
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Public Health, 21 February 2025
Sec. Aging and Public Health
Volume 13 - 2025 | https://doi.org/10.3389/fpubh.2025.1410342
Chronic obstructive pulmonary disease (COPD) is a major global public health concern. In this study, we examined the comparative efficacy of non-pharmacological interventions within East Asian traditional medicine (EATM-NPI) for enhancing pulmonary function and exercise capacity in patients with stable COPD. A thorough search of electronic databases conducted until May 22, 2022, identified studies employing EATM-NPI in such patients. The evaluation focused on the impact adjunctive therapies on pulmonary function (forced expiratory volume in 1 s [FEV1]) and exercise capacity (6-min walking distance [6MWD]). The qualitative assessment encompassed 142 studies, with 133 studies included in one of three network meta-analyses. Participants, aged 49–76 years, ranged from 9 to 139 per group, predominantly from China (87.7% of studies). Overall study quality was generally low, and reported adverse events were mild. Notably, moxibustion and qigong adjunctive therapies demonstrated significant improvements in FEV1 (L) and FEV1 (%). Additionally, chuna, acupuncture, qigong and moxibustion adjunctive therapies were associated with significant improvements in 6MWD. In conclusion, EATM-NPI adjunctive therapy, when combined with standard pharmacological treatment, exhibited effects on pulmonary function and exercise capacity in patients with COPD.
Systematic review registration: The protocol was registered with PROSPERO (CRD42023389431), https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42023389431.
Chronic obstructive pulmonary disease (COPD) is a disease marked by irreversible airway obstruction on the pulmonary function test along with symptoms such as chronic dyspnea, cough, and sputum (1). COPD is a major disease that poses economic and social burdens, and its global burden is consistently increasing (2–4). In 2017, COPD was the third leading cause of death globally (5). In 2019, the global prevalence of COPD was 10.3% with approximately 391.9 million people estimated to be have been affected by the disease (5, 6). Its prevalence in East Asia has been reported to be slightly higher than the global average. The trends in the prevalence of COPD in South Korea were reported within the range of approximately 13.1 to 14.6% during the period from 2010 to 2015 (7), and that in China was 13.6% during 2014–2015 (8). COPD typically manifests in individuals aged 40 years and older; thus, its prevalence is expected to increase in an aging society. Therefore, COPD has been incorporated into the WHO Global Action Plan to prevent and control non-communicable diseases.
To mitigate the mounting burden of respiratory illnesses that have surged since the 20th century, it is important to explore alternative strategies that can more effectively manage COPD in conjunction with the standard pharmacological therapy proposed by the Global Initiative for Chronic Obstructive Lung Disease (GOLD) (9). Pharmacological therapy alone falls short of effectively managing these chronic, irreversible symptoms and respiratory exacerbations, along with systemic repercussions. Therefore, non-pharmacological therapy plays a pivotal role in managing patients with stable COPD (1).
The non-pharmacological intervention of East Asian traditional medicine (EATM-NPI) represents an enticing alternative that can be added to standard pharmacological therapy. The EATM-NPI encompasses various traditional medicine practices. Although acupuncture, which stimulates the surface of the body using needles, is the most well-known method, other EATM-NPIs include moxibustion, which involves thermal stimulation of the body’s surface; cupping therapy, which creates negative pressure on the skin; qigong, which involves breathing regulation and mental focus; and chuna, a manual therapy that alters the body’s function and structure through the practitioner’s hands. These EATM-NPIs have been sporadically studied for their potential to provide additional benefits to patients with COPD.
A network meta-analysis (NMA) comparing traditional exercise therapies revealed that Wuqinxi improved pulmonary function and exercise capacity, whereas Yijinjing improved quality of life (QOL) (10). A meta-analysis of studies on acupuncture-related treatments showed that acupressure enhances QOL, whereas acupuncture improves pulmonary function, exercise capacity, and QOL (11, 12). Furthermore, the 2023 GOLD guidelines presented acupuncture and acupressure as elective adjunctive therapies for dyspnea (1). In a meta-analysis on chuna therapy, the authors could not draw a concrete conclusion on whether chuna improves pulmonary function and exercise capacity, but they found that non-pharmacological therapies generally are effective on COPD, indicating that non-pharmacological therapies could be promising for COPD (13).
There is a dearth of comprehensive evidence for EATM-NPI as a new potential approach for the management and treatment of stable COPD. Nearly all studies on EATM-NPIs for patients with COPD show that they have been ethically designed as add-on therapies in conjunction with standard pharmacological treatments. Additionally, in actual East Asian clinical practice, various combinations of EATM-NPI therapies are used concurrently to treat patients with COPD (14–16), so clinicians face the challenge of determining which EATM-NPI therapy to prioritize for patients with COPD. While traditional pairwise meta-analysis (PMA) is limited to analyzing one intervention at a time, NMA allows for a relative ranking of the therapeutic efficacy of multiple interventions, thereby empowering clinicians and patients to make more informed decisions. This study aimed to investigate the comparative effects of EATM-NPIs added to standard pharmacological therapy for patients with stable COPD by using NMA. Therefore, here we aimed to investigate the therapeutic efficacy and comparative advantages of non-pharmacological therapies and derive treatment strategies for patients with stable COPD in an aging society.
This study adheres to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses NMA guideline (Supplement 1) (17), and the protocol was registered with PROSPERO (CRD42023389431).
The eligibility criteria were established based on the participant, intervention, comparison, outcome, and study design (PICOS) framework.
Studies that made the diagnosis based on the GOLD guideline (1) or “forced expiratory volume in 1 s (FEV1)/forced vital capacity (FVC) <0.7” and specified the diagnosis were included. Randomized controlled trials (RCTs) and crossover RCTs were included, whereas non-RCTs, observational studies, case reports, and animal studies were excluded. If a particular arm did not meet the eligibility criteria in a multi-arm trial, that study was still included, but the data from the specific arm were not used.
Patients with stable COPD were included, and patients with acute exacerbation of COPD were excluded. There were no limitations on age, sex, and COPD severity. Patients who did not receive the standard pharmacological therapy as specified in the GOLD guideline during the study period were also excluded.
The main intervention was EATM-NPI. Herbal medicine and pharmacoacupuncture therapy were excluded. EATM-NPI was broadly categorized into qigong (unspecified qigong, Wuqinxi, Liuzijue, Yijinjing, Taichi, and Baduanjin), moxibustion, cupping, chuna (fascia chuna therapy, joint mobilization and distraction, and spine and joint manipulation), and acupuncture (traditional stimulation of acupoints without the use of thermal stimulation). The treatment for the control group was not limited, but studies that used additional drugs or an herbal regimen for the control group were excluded. The treatment of the control group was broadly divided into pharmacological treatment (pharmacological therapy specified in the GOLD guidelines), exercise therapy (aerobic exercise prescribed in PR that is not considered an EATM-NPI, e.g., pursed-lip breathing and abdominal respiration), and placebo (with blinded).
The outcome measures were pulmonary function and exercise capacity. Pulmonary function was assessed based on FEV1 measured through spirometry, and exercise capacity was assessed based on the 6-min walking distance (6MWD). Specifically, FEV1 was measured using 2 units: FEV1 (L), which represents the actual exhalation volume, and FEV1 (%), which indicates the percentage of the predicted value based on the normal range for healthy individuals. Adverse events (AEs) reported in the included studies that reported FEV1 and 6MWD as the primary outcomes were collected.
A comprehensive search strategy was formulated using a combination of search terms pertaining to disease and intervention (Supplement 2). The language was not limited. The literature search was conducted in the following electronic databases from the beginning of the database to May 22, 2022: Medline via PubMed, EMBASE via Elsevier, CENTRAL (The Cochrane Central Register of Controlled Trials), China National Knowledge Infrastructure, DBpia, Korean Studies Information Service System, Research Information Service System, and Oriental Medicine Advanced Searching Integrated System.
The references of the included studies and systematic reviews of relevant topic were manually searched. Ongoing protocols and conference abstracts were searched in Clinicaltrials.gov and the World Health Organization International Clinical Trials Registry Platform.
After uploading all the search results into EndNote X9.3.3 (Clarivate Analytics), two researchers (JAR and KIK) independently screened the titles and abstracts and then reviewed the full texts to select the studies. The same two researchers exported the title, author, publication. Year, country of origin, study design, enrolled and analyzed sample sizes, population age, disease severity, diagnostic criteria of COPD, treatment modalities and details of each assigned group, total treatment duration, treatment schedule, follow-up, reported AEs, and outcome measures of the studies as a spreadsheet (Microsoft Excel; Microsoft Corp.).
Any disagreements between the two researchers were resolved upon discussion. If an agreement could not be reached, a third researcher (JL) was involved to reach a consensus.
Two researchers (JAR and KIK) independently assessed the risk of bias of the included studies using the Cochrane Handbook 5.1.0. assessment tool (18). The following items were rated as low risk, high risk, or unclear risk: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of the outcome assessment, incomplete outcome data, selective reporting, and other bias.
First, PMA was performed for each intervention using Cochrane’s Review Manager (RevMan 5.4). The effect sizes of EATM-NPI were calculated based on all the included studies that could be included in the NMA. The primary outcome measures FEV1 (both L and %) and 6MWD were statistically analyzed using mean differences (MDs) and 95% confidence intervals (CIs). Data at the end of treatment were used; a positive MD indicated greater improvement of pulmonary function and exercise capacity.
A network model with a random effects model (19) was setup using the R package “netmeta (20)” for of the free software R-4.2.1 for Windows and RStudio (21) to conduct NMA using the frequentist method (22, 23). FEV1 was analyzed separately for each scale, and the results were presented in a forest plot and league table. P-scores, the probability of comparative advantage in non-pharmacological therapy, were calculated using the “netrank” function (21). The Egger’s test was used, and the results were visualized in a funnel plot to assess potential publication bias and overall bias of the included studies (21). Regarding the assumptions of NMA, connectivity was assessed using a network plot, and heterogeneity was assessed using I2. Network transitivity and consistency were verified through a global approach using Q-statistics, and consistency between direct and indirect comparisons was verified through a local approach using the node-splitting method.
In total, 2,272 studies were identified, and after removing duplicate results and ineligible studies per PICOS, 142 studies were included (Figure 1) (24–165). With the exception of one cross-over RCT (133), all studies were RCTs. The number of participants assigned to each group was 9–139. Participants’ mean age was 49–76 years, and COPD severity varied. Most studies (87.7%) were conducted in China. No studies used cupping therapy as the intervention. The qigong group included qigong, health qigong integrated for lung health, Wuqinxi, Liujizue, Yijinjing, Taichi, and Baduanjin (24–110). The moxibustion group included unspecified moxibustion, ginger moxibustion, heat-sensitive point’s moxibustion, Yi Fei moxibustion, and fire-dragon moxibustion (111–130). The chuna group included osteopathic manipulative therapy, specialized physiotherapy, and chuna (131–136). The acupuncture group included filiform acupuncture, Acu-TENS, warm needle acupuncture, auricular acupressure, electroacupuncture, pressing needle acupuncture, and acupressure (137–165). Treatment duration ranged from once to 1 year (Table 1). If FVC was also reported in the included study, the data were presented in the table to aid in qualitative interpretation (Supplementary Table S1). Outcome variables presented as medians, mean differences, or points were excluded from the meta-analysis (33, 47, 64, 70, 71, 91, 105, 133, 142). Of 142 studies, 27 studies (27, 58, 64, 66–71, 86, 93, 132, 133, 137, 140, 141, 147, 150–156, 159, 163, 164) reported AEs (18.5%), and AEs requiring treatment were not reported (Table 1).
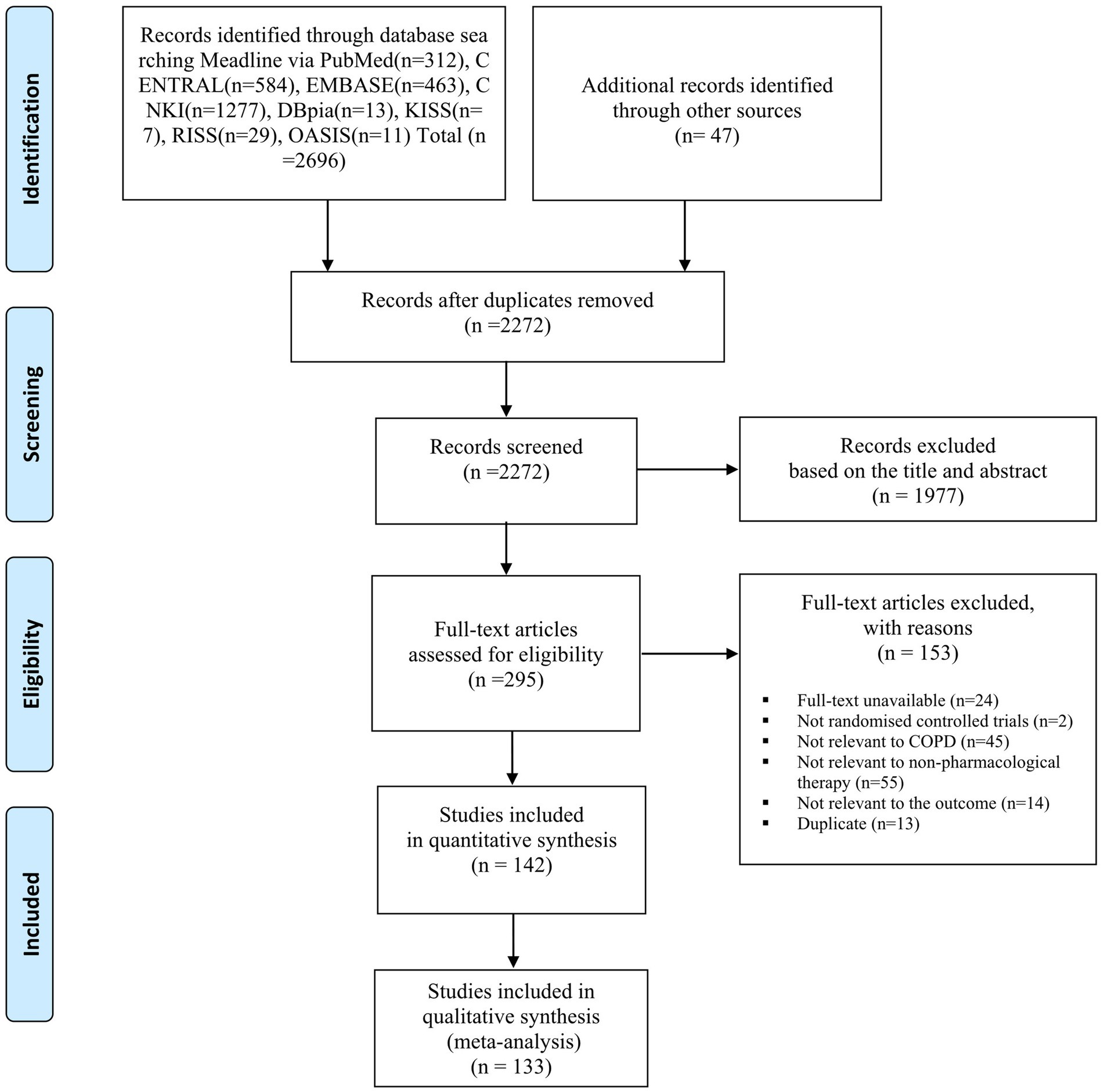
Figure 1. Flowchart of identification and screening for the eligible studies. COPD, chronic obstructive pulmonary disease; CNKI, China National Knowledge Infrastructure; KISS, Korean Studies Information Service System; RISS, Research Information Service System; OASIS, Oriental Medicine Advanced Searching Integrated System.
The studies had a low risk of bias in terms of random sequence generation (61.3%) (24–26, 31, 32, 34, 37, 38, 40–44, 46–48, 50, 52–54, 56–58, 60–64, 66–, 68–72, 78, 80–82, 85, 86, 88, 89, 92–100, 110, 117–119, 121, 125, 127, 128, 130–133, 135, 139–142, 145–147, 149–153, 155, 156, 158, 160, 161, 163–165) and incomplete outcome data (83.8%) (24, 25, 28, 30–38, 40–44, 46–52, 54–72, 74, 75, 78–81, 83–85, 87, 93, 95–139, 141–153, 156, 158, 159, 161, 162, 164, 165), but there was unclear risk of bias in terms of allocation concealment (80.9%) (26–33, 35, 36, 38–40, 42–45, 47, 49, 51–57, 59–67, 70, 73–85, 87, 88, 90–93, 96–117, 119–130, 132–134, 136–141, 143–149, 154–159, 161, 162, 164, 165) and blinding of the outcome assessment (78.2%) (27–33, 35, 39–45, 47–49, 51–57, 59–63, 65, 67, 69, 73–88, 90–94, 96–130, 133–136, 138, 143–149, 154–159, 161, 162, 164, 165). Because of the nature of non-pharmacological treatment, there were no studies with a low risk of bias in terms of blinding of participants and personnel, and 14.8% of the studies (25–27, 34, 36–38, 46, 66, 68, 89, 131, 133, 140–142, 150–153, 160) had a high risk of bias in this aspect. One study published the protocol (64), and the remaining studies had an unclear risk of bias in terms of selective reporting, as shown in Supplementary Table S2.
PMA of 133 RCTs (24–32, 34–46, 48–63, 65–69, 72–75, 77–104, 106–132, 134–141, 143–165) revealed that qigong, moxibustion, and acupuncture adjunctive therapies improved pulmonary function and exercise capacity, whereas chuna adjunctive therapy only improved exercise capacity (Supplement 4). In NMA, there were no issues with network connectivity and inconsistency in each of the three outcome measures (Figures 2A–C and Supplementary Figures S1–S3). NMA of the same 133 RCTs included in the PMA (24–32, 34–46, 48–63, 65–69, 72–75, 77–104, 106–132, 134–141, 143–165) showed that all types of EATM-NPI added to standard pharmacological treatment led to improvements in exercise capacity compared to standard pharmacological treatment alone, and qigong and moxibustion adjunctive therapies led to improvements in pulmonary functions.
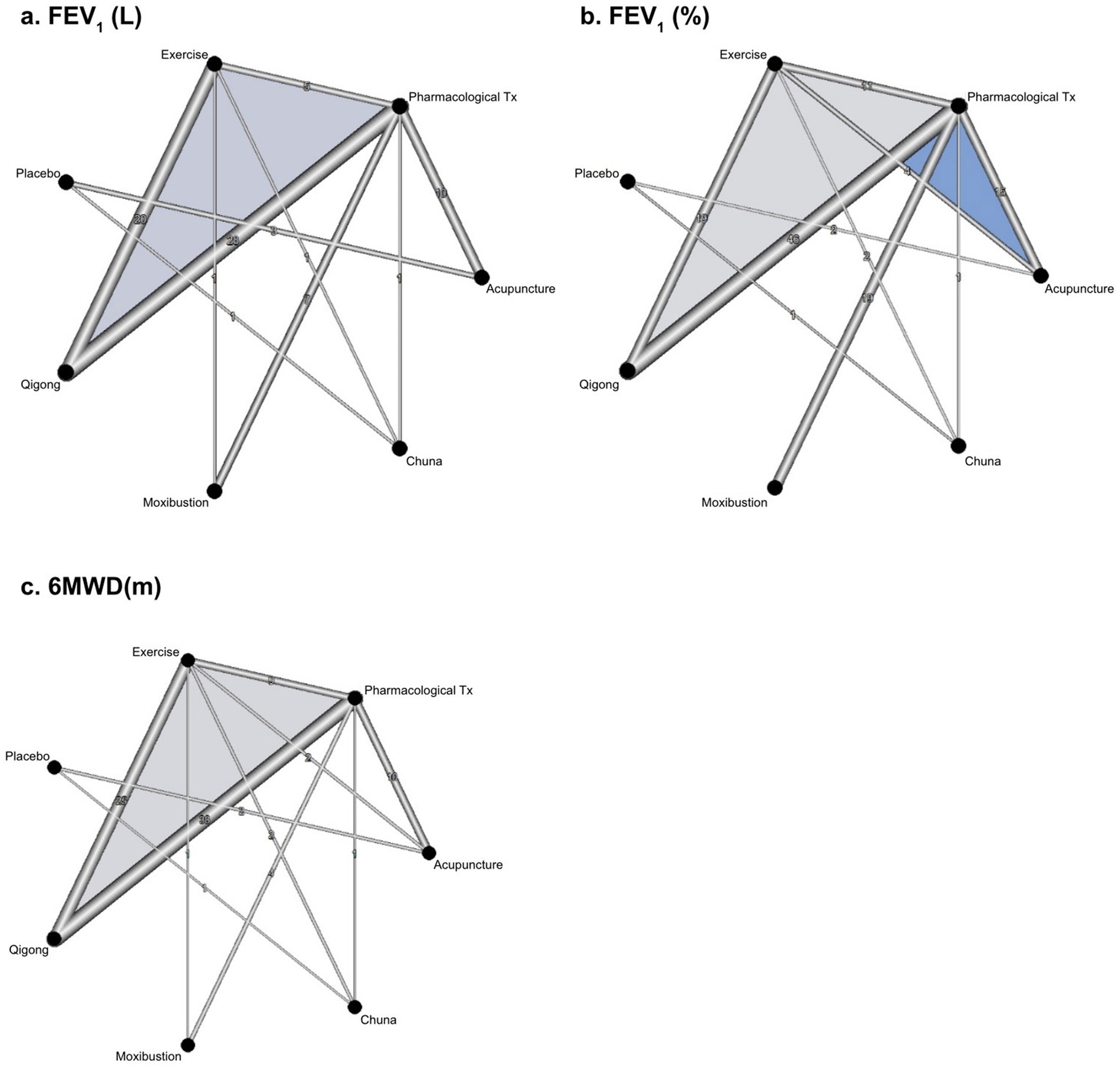
Figure 2. Network evidence map of eligible comparisons: (A) FEV1(L); (B) FEV1(%); (C) 6MWD(m). FEV1: forced expiratory volume in a 1 s; 6MWD, 6-min walking distance; Tx, treatment.
NMA results were as follows. FEV1 (L) was most improved by moxibustion (113, 114, 121–125, 128, 129), followed by qigong (25, 30–32, 35, 37, 39, 41, 43, 49, 50, 53, 56, 59, 60, 62, 63, 66–69, 72, 74, 77–82, 84, 85, 88, 91, 92, 94–96, 101–103, 107, 108, 110), acupuncture (137, 140, 141, 145, 148, 149, 152, 153, 156–159), placebo, chuna (132, 134, 136), exercise therapy, and standard pharmacological treatment (Table 2A). P-scores were as follows: moxibustion, B: 0.7752; qigong, A: 0.7537; acupuncture, D: 0.5603; placebo, 3: 0.5510; chuna, C: 0.3894; exercise therapy, 2: 0.3490; and standard pharmacological treatment 1: 0.1213. Compared to the reference (standard pharmacological treatment), chuna and acupuncture adjunctive therapies had overlapping CIs, and qigong (A: MD 0.228, 95% CI 0.122–0.334) and moxibustion adjunctive therapies (B: MD 0.252, 95% CI 0.046–0.458) were statistically significant (Figure 3A and Supplementary Table S3).
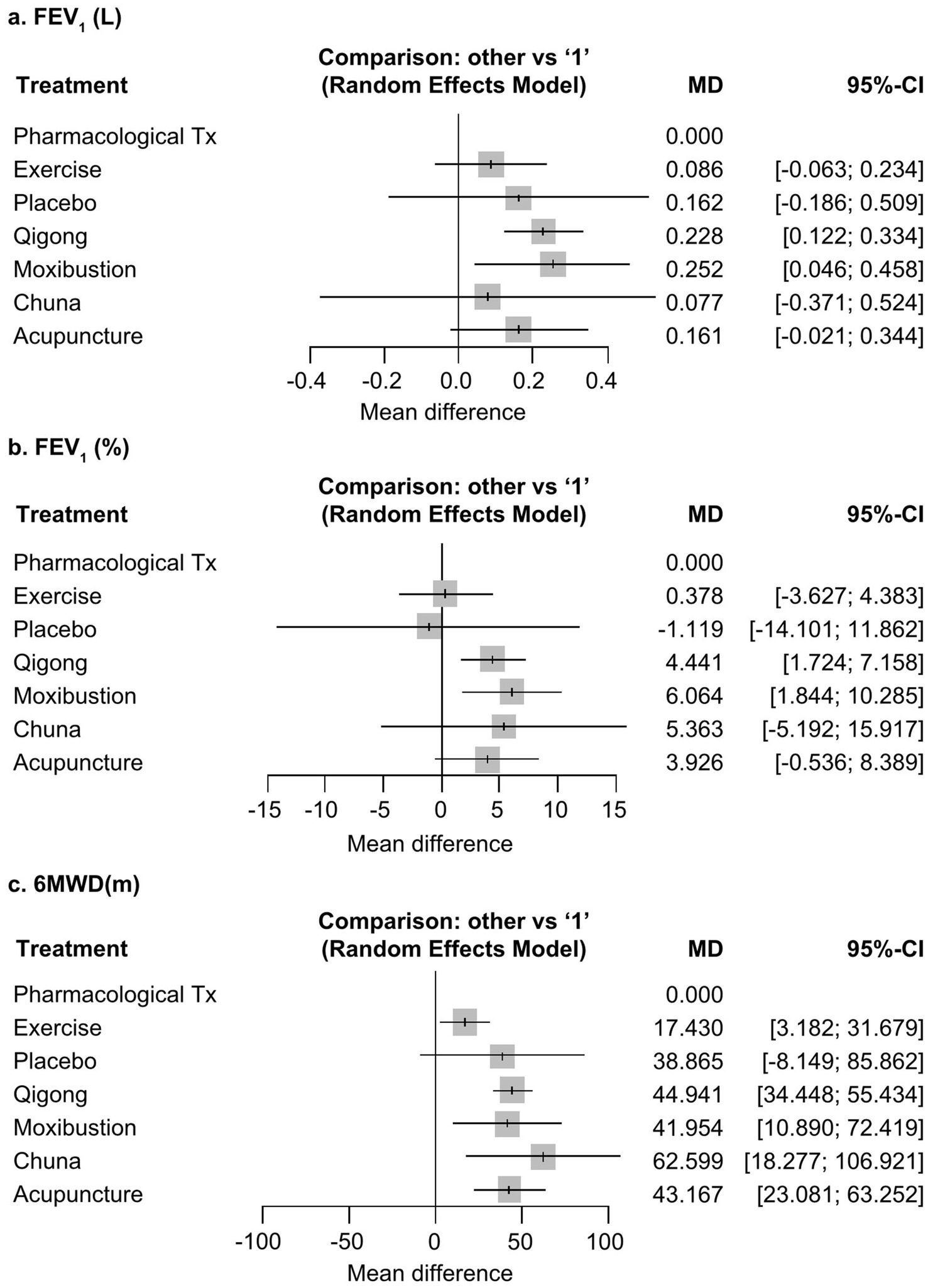
Figure 3. Network forest plots. All non-pharmacological interventions of East Asian Traditional Medicine (EATM-NPIs) were compared with pharmacological Tx (“1”) using a random-effects model: (A) FEV1(L); (B) FEV1(%); (C) 6MWD(m). FEV1: forced expiratory volume in a 1 s; 6MWD, 6-min walking distance; Tx, treatment; MD, mean difference; CI, confidence interval.
FEV1 (%) was most improved by moxibustion (111–113, 115–122, 124–130), followed by chuna (132, 134–136), qigong (25–31, 34, 35, 37–41, 43–45, 49, 51, 53–55, 57, 59–63, 65, 66, 68, 69, 73, 75, 78, 80, 82, 84, 85, 88, 91, 93–99, 101–107, 110), acupuncture (137–141, 143–145, 151, 154–163, 165), placebo, exercise therapy, and standard pharmacological treatment (Table 2B). P-scores were as follows: moxibustion, B: 0.8094; chuna, C: 0.6825; qigong, A: 0.6753; acupuncture, D: 0.6181; placebo, 3: 0.2677; exercise therapy, 2: 0.2472; and standard pharmacological treatment, 1: 0.1998. Compared to the reference, chuna and acupuncture adjunctive therapies had overlapping CIs, and moxibustion (B: MD 6.064, 95% CI 1.844–10.285) and qigong adjunctive therapies (A: MD 4.441, 95% CI 1.724–7.158) were statistically significant (Figure 3B and Supplementary Table S3).
6MWD (m) was most improved by chuna (131, 134–136), followed by qigong (24–27, 29–31, 34, 36, 38, 40, 42, 43, 46, 48, 49, 52, 55, 58–63, 65–69, 72–74, 78, 80–84, 86–90, 94–100, 103, 107–109), acupuncture (137, 138, 141, 144, 146–148, 150, 151, 156, 160, 161, 164, 165), moxibustion (112, 117, 122, 123, 125), placebo, exercise therapy, and standard pharmacological treatment (Table 2C). P-scores were as follows: chuna, C: 0.8539; qigong, A: 0.6599; acupuncture, D: 0.6229; moxibustion, B: 0.5954; placebo, 3: 0.5408; exercise therapy, 2: 0.2157; and standard pharmacological treatment, 1: 0.0113. Compared to the reference, qigong adjunctive therapy (A: MD 44.941, 95% CI 34.448–55.434), moxibustion adjunctive therapy (B: MD 41.654, 95% CI 10.890–72.419), chuna adjunctive therapy (C: MD 62.599, 95% CI 18.277–106.921), and acupuncture adjunctive therapy (D: MD 43.167, 95% CI 23.081–63.252) were statistically significant (Figure 3C and Supplementary Table S3).
Regarding publication bias, the distribution was symmetrical overall, but studies with a large sample size had a greater impact on the results. Further, the Egger’s test result suggested a possibility of publication bias in FEV1; thus, caution is needed when interpreting the findings (p < 0.01) (Supplementary Figure S4).
The present NMA sheds light on the comparative effects of EATM-NPI adjunctive therapy on pulmonary function and exercise capacity in patients with stable COPD. Compared to standard pharmacological treatment alone, qigong and moxibustion add-on therapies were more effective in improving FEV1, whereas qigong, moxibustion, chuna, and acupuncture add-on therapies were more effective in improving 6MWD. Hence, moxibustion may be considered over other adjunctive therapies when attempting to improve pulmonary function, whereas chuna may be considered first when the goal is to improve exercise capacity. AEs reported across the 27 studies (27, 58, 64, 66–71, 86, 93, 132, 133, 137, 140, 141, 147, 150–156, 159, 163, 164) were mostly mild. Some studies showed methodological issues related to random sequence generation, allocation concealment, and blinding of personnel.
Dyspnea and decline in physical activities among patients with COPD are linked to secondary musculoskeletal problems (166). Therefore, it is possible that controlling these musculoskeletal problems could improve respiratory symptoms even without directly improving pulmonary function. Additionally, exacerbation of pulmonary functions (e.g., ventilatory limitation, gas exchange limitation, and cardiac limitation) can limit exercise capacity, and if musculoskeletal limitations, particularly limitation due to lower limb muscle dysfunction becomes chronic (167, 168), respiratory functions may weaken due to muscle dysfunction (169).
There is extensive research on the treatment of musculoskeletal disorders with the following modalities: chuna that is performed using hands, (12, 170, 171), qigong that trains the mind for meditation and places emphasis on smooth respiration and motions (172–174), acupuncture that stimulates soft tissues at acupoints using acupuncture needle (175, 176), and moxibustion that uses mugwort instead of needles (177). Our study is significant in that it sheds light on the potential of treating respiratory disorders by improving reversible and modifiable musculoskeletal issues.
Moxibustion has positive effects on respiratory diseases, such as lung cancer (178), pulmonary fibrosis (179), asthma (180), allergic rhinitis (181), and joint and spinal disorders (182, 183) through the regulation of inflammatory responses. Moxibustion regulates the body’s immune system (184) by improving the CD4+/CD8+ ratio, tumor necrosis factor-α levels, interleukin (IL)-10 levels, and IL-10/IL-6 ratio (185–187), thus effectively reducing inflammation (188). Our finding that moxibustion more effectively improved FEV1 than 6MWD did might have been attributable its use in treating chronic inflammation of the lungs.
Acupuncture may be effective in patients with COPD, as it reduces the chronic inflammatory state and concurrently improves chest wall stiffness. Acupuncture provides anti-inflammatory effects by regulating vascular responses and cytokines (142, 189–191) and clinically reduces inflammatory conditions, e.g., asthma (192), allergic rhinitis (193), and inflammatory bowel disease (194). Additionally, acupuncture mechanically stimulates connective tissues (195–198) and improves musculoskeletal flexibility (199), exhibiting effectiveness in various musculoskeletal disorders, e.g., low back pain (200, 201), neck pain (202), and frozen shoulder (203). However, in our NMA, acupuncture was effective in improving only 6MWD. Improving the mobility of the thorax and back may be a more beneficial pathway for patients with COPD, and further research on this is required.
Qigong involves following a step-by-step movement while regulating breathing, which promotes a sense of self-confidence, enhances flexibility and overall body balance, and activates bodily functions (59, 173, 174, 204–206). Although the exact mechanism underlying Qigong’s effects remains unclear, it has been reported to improve the 6MWD in patients with ischemic heart failure (207) and chronic heart failure (208), enhance FEV1 (%) in patients with non-small cell lung cancer (209), and manage pain in patients with chronic pain (210, 211). Qigong has demonstrated benefits in regulating the movement of the respiratory muscles and the overall musculoskeletal system. Meta-analyses conducted in 2014 (212) and 2019 (213) on the use of qigong in COPD reported statistically significant improvements in 6MWD, FEV1 (L), and FEV1 (%). Consistent with these previous meta-analyses, our study confirmed that qigong improves both FEV1 and 6MWD.
Chuna therapy may help improve exercise capacity in patients with COPD by alleviating chest stiffness through manual manipulation. Although the exact mechanism remains unclear, previous studies (10, 214) have suggested that Chuna therapy can improve both pulmonary function and exercise capacity. However, in this study’s NMA, while Chuna therapy demonstrated the most prominent improvement in 6MWD, significant effects were observed only in exercise capacity. Given the limited number of studies on Chuna therapy, large-scale follow-up studies are warranted.
This is the first study to conduct the latest meta-analysis to compare the effectiveness of various EATM-NPIs in patients with COPD. We provided decisive evidence for the clinical prescription of EATM-NPI through NMA, and in addition to prior research, we also showed that EATM-NPI is a promising treatment approach for COPD.
A previous NMA on qigong (10) used FEV1/FVC (%) as the index for pulmonary function, but we used FEV1 instead. For COPD patients, the impairment of FEV1 is distinct and more crucial compared to FVC. Moreover, the GOLD guidelines categorize the severity of COPD based on FEV1, emphasizing the significance of FEV1 variability in COPD. In this study, we employed raw values of FEV1 rather than the FEV1/FVC ratio, distinguishing between absolute FEV1 in liters and the FEV1%. We conducted separate meta-analyses to examine the respective effects of each. There was no closed loop in the network diagram of Li et al.’s study, but we used a closed loop for a mixed comparison (10). Li et al. reported that Wuqinxi is the most effective traditional exercise modality for improving FEV1/FVC (%) and 6MWD (10). Herein, we examined broad categories of traditional interventions and showed that qigong is significantly more effective than other EATM-NPIs in improving FEV1 and 6MWD. Previous studies on acupuncture as an adjunctive therapy (11, 12) conducted PMA for acupuncture, Acu-TENS, moxibustion, acupressure, auricular acupuncture, and cupping, but we included acupuncture, Acu-TENS, warm needle acupuncture, auricular acupressure, electroacupuncture, pressing needle acupuncture, and acupressure in the acupuncture group and conducted NMA to compare it with other EATM-NPIs. One benefit of this analysis is that it provides the therapeutic efficacy estimates of each EATM-NPI as add-on treatment options to clinicians to improve motor and respiratory functions in patients with COPD who are refractory to standard treatment.
This study has several limitations. The scope of the included studies was broad, so it was not possible to control for all sources of heterogeneity. To conduct macroscopic analysis, we had to include heterogeneous treatments in each EATM-NPI, and the treatment schedules and severity of COPD varied across individual studies. Future studies should narrow the research question to focus on specific severities of COPD or capacities of intervention. Furthermore, our study was affected by the essential limitation of research on EATM-NPI; because of the intrinsic nature of non-pharmacological therapies, therapists could not be blinded, which led to low overall quality of the included studies and a lack of robustness in the NMA results. Moreover, we conducted a mixed comparison in macroscopic analysis, but the number of studies on each type of EATM-NPI varied, and few studies directly compared different EATM-NPIs. Finally, this study was limited by the lack of an evaluation of GRADE. Consequently, a constraint affects clearly determining the recommendation level. However, when RCTs conducted in China were assessed using GRADE, the recommendation levels were generally low, with little variation among different interventions. Considering these circumstances, the primary significance of this meta-analysis lies in its identification of information that can assist Traditional Chinese Medicine practitioners in clinical decision-making when faced with the challenge of selecting interventions under conditions of low research quality and evidence levels, i.e., in situations where information is limited. However, our evaluation of the evidence level for individual interventions was incomplete. Therefore, future research should involve subsequent studies applying the GRADE methodology to individual interventions through PMA rather than NMA.
For patients with COPD, pharmacological treatment alone has limitations in terms of adverse drug reactions, compliance, and satisfaction. Non-pharmacological treatments for patients with COPD have been established since the mid-2000s, and evidence has been accumulating for treatment modalities such as qigong, moxibustion, chuna, and acupuncture. This study provides clinical practitioners with additional therapeutic options for managing stable COPD that does not respond to standard therapy. Particularly, various types of exercises are recommended for patients who still have diminished exercise capacity even with improved parameters on respiratory function tests. Subsequent studies should investigate various exercise therapies and indications for qigong, an EATM intervention, to establish evidence-based personalized treatment for patient symptoms. Future studies should also comply with Standards for Reporting Interventions in Clinical Trials of Acupuncture (215) and Consolidated Standards of Reporting Trials extension for non-pharmacologic treatment (216) to improve methodological quality. Moreover, the severity of COPD is an important consideration in the treatment selection and subsequent studies should further analyze this.
We did not investigate pharmacological treatments, such as herbal medicine, pharmacopuncture, and aromatherapy. In the future, studies should also investigate EATM-pharmacological interventions and conduct NMA of the synergistic effects with herbal medicine. Since head-to-head trials are difficult for EATM interventions because of a lack of resources, the findings of such studies would help present the optimal EATM intervention for each symptom and present implications for clinical practice and clinical practice guidelines. The search in this study was conducted until May 2022, so caution should be exercised when interpreting its results. If further research is conducted, a GRADE assessment should be incorporated for a more comprehensive evaluation.
Our study confirmed that the addition of EATM-NPI to standard therapy can aid symptom management in patients with COPD. We confirmed that moxibustion or qigong therapies as adjunctive therapies to standard treatment improve pulmonary function and exercise capacity, whereas chuna and acupuncture adjunctive therapies improve exercise capacity in patients with stable COPD. Clinically, we provide evidence supporting the use of moxibustion add-on therapy to improve FEV1 and chuna add-on therapy to improve 6MWD in patients who do not respond well to standard treatment. We look forward to future research efforts aimed at identifying responders to each NPI among patients with COPD, thereby optimizing NPI methods for this population.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
J-AR: Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. JL: Data curation, Formal analysis, Methodology, Writing – review & editing. B-JL: Data curation, Writing – review & editing. K-IK: Conceptualization, Funding acquisition, Investigation, Methodology, Writing – original draft, Writing – review & editing. H-JJ: Conceptualization, Funding acquisition, Writing – review & editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant numbers: RS-2020-KH087748 and RS-2023-KH139413).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1410342/full#supplementary-material
AE, Adverse events; CAT, COPD-acupuncture trial; CI, Confidence interval; COPD, Chronic obstructive pulmonary disease; EATM, East Asian traditional medicine; FEV1, Forced expiratory volume in 1 s; FVC, Forced vital capacity; GOLD, Global Initiative for Chronic Obstructive Lung Disease; MD, Mean differences; NMA, Network meta-analysis; NTI, Non-pharmacological intervention; OASIS, Oriental Medicine Advanced Searching Integrated System; OMT, Osteopathic manipulative treatment; QOL, Quality of life; PICOS, Participant intervention comparison outcome and study; PMA, Pairwise meta-analysis; RCT, Randomized controlled trials; STRICTA, Standards for Reporting Interventions in Clinical Trials of Acupuncture; YLD, Years lived with disability.
1. GOLD. Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease (COPD). Available at: www.goldcopd.org (Accessed November 19, 2022) (2023).
2. Lozano, R, Naghavi, M, Foreman, K, Lim, S, Shibuya, K, Aboyans, V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the global burden of disease study 2010. Lancet. (2012) 380:2095–128. doi: 10.1016/S0140-6736(12)61728-0
3. Vos, T, Flaxman, AD, Naghavi, M, Lozano, R, Michaud, C, Ezzati, M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the global burden of disease study 2010. Lancet. (2012) 380:2163–96. doi: 10.1016/S0140-6736(12)61729-2
4. Liang, ZY, and Chen, RC. Revision to the guidelines for the diagnosis and management of chronic obstructive pulmonary disease (revised version 2021): process and perspective. Zhonghua Jie He He Hu Xi Za Zhi. (2021) 44:165–6. doi: 10.3760/cma.j.cn112147-20210207-00098
5. Adeloye, D, Song, P, Zhu, Y, Campbell, H, Sheikh, A, and Rudan, I. Global, regional, and national prevalence of, and risk factors for, chronic obstructive pulmonary disease (COPD) in 2019: a systematic review and modelling analysis. Lancet Respir Med. (2022) 10:447–58. doi: 10.1016/S2213-2600(21)00511-7
6. Adeloye, D, Chua, S, Lee, C, Basquill, C, Papana, A, Theodoratou, E, et al. Global and regional estimates of COPD prevalence: systematic review and meta-analysis. J Glob Health. (2015) 5:020415. doi: 10.7189/jogh.05.020415
7. Hwang, YI, Park, YB, and Yoo, KH. Recent trends in the prevalence of chronic obstructive pulmonary disease in Korea. Tuberc Respir Dis. (2017) 80:226–9. doi: 10.4046/trd.2017.80.3.226
8. Fang, L, Gao, P, Bao, H, Tang, X, Wang, B, Feng, Y, et al. Chronic obstructive pulmonary disease in China: a nationwide prevalence study. Lancet Respir Med. (2018) 6:421–30. doi: 10.1016/S2213-2600(18)30103-6
9. Pauwels, RA, Buist, AS, Calverley, PM, Jenkins, CR, and Hurd, SS. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. Am Rev Respir Dis. (2001) 163:1256–76. doi: 10.1164/ajrccm.163.5.2101039
10. Li, L, Huang, H, Song, J, Yu, Y, Jia, Y, Wang, Y, et al. Network Meta-analysis of the effects of different types of traditional Chinese exercises on pulmonary function, endurance capacity and quality of life in patients with COPD. Front Med. (2022) 9:806025. doi: 10.3389/fmed.2022.806025
11. Fernández-Jané, C, Vilaró, J, Fei, Y, Wang, C, Liu, J, Huang, N, et al. Filiform needle acupuncture for COPD: a systematic review and meta-analysis. Complement Ther Med. (2019) 47:102182. doi: 10.1016/j.ctim.2019.08.016
12. Fernández-Jané, C, Vilaró, J, Fei, Y, Wang, C, Liu, J, Huang, N, et al. Acupuncture techniques for COPD: a systematic review. BMC Complement Med Ther. (2020) 20:138. doi: 10.1186/s12906-020-02899-3
13. Roh, JA, Kim, KI, and Jung, HJ. The efficacy of manual therapy for chronic obstructive pulmonary disease: a systematic review. PLoS One. (2021) 16:e0251291. doi: 10.1371/journal.pone.0251291
14. Lee, B, and Kwon, CY. Comparative effectiveness of east Asian traditional medicine for childhood simple obesity: a systematic review and network meta-analysis. Int J Environ Res Public Health. (2022) 19:12994. doi: 10.3390/ijerph192012994
15. Wang, BR, Choi, IY, Kim, KJ, and Kwon, YD. Use of traditional Korean medicines by patients with musculoskeletal disorders. PLoS One. (2013) 8:e63209. doi: 10.1371/journal.pone.0063209
16. Sung, SH, Baik, YS, Han, JE, Lee, EJ, Kim, J, Park, M, et al. Traditional Korean medicine home Care for the Older Adults during the COVID-19 pandemic in South Korea. Int J Environ Res Public Health. (2022) 19:493. doi: 10.3390/ijerph19010493
17. Hutton, B, Salanti, G, Caldwell, DM, Chaimani, A, Schmid, CH, Cameron, C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. (2015) 162:777–84. doi: 10.7326/M14-2385
18. Higgins, JP, Altman, DG, Gøtzsche, PC, Jüni, P, Moher, D, Oxman, AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:d5928. doi: 10.1136/bmj.d5928
19. Borenstein, M, Hedges, LV, Higgins, JPT, and Rothstein, HR. Chapter 13. Fixed effect versus random effect models In: M Borenstein, LV Hedges, JPT Higgins, and HR Rothstein, editors. Introduction to Meta-analysis. Second ed. Hoboken, NJ: John Wiley & Sons Ltd (2021)
20. Rücker, G., Krahn, U., König, J., Efthimiou, O., Davies, A., Papakonstantinou, T., et al. Netmeta: network Meta-analysis using frequentist methods. Version 2.8-0. (2023) Available at: https://cran.r-project.org/web/packages/netmeta/index.html (Accessed March 1, 2023).
21. RStudio. RStudio: Integrated development for R. (2020) Available at: https://www.rstudio.com/ (Accessed October 15, 2020).
22. Shim, SR, and Kim, SJ. Intervention meta-analysis: application and practice using R software. Epidemiol Health. (2019) 41:e2019008. doi: 10.4178/epih.e2019008
23. Shim, SR, Kim, SJ, Lee, J, and Rücker, G. Network meta-analysis: application and practice using R software. Epidemiol Health. (2019) 41:e2019013. doi: 10.4178/epih.e2019013
24. Dong, X, Wang, X, Jia, N, Chen, X, and Ding, M. A comparison between qigong exercise and cycle ergometer exercise for the rehabilitation of chronic obstructive pulmonary disease: a pilot randomized controlled trial (CONSORT). Medicine. (2021) 100:e26010. doi: 10.1097/MD.0000000000026010
25. Li, P. Intervention effects of a home-based lung-supporting exercise prescription in patients with stable COPD. Master's thesis,. Shanghai: Shanghai Institute of Physical Education (2019).
26. Liu, XD, Jin, HZ, Ng, BH, Gu, YH, Wu, YC, and Lu, G. Therapeutic effects of qigong in patients with COPD: a randomized controlled trial. HK J Occup Ther. (2012) 22:38–46. doi: 10.1016/j.hkjot.2012.06.002
27. Liu, X. Clinical observation and mechanism of fitness qigong in preventing and treating patients with COPD in a stable stage. Doctoral dissertation,. Nanjing: Nanjing University of Traditional Chinese Medicine (2011).
28. Wei, S, Cheng, Y, and He, R. Effects of traditional Hua Tuo five-animal exercises on lung function in patients with chronic obstructive pulmonary disease in the stabilized stage. Clin J Trad Chin Med. (2015) 27:793–5.
29. Zhao, Q. Clinical study on five animal plays for the prevention and treatment of stable chronic obstructive pulmonary disease in the community. J Chin Med. (2015) 30:801–3.
30. Yao, WQ. Effect of moderate stabilization of chronic obstructive pulmonary disease in five animals. Changsha: Hunan Normal University (2021).
31. Jiang, M. The effect of strengthening the six character technique on respiratory function during the stabilization period of chronic obstructive pulmonary disease patients with lung and spleen Qi deficiency. Changsha: Changsha Hunan University of Traditional Chinese Medicine (2017).
32. Hou, M, and Cui, X. Observations on the quality of survival of COPD patients with lung and kidney qi deficiency by streamlining the six-character formula. Guangming Trad Chin Med. (2017) 32:3518–21.
33. Zhang, W, Chen, J, Zheng, G, Li, Z, Zheng, L, and Ge, L. Effects of the “six-character breathing technique” on exercise tolerance in patients with chronic obstructive pulmonary disease in the stabilized phase. Nurs Res. (2009) 23:2957–8.
34. Wu, W, Liu, X, Liu, J, Lial, P, and Wang, Z. Effectiveness of water-based Liuzijue exercise on respiratory muscle strength and peripheral skeletal muscle function in patients with COPD. Int J Chron Obstruct Pulmon Dis. (2018) 13:1713–26. doi: 10.2147/COPD.S165593
35. Zhu, Z. Effect of fitness qigong on respiratory function of 61 patients in stable stage of COPD. J Nanjing Univ Trad Chin Med. (2011) 27:235–7.
36. Xiao, CM, and Zhuang, YC. Efficacy of Liuzijue qigong in individuals with chronic obstructive pulmonary disease in remission. J Am Geriatr Soc. (2015) 63:1420–5. doi: 10.1111/jgs.13478
37. Wu, W, Liu, X, Li, P, Li, N, and Wang, Z. Effect of liuzijue exercise combined with elastic band resistance exercise on patients with COPD: a randomized controlled trial. Evid Based Complement Alternat Med. (2018) 2018:2361962. doi: 10.1155/2018/2361962
38. Li, P, Liu, J, Lu, Y, Liu, X, Wangal, Z, and Wu, W. Effects of long-term home-based Liuzijue exercise combined with clinical guidance in elderly patients with chronic obstructive pulmonary disease. Clin Interv Aging. (2018) 13:1391–9. doi: 10.2147/CIA.S169671
39. Chen, J, Zhang, W, Zheng, G, Zheng, L, Li, Z, and Ge, L. Application of the “six character technique” breathing method in pulmonary rehabilitation of patients with stable COPD. J Fujian Coll Trad Chin Med. (2008) 18:3–4.
40. Yan, L. Clinical study of clam Astragali Antiasthmatic granules combined with intensive six-word breathing exercises in the treatment of stable COPD. Jinan: Shandong University of Traditional Chinese Medicine (2020).
41. Deng, L, Chen, J, Chen, Y, Fan, L, Zhou, H, and Chen, F. Effect of the six-character technique in elderly patients with chronic obstructive pulmonary disease and lung qi deficiency. Chin Med Innov. (2020) 17:112–7.
42. Deng, L, Zhang, W, and Chen, J. Comparative study of the effects of the six-character technique and whole-body breathing exercise on respiratory function in elderly patients with chronic obstructive pulmonary disease. J Rehabil. (2018) 28:57–61.
43. Deng, L. Intervention study of “six-word secret” breathing exercise to improve the prognosis of patients with stable COPD. Fujian: Fujian College of Traditional Chinese Medicine (2009).
44. He, JF. Efficacy of the “six character technique” breathing method in the treatment of stable COPD and its effect on T-lymphocyte subpopulations. Beijing: Beijing University of Traditional Chinese Medicine (2019).
45. Lan, Y, Han, X, Wang, Y, Deng, W, Liu, S, and Feng, Y. Effects of tiotropium bromide combined with the “six character technique” exercise on quality of life and lung function in patients with chronic obstructive pulmonary disease in the stabilized stage. World J Integr Med. (2016) 11:1369–71.
46. Zhang, YX. A randomized controlled study on the effect of six-character training on exercise capacity in patients with stable COPD. Tianjin: Tianjin University of Traditional Chinese Medicine (2021).
47. Lu, F, and Wang, S. A randomized controlled multicenter clinical study of “six-character breathing exercise” for the treatment of stable COPD. Fujian Trad Chin Med. (2021) 52:1–3.
48. Liu, JX. Effects of six-character exercise in water on skeletal muscle dysfunction in patients with stable COPD. Shanghai: Shanghai Institute of Physical Education (2017).
49. Hu, J, Gui, L, Tu, H, Yang, P, Wang, Z, and Ji, S. Rehabilitation effects of the six-character technique in water on patients with chronic obstructive pulmonary disease in the stabilized stage. Pract Clin Med. (2021) 25:45–7.
50. Shen, Q. A study on the effects of “six character technique” on COPD patients in stable stage (Grade I). J External Treat Trad Chin Med. (2017) 26:3–6.
51. Ji, S, Luo, G, Shi, K, Yang, P, and Wang, Z. Clinical study of six-word intervention in patients with chronic obstructive pulmonary disease in the stable stage. West Trad Chin Med. (2019) 32:111–4.
52. Qu, LL, Huang, LL, and Lu, XP. Effect of six-character breathing exercises on the continuity of care for patients with chronic obstructive pulmonary disease. China Rural Med. (2019) 26:80–1.
53. Li, D. Study on the effect of “six-character technique” on chronic obstructive pulmonary disease from the perspective of respiratory mechanics. Fujian: Fujian University of Traditional Chinese Medicine (2011).
54. Li, R. Intervention study of fitness qigong-six-character technique on chronic obstructive pulmonary disease in older adults with stable stage. Beijing: Beijing Sports University (2018).
55. Yan, Y. Evaluation of therapeutic efficacy of six-character training of traditional Chinese medicine combined with conventional Western medicine for the treatment of chronic obstructive pulmonary disease. West Chin Med. (2021) 34:126–9.
56. Wang, ZW, Yang, PL, and Tang, J. A randomized controlled study of Chinese medicine pulmonary rehabilitation exercises on pulmonary function and acute exacerbation in COPD patients. China TCM Emerg. (2013) 22:23–4.
57. Quan, Y. Clinical study evaluating the effect of intensive six-character technique on respiratory function in stable COPD patients with lung and spleen Qi deficiency using breathing training as a control. Tianjin: Tianjin University of Traditional Chinese Medicine (2021).
58. Liu, X, Wu, W, Li, N, Li, P, Wang, Z, and Shan, C. Effects of water-based Liuzijue exercise on peak exercise capacity, functional exercise capacity, and quality of life in people with COPD. Clin Respir J. (2021) 15:956–66. doi: 10.1111/crj.13399
59. Zhang, M, Xv, G, Luo, C, Meng, D, and Ji, Y. Qigong Yi Jinjing promotes pulmonary function, physical activity, quality of life and emotion regulation self-efficacy in patients with chronic obstructive pulmonary disease: a pilot study. J Altern Complement Med. (2016) 22:810–7. doi: 10.1089/acm.2015.0224
60. Gao, E. Study on fitness qigong-Yi Jin Jing to promote pulmonary rehabilitation in patients with stabilized chronic obstructive pulmonary disease. Nanjing: Nanjing University of Traditional Chinese Medicine (2015).
61. Zhu, S, Shi, K, Yan, J, He, Z, Wang, Y, Yi, Q, et al. A modified 6-form tai chi in patients with COPD. Complement Ther Med. (2018) 39:36–42. doi: 10.1016/j.ctim.2018.05.007
62. Zhang, X, Cai, Y, Zhang, W, Chen, X, Jia, X, Zhang, X, et al. Effects of twenty-four-step taijiquan and adjunctive respiratory function training in Western medicine on stable chronic obstructive pulmonary disease. J Trad Chin Med. (2014) 55:1937–41.
63. Zhang, LH, Wu, JJ, and Wang, ZC. Effects of twenty-four forms of taijiquan combined with respiratory rehabilitation training on pulmonary function and quality of life of COPD patients. J Shanghai Univ Trad Chin Med. (2012) 26:53–6.
64. Yeh, GY, Litrownik, D, Wayne, PM, Beach, D, Klings, ES, Reyes Nieva, H, et al. BEAM study (Breathing, Education, Awareness, Movement): a randomised controlled feasibility trial of tai chi exercise in patients with COPD. BMJ open Respir Res. (2020) 7:e000697. doi: 10.1136/bmjresp-2020-000697
65. Wang, Y, Mo, J, Cheng, D, Liu, B, and Hu, X. Effects of tai chi exercise on survival quality and BODE index in patients with chronic obstructive pulmonary disease. Chin J Rehabil Med. (2014) 29:745–7.
66. Wang, L, Wu, K, Chen, X, and Liu, Q. The effects of tai chi on lung function, exercise capacity and health related quality of life for patients with chronic obstructive pulmonary disease: a pilot study. Heart Lung Circ. (2019) 28:1206–12. doi: 10.1016/j.hlc.2018.05.204
67. Polkey, MI, Qiu, ZH, Zhou, L, Zhu, MD, Wu, YX, Chen, YY, et al. Tai chi and Pulmonary rehabilitation compared for treatment-naive patients with COPD: a randomized controlled trial. Chest. (2018) 153:1116–24. doi: 10.1016/j.chest.2018.01.053
68. Niu, R, He, R, Luo, BL, and Hu, C. The effect of tai chi on chronic obstructive pulmonary disease: a pilot randomised study of lung function, exercise capacity and diaphragm strength. Heart Lung Circ. (2014) 23:347–52. doi: 10.1016/j.hlc.2013.10.057
69. Ng, L, Chiang, LK, Tang, R, Siu, C, Fung, L, Lee, A, et al. Effectiveness of incorporating tai chi in a pulmonary rehabilitation program for chronic obstructive pulmonary disease (COPD) in primary care—a pilot randomized controlled trial. Eur J Integr Med. (2014) 6:248–58. doi: 10.1016/j.eujim.2014.01.007
70. Yeh, GY, Roberts, DH, Wayne, PM, Davis, RB, Quilty, MT, and Phillips, RS. Tai chi exercise for patients with chronic obstructive pulmonary disease: a pilot study. Respir Care. (2010) 55:1475–82.
71. Moy, ML, Wayne, PM, Litrownik, D, Beach, D, Klings, ES, Davis, RB, et al. Long-term exercise after pulmonary rehabilitation (LEAP): a pilot randomised controlled trial of tai chi in COPD. ERJ Open Res. (2021) 7:00025–2021. doi: 10.1183/23120541.00025-2021
72. Kantatong, T, Panpanich, R, Deesomchok, A, Sungkarat, S, and Siviroj, P. Effects of the tai chi qigong programme on functional capacity, and lung function in chronic obstructive pulmonary disease patients: a ramdomised controlled trial. J Tradit Complement Med. (2020) 10:354–9. doi: 10.1016/j.jtcme.2019.03.008
73. Du, S, Ding, L, Wang, C, Yang, F, Xing, B, Liu, Z, et al. Effects of tai chi exercise on endurance and lung function in patients with chronic obstructive pulmonary disease. Chin J Rehabil Med. (2013) 28:374–6.
74. Chan, AW, Lee, A, Lee, DT, Suen, LK, Tam, WW, Chair, SY, et al. The sustained effects of tai chi qigong on physiological health for COPD patients: a randomized controlled trial. Complement Ther Med. (2013) 21:585–94. doi: 10.1016/j.ctim.2013.09.008
75. Zhang, Y, and Liu, D. Effects of twenty-four forms of taijiquan combined with respiratory rehabilitation training on lung function and quality of life in patients with chronic obstructive pulmonary disease. J Pract Chin Med. (2019) 35:350–1.
76. Cui, C, Xing, J, Yang, Y, and Li, J. Observation on the efficacy of home noninvasive ventilator combined with taijiquan in the treatment of stable chronic obstructive pulmonary disease. Chin J Clin. (2016) 44:96–8.
77. Li, F, Xing, JW, Zhang, HQ, Zhao, HZ, and Zhang, JM. Effects of tai chi combined with breathing training on quality of life in patients with stable COPD electronic. J Pract Clin Nurs. (2019) 4:36.
78. Li, S, Li, A, Sun, J, and Wang, H. Effects of Taijiquan rehabilitation on patients with chronic obstructive pulmonary disease. J Binzhou Med Coll. (2016) 39:275–7.
79. Li, Q, Fang, W, and Liu, C. Effect of taijiquan combined with respiratory function training on the rehabilitation of patients with stable chronic obstructive pulmonary disease. Chin J Rehabil Med. (2012) 27:825–8.
80. Pan, Y, Wang, Z, Min, J, Xiao, W, Huang, Y, Mao, B, et al. Evaluation of the efficacy of 24-posture simplified taijiquan in pulmonary rehabilitation during the stable phase of chronic obstructive pulmonary disease. Chin J Rehabil Med. (2018) 33:681–6.
81. Ren, Z, Zhang, X, Hou, C, Yang, B, Qian, X, Wang, Z, et al. Effects of tai chi Zen on the exercise capacity and quality of life in patients with COPD. Chin J Trad Chin Med. (2017) 32:3507–10.
82. He, N. Correlation study on the effect of Taiji mixed-element piles on lung function and quality of life in the stable stage of chronic obstructive pulmonary disease. Jinan: Shandong University of Traditional Chinese Medicine (2019).
83. Lu, Y, Li, J, Zhang, L, Guo, J, and Liu, S. Effects of fitness qigong Ba duan jin on quality of life and hospitalization satisfaction of patients with chronic obstructive pulmonary disease. China Med Herald. (2015) 12:161–4.
84. Feng, Y, Pan, H, Wen, X, Che, C, and Jiao, R. Efficacy of Ba Duan Jin exercise in elderly patients with stable chronic obstructive pulmonary disease. New Chin Med. (2009) 41:36–7.
85. Huang, B, Yao, Q, and Zhu, Y. Clinical observation of health qigong Ba Duan Jin on stable chronic obstructive pulmonary disease with lung and spleen deficiency. Hubei J Trad Chin Med. (2017) 39:4–6.
86. Yin, G. Clinical study on the effects of Ba Duan Jin and breathing exercises on the quality of life of patients with moderate to severe COPD. Guangzhou: Guangzhou University of Traditional Chinese Medicine, Guangdong Province (2013).
87. Chen, J, Deng, Y, Chen, Q, Zhang, W, and Deng, L. Effects of the third posture of the eight Duanjin on quality of life and exercise endurance of chronic obstructive pulmonary disease patients with lung, spleen, and qi deficiency. J Rehabil. (2015) 25:13–7.
88. Zhu, Z, and Chen, Y. Effects of seated eight-Duanjin exercise on pulmonary function in patients with COPD. World J Integr Chin West Med. (2014) 9:846–8.
89. Ng, BH, Tsang, HW, Jones, AY, So, CT, and Mok, TY. Functional and psychosocial effects of health qigong in patients with COPD: a randomized controlled trial. J Altern Complement Med. (2011) 17:243–51. doi: 10.1089/acm.2010.0215
90. Xu, Y, Wang, J, Li, H, Zhu, X, and Wang, G. Effects of rehabilitation training with Chinese and Western medicine on exercise capacity and quality of life of patients with chronic obstructive pulmonary disease: a randomized controlled clinical trial. J Integr Med. (2010) 8:432–7.
91. Huang, F, and Gao, Y. Application of Ba Duan Jin combined with respiratory training in the rehabilitation of community patients with chronic obstructive pulmonary disease. Nurs Pract Res. (2016) 13:146–7.
92. Chen, I. Effect of Badaanjin exercise rehabilitation nursing care on the rehabilitation of patients with chronic obstructive pulmonary disease. J Liaoning Univ Trad Chin Med. (2017) 19:213–5.
93. Chen, Y, Liu, S, Li, R, Zhang, X, Zhou, L, Yang, G, et al. Effects of fitness qigong eight-Duan Jin on lung function in patients with stable chronic obstructive pulmonary disease China traditional Chinese medicine. Mod Distance Educ. (2015) 13:16–8.
94. Zheng, Y. Clinical study of respiratory Baduanjin in patients with chronic obstructive pulmonary disease. Guangzhou: Guangzhou University of Traditional Chinese Medicine (2019).
95. Deng, Y. The effect of Baduanjin’s third part on chronic obstructive pulmonary disease stable patients with lung and spleen deficiency syndrome. Fujian: Fujian University of Traditional Chinese Medicine (2014).
96. Deng, W, Yang, L, Dong, H, and Zhang, W. Evaluation of the efficacy of Deng Lao’s eight Duan Jin in pulmonary rehabilitation for chronic obstructive pulmonary disease. Mass Rehabil Med. (2020) 11:41–4.
97. Zhang, L, Wang, T, Shi, L, Zou, Q, Zhu, T, Sun, Y, et al. Effect of eight-section brocade on therapeutics nutrition status and evaluation of cardiopulmonary function of chronic obstructive pulomonary disease rehabilitation by adjusting pectoral qi. J Changchun Univ Trad Chin Med. (2017) 33:954–6.
98. Sun, Y. Therapeutic efficacy of fitness qigong “Ba Duan Jin” in the treatment of patients with stabilized Grade II chronic obstructive pulmonary disease. Changchun: Changchun University of Traditional Chinese Medicine (2014).
99. Liu, S, and Chen, Y. Clinical study on health-qi-gong-Ba-duan-jin for the improvement of the 6min of patients with chronic obstructive pulmonary disease in stable period. Sichuan Med. (2013) 34:1090–2.
100. Ye, X. Effect of Baduanjin on the quality of life of elderly patients with chronic obstructive pulmonary disease in the stable stage. Contemp Nurse. (2016) 4:80–2.
101. Guo, J, Gao, Y, Xie, H, Fang, S, and Chen, G. The effect of Baduanjin exercise on the rehabilitation effect of patients with chronic obstructive pulmonary disease in the stabilized stage. Qilu Nurs J. (2016) 22:97–8.
102. Liang, X. Effect of a single lifting rehabilitation exercise performed by Ba Duan Jin on the rehabilitation of patients with chronic obstructive pulmonary disease. Nurs Pract Res. (2016) 13:156–7.
103. Pan, M, Luo, J, and Yang, S. Efficacy of standing Ba Duan Jin rehabilitation exercise in stabilized patients with chronic obstructive pulmonary disease. J Chengdu Univ Trad Chin Med. (2016) 39:49–52.
104. Pan, Z. Clinical efficacy observation of Chinese and Western medicine combined with pulmonary rehabilitation therapy in the treatment of patients with stable COPD. Guangzhou: Guangzhou University of Traditional Chinese Medicine (2019).
105. Xue, G, Feng, C, Yao, X, Qi, Y, and Wang, Y. Evaluation of the efficacy of fitness qigong Ba Duan Jin in pulmonary rehabilitation during the stabilization phase of chronic obstructive pulmonary disease. J Beijing Univ Chin Med. (2015) 38:139–44.
106. Yu, Y. Evaluation of the efficacy of fitness qigong Ba duan jin in pulmonary rehabilitation during the stabilization phase of chronic obstructive pulmonary disease. World Digest Recent Med Inf. (2019) 19:210–1.
107. Wang, L, and Fang, L. Effects of Ba Duan Jin on lung function during the stabilization period of chronic obstructive pulmonary disease. Chin Med Herald. (2018) 24:86–7.
108. Wang, Y, Wang, L, and Zheng, L. Effects of Ba Duan Jin combined with pulmonary rehabilitation training on pulmonary function in patients with stable COPD. China Rehabil. (2022) 37:232–5.
109. Yu, P, and Jiang, XF. Effect of qigong Ba Duan Jin exercise in patients with stabilized chronic obstructive pulmonary disease. J South Anhui Med Coll. (2019) 38:607–10.
110. Cao, C, Guo, X, Chen, N, Yan, X, and Zhang, H. Research of effects of eight-section brocade of TCM on treating anxiety and depression in the elderly patients with lung-spleen Qi deficiency in stable period of COPD. J Liaoning Univ Trad Chin Med. (2016) 18:120–3.
111. Wang, W, Qiu, Y, Huang, J, and Chen, M. Therapeutic efficacy observation and nursing care with moxibustion during the stabilization period of chronic obstructive pulmonary disease. Inner Mongolian Trad Chin Med. (2016) 35:69–70.
112. Li, B, Deng, Z, Dong, J, and Tong, X. Clinical efficacy of combined Chinese and Western medicine in the treatment of stable chronic obstructive pulmonary disease. J Hebei Med Univ. (2011) 32:10–3.
113. He, F, He, XF, and Mai, JQ. Combination of ginger moxibustion on Feishu (BL13) and Methoxyphenamine for chronic obstructive pulmonary disease in the remission stage: a report of 46 cases. Shanghai J Trad Chin Med. (2013) 47:54–5.
114. Cui, Y, Wang, J, Han, Q, Hou, Y, Wang, X, and Cao, J. Clinical observation on different Moxibustion on stationary phases chronic obstructive pulmonary disease. Guangming J Chin Medcine. (2017) 32:3601–3.
115. Liang, Y. Clinical observation of 44 patients with stable chronic obstructive pulmonary disease adjuvanted by acupoint heat sensitization suspended in moxibustion. J Trad Chin Med. (2018) 59:765–8.
116. Chen, G, Zhang, X, Yin, L, Hu, Z, Shuai, Y, and Hou, M. Efficacy of acupoint moxibustion combined with conventional Western medicine for the treatment of COPD and its effects on IL-6 and IL-8. Jiangxi Trad Chin Med. (2017) 48:53–5.
117. Fan, L, Lu, B, Chen, R, Zhang, M, Pan, X, and Zhou, Y. Clinical study on the treatment of chronic obstructive pulmonary disease in the stable stage by thunder fire moxibustion with identification of acupoints. Mod J Integr Chin West Med. (2021) 30:861–4.
118. Wang, X. Clinical efficacy of thermal moxibustion in the treatment of chronic obstructive pulmonary disease. Chinese Medicine Clin Res. (2011) 3:11–3.
119. Zhe, Y, Xue, Y, and Ni, X. Analysis of the effect of thermal moxibustion on the improvement of lung function and quality of life in patients with stable COPD. Pract Clin Med. (2017) 21:42–5.
120. Cheng, A, and Shu, C. Clinical study of “heat-sensitive point” moxibustion in the treatment of chronic obstructive pulmonary disease. Chin J Trad Chin Med. (2011) 29:1355–7.
121. Zhao, Y, Huang, B, and Zhu, Y. Observation of the therapeutic effect of moxibustion in treating lung, spleen, and kidney deficiency-type chronic obstructive pulmonary disease in the stable stage. Shaanxi Trad Chin Med. (2018) 34:25–7.
122. Na, L. Efficacy in chronic obstructive pulmonary disease patients at stable stage treated with Yi Fei Moxibustion. Henan: Henan College of Traditional Chinese Medicine (2015).
123. Huang, Y. Effectiveness of beneficial lung moxibustion used in the care of stable COPD patients and its effect on patients’ 6 min walking distance and dyspnea. Guangming Trad Chin Med. (2021) 36:4264–7.
124. Han, S. Clinical observation on moxibustion treatment of chronic obstructive pulmonary disease with deficiency of lung and kidney qi. Guangming Trad Chin Med. (2017) 32:2080–2.
125. Qian, H. Evaluation of the efficacy of beneficial lung Moxibustion in the treatment of lung and kidney Qi deficiencies in the stabilized stage of chronic obstructive pulmonary disease. Henan: Henan College of Traditional Chinese Medicine (2014).
126. Yang, X, and Fu, D. Observations on the therapeutic effect of acupuncture and moxibustion in treating chronic obstructive pulmonary disease with lung and kidney qi deficiency. People's Mil Med. (2016) 59:1036–7.
127. Cui, XX, and Liang, GL. Treatment of 60 cases of chronic obstructive pulmonary disease with lung and kidney qi deficiencies using Chinese medicine benefited from moxibustion. Clin Res Trad Chin Med. (2015) 7:10–2.
128. Zhou, QW, and Yang, QM. Moxibustion on the governor vessel for lung and kidney qi deficiency type in chronic obstructive pulmonary disease: a randomized controlled trial. Zhongguo Zhen Jiu. (2011) 31:31–4.
129. Zhang, JH, and Zhong, LH. Clinical observations of the treatment of lung-kidney-qi deficiency-type chronic obstructive pulmonary disease in remission by moxibustion. New Chin Med. (2012) 44:117–8.
130. Xu, J, Wu, Q, Liu, Y, Chen, L, Lin, X, and Zhang, L. Effects of fire-dragon moxibustion on lung function and quality of survival in patients with lung-kidney-qi deficiency syndrome in the stable stage of chronic obstructive pulmonary disease. J Guangzhou Univ Trad Chin Med. (2022) 39:593–9.
131. Rocha, T, Souza, H, Brandão, DC, Rattes, C, Ribeiro, L, Campos, SL, et al. The manual diaphragm release technique improves diaphragmatic mobility, inspiratory capacity and exercise capacity in people with chronic obstructive pulmonary disease: a randomised trial. J Physiother. (2015) 61:182–9. doi: 10.1016/j.jphys.2015.08.009
132. Noll, DR, Degenhardt, BF, Johnson, JC, and Burt, SA. Immediate effects of osteopathic manipulative treatment in elderly patients with chronic obstructive pulmonary disease. J Am Osteopath Assoc. (2008) 108:251–9.
133. Maskey-Warzechowska, M, Mierzejewski, M, Gorska, K, Golowicz, R, Jesien, L, and Krenke, R. Effects of osteopathic manual therapy on hyperinflation in patients with chronic obstructive pulmonary disease: a randomized Cross-over study. Adv Exp Med Biol. (2019) 1222:17–25. doi: 10.1007/5584_2019_418
134. Kurzaj, M, Wierzejski, W, Dor, A, Stawska, J, and Rożek, K. The impact of specialized physiotherapy methods on BODE index in patients with COPD patients during hospitalization. Adv Clin Exp Med. (2013) 22:721–30.
135. Buran Cirak, Y, Yilmaz Yelvar, GD, and Durustkan Elbasi, N. Effectiveness of 12-week inspiratory muscle training with manual therapy in patients with COPD: a randomized controlled study. Clin Respir J. (2022) 16:317–28. doi: 10.1111/crj.13486
136. Chen, Q, Zhong, LW, Liu, HB, Zhang, JF, Xie, GG, Jin, XQ, et al. Efficacy of massage therapy for chronic obstructive pulmonary disease. China Clin Rehab. (2006) 7:10–2.
137. Suzuki, M, Namura, K, Ohno, Y, Tanaka, H, Egawa, M, Yokoyama, Y, et al. The effect of acupuncture in the treatment of chronic obstructive pulmonary disease. J Altern Complement Med. (2008) 14:1097–105. doi: 10.1089/acm.2007.0786
138. Liu, L, Shi, M, Song, X, Zhang, W, and Jiang, C. Clinical effect observation on acupuncture for chronic obstructive pulmonary disease. J Acupunct Tuina Sci. (2015) 13:306–11. doi: 10.1007/s11726-015-0872-4
139. Deering, BM, Fullen, B, Egan, C, McCormack, N, Kelly, E, Pender, M, et al. Acupuncture as an adjunct to pulmonary rehabilitation. J Cardiopulm Rehabil Prev. (2011) 31:392–9. doi: 10.1097/HCR.0b013e31822f0f61
140. Suzuki, M, Muro, S, Ando, Y, Omori, T, Shiota, T, Endo, K, et al. A randomized placebo-controlled trial of acupuncture in patients with chronic obstructive pulmonary disease (COPD): the COPD-acupuncture trial (CAT). Arch Intern Med. (2012) 172:878–86. doi: 10.1001/archinternmed.2012.1233
141. Li, Y, Xiong, C, Zeng, Y, Wei, H, Zhuang, G, Zhao, L, et al. Acupuncture treatment of lung-spleen qi deficiency in stable chronic obstructive pulmonary disease: a randomized, open-label, controlled trial. J Tradit Chin Med. (2019) 39:885–91.
142. Feng, J, Wang, X, Li, X, Zhao, D, and Xu, J. Acupuncture for chronic obstructive pulmonary disease (COPD): a multicenter, randomized, sham-controlled trial. Medicine. (2016) 95:e4879. doi: 10.1097/MD.0000000000004879
143. Zhong, G. Clinical observation on Bo’s abdominal acupuncture for chronic obstructive pulmonary disease with kidney deficiency and insufficiency. New Chin Med. (2018) 50:190–2.
144. Deng, C, Zhang, D, and Wang, N. Application of abdominal acupuncture to treat 22 cases of stable chronic obstructive pulmonary disease. Yunnan J Trad Chin Med. (2016) 37:73–4.
145. Yang, JS, and Li, J. Evaluation of the efficacy of acupuncture on lung function and quality of life in patients with stable COPD. J Hubei Univ Trad Chin Med. (2018) 20:30–3.
146. Jiao, L. Acupuncture of lung Yu and Diaphragm Yu points to the treatment of 30 cases of chronic obstructive pulmonary disease in the stable stage. Res Trad Chin Med. (2020) 33:60–3.
147. Tang, G. Observations on the effect of acupuncture on the quality of life of patients during the stabilization period of COPD treated with ascending and Dispersing Square Acupoints. Master's thesis,. Fujian: Fujian University of Traditional Chinese Medicine (2017).
148. Li, D, and Liu, GY. Preventive value of tiotropium bromide combined with acupuncture against acute relapse in patients with stable COPD. Chin Health. (2020) 19:636–8.
149. Wang, X, and Wang, H. Effects of Pei Tu sheng Jin acupuncture therapy for chronic obstructive pulmonary disease on patients’ lung function and oxygen saturation. Acupunct Clin J. (2021) 37:27–31.
150. Ngai, SP, Jones, AY, Hui-Chan, CW, Ko, FW, and Hui, DS. Effect of 4 weeks of Acu-TENS on functional capacity and beta-endorphin level in subjects with chronic obstructive pulmonary disease: a randomized controlled trial. Respir Physiol Neurobiol. (2010) 173:29–36. doi: 10.1016/j.resp.2010.06.005
151. Liu, X, Fan, T, Lan, Y, Dong, S, Fu, J, and Mao, B. Effects of transcutaneous electrical acupoint stimulation on patients with stable chronic obstructive pulmonary disease: a prospective, single-blind, randomized, placebo-controlled study. J Altern Complement Med. (2015) 21:610–6. doi: 10.1089/acm.2014.0284
152. Lau, KS, and Jones, AY. A single session of Acu-TENS increased FEV1 and reduces dyspnoea in patients with chronic obstructive pulmonary disease: a randomised, placebo-controlled trial. Aust J Physiother. (2008) 54:179–84. doi: 10.1016/s0004-9514(08)70024-2
153. Jones, AY, Ngai, SP, Hui-Chan, CW, and Yu, HP. Acute effects of Acu-TENS on FEV1 and blood Β-endorphin level in chronic obstructive pulmonary disease. Altern Ther Health Med. (2011) 17:8–13.
154. Yang, JG. Effect of Sanjiu warm acupuncture on the quality of life of patients with stable COPD. Fujian: Fujian University of Traditional Chinese Medicine (2016).
155. Li, X. Clinical efficacy observation of warm acupuncture in the treatment of patients with stable COPD in three-volt day. Fujian: Fujian University of Traditional Chinese Medicine (2015).
156. Shi, Z, Ni, T, and Wang, X. Clinical study of warm acupuncture combined with salmeterol ticlopidine powder inhaler for the treatment of stable chronic obstructive pulmonary disease. New Chin Med. (2021) 53:150–3.
157. Pang, C, and Lai, Z. Effects of tonifying the kidney and strengthening the spleen on the nutritional status of COPD patients with spleen and kidney deficiencies. Guangming Trad Chin Med. (2014) 29:1863–4.
158. Li, D, Hong, X, and Huang, R. Effect of Meridian flow injection and time-selective auricular acupressure on the rehabilitation effect of patients with chronic obstructive pulmonary disease. J Nurs Peoples Lib Army. (2017) 34:31–4.
159. Jin, R, Lu, Y, and Liu, G. Effect of auricular acupressure on clinical evidence and quality of life in chronic obstructive pulmonary disease. Chin J Trad Chin Med. (2009) 27:1283–4.
160. He, Y, Li, GY, Zheng, ZG, Gao, Y, Pan, JH, Wang, F, et al. Effect of electroacupuncture on small airway function in patients with stable chronic obstructive pulmonary disease. Zhongguo Zhen Jiu. (2021) 41:861–5. doi: 10.13703/j.0255-2930.20200813-0001
161. Ge, Y, Yao, H, Tong, J, He, Y, Li, G, and Kong, X. Effects of acupuncture on peripheral skeletal muscle exercise ability in patients with chronic obstructive pulmonary disease at stable phase. Zhongguo Zhen Jiu. (2017) 37:366–71. doi: 10.13703/j.0255-2930.2017.04.005
162. Chen, L. The use of snap-needles combined with seated breathing exercises improves lung function in patients with COPD. Smart Health. (2018) 4:84–5.
163. Peng, H. Study on the effect of intradermal needle therapy of Wuqi Yu on the quality of life of patients with stable COPD. Chengdu: Chengdu University of Traditional Chinese Medicine (2015).
164. Wang, Y, Wang, H, and Pang, Y. Clinical study of snap-needle treatment for chronic obstructive pulmonary disease in remission. World Latest Med Inf. (2019) 19:47–9.
165. Tuo, J, Nong, M, Guo, J, Wu, G, Lai, H, and Huang, N. Effects of Meridian flow injection and time-selective acupressure on the rehabilitation effect of patients with chronic obstructive pulmonary disease. Integr Nurs Chin West Med. (2018) 4:66–9.
166. HajGhanbari, B, Garland, SJ, Road, JD, and Reid, WD. Pain and physical performance in people with COPD. Respir Med. (2013) 107:1692–9. doi: 10.1016/j.rmed.2013.06.010
167. Jaitovich, A, and Barreiro, E. Skeletal muscle dysfunction in chronic obstructive pulmonary disease. What we know and can do for our patients. Am J Respir Crit Care Med. (2018) 198:175–86. doi: 10.1164/rccm.201710-2140CI
168. Spruit, MA, Singh, SJ, Garvey, C, Zuwallack, R, Nici, L, Rochester, C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. (2013) 188:e13–64. doi: 10.1164/rccm.201309-1634ST
169. Kaneko, H, Shiranita, S, Horie, J, and Hayashi, S. Reduced chest and abdominal wall mobility and their relationship to lung function, respiratory muscle strength, and exercise tolerance in subjects with COPD. Respir Care. (2016) 61:1472–80. doi: 10.4187/respcare.04742
170. Lee, NW, Kim, GH, Heo, I, Kim, KW, Ha, IH, Lee, JH, et al. Chuna (or Tuina) manual therapy for musculoskeletal disorders: Adi systematic review and Meta-analysis of randomized controlled trials. Evid Based Complement Alternat Med. (2017) 2017:8218139. doi: 10.1155/2017/8218139
171. Moon, TW, Choi, TY, Park, TY, and Lee, MS. Chuna therapy for musculoskeletal pain: a systematic review of randomized clinical trials in Korean literature. Chin J Integr Med. (2013) 19:228–32. doi: 10.1007/s11655-012-1238-0
172. Li, Z, Liu, S, Wang, L, and Smith, L. Mind-body exercise for anxiety and depression in COPD patients: a systematic review and meta-analysis. Int J Environ Res Public Health. (2019) 17:22. doi: 10.3390/ijerph17010022
173. Wu, LL, Lin, ZK, Weng, HD, Qi, QF, Lu, J, and Liu, KX. Effectiveness of meditative movement on COPD: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis. (2018) 13:1239–50. doi: 10.2147/COPD.S159042
174. Jahnke, R, Larkey, L, Rogers, C, Etnier, J, and Lin, F. A comprehensive review of health benefits of qigong and tai chi. Am J Health Promot. (2010) 24:e1–e25. doi: 10.4278/ajhp.081013-LIT-248
175. Yang, FM, Yao, L, Wang, SJ, Guo, Y, Xu, ZF, Zhang, CH, et al. Current tracking on effectiveness and mechanisms of acupuncture therapy: a literature review of high-quality studies. Chin J Integr Med. (2020) 26:310–20. doi: 10.1007/s11655-019-3150-3
176. Jo, HR, Noh, EJ, Oh, SH, Choi, SK, Sung, WS, Choi, SJ, et al. Comparative effectiveness of different acupuncture therapies for neck pain. Medicine. (2022) 101:e29656. doi: 10.1097/MD.0000000000029656
177. Ferreira, RM, Torres, RT, Duarte, JA, and Gonçalves, RS. Non-pharmacological and non-surgical interventions for knee osteoarthritis: a systematic review and meta-analysis. Acta Reumatol Port. (2019) 44:173–217.
178. Zhang, M, Guan, L, Wang, L, and Li, Y. Effect of scar-producing moxibustion at the acupoints Zusanli (ST 36) and Feishu (BL 13) on neutrophil-to-lymphocyte ratio and quality of life in patients with non-small-cell lung cancer: a randomized controlled trial. J Tradit Chin Med. (2018) 38:439–46. doi: 10.1016/S0254-6272(18)30636-8
179. Cheng, L, Li, R, Zhou, M, Li, F, Chang, Q, Li, C, et al. Moxibustion has a positive effect on pulmonary fibrosis: an alternative approach. Afr J Tradit Complement Altern Med. (2017) 14:125–9. doi: 10.21010/ajtcam.v14i2.13
180. Qiao, Y, Lei, HT, Yi, W, Zhao, CJ, Xia, X, Zhou, B, et al. Intervention mechanism of moxa-cone moxibustion at Shu- and mu-acupoints on the expression of RORγt/Foxp3 in asthma mice: an analysis based on PI3K signaling pathway. Zhen Ci Yan Jiu. (2021) 46:272–7. doi: 10.13702/j.1000-0607.200491
181. Jung, D, Lee, S, and Hong, S. Effects of acupuncture and moxibustion in a mouse model of allergic rhinitis. Otolaryngol Head Neck Surg. (2012) 146:19–25. doi: 10.1177/0194599811421736
182. Jia, YJ, Li, TY, Han, P, Chen, Y, Pan, LJ, and Jia, CS. Effects of different courses of moxibustion treatment on intestinal flora and inflammation of a rat model of knee osteoarthritis. J Integr Med. (2022) 20:173–81. doi: 10.1016/j.joim.2022.01.004
183. Cheng, Y, Chen, Q, Huang, R, Lao, C, and Fu, W. Moxibustion treatment increases the survival rate of lung infection of patients bed-ridden due to osteoporotic fracture of the spine via regulation of the inflammatory responses. Arch Med Sci. (2023) 19:258–63. doi: 10.5114/aoms/155982
184. Xu, ZF, Gong, YN, Dou, BM, Fan, ZZ, and Zhang, Y. Current situation and prospect of researches on regularities and mechanisms of acupuncture-moxibustion in alleviating chronic inflammatory response. Zhen Ci Yan Jiu. (2023) 48:111–7. doi: 10.13702/j.1000-0607.20221095
185. Jiao, Z, Gu, Y, Li, L, Zong, L, Zhang, Q, and Liang, Y. Regulation effect of Moxibustion with small Moxa-cone about the size of a wheat grain at “Zusanli” point on cellular immune function in elderly bedridden patients. Chin J Trad Med Sci Technol. (2020) 27:59–60.
186. Zhao, Y, Li, TG, Pu, R, Shui, L, Lu, J, and Chen, YS. Effect of moxibustion on body weight and peripheral and cerebral cortical IL-6 and IL-10 levels in fatigue rats. Zhen Ci Yan Jiu. (2020) 45:215–9. doi: 10.13702/j.1000-0607.190815
187. Xu, J, Pan, LJ, and Jia, CS. Exploration on the feasibility of moxibustion in prevention and treatment of COVID-19 from the perspective of modern medical mechanism. World J Acupunct Moxibustion. (2020) 30:81–4. doi: 10.1016/j.wjam.2020.06.001
188. Li, Q, Wang, W, Ma, Q, Xia, R, Gao, B, Zhu, G, et al. Moxibustion improves chronic heart failure by inhibiting autophagy and inflammation via upregulation of mTOR expression. Evid Based Complement Alternat Med. (2021) 2021:6635876–12. doi: 10.1155/2021/6635876
189. Zijlstra, FJ, van den Berg-de Lange, I, Huygen, FJ, and Klein, J. Anti-inflammatory actions of acupuncture. Mediat Inflamm. (2003) 12:59–69. doi: 10.1080/0962935031000114943
190. Zhang, B, Shi, H, Cao, S, Xie, L, Ren, P, Wang, J, et al. Revealing the magic of acupuncture based on biological mechanisms: a literature review. Biosci Trends. (2022) 16:73–90. doi: 10.5582/bst.2022.01039
191. Li, Y, Wu, F, Cheng, K, Shen, XY, and Lao, LX. Mechanisms of acupuncture for inflammatory pain. Zhen Ci Yan Jiu. (2018) 43:467–75. doi: 10.13702/j.1000-0607.180196
192. Tang, W, Dong, M, Teng, F, Cui, J, Zhu, X, Wang, W, et al. TMT-based quantitative proteomics reveals suppression of SLC3A2 and ATP1A3 expression contributes to the inhibitory role of acupuncture on airway inflammation in an OVA-induced mouse asthma model. Biomed Pharmacother. (2021) 134:111001. doi: 10.1016/j.biopha.2020.111001
193. He, M, Qin, W, Qin, Z, and Zhao, C. Acupuncture for allergic rhinitis: a systematic review and meta-analysis. Eur J Med Res. (2022) 27:58. doi: 10.1186/s40001-022-00682-3
194. Pei, L, Geng, H, Guo, J, Yang, G, Wang, L, Shen, R, et al. Effect of acupuncture in patients with irritable bowel syndrome: a randomized controlled trial. Mayo Clin Proc. (2020) 95:1671–83. doi: 10.1016/j.mayocp.2020.01.042
195. Chen, T, Zhang, WW, Chu, YX, and Wang, YQ. Acupuncture for pain management: molecular mechanisms of action. Am J Chin Med. (2020) 48:793–811. doi: 10.1142/S0192415X20500408
196. Langevin, HM, Churchill, DL, Wu, J, Badger, GJ, Yandow, JA, Fox, JR, et al. Evidence of connective tissue involvement in acupuncture. FASEB J. (2002) 16:872–4. doi: 10.1096/fj.01-0925fje
197. Jiang, XM, Zhang, XQ, and Yuan, L. Advances in the study on the role of connective tissue in the mechanical signal transduction of acupuncture. Zhen Ci Yan Jiu. (2009) 34:136–9.
198. Lin, J, Gao, YF, Guo, Y, Li, M, Zhu, Y, You, R, et al. Effects of qigong exercise on the physical and mental health of college students: a systematic review and meta-analysis. BMC Complement Med Ther. (2022) 22:287. doi: 10.1186/s12906-022-03760-5
199. Clark, NG, Hill, CJ, Koppenhaver, SL, Massie, T, and Cleland, JA. The effects of dry needling to the thoracolumbar junction multifidi on measures of regional and remote flexibility and pain sensitivity: a randomized controlled trial. Musculoskelet Sci Pract. (2021) 53:102366. doi: 10.1016/j.msksp.2021.102366
200. Comachio, J, Oliveira, CC, Silva, IFR, Magalhães, MO, and Marques, AP. Effectiveness of manual and electrical acupuncture for chronic non-specific low back pain: a randomized controlled trial. J Acupunct Meridian Stud. (2020) 13:87–93. doi: 10.1016/j.jams.2020.03.064
201. Vickers, AJ, Vertosick, EA, Lewith, G, MacPherson, H, Foster, NE, Sherman, KJ, et al. Acupuncture for chronic pain: update of an individual patient data meta-analysis. J Pain. (2018) 19:455–74. doi: 10.1016/j.jpain.2017.11.005
202. Trinh, K, Graham, N, Irnich, D, Cameron, ID, and Forget, M. Acupuncture for neck disorders. Cochrane Database Syst Rev. (2016) 5:CD004870. doi: 10.1002/14651858.CD004870.pub4
203. Ben-Arie, E, Kao, PY, Lee, YC, Ho, WC, Chou, LW, and Liu, HP. The effectiveness of acupuncture in the treatment of frozen shoulder: a systematic review and Meta-analysis. Evid Based Complement Alternat Med. (2020) 2020:9790470. doi: 10.1155/2020/9790470
204. Chen, X, Cui, J, Li, R, Norton, R, Park, J, Kong, J, et al. Origin, development, potential mechanisms, and clinical applications. Evid Based Complement Alternat Med. (2019) 2019:1–11. doi: 10.1155/2019/3705120
205. Núñez-Cortés, R, Padilla-Acevedo, P, Vergara-Peña, F, Mollà-Casanova, S, Espinoza-Bravo, C, Torres-Castro, R, et al. Clinical assessment of balance and functional impairments in people with stable chronic obstructive pulmonary disease: a systematic review and meta-analysis. ERJ Open Res. (2022) 8:00164–2022. doi: 10.1183/23120541.00164-2022
206. Chang, PS, Knobf, MT, Funk, M, and Oh, B. Feasibility and acceptability of qigong exercise in community-dwelling older adults in the United States. J Altern Complement Med. (2018) 24:48–54. doi: 10.1089/acm.2017.0096
207. Li, J, Yu, M, Wang, Y, Li, S, Li, S, Feng, X, et al. Baduanjin for ischemic heart failure with mildly reduced/preserved ejection fraction (BEAR trial): a randomized controlled trial. J Evid Based Med. (2024) 17:526–34. doi: 10.1111/jebm.12631
208. Chen, X, Savarese, G, Cai, Y, Ma, L, Lundborg, CS, Jiang, W, et al. Tai chi and Qigong practices for chronic heart failure: a systematic review and Meta-analysis of randomized controlled trials. Evid Based Complement Alternat Med. (2020) 2020:2034625. doi: 10.1155/2020/2034625
209. Xu, J, Li, X, Zeng, J, Zhou, Y, Li, Q, Bai, Z, et al. Effect of Baduanjin qigong on postoperative pulmonary rehabilitation in patients with non-small cell lung cancer: a randomized controlled trial. Support Care Cancer. (2023) 32:73. doi: 10.1007/s00520-023-08194-4
210. Liu, X, Pan, F, Wang, Q, Wang, S, and Zhang, J. Traditional Chinese rehabilitation exercise (TCRE) for myofascial pain: current evidence and further challenges. J Pain Res. (2024) 17:2801–10. doi: 10.2147/JPR.S482424
211. Bai, Z, Guan, Z, Fan, Y, Liu, C, Yang, K, Ma, B, et al. The effects of qigong for adults with chronic pain: systematic review and Meta-analysis. Am J Chin Med. (2015) 43:1525–39. doi: 10.1142/S0192415X15500871
212. Ding, M, Zhang, W, Li, K, and Chen, X. Effectiveness of t'ai chi and qigong on chronic obstructive pulmonary disease: a systematic review and meta-analysis. J Altern Complement Med. (2014) 20:79–86. doi: 10.1089/acm.2013.0087
213. Tong, H, Liu, Y, Zhu, Y, Zhang, B, and Hu, J. The therapeutic effects of qigong in patients with chronic obstructive pulmonary disease in the stable stage: a meta-analysis. BMC Complement Altern Med. (2019) 19:239. doi: 10.1186/s12906-019-2639-9
214. Park, J, Kwon, M, Lee, BJ, Kim, KI, and Jung, HJ. The effectiveness and safety of chuna manual therapy adjuvant to western medicine in patients with chronic obstructive pulmonary disease: a randomized, single-blind, investigator-initiated, pilot trial. Health Care. (2024) 12:152. doi: 10.3390/healthcare12020152
215. MacPherson, H, Altman, DG, Hammerschlag, R, Youping, L, Taixiang, W, White, A, et al. Revised STandards for reporting interventions in clinical trials of acupuncture (STRICTA): extending the CONSORT statement. PLoS Med. (2010) 7:e1000261. doi: 10.1371/journal.pmed.1000261
Keywords: chronic obstructive pulmonary disease, non-pharmacological treatment, AddOn, systematic review, network meta-analysis
Citation: Roh J-A, Leem J, Lee B-J, Kim K-I and Jung H-J (2025) Comparative efficacy of traditional non-pharmacological add-on treatments in patients with stable chronic obstructive pulmonary disease: a systematic review and network meta-analysis. Front. Public Health. 13:1410342. doi: 10.3389/fpubh.2025.1410342
Received: 01 April 2024; Accepted: 31 January 2025;
Published: 21 February 2025.
Edited by:
Manuel Zeitelhofer, Karolinska Institutet (KI), SwedenReviewed by:
Marcos Edgar Herkenhoff, University of São Paulo, BrazilCopyright © 2025 Roh, Leem, Lee, Kim and Jung. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kwan-Il Kim, bXloYXBweTc4QG5hdmVyLmNvbQ==; S3dhbmlsa2ltQGtodS5hYy5rcg==; Hee-Jae Jung, aGFuZmlzaEBraG1jLm9yLmty
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.