- 1School of Politics and International Studies, University of Leeds, Leeds, United Kingdom
- 2Department of Maternal, Newborn, Child, Adolescent Health and Ageing, World Health Organization, Geneva, Switzerland
- 3School of Politics and International Relations, Queen Mary University London, London, United Kingdom
Introduction: The private health sector provides significant maternal and newborn health (MNH) services in mixed healthcare systems in many low- and middle-income countries (LMICs), making it an essential partner in achieving universal health coverage (UHC). Although some studies have mapped the private sector’s activities in MNH care in LMICs, limited knowledge exists about specific quality of care interventions. This scoping review addresses this gap by mapping quality of care interventions implemented by private healthcare providers for MNH care in LMICs.
Methods: Following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR), nine electronic databases were searched. Studies were included if they examined an intervention primarily designed to deliver MNH care by the private sector in LMICs.
Results: A total of 11,922 titles and abstracts were screened, with 38 meeting the inclusion criteria. Qualitative and quantitative data were extracted for descriptive statistics and thematic analysis, focusing on maternal mortality, maternal morbidity, newborn mortality, newborn morbidity, quality of care, experience of care, private sector care usage, and stillbirth. Findings are presented as a systematic narrative synthesis using the WHO’s National Quality Policy and Strategy (NQPS) framework’s quality intervention groups. While various interventions exist, public–private partnership (PPP) schemes and vertical programmes have received more scholarly attention. Most studies emphasised health outcome indicators.
Discussion: We argue that outcome reporting should be diversified to include stakeholders’ perspectives, helping researchers and policymakers understand how governments can engage the private sector in sustainable partnerships that strengthen health systems and advance UHC with quality. Interventions should be people-centred, incorporating feedback mechanisms that promote accountability and empower intended beneficiaries.
Introduction
Private sector providers play a crucial role in delivering health services in low- and middle-income countries (LMICs) (1–3). The private sector is present in the majority of healthcare systems and contributes significantly to providing maternal and newborn healthcare (MNH) services (3). Analysing 70 LMICs, Grépin (4) found that the private sector provides over one-third of maternal health services. Campbell et al. show that in LMICs, the private health sector provides on average 44% of antenatal care (ANC) and 40% of childbirth delivery services (5). As such, private sector providers are essential to achieving UHC in mixed (public–private) healthcare systems (6). It is therefore important to broaden the evidence base to better understand the role private providers play and could play, to facilitate more effective engagement, and to routinely integrate them in the improvement of MNH care delivery (6).
Despite the involvement of the private sector in MNH care delivery, few existing studies systematically examine the extent of the private sector in the delivery of MNH care across LMICs (7).
This scoping review aims to answer the question: What quality interventions have been designed and implemented by private health sector providers to deliver quality MNH care? We define private sector healthcare providers as individuals and organisations delivering health services that are not owned or directly controlled by governments, such as for-profit and not-for-profit entities, including private for-profit healthcare providers, charities, philanthropic organisations, faith-based organisations, and non-governmental organisations (NGOs) (8). Traditional and informal private sector providers are beyond the scope of this review, as are private sector providers that support the delivery of health services (e.g., supply chain, education, training, and insurance providers) (9). Maternal health covers the wellbeing of women throughout pregnancy, childbirth, and the postpartum phase while perinatal health covers the period from 22 completed weeks of gestation to 7 days after birth. Newborn health focuses on the first month of a baby’s life (10).
Methods
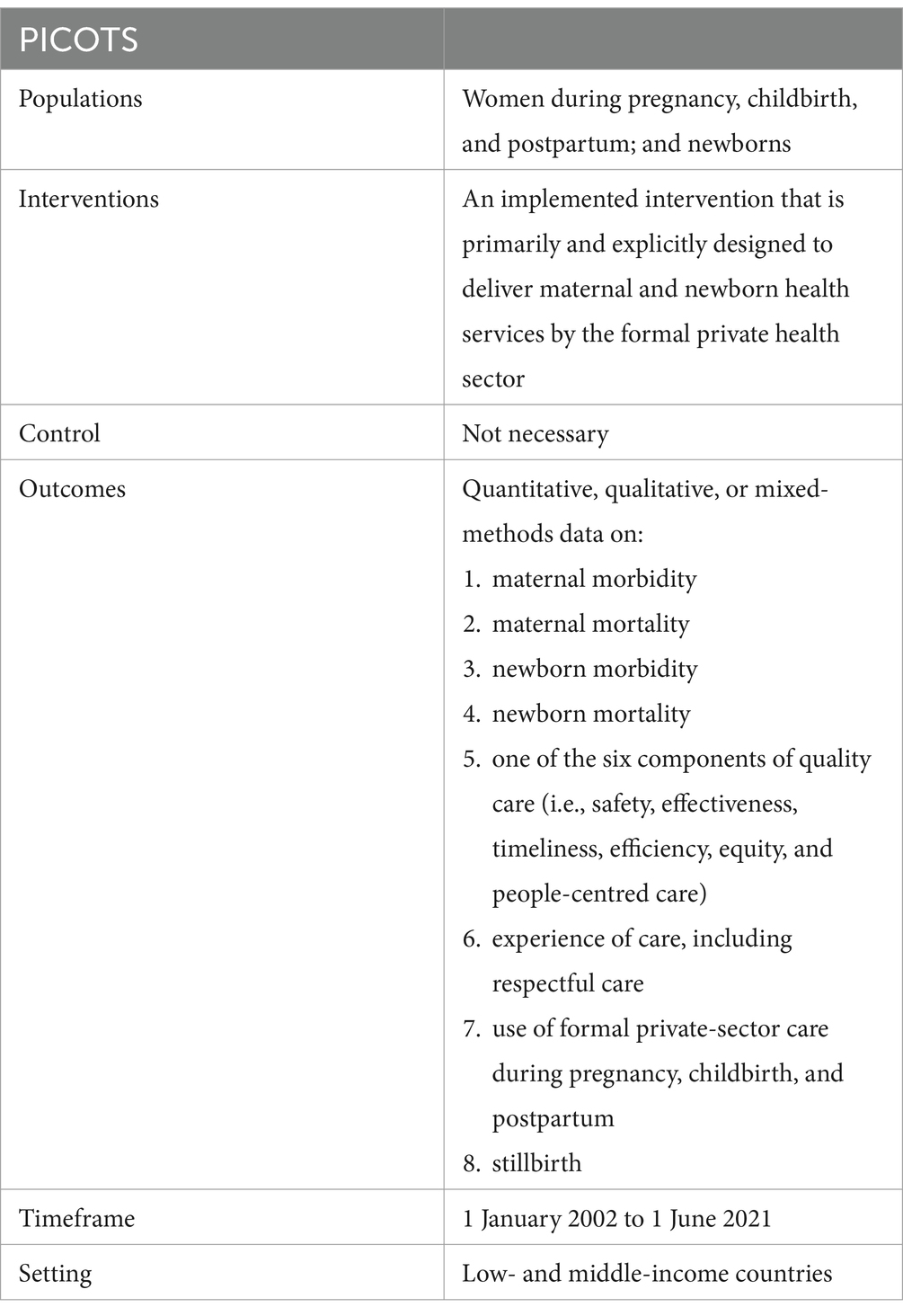
We conducted a transparent and reproducible scoping review using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) tool and reporting guidelines for protocols (11, 12). We chose a scoping review to identify and document private-sector MNH interventions in LMICs, anticipating varied types of evidence. The searches, application of in/exclusion criteria, screening, and data extraction were conducted following a rigorous protocol and utilising data extraction tools based on the PICOTS (Patient population, Intervention, Comparator, Outcome, Timing, and Setting) criteria (Table 1).
The scoping review considered peer-reviewed and non-reviewed studies, papers and conference abstracts, presentations, and reports on private sector involvement in MNH care interventions in LMICs classified according to the World Bank Atlas, published between 01 January 2002 and 01 June 2021. Studies had to report qualitative and/or quantitative data on one of the following outcomes: maternal mortality; maternal morbidity; newborn mortality; newborn morbidity; quality of care (QoC); experience of care, including respectful care; the use of private sector care during pregnancy, childbirth, and postpartum; and stillbirth.
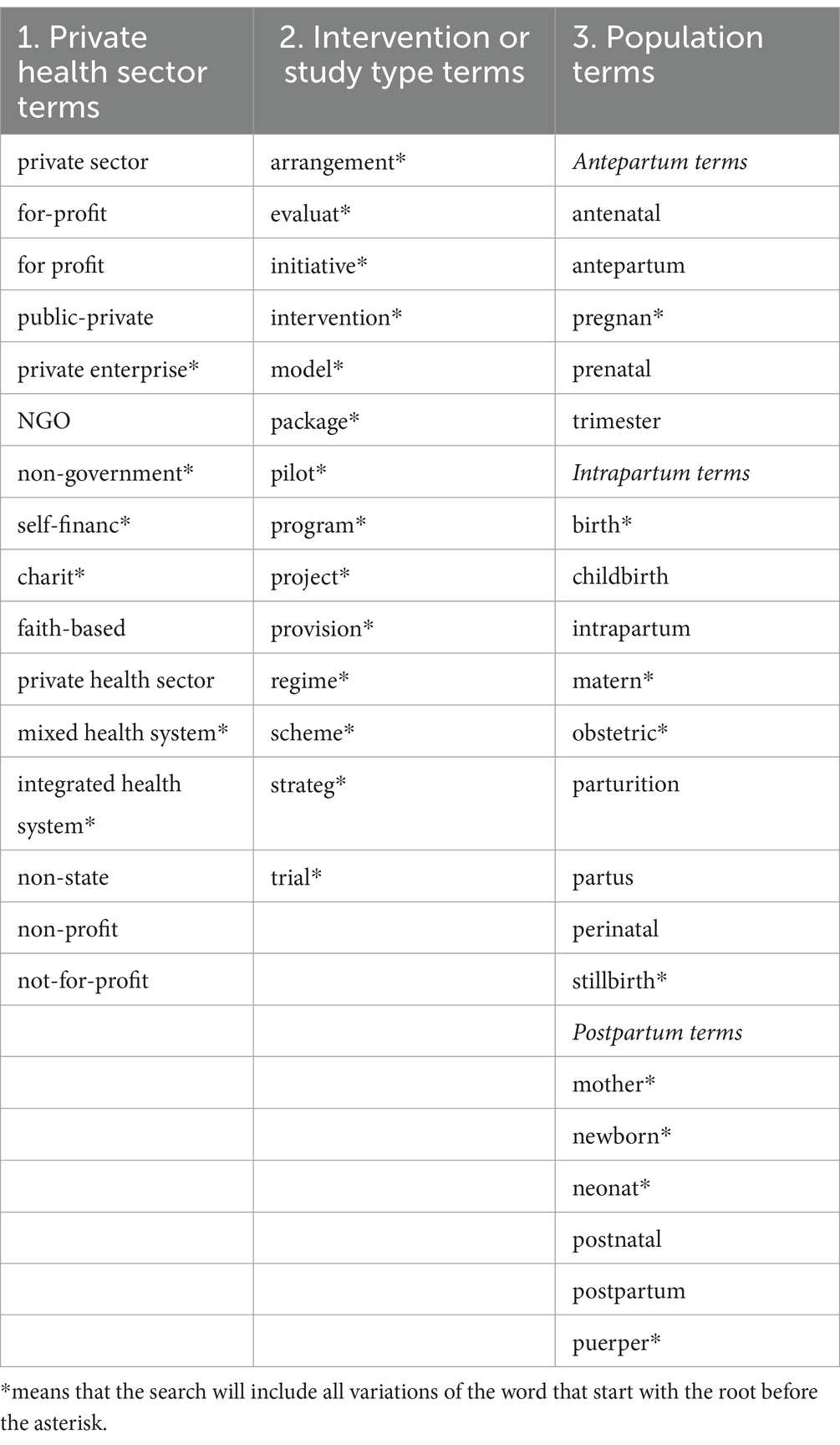
Nine electronic databases were searched using combinations of relevant search terms (Table 2) adapted to each database. The searched databases are the MET, HCPPR, Cumulative Index to Nursing and Allied Health, Excerpta Medica Database, International Bibliography of the Social Sciences, PubMed, ScienceDirect, Web of Science, and WHO Institutional Repository for Information Sharing. We included items in English, French, German, and Italian. We followed the PRISMA-ScR flow approach using our published protocol (9).
For inclusion, studies must evaluate service delivery interventions that have been primarily and explicitly designed to deliver MNH care by the formal private health sector in LMICs. As indicated in the PICOTS criteria (Table 1), included studies must report quantitative, qualitative, or mixed-methods data on at least one of the following outcomes: maternal morbidity, maternal mortality, newborn morbidity, newborn mortality, components of quality care (e.g., safety, effectiveness, timeliness, efficiency, equity, and people-centred care), experience of care (including respectful care), use of formal private sector care during pregnancy, childbirth, and postpartum, or stillbirth. For inclusion, items must be research articles, reports, or descriptions of the implemented services/interventions. As we are focused on service delivery, we limited the private health sector to formal private providers who deliver direct medical care (e.g., private health facilities, private healthcare providers, civil society organisations delivering MNH care, and charities delivering MNH care). Since MNH needs may be met through primary healthcare, titles and abstracts that mentioned primary healthcare without specific mention of MNH care were moved forward to full-text screening for verification of the population and intervention.
Items were excluded if they reported aggregated service delivery data (e.g., combined outcome data from public and private health sectors). The private non-health sector (e.g., private cars or buses transporting pregnant women to health facilities) and private sector entities that do not deliver direct medical care were excluded. For example, we excluded private pharmaceutical providers (including pharmacies) and private health insurance companies. We also excluded study protocols.
As a scoping review, we did not assess the risk of bias in individual studies. We analysed and synthesised the private sector involvement in MNH care delivery in LMICs by six themes with 103 indicators. These themes include descriptive statistics, intervention background, intervention details, outcomes, evaluation, and study description. One researcher (ASJ) coded all studies, and 10 randomly selected studies were analysed by another researcher (SRL) for quality control. In cases where outcomes deviated, clarification was sought through discussion between the researchers. We decided to include more information in cases of doubt and repeated this process until we reached a consensus.
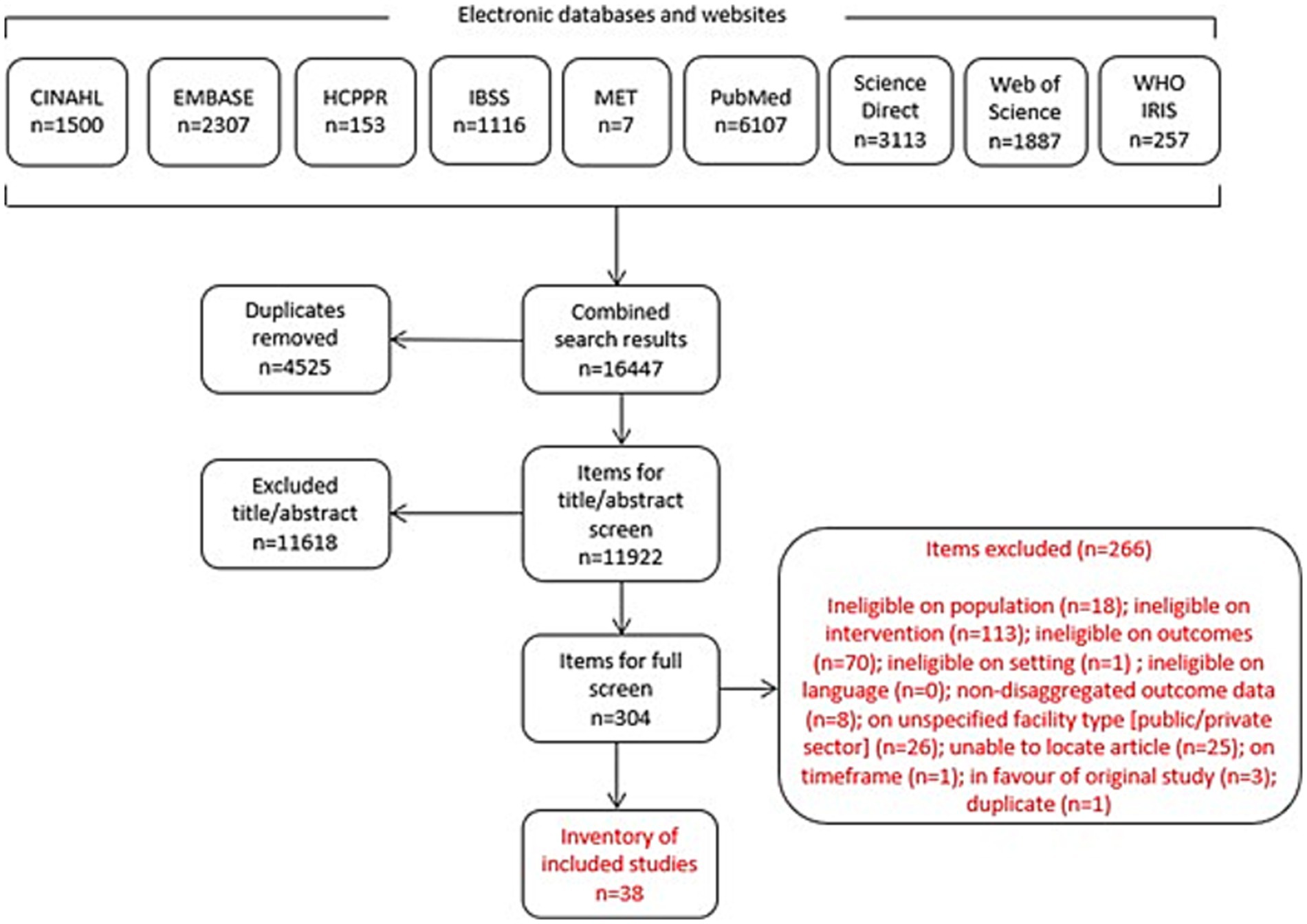
Our search generated 16,447 items for screening (Figure 1). After removing duplicates, the remaining 11,922 items were screened by title and abstract (TIAB) for inclusion. We determined the eligibility of all items, and unclear cases were discussed. In cases where exclusion could not be determined based on TIAB, the full text was reviewed. After TIAB screening, 304 studies remained for full-text review. Decisions were made in favour of an inclusive approach when questions arose; ultimately, 38 studies met all inclusion criteria.
We present the data using a systematic narrative synthesis, organised according to the QoC intervention groups proposed by the WHO’s National Quality Policy and Strategy (NQPS) guidance (13). Thematic reports are supplemented by tables of descriptive statistics on included studies and their outcomes. We excluded studies on private sector entities not delivering direct healthcare (e.g., teach-the-teacher, transportation services), as they do not solely focus on community and stakeholder engagement.
Framework
In this scoping review, we use the four groups of quality interventions as outlined by the WHO’s NQPS framework to structure our analysis (13). The NQPS framework provides a practical approach for developing policies and strategies to improve the QoC. Its four quality-related interventions are: system environment; reducing harm; improvement in clinical care; and patient, family, and community engagement and empowerment (Table 3).
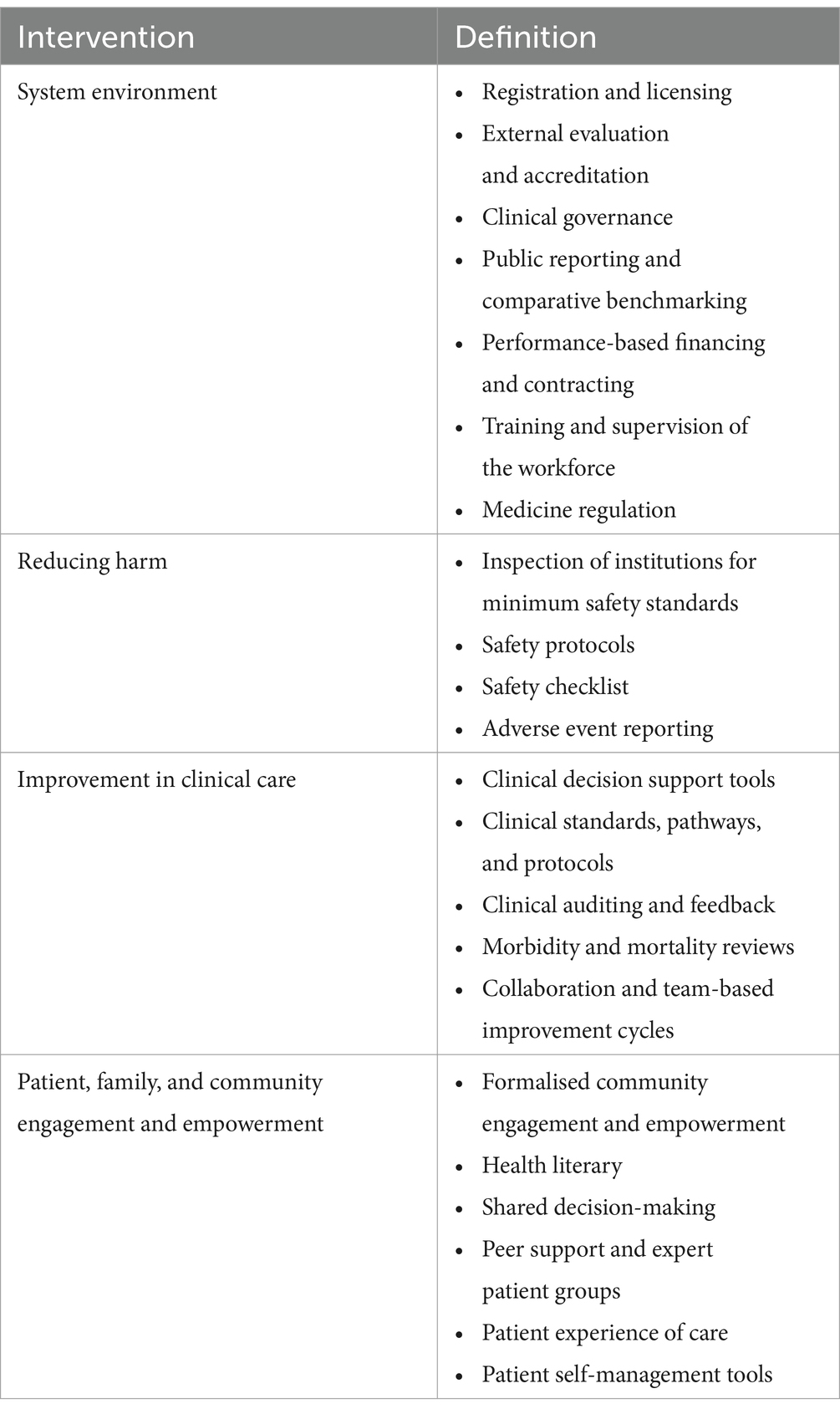
Table 3. Illustrative quality interventions according to the WHO’s Handbook for National Quality Policy and Strategy, 2018.
Results
We first present the descriptive statistics for studies included in this scoping review, followed by findings categorised by the four groups of the NQPS interventions. Twenty-two articles (58%) studied system environment interventions (group 1), two focused (5%) on harm reduction (group 2), nine (24%) addressed improvements in clinical care (group 3), one (3%) analysed patient, family, and community engagement and empowerment (group 4), and four (11%) described multi-component interventions. Quality-related interventions are often interrelated, with many frequently covering multiple components. For this scoping review, we categorised interventions based on the aspect most emphasised by the authors, in alignment with the NQPS quality-related intervention groups.
Descriptive results
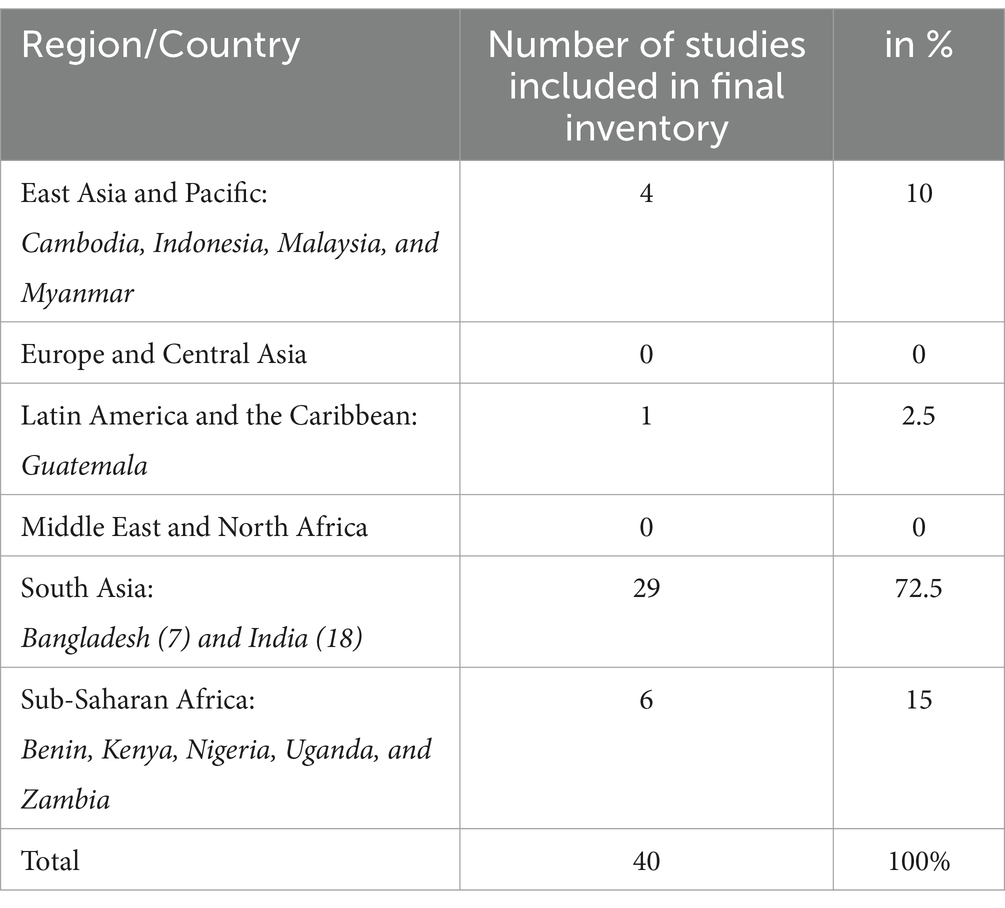
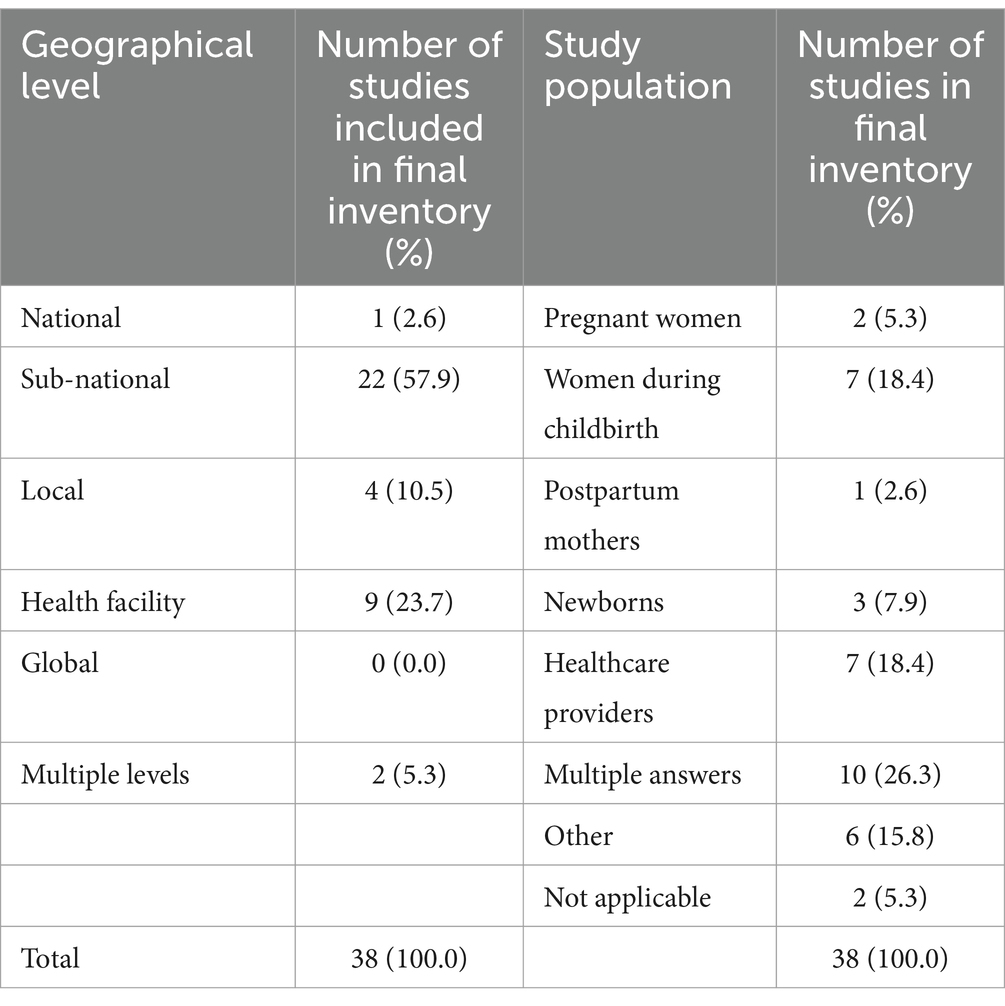
We reviewed 38 articles, which examined a total of 40 interventions. The majority of studies focused on interventions in South Asia (72.5%), with 45% specifically examining interventions in India, followed by 17.5% in Bangladesh (Table 4). Fifteen percent of interventions were in Sub-Saharan Africa. Studies on interventions in the Middle East, North Africa, and Latin America were notably absent. Table 4 provides an overview of interventions by region and country according to the World Bank Atlas classification. Less than a quarter of the studies (23.7%) were published by first authors affiliated with high-income country institutions, while nearly one-third originated from first authors based in India (31.6%).
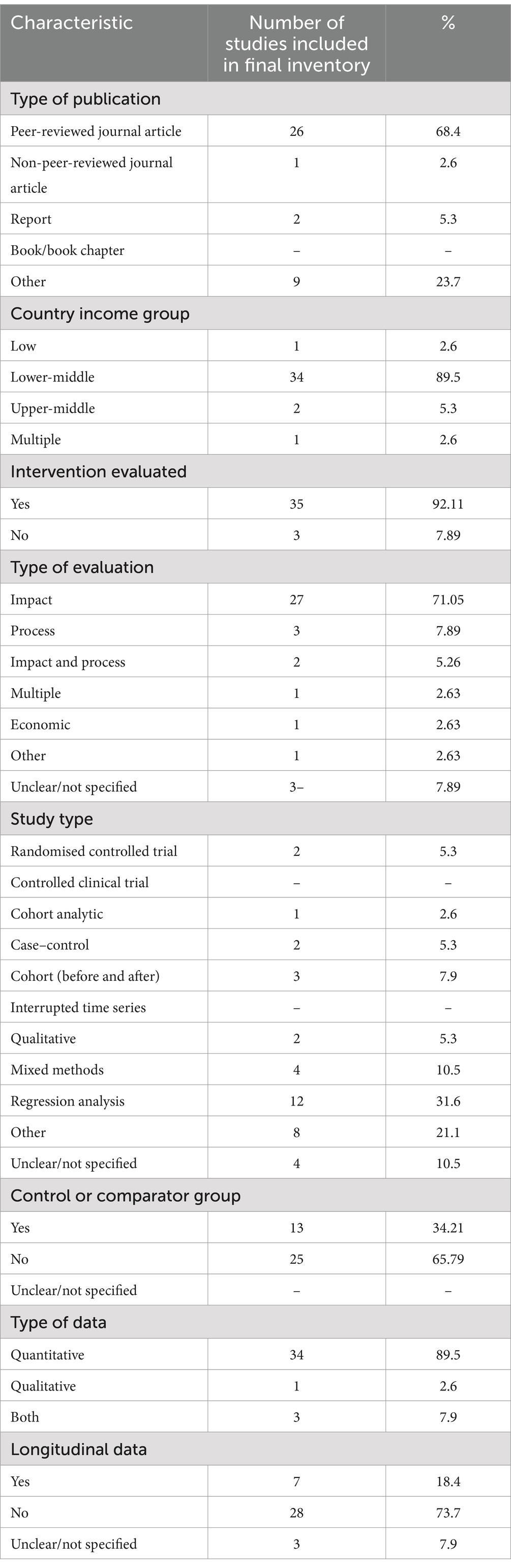
Eighty-nine point five and percent of studies analysed interventions in lower-middle-income countries, 2.6% focused on low-income countries, and 5.3% on upper-middle-income countries. One study covered multiple income levels. The majority of studies were quantitative, with 89.5% (n = 34) relying exclusively on quantitative data. Four studies included either qualitative data (n = 1) or both quantitative and qualitative data (n = 3). Half of the studies focused on the supply side, and 42.11% covered both the supply and demand side. Only 5.26% (n = 2) focused solely on the demand side. Table 5 provides an overview of study characteristics, including publication type, country income group, and data collection methods.
Just under one-third of studies (26.3%) involved multiple study populations, with 18.4% focusing on healthcare providers or women during childbirth, respectively. The majority of studies were conducted at the sub-national level (57.9%) or health facility level (23.7%) (see Table 6 for the study population and geographical scope).
System environment
Twenty-three out of the thirty-eight articles focused on system environment quality-related interventions. The primary interventions studied were performance-based financing and contracting (18 studies), where payments to healthcare providers were based on specific performance measures to improve quality. Payments were typically part of the total compensation and could be determined using various financing methods (13). The majority of these studies (n = 18) focused on public-private partnerships (PPPs), aimed at contracting in healthcare providers or contracting out to private sector providers. One study examined franchise models.
Nearly 50% of studies (n = 11) focused on two PPPs: the Chiranjeevi Yojana (CY) scheme in Gujarat, India (14–23), and its counterpart, the Janani Suraksha Yojana (JSY) in Maharashtra (24, 25). In these studies, private sector involvement involved public funding for private obstetricians to provide free health services to poorer populations. All reviewed studies reported positive outcomes, such as increased maternal mortality reduction, healthy deliveries, improved access to care, choice of delivery location, number of providers trained, increased number of ANC check-ups, and vaccination rates. However, it remains unclear whether this increase occurred primarily among the targeted populations (e.g., women below the poverty line) or broader lower-income families.
Four studies analysed contracting models beyond the two named PPPs. Two studies examined contracting out health services to NGOs in Pakistan (26) and Bangladesh (27), respectively. Zaidi et al. (26) found higher attendance by literate patients and increased out-of-pocket spending for ante- and postnatal services. Mercer et al. observed a decline in mortality in NGO-contracted areas (27). Caplain et al. analysed a contracting model, which provided a new degree to young healthcare providers to qualify as independent private community general practitioners (GPs) in rural areas (28). Cristia et al. (29) evaluated a large contracting programme in Guatemala in 1996, noting that better results were achieved under contracting-in models, with a 24% increase in nurse and physician utilisation for prenatal care.
One study analysed three franchise models designed to improve access to and the quality of maternal care in the private sector, while also better understanding the socio-economic profile of clients (30). The franchise covered only some of the services, making it a ‘fractional franchise’ model. Haemmerli et al. (30) observed that despite focusing on serving poorer populations, users of these services were primarily from higher wealth quintiles.
Three studies examined the impact of training and mentoring healthcare staff (31–33). Baig and Shahid, for example, analysed a competency-based training programme in Pakistan targeting community midwives and health facilities (32). This programme consisted of group- and classroom-based training of service providers, hands-on practice on mannequins and patients in clinical settings, and the development of standardised learning resource packages (32). The intervention targeted 112 community midwife-led clinics (CMW), 93 public (Department of Health) facilities, 109 private facilities, and 327 public–private partnership-led facilities across 15 districts in Sindh province. According to the authors, the preliminary analysis found significant improvements in the quality of antenatal, childbirth, and postnatal care at community midwife-led centres that received training, compared to those that did not (32). Two additional studies in Pakistan (31) and Nigeria (33) also reported improvement in the quality and availability of health services provided through the private sector, following the introduction of training programmes for community midwives operating in the private sector. Sini et al. analysed the effectiveness of a mobile obstetrics monitoring programme that used software solutions to better connect patients in rural areas with midwives and physicians, serving as a model for community-based antenatal care delivery in Indonesia (34). The study demonstrated that the programme improved decision-making and enhanced the skills and knowledge of the midwives.
Reducing harm
Two studies examined interventions aimed at reducing harm. Baniamin et al. analysed overtreatment by physicians in Bangladesh, revealing a higher rate of caesarean deliveries in private clinics than in public or non-profit facilities, suggesting a potential issue with overtreatment (35). The findings suggest that introducing competition in healthcare services may not effectively reduce unnecessary medical procedures, as increased competition does not necessarily lead to decreased overtreatment. Day et al. described the challenges and successes of implementing a Perinatal and Maternal Death Audit in a rural hospital in Bangladesh (36), emphasising the value of such audits and the importance of emotional support for healthcare workers to prevent emotional fatigue.
Improvement in clinical care
Nine studies focused on improving clinical care. Three studies examined morbidity and mortality reviews as a tool for clinicians to engage in self-reflection, identify areas for improvement, and promote a culture of learning (27, 37, 38). The remaining studies (n = 5) described and/or evaluated clinical programmes addressing access, auditing, and clinical standards (39–44). For example, Bhartia et al. (45) examined a programme that reduced caesarean section rates in a private, non-for-profit Indian hospital through a combination of hiring more nurses and experienced physicians, implementing audits, regularly presenting and reviewing data, developing clinical guidelines, establishing shared decision-making structures, and collaborating with other healthcare facilities. Jolly et al. (39) analysed a similar programme addressing maternal, neonatal, and child health issues among slum dwellers in Bangladesh. The study focused on clinical indicators, standards, and morbidity and mortality rates, and clinical audits to improve care. Similarly, Dangoria et al. (44) described access to ANC through non-profit hospitals in India, while Imtiaz et al. (40) measured the uptake of maternal and child health services after implementing a PPP in Pakistan.
Patient, family and community engagement, and empowerment
Interventions in this group sought to formalise community engagement and empowerment, enhance health literacy and shared decision-making, link people with shared experiences through peer support and expert patient groups, enhance patient self-management tools, and incorporate patient experience of care to design improvements in clinical care. Gatakaa et al. studied Ubuntu-Afya Kiosks in Kenya, a network of community-run medical centres developed through a private-community-government partnership. The study demonstrated improved uptake of skilled delivery and ANC, with the partnership model helping to create a self-sustaining healthcare service (46).
Multi-component interventions
Quality interventions are often interrelated. Four studies addressed multiple components. For example, Yadav et al. evaluated a private sector quality improvement programme in India that involved training healthcare workers, in-facility mentoring, advocacy for prioritising resources, data recording and reporting, peer assessments, and combining system environment and clinical care improvements (47). Hossain (48) and Baqui et al. (49) both analysed interventions aimed at improving the system’s environment. These included, for example, training private-community skilled birth attendants, formalising community engagement and empowerment through ‘social entrepreneurship capacity building’ (48), and conducting home visits by community health workers (49). Other studies, such as those related to the ‘Saving Mothers, Giving Life’ initiative in Uganda and Zambia, focused on enhancing integrated service delivery by linking public and private inputs, institutionalisation of maternal mortality surveillance, and auditing at the district level (50).
Discussion
This scoping review sought to answer the question of what service delivery interventions have been designed and implemented by private health sector providers to deliver quality MNH care. Using the WHO’s NQPS framework, this review demonstrated the breadth of private sector involvement in MNH care delivery.
The review shows that much of the private sector involvement focuses on system environments, particularly through performance-based financing and service contracting via PPP models. Nearly half of the studies in this review focused on PPPs, primarily in India. While these provide important insights, the engagement of policymakers with the private sector—especially in governance and service provision—appears skewed towards PPP models, which is also reflected in academic research and published articles. The majority of studies monitored access to quality care delivered by the PPPs, sparking ongoing debates about whether quality care can be better delivered through these sector providers and whether the models actually reach the targeted populations. This review has also revealed the prominence of interventions focused on training healthcare workers.
While increasing access to MNH care and improving provider training are key concerns for policymakers, it is critical that these interventions do not exacerbate underlying structural inequities. The reviewed studies engaged less with the structural factors and inequalities that impact the long-term success of MNH interventions. These factors include proper targeting, community and stakeholder involvement in designing the interventions, and linkages to ongoing health reforms that can improve sustainability. This is particularly important as many initiatives lose momentum when donor support ends or the project concludes. Another significant research gap involves analysing feedback mechanisms and considering the experiences of those receiving the interventions. Healthcare delivery must be people-centred, incorporating feedback and ensuring accountability at all levels. The following discussion will elaborate on these points, suggesting avenues for future exploration.
Context and sustainability
Health systems are deeply embedded in social, political, and economic contexts. As the private sector involvement in LMICs grows, concerns about equity, health financing, and access persist. However, no study specifically analysed interventions in relation to contextual factors or examined how structural drivers and political or economic contexts influence implementation and outcomes. While several studies targeted low-income households, they primarily measured whether the target groups were reached. An exception is Chaturvedi and Randive’s (25) study of the JSY PPP scheme in Maharashtra, which identified key design implementation issues, including specificities of what the scheme covers or neglects to cover.
Similarly, few studies analysed organisational factors. Understanding how interventions are designed, who decides on them, and how they are managed is critical to evaluating their success or failure.
The lack of focus on sustainability was also evident, as most interventions were project-based and dependent on donor funding. Few studies addressed how an intervention could lead to long-term change or become a regular part of health service provision.
Implementation science could offer a useful framework for further investigating private sector involvement in MNH care quality improvement. By focusing on sustainability, scalability, and the contextual factors (both inner and outer) that shape intervention delivery (51), implementation science frameworks (e.g., CFIR, RE-AIM, and the Health Equity Implementation Framework) can guide researchers’ process evaluations of interventions aimed at improving the quality of MNH care delivery (52–54).
People-centredness and accountability
With only three studies focusing on harm reduction and one on individual, family, and community engagement and empowerment, this review highlights a significant gap in the literature. The emphasis on patient-level health outcome indicators diverts attention from understanding patients’ experiences of care. Healthcare should be people-centred, grounded in human rights principles, and incorporate feedback from those it serves (55). Establishing feedback structures where communities can engage in intervention development, implementation, and evaluation is essential. These structures can also contribute to accountability at various levels.
Few studies incorporated stakeholder views—whether from physicians, nurses, or patients—and even fewer analysed mechanisms of accountability. Only seven studies reported on the experience of care, often through patient satisfaction surveys. Yet, for sustainable service delivery and improved MNH care quality, interventions should be co-produced with the communities they aim to serve (56). This approach is vital in addressing gendered, racialised, and other structural inequalities. Co-producing knowledge with communities has been shown to create feasible and acceptable solutions to healthcare concerns (56). Researchers and policymakers should diversify research designs, methods, and indicators, incorporating PROMS and PREMS (patient-reported outcome and experience measures) to enhance the QoC. However, these tools should be adapted to the specific contexts of LMICs.
Strengths and limitations
In line with the scoping review’s aim of providing a broad overview, this review included a variety of literature, from peer-reviewed research papers to conference abstracts. The strengths of the scoping review lie in its wide-ranging synthesis of private sector MNH care delivery in LMICs, identifying gaps and further research areas. The findings are directly applicable to practice and research in this field. However, there are limitations. Scoping reviews have inherent limitations because the focus is to provide breadth rather than depth of information on a particular topic. Our search focused on outcomes more easily measurable in quantitative terms, which may have resulted in a bias towards quantitative indicators over qualitative ones. We conducted the search in English only, which limited the included studies to those disseminated in English. As such, our results are generalisable to scoping reviews written in English. Additionally, the geographical focus of the studies was limited, with a bias towards South Asian countries, in particular India and its PPP models. Additionally, as much of the literature identified during this review focuses on PPPs, this review may not appeal to those interested in private sector impact. We also acknowledge that since July 2021, more studies will inevitably be published, yielding further insights into private-sector involvement in MNH care interventions. In the future, re-running the search will be valuable to update and refine the findings. Given these limitations, caution is advised when interpreting the findings.
Conclusion
This scoping review sought to identify the type of private-sector MNH care interventions in LMICs. By reviewing 38 studies through the NQPS’ quality interventions framework, the review highlights the wide-ranging involvement of the private sector in MNH care in LMICs. Private sector interventions show potential impact in reducing harm, improving front-line healthcare services, and building systemwide capacity for quality improvement. As the majority of studies prioritise health outcomes over patient experience, stakeholder perspectives, and feedback mechanisms, potential gaps arise, underscoring the need for more research to improve care quality in the private sector. The private sector’s role in MNH care is diverse and requires systematic research to leverage its contributions effectively. This review underscores the need to focus on how private sector MNH quality interventions are designed, by whom, and how knowledge is co-produced with those receiving care. Sustained funding and long-term planning are essential to ensuring these interventions contribute to the broader goal of strengthening mixed healthcare systems and achieving UHC.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
A-SJ: Conceptualization, Formal analysis, Methodology, Visualization, Writing – original draft, Writing – review & editing, Data curation. NY: Methodology, Writing – review & editing, Data curation, Conceptualization. SL: Conceptualization, Data curation, Formal analysis, Methodology, Writing – review & editing. JS: Writing – review & editing. BM: Methodology, Project administration, Writing – review & editing, Data curation, Conceptualization.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by MSD for Mothers and the Maternal, Newborn, Child, and Adolescent Health and Ageing Department of the World Health Organisation. MSD for Mothers had no role in the design and development of the study or the decision to publish.
Acknowledgments
We would like to thank Anshu Banerjee, Director of the Department of MCA in the WHO for their leadership and the WHO MNH Private Sector Working Group (2018–2022).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1332612/full#supplementary-material
References
1. Montagu, D, Goodman, C, Berman, P, Penn, A, and Visconti, A. Recent trends in working with the private sector to improve basic healthcare: a review of evidence and interventions. Health Policy Plan. (2016) 31:1117–32. doi: 10.1093/heapol/czw018
2. Montagu, D, and Goodman, C. Prohibit, constrain, encourage, or purchase: how should we engage with the private health-care sector? Lancet. (2016) 388:613–21. doi: 10.1016/S0140-6736(16)30242-2
3. Awor, P, Peterson, S, and Gautham, M. Delivering child health interventions through the private sector in low and middle income countries: challenges, opportunities, and potential next steps. BMJ. (2018) 362:k2950. doi: 10.1136/bmj.k2950
4. Grépin, KA. The role of the private sector in delivering maternal and child health services in low-income and middle-income countries: an observational, longitudinal analysis. Lancet. (2014) 384:S7. doi: 10.1016/S0140-6736(14)61870-5
5. Campbell, OMR, Benova, L, MacLeod, D, Baggaley, RF, Rodrigues, LC, Hanson, K, et al. Family planning, antenatal and delivery care: cross-sectional survey evidence on levels of coverage and inequalities by public and private sector in 57 low- and middle-income countries. Trop Med Int Health TM IH. (2016) 21:486–503. doi: 10.1111/tmi.12681
6. Morgan, R, Ensor, T, and Waters, H. Performance of private sector health care: implications for universal health coverage. Lancet Lond Engl. (2016) 388:606–12. doi: 10.1016/S0140-6736(16)00343-3
7. Basu, S, Andrews, J, Kishore, S, Panjabi, R, and Stuckler, D. Comparative performance of private and public healthcare systems in low- and middle-income countries: a systematic review. PLoS Med. (2012) 9:e1001244. doi: 10.1371/journal.pmed.1001244
9. Lattof, SR, Maliqi, B, Yaqub, N, and Jung, AS. Private sector delivery of maternal and newborn health care in low-income and middle-income countries: a scoping review protocol. BMJ Open. (2021) 11:e055600. doi: 10.1136/bmjopen-2021-055600
10. WHO. Maternal and newborn health EURO. Available online at: https://www.who.int/europe/health-topics/maternal-health (Accessed August 14, 2023).
11. Liberati, A, Altman, DG, Tetzlaff, J, Mulrow, C, Gøtzsche, PC, Ioannidis, JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. (2009) 339:b2700. doi: 10.1136/bmj.b2700
12. PRISMA. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. (2020). Available online at: https://www.prisma-statement.org/ (Accessed August 14, 2023).
13. WHO. Handbook for national quality policy and strategy: a practical approach for developing policy and strategy to improve quality of care. Geneva, Switzerland: World Health Organization (2018).
14. Mohanan, M, Bauhoff, S, La Forgia, G, Babiarz, KS, Singh, K, and Miller, G. Effect of Chiranjeevi Yojana on institutional deliveries and neonatal and maternal outcomes in Gujarat, India: a difference-in-differences analysis. Bull World Health Organ. (2014) 92:187–94. doi: 10.2471/BLT.13.124644
15. Iyer, V, Sidney, K, Mehta, R, and Mavalankar, D. Availability and provision of emergency obstetric care under a public–private partnership in three districts of Gujarat, India: lessons for universal health coverage. BMJ Glob Health. (2016) 1:e000019. doi: 10.1136/bmjgh-2015-000019
16. Yasobant, S, Shewade, HD, Vora, KS, Annerstedt, KS, Isaakidis, P, Dholakia, NB, et al. Effect of previous utilization and out-of-pocket expenditure on subsequent utilization of a state led public-private partnership scheme “Chiranjeevi Yojana” to promote facility births in Gujarat, India. BMC Health Serv Res. (2017) 17:302. doi: 10.1186/s12913-017-2256-6
17. Yasobant, S, Vora, KS, Shewade, HD, Annerstedt, KS, Isaakidis, P, Mavalankar, DV, et al. Utilization of the state led public private partnership program “Chiranjeevi Yojana” to promote facility births in Gujarat, India: a cross sectional community based study. BMC Health Serv Res. (2016) 16:266. doi: 10.1186/s12913-016-1510-7
18. Ng, M, Shanker-Raman, P, Mehta, R, Costa, AD, and Mavalankar, D. Initial results on the impact of Chiranjeevi Yojana: a public–private partnership programme for maternal health in Gujarat, India. Lancet. (2013) 381:S98. doi: 10.1016/S0140-6736(13)61352-5
19. Raman, PS, Mavalankar, D, Iyer, V, Sydney, K, Mehta, R, and Vora, K. Impact of a public–private performance-based financing partnership on the proportion of caesarean section deliveries: a cross-sectional study. Lancet. (2013) 381:S121. doi: 10.1016/S0140-6736(13)61375-6
20. Sidney, K, Iyer, V, Vora, K, Mavalankar, D, and De Costa, A. Statewide program to promote institutional delivery in Gujarat, India: who participates and the degree of financial subsidy provided by the Chiranjeevi Yojana program. J Health Popul Nutr. (2016) 35:2. doi: 10.1186/s41043-016-0039-z
21. Bhat, R, Mavalankar, DV, Singh, PV, and Singh, N. Maternal healthcare financing: Gujarat’s Chiranjeevi scheme and its beneficiaries. J Health Popul Nutr. (2009) 27:249–58. doi: 10.3329/jhpn.v27i2.3367
22. Ganguly, P, Jehan, K, de Costa, A, Mavalankar, D, and Smith, H. Considerations of private sector obstetricians on participation in the state led “Chiranjeevi Yojana” scheme to promote institutional delivery in Gujarat, India: a qualitative study. BMC Pregnancy Childbirth. (2014) 14:352. doi: 10.1186/1471-2393-14-352
23. Mavalankar, D, Singh, A, Patel, SR, Desai, A, and Singh, PV. Saving mothers and newborns through an innovative partnership with private sector obstetricians: Chiranjeevi scheme of Gujarat, India. Int J Gynecol Obstet. (2009) 107:271–6. doi: 10.1016/j.ijgo.2009.09.008
24. Krupp, K, and Madhivanan, P. Leveraging human capital to reduce maternal mortality in India: enhanced public health system or public-private partnership? Hum Resour Health. (2009) 7:18. doi: 10.1186/1478-4491-7-18
25. Chaturvedi, S, and Randive, B. Public private partnerships for emergency obstetric care: lessons from Maharashtra. Indian J Community Med. (2011) 36:21–6. doi: 10.4103/0970-0218.80788
26. Zaidi, S, Riaz, A, Rabbani, F, Azam, SI, Imran, SN, Pradhan, NA, et al. Can contracted out health facilities improve access, equity, and quality of maternal and newborn health services? Evidence from Pakistan. Health Res Policy Syst. (2015) 13:S54. doi: 10.1186/s12961-015-0041-8
27. Mercer, A, Uddin, N, Huq, NL, Haseen, F, Khan, MH, and Larson, CP. Validating neonatal mortality and use of NGO reproductive health outreach services in rural Bangladesh. Stud Fam Plan. (2006) 37:111–22. doi: 10.1111/j.1728-4465.2006.00090.x
28. Caplain, R, Yacoubou, I, Adedemy, D, Sani, A, Takam, S, and Desplats, D. Promouvoir des soins de proximité en Afrique: l’exemple de la médecine générale communautaire au Bénin. Sante Publique. (2014) S1:59–65. doi: 10.3917/spub.140.0059
29. Cristia, J, Prado, AG, and Peluffo, C. The impact of contracting in and contracting out basic health services: the Guatemalan experience. World Dev. (2015) 70:215–27. doi: 10.1016/j.worlddev.2015.02.003
30. Haemmerli, M, Santos, A, Penn-Kekana, L, Lange, I, Matovu, F, Benova, L, et al. How equitable is social franchising? Case studies of three maternal healthcare franchises in Uganda and India. Health Policy Plan. (2018) 33:411–9. doi: 10.1093/heapol/czx192
31. Mumtaz, Z, Levay, AV, Jhangri, GS, and Bhatti, A. Coverage of private sector community midwife services in rural Punjab, Pakistan: development and demand. Health Res Policy Syst. (2015) 13:S51. doi: 10.1186/s12961-015-0038-3
32. Baig, K, and Shahid, F. Abstract. ISQUA17-2981 training healthcare workers to improve the quality of maternal, newborn & child healthcare services in marginalized settings. Int J Qual Health Care. (2017) 29:41–2. doi: 10.1093/intqhc/mzx125.66
33. Ajuwon, AJ, Okuribido, B, Sadiq, GT, Ajibola, A, and Delano, GE. Outcome of interventions to improve the quality of reproductive health services provided by private health facilities in selected states in Nigeria. Afr J Med Sci. (2006) 35:369–74.
34. Sini, I, Djanas, D, Oktania, M, Polim, A, and Ulman, S. Pilot study. Mobile obstetrics monitoring (MOM) as a model for community-based antenatal care delivery in a low-resource setting. Koninklijke Philips. (2015). Available online at: https://www.philips.com/c-dam/b2bhc/master/Products/Category/enterprise-telehealth/mobile-obstetrics-monitoring/452299112911_MOM_WhitePaper_HR.pdf (Accessed August 14, 2023).
35. Baniamin, HM, and Jamil, I. Institutional design for credence goods: can the existence of financial incentive be problematic? Evidences from childbirth system of Bangladesh. Int J Public Adm. (2018) 41:1192–203. doi: 10.1080/01900692.2017.1362434
36. Day, LT, Mussell, F, Khatun, H, Verbiest, R, Biswas, L, Folia, R, et al. Abstract. Sustaining perinatal audit in the high stillbirth rate setting – a 20 year journey in rural Bangladesh In: Cork, vol. 17. Ireland: BMC Pregnancy Childbirth (2017). 1–47.
37. Fox-Lewis, S, Genasci Smith, W, Lor, V, McKellar, G, Phal, C, Fox-Lewis, A, et al. Get the basics right: a description of the key priorities for establishing a neonatal service in a resource-limited setting in Cambodia. J Trop Pediatr. (2019) 65:160–8. doi: 10.1093/tropej/fmy030
38. Mercer, A, Haseen, F, Huq, NL, Uddin, N, Hossain Khan, M, and Larson, CP. Risk factors for neonatal mortality in rural areas of Bangladesh served by a large NGO programme. Health Policy Plan. (2006) 21:432–43. doi: 10.1093/heapol/czl024
39. Jolly, SP, Rahman, M, Afsana, K, Yunus, FM, and Chowdhury, AMR. Evaluation of maternal health service indicators in urban slum of Bangladesh. PLoS One. (2016) 11:e0162825. doi: 10.1371/journal.pone.0162825
40. Imtiaz, A, Farooq, G, Haq, ZU, Ahmed, A, and Anwar, S. Public private partnership and utilization of maternal and child health services in district Abbottabad, Pakistan. J Ayub Med Coll Abbottabad. (2017) 5:275–9.
41. Min, MS, Htut, HN, Richards, A, Whelan, R, Htoo, E, Kyi, KP, et al. Care cascade achieved by a program for micro-elimination of perinatal HBV transmission among pregnant women in Peri-urban Yangon, Myanmar. Hepatol Int. (2019) 14:1–470. doi: 10.1007/s12072-020-10030-4
42. Bhatia, M, Banerjee, K, Dixit, P, and Dwivedi, LK. Assessment of variation in cesarean delivery rates between public and private health facilities in India from 2005 to 2016. JAMA Netw Open. (2020) 3:e2015022. doi: 10.1001/jamanetworkopen.2020.15022
43. Ismail, AI, Abdul Majid, AH, Zakaria, MN, Abdullah, NAC, Hamzah, S, and Mukari, SZMS. Factors predicting health practitioners’ awareness of UNHS program in Malaysian non-public hospitals. Int J Pediatr Otorhinolaryngol. (2018) 109:78–84.
44. Dangoria, D, Pampallona, S, Lata, NS, and Bollini, P. A retrospective observational study of obstetric care in rural Andhra Pradesh by Dangoria charitable trust (1979 to 2009). Indian J Med Res. (2013) 138:928–34.
45. Bhartia, A, Sen Gupta Dhar, R, and Bhartia, S. Reducing caesarean section rate in an urban hospital serving women attending privately in India – a quality improvement initiative. BMC Pregnancy Childbirth. (2020) 20:1–7. doi: 10.1186/s12884-020-03234-x
46. Gatakaa, H, Ombech, E, Omondi, R, Otiato, J, Waringa, V, Okomo, G, et al. Expanding access to maternal, newborn and primary healthcare services through private-community-government partnership clinic models in rural Kenya: the Ubuntu-Afya kiosk model. BMC Health Serv Res. (2019) 19:914. doi: 10.1186/s12913-019-4759-9
47. Yadav, V, Kumar, S, Pallipamula, S, Memon, P, Rodríguez-Benavente, A, Herrera-Usagre, M, et al. ISQUA17-3126 measuring and improving the quality of private maternity care: lessons learned from a private sector qi program in India. Int J Qual Health Care. (2017) 29:26.
48. Hossain, J, Laterra, A, Paul, RR, Islam, A, Ahmmed, F, and Sarker, BK. Filling the human resource gap through public-private partnership: can private, community-based skilled birth attendants improve maternal health service utilization and health outcomes in a remote region of Bangladesh? PLoS One. (2020) 15:e0226923. doi: 10.1371/journal.pone.0226923
49. Baqui, AH, Rosecrans, AM, Williams, EK, Agrawal, PK, Ahmed, S, Darmstadt, GL, et al. NGO facilitation of a government community-based maternal and neonatal health programme in rural India: improvements in equity. Health Policy Plan. (2008) 23:234–43. doi: 10.1093/heapol/czn012
50. Conlon, CM, Serbanescu, F, Marum, L, Healey, J, LaBrecque, J, Hobson, R, et al. Saving mothers, giving life: it takes a system to save a mother. Glob Health Sci Pract. (2019) 7:S6–S26. doi: 10.9745/GHSP-D-18-00427
51. Bauer, MS, and Kirchner, J. Implementation science: what is it and why should I care? Psychiatry Res. (2020) 283:112376. doi: 10.1016/j.psychres.2019.04.025
52. Nilsen, P. Making sense of implementation theories, models and frameworks. Implement Sci IS. (2015) 10:53. doi: 10.1186/s13012-015-0242-0
53. Damschroder, LJ, Aron, DC, Keith, RE, Kirsh, SR, Alexander, JA, and Lowery, JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. (2009) 4:50. doi: 10.1186/1748-5908-4-50
54. Means, AR, Kemp, CG, Gwayi-Chore, MC, Gimbel, S, Soi, C, Sherr, K, et al. Evaluating and optimizing the consolidated framework for implementation research (CFIR) for use in low- and middle-income countries: a systematic review. Implement Sci IS. (2020) 15:17. doi: 10.1186/s13012-020-0977-0
55. Haldane, V, Jung, AS, Foo, CD, Shrestha, P, Urdaneta, E, Turk, E, et al. Integrating HIV and substance misuse services: a person-centred approach grounded in human rights. Lancet Psychiatry. (2022) 9:676–88. doi: 10.1016/S2215-0366(22)00159-6
Keywords: maternal health, newborn health, private sector, WHO NQPS, quality of healthcare, healthcare delivery, healthcare service delivery, quality interventions
Citation: Jung A-S, Yaqub N, Lattof SR, Strong J and Maliqi B (2025) Private sector quality interventions to improve maternal and newborn health in low- and middle-income countries: a scoping review. Front. Public Health. 13:1332612. doi: 10.3389/fpubh.2025.1332612
Edited by:
Maximilian Pangratius de Courten, Victoria University, AustraliaReviewed by:
Zahra Hoodbhoy, Aga Khan University, PakistanMaisam Najafizada, Memorial University of Newfoundland, Canada
Ana Pires, Universidade Atlântica, Portugal
Copyright © 2025 Jung, Yaqub, Lattof, Strong and Maliqi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Blerta Maliqi, bWFsaXFpYkB3aG8uaW50
 Anne-Sophie Jung
Anne-Sophie Jung Nuhu Yaqub
Nuhu Yaqub Samantha R. Lattof
Samantha R. Lattof Joe Strong3
Joe Strong3 Blerta Maliqi
Blerta Maliqi