- 1Cardiff Business School, Cardiff University, Cardiff, United Kingdom
- 2Screening Unit, Azienda Zero, Padua, Italy
- 3Department of Economics and Management “Marco Fanno”, University of Padova, Padua, Italy
- 4Department of Economics (DEMS), University of Milano-Bicocca, Milan, Italy
- 5Hygiene and Public Health Unit, Azienda ULSS 6 Euganea, Este, Italy
Objectives: We study the introduction of a web portal allowing women to manage their appointments in the public cervical cancer screening program of an Italian Local Health Unit (LHU). We investigate how this intervention affects program participation and the ability of the LHU to collect information on women's screening outside the program.
Methods: We use administrative data from the LHU and a difference-in-differences design to compare outcomes of women in the treated group (n=870), who could reschedule appointments either through phone calls or through the portal, and the control group (n=768), who could only reschedule by phone.
Results: The portal reduces the number of appointments rescheduled by phone (b = −0.176, 95% CI = −0.228 to −0.114, p < 0.001). It also makes women more likely to report both screenings outside the program (b = 0.049, 95% CI = 0.006–0.912, p < 0.05) and the various reasons for canceling their appointments. However, the portal also decreases the probability of screening (b = −0.156, 95% CI = −0.216–0.096, p < 0.001). Two-thirds of this reduction is due to increased unjustified no-shows (b = 0.099, 95% CI = 0.043–0.155, p < 0.001).
Conclusions: Digital innovations increase efficiency of screening programs. However, they may discourage screening, by triggering behavioral biases such as limited attention and procrastination. Pairing portals with frequent reminders may help to boost participation.
1 Introduction
The digital world is becoming a crucial pillar of the effective functioning of societies (Hodson, 2018). For example, the rise of information and communication technologies (ICT henceforth) allows governments to provide a variety of digital services which can enhance the efficiency and the accountability of public institutions, facilitate information transmission between administrative offices and citizens, and results in substantial economic benefits for the public sector and citizens alike (Faulkner et al., 2019).
The digital transformation of services and the introduction of information and communication technologies (ICT) have interested the healthcare sector as well, considerably influencing healthcare provision and health systems in general (Ricciardi et al., 2019). A growing body of scientific literature tries to assess the impact of ICT innovations on the effectiveness, accessibility, and resilience of the healthcare systems (e.g., Agarwal et al., 2010; Marques and Ferreira, 2020; Kraus et al., 2021).
We report quasi-experimental evidence from a North-Eastern Italian local health unit (LHU) that introduced a user-friendly web portal allowing women enrolled in the national cervical cancer screening program to autonomously modify (either reschedule or cancel) their pre-assigned screening appointments. We employ administrative data from the LHU and a difference-in-differences design to compare the changes in several screening outcomes across the current and the previous invitation rounds for women in the control group—who had no access to the portal and could reschedule the appointment only through a phone call to the LHU—and in the treated group—who could reschedule their appointment either by phone or through the portal.
Aimed at testing the general, intuitive hypothesis that, by reducing the impact of frictions and other behavioral limitations, ICT innovations can significantly foster virtuous health behaviors, we assess the effects of the introduction of the web portal on three distinct outcomes. First, we study whether the web portal was effectively used by women to reschedule appointments. This is not a trivial question, given that the uptake of digital services is rather low, and governments struggle to make citizens use these services (Castelo et al., 2015). For example, according to Eurostat, only 55% of the EU population used online interfaces for interacting with the public authorities in 2019.
Second, we investigate whether the introduction of the web portal affects participation in the screening program. Providing women with an alternative digital solution to reschedule the date of the screening slot represents a nudge that can weaken the behavioral obstacles to cancer screening (Benartzi et al., 2017). For example, phone-averse women (LaRose, 1999; Rettie, 2007) who would like to reschedule the pre-specified screening slot may be reluctant to call the phone service of the LHU and, therefore, may eventually postpone the screening opportunity, with negative effects for cancer prevention and higher costs for the healthcare system (Berliner et al., 2020; Hallsworth et al., 2015). Nonetheless, if given the opportunity to reschedule the appointments online, phone averse women may benefit from this chance and attend the screening. While there is evidence that digital medical appointment systems can foster participation in the cervical cancer screening (Gallegos et al., 2023; Schliemann et al., 2022), the empirical literature on the effects of ICT on healthcare is still at its infancy, especially when focusing on proactive web interfaces that require the intervention of the patient to reschedule appointments.
Third, by using data on the reasons why women cancel their appointments, we assess whether the introduction of the portal increases the ability of the LHU to collect information on women's screening behavior outside the public screening program. In fact, the web portal asks women who do not intend to participate in the program to inform the LHU about the main reason for that. One option that women can select is to have already done a test outside the public screening program. In the portal, emphasis was posed on communicating to the women that reporting information about previous exams can help the health authorities to correctly schedule their future screening appointments.
Our paper contributes to the growing literature on digitalization in healthcare by leveraging a quasi-experiment to provide evidence of the impact of an online, proactive system made available to patients to reschedule appointments for cancer screenings.
A limited number of studies investigates the impact of proactive web services on healthcare utilization and health outcomes. In this respect, Bavafa et al. (2018) estimate the impact of e-visit usage on the frequency of office and phone visits as well as on patient health outcomes. The authors use panel data from a large healthcare system in the United States and achieve identification of the effect of e-visit use on later outcomes by conditioning on both patient and provider fixed effects, thereby leveraging only the observed variation in the timing of e-visits' use within patients and providers. To account for possible time-varying confounders, the authors utilize a matching approach and instrument patients' utilization of e-visits using the pre-determined variation across providers in the timing and intensity of e-visit adoption. The authors find that making use of e-visits increases the number of physical visits to the physicians, reduces the number of new patients accepted by the physicians, and has mixed results on phone visits and patient health.
Zhong et al. (2018) investigate the effects of utilization of a web portal in primary care in Florida on office visits, no-show, and cancellation to primary care physicians. The authors conduct a retrospective observational study employing a difference-in-differences approach. By comparing trends between users and non-users, the authors document a reduction in the portal users' office visits and no shows, with these effects materializing only >1 year after the introduction of the portal. Bao et al. (2020) use a similar design to examine the association between web portal utilization and health outcomes by exploiting a panel dataset of congestive heart failure patients in North Texas. Results indicate that portal use is associated with lower frequency of hospital and emergency visits, lower readmission risk, and lower length of stay.
A crucial difference between these studies and our contribution is that the former generally compare program participation and health outcomes of users and non-users in setups where the proactive system is already in place for everyone to use it and exploit the observed variation in the probability of using the portal. Therefore, a causal interpretation of the results is limited by the endogeneity in the effective utilization of the proactive system, that makes it difficult to properly address the self-selection of users. For instance, portal use may depend on individual expectations about future health and healthcare needs, generating reverse causality. In this respect, the key contribution of our study is to exploit a supply-driven quasi-experimental shock to the availability of the patient portal to study the impact of its introduction on women's screening outcomes. In our setting, the availability of the portal is exogenously manipulated, which allows us to establish a much cleaner causal relationship between the availability of a proactive web-portal and the behavior of eligible patients.
Our paper also departs from the literature analyzing the effects of ICT innovations in screening programs that give no proactive role to patients. These innovations concern platforms that are actively used by the program administrations for better management practices (e.g., Chaudhry et al., 2007; Oscarsson et al., 2008), computerized systems that send reminders to patients (e.g., Ruffin et al., 2007; DeFrank et al., 2009; Vidal et al., 2014), interactive web-pages providing information to the patients (e.g., Ruffin et al., 2007; Elkin et al., 2017). Unlike these studies, we assess the impact of a newly introduced digital technology in which women enrolled in the screening program have a proactive role and can autonomously reschedule their appointment after logging in to the web application with their credentials.
2 Methods
2.1 The institutional setting
In Italy, the implementation of public cervical screening programs has been recommended since 1996 (Cappelli et al., 2018; Ronco et al., 2015) and included in the Ministry of Health's “Essential Health Interventions” list since 2001. The management of the national cancer screening program is handled by the 20 Italian Regional health authorities following national guidelines. Regions are further organized in LHUs that cover smaller geographical areas (akin to provinces) and take care of the local implementation of the program by delivering invitations, handling appointments, and managing the screening operations within dedicated screening centers. Women are automatically linked to screening centers on the basis of their municipality of residence.
The intervention analyzed in this study was carried out by a LHU located in North-Eastern Italy. For privacy reasons, we have to anonymise all the information on the LHU. The cervical cancer screening program has been in place in this LHU since 1996, has population-level coverage and targets women aged 25–64. The actual coverage is above 80 percent, and the average screening take-up is around 65 percent once valid reasons for exclusion (recent test undertaken outside the program, pregnancy status, health conditions) are considered. Women aged 25–29 are offered to take a PAP test every 3 years while women aged 30-65 are offered to take a HPV test every 5 years.
Within the program, women receive closed-date invitations at regular intervals by regular mail. Invitations are scheduled 3 years after a missed invitation, 3 years after a PAP test, 5 years after a HPV test, and 1.5 years after a canceled invitation for pregnancy. Screening slots are allocated to women on a monthly basis, and the available time slots are randomly allocated among women eligible to screen within a given month. A text message reminds women about their appointment a few days before the scheduled date.
2.2 The invitation letters and the quasi-experimental manipulation
The intervention discussed in this study was carried out by a LHU located in North-Eastern Italy between November 2019 and January 2020. The population of women targeted by the intervention within the cervical cancer screening program was divided in two groups:
i) the “phone only” control group has access to the phone service only to manage the appointments. The web portal is not accessible to this group, and neither is this group formally aware of the existence of the web portal.
ii) the “web or phone” treatment group has access to both the phone service and the web portal. The invitation letter provides all the information needed to access and use the portal as well as the login credentials. Some information about the portal, such as the potential advantages to users in terms of flexibility and autonomy in managing their appointments, is printed on the back of the invitation letter. The invitation letters are reported in Appendix 1.
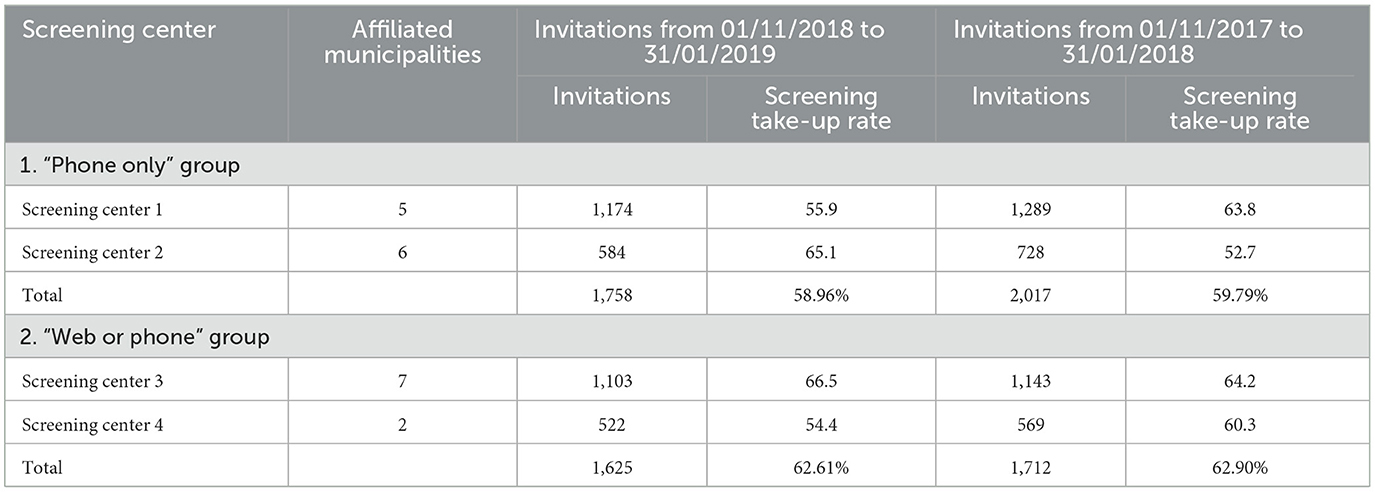
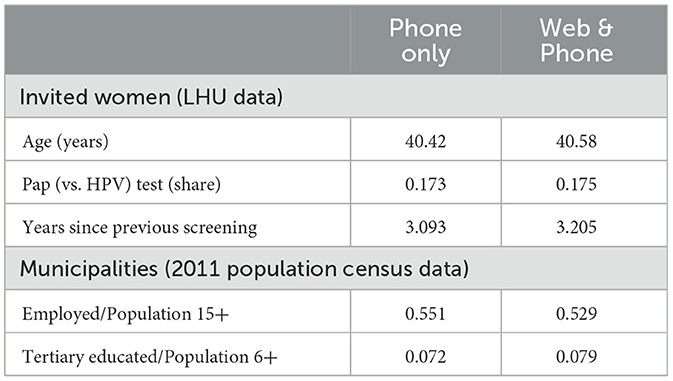
Four of the LHU's screening centers were involved in this program. Letters for each screening center are prepared and dispatched in separate batches. The solution adopted to generate variability in treatment status was to dispatch different letters to women affiliated with different screening centers (all females in a screening center received the same letter). Screening centers were allocated to different treatment groups in such a way that trends in screening take-up across the two groups for the periods November 2018–January 2019 vs. November 2017–January 2018 were comparable. The treatment received by each of the groups was then randomly assigned. The resulting allocation is depicted in Table 1, that also reports data on screening take-up during the periods mentioned above. Treatment and control groups look comparable in terms of pre-intervention average screening take-up trends, with some variability across individual centers. For instance, the share of screened patients grew faster in the control group, especially in center 2, which also had low take-up in the earliest monitored period. Table 2 reports instead some characteristics of treated and control municipalities, deriving from aggregate data obtained from the LHU and from the 2011 Italian population Census, and reports that the two resulting groups of municipalities have comparable composition.
Our study is based on a retrospective analysis of anonymized (individual) medical records and consists of a descriptive report of ordinary activities performed by our partner LHU for public health purposes. The retrospective study has been approved by the Ethical Committee “Comitato Etico Territoriale Area Centro-EST Veneto” on October 12, 2023 (5856/AZ/23). Each woman participating in the cervical cancer screening program provided a verbal consent that authorized the LHA to use her individual information for health purposes. The verbal consents were recorded and stored through an IT application specifically designed for the screening program. Moreover, in compliance with the General Data Protection Regulation (GDPR), when logging into the website of the LHA, each woman had access to an informative consent explicitly stating that her individual information could be used for monitoring and evaluating population participation in preventive medicine activities, as well as for research purposes.
2.3 Data
For each woman invited during the intervention, we collected information on the month and year of birth, the screening center of reference (and hence treatment status), the date of the screening invitation, the type of test proposed (PAP or HPV), and the outcome of the invitation. This is coded as follows:
• Screened: the invited woman participates in the program.
• No-show: the invited woman does not participate in the program and does not inform the LHU about her absence. Importantly, the screening program had to be stopped on March 1st, 2020, because of the COVID-19 pandemic, and all women who did not take part in the program or did not communicate their absence by that date are recorded as no-shows. As a result, during the current round we also monitor rescheduling for a shorter time-period than in previous rounds. Fortunately, this is not a concern empirically, as in previous rounds only 19 subjects in total rescheduled the appointment later than the end of the monitoring period during the current round. In addition, the distributions of rescheduling times in the previous and current round overlap largely.
• Canceled slot: the invited woman informs the LHU that she will not participate. Cancellation can be communicated over the phone in the control group and via the web portal or over the phone in the treatment group. The appointment can be canceled for the following reasons: (i) having already undertaken a PAP or HPV test in the last 3 years in a private facility or within the public sector following a GP or gynecologist prescription; (ii) pregnancy; (iii) other health reasons; (iv) general willingness to drop-out from the screening programme without any reason. In case of cancellation, women are asked to indicate the reasons for canceling and, eventually, to provide other relevant information (such as the date of the external examination and associated gynecologist prescription). If the reason for cancellations are the recent tests carried out privately, women are also requested to report the dates of these tests so that the next invitations can be correctly scheduled.
In addition, we know whether the appointments were rescheduled or canceled and whether the rescheduling or cancellation took place via phone or the portal.
We also gained access to the screening history of women involved in the intervention. For each previous invitation, we know the invitation year, the type of the test proposed (PAP or HPV), the outcome of the invitation and whether the appointment was handled (rescheduled or canceled) by women. As described in Appendix 3, where we describe our sample selection criteria, we limit the sample to the current and up to two previous invitations for each woman.
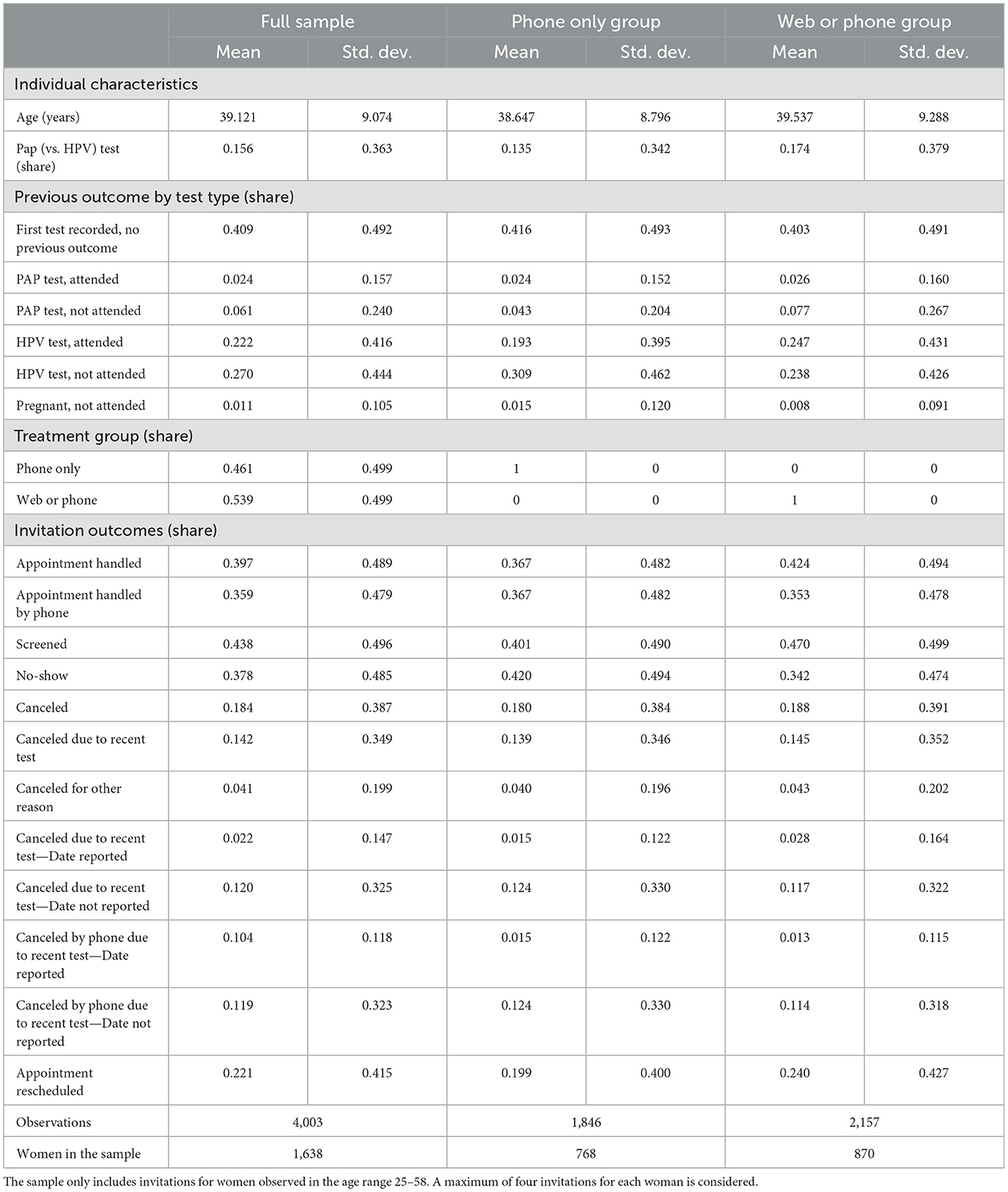
The initial sample consists of 5,642 invitations for 1,659 women aged 25–65 residing in the 20 municipalities related with the four screening centers of our partner LHU. The final sample is composed of 4,003 invitations for 1,638 women. In total, 1,005 women (61% of the sample) are observed 3 times, 355 (22%) are observed twice, and 278 (17%) are only observed once. Details on the sample selection procedures are reported in Appendix 3.
Table 3 reports descriptive statistics for the full final sample and by treatment group. In the full sample, average age is close to 39 years, and 15.6 percent undergo a PAP (vs. HPV) test. Table 3 also shows that close to 41 percent of observations concern first invitations observed in the data. For invitations beyond the first one, statistics about the outcome of the previous invitation is also reported in Table 3. As described in Section 2.1, this outcome determines the spacing between invitations. In terms of allocation to groups, 53.9 percent of observations belong to the treatment group and 46.1 to the control. Concerning the invitation outcomes, 39.7 percent of all appointments have been handled and roughly 90 percent of the handling took place over the phone. Close to 44 percent of appointments ended in a completed screening, 38 percent are no-shows, and 18 percent were canceled. Roughly 3 out 4 cancellations took place because of a recent test, and 1 in 4 for other reasons. Moreover, 22 percent of appointments were rescheduled. Finally, when we compare across treatment groups, we see that women in the treatment group are slightly older and less likely to undergo a PAP (vs. HPV) test on average. Average invitation outcomes also differ, but this also reflects the effect of access to the portal.
2.4 Empirical approach
We use a difference-in-differences (DiD) design. We identify treatment effects comparing the observed trends in the outcomes over invitations and across the treatment and the control groups. Identification of the effect of the web portal rests upon the assumption that, after the introduction of the portal, the treatment and the control groups would have followed the same trend in the outcomes had the web portal not been introduced. As discussed in Section 2.2, our design helps to support the validity of this assumption, as screening centers were allocated to treatment groups in such a way that the resulting average previous screening take-up trends were comparable. As shown in Table 1, this result holds on average, but there is variability across individual centers. Eventually, we will test the validity of this assumption in our final sample using data for invitations dating back to the period before the introduction of the web portal.
The identification strategy also requires that no shocks separately affect either the treatment or the control group during the intervention. The strong control over the institutional setup corroborates the validity of these assumptions. The program is implemented in a geographic area with a homogenous population, and the management of the program falls within a single LHU, that applies the same screening protocols throughout its territory.
Formally, we estimate the following model with Ordinary Least Squares (OLS):
In Equation (1), subscripts i, g and t stand for individual, treatment group and invitation, and Y is a vector of invitation outcomes. t equals 0 for the current (post-intervention) invitation, and −1 or −2 for the first- and second-to-last invitations, respectively. Postt is a dummy variable that equals 1 if t = 0 and 0 otherwise. WebOrPhoneg is a dummy variable that equals 1 for women in the treatment group and 0 otherwise. The main coefficient of interest is β, that identifies the DiD treatment effect. In addition, ϕt are invitation round fixed effects, and Xigt is a vector of invitation-specific controls that includes age at invitation dummies, a dummy for test type (PAP vs. HPV), and previous invitation test type-by-outcome dummies, that determine the spacing between invitations. To capture potential trends in screening behavior by different demographic groups, we allow the coefficients δt to vary by round. Finally, εigt is the error term. We cluster the standard errors by individual.
We test for parallel trends by estimating the following event study specification using OLS:
Equation (2) is analogous to Equation (1) but includes the parameter β−2, that identifies the lagged placebo treatment effect given by the comparison between the treatment and control groups between the t=-2 and t=-1 pre-intervention periods. Under the parallel-trends assumption, this coefficient should be equal to zero for all outcomes.
3 Results
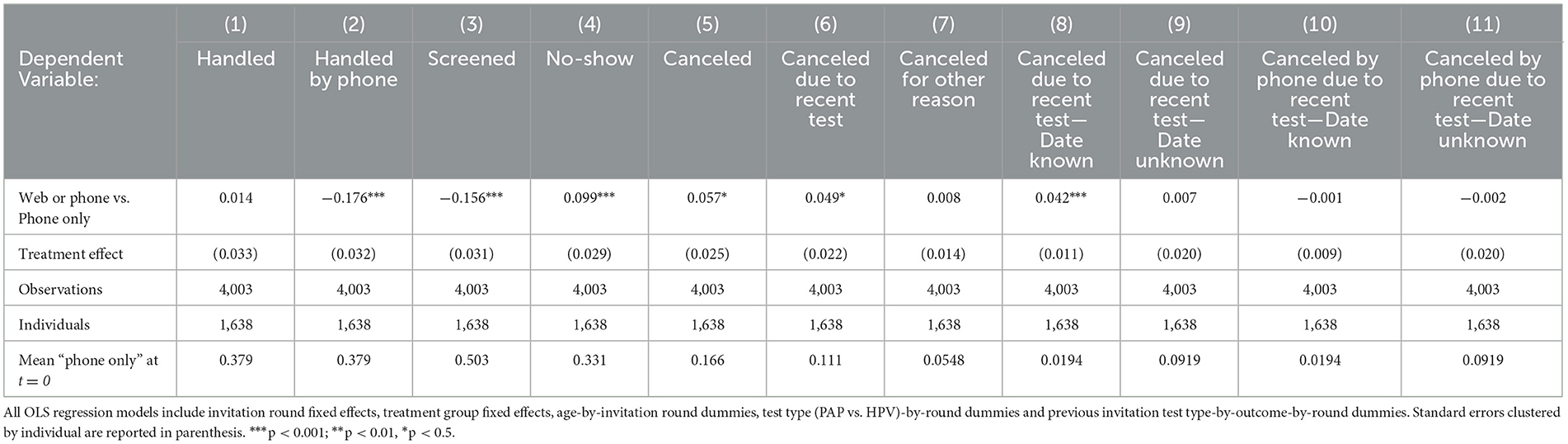
First, Column (1) of Table 4 shows that the treatment had no significant impact on the probability that an appointment was handled (canceled or rescheduled). However, Column (2) shows that the (unconditional) probability of handling the appointment by phone decreases starkly, by roughly 18 percentage points (pp) or by 50% of the control group mean, implying that eligible women who need to move or cancel their slot do take advantage of the possibility to do so online. From a descriptive perspective, women in the “web or phone” group who prefer the portal to the phone are younger on average (36 vs. 40 years old).
Second, results on the outcomes of screening appointments are reported in Columns (3) to (5) of Table 4. Access to the portal reduced screening by 16pp or roughly 30% of the control group mean. A big part of this result–around 10pp–is explained by the increased likelihood of no-shows. The remainder−6pp–is explained by the increased likelihood of appointment cancellations.
Treatment effects on cancellations deserve further investigation. To begin with, we report treatment effects on the (unconditional) probability of canceling a slot because the women had already undertaken a test over the last 3 years or because of other reasons (listed in Subsection 2.3) in Columns (6) and (7) of Table 4, respectively. The higher rate of cancellations detected for the treatment groups is because of a higher likelihood of reporting tests carried out over the previous year, and not because of other reasons. Considering that women in the treatment and control groups are comparable in terms of their screening behavior or health outcomes, this difference is likely due to changes in the probability of reporting a recent test, as this is explicitly mentioned as an option for cancellation in the web portal.
In addition, when they communicate recent tests, women are also asked to report the date of the test. Columns (8) and (9) of Table 4 illustrate that access to the portal increased the (unconditional) likelihood that women report this information by 4.4pp. Considering that the control group mean is 1.9pp, this is a very large effect in relative terms. A potential mechanism behind this finding could be the availability of more time to search for the latest appointment date if women cancel the appointments via the portal compared to canceling over the phone, with an operator waiting for inputs.
Finally, Columns (10) and (11) of Table 4 report insignificant treatment effects on the unconditional likelihood of cancellations with or without a reported date handled over the phone, confirming that the positive effect detected on overall cancellations with a reported date of recent screening is due to changes undertaken via the portal.
Importantly, the identification strategy relies on the parallel-trends assumption. We verify whether this assumption is satisfied in our final sample in Figure 1, where we report the estimates of the placebo tests and treatment effects estimated from Equation (2). The figure shows that—for all outcomes—the research design delivers parallel trends for the pre-intervention period, as the coefficients for the lagged treatment effect at time t = −2 are close to zero and insignificant.
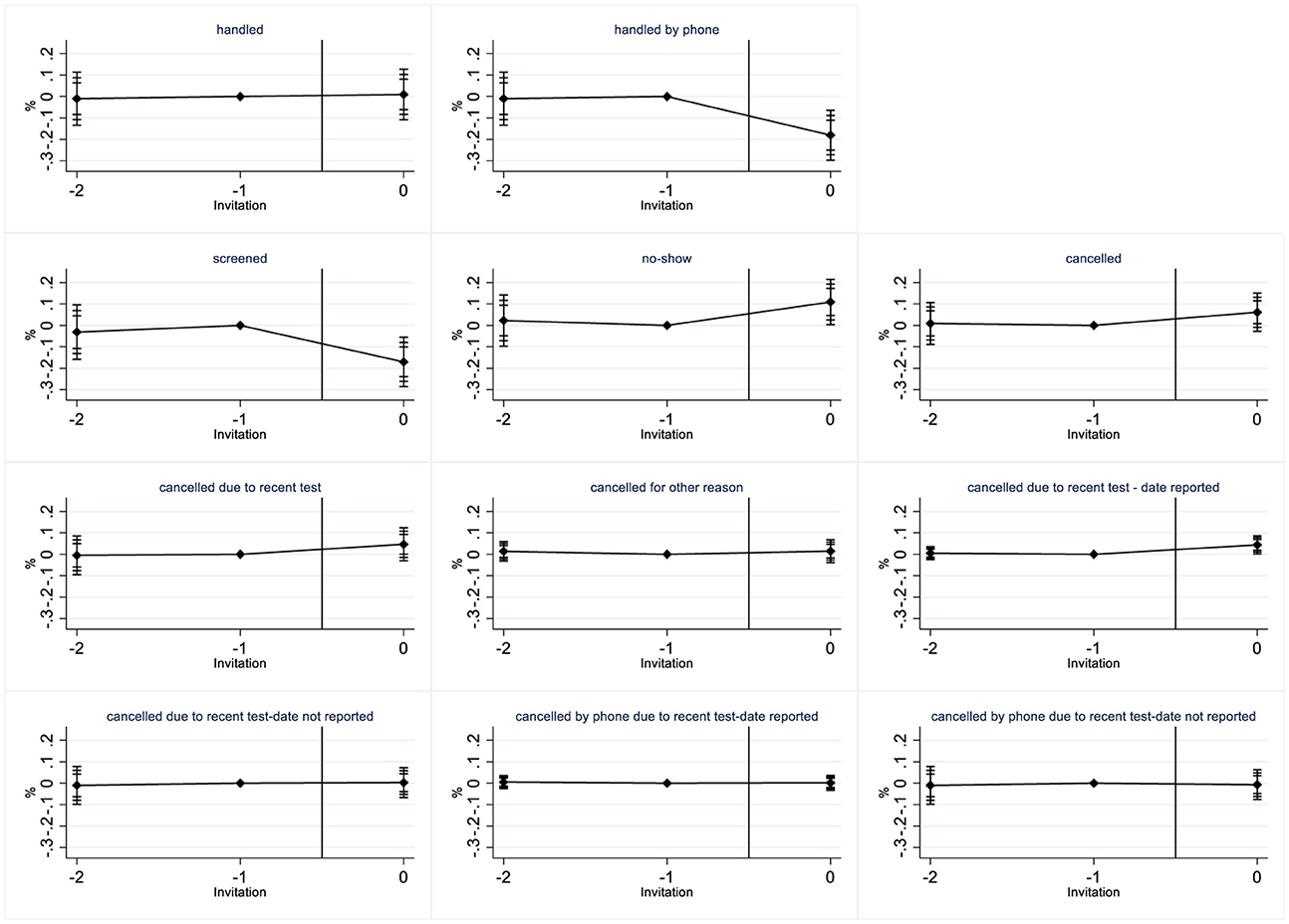
Figure 1. The effects of the web portal access on screening outcomes. The Figure reports the effects of the “web or phone” treatment vs. the “phone only” control group, as estimated from Equation 2, together with their 95, 99, and 99.9% confidence intervals.
In Table A4.1 in Appendix 4 we report the results of a battery of robustness checks. Specifically, our results are qualitatively robust to: (i) adjusting inference for multiple testing; (ii) dropping all invitation-specific controls and including only invitation round and treatment group fixed effects; (iii) introducing screening center fixed effects instead of a single “treatment group” dummy; (iv) reducing compositional imbalances over time by retaining only 1005 women for whom we observe three invitations and, in this balanced panel, including individual fixed effects; (v) dropping 365 women who changed municipality of residence across invitation rounds or who reside in three municipalities that changed screening center of affiliation across rounds; (vi) avoiding potential bias due to the onset of the pandemic by dropping 880 women invited for screening in 2020.
Lastly, in Table A4.2 in Appendix 4, we report the split-sample effects for women aged in 2019 below and above 40, the median age value in the sample. The overall pattern of effects is comparable across the two samples. This is not very surprising, considering that all women in the final sample are of working age, and thus familiar with the use of web services. Still, there are two notable differences. First, the effect on no-shows is predominantly due to younger women. Second, the effect on cancellation is mostly coming from senior women.
4 Discussion and concluding remarks
We document both positive and backfiring effects of introducing a web portal that allows eligible women to modify their screening slots. On a positive note, the portal reduces the organizational burden borne by the LHU since the number of phone calls to reschedule appointments substantially drops. The portal also increases the organizational aspects of the program, since women become more likely to report previous screenings and the reasons for canceling the appointments. This information is crucial for the correct scheduling of the invitations in the future.
On a negative note, giving access to the web portal decreases the probability of attending the screening by roughly 15pp, and around two thirds of this reduction is because of unjustified no-shows. Most likely, the portal triggers procrastination (Ariely and Wertenbroch, 2002; Rabin, 1998; Akerlof, 1991) when rescheduling appointments, and eventually these women do not screen.
In the “phone only” condition, phone-averse women (who avoid making phone calls) would most likely prefer screening on the assigned date to rescheduling their appointment via phone. Thus, the original invitation date is salient/important for these women, given the absence of alternative dates. In the “web or phone” condition, there are fewer psychological barriers to reschedule the appointment, since phone averse women can do this online. Consequently, the original invitation date loses its salience in the minds of phone averse women, as they can easily reschedule the appointment to many alternative dates through the portal. Most likely, women keep procrastinating given the possibility to reschedule online and eventually either forget about the appointment due to limited attention (Della Vigna, 2009) or cannot make it on the original date because of competing obligations even if reminded through a text message few days before. The positive relationship between portal availability and women's tendency to procrastinate is confirmed by the effect of portal availability on rescheduled appointments, that is negative and equal to−6.4pp (p-value = 0.023). Moreover, the larger treatment effect on the share of no-shows among younger women is also in line with this hypothesized mechanism, as there is evidence that procrastination is more common at young ages (Beutel et al., 2016; Gröpel and Steel, 2008). To solve the problem of procrastination, the LHU may decide to send frequent and early notifications to the invited women reminding them to reschedule the appointments. Reminders represent one of the most popular and effective interventions to steer individuals in a certain direction (Sunstein, 2014) and their positive impact is well-documented in health decisions (Antinyan et al., 2021a,b). More in general, the backfiring effect exerted by the web portal detected in our study might contrast the introduction of an ICT tool as simple nudge to more hard policies, such as the introduction of financial incentives for enhancing screening uptake (Halla et al., 2022).
Our study is not exempt from limitations. First, we can only monitor screening outcomes for the current invitation round, but it might be interesting to look at women adaptation to the presence of the portal in the long run. Second, while our administrative data have population coverage and minimize the potential for measurement error in treatment status and outcomes, they provide limited information on women's background. This may be useful for improving the heterogeneity analysis. Third, while procrastination provides a reasonable explanation for the backfiring result on participation in the screening program, other behavioral channels might be in place, including the loss of social accountability in online interactions compared to phone calls. Exploring the potential of chatbot interactions as a middle ground between impersonal online systems and human phone communication could be an interesting avenue for future research.
Data availability statement
The raw data supporting the conclusions of this article will be available from the authors upon request, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethical Committee “Comitato Etico Territoriale Area Centro-EST Veneto” on October 12, 2023 (5856/AZ/23). The studies were conducted in accordance with the local legislation and institutional requirements. The Ethics Committee/Institutional Review Board waived the requirement of written informed consent for participation from the participants or the participants' legal guardians/next of kin because the study is based on a retrospective analysis of anonymized (individual) medical records and consists of a descriptive report of ordinary activities performed by our partner LHU for public health purposes. Each woman participating in the cervical cancer screening program provided a verbal consent that authorized the LHA to use her individual information for health purposes. The verbal consents were recorded and stored through an IT application specifically designed for the screening program. Moreover, in compliance with the General Data Protection Regulation (GDPR), when logging into the website of the LHA, each woman had access to an informative consent explicitly stating that her individual information could be used for monitoring and evaluating population participation in preventive medicine activities, as well as for research purposes. Written informed consent was not obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article because the study is based on a retrospective analysis of anonymized (individual) medical records and consists of a descriptive report of ordinary activities performed by our partner LHU for public health purposes.
Author contributions
AA: Writing – original draft, Writing – review & editing. SB: Writing – original draft, Writing – review & editing. MB: Writing – original draft, Writing – review & editing. LC: Writing – original draft, Writing – review & editing. ML: Writing – original draft, Writing – review & editing. EN: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frbhe.2024.1458981/full#supplementary-material
References
Agarwal, R., Guodong, G., DesRoches, C., and Jha, A. K. (2010). The digital transformation of healthcare: current status and the road ahead. Inform. Syst. Res. 21, 796–809. doi: 10.1287/isre.1100.0327
Antinyan, A., Asatryan, Z., Dai, Z., and Wang, K. (2021a). Does the frequency of reminders matter for their effectiveness? A randomized controlled trial. J. Econ. Behav. Organ. 191, 752–764. doi: 10.1016/j.jebo.2021.09.023
Antinyan, A., Bertoni, M., and Corazzini, L. (2021b). Cervical cancer screening invitations in low- and middle-income countries: evidence from Armenia. Soc. Sci. Med. 273:113739. doi: 10.1016/j.socscimed.2021.113739
Ariely, D., and Wertenbroch, K. (2002). Procrastination, deadlines, and performance: self-control by precommitment. Psychol. Sci. 13, 219–224. doi: 10.1111/1467-9280.00441
Bao, C., Singh, H., Meyer, B., Kirksey, K., and Bardhan, I. (2020). Patient-provider engagement and its impact on health outcomes: A longitudinal study of patient portal use. MIS Quart. 44:14180. doi: 10.25300/MISQ/2020/14180
Bavafa, H., Hitt, L. M., and Terwiesch, C. (2018). The impact of e-visits on visit frequencies and patient health: Evidence from primary care. Manage. Sci. 64, 5461–5480. doi: 10.1287/mnsc.2017.2900
Benartzi, S., Beshears, J., Milkman, K. L., Sunstein, C. R., Thaler, R. H., Shankar, M., et al. (2017). Should governments invest more in nudging? Psychol. Sci. 28, 1041–1055. doi: 10.1177/0956797617702501
Berliner, S. A., Kornitzer, T., Lawrence, G., Zysman, H., Hallak, Y., Ariely, D., et al. (2020). It's how you say it: systematic A/B testing of digital messaging cut hospital no-show rates. PLoS ONE 15:e0234817. doi: 10.1371/journal.pone.0234817
Beutel, M. E., Klein, E. M., Aufenanger, S., Brähler, E., Dreier, M., Müller, K. W., et al. (2016). Procrastination, distress and life satisfaction across the age range–a German representative community study. PLoS ONE 11:e0148054. doi: 10.1371/journal.pone.0148054
Cappelli, M. G., Fortunato, F., Tafuri, S., Boccalini, S., Bonanni, P., Prato, R., et al. (2018). Cervical cancer prevention: an Italian scenario between organised screening and human papillomaviruses vaccination. Eur. J. Cancer Care. 27:e12905. doi: 10.1111/ecc.12905
Castelo, N., Hardy, E., House, J., Mazar, N., Tsai, C., and Zhao, M. (2015). Moving citizens online: using salience & message framing to motivate behavior change. Behav. Sci. Policy 1, 57–68. doi: 10.1177/237946151500100207
Chaudhry, R., Scheitel, S. M., McMurtry, E. K., Leutink, D. J., Cabanela, R. L., Naessens, J. M., et al. (2007). Web-based proactive system to improve breast cancer screening: a randomized controlled trial. Arch. Intern. Med. 167, 606–611. doi: 10.1001/archinte.167.6.606
DeFrank, J. T., Rimer, B. K., Gierisch, J. M., Bowling, J. M., Farrell, D., and Skinner, C. S. (2009). Impact of mailed and automated telephone reminders on receipt of repeat mammograms: a randomized controlled trial. Am. J. Prev. Med. 36, 459–467. doi: 10.1016/j.amepre.2009.01.032
Della Vigna, S. (2009). Psychology and economics: Evidence from the field. J. Econ. Lit. 47, 315–372. doi: 10.1257/jel.47.2.315
Elkin, E. B., Pocus, V. H., Mushlin, A. I., Cigler, T., Atoria, C. L., and Polaneczky, M. M. (2017). Facilitating informed decisions about breast cancer screening: development and evaluation of a web-based decision aid for women in their 40s. BMC Med. Inform. Decis. Mak. 17, 1–9. doi: 10.1186/s12911-017-0423-7
Faulkner, N., Jorgensen, B., and Koufariotis, G. (2019). Can behavioural interventions increase citizens' use of e-government? Evidence from a quasi-experimental trial. Gov. Inform. Q. 36, 61–68.
Gallegos, S., Roseth, B., Cuesta, A., and Sánchez, M. (2023). Increasing the take-up of public health services: An at-scale experiment on digital government. J. Public Econ. 227:104975. doi: 10.1016/j.jpubeco.2023.104975
Gröpel, P., and Steel, P. A. (2008). Mega-trial investigation of goal setting, interest enhancement, and energy on procrastination. Pers. Individ. Dif. 45, 406–411. doi: 10.1016/j.paid.2008.05.015
Halla, M., Pruckner, G. J., and Schober, T. (2022). Paying adolescents for health screenings works. Am. J. Health Econ. 8, 534–548. doi: 10.1086/721571
Hallsworth, M., Berry, D., Sanders, M., Sallis, A., King, D., Vlaev, I., et al. (2015). Stating appointment costs in SMS reminders reduces missed hospital appointments: findings from two randomised controlled trials. PLoS ONE 10:e0137306. doi: 10.1371/journal.pone.0137306
Kraus, S., Schiavone, F., Pluzhnikova, A., and Invernizzi, A. C. (2021). Digital transformation in healthcare: Analyzing the current state-of-research. J. Bus. Res. 123, 557–567. doi: 10.1016/j.jbusres.2020.10.030
LaRose, R. (1999). “Understanding personal telephone behavior,” in Progress in Communication Science Volume XV: Advances in Telecommunication Theory and Research, eds. H. Sawhney and G. Barnett (Norwood, NJ: Ablex), 1–28.
Marques, I. C., and Ferreira, J. J. (2020). Digital transformation in the area of health: systematic review of 45 years of evolution. Health Technol. 10, 575–586. doi: 10.1007/s12553-019-00402-8
Oscarsson, M. G., Wijma, B. E., and Benzein, E. G. (2008). Nonattendance in a cervical cancer screening program—what happens if women's requirements are met? Health Care Women Int. 29, 183–197. doi: 10.1080/07399330701738242
Rettie, R. (2007). Texters not talkers: phone aversion among mobile phone users. PsychNology J. 5, 33–57. Available at: https://psycnet.apa.org/record/2007-07642-002
Ricciardi, W., Pita Barros, P., Bourek, A., Brouwer, W., Kelsey, T., and Lehtonen, L. (2019). How to govern the digital transformation of health services. Eur. J. Public Health 29, 7–12. doi: 10.1093/eurpub/ckz165
Ronco, G., Giubilato, P., Carozzi, F., Maia, G., Giorgi Rossi, P., and Zappa, M. (2015). Italian cervical cancer screening survey group. (2015). Extension of organized cervical cancer screening programmes in Italy and their process indicators, 2011-2012 activity. Epidemiologia e Prevenzione 39, 61–76.
Ruffin, I. V. M. T., Fetters, M. D., and Jimbo, M. (2007). Preference-based electronic decision aid to promote colorectal cancer screening: results of a randomized controlled trial. Prev. Med. 45, 267–273. doi: 10.1016/j.ypmed.2007.07.003
Schliemann, D., Tan, M. M., Hoe, W. M. K., Mohan, D., Taib, N. A., Donnelly, M., et al. (2022). mHealth interventions to improve cancer screening and early detection: scoping review of reviews. J. Med. Internet Res. 24:e36316. doi: 10.2196/36316
Sunstein, C. R. (2014). Nudging: a very short guide. J. Consumer Policy 37, 583–588. doi: 10.1007/s10603-014-9273-1
Vidal, C., Garcia, M., Benito, L., Milà, N., Binefa, G., and Moreno, V. (2014). Use of text-message reminders to improve participation in a population-based breast cancer screening program. J. Med. Syst. 38, 1–7. doi: 10.1007/s10916-014-0118-x
Keywords: ICT in healthcare provision, cervical cancer screening, health decision making, nudging, quasi-experiment
Citation: Antinyan A, Bellio S, Bertoni M, Corazzini L, Longone M and Narne E (2024) Pros and cons of digital access to healthcare services and healthcare utilization: a quasi-experiment. Front. Behav. Econ. 3:1458981. doi: 10.3389/frbhe.2024.1458981
Received: 03 July 2024; Accepted: 30 September 2024;
Published: 06 November 2024.
Edited by:
Steven Stillman, Free University of Bozen-Bolzano, ItalyReviewed by:
Agne Suziedelyte, City University of London, United KingdomElisabeth Gsottbauer, Free University of Bozen-Bolzano, Italy
Copyright © 2024 Antinyan, Bellio, Bertoni, Corazzini, Longone and Narne. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Luca Corazzini, bHVjYS5jb3JhenppbmlAdW5pbWliLml0
†Present address: Armenak Antinyan, Thames Water Utilities, Reading, United Kingdom
 Armenak Antinyan
Armenak Antinyan Stefania Bellio2
Stefania Bellio2 Marco Bertoni
Marco Bertoni Luca Corazzini
Luca Corazzini