difference in COVID-19 related child emotions between the VPT (M = 16.97, SD = 9.16) and control (M = 15.66, SD = 5.84) groups, B = 0.77 [−3.71, 5.25], p = 0.73; and no difference in parent emotions between the VPT (M = 19.75, SD = 6.48) and control (M = 19.13, SD = 6.17) groups, B = −0.10 [−184, 3.63, 3.41], p = 0.95, after accounting for the aforementioned confounders.
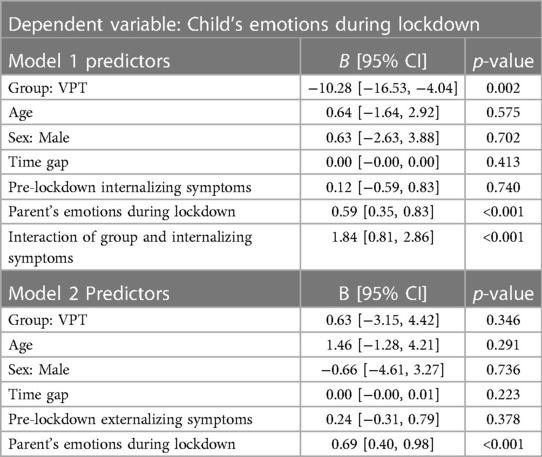
3.3. Pre-existing internalizing and externalizing symptoms and COVID-19 related child emotions
A model comparison via likelihood ratio F-test demonstrated that the model predicting child emotions during the lockdown from pre-existing internalizing symptoms (and adjusting for age, sex, time gap, and parent's emotions) was significantly improved by the inclusion of an interaction between group and pre-existing internalizing symptoms (F = 13.09, p < 0.001). The results of this model are shown in Table 3 (Model 1) and Figure 2A. A simple slope analysis revealed that, while in FT children there was no significant association between pre-existing internalizing symptoms and lockdown-related emotional problems (simple slope = 0.12, p = 0.74), VPT children showed a significant positive association between the two (simple slope = 1.95, p < 0.001), suggesting that higher pre-existing internalizing symptoms were associated with greater emotional problems and worries during the COVID-19 lockdown. Interestingly, after including these effects of pre-existing internalizing symptoms and their interaction with group, the main effect of group on COVID-19 related child emotions also became significant, indicating increased emotional problems in VPT compared to FT children (see Table 3) when taking internalizing problems into account. Inclusion of IQ in both the simple and interaction model did not alter the results of the model comparison (F = 12.89, p < 0.001).
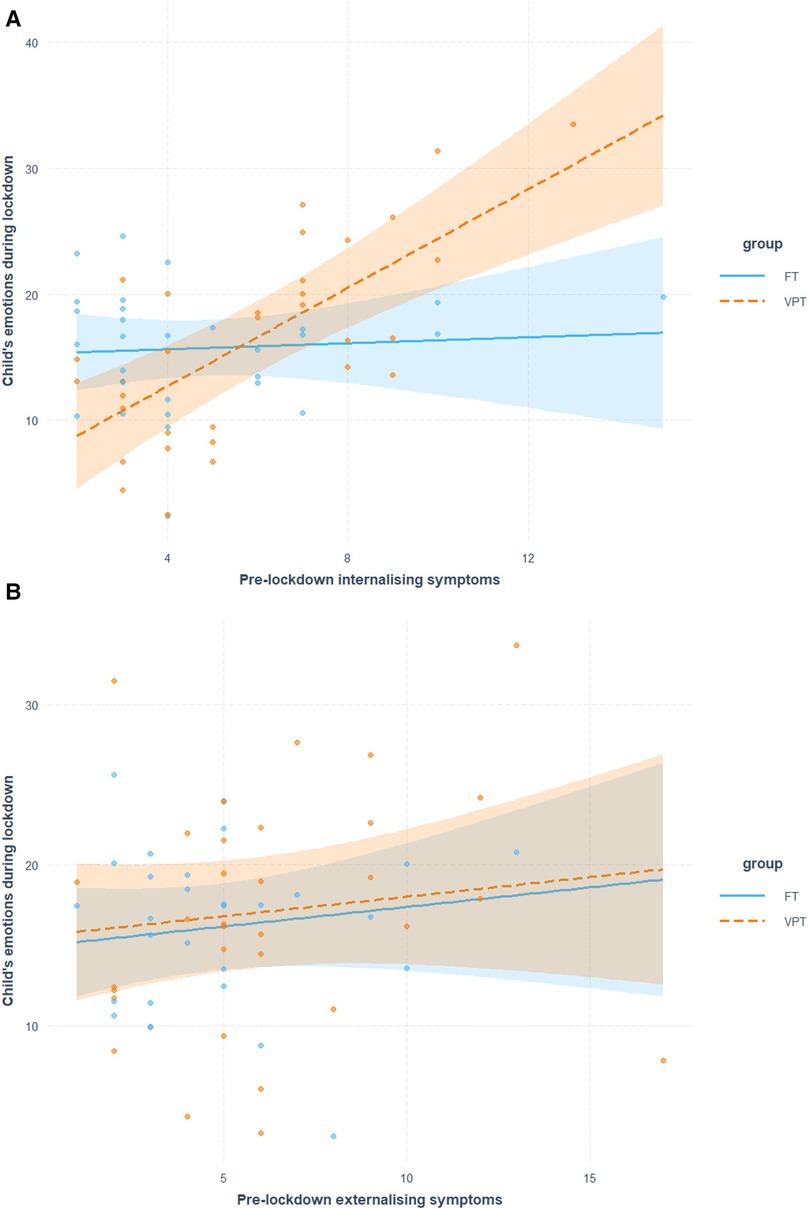
Figure 2. Scatter linear regression plot describing associations between pre-existing internalizing (A) and externalizing (B) symptoms and emotions during lockdown in VPT and FT children.
Another model comparison using the likelihood ratio F-test demonstrated that the fully adjusted model (age, sex, time gap, and parent emotions) predicting child emotions during the lockdown from pre-existing externalizing symptoms was not significantly improved by the inclusion of interaction between group and pre-existing externalizing symptoms (F = 17.97, p = 0.53). The results of this model are shown in Table 3 (Model 2) and Figure 2B. Results suggest that there was no association between externalizing symptoms and emotional problems and worries during the COVID-19 lockdown in either VPT or FT children. Inclusion of IQ in both the simple and interaction model did not alter the results of the model comparison (F = 0.24, p = 0.63).
4. Discussion
Results of this study indicate that the emotional impact of the COVID-19 lockdown did not differ between VPT children and their term-born peers as a whole; they also show comparable effects of lockdown-related stressors on emotions and worries of the parents of VPT and full-term children. However, results of this study indicate that specifically among VPT children, higher pre-existing internalizing symptoms were associated with more COVID-19 related emotional problems and concerns during the lockdown. Importantly, these findings controlled for key demographic variables as well as the parents' own lockdown-related emotions and worries. The latter was indeed found to be significantly associated with children's emotions, which likely reflects both shared familial effects of the lockdown on parent and child, as well as potential rater bias given that all scales were completed by the parent.
Our findings are in line with a recent longitudinal study which showed that preterm birth and pre-existing mental health problems were associated with a greater risk for emotional and attention-deficit/hyperactivity disorder symptoms during lockdown (26). Another study comparing the impact of the COVID-19 lockdown on three groups of children found that the lockdown had a substantial influence on the entire family and added stress to families with children who were at risk for neurodevelopmental deficits (6). Evidence from two British cohorts also suggested that children with autism and their parents, who had experienced more pre-pandemic mental health symptoms, were more likely to have more pandemic-related mental health symptoms (27).
In terms of the association between pre-existing psychiatric risk and the emotional impact of national lockdowns, findings to date have been inconsistent. A recent study indicated that the emotional impact of COVID-19 was not exacerbated in children with early brain injury or low IQ (28); another study showed a detrimental impact of lockdowns on mental well-being only in young people without pre-existing depressive symptoms (29). However, other studies found that the lockdown had severely increased pre-existing stress and depression (30, 31), suggesting there is substantial heterogeneity in COVID-19 related emotional impact across different populations (2, 9, 10, 32, 33). Our findings suggest that preterm children with pre-existing psychopathology represent a particularly vulnerable group in this context.
This study has several limitations. Firstly, the CRISIS questionnaire was administered only once and probed parents' and children's emotion during the course of COVID-19 lockdown, thus preventing a detailed evaluation of the timing and trajectories of lockdown effects on mental health. Some studies have in fact described gradually increasing symptom severity at the beginning of lockdown, which decreased after the lockdown ended (34, 35), while others suggested that the most severe mental health symptoms occurred in the early stages of lockdown, but declined fairly rapidly afterwards (36). Secondly, our sample size is relatively small for both groups, and findings therefore may not be generalizable to all VPT and term children; however, the studied sample did not significantly differ from the overall sample in terms of key characteristics such as age, sex, and psychopathology (37). Our study is also limited by the non-random sampling method for term-born peers, although this approach may ensure greater similarity between control and preterm participants (38). Thirdly, all assessments relied on parent-report, which could have led to measurement bias, although we included parents' emotional problems as a confounding variable in our analyses to control for this. Finally, as our findings relate to a UK-based sample, their generalizability to other countries may be limited, given substantial differences in relevant variables such as healthcare or severity of nationally imposed COVID-related restrictions.
5. Conclusion
This study demonstrates that internalizing problems were associated with greater susceptibility to a negative emotional impact of the COVID-19 lockdown in VPT, but not term-born children. Our results suggest that VPT children with pre-existing internalizing problems may be more vulnerable to the negative impact of certain societal and familial stressors, such as social restrictions during the national COVID-19 lockdown periods. Further rigorous work is required to assess the severity of increased risks for this particularly vulnerable group in the context of potentially stressful life changes and adjustments.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
This study was conducted in accordance with the ethical standards of the 1964 Helsinki Declaration. The study was approved by the King's College London Ethics Committee (REC: LRS/DP-20/21-21931); ePrime by the Hammersmith and Queen Charlotte's Research Ethics Committee (REC: 09/H0707/98); BIPP by the South East Research Ethics Committee (REC: 19/LO/1940) and the Stanmore Research Ethics Committee (REC: 18/LO/0048). Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
ZS, LH, CN, and LV made substantial contributions to the conception or design of the work as well as the acquisition, analysis, or interpretation of data for the work. All authors contributed to drafting the work or revising it critically for important intellectual content as well as the final approval of the version to be published. ZS, CN, and LV agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Medical Research Council (UK) (grant nos MR/S026460/1; MR/K006355/1; MR/L011530/1). The research was supported by the National Institute for Health Research (NIHR) Biomedical Research Centre based at Guy's and St Thomas’ NHS Foundation Trust and King's College London, by the NIHR Clinical Research Facility (CRF) at Guy's and St Thomas', and by the MRC Centre for Neurodevelopmental Disorders. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Acknowledgments
The authors would like to thank all the participants and their families who were involved in the project.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Meherali S, Punjani N, Louie-Poon S, Abdul Rahim K, Das JK, Salam RA, et al. Mental health of children and adolescents amidst COVID-19 and past pandemics: a rapid systematic review. Int J Environ Res Public Health. (2021) 18.
2. Panchal U, Salazar De Pablo G, Franco M, Moreno C, Parellada M, Arango C, et al. The impact of COVID-19 lockdown on child and adolescent mental health: systematic review. Eur Child Adolesc Psychiatry. (2021). doi: 10.1007/s00787-021-01856-w
3. Singh S, Roy D, Sinha K, Parveen S, Sharma G, Joshi G. Impact of COVID-19 and lockdown on mental health of children and adolescents: a narrative review with recommendations. Psychiatry Res. (2020) 293:113429. doi: 10.1016/j.psychres.2020.113429
4. Fegert JM, Vitiello B, Plener PL, Clemens V. Challenges and burden of the coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: a narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc Psychiatry Ment Health. (2020) 14:20. doi: 10.1186/s13034-020-00329-3
5. Newlove-Delgado T, Mcmanus S, Sadler K, Thandi S, Vizard T, Cartwright C, et al. Child mental health in England before and during the COVID-19 lockdown. The Lancet Psychiatry. (2021) 8:353–4. doi: 10.1016/S2215-0366(20)30570-8
6. Ehrler M, Werninger I, Schnider B, Eichelberger DA, Naef N, Disselhoff V, et al. Impact of the COVID-19 pandemic on children with and without risk for neurodevelopmental impairments. Acta Paediatr. (2021) 110:1281–8. doi: 10.1111/apa.15775
7. O'connor RC, Wetherall K, Cleare S, Mcclelland H, Melson AJ, Niedzwiedz CL, et al. Mental health and well-being during the COVID-19 pandemic: longitudinal analyses of adults in the UK COVID-19 mental health & wellbeing study. Br J Psychiatry. (2021) 218:326–33. doi: 10.1192/bjp.2020.212
8. Kola L, Kohrt BA, Hanlon C, Naslund JA, Sikander S, Balaji M, et al. COVID-19 mental health impact and responses in low-income and middle-income countries: reimagining global mental health. Lancet Psychiatry. (2021) 8:535–50. doi: 10.1016/S2215-0366(21)00025-0
9. Stinson EA, Sullivan RM, Peteet BJ, Tapert SF, Baker FC, Breslin FJ, et al. Longitudinal impact of childhood adversity on early adolescent mental health during the COVID-19 pandemic in the ABCD study cohort: does race or ethnicity moderate findings? Biol Psychiatry Glob Open Sci. (2021) 1:324–35. doi: 10.1016/j.bpsgos.2021.08.007
10. Viner R, Russell S, Saulle R, Croker H, Stansfield C, Packer J, et al. School closures during social lockdown and mental health, health behaviors, and well-being among children and adolescents during the first COVID-19 wave: a systematic review. JAMA Pediatr. (2022) 176:400–9. doi: 10.1001/jamapediatrics.2021.5840
11. Griffiths S, Allison C, Kenny R, Holt R, Smith P, Baron-Cohen S. The vulnerability experiences quotient (VEQ): a study of vulnerability, mental health and life satisfaction in autistic adults. Autism Res. (2019) 12:1516–28. doi: 10.1002/aur.2162
12. Garcini LM, Pena JM, Galvan T, Fagundes CP, Malcarne V, Klonoff EA. Mental disorders among undocumented Mexican immigrants in high-risk neighborhoods: prevalence, comorbidity, and vulnerabilities. J Consult Clin Psychol. (2017) 85:927–36. doi: 10.1037/ccp0000237
13. Brummelte S, Lieblich SE, Galea LA. Gestational and postpartum corticosterone exposure to the dam affects behavioral and endocrine outcome of the offspring in a sexually-dimorphic manner. Neuropharmacology. (2012) 62:406–18. doi: 10.1016/j.neuropharm.2011.08.017
14. Treyvaud K, Ure A, Doyle LW, Lee KJ, Rogers CE, Kidokoro H, et al. Psychiatric outcomes at age seven for very preterm children: rates and predictors. J Child Psychol Psychiatry. (2013) 54:772–9. doi: 10.1111/jcpp.12040
15. Johnson S, Hollis C, Kochhar P, Hennessy E, Wolke D, Marlow N. Psychiatric disorders in extremely preterm children: longitudinal finding at age 11 years in the EPICure study. J Am Acad Child Adolesc Psychiatry. (2010) 49(5):453–463.e1. doi: 10.1016/j.jaac.2010.02.002
16. Johnson S, O'reilly H, Ni Y, Wolke D, Marlow N. Psychiatric symptoms and disorders in extremely preterm young adults at 19 years of age and longitudinal findings from middle childhood. J Am Acad Child Adolesc Psychiatry. (2019) 58:820–826.e6. doi: 10.1016/j.jaac.2019.02.020
17. Rommel AS, James SN, Mcloughlin G, Brandeis D, Banaschewski T, Asherson P, et al. Association of preterm birth with attention-deficit/hyperactivity disorder-like and wider-ranging neurophysiological impairments of attention and inhibition. J Am Acad Child Adolesc Psychiatry. (2017) 56:40–50. doi: 10.1016/j.jaac.2016.10.006
18. Somhovd MJ, Hansen BM, Brok J, Esbjorn BH, Greisen G. Anxiety in adolescents born preterm or with very low birthweight: a meta-analysis of case-control studies. Dev Med Child Neurol. (2012) 54:988–94. doi: 10.1111/j.1469-8749.2012.04407.x
19. Edwards AD, Redshaw ME, Kennea N, Rivero-Arias O, Gonzales-Cinca N, Nongena P, et al. Effect of MRI on preterm infants and their families: a randomised trial with nested diagnostic and economic evaluation. Arch Dis Child Fetal Neonatal Ed. (2018) 103:F15–21. doi: 10.1136/archdischild-2017-313102
20. Vanes LD, Hadaya L, Kanel D, Falconer S, Ball G, Batalle D, et al. Associations between neonatal brain structure, the home environment, and childhood outcomes following very preterm birth. Biol Psychiatry Glob Open Sci. (2021) 1:146–55. doi: 10.1016/j.bpsgos.2021.05.002
21. Kanel D, Vanes LD, Pecheva D, Hadaya L, Falconer S, Counsell SJ, et al. Neonatal white matter microstructure and emotional development during the preschool years in children who were born very preterm. eNeuro. (2021) 8(5):ENEURO.0546-20.2021. doi: 10.1523/ENEURO.0546-20.2021
22. Nikolaidis A, Paksarian D, Alexander L, Derosa J, Dunn J, Nielson DM, et al. The coronavirus health and impact survey (CRISIS) reveals reproducible correlates of pandemic-related mood states across the atlantic. Sci Rep. (2021) 11:8139. doi: 10.1038/s41598-021-87270-3
23. Goodman R. The strengths and difficulties questionnaire: a research note. J Child Psychol Psychiatry. (1997) 38:581–6. doi: 10.1111/j.1469-7610.1997.tb01545.x
24. Goodman A, Lamping DL, Ploubidis GB. When to use broader internalising and externalising subscales instead of the hypothesised five subscales on the strengths and difficulties questionnaire (SDQ): data from British parents, teachers and children. J Abnorm Child Psychol. (2010) 38:1179–91. doi: 10.1007/s10802-010-9434-x
25. Wechsler D. Wechsler intelligence scale for children–(WISC-IV), 4th ed. San Antonio, TX: The Psychological Corporation (2003). 3.
26. Bailhache M, Monnier M, Moulin F, Thierry X, Vandentorren S, Cote SM, et al. Emotional and attention-deficit/hyperactivity disorder symptoms of preterm vs. Full-term children during COVID-19 pandemic restrictions. Pediatr Res. (2022) 92:1749–56. doi: 10.1038/s41390-022-02037-4
27. Palmer M, Chandler S, Leno VC, Mgaieth F, Yorke I, Hollocks M, et al. Factors associated with mental health symptoms among UK autistic children and young people and their parents during the COVID-19 pandemic. Res Sq Platform LLC. (2022). doi: 10.21203/rs.3.rs-1993442/v1
28. Williams TS, Deotto A, Roberts SD, Ford MK, Desire N, Cunningham S. COVID-19 mental health impact among children with early brain injury and associated conditions. Child Neuropsychol. (2022) 28:627–48. doi: 10.1080/09297049.2021.1998407
29. Joensen A, Danielsen S, Andersen PK, Groot J, Strandberg-Larsen K. The impact of the initial and second national COVID-19 lockdowns on mental health in young people with and without pre-existing depressive symptoms. J Psychiatr Res. (2022) 149:233–42. doi: 10.1016/j.jpsychires.2022.03.001
30. Buneviciene I, Bunevicius R, Bagdonas S, Bunevicius A. The impact of pre-existing conditions and perceived health status on mental health during the COVID-19 pandemic. J Public Health (Oxf). (2022) 44:e88–95. doi: 10.1093/pubmed/fdab248
31. Palit S, Yang H, Li J, Khan MAS, Hasan MJ. The impact of the COVID-19 pandemic on the mental health of rohingya refugees with pre-existing health problems in Bangladesh. Confl Health. (2022) 16:10. doi: 10.1186/s13031-022-00443-3
32. Ma L, Mazidi M, Li K, Li Y, Chen S, Kirwan R, et al. Prevalence of mental health problems among children and adolescents during the COVID-19 pandemic: a systematic review and meta-analysis. J Affect Disord. (2021) 293:78–89. doi: 10.1016/j.jad.2021.06.021
33. Lovato I, Vanes LD, Sacchi C, Simonelli A, Hadaya L, Kanel D, et al. Early childhood temperamental trajectories following very preterm birth and their association with parenting style. Children (Basel). (2022) 9(4):508. doi: 10.3390/children9040508.35455552
34. Castellini G, Rossi E, Cassioli E, Sanfilippo G, Innocenti M, Gironi V, et al. A longitudinal observation of general psychopathology before the COVID-19 outbreak and during lockdown in Italy. J Psychosom Res. (2021) 141:110328. doi: 10.1016/j.jpsychores.2020.110328
35. Caldiroli A, Capuzzi E, Tringali A, Tagliabue I, Turco M, Fortunato A, et al. The psychopathological impact of the SARS-CoV-2 epidemic on subjects suffering from different mental disorders: an observational retrospective study. Psychiatry Res. (2022) 307:114334. doi: 10.1016/j.psychres.2021.114334
36. Fancourt D, Steptoe A, Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatry. (2021) 8:141–9. doi: 10.1016/S2215-0366(20)30482-X
37. Leoni M, Vanes LD, Hadaya L, Kanel D, Dazzan P, Simonoff E, et al. Exploring cognitive, behavioral and autistic trait network topology in very preterm and term-born children. Front Psychol. (2023) 14:1119196. doi: 10.3389/fpsyg.2023.1119196
38. Marlow N, Wolke D, Bracewell MA, Samara M, Group EPS. Neurologic and developmental disability at six years of age after extremely preterm birth. N Engl J Med. (2005) 352:9–19. doi: 10.1056/NEJMoa041367
Keywords: COVID-19, child mental health, very preterm, internalizing symptoms, lockdown, crisis
Citation: Sun Z, Hadaya L, Leoni M, Dazzan P, Simonoff E, Counsell SJ, Edwards AD, Nosarti C and Vanes L (2023) Comparing the emotional impact of the UK COVID-19 lockdown in very preterm and full-term born children: a longitudinal study. Front. Child Adolesc. Psychiatry 2:1193258. doi: 10.3389/frcha.2023.1193258
Received: 24 March 2023; Accepted: 15 May 2023;
Published: 13 June 2023.
Edited by:
Maria Melchior, Institut National de la Santé et de la Recherche Médicale (INSERM), FranceReviewed by:
Marion Bailhache, Université de Bordeaux, FranceRoma Jusiene, Vilnius University, Lithuania
Sigita Lesinskiene, Vilnius University, Lithuania
© 2023 Sun, Hadaya, Leoni, Dazzan, Simonoff, Counsell, Edwards, Nosarti and Vanes. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lucy Vanes bHVjeS52YW5lc0BrY2wuYWMudWs=
 Zeyuan Sun
Zeyuan Sun Laila Hadaya
Laila Hadaya Marguerite Leoni
Marguerite Leoni Paola Dazzan
Paola Dazzan Emily Simonoff
Emily Simonoff Serena J. Counsell
Serena J. Counsell A. David Edwards
A. David Edwards Chiara Nosarti
Chiara Nosarti Lucy Vanes
Lucy Vanes