- 1Department of Oncology, The Second Affiliated Hospital of Anhui Medical University, Hefei, China
- 2Anhui Medical University, Hefei, China
- 3Department of Oncology Cancer Centre, Lu’an Hospital of Anhui Medical University, Lu’an, China
- 4Department of Oncology, The First Affiliated Hospital of Anhui Medical University, Hefei, China
Background: Single photon emission computed tomography (SPECT) is becoming increasingly popular in oncology. This study endeavors to scrutinize the radiation protection knowledge, attitude, and practice (KAP) exhibited by healthcare professionals involved in this imaging modality.
Methods: This cross-sectional study was conducted between September 23, 2023, and October 23, 2023, at the Second Affiliated Hospital of Anhui Medical University, the First Affiliated Hospital of Anhui Medical University, and the People’s Hospital of Liuan. Demographic data and KAP scores were acquired through the administration of questionnaires.
Results: A total of 450 healthcare professionals participated in the study. Correlation analyses revealed significant positive correlations between knowledge and attitude, knowledge and practice, as well as attitude and practice. Multivariate analysis indicated that being over 40 years old was independently associated with good knowledge, as well as positive attitudes. Occupations as nurses and having no contact with SPECT patients were independently associated with a lower level of knowledge, as well as negative attitudes. Furthermore, being female, having an occupation as a nurse, and not having received relevant training were independently associated with negative practice.
Conclusion: Oncology healthcare professionals had suboptimal knowledge, negative attitude and inactive practice towards radiation protection in SPECT.
Introduction
SPECT (Single-Photon Emission Computed Tomography) is an advanced imaging technique that offers significant advantages in the early detection and evaluation of bone metastasis, particularly in lung cancer. By using a radioactive isotope tracer, such as 99mTc-MDP, SPECT enables a comprehensive assessment of bone metabolism, blood flow changes, and early-stage metastatic sites in a single imaging session. Its ability to integrate physiological, biochemical, functional, and metabolic scans makes it a valuable tool in identifying asymptomatic bone metastases, thus allowing for more precise treatment planning and improved patient outcomes (1–3). Bone metastasis is a common complication across various cancer types, notably breast and prostate cancers, and is associated with a higher risk of mortality. Early detection of bone metastasis in lung cancer is crucial for timely intervention. Although symptoms like bone pain, elevated blood alkaline phosphatase, or hypercalcemia can suggest bone involvement, conventional imaging methods, including CT scans, often lack the sensitivity needed to detect metastasis early (4–6). SPECT has an important clinical role in the evaluation of bone lesions in these patients (7). SPECT has also other important clinical applications, such as lung ventilation/perfusion studies (8), and sentinel node biopsy in breast cancer (9) and sentinel node biopsy in melanoma (10).
The Knowledge, Attitude, and Practices (KAP) survey serves as a diagnostic research tool, shedding light on a group’s understanding, beliefs, and actions concerning a specific subject, particularly within the domain of health literacy. This tool operates on the premise that knowledge positively influences attitudes, subsequently shaping behaviors (11–13). While existing research has primarily concentrated on the technical aspects of SPECT imaging and the formulation of radiation protection guidelines (14–16), there is a notable gap in the literature concerning the actual KAP levels among oncology healthcare professionals, especially in the context of SPECT. Understanding these factors is crucial for identifying areas where educational interventions may be necessary to enhance radiation safety. Given the radiation involved in SPECT, it is essential to understand the safety awareness and operational standards of the healthcare professionals using this technology to ensure the safety of both patients and medical staff. However, current research tends to emphasize the theoretical aspects of radiation protection, often overlooking the practical challenges healthcare professionals face in implementing these principles in their daily clinical practice.
This study focuses on assessing the KAP of radiation protection among oncology healthcare professionals, specifically in the context of SPECT. The aim is to understand their attitudes, knowledge of radiation safety, and acceptance of protective measures in SPECT. By enhancing the protection levels of healthcare professionals, ensuring radiation safety for SPECT patients, and minimizing risks for both patients and medical personnel, the study seeks to improve the overall quality of medical services.
Materials and methods
Study design and participants
This cross-sectional study was conducted between September 23, 2023, and October 23, 2023, at the Second Affiliated Hospital of Anhui Medical University, the First Affiliated Hospital of Anhui Medical University, and Lu’an Hospital of Anhui Medical University. Participants in the study comprised healthcare professionals specializing in oncology, including medical students. This study was approved by the Ethic Committee of the Second Affiliated Hospital of Anhui Medical University (YX2023-153), and all participants provided written informed consent.
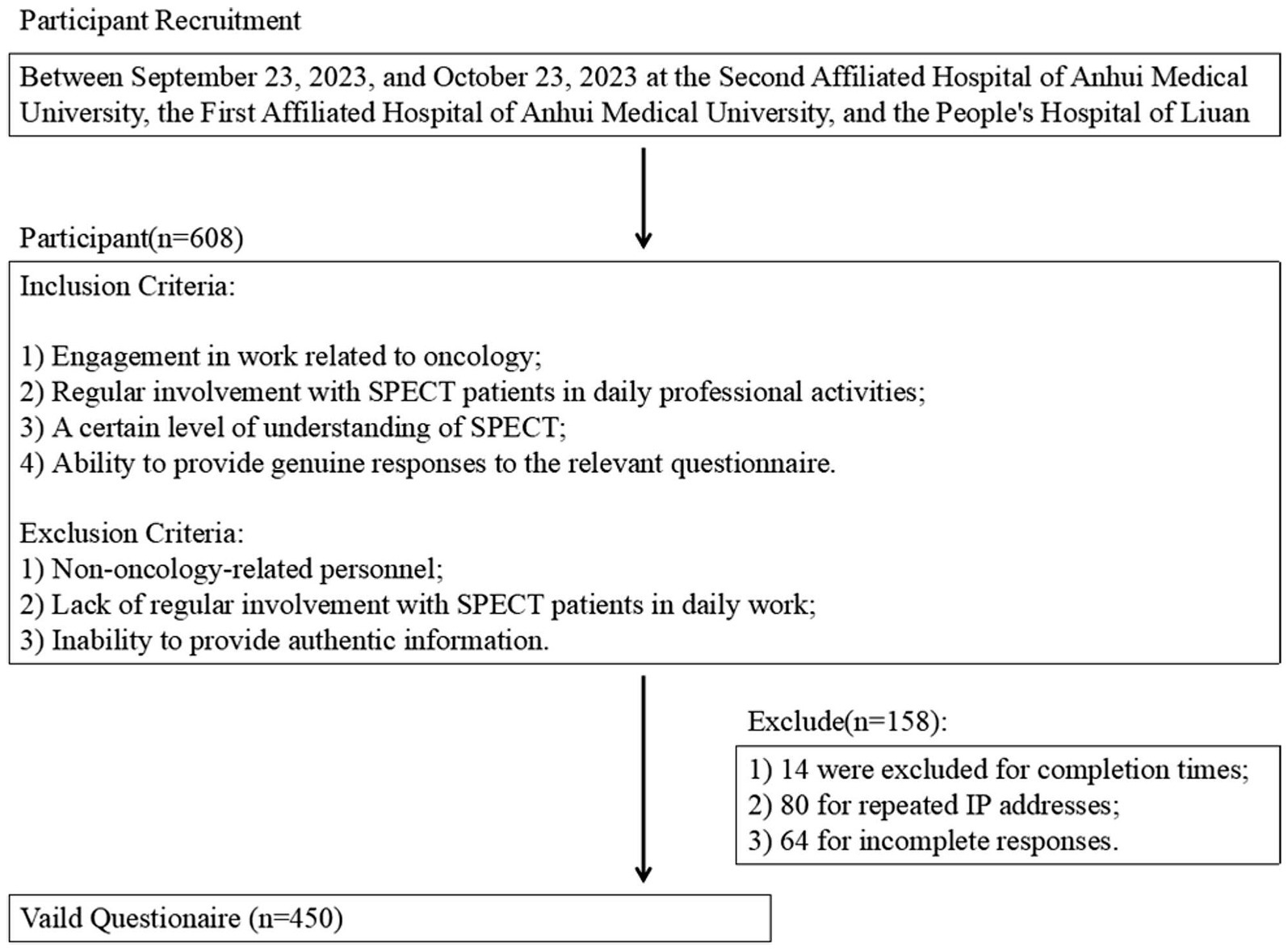
Inclusion criteria were defined as follows: (1) Engagement in work related to oncology; (2) Regular involvement with SPECT patients in daily professional activities; (3) A certain level of understanding of SPECT; and (4) Ability to provide genuine responses to the relevant questionnaire. Exclusion criteria encompassed: (1) Non-oncology-related personnel; (2) Lack of regular involvement with SPECT patients in daily work; and (3) Inability to provide authentic information.
The distribution of questionnaires to research subjects occurred through WeChat and QQ groups. The study encompassed a total of seven tertiary comprehensive hospitals, with specific involvement from three of these hospitals. The First Affiliated Hospital of Anhui Medical University comprised 4 wards in the oncology department and 4 wards in the radiotherapy department. The Second Affiliated Hospital of Anhui Medical University included 5 wards in the oncology department. People’s Hospital of Liuan comprised 2 wards in the oncology department and 1 ward in the radiotherapy department. The total number of healthcare professionals, including medical students, was approximately 700.
Sample size determination
The sample size was calculated using the following formula:
where z = 1.96 at 5% level of significance and 5%acceptable margin of error (d = 0.05). The proportion of the expected population based on previous studies or pilot studies is set at 50%. Based on the above, the sample size was calculated as 384 (17).
According to the inclusion and exclusion criteria, a total of 654 eligible medical staff from participating hospitals were identified. Ultimately, 608 questionnaires were distributed, and 450 valid responses were received, yielding an effective response rate of 74% (actual data to be filled). All data were collected in accordance with principles of confidentiality and voluntary participation, strictly for research purposes. For sample size calculation, prior studies in similar fields were referenced, with a significance level of α = 0.05 and a statistical power of 80%. Based on the objectives of the KAP survey in this study, the minimum required sample size was 384. The actual effective sample size of 450 met this requirement, ensuring sufficient statistical power for the analysis.
Procedures
Following the design of the questionnaire, feedback from three oncology experts was sought and incorporated for refinements. Subsequently, a pilot study was conducted with a limited sample size (30 responses), yielding a reliability coefficient of 0.814 and a Kaiser-Meyer-Olkin (KMO) measure of 0.815. Details of the questionnaire can be found in the Supplementary document “Questionnaire”.
The final questionnaire, presented in Chinese, encompasses data collection across four dimensions. It comprises 9 questions for basic information, 15 items for the knowledge dimension, 9 items for the attitude dimension, and 7 items for the practice dimension. During statistical analysis, scores were assigned based on the number of response options for each item. For instance, in the knowledge dimension, a correct answer was allocated 1 point, while an incorrect or unclear response received 0 points. In the attitude and practice dimensions, scores were assigned in descending order (positive to negative), with the final total score falling within a specified range (from lowest to highest). Items that could not be scored were treated as distinct categorical variables. Achieving scores exceeding 70% of the maximum in each section denoted sufficient knowledge, positive attitude, and proactive practice (18).
Statistical analysis
The sample size determination relied on a prior study (19), and subsequent descriptive analysis encompassed demographic information and dimension scores. Initial normality tests guided the choice between mean and standard deviation or median, 25th percentile, and 75th percentile representation for dimension scores. Count data for demographics and question responses were expressed as N(%). Dimension score differences among subjects with varied demographics were assessed using the Wilcoxon-Mann–Whitney test for non-normally distributed two-group comparisons, and Kruskal-Wallis analysis for three or more groups. Pearson correlation coefficients were used for normal distribution in correlation analyses; otherwise, Spearman coefficients were applied. In this analysis, we used the median score as the cut-off value for classification in both univariate and multivariate logistic regression analyses. Further details on how the median was determined and applied are provided in the Methods section to clarify the rationale and ensure consistency in the statistical approach. Variables inclusion in multivariate regression relied on univariate significance (p < 0.1), rounding p values to three decimal places, and considering p < 0.05 as statistically significant. A total of 608 questionnaires were collected; 14 were excluded for completion times, 80 for repeated IP addresses, and 64 for incomplete responses, resulting in 450 valid questionnaires.
Results
Demographic characteristics
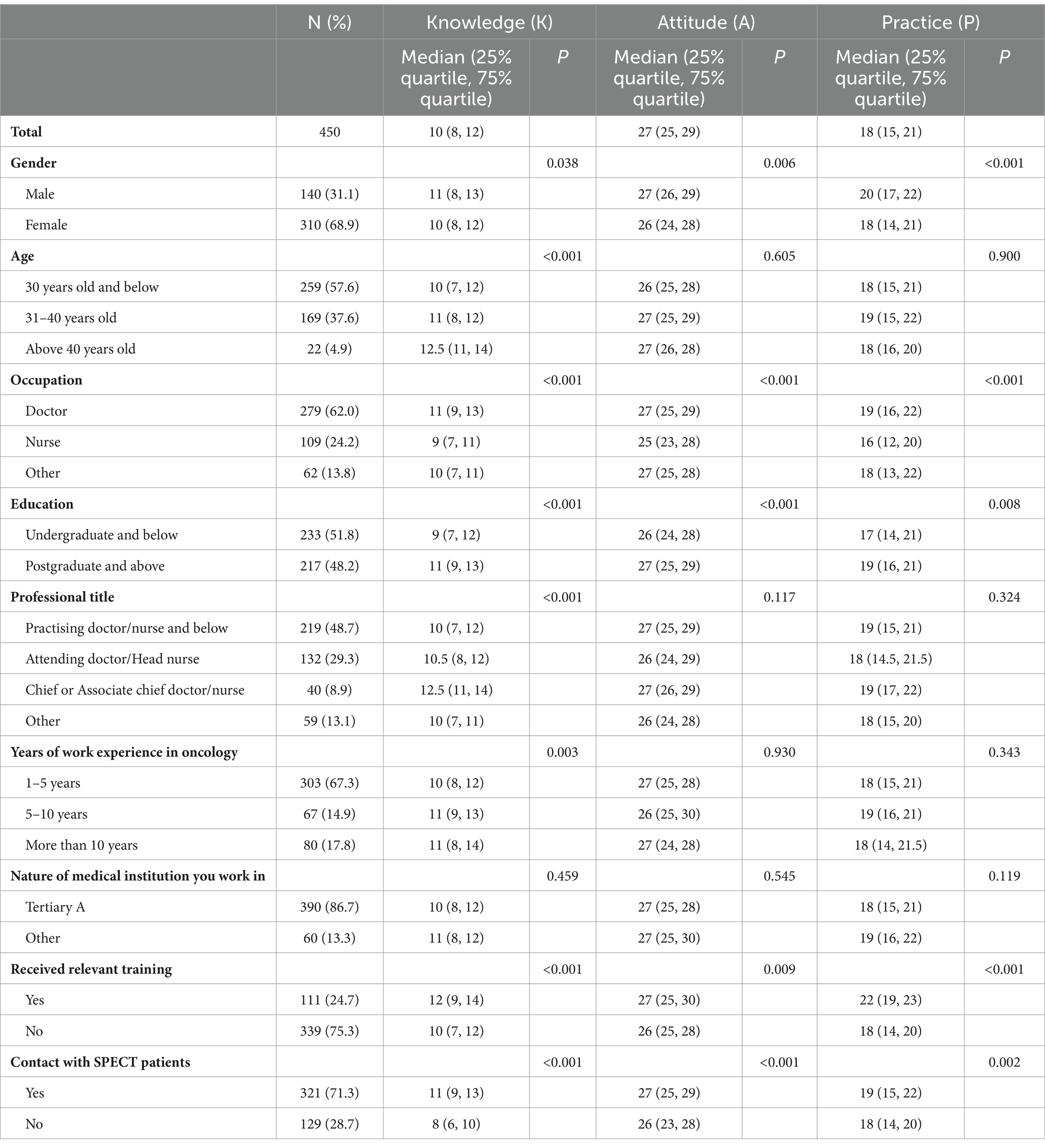
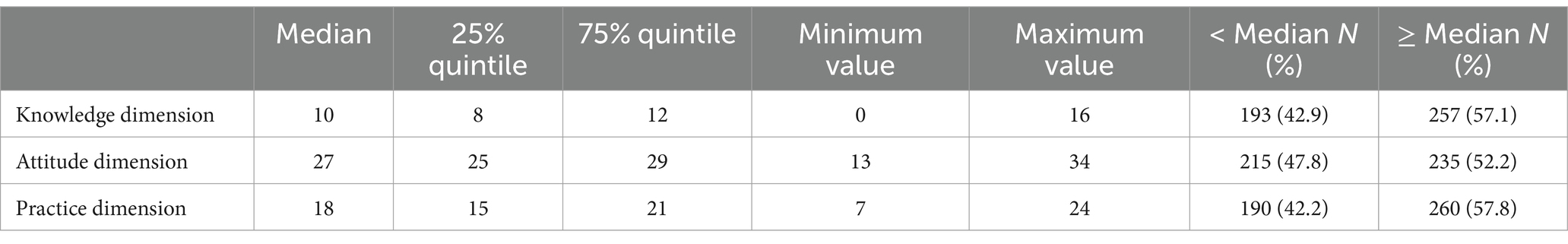
Among the healthcare professionals who participated in the study, 608 questionnaires were collected. Of these, 14 questionnaires were excluded because they were completed in less than 60 s or more than 1800 s, 80 questionnaires were excluded due to repeated IP addresses, and 64 questionnaires were incomplete, resulting in a total of 450 valid questionnaires (Figure 1). Of the valid respondents, 310 (68.9%) were female, 259 (57.6%) were aged 30 years and below, 279 (62.0%) were doctors, and 303 (67.3%) had worked in oncology for 1–5 years. In addition, 321 (71.3%) had contact with patients who required SPECT, while 339 (75.3%) had no SPECT-related training. The median (25th percentile, 75th percentile) score of knowledge, attitude, and practice were 10 (9, 20), 27 (21, 22) and 18 (12, 18) separately. Analyses of differences in demographic characteristics showed that differences in gender, occupation, education, receipt of relevant training, and contact with SPECT patients were more likely to have differences in knowledge, attitude, and practice scores. In addition, healthcare professionals with different age, professional title, years of work experience in oncology were more likely to have different levels of knowledge (p < 0.005) (Table 1). There were 54.1, 52.7, and 51.7%, respectively, had knowledge, attitude, and practice scores ≥ the median (Table 2).
Knowledge, attitudes, and practices
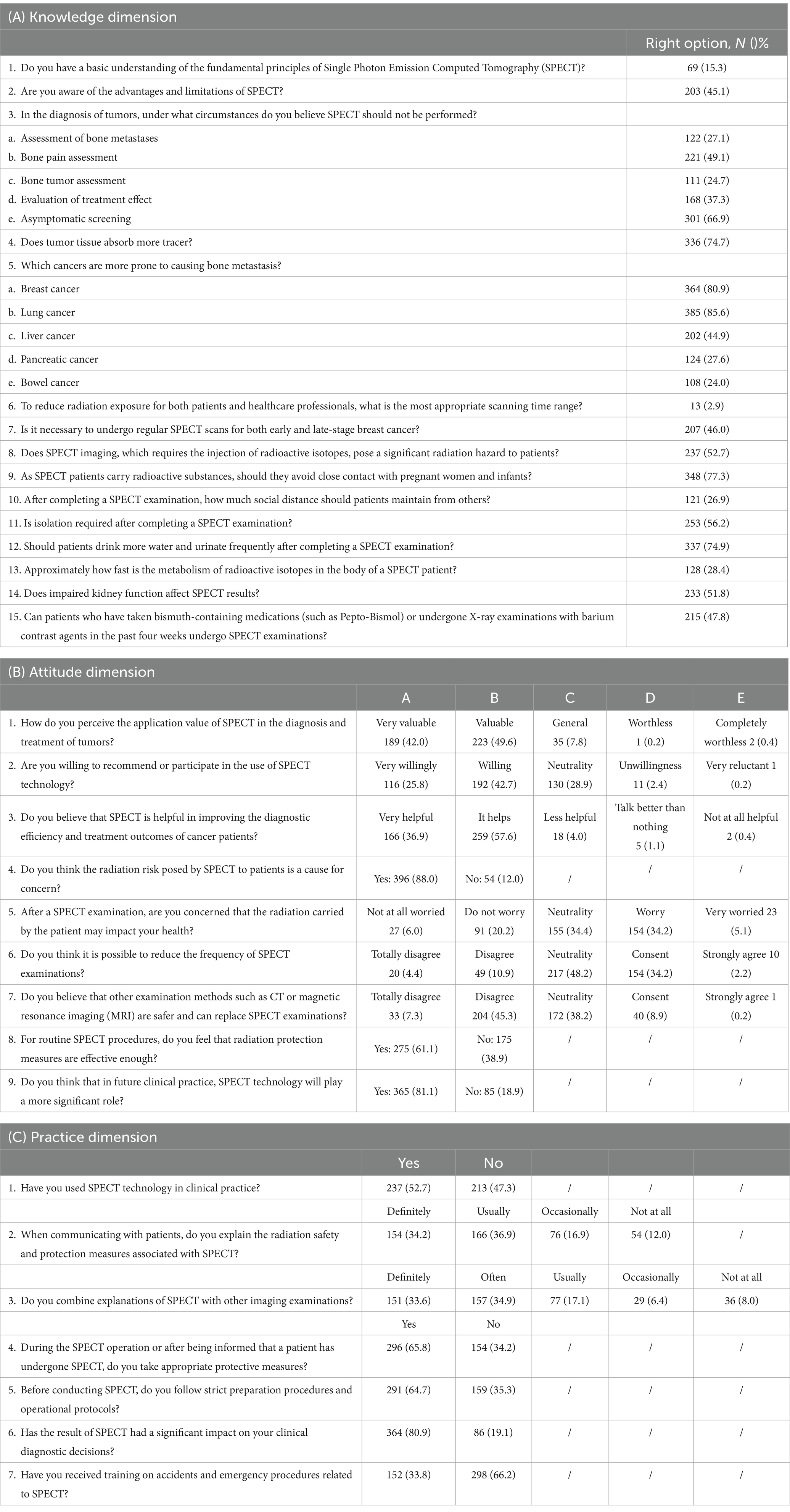
In the knowledge dimension, the highest proportion of participants answered correctly (77.3%) to the question “As SPECT patients carry radioactive substances, should they avoid close contact with pregnant women and infants?” (K9). On the contrary, for the question “To reduce radiation exposure for both patients and healthcare professionals, what is the most appropriate scanning time range? “(K6), only 2.9% of healthcare professionals answered correctly (Table 3A).
When it comes to attitudes related to SPECT, 88.0% of healthcare professionals believe that the risk of radiation to patients from SPECT should be a concern (A4). Concurrently, 57.6% reported that they considered SPECT to be more useful in improving the diagnostic efficiency and therapeutic outcomes of oncology patients (A3), and 42.7% were willing to recommend or participate in the usage of this technology (A2). Regarding the impact of patient-carried radiation on the participants’ own health (A5) and the possibility of reducing the times of SPECT (A6), 34.4 and 48.2% were neutral, respectively. In addition, 61.1% believed that current radiation protection measures were adequate (A8), and 81.1% believed that SPECT would play a more important role in clinical practice in the future (A9) (Table 3B).
The answer to the practice question revealed that 52.7% of healthcare professionals have used SPECT in their clinical practice (P1), 65.8% protect themselves when potentially exposed (P4), and 64.7% follow rigorous preparations and procedures before performing SPECT (P5). Further, 80.9% indicated that SPECT results had a significant impact on their clinical diagnostic decisions (P6). It is important to note that 66.2% reported that they had never received training on SPECT-related accidents and emergency handling (P7), indicating a significant risk (Table 3C).
Correlation analysis and multivariate logistic regression
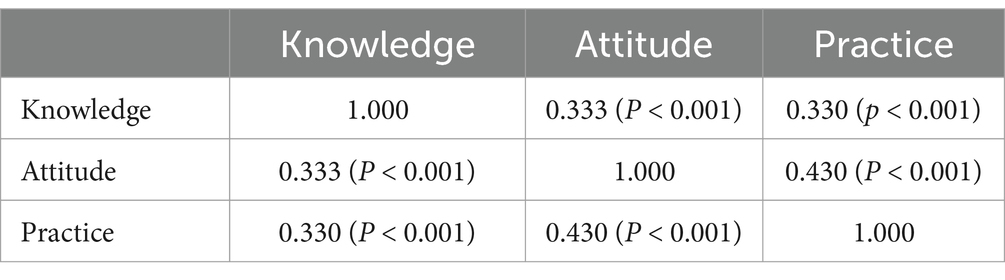
Correlation analyses shown that significant positive correlations were found between knowledge and attitude (r = 0.333, p < 0.001), knowledge and practice (r = 0.333, p < 0.001), as well as attitude and practice (r = 0.430, p < 0.001), respectively (Table 4).
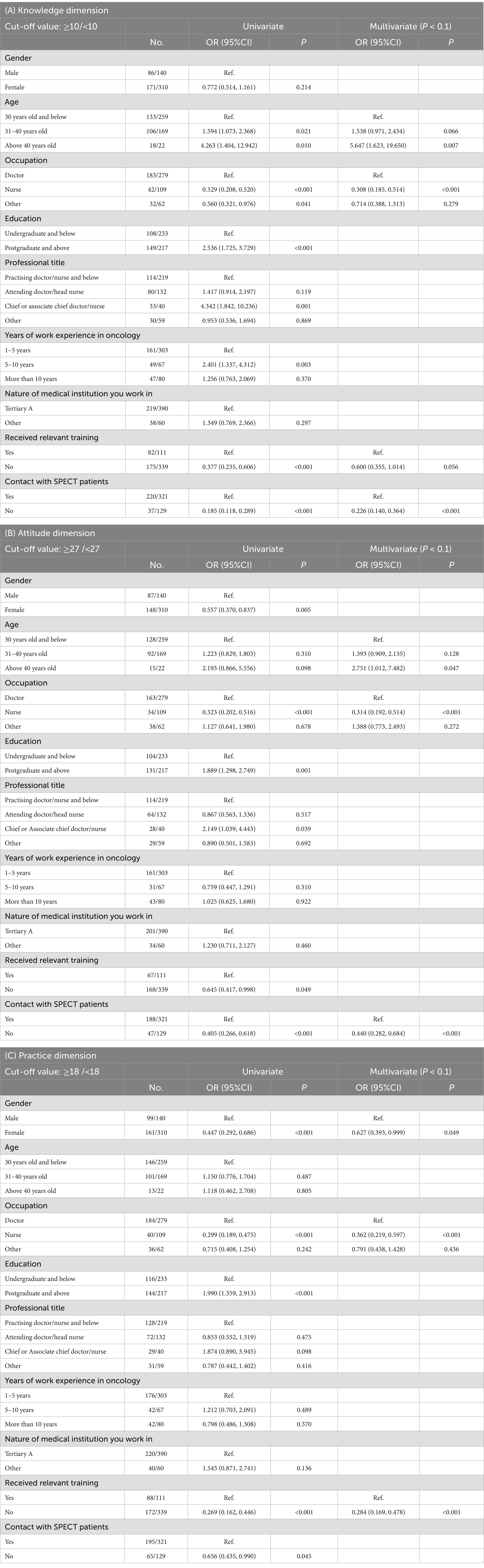
Variables with p < 0.1 in the univariate analysis were included in the multivariate analysis, which showed that being over 40 years was independently associated with good knowledge (OR = 5.647, 95% CI: [1.623–19.650], p = 0.007) as well as positive attitudes (OR = 2.751, 95% CI: [1.012–7.482], p = 0.047). An occupation as a nurse (OR = 0.308, 95% CI: [0.185–0.514], p < 0.001 and OR = 0.314, 95% CI: [0.192–0.514], p < 0.001) and no contact with SPECT patients (OR = 0.226, 95% CI: [0.140–0.364], p < 0.001 and OR = 0.440, 95% CI: [0.282–0.684], p < 0.001) were independently associated with a lower level of knowledge as well as negative attitudes (OR < 1, p < 0.005) (Tables 5A,B). Further, being female (OR = 0.627, 95% CI: [0.393–0.999], p = 0.049), an occupation as a nurse (OR = 0.362, 95% CI: [0.219–0.597], p < 0.001), and not having received relevant training (OR = 0.284, 95% CI: [0.169–0.478], p < 0.001) were independently associated with negative practice (Table 5C).
Discussion
The findings of this study indicate that oncology healthcare professionals exhibit suboptimal knowledge, negative attitudes, and inactive practices regarding radiation protection in SPECT. These results not only have implications for the operational behavior of healthcare workers but also significantly impact patient safety, the quality of care, and long-term health outcomes. To address these issues, the study recommends targeted educational interventions aimed at enhancing radiation protection practices among oncology healthcare professionals involved in SPECT. Key focus areas include healthcare professionals under 40, nurses, those without direct patient contact, and females. Tailored training programs addressing specific knowledge gaps and emphasizing protocol adherence are recommended to improve overall practice.
The study reveals deficiencies in medical management, primarily due to a lack of comprehensive SPECT-related training and experience disparities among healthcare professionals. This shortfall contributes to lower knowledge, attitude, and practice scores, indicating a broader systemic issue in ongoing professional development. Furthermore, the study reveals demographic disparities, with female healthcare workers and those with less direct contact with SPECT patients displaying lower proficiency. To address these issues, it’s crucial to implement mandatory, comprehensive training programs encompassing both theoretical and practical aspects of SPECT, tailored to different roles within the healthcare team. Additionally, fostering a culture of continuous learning through regular workshops and peer-led training sessions can help mitigate the experience gap, particularly for those less exposed to SPECT.
The median scores for knowledge, attitude, and practice were 10 (9, 20), 27 (21, 22), and 18 (12, 18), respectively, indicating room for improvement in all dimensions. A notable finding is the significant positive correlations between knowledge, attitude, and practice, reinforcing the interconnected nature of these components. Comparisons across demographic characteristics highlight variations in knowledge, attitude, and practice scores, emphasizing the need for targeted interventions. For instance, older age was independently associated with good knowledge and positive attitudes, while being a nurse and lacking contact with SPECT patients correlated with lower knowledge and negative attitudes. These results align with existing literature, emphasizing the influence of demographic factors on radiation protection awareness and practices among healthcare professionals (23).
In the knowledge dimension, this study identified significant gaps among oncology healthcare professionals regarding the fundamental principles and safety measures associated with SPECT technology. The lack of understanding, particularly in areas such as radiation metabolism, optimal scanning times, and patient management, indicates a need for more focused educational initiatives. Recent studies have highlighted strategies to address these gaps in radiation safety knowledge. For instance, a study propose comprehensive measures for advancing radiation protection and safety systems in nuclear medicine, which could be adapted to address these deficiencies in SPECT technology training (24). To address these deficiencies, it is recommended to implement targeted training programs that emphasize practical knowledge application. For instance, integrating case-based learning modules that simulate real-world scenarios involving SPECT can enhance the comprehension and retention of key concepts. Additionally, creating specialized workshops that focus on the nuances of radiation safety in SPECT, particularly tailored to different professional roles (e.g., technicians vs. physicians), can ensure that training is relevant and immediately applicable (21, 25). Reference to prior studies has shown that interactive training sessions significantly improve knowledge retention in similar contexts (26, 27).
In terms of attitude, although most healthcare professionals acknowledge the importance of SPECT in oncology, there is a notable lack of confidence in current radiation safety measures and a considerable concern about the potential risks posed by patients who have undergone SPECT. To improve these attitudes, it is crucial to implement regular feedback loops where healthcare professionals can share concerns and experiences related to radiation safety, which can then be addressed in subsequent training or guideline updates. Establishing a radiation safety mentorship program, where less experienced staff are paired with experts, can also help alleviate concerns and build confidence in safety protocols. Furthermore, promoting a culture of safety through regular, data-driven updates on the efficacy of existing safety measures, supported by transparent incident reporting and resolution processes, can reinforce the perceived value and effectiveness of radiation protection practices (22, 28).
In the practice dimension, while some healthcare professionals adhere to basic radiation protection guidelines during SPECT procedures, there is a significant portion that does not fully comply with established protocols, particularly regarding emergency procedures. To enhance compliance, it is recommended to incorporate mandatory, hands-on training sessions that simulate emergency scenarios involving radiation exposure. These sessions should be followed by debriefings that allow participants to reflect on their actions and learn from any mistakes in a controlled environment (29–31). Additionally, implementing periodic audits of radiation safety practices, with constructive feedback and targeted corrective actions, can help maintain high standards of safety. Specific strategies might include the use of real-time monitoring tools that alert staff when safety protocols are not followed, supported by immediate corrective training (32, 33). Furthermore, tailoring these interventions to the specific needs of different professional groups—such as differentiating training for those who primarily perform SPECT versus those who occasionally encounter it—can ensure that all healthcare professionals receive the most relevant and effective guidance (34).
Multivariate analysis further illuminates factors independently associated with knowledge, attitudes, and practices. Age over 40 emerged as a positive predictor of good knowledge and positive attitudes, aligning with studies emphasizing the cumulative experience and continuous learning associated with age (35, 36). Conversely, being a nurse and lacking contact with SPECT patients were linked to lower knowledge and negative attitudes, emphasizing the need for targeted interventions in these subgroups. Additionally, being female, working as a nurse, and lacking relevant training were independently associated with negative practices, emphasizing the role of gender and education in shaping healthcare professionals’ adherence to radiation protection protocols. These findings underscore the need for tailored educational programs targeting specific demographic groups and professional categories.
One limitation of this study is its cross-sectional design, which allows for the identification of associations but not causation. Additionally, the research was conducted in specific healthcare settings, potentially limiting the generalizability of the findings to other contexts. The reliance on self-reported data through questionnaires introduces the possibility of response bias, and the study’s focus on a specific geographical area may affect the external validity of the results. Furthermore, the study’s scope did not explore the impact of continuous professional development or specific training programs, and the reliance on healthcare professionals’ self-reported practices might not fully reflect their actual behavior in clinical settings. Moreover, the study did not examine whether there is a knowledge gap between youth who participate in similar sports without experiencing ACL injuries and those who have experienced ACL injuries, a potentially significant area for future investigation. Additionally, similar studies, such as the QUADRANT study (37), have provided systematic approaches for detecting knowledge, attitude, and practice deficiencies in medical fields, which could inform the design of future research. The use of online surveys and convenience sampling, while practical, may also introduce biases due to limited access for certain demographics and the accuracy of self-reported responses.
In conclusion, oncology healthcare professionals had suboptimal knowledge, negative attitude and inactive practice towards radiation protection in SPECT. Improving radiation protection practices among oncology healthcare professionals involved in SPECT can be achieved through targeted educational interventions. Specifically, efforts should focus on healthcare professionals under 40, nurses, and those without direct SPECT patient contact. Tailored training programs addressing these groups’ knowledge gaps and attitudes are recommended, emphasizing increased awareness and adherence to radiation protection protocols.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
This work has been carried out in accordance with the Declaration of Helsinki (2000) of the World Medical Association. This study was approved by the Ethic Committee of the Second Affiliated Hospital of Anhui Medical University (YX2023-153). All participants provided written informed consent.
Author contributions
MY: Conceptualization, Funding acquisition, Project administration, Supervision, Writing – original draft, Writing – review & editing. XC: Data curation, Resources, Validation, Visualization, Writing – original draft, Writing – review & editing. XL: Formal analysis, Validation, Writing – original draft, Writing – review & editing. XJ: Methodology, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. YD: Validation, Visualization, Writing – original draft, Writing – review & editing. FL: Methodology, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by the Institute of Energy, Hefei Comprehensive National Science Center (nos. GXXT-2022-003 and 21KZS202) to Min Yan.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1512686/full#supplementary-material
References
1. Asdahl, PH, Sundbøll, J, Adelborg, K, Rasmussen, TB, Seesaghur, AM, Hernandez, RK, et al. Cardiovascular events in Cancer patients with bone metastases-a Danish population-based cohort study of 23, 113 patients. Cancer Med. (2021) 10:4885–95. doi: 10.1002/cam4.4027
2. Brenner, AI, Koshy, J, Morey, J, Lin, C, and DiPoce, J. The bone scan. Semin Nucl Med. (2012) 42:11–26. doi: 10.1053/j.semnuclmed.2011.07.005
3. Yamagata, AS, Freire, PP, Jones Villarinho, N, Teles, RHG, Francisco, KJM, Jaeger, RG, et al. Transcriptomic response to acidosis reveals its contribution to bone metastasis in breast Cancer cells. Cells. (2022) 11:544. doi: 10.3390/cells11030544
4. Fang, Y, Qiu, J, Jiang, ZB, Xu, SR, Zhou, ZH, and He, RL. Increased serum levels of Mir-214 in patients with Pca with bone metastasis may serve as a potential biomarker by targeting Pten. Oncol Lett. (2019) 17:398–405. doi: 10.3892/ol.2018.9522
5. Ishibashi, N, Maebayashi, T, Kimura, Y, and Okada, M. Bone scan index on bone scintigraphy and radiation therapy for bone metastases from cancers other than prostate and breast cancers: a retrospective observational study. J Cancer Res Ther. (2022) 18:1716–21. doi: 10.4103/jcrt.JCRT_1558_20
6. Jian, L, Shi-Wei, L, Dan, J, Juan, W, and Wei, Z. Gpr 84 potently inhibits Osteoclastogenesis and alleviates Osteolysis in bone metastasis of colorectal Cancer. J Orthop Surg Res. (2023) 18:3. doi: 10.1186/s13018-022-03473-y
7. Van den Wyngaert, T, Strobel, K, Kampen, WU, Kuwert, T, van der Bruggen, W, Mohan, HK, et al. The Eanm practice guidelines for bone scintigraphy. Eur J Nucl Med Mol Imaging. (2016) 43:1723–38. doi: 10.1007/s00259-016-3415-4
8. Bajc, M, Schümichen, C, Grüning, T, Lindqvist, A, Le Roux, PY, Alatri, A, et al. Eanm guideline for ventilation/perfusion single-photon emission computed tomography (Spect) for diagnosis of pulmonary embolism and beyond. Eur J Nucl Med Mol Imaging. (2019) 46:2429–51. doi: 10.1007/s00259-019-04450-0
9. Mucientes Rasilla, J, Farge Balbín, L, Cardona Arboniés, J, Moreno Elola-Olaso, A, Delgado-Bolton, R, Izarduy Pereyra, L, et al. Spect-Ct: a new tool for localisation of sentinel lymph nodes in breast Cancer patients. Rev Esp Med Nucl. (2008) 27:183–90. doi: 10.1157/13121028
10. Mucientes Rasilla, J, Cardona Arboniés, J, Delgado Bolton, R, Izarduy Pereyra, L, Salazar Andía, G, Prieto Soriano, A, et al. Spect-Ct in sentinel node detection in patients with melanoma. Rev Esp Med Nucl. (2009) 28:229–34. doi: 10.1016/j.remn.2009.03.002
11. Khalid, A, Haque, S, Alvi, S, Ferdous, M, Genereux, O, Chowdhury, N, et al. Promoting health literacy about Cancer screening among Muslim immigrants in Canada: perspectives of imams on the role they can play in community. J Prim Care Community Health. (2022) 13:21501319211063051. doi: 10.1177/21501319211063051
12. Koni, A, Taha, S, Daifallah, A, Koni, M, Abutaha, S, Sabateen, A, et al. A cross-sectional evaluation of knowledge, attitudes, practices, and perceived challenges among Palestinian pharmacists regarding Covid-19. SAGE Open Med. (2022) 10:20503121211069278. doi: 10.1177/20503121211069278
13. Shubayr, MA, Kruger, E, and Tennant, M. Oral health Providers' views of Oral health promotion in Jazan, Saudi Arabia: a qualitative study. BMC Health Serv Res. (2023) 23:214. doi: 10.1186/s12913-023-09170-8
14. Coria-Domínguez, L, Vallejo-Armenta, P, Luna-Gutiérrez, M, Ocampo-García, B, Gibbens-Bandala, B, García-Pérez, F, et al. [(99m)Tc]Tc-Ifap Radioligand for Spect/Ct imaging of the tumor microenvironment: kinetics, radiation dosimetry, and imaging in patients. Pharmaceuticals (Basel). (2022) 15:590. doi: 10.3390/ph15050590
15. Fan, M, Yao, J, Zhao, Z, Zhang, X, and Lu, J. Application of (99m)Tc-labeled Wl12 peptides as a tumor Pd-L1-targeted Spect imaging agent: kit formulation, preclinical evaluation, and study on the influence of Coligands. Pharmaceuticals (Basel). (2024) 17:906. doi: 10.3390/ph17070906
16. Mostafa, R, Abdelhafez, YG, Abougabal, M, Nardo, L, and Elkareem, MA. Two-bed Spect/Ct versus planar bone scintigraphy: prospective comparison of reproducibility and diagnostic performance. Nucl Med Commun. (2021) 42:360–8. doi: 10.1097/mnm.0000000000001353
17. Bartlett, JE, Kotrlik, JW, and Higgins, CC. Organizational research: determining appropriate sample size in survey research. Inf Technol Learn Perform J. (2001) 19:43–50.
18. Lee, F, and Suryohusodo, AA. Knowledge, attitude, and practice assessment toward Covid-19 among communities in East Nusa Tenggara, Indonesia: a cross-sectional study. Front Public Health. (2022) 10:957630. doi: 10.3389/fpubh.2022.957630
19. Gebeyehu, DT, Bekele, D, Mulate, B, Gugsa, G, and Tintagu, T. Knowledge, attitude and practice of animal producers towards antimicrobial use and antimicrobial resistance in Oromia zone, north eastern Ethiopia. PLoS One. (2021) 16:e0251596. doi: 10.1371/journal.pone.0251596
20. Mota, JM, Armstrong, AJ, Larson, SM, Fox, JJ, and Morris, MJ. Measuring the unmeasurable: automated bone scan index as a quantitative endpoint in prostate Cancer clinical trials. Prostate Cancer Prostatic Dis. (2019) 22:522–30. doi: 10.1038/s41391-019-0151-4
21. Alqahtani, MM, Willowson, KP, Constable, C, Fulton, R, and Kench, PL. Optimization of (99m) Tc whole-body Spect/Ct image quality: a phantom study. J Appl Clin Med Phys. (2022) 23:e13528. doi: 10.1002/acm2.13528
22. Forsetlund, L, O'Brien, MA, Forsén, L, Reinar, LM, Okwen, MP, Horsley, T, et al. Continuing education meetings and workshops: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. (2021) 9:Cd003030. doi: 10.1002/14651858.CD003030.pub3
23. Kim, YJ, Cha, ES, and Lee, WJ. Occupational radiation procedures and doses in south Korean dentists. Community Dent Oral Epidemiol. (2016) 44:476–84. doi: 10.1111/cdoe.12237
24. Giammarile, F, Knoll, P, Kunikowska, J, Paez, D, Estrada Lobato, E, Mikhail-Lette, M, et al. Guardians of precision: advancing radiation protection, safety, and quality Systems in Nuclear Medicine. Eur J Nucl Med Mol Imaging. (2024) 51:1498–505. doi: 10.1007/s00259-024-06633-w
25. Knowland, J, Lipman, S, Lattanze, R, Kingg, J, Ryan, K, and Perrin, S. Technical note: characterization of technology to detect residual injection site radioactivity. Med Phys. (2019) 46:2690–5. doi: 10.1002/mp.13536
26. Besse, H, and Bailly, M. Case report: potential applications of using a 3d-ring Czt Spect for lymphoscintigraphic exploration of lower limb edema. Front Med (Lausanne). (2022) 9:866541. doi: 10.3389/fmed.2022.866541
27. Peters, SMB, van der Werf, NR, Segbers, M, van Velden, FHP, Wierts, R, Blokland, K, et al. Towards standardization of absolute Spect/Ct quantification: a multi-center and multi-vendor phantom study. EJNMMI Phys. (2019) 6:29. doi: 10.1186/s40658-019-0268-5
28. Longhini, J, Rossettini, G, and Palese, A. Massive open online courses for Nurses' and healthcare Professionals' continuous education: a scoping review. Int Nurs Rev. (2021) 68:108–21. doi: 10.1111/inr.12649
29. Mineki, T, Yoda, S, Hatta, T, Hayase, M, Monno, K, Hori, Y, et al. Risk stratification of cardiovascular events in very elderly patients with known or suspected coronary artery disease who had Normal single-photon emission computed tomographic myocardial perfusion imaging findings. Intern Med. (2019) 58:3351–9. doi: 10.2169/internalmedicine.2843-19
30. Wu, S, Ma, K, Qiao, WL, Zhao, LZ, Liu, CC, Guo, LL, et al. Anti-metastatic effect of 131i-labeled Buthus martensii Karsch Chlorotoxin in gliomas. Int J Mol Med. (2018) 42:3386–94. doi: 10.3892/ijmm.2018.3905
31. Zhang, J, Li, S, Krol, A, Schmidtlein, CR, Lipson, E, Feiglin, D, et al. Infimal convolution-based regularization for Spect reconstruction. Med Phys. (2018) 45:5397–410. doi: 10.1002/mp.13226
32. Dincer, N, Ugurluer, G, Zoto Mustafayev, T, Gungor, G, Atalar, B, Guven, K, et al. Magnetic resonance image-guided Hypofractionated ablative radiation therapy for hepatocellular carcinoma with tumor Thrombus extending to the right atrium. Cureus. (2022) 14:e23981. doi: 10.7759/cureus.23981
33. Fischli, S, Suter-Widmer, I, Nguyen, BT, Müller, W, Metzger, J, Strobel, K, et al. The significance of 18f-Fluorocholine-pet/Ct as localizing imaging technique in patients with primary hyperparathyroidism and negative conventional imaging. Front Endocrinol (Lausanne). (2017) 8:380. doi: 10.3389/fendo.2017.00380
34. Alvieri, F, Mamani, JB, Nucci, MP, Oliveira, FA, Filgueiras, IS, Rego, GNA, et al. Methods of granulocyte isolation from human blood and labeling with multimodal superparamagnetic Iron oxide nanoparticles. Molecules. (2020) 25:765. doi: 10.3390/molecules25040765
35. Gartz, J, and O'Rourke, J. Telehealth educational interventions in nurse practitioner education: an integrative literature review. J Am Assoc Nurse Pract. (2020) 33:872–8. doi: 10.1097/jxx.0000000000000488
36. Ju, IE, Trieu, D, Chang, SB, Mungovan, SF, and Patel, MI. Surgeon experience and erectile function after radical prostatectomy: a systematic review. Sex Med Rev. (2021) 9:650–8. doi: 10.1016/j.sxmr.2020.09.006
37. Delgado Bolton, RC, Giammarile, F, Howlett, DC, Jornet, N, Brady, AP, Coffey, M, et al. The Quadrant study: current status and recommendations for improving uptake and implementation of clinical audit of medical radiological procedures in Europe-the nuclear medicine perspective. Eur J Nucl Med Mol Imaging. (2023) 50:2576–81. doi: 10.1007/s00259-023-06203-6
Keywords: single photon emission computed tomography, healthcare professional, knowledge, attitude, practice
Citation: Yan M, Cheng X, Li X, Jin X, Dai Y and Li F (2024) Study on the knowledge, attitude and practice of single photon emission computed tomography among oncology healthcare professionals. Front. Public Health. 12:1512686. doi: 10.3389/fpubh.2024.1512686
Edited by:
Antoaneta Ene, Dunarea de Jos University, RomaniaReviewed by:
Roberto C. Delgado Bolton, Hospital San Pedro, SpainMihaela-Emilia Dumitru, Sfantul Apostol Andrei Emergency Clinic, Romania
Copyright © 2024 Yan, Cheng, Li, Jin, Dai and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fanfan Li, ZmZsYWh5a2R4QDE2My5jb20=; Min Yan, NjAzMzc3ODc3QHFxLmNvbQ==
 Min Yan
Min Yan Xiang Cheng
Xiang Cheng Xinyu Li1
Xinyu Li1 Xiangting Jin
Xiangting Jin Ying Dai
Ying Dai Fanfan Li
Fanfan Li