
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 19 February 2025
Sec. Children and Health
Volume 13 - 2025 | https://doi.org/10.3389/fpubh.2025.1377745
 Bo Zhou1†
Bo Zhou1† Qi Xu1†
Qi Xu1† Shaoli Li1†
Shaoli Li1† Jianhong Wang1†
Jianhong Wang1† Junting Liu1,2
Junting Liu1,2 Ting Zhang3
Ting Zhang3 Xia Qu1
Xia Qu1 Xi Wang1
Xi Wang1 Lili Zhang1
Lili Zhang1 Xiaoli Liu1
Xiaoli Liu1 Jialu Gu1
Jialu Gu1 Lijun Zhou1
Lijun Zhou1 Fangfang Chen4
Fangfang Chen4 Xinnan Zong5
Xinnan Zong5 Wenquan Niu6*
Wenquan Niu6* Lin Wang1*
Lin Wang1*Purpose: The aim of this prospective study was to assess the dynamic changes of persisting symptoms among children aged 6–18 years during 1–2 months after the Omicron infection based on the modified SBQ-LC in the Tongzhou cohort, Beijing.
Methods: This study includes 4 serial surveys performed within January 7–9, January 14–16, January 21–23, and February 12–14 in 2023, respectively. The prediction of age and survey for eight domains in the Rasch 0–100 linear score was undertaken by generalized additive mixed model.
Results: Total 1,536 children (median age: 13 years, boys: 49.9%) had completed questionnaires across 4 surveys. Information on 51 symptoms was collected, with each scored on a 4-point rating scale. Generally, the distribution of age with all domains followed the N-shaped geometry, and that of survey followed the inverse J-shaped geometry. The Rasch linear score hit the lowest level among children aged 6–8 years, and reached the peak among children aged 12–13 years. The scores of all domains sharply declined from the first to the third survey, and remained stable between the third and the fourth survey. At the fourth survey, 95.05 and 51.37% children still had one or more problems relating to breathing and mental health, respectively, and the percentage of rest six domains was reduced to less than 20%.
Conclusion: Our findings indicate the multifaceted impact of Omicron infection on childhood health, especially among children aged 12–13 years. Moreover, breathing and mental health related problems still persisted during 1-to-2-month Omicron infection period.
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has made a serious public health threat worldwide spreading to over 200 countries globally and infecting millions of people of all ages. Since firstly reported on November 9, 2021, the highly-contagious Omicron variant has swiftly swept around the world (1). In China, the fight against Omicron has lasted nearly a whole year, and on December 8, 2022, the epidemic prevention and control policy was officially optimized by releasing the zero-COVID approaches and lifting mandatory quarantine measures. As expected, the sudden arrival of Omicron has fueled a surge in coronavirus-infected cases across China, affecting all age groups, including children (2, 3). In spite of stronger transmission and immune escape abilities, Omicron infection is associated with shorter recovery time and lower fatality rate, and it seems that Omicron variants affect a large proportion of the younger population with the appearance of clinical manifestations similar to adults (4–6). The majority of children have fully recovered within 1 month following Omicron infection, yet a fraction of them still experienced one or more unexplained persistent residual or new-onset symptoms afterwards. These symptoms, collectively termed as long COVID or post-COVID sequelae, have constituted a major public health issue in the post-pandemic era (7). On average, one in four children experienced long COVID, which can more or less cause damage to many organ systems, possibly via fatigue, post-exertional dyspnea, headache, or sleep disorders (8). For example, Hassan and colleagues have conducted an excellent meta-analysis on the prevalence of mental health problems among children with post-COVID sequelae, by demonstrating that the higher prevalence of anxiety, depression and appetite problems among infected children than those uninfected might be attributable to long COVID (9). Moreover, a national cross-sectional study from Israel showed that symptoms including headache, weakness, fatigue and abdominal pain were more common among children with COVID infection than those without (10). Thus far, evidence on post-Omicron symptoms in children is primarily based on cross-sectional observations or case series, and a dynamic continuum for these symptoms are lacking. What’s more, a literature search has failed to reveal any evidence from Chinese children on this subject.
To fill this gap in knowledge and yield more reference for following investigations, we adopted the modified Symptom Burden Questionnaire for long COVID (SBQ-LC) (11) and prospectively surveyed children and adolescents 6–18 years of age in the Tongzhou district, Beijing from January 7 to February 14, 2023 at four serial intervals, aiming to assess the dynamic changes of persisting symptoms after Omicron waves from eight domains.
This is a prospective study involving four cross-sectional surveys performed on January 7–9, January 14–16, January 21–23 and February 12–14, respectively, in parallel to post-Omicron 2–3 weeks, 3–4 weeks, 4–5 weeks, and 8–9 weeks. The conduct of this study was reviewed and approved by the Ethics Committee at the Capital Institute of Pediatrics (Beijing, China), and informed consent was obtained from the parents or major supervisors of all study participants.
The data for this study were obtained from the Beijing Children and Adolescents Health Cohort conducted from 2022 to 2023, which was a prospective cohort study design established in Tongzhou district of Beijing. The cohort consisted of three primary, three junior and three high schools. Two classes of each grade in each school were randomly selected for cluster sampling survey. All school-aged children 6–18 years were surveyed using online questionnaires implemented on the Wenjuanxing platform.1 Questionnaires, circulated four times following the Omicron waves, were filled out by the parents or major supervisors of children involved. Children were excluded from this study if they were clinically diagnosed to have respiratory, digestive, cardiovascular, psychological and behavioral diseases prior to COVID-19 infection.
Initially, 2,900 children were surveyed, and due to incomplete information across four surveys, only 1,536 children formed the present analytical cohort. The study profile was described in Figure 1.
The questionnaire used in this study referred to the SBQ-LC version 1.0 (11), a comprehensive patient reported outcome instrument developed using modern psychometric methods. Considering that the SBQ-LC is primarily designed for adults, only domains suitable for children were selected. Specially, the original SBQ-LC was constructed based on 123 symptoms from 16 domains, and the modified SBQ-LC for children on 51 symptoms from 8 domains, that is, breathing (n = 7), pain (n = 4), circulation (n = 5), fatigue (n = 4), memory and thinking and communication (n = 10), movement (n = 3), muscles and joints (n = 9) and mental health (n = 9). Symptoms referred to the best description of experience over the last 7 days, and were scored on 4-point scales according to symptom severity, with 0 being none, 1 being mild, 2 being moderate and 3 being severe. The scale raw score of each domain was conversed to the Rasch 0–100 linear score, with higher scale scores denoting greater symptom burden for each domain. The 51 symptoms were translated into Chinese language with maintained integrity.
To avoid duplicated reports, the same device (smart phone) can be used only once to complete questionnaires at each survey. No personal information including names and identification number was covered in the questionnaire to ensure total anonymity and honest responses. In addition, to ensure information integrity, submitting questionnaires cannot be performed until the competition of all items. The questionnaire settings provided control over the questionnaires and prevented respondents from random selection.
Continuous data are expressed as mean (standard deviation) in the case of normal distributions or as median (interquartile range) in the case of skewed distributions. Categorical data are expressed as count (percent). Difference of continuous data between four surveys was tested by using the Analysis of Variance (ANOVA), and that of categorical data using the χ2-test. The joint distribution of age and sex was displayed by pyramid plot. Correlation of scale scores of eight domains was evaluated by the Spearman correlation coefficients upon stratified by surveys and displayed separately using heat maps. The prediction of age and survey for eight domains in the Rasch 0–100 linear score was undertaken by means of generalized additive mixed model, with knot values specified as 4 and using the Gaussian function with identity link. The age and survey were explored as smoothed factors, and sex as non-smoothed factor. Two-dimension (age or survey with each domain in the modified SBQ-LC) and three-dimension (age, survey and each domain) were depicted to inspect underlying nonlinear changes. The distribution of symptom combination within each domain was inspected using the Venn plot for four surveys. Statistical analyses and data representation were completed using the R programming language version 4.3.0 implemented under the Integrated Development Environment RStudio version 2023.03.1.
Of all study participants, 1,536 children had completed information across 4 surveys, and their basic characteristics and symptom distributions are shown in Table 1. The median age of 1,536 study children was 13 years, and 49.9% of them were boys. In total, 51 symptoms were surveyed, and each was scored on a 4-point rating scale.
The changes on the presence of any post-Omicron symptoms between the first and fourth survey are provided in Figure 2. On the first survey following Omicron waves, 96.22% children reported the presence of breathing-related problems, 90.49% mental health-related problems, 72.98% fatigue-related problems, 45.64% memory-related problems, 43.03% muscles and joints-related problems, 39.52% circulation-related problems, 23.11% movement-related problems and 22.53% pain-related problems. On the fourth survey, 95.05 and 51.37% of children still had one or more problems relating to breathing and mental health, respectively, and the percentage of rest six domains was reduced to less than 20%.
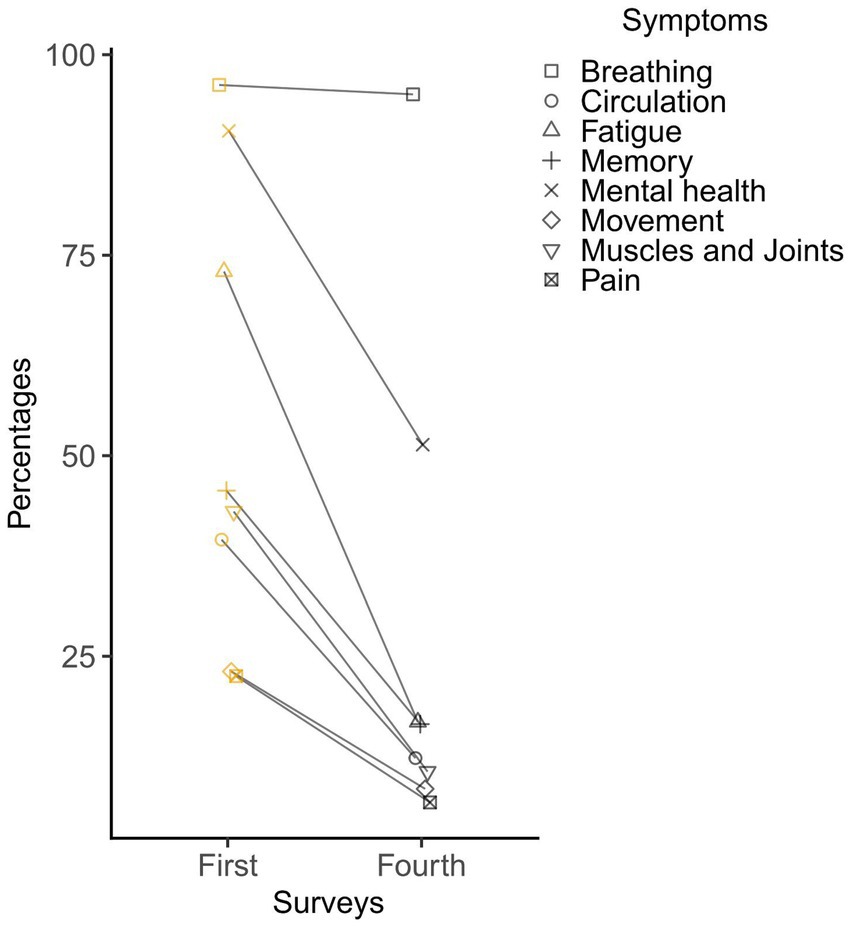
Figure 2. The changes on the presence of post-Omicron symptoms between the first (1st month) and fourth (2nd month) survey.
Eight domains were generated based on 51 symptoms, and the raw score of each domain was translated into the Rasch 0–100 linear score according to the User Manual of the SBQ-LC. The distribution of the Rasch linear score for each domain was compared across 4 surveys, as presented in Figure 3. The F-based Welth test showed overall statistical significance of eight domains, and pairwise comparisons across surveys were also significant at a level of 5%.
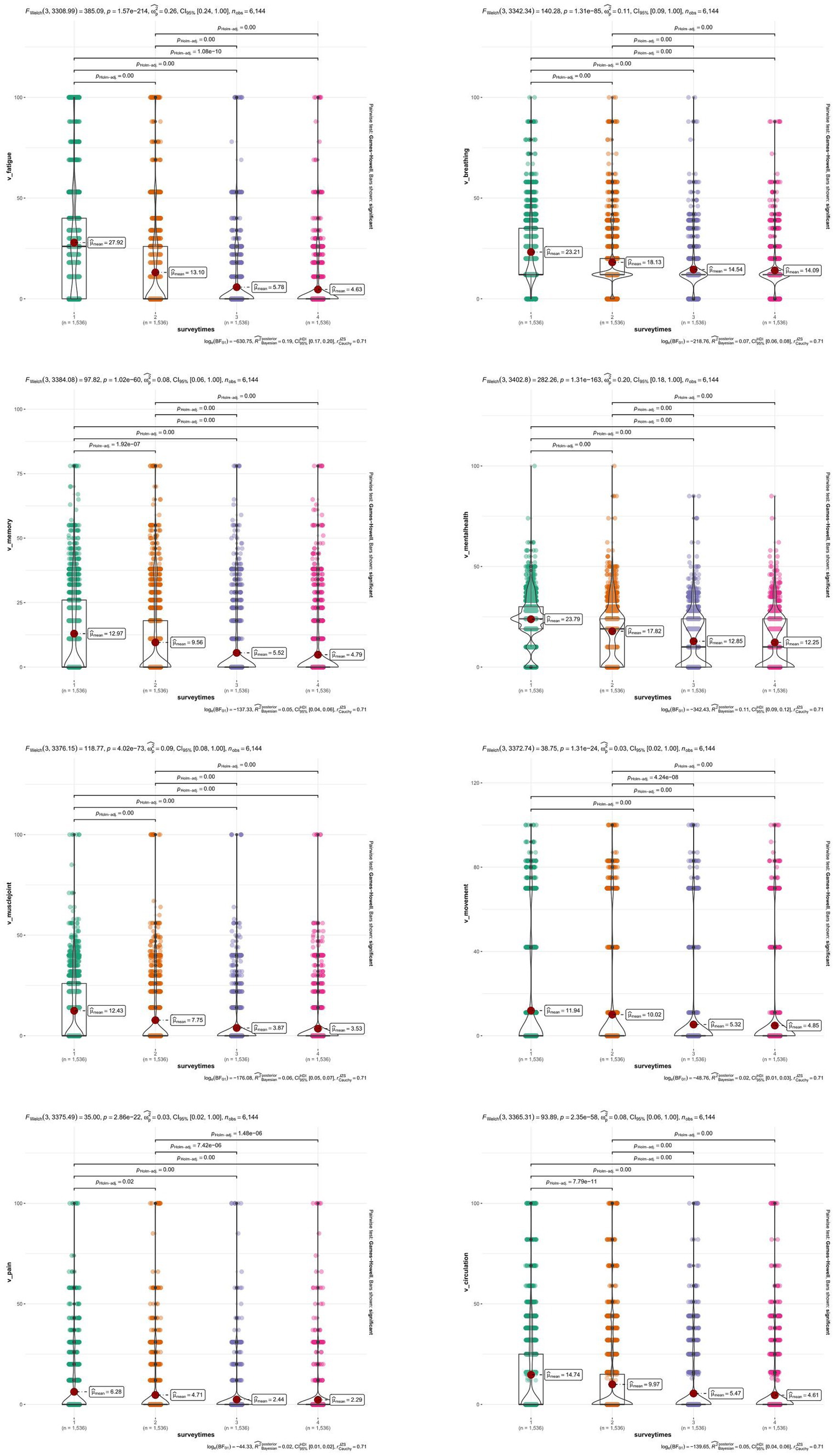
Figure 3. Distribution and comparison of eight domains in the modified SBQ-LC across 4 surveys. SBQ-LC, Symptom Burden Questionnaire for long COVID.
The correlation of the Rasch 0–100 linear scores of eight domains across four surveys is illustrated in Figure 4. The overall correlation of eight domains was statistically significant. The correlation of fatigue with movement, pain, muscles and joints, and memory differed obviously across four surveys.
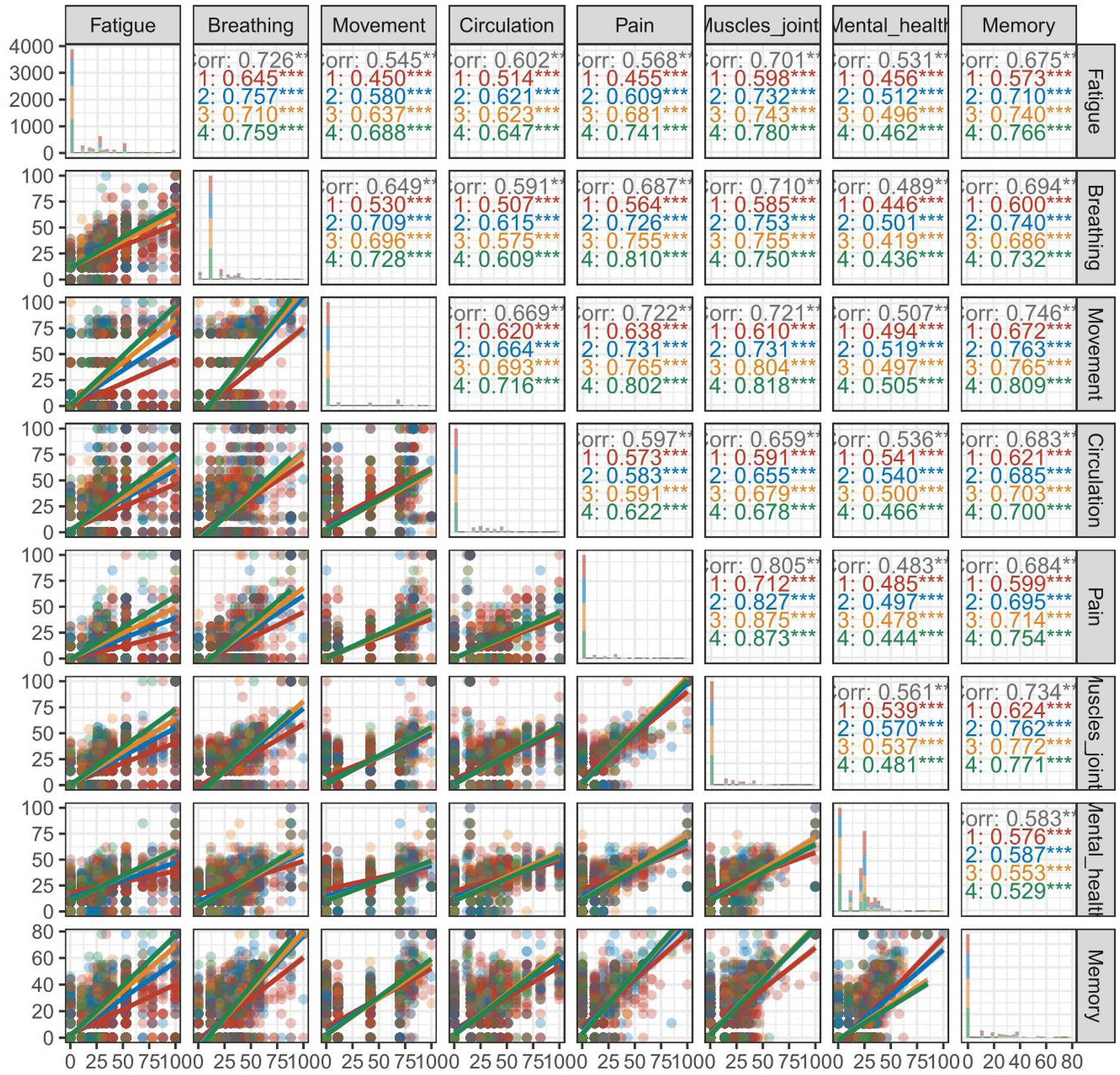
Figure 4. Correlation of eight domains in the modified SBQ-LC stratified by 4 surveys. SBQ-LC, Symptom Burden Questionnaire for long COVID.
For each survey, the correlation of eight domain scores is illustrated in Supplementary Figure S1. Across the four surveys conducted, a positive correlation was observed for the eight domains. Notably in the fourth survey, the correlation coefficient for mental health with the other domains was found to be relatively weaker than the other comparisons.
The restricted cubic spline smoothed curves for age and survey are provided in Figure 5 for eight domains. Overall, the distribution of age with all domains followed the N-shaped geometry, and that of survey followed the inverse J-shaped geometry. For age, the Rasch linear score hit the lowest level among children aged 6–8 years, and reached the peak among children aged 12–13 years. It is also worth noting that at the 4th survey, 56.95% children had one or more mental health-related problems among children aged 12–13 years, higher than the average level of other age groups at 50.53%. For survey, the scores of all domains sharply declined from the first to the third survey, and remained stable between the third and the fourth survey.
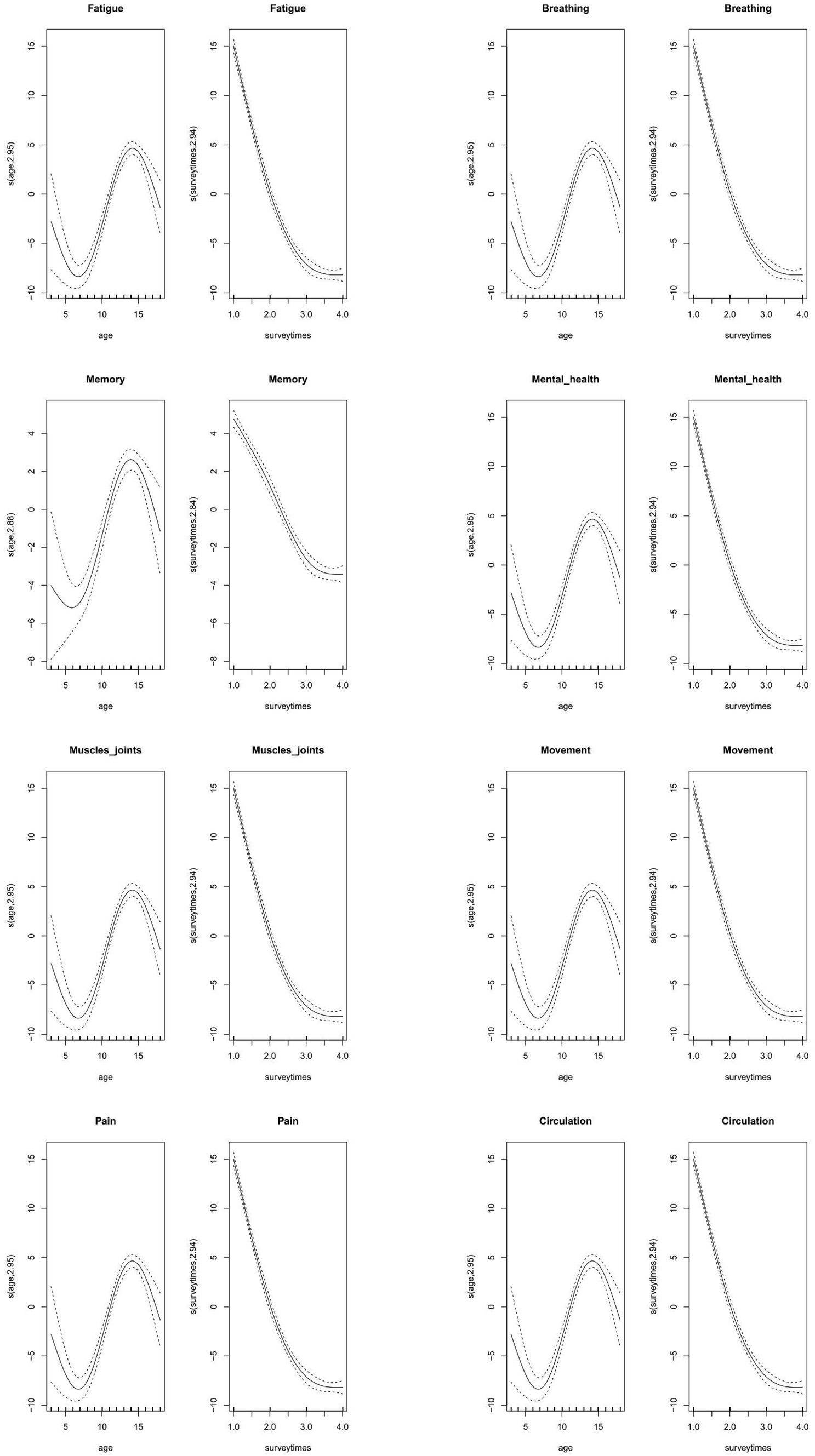
Figure 5. Prediction cubic curves of age and survey for eight domains in the modified SBQ-LC under the generalized additive mixed model. Abbreviations: SBQ-LC, Symptom Burden Questionnaire for long COVID.
Besides, the combined distribution of age and survey for each domain was also explored under the generalized additive mixed model (Supplementary Figure S2). Eight domains exhibited a saddle-shaped trend with respect to age and survey time, peaking at 12–13 years of age, and all eight domains demonstrated an upward trajectory during the first survey.
Considering the autocorrelational structure of eight domains under study, generalized additive mixed model was adopted and it is an extension of the generalized linear mixed model. Two factors were smoothed in this study, that is, age and survey, and sex was treated as nonsmoothed factor. As shown in Table 2, the association of sex was statistically significant with pain only. Age was associated with all domains at a significance level of 5%, and besides muscles and joints (p = 0.058), survey with the other seven domains was significant.
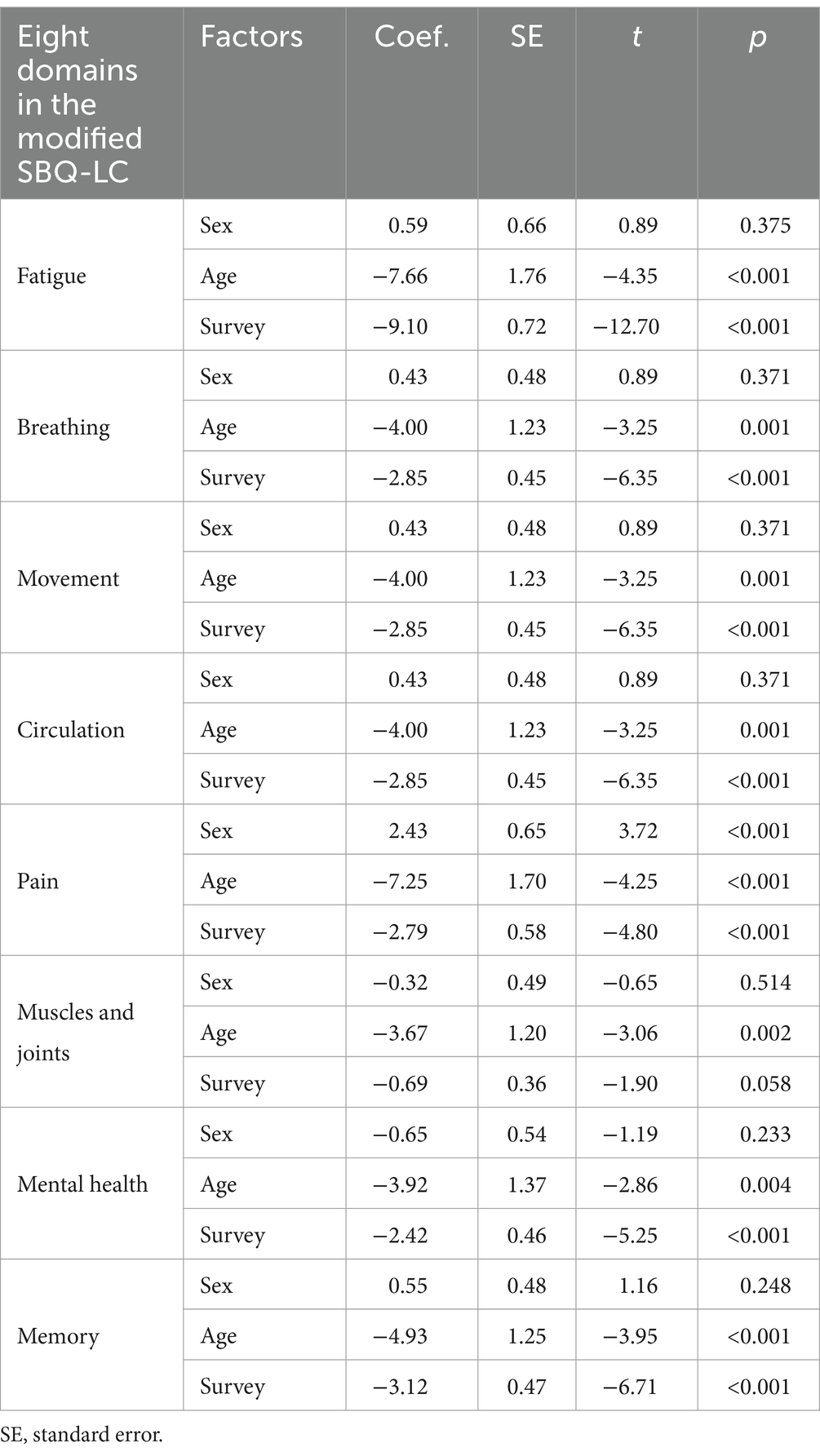
Table 2. Association of sex, age and survey with eight domains in the modified SBQ-LC under generalized additive mixed model.
The survey-dependent changes of the Rasch scores of eight domains are provided in Supplementary Figure S3. The difference between the first and second survey across eight domains was predominantly increased, the difference between the second and third survey has comparable ups and downs, and the difference between the third and fourth survey was predominantly decreased.
The symptom combinations of each domain across 4 surveys are displayed in the form of Venn plots in Supplementary Figures S4–S7, respectively. In the first survey, 51.8% of children reported the simultaneous presence of four symptoms in fatigue domain; 44.4 and 44.5% of children reported one symptom in breathing and mental health domains; 76.9 60.5, 77.5, 56.9, and 54.4% of children reported no presence of any symptom in movement, circulation, pain, muscles and joints and memory domains. In the second survey, 65.6 and 43.1% of children reported one symptom in breathing and mental health domains; 62.6, 82.7, 74.3, 85.5, 75.6, and 68.9% of children reported no presence of any symptom in fatigue, movement, circulation, pain, muscles and joints and memory domains. In the third survey, 78.8% of children reported one symptom in breathing domain; 79.8, 90.6, 84.5, 92.7, 87.9, 46.2, and 81.1% of children reported no presence of any symptom in fatigue, movement, circulation, pain, muscles and joints, mental health and memory domains. In the fourth survey, 81.6% of children reported one symptom in breathing domain; 83.2, 91.5, 87.7, 93.2, 89.4, 48.6, and 83.5% of children reported no presence of any symptom in fatigue, movement, circulation, pain, muscles and joints, mental health and memory domains.
The aim of this prospective study was to assess the dynamic changes of persisting symptoms among children aged 6–18 years during 1–2 months after the Omicron infection based on the modification of SBQ-LC from eight domains in Beijing, China. The key findings of this study are that the impact of Omicron infection on the health of children is multifaceted, and of eight domains evaluated, breathing- and mental health-related problems persisted during 1-to-2-month Omicron infection period. Moreover, the impact of Omicron infection on the health of children peaked among children aged 12–13 years, who are experiencing the transition from primary school to junior high school in practice. To hasten post-COVID-19 recovery, special attention should be given to vulnerable age groups who had the highest risk of detrimental multisystem symptoms. As far as we know, this is thus far the first prospective survey on post-Omicron symptoms among Chinese children in the literature.
It is universally accepted that children, as a special group, are very sensitive and vulnerable, and warrant special care, especially when facing regional or global serious pandemics, such as COVID-19. Global statistics show that of all confirmed cases, pediatric COVID-19 is estimated to account for 2–7%. Currently, there is wide recognition that in the long-term, COVID-19 has left a large proportion of adults and children suffering unexplained persistent residual or new-onset symptoms that may affect routine functioning and fluctuate or relapse over time (12–15). These symptoms, collectively termed as long COVID, are prevalent and present among 25% of children according to a meta-analytical report (8). It is clearly important to achieve a better understanding of the symptoms that prevail during the long COVID period, so that preventive or interventive measures may be put in place to improve quality of life and reduce the burden of disease and disability. At present, evidence on post-Omicron symptoms mainly draws from mono cross-sectional surveys and outpatient or inpatient patients (10, 16–20), and the dynamic picture of these symptoms, especially following Omicron waves, is not fully understood in children from China. To shed some light, we designed this prospective study by monitoring the 1-to-2-month changes of post-Omicron symptoms of 1,536 children aged 6–18 years from Tongzhou district, Beijing at serial even intervals.
In this study, it is worth noting that the impact of Omicron infection on the health of children involves multiple systems, in particular breathing and mental health with over 90% children suffering one or more relevant symptoms one-month post-Omicron, even after 3 months, one or more these symptoms persisted among over half children. Persisting breathing-related problems are very easy to trigger the development of lower respiratory tract infection, an important cause of children morbidity and mortality around the globe (21). Moreover, systematic evidence suggests that children with confirmed lower respiratory tract infection during the first 3 years of life often have abnormal pulmonary function testing and are susceptible to obstructive airways diseases (22, 23). As such, our public health decision-makers and healthcare professionals working in primary care settings should attach much emphasis to the respiratory health of children following Omicron waves. Our findings underscore the need for enhanced comprehensive monitoring on the patterns and progressions of breathing-related symptoms in practice, as well as the need for early identification and targeted intervention of high-risk children for lower respiratory tract infection and pneumonia to reduce the escalating burden of COVID-19 pandemic globally. Besides, there is evidence that COVID-19 infection can accelerate the adverse psychological and behavioral outcomes, and a wide range of brain changes were reported in patients with pediatric mental illness (24). Other studies have shown that mental health continued to deteriorate through the COVID-19 pandemic even after easing restrictions (25). According to our recent report, longtime home study was associated with a high rate of psychological and behavioral problems in children after the COVID-19 pandemic, and this rate reached 13.51% in children aged 6–11 years and 18.08% in children aged 12–16 years (26). Further, we found that reasons behind these psychological and behavioral problems might be attributable to parent–child conflict, sleep problems, prolonged online study time and video-game time and increased sedentary time (27). At the time of our serial surveys, children infected with COVID-19 were required to study at home again, with their psychological behaviors facing great challenges. Hence, the implication of this study is a call for action to pay special attention to mental health in children after the Omicron infection.
Another important finding of this study is that the detrimental impact of Omicron infection in childhood health was largest among children 12–13 years of age especially in terms of breathing and mental health, who are undergoing the transition from primary school to junior high school during the period from 2019 to 2022 in Beijing. It is generally accepted that children of this age group are experiencing periodical changes in physiological, mental and behavioral aspects throughout the human lifespan. These changes are potentially worsened when facing the repeated COVID-19 outbreaks. We all agree that compulsory education builds a foundation upon which every aspect of children’s development relies, yet studying online at home disrupts normal education, prevents children from getting their education off the best possible start, and reduces face-to-face communication as well. As stated by Sun and colleagues, China needs a scientific long COVID recovery-support platform, which can help the public understand the symptoms and effects of long COVID, and provide guidance to patients on how to cope with symptoms during their recovery (28). In the post-pandemic era, childcare is hence essential in providing children with integrated services and protection, as well as developing social, emotional and cognitive skills, especially for children aged 12–13 years.
The findings of this prospective study provide schools and healthcare professionals with valuable information, as reflected in the following aspects. First, 1–2 weeks are required for children to adjust and adopt the early stage of reopening schools. Second, the intensity of physical and school assignment objectives should be increased gradually according to the status of children. Third, mental health-related problems should be closely monitored and channeled out in time via the integrated efforts of both parents and teachers.
Some limitations should be acknowledged for this study. First, our questionnaire was designed by referring to the SBQ-LC version 1.0, which is suitable for adults only and constructed from 16 domains. Contrastingly, we only adopted 8 domains suitable for children, and whether doing so can be applicable deserves special concerns, as no official questionnaires are currently available for children under long COVID. Second, only data on four serial surveys following Omicron waves were available for the present study, and considering the persisting health-related problems, further longitudinal surveys, which are ongoing, necessitate. Third, only data on eight groups of clinical symptoms were collected, and as incorporating dynamic lung imaging and viral nucleic acid CT values would have been more meaningful, this substantially weakened the results. Fourth, study children were enrolled from the Tongzhou district, Beijing, and whether our regional observations can be extrapolated to other regions warrants further validation. What’s more, all children are of Chinese origin, and generalizability to other racial or ethnical groups should be done with caution.
Despite above potential limitations, our findings indicate the multifaceted impact of Omicron infection on childhood health, especially among children aged 12–13 years. Moreover, of eight domains evaluated, breathing and mental health related problems persisted during 1–2-month Omicron infection period and the rest six domains were significantly improved. Importantly, the implication of this study is a call for action to build a long COVID recovery-support platform for children around the world, especially in the domain of respiratory and mental health and among children currently attending junior high schools.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by the Ethics Committee at the Capital Institute of Pediatrics (Beijing, China). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
BZ: Data curation, Formal analysis, Investigation, Methodology, Writing – original draft. QX: Data curation, Investigation, Methodology, Writing – original draft. SL: Investigation, Methodology, Supervision, Writing – original draft. JW: Investigation, Supervision, Writing – original draft. JL: Investigation, Methodology, Supervision, Writing – original draft. TZ: Project administration, Supervision, Writing – review & editing. XQ: Data curation, Investigation, Methodology, Writing – original draft. XW: Data curation, Investigation, Writing – original draft. LZha: Data curation, Investigation, Writing – original draft. XL: Investigation, Methodology, Writing – original draft. JG: Data curation, Investigation, Writing – original draft. LZho: Data curation, Investigation, Writing – original draft. FC: Investigation, Methodology, Project administration, Supervision, Writing – review & editing. XZ: Methodology, Project administration, Supervision, Writing – review & editing. WN: Data curation, Formal analysis, Methodology, Project administration, Supervision, Writing – original draft. LW: Funding acquisition, Investigation, Project administration, Supervision, Visualization, Writing – review & editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This research was supported by the Beijing Hospitals Authority’s Ascent Plan (DFL20221103), High-level Public Health Talents Training Program of Beijing Municipal Health Commission (2022-02-19).
We are grateful to all participating children and their parents or supervisors for their cooperation and willingness, as well as teachers and all of the medical staff for their great help.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1377745/full#supplementary-material
SBQ-LC, Symptom Burden Questionnaire for long COVID.
1. Taylor, L. Covid-19: Omicron drives weekly record high in global infections. BMJ. (2022) 376:o66. doi: 10.1136/bmj.o66
2. Chang, H, Zhang, X, Su, H, Cai, J, Liu, X, Li, J, et al. Epidemiological characteristics of paediatric Omicron infection during the outbreak of SARS-CoV-2 infection during March–May in 2022 in Shanghai, China. J Hyg. (2023) 151:e81:e81. doi: 10.1017/S0950268823000663
3. Li, YC, Ma, Z, Zhong, HY, and You, HL. Clinical characteristics of children with Omicron SARS-CoV-2 infection in Changchun, China from March to April 2022: a retrospective study. Front Pediatr. (2022) 10:990944. doi: 10.3389/fped.2022.990944
4. Morello, R, Mariani, F, Mastrantoni, L, De Rose, C, Zampino, G, Munblit, D, et al. Risk factors for post-COVID-19 condition (long Covid) in children: a prospective cohort study. EClinicalMedicine. (2023) 59:101961:101961. doi: 10.1016/j.eclinm.2023.101961
5. Khemiri, H, Ayouni, K, Triki, H, and Haddad-Boubaker, S. SARS-CoV-2 infection in pediatric population before and during the Delta (B.1.617.2) and Omicron (B.1.1.529) variants era. Virol J. (2022) 19:144. doi: 10.1186/s12985-022-01873-4
6. Khemiri, H, Gdoura, M, Ben Halima, S, Krichen, H, Camma, C, Lorusso, A, et al. SARS-CoV-2 excretion kinetics in nasopharyngeal and stool samples from the pediatric population. Front Med. (2023) 10:1226207. doi: 10.3389/fmed.2023.1226207
7. Hastie, CE, Lowe, DJ, McAuley, A, Mills, NL, Winter, AJ, Black, C, et al. Natural history of long-Covid in a Nationwide, population cohort study. Nat Commun. (2023) 14:3504. doi: 10.1038/s41467-023-39193-y
8. Campos, C, Prokopich, S, Loewen, H, and Sanchez-Ramirez, DC. Long-term effect of COVID-19 on lung imaging and function, cardiorespiratory symptoms, fatigue, exercise capacity, and functional capacity in children and adolescents: a systematic review and meta-analysis. Healthcare. (2022) 10:2492. doi: 10.3390/healthcare10122492.
9. Mat Hassan, N, Salim, HS, Amaran, S, Yunus, NI, Yusof, NA, Daud, N, et al. Prevalence of mental health problems among children with long Covid: a systematic review and meta-analysis. PLoS One. (2023) 18:e0282538. doi: 10.1371/journal.pone.0282538
10. Adler, L, Israel, M, Yehoshua, I, Azuri, J, Hoffman, R, Shahar, A, et al. Long Covid symptoms in Israeli children with and without a history of SARS-CoV-2 infection: a cross-sectional study. BMJ Open. (2023) 13:e064155. doi: 10.1136/bmjopen-2022-064155
11. Hughes, SE, Haroon, S, Subramanian, A, McMullan, C, Aiyegbusi, OL, Turner, GM, et al. Development and validation of the symptom burden questionnaire for long Covid (SBQ-LC): Rasch analysis. BMJ. (2022) 377:e070230. doi: 10.1136/bmj-2022-070230
12. Wacks, M, Wortley, E, Gregorowski, A, Segal, TY, and Whittaker, E. Fifteen-minute consultation: managing post-COVID-19 syndrome (long Covid) in children and young people. Arch Dis Child Educ Pract Ed. (2023) 109:29–34. doi: 10.1136/archdischild-2022-324950
13. Warschburger, P, Kamrath, C, Lanzinger, S, Sengler, C, Wiegand, S, Goldel, JM, et al. A prospective analysis of the long-term impact of the COVID-19 pandemic on well-being and health care among children with a chronic condition and their families: a study protocol of the kick-Covid study. BMC Pediatr. (2023) 23:130. doi: 10.1186/s12887-023-03912-7
14. Buonsenso, D, Morello, R, Mariani, F, De Rose, C, Mastrantoni, L, Zampino, G, et al. Risk of long Covid in children infected with Omicron or pre-Omicron SARS-CoV-2 variants. Acta Paediatr. (2023) 112:1284–6. doi: 10.1111/apa.16764
15. Coker, TR, Cheng, TL, and Ybarra, M. Addressing the long-term effects of the COVID-19 pandemic on children and families. JAMA. (2023) 329:1055–6. doi: 10.1001/jama.2023.4371
16. Ahn, B, Choi, SH, and Yun, KW. Non-neuropsychiatric long Covid symptoms in children visiting a pediatric infectious disease clinic after an Omicron surge. Pediatr Infect Dis J. (2023) 42:e143–5. doi: 10.1097/INF.0000000000003862
17. Baptista de Lima, J, Salazar, L, Fernandes, A, Teixeira, C, Marques, L, and Afonso, C. Long Covid in children and adolescents: a retrospective study in a pediatric cohort. Pediatr Infect Dis J. (2023) 42:e109–11. doi: 10.1097/INF.0000000000003829
18. Buonsenso, D, Morello, R, Mariani, F, De Rose, C, Cortese, R, Vetrugno, L, et al. Role of lung ultrasound in the follow-up of children with previous SARS-CoV-2 infection: a case-control assessment of children with long Covid or fully recovered. J Clin Med. (2023) 12:3342. doi: 10.3390/jcm12093342
19. Jamaica Balderas, L, Navarro Fernandez, A, Dragustinovis Garza, SA, Orellana Jerves, MI, Solis Figueroa, WE, Koretzky, SG, et al. Long Covid in children and adolescents: COVID-19 follow-up results in third-level pediatric hospital. Front Pediatr. (2023) 11:1016394. doi: 10.3389/fped.2023.1016394
20. Goretzki, SC, Brasseler, M, Dogan, B, Huhne, T, Bernard, D, Schonecker, A, et al. High prevalence of alternative diagnoses in children and adolescents with suspected long Covid-a single center cohort study. Viruses. (2023) 15:579. doi: 10.3390/v15020579
21. Verwey, C, Ramocha, L, Laubscher, M, Baillie, V, Nunes, M, Gray, D, et al. Pulmonary sequelae in 2-year-old children after hospitalisation for respiratory syncytial virus lower respiratory tract infection during infancy: an observational study. Respir Res. (2023) 10:e001618. doi: 10.1136/bmjresp-2023-001618
22. Verwey, C, Nunes, MC, Dangor, Z, and Madhi, SA. Pulmonary function sequelae after respiratory syncytial virus lower respiratory tract infection in children: a systematic review. Pediatr Pulmonol. (2020) 55:1567–83. doi: 10.1002/ppul.24804
23. Englund, JA, Cohen, RA, Bianco, V, Domachowske, JB, Langley, JM, Madhi, SA, et al. Evaluation of clinical case definitions for respiratory syncytial virus lower respiratory tract infection in young children. J Pediatric Infect Dis Soc. (2023) 12:273–81. doi: 10.1093/jpids/piad028
24. Yuan, TF, Ng, CH, and Hu, S. Addressing the mental health of children in quarantine with Covid-19 during the Omicron variant era. Asian J Psychiatr. (2023) 80:103371. doi: 10.1016/j.ajp.2022.103371
25. Payne, L, Goijen, HJ, Cobham, V, Bor, W, Stathis, SS, Coghill, DC, et al. The impact ofCOVID‐19 on children and adolescents attending child and youth mental health services in Queensland, Australia. Early Interv Psychiatry. (2023) 17:1180–8. doi: 10.1111/eip.13421
26. Wang, L, Zhang, Y, Chen, L, Wang, J, Jia, F, Li, F, et al. Psychosocial and behavioral problems of children and adolescents in the early stage of reopening schools after the Covid-19 pandemic: a National Cross-Sectional Study in China. Transl Psychiatry. (2021) 11:342. doi: 10.1038/s41398-021-01462-z
27. Wang, L, Chen, L, Jia, F, Shi, X, Zhang, Y, Li, F, et al. Risk factors and prediction nomogram model for psychosocial and behavioural problems among children and adolescents during the Covid-19 pandemic: a National Multicentre Study: risk factors of childhood psychosocial problems. J Affect Disord. (2021) 294:128–36. doi: 10.1016/j.jad.2021.06.077
Keywords: Omicron infection, long Covid, children, Symptom Burden Questionnaire, prospective cohort
Citation: Zhou B, Xu Q, Li S, Wang J, Liu J, Zhang T, Qu X, Wang X, Zhang L, Liu X, Gu J, Zhou L, Chen F, Zong X, Niu W and Wang L (2025) Impact of Omicron infection on childhood health: the Beijing long-COVID study. Front. Public Health. 13:1377745. doi: 10.3389/fpubh.2025.1377745
Received: 28 January 2024; Accepted: 05 February 2025;
Published: 19 February 2025.
Edited by:
Mehdi Benamar, Harvard Medical School, United StatesReviewed by:
Xueping Yu, Fujian Medical University, ChinaCopyright © 2025 Zhou, Xu, Li, Wang, Liu, Zhang, Qu, Wang, Zhang, Liu, Gu, Zhou, Chen, Zong, Niu and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lin Wang, Y2Fyb2xpbl93YW5nQGJqbXUuZWR1LmNu; Wenquan Niu, bml1d2VucXVhbl9zaGNuQDE2My5jb20=
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.