- 1Shanghai Health Development Research Center (Shanghai Medical Information Center), Shanghai, China
- 2Shanghai Health Statistics Center, Shanghai, China
Background: The aging problem in Shanghai is rapidly increasing, leading to the development of chronic comorbidities in older adults. Studying the correlations within comorbidity patterns can assist in managing disease prevention and implicate early control.
Objectives: This study was a cross-sectional analysis based on a large sample size of 3,779,756 medical records. A network analysis and community classification were performed to illustrate disease networks and the internal relationships within comorbidity patterns among older adults in Shanghai.
Methods: The network analysis and community classification were performed using the IsingFit and Fast-greedy community functions. Datasets, including disease codes and disease prevalence, were collected from medical records.
Results: The top five prevalent diseases were hypertension (64.78%), chronic ischemic heart disease (39.06%), type 2 diabetes mellitus (24.97%), lipid metabolism disorders (21.79%), and gastritis (19.71%). The sampled population showed susceptibility to 11 comorbidities associated with hypertension, 9 with diabetes, 28 with ischemic heart disease, 26 with gastritis, and 2 with lipid metabolism disorders in male patients. Diseases such as lipid metabolism disorders, gastritis, fatty liver, polyps of the colon, osteoporosis, atherosclerosis, and heart failure exhibited strong centrality.
Conclusion: The most common comorbidity patterns were dominated by ischemic heart disease and gastritis, followed by a ternary pattern between hypertension, diabetes, and lipid metabolism disorders. Male patients were more likely to have comorbidities related to cardiovascular and sleep problems, while women were more likely to have comorbidities related to thyroid disease, inflammatory conditions, and hyperuricemia. It was suggested that healthcare professionals focus on monitoring relevant vital signs and mental health according to the specific comorbidity patterns in older adults with chronic diseases, to prevent the development of new or more severe comorbidities.
1 Introduction
The World Health Organization (WHO) defines comorbidity as the presence of two or more persistent health conditions in the same individual, requiring prolonged intervention for maintenance (1). By the middle of this century, it is projected that the population aged 60 years and above in China will reach 430 million (2). Chronic comorbidity has long been a significant health challenge among older adults. In Shanghai, one of the regions undergoing severe aging problems, the detection rate of chronic diseases among older adults has reached 70% (3). Compared to single-diagnosed diseases, comorbidity poses a more substantial threat to health, as the interplay of various diseases creates a complex network of risk factors, further increasing mortality risk among patients (4). The growing trend of comorbidity not only complicates diagnosis and treatment but also places a significant economic burden on families as well as society. Therefore, there is an urgent need for effective strategies to prevent and manage comorbidities, as well as to provide professional guidance for caregiving to older adults and their families.
Several domestic and international studies have conducted in-depth research on the prevalence of comorbidity and the associations between different chronic conditions among older adults in various regions, utilizing data collected from epidemiological surveys and medical records, combined with the practical application of various network theories. These studies also provided recommendations for control approaches of different comorbidity patterns. A study applied a self-organizing map (SOM) neural network to visually present the associations between various common chronic diseases among middle-aged and older adults in China. They explored the differences in comorbidity patterns affected by age, gender, urban–rural residence, and treatment outcomes through visual cluster analysis (5). A study used a network mapping strategy to explore comorbidity patterns among the Zhuang population in Guangxi, identifying nine patterns strongly associated with hypertension. These findings helped improve the health condition of the study population (6). Another study examined comorbidity networks in communities within Jiangsu Province based on large-scale network analysis tools to figure out comorbidity patterns, disease prevalence, clustering characteristics, risk factors, and preventive strategies (7). In addition, a South Korean study focused on comorbidity patterns among obese populations demonstrated the relationship between several chronic diseases and obesity across different genders (8). However, there were still some limitations to the current research progress. Previous studies had been limited to a few common diseases and had primarily focused on specific regions, lacking normality across the whole target population in China. Although some studies had collected data from whole areas within the country, the dataset required an update.
Currently, the situation regarding comorbidity among older adults in Shanghai remains unclear. This study applied visual network approaches to medical records from outpatient, emergency, and hospital visits among individuals aged 60 to 99 years in Shanghai, aiming to illustrate the coexistent diseases associated with the top five most prevalent conditions: hypertension, chronic ischaemic heart disease, type 2 diabetes mellitus, gastritis, and lipoprotein metabolism disorders. The study focused on analyzing potential comorbidities of these five diseases and aimed to provide insights into the prevention and management of chronic comorbidity among older adults in Shanghai. Additionally, it might lay a solid foundation for future exploration of potential associations and control of chronic disease incidence.
2 Materials and methods
2.1 Data processing and study population
The dataset was collected from the Shanghai Municipal Health Commission database (9). It was derived from a collection of medical records of outpatient visits, emergency visits, and hospitalized records from a total number of 520 public, private, and community hospitals, based on the enrollment of country’s national basic medical insurance programs. Medical visits were traced by ID number enrolled in the insurance system during July 2022 and June 2023. The accuracy of the medical records uploaded was inspected under rigorous quality control. Repeat visits under one ID for the same disease were only counted once and combined into one record. In this case, each line of record represented the occurrence of all diseases for a single patient without duplication, no matter how many times patients repeat their visits for the same disease. In this study, we defined that the number of visiting records represented the prevalence of each disease.
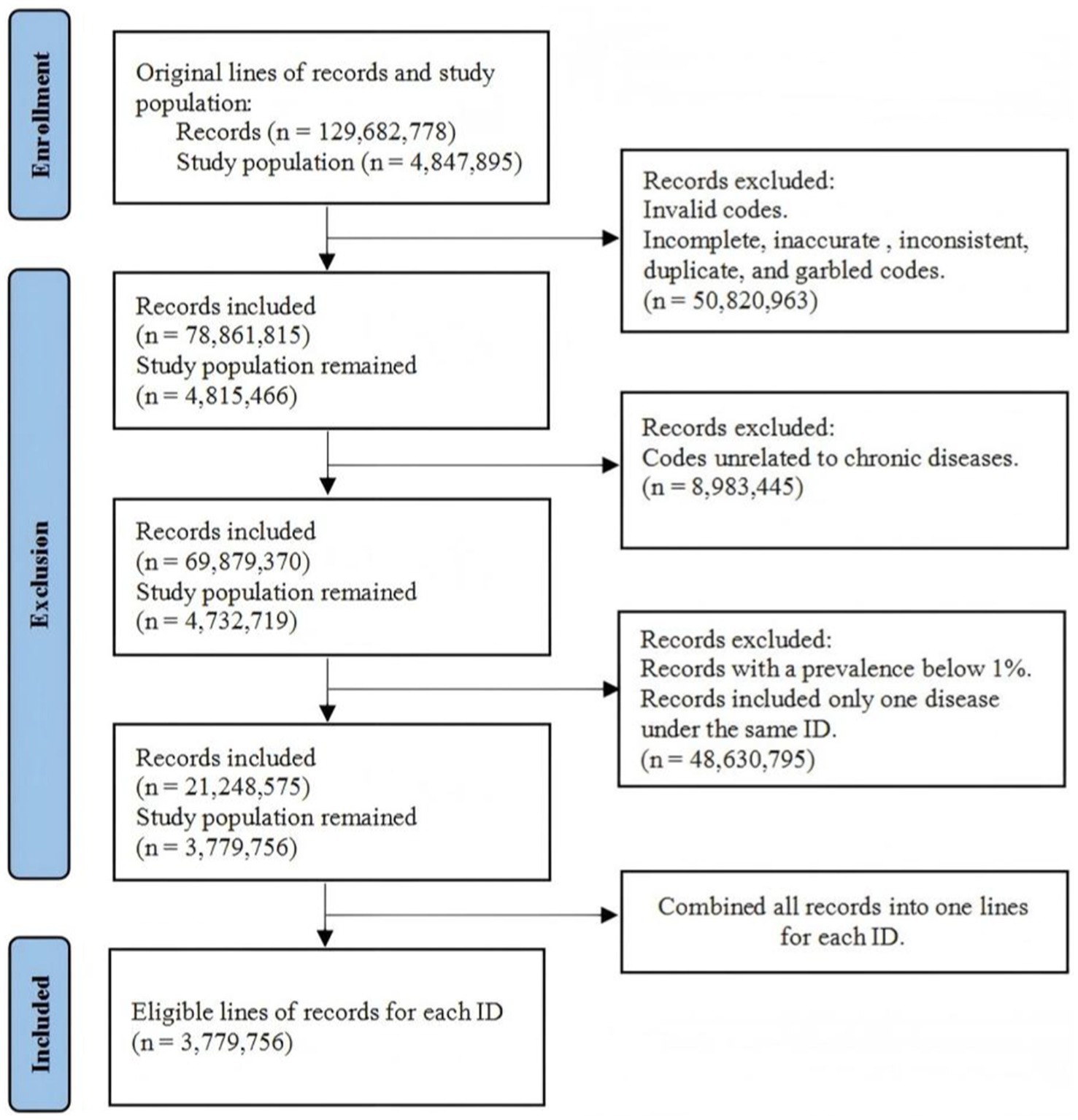
All disease codes were referred to ICD-10 (International Classification of Diseases, 10th Revision). Only the records that met ICD-10 coding rules were selected (e.g., A01.001). Incomplete, inaccurate, inconsistent, duplicate, and garbled codes were also directly excluded from the database. Additionally, records that contained only one disease under the same ID were excluded since they were not meaningful for comorbidity analysis. Diseases that were unrelated to chronic diseases were excluded. Diseases with a prevalence below 1% of the total number of records were also excluded. The dataset originally contained 129,682,778 records from 4,847,895 patients aged 60 to 99 years. After processing, this study included 3,779,756 lines of records (1,734,188 for men and 2,045,568 for women) (Figure 1). Then, 150,000 records were randomly sampled by gender for further network analysis and community classification.
2.2 Re-coding of diseases
ICD-10 codes contain similar diseases under the same code level, some of which were disordered and included insufficient subjects for analysis. For statistical feasibility, diseases that occur in the same body part with similar pathogenesis were combined to generate a new code. For example, EE03 referred to a combination of E03.8 and E03.9, which represented a sum of hypothyroidism. II2520 referred to a combination of diseases under I25 (chronic ischaemic heart disease) and I20 (angina pectoris) since I20 might be an outcome of I25.
Based on the new coding rules, the top five prevalent diseases were determined first. They were hypertension, ischaemic heart disease (IHD), type 2 diabetes mellitus (T2DM), lipoprotein metabolism disorders (LMD), and gastritis. Then, the top 40 diseases with their respective comorbidity rate of these five diseases were determined. A total number of 38 chronic diseases were retained after deleting duplication (new codes were listed in Table 1). The 38 diseases were hypertension, IHD, T2DM, gastritis, LMD, hypothyroidism, non-toxic diffuse goiter, sleep disorders, sleep apnea, acute myocardial infarction, cardiac arrhythmia, cerebral infarction, cerebrovascular disease, chronic rhinitis, chronic pharyngitis, bronchitis, gastro-esophageal reflux disease with esophagitis (GERD with esophagitis), non-infective gastroenteritis and colitis, constipation, functional diarrhea, polyps of the colon, non-alcoholic fatty liver disease (NAFLD), dermatitis, arthritis, osteoporosis, chronic kidney disease, dizziness and giddiness, anxiety disorders, neurotic disorders, atrial fibrillation and flutter, heart failure, atherosclerosis, chronic obstructive pulmonary disease (COPD), gastric ulcer, hyperuricemia, gonarthrosis, spondylosis, and (peri-)menopausal disorder.
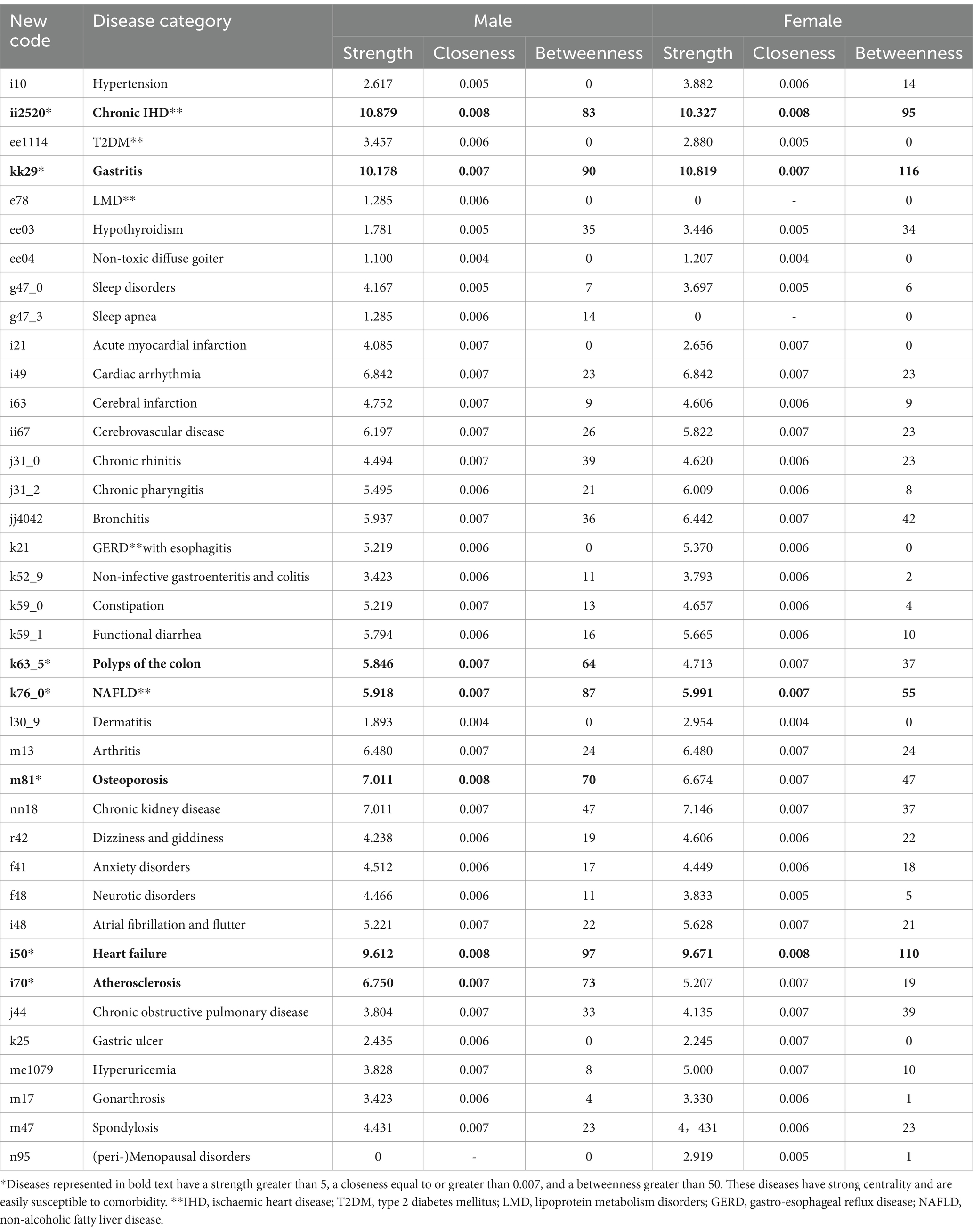
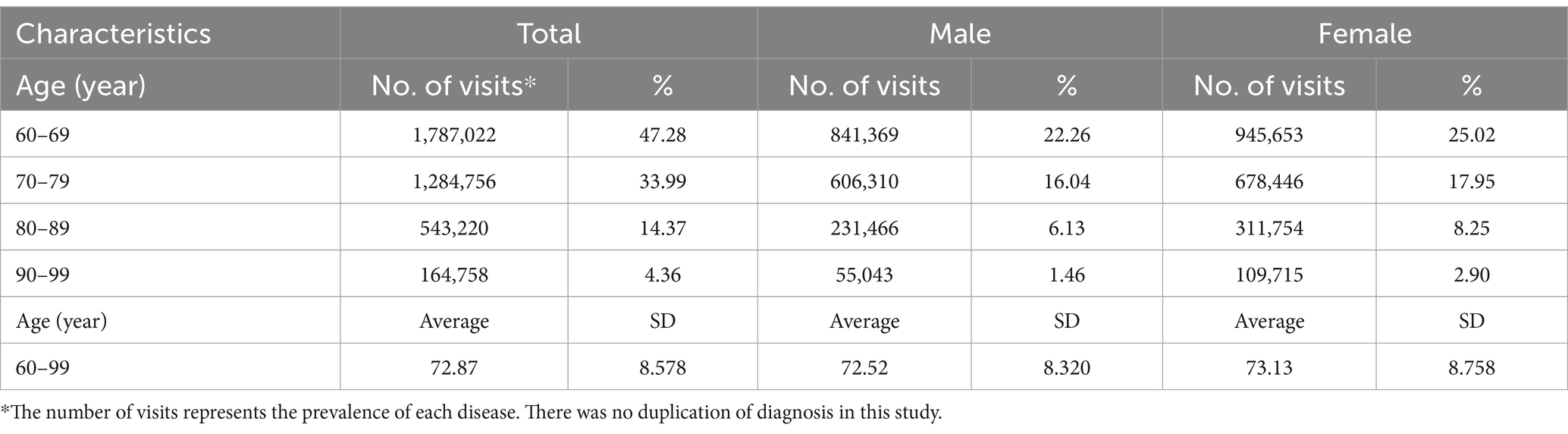
Table 1. Results of the centrality of each disease in the comorbidity network of male and female patients.
2.3 Statistical analysis
The database was generated using Excel 2013. The characteristics of age were presented as weighted means with a standard deviation (SD). The number of medical visits of the study population by age group and the prevalence of the top five diseases were presented as weighted percentages.
2.4 Comorbidity network analysis
Network analysis was conducted using the IsingFit function (α = 0.05) with R version 4.3.0. This network estimation employed eLasso, which combines l1-regularized logistic regression with model selection based on the Extended Bayesian Information Criterion (EBIC), enabling the identification of relevant relationships between diseases:
A coefficient wij greater than 0 indicates a higher frequency of two diseases occurring simultaneously, suggesting a higher likelihood of comorbidity. On the contrary, a coefficient smaller than 0 indicates a lower frequency of simultaneous occurrence. This is because the appearance of the two diseases in the 0/1 statistical matrix was decentralized, but the association still exists. In this study, positive and negative associations were used to describe the comorbidity frequency. The weight value of edges was used to describe this association in this study.
The network results included diseases as nodes and relevant associations as edges (10, 11). A node represents a single chronic disease. Edge connects two comorbid diseases. The thickness of the edge is proportional to the intensity of comorbidity. A thicker edge indicates a stronger correlation of comorbidity. Strength is defined as the sum of the weights of all nodes. Closeness quantified the indirect distance between two diseases. A greater closeness indicates a shorter distance between two diseases, and they may co-occur more easily. Betweenness indicates the number of times a disease acts as a connecting pathway to other pairs of comorbidity. A higher betweenness emphasizes the importance of the disease and its strong relationship with others (12).
2.5 Community classification
The comorbidity network conducted preliminary correlations among the studied diseases. Then, community classification was applied to further examine those positive correlations in depth to focus the results on comorbidity patterns. The analysis of clustering was based on the weights of the edges generated in the network, which introduced a concept of modularity, a quality index. The fast-greedy community function was applied to calculate modularity based on the weights of the edge. Modularity defined as
where m is the number of edges, Aij is the element of the A adjacency matrix in disease i and disease j. ki is the sum of weights of adjacent edges for disease i. kj is the degree of disease j. ci and cj are the components of diseases i and j.γ is a resolution parameter to weight random null model and it is usually set to 1 (13).
2.6 Ethics statement
There was no personal information included in the dataset. The Shanghai Medical and Technology Information Institute Ethics Committee approved this study and the use of the dataset (No.2024004). All participants and procedures followed the required guidelines (14).
3 Results
3.1 Characteristics of the study population
This study initially analyzed the distribution of the study population based on their number of visits regarding single-diagnosed diseases across different age groups, stratified by gender. The overall percentage of medical visits of patients aged 60 to 69 years was 47.28% (men: 22.26%, women: 25.02%). The percentages for age groups 70–79, 80–89, and 90–99 were 33.99% (men: 16.04%, women: 17.95%), 14.37%, (men: 6.13%, women: 8.25%) and 4.36% (men: 1.46%, women: 2.90%), respectively. The average age for the study population was 72.87 (SD, 8.578) years. 72.52 (SD, 8.320) for men and 73.13 (SD, 8.758) for women (Table 2).
3.2 Top 10 most visiting diseases
Hypertension had the highest frequency of visits among all the study subjects, with a total of 11,422,288 visits for men and 1,306,260 visits for women. The top 10 diseases were hypertension, IHD, T2DM, LMD, gastritis, sleep disorders, conjunctivitis, intestinal disorders, bronchitis, and respiratory disorders (Table 3).
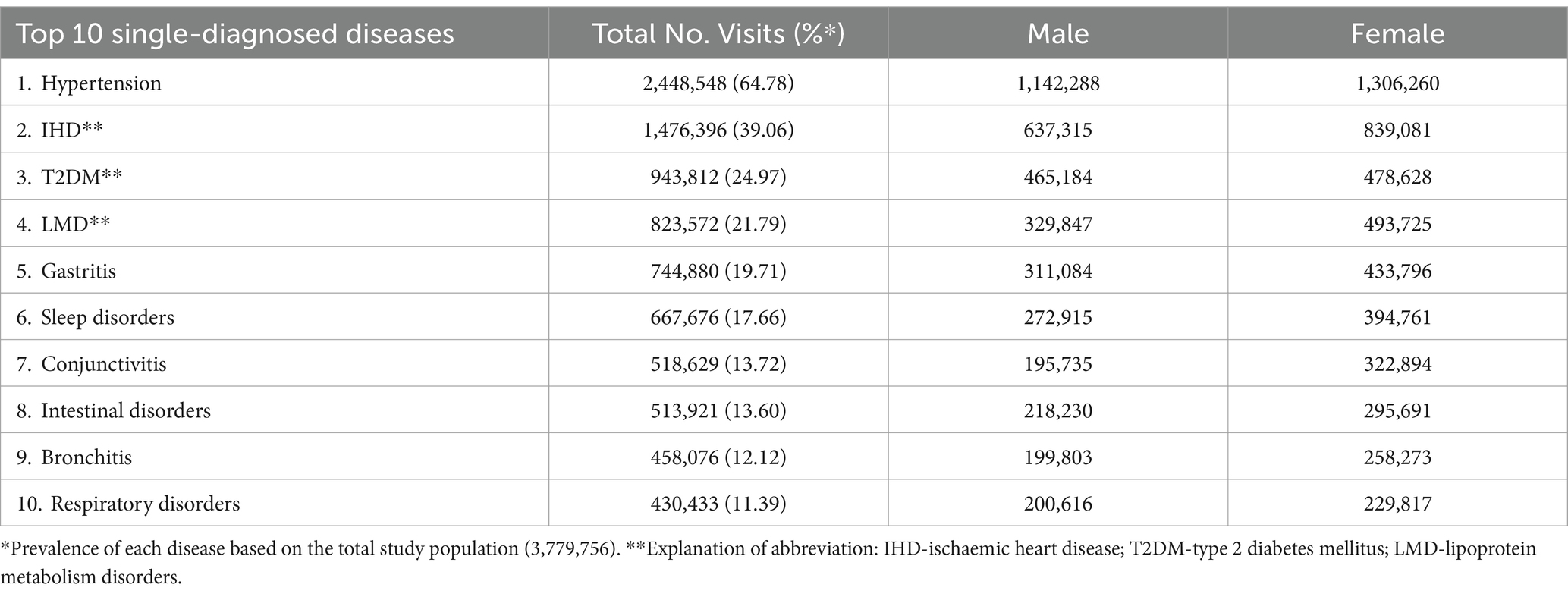
Table 3. Top 10 single-diagnosed diseases based on the number of medical visits of the study population.
3.3 The comorbidity network of the top five diseases within all 38 analyzed diseases
Both comorbidity networks for men and women, as illustrated in Figure 2, indicated that hypertension positively correlated with 11 diseases. These included IHD, hyperuricemia, chronic kidney failure, cerebral infarction, T2DM, cerebrovascular disease, arthritis, cardiac arrhythmia, dizziness and giddiness, bronchitis, and NAFLD (weight of edges greater than 0, see Supplementary Tables 1, 2). Conversely, hypertension exhibited a negative correlation with chronic pharyngitis, gastritis, polyps of the colon, sleep disorders, and dermatitis (weight of edges lower than 0, see Supplementary Tables 1, 2). There was an additional negative association with neurotic disorder, chronic rhinitis, and COPD in men than in women. These diseases had a lower frequency of occurring simultaneously due to the decentralization of the records. Hypertension had an additional positive correlation between atrial fibrillation and flutter, constipation, and gonarthrosis, and an additional negative correlation with osteoporosis, spondylosis, hypothyroidism, and (peri-)menopausal disorders.
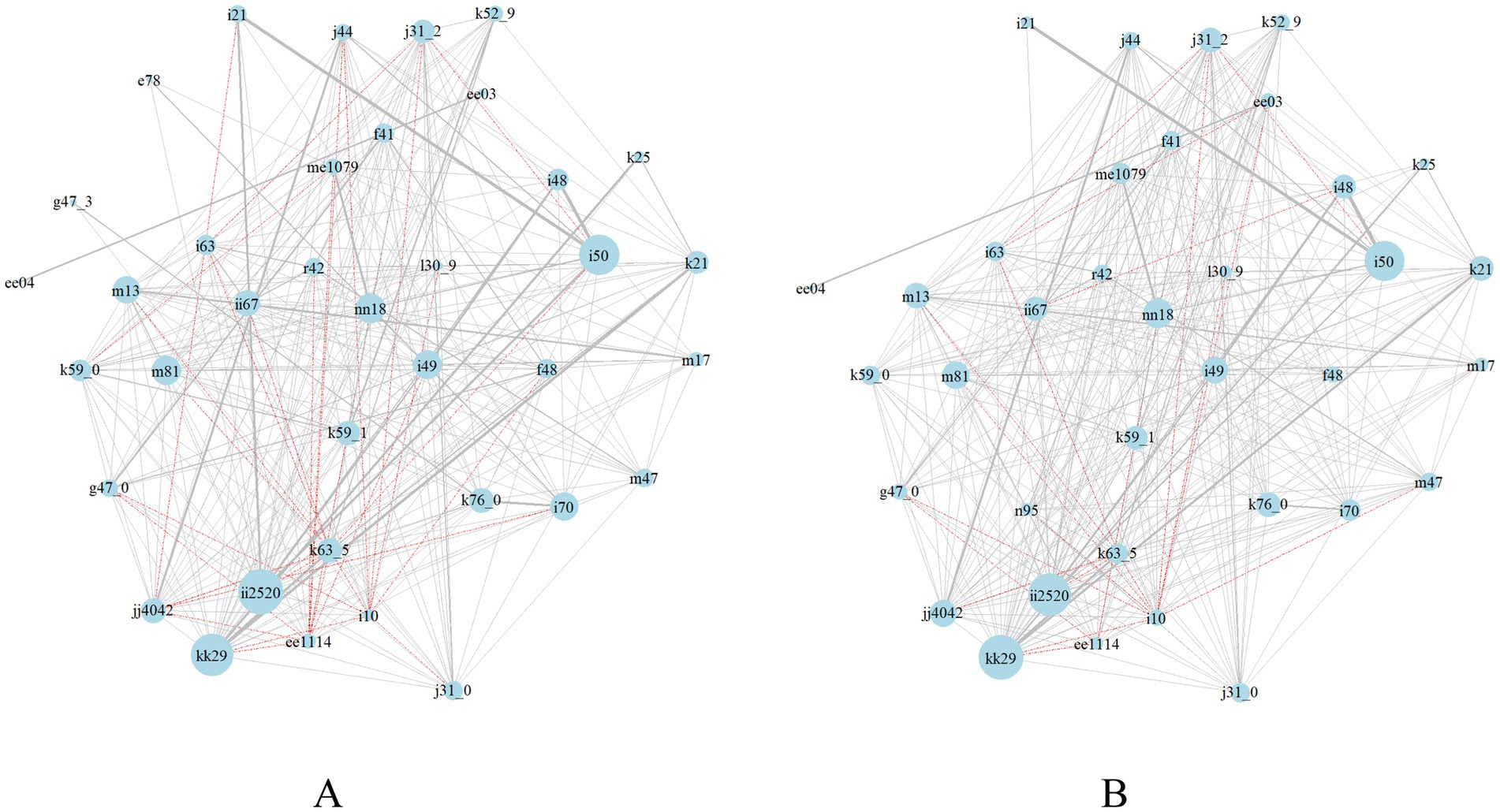
Figure 2. Comorbidity network in men (A) and women (B) aged 60 to 99 years. Nodes represent chronic diseases. Node size is proportional to the strength of diseases. Edges connect comorbid diseases. Black edges indicate positive correlations and red edge indicates negative correlations. Edge thickness indicates the intensity of the correlation.
T2DM was found to be positively associated with nine diseases and negatively associated with three diseases. The nine diseases were chronic kidney failure, NAFLD, hypertension, atherosclerosis, heart failure, IHD, cerebral infarction, osteoporosis, and constipation. The three diseases were chronic pharyngitis, sleep disorders, and gastritis. Additionally, men were more likely than women to have acute myocardial infarction and less likely to have dizziness and giddiness, polyps of the colon, bronchitis, hyperuricemia, and COPD alongside T2DM. In women, T2DM additionally exhibited positive associations with hyperuricemia, arthritis, bronchitis, gastroenteritis and colitis, and dermatitis.
There were positive correlations between IHD and 28 diseases which included cardiovascular pathology (e.g., acute myocardial infarction, heart failure, cardiac arrhythmia, atrial fibrillation and flutter, cerebrovascular disease, hypertension, cerebral infarction, atherosclerosis, and LMD), chronic kidney failure, osteoporosis, arthritis, bronchitis, chronic pharyngitis, sleep disorders, T2DM, functional diarrhea, NAFLD, chronic rhinitis, gonarthrosis, and gastroenteritis and colitis. Women were additionally found to have hyperuricemia, gastric ulcer, spondylosis, and dermatitis with IHD.
Gastritis was positively associated with gastrointestinal (GI) disorders such as GERD with esophagitis, gastric ulcers, polyps of the colon, gastroenteritis and colitis, functional diarrhea, and constipation. It was also positively correlated with 26 other diseases, such as chronic pharyngitis, chronic rhinitis, NAFLD, anxiety disorders, bronchitis, osteoporosis, cardiac arrhythmia, IHD, sleep disorders, and COPD. Furthermore, it was negatively correlated with T2DM and hypertension. As mentioned above, the negative correlation indicated a lower frequency of existing simultaneously. The comorbidity pairs still existed. Women additionally had cerebral infarction, hyperuricemia, and (peri-) menopausal disorders positively associated with gastritis.
In men, LMD was positively associated with atherosclerosis, IHD, and hyperuricemia. It should be noted that women were not sampled for LMD and its associated diseases due to the low frequency of comorbidity (Figure 2).
3.4 Network centrality of the 38 analyzed diseases
This study identified diseases with a strength greater than 5, a closeness equal to or greater than 0.007, and a betweenness greater than 50 as having strong centrality and were easily susceptible to comorbidity. Regarding the top five prevalent diseases, IHD (men: s = 10.879, c = 0.008, b = 83; women: s = 10.327, c = 0.008, b = 95) and gastritis (men: s = 10.178, c = 0.007, b = 90; women: s = 10.819, c = 0.007, b = 116) were the major two diseases that would easily be susceptible to comorbidity in both men and women. Among the 38 diseases, NAFLD (men: s = 5.918, c = 0.007, b = 87; women: s = 5.991, c = 0.007, b = 55), polyps of the colon (men: s = 5.846, c = 0.007, b = 64), osteoporosis (men: s = 7.011, c = 0.008, b = 70), and atherosclerosis (men: s = 6.750, c = 0.007, b = 73) were strongly associated with other diseases. Furthermore, the centrality of heart failure (men: s = 9.612, c = 0.008, b = 97; women: s = 9.671, c = 0.008, b = 110) was strong, indicating that this disease could commonly develop into outcome complications and thus correlated with the majority of the analyzed chronic diseases (Table 1).
3.5 Network-based community classification of the top five prevalent diseases
Modularities for clustering were both greater than 0.3 by gender (men: 0.34, women: 0.31), indicating that this method is effective in clearly categorizing the target diseases into smaller communities. In men, a cluster was observed among T2DM, hypertension, chronic kidney failure, hyperuricemia, NAFLD, atherosclerosis, LMD, and sleep apnea. A cluster was identified among IHD, cardiac arrhythmia, heart failure, acute myocardial infarction, and atrial fibrillation and flutter. Gastritis clustered with polyps of the colon, gastroenteritis and colitis, GERD with esophagitis, and gastric ulcers (Figure 3A). In women, a cluster was observed among T2DM, chronic kidney failure, hyperuricemia, hypothyroidism, NAFLD, atherosclerosis, non-toxic diffuse goiter, and hypertension. Gastritis clustered with polyps of the colon, gastritis, GERD with esophagitis, functional diarrhea, and gastric ulcers. IHD clustered with cardiac arrhythmias, atrial fibrillation flutter, heart failure, and acute myocardial infarction (Figure 3B).
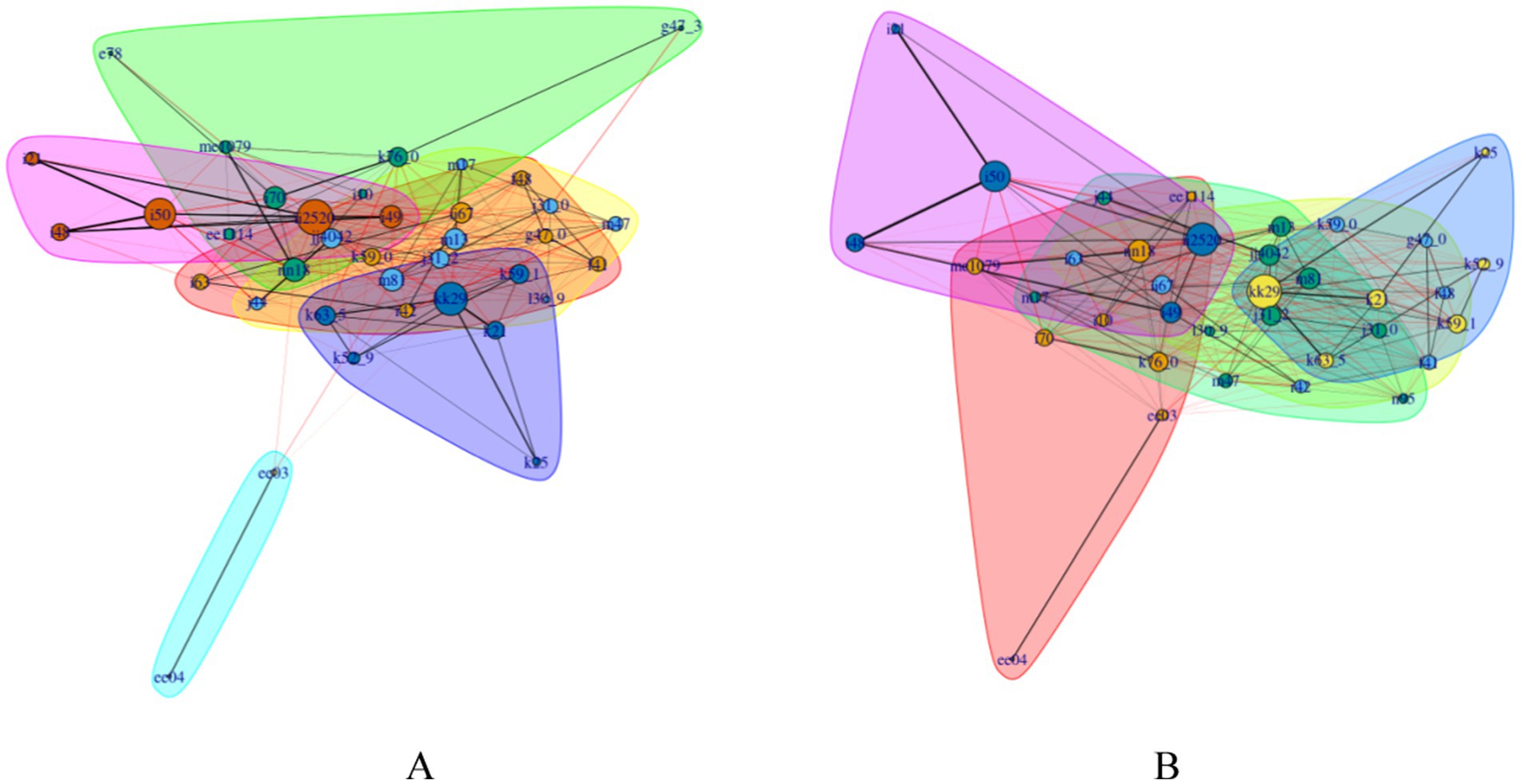
Figure 3. Network-based community clustering in men (A) and women (B) aged 60 to 99 years. Definitions of node, node size, and edge thickness remain constant, as described in Figure 2. Each cluster with a specific color refers to a disease community. Edges within the same cluster are in black. Edges across different clusters are in red. The color of nodes remains the same within the cluster.
Additional clusters were identified. In men, sleep disorders were clustered with cerebral infarction, cerebrovascular disease, dizziness and giddiness, neurotic disorders, constipation, and anxiety disorders. Bronchitis was associated with arthritis, dermatitis, COPD, chronic rhinitis and pharyngitis, osteoporosis, gonarthrosis, and spondylosis. Hypothyroidism was associated with non-toxic diffuse goiter. In women, sleep disorders were clustered with constipation, cerebral infarction, cerebrovascular disease, dizziness and giddiness, anxiety disorders, and neurotic disorders. Bronchitis was clustered with osteoporosis, arthritis, dermatitis, chronic rhinitis and pharyngitis, osteoarthrosis, gonarthrosis, spondylosis, (peri-)menopausal disorders, and COPD (Figure 3).
4 Discussion
4.1 Chronic ischemic heart disease and its comorbidity patterns
IHD is associated with chronic diseases such as cardiovascular pathology, GI disorders, chronic kidney failure, osteoporosis, arthritis, bronchitis, chronic pharyngitis, sleep disorders, T2DM, NAFLD, chronic rhinitis, and gonarthrosis. IHD is one of the major types of cardiovascular disease (CVD) developing in China. Known studies have analyzed that IHD is closely associated with hypertension, T2DM, LMD, overweight or obesity, and unhealthy lifestyles. Risk factors are not significantly different between men and women (15). This study indicated that IHD is associated with not only commonly recognized CVD, cerebrovascular diseases, and T2DM but also abnormalities of hepatic and renal function, upper respiratory problems, lung diseases, bone and joint diseases, mental disorders, and GI disorders, which are susceptible to comorbidity in older patients with IHD. Deterioration of renal function is one of the most common comorbidities of IHD and CVD, which is often accompanied by heart failure as well (16, 17). NAFLD and CVD are manifestations of end-organ damage in the metabolic syndrome, and they are associated with each other through multiple mechanisms. Patients with IHD are likely to have atherosclerosis, cardiomyopathy, and arrhythmia, which contribute to CVD morbidity and mortality (18). CVD and IHD are also the most common comorbidities of COPD, accelerating disease progression, increasing risk factors, and resulting in the usage of therapeutic agents (19). Gastritis, gastric ulcers, osteoarthritis, and upper respiratory tract problems, such as chronic nasopharyngitis and bronchitis, induced by IHD are triggered by inflammatory mechanisms, a very common comorbidity pattern in older patients (20). Mental disorders such as sleep disorders, anxiety disorders, and vertigo are triggered by stress (21). This pattern is associated with a long duration of illness, high therapeutic difficulty, and high mortality of IHD. In addition, the comorbidity of hyperuricemia, dermatitis, and spondylosis in women with IHD was identified. Although asymptomatic hyperuricemia has long been considered to be a marker of metabolic disorders, several prospective large-scale clinical studies suggested that it may be an independent risk factor for CVD and IHD, and is strongly associated with poor outcomes of cardiac, vascular, and renal problems (22, 23).
4.2 Early detection and implications for disease control for chronic ischemic heart disease comorbidity patterns
Due to the complexity of IHD comorbidity patterns in older patients, it is necessary to apply a multidisciplinary diagnosis strategy to monitor these conditions in the early stage. It is crucial to regularly screen blood pressure, blood glucose, serum lipid level, hepatic and renal function, cardio-respiratory function, inflammatory response, and other physiological conditions for IHD patients (24–26). The intervention strategy should focus on preventing end-organ damages associated with metabolic syndrome, such as atherosclerosis, myocardial problems, and arrhythmias. Due to the strong association between IHD, heart failure, CVD, COPD, and decline in renal function, it is therefore recommended that monitoring cardiac, pulmonary, and renal functions plays an important role in preventing the potential morbidity of IHD (16). NAFLD and IHD interact through similar metabolic pathways. We recommended that IHD patients ease the double burden of the liver and cardiovascular system by weight management and glycaemic control. Women with IHD are more likely to have hyperuricemia, dermatitis, and spondylosis problems. It will be helpful to monitor inflammatory levels of the whole body to prevent adverse complications (27).
4.3 Chronic gastritis and its comorbidity patterns
Although the results of the community classification demonstrated that gastritis comorbidity patterns in older patients were predominantly associated with conventional GI diseases, network analysis provided a more general vision of all the potential diseases that are susceptible to gastritis. The comorbidity of gastritis with upper respiratory tract diseases may be attributed to acid reflux, which irritates the mucosa of the digestive system and ultimately exacerbates symptoms (28). A long-term diet high in fat and cholesterol may impact hepatic metabolism, potentially leading to the development of NAFLD. This is followed by the presentation of impaired endocrine function, which reduces the decomposition ability of greasy food, and then elevated GI burden (29). The prevalence of gastritis, ulcerative esophagitis, duodenitis, and other GI diseases is increased in patients with chronic kidney failure and hyperuricemia (30). Patients with gastritis are also susceptible to mental disorders, which result from the psychological burden due to long-term treatment (31). The comorbidity pattern between gastritis and hypothyroidism is also significant in older patients because hypothyroidism may lower appetite and slow down GI peristalsis. In this case, gastric disorders such as gastritis, dyspepsia, and constipation may happen (32, 33). Additionally, chronic gastritis may result in a systemic low-grade inflammatory response, thereby increasing the risk of vascular endothelial damage and CVD (34). It is important to highlight the increased prevalence of menopausal disorders, cerebral infarction, and hyperuricemia in women with gastritis compared to men. During the menopausal stage, as the decline of ovarian function lowers estrogen levels, it leads to endocrine disruption and results in changes in hormone levels, which may affect GI tract function, thereby increasing the risk of gastritis (35). Hormone fluctuation affects gut microbiota dysbiosis in the menopausal stage, which can also affect GI functions (36). In addition, cerebral infarction and hyperuricemia are risks resulting from the long-term use of non-steroidal anti-inflammatory drugs (NSAIDs) and unhealthy diets.
4.4 Early detection and implications for disease control for gastritis comorbidity patterns
Most patients with chronic gastritis and its morbidity have been taking anti-inflammatory agents and other medications for a long period. Consequently, the primary objective of risk prevention should be protecting GI mucosa by selecting appropriate medications (37). It is recommended that patients should take medications with less irritation to GI mucosa, along with mucosal protectors and slow-released preparations, or take medicine after meals (38). The side effects of medications should be regularly assessed. It is recommended that older patients should intake low-fat, low-cholesterol diets to promote GI function. GI symptoms such as dyspepsia and constipation in gastritis patients with hypothyroidism need to be monitored frequently to facilitate timely intervention. Additionally, chronic gastritis can also impose a systemic low-grade inflammatory response, thereby increasing the risk of CVD (34). In treating complications, the usage of medications with multi-target effects is a priority, along with appropriate adjustment of quantity, dosage, and frequency to reduce side effects. Furthermore, women with gastritis around 60 years should be particularly concerned about the potential comorbidities associated with menopausal diseases, such as cerebral infarction and hyperuricemia. Given the fluctuations in hormone levels during this phase of the disease, it is important to monitor endocrine function frequently, as it may impact GI conditions (39).
4.5 A ternary comorbidity pattern of type 2 diabetes mellitus, hypertension, and lipid metabolism disorders
T2DM, hypertension, and LMD were identified in the same community with some other chronic diseases such as hyperuricemia and hypothyroidism for women and sleep apnea for men, which indicated that these chronic diseases were closely related, and hypertension is prone to comorbid with metabolic syndromes (40). The major causes of this comorbidity pattern include insulin resistance, chronic inflammatory response, obesity, genetic factors, endothelial dysfunction, unhealthy lifestyle, and renal impairment. These factors interact to form a complex network of metabolic syndromes. The coexistence of chronic renal failure and hyperuricemia in this pattern may result from the fact that insulin resistance elevated uric acid levels (41, 42). Chronic inflammatory response exacerbates insulin resistance by triggering responses of C-reactive protein (CRP), tumor necrosis factor-alpha (TNF-α), and interleukin-6 (IL-6), resulting in T2DM and renal impairment and increasing uric acid levels (43, 44). Meanwhile, elevated blood glucose in the liver activates glycogen synthase to accumulate hepatic fat, leading to LMD and NAFLD (45). In women, the decreasing insulin sensitivity is associated with the decreased metabolic rate of thyroid hormones, which triggers hypothyroidism and goiter (46). Both T2DM and hypothyroidism increase the risk of high cholesterol and hypertension, which are common cardiovascular risk factors in people with T2DM. Sleep apnea syndrome in male patients will lead to frequent apneic episodes and hypoxemia, which is associated with hypertension by activating and raising oxidation (47). Activating the sympathetic nervous system may contribute to insulin resistance, which can increase the risk of T2DM (48).
4.6 Early detection and implications for disease control for comorbidity pattern of type 2 diabetes mellitus, hypertension, and lipid metabolism disorders
The prevention of this ternary comorbidity pattern should focus on regulating blood glucose and insulin levels by pharmacological approaches such as in-taking metformin and insulin sensitizers. It is recommended that a healthy lifestyle, including weight management, frequent physical activity, and low-sugar, low-fat diets, can improve insulin sensitivity, overall metabolic status, and lower inflammation makers (49, 50). Regular detections of hepatic and renal function can help identify early impairment in older patients with T2DM and hyperuricemia.
It is also essential to consider gender factors in this comorbidity pattern. Female patients are recommended to regularly assess thyroid gland function and hormone levels due to the potential interaction between hypothyroidism and T2DM. Male patients undergoing sleep apnea syndrome should specifically screen their blood pressure and blood glucose. Using a respiratory assistant device and modifying sleeping posture to improve sleep quality. Taking less fats, sugar, salts, and alcohol will reduce the progression of comorbidity.
4.7 Mental health management and patient self-management
Neurotic disorders, sleep disorders, and other psychiatric factors were prevalent in the comorbidity pattern discussed above. It can be inferred that the long-term treatment of comorbidity in older adults is often accompanied by challenges on the psychological burden, such as anxiety and depression, which have a significant impact on patients’ life quality and motivation for treatment. Comorbidities, such as insomnia and neurotic disorders, will develop into a chronic inflammatory response that affects cardiovascular, cerebral, respiratory, and GI health. Therefore, strengthening emotional support for older patients with comorbidity is an indispensable part of their treatment. This not only helps to reshape their confidence but also significantly improves their cooperation and ensures the effectiveness of treatment plans. For patients presenting with severe emotional disturbances, it is recommended that close collaboration with psychologists be established to implement psychological interventions and emotional relief strategies. Furthermore, self-management plays an active role in maintaining health conditions. Patients are encouraged to learn basic disease mechanisms and how to utilize medical tools to regularly monitor their health data, such as heart rate, blood pressure, blood glucose, and uric acid, to take immediate action to any potential health problems.
4.8 Implications and potential policy actions
Shanghai is a typical region in China facing comorbidity challenges. The network analysis is an effective approach for public health practitioners to quickly identify potential comorbidity patterns among the target population and then take action to reduce risk factors of disease development. This study discovered pre-existing comorbidity patterns and unusual ones, providing evidence to strengthen more effective management strategies. New-identified patterns may draw more attention from practitioners for the development of novel technology and strategies to monitor and prevent risk factors. Currently, China is implementing community-based primary medical services. It offers free screening for common chronic diseases such as T2DM, ICH, and GI diseases. Patients with T2DM could have additional screenings on thyroid function, uric acid levels, and sleeping quality. In addition, residents are encouraged to enroll in the family doctor program. Family doctors are suggested to provide personalized medical consultations regarding the potential comorbidity patterns older adults may have, helping them strengthen comorbidity monitoring, arrange appropriate follow-up visits, and maintain good mental health. These actions aim to prevent and slow down the development of comorbidity and reduce any further medical burden for both patients and the public health system.
4.9 Limitations
The dataset was derived from cross-sectional medical records, so it is not appropriate to conclude causality. There were no covariates, such as educational level, smoking, and drinking alcohol, including for data analysis because medical records did not contain such information. In addition, some diseases were initially categorized vigorously in ICD-10. In this case, the final subjects included in some disease groups might be less than or more than expected, which leads to bias in the analysis. Moreover, the results only represented some general comorbidity patterns in the region of Shanghai, which lacked normality across the whole target population in China. Therefore, the implications for disease control could only be applied within the specific region.
5 Conclusion
The visualized analysis revealed that the most two prevalent comorbidity patterns among the study population were dominated by IHD and gastritis, followed by a ternary pattern of hypertension, T2DM, and LMD. Men are more likely to simultaneously have cardiovascular and sleep problems than women when they suffer from the top five prevalent diseases, whereas thyroid disease, chronic inflammatory diseases, and hyperuricemia are more commonly comorbid within women. By monitoring vital signs, such as heart rate, blood pressure, blood glucose, hepatic and renal function, and inflammatory markers, and their influencing factors within comorbidity patterns, healthcare professionals may take immediate actions toward the potential onset of comorbidity. Furthermore, it is vital to pay more attention to the mental health of patients who suffer from long-term chronic diseases and undergo complex treatment over a long period. Given the accelerating aging problem in Shanghai, it is insufficient to intervene after diseases occur. Early detection and prevention strategies are also necessary to control the onset, progression, and mortality rates. This study provided a general insight into the current comorbidity situation among older adults in Shanghai and suggestions on prevention strategies, which may help control the prevalence of chronic diseases.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: Dataset is not available to the public due to ethical restrictions. Requests to access these datasets should be directed to bml1eXVob25nQDEyNi5jb20=.
Ethics statement
The studies involving humans were approved by the Shanghai Medical and Technology Information Institute Ethics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
YS: Conceptualization, Data curation, Formal analysis, Writing – original draft, Writing – review & editing. WT: Data curation, Formal analysis, Visualization, Writing – review & editing. NL: Conceptualization, Writing – review & editing. YN: Conceptualization, Funding acquisition, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by the Natural Science Foundation of Shanghai Municipality under Grant No. 23ZR1458400.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1516215/full#supplementary-material
References
1. WHO. Multimorbidity: Technical Series on Safer Primary Care. Geneva: World Health Organization (2016).
2. Du, P, Zhai, ZZ, and Chen, W. The elderly population of China: a century -long projection. Popul. Res. (2005) 29:90–3.
3. Wang, J, Wang, Y, Bao, Z, Zhang, Z, Zhao, C, and Huang, Y. Epidemiological analysis on chronic disease and multi·morbidity in middle and elderly health-examination population in Shanghai city. Geriatr Health Care. (2016) 22:116–20. doi: 10.3969/j.issn.1008-8296.2016.02.17
4. Fu, L, Ding, L, and Chen, Q. Effects of multimorbidity on medical services utilization, cost and urban-rural difference among the middle-aged and elderly:an empirical analysis based on the data from CHARLS. Chinese Rural Health Serv Adm. (2015, 2021) 41:6.
5. Wang, FL, Yang, C, Du, J, Kong, GL, and Zhang, LX. Patterns of multimorbidity in the middle-aged and elderly population in China: a cluster analysisbased on self-organizing map. Med J Chin PLA. (2022) 47:1217–25. doi: 10.11855/j.issn.0577-7402.2022.12.1217
6. Tang, J, Liu, X, Mo, Q, Liu, Y, Huang, D, Liu, S, et al. Analysis of the influencing factors and patterns of comorbidity among the Zhuang population in Guangxi. J Guangxi Med Univ. (2023) 40:2084–92. doi: 10.16190/j.cnki.45-1211/r.2023.12.023
7. Shi, C, and Chen, MS. Prevalence and control multimorbidity of non-communicable chronic diseases in the communities in Jiangsu Province based on network analysis. Chinese Health Econ. (2021) 40:52–5.
8. Lee, HA, and Park, H. Comorbidity network analysis related to obesity in middle-aged and older adults: findings from Korean population-based survey data. Epidemiol Health. (2021) 43:e2021018. doi: 10.4178/epih.e2021018
9. Chen, M, Li, C, Liao, P, Cui, X, Tian, W, Wang, Q, et al. Epidemiology, management, and outcomes of atrial fibrillation among 30 million citizens in Shanghai, China from 2015 to 2020: a medical insurance database study. Lancet Regional Health Western Pacific. (2022) 23:100470. doi: 10.1016/j.lanwpc.2022.100470
10. Chen, JH, and Chen, ZH. Extended Bayesian information criteria for model selection with large model spaces. Biometrika. (2008) 95:759–71. doi: 10.1093/biomet/asn034
11. Foygel, R, and Drton, M. Bayesian model choice and information criteria in sparse generalized linear models. arXiv. (2011). doi: 10.48550/arXiv.1112.5635
12. Ravikumar, P, Wainwright, MJ, and Lafferty, JD. High-dimensional Ising model selection using ℓ1-regularized logistic regression. Ann Stat. (2010) 38:1287–319. doi: 10.1214/09-AOS691
13. Clauset, A, Newman, ME, and Moore, C. Finding community structure in very large networks. Phys Rev E Stat Nonlinear Soft Matter Phys. (2004) 70:066111. doi: 10.1103/PhysRevE.70.066111
14. National Health Commission of the PRC. Approaches to ethical review of research in the life sciences and medicine involving human beings. Beijing: National Health Commission of the PRC (2023).
15. Lin, S, Peng, W, Lin, X, Lu, J, Huang, F, and Li, J. A systematic review of the main risk factors of ischemic heart disease in China. Disease Surveillance. (2024) 39:488–96. doi: 10.3784/jbjc.202311150595
16. Sun, YQ, Lyu, Q, Du, X, and Dong, JZ. Advances in the diagnosis and treatment of worsening renal function in patients with heart failure. Zhonghua Xin Xue Guan Bing Za Zhi. (2023) 51:443–8. doi: 10.3760/cma.j.cn112148-20221122-00918
17. Mathew, RO, Bangalore, S, Lavelle, MP, Pellikka, PA, Sidhu, MS, Boden, WE, et al. Diagnosis and management of atherosclerotic cardiovascular disease in chronic kidney disease: a review. Kidney Int. (2017) 91:797–807. doi: 10.1016/j.kint.2016.09.049
18. Stahl, EP, Dhindsa, DS, Lee, SK, Sandesara, PB, Chalasani, NP, and Sperling, LS. Nonalcoholic fatty liver disease and the heart: JACC state-of-the-art review. J Am Coll Cardiol. (2019) 73:948–63. doi: 10.1016/j.jacc.2018.11.050
19. Chen, RC, Kang, J, and Sun, YC. Chinese expert consensus on the management of cardiovascular comorbidities in patients with chronic obstructive pulmonary disease. Chinese J Tuberculosis Respiratory Dis. (2022) 45:1180–91. doi: 10.3760/cma.j.cn112147-20220505-00380
20. Vilela, EM, and Fontes-Carvalho, R. Inflammation and ischemic heart disease: the next therapeutic target? Rev Port Cardiol. (2021) 40:785–96. doi: 10.1016/j.repc.2021.02.011
21. Miao, Z, Wang, Y, and Sun, Z. The relationships between stress, mental disorders, and epigenetic regulation of BDNF. Int J Mol Sci. (2020) 21:1375. doi: 10.3390/ijms21041375
22. Hyperuricemia-expert-group. The diagnosis and treatment advice of cardiovascular disease combined asymptomatic hyperuricemia (second edition). Chinese J Cardiovasc Res. (2012) 10:241–9. doi: 10.3969/j.issn.1672-5301.2012.04.001
23. Feng, GK, and Xu, L. Interpretation of the expert consensus for the diagnosis and treatment of patient with hyperuricemia and high cardiovascular risk: 2021 update. Pract J Cardiac Cerebral Pneumal Vasc Dis. (2021) 5:1–7. doi: 10.5603/CJ.a2021.0001
24. Shah, MU, Roebuck, A, Srinivasan, B, Ward, JK, Squires, PE, Hills, CE, et al. Diagnosis and management of type 2 diabetes mellitus in patients with ischaemic heart disease and acute coronary syndromes - a review of evidence and recommendations. Front Endocrinol. (2024) 15:1499681. doi: 10.3389/fendo.2024.1499681
25. Yang, L, Wang, L, Deng, Y, Sun, L, Lou, B, Yuan, Z, et al. Serum lipids profiling perturbances in patients with ischemic heart disease and ischemic cardiomyopathy. Lipids Health Dis. (2020) 19:89. doi: 10.1186/s12944-020-01269-9
26. Niu, Y, Wang, G, Feng, X, Niu, H, and Shi, W. Significance of fatty liver index to detect prevalent ischemic heart disease: evidence from national health and nutrition examination survey 1999-2016. Front Cardiovasc Med. (2023) 10:1171754. doi: 10.3389/fcvm.2023.1171754
27. Cappannoli, L, Galli, M, Borovac, JA, Valeriani, E, Animati, FM, Fracassi, F, et al. Editorial: inflammation in ischemic heart disease: pathophysiology, biomarkers, and therapeutic implications. Front Cardiovasc Med. (2024) 11:1469413. doi: 10.3389/fcvm.2024.1469413
28. Durazzo, M, Adriani, A, Fagoonee, S, Saracco, GM, and Pellicano, R. Helicobacter pylori and respiratory diseases: 2021 update. Microorganisms. (2021) 9:2033. doi: 10.3390/microorganisms9102033
29. Wu, W, Ma, W, Yuan, S, Feng, A, Li, L, Zheng, H, et al. Associations of unhealthy lifestyle and nonalcoholic fatty liver disease with cardiovascular healthy outcomes. J Am Heart Assoc. (2023) 12:e031440. doi: 10.1161/JAHA.123.031440
30. Thomas, R, Panackal, C, John, M, Joshi, H, Mathai, S, Kattickaran, J, et al. Gastrointestinal complications in patients with chronic kidney disease—a 5-year retrospective study from a tertiary referral center. Ren Fail. (2013) 35:49–55. doi: 10.3109/0886022X.2012.731998
31. Goodwin, RD, Cowles, RA, Galea, S, and Jacobi, F. Gastritis and mental disorders. J Psychiatr Res. (2013) 47:128–32. doi: 10.1016/j.jpsychires.2012.09.016
32. Maser, C, Toset, A, and Roman, S. Gastrointestinal manifestations of endocrine disease. World J Gastroenterol. (2006) 12:3174–9. doi: 10.3748/wjg.v12.i20.3174
33. Kyriacou, A, McLaughlin, J, and Syed, AA. Thyroid disorders and gastrointestinal and liver dysfunction: a state of the art review. Eur J Intern Med. (2015) 26:563–71. doi: 10.1016/j.ejim.2015.07.017
34. Hofseth, LJ, and Hébert, JR. Chapter 3 - diet and acute and chronic, systemic, low-grade inflammation In: JR Hébert and LJ Hofseth, editors. Diet, inflammation, and health. Cambridge, MA: Academic Press (2022). 85–111.
35. Liu, Z, Zhang, Y, Lagergren, J, Li, S, Li, J, Zhou, Z, et al. Circulating sex hormone levels and risk of gastrointestinal Cancer: systematic review and Meta-analysis of prospective studies. Cancer Epidemiol Biomarkers Prevent. (2023) 32:936–46. doi: 10.1158/1055-9965.EPI-23-0039
36. Liu, Y, Zhou, Y, Mao, T, Huang, Y, Liang, J, Zhu, M, et al. The relationship between menopausal syndrome and gut microbes. BMC Womens Health. (2022) 22:437. doi: 10.1186/s12905-022-02029-w
37. Sostres, C, Gargallo, CJ, Arroyo, MT, and Lanas, A. Adverse effects of non-steroidal anti-inflammatory drugs (NSAIDs, aspirin and coxibs) on upper gastrointestinal tract. Best Pract Res Clin Gastroenterol. (2010) 24:121–32. doi: 10.1016/j.bpg.2009.11.005
38. Kanno, T, and Moayyedi, P. Who needs Gastroprotection in 2020? Curr Treat Options Gastroenterol. (2020) 18:557–73. doi: 10.1007/s11938-020-00316-9
39. Di Ciaula, A, Wang, DQH, Sommers, T, Lembo, A, and Portincasa, P. Impact of endocrine disorders on gastrointestinal diseases In: P Portincasa, G Frühbeck, and HM Nathoe, editors. Endocrinology and systemic diseases. Cham: Springer International Publishing (2021). 179–225.
40. Ginsberg, HN, and MacCallum, PR. The obesity, metabolic syndrome, and type 2 diabetes mellitus pandemic: part I. Increased cardiovascular disease risk and the importance of atherogenic dyslipidemia in persons with the metabolic syndrome and type 2 diabetes mellitus. J Cardiometab Syndr. (2009) 4:113–9. doi: 10.1111/j.1559-4572.2008.00044.x
41. Schrauben, SJ, Jepson, C, Hsu, JY, Wilson, FP, Zhang, X, Lash, JP, et al. Insulin resistance and chronic kidney disease progression, cardiovascular events, and death: findings from the chronic renal insufficiency cohort study. BMC Nephrol. (2019) 20:60. doi: 10.1186/s12882-019-1220-6
42. Han, T, Lan, L, Qu, R, Xu, Q, Jiang, R, Na, L, et al. Temporal relationship between hyperuricemia and insulin resistance and its impact on future risk of hypertension. Hypertension. (2017) 70:703–11. doi: 10.1161/HYPERTENSIONAHA.117.09508
43. Li, M, Chi, X, Wang, Y, Setrerrahmane, S, Xie, W, and Xu, H. Trends in insulin resistance: insights into mechanisms and therapeutic strategy. Signal Transduct Target Ther. (2022) 7:216. doi: 10.1038/s41392-022-01073-0
44. Yu, W, Xie, D, Yamamoto, T, Koyama, H, and Cheng, J. Mechanistic insights of soluble uric acid-induced insulin resistance: insulin signaling and beyond. Rev Endocr Metab Disord. (2023) 24:327–43. doi: 10.1007/s11154-023-09787-4
45. Samuel, VT, Liu, Z-X, Qu, X, Elder, BD, Bilz, S, Befroy, D, et al. Mechanism of hepatic insulin resistance in non-alcoholic fatty liver disease*. J Biol Chem. (2004) 279:32345–53. doi: 10.1074/jbc.M313478200
46. Choi, YM, Kim, MK, Kwak, MK, Kim, D, and Hong, E-G. Association between thyroid hormones and insulin resistance indices based on the Korean National Health and nutrition examination survey. Sci Rep. (2021) 11:21738. doi: 10.1038/s41598-021-01101-z
47. Van Ryswyk, E, Mukherjee, S, Chai-Coetzer, CL, Vakulin, A, and McEvoy, RD. Sleep disorders, including sleep apnea and hypertension. Am J Hypertens. (2018) 31:857–64. doi: 10.1093/ajh/hpy082
48. Reutrakul, S, and Mokhlesi, B. Obstructive sleep apnea and diabetes: a state of the art review. Chest. (2017) 152:1070–86. doi: 10.1016/j.chest.2017.05.009
49. Bird, SR, and Hawley, JA. Update on the effects of physical activity on insulin sensitivity in humans. BMJ Open Sport Exerc Med. (2016) 2:e000143. doi: 10.1136/bmjsem-2016-000143
Keywords: older adults, aging, chronic disease, comorbidity network, community classification, disease prevention
Citation: Shen Y, Tian W, Li N and Niu Y (2025) Comorbidity patterns and implications for disease control: a network analysis of medical records from Shanghai, China. Front. Public Health. 13:1516215. doi: 10.3389/fpubh.2025.1516215
Edited by:
Jaideep Menon, Amrita Vishwa Vidyapeetham University, IndiaReviewed by:
Zhipeng Wu, Central South University, ChinaPanniyammakal Jeemon, Sree Chitra Tirunal Institute for Medical Sciences and Technology (SCTIMST), India
Copyright © 2025 Shen, Tian, Li and Niu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuhong Niu, bml1eXVob25nQDEyNi5jb20=
†ORCID: Yifei Shen, https://orcid.org/0009-0008-3285-0380
 Yifei Shen
Yifei Shen Wenqi Tian2
Wenqi Tian2