- 1Department of Psychology, Korea University, Seoul, Republic of Korea
- 2KU Mind Health Institute, Korea University, Seoul, Republic of Korea
- 3Mindeep Cognitive Behavioral Therapy Center, Seoul, Republic of Korea
Background: The COVID-19 pandemic has caused significant unprecedented changes in lives. In particular, core daily activities, such as sleep, diet, physical activity, education, and social activities have significantly changed. Restrictions on daily activities are associated with the deterioration of mental health. However, few studies have comprehensively explored the relationship between daily activities and mental health during the COVID-19 pandemic, and longitudinal studies of these relationships are lacking. Therefore, this study examined the dynamic interaction between core daily activities and mental health during the COVID-19 pandemic.
Methods: An online survey was conducted with 586 adults (age: M = 46.80, SD = 12.515) in three waves: September 2020, December 2020, and April 2021. Depressive symptoms, anxiety, and suicidality were assessed using Mental Health Screening Tool. Daily activities were assessed using Core Life Activities Inventory. Autoregressive and cross-lagged effects were investigated using a cross-lagged panel analysis.
Results: Reduced daily activities contributed to increased depression, anxiety, and suicidality, which, in turn, resulted in further decreases in daily activities in subsequent waves. These autoregressive and reciprocal effects persisted for 7 months during the pandemic. Among core daily activities, sleep quality, physical activity, and social activities had reciprocal relationships with depression. Moreover, only social activities showed a reciprocal relationship with anxiety and suicidality.
Conclusion: These findings highlight the complex relationship between core daily activities and mental health and provide valuable insights for targeted therapeutic strategies. Implementing timely and effective interventions to maintain and enhance key activities, particularly social engagement, is crucial for alleviating negative mood symptoms. Clinical support and promotion of these essential daily activities are necessary to improve mental health outcomes.
Introduction
The novel coronavirus (COVID-19) was first detected in Wuhan Province, China, in December 2019 (1). The outbreak of the COVID-19 pandemic led to unprecedented challenges that affected various aspects of daily life globally (2). To curb the spread of the virus, governments enacted stringent regulations, including lockdowns, for individuals exhibiting symptoms or those in contact with them. Public health strategies, such as social distancing, home confinement, and lifestyle changes significantly affected mental health (3). Quarantine and social distancing measures constrained daily activities, deteriorating mental wellbeing (4–6).
Five key daily activities—sleep, diet, exercise, education, and social connections—are particularly important in mental and physical health (7–10). Extended home confinement caused increased issues with sleep, including poor sleep quality and symptoms of sleep disorders (11, 12). Moreover, changes in dietary habits emerged, marked by increased snacking, late-night eating, weight gain, and an increase in home-cooked meals (8, 13). Physical activity decreased, whereas sedentary behavior increased (14, 15). Furthermore, the pandemic disrupted global education systems (16) and severely restricted social gatherings.
Deficiencies in daily activities increased depression and anxiety, and depression and anxiety reduced daily activities. One study found that these reciprocal autoregressive effects persisted throughout a seven-month period of the pandemic (17). A meta-analysis of 0.9 million people across 32 countries found that disrupted daily routines were strongly associated with depressive symptoms and anxiety (18). For instance, sleep disturbance, a common feature of depression and anxiety (19, 20), exhibited a bidirectional relationship with disrupted daily routines (21). Poor sleep and diet quality were correlated with negative moods (22). Sleep disturbances, including nightmares and insomnia showed a significant link between suicidal ideation, suicide attempts, and actual suicides, as found in longitudinal studies (23, 24). Additionally, there was much evidence of associations between poor dietary quality and depression, anxiety, and suicidal ideation (25). Physical inactivity during the pandemic was linked to increased depression scores (26), and reduced social contact and mobility were associated with higher levels of depression and anxiety (27). Reduced physical activity combined with increased sedentary behavior substantially raised the risk of suicidal ideation and planning among adolescents of both genders and correlated with a greater frequency of suicide attempts in males, compared to those maintaining sufficient physical activity and lower levels of sedentary behavior (28, 29). Solitude and the experience of loneliness were significantly associated with suicidal ideation and attempts, as found in research (30).
Disruption of daily activities was found to be correlated with increased symptoms of depression and anxiety and increased suicidal thoughts and behaviors (31, 32). Although previous studies have highlighted the link between lifestyle factors and mental health, they mainly focused on a single factor, and few have examined the comprehensive relationship between activities in daily life and mental health outcomes. Moreover, most studies have relied on cross-sectional designs that lack the longitudinal and dynamic perspectives necessary to understand the evolving relationships during a global health crisis.
Therefore, this study examined the autoregressive, temporal, and reciprocal relationships between daily activities and mental health during the COVID-19 pandemic using a three-wave cross-lagged analysis. In contrast to cross-sectional designs, cross-lagged analyses evaluate multiple time points, rendering them particularly suitable for determining the directionality of relationships between lifestyle factors and mental health states. By integrating autoregressive and cross-lagged pathways, these analyses provide insights into the stability and bidirectional effects of lifestyle factors (33). Moreover, this study aimed to identify the impact of demographic factors, such as age, gender, income, and educational status, on these relationships. The hypotheses are that lower levels of daily activities are associated with higher levels of depression, anxiety, and suicidality in subsequent periods. Conversely, higher levels of depression, anxiety, and suicidality are associated with lower levels of daily activities across three waves.
Methods
Participants and design
We conducted an online questionnaire survey on daily activities, depression, anxiety, and suicide risk among adults in South Korea. We recruited representative samples of participants in three waves: September 1–8, 2020 (Wave 1), December 16–23, 2020 (Wave 2), and April 19–28, 2021 (Wave 3). Participants aged 18–68 years were recruited through an online research company using a stratified sampling method based on age, gender, and geographic area. No other exclusion criteria were applied. A total of 817 individuals responded to the survey (Wave 1: 817, Wave 2: 684, and Wave 3: 586). The data of participants who provided complete responses in all three waves (n = 586) were analyzed. This study was approved by the Institutional Review Board of Korea University (KUIRB-2021-0013-02). All participants voluntarily provided written online informed consent prior to participating in the study. Participants were compensated with 1,500 KRW (roughly 1.12 USD) for completing each survey.
Measures
Anxiety
Anxiety was measured using the 11-item Mental Health Screening Tool for Anxiety Disorders (MHS-A) (34), which evaluates respondents’ anxiety over the preceding 2 weeks. Responses are rated on a 5-point Likert scale (0 = never; 4 = most of the time). The Cronbach’s alpha coefficients for the MHS-A in Waves 1–3 were 0.962, 0.969, and 0.964, respectively, indicating good internal consistency.
Depressive symptoms
Depressive symptoms were measured using the 12-item Mental Health Screening Tool for Depressive Disorders (MHS-D) (35), which evaluates respondents’ depression symptoms over the preceding two weeks. Responses are rated on a 5-point Likert scale (0 = not at all; 4 = strongly agree). The Cronbach’s alpha coefficients for the MHS-D for Waves 1–3 were 0.947, 0.947, and 0.946, respectively, indicating good internal consistency.
Suicidality
Suicidality was measured using the four-item Mental Health Screening Tool for Suicide Risk (MHS-S) (36), which evaluates respondents’ willingness to live, suicidal ideation, and consideration or plans to commit suicide over the preceding two weeks as well as previous suicide attempts. Responses are rated on a 5-point Likert scale (0 = never; 4 = always). The Cronbach’s alpha coefficients for the MHS-S in Waves 1–3 were 0.909, 0.917, and 0.917, respectively, indicating good internal consistency.
Daily activities
Daily activities were measured using the five-item Core Life Activities Inventory (CORE) (7), which evaluates respondents’ sleep quality, diet, physical activity, education, and social activities over the preceding week. Responses are rated on a 5-point Likert scale (1 = not at all; 5 = strongly agree). The Cronbach’s alpha coefficients for CORE in Waves 1–3 were 0.767, 0.776, and 0.815, respectively, indicating good internal consistency.
Statistical analysis
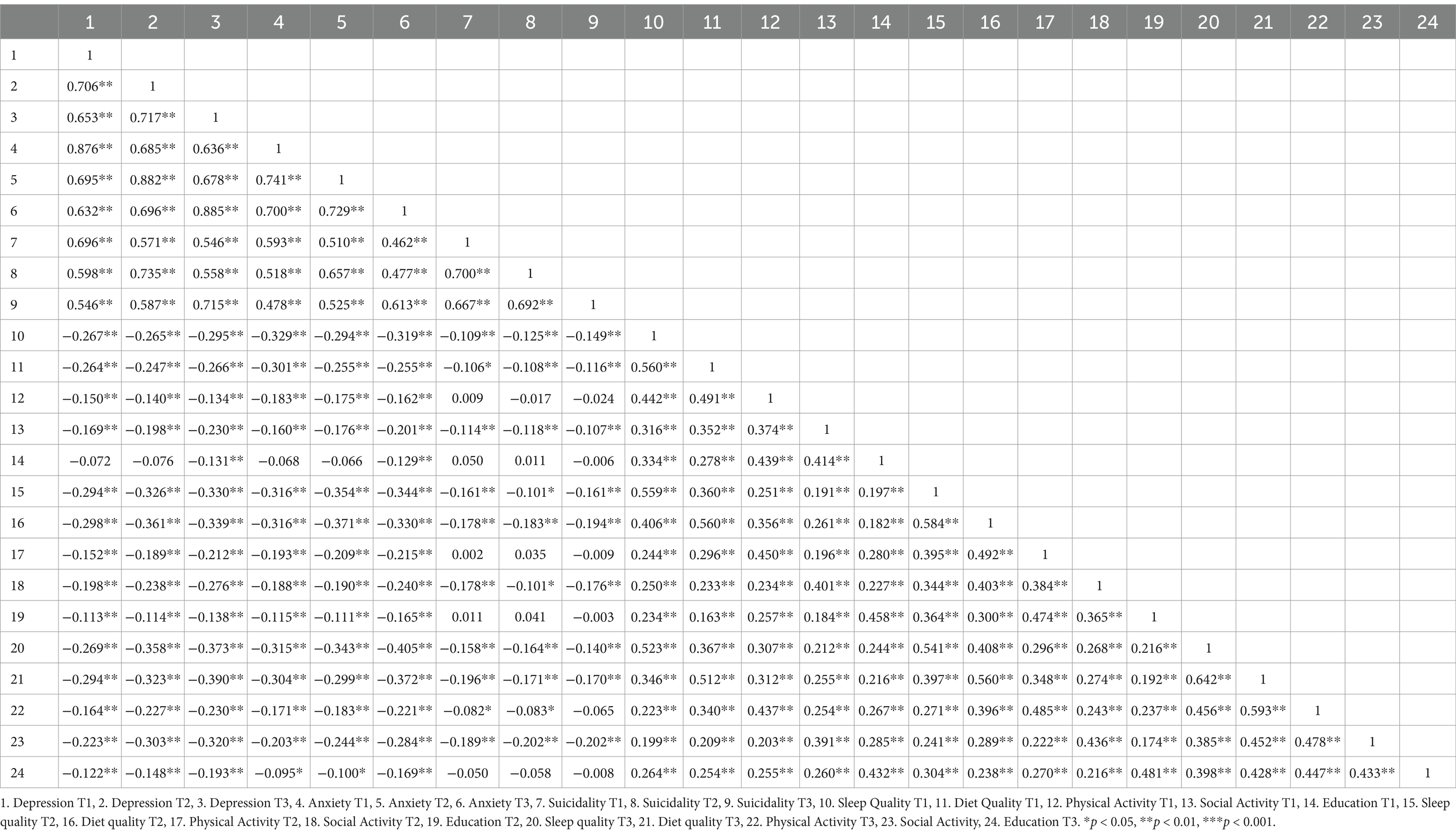
Tables 1 and 2 present the descriptive statistics, and Table 3 presents the correlations among the research variables. Pearson’s correlation analysis was conducted using SPSS 25.0 to investigate cross-sectional and longitudinal associations among the variables.
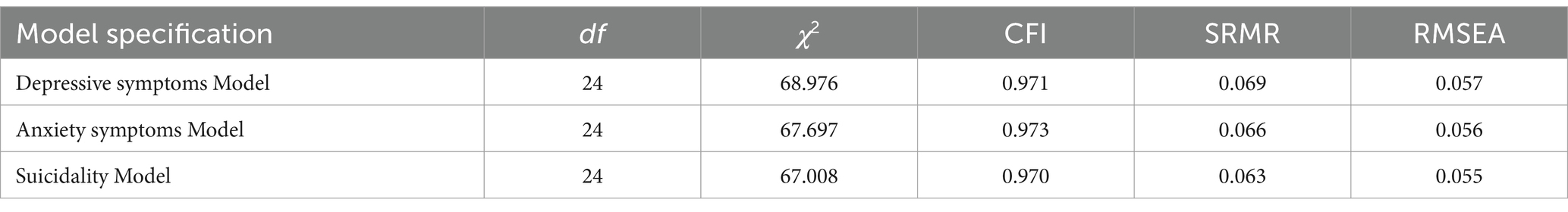
To explore the reciprocal and cross-sectional relationships between variables, we used structural equation modeling (SEM) for cross-lagged panel models (CLPMs) in a three-stage process. First, we validated the measurement model. We established confirmatory factor analysis models for the variables (depression, anxiety, suicidality, and daily activities) for each wave. We evaluated model fit using the comparative fit index (CFI), standardized root mean squared residual (SRMR), and root mean square error of approximation (RMSEA). CFI ≥ 0.90, SRMR and RMSEA ≤0.08 indicate acceptable model fit (37, 38).
Next, we evaluated measurement invariance across time for all main variables. Variations in response patterns to survey questions across time points might reflect distinct latent constructs or measurement errors. Therefore, measurement invariance is necessary for valid comparisons over time (39). Alignment of measurement invariance is recommended, as it allows for latent mean differences and comparisons across groups in large longitudinal samples (40).
Finally, we constructed autoregressive CLPMs using SEM in Mplus Version 8.3 (41). CLPMs facilitate the examination of autoregressive, reciprocal, and causal relationships over time while controlling for both autoregressive and cross-sectional effects (42).
Results
Preliminary analyses
Little’s Missing Completely at Random (MCAR) test [χ2(12) = 19.974, p = 0.068] revealed that characteristics of missing data were random (43). The independent t-test analysis found no significant differences in gender, age, or income between the dropout and final samples. This indicated that missing data were not dependent on specific variables, supporting the listwise approach (44). As missing data accounted for 28.2% (n = 231) of the total data, using methods to impute missing values could lead to inaccurate results. The listwise method can be suitable for this data, as it minimizes the risk of biased results. The participants with missing data were excluded from the hypothetical analysis.
Descriptive statistics and bivariate correlations
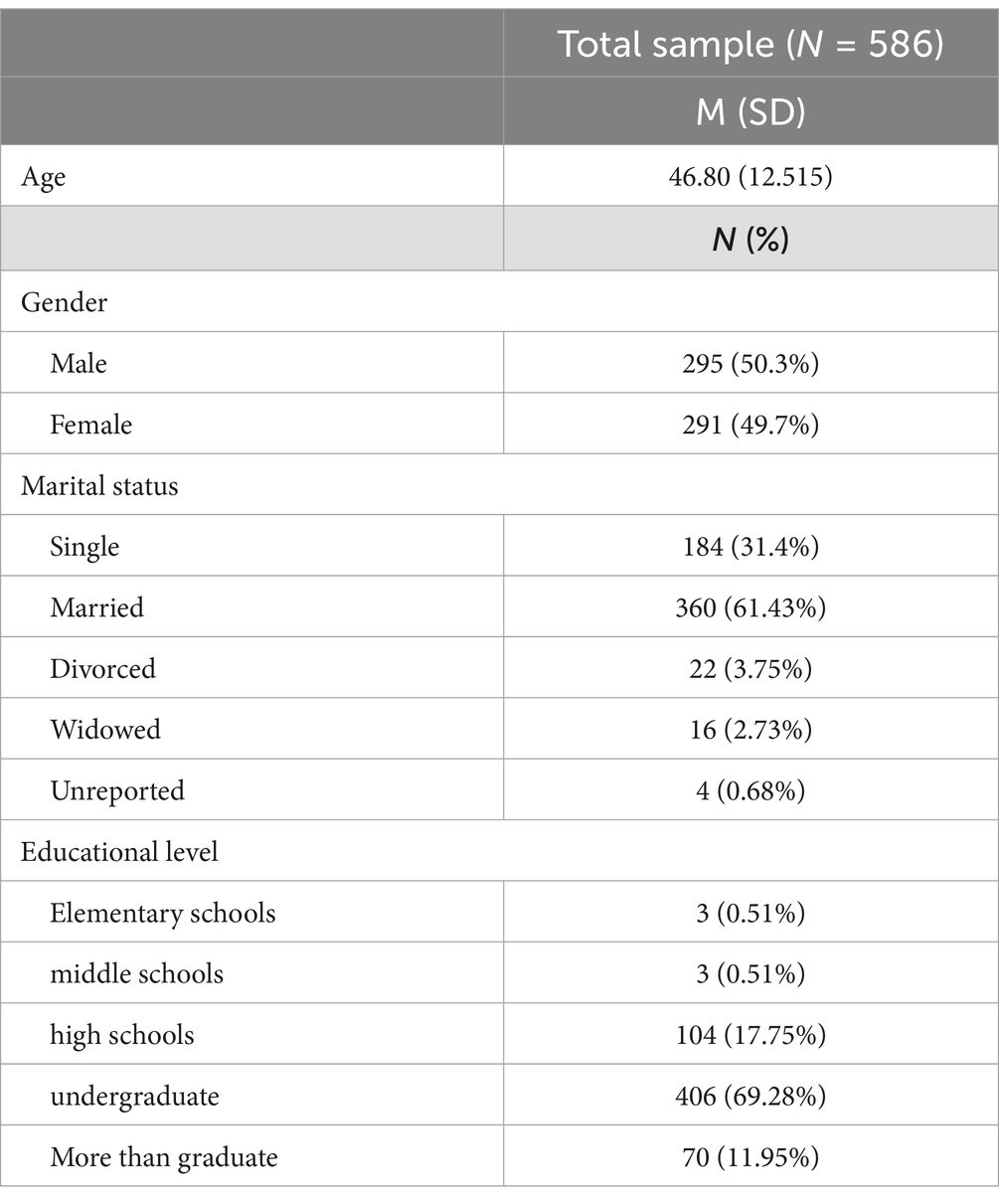
The participants’ demographic information is presented in Table 1. Of the 586 participants, 295 (50.3%) were men and 291 (49.7%) were women. Their age ranged from 20 to 68 years, with a mean age of 46.80 (SD = 12.515) years.
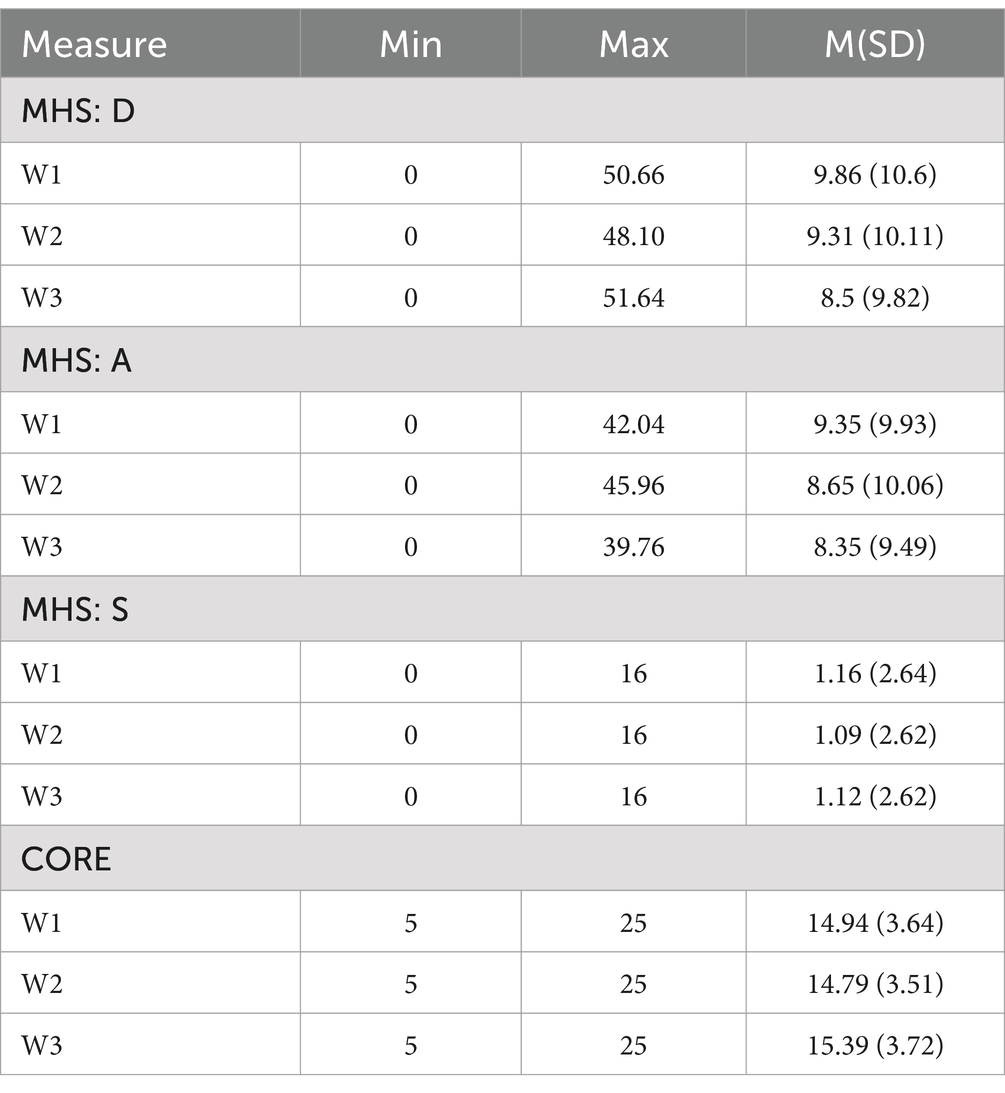
Depressive symptoms, anxiety, suicidality, and daily activities were significantly correlated throughout the study period. The descriptive statistics and bivariate correlations are presented in Tables 2 and 3, respectively.
The mental health prevalence rates for each period were measured. The cutoff values for depression, anxiety, and suicidality levels are shown in Supplementary Table S1. Of the participants, 27.8, 24.4, and 23.4% were classified as having moderate-to-severe depressive symptoms in Waves 1–3, respectively; 26.3, 24.2, and 21.7% were classified as having moderate-to-severe anxiety in Waves 1–3, respectively; and 19.1, 16.2, and 18.9% were classified as having moderate-to-severe suicidality in Waves 1–3, respectively.
Measurement invariance
In longitudinal studies, time invariance is a critical assumption for panel models, ensuring an accurate interpretation of temporal changes. This study assessed the measurement invariance of the latent constructs (depression, anxiety, suicidality, and daily activities) using alignment of measurement invariance. This approach was used to verify the absence of latent mean differences across the three waves before testing the main hypotheses. Each latent variable was independently verified using alignment of measurement invariance. The configural model fit indices indicated satisfactory results for each construct; comprehensive details are provided in Supplementary Table S2. These findings demonstrated longitudinal measurement invariance across all assessments, indicating a consistent measurement of constructs over time.
Cross-lagged results
Cross-lagged panel analysis
Cross-lagged regression models were used to analyze the causal associations among depressive symptoms, anxiety, suicidality, and daily activities, controlling for demographic variables. First, the paths represented the temporal stability of each variable. Second, the paths represented the cross-lagged effects between variables. Finally, the specific daily activities model represented the paths of the demographic variables.
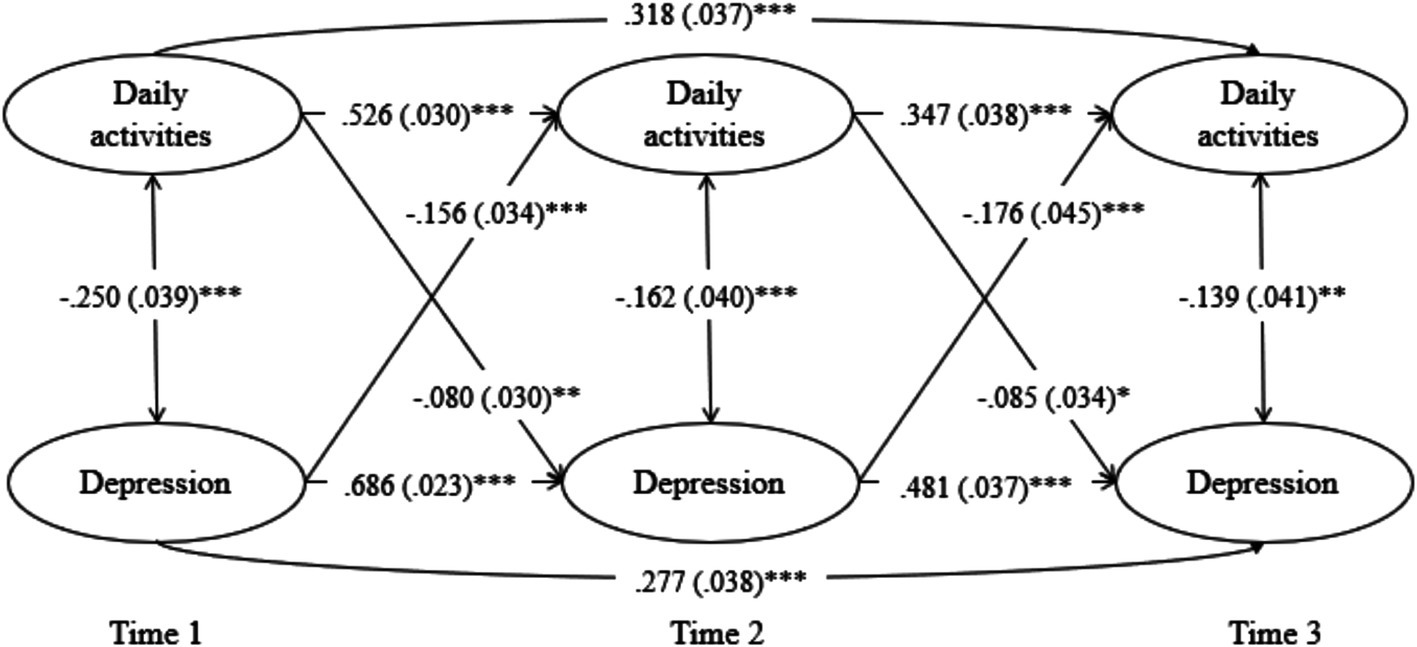
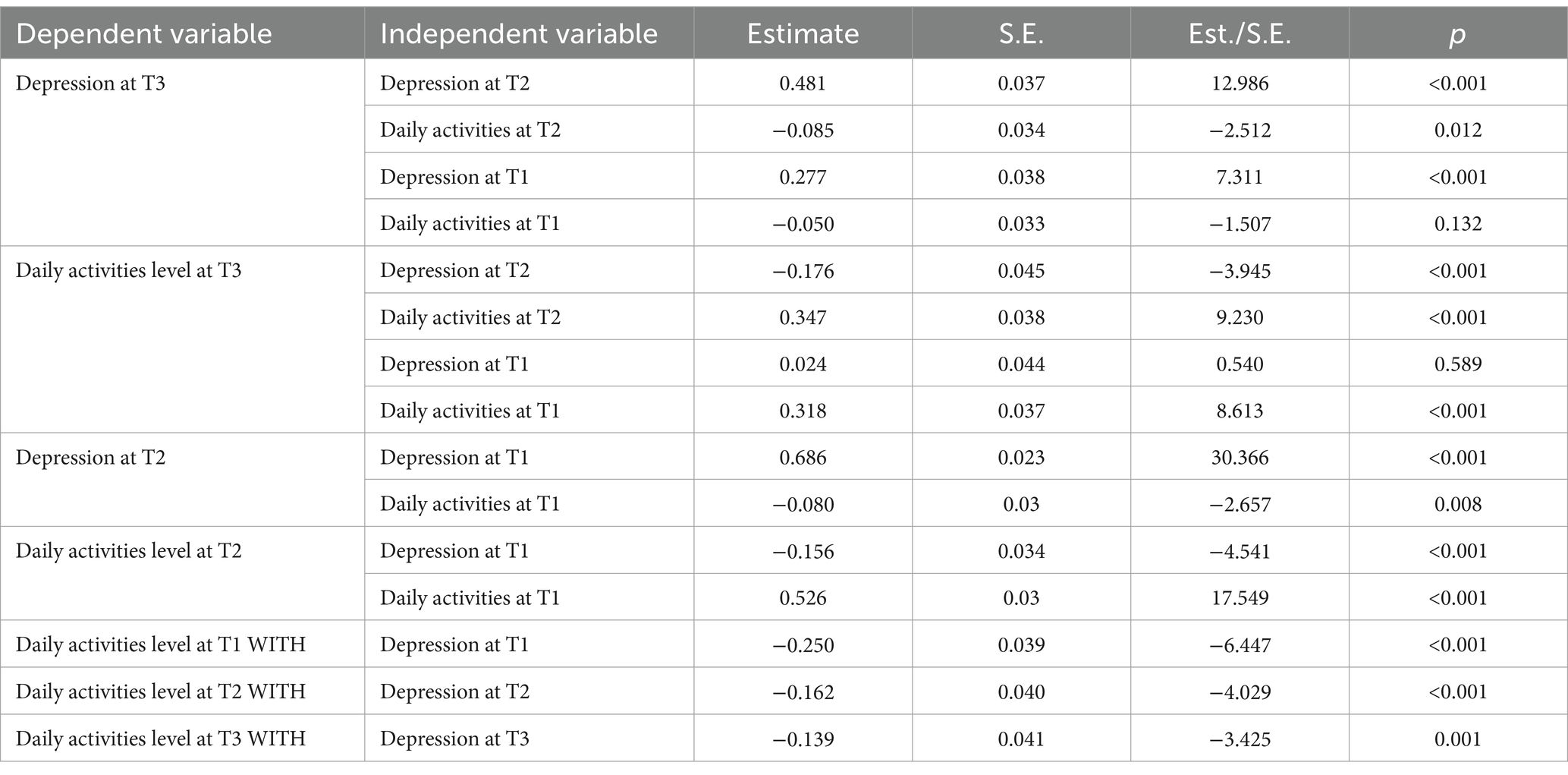
General daily activities and mental health
The CLPM for depressive symptoms and general daily activities exhibited a good fit (Table 4) and significant autoregressive and cross-lagged paths. This implies reciprocal effects, with depressive symptoms in Wave 1 predicting high depressive symptoms (β = 0.686, p < 0.001) and low daily activities in Wave 2 (β = −0.156, p < 0.001). Daily activity level in Wave 1 predicted depressive symptoms (β = −0.080, p = 0.008) and level of daily activities in Wave 2 (β = 0.526, p < 0.001). Subsequently, depressive symptoms in Wave 2 predicted depressive symptoms (β = 0.481, p < 0.001) and level of daily activities in Wave 3 (β = −0.176, p < 0.001). Moreover, the level of daily activities in Wave 2 predicted depressive symptoms (β = −0.085, p = 0.012) and level of daily activities in Wave 3 (β = 0.347, p < 0.001). Depressive symptoms in Wave 1 persisted in Wave 3 (β = 0.227, p < 0.001), and daily activities in Wave 1 influenced those in Wave 3 (β = 0.318, p < 0.001). However, daily activities and depressive symptoms did not cross-influence each other between Waves 1 and 3 (Figure 1; Table 5).
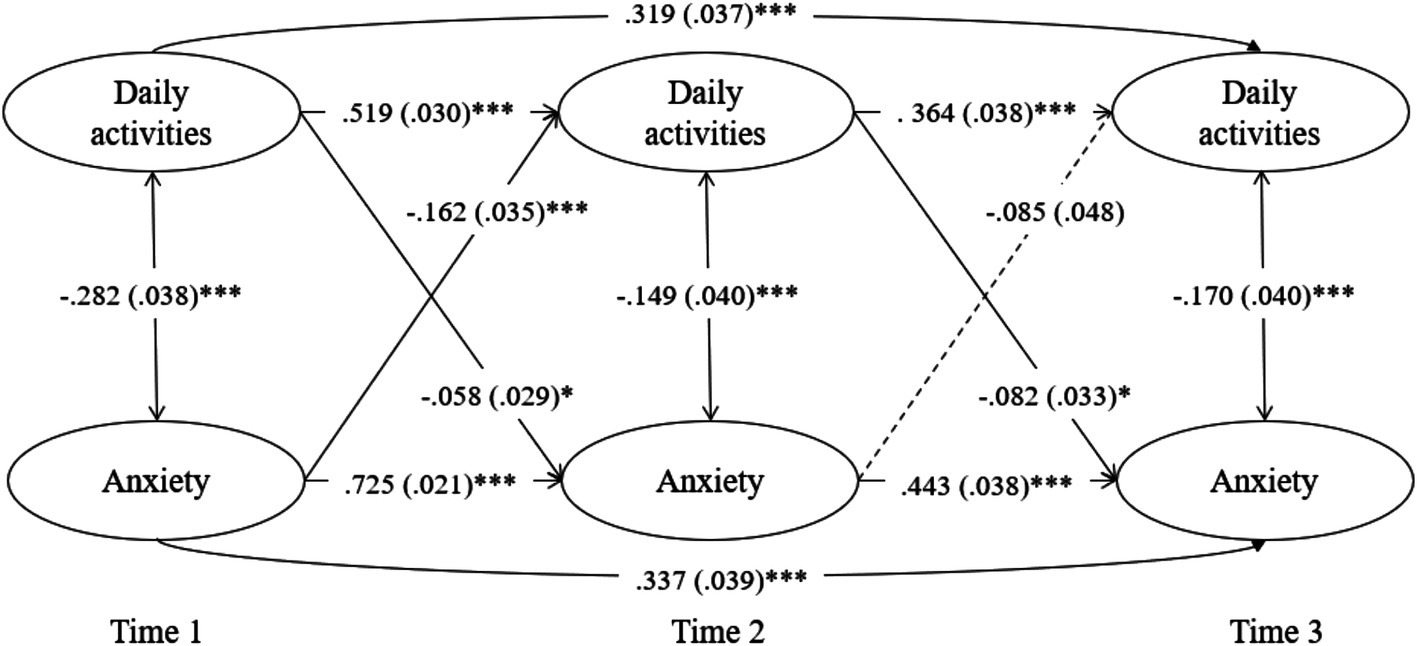
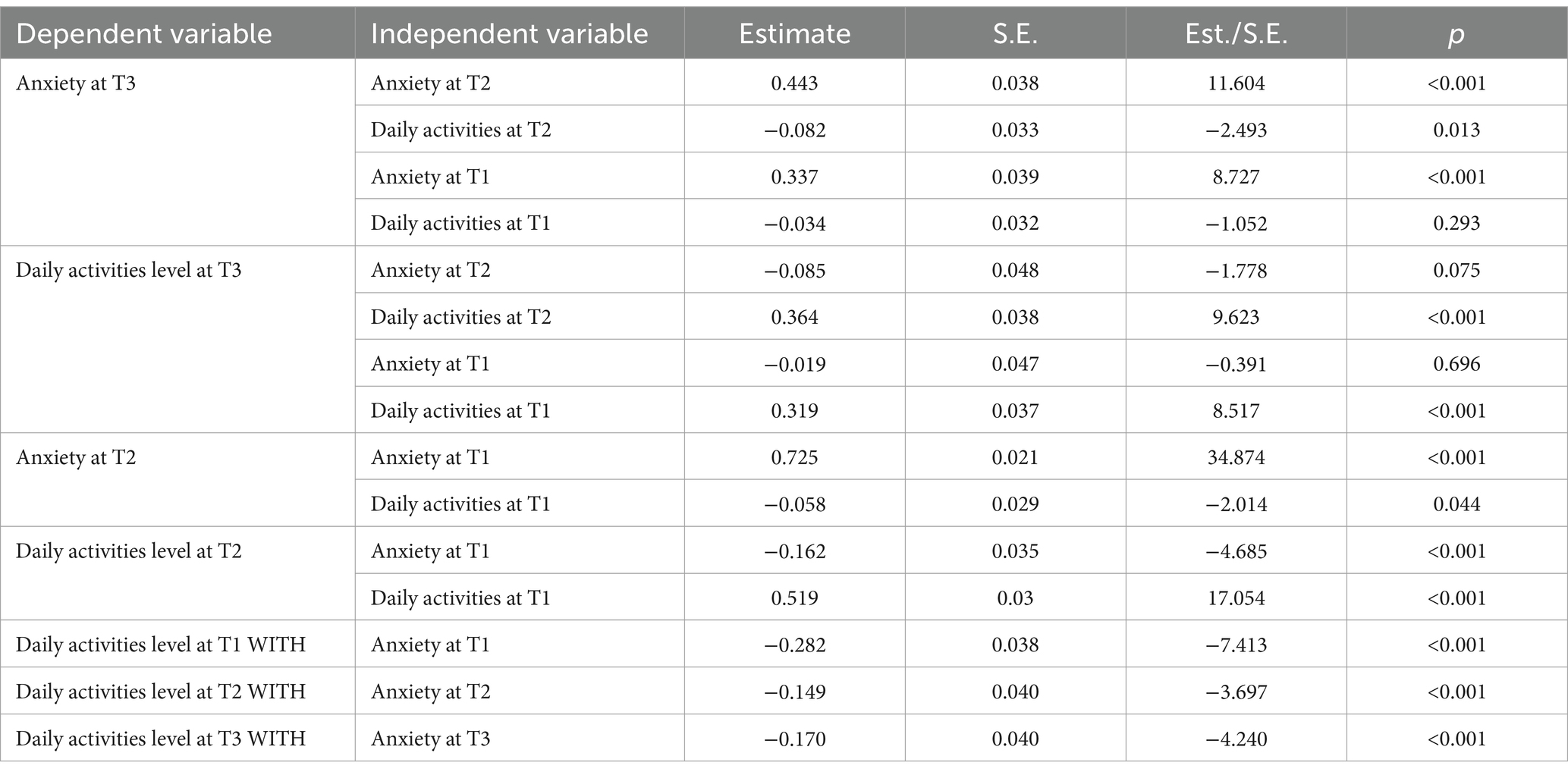
The CLPM for anxiety exhibited a good fit (Table 4) and stable patterns with significant autoregressive and cross-lagged paths. Significant reciprocal effects were observed, with anxiety in Wave 1 predicting high anxiety (β = 0.725, p < 0.001) and low daily activities in Wave 2 (β = −0.162, p < 0.001). Daily activity level in Wave 1 predicted anxiety (β = −0.058, p = 0.044) and level of daily activities in Wave 2 (β = 0.519, p < 0.001). Subsequently, anxiety in Wave 2 predicted anxiety in Wave 3 (β = 0.443, p < 0.001) but did not significantly predict level of daily activities in Wave 3 (β = −0.085, p = 0.075). Moreover, the level of daily activities in Wave 2 predicted anxiety 3 (β = −0.082, p = 0.013) and level of daily activities in Wave 3 (β = 0.364, p < 0.001). Anxiety in Wave 1 persisted in Wave 3 (β = 0.337, p < 0.001), and daily activities in Wave 1 influenced those in Wave 3 (β = 0.319, p < 0.001). However, daily activities and anxiety did not cross-influence each other between Waves 1 and 3 (Figure 2; Table 6).
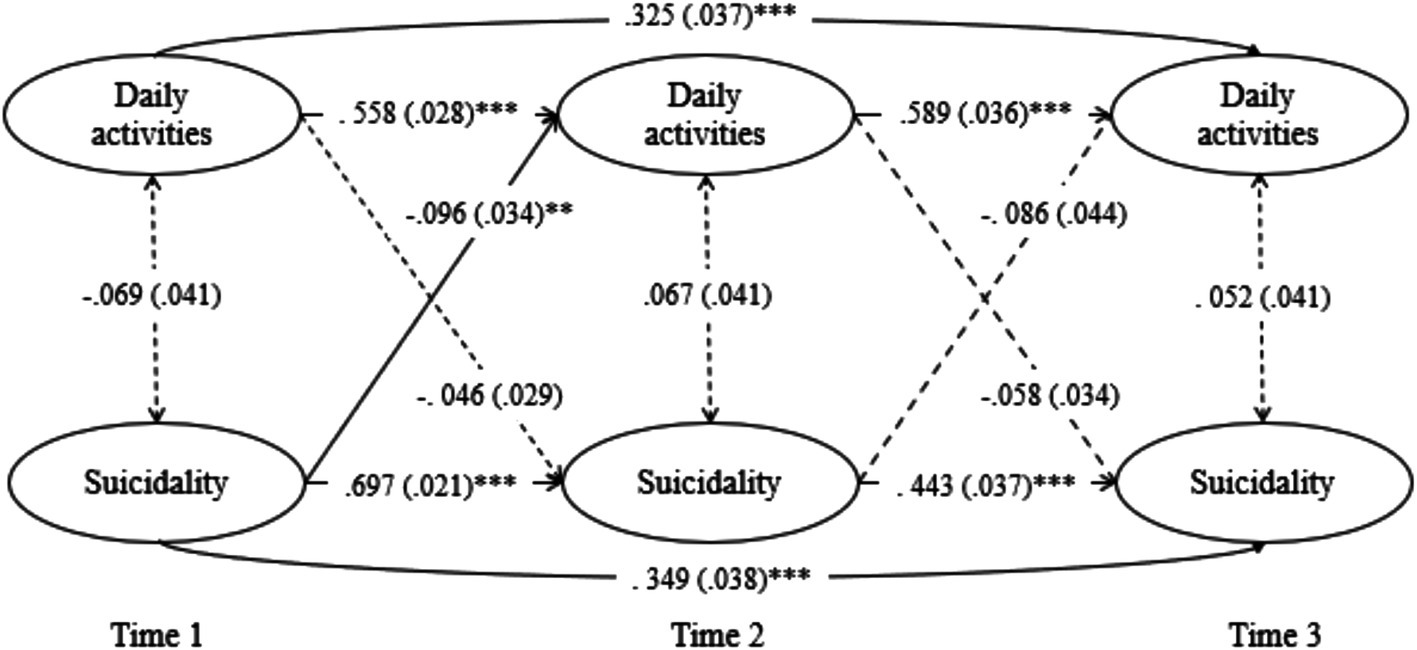
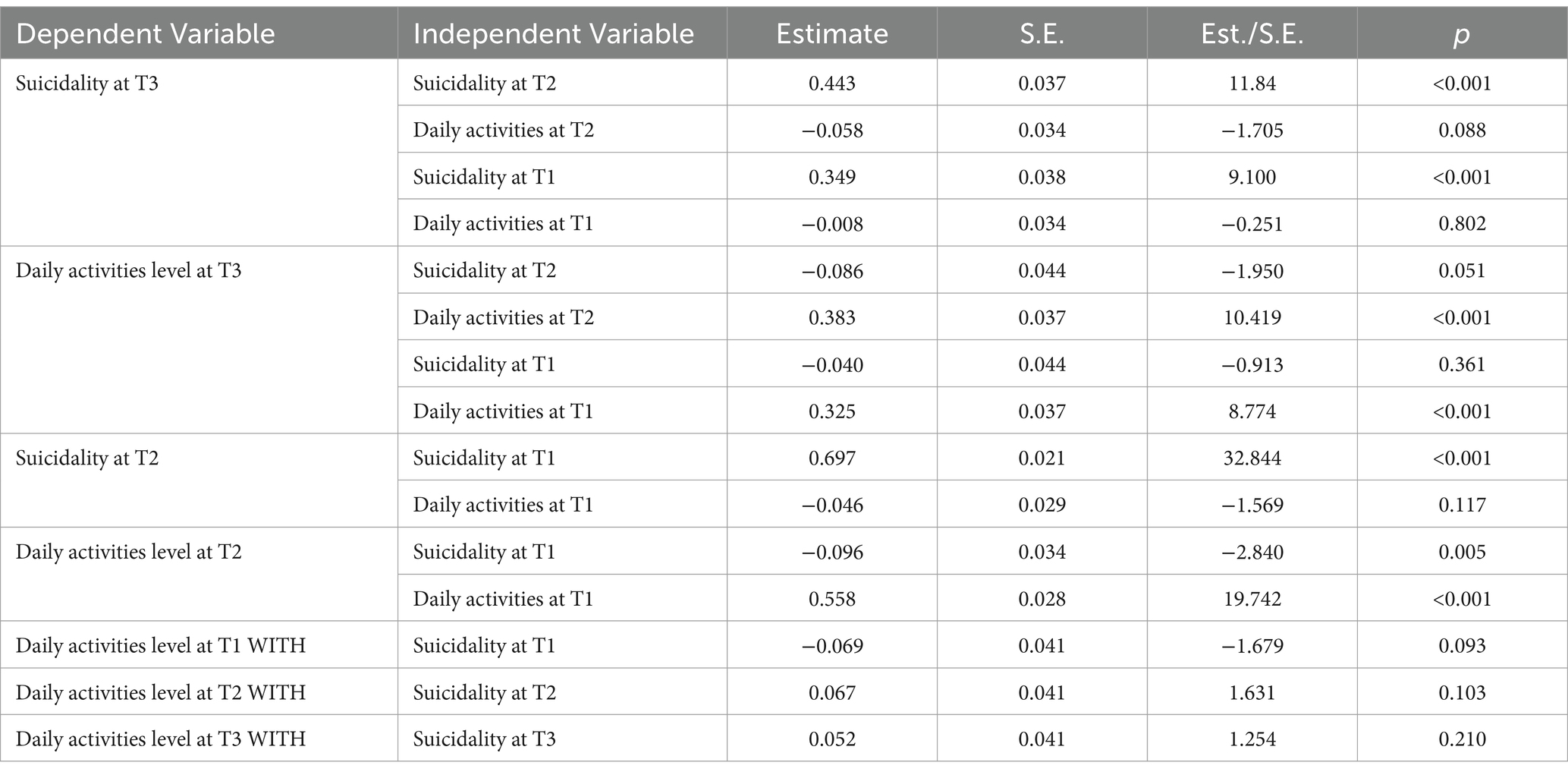
The CLPM for suicidality exhibited a good fit (Table 4) and reciprocal patterns with significant autoregressive and partial cross-lagged paths. Significant stable effects were observed, with suicidality in Wave 1 predicting high suicidality (β = 0.697, p < 0.001) and low level of daily activities in Wave 2 (β = −0.096, p = 0.005). Daily activity level in Wave 1 predicted daily activity level in Wave 2 (β = 0.558, p < 0.001) but did not significantly predict suicidality in Wave 2 (β = −0.046, p = 0.117). Subsequently, suicidality in Wave 2 predicted suicidality in Wave 3 (β = 0.443, p < 0.001) but did not significantly influence daily activities in Wave 3 (β = −0.086, p = 0.051). Moreover, daily activity level in Wave 2 predicted daily activity level in Wave 3 (β = 0.383, p < 0.001) but did not significantly predict suicidality in Wave 3 (β = −0.058, p = 0.088). Suicidality in Wave 1 persisted in Wave 3 (β = 0.349, p < 0.001), and daily activities in Wave 1 influenced those in Wave 3 (β = 0.325, p < 0.001). However, daily activities and suicidality did not cross-influence each other between Waves 1 and 3 (Figure 3; Table 7).
Specific daily activities and mental health
We analyzed the impact of five daily activities on negative mental health outcomes. The model of mental health and daily activities exhibited a good fit (Supplementary Table S3). Individual daily activities exhibited autoregressive paths between the study waves (Supplementary Tables S4–S6). However, few cross-lagged paths with mental health were identified.
Significant autoregressive and cross-lagged paths were identified between depression and sleep, physical activities, and social activities. Diet did not affect depression, and educational activities partially affected subsequent depressive symptoms. This indicated that sleep quality impacted subsequent sleep quality, and depressive symptoms impacted subsequent depressive symptoms. Furthermore, significant reciprocal negative effects were observed, with sleep quality predicting subsequent depression levels, and the severity of depression affecting subsequent sleep quality. Physical activity and depressive symptoms showed significant autoregressive pathways. Moreover, physical activity was partially and reciprocally negatively correlated with depression. In other words, physical activity influenced subsequent depression levels, and the severity of depression affected subsequent physical activity. The relationship between social activities and depressive symptoms showed significant autoregressive paths between each social activities and depressive symptoms, and social activity was negatively associated with depression. That is, social activities influenced subsequent depression levels, and the severity of depression affected subsequent social activities (Supplementary Table S4).
Only social activities exhibited a reciprocal effect on anxiety. This indicates partially reciprocal negative effects, with social activities predicting subsequent anxiety levels, and severity of anxiety affecting subsequent social activities. That is, a higher level of social activities predicted lower levels of anxiety, and more severe anxiety resulted in fewer social activities (Supplementary Table S5).
In the models of suicidality and daily activities, only social activities showed reciprocal effects on suicidality. Higher social activities predicted a lower level of suicidality in the future. The other activities did not show cross-lagged paths to suicidality (Supplementary Table S6).
In addition to demographic variables, lower income and educational status were associated with higher levels of depression, lower income was associated with higher anxiety, and none of the demographic variables were associated with suicidality. Regarding the relationship between demographic variables and specific daily activities, men engaged in more physical activities, whereas women engaged in more social activities. Older participants engaged in more physical activities compared with younger participants (Supplementary Tables S4–S6).
Discussion
This study examined the longitudinal reciprocal relationships between daily activities and mental health, including depressive symptoms, anxiety, and suicidality. Our findings revealed the stable and longitudinal effects of daily activities, depressive symptoms, anxiety, and suicidality, controlling for age, gender, income, and educational status. Over a seven-month period, general daily activities negatively affected the severity of depressive symptoms, anxiety, and suicidality. Moreover, the severity of mental health issues negatively affected daily activities. Reduced engagement in daily activities was associated with increased severity of depressive symptoms, anxiety, and suicidality, which, in turn, decreased activity levels. In addition, poor mental health was linked to the subsequent worsening of mental health and further decline in critical daily activities. Previous cross-sectional studies have identified a significant negative correlation between daily activities, depression, and anxiety (45–48). A nationwide survey in South Korea found that individuals with severely restricted daily activities had more than twice the risk of depression than those with unchanged or slightly restricted activities (46). Studies before the COVID-19 pandemic demonstrated that restricted daily activities predicted suicidal ideation in women (49), whereas participation in productive activities reduced suicidal ideation in older women (50).
Additional analyses were conducted to explore the impact of specific activities on mental health. Sleep and physical and social activities exhibited a good model fit and significant reciprocal paths toward depressive symptoms. Poor sleep quality was correlated with greater depressive symptoms and continued poor sleep quality in subsequent assessments. Similarly, depression affected sleep quality and led to further depressive symptoms. This finding aligns with the findings of prior studies. To be specific, participants exhibiting poor sleep quality reported elevated levels of anxiety and depression (51, 52). Similarly, lower physical activity predicted depressive symptoms, and greater depressive symptoms predicted lower physical activity. Social activities and depression exhibited negative cross-lagged effects, with reduced social activities predicting subsequent depression, and vice versa. This aligns with previous research demonstrating the influence of social network size on depressive symptoms over four waves during COVID-19, where smaller social networks were linked to greater loneliness, which in turn predicted higher depression and further reductions in social network size (53).
The CLPM results for anxiety and daily activities exhibited a good fit. Higher levels of anxiety were associated with poorer sleep and diet quality and decreased physical activity. However, sleep quality, diet, and physical activity did not significantly impact the severity of anxiety. Similarly, previous studies have identified a significant negative correlation between sleep quality and anxiety (54). Social activities and anxiety exhibited significant autoregressive and cross-lagged effects over the seven-month study period. Low social activities contributed to higher anxiety, and higher anxiety predicted fewer social activities. Similarly, a previous study demonstrated that low social activities were linked to greater anxiety during the COVID-19 quarantine (55).
In the suicidality model, satisfactory fit indices to identify the reciprocal effects between daily activities and suicidality were not achieved. Only social activities exhibited significant cross-lagged paths toward suicidality. Previous studies have shown that decreased social networks and relationships, along with loneliness and living in solitude, are strongly associated with suicidal ideation and behavior (30, 56). Prolonged social distancing exacerbates these risks, with loneliness being a long-term risk factor (57).
We explored the differences in daily activities and found that women were more likely to engage in social activities than men. In an analysis of gender differences across 59 countries, a previous study found that women were more inclined to seek emotional support as a coping mechanism compared to men during the COVID-19 pandemic (58). The current study also found that lower income and educational status were correlated with higher depression symptoms, whereas only income was correlated with anxiety. None of the demographic variables were significantly correlated with suicidality in our models. Previous studies have linked socioeconomic status, including education, income, and occupational skills, to major depressive disorder (59).
Our findings confirm the reciprocal relationship between daily activities and mental health, where disruptions in daily activities—often indicated as signs of functional impairment in diagnostic criteria for mental disorders—can either worsen or mitigate mental health issues. Behavioral Activation (BA), an intervention that emphasizes monitoring and increasing engagement in important activities, has been shown to enhance this relationship (60). According to a meta-analysis, BA outperformed inactive controls in improving depression with a large effect size, anxiety with a small effect size, and increasing activation with a moderate effect size (61).
The reciprocal relationship between daily activities and mental health has been explored before the COVID-19 era (62–64). The present study corroborates the relationship between daily activities and mental health persisted even through the pandemic’s changing circumstances. The findings of previous studies examining the association between daily activities and mental health are consistent with our results, supporting the robustness of this relationship across different contexts. However, the effects of restrictions on daily activities during the pandemic and their potential impacts in the post-pandemic period require further investigation.
This study had several advantages over previous studies. First, it used a large, stratified sample and achieved greater representativeness. While many prior studies predominantly focused on older adults, this study encompassed participants from a wide range of age groups. Furthermore, our research provides a more detailed understanding of how daily activities impact mental states across diverse populations by controlling demographic variables such as age, gender, income, and educational status. This methodological rigor goes beyond cross-sectional studies to further elucidate complex reciprocal relationships between daily activities and mental health (65). Examining both the overall activities and each specific activity, these results are expected to stimulate future research about the relationship between activities and mental health.
Beyond analyzing overall daily activities, identifying populations with reduced activity levels at an early stage and the following changes in mental health emphasize the importance of the development and application of early interventions. This study explored the impact of specific activities on mental health, providing valuable insights into which activities are beneficial for various demographic groups. This information can be used to provide tailored behavioral strategies in clinical settings.
However, this study had several limitations. First, it relied on self-reported data on daily activities and mental states. In future research, various methods such as ecological momentary assessments can be used. Second, we investigated the relationship between daily activities and mental health for 7 months. Future research should explore the sustained negative impacts in the post-pandemic era. Finally, our results should be replicated with a larger sample size. Although physical and learning activities did not show significant paths in this study, previous research has indicated their impact on mental health during the pandemic (66).
Conclusion
Maintaining a balanced level of core daily activities is crucial for maintaining mental health. Tailored behavioral activation interventions for individual types of activities may be beneficial. Activities should be promoted equitably by considering differences in core activities based on demographic factors.
Data availability statement
The datasets presented in this article are not readily available because the data set belongs to the Korea University SMI laboratory and is accessible to relevant researchers. Requests to access the datasets should be directed to Juhee Choi, Y2poZWUwMTEyQGdtYWlsLmNvbQ==.
Ethics statement
The studies involving humans were approved by Institutional Review Board of Korea University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
JC: Data curation, Formal analysis, Investigation, Methodology, Visualization, Writing – original draft, Writing – review & editing. GS: Data curation, Formal analysis, Methodology, Visualization, Writing – original draft, Writing – review & editing. K-HC: Data curation, Funding acquisition, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by a grant from the National Research Foundation of Korea (grant number NRF-2023S1A5C2A0709598711).
Acknowledgments
We would like to thank Editage (www.editage.co.kr) for English-language editing.
Conflict of interest
The authors declare that the research was conducted without any commercial or financial affiliations that could be interpreted as potential conflicts of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1459300/full#supplementary-material
References
1. Organization WH (2020). Mental health and psychosocial considerations during the COVID-19 outbreak, 18 march 2020: World Health Organization. 1. Available at: https://iris.who.int/bitstream/handle/10665/331490/WHO-2019-nCoV-MentalHealth-2020.1-eng.pdf. (Accessed June 20, 2024).
2. Dong, E, Du, H, and Gardner, L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. (2020) 20:533–4. doi: 10.1016/S1473-3099(20)30120-1
3. Marroquin, B, Vine, V, and Morgan, R. Mental health during the COVID-19 pandemic: effects of stay-at-home policies, social distancing behavior, and social resources. Psychiatry Res. (2020) 293:113419. doi: 10.1016/j.psychres.2020.113419
4. Brooks, SK, Webster, RK, Smith, LE, Woodland, L, Wessely, S, Greenberg, N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. doi: 10.1016/S0140-6736(20)30460-8
5. de Oliveira, AK, Nogueira Alves, IG, de Queiroz, RS, de Castro, MR, Gomes, VA, Santos Fontoura, FC, et al. A systematic review on physical function, activities of daily living and health-related quality of life in COVID-19 survivors. Chronic Illn. (2023) 19:279–303. doi: 10.1177/17423953221089309
6. Rubio-Tomas, T, Skouroliakou, M, and Ntountaniotis, D. Lockdown due to COVID-19 and its consequences on diet, physical activity, lifestyle, and other aspects of daily life worldwide: a narrative review. Int J Environ Res Public Health. (2022) 19:6832. doi: 10.3390/ijerph19116832
7. Cho, S, Park, K, Jung, D, Son, G, Cho, E, and Choi, KH. Development and validation of the core life activities scale. Front Psychol. (2024) 15:1359276. doi: 10.3389/fpsyg.2024.1359276
8. Cruyt, E, De Vriendt, P, De Letter, M, Vlerick, P, Calders, P, De Pauw, R, et al. Meaningful activities during COVID-19 lockdown and association with mental health in Belgian adults. BMC Public Health. (2021) 21:622. doi: 10.1186/s12889-021-10673-4
9. Hamer, M, O'Donovan, G, and Stamatakis, E. Lifestyle risk factors, obesity and infectious disease mortality in the general population: linkage study of 97,844 adults from England and Scotland. Prev Med. (2019) 123:65–70. doi: 10.1016/j.ypmed.2019.03.002
10. Arden, J. The brain bible: How to stay vital, productive, and happy for a lifetime. New York, NY, USA: McGraw-Hill Education. (2014).
11. Jahrami, H, BaHammam, AS, Bragazzi, NL, Saif, Z, Faris, M, and Vitiello, MV. Sleep problems during the COVID-19 pandemic by population: a systematic review and meta-analysis. J Clin Sleep Med. (2021) 17:299–313. doi: 10.5664/jcsm.8930
12. Souza, TC, Oliveira, LA, Daniel, MM, Ferreira, LG, Della Lucia, CM, Liboredo, JC, et al. Lifestyle and eating habits before and during COVID-19 quarantine in Brazil. Public Health Nutr. (2022) 25:65–75. doi: 10.1017/S136898002100255X
13. Bennett, G, Young, E, Butler, I, and Coe, S. The impact of lockdown during the COVID-19 outbreak on dietary habits in various population groups: a scoping review. Front Nutr. (2021) 8:626432. doi: 10.3389/fnut.2021.626432
14. Lopez-Valenciano, A, Suarez-Iglesias, D, Sanchez-Lastra, MA, and Ayan, C. Impact of COVID-19 pandemic on university Students' physical activity levels: An early systematic review. Front Psychol. (2020) 11:624567. doi: 10.3389/fpsyg.2020.624567
15. Stockwell, S, Trott, M, Tully, M, Shin, J, Barnett, Y, Butler, L, et al. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: a systematic review. BMJ Open Sport Exerc Med. (2021) 7:e000960. doi: 10.1136/bmjsem-2020-000960
16. Donnelly, R, and Patrinos, HA. Learning loss during Covid-19: An early systematic review. Prospects (Paris). (2022) 51:601–9. doi: 10.1007/s11125-021-09582-6
17. Puccinelli, PJ, da Costa, TS, Seffrin, A, de Lira, CAB, Vancini, RL, Nikolaidis, PT, et al. Reduced level of physical activity during COVID-19 pandemic is associated with depression and anxiety levels: an internet-based survey. BMC Public Health. (2021) 21:425. doi: 10.1186/s12889-021-10470-z
18. Liu, H, Tao, TJ, Chan, SKY, Ma, JCH, Lau, AYT, Yeung, ETF, et al. Daily routine disruptions and psychiatric symptoms amid COVID-19: a systematic review and meta-analysis of data from 0.9 million individuals in 32 countries. BMC Med. (2024) 22:49. doi: 10.1186/s12916-024-03253-x
19. American Psychiatric Association DSM Task Force. Diagnostic and statistical manual of mental disorders: DSM-5. Washington, DC: American Psychiatric Association (2013). 947 p.
20. Cox, RC, and Olatunji, BO. Sleep in the anxiety-related disorders: a meta-analysis of subjective and objective research. Sleep Med Rev. (2020) 51:101282. doi: 10.1016/j.smrv.2020.101282
21. Alvaro, PK, Roberts, RM, and Harris, JK. A systematic review assessing Bidirectionality between sleep disturbances, anxiety, and depression. Sleep. (2013) 36:1059–68. doi: 10.5665/sleep.2810
22. Ingram, J, Maciejewski, G, and Hand, CJ. Changes in diet, sleep, and physical activity are associated with differences in negative mood during COVID-19 lockdown. Front Psychol. (2020) 11:588604. doi: 10.3389/fpsyg.2020.588604
23. Harris, LM, Huang, X, Linthicum, KP, Bryen, CP, and Ribeiro, JD. Sleep disturbances as risk factors for suicidal thoughts and behaviours: a meta-analysis of longitudinal studies. Sci Rep. (2020) 10:13888. doi: 10.1038/s41598-020-70866-6
24. Pigeon, WR, Pinquart, M, and Conner, K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J Clin Psychiatry. (2012) 73:e1160–7. doi: 10.4088/JCP.11r07586
25. Li, Y, Zhang, J, and McKeown, RE. Cross-sectional assessment of diet quality in individuals with a lifetime history of attempted suicide. Psychiatry Res. (2009) 165:111–9. doi: 10.1016/j.psychres.2007.09.004
26. Coughenour, C, Gakh, M, Pharr, JR, Bungum, T, and Jalene, S. Changes in depression and physical activity among college students on a diverse campus after a COVID-19 stay-at-home order. J Community Health. (2021) 46:758–66. doi: 10.1007/s10900-020-00918-5
27. Benke, C, Autenrieth, LK, Asselmann, E, and Pane-Farre, CA. Lockdown, quarantine measures, and social distancing: associations with depression, anxiety and distress at the beginning of the COVID-19 pandemic among adults from Germany. Psychiatry Res. (2020) 293:113462. doi: 10.1016/j.psychres.2020.113462
28. Jiang, L, Cao, Y, Ni, S, Chen, X, Shen, M, Lv, H, et al. Association of Sedentary Behavior with Anxiety, depression, and suicide ideation in college students. Front Psychol. (2020) 11:566098. doi: 10.3389/fpsyt.2020.566098
29. Uddin, R, Burton, NW, Maple, M, Khan, SR, Tremblay, MS, and Khan, A. Low physical activity and high sedentary behaviour are associated with adolescents' suicidal vulnerability: evidence from 52 low- and middle-income countries. Acta Paediatr. (2020) 109:1252–9. doi: 10.1111/apa.15079
30. Calati, R, Ferrari, C, Brittner, M, Oasi, O, Olie, E, Carvalho, AF, et al. Suicidal thoughts and behaviors and social isolation: a narrative review of the literature. J Affect Disord. (2019) 245:653–67. doi: 10.1016/j.jad.2018.11.022
31. Jin, Y, Sun, T, Zheng, P, and An, J. Mass quarantine and mental health during COVID-19: a meta-analysis. J Affect Disord. (2021) 295:1335–46. doi: 10.1016/j.jad.2021.08.067
32. Xu, H, Qin, L, Wang, J, Zhou, L, Luo, D, Hu, M, et al. A cross-sectional study on risk factors and their interactions with suicidal ideation among the elderly in rural communities of Hunan, China. BMJ Open. (2016) 6:e010914. doi: 10.1136/bmjopen-2015-010914
33. McCoy, DC, Roy, AL, and Sirkman, GM. Neighborhood crime and school climate as predictors of elementary school academic quality: a cross-lagged panel analysis. Am J Community Psychol. (2013) 52:128–40. doi: 10.1007/s10464-013-9583-5
34. Kim, SH, Park, K, Yoon, S, Choi, Y, Lee, SH, and Choi, KH. A brief online and offline (paper-and-pencil) screening tool for generalized anxiety disorder: the final phase in the development and validation of the mental health screening tool for anxiety disorders (MHS: a). Front Psychol. (2021) 12:639366. doi: 10.3389/fpsyg.2021.639366
35. Park, K, Yoon, S, Cho, S, Choi, Y, Lee, SH, and Choi, KH. Final validation of the mental health screening tool for depressive disorders: a brief online and offline screening tool for major depressive disorder. Front Psychol. (2022) 13:992068. doi: 10.3389/fpsyg.2022.992068
36. Yoon, S, Park, K, and Choi, KH. The ultra brief checklist for suicidality. J Affect Disord. (2020) 276:279–86. doi: 10.1016/j.jad.2020.07.037
37. Cheung, GW, and Rensvold, RB. Evaluating goodness-of-fit indexes for testing measurement invariance. Struct Equ Model Multidiscip J. (2002) 9:233–55. doi: 10.1207/s15328007sem0902_5
38. Lt, H, and Bentler, PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model Multidiscip J. (1999) 6:1–55. doi: 10.1080/10705519909540118
39. Seddig, DLH. Approximate measurement invariance and longitudinal confirmatory factor analysis: concept and application with panel data. Surv Res Methods. (2018). doi: 10.18148/srm/2018.v12i1.7210
40. Byrne, BM, and van de Vijver, FJR. The maximum likelihood alignment approach to testing for approximate measurement invariance: a paradigmatic cross-cultural application. Psicothema. (2017) 4:539–51. doi: 10.7334/psicothema2017.178
42. Kenny, DA. Cross-lagged panel correlation: a test for spuriousness. Psychol Bull. (1975) 82:887–903. doi: 10.1037/0033-2909.82.6.887
43. RJA L. A test of missing completely at random for multivariate data with missing values. J Am Stat Assoc. (1988) 83:1198–202. doi: 10.1080/01621459.1988.10478722
44. RJA L. Regression with missing X’s: a review. J Am Stat Assoc. (1992) 87:1227–37. doi: 10.1080/01621459.1992.10476282
45. Bozo, O, Toksabay, NE, and Kurum, O. Activities of daily living, depression, and social support among elderly Turkish people. Aust J Psychol. (2009) 143:193–206. doi: 10.3200/JRLP.143.2.193-206
46. Cho, S, Ju, HR, Oh, H, Choi, ES, and Lee, JA. The association between the restriction of daily life and depression during the COVID-19 pandemic in Korea: a nationwide based survey. Sci Rep. (2022) 12:17722. doi: 10.1038/s41598-022-21301-5
47. Steger, MF, and Kashdan, TB. Depression and everyday social activity, belonging, and well-being. J Couns Psychol. (2009) 56:289–300. doi: 10.1037/a0015416
48. Dİ, TB, Ünal, N, Güngör, S, and Tosun, N. Investigation of activities of daily living and hospital anxiety and depression levels of COVID-19 patients: a descriptive study. Cyprus Turk J Psychiatry Psychol. (2022) 4:171–9. doi: 10.35365/ctjpp.22.2.07
49. Choi, SB, Lee, W, Yoon, JH, Won, JU, and Kim, DW. Risk factors of suicide attempt among people with suicidal ideation in South Korea: a cross-sectional study. BMC Public Health. (2017) 17:579. doi: 10.1186/s12889-017-4491-5
50. Choi, J-Y. Engagement in productive activities and suicidal ideation among female older adults in South Korea. Cogent. Psychology. (2023) 10:7179. doi: 10.1080/23311908.2023.2187179
51. Alkhatatbeh, MJ, Abdul-Razzak, KK, and Khwaileh, HN. Poor sleep quality among young adults: the role of anxiety, depression, musculoskeletal pain, and low dietary calcium intake. Perspect Psychiatr Care. (2021) 57:117–28. doi: 10.1111/ppc.12533
52. Becker, NB, Jesus, SN, Joao, K, Viseu, JN, and Martins, RIS. Depression and sleep quality in older adults: a meta-analysis. Psychol Health Med. (2017) 22:889–95. doi: 10.1080/13548506.2016.1274042
53. Domenech-Abella, J, Mundo, J, Switsers, L, van Tilburg, T, Fernandez, D, and Aznar-Lou, I. Social network size, loneliness, physical functioning and depressive symptoms among older adults: examining reciprocal associations in four waves of the longitudinal aging study Amsterdam (LASA). Int J Geriatr Psychiatry. (2021) 36:1541–9. doi: 10.1002/gps.5560
54. Yang, J, Fu, X, Liao, X, and Li, Y. Association of problematic smartphone use with poor sleep quality, depression, and anxiety: a systematic review and meta-analysis. Psychiatry Res. (2020) 284:112686. doi: 10.1016/j.psychres.2019.112686
55. Luo, H, Luo, D, Tang, Q, Niu, Z, Xu, J, and Li, J. The combined impact of social networks and connectedness on anxiety, stress, and depression during COVID-19 quarantine: a retrospective observational study. Front Public Health. (2023) 11:1298693. doi: 10.3389/fpubh.2023.1298693
56. Gabarrell-Pascuet, A, Felez-Nobrega, M, Cristobal-Narvaez, P, Mortier, P, Vilagut, G, Olaya, B, et al. The role of social support, detachment, and depressive and anxiety symptoms in suicidal thoughts and behaviours during the Covid-19 lockdown: potential pathways. Curr Psychol. (2023) 42:9237–48. doi: 10.1007/s12144-021-02205-5
57. Antonelli-Salgado, T, Monteiro, GMC, Marcon, G, Roza, TH, Zimerman, A, Hoffmann, MS, et al. Loneliness, but not social distancing, is associated with the incidence of suicidal ideation during the COVID-19 outbreak: a longitudinal study. J Affect Disord. (2021) 290:52–60. doi: 10.1016/j.jad.2021.04.044
58. Kolakowsky-Hayner, SA, Goldin, Y, Kingsley, K, Alzueta, E, Arango-Lasprilla, JC, Perrin, PB, et al. Psychosocial impacts of the COVID-19 quarantine: a study of gender differences in 59 countries. Medicina (Kaunas). (2021) 57:789. doi: 10.3390/medicina57080789
59. Domenech-Abella, J, Mundo, J, Leonardi, M, Chatterji, S, Tobiasz-Adamczyk, B, Koskinen, S, et al. The association between socioeconomic status and depression among older adults in Finland, Poland and Spain: a comparative cross-sectional study of distinct measures and pathways. J Affect Disord. (2018) 241:311–8. doi: 10.1016/j.jad.2018.08.077
60. Cuijpers, P, van Straten, A, and Warmerdam, L. Behavioral activation treatments of depression: a meta-analysis. Clin Psychol Rev. (2007) 27:318–26. doi: 10.1016/j.cpr.2006.11.001
61. Stein, AT, Carl, E, Cuijpers, P, Karyotaki, E, and Smits, JAJ. Looking beyond depression: a meta-analysis of the effect of behavioral activation on depression, anxiety, and activation. Psychol Med. (2021) 51:1491–504. doi: 10.1017/S0033291720000239
62. Sato, A, Eguchi, E, Hayashi, F, Funakubo, N, Okada, T, Kiyama, M, et al. A prospective study of the association between lifestyle and the risk of depressive symptoms. J Affect Disord. (2025) 376:269–79. doi: 10.1016/j.jad.2025.01.040
63. Fossati, C, Torre, G, Vasta, S, Giombini, A, Quaranta, F, Papalia, R, et al. Physical exercise and mental health: the routes of a reciprocal relation. Int J Environ Res Public Health. (2021) 18:2364. doi: 10.3390/ijerph182312364
64. Morbee, S, Beeckman, M, Loeys, T, Waterschoot, J, Cardon, G, Haerens, L, et al. An examination of the reciprocal associations between physical activity and anxiety, depressive symptoms, and sleep quality during the first 9 weeks of the COVID-19 pandemic in Belgium. Ment Health Phys Act. (2023) 24:100500. doi: 10.1016/j.mhpa.2022.100500
65. Efstathiou, V, Stefanou, MI, Siafakas, N, Makris, M, Tsivgoulis, G, Zoumpourlis, V, et al. Suicidality and COVID-19: suicidal ideation, suicidal behaviors and completed suicides amidst the COVID-19 pandemic (review). Exp Ther Med. (2022) 23:107. doi: 10.3892/etm.2021.11030
Keywords: depressive symptoms, anxiety, suicidality, daily activities, cross-lagged panel model, longitudinal, COVID-19
Citation: Choi J, Son G and Choi K-H (2025) Longitudinal relationships between daily activities, depressive symptoms, anxiety, and suicidality during the COVID-19 pandemic: a three-wave cross-lagged study. Front. Public Health. 13:1459300. doi: 10.3389/fpubh.2025.1459300
Edited by:
Feten Fekih-Romdhane, Tunis El Manar University, TunisiaReviewed by:
William Sulis, McMaster University, CanadaGabriela Fernández-Theoduloz, Universidad de la República, Uruguay
Copyright © 2025 Choi, Son and Choi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kee-Hong Choi, a2Nob2kxQGtvcmVhLmFjLmty
 Juhee Choi
Juhee Choi Gaeun Son
Gaeun Son Kee-Hong Choi
Kee-Hong Choi