- 1School of Health Policy and Management, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China
- 2National Cancer Center, Chinese Academy of Medical Sciences, Beijing, China
Objectives: This study aimed to develop a patient-reported questionnaire to assess service utilization and patient satisfaction among older adults with hypertension and diabetes in primary health-care centers operating under China’s National Essential Public Health Service Program (NEPHSP).
Methods: The questionnaire’s item pool was constructed on the basis of a logic model. A cross-sectional survey was conducted in three provinces of mainland China between November and December 2019. The questionnaire was evaluated using Cronbach’s alpha coefficients and confirmatory factor analysis (CFA) to refine items and assess internal consistency, construct validity, convergent validity, and discriminant validity.
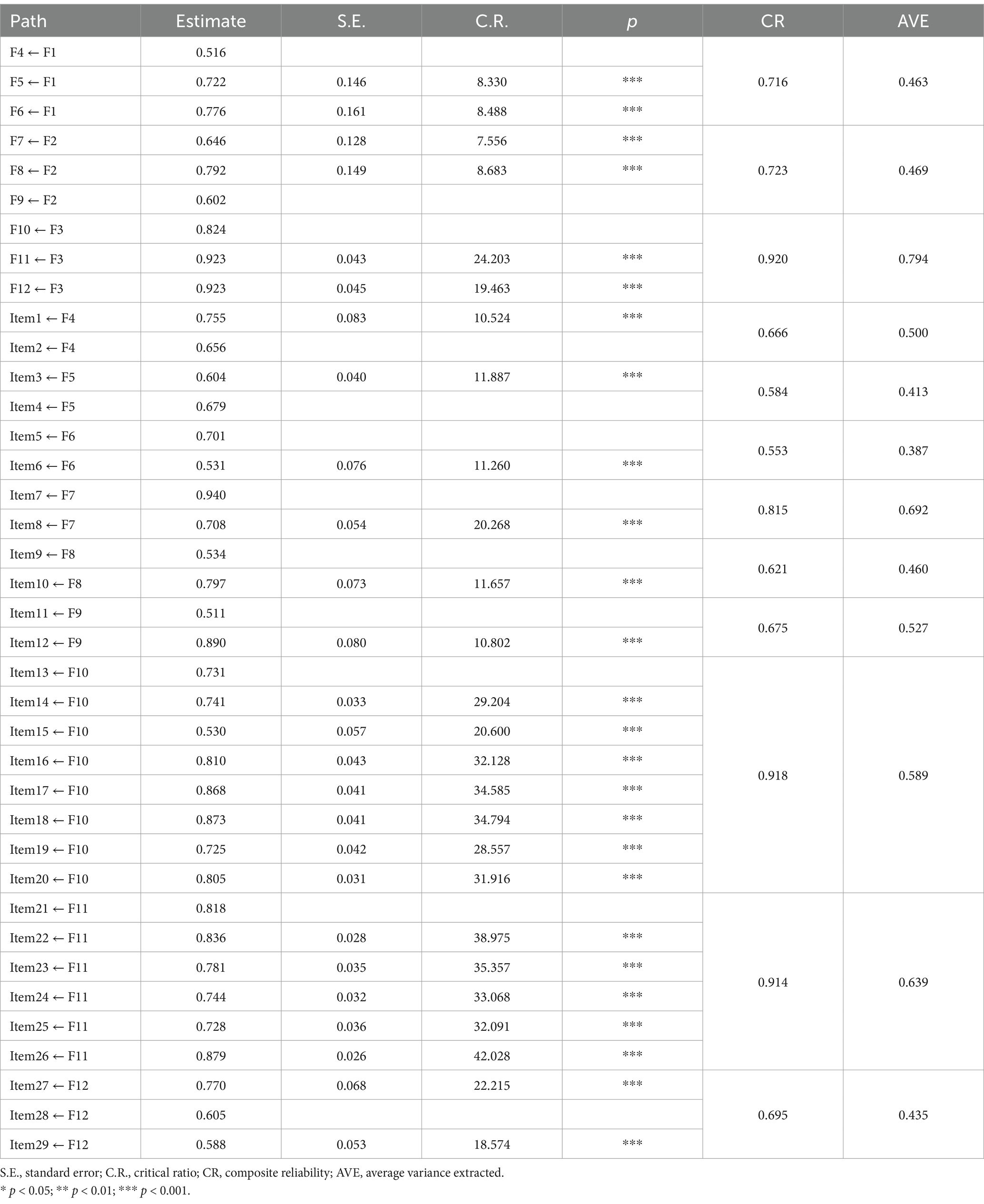
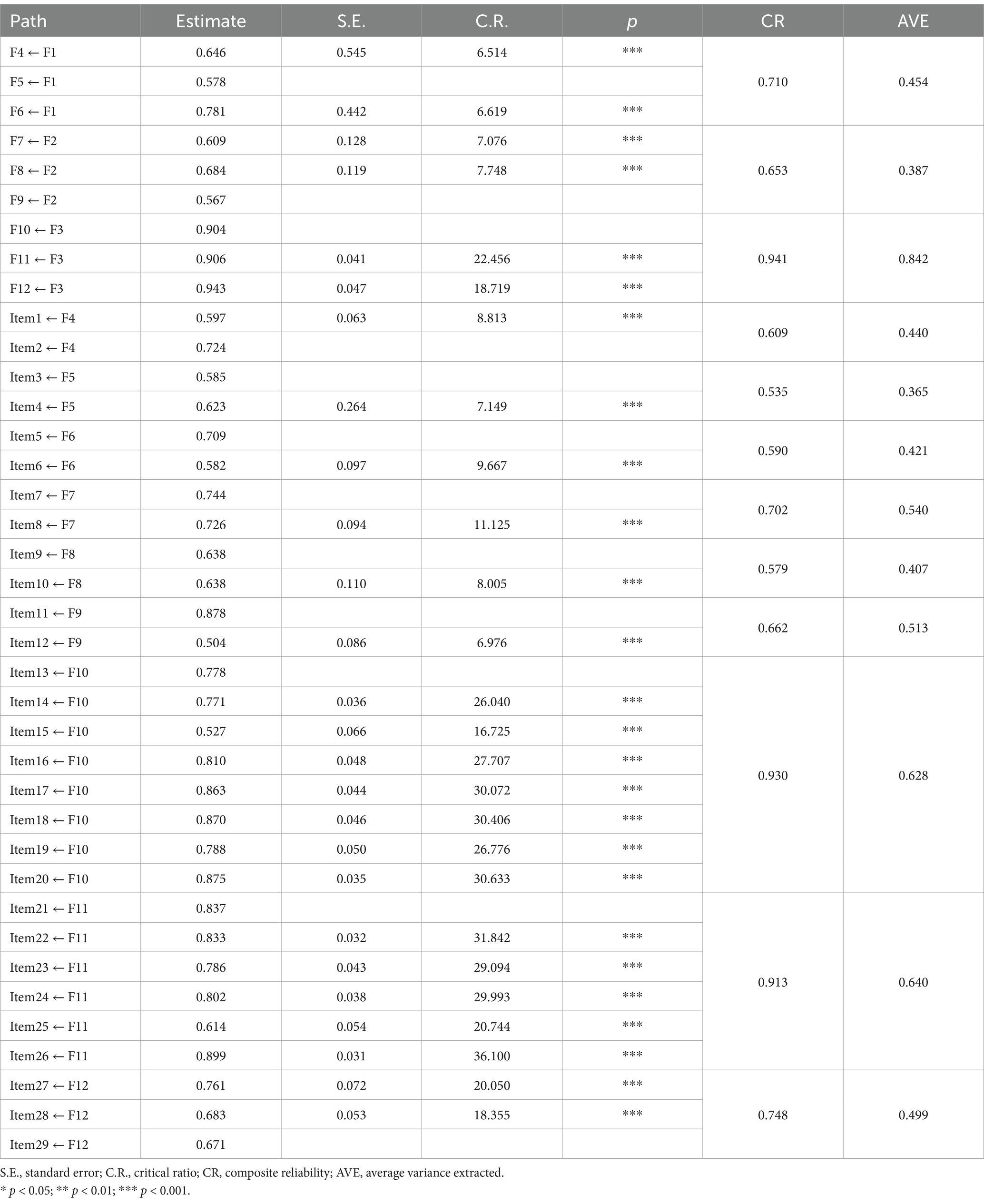
Results: The final questionnaire adopted a second-order factor model comprising three domains: essential services for all older adults, follow-up services for older adults with hypertension or diabetes, and patient satisfaction assessment. Through a two-step refinement process, nine factors encompassing 29 items were selected, including elements such as “health records and health education,” “blood pressure/glucose monitoring,” and “health education in follow-up.” Cronbach’s alpha coefficients indicated excellent reliability, with values of 0.899 and 0.906. The 29-item instrument had robust model fit for both hypertension and diabetes cohorts. The fit indices for the hypertension model included a Bollen–Stine bootstrap chi-square to degrees of freedom ratio (χ2/df) of 1.78, root mean square error of approximation (RMSEA) of 0.03, and goodness-of-fit index (GFI) of 0.97. Similarly, for the diabetes model, the fit indices were a Bollen–Stine bootstrap χ2/df ratio of 1.38, RMSEA of 0.02, and GFI of 0.97. CFA revealed factor loadings ranging from 0.516 to 0.940 for the hypertension model and from 0.504 to 0.943 for the diabetes model. All three first-order factors were significantly correlated with each other (p < 0.01), and their correlation coefficients were lower than the square root of the average variance extracted. The models demonstrated strong structural validity, convergent validity, and discriminant validity.
Conclusion: A valid and reliable questionnaire for evaluating service utilization and patient satisfaction among older adults with hypertension and diabetes in primary health-care center was developed in China. This instrument will serve as a practical tool for patient-reported assessments within the NEPHSP framework at primary health-care centers.
Introduction
The rapid aging of the population and shifts in lifestyle patterns have led to a substantial increase in the prevalence of chronic noncommunicable diseases among older adults. Among these, hypertension and diabetes are particularly prominent, ranking as leading causes of all-cause mortality and disability worldwide (1–6). In China, the estimated number of adults with hypertension reached 245 million in 2020, with more than 50% of individuals aged ≥65 years affected by the condition (7). Additionally, China has the largest population of patients with diabetes globally (8). As of 2017, the country was home to approximately 260.4 million older adults, approximately 30% of whom were reported to have diabetes (9). These chronic diseases often lead to severe comorbidities, characterized by high rates of disability and mortality, imposing substantial burdens on families and society (10, 11). Consequently, the effective control and management of hypertension and diabetes among older adults have become critical public health challenges in China (12, 13).
In 2009, China initiated ambitious health reforms, one of which was the implementation of the National Essential Public Health Service Program (NEPHSP). This initiative aligns with the Basic Health Service Package and essential service packages promoted by the World Health Organization (3), which have been adopted in many countries worldwide (14, 15). The NEPHSP offers free services through service packages accessible to all citizens via a network of over 800,000 primary health-care centers (PHCCs), thereby providing primary health care to China’s population of 1.4 billion. The program prioritizes key populations, including maternal and child health groups; older adults; and patients with hypertension, diabetes, and severe mental disorders (16, 17). Funded by the Chinese government, the NEPHSP aims to address essential public health needs. As of 2019, the NEPHSP delivers 12 types of service packages to residents through PHCCs, which are categorized into population-based public health services for all residents and individual health management services targeted at key populations (18).
Population-based public health services under the NEPHSP comprise five service packages: (1) resident health records management, (2) health education, (3) vaccination, (4) reporting of infectious diseases and public health emergencies, and (5) family planning education and sanitary inspections for all residents. Additionally, individual health management services include seven service packages: (1) maternal health management, (2) children’s health management, (3) health management for older adults, (4) health management for patients with chronic disease (hypertension and type 2 diabetes), (5) health management for patients with severe mental disorders, (6) health management for patients with tuberculosis, and (7) health management using traditional Chinese medicine (TCM). These services, delivered through PHCCs, ensure that all residents have access to essential public health services that are affordable, equitable, and of high quality. This approach aligns with the goal of achieving universal health coverage, regardless of geographic location or socioeconomic status (19).
Patients with a confirmed diagnosis of hypertension aged ≥35 years who consented to health management by general practitioners in community health centers (CHCs) are enrolled in an electronic health record system. These patients subsequently receive comprehensive interventions provided by multidisciplinary teams comprising general practitioners, nurses, and public health doctors based at their local CHC (20). The services offered include screening, lifestyle and health status assessments, physical examinations, ancillary examinations, health checkups, and personalized health guidance, among others (18). Between 2009 and 2019, the NEPHSP achieved remarkable progress, with the health management rate for older adults with increasing by 26.23%, reaching 67.41% (21). During the mass disruptions to health systems caused by the SARS-CoV-2 pandemic, the NEPHSP played a pivotal role in maintaining continuity of care for these patients. Community-based measures implemented by PHCCs included long-prescription policies, follow-up visits by general practitioners via phone or video conferencing, and home delivery of medications facilitated by community health workers (22, 23).
To date, evaluations of the effectiveness of the NEPHS have primarily relied on monitoring data reported by government sources (24, 25). In this study, we developed a patient-reported questionnaire specifically designed to assess the utilization of health management services for patients with hypertension and diabetes within the NEPHSP. Notably, our focus extended beyond service utilization to also include patient satisfaction. This study developed a reliable and valid patient-reported questionnaire to accurately measure the utilization of and satisfaction with health management services for older patients in the community. This questionnaire will serve as a robust and valid instrument for health management service surveys in the primary health-care sector.
Methods
Item pool formation
The primary objective in developing the assessment instrument was to comprehensively generate items and domains that accurately capture the quality of services received by patients and their satisfaction levels. To achieve this, a systematic review of relevant literature databases and policy documents was conducted. The review focused on the Code of the NEPHSP (Third Edition) (18), the National Guidelines for the Prevention and Control of Diabetes in Primary Care (26), and the National Guidelines for the Prevention and Control of Hypertension in Primary Care (27). Based on this review, an expert panel was convened to provide insights. Through multiple rounds of expert consultations, a set of survey instrument domains and an item pool of 40 items were generated (Supplementary Table 1).
Logical analysis
A logic model was employed to analyze the management service processes for older adults with hypertension or diabetes. Widely employed in the public health sector and increasingly adopted by various organizations outside the public health sector (28, 29), logic models are instrumental in meticulously tracking program activities from inception to completion. Logic models involve “modeling or simulating” real-life scenarios in a manner that highlights the underlying logic governing them. These models elucidate the causal relationships between different components of a program, offering a systematic approach to understanding the pathway toward achieving desired outcomes. These models comprise causal chains, which elucidate why certain phenomena occur, or fail to occur, through a series of manageable activities.
Based on the Code of the NEPHSP (Third Edition, 2017) (18), we comprehensively summarized and analyzed the core components of service packages designed for older patients. These components includes inputs, such as service components; activities, which cover the implementation process and program outputs; and the program objectives (Figure 1). The services offered under the NEPHSP can be broadly categorized into two primary domains:
1. Essential services for all older adults: This domain encompasses the establishment of health records, health education, annual free physical examinations (including physical measurements, functional assessments, and auxiliary examinations), and TCM management. Physical examination includes measurements of temperature, pulse, respiration, blood pressure, height, weight, waist circumference, skin condition, the superficial lymph nodes, the lungs, the heart, the abdomen, gross oral cavity examinations, vision, hearing, and motor function. Auxiliary examinations include routine blood and urine tests, liver function tests (serum glutamic oxaloacetic transaminase, serum glutamic alanine transaminase, and total bilirubin), renal function tests (serum creatinine and blood urea), fasting glucose, lipid profile (total cholesterol, triglycerides, low-density lipoprotein cholesterol, and high-density lipoprotein cholesterol), electrocardiograms, and abdominal ultrasounds (hepatobiliary, pancreatic, and splenic assessments).
2. Follow-up services for older patients with diabetes or hypertension: These services encompass health monitoring, examinations, evaluations, and interventions provided through outpatient visits, home visits, or telephone consultations. Follow-ups are conducted four times a year.
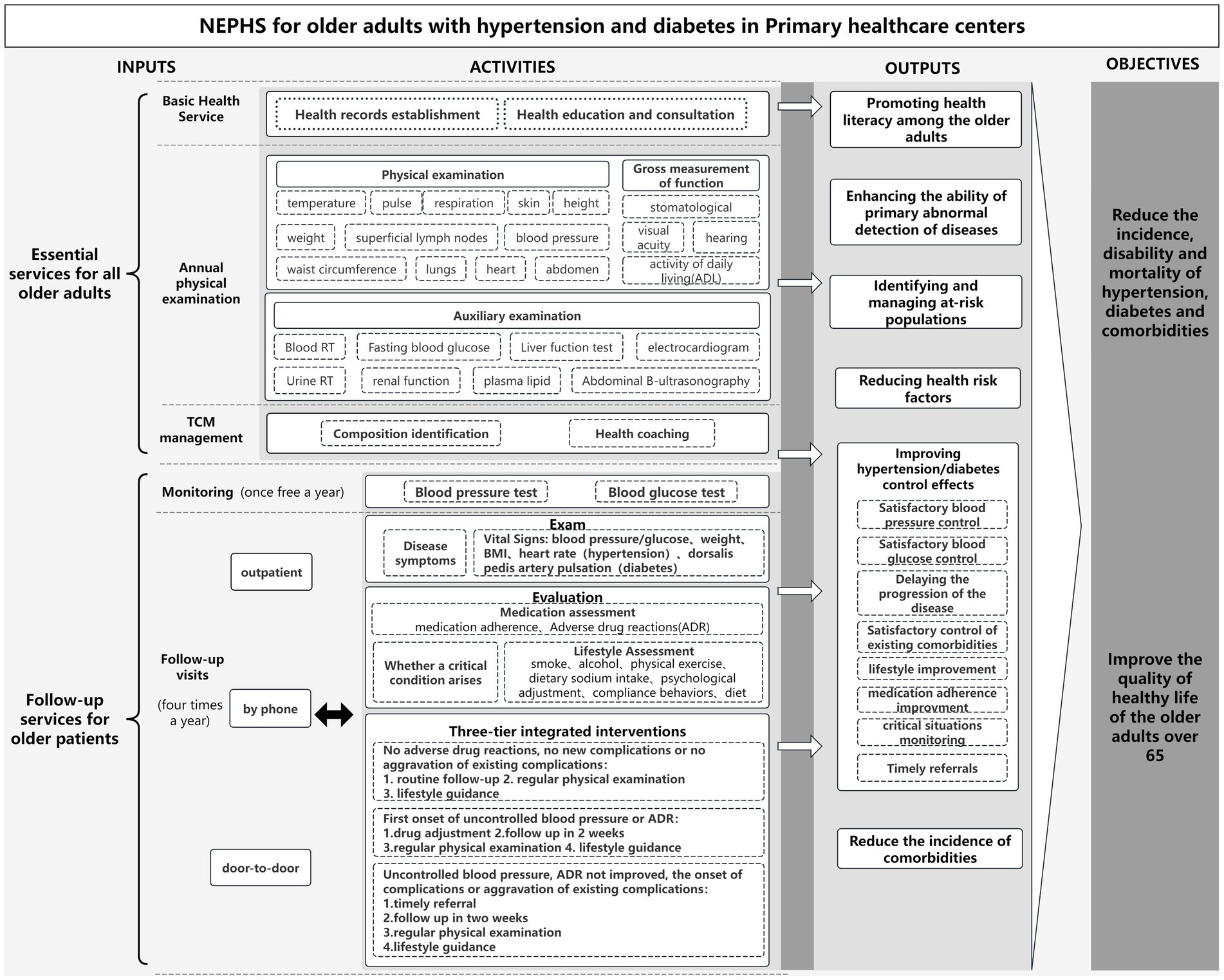
Figure 1. Logical model of management services for older adults with hypertension or diabetes under the NEPHSP.
These services actively promote health literacy and reduce health risk factors among older adults. This is achieved through the widespread implementation of electronic health records, resident health education lectures and consultations, identification of health components, and provision of TCM health coaching. Additionally, the program enhances disease detection capabilities at the grassroots level, enabling the early identification and management of high-risk populations through annual medical checkups, which include physical examinations, functional assessments, and auxiliary examinations. Furthermore, follow-up services contribute to more efficient management of hypertension or diabetes mellitus among older adults. During these follow-up services, health-care professionals at community or township health centers monitor patients’ vital signs and assess their disease symptoms, medication adherence, and lifestyles. Through a three-tiered integrated disease management approach, these health-care workers help improve blood pressure or glucose control, promote medication adherence and healthy lifestyle behaviors, delay disease progression, and ensure timely referrals for patients with severe or critical conditions. This integrated strategy helps reduce the incidence of complications associated with chronic diseases. The objectives of the service package are to reduce mortality rats associated with chronic diseases in China, improve the health status of older adults, and enhance their overall quality of life. The logic model developed in this study serves as the theoretical foundation for the assessment system.
Study setting
From November to December 2019, we conducted a demand-side survey by using self-designed questionnaires. A multi-stage stratified random sampling method was employed: (1) Province selection: Three provinces were selected, one from each region of China: Eastern (Zhejiang Province), Central (Shanxi Province), and Western (Chongqing Municipality). (2) City selection: Based on the economic development level, four prefecture-level cities and one municipality were selected. In Zhejiang Province and Shanxi Province, one city with a higher level of economic development and one with a lower level of economic development were selected. Chongqing City was directly included as a municipality. (3) CHC selection: In each city, one district or one county were randomly selected. Multiple CHCs and township health centers were then selected on the basis of a combination of local recommendations and random sampling. (4) Survey procedure: Local health commissions assisted in recruiting investigators for the on-site survey. At each survey site, patients with hypertension and diabetes who had recently received medical services were surveyed using paper-based questionnaires. Prior to the on-site survey, investigators received training to ensure the quality of the survey process (understanding and completeness of the survey content). Questionnaire quality control was implemented twice at both the township and county levels. If quality control failed, additional questionnaires were administered until the required sample size was reached. All questionnaires were uniquely coded and inserted into the database by the questionnaire company. All participants provided written informed consent prior to their inclusion in the study.
The following patients were included in the survey: (1) older adults aged >65 years with hypertension or diabetes, attending CHCs on the day of the survey and (2) patients who consented to participate in this survey. Older adults aged >65 years who had not received a diagnosis of hypertension and diabetes and those patients with severe mental illness were excluded from the survey.
Reliability and validity test
The reliability and validity of the questionnaire were evaluated using Cronbach’s alpha coefficient and confirmatory factor analysis (CFA). Specifically, internal consistency was assessed by calculating Cronbach’s alpha coefficients with 95% confidence intervals for each model (30, 31). Cronbach’s alpha coefficient estimates should be at least ≥0.6 and ideally ≥0.8 (32).
CFA and structural equation modeling were employed to evaluate the construct, convergent, and discriminant validity of the questionnaire, both of which are widely recognized methods for evaluating the structural validity of a model. In this study, the maximum likelihood method was employed for parameter estimation in the assessment models for hypertension and diabetes. Construct validity was evaluated using multiple goodness-of-fit indices, which include three absolute fit indices and four comparative fit indices from the CFA. The following thresholds were considered acceptable for good construct validity: the chi-square to degrees of freedom (X2/df) ratio should be <3, the root mean square error of approximation (RMSEA) should be <0.05 (33, 34), the goodness-of-fit index (GFI) should be >0.9, the confirmatory fit index should be >0.9 (35), the normed fit index (NFI) should be >0.9, the non-normed fit index (NNFI) should be >0.9, and the incremental fit index should be >0.9 (36–38).
To assess the convergent validity of each factor, we evaluated the composite reliability (CR), average variance extracted (AVE), and factor loadings of each item. A widely accepted rule of thumb is that standard loading estimates should be ≥0.5. For CR, a value of >0.6 is considered acceptable, and a value of >0.7 is considered good (39). For AVE, a value between 0.36 and 0.5 is considered acceptable, and a value of >0.5 is considered good (40). Good discriminant validity was defined as the condition where the AVE for each construct exceeds the squared value of the correlation coefficient between pairs of variables (24).
Statistical analysis
Statistical analyses were conducted using SPSS 26.0 and AMOS 26.0. Cronbach’s alpha coefficients, CR, and AVE values were calculated using SPSS, and CFA was conducted using AMOS. Descriptive data are presented as means ± standard deviations (x ± SD) and percentages (%).
Results
Participants
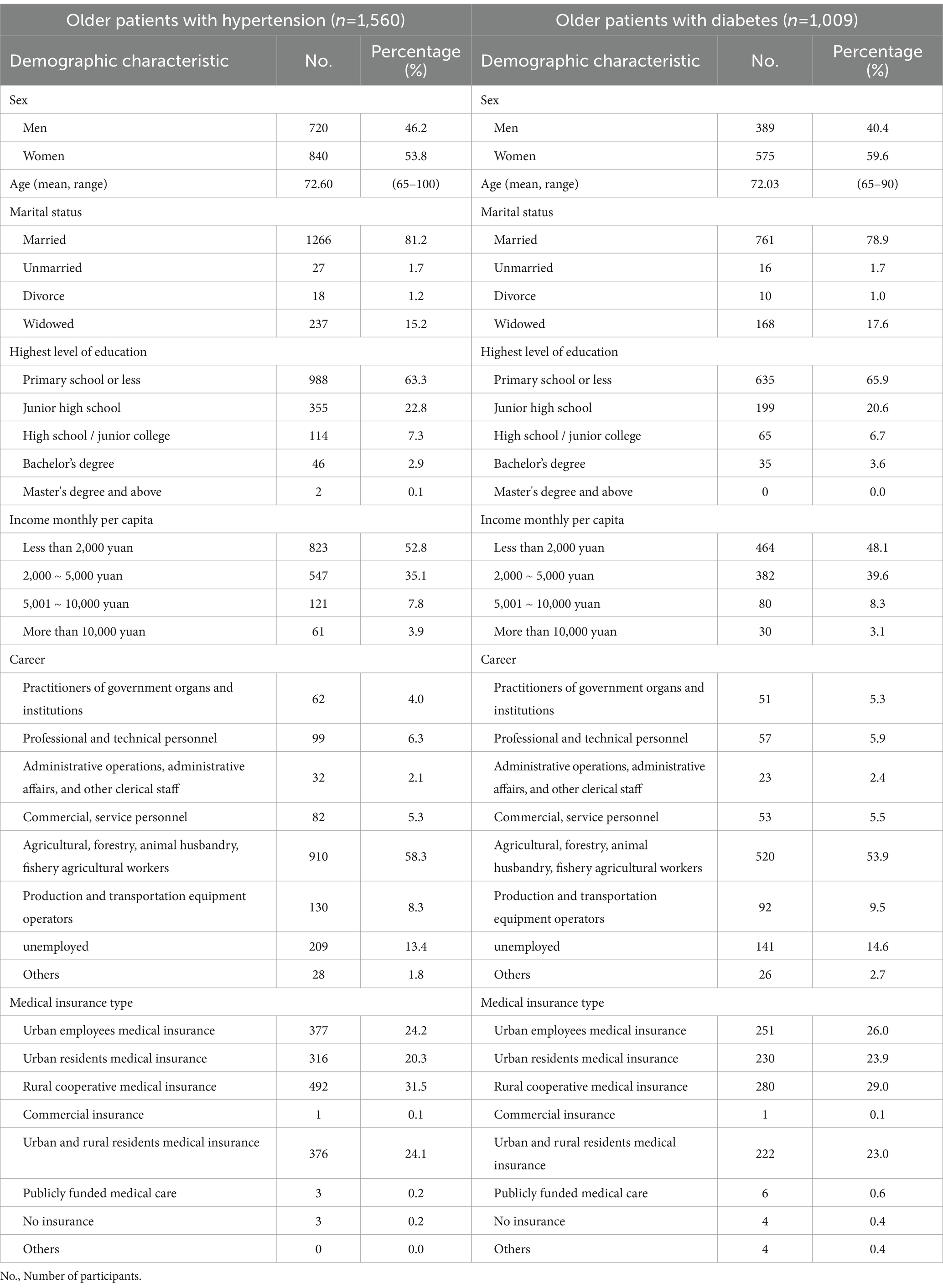
A total of 1,560 older patients with hypertension (46.2% men; mean age, 72.60 years) and 964 older patients with diabetes (40.4% men; mean age, 72.03 years) completed the survey. Table 1 presents the descriptive characteristics of the two patient samples.
The majority of patients with hypertension and diabetes (81.2 and 78.9%, respectively) were married. More than half of the participants (63.3% of the patients with hypertensive and 65.9% of the patients with diabetes) had received primary education or less. Nearly half of the participants (52.8% of the patients with hypertension and 48.1% of the patients with diabetes) reported a monthly per capita income of <2000 RMB. The participants were ever involved in various occupations, including husbandry, fishery, and agriculture (58.3% of the patients with hypertension and 53.9% of the patients with diabetes) and production and transportation equipment work (8.3% of the patients with hypertension and 9.5% of the patients with diabetes), whereas 13.4% of the patients with hypertension and 14.6% of the patients with diabetes were unemployed. The four major types of medical insurance among the participants were basic medical insurance for urban employees (24.2% of the patients with hypertension and 26.0% of the participants with diabetes), basic medical insurance for urban residents (20.3% of the patients with hypertension and 23.9% of the patients with diabetes), new rural cooperative medical insurance (31.5% of the patients with hypertension and 29.0% of the patients with diabetes), and basic medical insurance for urban and rural residents (24.1% of the patients with hypertension and 23.0% of the patients with diabetes). Together, these four insurance schemes accounted for over 90% of the participants’ medical coverage (Table 1).
Item selection and modification
To assess the interrelationships among the 40 selected items and determine whether further item reduction was necessary, two steps were taken to refine the items.
Step 1: Exclusion of items unsuitable for factor analysis. Three items were excluded from the analysis due to their inappropriate response categories for CFA, despite their relevance to the survey content. These items were as follows: “ways to view health records” (item 3, factor 1), “suggestions for free health checkups” (item 7, factor 2), and “reasons for not testing blood pressure/glucose in CHCs/THCs” (item 12, factor 4).
Step 2: To verify the factor structure of the questionnaire and evaluate the relationship between observed variables and their underlying latent constructs, CFA was performed on the remaining 37 items. The results indicated that some items required modification to more accurately and conveniently assess chronic disease management services for older patients. Items with Cronbach’s alpha coefficients of <0.5 and factor loadings of <0.5 were considered for deletion. Following expert group discussions on the content validity of these items, among the 37 items, the items “patient’s BMI” (item 13), “patient’s waist circumference” (item 14), “patient’s smoking status” (item 15), “patient’s alcohol consumption” (item 16), and “complications in patients” (item 17) were removed from the factor “examinations and assessment in follow-up” because their factor loadings were substantially lower than those of the others and were similar to baseline values rather than values obtained at follow-up assessments. The items “disease detection at CHCs/THCs” (item 6), “satisfaction with health record updates in follow-up visits” (item 35), and “satisfaction with the TCM treatment in follow-up visits” (item 39) were deleted due to their low validity scores, suggesting that they were more suitable for a more comprehensive study of factors influencing blood pressure and glucose follow-up. Finally, the response options for items 8, 9, 18, and 21 were modified to ensure that all the participants could provide suitable responses (Supplementary Table 1).
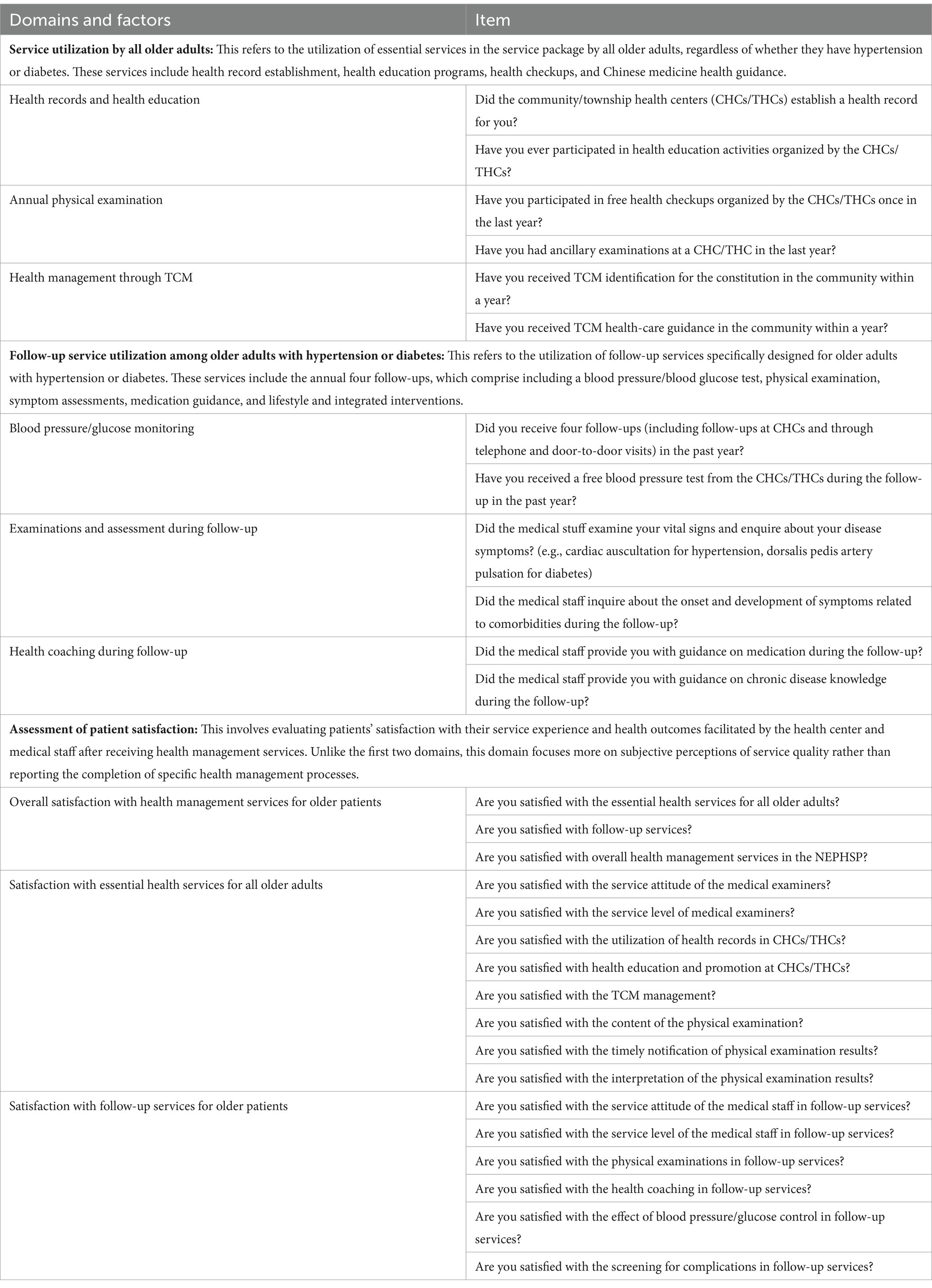
Through a two-step screening process, we developed a second-order factor assessment model. The final model comprises 29 items, which are categorized into three core areas of the NEPHSP: “essential health management services for all older adults,” “health management services for older adults with hypertension or diabetes,” and “self-assessment of patient experience satisfaction.” These categories encompass a total of nine factors: “health records and health education,” “annual examination,” “health management with TCM,” “blood pressure/glucose monitoring,” “examinations and assessment in follow-up,” “health coaching in follow-up,” “overall satisfaction with health management services for older patients,” “satisfaction with essential health services for all older adults,” and “satisfaction with follow-up services for older patients.” Table 2 presents the 29-item instrument used in the assessment model (Table 3).
Internal consistency
The hypertension and diabetes models had satisfactory internal consistency. The Cronbach’s α coefficients for the three domains of the hypertension model were 0.613, 0.638, and 0.946, all exceeding the acceptable threshold of 0.6. The diabetes model had comparable results (Supplementary Table 2).
Construct validity
A fundamental assumption of structural equation modeling and maximum likelihood estimation is the presence of a multivariate normal distribution. If this assumption is violated, the X2 value derived from maximum likelihood estimation may be overestimated, and some fit indices may be modestly underestimated (37). Thus, the critical ratio of multivariate kurtosis was tested, with values of >5.00 indicative of nonnormal data distribution (41). In this study, the critical ratios for the hypertension and diabetes models were 480.101 and 177.004, respectively, indicating nonnormality in the data. To address this, the Bollen–Stine bootstrap method was applied to correct the X2 value and goodness-of-fit indices of multivariate nonnormal data (42).
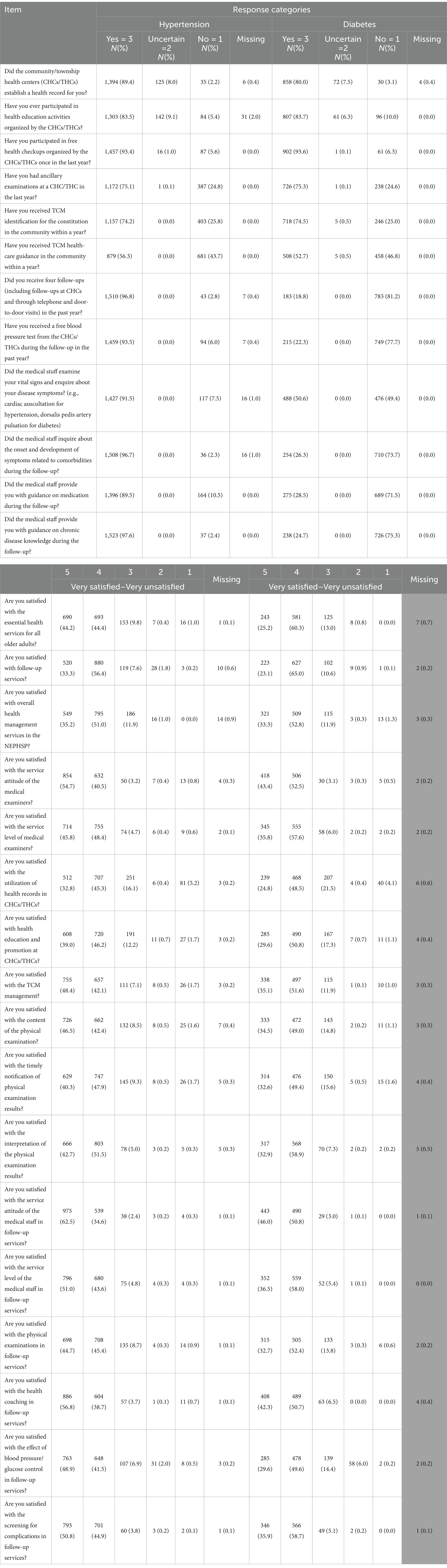
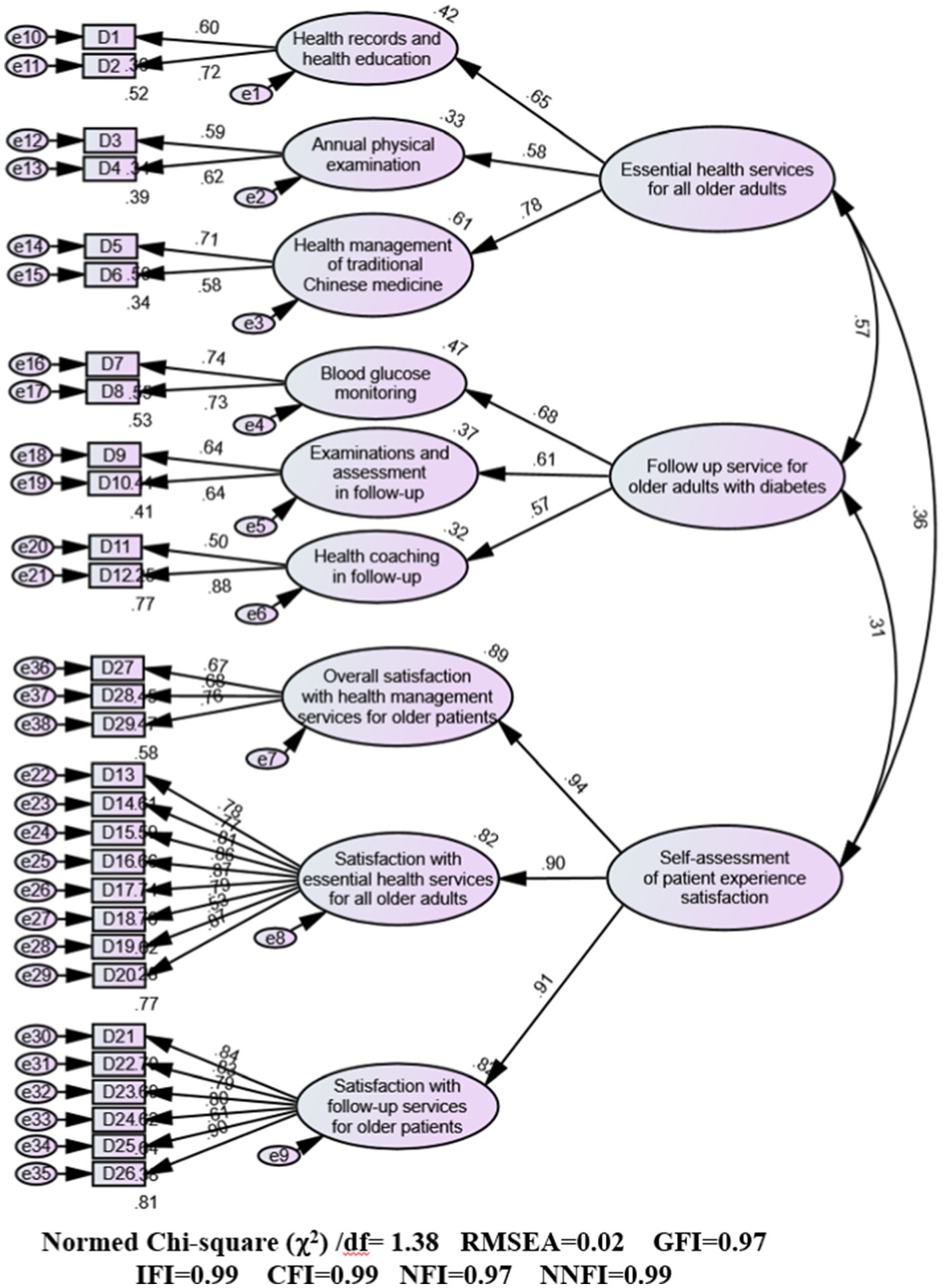
The bootstrap analysis conducted for 2000 iterations revealed a relatively good fit between the proposed model and observed data (Figures 2, 3). For the hypertension model, the absolute fit indices were as follows: Bollen–Stine bootstrap χ2/df = 1.78, GFI = 0.97, and RMSEA = 0.03. The comparative fit indices were as follows: incremental fit index = 0.99, confirmatory fit index = 0.99, NFI = 0.97, and NNFI = 0.99. The χ2/df value of 1.38 was below the threshold of 3, the RMSEA value of 0.03 was below the accepted cutoff of 0.05, and all other indices exceeded the benchmark of 0.90, confirming a good model fit. Similarly, the diabetes model also demonstrated strong fit indices: Bollen–Stine bootstrap χ2/df = 1.38, GFI = 0.97, and RMSEA = 0.02. The comparative fit indices were incremental fit index = 0.99, confirmatory fit index = 0.99, NFI = 0.97, and NNFI = 0.99. The χ2/df value of 1.38 was lower than the threshold of 3 and the RMSEA value of 0.02 was below the threshold of 0.05, with all other indices exceeding 0.90. The fit indices across the three domains—“essential health management services for older adults,” “follow-up service for older adults with hypertension or diabetes,” and “self-assessment of patient experience satisfaction”—indicate that the resultant hypertension and diabetes models fit the data well.
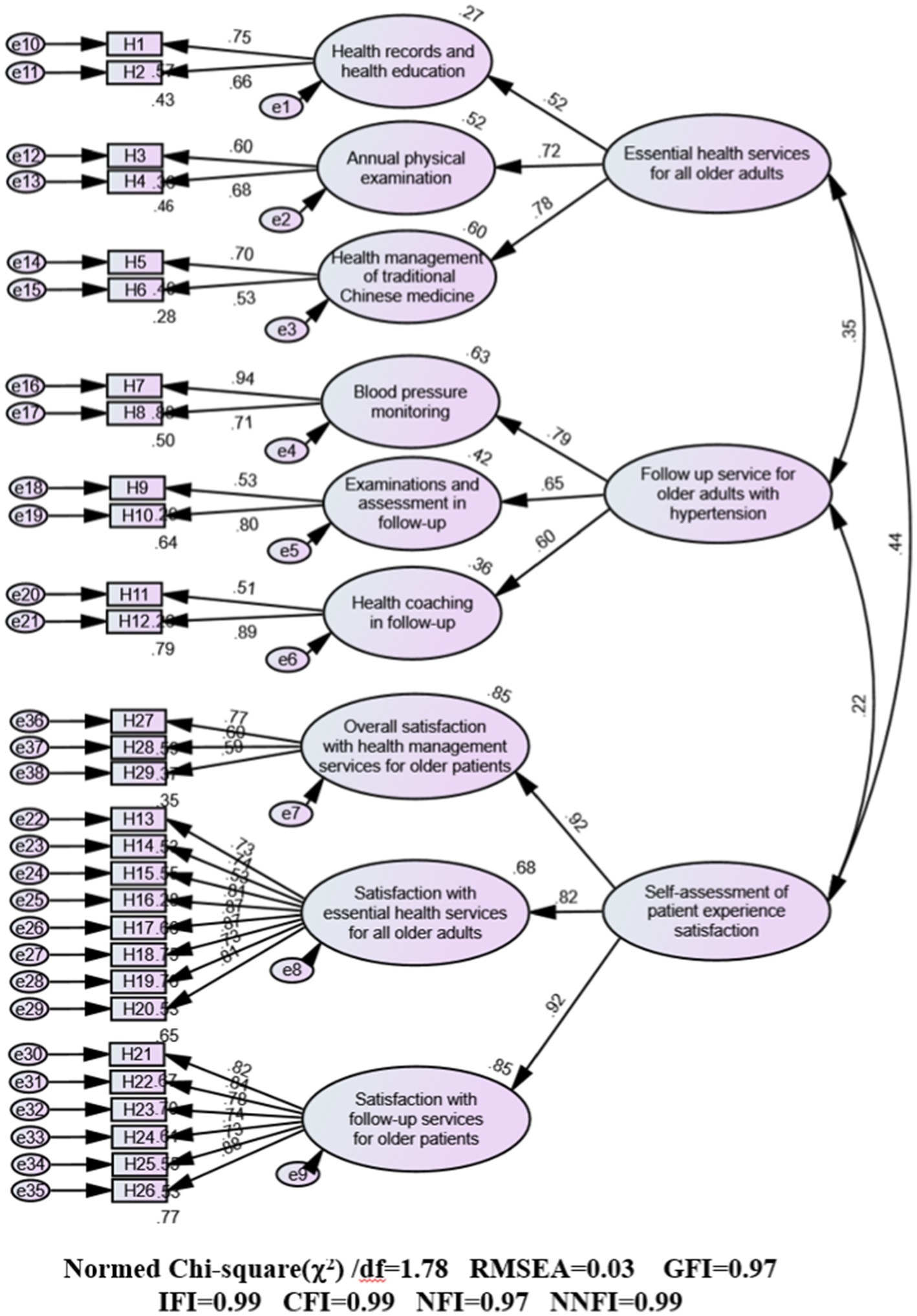
Figure 2. Standardized path diagram of confirmatory factor analysis (CFA) for the hypertension model.
Convergent validity
The convergent validity results for the three-factor and item measures are detailed in Tables 4, 5. Factor loadings obtained from the CFA ranged from 0.516 to 0.940 for the hypertension model and from 0.504 to 0.943 for the diabetes model. These values indicate that each latent variable was well represented by its associated observed variables. The AVE ranged from 0.387 to 0.692 for the hypertension model and from 0.365 to 0.640 for the diabetes model, meeting the acceptable threshold of 0.36. Similarly, the CR values were acceptable, ranging from 0.553 to 0.920 for the hypertension model and from 0.535 to 0.941 for the diabetes model. The “annual physical examination” (AVE: 0.413 for the hypertension model and 0.365 for the diabetes model), “health management of TCM” (AVE: 0.387 for the hypertension model and 0.421 for the diabetes model), and “examinations and assessment in follow-up” (AVE: 0.460 for the hypertension model and 0.407 for the diabetes model) had borderline AVE values but were still within a reasonable fit range. Additionally, “overall satisfaction with health management services for older patients” (AVE: 0.435) in the hypertension model also had reasonable fit with borderline AVE. In summary, the three indicators—factor loadings, AVE, and CR—fall within acceptable ranges, confirming that the models have convergent validity.
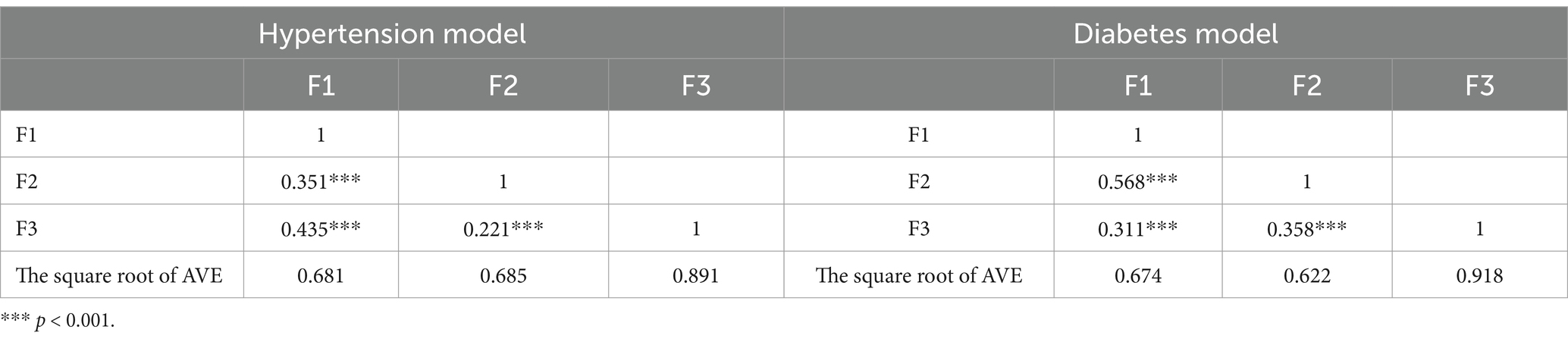
Discriminant validity
The models had discriminant validity. The analysis revealed that all the three first-order factors were significantly correlated with each other (p < 0.01), with their correlation coefficients lower than the square root of AVE for each respective factor in both models (Table 6). This finding indicates that although the latent variables exhibit some degree of correlation, they remain sufficiently distinct from one another.
Discussion
This study developed and validated the questionnaire designed to assess the utilization of the NEPHS from the perspective of older patients. The questionnaire is a comprehensive tool focused on patients’ accessibility to and satisfaction with health management services delivered through community-based interventions rather than traditional organizational measures or monitoring frameworks (43–45). The CFA, internal consistency assessment, and intercorrelation analyses across the 29 items demonstrated that the instrument is valid and reliable. These findings were consistent across various cities in regions with different levels of socioeconomic development in China.
This questionnaire is considered suitable for use not only in China but also in other countries. Health administration authorities can employ this tool to assess the effectiveness of public health programs in a phased manner, enhancing and supporting chronic disease management among older patients and ultimately improving their quality of life. For health-care providers, the 29-item scale offers three notable advantages. First, the study adopted a demand-side perspective, and the scale may more efficiently capture the items or domains that may be challenging to assess through service providers, particularly direct patient benefit variables rather than indirect process indicators. For example, evaluating the effectiveness of health education, literacy, and guidance is difficult because the outcome can substantially differ between project monitoring metrics and patients’ subjective experiences (46). Second, this assessment system encompassed the core health management services provided to older adults with chronic conditions under the NEPHSP. This comprehensive coverage facilitates comparisons of service effectiveness across different health-care centers over time. Third, considering the digital divide among older populations and their preference for on-site, paper-based surveys over online formats (47, 48), the questionnaire is designed with less technical language and has a hard copy version. This format is particularly suited to older adults in the study sample, most of whom did not have a high education level. Additionally, investigators are trained to implement relevant measures to assist participants in completing the questionnaire. Built on this foundation, the assessment tool is expected to be comprehensible, intuitive, and relevant to patient experiences.
Limitations
Despite the recruitment of a large and diverse sample, the study was limited to patients attending community health-care centers rather than encompassing a broader section of the population. Consequently, survey responses may reflect more favorable assessments of health examination and monitoring services among older patients, whose health management patterns may not fully represent those of broader or clinically managed populations. Consequently, this validated tool will continue to be used for assessing the effectiveness of chronic disease management and long-term monitoring programs, with plans for nationwide implementation in China. In developing the item pool, the focus was on capturing patients’ actual utilization of core services within the NEPHSP and their satisfaction with service processes, outcomes, and provider attitudes. However, items addressing ethical implications and professional responsibilities during service delivery, which are crucial to the patient experience, were not included. Continuous NEPHSP services for older patients with chronic disease depend on dynamically updated electronic health records containing sensitive personal information, such as annual physical examination data and quarterly follow-up results (49). This raises concerns regarding the core ethical and professional responsibilities of medical professionals, particularly regarding the safeguarding of such sensitive data (50). Future studies will address this gap by incorporating patients’ perspectives on these critical concerns into the assessment tool, refining its scope to better capture this essential aspect of health care.
Conclusion
In this study, a valid and reliable tool for assessing health management service utilization among older adults with hypertension and diabetes was developed. Data from a large and diverse sample of patients revealed very good to excellent fit by the logical model. The tool serves as a foundational framework for further tool development and holds promise for broader application in the evaluation of essential public health and primary health-care services. However, further validation in diverse health-care settings is required to fully establish its generalizability and effectiveness.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
This study was performed in accordance with the principles of the Declaration of Helsinki, and approval was granted by the Ethics Committee of the Chinese Academy of Medical Sciences and Peking Union Medical College (no. CAMS-PUMC-IEC-2022-025). Informed consent was obtained from all individual participants included in the study.
Author contributions
LL: Writing – original draft. ML: Investigation, Writing – review & editing. LYa: Investigation, Writing – review & editing. XC: Investigation, Writing – review & editing. YL: Conceptualization, Resources, Writing – review & editing. LYo: Conceptualization, Funding acquisition, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was funded by the China Medical Board (grant no. 18-296).
Acknowledgments
The study was supported by the Department of Primary Health of the National Health Commission of the PRC and the Health Commission of Shanxi, Zhejiang, and Chongqing Provinces. We sincerely thank the patients who participated in this study and all the community health professionals involved.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1459754/full#supplementary-material
References
1. World Health Organization. (2017). Cardiovascular diseases (cvds). Available online at:. (https://www.who.int/zh/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)).
2. Chinese Medical Association Diabetes Society Diabetes Chronic Complications Survey Group XH. A 10-year retrospective survey of chronic complications and associated risk factors in hospitalized diabetic patients. Chin J Diabetes. (2003) 6:5–10.
3. Olsen, MH, Angell, SY, Asma, S, Boutouyrie, P, Burger, D, Chirinos, JA, et al. A call to action and a lifecourse strategy to address the global burden of raised blood pressure on current and future generations: the lancet commission on hypertension. Lancet. (2016) 388:2665–712. doi: 10.1016/S0140-6736(16)31134-5
4. Mijajlovic, MD, Pavlovic, A, Brainin, M, Heiss, WD, Quinn, TJ, Ihle-Hansen, HB, et al. Post-stroke dementia - a comprehensive review. BMC Med. (2017) 15:11. doi: 10.1186/s12916-017-0779-7
5. Bundy, JD, Li, CW, Stuchlik, P, Bu, XQ, Kelly, TN, Mills, KT, et al. Systolic blood pressure reduction and risk of cardiovascular disease and mortality a systematic review and network meta-analysis. JAMA Cardiol. (2017) 2:775–81. doi: 10.1001/jamacardio.2017.1421
6. Collins, R, Peto, R, Godwin, J, and Macmahon, S. Blood pressure and coronary heart disease. Lancet. (1990) 336:370–1. doi: 10.1016/0140-6736(90)91908-S
7. National Center for Cardiovascular Diseases. Annual report on cardiovascular health and diseases in China (2020). Beijing: National Center for Cardiovascular Diseases (2021).
8. Magliano, DJ, and Boyko, EJ. Idf diabetes atlas. Brussels: International Diabetes Federation (2021).
9. Chinese Elderly Type 2 Diabetes Prevention and Treatment of Clinical Guidelines Writing Group; Geriatric Endocrinology and Metabolism Branch of Chinese Geriatric Society; Geriatric Endocrinology and Metabolism Branch of Chinese Geriatric Health Care Society, et al. clinical guidelines for prevention and treatment of type 2 diabetes mellitus in the elderly in China (2022 edition). Zhonghua Nei Ke Za Zhi. (2022) 1:12–50. doi: 10.3760/cma.j.cn112138-20211027-00751
10. Zhou, B, Perel, P, Mensah, GA, and Ezzati, M. Global epidemiology, health burden and effective interventions for elevated blood pressure and hypertension. Nat Rev Cardiol. (2021) 18:785–802. doi: 10.1038/s41569-021-00559-8
11. Oparil, S, Acelajado, MC, Bakris, GL, Berlowitz, DR, Cífková, R, Dominiczak, AF, et al. Hypertension. Nat Rev Dis Primers. (2018) 4:18014. doi: 10.1038/nrdp.2018.14
12. Jiang, Y, Sun, P, Chen, Z, Guo, J, Wang, S, Liu, F, et al. Patients’ and healthcare providers’ perceptions and experiences of telehealth use and online health information use in chronic disease management for older patients with chronic obstructive pulmonary disease: a qualitative study. BMC Geriatr. (2022) 22:9. doi: 10.1186/s12877-021-02702-z
13. United Nations, Population Division. World population ageing, 2019: Highlights. New York: United Nations, Population Division (2019).
14. World Health Organization. Working paper on the use of essential packages of health services in protracted emergencies. Geneva: World Health Organization (2018).
15. Watkins, DA, Jamison, DT, Mills, A, Atun, R, Danforth, K, Glassman, A, et al. Universal health coverage and essential packages of care In: DT Jamison, H Gelband, S Horton, P Jha, R Laxminarayan, and CN Mock, editors. Disease control priorities: improving health and reducing poverty. Washington, DC: The World Bank (2017)
16. World Health Organization. Management of physical health conditions in adults with severe mental disorders. Geneva: World Health Organization (2018).
17. National Health Commission of China. Management of reporting on the incidence of serious mental disorders. Beijing: National Health Commission of China (2013).
18. National Health Commission of China. Code of the national essential public health services program. Beijing: National Health Commission of China (2017).
19. World Health Assembly. Sustainable health financing, universal coverage and social health insurance. Geneva: World Health Organization (2005).
20. Liu, S, Jiang, C, Wang, J, and Liu, Y. The factors correlated with covid-19 vaccination coverage in chinese hypertensive patients managed by community general practitioner. Hum Vaccin Immunother. (2023) 19:2197839. doi: 10.1080/21645515.2023.2197839
21. You, L, Zhao, J, Chen, X, Yang, L, Liu, M, Pan, Y, et al. Progress and achievements of the implementation of national essential public health services programs over the past decade. Chin Gen Pract. (2022) 25:3209–20. doi: 10.12114/j.issn.1007-9572.2022.0407
22. Beran, D, Aebischer Perone, S, Castellsague Perolini, M, Chappuis, F, Chopard, P, Haller, DM, et al. Beyond the virus: ensuring continuity of care for people with diabetes during covid-19. Prim Care Diabetes. (2021) 15:16–7. doi: 10.1016/j.pcd.2020.05.014
23. Kang, L, Shang, W, Liu, J, and Liu, M. Policies implemented in Beijing for guaranteeing healthcare for community-dwelling patients with noncommunicable diseases during the covid-19 pandemic. Chin Gen Pract. (2022) 25:1172–6. doi: 10.12114/j.issn.1007-9572.2022.0091
24. You, L, Zhao, J, Chen, X, Yang, L, Liu, M, and Pan, Y. National essential public health services programs over the past decade research report two: progress and achievements of the implementation of national essential public health services programs over the past decade. Chin Gen Pract. (2022) 25:3209–20. doi: 10.12114/j.issn.1007-9572.2022.0406
25. Yang, Z, and Jiang, C. Impact of social capital, sex and education on the utilization of public health services: a cross sectional study based on the China migrant dynamic survey. BMC Public Health. (2021) 21:751. doi: 10.1186/s12889-021-10803-y
26. Chinese Diabetes Society; National Offic for Primary Diabetes Care. National guidelines for the prevention and control of diabetes in primary care. Zhonghua Nei Ke Za Zhi. (2018) 57:885–93. doi: 10.3760/cma.j.issn.0578-1426.2018.12.003
27. National Center for Cardiovascular Diseases. National guidelines for the management of hypertension prevention and treatment in primary care. Beijing: National Center for Cardiovascular Diseases (2021).
28. Goeschel, CA, Weiss, WM, and Pronovost, PJ. Using a logic model to design and evaluate quality and patient safety improvement programs. Int J Qual Health Care. (2012) 24:330–7. doi: 10.1093/intqhc/mzs029
29. Millar, A, Simeone, RS, and Carnevale, JT. Logic models: a systems tool for performance management. Eval Program Plann. (2001) 24:73–81. doi: 10.1016/S0149-7189(00)00048-3
30. Revelle, W, and Zinbarg, RE. Coefficients alpha, beta, omega, and the glb: comments on sijtsma. Psychometrika. (2009) 74:145–54. doi: 10.1007/s11336-008-9102-z
31. Wen, Z, and Ye, B. Test reliability estimation: from alpha coefficient to internal consistency reliability. Xin Li Xue Bao. (2011) 43:821–9.
32. Devellis, RF, and Thorpe, CT. Scale development: theory and applications. Thousand Oaks, CA: Sage publications (2021).
33. Browne, MW, and Cudeck, R. Alternative ways of assessing model fit. Sociol Methods Res. (1992) 21:230–58. doi: 10.1177/0049124192021002005
34. Jöreskog, KG. Lisrel 8: Structural equation modeling with the simplis command language. Chicago, IL: Scientific Software International (1993).
35. Hooper, D, Mullen, J, Hooper, D, Coughlan, J, and Mullen, MR. Structural equation modeling: guidelines for determining model fit. Electron J Bus Res Methods. (2008) 6:53–60. doi: 10.21427/D7CF7R
36. Bentler, PM. Comparative fit indexes in structural models. Psychol Bull. (1990) 107:238–46. doi: 10.1037/0033-2909.107.2.238
37. Hu, LT, and Bentler, PM. Fit indices in covariance structure modeling: sensitivity to underparameterized model misspecification. Psychol Methods. (1998) 3:424–53. doi: 10.1037//1082-989X.3.4.424
38. Hu, LT, and Bentler, PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. (1999) 6:1–55. doi: 10.1080/10705519909540118
39. Fornell, CLD. Evaluating structural equation models with unobservable variables and measurement error. J Mark Res. (1981) 18:39–50. doi: 10.1177/002224378101800104
40. Zhang, Z, and Zheng, L. Consumer community cognition, brand loyalty, and behaviour intentions within online publishing communities: an empirical study of epubit in China. Learn Publ. (2021) 34:116–27. doi: 10.1002/leap.1327
41. Byrne, B. Application 1: testing for the factorial validity of a theoretical construct (first order cfa model) In: MB Barbara, editor. Structural equation modeling with AMOS: Basic concepts, applications, and programming. New York: Psychology Press (2001)
42. Enders, CK. An sas macro for implementing the modified bollen-stine bootstrap for missing data: implementing the bootstrap using existing structural equation modeling software. Struct Equ Model. (2005) 12:620–41. doi: 10.1207/s15328007sem1204_6
43. Huang, P, Wang, M, Zhang, A, Chang, P, Li, L, and Gao, Z. Evaluation of the ten-year effect of implementing national basic public health services in shanghai. Chin Gen Prac. (2020) 18:1979–83. doi: 10.16766/j.cnki.issn.1674-4152.001668
44. You, L, Chen, X, Yang, L, Zhao, J, Zan, Z, Zhang, B, et al. Construction of health effect-oriented comprehensive evaluation index system for essential national public health service. Chin J Public Health. (2022) 38:589–96. doi: 10.11847/zgggws1137292
45. Zhang, K, Liang, Y, Gu, S, and Yang, J. Comprehensive evaluation of basic public health services in Anhui. Modern Prev Med. (2021) 48:1206–10. doi: 10.20043/j.cnki.mpm.2021.07.014
46. Kivelä, K, Elo, S, Kyngäs, H, and Kääriäinen, M. The effects of health coaching on adult patients with chronic diseases: a systematic review. Patient Educ Couns. (2014) 97:147–57. doi: 10.1016/j.pec.2014.07.026
47. Hargittai, E, Piper, AM, and Morris, MR. From internet access to internet skills: digital inequality among older adults. Univ Access Inf Soc. (2019) 18:881–90. doi: 10.1007/s10209-018-0617-5
48. Choi, NG, and Dinitto, DM. The digital divide among low-income homebound older adults: internet use patterns, ehealth literacy, and attitudes toward computer/internet use. J Med Internet Res. (2013) 15:e93. doi: 10.2196/jmir.2645
49. Nittari, G, Khuman, R, Baldoni, S, Pallotta, G, Battineni, G, Sirignano, A, et al. Telemedicine practice: review of the current ethical and legal challenges. Telemed J E Health. (2020) 26:1427–37. doi: 10.1089/tmj.2019.0158
Keywords: health management, older adults, hypertension, diabetes, construct validity, confirmatory factor analysis
Citation: Liu L, Liu M, Yang L, Chen X, Liu Y and You L (2025) A patient-reported questionnaire for evaluating utilization of the National Essential Public Health Service Program in China among older adults with hypertension and diabetes. Front. Public Health. 13:1459754. doi: 10.3389/fpubh.2025.1459754
Edited by:
Roberta Lamptey, Korle Bu Teaching Hospital, GhanaReviewed by:
Giovanna Ricci, University of Camerino, ItalyVimal Satodiya, Inland Psychiatric Medical Group, United States
Copyright © 2025 Liu, Liu, Yang, Chen, Liu and You. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lili You, eW91bGlseV9wdW1jQDE2My5jb20=
 Lu Liu
Lu Liu Meicen Liu
Meicen Liu Linghe Yang
Linghe Yang Xinyue Chen1
Xinyue Chen1 Yuanli Liu
Yuanli Liu Lili You
Lili You