
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Aging, 29 November 2022
Sec. Interventions in Aging
Volume 3 - 2022 | https://doi.org/10.3389/fragi.2022.915292
This article is part of the Research TopicLongevity with Functionality and Quality of LifeView all 9 articles
 Joel de Almeida Siqueira Junior1*
Joel de Almeida Siqueira Junior1* Adalberto Aparecido dos Santos Lopes1,2
Adalberto Aparecido dos Santos Lopes1,2 Carla Elane Silva Godtsfriedt1
Carla Elane Silva Godtsfriedt1 Marcelo Dutra Della Justina1
Marcelo Dutra Della Justina1 Karina Mary de Paiva3
Karina Mary de Paiva3 Eleonora d’Orsi4
Eleonora d’Orsi4 Cassiano Ricardo Rech1
Cassiano Ricardo Rech1This study aims to analyse the association between walkability index and depressive symptoms and cognitive impairment and test the mediating role of moderate-vigorous physical activity (MVPA) in this relationship among older adults from Florianópolis, Brazil. This is cross-sectional research with data from the third wave of the EpiFloripa Aging cohort study, conducted in 2017–2019. Depressive symptoms were assessed using the short version of the Geriatric Depression Scale (GDS), and cognitive impairment, using the Mini-Mental State Examination (MMSE) scales. The neighbourhood environment was assessed using a walkability index, which considered 500-m network buffers around the participants’ homes. Binary logistic regression analysis the association between the walkability index (quartile) and mental health outcomes (yes vs. no). Structural equation modelling evaluated the mediation between the walkability index and cognitive impairment by MVPA with an estimator of dichotomous variables. 1,162 people participated in the study (61.5% women, average age = 73.1). Older adults residing in places with a high and highest walkability index were 38% and 44% less likely to have cognitive impairment, respective. There was no association between depressive symptoms and walkability index in crude nor adjusted analysis. Engaging in MVPA had a partial but not significant effect (14%; p = 0.087), showing a tendency for this relationship to be partially explained by the greater engagement in physical activities in places with greater walkability. Policy planning to prevent and reduce the risks of cognitive impairment should consider factors of the physical environment as determinants in older adults.
In recent years, mental disorders have increased among older adults and represent a significant risk factor for loss of functional independence and longevity. It also has a personal impact, such as loss of functional capacity, family dependency and can affect healthcare systems (Giebel et al., 2016). Thus, the ability to age with preserved mental health has been the focus of attention in recent decades (Billal et al., 2021). The prevalence of depressive symptoms in older adults (≥60 years) has increased considerably around the world in recent years, ranging from 16% to 22% (Ismail et al., 2017), and the projection for 2050 is for an increase from 57.4% to 117% in the prevalence of cognitive impairment, affecting up to 152 million older adults (Nichols et al., 2019). These numbers can be even more worrying in low- and middle-income countries due to precarious access to health care, low level of education, many people residing in urban areas with poor infrastructure, and low social support (Li & Shou, 2021). Prospects also evidence a synergy between diseases, in the sense that the incidence of depressive symptoms can increase the risk of progression to cognitive impairment by two to five times (Mussele et al., 2014).
Despite the morbidities and increased chances of mortality due to a combination of health risk factors in the older adults, it is possible to compensate or decrease these risk factors by adopting healthier habits. The relationship between physical activity and mental health conditions has been well established (Hanson & Jones, 2015). Regular physical activity can promote cognitive development, delay symptoms of dementia, and prevent and treat depressive symptoms in older adults (Chen et al., 2017). Walking stood out, being the most prevalent activity in this population and considered a simple, low-cost strategy that makes them physically active and reduces mental health issues (Bonaccorsi et al., 2020). Therefore, providing better spaces for leisure-time walking has become one of the biggest challenges in global government agendas to boost care actions aimed at the mental health of older adults (Roe et al., 2020).
The physical and organizational structure of neighbourhoods can influence the mental health of senior citizens, either through their perception of aesthetics, safety and accessibility conditions or even through the geographic variations of the built environment (Melis et al., 2015; Wu et al., 2015). Thus, considering the characteristics of the neighbourhood environment in the formulation and implementation of public policies has presented significant evidence that makes it possible to encourage walking among older adults (Paiva Neto et al., 2021). The walkability, as an index of a neighbourhood’s ability to support walking in people’s daily lives (Frank et al., 2021), can be a means to monitor cities to create urban spaces that increase engagement in healthy behaviours (Mayne et al., 2018). Possible to measure using geospatial data, this index is composed of a set of indicators, such as residential density, the intersection of streets, mixed land use, and retail area (Frank et al., 2010), providing a better understanding of the urban environment, due to the complexity of factors that act in the same period in the daily life of citizens. A walkable neighbourhood can be better explored by the population, stimulating local commerce, social interactions among neighbours, and softening the impacts of depressive symptoms and cognitive decline in the older population (Gong et al., 2016).
From this perspective, the characteristics of the neighbourhood environment, such as mixed land use, availability of green areas and street connectivity, stimulate high levels of walkability (Watts et al., 2015; Wu et al., 2017). In the opposite direction, insecurity, inaccessible or poorly maintained sidewalks, and disruptions in the surrounding environment can impair cognitive performance in older adults (Cassarino & Setti, 2015). Also, in this context leisure-time physical activity can play an essential mediating role and explain the relationship between walkability and the cognitive, affective and social processes that justify aspects of mental health in urban centres (Solis-Urra et al., 2020).
After considering the characteristics of the neighbourhood environment as a potential for increasing neighbourhood walkability by older adults, this study hypothesizes that those older adults who reside in neighbourhoods with a higher walkability index are less likely to develop cognitive impairment and that moderate to vigorous leisure-time physical activity can mediate this relationship. Thus, the objective of this study was to analyse the association that the walkability index has with depressive symptoms and cognitive impairment, as well as to test the mediating role of moderate-vigorous physical activity (MVPA) in this relationship among older adults from Florianópolis, Brazil.
This is population-based, cross-sectional research using data from the third wave of the “EpiFloripa Aging: Living Conditions and Health of Older Adults from Florianópolis” cohort study, conducted between October 2017 and December 2019. The capital of the state of Santa Catarina had a population of 421,240 inhabitants, according to the last census of the Brazilian Institute of Geography and Statistics in 2010 (IBGE, 2011), and a territorial area of 675,409 km2 divided into 651 census sectors—603 urban and 48 rural. The city also had a Municipal Human Development Index (HDI-M) of 0.847, with the third best among Brazilian municipalities (UNDP, 2013).
The study involved older adults (≥60 years) living in the urban area of Florianópolis, Brazil. The third wave of the research became an open-cohort study with the inclusion of new older adults in the sample and those who participated in the previous waves and were being followed up. It started in 2017 and ended in 2019 with 1,335 older adults interviewed. To set the sample size, the formula for calculating the unknown prevalence (50%) was used, based on the reference more ageing population of 44,460 inhabitants, through a simple casual sample (confidence level of 1.96 standard deviations, 4% sampling error.
From identifying the profile of the older adults eligible to compose the Wave 3 sample of the EpiFloripa Aging study and maintaining an average of 20 older adults per sector, it was identified that between 3 and 16 older adults should be interviewed in each census sector. In this way, the average number of people per household (421,240 inhabitants/147,406 homes) and the proportion of older adults in the municipality (11.4%) were considered, resulting in an average of one older adult for every three households, with this formula being used: number of new older adults needed in the sector, with an increase of 20% for expected losses, multiplied by three (number of older adults in each household). Institutionalized older adults were considered as an exclusion criterion. Previous publications present the details of the study sample and methodology (Schneider et al., 2017; Confortim et al., 2019).
The presence of depressive symptoms was assessed using the short version of the Geriatric Depression Scale (GDS), a structured questionnaire ranging from 15-item (no/yes response options), which has a score ranging from 0 (absence of depressive symptoms) to 15 points (maximum score for depressive symptoms). For analytical purposes, the cut-off point of >6 was considered indicative of depressive symptoms in older adults (Almeida and Almeida, 1999).
Cognitive impairment was assessed using the Mini-Mental State Examination (MMSE) questionnaire, ranging from 0 to 30 points. The MMSE is a cognitive assessment test that analyzes different cognitive domains, such as time perception, spatial orientation, short-term memory, calculation, comprehension and writing (Folstein et al., 1975). In this study, the cut-off points used were that probable cognitive decline is indicated by a score of <19 points for individuals with no education and <24 points for those with some level of education (Almeida, 1998). For data analysis, the older adults were classified into “absence” and “presence” of cognitive impairment.
For the 1,335 participants in Wave 3 of the EpiFloripa Aging cohort study, it was possible to georeference 1,162 older adults who had complete address data. Then, 500-m network buffers were created around each participant’s residence (Frank et al., 2017). The walkability index was built using the ArcGIS software, version 10.5, owned by ESRI®, and taking into account three indicators: residential density, obtained by the ratio of the total number of residences divided by the total area of the buffer in Km2; the intersection of streets, estimated from the balance between the number of junctions formed by three or more segments, divided by the total area of the buffer in Km2; and mixed land use, obtained by calculating the entropy, which varies from zero (only one type of land use) to one (equal distribution among all land use categories) (Frank et al., 2010). For analysis purposes, the quartile values of the walkability index were considered and categorized as lowest (<−2.16), low (−2.17; −0.97), high (−0.98; 0.75) and highest (>0.76). Details on the walkability index development can be accessed in the preview publication (Justina, 2021).
Sociodemographic information was used as control variables, with sex (female and male) being obtained through observation by the researcher. Age was obtained through the participant’s date of birth, computed along with the date of their respective interview and classified into three categories—“60–69 years old,” “70–79 years old,” and “80 years old” or more. Marital status was obtained and classified as “married”, “single”, “divorced” and “widowed”. Education was collected in complete years of study and classified into three categories—“≤4 years,” “5–8 years,” and “≥9 years”. The percentage of older adults with a monthly income equal to or less than one minimum wage was calculated in accordance with the current value of the per capita income, between R$1,387.00 and R$1,406.00, in the year of the interview.
Alcohol consumption was obtained through the “The Alcohol Use Disorders Identification Test-Concise” (AUDIT-C) questionnaire (Babor et al., 2001) and categorized as “never,” “moderate use,” and “high”. Tobacco consumption was defined by the affirmative answer and classified as “never”, “smoked and quit”, and “currently smokes”. Body Mass Index (BMI) was calculated by dividing weight by height squared and classified as underweight (<22 kg/m2), normal weight (22–27 kg/m2) and overweight (>27 kg/m2) (Lipschitz, 1994). To estimate self-perception of health, the “regular”, “poor”, and “very poor” categories were classified as negative self-perception of health, while “very good” and “good” were grouped and classified as positive self-perception of health (Ware Junior, 1996). Moderate and vigorous physical activity (MVPA) in the leisure domain was assessed using the International Physical Activity Questionnaire (IPAQ) extended version, which was validated to be used with older people in Brazil (Benedetti et al., 2004); based on weekly frequency and length in minutes, it was categorized as insufficiently active (0–149 min/wk) and active (>150 min/wk).
The categorical variables were described utilizing their frequency distributions (absolute and relative), and the quantitative variables, by the central tendency and dispersion measures (mean and standard error). The association between the walkability index and the mental health of the older adults was tested using Binary Logistic Regression, considering the dichotomous character of the outcomes (depressive symptoms and cognitive impairment) and the non-normality of the exposure (walkability index), which was classified as lowest, low, high and highest walkability, by the quartile values. In addition to the crude models, adjusted models were tested, which considered the sociodemographic profile and health behaviours associated with the outcomes in the crude analysis. The binary logistic regression analyses were run on the SPSS® statistical software, version 21.0.
The model for mediation of physical activity in cognitive decline was assessed with the aid of the Mplus 13.1 software, using the WLSMV (Mean and Variance-Adjusted Weighted Square) method applied to the original items. The model’s goodness of fit analysis used the CFI (Comparative fit index) and GFI (Goodness-of-fit index), which were considered to indicate a good fit for values greater than 0.90. The RMSEA (Root mean square error of approximation) was also used, with 90%CI with an upper limit lower than 0.05 as a good fit (Maroco, 2010). The mediation model was only tested for cognitive decline, as it met the following conditions: 1) the exposure variable (walkability) was significantly associated with the outcome (depressive symptoms or cognitive impairment); 2) the exposure variable (walkability) was significantly associated with the mediator (MVPA); 3) the mediating variable (MVPA) was significantly associated with the outcome variable, and; 4) the exposure variable had its magnitude of association with the outcome reduced after the insertion of the mediating variable (Baron & Kenny, 1986). For all analyses, a significance of 5% was adopted.
A total of 1,335 older adults participated in the study, 173 of which (12.9%) were considered losses due to non-response in any outcome or exposure variables. The analysis included 1,162 people (61.5% women), aged 60 years (mean = 73.1; standard deviation = 7.82). Most of the sample was between 70 and 79 years old (41.4%), were married (56.5%), had more than 9 years of education (46.9%), and 90.7% had an income of up to one minimum wage. In the sample, 57% reported not consuming alcohol, 58.7% did not smoke, 54.6% were overweight, 62.6% reported a positive perception of health, and 88.1% were inactive. As for mental health, 14.7% had depressive symptoms, and 16.8% had cognitive impairment (Table 1).
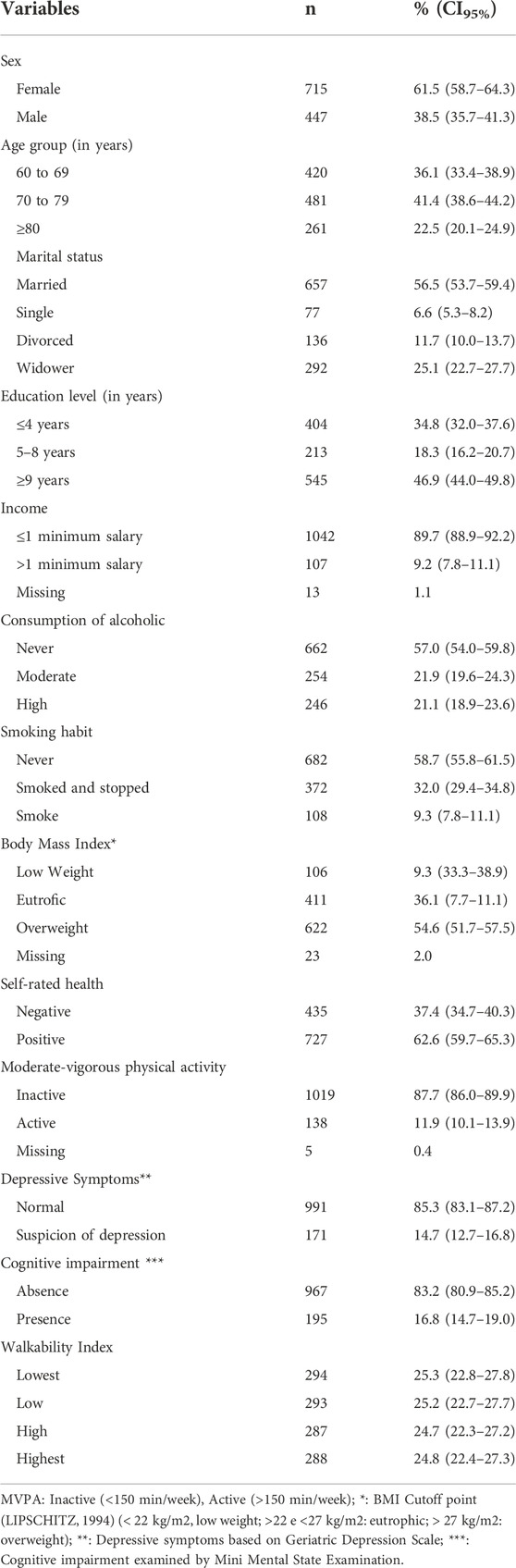
TABLE 1. Characteristics of the participants of the EpiFloripa Aging Study. Florianopolis, Brazil, 2017–2019 (n = 1,162).
The crude analysis showed that older adults aged 80 years and older (OR: 1.62; 95%CI: 1.07–2.45) have a higher chance of having depressive symptoms, on the other hand those older adults with a higher level of education (OR: 0.33; 95%CI: 0.23–0.49), who consume alcohol in moderate amounts (OR: 0.52; 95%CI: 0.34–0.81) and in high amounts (OR: 0.29; 95%CI: 0.17–0.50) are less likely to have depressive symptoms. Regarding cognitive impairment, those with a higher level of education (OR = 0.06; 95%CI: 0.03–0.10), who consume alcohol in moderate amounts (OR: 0.34; 95%CI: 0 0.21–0.54) and high amounts (OR:0.46; 95%CI: 0.30–0.71) are less likely to have this outcome. On the other hand, those who are older (≥80 years) (OR: 3.83; 95%CI: 2.53–5.81) and who are widowed (OR: 2.74; 95%CI: 1.94–3.86) are more likely to go through a cognitive decline (Table 2).

TABLE 2. Crude association between descriptive characteristics and mental health from older adults in Florianopolis, Brazil. EpiFloripa Aging Study, 2017–2019 (n = 1,162).
There was an association in both crude and adjusted analysis between walkability and cognition. The adjusted analysis shows that older adults residing in places with a high and highest walkability index were 38% OR = 0.62; 95%CI: 0.38–0.99) and 44% (OR = 0.56; 95%CI: 0.34–0.92) less likely to experience cognitive impairment. There was no association between depressive symptoms and walkability index (OR = 0,96; 95%CI: 0.58–1.59) in crude nor adjusted analysis (Tables 2, 3).
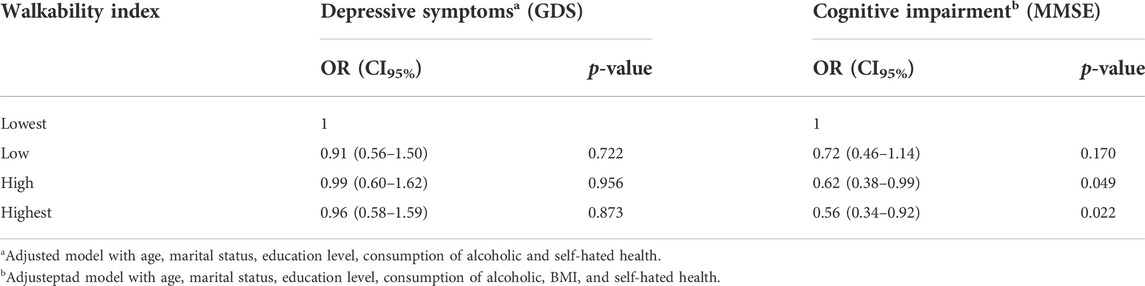
TABLE 3. Adjusted association between neighborhood walkability and mental health in older adults from Florianopolis, Brazil. EpiFloripa Aging Study, 2017–2019 (n = 1,162).
Engagement in moderate and vigorous physical activity had a partial and not statistically significant effect (14%; p = 0.087) on the relationship between walkability and cognitive impairment (Table 4).
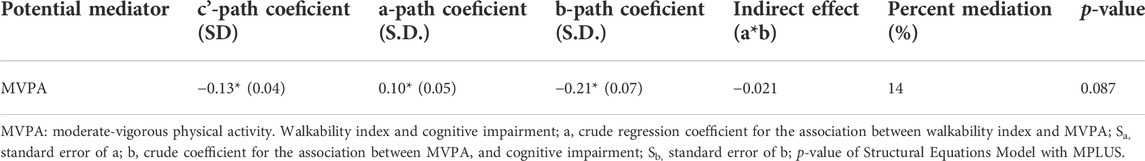
TABLE 4. Model of mediation by physical activity and association between neighborhood walkability and cognitive decline in older adults. EpiFloripa Aging Study. Florianópolis, Brazil, 2017–2019 (n = 1,162).
The study results showed that older adults living in places with better conditions for walking, with greater street connectivity, greater residential density and greater mixed land use have a lower prevalence of cognitive impairment. Moreover, a higher level of education, being physically active and having a positive perception of health decrease the chances of experiencing depressive symptoms and cognitive impairment. These findings are essential when it comes to prioritizing urban characteristics, directing them toward active mobility through walking-friendly environments, creating and maintenance of public roads aimed at pedestrians, enabling the promotion of mental health in the population through regular engagement in physical activities in urban centres (Lee et al., 2019).
There was no association between the walkability index and the prevalence of depressive symptoms in this study. Depression is considered the most frequent mental disorder in the population over 60 years of age and represents an important risk factor for dementia and decreased functional capacity (Fiske et al., 2009). In the present study, 14.5% of the participants presented depressive symptoms, with a higher prevalence in women (16.2%) and in older adults at a more advanced age (19.9%). Even with a difference in the prevalence of depressive symptoms, this condition did not differ significantly according to the neighbourhood walkability index. This result disagrees with studies that show that senior citizens who live in places with unfavourable environmental conditions for walking are more likely to have depressive symptoms (Bolstad et al., 2020). Additionally, residing in these places could mean greater unsafety due to poorer street lighting, uneven sidewalks and heavy traffic, which can interfere with the social interaction of older adults with their neighbours, reducing social support and time for physical activity, consequently leading to an increased prevalence of depressive symptoms (Bolstad et al., 2020). The non-association between the walkability index and depressive symptoms in this study can be related to using of the macroscale of the environment (walkability), and other factors more relationship to the microscale as proximity to green areas or blue places can explain this relation in the Latin context.
Older adults living in neighbourhoods with a higher walkability index had lower cognitive impairment. Similar results have been found in the literature and confirmed that community centres, bus stops, libraries, restaurants and quality public spaces are shown to be positively associated with cognitive function (Guo et al., 2019; Finlay et al., 2020). This is possibly due to the opportunities for engaging in healthy behaviours or to a greater cognitive stimulation provided by social interaction among peers (Clarke et al., 2015). In this sense, improving public urban planning policies that provide more friendly community environments, with less pollution and noise, for older adults is imperative on government agendas (Burton, 2012). So is developing social and health promotion programs that strengthen the mental health of this population (World Health Organization, 2017), mainly because of their greater vulnerability, which can limit active commuting, leading older adults to spend more time in their residential neighbourhoods and depend primarily on the services offered, such as convenience and grocery stores (Zhang et al., 2020).
In a causal relationship, the literature suggests that people with high levels of physical activity substantially reduces the risk of developing cognitive impairment (Blondell et al., 2014). Likewise, high levels of walkability can increase physical activity by up to 57% by providing environments with a diversity of options and access to businesses and services in the neighbourhood, parks with adequate structures for use, regular and well-maintained sidewalks, and well-connected streets (Reis et al., 2013; Balcetis et al., 2020). Thus, statistical models interpreted in isolation may establish that genuine relationships between variables are to be discarded (Mc Shane et al., 2019; Wasserstein et al., 2019). Assuming statistically significant differences simply refers to accepting or rejecting a null hypothesis without providing information about its magnitude or direction (Agler & Boeck, 2017). The findings of the present study show that, although there is no statistical significance (p = 0.087), the indirect effect of physical activity between outcome and exposure has an important clinical and epidemiological character. Indeed, physical activity behaviours have shown a considerable mediation between characteristics of the physical environment and the mental health of older adults (Van-Dyck et al., 2015). The 14% relationship for physical activity mediation found in this study can be explained, in part, by the fact that regions with better urban design characteristics offer more options for active behaviour, which is related to more significant social interaction (Igi-Elegbede et al., 2020), thus attenuating cognitive impairment. In this way, prioritizing interventions that restructure the urban landscape, allowing greater access to green spaces close to home by means of quality sidewalks, public safety, well-maintained street furniture, seems to be a feasible strategy to enable greater engagement in physical activity and reduced levels of cognitive impairment in the course of life (Gelius et al., 2020; Igi-Elegbede et al., 2020).
The interpretation of the results must consider some limitations. The statistical analysis was based on cross-sectional data that does not allow for establishing a causal relationship between the variables; the effect of the neighbourhoods walkability on mental health may require a specific exposure time so that it is possible to identify changes in outcomes, and this was not considered; data on race/ethnicity were not used in this study and would be able to elucidate individual and sociocultural characteristics, sense of belonging and walkability in the neighborhood. However, 13.9% of the older adults reported living at the same address for at least 15 years, which may have mitigated this limitation; objective measures referring to the environment (walkability) were used, but the adoption of subjective measures could consider the value, feelings and thoughts of older adults about the neighbourhood environment; the physical activity measure was self-reported, and although a valid instrument that has been widely used in investigations with older adults was applied, it may be less precise in measuring specific intensities of physical activity, such as vigorous-intensity, when compared with accelerometer measures; the assessment of the cognitive variables and depressive symptoms was based on valid instruments, but may differ from clinical diagnosis standards; finally, the sample consisted of older adults from a city in the south of Latin America, so extrapolation to other contexts must be done with caution, as the measures of the environment may be different from those presented here.
The study’s strength is analysing a representative sample of older adults from a coastal capital. All participants were interviewed face-to-face at their homes, which can improve the quality of the information obtained. Instruments with validity were used to assess cognitive deficits and depressive symptoms in Latin America. It was possible to use the neighbourhood walkability index, an internationally accepted measure, to analyse the macroscale conditions of the place to walk. Finally, to the best of our knowledge, this is one of the first studies to deepen the discussion of the relationship between the neighbourhood environment and mental health among older adults in the Latin American context, testing the mediating role of physical activity in this association.
The results of this study reinforce the association observed between the neighbourhood environment and cognitive impairment in the older population and that there is a tendency that this relationship is partially explained by a greater engagement in physical activities in places with greater walkability. Policy planning for the prevention and/or reduction of dementia risks should consider improving the walkability of cities to promote the population’s mental health. The WHO has established 2020–2030 as the decade of healthy ageing, and one of the focuses is to ensure the creation of more age-friendly cities, so it is important to consider that places with lower walkability may represent possible risk factors for cognitive decline. On the other hand, encouraging physical activity by revitalizing public spaces or programs to support healthy habits can be essential to reducing the effects of low walkability on mental health. Longitudinal population-based studies are needed to clarify causal directions and investigate possible explanatory mechanisms between the built environment and mental health.
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: https://repositorio.ufsc.br/handle/123456789/219631.
The studies involving human participants were reviewed and approved by Comitê de Ética em Pesquisa com Seres Humanos (CEPSH-UFSC). The patients/participants provided their written informed consent to participate in this study.
JS and AL, acted in the initial study design, data analysis, preparation of the graphical representations, literature review, interpretation of results, writing and critical revision of the manuscript; CG and MJ, were involved in the initial conception of the study, writing and reviewing the manuscript; KP and Ed’O, acted as principal investigators of the EpiFloripa Ageing Cohort Study, in the initial study design, writing and critical revision of the manuscript in all its stages; CR, acted as mentor, reviewer senior of conceptual and operational technical terms, in the initial conception of the study, writing and critical review of the manuscript in all its stages.
This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior—Brasil (CAPES)—Finance Code 001. Economic and Social Research Council (ESRC) of the United Kingdom through the Multicenter Promoting Independence in Dementia (PRIDE) project.
Special thanks to the EpiFloripa Ageing team for developing the three waves of the study, and also the study participants.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Agler, R., and Boeck, P. (2017). On the interpretation and use of mediation: Multiple perspectives on mediation analysis. Front. Psychol. 8, 1984. doi:10.3389/fpsyg.2017.01984
Almeida, O. P., and Almeida, S. A. (1999). [Reliability of the Brazilian version of the ++abbreviated form of Geriatric Depression Scale (GDS) short form]. Arq. Neuropsiquiatr. 57 (2B), 421–426. doi:10.1590/S0004-282X1999000300013
Almeida, O. P. (1998). Mini mental state examination and the diagnosis of dementia in Brazil. Arq. Neuropsiquiatr. 56, 605–612. doi:10.1590/S0004-282X1998000400014
Babor, T. F., Higgins-Biddle, J., Saunders, J., and Monteiro, M. (2001). AUDIT, the alcohol use disorders identification test: Guidelines for use in primary care. Geneva: Switzerland: Author.
Balcetis, E., Riccio, M., Duncan, D., and Cole, S. (2020). Keeping the goal in sight: Testing the influence of narrowed visual attention on physical activity. Pers. Soc. Psychol. Bull. 46 (3), 485–496. doi:10.1177/0146167219861438
Baron, R. M., and Kenny, D. A. (1986). The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 51 (6), 1173–1182. doi:10.1037//0022-3514.51.6.1173
Benedetti, T. R., Mazo, G. Z., and Barros, M. V. (2004). Application of the international physical activity questionnaire (IPAQ) for evaluation of elderly women: Concurrent validity and test-retest reprodutibility. R. Bras. Ci. E Mov. 12 (1), 25–34. doi:10.18511/rbcm.v12i1.538
Bilal, U., Hessel, P., Perez-Ferrer, C., Michael, Y. L., Alfaro, T., Tenorio-Mucha, J., et al. Salurbal group. (2021). Life expectancy and mortality in 363 cities of Latin America. Nat. Med. 27, 463–470. doi:10.1038/s41591-020-01214-4
Blondell, S. J., Hammersley-Mather, R., and Veerman, L. (2014). Does physical activity prevent cognitive decline and dementia? A systematic review and meta-analysis of longitudinal studies. BMC Public Health 14 (510), 510. doi:10.1186/1471-2458-14-510
Bolstad, C. J., Moak, R., Brown, C. J., Kennedy, R. E., and Buys, D. R. (2020). Neighborhood disadvantage is associated with depressive symptoms but not depression diagnosis in older adults. Int. J. Environ. Res. Public Health 17 (16), 5745. doi:10.3390/ijerph17165745
Bonaccorsi, G., Manzi, F., Del Riccio, M., Setola, N., Naldi, E., Milani, C., et al. (2020). Impact of the built environment and the neighborhood in promoting the physical activity and the healthy aging in older people: An umbrella review. Int. J. Environ. Res. Public Health 17 (17), 6127. doi:10.3390/ijerph17176127
Brazilian Institute of Geography and Statistics (2011). Resident population by sex and age groups according to major regions and Federation units – 2010. Rio de Janeiro, Brazil: Author.
Burton, E. (2012). Streets ahead? The role of the built environment in healthy ageing. Perspect. Public Health 132 (4), 161–162. doi:10.1177/1757913912449570
Cassarino, M., and Setti, A. (2015). Environment as 'brain training': A review of geographical and physical environmental influences on cognitive ageing. Ageing Res. Rev. 23, 167–182. Pubmed ID: 26144974. doi:10.1016/j.arr.2015.06.003
Chen, H., Kwong, J. C., Copes, R., Tu, K., Villeneuve, P. J., Donkellar, A. V., et al. (2017). Living near major roads and the incidence of dementia, Parkinson's disease, and multiple sclerosis: A population-based cohort study. Lancet 389 (10070), 718–726. Pubmed ID: 28063597. doi:10.1016/S0140-6736(16)32399-6
Clarke, J. P., Weuve, J., Barnes, L., Evans, D. A., and Leon, C. F. M. (2015). Cognitive decline and the neighborhood environment. Ann. Epidemiol. 25 (11), 849–854. doi:10.1016/j.annepidem.2015.07.001
Confortin, S. C., Schneider, I. J. C., Danielewicz, A. L., Fassula, A. S., Souza, B. B., Santos, C. E. S., et al. (2019). Estudo Longitudinal EpiFloripa Idoso – rotinas de organização e protocolos referentes à coleta, análise e armazenamento de material biológico, exames de imagem e capacidade físico-funcional. Cad. saude Colet. 27 (2), 210–224. doi:10.1590/1414-462x201900020169
Finlay, J., Esposito, M., Tang, S., Gomez-Lopez, I., Sylvers, D., Judd, S., et al. (2020). Fast-food for thought: Retail food environments as resources for cognitive health and wellbeing among aging Americans? Health Place 64, 102379. doi:10.1016/j.healthplace.2020.102379
Fiske, A., Wetherell, J. L., and Gatz, M. (2009). Depression in older adults. Annu. Rev. Clin. Psychol. 5, 363–389. doi:10.1146/annurev.clinpsy.032408.153621
Folstein, M. F., Folstein, S. E., and McHugh, P. R. (1975). Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 12 (3), 189–198. doi:10.1016/0022-3956(75)90026-6
Frank, L. D., Appleyar, B. S., Ulmer, J. M., Chapman, J. E., and Fox, E. H. (2021). Comparing walkability methods: Creation of street smart walkscore and efficacy of a code-based 3D walkability index. J. Transp. Health 21, 101005. doi:10.1016/j.jth.2020.101005
Frank, L. D., Fox, E. H., Ulmer, J. M., Chapman, J. E., Kershaw, S. E., Sallis, J. F., et al. (2017). International comparison of observation-specific spatial buffers: Maximizing the ability to estimate physical activity. Int. J. Health Geogr. 16 (4), 4. doi:10.1186/s12942-017-0077-9
Frank, L. D., Sallis, J. F., Saellens, B. E., Leary, L., Cain, K., Conway, T. L., et al. (2010). The development of a walkability index: Application to the neighborhood quality of life study. Br. J. Sports Med. 44 (13), 924–933. doi:10.1136/bjsm.2009.058701
Gelius, P., Messing, S., Goodwin, L., Schow, D., and Abu-Oma, K. (2020). What are effective policies for promoting physical activity? A systematic review of reviews. Prev. Med. Rep. 18, 101095. doi:10.1016/j.pmedr.2020.101095
Giebel, C., Sutcliffe, C., Verbeek, H., Zabalegui, A., Soto, M., Hallberg, I. R., et al. (2016). Depressive symptomatology and associated factors in dementia in europe: Home care versus long-term care. Int. Psychogeriatr. 28 (4), 621–630. Pubmed ID: 26652662. doi:10.1017/S1041610215002100
Gong, Y., Palmer, S., Gallacher, J., Marsden, T., and Fone, D. (2016). A systematic review of the relationship between objective measurements of the urban environment and psychological distress. Environ. Int. 96, 48–57. doi:10.1016/j.envint.2016.08.019
Guo, Y., Chan, C. H., Chang, Q., Liu, T., and Yip, P. S. F. (2019). Neighborhood environment and cognitive function in older adults: A multilevel analysis in Hong Kong. Health Place 58, 102146. doi:10.1016/j.healthplace.2019.102146
Hanson, S., and Jones, A. (2015). Is there evidence that walking groups have health benefits? A systematic review and meta-analysis. Br. J. Sports Med. 49 (11), 710–715. Pubmed ID: 25601182. doi:10.1136/bjsports-2014-094157
Igi-Elegbede, J., Pilkington, P., Orme, J., Williams, B., Prestwood, E., Black, D., et al. (2020). Designing healthier neighbourhoods: A systematic review of the impact of the neighbourhood design on health and wellbeing. Cities Health, 1–16. doi:10.1080/23748834.2020.1799173
Ismail, Z., Elbayoumi, H., Fischer, C. E., Hogan, D. B., Millikin, C. P., Schweizer, T., et al. (2017). Prevalence of depression in patients with mild cognitive impairment: A systematic review and meta-analysis. JAMA Psychiatry 74 (1), 58–67. Pubmed ID: 27893026. doi:10.1001/jamapsychiatry.2016.3162
Justina, M. D. D. (2021). Development, validation and association between the walkability index and in the older adults in Florianópolis Master's thesis. Florianópolis, Santa Catarina: Federal University of. Santa Catarina. Available from: https://repositorio.ufsc.br/handle/123456789/227235. Development, validation and association between the walkability index and in the older adults in Florianópolis.
Lee, K., and So, W. Y. (2019). Differences in the levels of physical activity, mental health, and quality of life of elderly Koreans with activity-limiting disabilities. Int. J. Environ. Res. Public Health 16 (15), 2736. doi:10.3390/ijerph16152736
Li, N., and Shou, J. (2021). The prevalence and correlates of depression in elderly outpatients in community health centers. J. Affect. Disord. Rep. 3, 100044. doi:10.1016/j.jadr.2020.100044
Lipschitz, D. A. (1994). Screening for nutritional status in the elderly. Prim. Care Clin. Office Pract. 21 (1), 55–67. doi:10.1016/s0095-4543(21)00452-8
Mayne, D. J., Morgan, G. G., Jalaludin, B. B., and Bauman, A. (2018). Does walkability contribute to geographic variation in psychosocial distress? A spatial analysis of 91, 142 members of the 45 and up study in sydney, Australia. Int. J. Environ. Res. Public Health 15 (2), 275. doi:10.3390/ijerph15020275
Mc Shane, B. B., Gal, D., Gelman, A., Robert, C., and Tackett, J. L. (2019). Abandon statistical significance. Am. Statistician 73 (1), 235–245. doi:10.1080/00031305.2018.1527253
Melis, G., Gelormino, E., Marra, G., Ferracin, E., and Costa, G. (2015). The effects of the urban built environment on mental health: A cohort study in a large northern Italian city. Int. J. Environ. Res. Public Health 12, 14898–14915. doi:10.3390/ijerph121114898
Mussele, S. V., Fransen, E., Struyfs, H., Luyckx, J., Marien, P., Saerens, J., et al. (2014). Depression in mild cognitive impairment is associated with progression to alzheimer's disease: A longitudinal study. J. Alzheimers Dis. 42 (4), 1239–1250. Pubmed ID: 25024328. doi:10.3233/JAD-140405
Nichols, E., Szoeke, C. E. I., Vollset, S. E., Abbasi, N., Abd-Allah, F., Abdela, J., et al. (2019). Global, regional, and national burden of alzheimer's disease and other dementias, 1990–2016: A systematic analysis for the global burden of disease study 2016. Lancet Neurol. 18 (1), 88–106. doi:10.1016/S1474-4422(18)30403-4
Paiva Neto, F. T., Arins, G. C. B., d’Orsi, E., and Rech, C. R. (2021). Are changes in walking for transportation in brazilian older adults associated with attributes of the neighborhood environment? J. Aging Phys. Act. 29 (4), 686–694. doi:10.1123/japa.2020-0120
Roe, J., Mondschein, A., Neale, C., Barnes, C., Boukhechba, M., and Lopez, S. (2020). The urban built environment walking and mental health outcomes among older adults: A pilot study. Front. Public Health 8, 575946. doi:10.3389/fpubh.2020.575946
Schneider, I. J. C., Confortin, S. C., Bernardo, C. O., Bolsoni, C. C., Antes, D. L., Pereira, K. G., et al. (2017). EpiFloripa aging cohort study: Methods, operational aspects, and follow-up strategies. Rev. Saude Publica 51, 104. doi:10.11606/s1518-8787.2017051006776
Solis-Urra, P., Plaza-Diaz, J., Álvarez-Mercado, A. I., Rodríguez-Rodriguez, F., Montero, C., Zavala-Crichton, J. P., et al. (2020). The mediation effect of self–report physical activity patterns in the relationship between educational level and cognitive impairment in elderly: A cross-sectional analysis of Chilean health national survey 2016–2017. Int. J. Environ. Res. Public Health 17 (8), 2619. doi:10.3390/ijerph17082619
United Nations Development Program (2013). Atlas of human development in Brazil. new atlas of human development in brazil: Florianopolis, Brazil. Author. New York, USA.
Van Dyck, D., Teychenne, M., McNaughton, S. A., De Bourdeaudhuij, I., and Salmon, J. (2015). Relationship of the perceived social and physical environment with mental health-related quality of life in middle-aged and older adults: Mediating effects of physical activity. PLoS ONE 10 (3), e0120475. doi:10.1371/journal.pone.0120475
Ware, J., Kosinski, M., and Keller, S. D. (1996). A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Med. Care 34 (3), 220–233. doi:10.1097/00005650-199603000-00003
Wassertein, R. L., Schirm, A. L., and Lazar, N. A. (2019). Moving to a world beyond "p < 0.05. Am. Statistician 73 (1), 1–19. doi:10.1080/00031305.2019.1583913
Watts, N., Adger, W. N., Agnolucci, P., Blackstock, J., Byass, P., Cai, W., et al. (2015). Health and climate change: Policy responses to protect public health. Lancet 386 (10006), 1861–1914. doi:10.1016/S0140-6736(15)60854-6
World Health Organization, (2017). Depression and other common mental disorders. Geneva, Switzerland: Global health estimates.
Wu, Y. T., Prina, A. M., Jones, A., Matthews, F. E., and Brayne, C. (2015). Older people, the natural environment and common mental disorders: Cross-sectional results from the cognitive function and ageing study. BMJ Open 5, e007936. doi:10.1136/bmjopen-2015-007936
Wu, Y. T., Prina, A. M., Jones, A., Matthews, F. E., and Brayne, C. (2017). The built environment and cognitive disorders: Results from the cognitive function and ageing study II. Am. J. Prev. Med. 53 (1), 25–32. doi:10.1016/j.amepre.2016.11.020
Keywords: walkability index, cognitive impairment, depressive symptoms, physical activity, older adults
Citation: Siqueira Junior JdA, Lopes AAdS, Godtsfriedt CES, Justina MDD, Paiva KMd, d’Orsi E and Rech CR (2022) Neighbourhood walkability and mental health in older adults: A cross-sectional analysis from EpiFloripa Aging Study. Front. Aging 3:915292. doi: 10.3389/fragi.2022.915292
Received: 07 April 2022; Accepted: 31 October 2022;
Published: 29 November 2022.
Edited by:
Evelyne Yehudit Bischof, Shanghai University of Medicine and Health Sciences, ChinaReviewed by:
Mathew Hill, Coventry University, United KingdomCopyright © 2022 Siqueira Junior, Lopes, Godtsfriedt, Justina, Paiva, d’Orsi and Rech. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Joel de Almeida Siqueira Junior, am9lbGFsbWVpZGEuZWZAZ21haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.