
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 05 March 2025
Sec. Substance Use Disorders and Behavioral Addictions
Volume 13 - 2025 | https://doi.org/10.3389/fpubh.2025.1533051
This article is part of the Research Topic Innovations in Recovery Science: Pathways, Policies, and Platforms that Promote Thriving After Addiction View all 11 articles
Introduction: Peer recovery support services (PRSS) are flexible, evidence-informed interventions that can be provided in a variety of settings and are delivered by credentialed people with lived-experience of mental health and substance use disorders. PRSS are a promising intervention that may increase linkage to care, treatment retention, and long-term recovery; however, there remains a sizable gap in the literature to disseminate these services to scale. Misunderstanding of the peer worker role, and a lack of consistent nomenclature to describe PRSS activities are barriers to studying PRSS effectiveness.
Methods: This sequential exploratory mixed-methods study began with a qualitative and methodological review of a previous peer worker survey instrument by eight subject matter experts with lived experience of substance use disorder. The improved 38-item web-based survey was then disseminated to a non-probability sample of peer workers in nine U.S. states.
Results: A total of 659 peer workers responded to the survey indicating that they perform an average of 24 different service activities most of the time (M = 23.6; SD = 16.7). PRSS interventions were most commonly delivered in communities and neighborhoods, client homes, and recovery community organizations. Survey participants reported spending approximately half of their time (M = 43.1, SD = 26.1) providing Emotional support, and less than one quarter of their time providing Affiliational (M = 21.3%; SD = 18.5), Informational (M = 18.0%; SD = 15.5), and Instrumental (M = 15.0%; SD = 15.3) support.
Discussion: This study may be the first of its kind to explore the broad array of service activities peer workers perform in multiple settings across regional service networks, also known as recovery ecosystems. Notably, peer worker respondents selected an average of 24 activities that they perform most of the time, and Emotional support was the most commonly delivered support type. Study results provide preliminary evidence about where PRSS are performed within both macro and micro settings indicating that services are frequently delivered in non-clinical community-based settings and client homes which may confer added benefit. These results can be used to inform future studies that examine the effectiveness of PRSS across the continuum of care.
It is estimated that 48.5 million people in the U.S. are living with a substance use disorder (1). Overdose deaths, driven by illicit fentanyl, reached an all-time high in 2023, exceeding 112,000 in a 12-month period (2). Encouraging new estimates from 2024 suggest that overdose deaths may be on the decline and decreasing significantly in some areas of the country; and yet, overdose is still the leading cause of death among Americans between ages 18–25 years (3). Every 4 and ½ minutes a drug-related death occurs in the U.S. despite increases in federal funding to control the illicit fentanyl supply and policy-level changes that improve access to opioid overdose reversal medications (4). Moreover, certain populations, such as older Black men (5) and Native Americans (6), are now at even greater risk than ever before.
There are currently more than 17,000 drug treatment programs in the U.S.; however, limited regulations, inconsistent treatment protocols, and stigma against effective medications are leaving many vulnerable (4). Medications for opioid use disorder (MOUD) are considered the gold standard for treating opioid use disorder (OUD) and are proven to save lives and increase treatment retention, however most physicians still do not prescribe them (7). Stigma among healthcare workers remains a significant barrier to engaging persons with a substance use disorder (SUD) in treatment (8, 9), and specific strategies for linkage to care among high-risk, underrepresented populations is still widely misunderstood (10). Fewer than 1 in 5 individuals who need specialty treatment for SUD receive care (11), and many people who have an SUD do not believe they need treatment (12).
Despite the exceeding challenges in doing so, over 22 million U.S. adults have resolved a past substance use concern, and some do so without formal assistance (13, 14). Recovery from an SUD occurs through multiple pathways, and most people who engage in services do so within communities where they live and work (14, 15). Regional SUD treatment and recovery service networks, also known as “recovery ecosystems,” contain a wide variety of programs from harm reduction to clinical treatment and recovery support; however, people who may benefit most from these services may not know about them, and even if they do, the complexity of navigating the service continuum can be challenging (15, 16). In the U.S., there have historically been two well-known types of helpers supporting persons seeking recovery from SUD: the clinical addiction service provider and the mutual-aid sponsor with lived experience who has been well recognized as serving in Twelve-step recovery and other mutual-aid groups (17–19). A new helper has recently emerged following the 2007 Centers for Medicare and Medicaid Services letter to state Medicaid offices approving reimbursement for peer recovery support services (PRSS) provided by credentialed peer workers (20). Georgia was the first state to initiate reimbursement for PRSS and most states have now followed suit (21).
PRSS, as defined here, are flexible, evidence-informed interventions that can be provided in a variety of settings over varying lengths of time and are delivered by credentialed people in long-term recovery from substance use and mental health disorders (22, 23). Peer-delivered interventions are focused on supporting individuals through the recovery process and across each stage of behavioral change. Because they are available across multiple settings, they may provide distinct benefits, however, to date, methodologically rigorous research verifying the effectiveness of these interventions is limited due in part to highly variant descriptions of job titles, service activities, and settings (11, 24–27). The peer worker role remains widely misunderstood, serving as a barrier to studying its effectiveness. Recent studies have demonstrated positive effects from PRSS interventions (11, 24, 25), but the most rigorous studies are focused on opioid use disorder (OUD) exclusively and are limited to clinical treatment or hospital settings such as emergency departments, which may disproportionately exclude vulnerable populations less likely to seek medical treatment (11). It is also not well-understood how peer workers serve to improve and facilitate client navigation of services within their respective recovery ecosystems (28, 29). PRSS are intentional, person-driven approaches that center recovery goals at the individual level, and thus, may not be easily evaluated through standard clinical criteria such as abstinence, treatment adherence, or symptom reduction (30, 31).
PRSS have broad support in the U.S. and the Biden-Harris administration called for expanded access to peer support as a component of the 2022 Presidential Unity Agenda (32). The Substance Abuse and Mental Health Services Administration (SAMHSA) has released numerous resources on the implementation of PRSS including the recently released National Model Standards for Peer Support Certification (33). SAMHSA defines PRSS support across four distinct categories: Emotional (demonstrating empathy, caring, or concern to bolster self-esteem and confidence), Informational (sharing knowledge and information and/or providing life or vocational skills training), Instrumental (providing concrete assistance to help other accomplish tasks), and Affiliational (facilitating contacts with others to promote learning of social and recreational skills to acquire a sense of belonging) (34). In addition to providing individualized support to patients and clients, peer workers serve as valuable members of interdisciplinary treatment teams promoting non pejorative language among clinical staff and demonstrating what recovery can look like, thereby reducing stigma and promoting more positive attitudes toward persons with SUD (35). PRSS are implemented throughout the continuum of care and peer workers may fill distinct gaps due to behavioral health workforce shortages (23, 36).
While PRSS are a promising intervention that may increase linkage to care, motivation to change, treatment retention, and long-term recovery, there remains a sizable gap in the empirical literature to effectively disseminate PRSS to scale (11). Furthermore, as minority and marginalized populations share a disproportionate burden of SUD related consequences, PRSS delivered by peer workers at the intersection of race, ethnicity, gender, sexual orientation, gender identity, and key life experiences may confer added benefit to these populations (23). Misunderstanding of the peer role, and a lack of a consistent nomenclature to describe PRSS activities that occur across multiple service settings is a barrier to studying PRSS effectiveness. The present study engages peer workers in nine U.S. states to identify and classify common work activities and the service settings in which they are delivered, thereby pinpointing salient interventions for future study.
This sequential exploratory mixed-methods study began with a qualitative and methodological review of a previous peer worker survey instrument and corresponding results (27). An 8-member panel of subject matter experts assessed the quality of the existing survey instrument during a 30-day review period by providing an extensive critique on a pre-populated web-based feedback form. All experts had lived experience with SUD and included recovery scientists, peer workers, doctoral students, and expert psychometricians. Each expert provided feedback to improve the validity and reliability of the new survey instrument. Upon completion, the final quantitative survey was programmed into the Qualtrics survey platform and approved by the East Tennessee State University Internal Review Board (IRB) in February of 2023.
The final web-based peer worker survey contained 38 questions that followed an approved electronic informed consent document. Three additional prompts separate from the survey responses allowed participants to leave their email address if they were interested in a gift card lottery, participating in future research, and receiving a final copy of the study results. The web-based survey link was disseminated by email to a non-probability-based sample of peer workers by certification boards and peer associations in nine U.S. states. Participating states were selected from four US sub-regions (Northeast, Midwest, South, West) based on substance-related risk factors (treatment admissions, overdose death rates, and treatment access) and willingness to participate in survey dissemination. To be included in the study, each identified state had to have a ready champion willing to disseminate the survey email followed by two email reminders to a minimum sample of 200 certified and employed PRSS. When an identified high-risk state did not have a champion or adequate sample frame, the next “riskiest” state was then selected. Additionally, a Central Appalachian sample was utilized as the “fifth” sub-region via email addresses from the previous sample of peer workers who indicated a willingness to participate in future research (n = 423). The resulting final list of states in this sample included Florida, Kentucky, North Carolina, New Mexico, Pennsylvania, Tennessee, Virginia, Wisconsin, and West Virginia. Eligibility criteria required that participants be 18 years of age or older, hold a valid state, national or international peer certification, and be employed or previously employed as a peer in one of the nine states for at least 12-months. The survey link remained open for 30-days.
As a result of the qualitative and methodological review of the original survey instrument, the list of PRSS activities from which peer workers would choose expanded from the original 14 derived from the work of Ashford et al. (15) to 62 to adequately capture the full range of services peer workers provide (see Supplementary Material A). A major factor in the expansion of the items was the large number of participants who selected “Other” in the previous version of the survey (27). Therefore, an additional 48 activities informed by the existing literature, state and national training competencies, and the open-ended responses provided by peer workers in the previous survey were included.
A similar approach was used to generate a more comprehensive list of employer types and service settings (see Supplementary Material B). The previous iteration of the peer worker survey included 15 service settings (15), and the updated instrument included both macro settings (n = 8)—referring to general organization and agency types—and micro settings (n = 28) —that is, settings in which specific activities frequently take place (e.g., syringe services programs, jails, client homes, and online or digital platforms).
The survey opened with questions related to employment status, case load, and additional training or certifications (NCPRSS, NCPS, IC&RC, and CCAR). Participants were also asked about administrative and clinical supervision requirements at their current place of employment and the extent to which their state certification training prepared them for their work in the field.
The next set of questions queried employer type from eight general/macro settings: healthcare, behavioral health/community mental health, education, not for profit/community organization, justice system, faith-based entity, government agency, and treatment clinic or agency. Additional questions collected information about a job description, and client population by age group served. Participants were also asked to estimate the average amount of time spent conducting each of the four SAMHSA-defined types of peer support: Emotional, Informational, Instrumental, and Affiliational (34). A case definition and example for each type of support was provided in the survey prompt. Another question derived from a previous study of peer workers in Michigan assessed job satisfaction (37).
Specific activities in which the peer workers were engaging was assessed by the following item: “This next question is one of the most important in the survey. The question has 62 work activities that peer workers like yourself have asked us to include in this survey. Please read and scroll through all of the choices carefully and select ALL that apply. After selecting all of the activities that they performed most of the time, survey skip logic provided two carryforward questions for each selection requesting that the participant select both a general/macro and then specific/micro setting in which the activity was performed. A comprehensive list of items included in this survey prompt are included in the Supplementary Material and contains 62 distinct service activities, eight general/macro settings, and more than 30 unduplicated specific/micro settings.
Survey items related to participant demographics and their personal history with recovery included type of recovery (mental health, SUD, or both), duration of recovery, criminal justice involvement, and the following demographic variables: gender identity, race, ethnicity, age, and educational level attained.
Descriptive analyses were conducted on each variable using SPSS 29.0.2.0 including measures of frequency distribution, central tendency, and data set variability. To determine how many total times each specific/micro setting was endorsed, a new variable was coded for each response option (e.g., community/neighborhood) and frequencies were run on each new, re-coded variable which corresponded to each specific/micro setting. Next, data were then stratified by setting using SPSS. Using this stratification, frequency analyses were conducted for activities separately within each general/macro setting, and their subsequent specific/micro settings. The two most common general/macro settings, and three most common specific/micro settings, were examined for each of the 62 activities.
A total of 659 peer workers responded to the web-based survey. Seventy-six (76%) percent of respondents identified as White Non-Hispanic, 10% Black, 7% Native American/Alaskan Indian, 5% Asian, 2% Native Hawaiian or Pacific Islander, and 4% identified as another or “Other” race. Twenty-six percent (26%) also identified as Hispanic. The average age of respondents was 43 years (M = 43.8, SD = 13.1); 54% were female identifying, 41% were male identifying, and 4% identified as a gender other than male or female. Ninety-two percent (92%) had a high school diploma or higher level of education. Table 1 includes a comprehensive list of demographic characteristics for survey respondents and total participants by state. New Mexico (n = 158) had the highest number of respondents while West Virginia (n = 25) had the fewest.
Sixty-seven percent (67%, n = 439) of survey respondents had a state level certification. Additionally, 216 had the NAADAC Certified Peer Recovery Support Specialist credential (NCPRSS), 197 had the IC&RC Peer Recovery credential, 196 had the Mental Health America National Certified Peer Specialist credential (NCPS), and 173 had the Connecticut Community for Addiction Recovery (CCAR) Recovery Coach credential. Ninety-four percent (94%) of respondents were employed at the time of survey dissemination, with an average of 6 years working as a professional in the addictions field (M = 6.2, SD = 7.3). Most of the peer workers in the sample (87.0%) had fewer than 50 clients on their active caseload and reported working an average of 35 h per week (M = 34.8, SD = 14.0). Seventy-seven percent had an established job description, and 76% were required to receive clinical or administrative supervision as a component of their job or peer certification requirements. However, only 20% received this supervision from another credentialed peer. Peer worker respondents reported that they were satisfied or very satisfied with most features of their job including physical safety (89%), job security (83%), and other peer staff supportiveness (78%); however, fewer were satisfied with supervisor supportiveness (70%), work-related stress (69%), and promotion opportunities (65%). Regarding hourly wages, 39% reported an hourly wage of $16–$20 dollars, 25% made more than $20 per hour, and 22% made $10–$15 per hour. Fewer than 3% reported making less than $10 per hour. Table 2 includes additional detail on these results.
Most of the peer worker respondents were employed by a behavioral health/community mental health agency (40%) or a not-for-profit community organization (27%) followed by treatment clinics (9%) and healthcare organizations (9%). Fewer than 20% were working in the justice system, education, faith-based entities, or government agencies combined. When asked what percent of their work time was spent in each of the four types of peer support as defined by SAMHSA, respondents reported spending nearly half of their time providing Emotional support (M = 43.1%; SD = 26.1), followed by Affiliational (M = 21.3%; SD = 18.5), Informational (M = 18.0%; SD = 15.5), and Instrumental support (M = 15.0%; SD = 15.3).
When asked to select activities that they performed most frequently, respondents selected 24 activity choices on average (M = 23.6, SD = 16.7) from the list of 62 discrete activities. As illustrated in Figure 1, peer workers in this sample most frequently endorsed activities that could be categorized as Emotional support (e.g., understanding and relating to clients, providing emotional support, sharing recovery stories, being present without judgment, inspiring hope, encouraging or empowering, showing empathy, etc.).
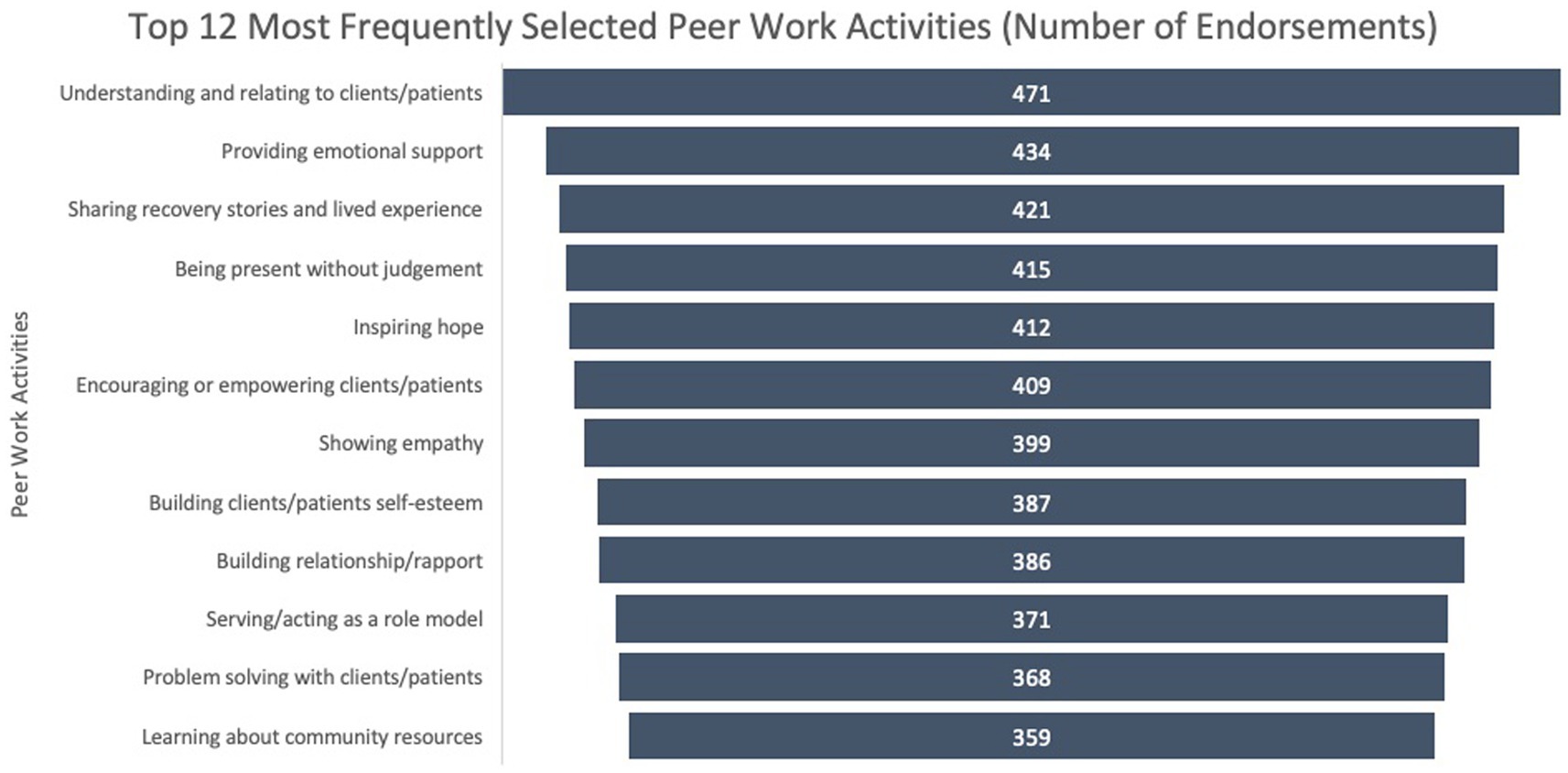
Figure 1. Number of participants who endorsed each of the top 12 most frequently selected activities from the total list of 62 discrete work activities.
The nested general/macro and specific/micro setting prompts that followed each activity endorsement indicate that the general/macro settings associated with each activity closely follow the employer by type results: the majority of endorsed activities occur in either not-for-profit/community organization (32%) or behavioral health/community mental health (31%) general/macro settings. However, the specific/micro settings where activities were performed had greater variance. Figure 2 illustrates this variability, with most activity endorsements occurring in communities and neighborhoods where patients/clients live and not in clinical or agency settings.
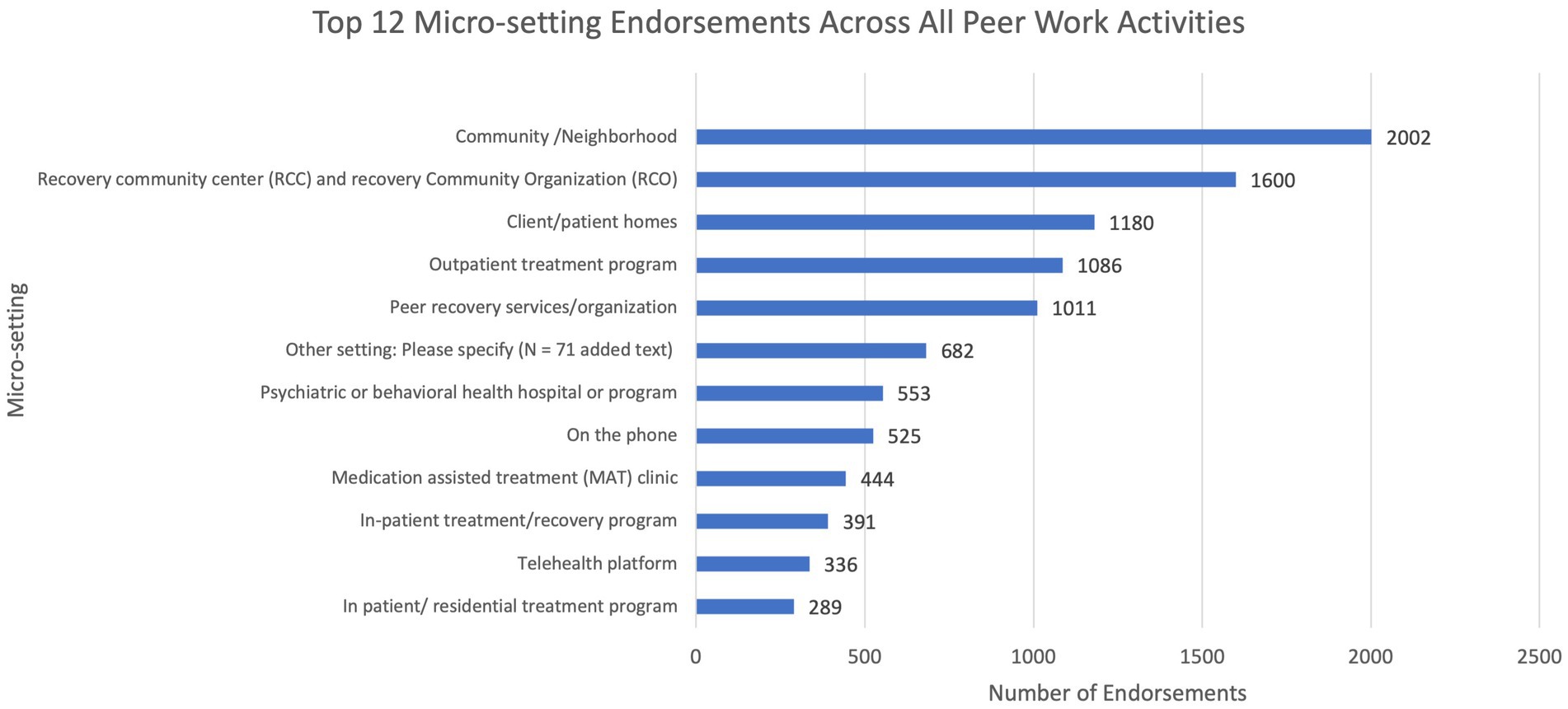
Figure 2. Most common micro-setting endorsements (the actual location where the work activity is performed) for all 62 discrete work activity selections.
Table 3 provides further detail outlining the nested nature of survey responses and corresponding results. When PRSS respondents selected an activity, they commonly reported performing that activity in either a behavioral health/community mental health agency or a not-for-profit organization macro/general setting. Yet, a wider variety of specific/micro settings within these two general/macro categories were selected. For instance, respondents most commonly endorsed performing the “understanding and relating to clients” activity in a peer recovery services organization, yet they most commonly performed the “building self-esteem” activity in a community/neighborhood setting. Finally, community/neighborhood settings account for the greatest number of specific/micro setting endorsements (n = 2002, 15.2%), followed by recovery community centers/recovery community organizations (n = 1,600, 7.1%). Table 4 illustrates frequency and percent for all specific/micro setting endorsements.
Peer worker respondents (N = 659) had an average of 9 years in recovery (M = 9.3, SD = 8.5). Forty-four (44%) percent had previous criminal legal system involvement, and 41% reported being in recovery from both an SUD and a mental health condition. Only 15% were in recovery from SUD alone, while 23% were in recovery from a mental health condition alone.
This study addresses a universal call in the literature for clarity in describing PRSS interventions, the peer worker role, and a uniform classification of service activities that can serve as a foundation for effectiveness research. Cited barriers to conducting effectiveness studies include highly variant titles for peer workers, a broad range of interventions conducted in numerous settings, outcome measures across all types of SUD, and disaggregation of the effects of PRSS from other types of treatment and recovery services (11, 22, 26). It is hypothesized that PRSS may lead to a broad array of proximal and distal outcomes that may extend beyond SUD treatment adherence, reduction in substance use, and long-term recovery (29). A comprehensive classification of PRSS activities and settings in which they are performed does not yet exist for this relatively new workforce.
The present study examined survey results from 659 peer workers in nine U.S. states and may be the first of its kind to explore the broad array of service activities peer workers perform in multiple settings across regional recovery ecosystems. Notably, peer worker respondents selected an average of 24 discrete activities that they perform most of the time. These results also provide preliminary evidence about where service activities are performed within both general/macro and specific/micro settings.
Peer workers reported that they spend about half of their time providing Emotional support and less than ¼ of their time providing each of the other types of SAMHSA-defined peer support (Informational, Instructional, and Affiliational). These results support findings from a previous study in which Central Appalachian peer workers (N = 565) reported spending 52% of their time providing Emotional support (27). Recommendations for future research would include an exploration of the manner in which these Emotional support activities are delivered and the underlying mechanisms of action that may lead to positive outcomes.
These study results also indicate that PRSS interventions are delivered in neighborhoods, client homes, and recovery community organizations more frequently than in clinical treatment settings. It is hypothesized that engagement at the community level may confer specific advantages due to cited barriers to clinical treatment engagement and retention (8, 16, 38). PRSS provided in community settings may also lead to increased engagement among vulnerable communities as peer workers may be uniquely poised to engage in a culturally competent manner using their shared lived experience (29, 35). Peer workers in this sample also frequently provide services in peer-led organizations such as recovery community centers (RCCs) and recovery community organizations (RCOs) that offer free, low-threshold points of engagement that may be particularly appealing to persons who may be ambivalent about clinical treatment, have experienced stigma in healthcare settings (8), or who are concerned that they cannot pay for specialty treatment (16).
The inclusion of PRSS in the cascade of SUD care has gained enormous momentum in the U.S. (29), and Medicaid and third-party reimbursement for peer support has led to integration of PRSS in medical settings such as emergency departments, inpatient treatment centers, and primary care. Peer workers’ lived experience may make them more relatable, and perhaps more equipped to establish and maintain rapport, than clinical staff, which may lead to greater treatment engagement and sustainment of long-term recovery (19, 29). However, notably, peer workers are commonly paid less than other behavioral health staff, and while they are generally satisfied with their work, work related stress and career advancement are areas of concern (27). Peer workers also report feeling stigmatized by non-peer colleagues who also frequently misunderstand their role (39), and they are often asked to perform tasks that do not align with the intent of the peer model, such as providing transportation, documentation, and case management (27). Peer workers frequently seek and attain additional training and national and international certifications, but there are relatively few options for increased pay and career advancement for this workforce (27). To address the challenges faced by this emergent workforce, future studies should include peer workers in all aspects of study design and include an explicit focus on how to support and sustain this vital workforce.
The present study represents one of the first comprehensive accounts of the activities in which peer workers engage with respondents representing a national sample, and as such, the findings hold promise for future studies focused on the impact these activities have on substance use outcomes. Although the sample was national in scope, it was not obtained randomly, nor based on probability sampling; therefore, the generalizability may be limited to the present respondents. Future work should replicate the methods and measures but use sampling frames that could involve random selection and stratification on key variables. A second limitation was with the survey instrument itself. Although the rates of survey completion were high for research of this kind (85% of respondents completed the instrument), approximately 15% of participants exited the survey during the section on PRSS activities. Whereas we believe the comprehensive account of activities, along with general/macro and specific/micro settings, is a strength of the present study, considerations could be made for the optimal placement of these questions in the overall instrument. Finally, the results are impacted by self-report bias; however, we assume that as the questions focus on daily routines, the impact may be minimal.
It is currently estimated that fewer than 1 in 5 individuals in the U.S. receive specialty treatment for their OUD or SUD (11), and many people who have an SUD do not believe they need treatment (1). PRSS activities, specifically those that offer Emotional support, may provide unique benefit when delivered by persons with shared lived experience across the continuum of care. However, not knowing specifically what peers are doing across multiple settings, has limited effectiveness research and outcome measurement. Furthermore, it is not well understood how regional recovery service settings and SUD recovery and treatment providers are supporting and sustaining this valuable workforce. This study seeks to advance the science of PRSS through the categorization of common service activities and settings among a large sample of peer workers (N = 659) in nine U.S. states. A future direction for this line of research will include a random sample of peer workers across the U.S. to inform the development of a formal nomenclature for PRSS activities and service settings.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by East Tennessee State University Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
AH: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Resources, Validation, Writing – original draft, Writing – review & editing. HW: Data curation, Formal analysis, Writing – original draft, Writing – review & editing. RM: Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. CH: Data curation, Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by the National Institute on Drug Abuse of the National Institutes of Health under award number R24DA051950 Justice-involved and Emerging Adult Populations (JEAP). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The study team would like to acknowledge the unique contributions of the subject matter experts, and Jason Chapman, Senior Research Scientist at Chestnut Health System, for their support in improving the validity and reliability of the survey instrument. We would also like to thank Ashli Sheidow, MPI of the JEAP initiative, who served as a mentor to first author Angela Hagaman as she conducted this pilot study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1533051/full#supplementary-material
1. Substance Abuse and Mental Health Services Administration. 2023 companion infographic report: Results from the 2021, 2022, and 2023 National Surveys on drug use and health. Center for Behavioral Health Statistics and Quality (2024)
2. Ahmad, F, Cisewski, J, Rossen, L, and Sutton, P. Provisional drug overdose death counts. Washington, D.C.: The National Center for Health Statistics (2024).
3. U.S. Overdose deaths decrease in 2023, first time since 2018 [press release]. National Center for Health Statistics. Centers for Disease Control and Prevention (CDC). (2024).
4. Mann, B. In 2023 fentany overdoses ravaged the U.S. and fueled a new culture war fight (2023). Available online at: https://www.npr.org/2023/12/28/1220881380/overdose-fentanyl-drugs-addiction#:~:text=In%202023%20the%20overdose%20death,for%20Disease%20Control%20and%20Prevention (Accessed February 23, 2024).
5. Volkow, N. Nora’s blog: National Insitute on drug Abuse (2024). Available online at: https://nida.nih.gov/about-nida/noras-blog/2024/08/older-black-men-are-disproportionately-affected-by-overdose-crisis (Accessed February 23, 2024).
6. Centers for Disease Control. Opioid overdose prevention in tribal communities. Centers for Disease Control and Prevention (CDC), U.S. Department of Health & Human Services (HHS). (2024).
7. Jones, CW, Christman, Z, Smith, CM, Safferman, MR, Salzman, M, Baston, K, et al. Comparison between buprenorphine provider availability and opioid deaths among US counties. J Subst Abus Treat. (2018) 93:19–25. doi: 10.1016/j.jsat.2018.07.008
8. Bielenberg, J, Swisher, G, Lembke, A, and Haug, NA. A systematic review of stigma interventions for providers who treat patients with substance use disorders. J Subst Abus Treat. (2021) 131:108486. doi: 10.1016/j.jsat.2021.108486
9. Ashford, RD, Brown, AM, and Curtis, B. Systemic barriers in substance use disorder treatment: a prospective qualitative study of professionals in the field. Drug Alcohol Depend. (2018) 189:62–9. doi: 10.1016/j.drugalcdep.2018.04.033
10. Hogue, A, Satcher, MF, Drazdowski, TK, Hagaman, A, Hibbard, PF, Sheidow, AJ, et al. Linkage facilitation services for opioid use disorder: taxonomy of facilitation practitioners, goals, and activities. J Substance Use Addict Treat. (2024) 157:209217. doi: 10.1016/j.josat.2023.209217
11. Gormley, MA, Pericot-Valverde, I, Diaz, L, Coleman, A, Lancaster, J, Ortiz, E, et al. Effectiveness of peer recovery support services on stages of the opioid use disorder treatment cascade: a systematic review. Drug Alcohol Depend. (2021) 229:109123. doi: 10.1016/j.drugalcdep.2021.109123
12. SAMHSA announces National Survey on drug use and health (NSDUH) results detailing mental illness and substance use levels in 2021 [press release]. Substance Abuse Mental Health Serv Admin ; (2023)
13. Ashford, RD, Brown, A, Canode, B, Sledd, A, Potter, JS, and Bergman, BG. Peer-based recovery support services delivered at recovery community organizations: predictors of improvements in individual recovery capital. Addict Behav. (2021) 119:106945. doi: 10.1016/j.addbeh.2021.106945
14. Kelly, JF, Bergman, B, Hoeppner, BB, Vilsaint, C, and White, WL. Prevalence and pathways of recovery from drug and alcohol problems in the United States population: implications for practice, research, and policy. Drug Alcohol Depend. (2017) 181:162–9. doi: 10.1016/j.drugalcdep.2017.09.028
15. Ashford, R, Brown, AM, Ryding, R, and Curtis, B. Building recovery ready communities: the recovery ready ecosystem model and community framework. Addict Res Theory. (2019) 28:1–11. doi: 10.1080/16066359.2019.1571191
16. Addiction Policy Forum Patient Journey Map: Substance use disorder treatment and recovery experiences. Addiction Policy Forum. (2022).
17. Hagaman, A. Peer recovery support specialists: Role clarification and fit within the recovery ecosystems of central Appalachia. Johnson City, TN: East Tennessee State University (2021).
18. Hymes, AS. A phenomenological study of the experiences of substance abuse peer recovery coaches career motivation and professional experiences. Doctoral dissertation. The University of North Carolina at Charlotte. (2015). Available at: https://ninercommons.charlotte.edu/islandora/object/etd:1810 (Accessed February 23, 2024).
19. White, WL. Peer-based addiction recovery support: history, theory, practice, and scientific evaluation. Counselor. (2009) 10:54–9.
20. Centers for Medicare and Medicaid Services. Letter to state Medicaid directors. U.S. Department of Health & Human Services, Centers for Medicare & Medicaid Services. (2007).
21. Myrick, K, and Del Vecchio, P. Peer support Services in the Behavioral Healthcare Workforce: state of the field. Psychiatr Rehabil J. (2016) 39:197–203. doi: 10.1037/prj0000188
22. Eddie, D, Hoffman, L, Vilsaint, C, Abry, A, Bergman, B, Hoeppner, B, et al. Lived experience in new models of Care for Substance use Disorder: a systematic review of peer recovery support services and recovery coaching. Front Psychol. (2019) 10:1052. doi: 10.3389/fpsyg.2019.01052
23. Castedo de Martell, S, Wilkerson, JM, Howell, J, Brown, HS, Ranjit, N, Holleran Steiker, L, et al. The peer to career pipeline: an observational study of peer worker trainee characteristics and training completion likelihood. J Substance Use Addict Treatment. (2024) 159:209287. doi: 10.1016/j.josat.2023.209287
24. Bassuk, EL, Hanson, J, Greene, RN, Richard, M, and Laudet, A. Peer-delivered recovery support Services for Addictions in the United States: a systematic review. J Subst Abus Treat. (2016) 63:1–9. doi: 10.1016/j.jsat.2016.01.003
25. Eddie, D, Greene, MC, White, WL, and Kelly, JF. Medical burden of disease among individuals in recovery from alcohol and other drug problems in the United States: findings from the National Recovery Survey. J Addict Med. (2019) 13:385–95. doi: 10.1097/ADM.0000000000000512
26. Reif, S, Braude, L, Lyman, DR, Dougherty, RH, Daniels, AS, Ghose, SS, et al. Peer recovery support for individuals with substance use disorders: assessing the evidence. Psychiatr Serv. (2014) 65:853–61. doi: 10.1176/appi.ps.201400047
27. Hagaman, A, Foster, K, Kidd, M, and Pack, R. An examination of peer recovery support specialist work roles and activities within the recovery ecosystems of central Appalachia. Addict Res Theory. (2023) 31:328–34. doi: 10.1080/16066359.2022.2163387
28. White, W. Sponsor, recovery coach, addiction counselor: The importance of role clarity and role integrity. Philadelphia, PA: Philadelphia Department of Behavioral Health (2006).
29. Stack, E, Hildebran, C, Leichtling, G, Waddell, EN, Leahy, JM, Martin, E, et al. Peer recovery support services across the continuum: in community, hospital, corrections, and treatment and recovery agency settings–a narrative review. J Addict Med. (2022) 16:93–100. doi: 10.1097/ADM.0000000000000810
30. Ashford, RD, Brown, A, Brown, T, Callis, J, Cleveland, HH, Eisenhart, E, et al. Defining and operationalizing the phenomena of recovery: a working definition from the recovery science research collaborative. Addict Res Theory. (2019) 27:179–88. doi: 10.1080/16066359.2018.1515352
31. Fortuna, KL, Solomon, P, and Rivera, J. An update of peer support/peer provided services underlying processes, benefits, and critical ingredients. Psychiatry Q. (2022) 93:571–86. doi: 10.1007/s11126-022-09971-w
32. The White House. Fact sheet: Biden-Harris Administration announces new actions to tackle Nation’s mental health crisis [press release]. Available at: https://www.whitehouse.gov/ (2023).
33. Substance Abuse and Mental Health Services Administration. National Model Standards for peer support certification. Rockville, MD: (2023).
34. Substance Abuse and Mental Health Services Administration Center for Substance Abuse Treatment. What are peer recovery support services? Rockville, MD: Substance Abuse and Mental Health Services Administration, U.S. Department of Health and Human Services. (2009).
35. Slater, TM, Rodney, T, and Finnell, DS. Promoting the integration of peer support specialists into the healthcare team. Nursing. (2023) 53:50–5. doi: 10.1097/01.NURSE.0000903972.32588.ad
36. Gaiser, MG, Buche, JL, Wayment, CC, Schoebel, V, Smith, JE, Chapman, SA, et al. A systematic review of the roles and contributions of peer providers in the behavioral health workforce. Am J Prev Med. (2021) 61:e203–10. doi: 10.1016/j.amepre.2021.03.025
37. Lapidos, A, Jester, J, Ortquist, M, Werner, P, Ruffolo, MC, and Smith, M. Survey of peer support specialists: professional activities, self-rated skills, job satisfaction, and financial well-being. Psychiatric Serv. (2018) 69:1264–7. doi: 10.1176/appi.ps.201800251
38. Yang, Y, Perkins, DR, and Stearns, AE. Barriers and facilitators to treatment engagement among clients in inpatient substance abuse treatment. Qual Health Res. (2018) 28:1474–85. doi: 10.1177/1049732318771005
Keywords: peer support, recovery supports, substance use disorder, opioid use disorder, drug abuse and addiction, SUD treatment, peer workforce, peer worker
Citation: Hagaman A, Warren HL, Miller R and Henderson C (2025) Peer support service activity prevalence by setting: a nine-state survey of peer workers. Front. Public Health. 13:1533051. doi: 10.3389/fpubh.2025.1533051
Received: 22 November 2024; Accepted: 17 February 2025;
Published: 05 March 2025.
Edited by:
George Unick, University of Maryland, United StatesReviewed by:
Robert J. Wellman, UMass Chan Medical School, United StatesCopyright © 2025 Hagaman, Warren, Miller and Henderson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Angela Hagaman, SGFnYW1hbkBldHN1LmVkdQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.