- 1School of Economics and Management, Anhui Normal University, Wuhu, China
- 2Oregon State University, Corvallis, OR, United States
Introduction: With the intensification of global aging, health management for the older adult has become a significant societal concern. Addressing challenges such as data diversity, health status complexity, long-term dependence, and data privacy is crucial for predicting older adult health behaviors.
Methods: This study designs and implements a smart older adult care service model incorporating modules like multimodal data fusion, data loss processing, nonlinear prediction, emergency detection, and privacy protection. It leverages multi-source datasets and market research for accurate health behavior prediction and dynamic management.
Results: The model demonstrates excellent performance in health behavior prediction, emergency detection, and delivering personalized services. Experimental results show an increase in accuracy and robustness in health behavior prediction.
Discussion: The model effectively addresses the needs of smart older adult care, offering a promising solution to enhance prediction accuracy and system robustness. Future improvements, integrating more data and optimizing technology, will strengthen its potential for providing comprehensive support in older adult care services.
1 Introduction
As the global population ages, the health issues of the older adult population are receiving increasing attention (1–3). According to statistics, the proportion of the global older adult population continues to rise. By 2050, the population aged 60 and above will account for 22% of the worldwide population. This trend brings many challenges. In particular, in the context of limited medical resources and insufficient older adult care services, how to predict the health behaviors of the older adult through scientific and effective methods and take preventive measures promptly has become an urgent problem to be solved in many fields such as public health, social security, and smart older adult care. The prediction of the health behaviors of the older adult is not only related to improving individual health and quality of life but also has important significance for reducing medical costs and alleviating family and social burdens.
The research on the prediction of health behaviors of the older adult can be traced back to decades ago. Early studies mainly relied on traditional health assessment methods, such as regular physical examinations, questionnaires, and expert interviews. Although these methods can provide an overview of health status to a certain extent, their drawbacks are also becoming increasingly apparent. First, these methods are highly dependent on the participation and cooperation of the older adult themselves. The data acquisition process is complex and time-sensitive, making it difficult to reflect the dynamic health status of the older adult promptly. Second, traditional methods make it difficult to quantify individual differences and cannot meet the needs of personalized health management. With the rapid growth of the older adult population, traditional health prediction methods have gradually exposed problems such as insufficient data and low prediction accuracy. New technical means are urgently needed to improve the prediction effect.
In recent years, the rapid development of the Internet of Things (IoT), big data, and artificial intelligence technologies has provided new opportunities for predicting the health behavior of the older adult. Smart older adult care has gradually become a frontier research field. By combining sensor networks, wearable devices, smart home systems, and artificial intelligence algorithms, real-time monitoring and analysis of the daily behavior and health data of the older adult can be achieved (4–6). Smart older adult care technology can not only help the older adult live independently but also effectively reduce the incidence of emergencies caused by health problems. For example, smart bracelets can monitor the older adult's heart rate, blood pressure, body temperature and other physiological data in real-time, and transmit the data to the cloud through wireless networks, and combine big data analysis technology to dynamically evaluate health behaviors. At the same time, smart home devices can identify potential health risks and provide timely warnings by monitoring the older adult's daily activities, such as getting up, going to bed, eating, and exercising. These technical means based on the Internet of Things and artificial intelligence have opened up new paths for research on predicting the health behavior of the older adult. However, although current smart older adult care technologies have shown great potential in older adult health management, they still face many challenges. First, the prediction of older adult health behaviors involves the processing of multi-source heterogeneous data, such as physiological data from wearable devices, activity data from smart homes, and electronic medical records and medication records (4, 7). How to effectively integrate these data to form a high-quality prediction model is an urgent problem to be solved. Secondly, the health behaviors of the older adult are highly individualized and uncertain. There are significant differences in the living habits, health conditions, and disease risks of different individuals, which makes health behavior prediction face complex modeling challenges. In addition, how to provide accurate and timely health behavior predictions while ensuring data privacy and security is also an issue that needs to be considered in current smart older adult care research.
To cope with the multiple challenges in predicting the health behavior of the older adult, this paper proposes and implements a health behavior prediction platform for the older adult that integrates multi-source data. The platform collects the health data of the older adult in real-time through IoT devices and uses multimodal data fusion technology to effectively integrate data from different sources. The platform can comprehensively monitor and analyze the physiological parameters, daily activities, environmental factors, etc. of the older adult, and handle the problem of missing data through data interpolation and robustness enhancement algorithms. The platform also pays special attention to data privacy protection, and adopts federated learning and differential privacy mechanisms to ensure that the data of the older adult are processed in a safe environment. Through these technologies, the platform can not only automatically collect and analyze data, but also provide personalized health management suggestions based on the health status of the older adult, thereby improving the quality of life of the older adult and reducing the care burden of society and family.
To verify the effectiveness of the proposed platform, this paper designed and conducted several experiments, which were tested in different scenarios such as community care, home care, and hospital care. The experimental data came from multiple sources, including physiological data from wearable devices of the older adult, activity data from smart home systems, and electronic medical record data from hospitals. The experimental results show that the proposed prediction platform has good adaptability and stability in different scenarios, and the prediction accuracy is significantly better than traditional methods. In the community care scenario, the platform can accurately predict the risk of falls of the older adult and issue early warnings in time; in the home care scenario, the platform can identify abnormal living habits of the older adult, such as long-term sedentary or increased nighttime activities; in the hospital care scenario, the platform predicts the risk of disease recurrence by analyzing the historical medical records of the older adult, and provides scientific intervention suggestions for medical staff.
The main contributions of this paper are as follows:
1. Firstly, a health behavior prediction platform for the older adult that integrates multi-source data was designed and implemented, and effective data fusion and modeling methods were proposed, which can accurately predict the health behavior of the older adult and issue early warnings promptly.
2. Secondly, the deep learning model proposed in this paper combines the advantages of convolutional neural networks and long short-term memory networks and enhances the capture of key health characteristics through the attention mechanism, thereby significantly improving the accuracy of prediction.
3. Thirdly, through experimental verification in different older adult care scenarios, the wide applicability and robustness of the platform were demonstrated, providing theoretical and technical support for further research in the field of smart older adult care.
4. Finally, this paper discusses the challenges and development directions in future research on predicting health behaviors of the older adult, especially proposing new ideas in multi-source data fusion, personalized health management, and data privacy protection.
In short, with the rapid growth of the older adult population, how to use advanced technical means to predict and manage the health behavior of the older adult is an important issue that needs to be solved urgently. This paper demonstrates the broad prospects of the field of smart older adult care by building a health behavior prediction platform for the older adult that integrates multi-source data, and provides strong theoretical support and practical reference for future research.
2 Related work
As an important part of smart older adult care, health behavior prediction for the older adult has received extensive attention and in-depth research in recent years. The progress of related work is mainly concentrated in the following aspects: improvement of traditional health behavior prediction methods, health monitoring systems based on the Internet of Things, and health behavior prediction in smart older adult care.
2.1 Traditional health behavior prediction methods
In the early research on predicting the health behavior of the older adult, traditional methods (8–10) mainly relied on questionnaires, health examinations, and expert evaluations. These methods collect basic health data of the older adult, such as blood pressure, blood sugar, heart rate, etc., and combine their living habits and medical history to assess health risks and predict possible health problems. However, these traditional methods face many challenges. First, these methods are highly dependent on the participation and cooperation of the older adult themselves. The data collection process is usually complicated and the amount of data is limited. This static data cannot fully reflect the dynamic changes in the health status of the older adult, resulting in insufficient timeliness and accuracy of the prediction (11). Second, traditional methods make it difficult to quantify individual differences, especially when facing a diverse older adult population, and it is difficult to provide personalized health management plans. In addition, methods such as health examinations and questionnaires often require high human and material resources are not sustainable, and cannot be promoted on a large scale. Nevertheless, traditional methods laid the foundation for early research on the health of the older adult and provided a reference for subsequent research. With the advancement of data collection technology and analysis methods, researchers have gradually realized the need to combine emerging technologies to make up for the shortcomings of traditional methods, to achieve more accurate and real-time health behavior prediction.
2.2 Health monitoring system based on internet of things
The development of IoT technology has brought new opportunities for monitoring and predicting the health behavior of the older adult. In recent years, researchers have increasingly used IoT devices for real-time health monitoring, such as smart bracelets, smart homes, and wearable sensors. These devices can collect physiological data and daily activity data of the older adult in real-time, and transmit the data to the cloud for analysis through wireless networks, thereby realizing dynamic monitoring of health status (12–14). Health monitoring systems based on IoT have many advantages. First, these systems can collect data in real-time and discover changing trends in the health status of the older adult through data analysis. For example, smart bracelets can monitor data such as heart rate, blood pressure, and body temperature of the older adult in real-time and immediately issue an alarm when an abnormality is detected. Similarly, smart home systems can identify potential health risks by monitoring the daily activities of the older adult, such as getting up, eating, and going out. Second, the data collection process of IoT devices is usually automated, reducing the reliance on the active participation of the older adult and ensuring the continuity and integrity of the data. In addition, the data collected by IoT devices can be combined with other data sources (such as electronic medical records, medication records, etc.) to achieve more comprehensive health behavior prediction (4, 7). However, health monitoring systems based on IoT also face some challenges. For example, how to effectively process and analyze a large amount of heterogeneous data is a key issue. Different types of IoT devices may generate data in different formats. The fusion and analysis of these data require powerful data processing capabilities and advanced algorithm support. In addition, data privacy and security are also issues that cannot be ignored. How to achieve data sharing and analysis while ensuring data security and user privacy is one of the important directions of current research.
2.3 Prediction of health behavior in smart older adult care
Smart older adult care is a new older adult care model that combines information technology, artificial intelligence, and older adult care services. Its core goal is to improve the quality of life and safety of the older adult through technical means. In the framework of smart older adult care, health behavior prediction plays a vital role. Through real-time analysis and prediction of daily behavior data of the older adult, the smart older adult care system can provide personalized health management services for the older adult, reduce health risks, and improve the quality of life. Health behavior prediction in smart older adult care covers multiple fields, including fall prediction, chronic disease management, emotional state monitoring, etc. (15, 16). For example, falls are a common and serious health problem for the older adult. Using machine learning and deep learning technologies, researchers have developed a variety of fall detection and prediction systems. These systems can identify the risk of falls in advance by analyzing the gait, posture, and movement patterns of the older adult, and issue alarms to reduce the incidence of accidents. For example, based on data from wearable devices, researchers can analyze the gait of the older adult through convolutional neural networks (CNN) and long short-term memory networks (LSTM) models to predict potential fall risks (17, 18).
In addition, chronic disease management is also an important application area in smart older adult care. By monitoring the daily activities and physiological data of the older adult, the smart older adult care system can promptly identify early signs of chronic disease onset and provide personalized intervention measures. For example, using IoT devices and big data analysis technology, researchers can monitor indicators such as blood sugar levels and heart rate changes of the older adult, and combine historical data to predict risks, thereby helping medical personnel to develop more accurate treatment plans. Emotional state monitoring is also an emerging direction in smart older adult care in recent years. The mental health of the older adult is also crucial, and fluctuations in emotional state may have a significant impact on their overall health. By analyzing the older adult's voice, facial expressions, and social activity data, the smart older adult care system can assess their emotional state and provide psychological counseling and support when abnormalities are detected. These technical means based on artificial intelligence and data analysis provide more comprehensive and personalized health management services for the older adult (19–21).
In summary, as an important part of smart older adult care, the prediction of the health behavior of the older adult has made significant research progress. Traditional health behavior prediction methods have laid the foundation for research, but they are insufficient in the face of dynamic changes and personalized needs. The health monitoring system based on the Internet of Things provides a real-time and comprehensive means of data collection, but how to effectively process and analyze this data remains a challenge. Health behavior prediction in smart older adult care covers multiple application areas, and through advanced technical means, it provides personalized health management services for the older adult. Future research will further explore the application of multi-source data fusion technology to improve the accuracy and reliability of health behavior prediction, and solve problems such as data privacy and security, to provide a more comprehensive solution for the health management of the older adult.
3 Methodology
3.1 Related theories
In the design and implementation of the smart older adult care platform, the selection and application of theoretical foundations are crucial. To ensure that the platform can effectively meet the needs of the older adult, this study combines theories from multiple fields such as geriatrics, health behavior, Internet of Things technology, big data analysis, and artificial intelligence (22, 23) and applies these theories to the design, data processing, and decision support of the platform.
The older adult population has unique needs in terms of physiological, psychological and social characteristics. Physiologically, the older adult's body functions gradually decline, they are prone to chronic diseases, and their ability to adapt to the external environment decreases. Psychologically, the older adult are prone to loneliness and anxiety, and their emotional needs are more prominent. Socially, the older adult's social circle is relatively small, and they rely on the support system of family and community. Therefore, when designing a smart older adult care platform, these characteristics of the older adult population must be fully considered to ensure that the platform can provide services that meet actual needs. To cope with these characteristics of the older adult population, the platform design is based on the Healthy Aging theory (24). This theory emphasizes delaying the process of health decline and improving the quality of life of the older adult through preventive health management, personalized care, and active social participation. Specifically in the implementation of the platform, the Healthy Aging theory guides us to design functional modules such as real-time health monitoring, psychological care, and social support, to provide comprehensive health management services for the older adult.
Health behavior theory provides theoretical support for the prediction of health behavior of the older adult. Health behavior research shows that health behavior is affected by multiple factors such as personal physiology, psychology, social environment, and behavioral habits. These factors interact with each other and jointly determine the occurrence and change of health behavior. Taking the Theory of Planned Behavior (TPB) (25) as an example, this theory believes that an individual's behavioral intention is influenced by attitudes, subjective norms, and perceived behavioral control, which are the key to behavior change. In the smart older adult care platform, health behavior theory is used to guide the design of behavior prediction models (26, 27). By collecting physiological data, activity data, and psychological state data of the older adult, the platform can comprehensively evaluate the influencing factors of their health behavior and predict possible health risks. The platform uses health behavior theory to integrate these factors into the prediction model, thereby improving the accuracy and effectiveness of the prediction. For example, the platform can predict possible falls or abnormal health events of the older adult based on their behavioral intentions and daily activity patterns, and provide corresponding warnings and intervention suggestions.
The core of the smart older adult care platform lies in the collection and analysis of data, so the IoT and big data theory occupy an important position in the construction of the platform. The Internet of Things theory supports the collection and transmission of health behavior data of the older adult. Through smart devices and sensor networks, the platform can monitor the physiological indicators, behavior patterns, and environmental conditions of the older adult in real time. The data is transmitted to the cloud or edge computing devices through the Internet of Things system for processing, realizing dynamic analysis, and real-time feedback of health data. Big data theory provides a basis for the storage, processing, and analysis of data. The platform's data sources are extensive, including real-time data from smart devices, historical health records, and social and psychological status data. Through big data technology, the platform can effectively process these massive and diverse data and extract high-value health behavior characteristics. At the same time, based on big data analysis theory, the platform can identify complex associations hidden in the data and generate personalized health predictions and management plans.
In addition, the platform also combines expert systems and decision support theories and uses AI algorithms to provide scientific health management suggestions for the older adult and caregivers. By learning the health patterns of the older adult population, the platform automatically generates personalized care plans and provides emotional care and social support. This AI-based decision support system can not only improve the accuracy of health management but also significantly enhance the user experience of the platform.
3.2 Smart older adult care service model
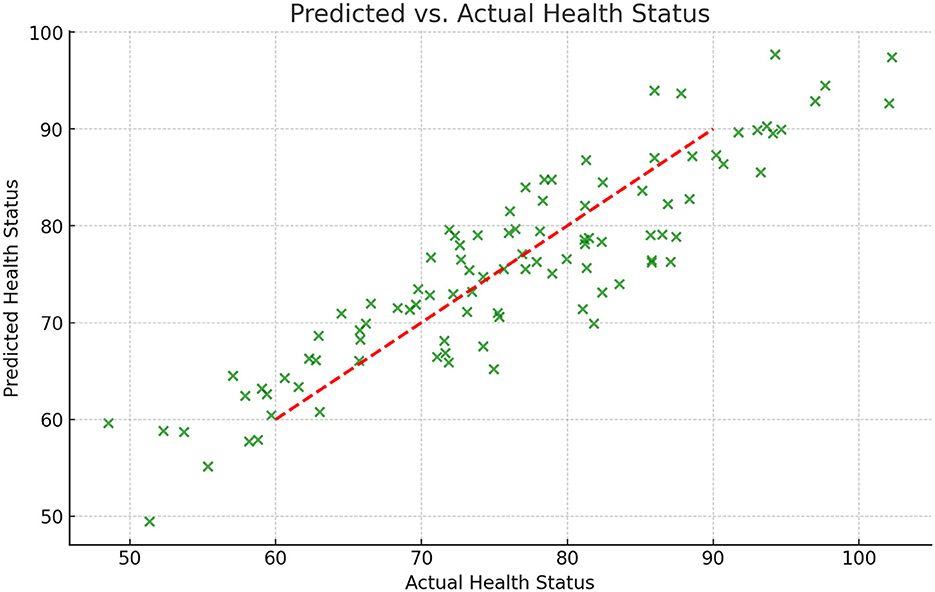
The core of the smart older adult care service model is to achieve all-around support for the older adult population through effective resource allocation, accurate health behavior prediction, and reasonable cost-benefit analysis. To build this model, we combined the theoretical foundations of multiple disciplines and described them through mathematical formulas to ensure that the model is operational in practice and rigorous in theory. The overall framework is shown in Figure 1. The main goal of smart older adult care is to provide comprehensive health management services for the older adult through information technology and intelligent means, including daily health monitoring, emergency warnings, chronic disease management, and quality of life improvement. In this context, our model first starts from the three core perspectives of resource allocation, dynamic changes in health behavior, and cost-benefit analysis to ensure that the system can effectively respond to the diverse needs of the older adult population.
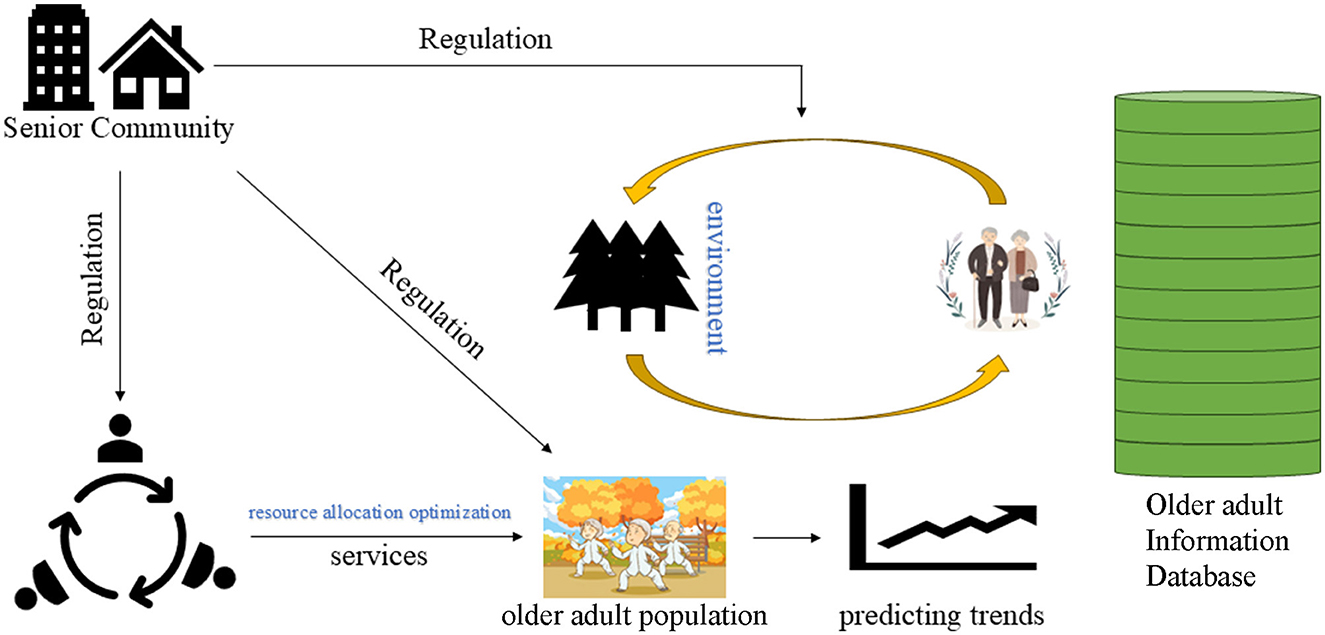
Figure 1. The overall framework structure of our model for predicting health behavior among the older adult.
3.2.1 Resource allocation and optimization
In smart older adult care services, the optimal allocation of resources is the key to maximizing the effect of health management. Resource allocation issues usually involve multiple participants, such as the government, social capital, medical institutions, and older adult families. When resources are limited, how to allocate resources to maximize health benefits is the primary issue in model design. Assume that the allocation of resources Ri follows the following utility function:
among them, ai and bi are utility coefficients, θi and δi are utility indices. This utility function reflects the phenomenon of diminishing marginal returns of resource allocation, that is, as resource input increases, the increase in utility gradually decreases. When resource allocation reaches a certain level, the effect of continuing to increase resource input will become insignificant. This feature is particularly important in smart older adult care, because resources (such as funds, medical equipment, nursing staff, etc.) are usually limited, so they need to be reasonably allocated to maximize the overall benefit. In practical applications, the solution of the utility function can be achieved through optimization algorithms such as the Lagrange multiplier method. By solving the maximum value of the utility function, the system can determine the optimal resource allocation strategy for each participant. This strategy can be dynamically adjusted according to variables such as the health status, social support, and environmental factors of the older adult to ensure the effective use of resources.
3.2.2 Dynamic changes in health behaviors
The health status of the older adult is not only closely related to resource input but also affected by their daily behavior, psychological state, social support, and external environment. To model these complex factors, we introduced the dynamic change equation of health behavior. Assume that the change of the health status H(t) of the older adult over time t can be described by the following differential equation:
in this equation, S(t) represents the intensity of social support, P(t) represents the psychological state, E(t) represents the influence of environmental factors, and C(t) represents the cost of health behavior. Parameters α1, α2, α3 represent the positive effects of different factors on health status, and β represents the negative effect of cost on health status. This equation can be numerically solved to obtain the trajectory of changes in the health status of the older adult. This model is particularly suitable for predicting the evolution of long-term health behaviors, such as the cumulative impact of long-term exercise and healthy diet on the health status of the older adult. Through this model, the smart older adult care service platform can provide personalized health management advice for the older adult and take intervention measures at the early stage of health deterioration.
3.2.3 Interactions between environmental factors and health status
To further characterize the complex relationship between the health behavior of the older adult and the external environment, we introduce external environmental factors into the dynamic change equation of health behavior. Assuming that the health state of the older adult H(t) is affected by the external environment E(t), this can be described by the following equation:
where, Rh(t) represents the resources obtained by the older adult, and κ is the inhibition coefficient of the environment on health status. The equation shows that as the environment deteriorates (such as air pollution, noise pollution climate change, etc.), the improvement of the health status of the older adult will be inhibited. This means that in harsh environments, more resources are needed to maintain the health status of the older adult. To alleviate this impact, the smart older adult care service platform can combine environmental monitoring data to dynamically adjust the health management strategy of the older adult population. For example, during periods of severe air pollution, the platform can advise the older adult to reduce outdoor activities and provide them with appropriate indoor exercise plans. At the same time, the platform can also monitor environmental data in real-time through smart devices and automatically adjust resource allocation according to environmental changes.
3.2.4 Dynamic resource allocation and health management
In the process of providing health management services, the smart older adult care platform needs to dynamically adjust the resource allocation strategy according to the changes in the health status of the older adult. Assume that resource allocation follows the following rules:
among them, λ is the total amount of resources, and γ represents the sensitivity coefficient of health status. The equation shows that when the health status of the older adult is poor [that is, H(t) is low], resource allocation will increase significantly to improve the health status; when the health status is good, the increase in resource allocation will tend to be flat. This dynamic adjustment mechanism enables smart older adult care services to provide the most appropriate resource support in different periods and avoid the problem of resource waste or insufficient allocation. In addition, we also consider the impact of social capital on the health behavior cost of the older adult. Assuming that the participation of social capital indirectly affects the health status of the older adult by affecting the health behavior cost C(t), we can describe this process through the following equation:
among them, C0 is the initial health behavior cost, Sc(t) is the support of social capital for the health behavior of the older adult, Rm(t) is the resource input of social capital, δ and η represent the impact factor and resource sensitivity coefficient of social capital, respectively. This formula shows that with the increase of social capital support and investment, the health behavior cost of the older adult will decrease accordingly, thereby promoting the improvement of health status.
3.2.5 Cost-benefit analysis and optimization
In smart older adult care services, cost-benefit analysis is the key to achieving rational resource allocation. Assume that the total benefit E(T) of smart older adult care services can be decomposed into the weighted sum of health benefits, social benefits, and economic benefits:
At the same time, the total cost of the system B(T) can be decomposed into the weighted sum of direct cost, operating cost, and maintenance cost:
Therefore, the cost-benefit ratio (CBR) can be expressed as:
By analyzing the cost-benefit ratio in different scenarios, the platform can dynamically adjust the resource allocation strategy to maximize benefits. For example, when resources are sufficient, the platform can prioritize health benefits; when resources are tight, the system can be kept running efficiently by optimizing operation and maintenance costs.
Through the above platform, we can comprehensively model resource allocation, health status evolution, and the role of social capital in the smart older adult care service model. Each formula represents the adjustment mechanism of the platform to deal with different scenarios during actual operation. Through these mathematical models, the platform can achieve dynamic management and personalized services for the older adult population, thereby effectively improving the efficiency and effectiveness of health management. These models can be further extended to complex scenarios. For example, in a multi-player game model, different stakeholders (such as the government, social capital, and older adult families) may choose different strategies based on their respective goals. In this case, the allocation of resources and the sharing of costs can be coordinated through a multi-objective optimization model to find a balance between the interests of multiple parties. In addition, these models can be calibrated with real-time data, allowing the smart older adult care platform to adaptively adjust parameters to meet the health management needs of the older adult in different periods and under different environmental conditions. For example, during periods of climate change or infectious disease epidemics, the platform can increase resource allocation and adjust the parameters of health behavior prediction models in real-time, thereby reducing health risks among the older adult population.
4 Experiment
4.1 Difficulties in predicting health behaviors of the older adult
In the process of building a smart older adult care service platform, the prediction of the health behavior of the older adult is a key link. However, due to the particularity of the older adult population and the complexity of their health conditions, health behavior prediction faces many challenges and difficulties (28–30). The following are several major difficulties.
4.1.1 Data diversity and heterogeneity
The health behaviors of the older adult are affected by many factors, including physiological, psychological, social, and environmental factors. To accurately predict health behaviors, the platform needs to integrate multi-source data, such as physiological data from wearable devices, activity data from smart home devices, medical records, mental health assessments, and data from environmental sensors. These data not only come from diverse sources, but also have different formats, frequencies, and accuracies, and are highly heterogeneous. How to effectively integrate these diverse data and eliminate noise and redundant information is a major challenge in prediction.
4.1.2 Complexity and individual differences in health status
The health status of the older adult is often complex and highly individual. Even in similar age groups, there may be significant differences in physical function, medical history, lifestyle, and coping mechanisms. In addition, as they age, the decline of physical function and the onset of diseases in the older adult are often irregular and unpredictable. Health behavior prediction models need to be able to capture these complexities and differences to accurately predict individual health behaviors. However, traditional prediction methods are often based on group statistical models, which make it difficult to accurately model individuals.
4.1.3 Long-term dependency and data loss issues
Predicting the health behavior of the older adult requires modeling and analysis based on long-term historical data. However, in practical applications, it is not easy to obtain long-term data. On the one hand, the health status of the older adult may be unstable or the improper use of technical equipment, resulting in discontinuous data records; on the other hand, the older adult may have incomplete data collection due to cognitive decline or low technology acceptance. In addition, the data of the older adult group may also be affected by multiple factors such as socioeconomic status, cultural background, and living environment, further increasing the complexity and missing problems of the data.
4.1.4 The suddenness and nonlinearity of behavioral changes
The health behavior and health status of the older adult may change suddenly, such as sudden falls, acute illness attacks, or sharp fluctuations in emotional states. This suddenness and nonlinearity make prediction more difficult. Traditional prediction methods usually rely on the stationary and linear assumptions of data, but they are often powerless in the face of the highly nonlinear and unpredictable health behavior of the older adult. Therefore, the prediction model needs to have strong flexibility and robustness to cope with these sudden changes.
4.1.5 Data privacy and ethical issues
older adult health data usually involves sensitive personal information, such as health status, behavioral habits, emotional state, etc. How to protect the privacy and data security of the older adult during data collection, storage, and analysis is an important ethical issue. In addition, in data-driven prediction models, how to ensure the fairness of the algorithm and avoid discrimination or wrong decisions caused by data bias is also a challenge that needs to be solved urgently. To cope with the above difficulties, this study comprehensively considered multi-source data fusion, personalized modeling, data missing processing, nonlinear prediction methods, and privacy protection mechanisms in the experimental design to build a model that can accurately and real-time predict the health behavior of the older adult. Next, the specific design of the experiment, the data processing process and the implementation of the model will be described in detail.
4.2 Implementation details
4.2.1 Dynamic data collection
The proposed older adult health behavior prediction platform integrates real-time data collection using IoT devices, such as wearable health monitors, smart home sensors, and environmental sensors. These devices continuously capture dynamic health indicators (e.g., heart rate, blood pressure, movement patterns) and environmental factors (e.g., temperature, humidity, air quality). The data is transmitted in real-time to a central server via secure wireless communication protocols. This dynamic data collection enables the system to continuously monitor changes in health status, capturing both gradual trends and sudden fluctuations, thus supporting timely intervention.
4.2.2 Feedback mechanisms
The platform incorporates an adaptive feedback mechanism on multiple levels: user feedback, family and caregiver alerts, and healthcare provider notifications. When a potential health risk is detected, the system immediately alerts relevant stakeholders via mobile apps, SMS, or emails. For the older adult user, personalized feedback is delivered through a user-friendly interface, including daily health reports, reminders for medication or physical activity, and warnings about potential health risks. Caregivers and healthcare providers receive summaries of abnormal patterns, along with recommended interventions based on historical data and current health status. This continuous feedback loop ensures that all stakeholders are informed in real-time, enabling proactive management of the older adult's health.
4.2.3 Control algorithms
The platform employs advanced control algorithms that dynamically adjust health recommendations and alerts based on the individual's ongoing health status and historical data. These control algorithms are built using rule-based systems combined with predictive models to ensure responsiveness and adaptability. For example, if a significant drop in activity levels is detected alongside a rise in heart rate, the control algorithm will flag this combination as a potential health risk and escalate the level of alerts. Moreover, the system periodically retrains these algorithms using new data to improve accuracy and relevance, adapting to the changing needs and conditions of the older adult individual. By incorporating both automated adjustments and clinician-configurable thresholds, the control algorithms provide a balance between user customization and system-driven optimization.
4.2.4 Revised evaluation strategy
To effectively assess the platform's real-world applicability and effectiveness, the evaluation process includes extensive testing under real-life conditions. Continuous data from various older adult users is analyzed to assess the accuracy of health predictions, the timeliness of feedback, and the relevance of control adjustments. Additionally, stakeholder feedback is gathered regularly to refine the feedback mechanisms and control algorithms further. This real-world testing provides essential insights into the platform's adaptability, scalability, and reliability, ensuring it can meet the demands of dynamic and complex older adult care environments.
4.3 Model design and experimental results analysis
To address various challenges in predicting the health behavior of the older adult and verify the effectiveness of our proposed method, this study designed and implemented a complete health behavior prediction service model for the older adult. The model aims to address challenges such as data diversity and heterogeneity, complexity and individual differences in health status, long-term dependence, and data loss, sudden and nonlinear behavior changes, and data privacy and ethical issues.
4.3.1 Design of service model for the older adult
4.3.1.1 Data collection
Considering the diversity and heterogeneity of data, the model first collects multi-source data in real-time through IoT devices (such as wearable devices, smart home sensors, etc.). These data include physiological parameters of the older adult (such as heart rate, blood pressure, body temperature, etc.), daily activities (such as steps, sleep patterns, etc.), psychological states (such as emotions, stress levels, etc.), environmental information (such as air quality, temperature and humidity, etc.), and medical records (such as medical history, medication information, etc.). To solve the problem of data heterogeneity, we use multimodal data fusion technology to standardize and fuse data from different sources to form a unified feature representation. Specifically, we use a fusion network based on the attention mechanism to extract key health behavior features by weighting and merging the importance of different data sources.
4.3.1.2 Data missing processing and robustness enhancement module
To address the long-term dependency and data missing issues, we integrated data interpolation and robustness enhancement algorithms into the model. For short-term data missing, we used an interpolation method based on Gaussian processes to infer missing values and complete the data. For long-term data missing, we used a self-supervised learning framework to improve the model's robustness to missing data by constructing comparative learning tasks, ensuring that prediction accuracy is not affected by data missing.
4.3.1.3 Privacy protection and security module
Considering data privacy and ethical issues, the model is designed with special attention to data security and privacy protection. We use federated learning technology to train data on local devices, avoid uploading data to the cloud, and reduce the risk of privacy leakage. In addition, through the differential privacy mechanism, we ensure that during the data analysis and model training process, even if the data is maliciously accessed, no specific personal information can be obtained.
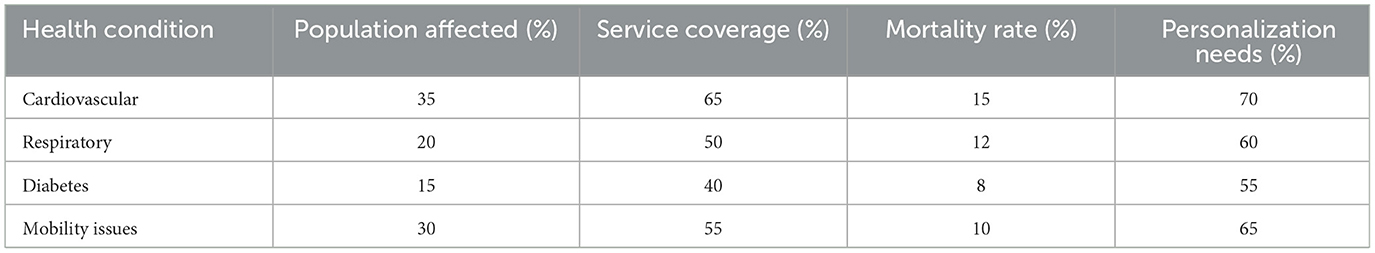
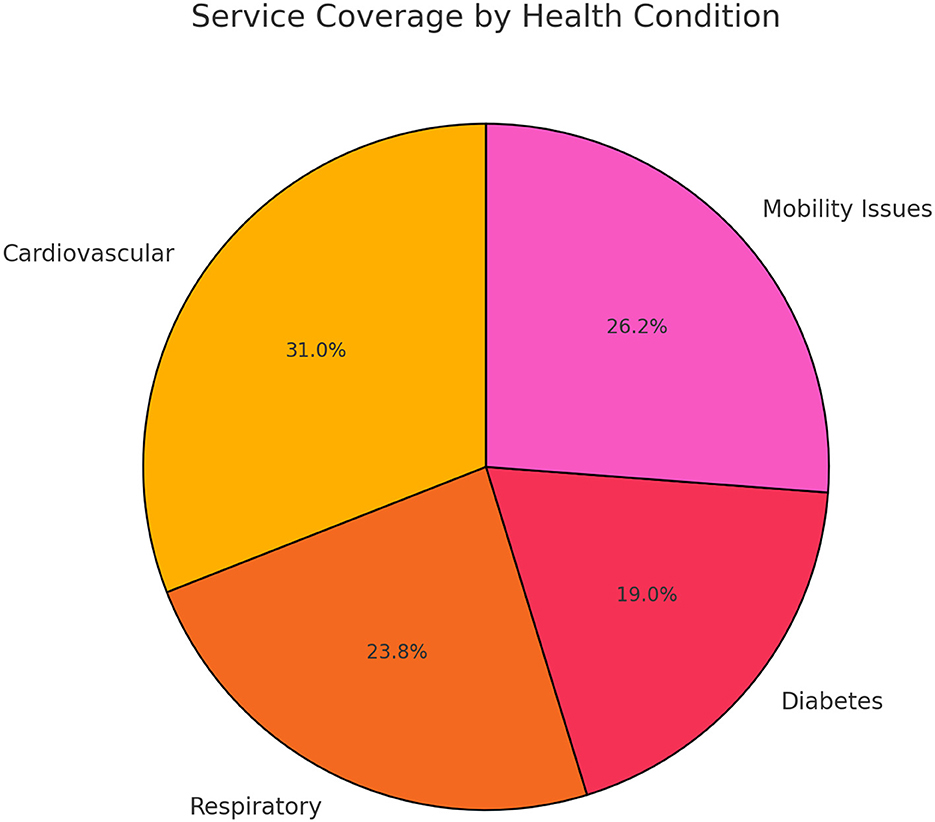
4.3.1.4 Market research analysis and data-driven decision-making
Before model design, this study conducted detailed market research to understand the gap between current market demand and existing smart older adult care services and guided the model design in a data-driven manner. By analyzing market research data, model functions can be optimized to ensure that they meet user needs. Table 1 summarizes the importance of different functions in market research and the comparison of their availability in the current market. As shown in Table 1, real-time monitoring and prediction accuracy are the functions that users care about most, but there is still much room for improvement in their availability in the market.
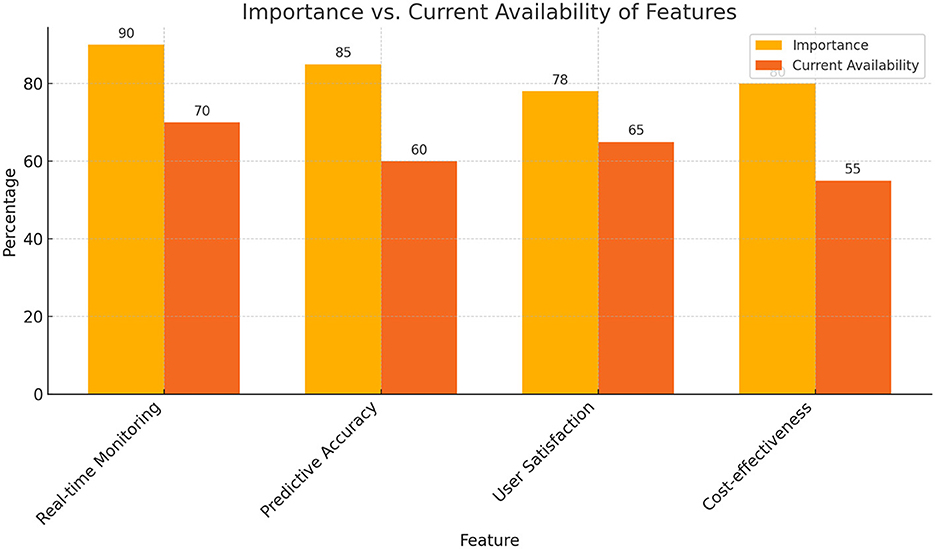
According to the survey results, the model was designed with priority given to improving the coverage and practical application effects of these functions. In addition, the service coverage of different health conditions was analyzed, as shown in Table 2, indicating that the current service coverage still needs to be improved in high-risk health conditions such as cardiovascular disease.
The results of these market surveys helped us clarify the key goals in the current model design and optimize resource allocation and service design through a data-driven approach.
4.3.2 Experimental results and analysis
The experimental results show that the proposed health behavior prediction model performs well in multiple dimensions. With the support of data fusion and missing data processing, the model demonstrates efficient prediction capabilities in a multimodal data environment. At the same time, through the nonlinear prediction and emergency detection modules, the model performs well in dealing with sudden changes in health status. Figure 1 shows the comparison between the importance of functions in market research and the current availability, reflecting the functional gaps in the current market. As shown in Figure 2, although real-time monitoring and prediction accuracy are of high importance, their availability in the current market is not ideal, indicating that there is a lot of room for improvement.
In the analysis of health status service coverage, as shown in Figure 3, there are significant differences in service coverage under different health statuses. Especially in high-risk groups such as cardiovascular disease, the service coverage still needs to be further improved to meet actual needs.
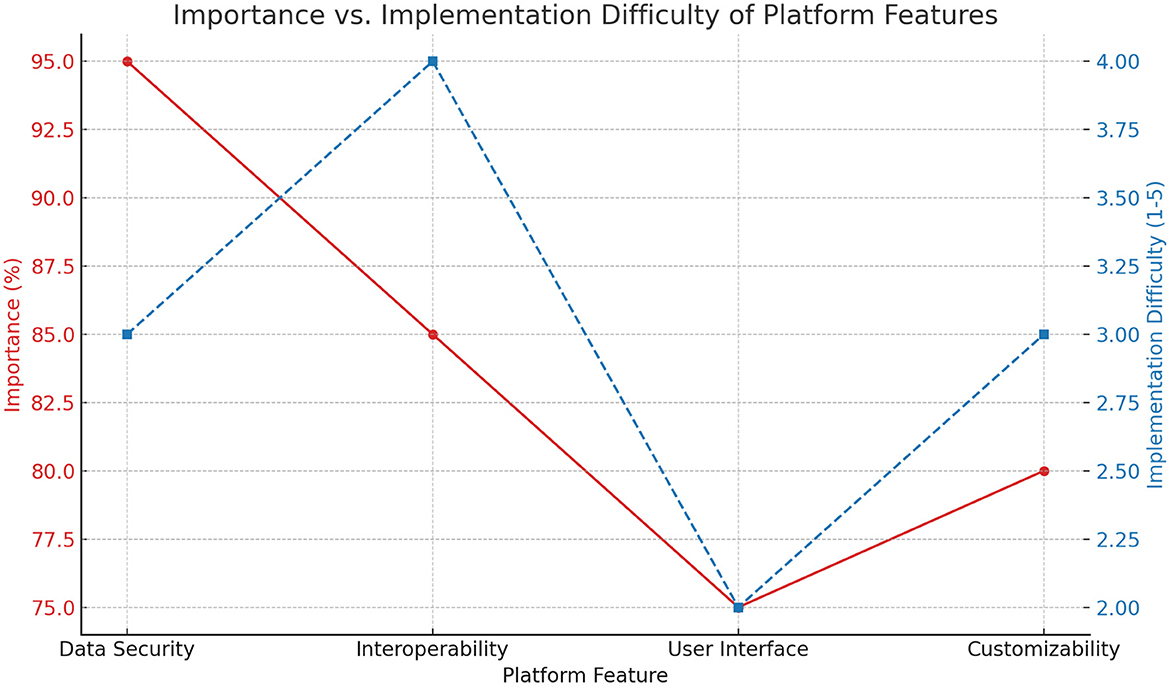
In addition, the line graph of the importance and implementation difficulty of platform functions (as shown in Figure 4) reveals the trade-off between the importance and implementation difficulty of different functions during system design. Figure 4 shows that data security and interoperability are of high importance, but are also relatively difficult to implement, reminding us that we need to focus on overcoming these technical difficulties during the design process.
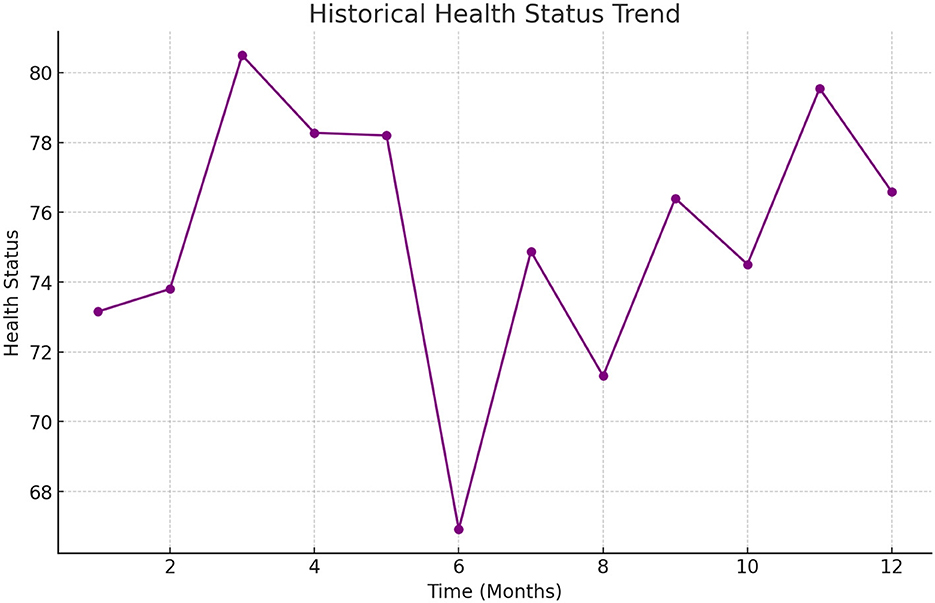
The health prediction results in the experiment were further verified by visual analysis. Figure 5 shows a scatter plot of the health status predicted by the model and the actual health status. The red dotted line in Figure 5 represents the situation where the prediction under the ideal state is consistent with the actual value. The results show that most of the prediction points are close to the dotted line, indicating that the model performs well in prediction accuracy.
Finally, Figure 6 shows the historical trend of changes in the health status of an older adult person during the experiment. Through the time series analysis of health status, it can be found that the model can capture the changing trend of health status promptly and make predictions and adjustments at key nodes to ensure that the older adult receive timely health interventions.
4.3.3 Extended experiment
To comprehensively evaluate its applicability and accuracy in different older adult populations, we designed multiple environments to test the health status of different older adult populations.
(1) Urban vs. rural environment
Experimental design: sample selection: 500 older adult people in urban and rural areas were selected. Data collection: Collect data on their lifestyle, medical records, environmental pollution exposure, etc. Test items: Cardiovascular health, respiratory system function, mental health status.
Experimental results: urban older adult: the incidence of cardiovascular disease is higher, which may be related to high-pressure life and air pollution. Rural older adult: fewer respiratory diseases, but more musculoskeletal problems, which may be related to physical labor.
(2) High-income vs. low-income older adult population
Experimental design: sample selection: according to income level, 500 high-income and low-income older adult people were selected. Data collection: income, access to medical care, eating habits, exercise frequency. Test items: prevalence of chronic diseases, nutritional status, mental health.
Experimental results: high-income group: better control of chronic diseases and better mental health. Low-income group: higher incidence of chronic diseases such as hypertension and diabetes, more common symptoms of depression and anxiety.
(3) Active lifestyle vs. sedentary lifestyle
Experimental design: Sample selection: 500 active and 500 sedentary older adult people were selected based on their daily activity levels. Data collection: exercise habits, physical function test results, cognitive function test. Test items: cardiopulmonary function, muscle strength, cognitive ability.
Experimental results: active older adult people: better cardiopulmonary function and muscle strength, better cognitive ability. Sedentary older adult people: more prone to cardiovascular problems and cognitive decline.
(4) Different dietary patterns
Experimental design: sample selection: According to dietary habits, the subjects were divided into balanced diet, high-fat and high-sugar diet, and vegetarian groups, with 300 older adult people in each group. Data collection: Diet records, body mass index, blood sugar and cholesterol levels. Test items: Metabolic health indicators, cardiovascular risk assessment.
Experimental results: balanced diet group: Normal weight and metabolic indicators, low cardiovascular risk. High-fat and high-sugar group: High obesity rate, high blood sugar and cholesterol levels, increased cardiovascular risk.
(5) Social activity
Experimental design: sample selection: According to the frequency of social activities, the older adult were divided into three groups: high, medium and low, with 400 older adult people in each group. Data collection: Social activity records, mental health assessment, cognitive function test. Test items: Depression and anxiety assessment, memory and attention test.
Experimental results: high social activity: Good mental health and good cognitive function. Low social activity: More obvious symptoms of depression and anxiety, and increased risk of cognitive decline.
(6) Environmental pollution exposure
Experimental design: sample selection: 500 older adult people living in high-pollution and low-pollution areas were selected. Data collection: Environmental pollution indicators, respiratory health data, long-term disease records. Test items: Lung function test, respiratory disease screening.
Experimental results: high-pollution areas: The incidence of respiratory diseases increased significantly and lung function decreased. Low-pollution areas: The respiratory health status is better.
5 Conclusion
In view of the multiple challenges in predicting the health behavior of the older adult, this study proposed and implemented a smart older adult care service model. The model integrates multiple advanced technologies such as multimodal data fusion, nonlinear prediction, data missing processing, emergency detection and privacy protection to form a health management platform for the older adult with high robustness and accuracy. Through market research and analysis, we clarified the key functional requirements of current smart older adult care services and verified the superior performance of the model in practical applications through experiments. The experimental results show that the model not only significantly improves the accuracy of health behavior prediction for the older adult, but also enhances the robustness and security of the system through effective data fusion and processing mechanisms. In addition, the model performs well in coping with sudden changes in health status and providing personalized services.
In future research, the model will continue to be optimized to expand its application scope and data set coverage, especially for the older adult groups in different regions and cultural backgrounds. Further integration of artificial intelligence and deep learning technologies can improve the adaptability and intelligence level of the system. At the same time, with the increasing demand for smart older adult care services, the model needs to be optimized in terms of large-scale deployment and real-time response to meet a wider range of market needs. In summary, this study provides important technical support for the development of smart older adult care services and lays a solid foundation for future research in related fields.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
QG: Data curation, Methodology, Writing – original draft. PC: Software, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The research was supported by the Youth Project of Social Science Foundation of Anhui Province under grant No. AHSKQ2022D069.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ma B, Yang J, Wong FKY, Wong AKC, Ma T, Meng J, et al. Artificial intelligence in elderly healthcare: a scoping review. Ageing Res Rev. (2023) 83:101808. doi: 10.1016/j.arr.2022.101808
2. Frishammar J. Essén A, Bergström F, Ekman T. Digital health platforms for the elderly? Key adoption and usage barriers and ways to address them. Technol Forecast Soc Change. (2023) 189:122319. doi: 10.1016/j.techfore.2023.122319
3. Ernst ME, Broder JC, Wolfe R, Woods RL, Nelson MR, Ryan J, et al. Health characteristics and aspirin use in participants at the baseline of the ASPirin in reducing events in the elderly—eXTension (ASPREE-XT) observational study. Contemp Clin Trials. (2023) 130:107231. doi: 10.1016/j.cct.2023.107231
4. Kulurkar P, kumar Dixit C, Bharathi V, Monikavishnuvarthini A, Dhakne A, Preethi P. AI based elderly fall prediction system using wearable sensors: a smart home-care technology with IOT. Meas Sens. (2023) 25:100614. doi: 10.1016/j.measen.2022.100614
5. Wang K, Cao S, Kaur J, Ghafurian M, Butt ZA, Morita P. Heart rate prediction with contactless active assisted living technology: a smart home approach for older adults. Front Artif Intell. (2024) 6:1342427. doi: 10.3389/frai.2023.1342427
6. Addae S, Kim J, Smith A, Kang M, Rajana P. Smart solutions for detecting, predicting, monitoring, and managing dementia in the elderly: a survey. IEEE Access. (2024) 12:3421966. doi: 10.1109/ACCESS.2024.3421966
7. Hosseinzadeh M, Koohpayehzadeh J, Ghafour MY, Ahmed AM, Asghari P, Souri A, et al. An elderly health monitoring system based on biological and behavioral indicators in internet of things. J Amb Intell Human Comp. (2023) 14, 5085–5095. doi: 10.1007/s12652-020-02579-7
8. Faul JD, Kim JK, Levine ME, Thyagarajan B, Weir DR, Crimmins EM. Epigenetic-based age acceleration in a representative sample of older Americans: associations with aging-related morbidity and mortality. Proc Nat Acad Sci USA. (2023) 120:e2215840120. doi: 10.1073/pnas.2215840120
9. Younis NM, Ibrahim RM, Ahmed MM. Health problems related to quality of life among aging in Iraq. J Curr Med Res Opin. (2024) 7:3015–24. doi: 10.52845/CMRO/2024/7-6-35
10. Ibrahim FM, Fadila DE, Elmawla DAEA. Older adults' acceptance of the COVID-19 vaccine: application of the health belief model. Nursing Open. (2023) 10:6989–7002. doi: 10.1002/nop2.1954
11. Li T, Pang G, Bai X, Zheng J, Zhou L, Ning X. Learning adversarial semantic embeddings for zero-shot recognition in open worlds. Pattern Recognit. (2024) 149:110258. doi: 10.1016/j.patcog.2024.110258
12. Facchinetti G, Petrucci G, Albanesi B, De Marinis MG, Piredda M. Can smart home technologies help older adults manage their chronic condition? A systematic literature review. Int J Environ Res Public Health. (2023) 20:1205. doi: 10.3390/ijerph20021205
13. Sorwar G, Aggar C, Penman O, Seton C, Ward A. Factors that predict the acceptance and adoption of smart home technology by seniors in Australia: a structural equation model with longitudinal data. Inf Health Soc Care. (2023) 48:80–94. doi: 10.1080/17538157.2022.2069028
14. He Z, Dieciuc M, Carr D, Chakraborty S, Singh A, Fowe IE, et al. New opportunities for the early detection and treatment of cognitive decline: adherence challenges and the promise of smart and person-centered technologies. BMC Digital Health. (2023) 1:7. doi: 10.1186/s44247-023-00008-1
15. Yu S, Chai Y, Samtani S, Liu H, Chen H. Motion sensor-based fall prevention for senior care: a Hidden Markov Model with generative adversarial network approach. Inf Syst Res. (2024) 35:1–15. doi: 10.1287/isre.2023.1203
16. Bargiotas I, Wang D, Mantilla J, Quijoux F, Moreau A, Vidal C, et al. Preventing falls: the use of machine learning for the prediction of future falls in individuals without history of fall. J Neurol. (2023) 270:618–31. doi: 10.1007/s00415-022-11251-3
17. Ran H, Li W, Li L, Tian S, Ning X, Tiwari P. Learning optimal inter-class margin adaptively for few-shot class-incremental learning via neural collapse-based meta-learning. Inf Process Manag. (2024) 61:103664. doi: 10.1016/j.ipm.2024.103664
18. Hao M, Zhang Z, Li L, Dong K, Cheng L, Tiwari P, et al. Coarse to fine-based image–point cloud fusion network for 3D object detection. Inf Fus. (2024) 112:102551. doi: 10.1016/j.inffus.2024.102551
19. Oyebode O, Fowles J, Steeves D, Orji R. Machine learning techniques in adaptive and personalized systems for health and wellness. Int J Hum Comput Interact. (2023) 39:1938–62. doi: 10.1080/10447318.2022.2089085
20. Calbimonte JP, Aidonopoulos O, Dubosson F, Pocklington B, Kebets I, Legris PM, et al. Decentralized semantic provision of personal health streams. J Web Semant. (2023) 76:100774. doi: 10.1016/j.websem.2023.100774
21. Illert AL, Stenzinger A, Bitzer M, Horak P, Gaidzik VI, Möller Y, et al. The German Network for Personalized Medicine to enhance patient care and translational research. Nat Med. (2023) 29:1298–301. doi: 10.1038/s41591-023-02354-z
22. Lin KP Li HY, Chen JH, Lu FP, Wen CJ, Chou YC, et al. Prediction of adverse health outcomes using an electronic frailty index among nonfrail and prefrail community elders. BMC Geriatr. (2023) 23:474. doi: 10.1186/s12877-023-04160-1
23. Das A, Dhillon P. Application of machine learning in measurement of ageing and geriatric diseases: a systematic review. BMC Geriatr. (2023) 23:841. doi: 10.1186/s12877-023-04477-x
24. Peel NM, McClure RJ, Bartlett HP. Behavioral determinants of healthy aging. Am J Prev Med. (2005) 28:298–304. doi: 10.1016/j.amepre.2004.12.002
25. Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. (1991) 50:179–211. doi: 10.1016/0749-5978(91)90020-T
26. Glanz K, Rimer BK, Viswanath K. Health Behavior: Theory, Research, and Practice. John Wiley & Sons (2015). Available at: https://books.google.nl/books?hl=zh-CN&lr=&id=PhUWCgAAQBAJ&oi=fnd&pg=PR11&dq=+Health+Behavior:+Theory,+Research,+and+Practice&ots=-foQcQFaID&sig=oZ-jQyqCAwaQ_zlp25BOSTEhJ8c&redir_esc=y#v=onepage&q=Health%20Behavior%3A%20Theory%2C%20Research%2C%20and%20Practice&f=false
27. Painter JE, Borba CP, Hynes M, Mays D, Glanz K. The use of theory in health behavior research from 2000 to 2005: a systematic review. Ann Behav Med. (2008) 35:358–62. doi: 10.1007/s12160-008-9042-y
28. Lima-Costa MF, Cesar CC, Chor D, Proietti FA. Self-rated health compared with objectively measured health status as a tool for mortality risk screening in older adults: 10-year follow-up of the Bambuí Cohort Study of Aging. Am J Epidemiol. (2012) 175:228–35. doi: 10.1093/aje/kwr290
29. Bertini F, Bergami G, Montesi D, Veronese G, Marchesini G, Pandolfi P. Predicting frailty condition in elderly using multidimensional socioclinical databases. Proc. IEEE. (2018) 106:723–37. doi: 10.1109/JPROC.2018.2791463
Keywords: smart older adult care, health behavior prediction, data privacy, aging, medical data analysis
Citation: Guo Q and Chen P (2024) Construction and optimization of health behavior prediction model for the older adult in smart older adult care. Front. Public Health 12:1486930. doi: 10.3389/fpubh.2024.1486930
Received: 29 August 2024; Accepted: 22 November 2024;
Published: 18 December 2024.
Edited by:
Kofi Sarpong Adu-Manu, University of Ghana, GhanaCopyright © 2024 Guo and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qian Guo, Z3VvcWlhbjU1MjcmI3gwMDA0MDthaG51LmVkdS5jbg==
 Qian Guo
Qian Guo Peiyuan Chen2
Peiyuan Chen2