
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 20 March 2025
Sec. Public Mental Health
Volume 13 - 2025 | https://doi.org/10.3389/fpubh.2025.1559582
This article is part of the Research Topic The Intersection of Psychology, Healthy Behaviors, and its Outcomes View all 79 articles
 KeZhen Lv1†
KeZhen Lv1† ShengJie Xu1†
ShengJie Xu1† YuQi Sun1†
YuQi Sun1† Rui Zhou1†
Rui Zhou1† Hanyuan Xu1†
Hanyuan Xu1† Junhao He1†
Junhao He1† Cheng Xu1*
Cheng Xu1* Hui Xu1*
Hui Xu1* Jing Xu1*
Jing Xu1* Jun Qian1,2*
Jun Qian1,2*Objective: With the rising global obesity rates, increasing research has been directed toward understanding how obesity affects cognitive ability in young adults. This study aims to explore the impact of body mass index (BMI) on general cognitive ability and how sleep quality and impulsive trait mediate this relationship.
Methods: A total of 1,205 young adults from Human Connectome Project(HCP) project were included, and questionnaires and cognitive assessment tools were conducted.
Results: BMI was negatively correlated with general cognitive ability, with sleep quality and impulsive trait acting as chain mediators between BMI and general cognitive ability. Additionally, gender moderated the effect of BMI on sleep quality, with this effect being more pronounced in female young adults.
Conclusion: This study not only provided new insights into the impact of BMI on general cognitive ability in young adults but also offered an important perspective on how sleep quality and impulsive trait influenced this process. These findings provide a scientific basis for preventive measures against obesity and cognitive impairment in young adults.
Globally, obesity has become an increasingly severe public health issue. According to data from the World Health Organization in 2021, the number of individuals with obesity worldwide has tripled since 1975 (1). Obesity has been shown to be associated with all-cause mortality and poorer health outcomes, and it may impair cognitive function (2). A survey in 2024 on the global prevalence rate of obesity in 99% of the population revealed that obesity-related symptoms have become predominant in adults and are rapidly obeserved among young individuals, with the double prevalence rate of youth with obesity among most countries (3). This means that obesity among teenagers is gradually becoming a common problem that needs urgent attention. However, current research mostly focuses on the entire age range of individuals with obesity, with few studies specifically examining the characteristics of obesity in large samples of young adults.
Body mass index (BMI) is one of the indicators used to measure the degree of obesity in individuals. High BMI is almost universally associated with declines in cognitive ability across all domains (4, 5). General cognitive ability can be divided into fluid cognitive ability and crystallized cognitive ability. Fluid intelligence primarily involves the ability to process new information, logical reasoning, and solving new problems, while crystallized intelligence involves knowledge and skills accumulated through experience and education (6). Executive function, as a type of fluid intelligence, is often impaired by inflammation factors induced by obesity, affecting working memory and inhibitory control (7). It has found that students with high BMI have significantly lower academic performance compared to those with normal weight, indicating that their crystallized intelligence is also impaired (5). Therefore, we hypothesized that high BMI may damage an individual’s general cognitive ability. Previous research investigated how BMI affects cognition from a physiological perspective (8), while few studies have taken psychological factors as mediators into account. Research indicates that the interaction between physiological and psychological factors plays a crucial role in the onset and development of obesity (9). Furthermore, the relationship between BMI and general cognitive ability inherently involves a transition from physiological to psychological factors, necessitating the interaction of these factors. Therefore, we propose constructing a chain mediation model comprising both physiological and psychological factors to explain the relationship between obesity and cognitive ability.Sleep quality refers to personal overall sleep health and is often influenced by physiological functions such as cardiovascular function (10).
Among these psychological factors, sleep quality and impulsive traits are particularly noteworthy. Sleep quality refers to personal overall sleep health and is often influenced by physiological functions such as cardiovascular function (10). In non-clinical populations, sleep quality is typically assessed using the Pittsburgh Sleep Quality Index (PSQI) (11). Poor sleep quality is often associated with elevated BMI, as individuals with high BMI tend to consume unhealthy foods characterized by high fat and carbohydrate intake and poor diet quality can affect sleep quality (12, 13). Additionally, poor sleep quality can lead to a decline in cognitive ability (14–16). Previous research has found that sleep quality played a crucial mediating role in the relationship betwwen BMI and their cognitive function in children (17), but there is less evidence supporting this mediating relationship in young adults.
Beyond sleep disturbances, individuals with higher BMI also tend to exhibit greater impulsivity, which further contributes to cognitive deficits. Impulsive trait is a tendency to act on desires and urges without considering the consequences and is a cognitive trait that operates in specific situations (18, 19). Individuals with high BMI often exhibit higher levels of impulsivity (20), possibly due to neuroendocrine abnormalities that make it more difficult for them to resist cravings for food (21). Higher BMI is associated with reductions in the volume of various brain regions involved in reward and impulse control, such as the nucleus accumbens and striatum. These changes may lead to diminished control over food intake and other impulsive behaviors (22). The increase in impulsivity is associated with a decline in overall cognitive ability (23). For instance, attentional impulsivity and non-planning impulsivity significantly contribute to the reduction of cognitive abilities (24). This suggests that impulsivity may mediate the relationship between BMI and general cognitive ability, although this has not yet been empirically verified. Delay discounting, which refers to the preference for smaller immediate rewards over larger delayed rewards, is an external manifestation of impulsivity. High levels of delay discounting are associated with weaker self-control, higher impulsivity, and greater immediate gratification needs (25). Higher levels of delay discounting are often associated with greater possibility of becoming obesity, as individuals with obesity tend to have a weaker ability to inhibit their cravings for food (25), thus this study will adopt this experimental method.
Given the strong association between high impulsivity and poor sleep quality, these two variables may not contribute solely to the relationship between BMI and general cognitive ability (26–28). Researchers found that reduced sleep duration and abnormal sleep patterns can make individuals more impulsive and prone to taking risks (29–31). This may be due to the negative impact of decreased sleep quality on function activity of prefrontal cortex, which is responsible for higher-level cognitive processes, including judgment and decision-making (30). In another study, participants underwent 8 days of normal sleep followed by 3 days of sleep deprivation, during which they slept 2 h less each day (31). It has found that sleep deprivation significantly increased impulsivity and decreased the positive affect experienced by individuals. Conversely, good sleep quality can lead to positive emotions, which help enhance self-control abilities (32). Previous study also pointed out that individuals with better sleep quality tended to perform better on delay discounting tasks (33). Given the correlation between sleep quality and impulsivity, we propose that sleep quality and impulsivity will serve as chain mediators in the relationship between BMI and general cognitive ability.
Among the various impacts triggered by BMI, gender often serves as a moderating factor. This is likely due to differences between males and females in body fat distribution, hormone levels, and health risks associated with obesity (34). The pattern of BMI’s influence on general cognitive ability varies by gender (35). Across all age groups, BMI has a greater effect on general cognitive ability in male than that in female (36). Furthemore, women’s sleep quality, rather than men’s, is more likely to deteriorate with increasing BMI (34, 37). High BMI is significantly associated with both excessively long and short sleep durations in women, whereas it is only associated with excessively long sleep durations in men (34). Based on these findings, we hypothesize that gender may moderate the impact of BMI on sleep quality, leading to changes in general cognitive ability.
Considering that a single mediation model can usually only reveal the role of one mediating variable between the independent variable and the dependent variable, the chain mediation model provides a more detailed perspective, which can reveal how multiple mediating variables work together and influence each other, thereby providing a deeper understanding of the influencing mechanism, which is also more conducive to revealing how the joint action of psychological and physiological factors affects cognitive ability. In addition, considering that in current research, few studies specifically examine the obesity characteristics of large samples of young people, ignore how the interaction between psychology and physiology affects the consequences of obesity and do not pay attention to gender differences. In summary, this study aims to explore how BMI affects general cognitive ability of young adults by constructing a chain mediation model (Figure 1). The research hypotheses are as follows: H1: An increase in BMI will lead to a decrease in general cognitive ability in young adults; H2: Sleep quality mediates the relationship between BMI and general cognitive ability; H3: Impulsive trait mediate the relationship between BMI and general cognitive ability; H4: Sleep quality and impulsive trait will serve as chain mediators between BMI and general cognitive ability, i.e., high BMI reduces general cognitive ability by decreasing sleep quality and increasing impulsive trait; H5: Gender will moderate the impact of BMI on sleep quality and thus play a role in this chain mediation model.
This study used the HCP Release S1200 dataset. 1,206 Participants were recruited at Washington University in St. Louis between August 2012 and October 2015 (D. C. Van Essen et al.). This study was approved by the research ethics board of each institution and was conducted in accordance with the Declaration of Helsinki. All participants provided written informed consent and were young adults aged 22–35 years. The exclusion criteria were as follows: history of psychiatric disorder, substance abuse, neurodevelopmental disorder or damage, cardiovascular disease, severe health conditions (diabetes, multiple sclerosis, cerebral palsy, and premature birth), or magnetic resonance imaging contraindications (large tattoos, non-removable piercings, metal devices in the body, and claustrophobia). All participants were young adults with age between 22 and 35 years old. All participants provided written informed consent. All procedures were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration.
In terms of clinical assessments, sleep quality was measured by the total score on the Pittsburgh Sleep Quality Index (PSQI), which assesses seven components of sleep: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medication, and daytime dysfunction. Higher scores of PSQI indicate lower levels of sleep quality (38).
Impulsive trait was assessed using the Delay Discounting Task (DDT), which measures the tendency to undervalue rewards that are delayed in time (39, 40). At the indifference points in the version of the DDT employed in the HCP, participants were equally likely to choose a larger reward later (e.g., $40 K in 3 years) or a smaller reward sooner (e.g., $200). The task utilized two initial reward amounts ($200 and $40 K) and six fixed delays (1, 6 months, 1, 3, 5, and 10 years) (41). The Area under the Curve (AUC) measure provided an index of how steeply an individual discounted delayed rewards. The AUC is the sum of the areas of 6 trapezoids; for each trapezoid, the area is calculated as (x2 − x1) ([y1 + y2]/2), where x1 and x2 represent the delays, and y1 and y2 are the subjective values associated with these delays. All x and y values were normalized by dividing by the largest x and y values, respectively, so the AUC ranged from 0 (maximum discounting) to 1 (no discounting), with a smaller AUC reflecting greater discounting and impulsivity (42). Given that individuals may have different perceptions of the value of $200 and $40 K due to their socioeconomic status, impulsivity in our study was measured as the average AUC for both the $200 and $40 K delayed discounting curves.
Neurocognitive ability was examined across several cognitive domains, including general cognitive ability and working memory. The fluid cognitive ability was derived by averaging the normalized scores of each of the Toolbox tests that are fluid ability measures, including Flanker, Dimensional Change Card Sort, Picture Sequence Memory, List Sorting and Pattern Comparison. Similarly, the crystallized cognitive ability was derived by averaging the normalized scores of each of the Toolbox tests that are crystallized measures, including Picture Vocabulary and Reading Tests. Hence, the general cognitive ability was derived by averaging the scores of the fluid cognitive ability and crystallized cognitive ability. Higher scores indicate higher levels of cognitive ability (43).
In our study, BMI was derived from self-reported height and weight data, as this was the method available in the dataset we utilized. The dataset has been previously validated and widely used in similar research contexts (44).
SPSS 24.0 was used to perform descriptive and correlation analyses of the study variables and demographic variables. Since the research variables in this study are continuous variables, Pearson correlation was used to explore the correlation between the variables. After that, PROCESS was used to test the mediating model and moderated chain mediation model (45). Parameter estimation was performed using the bootstrap method with 5,000 replicate samples and a confidence interval (CI) with a confidence level of 95%, which indicates that the corresponding effect is significant if the confidence interval (CI) does not include zero, and not significant if the confidence interval (CI) includes zero.
Demographic characteristics of the participants were shown in Table 1 and correlation analysis results for the variables were shown in Table 2. Impulsive trait was significantly negatively correlated with sleep quality and BMI, while being significantly positively correlated with general cognitive ability. Additionally, sleep quality showed significantly positive correlation with BMI and significantly negative correlation with general cognitive ability. Furthermore, BMI was significantly negatively correlated with general cognitive ability.
We used Model 6 from the SPSS macro (46) (Model 6 assumes that all paths in the chain mediation model are not moderated) to test the mediating roles of sleep quality and impulsive trait between BMI and general cognitive ability (see Figure 2; Table 3). The results showed that BMI was negatively correlated with general cognitive ability (β = −0.15, p < 0.001). BMI was positively correlated with sleep quality (β = 0.12, p < 0.001), and sleep quality negatively was negatively correlated with general cognitive ability (β = −0.08, p < 0.01). BMI was negatively correlated with impulsive trait (β = −0.15, p < 0.001), and impulsive trait was positively correlated with general cognitive ability (β = 0.18, p < 0.001). Additionally, sleep quality was negatively correlated with impulsive trait (β = −0.16, p < 0.001). The confidence intervals are not including 0, indicating that three pathway of mediating effects are significant. The results of the mediation effect analysis showed that the total indirect effect was −0.0389. The mediating effect of sleep quality was −0.0087, the mediating effect of impulsive traits was −0.0268, and the effect size of chain mediation was −0.034 (see Table 4).
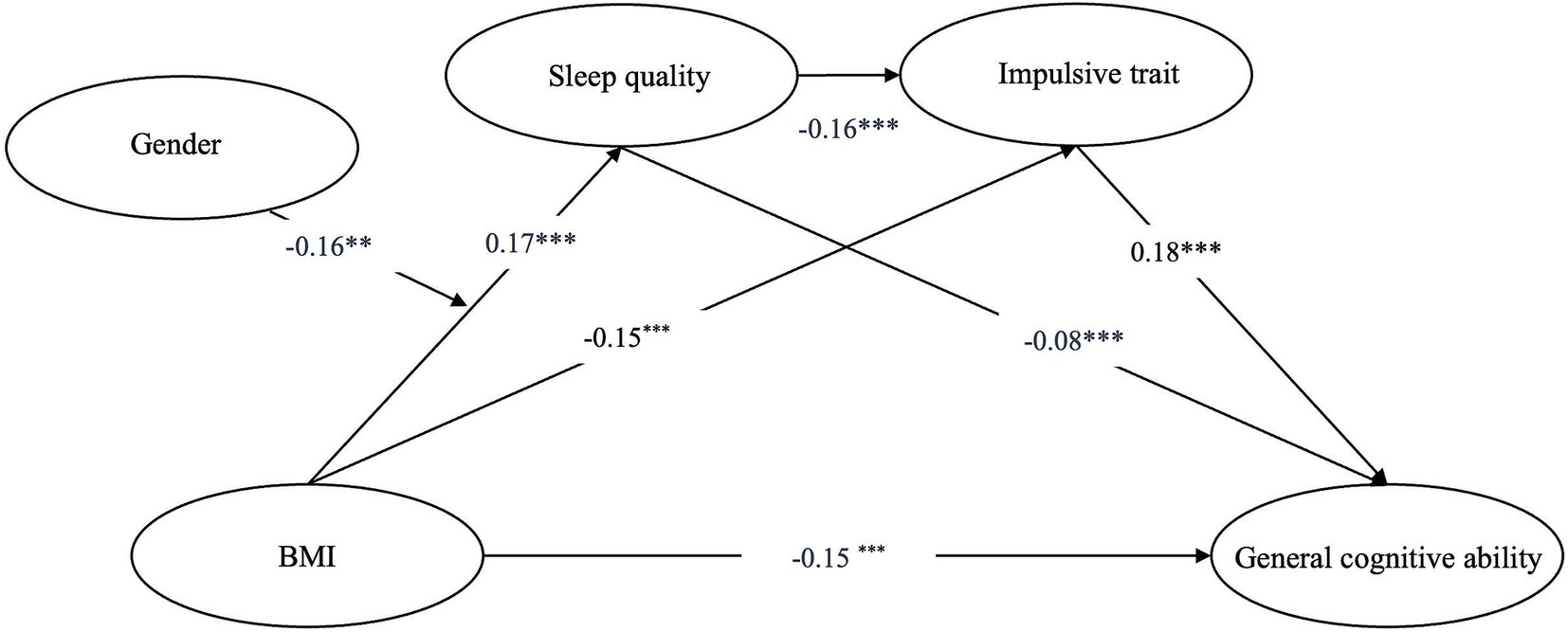
Figure 2. Moderated chain mediation model. BMI, body mass index. *p < 0.01, **p < 0.01, ***p < 0.001.
We used Model 83 from the SPSS macro (46) (Model 83 assumes that all paths in the mediation model are moderated) to test the moderated mediation model (Figure 3). The results indicated that gender moderated the relationship between BMI and sleep quality (β = −0.16, p < 0.001), while the moderating effects on other paths in the mediation model were not significant. Further simple slope analysis showed that BMI’s effect on sleep quality was stronger in females (bsimple = 0.174, p < 0.001) compared to that in males (bsimple = 0.008, p = 0.872).

Figure 3. Moderating effects of gender on the relationship between BMI and sleep quality. BMI, body mass index.
This study found that higher BMI in young adults was associated with cognitive impairment. Further analysis revealed that sleep quality and impulsive trait acted as chain mediators between BMI and general cognitive ability. We also confirmed that gender is a moderating variable, with the effect of BMI on sleep quality being greater in females than in males, supporting our research hypotheses.
The results showed that BMI is negatively correlated with general cognitive ability in young adults, further supporting previous research that high BMI might be a significant risk factor for cognitive impairment in young individuals (47–49). Currently, previous studies have explained how BMI affects cognitive abilities from physiological perspectives, such as diabetes (9) and endocrine hormones (50). It also found that obesity in young individuals leads to iron deficiency, resulting in a decline in cognitive abilities (47–51). Additionally, due to young people’s pursuit of perfectionism but also due to their ongoing social comparison processes, where the combination of internal and external factors leads to catastrophic thinking, resulting in greater stress and anxiety (52, 53). Psychological stress and emotional problems can distract young students, making it difficult for them to concentrate on studies and tasks, resulting in a decline in cognitive performance (52). According to the “weight scarring hypothesis,” even after weight loss, past obesity is associated with poorer psychological outcomes, which may also lead to physical illness (54). This means that the process by which being overweight worsens an individual’s psychological state and impairs general cognitive ability may be long-lasting.
Second, the analysis showed that sleep quality mediated the relationship between BMI and general cognitive ability. High BMI is a risk factor for several sleep disorders and forms a vicious circle with poor sleep quality (37, 55). Sleep quality has been shown to influence cognition, particularly in children (14, 36, 56). Recent research on the relationship between BMI, sleep quality, and cognitive ability has predominantly focused on children (17). However, the underlying mechanism was still unclear in other populations. Our study is the first to reveal that the mediating effect of sleep quality in young adults, which offered us a new perspective and helped us to understand how BMI affects general cognitive ability in young adults.
We also found that impulsive trait mediated the relationship between BMI and general cognitive ability. High BMI often leads to increased impulsive trait, making it difficult for individuals to resist the need for immediate rewards (20). A review indicated that excessive food intake in individuals with high BMI is related to abnormalities in neuroendocrine function, which may be a trigger for impulsive behavior (21). In this study, impulsive trait were measured using a delay discounting task, involving brain regions such as the prefrontal cortex, striatum, and insula (25), which are related to the brain’s reward circuitry and mediate individuals’ high BMI and abnormal reward processing (57). That is, individuals with a high BMI are more likely to receive immediate rewards in the delay discounting task. In addition, high impulsive trait can lead to a decline in general cognitive ability. Impulsive trait are considered one of the four core factors impairing general cognitive ability, with attentional and non-planning impulsivity potentially lowering subjective general cognitive ability (24).
Our results also show that sleep quality and impulsive trait act as chain mediators between BMI and general cognitive ability. Specifically, an increase in BMI leads to lower sleep quality, which in turn increases impulsive trait, resulting in cognitive decline. Previous research in young populations has found that low sleep quality leads to increased impulsive traits (28, 31). Additionally, low sleep quality and high impulsive traits can jointly contribute to a decline in cognitive abilities (24). The results of this study further support these conclusions and provide an explanation of the relationship between BMI and cognitive ability.
Additionally, this study found that in the BMI-general cognitive ability pathway, gender moderates the impact of BMI on sleep quality, specifically showing that compared to men, women’s sleep quality is more likely to deteriorate with increasing BMI compared to men. The BMI-sleep quality-general cognitive ability pathway only holds true for women. One explanation for this is that the relationship between BMI and sleep quality in women often involves emotional eating behaviors, which are less evident in men. These behaviors make BMI and sleep quality interdependent in women (55). Second, hormonal differences between the sexes lead to differences in food intake behaviors and sleep–wake cycles, such as sleep duration, latency (time to fall asleep), and temporal structure. These differences make women’s sleep quality more vulnerable to increases in BMI (37, 58). Research has found that increased body fat is more directly detrimental to general cognitive ability (26), and women generally have higher body fat percentages than men, with weight gain contributing more to body fat increase (34, 59). Therefore, women’s general cognitive ability are more likely to be affected by BMI, which may be one of the factors why the BMI-sleep quality- general cognitive ability pathway is only valid for women. Additionally, previous research has found that men and women have different subjective reporting standards for sleep quality, with women more likely to report poor sleep quality (58). Therefore, analyses related to sleep quality may be influenced by subjective reporting differences. In summary, unlike previous studies on older adults or across all age groups (34, 37), this study specifically explored young adults and found that gender moderates the effect of BMI on sleep quality among this group, providing more evidence for understanding obesity in young populations.
Given the complex interactions between obesity and cognitive function, understanding these physiological and psychological mechanisms is crucial for developing effective prevention and intervention strategies. This study found that sleep quality and impulsive trait mediated the relationship between BMI and general cognitive ability, while gender moderated the relationship between BMI and sleep quality. We hope that the findings of this study can provide a scientific basis for future practical interventions to promote adolescent health. Given that our results show a strong association between cognitive decline and BMI and sleep quality, public health strategies should focus more on weight management and sleep health issues among young people (27), and provide activities or training that can help improve self-control and reduce impulsivity, such as mindfulness training (60, 61). Furthermore, it is important to consider gender differences and provide additional support for females, who are more vulnerable to the negative effects of increased BMI.
Limitations of this study include the following: First, the model is based on cross-sectional data, making it difficult to establish causal relationships between variables. Future longitudinal studies may provide stronger evidence. Second, there may be moderating variables other than gender in the model, which means that we may have missed other significant moderating effects. Future research can explore these additional variables. Third, sleep quality was measured using questionnaires, and as mentioned above, men and women have different subjective reporting standards for sleep quality. This discrepancy might cause the observed gender differences to deviate from objective reality. We hope that future research will use more objective methods of data collection. Fourth, our study only utilizes the HCP Release S1200 dataset. This chain mediation model can be validated across additional datasets to enhance its generalizability in the future. In addition, this study used BMI as a measure of overweight and obesity. Although BMI remains the most commonly used measurement standard worldwide and is widely recognized, it cannot distinguish between muscle mass and fat mass, nor does it reflect the specific distribution of body fat. Therefore, BMI may not be able to fully and accurately assess an individual’s obesity level and its impact on cognitive ability. Future studies should further consider body fat percentage or other more precise measurement indicators to more fully explore the relationship between obesity and cognitive ability.
BMI is significantly and negatively correlated with general cognitive ability, with sleep quality and impulsive acting as chain mediators between BMI and general cognitive ability. In addition, gender moderated the effect of BMI on sleep quality. The findings of this study not only provide a new theoretical perspective on the relationship between obesity and cognitive ability, but also provide practical guidance for health intervention, public health policy and individual health management. Future intervention strategies should not only focus on BMI management, but also combine sleep optimization and pay more attention to women’s sleep quality.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
This study was approved and consented by the Ethics Committee of Wenzhou Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
KL: Conceptualization, Data curation, Formal analysis, Methodology, Resources, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. SX: Investigation, Methodology, Software, Validation, Writing – original draft, Writing – review & editing. YS: Formal analysis, Project administration, Resources, Visualization, Writing – original draft, Writing – review & editing. RZ: Conceptualization, Methodology, Project administration, Validation, Writing – original draft, Writing – review & editing. HaX: Conceptualization, Investigation, Methodology, Software, Writing – original draft, Writing – review & editing. JH: Conceptualization, Investigation, Validation, Visualization, Writing – original draft, Writing – review & editing. HuX: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. CX: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. JX: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. JQ: Formal analysis, Funding acquisition, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing.
The author(s) declare that financial support was received for the research and/or publication of this article. This study was funded by the Natural Science Foundation of Zhejiang Province (no. LQN25H090020), the Special Foundation for Young Scientists of Wenzhou Medical University (no. QTJ23027), and Philosophy and Social Science Research Grant of Wenzhou (no. 24WSK126YBM), the National Innovation and Entrepreneurship Training Program for College Students (no. 202410343067), Zhejiang Provincial Science and Technology Innovation Program (New Young Talent Program) for College Students (nos. 2023R413044 and 2024R413B074), and Ministry of Education College Student Mental Health and Comprehensive Quality Training Base.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors declare that no Gen AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Boutari, C, and Mantzoros, CS. A 2022 update on the epidemiology of obesity and a call to action: as its twin COVID-19 pandemic appears to be receding, the obesity and dysmetabolism pandemic continues to rage on. Metabolism. (2022) 133:155217. doi: 10.1016/j.metabol.2022.155217
2. Miller, AA, and Spencer, SJ. Obesity and neuroinflammation: a pathway to cognitive impairment. Brain Behav Immun. (2014) 42:10–21. doi: 10.1016/j.bbi.2014.04.001
3. Phelps, NH, Singleton, RK, Zhou, B, Heap, RA, Mishra, A, Bennett, JE, et al. Worldwide trends in underweight and obesity from 1990 to 2022: a pooled analysis of 3663 population-representative studies with 222 million children, adolescents, and adults. Lancet. (2024) 403:1027–50. doi: 10.1016/S0140-6736(23)02750-2
4. Prickett, C, Brennan, L, and Stolwyk, R. Examining the relationship between obesity and cognitive function: a systematic literature review. Obes Res Clin Pract. (2015) 9:93–113. doi: 10.1016/j.orcp.2014.05.001
5. Raine, L, Drollette, E, Kao, SC, Westfall, D, Chaddock-Heyman, L, Kramer, AF, et al. The associations between adiposity, cognitive function, and achievement in children. Med Sci Sports Exerc. (2018) 50:1868–74. doi: 10.1249/MSS.0000000000001650
6. Xu, H, Xu, C, Yang, Z, Bai, G, and Yin, B. Two sides of the same coin: distinct neuroanatomical patterns predict crystallized and fluid intelligence in adults. Front Neurosci. (2023) 17:1199106. doi: 10.3389/fnins.2023.1199106
7. Yang, Y, Shields, GS, Guo, C, and Liu, Y. Executive function performance in obesity and overweight individuals: a meta-analysis and review. Neurosci Biobehav Rev. (2018) 84:225–44. doi: 10.1016/j.neubiorev.2017.11.020
8. Xu, C, Xu, H, Yang, Z, and Guo, C. Regional shape alteration of left thalamus associated with late chronotype in young adults. Chronobiol Int. (2023) 40:234–45. doi: 10.1080/07420528.2022.2162916
9. Dye, L, Boyle, NB, Champ, C, and Lawton, C. The relationship between obesity and cognitive health and decline. Proc Nutr Soc. (2017) 76:443–54. doi: 10.1017/S0029665117002014
10. Baranwal, N, Yu, PK, and Siegel, NS. Sleep physiology, pathophysiology, and sleep hygiene. Prog Cardiovasc Dis. (2023) 77:59–69. doi: 10.1016/j.pcad.2023.02.005
11. Mollayeva, T, Thurairajah, P, Burton, K, Mollayeva, S, Shapiro, CM, and Colantonio, A. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: a systematic review and meta-analysis. Sleep Med Rev. (2016) 25:52–73. doi: 10.1016/j.smrv.2015.01.009
12. Mondin, TC, Stuart, AL, Williams, LJ, Jacka, FN, Pasco, JA, and Ruusunen, A. Diet quality, dietary patterns and short sleep duration: a cross-sectional population-based study. Eur J Nutr. (2019) 58:641–51. doi: 10.1007/s00394-018-1655-8
13. Muscogiuri, G, Barrea, L, Annunziata, G, di Somma, C, Laudisio, D, Colao, A, et al. Obesity and sleep disturbance: the chicken or the egg? Crit Rev Food Sci Nutr. (2019) 59:2158–65. doi: 10.1080/10408398.2018.1506979
14. El-Sheikh, M, Philbrook, LE, Kelly, RJ, Hinnant, JB, and Buckhalt, JA. What does a good night’s sleep mean? Nonlinear relations between sleep and children’s cognitive functioning and mental health. Sleep. (2019) 42:pzsz078. doi: 10.1093/sleep/zsz078
15. Leng, Y, Knutson, K, Carnethon, MR, and Yaffe, K. Association between sleep quantity and quality in early adulthood with cognitive function in midlife (2024) 102:e208056. doi: 10.1212/WNL.0000000000208056
16. Yang, Z, Wang, B, Xu, C, Xu, J, and Xu, H. How late nights influence brain cortical structures: distinct neuroanatomical measures associated with late Chronotype in young adults. Brain Topogr. (2024) 38:9. doi: 10.1007/s10548-024-01085-9
17. Spruyt, K, and Gozal, D. A mediation model linking body weight, cognition, and sleep-disordered breathing. Am J Respir Crit Care Med. (2012) 185:199–205. doi: 10.1164/rccm.201104-0721OC
18. VandenBos, GR. APA dictionary of psychology. Washington, DC: American Psychological Association (2007).
19. Paciello, M, Corbelli, G, di Pomponio, I, and Cerniglia, L. Protective role of self-regulatory efficacy: a moderated mediation model on the influence of impulsivity on cyberbullying through moral disengagement. Children. (2023) 10:219. doi: 10.3390/children10020219
20. Kollei, I, Rustemeier, M, Schroeder, S, Jongen, S, Herpertz, S, and Loeber, S. Cognitive control functions in individuals with obesity with and without binge-eating disorder. Int J Eat Disord. (2018) 51:233–40. doi: 10.1002/eat.22824
21. Steward, T, Miranda-Olivos, R, Soriano-Mas, C, and Fernández-Aranda, F. Neuroendocrinological mechanisms underlying impulsive and compulsive behaviors in obesity: a narrative review of fMRI studies. Rev Endocr Metab Disord. (2019) 20:263–72. doi: 10.1007/s11154-019-09515-x
22. Garcia-Garcia, I, Neseliler, S, Morys, F, Dadar, M, Yau, YHC, Scala, SG, et al. Relationship between impulsivity, uncontrolled eating and body mass index: a hierarchical model. Int J Obes. (2022) 46:129–36. doi: 10.1038/s41366-021-00966-4
23. Saari, T, Smith, EE, and Ismail, ZJIP. Network analysis of impulse dyscontrol in mild cognitive impairment and subjective cognitive decline. Int Psychogeriatr. (2022) 34:553–62. doi: 10.1017/S1041610220004123
24. Hamvai, C, Kiss, H, Vörös, H, Fitzpatrick, KM, Vargha, A, and Pikó, BF. Association between impulsivity and cognitive capacity decrease is mediated by smartphone addiction, academic procrastination, bedtime procrastination, sleep insufficiency and daytime fatigue among medical students: a path analysis. BMC Med Educ. (2023) 23:537. doi: 10.1186/s12909-023-04522-8
25. Zehra, SA, Shah, HH, and Jaffer, SM. Impulsivity and obesity: Unraveling the four facets. Eating-Pathology and Causes. (2023).
26. Sánchez-SanSegundo, M, Zaragoza-Martí, A, Martin-LLaguno, I, Berbegal, M, Ferrer-Cascales, R, and Hurtado-Sánchez, JA. The role of BMI, body fat mass and visceral fat in executive function in individuals with overweight and obesity. Nutrients. (2021) 13:2259. doi: 10.3390/nu13072259
27. Xu, C, Lin, N, Shen, Z, Xie, Z, Xu, D, Fu, J, et al. Bedtime procrastination related to loneliness among Chinese university students during post-pandemic period: a moderated chain mediation model. BMC Public Health. (2024) 24:491. doi: 10.1186/s12889-024-18019-6
28. Zhong, Y, He, J, Luo, J, Zhao, J, Cen, Y, Wu, Y, et al. The mediating role of impulsivity between sleep quality and suicidal ideation in adolescent population: a multicenter cross-sectional study in the northeastern Sichuan, China. Front Psych. (2024) 15:1301221. doi: 10.3389/fpsyt.2024.1301221
29. Abe, T, Hagihara, A, and Nobutomo, KJJOA. Sleep patterns and impulse control among Japanese junior high school students. J Adolesc. (2010) 33:633–41. doi: 10.1016/j.adolescence.2009.11.007
30. Killgore, WD, and Balkin, TJ. Wesensten, impaired decision making following 49 h of sleep deprivation. J Sleep Res. (2006) 15:7–13. doi: 10.1111/j.1365-2869.2006.00487.x
31. Saksvik-Lehouillier, I, Saksvik, SB, Dahlberg, J, Tanum, TK, Ringen, H, Karlsen, HR, et al. Mild to moderate partial sleep deprivation is associated with increased impulsivity and decreased positive affect in young adults. Sleep. (2020) 43:zsaa078. doi: 10.1093/sleep/zsaa078
32. Liu, J, Zhu, L, and Liu, C. Sleep quality and self-control: the mediating roles of positive and negative affects. Front Psychol. (2020) 11:607548. doi: 10.3389/fpsyg.2020.607548
33. Guerrero, MD, Barnes, JD, Walsh, JJ, Chaput, JP, Tremblay, MS, and Goldfield, GS. 24-hour movement behaviors and impulsivity. Pediatrics. (2019) 144:187. doi: 10.1542/peds.2019-0187
34. Kohanmoo, A, Kazemi, A, Zare, M, and Akhlaghi, M. Gender-specific link between sleep quality and body composition components: a cross-sectional study on the elderly. Sci Rep. (2024) 14:8113. doi: 10.1038/s41598-024-58801-5
35. Huang, T, Chen, Z, Shen, L, Fan, X, and Wang, K. Associations of cognitive function with BMI, body fat mass and visceral fat in young adulthood. Medicina (Kaunas). (2019) 55:221. doi: 10.3390/medicina55060221
36. Karlsson, IK, Gatz, M, Arpawong, TE, Dahl Aslan, AK, and Reynolds, CA. The dynamic association between body mass index and cognition from midlife through late-life, and the effect of sex and genetic influences. Sci Rep. (2021) 11:7206. doi: 10.1038/s41598-021-86667-4
37. Hur, S, Oh, B, Kim, H, and Kwon, O. Associations of diet quality and sleep quality with obesity. Nutrients. (2021) 13:181. doi: 10.3390/nu13093181
38. Jiang, C, Cai, S, and Zhang, L. Functional connectivity of white matter and its association with sleep quality. Nat Sci Sleep. (2023) 15:287–300. doi: 10.2147/NSS.S406120
39. Owens, MM, Hyatt, CS, Xu, H, Thompson, MF, Miller, JD, Lynam, DR, et al. Test-retest reliability of the neuroanatomical correlates of impulsive personality traits in the adolescent brain cognitive development study. J Psychopathol Clin Sci. (2023) 132:779–92. doi: 10.1037/abn0000832
40. Xu, H, MacKillop, J, and Owens, MM. A machine learning-derived neuroanatomical pattern predicts delayed reward discounting in the human connectome project young adult sample. J Neurosci Res. (2023) 101:1125–37. doi: 10.1002/jnr.25185
41. Li, G, Zhang, S, le, TM, Tang, X, and Li, CSR. Neural responses to reward in a gambling task: sex differences and individual variation in reward-driven impulsivity. Cereb Cortex Commun. (2020) 1:tgaa025. doi: 10.1093/texcom/tgaa025
42. Myerson, J, Green, L, and Warusawitharana, M. Area under the curve as a measure of discounting. J Exp Anal Behav. (2001) 76:235–43. doi: 10.1901/jeab.2001.76-235
43. Cohen, DE, Kim, H, Levine, A, Devanand, DP, Lee, S, and Goldberg, TE. Effects of age on the relationship between sleep quality and cognitive performance: findings from the human connectome project-aging cohort. Int Psychogeriatr. (2023) 36:1171–81. doi: 10.1017/S1041610223000911
44. Wang, J, Dong, D, Liu, Y, Yang, Y, Chen, X, He, Q, et al. Multivariate resting-state functional connectomes predict and characterize obesity phenotypes. Cereb Cortex. (2023) 33:8368–81. doi: 10.1093/cercor/bhad122
45. Hayes, AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York: Guilford Publications (2017).
46. Hayes, AF. PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling. Kansas: University of Kansas (2012).
47. Lee, CM, Woodward, M, Batty, GD, Beiser, AS, Bell, S, Berr, C, et al. Association of anthropometry and weight change with risk of dementia and its major subtypes: a meta-analysis consisting 2.8 million adults with 57 294 cases of dementia. Obes Rev. (2020) 21:e12989. doi: 10.1111/obr.12989
48. Mamrot, P, Hanć, TJN, and Reviews, B. The association of the executive functions with overweight and obesity indicators in children and adolescents: a literature review. Neurosci Biobehav Rev. (2019) 107:59–68. doi: 10.1016/j.neubiorev.2019.08.021
49. Tanaka, H, Gourley, DD, Dekhtyar, M, and Haley, AP. Cognition, brain structure, and brain function in individuals with obesity and related disorders. Curr Obes Rep. (2020) 9:544–9. doi: 10.1007/s13679-020-00412-y
50. Zhang, Y, Huang, B, Yang, W, Zhong, S, Lai, S, Zhao, H, et al. Correlations between endocrine hormones and cognitive function in patients with obesity: a cross-sectional study. Obes Surg. (2022) 32:2299–308. doi: 10.1007/s11695-022-06076-y
51. Smith, L, Toussaint, L, Micoli, A, and Lynch, B. Obesity, putative biological mediators, and cognitive function in a national sample of children and adolescents. Prev Med. (2021) 150:106659. doi: 10.1016/j.ypmed.2021.106659
52. Durlak, JA, Mahoney, JL, and Boyle, AEJPB. What we know, and what we need to find out about universal, school-based social and emotional learning programs for children and adolescents: a review of meta-analyses and directions for future research. Psychol Bull. (2022) 148:765–82. doi: 10.1037/bul0000383
53. Fu, J, Xu, C, Yan, W, and Li, L. The effect of intolerance of uncertainty on state anxiety in the regular epidemic prevention and control phase in the context of Informatization: a moderated chain mediation model. Appl Res Qual Life. (2023) 18:1849–73. doi: 10.1007/s11482-023-10165-0
54. Putra, IGNE, Daly, M, Sutin, A, Steptoe, A, and Robinson, E. The psychological legacy of past obesity and early mortality: evidence from two longitudinal studies. BMC Med. (2023) 21:448. doi: 10.1186/s12916-023-03148-3
55. Du, C, Adjepong, M, Zan, MC, Cho, MJ, Fenton, JI, Hsiao, PY, et al. Gender differences in the relationships between perceived stress, eating behaviors, sleep, dietary risk, and body mass index. Nutrients. (2022) 14:1045. doi: 10.3390/nu14051045
56. Pearl, RL, Puhl, RM, Lessard, LM, Himmelstein, MS, and Foster, GD. Prevalence and correlates of weight bias internalization in weight management: a multinational study. SSM Popul Health. (2021) 13:100755. doi: 10.1016/j.ssmph.2021.100755
57. Nummenmaa, L, Hirvonen, J, Hannukainen, JC, Immonen, H, Lindroos, MM, Salminen, P, et al. Dorsal striatum and its limbic connectivity mediate abnormal anticipatory reward processing in obesity. PLoS One. (2012) 7:e31089. doi: 10.1371/journal.pone.0031089
58. Mallampalli, MP, and Carter, CL. Exploring sex and gender differences in sleep health: a Society for Women's Health Research report. J Womens Health (Larchmt). (2014) 23:553–62. doi: 10.1089/jwh.2014.4816
59. Schorr, M, Dichtel, LE, Gerweck, AV, Valera, RD, Torriani, M, Miller, KK, et al. Sex differences in body composition and association with cardiometabolic risk. Biol Sex Differ. (2018) 9:28. doi: 10.1186/s13293-018-0189-3
60. Liu, X, Xu, W, Wang, Y, Williams, JMG, Geng, Y, Zhang, Q, et al. Can inner peace be improved by mindfulness training: a randomized controlled trial. Stress Health. (2015) 31:245–54. doi: 10.1002/smi.2551
61. Xu, C, Shen, Z, Lin, N, Xie, Z, Xie, L, Wang, Z, et al. The effect of COVID-19 information overload on emotional eating in post-pandemic period in China: the mediating role of fear of COVID-19 and the moderating role of self-compassion. Appl Res Qual Life. (2023) 18:2935–54. doi: 10.1007/s11482-023-10213-9
Keywords: BMI, general cognitive ability, sleep quality, impulsive trait, chain mediation model, gender differences
Citation: Lv K, Xu S, Sun Y, Zhou R, Xu H, He J, Xu C, Xu H, Xu J and Qian J (2025) How individual BMI affected general cognitive ability in young adults: a moderated chain mediation model. Front. Public Health. 13:1559582. doi: 10.3389/fpubh.2025.1559582
Received: 13 January 2025; Accepted: 07 March 2025;
Published: 20 March 2025.
Edited by:
Yibo Wu, Peking University, ChinaReviewed by:
Sussanne Reyes, University of Chile, ChileCopyright © 2025 Lv, Xu, Sun, Zhou, Xu, He, Xu, Xu, Xu and Qian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jing Xu, eGpAd211LmVkdS5jbg==; Hui Xu, aHVpeHVAZ21haWwuY29t; Cheng Xu, eHU0MTMyOTRAMTYzLmNvbQ==; Jun Qian, cWlhbmp1bkB3bXUuZWR1LmNu
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.