
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 10 February 2025
Sec. Occupational Health and Safety
Volume 13 - 2025 | https://doi.org/10.3389/fpubh.2025.1416609
This article is part of the Research Topic The Interplay of Stress, Health, and Well-being: Unraveling the Psychological and Physiological Processes - Volume II View all 35 articles
Background: Work-related complaints are often caused by stress and increased mental strain. Support from your immediate boss and colleagues is crucial to buffer against the negative health effects of the psychosocial working environment.
Aim: The aim of this study was to investigate if support from the immediate boss and colleagues was associated with biological stress levels, unsafety at work, and other work-related conditions.
Methods: Data derives from a subsample of the SCAPIS study, a major Swedish prospective population-based study. In this subsample, a total of N = 5 058 middle-aged persons (50-64 years) from the general population participated; of these, 68.4% (N = 3 462 individuals) provided hair samples. Questionnaires included socio-demographic and self-reports of occupation, stress, and health status. The demand and control questionnaires were used. A biomarker of long-term stress, hair cortisol concentrations (HCC), was also applied.
Results: In this studied cohort, 9.1 % reported a lack of support from their immediate boss, while 90.9% reported that they did get support at work. Significantly more women (p < 0.001) reported non-support. Those with support or not did not differ in terms of age, education, civil status, smoking, or ethnicity. Those with non-support reported a higher extent (p < 0.001) of lower perceived health. The risk for hypertension and high cholesterol was increased by 28 %, respectively, 13 % being in the non-support group. The main findings were associations between lack of support and feelings of unsafety at work (p < 0.001), higher long-term cortisol levels (p < 0.009), lack of support from colleagues (p < 0.001), and feelings of dejected/sad (p < 0.001) and high work pace (p = 0.03).
Conclusion: Individuals who did not have the necessary support from their immediate boss and colleagues reported they felt more insecure at work and had higher biological long-term stress. In workplace health promotion, an awareness of the link between social support at work and health could be an important component.
An unhealthy psychosocial work environment can be defined as a job in which the work atmosphere, the colleagues and leadership at work, or a combination of these might negatively affect an employee's health. A poor work environment can lead to serious consequences, especially in the form of chronic stress. Various physical and mental factors can cause chronic stress at work. Chronic stress could have negative effects on many health aspects, like cardiovascular diseases and mental illness (1–4). Chronic stress is also a general risk factor for mental health and well-being in the working population (5, 6). However, one could also consider that a workplace is not necessarily just a source of stress; it could also create a salutogenetic and healthy environment, which would benefit the employees' health (7, 8).
One of the most influential and widely used models in studies on the health effects of psychosocial working conditions and occupational stress is the job-strain or Job-Demand-Control model, initially introduced by Karasek and Theorell (9–11). This model is separated into three aspects regarding workplace qualities: demand, control, and support. The hypothesis behind this model is that work with high demands in combination with high control gives an average strain level and jobs with low demands and low control. The workers suffering from high strain with adverse psychological reactions, such as anxiety and depression, are associated with high demands and low control. High demands, low control, and low support are separate risk factors for anxiety and depression; however, the correlation is even stronger if they are combined (12). Almost all Job Demand-Control model-related studies have principally focused on the combinations of job demands, job control, and social support (12). Another approach to analyze the psychosocial working conditions is the effort-reward model, which has shown adverse health effects yielding high efforts but low rewards (13).
Psychosocial work stress as a potential risk factor for coronary heart disease has been debated. Some researchers have found a causal association, while others found the effect on specific health conditions either negligible or confounded. A major review of evidence from 27 cohort studies in Europe, the USA, and Japan based on data from over 600,000 men and women, suggests that work stressors, such as job strain, are associated with a moderately elevated risk of incident coronary heart disease and stroke. The excess risk for exposed individuals was up to 40% compared to those without such stressors (14). Other studies suggest that job strain could be associated with a consistently increased risk of an incident event of cardiovascular heart disease. Adjustment for conventional risk factors and lifestyle factors together with age, sex, and socioeconomic status, did not substantially change the strength of this association. Prevention of workplace stress can reduce the incidence of cardiovascular diseases, but a more powerful preventive effect is to reduce standard cardiovascular risk factors like smoking (15).
The fear and anxiety of an individual losing their job is another individual stressor (16). Compared to actual job loss, job insecurity is the perception of the employee that his/her job is at risk and could result in employees losing their ability to cope with workplace challenges and threats.
Studies of intermediary pathways from psychosocial job conditions to biomarkers are scarce. Hypertension and high cholesterol are the most investigated cardiovascular risk factors, but the potential associations between psychosocial job conditions and biomarkers of long-term stress are not so well investigated (6).
Social support from jobmates and support from immediate bosses at the workplace are important psychosocial factors in working life. However, the relative impact on health from support at work of the immediate boss has not been extensively studied. Could this type of support at work impact biologically measured stress levels expressed as hair cortisol concentrations (HCC) and perceived stress, and further, if this also affects feelings of unsafety and sadness at work?
The study aimed to investigate if a lack of support from the immediate boss and colleagues at the workplace is associated with increased biological and perceived stress levels and feelings of unsafety at work and other adverse working conditions for middle-aged people.
Data in the present study constitute a subsample from The Swedish Cardio Pulmonary BioImage Study (SCAPIS). This major prospective national observational study with a randomly selected sample of middle-aged persons (50–64 years) from the general population in Sweden (17–19). The study participants in SCAPIS were recruited from six Swedish university hospitals, and at one of these sites (the Linköping site), additional data collection was initiated, focusing on measuring hair cortisol concentrations (HCC). The total sample at this site was N = 5 058 participants; of these, N = 3 462 individuals provided hair samples, which were included in this report. Hair samples and thereby also cortisol measurements were unobtainable in 31.5% (N = 1 596), mainly due to short hair length. Only a few participants with sufficient hair length were hesitant to provide hair samples. All hair samples were analyzed at the research laboratory of Clinical Chemistry at The University Hospital in Linköping, Sweden.
The questionnaire includes a comprehensive set of data covering social factors, lifestyle and psychosocial factors. Socioeconomic status was based on educational level and divided into low, medium, and high; smoking was divided into yes, now, or earlier and no. Age was divided into three age groups based on age at study inclusion: 50–54, 55–59, and 60–65. In this studied sample 94.4 % were Swedish and the non-Swedish attendees these were categorized as Nordic, European, or outside Europe. Marital status was divided into single, married/cohabited. The question of economic problems was divided into yes now or earlier and no. A question about self-reported stress was divided into a 2-grade scale of never stressed and quiet or constantly stressed now and the last 5 years. Self-reported health was derived from the SF-36 scale and was dichotomized into good or bad health, and a question about self-reported sleeping habits was also asked. Reports of diagnosed hypertension and elevated plasma cholesterol concentrations were based on self-reports and dichotomized into yes or no. The feeling of dejection was dichotomized into often now or earlier and no. Questions about feeling unsafe at work and forced to change work were divided into yes now or earlier and no. Questions about demand-control-support derived from The Job Demand-Control (JDC) or job-strain models (9, 10).
Hair cortisol was extracted and analyzed through a competitive radioimmunoassay (RIA). The hair samples were cut into small pieces. Each sample was put into a 2 mL QiaGenRB sample tube with a 0.5 mm QuiGen stainless steel bead. All samples from the SCAPIS study (4) were analyzed using the same reagents and calibrators to minimize the risk of between-assay bias influencing the study's conclusions. Hair samples over 5–10 mg were required to maintain a total inter-assay coefficient of variation below 8% for hair extraction and measurement of cortisol by the radioimmunoassay. The method is fully described elsewhere (20).
The study population was described using Chi-square and ANOVA tests to analyze discrepancies between groups, expressed as median and percentage. Categorical measures are reported as counts and percentages. HCC values and the distribution of HCC were described by median cortisol values and interquartile range (IQR). Hair cortisol was analyzed as an indicator of biological stress where the median is reported. Tests of normality were made with Shapiro-Wilk tests. This showed a non-normal distribution of HCC with a long right-hand tail in the distribution, which is why median and IQR were used. The odds ratio and 95% CI were used as risk estimates.
To correct for potential confounding factors or mediating effects, a multivariate regression analysis based on created models with support from the immediate boss as the dependent variable was performed. Three regression models were made to analyze factors associated with support at work from the immediate boss. Model I (basic model) included only demographic characteristics, HCC, and workplace unsafety. Model II included all covariates from Model I plus work-related factors. The final Model III (or fully adjusted model) included all covariates from Model I and Model II plus health-related factors. A p < 0.05 was considered significant in all the analyses. All analyses were performed using SPSS version 28.
Of the participants in this study who were working (N = 2724) 9.1 % reported that they did not get support from their immediate boss, while 90.9% reported that they did get support at work. A fraction of 21.3 % of the participants N = 738 in this study reported that they were presently not working.
Comparisons of those who did not get support vs. those who got support from their immediate boss at work revealed that significantly more women (p < 0.001) reported non-support. Those with support or not did not differ in terms of age, education, civil status, smoking, or ethnicity. However, those with non-support at work reported a higher and significant (p < 0.001) bad health (OR 1.63, 95% CI 1.25–2.13) and everyday stress (p < 0.001). They also had tendencies of increased risk for hypertension, high cholesterol, and inferior sleeping habits being in the non-support group. Significantly higher HCC (p < 0.001) could also be seen among those who reported bad health. Being a citizen born outside Sweden only showed some increase in HCC concentration (see Table 1).
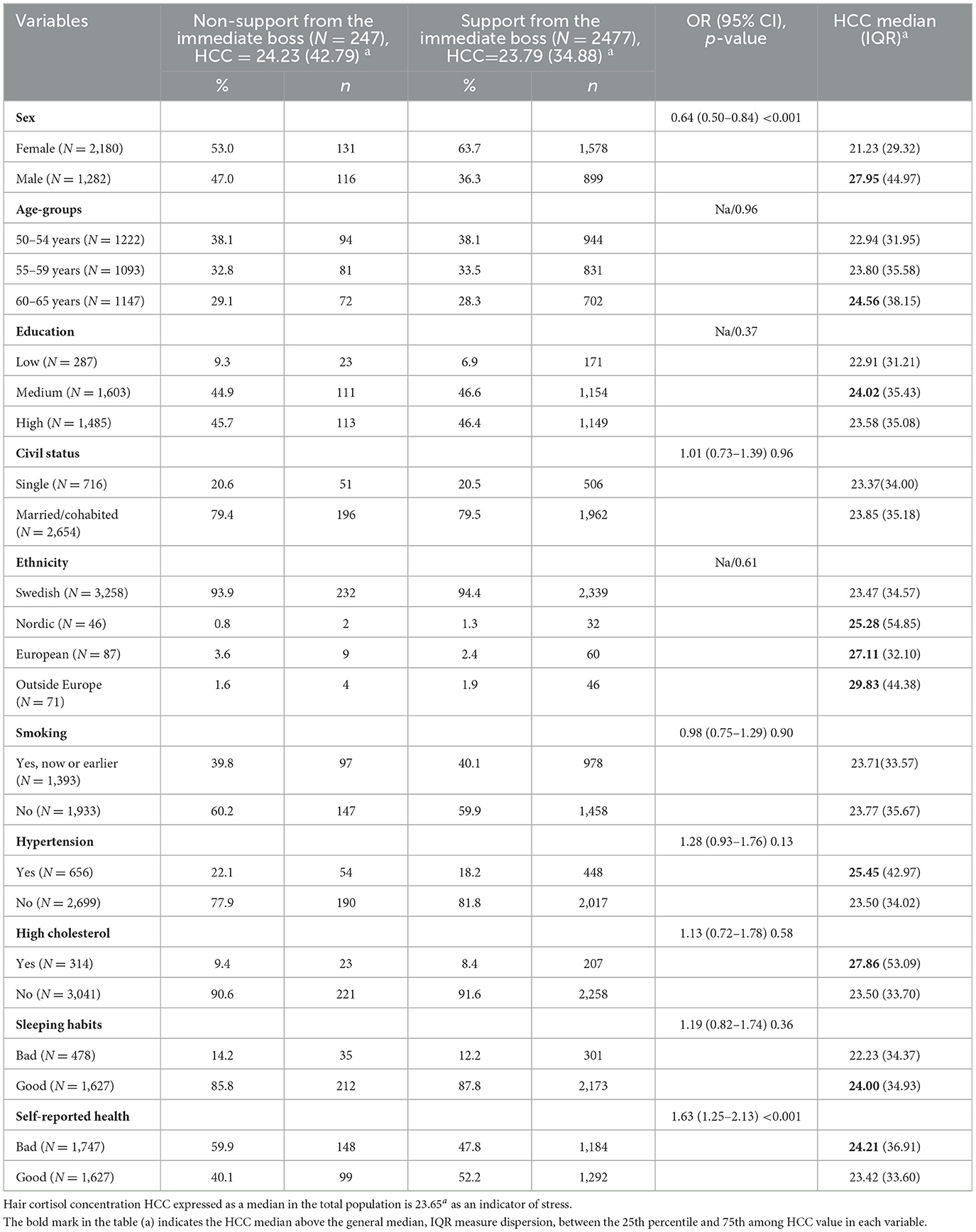
Table 1. Association and odds ratio between non-support and support from the immediate boss at work concerning socio-demographic and health factors (N = 3 462).
There was almost a double risk OR 2.27 (95 % CI 1.65–2.85) of Feeling unsafe at work (39.2% respective 22.9%, p < 0.001) being in the non-support group at work compared to those with support. Significant differences were also seen concerning the non-support group compared with the support group among those which was forced to change their work (24% vs. 17.6%, p = 0.013, OR 1.47, 95% CI 1.08–2.02), those who reported economic problems (10.5% vs. 6.5%, p = 0.02, OR 1.69 (95% CI 1.10–2.61). Non-support and help from colleagues was the strongest indicator for non-support from the immediate boss, 23.8% vs. 1.7%, p < 0.001 (OR 17.60, 95% CI 11.55–26.83). Even if the participants had to work fast often a difference was seen 48.6 % vs. 36.4%, p < 0.001 (OR 1.65, 95% CI 1.27–2.15). Feeling dejected/sad and always stressed also showed significant differences between the two groups p < 0.001 (OR 2.25 95% CI 1.66–3.05) and p < 0.001 (OR: 2.22, 95% CI 1.68–2.95).
HCC was also raised among those unsupported at work, always stressed, and rarely received colleague support and help. Being on long-term sick leave was also associated with a small rise in HCC (see Table 2).
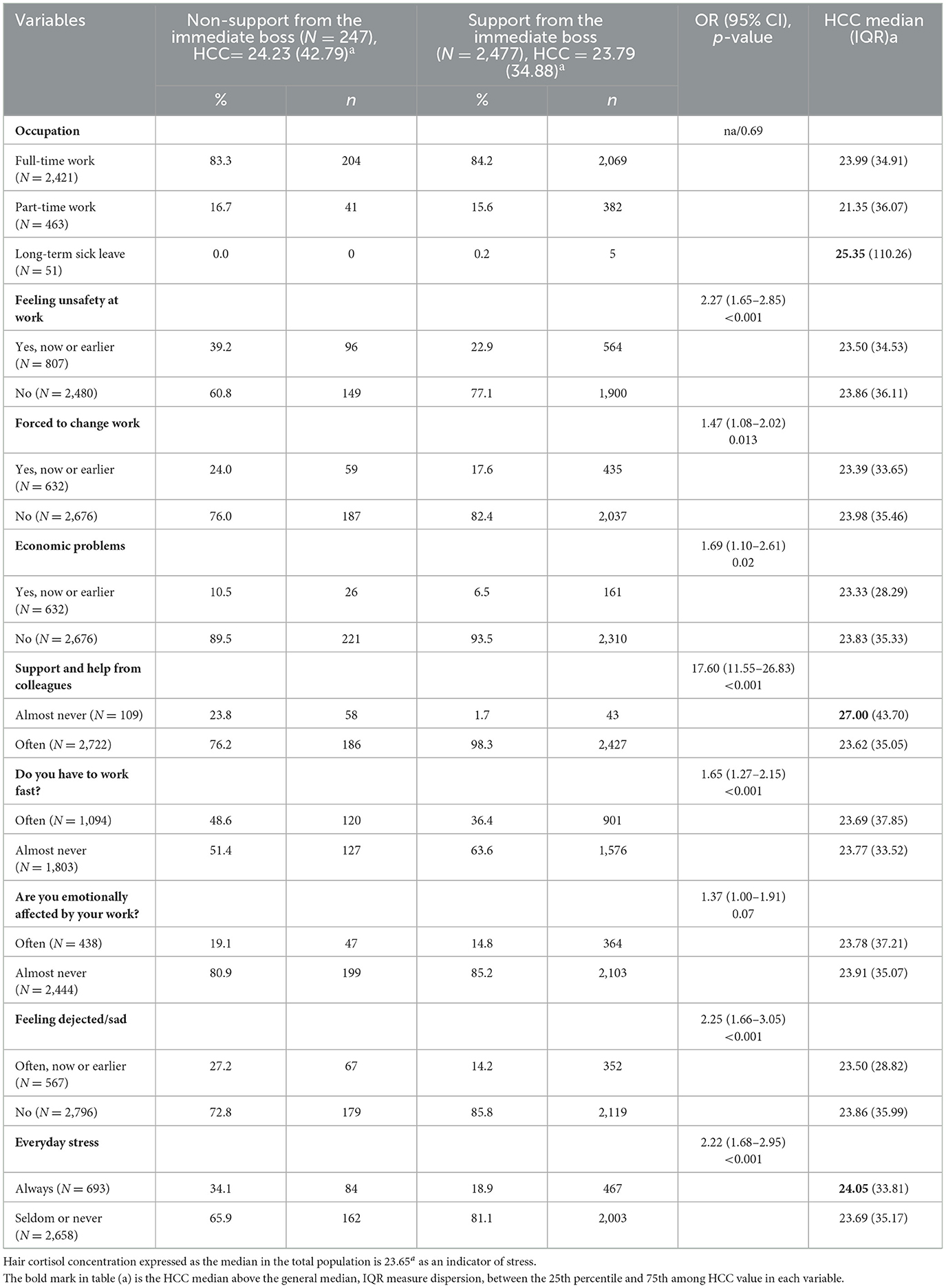
Table 2. Associations between relevant psychosocial work-related factors concerning support at work from immediate boss.
In a set of regression models (see Table 3), demographic, health, and working factors were analyzed as co-variants, with support at work from the immediate bosses as the dependent factor. The variables unsafety at work, HCC, work pace, feeling dejected/sad, sex, and colleague support were independently and significantly associated with non-support from the immediate boss at work.
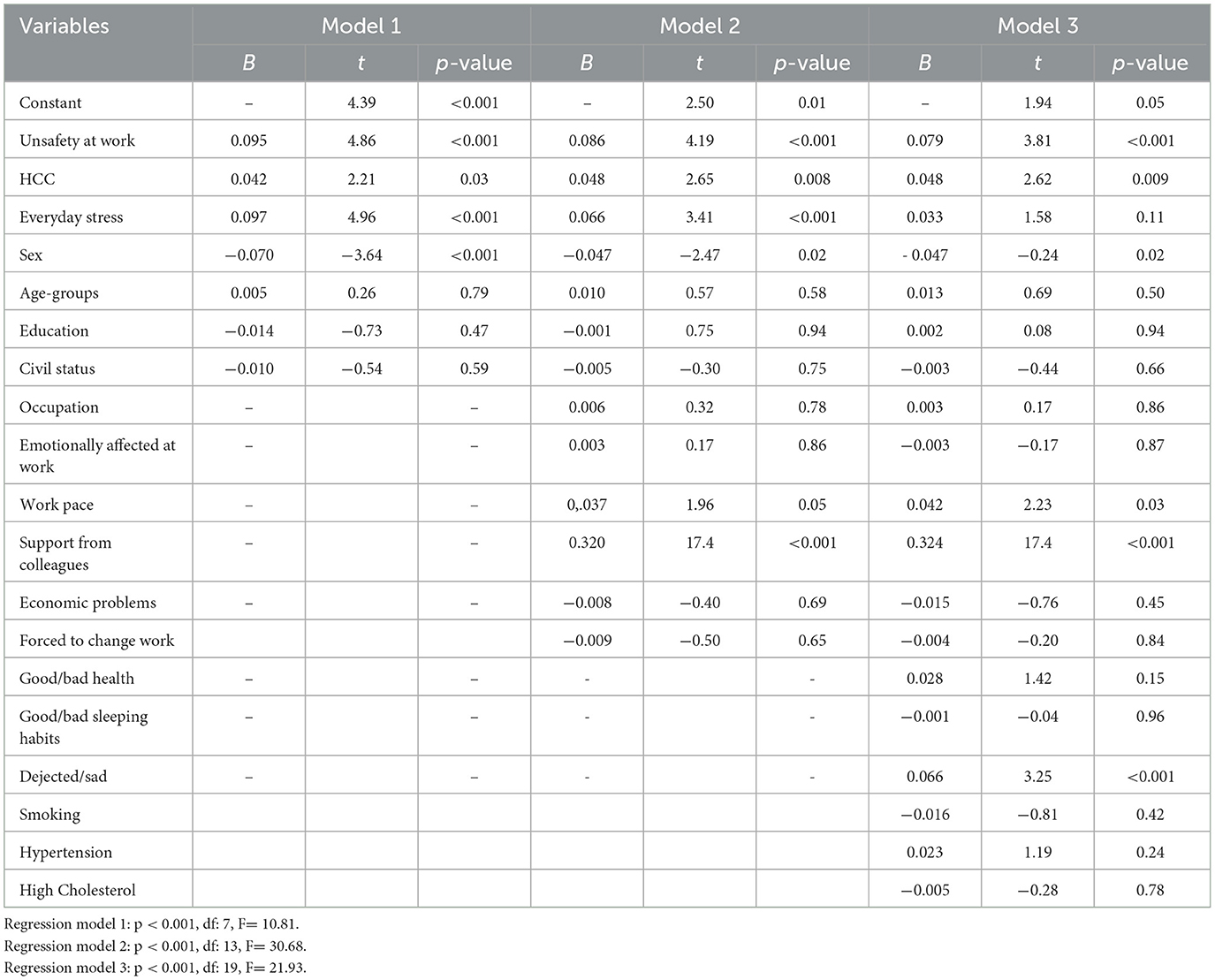
Table 3. Three regression models include demographic, health, and working factors as co-variants with support at work from the immediate bosses, as the dependent variable for the whole study population (N = 3 462).
Different clinical and other measures were analyzed for some defined occupational areas, as shown in Supplementary Table S1. The group “workers” showed higher HCC values and more frequently had hypertension and high cholesterol. A higher percentage of the workers did not get any support from the immediate boss. Individuals in service jobs, police/firefighters/bosses, and the military revealed a higher median HCC than the general median in this study population. Among those who were “academics”, support from the immediate boss was higher than in the general population. Often emotionally affected at work was more frequently seen among health care workers, teachers, and those working in children's care, but even among bosses (see Supplementary Table S1).
Social support is regarded as an important factor for health and one of the main dimensions of the classical Demand–control–support model within the field of occupational health (10). The main results of this study reveal that social support from the immediate boss and colleagues at work seems to be an important factor for a healthy workplace. Non-support at work from the immediate bosses, supervisors, or managers was in the final multivariate analysis associated with feeling unsafe at work (p < 0.001), higher long-term cortisol levels (p < 0.009), lack of support from colleagues (p < 0.001) also feelings of dejected/sad (p < 0.001) and high work pace (p = 0.03), this was more predominant among women (p = 0.02). All these factors are related to the internal working environment and the individual.
The results also point to the role of leadership in organizations. Some previous studies have shown a relationship between managers' leadership behaviors and job satisfaction and the performance of employees (21). Leaders with a positive and supportive attitude might motivate employees with a shared vision and activate their inner skills and identities. On the other hand, it has also been seen that abusive leader behavior has negative health consequences for employees. Disinterest or even aggression from immediate bosses, supervisors, or managers could drain employee energies and weaken their psychological resourcefulness, which might result in work withdrawal (22). Accordingly, abusive leadership also affects employees' engagement, ultimately affecting their proactive behavior at work (23, 24). It also puts extra stress on employees, leading to psychological distress and adversely affecting the workplace environment.
The factor of support from colleagues was in this study also significantly associated with non-support from immediate bosses. This illustrates that these two factors are intertwined in many aspects and reflect a positive work environment where social support as a culture is present in the whole organization.
A perception within the Demand–Control–Support model is that social support could act as a buffer against the negative effects of a high job demand on health. Several studies have evaluated this hypothesis to predict worker health, even though it has given some inconclusive results (25). Nevertheless, social support at work seems to be mediated by social support from supervisors and coworkers in different studies of the association of job control with job strain (25).
In this study, the stress indicator HCC was significantly associated with the factor support at work. However, in a previous large Swedish study it was found that the demand control model was not associated with saliva cortisol concentrations (26). However, that study focused on measuring spot-time saliva cortisol levels. In contrast, in the present study, we measured long-term stress exposure through cortisol levels in hair, reflecting the mean cortisol levels for months.
A major strength of this study is the sample size of middle-aged people and that the participants were randomly selected from the general population. Although the initial purpose of the SCAPIS study was directed toward cardiovascular risk factors, it also included some factors reflecting occupational life. This means that we only have a limited set of relevant factors for measuring psychosocial factors in working life, which gives the analysis some limitations. However, the variables included are well-established and validated.
A general limitation in studies measuring hair cortisol is that individuals with insufficient hair length cannot be included. If insufficient hair length is related to chronic stress, this might be a confounder and impact the results. However, there is no evidence that this might be a confounder in this studied population. A previous analysis of the non-attendees (men without hair samples vs. men with hair samples) in this SCAPIS cohort revealed that they neither differ from the participants concerning socioeconomic background or cardiovascular risk factors (4).” No evidence is at hand that issues and problems in the psychosocial working environment might affect the risk for hair loss.
Ethnicity might be a relevant factor, but in this studied Swedish sample there were relatively few non-Swedish attendees only around 5%. This is mainly explained by the fact that the sample covers older adults in the ages between 50 and 65 years. The Swedish context in this study provides valuable data, but the generalizability of results across contexts in other regions might be limitative. Workplace dynamics may differ significantly in other countries and regions.
Lack of social support from immediate bosses and colleagues is associated with an increased risk of feeling unsafe at work and higher long-term stress, as measured by cortisol in hair. There are also physical effects such as tendencies to higher blood pressure and cholesterol levels, perceived bad health, feelings of dejected/sad, and sleeping problems.
The prevention of psychosocial stressors in the workplace should emphasize improving a culture where social support is a focus between colleagues, staff, and employees for a good work environment. Promoting awareness of the link between social support at work and health is an important component of workplace health promotion. Social support at work could serve as a salutogenic factor in the workplace.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by the Research Protocol and all methods in the study were carried out following relevant guidelines and regulations. The SCAPIS study was approved by the Umeå Ethical Review Board (Dnr 2010-228-31M). All participants gave their written informed consent to participate. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
ÅF: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. ET: Data curation, Methodology, Validation, Writing – original draft, Writing – review & editing. MJ: Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. FI: Conceptualization, Data curation, Writing – original draft, Writing – review & editing. TF: Conceptualization, Formal analysis, Funding acquisition, Methodology, Writing – original draft, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was funded by the Swedish AFA Insurance, Stockholm (Grant number Dnr: 160340).
The authors thank all the participants and staff in the SCAPIS study at the University Hospital in Linköping, Sweden.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1416609/full#supplementary-material
1. Steptoe A, Kivimaki M. Stress and cardiovascular disease: an update on current knowledge. Annu Rev Public Health (2013) 34:337. doi: 10.1146/annurev-publhealth-031912-114452
2. Staufenbiel SM, Penninx BW, Spijker AT, Elzinga BM, van Rossum EF. Hair cortisol, stress exposure, and mental health in humans: a systematic review. Psychoneuroendocrinology. (2013) 38:1220. doi: 10.1016/j.psyneuen.2012.11.015
3. Vinkers CH, Joels M, Milaneschi Y, Kahn RS, Penninx BW, Boks MP. Stress exposure across the life span cumulatively increases depression risk and is moderated by neuroticism. Depress Anxiety (2014) 31:737. doi: 10.1002/da.22262
4. Faresjö, T, Stromberg S, Jones M, Stomby A, Karlsson JE, Ostgren CJ et al. Elevated levels of cortisol in hair precede acute myocardial infarction. Sci Rep. (2020) 10:22456–224 doi: 10.1038/s41598-020-80559-9
5. Goetzel RZ, Roemer EC, Holingue C, Fallin D, McClearly K, Eaton W, et al. Mental health in the workplace: a call to action proceedings from the mental health in the workplace—public health summit. J Occup Environ Med. (2018) 60:322. doi: 10.1097/JOM.0000000000001271
6. Hassard J, Teoh KRH, Visockaite G, Dewe P, Cox T. The cost of work-related stress to society: a systematic review. J Occup Health Psychol. (2018) 23:1. doi: 10.1037/ocp0000069
7. Carolan S, Harris PR, Cavanagh K. Improving employee well-being and effectiveness: systematic review and meta-analysis of webbased psychological interventions delivered in the workplace. J Med Internet Res. (2017) 19:e2 doi: 10.2196/jmir.7583
8. Bhui KS, Dinos S, Stansfeld SA, White PD. A synthesis of the evidence for managing stress at work: a review of the reviews reporting on anxiety, depression, and absenteeism. J Environ Public Health. (2012) 2012:5158 doi: 10.1155/2012/515874
9. Karasek RA. Job demands, job decision latitude, and mental strain: implications for job redesign. Admin Sci Q. (1979) 24:285–308. doi: 10.2307/2392498
10. Karasek R, Thorell T. Healthy Work, Stress, Productivity, and the Reconstruction of Working Life. New York: Basic Books Inc. Publications (1990).
11. Bjarte S, Mykletun A, Dahl A, Moen B, Tell G. Testing the job demand-control-support model with anxiety and depression as outcomes: The Hordaland Health Study. Occup Med-Oxford. (2005) 55:463. doi: 10.1093/occmed/kqi071
12. Portoghese I, Galletta M, Leiter M, Finco G, d'Aloja E, Campagna M. Job demand-control-support latent profiles and their relationships with interpersonal stressors, job burnout, and intrinsic work motivation. Int J Environ Res Public Health. (2020) 17:9430 doi: 10.3390/ijerph17249430
13. Siegrist J. Adverse health effects of high-effort/low-reward conditions. Occup Health Psychol. (1996) 1:27. doi: 10.1037//1076-8998.1.1.27
14. Kivimäki M, Kawachi I. Need for more individual-level meta-analyses in social epidemiology: example of job strain and coronary heart disease. Am J Epidemiol. (2013) 177:1–2. doi: 10.1093/aje/kws407
15. Kivimäki M, Nyberg S, Batty D, Fransson E, Heikkilä K, Alfredsson L, et al. Job strain as a risk factor for coronary heart disease: a collaborative meta-analysis of individual participant data. Lancet. (2012) 380:1491–7. doi: 10.1016/S0140-6736(12)60994-5
16. Sverke M, Hellgren J. The nature of job insecurity: understanding employment uncertainty on the brink of a new millennium. Appl. Psychol. (2002) 51:23. doi: 10.1111/1464-0597.0077z
17. Bergström, G, Berglund G, Blomberg A, Brandberg J, Engström G, Engvall J et al. The Swedish cardiopulmonary bioimage study: objectives and design. J Intern Med. (2015) 278:645. doi: 10.1111/joim.12384
18. Bergström, G, Persson M, Adiels M, Björnson E, Bonander C, Ahlström H, et al. Prevalence of subclinical coronary artery atherosclerosis in the general population. Circulation. (2021): 144:916. doi: 10.1161/CIRCULATIONAHA.121.055340
19. Östgren, CJ, Söderberg S, Festin K, Angerås O, Bergström G, Blomberg A, et al. Systematic coronary risk evaluation estimated risk and prevalent subclinical atherosclerosis in coronary and carotid arteries: a population-based cohort analysis from the Swedish Cardiopulmonary Bioimage Study. Eur J Prev Cardiol. (2021) 28:250. doi: 10.1177/2047487320909300
20. Karlen J, Ludvigsson J, Frostell A, Teodorsson E, Faresjo, T. Cortisol in hair measured in young adults - a biomarker of major life stressors? BMC Clin Pathol. (2011) 11:12. doi: 10.1186/1472-6890-11-12
21. Koç H. The impact of managers' leadership behaviors on job satisfaction and performance of employees. Afr J Bus Manage. (2011) 5:11836–118 doi: 10.5897/AJBM10.1229
22. Chi SCS, Liang SG. When do subordinates' emotion-regulation strategies matter? Abusive supervision, subordinates' emotional exhaustion, and work withdrawal. Leadersh Q. (2013) 24:125–1 doi: 10.1016/j.leaqua.2012.08.006
23. Stradovnik K, Stare J. Correlation between Machiavellian leadership and emotional exhaustion of employees: case study: Slovenian municipalities. Leader Organ Dev J. (2018) 39:1037–10 doi: 10.1108/LODJ-06-2018-0232
24. Wang CC, Hsieh H H, Wang Y.D. Abusive supervision and employee engagement and satisfaction: the mediating role of employee silence. Pers Rev. (2020) 49:1845–18 doi: 10.1108/PR-04-2019-0147
25. Blanch A. Social support as a mediator between job control and psychological strain. Soc Sci Med. (2016) 157:148. doi: 10.1016/j.socscimed.2016.04.007
Keywords: working conditions, support at work, middle-aged population, job-strain, biological stress, perceived stress
Citation: Iredahl F, Theodorsson E, Jones M, Faresjö T and Faresjö Å (2025) Non-support from the immediate boss is associated with stress and unsafety at work. Front. Public Health 13:1416609. doi: 10.3389/fpubh.2025.1416609
Received: 12 April 2024; Accepted: 20 January 2025;
Published: 10 February 2025.
Edited by:
Adelinda Araujo Candeias, University of Evora, PortugalReviewed by:
Raina Chhajer, Indian Institute of Management, IndiaCopyright © 2025 Iredahl, Theodorsson, Jones, Faresjö and Faresjö. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Åshild Faresjö, YXNoaWxkLm9sc2VuLmZhcmVzam9AbGl1LnNl
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.