
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 26 February 2025
Sec. Children and Health
Volume 13 - 2025 | https://doi.org/10.3389/fpubh.2025.1497136
Introduction: The association between parental smoking and adolescent mental health is not well understood. We aimed to examine the association between parental smoking and adolescent loneliness using global data collected from the Global School-based Student Health Survey (GSHS) between 2009 and 2019.
Methods: A total of 187,552 adolescents aged 12–15 years in 71 low- and middle-income countries (LMIC) from the GSHS with cross-sectional design were included in this study. Loneliness was defined as feeling lonely sometimes or more frequently in the past 12 months. Parental smoking, reported by the adolescent, was defined as the use of any form of tobacco by the father and/or mother. Logistic regression models were used to examine the odds ratio (OR) of adolescent loneliness according to parental smoking status.
Results: Compared with neither parent smoking, parental smoking was associated with adolescent loneliness (father only: OR = 1.18, 95% CI = 1.10–1.26; mother only: OR = 1.39, 95% CI = 1.15–1.67; both: OR = 1.65, 95% CI = 1.41–1.93) after adjustment for potential covariates. Subgroup analyses stratified by sex, age, and WHO region showed similar results (except not in the African and Western Pacific regions).
Discussion: Parental smoking is associated with loneliness in adolescents from LMIC. Our finding expands the well-known physical damage of parental smoking in adolescents to the psychological damage. Strict policies and strategies should be established to encourage smoking cessation for parents who are current smokers.
Secondhand smoke exposure among adolescents has been identified as a major modifiable risk factor for morbidity and mortality (1). Globally, the proportion of adolescents exposed to secondhand smoke at any place on more than 1 day in the past 7 days exceeded 60% based on data from 142 countries/territories in 2010–2018, with more than 30% of adolescents exposed to secondhand smoke at home (2). Parental smoking is the main source of secondhand smoke exposure at home (3). It has been shown that adolescents with parents that smoked were more likely to start smoking (4, 5). In addition, parental smoking has been associated with adverse effects on adolescent health such as an increased likelihood of elevated blood pressure, obesity, cardiometabolic risk in childhood, respiratory symptoms, reduced lung function, and multiple sclerosis during adolescence (6–11).
Parental smoking not only increases physical health risk but also contributes to psychological harm. A study involving six European countries found that maternal smoking was associated with inattention and hyperactivity of their offspring, and another study of 617 families found that parental smoking was associated with an increased risk of disruptive behavior disorders, preference for risk taking, and aggressive attitudes (12, 13). Loneliness is defined as a painful encounter when the need for a person's intimacy is not met, or when a person's social network does not match his/her preference in terms of number or attributes. A study based on data from 25 countries showed that more than 18% of middle-school students reported feeling lonely most of the time or constantly (14). Another survey based on data from 37 countries indicated that the prevalence of loneliness among adolescents aged 15–16 years had nearly doubled in 2018 (30.9%) since 2012 (17.1%) (15). Adolescent loneliness has been identified as a significant risk factor for mental health disorders and suicidal ideation during adolescence and mental illness in adulthood (16–19). Epidemiological studies have assessed exposure to environmental tobacco smoke as a risk factor for a variety of behavioral and neurodevelopmental disorders in children (20, 21). In addition, maternal smoking during pregnancy is associated with mental deficits and behavioral problems in childhood (13). McCarthy et al. (22) also found that nicotine exposure has negative effects on the developing brain and has lasting effects on brain structure and neurotransmitter signaling. Although secondhand smoke exposure has been shown to be associated with adolescent loneliness (23), the association between parental smoking, as a proxy of secondhand smoke exposure, and adolescent loneliness remains unclear.
Using data from the Global School-based Student Health Survey (GSHS) conducted in 2009–2019, we aimed to assess the relationship between parental smoking and feelings of loneliness in adolescents aged 12–15 years from 71 low- and middle-income countries (LMIC).
The data were obtained from the GSHS, which was jointly developed by the WHO, the US Center for Disease Control and Prevention (CDC), and other United Nations allies. This survey is conducted in LMIC and follows standardized procedures to randomly select a study sample from schools. The aims of GSHS are to collect data on adolescents' health behaviors using the same standardized two-stage sampling methodology in each participating country. In the first stage, schools were randomly selected with a probability proportional to their enrolment size. In the second stage, classes with students in the targeted age groups (ages 12–15 years old) were also randomly selected. All students from each selected class were invited to fill in the structured questionnaire during normal school hours. The country-specific self-administration questionnaire consists of core questionnaire modules and country-specific questions. The questionnaires in English were translated into local language of each country and were pilot-tested for comprehension to ensure clarity for the participants. All responses were collected using self-administered, anonymous, computer-scannable forms to maintain privacy and facilitate efficient data collection. Participation was voluntary for all students and informed verbal or written consent was obtained from all students and their parents/guardians. A flowchart of exclusion/inclusion of the study participants is shown as Figure 1. A total of 187,552 students with complete information on parental smoking and loneliness were included in the study.
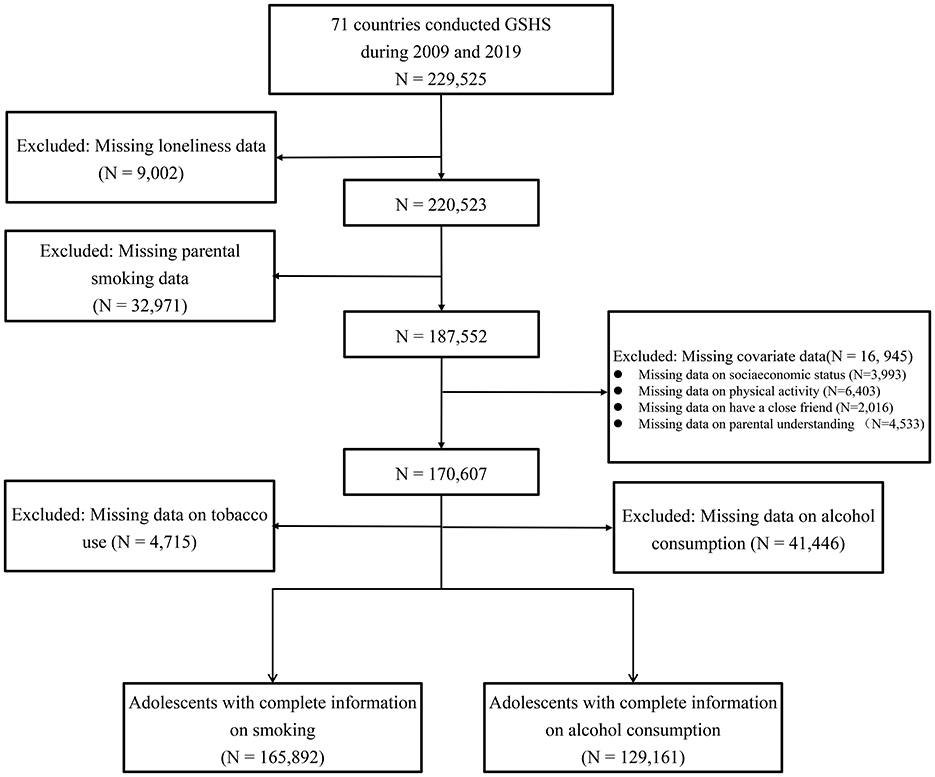
Figure 1. Flowchart of inclusion and exclusion of study participants. GSHS, Global School-based Student Health Survey.
Following previous studies (14, 24), the measure of adolescent loneliness was based on responses to the following question: “How often have you felt lonely in the past 12 months?” with five independent options representing the experience of participants (never, rarely, sometimes, most of the time, always) available for selection. For data analysis, participants were dichotomized into two groups based on the responses: (1) no loneliness (never or rarely); and (2) affirmative loneliness (sometimes, most of the time or always). In sensitivity analysis, participants were re-classified into two groups: (1) no loneliness (never, rarely or sometimes); and (2) affirmative loneliness (most of the time or always).
Parental smoking status was assessed by adolescent response to the question “Which of your parents or guardians use any form of tobacco?”, and the corresponding answers included “neither”, “my father or male guardian”, “my mother or female guardian”, and “both”.
Covariates of sex, age, socioeconomic status, sufficient physical activity, having close friends, parental understanding, survey year, and country were adjusted in our regression models because they may confound the association between parental smoking and adolescent loneliness. Based on previous studies, low socioeconomic status measured by hunger due to a lack of food, was defined as getting hungry most of the time or always due to a lack of food (25, 26). Sufficient physical activity was defined as participants engaging in active exercises on at least 60 min per day (27). Having close friends was defined as having at least one close friend (14). Parental understanding was defined as parents or guardians understanding adolescents' problems or worries most of the time or always (24). Based on participants' responses to the questions “During the past 30 days, on how many days did you smoke cigarettes?” and “During the past 30 days, on how many days did you use any tobacco products other than cigarettes, such as pipe, hand-rolled tobacco, or chewing tobacco?”, we categorized tobacco use into never, 1–9 days, and ≥10 days. Similarly, based on participants' responses to the question “During the past 30 days, on how many days did you have at least one drink containing alcohol?”, we categorized alcohol consumption into never, 1–9 days, and ≥10 days (28). Hunger due to lack of food was not adjusted for in Bhutan as this variable was not collected. Information on physical activity was not collected in Maldives and Malawi. In Cambodia parental understanding was not adjusted as information on this variable was not collected. Myanmar did not collect information on tobacco use, so this variable was not included for adjustment in this country. Similarly, Afghanistan, Bahrain, Egypt, Iraq, Kuwait, Morocco, Pakistan, Palestine, Qatar, United Arab Emirates, and Yemen did not collect information on alcohol consumption, and therefore this variable was not considered for adjustment in these countries.
Strata, primary sampling units, and sampling weights were considered in all data analyses based on the methodology of GSHS. Proportion estimates and standard errors of basic characteristics in each country were calculated. A Chi-square test was used to compare the prevalence of adolescent loneliness across different parental smoking categories, overall and by subgroup (sex, age group, and WHO region group). After adjusting for potential covariates, multivariable logistic regression models were used to assess the relationship between parental smoking and adolescent loneliness using odds ratios (ORs) and their 95% confidence intervals (CIs). Model 1 was adjusted for age, sex, and hunger due to lack of food. Model 2 was additionally adjusted for having a close friend, parent understanding your problem, doing enough physical activity, survey year, and country. Furthermore, we conducted a subgroup analysis by the categories of tobacco use and alcohol consumption. We also conducted a mediation analysis using bootstrap method (with 1,000 simulations) to examine the mediation effect of adolescent tobacco use or alcohol consumption in association between parental smoking and adolescent loneliness. A sensitivity analysis was performed using a different definition of loneliness based on participants' responses (detailed earlier). A two-sided P < 0.05 was considered statistically significant. All statistical analyses were conducted using SAS 9.4 (SAS Institute, Cary, North Carolina, USA), while the mediation analysis was performed using R version 4.3.1 with the mediation package (version 4.5.0).
Table 1 shows participant characteristics from 71 LMICs in five WHO regions surveyed from 2009 to 2019. A total of 187,552 adolescents aged 12–15 years with complete data on loneliness and parental smoking were included. Of these adolescents, 36.8% had at least one parental smoker, ranging from 7.1% in Panama to 76.6% in Tokelau; 39.6% reported feeling lonely sometimes or more frequently in the past 12 months, ranging from 17.9% in Tanzania to 67.8% in the Solomon Islands. Among those adolescents, 6.4% reported low socioeconomic status, 15.6% reported sufficient physical activity, 94.3% reported having at least one close friend, and 38.3% reported that their parent understood their problems. For tobacco use in the past 30 days, 90.0% reported no use, 7.8% used on 0–9 days, and 2.1% on 10 or more days. For alcohol consumption in the past 30 days, 90.0% reported no use, 9.2% drinked on 0–9 days, and 0.8% on 10 or more days (Supplementary Table S1).
The prevalence of loneliness among adolescents whose parents used any form of tobacco (father only: 41.0%; mother only: 45.6%; both: 49.4%) was higher than that among adolescents whose parents did not smoke (35.5%). The results were similar in the subgroup analyses by sex, age, and WHO region (Table 2). In the sensitivity analysis, we also observed similar results overall or in the subgroups according to the alternate definition of loneliness (Supplementary Table S2).

Table 2. Prevalence of adolescent loneliness across different categories of parental smoking stratified by sex, age, and WHO region.
After adjusting for age, sex, socioeconomic status, physical activity time, number of close friends, parental understanding, survey year, and country, parental smoking was positively associated with adolescent loneliness (neither as reference; father only: OR = 1.18, 95% CI = 1.10–1.26; mother only: OR = 1.39, 95% CI = 1.15–1.67; both: OR = 1.65, 95% CI = 1.41–1.93). In subgroup analyses by sex, age, and WHO region, the results were similar to the primary analysis (Table 3) except that the association was not significant in the African and Western Pacific regions. In the sensitivity analysis, similar results were observed overall and in the subgroups (by sex, age, and WHO region) according to the alternate definition of loneliness (Supplementary Table S3). Meanwhile, the association was not significant in adolescents with high frequency of tobacco use or alcohol consumption (Supplementary Tables S4, S5). The mediation analysis suggested that adolescent tobacco use and alcohol consumption partially mediated the association between parental smoking and adolescent loneliness, with the mediation proportion of 11.6% for adolescent tobacco use and 10.3% for adolescent alcohol consumption.
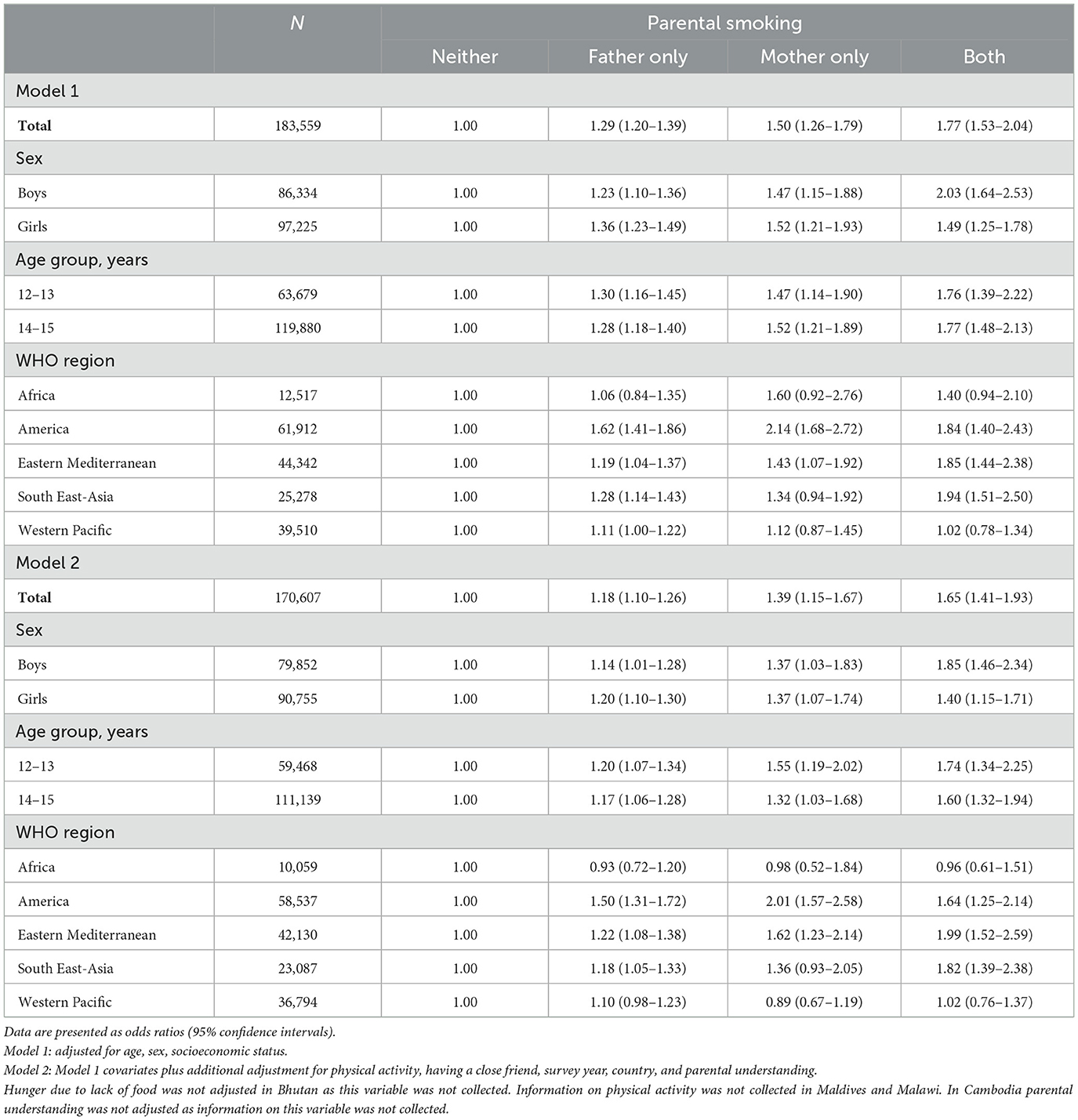
Table 3. Association between parental smoking and adolescent loneliness stratified by sex, age group, and WHO region.
Of these 187,552 adolescents included in this study, 37% had at least one parental smoker, and nearly 40% felt lonely sometimes or more frequently in the past 12 months. After adjusting for all covariates, parental smoking was positively associated with adolescent loneliness. The association was stronger in adolescents whose parents were both smokers compared to those who had a single parent who was a smoker. In addition, the association was statistically significant in three WHO regions including regions of America, Eastern Mediterranean, and South East-Asia, rather than in regions of Africa and Western Pacific.
Our study offers important implications for mental health prevention via reducing passive smoking in LMIC adolescents. Previous studies have mainly examined the association between passive smoking and adolescent physical health. For example, it was reported that secondhand smoke exposure is associated with adolescent obesity among adolescents in LMICs (29). In addition, secondhand smoke exposure is associated with respiratory symptoms in adolescents from Hong Kong (30). Besides, our study showed that parental smoking can have a negative impact on the mental health of adolescents. Furthermore, our findings broaden the understanding of the health impacts of passive smoke exposure and reinforce the need to limit secondhand smoke exposure among adolescents.
Relevant studies on the association between parental smoking and adolescent loneliness are rare. To our knowledge, only two studies have focused on the association between passive smoking and adolescent loneliness (23, 31). One study including 191,613 non-smoking adolescents showed that exposure to secondhand smoke was positively associated with the likelihood of adolescent loneliness, with the odds of loneliness increasing with the number of days in the past 7 days exposed to secondhand smoke (0 days as reference; 1–2 days: OR = 1.11, 95% CI = 1.02–1.21; 3-−4 days: OR = 1.41, 95% CI = 1.27–1.57; 5-6 days: OR = 1.67, 95% CI = 1.44–1.93; 7 days: OR = 1.77, 95% CI = 1.60–1.96) (23). Another study including 9,143 adolescents from Caribbean countries showed that passive smoking was associated with adolescent loneliness (boys: OR = 1.28, 95% CI = 1.11–1.48; girls: OR = 1.21, 95% CI = 1.06–1.37) (31). These studies partly support our findings.
Previous studies have shown that parental smoking increases the likelihood of adolescent smoking (32, 33). In this study, the association between parental smoking and adolescent loneliness was not significant in adolescents who have high frequency of tobacco use or alcohol consumption. Our finding suggested that the association of parental smoking with adolescent loneliness was partly mediated by adolescent smoking or alcohol consumption. Previous studies have shown that the use of tobacco products and secondhand smoke exposure were associated with mental health issues such as depression and anxiety in adults (34, 35). Thus, parental smoking may influence adolescent mental health by affecting parental mental health. According to a Finnish cohort study, individuals exposed to parental smoking throughout childhood or adolescence had lower cognitive skills in midlife (RR = 1.38, 95% CI: 1.01–1.75) (36). This finding indicates that parental smoking during an individual's adolescence or childhood can have lifelong psychological consequences.
The potential explanation of the association between tobacco smoking and a sense of loneliness is that nicotine exposure can create more negative sentiments and a commensurate rise in adolescent loneliness (37, 38). It has been found that family smoking and exposure to secondhand smoke at home were risk factors for childhood unhappiness (39). In addition, exposure to secondhand smoke was associated with depressive symptoms, and suicidal ideation in Korean adolescents (40). These findings are consistent with our study. An additional explanation is that parental smoking behavior directly affects adolescent mental health. Nicotine can regulate the transmission of various neurochemicals in various mesocorticolimbic structures, which can affect mental health among adolescents (41). Additionally, both tobacco use and the use of E-cigarettes have been found to have adverse effects on the mental health of adolescents (42, 43). Although secondhand smoke exposure is decreasing among adolescents worldwide, adolescents with low socioeconomic status are still at increased odds of secondhand smoke exposure in public places and at home (2). Adolescents with smoking parents may have a lower socioeconomic status, making them at higher odds of loneliness. Additionally, adolescents whose parents smoke may face increased familial pressure, which can further contribute to feelings of loneliness among them. Our study findings suggest that maternal smoking has a more substantial effect on adolescent loneliness than paternal smoking. The stronger association between mothers and adolescents may play a crucial role in this phenomenon, in addition to the possibility that maternal smoking, as a central feature of the family environment, might contribute to a more hostile home environment (44).
Our study found that the association between single parental smoking and adolescent loneliness was stronger among girls than boys. This could be partly explained by the higher prevalence of tobacco use among boys, potentially normalizing smoking behavior within boys' social network, thereby mitigating feelings of loneliness (45). However, in our study, the association between both parental smoking and a sense of loneliness is stronger in boys than in girls. A plausible explanation is that smoking by both parents may create a high-stress family environment, which can have a greater impact on adolescent boys. Boys, who are more prone to risk-taking and externalizing behaviors, may be more sensitive to family stress and disadvantage than girls (46). Additionally, a global study of secondhand smoke exposure among adolescents, adolescents in regions of South-East Asia, Eastern Mediterranean, and Americas had a higher prevalence of secondhand smoke exposure at home on more than 5 days in the past 7 days than regions of Africa and the Western Pacific (2). This might explain the stronger association between parental smoking and loneliness among adolescents in these WHO regions.
This study has two strengths. First, to our knowledge, this is the first study to examine the association between parental smoking and adolescent loneliness based on a large sample size. Second, the same questionnaire and methodology were used in all GSHS participating countries, allowing the pooled analysis of data from all included countries. However, there are also some notable limitations. First, only students in low- and middle-income countries were surveyed and included, and the results may not be generalizable to adolescents in high-income countries. Second, the GSHS was conducted among students who were in school, and data may not be representative of adolescents in that country who were not in school for various reasons during the survey. Third, because GSHS is a cross-sectional survey, a causal relationship between adolescent parental smoking and adolescent loneliness should be made with caution. Fourth, other substance use that might confound the association were not adjusted in our study. Fifth, both exposure and outcome variables were collected via a self-report questionnaire, which may be subject to recall bias and desirability bias, potentially leading to inaccuracy in reporting. Sixth, insufficient effort responding (IER) is another potential limitation. The reliance on self-report data can increase the risk of IER, and respondents may provide careless or inattentive answers, leading to both random and systematic measurement errors. Given the standard procedures and quality control measurements implemented in the GSHS survey, we believe that the extent of IER in our study is likely to be mild. However, future research should adopt strategies to detect IER and reduce its potential impact on the results. Seventh, the evaluation of parental smoking in this study seemed to overlook ex-smokers, dosage, and environmental factors, thereby reducing the precision and granularity of the study. Eighth, while our study is the first to examine the association between parental smoking and adolescent loneliness in such a large sample, it is important to acknowledge the limitation of using a single-item measure to define constructs like parental smoking, as it may not fully capture the complexity of the variable.
Our study indicates that parental smoking might be an independent risk factor for adolescent loneliness, which is independent of many potential variables. Our finding expands the well-known physical damage of parental smoking in adolescents to the psychological damage. Thus, strict policies and strategies should be established to encourage smoking cessation for parents who are current smokers.
The Global School-based Student Health Survey is a public dataset with de-identified information. The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: Data are available from the websites of the United States Centers for Disease Control and Prevention (https://archive.cdc.gov/#/details?url=https://www.cdc.gov/gshs/index.htm).
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the participants was not required to participate in this study in accordance with the national legislation and the institutional requirements.
JX: Conceptualization, Data curation, Formal analysis, Methodology, Validation, Writing – original draft. HY: Methodology, Visualization, Writing – review & editing. MZ: Methodology, Validation, Visualization, Writing – review & editing. CM: Methodology, Visualization, Writing – review & editing. BX: Conceptualization, Supervision, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1497136/full#supplementary-material
1. Oberg M, Jaakkola MS, Woodward A, Peruga A, Prüss-Ustün A. Worldwide burden of disease from exposure to second-hand smoke: a retrospective analysis of data from 192 countries. Lancet. (2011) 377:139–46. doi: 10.1016/S0140-6736(10)61388-8
2. Ma C, Heiland EG, Li Z, Zhao M, Liang Y, Xi B. Global trends in the prevalence of secondhand smoke exposure among adolescents aged 12–16 years from 1999 to 2018: an analysis of repeated cross-sectional surveys. Lancet Global Health. (2021) 9:e1667–78. doi: 10.1016/S2214-109X(21)00365-X
3. Flay BR, Hu FB, Siddiqui O, Day LE, Hedeker D, Petraitis J, et al. Differential influence of parental smoking and friends' smoking on adolescent initiation and escalation of smoking. J Health Soc Behav. (1994) 35:248–65. doi: 10.2307/2137279
4. Mays D, Gilman SE, Rende R, Luta G, Tercyak KP, Niaura RS. Parental smoking exposure and adolescent smoking trajectories. Pediatrics. (2014) 133:983–91. doi: 10.1542/peds.2013-3003
5. Wang MP, Ho SY, Lam TH. Parental smoking, exposure to secondhand smoke at home, and smoking initiation among young children. Nicotine Tobacco Res. (2011) 13:827–32. doi: 10.1093/ntr/ntr083
6. Simonetti GD, Schwertz R, Klett M, Hoffmann GF, Schaefer F, Wühl E. Determinants of blood pressure in preschool children: the role of parental smoking. Circulation. (2011) 123:292–8. doi: 10.1161/CIRCULATIONAHA.110.958769
7. Riedel C, Schönberger K, Yang S, Koshy G, Chen YC, Gopinath B, et al. Parental smoking and childhood obesity: higher effect estimates for maternal smoking in pregnancy compared with paternal smoking—a meta-analysis. Int J Epidemiol. (2014) 43:1593–606. doi: 10.1093/ije/dyu150
8. Li Y, Wang D, Wang Y, Zhao Y, Han L, Zhong L, et al. Impact of parental smoking on adipokine profiles and cardiometabolic risk factors in Chinese children. Atherosclerosis. (2020) 301:23–29. doi: 10.1016/j.atherosclerosis.2020.03.023
9. Thacher JD, Schultz ES, Hallberg J, Hellberg U, Kull I, Thunqvist P, et al. Tobacco smoke exposure in early life and adolescence in relation to lung function. Eur Respir J. (2018) 51:1702111. doi: 10.1183/13993003.02111-2017
10. Pugmire J, Vasquez MM, Zhou M, Sherrill DL, Halonen M, Martinez FD, et al. Exposure to parental smoking in childhood is associated with persistence of respiratory symptoms into young adult life. J Allergy Clin Immunol. (2014) 134:962–5.e4. doi: 10.1016/j.jaci.2014.07.030
11. Mikaeloff Y, Caridade G, Tardieu M, Suissa S, Cook DG, Strachan DP. Parental smoking at home and the risk of childhood-onset multiple sclerosis in children. Brain. (2007) 130:2589–95. doi: 10.1093/brain/awm198
12. Kovess V, Keyes KM, Hamilton A, Pez O, Bitfoi A, Koç C, et al. Maternal smoking and offspring inattention and hyperactivity: results from a cross-national European survey. Eur Child Adolesc Psychiatry. (2015) 24:919–29. doi: 10.1007/s00787-014-0641-9
13. Steeger CM, Bailey JA, Epstein M, Hill KG. The link between parental smoking and youth externalizing behaviors: effects of smoking, psychosocial factors, and family characteristics. Psychol Addict Behav. (2019) 33:243–53. doi: 10.1037/adb0000444
14. Sauter SR, Kim LP, Jacobsen KH. Loneliness and friendlessness among adolescents in 25 countries in Latin America and the Caribbean. Child and adolescent mental health. (2020) 25:21–7. doi: 10.1111/camh.12358
15. Twenge JM, Haidt J, Blake AB, McAllister C, Lemon H, Le Roy A. Worldwide increases in adolescent loneliness. J Adolesc. (2021) 93:257–69. doi: 10.1016/j.adolescence.2021.06.006
16. Xerxa Y, Rescorla LA, Shanahan L, Tiemeier H, Copeland WE. Childhood loneliness as a specific risk factor for adult psychiatric disorders. Psychol Med. (2021) 14:1–9. doi: 10.1017/S0033291721001422
17. Adam EK, Chyu L, Hoyt LT, Doane LD, Boisjoly J, Duncan GJ, et al. Adverse adolescent relationship histories and young adult health: cumulative effects of loneliness, low parental support, relationship instability, intimate partner violence, and loss. J Adolesc Health. (2011) 49:278–86. doi: 10.1016/j.jadohealth.2010.12.012
18. Matthews T, Qualter P, Bryan BT, Caspi A, Danese A, Moffitt TE, et al. The developmental course of loneliness in adolescence: implications for mental health, educational attainment, and psychosocial functioning. Dev Psychopathol. (2022) 35:537–46. doi: 10.1017/S0954579421001632
19. Jones AC, Schinka KC, van Dulmen MH, Bossarte RM, Swahn MH. Changes in loneliness during middle childhood predict risk for adolescent suicidality indirectly through mental health problems. J Clin Child Adolesc Psychol. (2011) 40:818–24. doi: 10.1080/15374416.2011.614585
20. Liu J, Liu Q, Li Z, Du J, Wang C, Gao Y, et al. Prevalence of metabolic syndrome and risk factors among chinese adults: results from a population-based study—Beijing, China, 2017–2018. China CDC Wkly. (2022) 4:640–5. doi: 10.46234/ccdcw2022.138
21. Rückinger S, Rzehak P, Chen CM, Sausenthaler S, Koletzko S, Bauer CP, et al. Prenatal and postnatal tobacco exposure and behavioral problems in 10-year-old children: results from the GINI-plus prospective birth cohort study. Environ Health Perspect. (2010) 118:150–4. doi: 10.1289/ehp.0901209
22. McCarthy DM, Zhang L, Wilkes BJ, Vaillancourt DE, Biederman J, Bhide PG. Nicotine and the developing brain: insights from preclinical models. Pharmacol Biochem Behav. (2022) 214:173355. doi: 10.1016/j.pbb.2022.173355
23. Guan Q, Huan F, Wang Y, Wang L, Shen L, Xiong J, et al. The relationship between secondhand smoking exposure and mental health among never-smoking adolescents in school: data from the Global School-based Student Health Survey. J Affect Disord. (2022) 311:486–93. doi: 10.1016/j.jad.2022.05.121
24. Tian S, Zhang TY, Miao YM, Pan CW. Psychological distress and parental involvement among adolescents in 67 low-income and middle-income countries: a population-based study. J Affect Disord. (2021) 282:1101–9. doi: 10.1016/j.jad.2021.01.010
25. Kushal SA, Amin YM, Reza S, Shawon MSR. Parent-adolescent relationships and their associations with adolescent suicidal behaviours: secondary analysis of data from 52 countries using the Global School-based Health Survey. EClinicalMedicine. (2021) 31:100691. doi: 10.1016/j.eclinm.2020.100691
26. Wu H, Gu Z, Zeng L, Guo T. Do global adolescents with food insecurity feel lonely? Front Public Health. (2022) 10:820444. doi: 10.3389/fpubh.2022.820444
27. Xu G, Sun N, Li L, Qi W, Li C, Zhou M, Chen Z, Han L. Physical behaviors of 12–15 year-old adolescents in 54 low- and middle-income countries: results from the Global School-based Student Health Survey. J Global Health. (2020) 10:010423. doi: 10.7189/jogh.10.010423
28. Liu H, Ma X, Shi L, Wang J, Juan JTH, Ma D, et al. Associations between tobacco and alcohol use and aggressive behavior among adolescents in 55 Low- and Middle-Income countries. J Affect Disord. (2023) 329:519–24. doi: 10.1016/j.jad.2023.02.131
29. Koyanagi A, Smith L, Oh H, Yang L, Jackson SE, Haro JM, et al. Secondhand smoking and obesity among nonsmoking adolescents aged 12–15 years from 38 low- and middle-income countries. Nicotine Tobacco Res. (2020) 22:2014–21. doi: 10.1093/ntr/ntaa053
30. Leung LT, Ho SY, Wang MP, Lam TH. Secondhand smoke from multiple sources, thirdhand smoke and respiratory symptoms in Hong Kong adolescents. Nicotine Tobacco Res. (2018) 20:192–198. doi: 10.1093/ntr/ntw302
31. Pengpid S, Peltzer K. Loneliness is associated with poor mental health, social-environmental factors, and health risk behaviours among national samples of in-school adolescents in four Caribbean countries. Psychol Health Med. (2022) 27:559–70. doi: 10.1080/13548506.2021.1883071
32. Harakeh Z, Scholte RH, Vermulst AA, de Vries H, Engels RC. Parental factors and adolescents' smoking behavior: an extension of The theory of planned behavior. Prevent Med. (2004) 39:951–61. doi: 10.1016/j.ypmed.2004.03.036
33. Alves J, Perelman J, Soto-Rojas V, Richter M, Rimpelä A, Loureiro I, et al. The role of parental smoking on adolescent smoking and its social patterning: a cross-sectional survey in six European cities. J Public Health. (2017) 39:339–46. doi: 10.1093/pubmed/fdw040
34. Patten SB, Williams JVA, Lavorato DH, Woolf B, Wang JL, Bulloch AGM, et al. Major depression and secondhand smoke exposure. J Affect Disord. (2018) 225:260–4. doi: 10.1016/j.jad.2017.08.006
35. Fluharty M, Taylor AE, Grabski M, Munafò MR. The association of cigarette smoking with depression and anxiety: a systematic review. Nicotine Tobacco Res. (2017) 19:3–13. doi: 10.1093/ntr/ntw140
36. Rovio SP, Pihlman J, Pahkala K, Juonala M, Magnussen CG, Pitkänen N, et al. Childhood exposure to parental smoking and midlife cognitive function. Am J Epidemiol. (2020) 189:1280–91. doi: 10.1093/aje/kwaa052
37. Wootton RE, Greenstone HSR, Abdellaoui A, Denys D, Verweij KJH, Munafò MR, et al. Bidirectional effects between loneliness, smoking and alcohol use: evidence from a Mendelian randomization study. Addiction. (2021) 116:400–6. doi: 10.1111/add.15142
38. Dyal SR, Valente TW. A systematic review of loneliness and smoking: small effects, big implications. Substance Use Misuse. (2015) 50:1697–716. doi: 10.3109/10826084.2015.1027933
39. Chen JJ, Ho SY, Au WM, Wang MP, Lam TH. Family smoking, exposure to secondhand smoke at home and family unhappiness in children. Int J Environ Res Public Health. (2015) 12:14557–70. doi: 10.3390/ijerph121114557
40. Kim B, Kim HR. Associations between secondhand smoke and mental health in korean adolescents. Asia-Pacific J Public Health. (2020) 32:406–13. doi: 10.1177/1010539520957846
41. Laviolette SR. Molecular and neuronal mechanisms underlying the effects of adolescent nicotine exposure on anxiety and mood disorders. Neuropharmacology. (2021) 184:108411. doi: 10.1016/j.neuropharm.2020.108411
42. Livingston JA, Chen CH, Kwon M, Park E. Physical and mental health outcomes associated with adolescent E-cigarette use. J Pediatr Nurs. (2022) 64:1–17. doi: 10.1016/j.pedn.2022.01.006
43. Hong SW, Teesdale-Spittle P, Page R, Ellenbroek B, Truman P. Biologically active compounds present in tobacco smoke: potential interactions between smoking and mental health. Front Neurosci. (2022) 16:885489. doi: 10.3389/fnins.2022.885489
44. Keizer R, Helmerhorst KOW, van Rijn-van Gelderen L. Perceived quality of the mother-adolescent and father-adolescent attachment relationship and adolescents' self-esteem. J Youth Adolesc. (2019) 48:1203–17. doi: 10.1007/s10964-019-01007-0
45. Ma C, Xi B, Li Z, Wu H, Zhao M, Liang Y, et al. Prevalence and trends in tobacco use among adolescents aged 13–15 years in 143 countries, 1999-2018: findings from the Global Youth Tobacco Surveys. Lancet Child Adolesc Health. (2021) 5:245–55. doi: 10.1016/S2352-4642(20)30390-4
Keywords: loneliness, adolescent, tobacco use, mental health, parental smoking
Citation: Xie J, Yang H, Zhao M, Magnussen CG and Xi B (2025) Parental smoking is associated with adolescent loneliness: evidence from 71 low- and middle-income countries. Front. Public Health 13:1497136. doi: 10.3389/fpubh.2025.1497136
Received: 16 September 2024; Accepted: 10 February 2025;
Published: 26 February 2025.
Edited by:
Cesar Merino-Soto, Monterrey Institute of Technology and Higher Education (ITESM), MexicoReviewed by:
Rossella Alfano, University of Hasselt, BelgiumCopyright © 2025 Xie, Yang, Zhao, Magnussen and Xi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bo Xi, eGlibzIwMTBAc2R1LmVkdS5jbg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.