Abstract
Background: Dementia is the one of the most common and prominent disease in the elderly person that results in the Cognitive interventions. In this study, we aim to conceptualize the cognitive intervention for older adults with and without cognitive dysfunction and to clarify the heterogeneity existing in this literature field by determining the main variables implicated.
Methods: We conducted a study analysis using previous literature highlighting the significant data reporting empirical results from cognitive intervention for healthy older adults and other seniors with different types of dementia. Each paper was reviewed in terms of compensatory cognitive training, cognitive remediation, enrichment, cognitive activation, brain training, cognitive stimulation, cognitive training, and cognitive rehabilitation. The research analysis was performed following rigorous inclusion and exclusion criteria with the purpose of collecting relevant answers to our research questions.
Results: We included a total of 168 studies in our review. Our findings indicated heterogeneity regarding methods, concepts, and procedures. Additionally, the values were integrated using different information existing in this field.
Conclusion: In conclusion, we highlighted that this is the first review that clarify the discrepancy of various existing definitions, methods, and procedures, as well as the overlapping information in the cognitive interventions.
Introduction
According to the World Health Organization (World Health Organization, 2017b), the world’s population is rapidly aging. By 2050, it is been estimated that people over the age of 60 will account for about 22% of the world’s total population. Falls, diabetes, depression and dementia continue to be the major causes of disability in the elderly (World Health Organization, 2017). Besides musculoskeletal, sensory, immune and other disorders, cognitive functioning is also a matter of concern regarding the health of the elderly, impacting their intrinsic and functional capacity (World Health Organization, 2015b). Intrinsic capacity encompasses both physical and mental attributes people can rely on, throughout the course of their life, while functional capacity is related to having the abilities that allow them to be what they want to be (World Health Organization, 2015a). The significant increase in the average life expectancy in the last century has had consequences in this age group, namely the rapid growth of neurodegenerative dementias (Murman, 2015). Moreover, consequences have been seen at social and economic levels, particularly on both the health system and the labor market, directly affecting the elderly, who face new challenges related to cognitive deterioration (Hedden and Gabrieli, 2004).
Normal aging is a process of human development that inevitably entails biological and physiological (structural and functional) brain changes with neuropsychological and social consequences. However, the age factor may lead to different degrees of physical or mental decline (World Health Organization, 2015a). The key to healthy aging is to engage in both physically and mentally stimulating activities (Lee, 2000). Limitations in the ability to independently perform activities of daily living (ADL) are negatively associated with physical and mental well-being (Willis, 1996). In fact, the concept of ‘activities of daily living’ in the elderly is related to physical, emotional, and cognitive aspects. Cognitive aging in particular depends on intelligence, education, and sensory abilities (Drag and Bieliauskas, 2010).
The concept of healthy aging has been defined as a process of development and maintenance of functional capacity (World Health Organization, 2015) or adaptation to the physical, social, and psychological changes that allow the well-being of the elderly (Peel et al., 2004). Cognitive changes are core in this concept because of their close relationship to impairment that affects ADL and functional capacity (Yam and Marsiske, 2013). Thus, in the last decade, we have witnessed an increase in research on healthy aging and lifestyle associated with older adults’ cognitive functioning, namely, the development of neuropsychological interventions using new technologies capable of promoting the older adults’ quality of life (QoL).
There are three types of cognitive decline in the elderly: normal aging (normal cognitive decline), pre-dementia (mild cognitive deficit) (Petersen et al., 2001), and different types of dementia (severe cognitive deficit) (Alves et al., 2013). Cognitive intervention consists of various treatments based on different theoretical constructs, aimed to improve an impaired function, prevent cognitive decline, or, at least, maintain the functional level (Gates and Sachdev, 2014). Given that cognitive intervention encompasses several distinct concepts (e.g., compensatory cognitive training, cognitive remediation, cognitive training), it is important to further analyze these concepts, clarify their similarities and differences, so that these can be considered in future research. Therefore, the main aim of this study is to define the types of cognitive intervention and corresponding methodologies usually applied in older adults and clearly distinguishing the terms usually used in the literature. After reviewing the literature regarding older adults, there seem to be eight different types of cognitive interventions that are most commonly used, and main motivations are to focus on this work: Compensatory Cognitive Training, Cognitive Remediation, Enrichment, Cognitive Activation, Brain Training, Cognitive Stimulation, Cognitive Training, and Cognitive Rehabilitation.
Consequently, it is important to discuss what are the most critical differences between these distinct non-pharmacological treatments, relating to definitions, methods, and procedures.
Studies Characteristics
We found total 168 articles (Figure 1) through database searching (Supplementary Appendix S1) in which 59 were randomized controlled studies with post-intervention follow-up of the participants, 74 were randomized controlled trials without follow-up, 28 used a pre and post-test design with a 3–12-month post-intervention follow-up, two non-randomized pilot studies, two were descriptive and exploratory studies, two were longitudinal studies, and one was a single-blind wait list-controlled study.
FIGURE 1
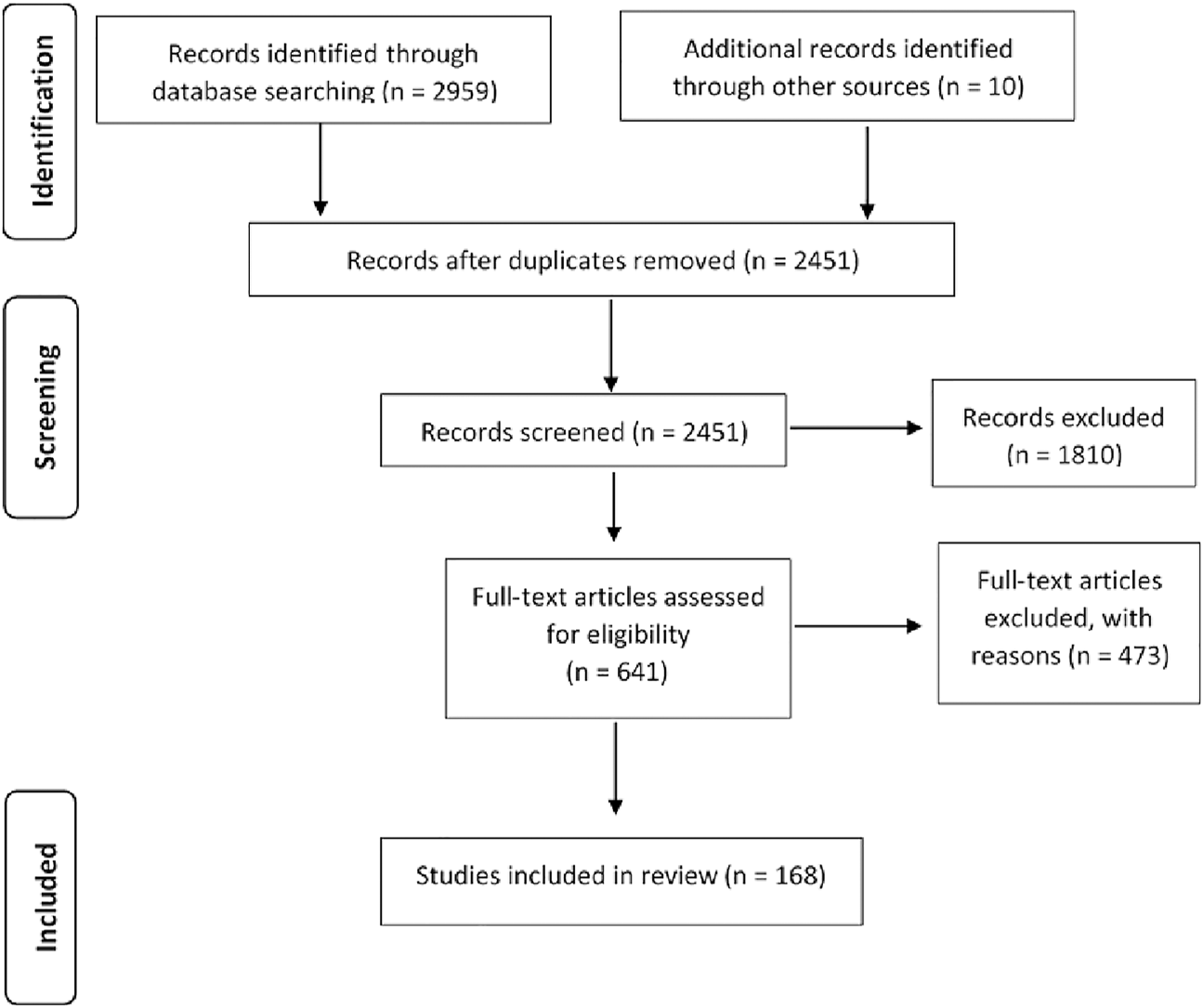
Literature search flow on cognitive interventions.
Mostly in studies investigated the sample size was approximately 97 both healthy or composed healthy older adults, 26 studies were on older adults with mild cognitive impairment (MCI) or amnestic MCI (aMCI), two studies on psychotic disorders, 19 studies on older adults with dementia or mild to moderate dementia, 21 studies on Parkinson’s disease (PD), Alzheimer’s disease (AD), and older adults with cognitive impairment, and one studied stroke, HIV-associated neurocognitive disorders in older adults, and older adults with major depression.
The studies included were thoroughly reviewed in terms of the following types of cognitive intervention: Compensatory Cognitive Training, Cognitive Remediation, Enrichment, Cognitive Activation, Brain Training, Cognitive Stimulation, Cognitive Training, and Cognitive Rehabilitation (Table 1). The criteria for determining the type of cognitive intervention used in each study are summarized in Table 2. Our review includes 35 studies on Cognitive Stimulation and 11 on Cognitive Rehabilitation intervention where most of the tasks did not include computerized tasks; 102 studies on Cognitive Training intervention where most of the tasks were presented in computerized form; three studies on Enrichment, six on Cognitive Remediation and seven on Brain Training that included computer-based training or video game; and four studies on Compensatory Cognitive Training where external compensation strategies were used.
TABLE 1
| Cognitive intervention | Definition | Authors |
|---|---|---|
| Compensatory cognitive training | Use of low-tech intervention strategies (internal, external, or environmental) to compensate for cognitive impairment, reducing its impact on activities of daily living and quality of life | Greenaway et al. (2013), Huckans et al. (2013), Kim and Kim (2014), Lenze and Bowie (2018), Twamley et al. (2012), Velligan et al. (2000) |
| Cognitive remediation | Neuropsychological intervention proposed by therapists for life functional and social recovery and competence development. May or not include computerized exercises to improve cognitive performance | Lenze and Bowie (2018), Medalia et al. (2002), Medalia and Richardson (2005), Medalia and Choi (2009), Mowszowski et al. (2010), Vance (2009), Vance et al. (2009) |
| Enrichment | All activities (activity/cognitive stimulation, social, physical, and intellectual) with a positive impact on cognitive functioning that enhance cognitive enrichment. Implementation of motor, sensory, and cognitive stimuli in the person’s environment | Hertzog et al. (2008), Steinerman (2010), Patel (2012) |
| Cognitive activation | Computer-based training to maintain their functioning, often with at least orientation or facilitation by people who are not therapists | Lenze and Bowie (2018) |
| Brain training | Is a concept mostly used by companies that commercialize to the public cognitive intervention programs. A program or activity (e.g., video games, music, computerized training, physical exercise) repeated over a period of time to improve cognitive deficits or performance in other cognitive tasks, including daily life activities (e.g., driving). brain training (Simons et al., 2016) | Heugten et al. (2016), Rabipour and Raz (2012), Simons et al. (2016) |
| Cognitive stimulation | Participation in activities that generally improve cognitive and social functioning. Includes multiple group activities under a social environment and multisensory stimulation | Clare and Woods (2004), Eckroth-Bucher and Siberski (2009), Gates and Sachdev (2014), Kim and Kim (2014), Kueider et al. (2014), Mowszowski et al. (2010), Steinerman (2010) |
| Cognitive training | Training of specific cognitive functions such as memory, executive functioning, language, and attention, involving guided practice and repetitive training | Bahar-Fuchs et al. (2013), Chaikham et al. (2016), Clare et al. (2003), Clare and Woods (2004), Eckroth-Bucher and Siberski (2009) |
| Presented in paper and pencil or computerized form, with the objective of identifying, tracking, and monitoring the user | Gates et al. (2019), Kueider et al. (2014), Lenze and Bowie (2018), Mowszowski et al. (2010), Steinerman (2010) | |
| Cognitive rehabilitation | Individualized approach, developed based on the goals of each user, i.e., in cognitive deficits, functional, and behavioral problems, and in real life. The planning and implementation of the cognitive rehabilitation plan involves the person with cognitive deficits, family members, and a set of health professionals | Bahar-Fuchs et al. (2013), Cicerone et al. (2000), Clare et al. (2003), Kueider et al. (2014), Mowszowski et al. (2010), Steinerman (2010), Wilson (2002) |
Types of cognitive intervention defined in the literature.
TABLE 2
| Cognitive intervention | Characteristics | Tasks |
|---|---|---|
| Compensatory cognitive training | Attention, memory, executive functioning, learning of meta-cognitive strategies | External strategies such as calendar use, self-talk, note-taking, navigation devices, and a six-step problem-solving method |
| Internal strategies such as mnemonic techniques, using visual imagery; using structured problem-solving, and planning methods | ||
| Environmental strategies such as alter the workplace by removing visually distracting stimuli | ||
| Cognitive remediation | Attention, memory, processing speed, and executive function training | Computer-based cognitive training |
| Cognitive-behavioral therapy and attention process training intervention; do not include computerized tasks | ||
| Enrichment | Learning, perceptual speed, memory, visuospatial skills, attention, processing speed, concentration, and executive functions | Internet-based training |
| Combined physical and cognitive intervention | ||
| Brain training | Working memory, attention, memory, visuoperceptual and visuospatial skills, intelligence, language, executive functions, processing speed, and reasoning | Video games and computer-based cognitive training |
| Cognitive stimulation | Global cognition, fluid intelligence, executive functions, working memory, praxis, language, memory, attention, concentration, orientation, perception, processing speed, problem-solving, reasoning, and visuospatial skills | Computer-based cognitive training |
| Combined physical and cognitive intervention | ||
| Mobile and tablet-based cognitive training programs | ||
| Cognitive stimulating activities (e.g., puzzles, quizzes, origami, autobiographical memory) that do not include computerized training | ||
| Multiple group activities (e.g., music, poetry, museums, visual arts) | ||
| Cognitive training | Global cognition, fluid intelligence, executive functions, working memory, praxis, language, memory, attention, orientation, perception, processing speed, problem-solving, reasoning and visuospatial skills | Computer-based cognitive training |
| Video games | ||
| TV and tablet-based cognitive training programs | ||
| Combined physical and cognitive intervention | ||
| Combined behavioral interventions and computerized tasks | ||
| Paper and pencil tasks | ||
| Cognitive rehabilitation | Global cognition, language, memory, executive functions, attention, concentration, problem-solving, reasoning, perception, and visuospatial abilities | Computer-based cognitive training |
| Virtual environment | ||
| Multiple group activities (e.g., self-assertiveness training, relaxation techniques, stress management, anxiety management strategies) | ||
| Internal and external strategies such as books, diaries, post-it notes, timers, calendars that do not include computerized training | ||
| Cognitive rehabilitation groups to train specific cognitive functions (e.g., language, memory) |
Criteria for type of cognitive intervention: compensatory cognitive training, cognitive remediation, enrichment, cognitive activation, brain training, cognitive stimulation, cognitive training, and cognitive rehabilitation.
Cognitive Interventions
Cognitive Interventions (CI) is used as term to describe the variety of therapeutic approaches designed to address psychological problems at the cognitive (conscious mind) level, by the activation and analysis of thoughts, experiences, senses and memories. By using these techniques therapist helps enlist patients to develop solutions to problems going on in their mind that will be effective and permanent. Through intervention, therapist can draw the attention of the patients to the unreasonable pictures that mind has created and then begin to create tools for dealing with those pictures.
The cognitive approach to psychology assumes that your emotions, behaviors and psychology are controlled by the way you view the things that have happened around you, and cognitive interventions are launched from this point of view. In other words, if you see problems that minds create, they can be removed by changing the way of thinking and exercising your mind to work in different ways.
Types of Cognitive Intervention
Compensatory Cognitive Training
The literature refers to Compensatory Cognitive Training as the use of low-tech intervention strategies (internal, external, or environmental) to compensate for cognitive impairment in order to reduce its impact on ADL and QoL (Velligan et al., 2000; Twamley et al., 2012; Greenaway et al., 2013; Huckans et al., 2013; Kim and Kim, 2014; Lenze and Bowie, 2018). In general terms, it has been shown to improve memory and functionality in ADL (Greenaway et al., 2013).
This type of cognitive intervention has been implemented in various populations, including older adults, namely, individuals with aMCI, using external memory compensatory strategies (Troyer et al., 2008; Greenaway et al., 2013), and individuals with psychotic disorders (Twamley et al., 2012). Velligan et al. (2000), who tested the effect of compensatory strategies on apathy, disinhibition, and improvement of executive functions in 45 older adults with schizophrenia, indicated that patients using compensatory strategies showed greater improvement in motivation and overall functioning than those under other treatments.
However, this type of intervention’s training and applicability are controversial. It is intended for people with severe cognitive impairment and considerable functional impairment (Lenze and Bowie, 2018). Compensation focused interventions encompass cognitive interventions mainly aiming to enhance frontally mediating functions or to compensate specific cognitive functions that are adversely affected by aging. The results of a literature review by Kim and Kim (2014), which considered empirical studies with healthy, impaired, or demented older adults, indicated that Compensatory Cognitive Training is probably most effective when the intervention specifically supports frontal mediation activity and facilitates primarily compensatory adaptation in the brain according to the direction of indigenous adjustments in the aging brain.
Cognitive Remediation
Cognitive remediation is a therapy that uses set of techniques designed to teach ‘thinking skills’ that can be thought as a form of cognitive rehabilitation. This involves training in a set of tasks that are designed to improve cognitive abilities and social functioning. The domain targeted depends upon client needs, but might include attention, working memory, planning, and executive function. However, CRT has been studied most often in schizophrenia/psychosis, but also in other conditions such as anorexia nervosa. Schizophrenia patients mainly show cognitive deficits in executive functioning, verbal fluency, and distractibility (Wykes and van der Gaag, 2001). Whereas, patients with anorexia nervosa have difficulties in set shifting tasks which are believed to correspond to cognitive inflexibility/rigid thinking that is seen in these patients group (Tchanturiaet al., 2007).
Cognitive Remediation mainly focuses on global cognitive training (e.g., theater training) or particular cognitive competencies (e.g. memory) and uses different techniques/methods of intervention, such as paper and pencil exercises, group activities, workshops, video, or computers (Vance, 2009; Vance et al., 2010). Based on a neuropsychological approach, this cognitive intervention uses a set of exercises to maintain, ameliorate, or mitigate the loss of cognition or abilities in the elderly (Vance et al., 2009). Therapists propose this type of intervention for functional and social recovery, as well as competence development (Medalia et al., 2002; Medalia and Richardson, 2005; Medalia and Choi, 2009; Vance, 2009; Vance et al., 2009; Mowszowski et al., 2010; Lenze and Bowie, 2018).
Currently, most Cognitive Remediation programs use computerized tasks to train various cognitive functions, namely, attention, memory, processing speed, and executive function (Morimoto et al., 2014). Examples are the game exercises (Sweep Seeker, Bird Safari, Target Tracker, Master Gardener, and Double decision) from the ACTIVE study (Vance et al., 2017), Mindfit (Verghese et al., 2010), and PSSCogRehab (Choi et al., 2018). Only two of the included studies followed a pre and post-test design, including cognitive-behavioral therapy and attention process training (not using computerized tasks), applied to participants with PD (Mohlman et al., 2011; Mohlman et al., 2017).
Besides the elderly, Cognitive Remediation has also been used in psychiatric populations (e.g., schizophrenia). In this case, this intervention is applied according to different theoretical perspectives, often in conjunction with psychosocial interventions or complementary to pharmacological treatment (Morimoto et al., 2012).
Cognitive Activation
Contrary to Cognitive Remediation, the Cognitive Activation intervention is directed to healthy individuals or individuals with MCI who are autonomous and functional. Thus, therapists are not mandatory for its administration, as computer tasks are used. Moreover, there is no group intervention, and the transfer of cognitive gains to the functioning of ADL is not expected (Lenze and Bowie, 2018). Actually, the main aim of Cognitive Activation is to maintain the users’ functioning. However, for this review, we have emphasized very few results of this type of intervention on relevant literature.
Cognitive Training
Cognitive Training involves the guided practice and repetitive training of cognitive functions using either computerized or paper and pencil methods. These cognitive intervention aims both to improve cognitive deficits (Duda and Sweet, 2020) and to identify, track, and monitor the user’s cognitive performance (Clare et al., 2003; Clare and Woods, 2004; Eckroth-Bucher and Siberski, 2009; Zelinski, 2009; Mowszowski et al., 2010; Steinerman, 2010; Bahar-Fuchs et al., 2013; Kueider et al., 2014; Chaikham et al., 2016; Lenze and Bowie, 2018; Gates et al., 2019). It has been used in persons with age-related cognitive decline (VanVleet et al., 2018), mild to moderate AD (Farina et al., 2006; Kanaan et al., 2014; Amieva et al., 2016; Giuli et al., 2016; Nousia et al., 2018; Liang et al., 2019), and loss of functionality or mild to moderate dementia, which may include structured weekly training facilitated by a therapist (De Luca et al., 2016).
Cognitive Training essentially trains specific rational functions, such as memory, executive functioning, processing speed, language and attention, through repetitive training, in older adults with or without cognitive impairment (Auffray and Juhel, 2001; Clare et al., 2003; Günther et al., 2003; Clare and Woods, 2004; Barnes et al., 2009; Eckroth-Bucher and Siberski, 2009; Irigaray et al., 2011; Zelinski et al., 2011; Cheng et al., 2012; Herrera et al., 2012; Irigaray et al., 2012; Bahar-Fuchs et al., 2013; Ball et al., 2013; Garcia-Campuzano et al., 2013; Naismith et al., 2013; Netto et al., 2013; Rebok et al., 2013; Kanaan et al., 2014; Peña et al., 2014; Rebok et al., 2014; Nouchi et al., 2016; Lee et al., 2018; Marusic et al., 2018; Smith et al., 2018; Gates et al., 2019; Matysiak et al., 2019). Previously, Kim and Kim (2014) or Thompson and Foth (2005) in most of there studies focus on memory training because problems in this cognitive domains are the most prominent concerns in the elderly.
A significant part of the studies in this review (Supplementary Appendix S1) used computerized programs to train various cognitive functions in older adults with or without cognitive alterations. Souders et al. (2017) applied the Mind Frontiers Game to 60 healthy older adults to train general reasoning, spatial reasoning, planning, processing speed, task switching and working memory. Similarly, Whitlock et al. (2012) applied the game World of Warcraft to 39 older adults to train spatial ability, executive function, and memory to detect an improvement in the intervention group’s attention. Furthermore, Basak et al. (2008) designed a video game (Rise of Nations) to train executive control functions (switching, inhibition, reasoning, working memory, short-term memory) in 40 older adults and achieved an improvement in the executive control functions. Simpson et al. (2012) also applied computerized Cognitive Training (www.mybraintrainer.com) to 34 healthy older adults, using a randomized, single-blind design with a 3-week follow-up period, and observed an improvement in reaction time, choice reaction time, and processing speed in the intervention group.
Several studies focused on the applicability of TV (Nouchi et al., 2019) and tablet-based Cognitive Training programs, either in healthy older adults (Vaportzis et al., 2017) or older adults with cognitive impairment. For example, Savulich et al. (2017) applied the Game Show to 21 older adults with MCI using a tablet and observed an improvement in episodic memory and visuospatial capacity, besides high levels of enjoyment and motivation. Chan et al. (2016) and Binder et al. (2016) also used a tablet to train cognitive functions of older adults, such as processing speed, visuospatial processing, attentional and mental control, episodic and working memory, and executive functions, and achieved an improvement in processing speed and episodic memory but no differences in mental control and visuospatial processing.
In turn, González-Palau et al. (2013) and Gonzá lez-Palau et al. (2014) used the GRADIOR software in a sample of older adults with MCI compared to healthy older adults to train perception, attention, episodic memory, and working memory. The users showed good usability and satisfaction with the intervention platform, improved verbal memory and attention, and reduced depressive symptomatology. In the same line, Fellman et al. (2020) used an internet-based platform to apply a Cognitive Training program focused on working memory in a sample of older adults with PD and verified improved working memory and reduced depression. Navarro et al. (2009) used the software How to Improve Your Mental Skills in healthy older adults to train memory and other cognitive functions and observed improved memory scores.
Other studies reinforce the use of Cognitive Training to address other cognitive domains of older adults at risk of cognitive decline. Maseda et al. (2013) developed a study on the efficacy of a Cognitive Training application (Telecognition) involving older adults with and without memory impairments. That application focused on memory, attention, language, calculation, abstract reasoning, perception, orientation and praxis. The results showed improvements in global cognitive, episodic memory, visuospatial, and verbal fluency skills on post-intervention patients without significant memory deficits. The same program was also used in older adults to address cognitive function and depressive symptomatology (Millán-Calenti et al., 2015), revealing improvement in overall cognitive functioning.
Several studies evaluated the BrainFitness program in older adults for the training of attention, working memory (Leung et al., 2015), executive function (Gooding et al., 2015) and processing speed (Smith et al., 2018; Valdés et al., 2019). Other computer-based training programs, such as CogniFit, SmartBrain, Cogmed, Lumosity, and COGPACK, have also been used to train the same cognitive functions (working memory, attention, memory and processing speed) in samples of healthy older adults (Gigler et al., 2013; Shatil, 2013) and older adults with PD (Paris et al., 2011), MCI (Belleville et al., 2006; Finn and McDonald, 2011; Vermeij et al., 2016), or subjective memory complaints (Frankenmolen et al., 2018).
Several studies applied Cognitive Training in older adults using several computerized tasks (examples are Borella et al., 2010; Wang et al., 2011; Zajac-Lamparska and Trempała, 2016; Bellander et al., 2017; Buitenweg et al., 2017; Golino et al., 2017; Grönholm-Nyman et al., 2017; Reijnders et al., 2017; Goghari and Lawlor-Savage, 2018; Withiel et al., 2019; Brum et al., 2020). Also, the results of a randomized controlled trial that included both behavioral interventions and computerized tasks—the ACTIVE Study (some examples: Ball et al., 2002; Margrett and Willis, 2006; Willis et al., 2006; Wolinsky et al., 2006; Wolinsky et al., 2009; Ball et al., 2010; Gross et al., 2011; Jones et al., 2013; Rebok et al., 2013; Sisco et al., 2013; Rebok et al., 2014; Ross et al., 2016; Ross et al., 2017; Ross et al., 2018) revealed that successful performance in daily tasks depends on executive function (Gross et al., 2011).
On the other hand, several studies applied Cognitive Training with paper and pencil or non-computerized tasks in older-adult samples with or without cognitive impairment. Some studied the Cognitive Training effects on global cognitive function in healthy older adults, which is often measured by tests that assess multiple cognitive domains (Park et al., 2009; Kwok et al., 2013; Chen et al., 2018; Rizkalla, 2018), while others focused on specific cognitive functions such as attention, working memory, language, executive functions, reasoning and visuospatial construction (Irigaray et al., 2011; Cheng et al., 2012; Irigaray et al., 2012; Jackson et al., 2012; Carretti et al., 2013; Netto et al., 2013; Feng et al., 2014; Li et al., 2016; Lopes and Argimon, 2016; Nouchi et al., 2016; Cantarella et al., 2017; Kuo et al., 2018; Rizkalla, 2018; Tagliabue et al., 2018). Regarding older adults with MCI, interventions not using computerized tasks were also focused either on global cognitive functioning (Rojas et al., 2013; Cohen-Mansfield et al., 2015; Sukontapol et al., 2018) or specific cognitive domains such as attention, memory (Cohen-Mansfield et al., 2015), language (Yan et al., 2016) and executive functions (López-Higes et al., 2018a; López-Higes et al., 2018b; López-Higes et al., 2018). In the same line, Petrelli et al. (2014) and Petrelli et al. (2015) tested the NEUROvitalis program and Peña et al. (2014) the REHACOP Cognitive Training program in older adults with PD, and both found evidence of benefits in terms of memory.
Studies on Cognitive Training have significantly increased the possibility of delaying, improving, or reversing physiological changes related to the aging process (Lustig et al., 2009; Brinke et al., 2018). However, the results of Cognitive Training are controversial, as they differ in terms of transfer effects to ADL and gains in QoL and wellbeing. Gains in the global cognitive functioning are polemic and differ with the type of population studied. However, the transfer effect seems to depend on the training time (over 30 min), its frequency (limited to one to three times a week) (Lampit et al., 2015), the age of the participants and the type of tasks (attention and working memory) (Zajac-Lamparska and Trempała, 2016). Cognitive Training may become more efficient or effective when other components satisfy compensatory function needs (Kim and Kim, 2014), as it is not always enough on its own for older adults.
Enrichment
Some studies report the positive effect of an active lifestyle on improving overall cognitive functioning (Küster et al., 2016) in older adults without cognitive impairment or with MCI (Park and Park, 2018) and subjective memory impairments (McEwen et al., 2018). Enrichment refers to all activities (e.g., activity/cognitive, social, and physical stimulation) with a positive impact on cognitive functioning that enhance cognitive enrichment. It also comprises the implementation of motor, sensory, and cognitive stimuli in the person’s environment (Hertzog et al., 2008; Steinerman, 2010; Patel, 2012).
Different Enrichment methods are described in the literature. Linde and Alfermann (2014) developed an Enrichment intervention combining physical activity and cognitive intervention in healthy older adults. Brinke et al. (2018) applied the Fit Brains Program to older adults who received fit cognitive training, exercise and a combination of both. In the same line, Eggenberger et al. (2015) implemented a multicomponent physical exercise with simultaneous cognitive training of executive functions, episodic memory and processing speed in older adults. In turn, Best et al. (2018) combined physical, social, and cognitive enrichment using the Lumosity training program to improve cognitive function in chronic stroke. Candela et al. (2015) also applied physical activity together with the training of long-term memory and selective attention. Finally, Kalbe et al. (2018) used a specific approach involving cognitive training and physical activity with group counseling.
Enrichment can be implemented as a potential treatment for neurodegenerative diseases (Patel, 2012), after stroke (Best et al., 2018), or after traumatic brain injury (Bondi et al., 2014). Because this approach provides cognitive and physical stimulation at home, it favors an enriching environment for patients, benefiting their recovery. The older adults’ individual cognitively enriched behaviors (cognitive activity, physical exercise, among others) significantly impact their cognitive functioning improvement (Hertzog et al., 2008; Schmiedek et al., 2010).
Cognitive Stimulation
Another technique that prevents cognitive decline is Cognitive Stimulation, which involves engaging in activities (e.g., puzzles) to improve general and social cognitive functioning (Woods et al., 2012). This approach includes multiple group activities under a social environment and multisensory stimulation (Clare and Woods, 2004; Eckroth-Bucher and Siberski, 2009; Mowszowski et al., 2010; Steinerman, 2010; Gates and Sachdev, 2014; Kim and Kim, 2014; Kueider et al., 2014).
While Cognitive Training focuses on specific cognitive domains, Cognitive Stimulation consists of engaging patients in non-specific activities to produce improvements in general mental functioning (Miranda-Castillo et al., 2012; Bahar-Fuchs et al., 2013; Herrera et al., 2017). For example, in a population with AD, the first method aims to improve, or at least maintain, cognitive and social function, while the second tries to reduce cognitive impairment (Clare and Woods, 2004; Mowszowski et al., 2010; Kueider et al., 2014). In terms of results, a meta-analysis (Liang et al., 2019) confirmed that Cognitive Training is the ideal cognitive intervention to reduce cognitive decline in people with AD, while another meta-analysis (Lin et al., 2013) concluded that Cognitive Stimulation improves the global cognitive functioning in 6–12 months in people with mild cognitive deficit or dementia.
Cognitive stimulation is applied using both computer-based and other cognitively stimulating activities (e.g., museum visits). The literature shows the usefulness of mobile applications like iBeni (Martínez-Alcalá et al., 2018), the tablet application Stim’Art (Yasini and Marchand, 2016), or video game devices such as Actively Station (Ordonez et al., 2017) and Wizard-of-Woz (Dethlefs et al., 2017) in older adults. For persons with mild to moderate cognitive impairment, the Cognitive Stimulation KODRO software can be useful to train global cognitive function, executive functions, language, working memory, processing speed, and attention (Malvy, 2016; Djabelkhir et al., 2017; Djabelkhir-Jemmi et al., 2018). Other examples using this type of intervention are the Bike Labyrinth interactive virtual bike tours, used by Karssemeijer et al. (2019) in older adults with dementia, or the Road Sign Test computer training focused on processing speed in people with MCI (Valdés et al., 2019).
In turn, most Cognitive stimulation studies that did not include computerized tasks found gains on several cognitive domains in healthy older adults (Tranter and Koutstaal, 2008; Ferná ndez-Prado et al., 2012; De Oliveira et al., 2014; Suzuki et al., 2014; Zimmermann et al., 2014; Zon et al., 2016; Grimaud et al., 2017; Herrera et al., 2017; Young, 2020) and older adults with mild to moderate dementia (Spector et al., 2003; Woods et al., 2006; Moro et al., 2012; Yamanaka et al., 2013; Moro et al., 2015; Capotosto et al., 2017; Piras et al., 2017; Stewart et al., 2017; Young et al., 2019). This intervention has also been proved to reduce cognitive decline in people with AD (Vidovich et al., 2011; Miranda-Castillo et al., 2012). Other improvements were observed in apathy and depression symptomatology (Niu et al., 2010) and conversation and communication skills (Spector et al., 2010).
Cognitive Stimulation has also been combined with physical activity. Dannhauser et al. (2014) found that this combination benefited the working memory, physical health, and fitness of older adults with MCI. Thiel et al. (2012) demonstrated that Cognitive Stimulation and physical activity might prevent age-related cognitive decline.
These positive results can be explained by the fact that Cognitive Stimulation has excellent adherence and completion rates, reasonable costs and high experiential relevance to participants, as confirmed by Alves et al. (2014) in a study involving older adults with cognitive impairment. However, Cognitive Stimulation components are controversial among authors. On one hand, Kim and Kim (2014) reported that Cognitive Stimulation includes visual, sensory, auditory, motor or social, and deep brain stimulation. On the other hand, other authors (Clare and Woods, 2004; Mowszowski et al., 2010; Steinerman, 2010; Kueider et al., 2014) describe it as involving social activities aimed to reduce cognitive decline (Newson and Kemps, 2006), improving cognitive functioning, health and well-being (Tranter and Koutstaal, 2008; Yuill and Hollis, 2011; Woods et al., 2012; Toh et al., 2016; Castel et al., 2017). Others yet report that Cognitive Stimulation can facilitate the preservation of cognitive functions, improve them with a purpose (e.g., improving attention to improve driving), or reduce the effects of aging in neurological patients (Bigand and Tillmann, 2015; Capotosto et al., 2017; Djabelkhir et al., 2017; Martínez-Alcalá et al., 2018; Rosell, 2018). This intervention also provides a non-pharmacological approach for the recovery of brain and motor functions after a disease or brain injury (Bigand and Tillmann, 2015).
Brain Training
Brain Training is usually based on repeatedly using programs (“brain games”) focused on performance in cognitive tasks over a period of time to improve cognitive deficits. This type of intervention should include ADL such as video games, music, computerized training, or physical exercise (Rabipour and Raz, 2012; Heugten et al., 2016; Simons et al., 2016).
Some studies used Lumosity, a Brain Training platform, for the training of several cognitive domains. Ballesteros et al. (2015) and Ballesteros et al. (2017) conducted two studies focused on the effects of video games on the training of a set of cognitive functions in healthy older adults and observed improvements in the trained group in attention, working memory, processing speed, visual recognition memory, and well-being, compared to a control group. Mayas et al. (2014) also used Lumosity with older adults to train problem-solving, mental calculation, working memory, attention and confirmed the game training effects on reducing distraction and improving alertness. In turn, Nouchi et al. (2012) covered the effects of video game training with Brain Age and Tetris on executive functions and processing speed in a sample of older adults, and their results indicated transfer effects of the Brain Training game in the same cognitive domains.
Van de Ven et al. (2017) used several computerized tasks in older adults with cognitive impairment targeting executive functions, attention, reasoning, and psychomotor speed (www.braingymmer.com). Two other studies have used the Nintendo DS video games in older adults as a Brain Training method (Power et al., 2011; McDougall et al., 2012).
For some authors (McDougall and House, 2012), the older adults who benefit from Brain Training show improved perception of their cognitive functioning and QoL. However, even though there is evidence that Brain Training plays an important role in the improvement of cognitive functions, this intervention alone has no potential to achieve rehabilitation goals (namely, in functional terms) and should only be offered in combination with neuropsychological rehabilitation programs (Heugten et al., 2016).
Throughout our review, we found that the concept of Brain Training seems to be used more commercially and some researchers call it “cognitive training” (e.g., Buitenweg et al., 2017).
Cognitive Rehabilitation
Cognitive Rehabilitation is defined as a systematic and multidisciplinary process oriented to therapeutic activities. It can follow different approaches, namely: reinforcement and reestablishment of behavior patterns; creation of new patterns of cognitive activity through the compensation of neurological deficit mechanisms, and training of compensation strategies involving the learning of cognitive skills, memory techniques, problem-solving, concentration, and critical thinking; establishment of external compensation mechanisms or environmental structuring; and adaptation and understanding of current cognitive deficits (Cicerone et al., 2000).
This intervention is an individualized approach, i.e., developed based on each user’s goals, with a comprehensive view of individual difficulties (cognitive deficits, functional and behavioral problems, and real life). The planning and implementation of Cognitive Rehabilitation involve the person with the cognitive deficit, their family members, and a team of health professionals (Cicerone et al., 2000; Wilson, 2002; Clare et al., 2003; Mowszowski et al., 2010; Steinerman, 2010; Bahar-Fuchs et al., 2013; Kueider et al., 2014).
Cognitive Rehabilitation can be focused on several cognitive domains, namely attention, concentration, memory, perception, communication, reasoning, and planning (Cicerone et al., 2000; Stuss et al., 2007). It can be computer-based or administered in a paper and pencil format (LoPresti et al., 2004; Maggio et al., 2018). Cognitive Rehabilitation has different general objectives than Cognitive Training, despite having the same approach (e.g., teaching problem-solving strategies). Specifically, Cognitive Rehabilitation uses a compensatory approach, adjusted to each person’s goals, with an intervention aiming to improve cognitive and everyday life functioning both functional and behavioral.
Cognitive Rehabilitation has been applied in a very wide range of populations, such as patients with acquired brain injury for remediation of cognitive deficits (Cicerone et al., 2000; Cicerone et al., 2005; Gordon et al., 2006; Rees et al., 2007; Rohling et al., 2009), older adults with AD (Loewenstein et al., 2004), older adults with mild cognitive deficits (Mansbach et al., 2017), and older adults with dementia (Clare et al., 2019).
Regarding the population with cognitive deficits, Vanova et al. (2018) conducted a randomized controlled trial with follow-up involving adults with MCI and mild dementia who completed a computer and internet-based program (GRADIOR and ehcoBUTLER) and observed an improvement in cognition, mood, QoL, ADL, and quality of patient-career relationship. Jelcic et al. (2014) applied the same intervention adding teleconference technology (Skype) in older adults with AD compared to a group that had face-to-face/conventional rehabilitation and a third control group that underwent face-to-face unstructured Cognitive Stimulation (e.g., practicing manual skills, reading the newspaper), and concluded that Cognitive Rehabilitation via teleconferencing improved the global cognitive functioning and language (phonemic and semantic) of people with AD. In turn, Mansbach et al. (2017) applied a computer-assisted online Cognitive Rehabilitation module (Memory Match) to 43 older adults with mild cognitive deficits and achieved an improvement in global cognition, attention, and memory in the intervention group. Another study by Kurz et al. (2009), involving older adults with MCI and AD, comprised diverse Cognitive Rehabilitation activities, namely relaxation techniques, activity planning, self-assertiveness training, stress management, external memory aids, memory training, and motor exercises.
Fasilis et al. (2018) applied a virtual environment (Main Tasks) to a group of older adults with mild dementia to train working memory, attention, problem solving, motivation, organization, impulsivity and found a relative improvement in cognitive variables. Another study by Maggio et al. (2018), with a sample of older adults with PD, used a semi-immersive therapy (virtual scenarios) system for motor and Cognitive Rehabilitation of patients with neurological diseases—BTS Nirvana—and achieved greater improvement at cognitive functioning, executive, and visuospatial abilities.
In the healthy population, Levine et al. (2007) applied a Goal Management Training program to simulate real-life tasks in healthy older adults, and the results showed an improvement in performance and self-rated executive. Craik et al. (2007) applied a program for memory training to healthy older adults that did not include computerized tasks, and there were no effects of training on working memory, primary memory, and recognition memory.
Conclusion
To our knowledge, this is the first study to identify the various existing definitions, methods, and procedures, as well as the overlapping information regarding the cognitive intervention known including their discrepancies. This literature review aimed to discuss and characterize different types of cognitive intervention in older adults commonly reported in the relevant literature and determines what main factors may contribute to their efficacy and inefficacy. We have also seen some weaknesses in this field. Most of the studies considered (Supplementary Appendix S1) using computer-based training interventions for both healthy and neurocognitive disorders older adults, mild to moderate cognitive impairment, AD, or dementia. However, several studies did not include computerized tasks in the interventions involving healthy older adults and older adults with AD, PD, neurocognitive disorders, mild to moderate dementia, or MCI.
We also concluded that the presented studies show heterogeneity of methods regarding sample size and characteristics, outcome domains, duration and content of the intervention, number of individual treatment sessions, control condition, and main intervention. Moreover, some studies confuse certain concepts; for example, use the concept of Cognitive Stimulation or Enrichment for Cognitive Training. This inconsistency does not allow a concrete definition of the most effective intervention, its durability and the best format for older adults. Thus, it is necessary to harmonize the methodology of intervention applied to the study population.
Our conclusions should be interpreted considering some limitations. Firstly, our research was restricted to electronic databases via EBSCO (although these are the most representative and significant in the field at hand). Secondly, our attempt to contact authors and experts to access some unavailable studies was not altogether successful, but we believe that this is unlikely to have determinatively influenced our findings. Lastly, due to rigorous research with strict inclusion/exclusion criteria, we gathered a restricted pool of analyzed papers (168 studies included from 641 full-text articles assessed for eligibility). Despite these limitations, the current review allows us to find some answers to our initial research questions.
We also consider that our main purpose was achieved since a conceptualization of cognitive interventions for healthy and older adults with several types of cognitive impairments was possible. Nevertheless, a few questions remain for additional research to further enhance this non-pharmacological approach involving the elderly. In future researches, we suggest a comprehensive view to discuss the methodology of each type of intervention presented in this research and subsequently demonstrate its results and efficacy (or not) in specific older-adult populations (e.g., healthy older adults, people with different levels of cognitive decline), comparing different approaches, namely computer-based interventions and applications without computerized tasks. We also cogitate that additional studies are further needed that highlight the durability of the observed gains (or not), the transfer effects for daily functioning and well-being, the probability and risk of developing cognitive morbidity.
Statements
Author contributions
LM and JO contributed to literature review and organized the database. LM wrote the first draft of the manuscript. LM, JO, FB, and MC-B contributed to manuscript revision, read, and approved the submitted version.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was funded by the Portuguese Foundation for Science and Technology: FCT/UIDB/4950/Base/2020 and FCT/UIDP/4950/Programatico/2020.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fragi.2022.844725/full#supplementary-material
References
1
Alves J. Alves-Costa F. Magalhães R. Gonçalves Ó. F. Sampaio A. (2014). Cognitive Stimulation for Portuguese Older Adults with Cognitive Impairment. Am. J. Alzheimers Dis. Other Demen.29 (6), 503–512. 10.1177/1533317514522541
2
Alves J. Magalhães R. Machado A. Gonçalves O. F. Sampaio A. Petrosyan A. (2013). Non-pharmacological Cognitive Intervention for Aging and Dementia: Current Perspectives. Wjcc1 (8), 233–241. 10.12998/wjcc.v1.i8.233
3
Amieva H. Robert P. H. Grandoulier A.-S. Meillon C. De Rotrou J. Andrieu S. et al (2016). Group and Individual Cognitive Therapies in Alzheimer's Disease: the ETNA3 Randomized Trial. Int. Psychogeriatr.28 (5), 707–717. 10.1017/s1041610215001830
4
Auffray C. Juhel J. (2001). Effets généraux et différentiels d'un programme d'entraînement cognitif multimodal chez la personne âgée. psy101 (1), 65–89. 10.3406/psy.2001.29716
5
Bahar-Fuchs A. Clare L. Woods B. (2013). Cognitive Training and Cognitive Rehabilitation for Mild to Moderate Alzheimer's Disease and Vascular Dementia. Cochrane Database Syst. Rev.6, CD003260. 10.1002/14651858.CD003260.pub2
6
Ball K. Berch D. B. Helmers K. F. Jobe J. B. Leveck M. D. Marsiske M. et al (2002). Effects of Cognitive Training Interventions with Older AdultsEffects of Cognitive Training Interventions with Older Adults: a Randomized Controlled Trial. JAMA288 (18), 2271–2281. 10.1001/jama.288.18.2271
7
Ball K. Edwards J. D. Ross L. A. McGwin Jr. G. (2010). Cognitive Training Decreases Motor Vehicle Collision Involvement of Older Drivers. J. Am. Geriatr. Soc.58 (11), 2107–2113. 10.1111/j.1532-5415.2010.03138.x
8
Ball K. K. Ross L. A. Roth D. L. Edwards J. D. (2013). Speed of Processing Training in the ACTIVE Study: How Much Is Needed and Who Benefits?J. Aging Health25 (80), 65S–84S. 10.1177/0898264312470167
9
Ballesteros S. Mayas J. Prieto A. Toril P. Pita C. Laura P. d. L. et al (2015). A Randomized Controlled Trial of Brain Training with Non-action Video Games in Older Adults: Results of the 3-month Follow-Up. Front. Aging Neurosci.7, 45. 10.3389/fnagi.2015.00045
10
Ballesteros S. Mayas J. Ruiz-Marquez E. Prieto A. Toril P. Ponce de Leon L. et al (2017). Effects of Video Game Training on Behavioral and Electrophysiological Measures of Attention and Memory: Protocol for a Randomized Controlled Trial. JMIR Res. Protoc.6 (1), e8. 10.2196/resprot.6570
11
Barnes D. E. Yaffe K. Belfor N. Jagust W. J. DeCarli C. Reed B. R. et al (2009). Computer-based Cognitive Training for Mild Cognitive Impairment. Alzheimer Dis. Associated Disord.23 (3), 205–210. 10.1097/wad.0b013e31819c6137
12
Basak C. Boot W. R. Voss M. W. Kramer A. F. (2008). Can Training in a Real-Time Strategy Video Game Attenuate Cognitive Decline in Older Adults?Psychol. Aging23 (4), 765–777. 10.1037/a0013494
13
Bellander M. Eschen A. Lövdén M. Martin M. Bäckman L. Brehmer Y. (2017). No Evidence for Improved Associative Memory Performance Following Process-Based Associative Memory Training in Older Adults. Front. Aging Neurosci.8 (326), 1–11. 10.3389/fnagi.2016.00326
14
Belleville S. Gilbert B. Fontaine F. Gagnon L. Ménard É. Gauthier S. (2006). Improvement of Episodic Memory in Persons with Mild Cognitive Impairment and Healthy Older Adults: Evidence from a Cognitive Intervention Program. Dement Geriatr. Cogn. Disord.22, 486–499. 10.1159/000096316
15
Best J. R. Eng J. J. Davis J. C. Hsiung R. Hall P. A. Middleton L. E. et al (2018). Study Protocol for Vitality: A Proof-Of-Concept Randomised Controlled Trial of Exercise Training or Complex Mental and Social Activities to Promote Cognition in Adults with Chronic Stroke. BMJ Open8 (3), e021490. 10.1136/bmjopen-2018-021490
16
Bigand E. Tillmann B. (2015). “Introduction to the Neurosciences and Music V: Cognitive Stimulation and Rehabilitation,” in Annals of the New York Academy of Sciences. New York: John Wiley and Sons, 1337, vii–ix. 10.1111/nyas.12732
17
Binder J. C. Martin M. Zöllig J. Röcke C. Mérillat S. Eschen A. et al (2016). Multi-domain Training Enhances Attentional Control. Psychol. Aging31 (4), 390–408. 10.1037/pag0000081
18
Bondi C. O. Klitsch K. C. Leary J. B. Kline A. E. (2014). Environmental Enrichment as a Viable Neurorehabilitation Strategy for Experimental Traumatic Brain Injury. J. Neurotrauma31, 873–888. 10.1089/neu.2014.3328
19
Borella E. Carretti B. Riboldi F. De Beni R. (2010). Working Memory Training in Older Adults: Evidence of Transfer and Maintenance Effects. Psychol. Aging25 (4), 767–778. 10.1037/a0020683
20
Brum P. S. Borella E. Carretti B. Sanches Yassuda M. (2020). Verbal Working Memory Training in Older Adults: an Investigation of Dose Response. Aging Ment. Health24 (1), 81–91. 10.1080/13607863.2018.1531372
21
Buitenweg J. Van de Ven R. Prinssen S. Murre J. Ridderinkhof K. (2017). Cognitive Flexibility Training: A Large-Scale Multimodal Adaptive Active-Control Intervention Study in Healthy Older Adults. Front. Hum. Neurosci.11 (529), 1–14. 10.3389/fnhum.2017.00529
22
Candela F. Zucchetti G. Magistro D. Rabaglietti E. (2015). The Effects of a Physical Activity Program and a Cognitive Training Program on the Long-Term Memory and Selective Attention of Older Adults: A Comparative Study. Activities, Adaptation & Aging39 (1), 77–91. 10.1080/01924788.2014.977191
23
Cantarella A. Borella E. Carretti B. Kliegel M. de Beni R. (2017). Benefits in Tasks Related to Everyday Life Competences after a Working Memory Training in Older Adults. Int. J. Geriatr. Psychiatry32, 86–93. 10.1002/gps.4448
24
Capotosto E. Belacchi C. Gardini S. Faggian S. Piras F. Mantoan V. et al (2017). Cognitive Stimulation Therapy in the Italian Context: its Efficacy in Cognitive and Non‐cognitive Measures in Older Adults with Dementia. Int. J. Geriatr. Psychiatry32 (3), 331–340. 10.1002/gps.4521
25
Carretti B. Borella E. Zavagnin M. de Beni R. (2013). Gains in Language Comprehension Relating to Working Memory Training in Healthy Older Adults. Int. J. Geriatr. Psychiatry28, 539–546. 10.1002/gps.3859
26
Castel A. Lluch C. Ribas J. Borràs L. Moltó E. (2017). Effects of a Cognitive Stimulation Program on Psychological Well-Being in a Sample of Elderly Long-Term Care Hospital Inpatients. Aging Ment. Health21 (1), 88–94. 10.1080/13607863.2015.1099033
27
Chaikham A. Putthinoi S. Lersilp S. Bunpun A. Chakpitak N. (2016). Cognitive Training Program for Thai Older People with Mild Cognitive Impairment. Proced. Environ. Sci.36, 42–45. 10.1016/j.proenv.2016.09.007
28
Chan M. Y. Haber S. Drew L. M. Park D. C. (2016). Training Older Adults to Use Tablet Computers: Does it Enhance Cognitive Function?Geront56 (3), 475–484. 10.1093/geront/gnu057
29
Chen B. Wei Y. Deng W. Sun S. (2018). The Effects of Cognitive Training on Cognitive Abilities and Everyday Function: A 10-week Randomized Controlled Trial. Int. J. Aging Hum. Dev.86 (1), 69–81. 10.1177/0091415017697725
30
Cheng Y. Wu W. Feng W. Wang J. Chen Y. Shen Y. et al (2012). The Effects of Multi-Domain versus Single-Domain Cognitive Training in Non-demented Older People: a Randomized Controlled Trial. BMC Med.10, 30. 10.1186/1741-7015-10-30
31
Choi K.-H. Kang J. Kim S.-M. Lee S.-H. Park S.-C. Lee W.-H. et al (2018). Cognitive Remediation in Middle-Aged or Older Inpatients with Chronic Schizophrenia: A Randomized Controlled Trial in Korea. Front. Psychol.8, 2364. 10.3389/fpsyg.2017.02364
32
Cicerone K. D. Dahlberg C. Kalmar K. Langenbahn D. M. Malec J. F. Bergquist T. F. et al (2000). Evidence-based Cognitive Rehabilitation: Recommendations for Clinical Practice. Arch. Phys. Med. Rehabil.81 (12), 1596–1615. 10.1053/apmr.2000.19240
33
Cicerone K. D. Dahlberg C. Malec J. F. Langenbahn D. M. Felicetti T. Kneipp S. et al (2005). Evidence-based Cognitive Rehabilitation: Updated Review of the Literature from 1998 through 2002. Arch. Phys. Med. Rehabil.86 (8), 1681–1692. 10.1016/j.apmr.2005.03.024
34
Clare L. Woods R. T. Moniz Cook E. D. Orrell M. Spector A. (2003). Cognitive Rehabilitation and Cognitive Training for Early-Stage Alzheimer's Disease and Vascular Dementia. Cochrane Database Syst. Rev. (4), CD003260. 10.1002/14651858.CD003260
35
Clare L. Kudlicka A. Oyebode J. R. Jones R. W. Bayer A. Leroi I. et al (2019). Individual Goal‐oriented Cognitive Rehabilitation to Improve Everyday Functioning for People with Early‐stage Dementia: A Multicentre Randomised Controlled Trial (The GREAT Trial). Int. J. Geriatr. Psychiatry34 (5), 709–721. 10.1002/gps.5076
36
Clare L. Woods R. T. (2004). Cognitive Training and Cognitive Rehabilitation for People with Early-Stage Alzheimer's Disease: A Review. Neuropsychological Rehabil.14 (4), 385–401. 10.1080/09602010443000074
37
Cohen-Mansfield J. Cohen R. Buettner L. Eyal N. Jakobovits H. Rebok G. et al (2015). Interventions for Older Persons Reporting Memory Difficulties: a Randomized Controlled Pilot Study. Int. J. Geriatr. Psychiatry30 (5), 478–486. 10.1002/gps.4164
38
Craik F. I. Winocur G. Palmer H. Binns M. A. Edwards M. Bridges K. et al (2007). Cognitive Rehabilitation in the Elderly: Effects on Memory. J. Int. Neuropsychol. Soc.13 (1), 132–142. 10.1017/S1355617707070166
39
Dannhauser T. M. Cleverley M. Whitfield T. J. Fletcher B. Stevens T. Walker Z. (2014). A Complex Multimodal Activity Intervention to Reduce the Risk of Dementia in Mild Cognitive Impairment-ThinkingFit: Pilot and Feasibility Study for a Randomized Controlled Trial. BMC psychiatry14, 129. 10.1186/1471-244x-14-129
40
De Luca R. Bramanti A. De Cola M. C. Leonardi S. Torrisi M. Aragona B. et al (2016). Cognitive Training for Patients with Dementia Living in a Sicilian Nursing home: a Novel Web-Based Approach. Neurol. Sci.37 (10), 1685–1691. 10.1007/s10072-016-2659-x
41
De Oliveira T. C. Soares F. C. De Macedo L. D. Diniz D. L. Bento-Torres N. V. Picanço-Diniz C. W. (2014). Beneficial Effects of Multisensory and Cognitive Stimulation on Age-Related Cognitive Decline in Long-Term-Care Institutions. Clin. Interv. Aging9, 309–320. 10.2147/CIA.S54383
42
Dethlefs N. Milders M. Cuayáhuitl H. Al-Salkini T. Douglas L. (2017). A Natural Language-Based Presentation of Cognitive Stimulation to People with Dementia in Assistive Technology: A Pilot Study. Inform. Health Soc. Care42 (4), 349–360. 10.1080/17538157.2016.1255627
43
Djabelkhir L. Wu Y. H. Vidal J. S. Cristancho-Lacroix V. Marlats F. Lenoir H. et al (2017). Computerized Cognitive Stimulation and Engagement Programs in Older Adults with Mild Cognitive Impairment: Comparing Feasibility, Acceptability, and Cognitive and Psychosocial Effects. Clin. Interv. Aging12, 1967–1975. 10.2147/CIA.S145769
44
Djabelkhir-Jemmi L. Wu Y.-H. Boubaya M. Marlats F. Lewis M. Vidal J.-S. et al (2018). Differential Effects of a Computerized Cognitive Stimulation Program on Older Adults with Mild Cognitive Impairment According to the Severity of white Matter Hyperintensities. CiaVol. 13, 1543–1554. 10.2147/cia.s152225
45
Drag L. L. Bieliauskas L. A. (2010). Contemporary Review 2009: Cognitive Aging. J. Geriatr. Psychiatry Neurol.23 (2), 75–93. 10.1177/0891988709358590
46
Duda B. M. Sweet L. H. (2020). Functional Brain Changes Associated with Cognitive Training in Healthy Older Adults: A Preliminary ALE Meta-Analysis. Brain Imaging Behav.14 (4), 1247–1262. 10.1007/s11682-019-00080-0
47
Eckroth-Bucher M. Siberski J. (2009). Preserving Cognition through an Integrated Cognitive Stimulation and Training Program. Am. J. Alzheimers Dis. Other Demen.24 (3), 234–245. 10.1177/1533317509332624
48
Eggenberger P. Schumacher V. Angst M. Theill N. de Bruin E. D. (2015). Does Multicomponent Physical Exercise with Simultaneous Cognitive Training Boost Cognitive Performance in Older Adults? A 6-month Randomized Controlled Trial with a 1-year Follow-Up. Clin. Interv. Aging10, 1335–1349. 10.2147/CIA.S87732
49
Farina E. Mantovani F. Fioravanti R. Pignatti R. Chiavari L. Imbornone E. et al (2006). Evaluating Two Group Programmes of Cognitive Training in Mild-To-Moderate AD: Is There Any Difference between a 'global' Stimulation and a 'cognitive-specific' One?Aging Ment. Health10 (3), 211–218. 10.1080/13607860500409492
50
Fasilis T. Patrikelis P. Patrikelis P. Siatouni A. Alexoudi A. Veretzioti A. et al (2018). A Pilot Study and Brief Overview of Rehabilitation via Virtual Environment in Patients Suffering from Dementia. Psychiatriki29 (1), 42–51. 10.22365/jpsych.2018.291.42
51
Fellman D. Salmi J. Ritakallio L. Ellfolk U. Rinne J. O. Laine M. (2020). Training Working Memory Updating in Parkinson's Disease: A Randomised Controlled Trial. Neuropsychological Rehabil.30 (4), 673–708. 10.1080/09602011.2018.1489860
52
Feng W. Li C. Chen Y. Cheng Y. Wu W. (2014). Five-year Follow-Up Study of Multi-Domain Cognitive Training for Healthy Elderly Community Members. Shanghai Arch. Psychiatry26 (1), 30–41. 10.3969/j.issn.1002-0829.2014.01.005
53
Fernández-Prado S. Conlon S. Mayán-Santos J. M. Gandoy-Crego M. (2012). The Influence of a Cognitive Stimulation Program on the Quality of Life Perception Among the Elderly. Arch. Gerontol. Geriatr.54 (1), 181–184. 10.1016/j.archger.2011.03.003
54
Finn M. McDonald S. (2011). Computerised Cognitive Training for Older Persons with Mild Cognitive Impairment: A Pilot Study Using a Randomised Controlled Trial Design. Brain Impairment12 (3), 187–199. 10.1375/brim.12.3.187
55
Frankenmolen N. L. Overdorp E. J. Fasotti L. Claassen J. A. H. R. Kessels R. P. C. Oosterman J. M. (2018). Memory Strategy Training in Older Adults with Subjective Memory Complaints: A Randomized Controlled Trial. J. Int. Neuropsychol. Soc.24 (10), 1110–1120. 10.1017/s1355617718000619
56
Garcia-Campuzano M. T. Virues-Ortega J. Smith S. Moussavi Z. (2013). Effect of Cognitive Training Targeting Associative Memory in the Elderly: a Small Randomized Trial and a Longitudinal Evaluation. J. Am. Geriatr. Soc.61 (12), 2252–2254. 10.1111/jgs.12574
57
Gates N. J. Rutjes A. W. Di Nisio M. Karim S. Chong L. Y. March E. et al (2019). Computerised Cognitive Training for Maintaining Cognitive Function in Cognitively Healthy People in Late Life. Cochrane Database Syst. Rev.3 (3), CD012277. 10.1002/14651858.CD012277.pub2
58
Gates N. J. Sachdev P. (2014). Is Cognitive Training an Effective Treatment for Preclinical and Early Alzheimer's Disease?J. Alzheimers Dis.42 Suppl 4 (Suppl. 4), S551–S559. 10.3233/JAD-141302
59
Gigler K. L. Blomeke K. Shatil E. Weintraub S. Reber P. J. (2013). Preliminary Evidence for the Feasibility of at-home Online Cognitive Training with Older Adults. Gerontechnology12 (1), 26–35. 10.4017/gt.2013.12.1.007.00
60
Giuli C. Papa R. Lattanzio F. Postacchini D. (2016). The Effects of Cognitive Training for Elderly: Results from My Mind Project. Rejuvenation Res.19 (6), 485–494. 10.1089/rej.2015.1791
61
Goghari V. M. Lawlor-Savage L. (2018). Self-Perceived Benefits of Cognitive Training in Healthy Older Adults. Front. Aging Neurosci.10 (112), 112–210. 10.3389/fnagi.2018.00112
62
Golino M. T. S. Flores Mendoza C. Golino H. F. (2017). Effects of Cognitive Training on Cognitive Performance of Healthy Older Adults. Span. J. Psychol.20, E39. 10.1017/sjp.2017.38
63
González-Palau F. Franco M. Bamidis P. Losada R. Parra E. Papageorgiou S. G. et al (2014). The Effects of a Computer-Based Cognitive and Physical Training Program in a Healthy and Mildly Cognitive Impaired Aging Sample. Aging Ment. Health18 (7), 838–846. 10.1080/13607863.2014.899972
64
González-Palau F. Franco M. Toribio J. Losada R. Parra E. Bamidis P. (2013). Designing a Computer-Based Rehabilitation Solution for Older Adults: The Importance of Testing Usability. PsychNology J.11 (2), 119–136.
65
Gooding A. L. Choi J. Fiszdon J. M. Wilkins K. Kirwin P. D. Van Dyck C. H. et al (2015). Comparing Three Methods of Computerised Cognitive Training for Older Adults with Subclinical Cognitive Decline. Neuropsychol. Rehabil.26 (5-6), 810–821. 10.1080/09602011.2015.1118389
66
Gordon W. A. Cantor J. Ashman T. Brown M. (2006). Treatment of Post-TBI Executive Dysfunction. J. Head Trauma Rehabil.21 (2), 156–167. 10.1097/00001199-200603000-00008
67
Greenaway M. C. Duncan N. L. Smith G. E. (2013). The Memory Support System for Mild Cognitive Impairment: Randomized Trial of a Cognitive Rehabilitation Intervention. Int. J. Geriatr. Psychiatry28 (4), 402–409. 10.1002/gps.3838
68
Grimaud É. Taconnat L. Clarys D. (2017). Cognitive Stimulation in Healthy Older Adults: a Cognitive Stimulation Program Using Leisure Activities Compared to a Conventional Cognitive Stimulation Program. Gériatrie Psychol. Neuropsychiatrie du Vieillissement15 (2), 214–223. 10.1684/pnv.2017.0669
69
Grönholm-Nyman P. Soveri A. Rinne J. O. Ek E. Nyholm A. Stigsdotter Neely A. et al (2017). Limited Effects of Set Shifting Training in Healthy Older Adults. Front. Aging Neurosci.9 (69), 69–21. 10.3389/fnagi.2017.00069
70
Gross A. L. Rebok G. W. Unverzagt F. W. Willis S. L. Brandt J. (2011). Cognitive Predictors of Everyday Functioning in Older Adults: Results from the Active Cognitive Intervention Trial. Journals Gerontol. Ser. B: Psychol. Sci. Soc. Sci.66B (5), 557–566. 10.1093/geronb/gbr033
71
Günther V. Schäfer P. Holzner B. Kemmler G. (2003). Long-term Improvements in Cognitive Performance through Computer-Assisted Cognitive Training: A Pilot Study in a Residential home for Older People. Aging Ment. Health7 (3), 200–206. 10.1080/1360786031000101175
72
Hedden T. Gabrieli J. D. E. (2004). Insights into the Ageing Mind: a View from Cognitive Neuroscience. Nat. Rev. Neurosci.5 (2), 87–96. 10.1038/nrn1323
73
Herrera C. Chambon C. Michel B. F. Paban V. Alescio-Lautier B. (2012). Positive Effects of Computer-Based Cognitive Training in Adults with Mild Cognitive Impairment. Neuropsychologia50, 1871–1881. 10.1016/j.neuropsychologia.2012.04.012
74
Hertzog C. Kramer A. F. Wilson R. S. Lindenberger U. (2008). Enrichment Effects on Adult Cognitive Development. Psychol. Sci. Public Interest9 (1), 1–65. 10.1111/j.1539-6053.2009.01034.x
75
Huckans M. Hutson L. Twamley E. Jak A. Kaye J. Storzbach D. (2013). Efficacy of Cognitive Rehabilitation Therapies for Mild Cognitive Impairment (MCI) in Older Adults: Working toward a Theoretical Model and Evidence-Based Interventions. Neuropsychol. Rev.23 (1), 63–80. 10.1007/s11065-013-9230-9
76
Irigaray T. Filho I. Schneider R. (2012). Efeitos de um treino de atenção, memória e funções executivas na cognição de idosos saudáveis. Psicologia: Reflexão e Crítica25 (1), 188–202. 10.1590/s0102-79722012000100023
77
Irigaray T. Q. Schneider R. H. Gomes I. (2011). Efeitos de um treino cognitivo na qualidade de vida e no bem-estar psicológico de idosos. Psicol. Reflex. Crit.24 (4), 810–818. 10.1590/s0102-79722011000400022
78
Jackson J. J. Hill P. L. Payne B. R. Roberts B. W. Stine-Morrow E. A. L. (2012). Can an Old Dog Learn (And Want to Experience) New Tricks? Cognitive Training Increases Openness to Experience in Older Adults. Psychol. Aging27 (2), 286–292. 10.1037/a0025918
79
Jelcic N. Agostini M. Meneghello F. Bussè C. Parise S. Galano A. et al (2014). Feasibility and Efficacy of Cognitive Telerehabilitation in Early Alzheimer's Disease: a Pilot Study. Clin. Interv. Aging9, 1605–1611. 10.2147/CIA.S68145
80
Jones R. N. Marsiske M. Ball K. Rebok G. Willis S. L. Morris J. N. et al (2013). The ACTIVE Cognitive Training Interventions and Trajectories of Performance Among Older Adults. J. Aging Health25 (0), 186S–208S. 10.1177/0898264312461938
81
Kalbe E. Roheger M. Paluszak K. Meyer J. Becker J. Fink G. R. et al (2018). Effects of a Cognitive Training with and without Additional Physical Activity in Healthy Older Adults: A Follow-Up 1 Year after a Randomized Controlled Trial. Front. Aging Neurosci.10, 407. 10.3389/fnagi.2018.00407
82
Kanaan S. F. McDowd J. M. Colgrove Y. Burns J. M. Gajewski B. Pohl P. S. (2014). Feasibility and Efficacy of Intensive Cognitive Training in Early-Stage Alzheimer's Disease. Am. J. Alzheimers Dis. Other Demen.29 (2), 150–158. 10.1177/1533317513506775
83
Karssemeijer E. G. A. Aaronson J. A. Bossers W. J. R. Donders R. Olde Rikkert M. G. M. Kessels R. P. C. (2019). The Quest for Synergy between Physical Exercise and Cognitive Stimulation via Exergaming in People with Dementia: a Randomized Controlled Trial. Alz Res. Ther.11 (1), 3. 10.1186/s13195-018-0454-z
84
Kim E. Y. Kim K. W. (2014). A Theoretical Framework for Cognitive and Non-cognitive Interventions for Older Adults: Stimulation versus Compensation. Aging Ment. Health18 (3), 304–315. 10.1080/13607863.2013.868404
85
Koltai D. Welsh-Bohmer K. Schmechel D. (2001). Influence of Anosognosia on Treatment Outcome Among Dementia Patients. Neuropsychological Rehabil.11 (3-4), 455–475. 10.1080/09602010042000097
86
Kueider A. Bichay K. Rebok G. (2014). “Cognitive Training for Older Adults: What Is it and Does it Work?,” in Center on Aging at American Institutes for Research. Washington: American Institutes for Research, 1–8.
87
Kuo C. Y. Huang Y. M. Yeh Y. Y. (2018). Let's Play Cards: Multi-Component Cognitive Training with Social Engagement Enhances Executive Control in Older Adults. Front. Psychol.9 (2482), 2482. 10.3389/fpsyg.2018.02482
88
Kurz A. Pohl C. Ramsenthaler M. Sorg C. (2009). Cognitive Rehabilitation in Patients with Mild Cognitive Impairment. Int. J. Geriat. Psychiatry24, 163–168. 10.1002/gps.2086
89
Küster O. C. Fissler P. Laptinskaya D. Thurm F. Scharpf A. Woll A. et al (2016). Cognitive Change Is More Positively Associated with an Active Lifestyle Than with Training Interventions in Older Adults at Risk of Dementia: A Controlled Interventional Clinical Trial. BMC Psychiatry16 (315), 315. 10.1186/s12888-016-1018-z
90
Kwok T. Wong A. Chan G. Shiu Y. Y. Lam K. C. Young D. et al (2013). Effectiveness of Cognitive Training for Chinese Elderly in Hong Kong. Cia8, 213–219. 10.2147/cia.s38070
91
Lampit A. Valenzuela M. Gates N. J. (2015). Computerized Cognitive Training Is Beneficial for Older Adults. J. Am. Geriatr. Soc.63 (12), 2610–2612. 10.1111/jgs.13825
92
Lee G. J. Bang H. J. Lee K. M. Kong H. H. Seo H. S. Oh M. et al (2018). A Comparison of the Effects between 2 Computerized Cognitive Training Programs, Bettercog and COMCOG, on Elderly Patients with MCI and Mild Dementia: A Single-Blind Randomized Controlled Study. Medicine (Baltimore)97 (45), e13007. 10.1097/MD.0000000000013007
93
Lee Y. (2000). The Predictive Value of Self Assessed General, Physical, and Mental Health on Functional Decline and Mortality in Older Adults. J. Epidemiol. Community Health54 (2), 123–129. 10.1136/jech.54.2.123
94
Lenze E. J. Bowie C. R. (2018). Cognitive Training for Older Adults: What Works?J. Am. Geriatr. Soc.66 (4), 645–647. 10.1111/jgs.15230
95
Leung N. T. Y. Tam H. M. K. Chu L. W. Kwok T. C. Y. Chan F. Lam L. C. W. et al (2015). Neural Plastic Effects of Cognitive Training on Aging Brain. Neural Plasticity2015, 535618. 10.1155/2015/535618
96
Levine B. Stuss D. T. Winocur G. Binns M. A. Fahy L. Mandic M. et al (2007). Cognitive Rehabilitation in the Elderly: Effects on Strategic Behavior in Relation to Goal Management. J. Int. Neuropsychol. Soc.13 (1), 143–152. 10.1017/S1355617707070178
97
Li B. Zhu X. Hou J. Chen T. Wang P. Li J. (2016). Combined Cognitive Training vs. Memory Strategy Training in Healthy Older Adults. Front. Psychol.7, 834. 10.3389/fpsyg.2016.00834
98
Liang J.-H. Li J.-Y. Jia R.-X. Wang Y.-Q. Wu R.-K. Zhang H.-B. et al (2019). Comparison of Cognitive Intervention Strategies for Older Adults with Mild to Moderate Alzheimer's Disease: A Bayesian Meta-Analytic Review. J. Am. Med. Directors Assoc.20 (3), 347–355. 10.1016/j.jamda.2018.09.017
99
Lin J. S. O'Connor E. Rossom R. C. Perdue L. A. Eckstrom E. (2013). Screening for Cognitive Impairment in Older Adults: A Systematic Review for the U.S. Preventive Services Task Force. Ann. Intern. Med.159 (9), 601–612. 10.7326/0003-4819-159-9-201311050-00730
100
Linde K. Alfermann D. (2014). Single versus Combined Cognitive and Physical Activity Effects on Fluid Cognitive Abilities of Healthy Older Adults: a 4-month Randomized Controlled Trial with Follow-Up. J. Aging Phys. activity22 (3), 302–313. 10.1123/japa.2012-0149
101
Loewenstein D. A. Acevedo A. Czaja S. J. Duara R. (2004). Cognitive Rehabilitation of Mildly Impaired Alzheimer Disease Patients on Cholinesterase Inhibitors. Am. J. Geriatr. Psychiatry12 (4), 395–402. 10.1097/00019442-200407000-00007
102
Lopes R. M. F. Argimon I. I. d. L. (2016). El entrenamiento cognitivo en los ancianos y efectos en las funciones ejecutivas. Act.Colom.Psicol.19 (2), 159–176. 10.14718/acp.2016.19.2.8
103
López-Higes R. Martín-Aragoneses M. Rubio-Valdehita S. Delgado-Losada M. Montejo P. Montenegro M. et al (2018a). Efficacy of Cognitive Training in Older Adults with and without Subjective Cognitive Decline Is Associated with Inhibition Efficiency and Working Memory Span, Not with Cognitive reserve. Front. Aging Neurosci.10 (23).
104
López-Higes R. Prados J. Rubio-Valdehita S. Rodríguez-Rojo I. Frutos-Lucas J. Montenegro M. et al (2018b). Factors Explaining Language Performance after Training in Elders with and without Subjective Cognitive Decline. Front. Aging Neurosci.10 (264).
105
LoPresti E. F. Mihailidis A. Kirsch N. (2004). Assistive Technology for Cognitive Rehabilitation: State of the Art. Neuropsychological Rehabil.14 (1/2), 5–39. 10.1080/09602010343000101
106
Lustig C. Shah P. Seidler R. Reuter-Lorenz P. A. (2009). Aging, Training, and the Brain: A Review and Future Directions. Neuropsychol. Rev.19 (4), 504–522. 10.1007/s11065-009-9119-9
107
Maggio M. G. De Cola M. C. Latella D. Maresca G. Finocchiaro C. La Rosa G. et al (2018). What about the Role of Virtual Reality in Parkinson Disease's Cognitive Rehabilitation? Preliminary Findings from a Randomized Clinical Trial. J. Geriatr. Psychiatry Neurol.31 (6), 312–318. 10.1177/0891988718807973
108
Malvy L. (2016). Bénéfice de l'utilisation d'un programme de stimulation cognitive sur tablettes tactiles chez des personnes âgées dépendantes et institutionnalisées : programme KODRO. NPG Neurologie - Psychiatrie - Gériatrie16, 344–352. 10.1016/j.npg.2016.02.006
109
Mansbach W. E. Mace R. A. Clark K. M. (2017). The Efficacy of a Computer-Assisted Cognitive Rehabilitation Program for Patients with Mild Cognitive Deficits: A Pilot Study. Exp. Aging Res.43 (1), 94–104. 10.1080/0361073x.2017.1258256
110
Margrett J. A. Willis S. L. (2006). In-home Cognitive Training with Older Married Couples: Individual versus Collaborative Learning. Aging Neuropsychol. CognitionSection B, Aging Neuropsychol. Cogn.13 (2), 173–195. 10.1080/138255890969285
111
Martínez-Alcalá C. Rosales-Lagarde A. Hernández-Alonso E. Melchor-Agustin R. Rodriguez-Torres E. Itzá-Ortiz B. (2018). A mobile App (iBeni) with a Neuropsychological Basis for Cognitive Stimulation for Elderly Adults: Pilot and Validation Study. JMIR Res. Protoc.7 (8), e172. 10.2196/resprot.9603
112
Marusic U. Giordani B. Moffat S. D. Petrič M. Dolenc P. Pišot R. et al (2018). Computerized Cognitive Training during Physical Inactivity Improves Executive Functioning in Older Adults. Aging Neuropsychol. Cogn.25 (1), 49–69. 10.1080/13825585.2016.1263724
113
Maseda A. Millán-Calenti J. C. Lorenzo-López L. Núñez-Naveira L. (2013). Efficacy of a Computerized Cognitive Training Application for Older Adults with and without Memory Impairments. Aging Clin. Exp. Res.25 (4), 411–419. 10.1007/s40520-013-0070-5
114
Matysiak O. Kroemeke A. Brzezicka A. (2019). Working Memory Capacity as a Predictor of Cognitive Training Efficacy in the Elderly Population. Front. Aging Neurosci.11 (126), 126. 10.3389/fnagi.2019.00126
115
Mayas J. Parmentier F. B. R. Andrés P. Ballesteros S. (2014). Plasticity of Attentional Functions in Older Adults after Non-action Video Game Training: a Randomized Controlled Trial. PLoS One9 (3), e92269. 10.1371/journal.pone.0092269
116
McDougall S. House B. (2012). Brain Training in Older Adults: Evidence of Transfer to Memory Span Performance and Pseudo-matthew Effects. Neuropsychol. Dev. Cogn. B Aging Neuropsychol. Cogn.19 (1-2), 195–221. 10.1080/13825585.2011.640656
117
McEwen S. C. Siddarth P. Abedelsater B. Kim Y. Mui W. Wu P. et al (2018). Simultaneous Aerobic Exercise and Memory Training Program in Older Adults with Subjective Memory Impairments. Jad62 (2), 795–806. 10.3233/jad-170846
118
Medalia A. Revheim N. Casey M. (2002). Remediation of Problem-Solving Skills in Schizophrenia: Evidence of a Persistent Effect. Schizophr Res.57 (2-3), 165–171. 10.1016/s0920-9964(01)00293-6
119
Medalia A. Choi J. (2009). Cognitive Remediation in Schizophrenia. Neuropsychol. Rev.19 (3), 353–364. 10.1007/s11065-009-9097-y
120
Medalia A. Richardson R. (2005). What Predicts a Good Response to Cognitive Remediation Interventions?Schizophrenia Bull.31 (4), 942–953. 10.1093/schbul/sbi045
121
Melguizo Herrera E. Bertel De La Hoz A. Paternina Osorio D. Felfle Fuentes Y. Porto Osorio L. (2017). Cognitive Stimulation of Elderly Residents in Social Protection Centers in Cartagena, 2014. Revista Colombiana de Psiquiatría46 (4), 229–236. 10.1016/j.rcp.2016.09.008
122
Millán-Calenti J. C. Lorenzo T. Núñez-Naveira L. Buján A. Rodríguez-Villamil J. L. Maseda A. (2015). Efficacy of a Computerized Cognitive Training Application on Cognition and Depressive Symptomatology in a Group of Healthy Older Adults: A Randomized Controlled Trial. Arch. Gerontol. Geriatr.61 (3), 337–343.
123
Miranda-Castillo C. Tapia F. Herrera A. Ghigliotto F. Guerra L. (2012). Implementación de un programa de estimulación cognitiva en personas con demencia tipo Alzheimer: Un estudio piloto en chilenos de la tercera edad. Universitas Psychologica12 (2), 445–455.
124
Mohlman J. Chazin D. Georgescu B. (2011). Feasibility and Acceptance of a Nonpharmacological Cognitive Remediation Intervention for Patients with Parkinson Disease. J. Geriatr. Psychiatry Neurol.24 (2), 91–97. 10.1177/0891988711402350
125
Mohlman J. DeVito A. Lauderdale S. Dobkin R. (2017). Initial Outcomes of a Combined Cognitive-Behavioral Therapy and Attention Process Training Intervention for Older Adults with Parkinson's Disease. Pract. Innov.2 (4), 234–242. 10.1037/pri0000056
126
Morimoto S. S. Wexler B. E. Alexopoulos G. S. (2012). Neuroplasticity-based Computerized Cognitive Remediation for Geriatric Depression. Int. J. Geriatr. Psychiatry27 (12), 1239–1247. 10.1002/gps.3776
127
Morimoto S. S. Wexler B. E. Liu J. Hu W. Seirup J. Alexopoulos G. S. (2014). Neuroplasticity-based Computerized Cognitive Remediation for Treatment-Resistant Geriatric Depression. Nat. Commun.5, 4579. 10.1038/ncomms5579
128
Moro V. Condoleo M. T. Sala F. Pernigo S. Moretto G. Gambina G. (2012). Cognitive Stimulation in A-MCI. Am. J. Alzheimers Dis. Other Demen.27 (2), 121–130. 10.1177/1533317512441386
129
Moro V. Condoleo M. T. Valbusa V. Broggio E. Moretto G. Gambina G. (2015). Cognitive Stimulation of Executive Functions in Mild Cognitive Impairment. Am. J. Alzheimers Dis. Other Demen.30 (2), 153–164. 10.1177/1533317514539542
130
Mowszowski L. Batchelor J. Naismith S. L. (2010). Early Intervention for Cognitive Decline: Can Cognitive Training Be Used as a Selective Prevention Technique?Int. Psychogeriatr.22 (4), 537–548. 10.1017/s1041610209991748
131
Murman D. L. (2015). The Impact of Age on Cognition. Semin. Hear.36 (3), 111–121. 10.1055/s-0035-1555115
132
Naismith S. L. Mowszowski L. Diamond K. Lewis S. J. G. (2013). Improving Memory in Parkinson's Disease: A Healthy Brain Ageing Cognitive Training Program. Mov Disord.28 (8), 1097–1103. 10.1002/mds.25457
133
Navarro J. Menacho I. Alcalde C. Marchena E. Ruiz G. Aguilar M. (2009). Cognitive Changes Among Institutionalized Elderly People. Uedg35 (6), 523–540. 10.1080/03601270802608568
134
Netto T. M. Greca D. V. Zimmermann N. Oliveira C. R. d. Teixeira-Leite H. M. Fonseca R. P. et al (2013). Efeito de um programa de treinamento da memória de trabalho em adultos idosos. Psicol. Reflex. Crit.26 (1), 122–135. 10.1590/s0102-79722013000100014
135
Newson R. S. Kemps E. B. (2006). The Influence of Physical and Cognitive Activities on Simple and Complex Cognitive Tasks in Older Adults. Exp. Aging Res.32 (3), 341–362. 10.1080/03610730600699134
136
Niu Y.-X. Tan J.-P. Guan J.-Q. Zhang Z.-Q. Wang L.-N. (2010). Cognitive Stimulation Therapy in the Treatment of Neuropsychiatric Symptoms in Alzheimer's Disease: a Randomized Controlled Trial. Clin. Rehabil.24 (12), 1102–1111. 10.1177/0269215510376004
137
Nouchi R. Taki Y. Takeuchi H. Hashizume H. Akitsuki Y. Shigemune Y. et al (2012). Brain Training Game Improves Executive Functions and Processing Speed in the Elderly: A Randomized Controlled Trial. PLoS ONE7 (1), e29676. 10.1371/journal.pone.0029676
138
Nouchi R. Taki Y. Takeuchi H. Nozawa T. Sekiguchi A. Kawashima R. (2016). Reading Aloud and Solving Simple Arithmetic Calculation Intervention (Learning Therapy) Improves Inhibition, Verbal Episodic Memory, Focus Attention and Processing Speed in Healthy Elderly People: Evidence from a Randomized Controlled Trial. Front. Hum. Neurosci.10 (217), 1–14. 10.3389/fnhum.2016.00217
139
Nouchi R. Kobayashi A. Nouchi H. Kawashima R. (2019). Newly Developed Tv-Based Cognitive Training Games Improve Car Driving Skills, Cognitive Functions, and Mood in Healthy Older Adults: Evidence from a Randomized Controlled Trial. Front. Aging Neurosci.11 (99), 1–15. 10.3389/fnagi.2019.00099
140
Nousia A. Siokas V. Aretouli E. Messinis L. Aloizou A.-M. Martzoukou M. et al (2018). Beneficial Effect of Multidomain Cognitive Training on the Neuropsychological Performance of Patients with Early-Stage Alzheimer's Disease. Neural Plasticity2018 (2845176), 1–9. 10.1155/2018/2845176
141
Ordonez T. N. Borges F. Kanashiro C. S. Santos C. C. d. N. Hora S. S. Lima-Silva T. B. (2017). Actively Station: Effects on Global Cognition of Mature Adults and Healthy Elderly Program Using Eletronic Games. Dement. Neuropsychol.11 (2), 186–197. 10.1590/1980-57642016dn11-020011
142
París A. P. Saleta H. G. de la Cruz Crespo Maraver M. Silvestre E. Freixa M. G. Torrellas C. P. et al (2011). Blind Randomized Controlled Study of the Efficacy of Cognitive Training in Parkinson's Disease. Mov. Disord.26 (7), 1251–1258. 10.1002/mds.23688
143
Park J.-H. Park J.-H. (2018). Does Cognition-specific Computer Training Have Better Clinical Outcomes Than Non-specific Computer Training? A Single-Blind, Randomized Controlled Trial. Clin. Rehabil.32 (2), 213–222. 10.1177/0269215517719951
144
Park M. H. Kwon D. Y. Seo W. K. Lim K. S. Song M. S. (2009). The Effects of Cognitive Training on Community-Dwelling Elderly Koreans. J. Psychiatr. Ment. Health Nurs.16 (10), 904–909. 10.1111/j.1365-2850.2009.01467.x
145
Patel T. R. (2012). Environmental Enrichment: Aging and Memory. Yale J. Biol. Med.85 (4), 491–500.
146
Peel N. Bartlett H. McClure R. (2004). Healthy Ageing: How Is it Defined and Measured?Australas. J. Ageing23 (3), 115–119. 10.1111/j.1741-6612.2004.00035.x
147
Peña J. Ibarretxe-Bilbao N. García-Gorostiaga I. Gomez-Beldarrain M. A. Díez-Cirarda M. Ojeda N. (2014). Improving Functional Disability and Cognition in Parkinson Disease: Randomized Controlled Trial. Neurology83 (23), 2167–2174. 10.1212/WNL.0000000000001043
148
Petersen R. C. Doody R. Kurz A. Mohs R. C. Morris J. C. Rabins P. V. et al (2001). Current Concepts in Mild Cognitive Impairment. Arch. Neurol.58 (12), 1985–1992. 10.1001/archneur.58.12.1985
149
Petersen R. C. (2004). Mild Cognitive Impairment as a Diagnostic Entity. J. Intern. Med.256 (3), 183–194. 10.1111/j.1365-2796.2004.01388.x
150
Petrelli A. Kaesberg S. Barbe M. T. Timmermann L. Fink G. R. Kessler J. et al (2014). Effects of Cognitive Training in Parkinson's Disease: a Randomized Controlled Trial. Parkinsonism Relat. Disord.20 (11), 1196–1202. 10.1016/j.parkreldis.2014.08.023
151
Petrelli A. Kaesberg S. Barbe M. T. Timmermann L. Rosen J. B. Fink G. R. et al (2015). Cognitive Training in Parkinson's Disease Reduces Cognitive Decline in the Long Term. Eur. J. Neurol.22 (4), 640–647. 10.1111/ene.12621
152
Piras F. Carbone E. Faggian S. Salvalaio E. Gardini S. Borella E. (2017). Efficacy of Cognitive Stimulation Therapy for Older Adults with Vascular Dementia. Dement. Neuropsychol.11 (4), 434–441. 10.1590/1980-57642016dn11-040014
153
Power K. Kirwan G. Palmer M. (2011). A Comparison of Text and Technology Based Training Tools to Improve Cognitive Skills in Older Adults. Stud. Health Technol. Inform.167, 98–102.
154
Rabipour S. Raz A. (2012). Training the Brain: Fact and Fad in Cognitive and Behavioral Remediation. Brain Cogn.79, 159–179. 10.1016/j.bandc.2012.02.006
155
Rebok G. W. Langbaum J. B. Jones R. N. Gross A. L. Parisi J. M. Spira A. P. et al (2013). Memory Training in the ACTIVE Study: How Much Is Needed and Who Benefits?J. Aging Health25 (0), 21S–42S. 10.1177/0898264312461937
156
Rebok G. W. Ball K. Guey L. T. Jones R. N. Kim H.-Y. King J. W. et al (2014). Ten-Year Effects of the Advanced Cognitive Training for Independent and Vital Elderly Cognitive Training Trial on Cognition and Everyday Functioning in Older Adults. J. Am. Geriatr. Soc.62 (1), 16–24. 10.1111/jgs.12607
157
Rees L. Marshall S. Hartridge C. Mackie D. Weiser M. (2007). Cognitive Interventions post Acquired Brain Injury. Brain Inj.21 (2), 161–200. 10.1080/02699050701201813
158
Reijnders J. S. A. M. Geusgens C. A. V. Ponds R. W. H. M. Van Boxtel M. P. J. (2017). "Keep Your Brain Fit!" Effectiveness of a Psychoeducational Intervention on Cognitive Functioning in Healthy Adults: A Randomised Controlled Trial. Neuropsychological Rehabil.27 (4), 455–471. 10.1080/09602011.2015.1090458
159
Rizkalla M. N. (2018). Cognitive Training in the Elderly: A Randomized Trial to Evaluate the Efficacy of a Self-Administered Cognitive Training Program. Aging Ment. Health22 (10), 1384–1394. 10.1080/13607863.2015.1118679
160
Rohling M. L. Faust M. E. Beverly B. Demakis G. (2009). Effectiveness of cognitive rehabilitation following acquired brain injury: a meta-analytic re-examination of Cicerone et al.'s (2000, 2005) systematic reviews. Neuropsychology23 (1), 20–39. 10.1037/a0013659
161
Rojas G. J. Villar V. Iturry M. Harris P. Serrano C. M. Herrera J. A. et al (2013). Efficacy of a Cognitive Intervention Program in Patients with Mild Cognitive Impairment. Int. Psychogeriatr.25 (5), 825–831. 10.1017/s1041610213000045
162
Rosell J. (2018). Cognitive stimulation for healthy older adults through computer-based programs: A review of the literature/Estimulación cognitiva para personas mayores sanas mediante programas computarizados: Una revisión de la literatura. Estudios de Psicología39 (2-3), 407–436. 10.1080/02109395.2018.1494678
163
Ross L. A. Freed S. A. Edwards J. D. Phillips C. B. Ball K. (2017). The Impact of Three Cognitive Training Programs on Driving Cessation across 10 years: A Randomized Controlled Trial. Gerontologist57 (5), 838–846. 10.1093/geront/gnw143
164
Ross L. A. Edwards J. D. O’Connor M. L. Ball K. K. Wadley V. G. Vance D. E. (2016). The Transfer of Cognitive Speed of Processing Training to Older Adults' Driving Mobility across 5 Years. Geronb71 (1), 87–97. 10.1093/geronb/gbv022
165
Ross L. A. Sprague B. N. Phillips C. B. O’Connor M. L. Dodson J. E. (2018). The Impact of Three Cognitive Training Interventions on Older Adults' Physical Functioning across 5 Years. J. Aging Health30 (3), 475–498. 10.1177/0898264316682916
166
Savulich G. Piercy T. Fox C. Suckling J. Rowe J. B. O’Brien J. T. et al (2017). Cognitive Training Using a Novel Memory Game on an Ipad in Patients with Amnestic Mild Cognitive Impairment (aMCI). Int. J. Neuropsychopharmacol.20 (8), 624–633. 10.1093/ijnp/pyx040
167
Schmiedek F. Bauer C. Lövdén M. Brose A. Lindenberger U. (2010). Cognitive Enrichment in Old Age. GeroPsych23 (2), 59–67. 10.1024/1662-9647/a000013
168
Shatil E. (2013). Does Combined Cognitive Training and Physical Activity Training Enhance Cognitive Abilities More Than Either Alone? A Four-Condition Randomized Controlled Trial Among Healthy Older Adults. Front. Aging Neurosci.5 (8), 8–12. 10.3389/fnagi.2013.00008
169
Simons D. J. Boot W. R. Charness N. Gathercole S. E. Chabris C. F. Hambrick D. Z. et al (2016). Do "brain-training" Programs Work?Psychol. Sci. Public Interest17 (3), 103–186. 10.1177/1529100616661983
170
Simpson T. Camfield D. Pipingas A. Macpherson H. Stough C. (2012). Improved Processing Speed: Online Computer-Based Cognitive Training in Older Adults. Educ. Gerontol.38 (7), 445–458. 10.1080/03601277.2011.559858
171
Sisco S. M. Marsiske M. Gross A. L. Rebok G. W. (2013). The Influence of Cognitive Training on Older Adults' Recall for Short Stories. J. Aging Health25 (80), 230S–48S. 10.1177/0898264313501386
172
Smith M. Jones M. P. Dotson M. M. Wolinsky F. D. (2018). Speed-of-Processing Training in Assisted and Independent Living: A Randomized Controlled Trial. J. Am. Geriatr. Soc.66 (8), 1538–1545. 10.1111/jgs.15423
173
Souders D. J. Boot W. R. Blocker K. Vitale T. Roque N. A. Charness N. (2017). Evidence for Narrow Transfer after Short-Term Cognitive Training in Older Adults. Front. Aging Neurosci.9, 41. 10.3389/fnagi.2017.00041
174
Spector A. Orrell M. Woods B. (2010). Cognitive Stimulation Therapy (CST): Effects on Different Areas of Cognitive Function for People with Dementia. Int. J. Geriat. Psychiatry25 (12), 1253–1258. 10.1002/gps.2464
175
Spector A. Thorgrimsen L. Woods B. Royan L. Davies S. Butterworth M. et al (2003). Efficacy of an Evidence-Based Cognitive Stimulation Therapy Programme for People with Dementia. Br. J. Psychiatry183, 248–254. 10.1192/bjp.183.3.248
176
Steinerman J. R. (2010). Minding the Aging Brain: Technology-Enabled Cognitive Training for Healthy Elders. Curr. Neurol. Neurosci. Rep.10 (5), 374–380. 10.1007/s11910-010-0124-4
177
Stewart D. B. Berg-Weger M. Tebb S. Sakamoto M. Roselle K. Downing L. et al (2017). Making a Difference: A Study of Cognitive Stimulation Therapy for Persons with Dementia. J. Gerontological Soc. Work60 (4), 300–312. 10.1080/01634372.2017.1318196
178
Stuss D. T. Robertson I. H. Craik F. I. Levine B. Alexander M. P. Black S. et al (2007). Cognitive Rehabilitation in the Elderly: a Randomized Trial to Evaluate a New Protocol. J. Int. Neuropsychol. Soc.13 (1), 120–131. 10.1017/S1355617707070154
179
Sukontapol C. Kemsen S. Chansirikarn S. Nakawiro D. Kuha O. Taemeeyapradit U. (2018). The Effectiveness of a Cognitive Training Program in People with Mild Cognitive Impairment: A Study in Urban Community. Asian J. Psychiatry35, 18–23. 10.1016/j.ajp.2018.04.028
180
Suzuki H. Kuraoka M. Yasunaga M. Nonaka K. Sakurai R. Takeuchi R. et al (2014). Cognitive Intervention through a Training Program for Picture Book reading in Community-Dwelling Older Adults: a Randomized Controlled Trial. BMC Geriatr.14, 122. 10.1186/1471-2318-14-122
181
Tagliabue C. F. Guzzetti S. Gualco G. Boccolieri G. Boccolieri A. Smith S. et al (2018). A Group Study on the Effects of a Short Multi-Domain Cognitive Training in Healthy Elderly Italian People. BMC Geriatr.18 (321), 1–11. 10.1186/s12877-018-1014-x
182
Tchanturia K. Davies H. Campbell I. C. (2007). Cognitive Remediation Therapy for Patients with Anorexia Nervosa: Preliminary Findings. Annals of General Psychiatry6, 14. 10.1186/1744-859X-6-14
183
Ten Brinke L. F. Best J. R. Crockett R. A. Liu-Ambrose T. (2018). The Effects of an 8-week Computerized Cognitive Training Program in Older Adults: A Study Protocol for a Randomized Controlled Trial. BMC Geriatr.18 (31), 31–11. 10.1186/s12877-018-0730-6
184
Thiel C. Vogt L. Tesky V. A. Meroth L. Jakob M. Sahlender S. et al (2012). Cognitive Intervention Response Is Related to Habitual Physical Activity in Older Adults. Aging Clin. Exp. Res.24 (1), 47–55. 10.3275/7569
185
Thompson G. Foth D. (2005). Cognitive-training Programs for Older Adults: What Are They and Can They Enhance Mental Fitness?Educ. Gerontol.31 (8), 603–626. 10.1080/03601270591003364
186
Toh H. M. Ghazali S. E. Subramaniam P. (2016). The Acceptability and Usefulness of Cognitive Stimulation Therapy for Older Adults with Dementia: A Narrative Review. Int. J. Alzheimer's Dis.2016 (2), 1–11. 10.1155/2016/5131570
187
Tranter L. J. Koutstaal W. (2008). Age and Flexible Thinking: An Experimental Demonstration of the Beneficial Effects of Increased Cognitively Stimulating Activity on Fluid Intelligence in Healthy Older Adults. Aging Neuropsychol. Cogn.15 (2), 184–207. 10.1080/13825580701322163
188
Troyer A. K. Murphy K. J. Anderson N. D. Moscovitch M. Craik F. I. M. (2008). Changing Everyday Memory Behaviour in Amnestic Mild Cognitive Impairment: a Randomised Controlled Trial. Neuropsychological Rehabil.18 (1), 65–88. 10.1080/09602010701409684
189
Twamley E. W. Vella L. Burton C. Z. Heaton R. K. Jeste D. V. (2012). Compensatory Cognitive Training for Psychosis: Effects in a Randomized Controlled Trial. J. Clin. Psychiatry73 (9), 1212–1219. 10.4088/JCP.12m07686
190
Valdés E. G. Andel R. Lister J. J. Gamaldo A. Edwards J. D. (2019). Can Cognitive Speed of Processing Training Improve Everyday Functioning Among Older Adults with Psychometrically Defined Mild Cognitive Impairment?J. Aging Health31 (4), 595–610. 10.1177/0898264317738828
191
Van de Ven R. M. Buitenweg J. I. Schmand B. Veltman D. J. Aaronson J. A. Nijboer T. C. et al (2017). Brain Training Improves Recovery after Stroke but Waiting List Improves Equally: A Multicenter Randomized Controlled Trial of a Computer-Based Cognitive Flexibility Training. PLoS ONE12 (3), e0172993. 10.1371/journal.pone.0172993
192
van Heugten C. M. Ponds R. W. H. M. Kessels R. P. C. (2016). Brain Training: Hype or hope?Neuropsychological Rehabil.26, 639–644. 10.1080/09602011.2016.1186101
193
van Zon L. Kirby J. R. Anderson N. (2016). The Efficacy of a Volunteer-Administered Cognitive Stimulation Program in Long-Term Care Homes. Int. Psychogeriatr.28 (6), 995–1004. 10.1017/s1041610215002392
194
Vance D. E. Keltner N. L. McGuinness T. Umlauf M. G. Yuan Y. Y. (2010). The Future of Cognitive Remediation Training in Older Adults. J. Neurosci. Nurs.42 (5), 255–256. 10.1097/jnn.0b013e3181ecb003
195
Vance D. E. McNees P. Meneses K. (2009). Technology, Cognitive Remediation, and Nursing: Directions for Successful Cognitive Aging. J. Gerontol. Nurs.35 (2), 50–56. 10.3928/00989134-20090201-09
196
Vance D. E. (2009). The Emerging Role of Cognitive Remediation Therapy. Activities, Adaptation & Aging33 (1), 17–30. 10.1080/01924780902718541
197
Vance D. Fazeli P. Shacka J. Nicholson W. McKie P. Raper J. et al (2017). Testing a Computerized Cognitive Training Protocol in Adults Aging with Hiv-Associated Neurocognitive Disorders: Randomized Controlled Trial Rationale and Protocol. JMIR Res. Protoc.6 (4), e68. 10.2196/resprot.6625
198
Vanova M. Irazoki E. García-Casal J. A. Martínez-Abad F. Botella C. Shiells K. R. et al (2018). The Effectiveness of ICT-Based Neurocognitive and Psychosocial Rehabilitation Programmes in People with Mild Dementia and Mild Cognitive Impairment Using GRADIOR and ehcoBUTLER: Study Protocol for a Randomised Controlled Trial. Trials19 (100), 100–115. 10.1186/s13063-017-2371-z
199
VanVleet T. Voss M. Dabit S. Mitko A. DeGutis J. (2018). Randomized Control Trial of Computer-Based Training Targeting Alertness in Older Adults: The ALERT Trial Protocol. BMC Psychol.6 (22), 22–14. 10.1186/s40359-018-0233-4
200
Vaportzis E. Martin M. Gow A. J. (2017). A Tablet for Healthy Ageing: The Effect of a Tablet Computer Training Intervention on Cognitive Abilities in Older Adults. Am. J. Geriatr. Psychiatry25 (8), 841–851. 10.1016/j.jagp.2016.11.015
201
Velligan D. I. Bow-Thomas C. C. Huntzinger C. Ritch J. Ledbetter N. Prihoda T. J. et al (2000). Randomized Controlled Trial of the Use of Compensatory Strategies to Enhance Adaptive Functioning in Outpatients with Schizophrenia. Ajp157 (8), 1317–1328. 10.1176/appi.ajp.157.8.1317
202
Verghese J. Mahoney J. Ambrose A. F. Wang C. Holtzer R. (2010). Effect of Cognitive Remediation on Gait in Sedentary Seniors. Journals Gerontol. Ser. A: Biol. Sci. Med. Sci.65A (12), 1338–1343. 10.1093/gerona/glq127
203
Vermeij A. Claassen J. A. Dautzenberg P. L. Kessels R. P. (2016). Transfer and Maintenance Effects of Online Working-Memory Training in normal Ageing and Mild Cognitive Impairment. Neuropsychol. Rehabil.26 (5-6), 783–809. 10.1080/09602011.2015.1048694
204
Vidovich M. R. Shaw J. Flicker L. Almeida O. P. (2011). Cognitive Activity for the Treatment of Older Adults with Mild Alzheimer's Disease (AD) - PACE AD: Study Protocol for a Randomised Controlled Trial. Trials12, 47. 10.1186/1745-6215-12-47
205
Wang M-Y. Chang C-Y. Su S-Y. (2011). What’s Cooking? – Cognitive Training of Executive Function in the Elderly. Front. Psychol.2 (228), 1–11. 10.3389/fpsyg.2011.00228
206
Whitlock L. A. McLaughlin A. C. Allaire J. C. (2012). Individual Differences in Response to Cognitive Training: Using a Multi-Modal, Attentionally Demanding Game-Based Intervention for Older Adults. Comput. Hum. Behav.28 (4), 1091–1096. 10.1016/j.chb.2012.01.012
207
Willis S. L. (1996). Everyday Cognitive Competence in Elderly Persons: Conceptual Issues and Empirical Findings. The Gerontologist36 (5), 595–601. 10.1093/geront/36.5.595
208
Willis S. L. Tennstedt S. L. Marsiske M. Ball K. Elias J. Koepke K. M. et al (2006). Long-term Effects of Cognitive Training on Everyday Functional Outcomes in Older Adults. JAMA296 (23), 2805–2814. 10.1001/jama.296.23.2805
209
Wilson B. A. (2002). Towards a Comprehensive Model of Cognitive Rehabilitation. Neuropsychological Rehabil.12 (2), 97–110. 10.1080/09602010244000020
210
Winblad B. Palmer K. Kivipelto M. Jelic V. Fratiglioni L. Wahlund L.-O. et al (2004). Mild Cognitive Impairment - beyond Controversies, towards a Consensus: Report of the International Working Group on Mild Cognitive Impairment. J. Intern. Med.256 (3), 240–246. 10.1111/j.1365-2796.2004.01380.x
211
Withiel T. Wong D. Ponsford J. Cadilhac D. New P. Mihaljcic T. et al (2019). Comparing Memory Group Training and Computerized Cognitive Training for Improving Memory Function Following Stroke: A Phase II Randomized Controlled Trial. J. Rehabil. Med.51 (5), 343–351. 10.2340/16501977-2540
212
Wolinsky F. D. Unverzagt F. W. Smith D. M. Jones R. Wright E. Tennstedt S. L. (2006). The Effects of the ACTIVE Cognitive Training Trial on Clinically Relevant Declines in Health-Related Quality of Life. Journals Gerontol. Ser. B: Psychol. Sci. Soc. Sci.61 (5), S281–S287. 10.1093/geronb/61.5.s281
213
Wolinsky F. D. Vander Weg M. W. Martin R. Unverzagt F. W. Willis S. L. Marsiske M. et al (2009). Does Cognitive Training Improve Internal Locus of Control Among Older Adults?Journals Gerontol. Ser. B: Psychol. Sci. Soc. Sci.65B (5), 591–598. 10.1093/geronb/gbp117
214
Woods B. Aguirre E. Spector A. E. Orrell M. (2012). Cognitive Stimulation to Improve Cognitive Functioning in People with Dementia. Cochrane Database Syst. Rev. (2), CD005562. 10.1002/14651858.CD005562.pub2
215
Woods B. Thorgrimsen L. Spector A. Royan L. Orrell M. (2006). Improved Quality of Life and Cognitive Stimulation Therapy in Dementia. Aging Ment. Health10 (3), 219–226. 10.1080/13607860500431652
216
World Health Organization (2017a). Operationalising the Concept of Intrinsic Capacity in Clinical Settings. Available from https://www.who.int/ageing/health-systems/clinical-consortium/CCHA2017-backgroundpaper-1.pdf (Retrieved October 18, 2021).
217
World Health Organization (2017b). 10 Facts on Ageing and Health. Available from https://www.who.int/features/factfiles/ageing/en/(Retrieved April 19, 2019).
218
World Health Organization (2015). World Report on Ageing and Health. Available from https://www.who.int/ageing/publications/world-report-2015/en/(Retrieved October 18, 2021).
219
Wykes T. S. van der Gaag M. (2001). Is it time to develop a new cognitive therapy for psychosis--cognitive remediation therapy (CRT)?. Clinical Psychology Review21 (8), 1227–1256. 10.1016/S0272-7358(01)00104-0
220
Yam A. Marsiske M. (2013). Cognitive Longitudinal Predictors of Older Adults’ Self-Reported IADL Function. J. Aging Health25 (8S), 163S–185S. 10.1177/0898264313495560
221
Yamanaka K. Kawano Y. Noguchi D. Nakaaki S. Watanabe N. Amano T. et al (2013). Effects of Cognitive Stimulation Therapy Japanese Version (CST-J) for People with Dementia: A Single-Blind, Controlled Clinical Trial. Aging Ment. Health17 (5), 579–586. 10.1080/13607863.2013.777395
222
Yan L. Li L. Qing X. Zhi H. Lin L. Lei G. et al (2016). Cognitive Training in Older Adults with Mild Cognitive Impairment. Biomed. Environ. Sci.29 (5), 356–364.
223
Yasini M. Marchand G. (2016). Adoption and Use of a mobile Health Application in Older Adults for Cognitive Stimulation. Stud. Health Technol. Inform.221, 13–17. 10.3233/978-1-61499-633-0-13
224
Young D. K.-W. (2020). Multicomponent Intervention Combining a Cognitive Stimulation Group and Tai Chi to Reduce Cognitive Decline Among Community-Dwelling Older Adults with Probable Dementia: A multi-center, Randomized Controlled Trial. Dementia19 (6), 2073–2089. 10.1177/1471301218814637
225
Young D. K.-w. Ng P. Y.-n. Kwok T. Ho F. Cheng D. Mak V. et al (2019). The Effects of an Expanded Cognitive Stimulation Therapy Model on the Improvement of Cognitive Ability of Elderly with Mild Stage Dementia Living in a Community - a Randomized Waitlist Controlled Trial. Aging Ment. Health23 (7), 855–862. 10.1080/13607863.2018.1471586
226
Yuill N. Hollis V. (2011). A Systematic Review of Cognitive Stimulation Therapy for Older Adults with Mild to Moderate Dementia: An Occupational Therapy Perspective. Occup. Ther. Int.18 (4), 163–186. 10.1002/oti.315
227
Zajac-Lamparska L. Trempała J. (2016). Effects of Working Memory and Attentional Control Training and Their Transfer onto Fluid Intelligence in Early and Late Adulthood. Health Psychol. Rep.4 (1), 41–53. 10.5114/hpr.2016.56846
228
Zelinski E. M. (2009). Far Transfer in Cognitive Training of Older Adults. Restorative Neurol. Neurosci.27 (5), 455–471. 10.3233/rnn-2009-0495
229
Zelinski E. M. Spina L. M. Yaffe K. Ruff R. Kennison R. F. Mahncke H. W. et al (2011). Improvement in Memory with Plasticity-Based Adaptive Cognitive Training: Results of the 3-month Follow-Up. J. Am. Geriatr. Soc.59 (2), 258–265. 10.1111/j.1532-5415.2010.03277.x
230
Zimmermann N. Netto T. M. Amodeo M. T. Ska B. Fonseca R. P. (2014). Working Memory Training and Poetry-Based Stimulation Programs: Are There Differences in Cognitive Outcome in Healthy Older Adults?Nre35 (1), 159–170. 10.3233/nre-141104
Summary
Keywords
brain training, cognitive stimulation, cognitive training, cognitive rehabilitation, older adults
Citation
Mendes L, Oliveira J, Barbosa F and Castelo-Branco M (2022) A Conceptual View of Cognitive Intervention in Older Adults With and Without Cognitive Decline—A Systemic Review. Front. Aging 3:844725. doi: 10.3389/fragi.2022.844725
Received
28 December 2021
Accepted
28 February 2022
Published
24 March 2022
Volume
3 - 2022
Edited by
Stefano Tarantini, University of Oklahoma Health Sciences Center, United States
Reviewed by
Frances Louise Dark, Metro South Addiction and Mental Health Services, Australia
Rafael Penadés, Hospital Clínic de Barcelona, Spain
Updates
Copyright
© 2022 Mendes, Oliveira, Barbosa and Castelo-Branco.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Liliana Mendes, liliana.mendes@icnas.uc.pt
This article was submitted to Interventions in Aging, a section of the journal Frontiers in Aging
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.