
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 07 February 2025
Sec. Digital Public Health
Volume 13 - 2025 | https://doi.org/10.3389/fpubh.2025.1542477
 Walid Al-Qerem1
Walid Al-Qerem1 Osama N. Fadhil1
Osama N. Fadhil1 Anan Jarab2,3
Anan Jarab2,3 Alaa Hammad1
Alaa Hammad1 Fawaz Al-Asmari4
Fawaz Al-Asmari4 Rahaf Zidan1
Rahaf Zidan1 Judith Eberhardt5*
Judith Eberhardt5*Introduction: Amidst the rapid digitalization of healthcare, there is a need for tools that accurately assess eHealth literacy across cultural contexts. This study focused on the validation of an Arabic version of the eHealth Literacy Questionnaire (eHLQ), a tool to facilitate patient engagement and health outcomes in digital healthcare.
Method: Using a convenience sampling method, the study recruited a diverse sample of 657 participants from Jordan (58.9% females and 41.1% males).
Results: Confirmatory Factor Analysis and Rasch analysis supported a six-factor model and demonstrated satisfactory item performance within established thresholds. The findings revealed good internal consistency with Cronbach’s α ranging between ranging between 0.71 to 0.84. Differential Item Functioning analysis indicated no gender-specific variations.
Discussion: The validated Arabic eHLQ is a reliable tool that can help in supporting the development of tailored interventions to improve healthcare delivery in Arabic-speaking regions.
Health literacy involves understanding and interpreting health information to make health-related decisions (1). Education, health awareness, and the skills needed to read and interpret medicine bottles, appointment slips, transit cards, and doctor’s orders are all part of health literacy. It equips individuals with the ability to navigate the complex world of health care and disease management (2). Health literacy is essential for accessing and using healthcare. It enables individuals to make informed choices by understanding health issues, diseases, and treatment options (1).
Healthcare systems face the challenge of managing an increasing volume of healthcare-related information and clinical records (3). Simultaneously, evolving information technology offers solutions by enabling the management of vast amounts of information through computerized storage of health records (4, 5). The advent of computer technologies has prompted healthcare officials to prioritize their integration within the healthcare system. This initiative has proven effective in sectors such as laboratories and pharmacies (6). Norman and Skinner (7) proposed the concept of e-health literacy, which refers to the capacity to effectively access, locate, and evaluate health-related information from electronic sources in order to address health-related issues. E-health literacy encompasses six fundamental competencies: traditional literacy, which includes reading, understanding, communicating, and writing; health literacy, focused on accessing, comprehending, evaluating, and applying health-related information; information literacy, which entails the effective access and use of information; media literacy, involving the ability to select, understand, evaluate, and create media-based messages; scientific literacy, which uses scientific methods to understand, evaluate, and explain health situations; and computer literacy, particularly in troubleshooting computer issues. Successful use of eHealth resources requires individuals to possess digital health literacy skills.
Low health literacy has been linked to poorer health outcomes and increased healthcare disparities, which makes it an essential area of focus in public health interventions (8). With the increasing reliance on digital health platforms, individuals without adequate eHealth literacy may face additional barriers to accessing healthcare and using digital resources effectively (9).
Assessing eHealth literacy is essential for understanding the use of eHealth platforms and resources. One of the first tools that was developed to assess health literacy was the eHealth Literacy Scale (eHEALS) (9), which remains a widely used tool that was applied to evaluate eHealth literacy and its impact on different health outcomes in different settings and populations (10, 11). However, the connections between these studies’ findings and specific eHealth recommendations were generally unclear (10). Furthermore, as noted by eHEALS author (12), the digital environment had substantially evolved since 2006, especially in terms of interactivity and information and communication technologies (ICT) capabilities and suggested revising the eHealth Literacy concept and eHEALS. Moreover, the studies that evaluated the construct of the eHEALS produced inconsistent results related to the number of factors and the distribution of the items between the different factors (13–19).
To overcome these drawbacks the eHealth Literacy Questionnaire (eHLQ) (20) was developed. The tool is a 35-item measure comprising seven domains of eHealth literacy. It measures various domains of eHealth literacy such as using technology to process health information, understanding electronic health information, finding reliable electronic health information, engaging with digital health services, feeling secure when using eHealth resources, and being motivated to engage with digital health. While this questionnaire has been validated in English, Danish, and Norwegian populations, no equivalent tool currently exists for Arabic-speaking populations, despite the significant number of Arabic speakers globally (21) and their growing engagement with digital health platforms (22).
The present study aimed to validate, assess for trustworthiness, and test the stability of the Arabic eHLQ among Jordanian adults. Jordan, with its high internet penetration rate and increasing reliance on digital health platforms (23), provided an ideal setting for this study. By evaluating Arabic speakers’ electronic health literacy with a validated and culturally appropriate questionnaire, the study aimed to aid healthcare providers and researchers in designing targeted interventions to improve health literacy and health outcomes.
This cross-sectional study collected data using both paper-based and electronic questionnaires. Data was collected at a single time point from participants. Ethical approval was obtained from Al-Zaytoonah University of Jordan (Ref no:03/2023-2024), and the study adhered to the Declaration of Helsinki’s ethical principles for medical research involving human subjects.
This study employed a convenience sampling method. A participant-to-item ratio of 10:1 was used to obtain the required sample size for factor analysis (24). The study targeted all citizens residing in Jordan as its population. To ensure geographical representation, participants were recruited from various central regions across the country. Inclusion criteria required participants to be Jordanian citizens aged 18 years or older, and literate in reading and writing. Exclusion criteria stipulated that individuals under the age of 18 years and those residing outside Jordan were ineligible to participate in the study. The recruiters were instructed to approach individuals from different age groups and from different sociodemographic statuses.
A total of 657 participants completed the questionnaire. Paper and electronic data collection method was adopted, with approximately one-third of surveys distributed in paper format and the remainder electronically. Distribution channels included community centers, healthcare facilities, and online platforms. Both the online and paper questionnaires included an introductory paragraph that clarified the study’s aim, participants’ rights and roles, inclusion and exclusion criteria, and the consent form.
The survey instrument, consisting of 45 questions, gathered both demographic details and health literacy insights. The demographic data contained ten items to collect data about key sociodemographic aspects, including age, gender, monthly income, presence of chronic illnesses, self-assessed health status, education level, involvement in the medical field (study or work), preferred methods for accessing medical information online, and duration of daily online activity.
The second part of the survey consisted of the Arabic version of eHLQ (20), developed in accordance with the eHealth Literacy Framework (eHLF) proposed by Norgaard et al. (25). This self-report measure is composed of seven dimensions with a total of 35 items: five items for each of the first five dimensions, six items for the sixth dimension, and four items for the seventh dimension. The scale uses an ordinal response format, with responses graded on a Likert scale ranging from 0 (strongly disagree) to 3 (strongly agree). It comprises seven dimensions: 1- using technology to process health information, 2- understanding health concepts and language, 3- ability to actively engage with digital services, 4- feeling safe and in control, 5- motivated to engage, 6- access to working digital services, and 7- digital services that meet individual needs (20).
The eHLQ was chosen by an expert panel composed of two clinical pharmacists and one public health specialist. The selection was based on the questionnaire’s comprehensive coverage of various e-health literacy domains and its use of simplified language. The content validity of the questionnaire was confirmed by the expert panel and by members of the general population. The survey was translated into Modern Standard Arabic following the Brislin principle (26) to ensure that the Arabic version retained the original meaning of the questionnaire with cultural relevance. The forward-backward translation process was conducted by separate independent translators. The translated versions were compared, and a final Arabic version was produced. Thirty participants were recruited for a pilot study to assess the questionnaire’s face validity. Participants were randomly selected and briefed on the study’s purpose. They were asked to complete the questionnaire and participate in an open discussion to provide feedback. Specifically, they were asked to evaluate the relevance, clarity, content and simplicity of the items. Ultimately, the participants confirmed the adequacy of the eHLQ as all the participants found it easy to comprehend and complete, with no further modifications being necessary.
With the advancement of psychometric methods adopted to validate different health tools, the selection of the most adequate method may be demanding (27). The present paper applied Rasch model theory and classical test theory (CTT) to increase the validity and reliability of the study results.
The Statistical Package for the Social Sciences software (SPSS) version 23 (28) and RStudio Software (29) with packages TAM version 4.2–21 (30) and lavaan version 0.6–17 (31) were used for data analysis. All continuous variables were expressed as medians and interquartile ranges. For categorical variables, frequencies and percentages were reported. The internal consistency of each scale was evaluated by computing Cronbach’s alpha and McDonald’s ωt with acceptable values >0.7 (27, 32).
Confirmatory Factor Analysis (CFA) for ordinal data Diagonally Weighted Least Squares (DWLS) estimator was conducted to verify the fitness of the original 7-factor model, and scaled model fit indices, including Comparative Fit Index (CFI), Tucker-Lewis Index (TLI), Root Mean Square Error of Approximation (RSMEA), Standardized Root Mean Square Residual (SRMR), chi-square with degrees of freedom and p-value, and Minimum Discrepancy of Confirmatory Factor Analysis/Degrees of Freedom (CMIN/DF), were computed. The acceptable values were as follows: for CMIN/DF < 5 (33), for RMSEA <0.08 (34), for SRMR ≤0.08 (35) and for TLI and CFI values closer to 1 (36).
Multidimensional Rasch analysis was performed, and item thresholds were examined. Disordered thresholds may indicate irregularity and may arise when respondents fail to select the appropriate response options, which can result from unclear labeling or an excessive number of answer options. Model fit was assessed by computing item/person separation reliability. Item infit and outfit mean square values (MNSQs) were assessed, with acceptable range set between 0.5 and 1.5 (37). Additionally, differential item functioning (DIF) was evaluated to examine potential biases resulting from gender differences with acceptable logit differences of ≥0.43 (38). Moreover, ceiling or floor effects were evaluated by computing the frequency of participants who scored the maximum and minimum possible scores.
Table 1 presents the sociodemographic profile of the study participants. A total of 657 individuals took part. The median age was 26 years, with ages ranging from 22 to 31 years. Regarding gender distribution, 58.9% of participants identified as female and 41.1% as male. In terms of marital status, the majority (62.3%) reported being single, with the remaining 37.7% being married. Regarding income status, 51% reported earning less than 500 Jordanian Dinars (JOD) per month, 35% reported a monthly income between 500 and 1,000 JOD, and 14% earned more than 1,000 JOD per month. Concerning health, 11.4% of participants reported having a chronic disease, while 88.6% indicated no chronic conditions. Additionally, 42.8% of participants reported that at least one family member had a chronic disease, compared to 57.2% who reported no family history of chronic illness.
The participants’ perceptions of their current health status are depicted in Figure 1. The majority of participants rated their health status as 4 out of 5 (46.9%), followed by a rating of 5 out of 5 (27.1%).
Devices that participants used to access medical information online are presented in Figure 2. Most participants used smartphones (85.23%), followed by laptops (26.63%), with tablets being the least used (8.37%). Additionally, 7.30% of participants reported that they did not use the Internet to access medical information.
The evaluation of participants’ eHealth Literacy Questionnaire responses is summarized in Table 2. Most participants agreed or strongly agreed with Q6 (94%), followed by Q4 (92.5%). Conversely, most disagreed or strongly disagreed with Q3 (49%), followed by Q20 (46.6%). All items had a median score of 2.
Most participants indicated agreement or strong agreement across items, with Q7, Q11, and Q13 showing high levels of agreement (median = 2). However, items Q20 and Q25 had notable proportions of disagreement, suggesting variability in ease of use.
Participants generally agreed with items assessing health concept comprehension, as seen in Q5 and Q12 (median = 2), although some disagreement was observed for Q15 (24.5%).
High levels of agreement were reported, particularly for items like Q4 and Q6 (median = 2). Q8 showed a slightly higher disagreement rate (30.6%), which indicated some variability in engagement levels.
Most participants felt safe and in control when using digital health services, with items Q1 and Q10 reflecting strong agreement (median = 2). However, Q14 and Q22 had higher disagreement levels, which suggested some concerns around safety.
The majority agreed with items assessing motivation, such as Q2 and Q19 (median = 2), although Q24 showed more disagreement (34.2%), which indicated mixed motivation levels.
Responses varied, with some participants finding digital services functional and accessible, while others faced usability issues, as reflected in Q3 and Q16 (median = 2).
There was variability in whether services met individual needs. For example, Q18 and Q28 showed high agreement, though Q28 and Q31 had disagreement proportions around 27–30%.
Overall, none of the participants recorded the minimum score of 35, and only 1% achieved the maximum score of 140, indicating the absence of ceiling and floor effects. All items had a median score of 2, showing a general tendency toward agreement.
CFA was conducted to evaluate the 7-factor model suggested in the original questionnaire. However, the covariance matrix of latent variables was not positive definite due to excessive correlation between factors 6 and 7, which prevented model convergence. Consequently, these two factors were combined into a single factor, and a new analysis was conducted using a 6-factor model.
Cronbach’s alphas and McDonald’s ωt of the 6 factors are presented in Table 3. Across all scales, the reliability coefficients were notably high, affirming the internal consistency of the eHLQ and supporting its validity for assessing various aspects of engagement with digital health services. Specifically, all scales exhibited reliability coefficients above 0.7, ranging between 0.71 for Factor 3 to 0.84 for factor 6, confirming their adequacy for research use.
The chi-square test for the 6-factor model was significant (chi-square = 2.032, df = 545, p < 0.001) indicating inadequacy of the model. However, this was expected due to the large sample size; therefore, the method of dividing chi-square by degree of freedom was applied and yielded acceptable CMIN/DF = 3.72. Other scaled model fit indices were also acceptable including RMSEA = 0.064 (90Cl: 0.062–0.068), SRMR = 0.063, CFI = 0.93, and TLI = 0.92. Standardized factor loadings ranged from 0.42 to 0.81. The highest factor loadings were observed for Q14 and Q22 in Factor 4, while the lowest were recorded for Q3 in Factor 6 and only two items were < 0.5. Detailed standardized factor loadings for each item are provided in Table 4.
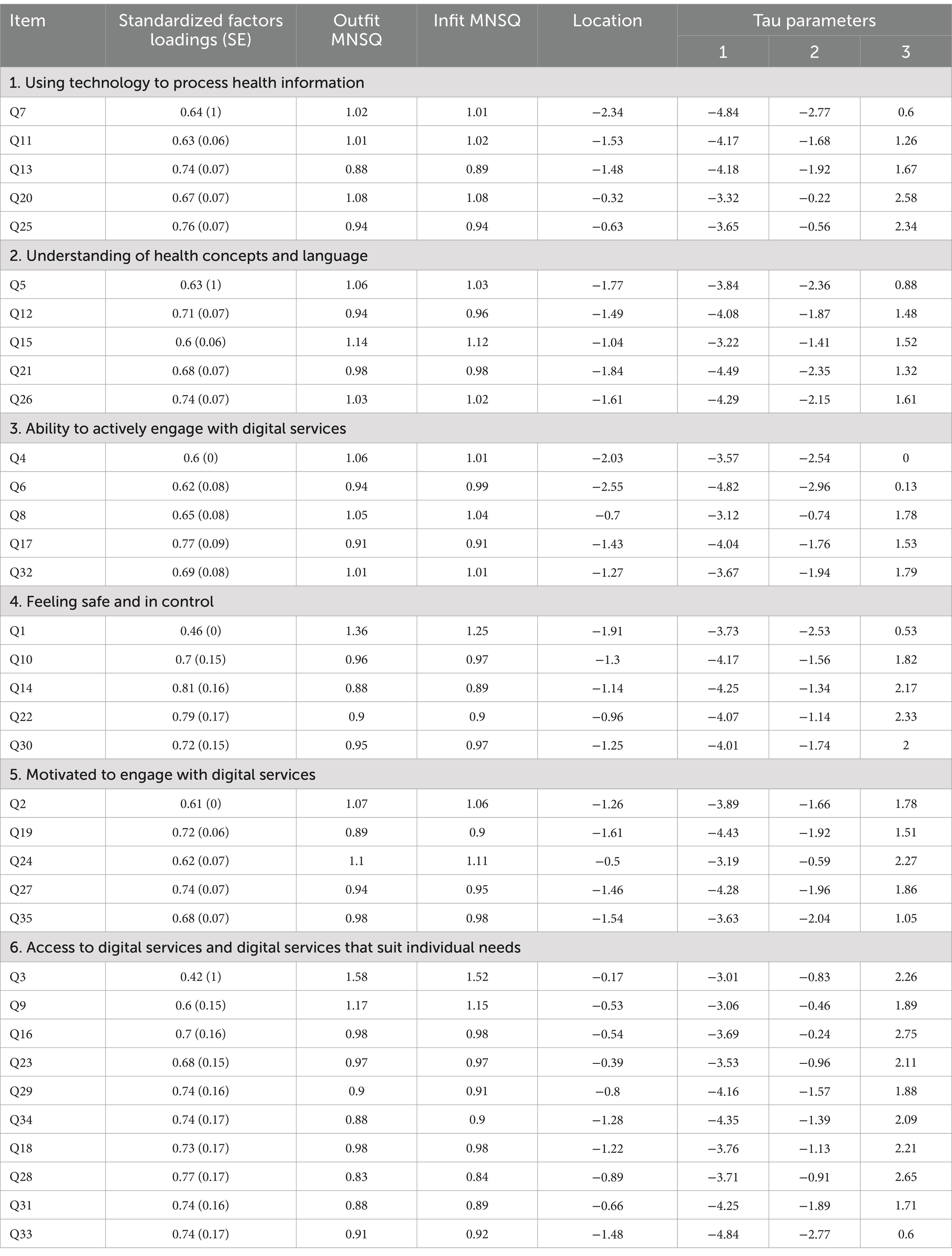
Table 4. Reliability, factor loadings, outfit and infit statistics, item locations, extraction rates, and Andrich-Rasch thresholds of the eHLQ.
A six-dimensional model was analyzed. The person reliability index for the 6 dimensions ranged between 0.68 for dimension 3 to 0.86 for dimension 6, and the item separation reliability ranged between 0.85 for dimension 3 to 0.91 for dimension 6. Table 4 displays the infit and Outfit mean square values, affirming the eHLQ’s ability to differentiate between various participant levels and confirming the model’s item hierarchy. Notably, the only item slightly exceeding the acceptable range was Q3, with an Outfit MNSQ of 1.58 and an infit MNSQ of 1.52. All questions were presented with ordered response categories. Analysis revealed that Q3 was the most challenging item for participants to answer, followed by Q20, whereas Q6 was the most straightforward. Furthermore, the easiest threshold to respond to was the first threshold of Q7, followed by Q6. Conversely, the third threshold of Q23 was identified as the most challenging. Scale 6 recorded the highest outfit and infit values for Q3, at 1.58 and 1.52, respectively. Following this, Scale 4 for Q1 showed values of 1.36 for outfit and 1.26 for infit. The lowest values were observed on Scale 6 for Q28, with outfit and infit values of 0.83 and 0.84, respectively.
DIF between genders was evaluated and the analysis revealed that the difference between the two genders on the logit scale was 0.16 logits, indicating no significant differences in DIFs between the two sexes as the recommended cutoff point is ≥0.43. Figure 3 displays the Wright map, showing that participants were distributed across all difficulty levels in all 6 domains, with the majority concentrated in the middle range. The item thresholds revealed a range of item difficulties, all with well-ordered thresholds.
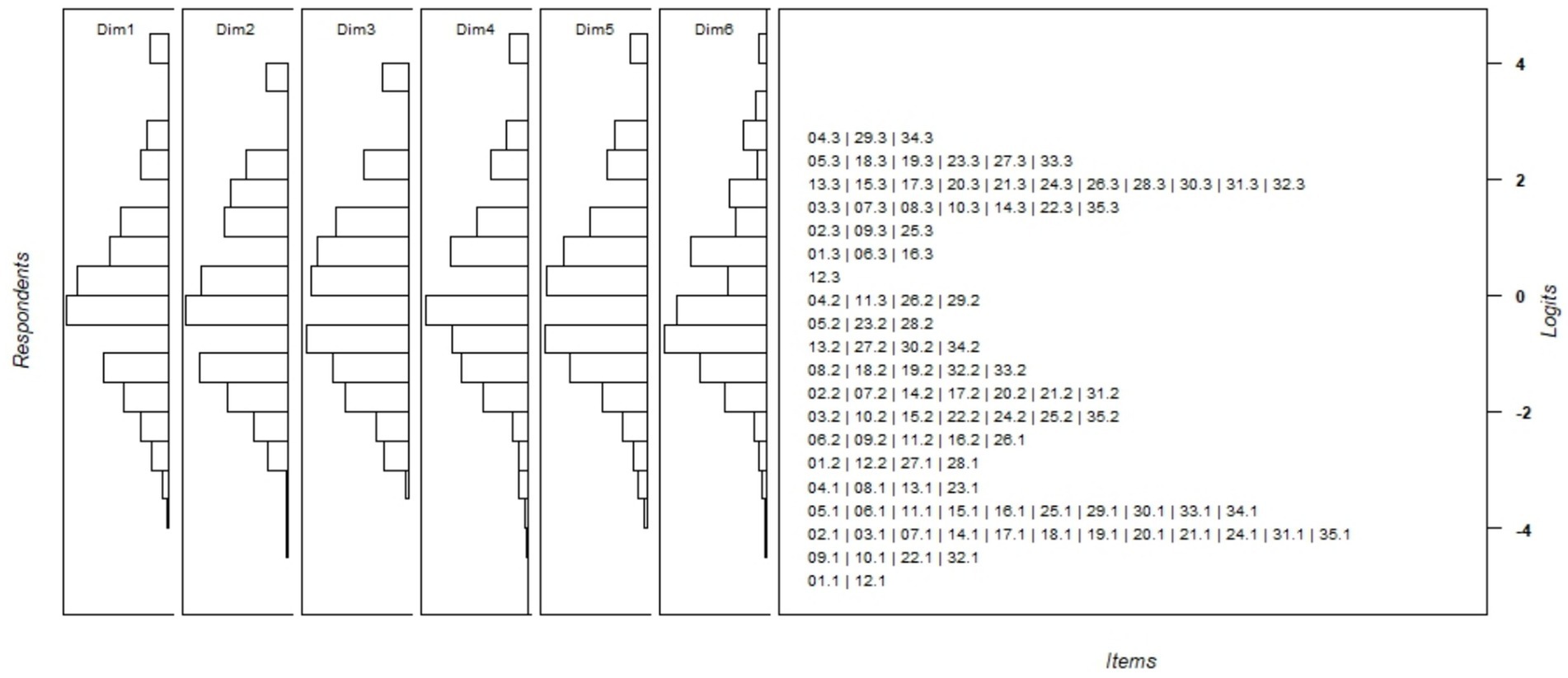
Figure 3. Wright map of the Rasch analysis. The left panel displays the ability level area of the respondents for both factors, while the right panel shows the item difficulty level area.
The current study focused on translating and validating the 35-item eHLQ into Arabic, aiming to facilitate its cross-cultural adaptation for researchers in Arabic-speaking healthcare contexts. The Arabic version of the eHLQ showed strong internal consistency, with acceptable alpha coefficients in all six domains. The results of this study are consistent with those from eHLQ validation studies conducted in other languages (39, 40) confirming the robustness of the questionnaire across different cultural and linguistic settings. In comparison, the reliability of the Arabic version of the eHLQ is on par with, or slightly exceeds, that of its counterparts in other languages. This finding reinforces its utility and robustness in Arabic-speaking healthcare contexts.
Our CFA supported a 6-factor model, which has a different number of factors to the original 7-factor model (20). This adjustment was due to a high correlation between the factors “Access to digital services” and “Digital services that suit individual needs,” which resulted in their combination into a single factor. The merging of these two factors can be theoretically justified, as both assess access to digital services with similar items, such as “eHealth systems provide me with easy ways to get what I need” from the original factor “Digital services that suit individual needs” and “I have access to health technology that works” from the original factor “Access to digital services.” Nevertheless, certain items, such as items 1 and 3, exhibited relatively lower factor loadings. These discrepancies suggest potential challenges in translation or variations in respondents’ perceptions, possibly influenced by demographic characteristics. These findings highlight the importance of further examining these discrepancies to improve the questionnaire’s validity and applicability in diverse cultural settings. Such an investigation could help identify specific cultural or linguistic factors that influence response patterns, thus enhancing the tool’s effectiveness for global health assessments. Addressing these challenges in future iterations may help to refine the tool further and enhance its cross-cultural applicability.
Utilizing Rasch analysis to assess the proposed model fit, most items demonstrated satisfactory fit within acceptable thresholds, except for Item 3 which exhibited a slightly high infit/outfit value, indicating potential under-discrimination. It is important to note that outfit statistics are particularly sensitive to responses to items whose difficulty differs significantly from an individual’s ability level while infit statistics is more sensitive to the pattern of responses to items targeted on the person (41, 42).
This study revealed a pronounced ease of interaction with digital tasks. The thresholds were consistently reasonably low, reflecting ease of engagement with digital health information and motivation to use digital services. Overall, while previous studies identified basic digital tasks as relatively easy, our study highlights a greater comfort and proficiency in using digital health platforms among respondents. Conversely, items Q20, Q5, Q4, Q1, Q35, Q23, and Q31, which were distributed across all the questionnaire domains, were identified as the most challenging, indicating that individuals with physical ailments may struggle to access information on managing mental health issues. These observed variations in participants’ health literacy levels are consistent with the understanding that health literacy encompasses not just knowledge, but also the ability to perform responsibilities and tasks related to health and healthcare effectively. This suggests that health literacy involves a dynamic set of skills that vary widely among individuals, impacting their ability to manage their health and interact with healthcare systems.
Consistent with previous validations of the eHLQ in other languages, the Arabic version exhibited strong reliability and validity. The overall internal consistency (Cronbach’s α = 0.71–0.86) is comparable to or slightly higher than the reliability coefficients reported in Danish (43)(α = 0.75–0.87) and Norwegian populations (α = 0.73–0.90) (20). Similar to these studies, the Arabic eHLQ demonstrated strong performance across multiple domains, particularly in assessing access to digital services and users’ motivation to engage with digital platforms. The merging of Factors 6 and 7 in this study aligns with findings from a prior validation, which reported high correlations between these domains (20). Additionally, certain items (e.g., Q3 and Q20) exhibited higher variability in response patterns, consistent with earlier research highlighting these items as universally challenging across diverse populations. These results reinforce the robustness of the eHLQ framework while emphasizing the importance of contextual adaptations to address subtle cultural differences in item interpretation.
The findings of the present study underscore the robust validity and reliability of the Arabic version of the eHLQ developed in this research, and evidence the proficiency of Jordanian participants in utilizing digital health services, consistent with trends in other cultural contexts. They also have practical implications for healthcare providers, policymakers, and researchers. The validated Arabic eHLQ offers a reliable tool to assess eHealth literacy, enabling the design of targeted interventions to improve digital health engagement in Arabic-speaking populations. For instance, the tool can be used to identify individuals or groups who may benefit from tailored educational programs or digital skill training, thereby promoting equitable access to healthcare resources.
One of the primary strengths of this study is the large sample size, which contributes significantly to the reliability and validity of our findings. A larger sample size helps mitigate random fluctuations and reduce sampling errors, thereby increasing confidence in the study’s results. Such reliability is essential for producing dependable research outcomes that can inform further studies and practical applications.
Furthermore, the substantial sample size facilitated detailed subgroup analyses, which enabled the exploration of nuances and variations among demographic and other relevant factors. This deeper exploration allowed for more insightful conclusions and the identification of important insights that might otherwise be missed.
However, despite these strengths, the study is not without its limitations. Convenience sampling techniques were applied which may be susceptible to selection bias, as certain individuals might be more inclined to participate than others, potentially skewing the results. Nevertheless, the young sample mimics the young Jordanian population, which has a median age of 22.4 years according to the Jordanian High Population Council (44). Moreover, like the present study sample, more than 41% of Jordanian population has a monthly household of less than 500 JDs (45). Furthermore, the study’s aim was to validate the tool within the general population. Additionally, with this being a study based on self-report, it may have been left susceptible to recall and social desirability biases, where participants may not have accurately remembered past events or may have responded in a manner they perceived as favorable rather than truthful. Although the present study went through a systemic translation process, semantic bias cannot be completely excluded.
Future research could benefit from employing a more stratified sampling technique to minimize selection bias and ensure a more representative cross-section of the population, including targeting special populations such as the older adult, patients of different chronic diseases, low education levels and rural residents. Additionally, to mitigate the effects of recall and social desirability biases inherent in self-report studies, future investigations could implement mixed methods approaches that include qualitative interviews could also provide deeper insights into the motivations behind participants’ responses, offering a more nuanced understanding of their health literacy and digital engagement. Finally, although this study applied rigorous validation methodology it did not evaluate test-rest reliability which could be conducted in future research.
This study provides a comprehensive development and evaluation of the Arabic version of the eHLQ, focusing on its accuracy, reliability, and applicability within Arabic-speaking populations. The findings demonstrate that the Arabic translation of the eHLQ maintains a high level of internal consistency, comparable to or surpassing the reliability of versions in other languages. CFA and Rasch analysis both supported the tool’s effectiveness, with the single-factor model fitting adequately and most items performing well within acceptable thresholds. With the six-factor model demonstrating adequate fit and most items performing well within acceptable thresholds. With this validation, the questionnaire can now be used to assess the e-health literacy of Arabic-speaking populations. This is crucial for enhancing health outcomes and facilitating greater patient involvement in digital healthcare settings.
The study’s findings provide useful insights for healthcare policymakers and practitioners aiming to improve digital health practices in Jordan and other Arabic-speaking countries. By utilizing a culturally and linguistically customized eHLQ, health workers can gain a deeper understanding of patients’ e-health literacy. This understanding, in turn, facilitates the enhancement of digital health resource utilization among patients in these countries. Such targeted improvements in e-health literacy can promote more effective and inclusive digital healthcare services, ultimately fostering better health outcomes.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Al-Zaytoonah University of Jordan (Ref no:03/2023-2024). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
WA-Q: Conceptualization, Data curation, Methodology, Validation, Visualization, Writing – original draft, Writing – review & editing. OF: Investigation, Resources, Writing – original draft. AJ: Conceptualization, Supervision, Validation, Writing – original draft. AH: Writing – original draft, Writing – review & editing. FA-A: Writing – original draft, Writing – review & editing. RZ: Formal analysis, Investigation, Writing – original draft. JE: Software, Writing – original draft, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the researchers supporting project number (RSP2025R235), King Saud University, Riyadh, Saudi Arabia.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors declare that no Gen AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Liu, C, Wang, D, Liu, C, Jiang, J, Wang, X, Chen, H, et al. What is the meaning of health literacy? A systematic review and qualitative synthesis. Fam Med Commun Health. (2020) 8:e000351. doi: 10.1136/fmch-2020-000351
2. Nielsen-Bohlman, L, Panzer, AM, and Kindig, DA. What is health literacy? (2004). Available at: https://www.ncbi.nlm.nih.gov/books/NBK216035/ (Accessed August 26, 2024).
3. Dash, S, Shakyawar, SK, Sharma, M, and Kaushik, S. Big data in healthcare: management, analysis and future prospects. J Big Data. (2019) 6:1–25. doi: 10.1186/S40537-019-0217-0/FIGURES/6
4. Kohli, R, and Tan, SS-L. How can IS researchers contribute to transforming healthcare? MIS Q. (2016) 40:553–74. doi: 10.25300/MISQ/2016/40.3.02
5. Malak, M, and Al-Shakanbeh, M. Factors correlate acceptance of applying electronic health solution records among emergency nurses. J Hum Behav Soc Environ. (2024) 34:119–29. doi: 10.1080/10911359.2023.2177228
6. Nazer, LH, and Tuffaha, H. Health care and pharmacy practice in Jordan. Can J Hosp Pharm. (2017) 70:150–5. doi: 10.4212/cjhp.v70i2.1649
7. Norman, CD, and Skinner, HA. eHealth literacy: essential skills for consumer health in a networked world. J Med Internet Res. (2006) 8:e9. doi: 10.2196/JMIR.8.2.E9
8. Sørensen, K, Van den Broucke, S, Fullam, J, Doyle, G, Pelikan, J, Slonska, Z, et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. (2012) 12:80. doi: 10.1186/1471-2458-12-80
9. Norman, CD, and Skinner, HA. eHEALS: the eHealth literacy scale. J Med Internet Res. (2006) 8:e507. doi: 10.2196/jmir.8.4.e27
10. Griebel, L, Enwald, H, Gilstad, H, Pohl, AL, Moreland, J, and Sedlmayr, M. eHealth literacy research—quo vadis? Inform Health Soc Care. (2018) 43:427–42. doi: 10.1080/17538157.2017.1364247
11. Karnoe, A, and Kayser, L. How is eHealth literacy measured and what do the measurements tell us? A systematic review. Knowledge Management E-Learning. (2015) 7:576–600. doi: 10.34105/J.KMEL.2015.07.038
12. Norman, C . eHealth literacy 2.0: problems and opportunities with an evolving concept. J Med Internet Res. (2011) 13:e125. doi: 10.2196/JMIR.2035
13. Dale, JG, Lüthi, A, Skaraas, BF, Rundereim, T, and Dale, B. Testing measurement properties of the norwegian version of electronic health literacy scale (EHEALS) in a group of day surgery patients. J Multidiscip Healthc. (2020) 13:241–7. doi: 10.2147/JMDH.S242985
14. Gazibara, T, Cakic, J, Cakic, M, Pekmezovic, T, and Grgurevic, A. EHealth and adolescents in Serbia: psychometric properties of eHeals questionnaire and contributing factors to better online health literacy. Health Promot Int. (2019) 34:770–8. doi: 10.1093/HEAPRO/DAY028
15. Soellner, R, Huber, S, and Reder, M. The concept of ehealth literacy and its measurement: German translation of the eHEALS. J Media Psychol. (2014) 26:29–38. doi: 10.1027/1864-1105/A000104
16. Richtering, SS, Hyun, K, Neubeck, L, Coorey, G, Chalmers, J, Usherwood, T, et al. EHealth literacy: predictors in a population with moderate-to-high cardiovascular risk. JMIR. Hum Factors. (2017) 4:e4. doi: 10.2196/HUMANFACTORS.6217
17. Hyder, SN, Ali Hasan, AK, and Mehmood, N. Poor lipid control among coronary heart disease patients receiving statins in India. Clin Exp. Cardiol. (2015) 6:795–7. doi: 10.4172/2155-9880.C1.027
18. Paige, SR, David Miller, M, Krieger, JL, Stellefson, M, and Cheong, JW. Electronic health literacy across the lifespan: measurement invariance study. J Med Internet Res. (2018) 20:e10434. doi: 10.2196/10434
19. Sudbury-Riley, L, FitzPatrick, M, and Schulz, PJ. Exploring the measurement properties of the eHealth literacy scale (eHEALS) among baby boomers: a multinational test of measurement invariance. J Med Internet Res. (2017) 19:e53. doi: 10.2196/JMIR.5998
20. Kayser, L, Karnoe, A, Furstrand, D, Batterham, R, Christensen, KB, Elsworth, G, et al. A multidimensional tool based on the eHealth literacy framework: development and initial validity testing of the eHealth literacy questionnaire (eHLQ). J Med Internet Res. (2018) 20:e8371. doi: 10.2196/jmir.8371
21. WorldData.info . Arabic speaking countries. (2024). Available at: https://www.worlddata.info/languages/arabic.php (Accessed December 22, 2024).
22. Rjoop, A, Zaied, MA, Al Rabadi, B, Gharib, L, Naser, M, Tayih, RA, et al. Navigating the digital landscape: telemedicine and e-health utilisation in non-communicable diseases in the Arab world: a systematic review. Global Digital Health Knowledge Exchange Empowerment Conference. (2024) 2024:1–8. doi: 10.1109/gDigiHealth.KEE62309.2024.10761413
23. World Population Review . Internet penetration by country 2024. (2024). Available at: https://worldpopulationreview.com/country-rankings/internet-penetration-by-country (Accessed December 22, 2024).
25. Norgaard, O, Furstrand, D, Klokker, L, Karnoe, A, Batterham, R, Kayser, L, et al. The e-health literacy framework: a conceptual framework for characterizing e-health users and their interaction with e-health systems. Knowledge Management E-Learning Int J. (2015) 7:522–40. doi: 10.34105/J.KMEL.2015.07.035
26. Brislin, RW . Back-translation for cross-cultural research. J Cross Cult Psychol. (1970) 1:185–216. doi: 10.1177/135910457000100301
27. Xu, RH, Wong, EL, Lu, SY, Zhou, L, Chang, J, and Wang, D. Validation of the Toronto empathy questionnaire (TEQ) among medical students in China: analyses using three psychometric methods. Front Psychol. (2020) 11:810. doi: 10.3389/fpsyg.2020.00810
28. IBM Corp . IBM SPSS statistics for windows. (2015). BM Corp. Released 2015. IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY: IBM Corp.
30. Robitzsch, A, Kiefer, T, and Wu, M. TAM: test analysis modules. (2024). Available at: https://cran.r-project.org/web/packages/TAM/index.html
31. Rosseel, Y . Lavaan: an R package for structural equation modeling. J Stat Softw. (2012) 48:1–36. doi: 10.18637/JSS.V048.I02
32. DeVellis, RF, and Thorpe, CT. Scale development: theory and applications. 5th ed. Thousand oaks, CA: SAGE Publications (2022).
33. Marsh, HW, and Hocevar, D. Application of confirmatory factor analysis to the study of self-concept: first- and higher order factor models and their invariance across groups. Psychol Bull. (1985) 97:562–82. doi: 10.1037/0033-2909.97.3.562
34. MacCallum, RC, Browne, MW, and Sugawara, HM. Power analysis and determination of sample size for covariance structure modeling. Psychol Methods. (1996) 1:130–49. doi: 10.1037/1082-989X.1.2.130
35. Hu, L, and Bentler, PM. Fit indices in covariance structure modeling: sensitivity to underparameterized model misspecification. Psychol Methods. (1998) 3:424–53. doi: 10.1037/1082-989X.3.4.424
36. Schumacker, RELRG . A beginner’s guide to structural equation modeling. New York: Psychology Press (2004).
37. Linacre, JM . What do infit and outfit, mean-square and standardized mean? Sci Res. (2002) 16:878.
38. An Adjustment for Sample Size in DIF Analysis . Available at: https://www.rasch.org/rmt/rmt203e.htm (Accessed November 2, 2024).
39. Sjöström, AE, Hajdarevic, S, Hörnsten, Å, Kristjánsdóttir, Ó, Castor, C, and Isaksson, U. The Swedish version of the eHealth literacy questionnaire: translation, cultural adaptation, and validation study. J Med Internet Res. (2023) 25:e43267. doi: 10.2196/43267
40. Cheng, C, Elsworth, GR, and Osborne, RH. Validity evidence of the eHealth literacy questionnaire (eHLQ) part 2: mixed methods approach to evaluate test content, response process, and internal structure in the Australian community health setting. J Med Internet Res. (2022) 24:e32777. doi: 10.2196/32777
41. Linacre, J. Comparing and choosing between “partial credit models” (PCM) and “rating scale models” (RSM). Rasch Measurement Transactions. (2000). Available at: https://www.rasch.org/rmt/rmt143k.htm (Accessed November 27, 2019).
42. Wright, B, and Linacre, J. Reasonable mean-square fit values. Rasch Measurement Transform. (1994) 8:370.
43. Hermansen, Å, Andersen, MH, Borge, CR, Dahl, KG, Larsen, MH, Lønning, K, et al. Preliminary validity testing of the eHealth literacy questionnaire (eHLQ): a confirmatory factor analysis (CFA) in Norwegian hospitalized patients. BMC Psychol. (2023) 11:409. doi: 10.1186/s40359-023-01449-z
44. General Secretariat Higher Population Council . Jordan-recent demographic indicators (April 2024) changes in population size of the Hashemite Kingdom of Jordan since the beginning of the millennium. (2024). Available at: http://dosweb.dos.gov.jo/DataBank/Population_Estimares/PopulationEstimates.pdf (Accessed November 2, 2024).
45. Department of Statistics . Population and housing. Amman. (2024). Available at: https://dosweb.dos.gov.jo/DataBank/household/2017/G3/Table3G3_Jor.pdf (Accessed December 22, 2024).
Keywords: eHealth, health literacy, validation, Confirmatory Factor Analysis, Rasch analysis, cultural contexts
Citation: Al-Qerem W, Fadhil ON, Jarab A, Hammad A, Al-Asmari F, Zidan R and Eberhardt J (2025) Validation of the Arabic eHealth literacy questionnaire: a factor and Rasch analysis study. Front. Public Health. 13:1542477. doi: 10.3389/fpubh.2025.1542477
Received: 09 December 2024; Accepted: 28 January 2025;
Published: 07 February 2025.
Edited by:
Wei Wang, Chongqing Medical University, ChinaReviewed by:
Richard Xu, Hong Kong Polytechnic University, Hong Kong SAR, ChinaCopyright © 2025 Al-Qerem, Fadhil, Jarab, Hammad, Al-Asmari, Zidan and Eberhardt. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Judith Eberhardt, ai5lYmVyaGFyZHRAdGVlcy5hYy51aw==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.