- 1School of Elderly Care Services and Management, Nanjing University of Chinese Medicine, Nanjing, China
- 2Nossal Institute for Global Health, School of Population and Global Health, The University of Melbourne, Melbourne, VIC, Australia
- 3Chinese Hospital Development Institute, Shanghai Jiaotong University School of Medicine, Shanghai, China
Objective: Frailty represents a significant health challenge among older adults, necessitating effective interventions to enhance their overall wellbeing. This study aims to investigate the impact of various types of activity participation on frailty in older adults and to elucidate their intrinsic associations, thereby providing a basis for targeted interventions.
Methods: This study constructed a classification of activities based on the framework proposed by the WHO regarding functional ability in healthy aging, innovatively dividing activities into five categories: physical activity, social activity, economic activity, information activity and sleep activity. Utilizing data from the China Health and Retirement Longitudinal Study (CHARLS 2020), the research employed multiple linear regression and mediation analysis to explore the effects of these activities on the frailty status of older adults and their underlying mechanisms. Furthermore, propensity score matching was conducted to robustly test the regression results.
Results: The study found that physical activity (β = −0.006, p < 0.01), social activity (β = −0.007, p < 0.01), economic activity (β = −0.017, p < 0.01), information activity (β = −0.040, p < 0.01) and sleep activity (β = −0.044, p < 0.01) all had significant positive effects on the frailty status of older adults. Additionally, sleep activity mediated the relationship between physical activity and frailty status, accounting for 4.819%. Social activity mediated the relationship between information activity and frailty status, accounting for 7.692%.
Conclusion: Older adults should enhance their participation in various activities to alleviate frailty. This can be further improved through the following three aspects: engaging in moderate physical exercise, fostering and promoting awareness of volunteer services, and popularizing the use of information technology.
1 Introduction
With the intensification of the aging population process, frailty among the older adults is becoming an increasingly prominent health challenge. Frailty is a common and complex geriatric condition, often defined as a decrease in physiological reserve and reduced resistance to stressors caused by cumulative declines in multiple physiological systems (1–3). Frailty is considered to be a dynamic process that worsens with age (4), leading to adverse consequences for the physical and mental health of older adults. During the period of frailty, the probability of older adults developing other diseases is 12%−24%, with a incidence rate as high as 46% to 49% in the early stage of frailty (5). Besides, frailty is closely associated with adverse health outcomes such as cognitive impairment (6), disabilities (7), hospitalization (8), and death (9). Fortunately, frailty is a reversible process, and early identification of risk factors as well as proactive interventions can delay the progression of older adults from pre-frailty to frailty (10). Among these factors, participation in activities stands out as a particularly significant influence on frailty in older adults (11–13). Activity theory posits that older adults with higher levels of activity tend to exhibit greater life satisfaction (14) and stronger social adaptation compared to those with lower activity levels. This positive effect can be attributed to the supportive roles provided by engagement in activities (14), which help older adults maintain a positive self-concept, prevent brain degeneration, reduce dysfunction, enhance positive emotions, and improve quality of life. Additionally, these activities bolster the ability to cope with environmental changes and organic frailty (14–16). Existing research indicates that, even after controlling for demographic variables, engagement in activities significantly elevates the overall health status of older individuals and mitigate the onset of frailty (17–19). However, the impact of different types of activities on frailty in older adults may vary (18). Therefore, it is essential to further delineate the types of activities and investigate the specific effects and underlying mechanisms of these activities on frailty in older adults.
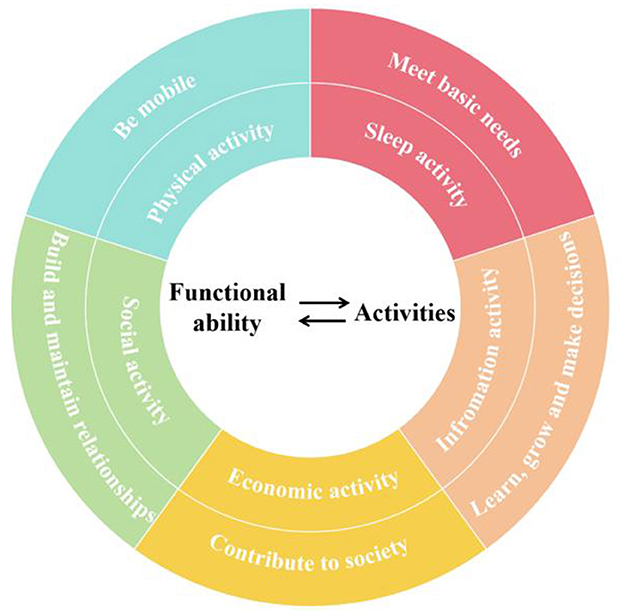
The World Health Organization (WHO) states that healthy aging is the process of developing and maintaining the functional ability that enables wellbeing in older individuals. Functional ability encompasses a person's capacity to move independently, build and maintain relationships, contribute to society, make decisions, learn and grow, as well as meet their basic needs (20). Older individuals demonstrate their functional ability through activity participation, which in turn affects their health status (21). Based on the WHO's framework for functional ability in older individuals, we categorize their activities into five types: physical activities, social activities, economic activities, information activities and sleep activities, as illustrated in Figure 1.
Physical activity refers to activities that require energy expenditure, muscle movement, and physical labor. It is commonly classified into three categories: vigorous physical activities (VPA), moderate physical activities (MPA), and low-intensity physical activities (LPA) (22). Physical activity can mitigate and delay several adverse health outcomes associated with frailty in older individuals, such as cognitive impairment, muscle loss, and depression (23). Consequently, it is considered one of the most effective methods for improving the quality of life and functional abilities in older individuals (24), and it may even serve as a predictor of frailty (25). Higher levels of moderate-to-vigorous physical activity (MVPA) are effective in improving frailty (26), reducing its incidence (27), preventing mobility disorders in frail older individuals (28), and counteracting the negative effects of sedentary behavior (29). However, despite the positive impacts of physical activity on the health of older individuals, it also increases the risk of falls and fractures due to decreased bone mineral density associated with aging (30). Therefore, Kwok et al. encouraged retirees to engage in physical activities following health activity guidelines to minimize these risks (31).
Social activity refers to various communication and interaction behaviors in social life that older adults participate in, involving visiting or socializing with friends, playing mahjong and chess, etc. After retirement, older adults are freed from the constraints of work schedules and social activities, providing them more leisure time. In this new stage of life, they can meet their needs for fulfillment through active social engagement, facilitating a smooth transition from work to retirement (10). Social activities are capable of promoting older adults to establish social networks, receive emotional support and recognition, enhance self-efficacy and enhance stress resistance, thereby reducing the risk of illness as well as improving quality of life (32). Conversely, insufficient engagement in social activities may lead to feelings of loneliness and social isolation among older adults, increasing their risk of frailty. Existing researches have indicated that living in socially active neighborhood is related to lower levels of frailty, highlighting the crucial role of enhancing social activity participation in frailty prevention (33). Most researchers suggested that social activities may impact the frailty status of older adults and researches primarily focused on impacts of different categories of activities (34). Some existing researches indicate that engaging in group games, joining sports clubs and participating in voluntary work can effectively reduce the risk of frailty among older adults. However, some basic social interactions, such as interacting with friends and joining community organizations, have not been proved to have a positive impact on alleviating frailty in older adults (35). Takatori et al. suggested that social factors have no significant improvement effect on frailty in older adults, but social activities based on the promotion of exercise could improve the status of older adults before frailty (36).
Economic activity means various behaviors undertaken by older adults for surviving and developing. Engaging in economic activities may lead to two distinctly different living conditions for older individuals, thereby affecting their physiological and psychological status in different ways. Academic researches on work and frailty in older adults has yielded mixed findings. Research by Jung et al. in the field of productive activities (including volunteer service, paid work, and childcare) showed that after controlling for age, disability, and cognition, work was irrelevant with the likelihood of accumulating frailty (37). However, another research showed that both shift work and low payment have negative effects on the frailty status of older adults. The disruption of circadian rhythms caused by shift work can exacerbate frailty in older adults (38). Retirement may have a protective effect on the health of the older adults who are engaged in low-paid work because of their negative social psychology, which in turn increases their frailty (39). A longitudinal study in the UK supported the aforementioned views, indicating that leaving paid employment before reaching retirement age is beneficial for slowing the progression of frailty in men, and continuing to work does not provide long-term health benefits (40). Furthermore, another study classified work frequency into light, moderate, and vigorous, analyzing their impacts on frail older adults. The results showed that moderate work significantly decreased the pre-frailty rate in older adults (41). What's more, work can also be categorized into intellectual and physical work, both of which have been shown to have positive effects on frailty in older adults (18).
Information activity means utilizing information and communication technologies by older adults. The choice of whether or not to use the internet can reflect the degree of social adaptation and attitude toward societal changes among older adults, which can further influence their living conditions and mindset. The rapid development of information and communication technology (ICT) provides opportunities for users to connect with society, and has become an important mean to help older adults improve frailty status. The use of ICT by older adults can facilitate connections with family members, potentially improving their psychological wellbeing. The lifting effect may be more pronounced in frail older adults (42). Meanwhile, A cross-sectional study indicated a negative correlation between frailty and the use of ICT, with non-use of ICT being a predictor of frailty, and concluded that older women who did not use ICT were more likely to be frail (43).
Sleep activity pertains to the sleeping behavior of older adults. Research on the impact of sleep activity on frailty in older adults can be divided into two categories: sleep quality and sleep duration. Older adults with poor sleep quality are at a higher risk of physical frailty (44). Specifically, sleep-related insomnia can lead to decreased physical performance in older adults (45), resulting in a 66% higher likelihood of frailty compared to peers (46). Additionally, after controlling for covariates such as demographic information, lifestyle, and health-related conditions, poor sleep quality is highly associated with the probability of cognitive frailty (47). Existing studies of sleep duration on frailty in older adults have shown a non-significant association between short sleep duration and risk of frailty (48), with only excessive sleep duration being significantly associated with a high risk of cognitive frailty (49). This may be attributable to the U-shaped relationship observed between sleep duration and all-cause mortality, wherein the lowest risk is associated with a sleep duration of 5.8 h from sleep onset (50).
Different types of activities may interact with each other, thereby influencing frailty in older adults. Regular physical activity promotes relaxation and energy consumption (51), and has been proposed as an effective non-pharmacological treatment option to improve sleep in older adults (52). Existing studies have shown that physical activity is associated with sleep quality in older adults (53), with those engaging in higher levels of physical activity exhibiting better sleep quality (54) and regularity (55). Regular moderate-intensity physical activity in older adults significantly improves sleep outcomes such as sleep quality, sleep disorders, and sleep duration (56). Improved sleep conditions may further slow down the progression of frailty in older adults. Therefore, it is hypothesized that sleep activity may have a mediating effect between physical activity and frailty in older adults. The emergence of ICT has created new possibilities for older people to stay socially connected (57). The use of ICT by older adults can enhance communication efficiency and frequency with family members and friends, facilitating closer connections between them (58). Furthermore, ICT can help older adults overcome spatial limitations, enabling them to connect with strangers online and even develop offline relationships, thereby expanding their social circles (59). Given that participation in social activities, both online and offline may influence frailty in older adults, it is hypothesized that social activity may mediate the relationship between information activity and frailty in older individuals.
All in all, academic researches on the effects of different activity types on frailty in older adults remain inconclusive. There might be variations in the effects of different activity types on frailty among older adults, and may exist correlations between different types of activities that subsequently influence frailty. However, current academic researches on the impact of various activities on frailty primarily focuses on the effects of single or limited categories of activities (18, 60), which has resulted in a fragmented body of studies. There is a lack of comprehensive and systematic research examining the influence of the main activities that older adults frequently engage in during their daily life on frailty. Therefore, this study constructed a classification of activities based on the framework proposed by the WHO regarding functional ability in healthy aging, innovatively dividing activities into five categories: physical activity, social activity, economic activity, information activity and sleep activity. In addition, this study differs from the majority of previous research that concentrates on the mechanisms of alleviating frailty in older adults by improving physiological and psychological factors (61, 62). The findings will clarify the individual and interactive effects of various activities on frailty, deepening and expanding existing academic researches on this topic. Furthermore, based on the results of this research, the study will further provide practical recommendations for improving frailty in the daily lives of older adults, ultimately enhancing their overall wellbeing. Based on the analysis above, this study proposes the following hypotheses:
H1: Physical activity can effectively mitigate the frailty in older adults, but participation in physical activities of different intensities has varying impacts on frailty.
H2: Social activity can effectively mitigate the frailty in older adults and participation in different social activities also has varying effects on frailty conditions.
H3: Economic activity can effectively mitigate the frailty in older adults.
H4: Information activity can effectively mitigate the frailty in older adults.
H5: Sleep activity can effectively mitigate the frailty in older adults.
H6: Sleep activity mediates the impact of physical activity on frailty in older adults.
H7: Social activity mediates the impact of information activity on frailty in older adults.
2 Methods
2.1 Data and participants
The study utilized the data from the fifth phase (2020) of the China Health and Retirement Longitudinal Survey (CHARLS), which is an ongoing longitudinal cohort study. The aim of CHARLS is to collect a high-quality set of micro data representing Chinese households and individuals aged 45 and above, investigating 150 counties and 450 communities (villages) across 28 provinces (autonomous regions, and municipalities) in China. The CHARLS National Baseline Survey was launched in 2011 and was tracked 2 to 3 years. In order to guarantee the unbiased and representativeness of the survey, CHARLS set a filtering section that can exclude invalid samples. CHARLS also conducted the sample through four phases at the county (district)-village (residential)-household-individual level. CHARLS used the Probability Proportional to Size (PPS) method for sampling at two levels: county (districts)-village (residential). By the completion of the follow-up in 2020, the sample has covered a total of 19,000 respondents from 11,400 households, making it a good-quality dataset that includes individual basic information, family structure, health status, economic conditions, social security, and other aspects. All participants in the study signed informed consent forms, and the protocol has been approved by the Ethics Committee of Peking University.
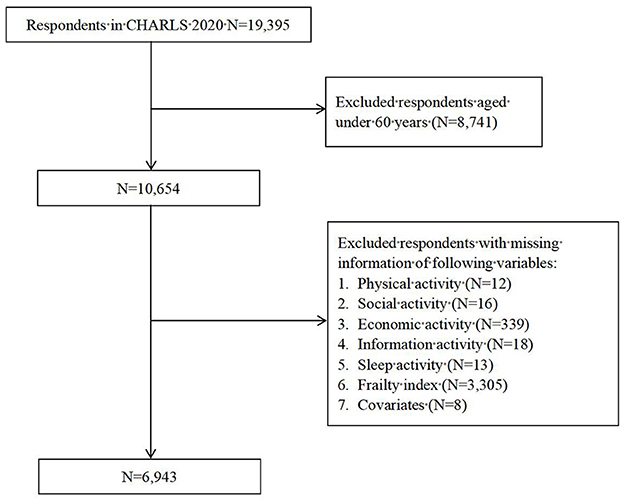
Since the research object was the older adults in this study, 8,741 respondents under the age of 60 were excluded. Among the remaining respondents, 12 were missing information on physical activity, 16 were missing information for social activity, 339 were missing information for economic activity, 18 were missing information for sleep activity, 3,305 were missing information on frailty index and 8 were missing information for covariates. Six thousand nine hundred and forty three respondents were finally included in our research and the sample selection process is depicted in Figure 2.
2.2 Dependent variable
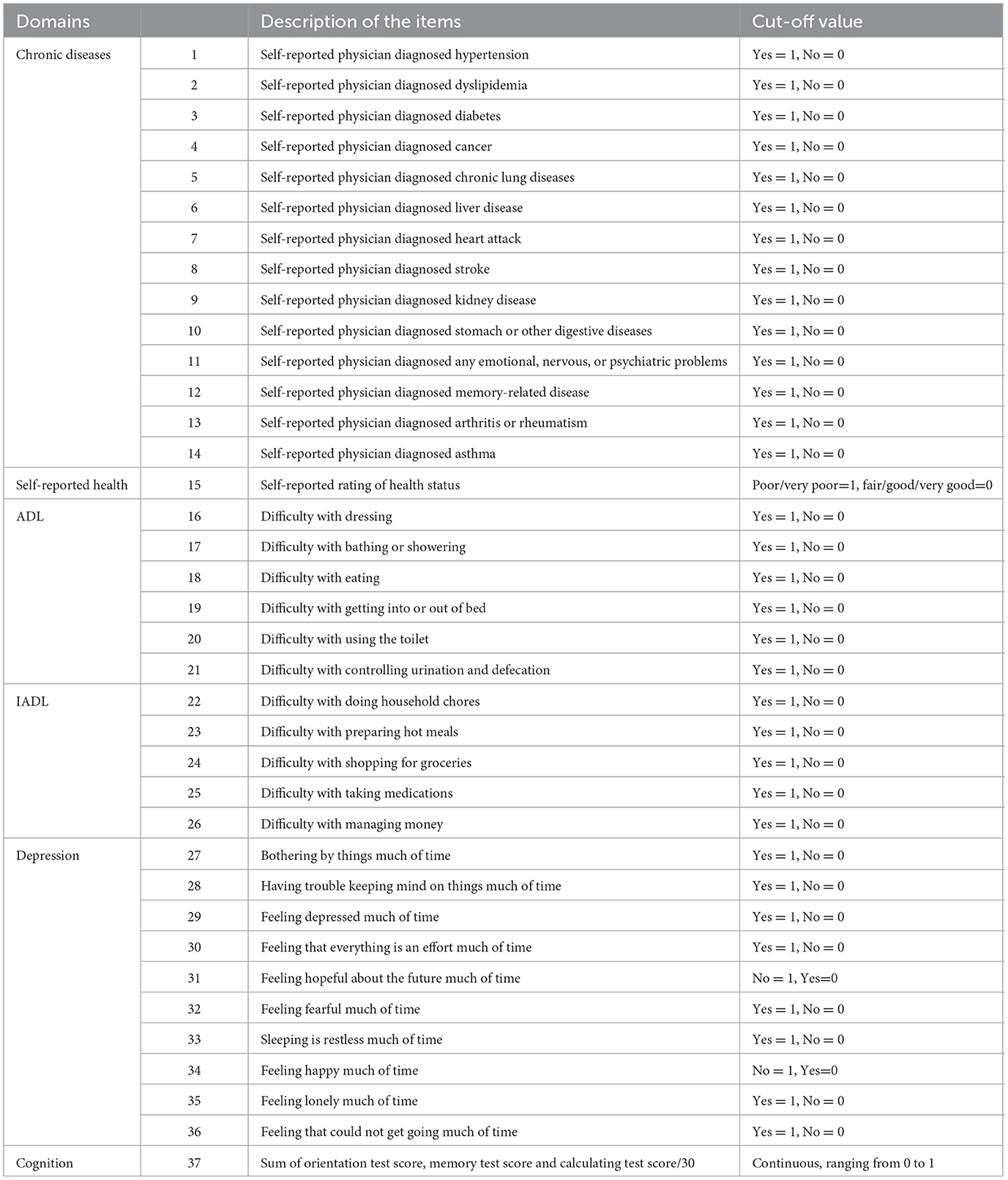
The dependent variable in this study was frailty, which was measured by frailty index (FI). The index was consistent with previous studies (63, 64). It encompassed 8 domains, including chronic diseases, self-reported health, ADL, IADL, depression, and cognitive, comprising a total of 37 indicators, which were derived from self-report and objective measurement of the study participants. The specific items were shown in Table 1. FI was calculated by dividing the sum of scores by the total number of items, with scores ranging from 0 to 1, and a higher score indicated a higher level of frailty among older adults.
2.3 Independent variables
This study selected different types of activities as independent variables, including physical activity, social activity, economic activity, information activity, and sleep activity. For physical activity, the study evaluated its impact on frailty based on varying intensity levels. The research also explored the impact of different types of social activities on frailty. For economic and informational activities, the study measured their impact on frailty based on participation status. Regarding sleep activities, the research evaluated the impact on frailty based on the duration of sleep.
Referring to previous literature (22), physical activity among older adults was categorized into three levels based on intensity: low-intensity physical activity (LPA) such as walking, including walking for work or from one place to another at home, as well as walk for leisure, exercise, or entertainment. Moderate physical activity (MPA), such as carrying light objects, regular-speed cycling, mopping, brisk walking, etc., leading to faster breathing than usual. Vigorous physical activity (VPA) that cause rapid breathing, such as lifting heavy objects, farming, aerobics, fast cycling, etc. Participants were asked to report the intensity, frequency, and duration of their physical activity per week. The frequency ranged from 0 to 7 days per week, and the daily duration of physical activity was divided into five categories, i.e., no physical activity physical activity = 0 min, physical activity <30 min, 30–119 min, 120–239 min, and >240 min. The total of physical activity (TPA) was calculated by multiplying the daily duration of each type of physical activity by its weekly frequency. To further standardize the measurement of physical activity, the study utilized metabolic equivalent value (MET). Based on previous research, 1 MET represents resting oxygen consumption, while VPA corresponds to 8 MET, MPA to 4 MET, and LPA can be expressed as 3.3 MET. Total physical activity (TPA) was calculated by the sum of MET of VPA, MPA and LPA. For statistical convenience, the TPA was divided by 60 to calculate the MET hours per week and presented in the final data form using the LN (TPA+1).
Social activity among older adults included seven categories: (1) visiting or socializing with friends, (2) playing mahjong, chess, cards, or attending community activities, (3) providing unpaid help to non-cohabiting relatives, friends, or neighbors, (4) participating in sports, social, or other types of clubs, (5) participating in community-related organizations, (6) participating in volunteer or charity activities or caring for non-cohabiting patients or disabled persons, (7) attending school or training courses. The study measured the dimension of social activity by calculating the number of social activities older adults participated in. According to previous research, the study further categorized social activity into four types (65): item (1) was categorized as simple interpersonal activities (SIA), items (2) and (7) as intellectual activities (INA), items (3) and (6) as volunteer activities (VOA), and items (4) and (5) as club activities (CLA).
The economic activity of older adults was measured by their participation in work, including farm work, wage labor, business activities, and assisting with family businesses. It was assigned to 1 if engaged in work, and 0 otherwise.
In this study, information activity participation among older adults was measured by their internet usage, which was assigned to 1 if older adults used the internet and 0 otherwise.
Sleep activity status among older adults was measured by their sleep duration. Based on previous research, older adults' sleep duration was categorized into three classes (66): short sleep duration ( ≤ 5 h), moderate sleep duration (5 h ~ 9 h), and long sleep duration (≥9 h), and assigned values of 0, 1, and 2, respectively.
2.4 Mediators
This study included two mediating variables, analyzing the mediating effect of sleep activity between physical activity and frailty status among older adults, and the mediating effect of social activity between information activity and frailty status among older adults.
2.5 Covariates
The control variables selected for this study encompassed gender (0 = female, 1 = male), age (in years), hukou (0 = agricultural, 1 = non-agricultural), education level (0 = low level of education, including elementary school and below; 1 = medium level of education, including middle school graduation to vocational school; 2 = high level of education, including 2-/3-Year College/Associate degree and above) and marital status (0 = married, 1 = separated/divorced/widowed/never married).
2.6 Statistical analysis
Stata18.0 and SPSS26.0 were used for statistical analysis. Descriptive statistics and multiple linear regression analysis were initially conducted using SPSS 26.0. Frequency and standard deviation were used to represent categorical data, while mean and standard deviation were used for continuous data. Further mediation analysis was conducted using SPSS 26.0, employing the SPSS macro developed by Hayes (Model 4). Bias-corrected percentile Bootstrap method was utilized to estimate the 95% confidence interval of the mediating effects, with 5,000 samples extracted after controlling for gender, age, hukou, education level, and marital status. The mediating effect was considered significant if the 95% confidence interval did not include 0 (67). Lastly, the study concluded with a robustness test of the analysis results using propensity score matching (PSM) via Stata 18.0.
3 Results
3.1 Descriptive analysis
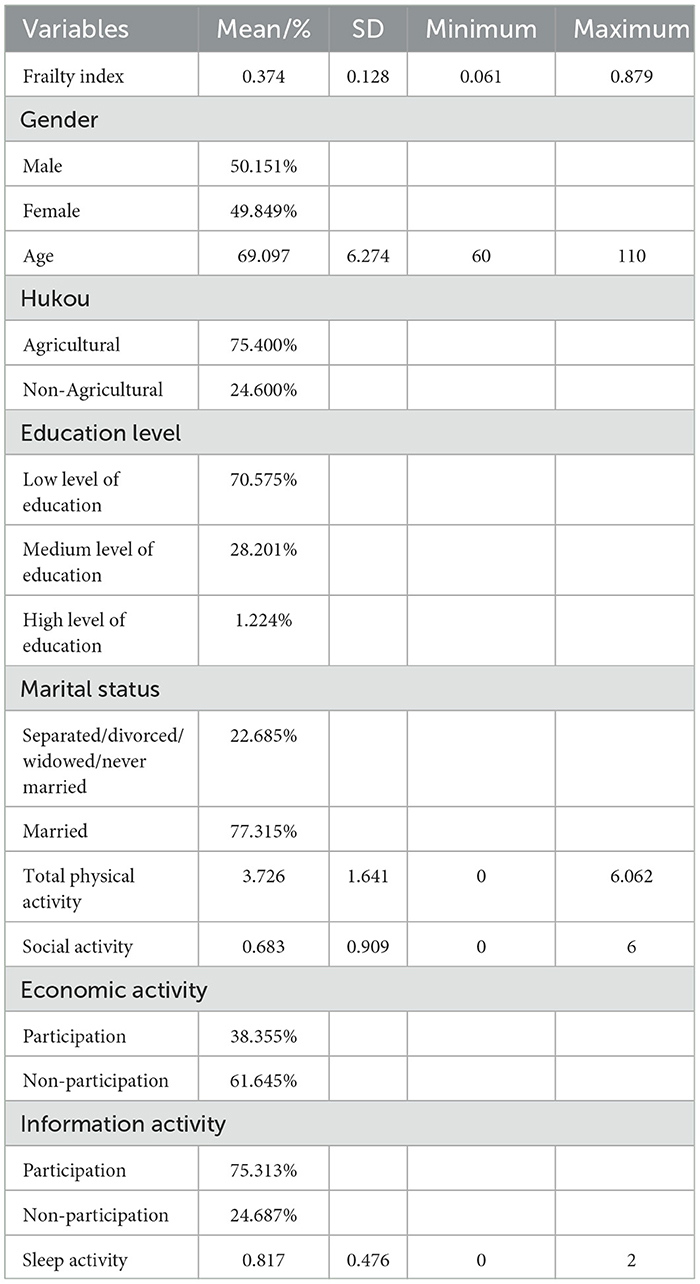
The descriptive results of the data are presented in Table 2. A total of 6,943 older participants were included in the study, with an average age of 69.1 years. Additionally, the gender proportion was balanced, with males and females accounting for 49.8% and 50.2% respectively. Moreover, the education level of the older adults was generally low, with 70.6% having the degree of primary school or below. Furthermore, a high proportion of older adults had agricultural hukou, accounting for 75.4%, and the majority of older adults were in a state of marriage, comprising approximately 77.3% of the total. The average FI of the older adults included in this study was 0.37, indicating that the overall frailty status of older adults was in the lower middle level. There were significant differences in the participation of older adults in different activities. For instance, the average MET for older adults was 3.73, with a standard deviation of 1.64, indicating that the TPA participation among older adults was moderate, but there were considerable individual differences. Moreover, older adults had a low frequency of participation in social activity, with 54.1% not participating in any social activity, 29.4% participating in one social activity, and only 16.5% participating in two or more social activities. What's more, most older adults were still involved in economic activity, accounting for approximately 61.6%. However, the participation in information activity was not ideal, with only 24.7% of older adults reporting the use of the internet in their daily lives. Lastly, the sleep duration of the older participants included in the study was relatively moderate, while 22.1% of older adults had insufficient sleep duration, and 3.85% had excessive sleep duration.
3.2 Effects of different activity types on frailty status of older adults
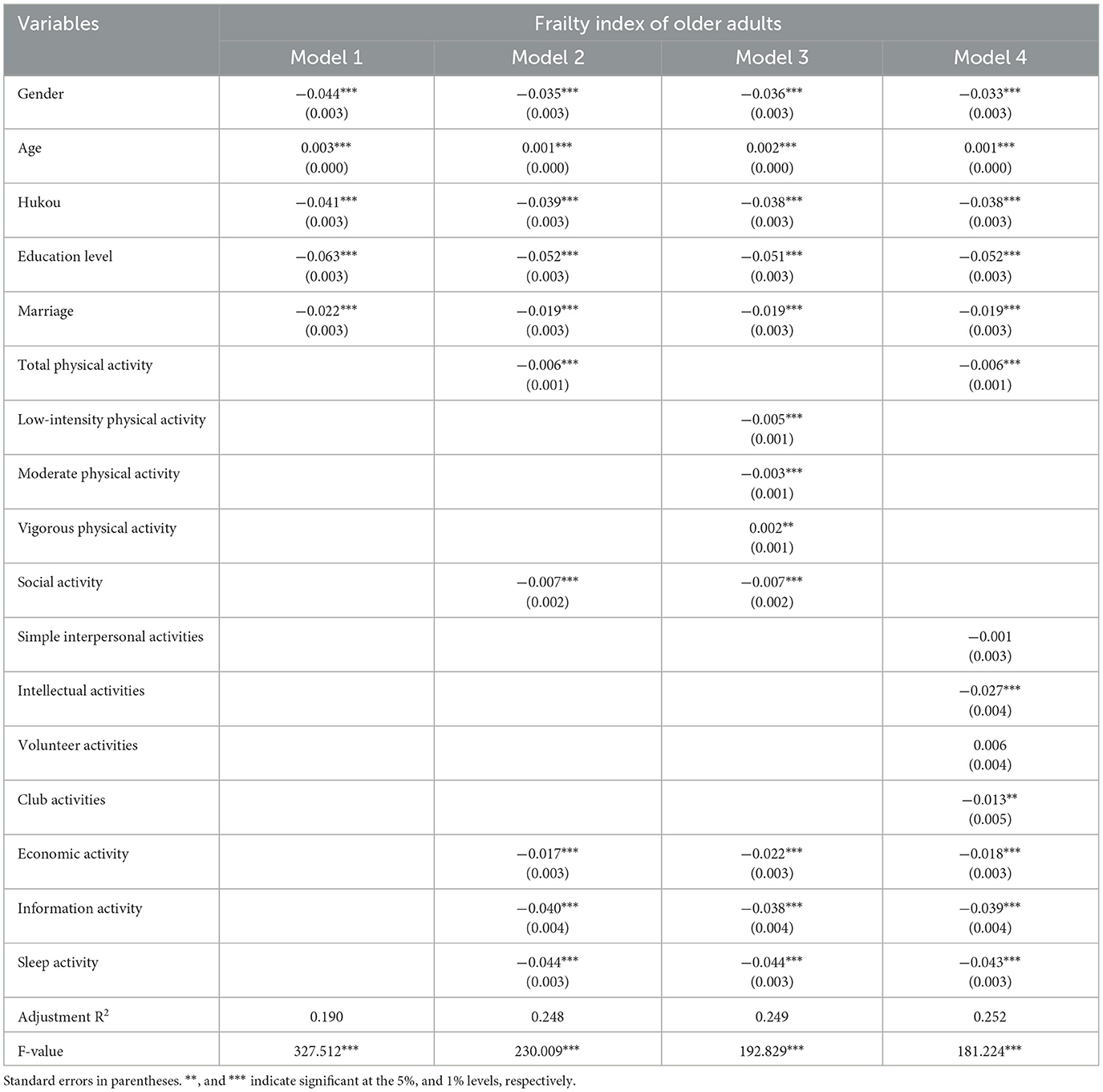
Table 3 presented the effects of different types of activities on the frailty status of older adults. Model 1 included only the control variables, while Model 2 added various activity variables based on Model 1. Model 3 and 4 further analyzed the impacts of different physical activity intensities and types of social activities on frailty in older adults respectively based on the foundation. After controlling for relevant covariates, TPA exhibited a significant negative effect on the frailty status of older adults (β = −0.006, p < 0.01). Further exploration revealed that LPA and MPA significantly predicted lower frailty status among older adults (β = −0.005, p < 0.01; β = −0.003, p < 0.01), whereas engaging in VPA could exacerbate frailty in older adults (β = 0.002, p < 0.05). The statistical results verified hypotheses H1. Overall participation in social activity showed a significant negative impact on the FI of older adults (β = −0.007, p < 0.01). Based on this, the study further investigated the influence of different categories of social activity participation on FI. The results indicated that engaging in INA and CLA significantly contributed to lower FI among older adults (β = −0.027, p < 0.01; β = −0.013, p < 0.05), while participating in SIA and VOA did not affect frailty status. The data analysis results showed that Hypothesis 2 is partially supported. Additionally, the study findings revealed that engaging in economic activity, information activity, and sleep activity all significantly predicted lower frailty status among older adults (β = −0.017, p < 0.01; β = −0.040, p < 0.01; β = −0.044, p < 0.01). These findings validated hypotheses H3, H4, and H5.
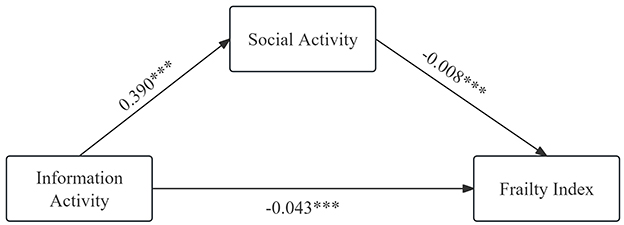
3.3 Mediation analysis
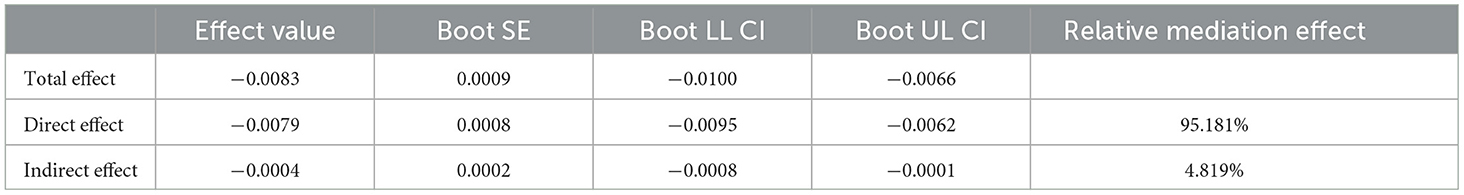
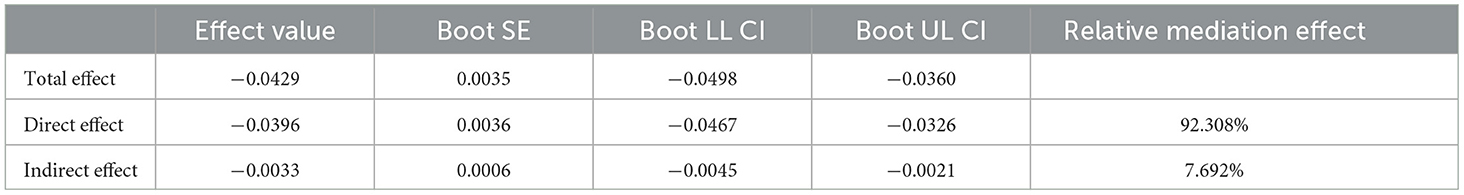
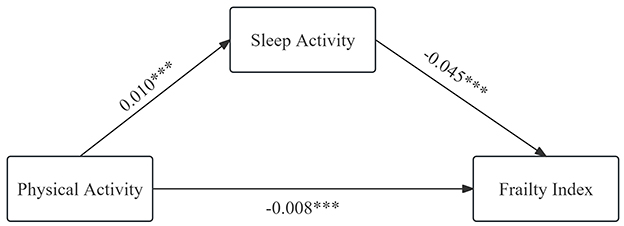
Regression analysis indicated that participation in physical, social, economic, information, and sleep activities all had varying degrees of negative effects on frailty status in older adults. However, previous studies have shown that there were also mutual influences among these activities. Therefore, further exploring the mechanisms of how different types of activities affect frailty status in older adults is of significant importance. In this study, sleep activity and social activity were selected as mediating variables to investigate the influence mechanisms of physical activity and informational activity on frailty status respectively. The results were presented in Tables 4, 5 and Figures 3, 4. Sleep activity was found to partially mediate the relationship between physical activity and the FI in older adults. The direct effect coefficient between physical activity and frailty index was −0.0083, and the mediating effect coefficient of sleep activity was −0.0004. The mediating effect accounted for 4.8% of the total effect. The mediation indicated that physical activity influenced frailty status in older adults by extending their sleep duration. Social activity partially mediated the relationship between information activity and frailty. The coefficient of direct effect between information activity and frailty was −0.0429, and the mediating effect coefficient of social activity was −0.0033. The mediating effect accounted for 7.7% of the total effect. The mediation suggested that information activity alleviated frailty status in older adults by promoting their participation in social activity. The statistical analysis results confirmed H6 and H7.
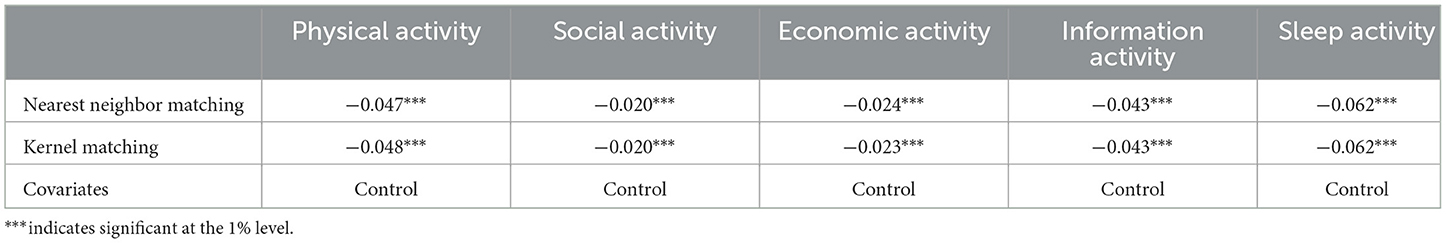
3.4 Robust test
We used two propensity score matching methods, including nearest neighbor matching and kernel matching in this study. The results were presented in Table 6. After controlling gender, age, hukou, education level as well as marital status, the effects of five different types of activities on frailty among older adults were all significant, suggesting that the baseline regression results were robust.
4 Discussion
This study investigated the effects of physical activity, social activity, economic activity, information activity, and sleep activity on frailty in older adults and explored the potential mechanisms underlying these effects. Our findings indicated that all five activity types have significant negative effects on frailty of older adults. Specifically, physical activity can alleviate frailty by extending sleep duration, and information activity can reduce frailty by enhancing social engagement.
Initially, participation in different types of activities had a significant negative impact on frailty in older adults. First of all, the effectiveness of PA interventions in coping with frailty in older adults has been documented (25, 68). PA is defined as all movements in daily life, including occupational, commuting, and leisure activities (69). It is closely associated with maintaining and improving physiological function and physical health, and the impact of different intensity of physical activity on frailty varies. LPA such as walking, climbing stairs, and rising from the floor or chair can improve muscle strength, enhance balance and flexibility, reduce the risk of chronic diseases and musculoskeletal issues, as well as improve cognitive function and mental health in older adults (70). The improvement is closely related to the functional capacity of older adults and can significantly alleviate frailty with aging (71). MPA such as cycling and brisk walking has been shown to be relevant to lower resting blood pressure, improved lipid and lipoprotein profiles, enhanced glucose homeostasis, reduced abdominal fat deposition, as well as extended active life expectancy (72). In addition, MPA can also induce rapid expansion of the mitochondrial compartment in muscle cells, which can alleviate the frailty outcomes caused by years of sedentary habits in older adults (73, 74). However, as intensity increases, PA may not necessarily have a sustained positive impact on older adults, since VPA often increases the risk of injury and sudden death in older adults (72). VPA can also lead to fatigue, respiratory difficulties, restricted mobility, anxiety, etc. (75). As a result, moderate exercise is beneficial for the physical and mental health of older adults.
Secondly, high level of social activity participation can alleviate frailty in older adults. Social activity participation is a broad concept, including involvement in volunteering, recreational activities, interpersonal interactions, etc. (76). Activity theory suggests that social engagement can provide role support for older adults and build social relationships (77), reduce feelings of loneliness (78), as well as encourage older adults to adopt healthy behaviors, thereby improving frailty. The effects of different social activities on frailty various. As individuals age, older adults may experience the loss of friends and partners (78), which may increase their risk of social isolation and loneliness, further leading to frailty (79) and increased risk of early death (80). However, CLA can create a friendly and sociable environment. Participating in these activities can enhance social contact and interaction, enhance their sense of belonging, address their social and psychological needs (81), improve their mental health and cognitive function (82), thus further alleviating frailty. Additionally, cognition decline, as an inevitable result of aging (83), further contributes to frailty in older adults (84). While participating in INA can significantly improve older adults' memory, attention, processing speed, and enhance cognitive reserve. It is an effective intervention to improve older adults' cognitive abilities (85), which can further inhibit the progression of functional decline and reduce the likelihood of disability in older adults (86). Interestingly, this study found that SIA and VOA did not have a significant impact on frailty in older adults. This may because simple interpersonal activities, which only involve visiting or communicating with others, are unlikely to affect the physiological functions and capabilities of older adults, thus having an insignificant impact on frailty conditions. Meanwhile, the volunteering awareness among older adults in China are not enough, leading to lower participation in volunteer work, thus not significantly affecting their frailty.
Thirdly, engaging in economic activity can positively influence the health of older adults. Participating in intellectual economic activities can provide cognitive stimulation, strengthen synaptic transmission (neural plasticity), and increase cognitive reserve, thus positively affecting the maintenance or improvement of cognitive function (87). This positive impact does not diminish with age, as older employees often have experienced more cognitively challenging, allowing for more cognitive exercises. Even older adults who want to take on new tasks after retirement can enhance the function of the prefrontal cortex and further improve the cognitive function through working (88). While engaging in physical economic activities as well as physical activities generated on the way to work, such as walking and cycling, all strengthen mobility and reduce the risk of disability and physical decline in older adults, thereby alleviating frailty status (88).
Fourthly, active engagement in information activity can have beneficial effects on both the physical and mental health of older adults, thereby alleviating frailty. As age increases, the prevalence of neurocognitive disorders (such as mild cognitive impairment or dementia) continues to rise (89). These cognitive impairments often lead to disability and dependence, thus exacerbating the overall frailty condition in older adults (90). However, the Internet, as an increasingly popular information technology, can provide older adults with a new source of positive stimulation. With the deep integration of Internet-based technologies (such as smartphones, wearable devices, etc.) into daily cognitive processing, older adults using the Internet can gradually develop various forms of online cognition in their aging brains and can leverage emerging online functions to achieve cognitive abilities (91). Furthermore, using the Internet can also improve the mental health of older adults. The emergence of the Internet has brought about many new types of online activities, such as playing online games, watching videos, online shopping, social interaction, etc., all of which can help older adults achieve the purpose of entertainment and leisure, thereby improving their negative emotions (92). Additionally, as the Internet provides abundant information, some older adults can regularly search for health-related information to manage their physical and mental health, so as to improving frailty condition (93).
Fifthly, extension of sleep duration can also effectively improve the frailty condition in older adults. In recent years, sleep disorders, as a risk factor for physical frailty in older adults, have gradually attracted widespread attention (94). This is mainly because sleep disorders may over activate the HPA axis, leading to increased secretion of cortisol, thereby accelerating the degradation of muscle protein (95). Sleep disorders may also lead to dysfunction of the hypothalamic-pituitary-gonadal (HPG) axis, reducing the secretion of testosterone, thereby inhibiting the synthesis of muscle protein. These imbalanced processes of degradation and synthesis lead to the deterioration of muscle mass, which in turn leads to the core of physical weakness, namely muscle weakness (96, 97). Other possible mechanisms include chronic inflammation (IL-6, TNF-α, and CRP) (98) and imbalance in growth hormone (GH) secretion (99). According to statistics, the prevalence of sleep disorders in people over 60 years old is 42.3% (100). Sleep is a modifiable lifestyle factor, which can effectively improve the overall health of older adults, reduce frailty risks, and decrease their late-stage consequences through early adoption of effective intervention measures (101).
This study found that the above five categories of activities can indirectly alleviate their frailty status through interaction. The results indicated that sleep activity played a partial mediating role in the influence of PA on frailty in older adults. Previous research has shown that regular PA can improve the sleep quality of older adults (102). This is mainly because regular PA promotes relaxation and energy consumption in older adults, which is conducive to initiating and maintaining sleep (103, 104). However, the frequency and intensity of PA among older adults need special attention. Research has found that a three times per week exercise program predicts beneficial sleep outcomes (105, 106). Specific types of activities such as Ba Duan Jin, Tai Qi, and yoga as well as combinations of different types of exercises are known to positively affect sleep in older adults (107). Improved sleep quality further enhances older adults' cognitive abilities and reduces the risk of dementia (108), alleviating physical and mental health problems, thus positively impacting the overall frailty status of older adults (109).
Moreover, social activities play a mediating role between information activity and frailty in older adults. Putnam defined social capital as “the connections between personal social networks and the norms of reciprocity and trust that arise from them” (110). Further research has divided social capital into psychological/cognitive dimensions and network/structural dimensions (111). Network social capital includes resources obtained through social networks (111) and can be measured through social participation and informatization (112). As an “network” itself, the Internet provides older adults with effective and convenient communication channels (113). In addition to enhancing communication with family and friends, the Internet also assists older adults to establish contact with strangers, conduct in-depth online communication and offline social activities (59). Simultaneously, as a platform carrying a large amount of information, the Internet hosts online and offline organizations classified according to interests and hobbies. Older adults can accumulate social capital, alleviate loneliness and enhance their sense of belonging by joining clubs of interest and participating in activities (114). Furthermore, active social participation also helps further enhance cognitive function, curb the progression of functional decline, and reduce the likelihood of disability, thereby alleviating the overall frailty status.
Above all, we believe that in the future, older adults should seize opportunities to engage in various activities according to their own circumstances. However, it is worth noting that engaging in activities with excessively high intensity may not alleviate the frailty status. The reasons of engaging in VPA in this study were for exercise partly, while others do so out of economic necessity. For older adults exercising for health, it is advisable to reduce the intensity appropriately to enhance individual safety and physical health. For those engaged in physical labor due to economic necessity, the government should enact relevant social security policies such as providing financial assistance to relieve the financial pressure. Currently, the participation of older adults in volunteer services is not satisfactory. Consequently, the communities and related organizations should strengthen advocacy and publicity of volunteer services among older adults (115). Moreover, the proportion of older adults participating in information activities is relatively low. It is necessary to rely on family members and communities to further improve the digital literacy of older adults, promote them to integrate into the information society and empower older adults (116). For rural and remote areas having issues of the digital divide (117), government departments should increase investment in communication infrastructure construction, and mobilize enterprises actively participate in promoting the popularization and application of communication technology.
This study differs from previous single or limited researches by innovatively constructing an activity classification based on the functional capability framework for healthy aging proposed by the WHO. The classification includes five categories: physical activity, social activity, economic activity, information activity, and sleep activity. The research explores the impact of these activities on frailty and further investigates the mediating roles of sleep activity and social activity in the relationship between physical activity, information activity, and frailty. The findings not only provide a detailed overview of how various daily activities affect frailty in older adults but also offer practical pathways for preventing and mitigating frailty in daily life, aligning closely with the current promotion of healthy aging concepts. However, this study has some limitations, including the use of cross-sectional data, which may not capture the dynamic relationship between activity participation and frailty. Future research should explore these relationships longitudinally to verify the temporal effects.
5 Conclusion
Frailty, as a medical syndrome characterized by specific physical symptoms, significantly impacts the wellbeing of older adults and imposed considerable economic and psychological burdens on their caregivers. To explore the effective mechanisms for mitigating frailty in older adults, this study summarized previous research and utilized microdata from the CHARLS 2020, combining it with the functional capability framework for healthy aging proposed by the WHO to construct a classification of different activities. The study empirically investigated the impact of participation in these activities on frailty in older adults. The results indicated that physical, social, economic, information, and sleep activities can effectively alleviate frailty. Additionally, the study examined how physical activity and information activity improved frailty status through their effects on sleep activity and social activity respectively. These findings will enrich the existing research on frailty in older adults and provide new perspectives on improving frailty status. They will enable older adults to identify clear pathways for enhancing their health in daily life and suggest that simple, feasible activity options can significantly improve their health, which holds important practical implications for enhancing the overall wellbeing of older populations.
Data availability statement
Data are available from the China Health and Retirement Longitudinal Study (CHARLS) (http://charls.pku.edu.cn/) for researchers who meet the criteria for access to CHARLS data.
Ethics statement
The studies involving humans were approved by the Institutional Review Board of Peking University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
ZN: Conceptualization, Formal analysis, Investigation, Writing – original draft. XiuZ: Formal analysis, Methodology, Software, Writing – original draft. YS: Formal analysis, Writing – original draft. XiaZ: Writing – review & editing. SX: Conceptualization, Supervision, Validation, Writing – review & editing. XY: Funding acquisition, Project administration, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Higher Education Philosophy and Social Sciences Program of the Jiangsu Provincial Department of Education: A Study on the Diffusion of Policy Innovation in Long-term Care Insurance in Jiangsu Province from the Perspective of Central-local Interaction [grant number 2022SJYB0328]; The Ministry of Education Humanities and Social Sciences Youth Project: A Case Study on the Diffusion of Healthcare Reform Policy Innovation Based on Text Mining Methods [grant number 19YJCZH217]; The Special Research Project of School of Elderly Care Services and Management, Nanjing University of Chinese Medicine under Grant [grant number 2024YLFWYGL018].
Acknowledgments
We thank the China Center for Economic Research, the National School of Development of Peking University for providing the data. Thanks to all the researchers who participated in the writing of the paper. The authors would like to express gratitude to the editors and reviewers of the journal.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Yang L, Xue B, Zheng X, Zhang X, Xiao S, Zhou C, et al. The independent and combined effects of physical activity and depressive symptoms on frailty in community-dwelling older adults: a cross-sectional study. J Clin Nurs. (2024) 2024:17331. doi: 10.1111/jocn.17331
2. Li S, Cui G, Yin Y, Lv F, Yao Y. Association between tea consumption and frailty among Chinese older adults: a cross-sectional study. Front Nutr. (2022) 9:987911. doi: 10.3389/fnut.2022.987911
3. Zhou T, Qu Z, Ge S, Wu X, Zhang X, Wang A, et al. Frailty knowledge level and its influencing factors among older adults in China. Geriatr Nurs. (2023) 50:247–54. doi: 10.1016/j.gerinurse.2023.01.004
4. Bandeen-Roche K, Seplaki CL, Huang J, Buta B, Kalyani RR, Varadhan R, et al. Frailty in older adults: a nationally representative profile in the United States. J Gerontol Series a-Biol Sci Med Sci. (2015) 70:1427–34. doi: 10.1093/gerona/glv133
5. O'Caoimh R, Sezgin D, O'Donovan MR, Molloy DW, Clegg A, Rockwood K, et al. Prevalence of frailty in 62 countries across the world: a systematic review and meta-analysis of population-level studies. Age Ageing. (2021) 50:96–104. doi: 10.1093/ageing/afaa219
6. Zhao XX, Chen Q, Zheng L, Ren LB, Zhai YH Li J, He J. Longitudinal relationship between frailty and cognitive impairment in Chinese older adults: a prospective study. J Appl Gerontol. (2022) 41:2490–8. doi: 10.1177/07334648221118352
7. Liu HX, Ding G, Yu WJ, Liu TF, Yan AY, Chen HY, et al. Association between frailty and incident risk of disability in community-dwelling elder people: evidence from a meta-analysis. Public Health. (2019) 175:90–100. doi: 10.1016/j.puhe.2019.06.010
8. Chang SF, Lin HC, Cheng CL. The relationship of frailty and hospitalization among older people: evidence from ameta-analysis. J Nurs Scholarship. (2018) 50:383–91. doi: 10.1111/jnu.12397
9. Shamliyan T, Talley KMC, Ramakrishnan R, Kane RL. Association of frailty with survival: a systematic literature review. Ageing Res Rev. (2013) 12:719–36. doi: 10.1016/j.arr.2012.03.001
10. Zhao M, Gao J, Li M, Wang KF. Relationship between loneliness and frailty among older adults in nursing homes: the mediating role of activity engagement. J Am Med Dir Assoc. (2019) 20:759–64. doi: 10.1016/j.jamda.2018.11.007
11. Li Y, Xiong M, Zhang Y, Su Y. The current status and influencing factors of frailty among community-dwelling old adults. Chinese J Behav Med Brain Sci. (2019) 28:1020–4.
12. van Assen M, Pallast E, El Fakiri F, Gobbens RJJ. Measuring frailty in Dutch community-dwelling older people: reference values of the Tilburg Frailty Indicator (TFI). Arch Gerontol Geriatr. (2016) 67:120–9. doi: 10.1016/j.archger.2016.07.005
13. Hoogendijk EO, Heymans MW, Deeg DJH, Huisman M. Socioeconomic inequalities in frailty among older adults: results from a 10-year longitudinal study in the Netherlands. Gerontology. (2018) 64:157–64. doi: 10.1159/000481943
14. Longino CF, Kart CS. Explicating activity theory: a formal replication. J Gerontol. (1982) 37:713–22. doi: 10.1093/geronj/37.6.713
15. James BD, Boyle PA, Buchman AS, Bennett DA. Relation of late-life social activity with incident disability among community-dwelling older adults. J Gerontol Series a-Biol Sci Med Sci. (2011) 66:467–73. doi: 10.1093/gerona/glq231
16. Menec VH. The relation between everyday activities and successful aging: a 6-year longitudinal study. J Gerontol Series B-Psychol Sci Soc Sci. (2003) 58:S74–82. doi: 10.1093/geronb/58.2.S74
17. Kamrani AAA, Shams A, Dehkordi PS, Mohajeri R. The effect of low and moderate intensity aerobic exercises on sleep quality in elderly adult males. Pakistan J Med Sci. (2014) 30:417–21. doi: 10.12669/pjms.302.4386
18. Yokote T, Yatsugi H, Chu TS, Liu X, Kishimoto H. Associations between various types of activity and physical frailty in older Japanese: a cross-sectional study. BMC Geriatr. (2023) 23:785. doi: 10.1186/s12877-023-04501-0
19. Ki S, Yun J-H, Lee Y, Won C-W, Kim M, Kim C-O, et al. Development of guidelines on the primary prevention of frailty in community-dwelling older adults. Ann Geriat Med Res. (2021) 25:237–44. doi: 10.4235/agmr.21.0072
20. Organization WH. Healthy ageing and functional ability. (2020). Available at: https://www.who.int/news-room/questions-and-answers/item/healthy-ageing-and-functional-ability (accessed July 30, 2024).
21. Gao M, Sa ZH, Li YY, Zhang WJ, Tian DH, Zhang SF, et al. Does social participation reduce the risk of functional disability among older adults in China? A survival analysis using the 2005-2011 waves of the CLHLS data. BMC Geriatr. (2018) 18:1–13. doi: 10.1186/s12877-018-0903-3
22. Lei XL, Gao K, Wang H, Chen W, Chen GR, Wen X. The role of physical activity on healthcare utilization in China. BMC Public Health. (2023) 23:2378. doi: 10.1186/s12889-023-16625-4
23. Lei XL, Gao K, Wang H, Chen W, Chen GR, Wen X. The role of physical activity on healthcare utilization in China. BMC Public Health. (2023) 23:2378. doi: 10.1186/s12889-023-16625-4
24. Pan B, Li H, Wang Y. Physical activity and the risk of frailty among community-dwelling healthy older adults: A protocol for systematic review and meta-analysis. Medicine. (2019) 98:e16955. doi: 10.1097/MD.0000000000016955
25. Huang TY, Chou MY, Liang CK, Lin YT, Chen RY, Wu PF. Physical activity plays a crucial role in multidomain intervention for frailty prevention. Aging Clin Exp Res. (2023) 35:1283–92. doi: 10.1007/s40520-023-02412-z
26. Chen S, Chen T, Kishimoto H, Yatsugi H, Kumagai S. Associations of objectively measured patterns of sedentary behavior and physical activity with frailty status screened by the frail scale in japanese community-dwelling older adults. J Sports Sci Med. (2020) 19:166–74.
27. Wu SC, Leu SY, Li CY. Incidence of and predictors for chronic disability in activities of daily living among older people in Taiwan. J Am Geriatr Soc. (1999) 47:1082–6. doi: 10.1111/j.1532-5415.1999.tb05231.x
28. Custodero C, Agosti P, Anton SD, Manini TM, Lozupone M, Panza F, et al. Effect of physical activity intervention on gait speed by frailty condition: a randomized clinical trial. J Am Med Dir Assoc. (2023) 24:489–96. doi: 10.1016/j.jamda.2023.01.023
29. Mañas A, Pozo-Cruz BD, Rodríguez-Gómez I, Losa-Reyna J, Rodríguez-Mañas L, García-García FJ, et al. Can physical activity offset the detrimental consequences of sedentary time on frailty? A moderation analysis in 749 older adults measured with accelerometers. J Am Med Dir Assoc. (2019) 20:634–638.e1. doi: 10.1016/j.jamda.2018.12.012
30. van Gameren M, Hoogendijk EO, van Schoor NM, Bossen D, Visser B, Bosmans JE, et al. Physical activity as a risk or protective factor for falls and fall-related fractures in non-frail and frail older adults: a longitudinal study. BMC Geriatr. (2022) 22:695. doi: 10.1186/s12877-022-03383-y
31. Kwok WS, Dolja-Gore X, Khalatbari-Soltani S, Byles J, Oliveira JS, Pinheiro MB, et al. Physical activity and injurious falls in older Australian women: adjusted associations and modification by physical function limitation and frailty in the Australian Longitudinal Study on Women's Health. Age and Ageing. (2023) 52:afad108. doi: 10.1093/ageing/afad108
32. Zhang Z, Zhang JX. Social participation and subjective well-being among retirees in China. Soc Indic Res. (2015) 123:143–60. doi: 10.1007/s11205-014-0728-1
33. Noguchi T, Murata C, Hayashi T, Watanabe R, Saito M, Kojima M, et al. Association between community-level social capital and frailty onset among older adults: a multilevel longitudinal study from the Japan Gerontological Evaluation Study (JAGES). J Epidemiol Commun Health. (2022) 76:182–9. doi: 10.1136/jech-2021-217211
34. Lestari SK, Eriksson M, de Luna X, Malmberg G, Ng N. Frailty and types of social relationships among older adults in 17 European countries: a latent class analysis. Arch Gerontol Geriatr. (2022) 101:104705. doi: 10.1016/j.archger.2022.104705
35. Xie BQ, Ma CN. Effect of social participation on the development of physical frailty: do type, frequency and diversity matter? Maturitas. (2021) 151:48–54. doi: 10.1016/j.maturitas.2021.06.015
36. Takatori K, Matsumoto D. Effects of social activity participation and trust in the community on the transition of frailty classification in late-stage older adults: a 4-year prospective cohort study. BMJ Open. (2023) 13:e072243. doi: 10.1136/bmjopen-2023-072243
37. Jung YY, Gruenewald TL, Seeman TE, Sarkisian CA. Productive activities and development of frailty in older adults. J Gerontol Series B-Psychol Sci Soc Sci. (2010) 65:256–61. doi: 10.1093/geronb/gbp105
38. Khan D, Verschoor C, Edgell H, Rotondi M, Tamim H. The association between shift work exposure and frailty among middle-aged and older adults results from the Canadian longitudinal study on aging. J Occupat Environ Med. (2023) 65:355–61. doi: 10.1097/JOM.0000000000002806
39. Kalousova L, de Leon CM. Increase in frailty of older workers and retirees predicted by negative psychosocial working conditions on the job. Soc Sci Med. (2015) 124:275–83. doi: 10.1016/j.socscimed.2014.11.055
40. Lu WT, Benson R, Glaser K, Platts LG, Corna LM, Worts D, et al. Relationship between employment histories and frailty trajectories in later life: evidence from the English Longitudinal Study of Ageing. J Epidemiol Commun Health. (2017) 71:439–45. doi: 10.1136/jech-2016-207887
41. Morishita-Suzuki K, Nakamura-Uehara M, Ishibashi T. The improvement effect of working through the Silver Human Resources Center on pre-frailty among older people: a two-year follow-up study. BMC Geriatr. (2023) 23:265. doi: 10.1186/s12877-023-03978-z
42. Fang Y, Chau AKC, Wong A, Fung HH, Woo J. Information and communicative technology use enhances psychological well-being of older adults: the roles of age, social connectedness, and frailty status. Aging Ment Health. (2018) 22:1516–24. doi: 10.1080/13607863.2017.1358354
43. Garcia-Vigara A, Cano A, Fernandez-Garrido J, Carbonell-Asins JA, Tarin JJ, Sanchez-Sanchez ML. Non-use of information and communication technology as a predictor of frailty in postmenopausal midlife and older women. Maturitas. (2022) 156:60–4. doi: 10.1016/j.maturitas.2021.05.010
44. Liu XY, Wang CL, Qiao XX Si HX, Jin YR. Sleep quality, depression and frailty among Chinese community-dwelling older adults. Geriatric Nursing. (2021) 42:714–20. doi: 10.1016/j.gerinurse.2021.02.020
45. Tang JYM, Luo H, Tse M, Lum TYS, Wong GHY Li SX. The relationship between insomnia symptoms and frailty in community-dwelling older persons: a path analysis. Sleep Med. (2021) 84:237–43. doi: 10.1016/j.sleep.2021.05.039
46. Aditi, Singh SK, Jaiswal AK, Verma M. Is there a ubiquitous association between sleep disorder and frailty? Findings from LASI (2017-18). BMC Geriatr. (2023) 23:429. doi: 10.1186/s12877-023-04148-x
47. Liu SY, Hu Z, Guo YC, Zhou FX Li SJ, Xu HL. Association of sleep quality and nap duration with cognitive frailty among older adults living in nursing homes. Front Public Health. (2022) 10:963105. doi: 10.3389/fpubh.2022.963105
48. Chen S, Wang Y, Wang Z, Zhang X, Deng C, Ma B, et al. Sleep duration and frailty risk among older adults: evidence from a retrospective, population-based cohort study. J Nutr Health Aging. (2022) 26:383–90. doi: 10.1007/s12603-022-1766-z
49. Chuang SC, Wu IC, Chang JJ, Tsai YF, Cheng CW, Chiu YF, et al. Sleep habits are associated with cognition decline in physically robust, but not in frail participants: a longitudinal observational study. Sci Rep. (2022) 12:11595. doi: 10.1038/s41598-022-15915-y
50. Chen MZ, Lu C, Zha JR. Long sleep duration increases the risk of all-cause mortality among community-dwelling older adults with frailty: evidence from NHANES 2009-2014. J Appl Gerontol. (2023) 42:1078–88. doi: 10.1177/07334648221147917
51. Fank F, Pereira FDS, Dos Santos L, De Mello MT, Mazo GZ. Effects of exercise on sleep in older adults: an overview of systematic reviews and meta-analyses. J Aging Phys Act. (2022) 30:1101–17. doi: 10.1123/japa.2021-0444
52. Vanderlinden J, Biddle GJH, Boen F, van Uffelen JGZ. Are reallocations between sedentary behaviour and physical activity associated with better sleep in adults aged 55+ years? An isotemporal substitution analysis. Int J Environ Res Public Health. (2020) 17:9549. doi: 10.3390/ijerph17249579
53. Christie AD, Seery E, Kent JA. Physical activity, sleep quality, and self-reported fatigue across the adult lifespan. Exp Gerontol. (2016) 77:7–11. doi: 10.1016/j.exger.2016.02.001
54. Sung RM. Comparison of cognitive function and sleep quality in the gender and physical activity of older adults. Korean Soc Sports Sci. (2011) 20:35–45.
55. Corral-Perez J, Casals C, avila-Cabeza-de-Vaca L, Gonzalez-Mariscal A, Mier A, Espinar-Toledo M, et al. Associations between physical activity and inactivity levels on physical function and sleep parameters of older adults with frailty phenotype. J Appl Gerontol. (2024) 43:910–21. doi: 10.1177/07334648231218095
56. Vanderlinden J, Boen F, van Uffelen JGZ. Effects of physical activity programs on sleep outcomes in older adults: a systematic review. Int J Behav Nutr Phys Activity. (2020) 17:1–15. doi: 10.1186/s12966-020-0913-3
57. Nguyen MH, Hunsaker A, Hargittai E. Older adults' online social engagement and social capital: the moderating role of Internet skills. Inform Commun Soc. (2022) 25:942–58. doi: 10.1080/1369118X.2020.1804980
58. Li W, Yue L, Xiao SF. Association between internet use, cognitive function, and globus pallidus volumes: a study among the elderly in Chinese communities. Front Public Health. (2022) 10:886974. doi: 10.3389/fpubh.2022.886974
59. Yuan W, Jiang M, Gong SY. How to improve the cognitive health of middle-aged and elderly people: evidence from China family panel studies. Front Public Health. (2022) 10:799255. doi: 10.3389/fpubh.2022.799255
60. Sagong H, Jang AR, Kim DE, Won CW, Yoon JY. The cross-lagged panel analysis between frailty and physical activity among community-dwelling older adults by age groups. J Aging Health. (2021) 33:387–95. doi: 10.1177/0898264320987365
61. Jeong H, Chang SJ. Association between social frailty and life satisfaction among older adults. Res Gerontol Nurs. (2023) 16:291–300. doi: 10.3928/19404921-20230817-02
62. Chen LY, Fang TJ, Lin YC, Hsieh HF. Exploring the mediating effects of cognitive function, social support, activities of daily living and depression in the relationship between age and frailty among community-dwelling elderly. Int J Environ Res Public Health. (2021) 18:12543. doi: 10.3390/ijerph182312543
63. Li CL, Ma YJ, Yang C, Hua R, Xie WX, Zhang LX. Association of cystatin c kidney function measures with long-term deficit-accumulation frailty trajectories and physical function decline. Jama Network Open. (2022) 5:e2234208. doi: 10.1001/jamanetworkopen.2022.34208
64. Sun BR, Wang JY, Wang YB, Xiao WB, Liu Y, Wang Y, et al. Associations of dynapenic abdominal obesity and frailty progression: evidence from two nationwide cohorts. Nutrients. (2024) 16:518. doi: 10.3390/nu16040518
65. Ding YF, Chen LS, Zhang Z. The relationship between social participation and depressive symptoms among Chinese middle-aged and older adults: a cross-lagged panel analysis. Front Public Health. (2022) 10:996606. doi: 10.3389/fpubh.2022.996606
66. Zhao YL, Lu Y, Zhao WY, Wang YY, Ge ML, Zhou LX, et al. Long sleep duration is associated with cognitive frailty among older community-dwelling adults: results from West China Health and Aging Trend study. BMC Geriatr. (2021) 21:1–8. doi: 10.1186/s12877-021-02455-9
67. Preacher KJ, Rucker DD, Hayes AF. Addressing moderated mediation hypotheses: theory, methods, and prescriptions. Multivariate Behav Res. (2007) 42:185–227. doi: 10.1080/00273170701341316
68. Kaushal N, Langlois F, Desjardins-Crépeau L, Hagger MS, Bherer L. Investigating dose-response effects of multimodal exercise programs on health-related quality of life in older adults. Clin Interv Aging. (2019) 14:209–17. doi: 10.2147/CIA.S187534
69. Hu G, Eriksson J, Barengo NC, Lakka TA, Valle TT, Nissinen A, et al. Occupational, commuting, and leisure-time physical activity in relation to total and cardiovascular mortality among Finnish subjects with type 2 diabetes. Circulation. (2004) 110:666–73. doi: 10.1161/01.CIR.0000138102.23783.94
70. Nagai K, Miyamato T, Okamae A, Tamaki A, Fujioka H, Wada Y, et al. Physical activity combined with resistance training reduces symptoms of frailty in older adults: a randomized controlled trial. Arch Gerontol Geriatr. (2018) 76:41–7. doi: 10.1016/j.archger.2018.02.005
71. Brown M, Sinacore DR, Ehsani AA, Binder EF, Holloszy JO, Kohrt WM. Low-intensity exercise as a modifier of physical frailty in older adults. Arch Phys Med Rehabil. (2000) 81:960–5. doi: 10.1053/apmr.2000.4425
72. Pescatello LS. Physical activity, cardiometabolic health and older adults: recent findings. Sports Med. (1999) 28:315–23. doi: 10.2165/00007256-199928050-00003
73. Chen YC, Lin KC, Chen CJ, Wang CH. Effects of leisure-time physical activity interventions on frailty-related characteristics of frail older adults in long-term care: a systematic review. Contemp Nurse. (2020) 56:34–48. doi: 10.1080/10376178.2020.1737555
74. Lewis CTA, Tabrizian L, Nielsen J, Laitila J, Beck TN, Olsen MS, et al. Physical activity impacts resting skeletal muscle myosin conformation and lowers its ATP consumption. J Gen Physiol. (2023) 155:e202213268. doi: 10.1085/jgp.202213268
75. Skelton DA. When physical activity increases risk of injurious falls: right activity, right person, right time. Age Ageing. (2023) 52:afad209. doi: 10.1093/ageing/afad209
76. Levasseur M, Richard L, Gauvin L, Raymond É. Inventory and analysis of definitions of social participation found in the aging literature: proposed taxonomy of social activities. Soc Sci Med. (2010) 71:2141–9. doi: 10.1016/j.socscimed.2010.09.041
77. Fang B, Huang J, Zhao X, Liu H, Chen B, Zhang Q. Concurrent and lagged associations of social participation and frailty among older adults. Health Soc Care Commun. (2022) 30:e4812–20. doi: 10.1111/hsc.13888
78. Brown TT, Scheffler RM, Seo S, Reed M. The empirical relationship between community social capital and the demand for cigarettes. Health Econ. (2006) 15:1159–72. doi: 10.1002/hec.1119
79. Leigh-Hunt N, Bagguley D, Bash K, Turner V, Turnbull S, Valtorta N, et al. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health. (2017) 152:157–71. doi: 10.1016/j.puhe.2017.07.035
80. Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci. (2015) 10:227–37. doi: 10.1177/1745691614568352
81. Zimmer C, McDonough MH, Hewson J, Toohey A, Din C, Crocker PRE, et al. Experiences with social participation in group physical activity programs for older adults. J Sport Exerc Psychol. (2021) 43:335–44. doi: 10.1123/jsep.2020-0335
82. Sun J, Lyu SJ. Social participation and urban-rural disparity in mental health among older adults in China. J Affect Disord. (2020) 274:399–404. doi: 10.1016/j.jad.2020.05.091
83. Li Y, Han WJ, Hu M. Does internet access make a difference for older adults' cognition in urban China? The moderating role of living arrangements. Health Soc Care Community. (2022) 30:e909–20. doi: 10.1111/hsc.13493
84. Panza F, Lozupone M, Solfrizzi V, Sardone R, Dibello V, Di Lena L, et al. Different cognitive frailty models and health- and cognitive-related outcomes in older age: from epidemiology to prevention. J Alzheimers Dis. (2018) 62:993–1012. doi: 10.3233/JAD-170963
85. Kim J, Lee J, Rodriguez M, Han A, Ju HJ. Identifying the relationships between types of leisure activities and cognitive functions in older adults. Am J Health Behav. (2023) 47:650–9. doi: 10.5993/AJHB.47.4.2
86. Huang Y, Guo X, Du J, Liu Y. Associations between intellectual and social activities with frailty among community-dwelling older adults in China: a prospective cohort study. Front Med. (2021) 8:693818. doi: 10.3389/fmed.2021.693818
87. Iizuka A, Suzuki H, Ogawa S, Kobayashi-Cuya KE, Kobayashi M, Takebayashi T, et al. Can cognitive leisure activity prevent cognitive decline in older adults? A systematic review of intervention studies. Geriatr Gerontol Int. (2019) 19:469–82. doi: 10.1111/ggi.13671
88. Fujiwara Y, Seino S, Nofuji Y, Yokoyama Y, Abe T, Yamashita M, et al. The relationship between working status in old age and cause-specific disability in Japanese community-dwelling older adults with or without frailty: A 36-year prospective study. Geriatr Gerontol Int. (2023) 23:855–63. doi: 10.1111/ggi.14686
89. Prince M, Bryce R, Albanese E, Wimo A, Ribeiro W, Ferri CP. The global prevalence of dementia: a systematic review and meta analysis. Alzheimers Dement. (2013) 9:63–75.e2. doi: 10.1016/j.jalz.2012.11.007
90. Sousa RM, Ferri CP, Acosta D, Albanese E, Guerra M, Huang Y, et al. Contribution of chronic diseases to disability in elderly people in countries with low and middle incomes: a 10/66 Dementia Research Group population-based survey. Lancet. (2009) 374:1821–30. doi: 10.1016/S0140-6736(09)61829-8
91. Firth J, Torous J, Stubbs B, Firth JA, Steiner GZ, Smith L, et al. The “online brain”: how the Internet may be changing our cognition. World Psychiatry. (2019) 18:119–29. doi: 10.1002/wps.20617
92. Fan S, Yang Y. How does internet use improve mental health among middle-aged and elderly people in rural areas in China? A quasi-natural experiment based on the china health and retirement longitudinal study (CHARLS). Int J Environ Res Public Health. (2022) 19:13332. doi: 10.3390/ijerph192013332
93. Bolle S, van Weert JC, Daams JG, Loos EF, de Haes HC, Smets EM. Online health information tool effectiveness for older patients: a systematic review of the literature. J Health Commun. (2015) 20:1067–83. doi: 10.1080/10810730.2015.1018637
94. Alqahtani BA. Association between physical frailty and sleep quality among saudi older adults: a community-based, cross-sectional study. Int J Environ Res Public Health. (2021) 18:12741. doi: 10.3390/ijerph182312741
95. Piovezan RD, Abucham J, Dos Santos RV, Mello MT, Tufik S, Poyares D. The impact of sleep on age-related sarcopenia: possible connections and clinical implications. Ageing Res Rev. (2015) 23:210–20. doi: 10.1016/j.arr.2015.07.003
96. Hyde Z, Flicker L, Almeida OP, Hankey GJ, McCaul KA, Chubb SA, et al. Low free testosterone predicts frailty in older men: the health in men study. J Clin Endocrinol Metab. (2010) 95:3165–72. doi: 10.1210/jc.2009-2754
97. Schakman O, Gilson H, Kalista S, Thissen JP. Mechanisms of muscle atrophy induced by glucocorticoids. Horm Res. (2009) 72:36–41. doi: 10.1159/000229762
98. Patel SR, Zhu X, Storfer-Isser A, Mehra R, Jenny NS, Tracy R, et al. Sleep duration and biomarkers of inflammation. Sleep. (2009) 32:200–4. doi: 10.1093/sleep/32.2.200
99. Yeap BB, Paul Chubb SA, Lopez D, Ho KK, Hankey GJ, Flicker L. Associations of insulin-like growth factor-I and its binding proteins and testosterone with frailty in older men. Clin Endocrinol (Oxf). (2013) 78:752–9. doi: 10.1111/cen.12052
100. Sánchez Romero EA, Martínez-Pozas O, García-González M, de-Pedro M, González-Álvarez ME, Esteban-González P, et al. Association between sleep disorders and sleep quality in patients with temporomandibular joint osteoarthritis: a systematic review. Biomedicines. (2022) 10:2143. doi: 10.3390/biomedicines10092143
101. Zhang Y, Yu G, Bai W, Wu SY, Geng XH, Zhang WY, et al. Association of depression and sleep quality with frailty: a cross-sectional study in China. Front Public Health. (2024) 12:1361745. doi: 10.3389/fpubh.2024.1361745
102. Stockelman KA, Bain AR, Dow CA, Diehl KJ, Greiner JJ, Stauffer BL, et al. Regular aerobic exercise counteracts endothelial vasomotor dysfunction associated with insufficient sleep. Am J Physiol-Heart Circul Physiol. (2021) 320:H1080–8. doi: 10.1152/ajpheart.00615.2020
103. Montgomery P, Dennis J. Physical exercise for sleep problems in adults aged 60+. Cochrane Database Syst Rev. (2002) 2002:Cd003404. doi: 10.1002/14651858.CD003404
104. Memon AA, Coleman JJ, Amara AW. Effects of exercise on sleep in neurodegenerative disease. Neurobiol Dis. (2020) 140:104859. doi: 10.1016/j.nbd.2020.104859
105. Chen KM, Chen MH, Chao HC, Hung HM, Lin HS Li CH. Sleep quality, depression state, and health status of older adults after silver yoga exercises: cluster randomized trial. Int J Nurs Stud. (2009) 46:154–63. doi: 10.1016/j.ijnurstu.2008.09.005
106. Chen KM, Chen MH, Lin MH, Fan JT, Lin HS Li CH. Effects of yoga on sleep quality and depression in elders in assisted living facilities. J Nurs Res. (2010) 18:53–61. doi: 10.1097/JNR.0b013e3181ce5189
107. De Nys L, Anderson K, Ofosu EF, Ryde GC, Connelly J, Whittaker AC. The effects of physical activity on cortisol and sleep: a systematic review and meta-analysis. Psychoneuroendocrinology. (2022) 143:105843. doi: 10.1016/j.psyneuen.2022.105843
108. Macaulay TR, Fisher BE, Schroeder ET. Potential indirect mechanisms of cognitive enhancement after long-term resistance training in older adults. Phys Ther. (2020) 100:907–16. doi: 10.1093/ptj/pzaa013
109. Yuan Y, Li J, Jing Z, Yu C, Zhao D, Hao W, et al. The role of mental health and physical activity in the association between sleep quality and quality of life among rural elderly in China: a moderated mediation model. J Affect Disord. (2020) 273:462–467. doi: 10.1016/j.jad.2020.05.093
110. Putnam RD. Bowling Alone: The Collapse and Revival of American Community. New York: Simon and Schuster (2001). p. 19. doi: 10.1145/358916.361990
111. Bassett E, Moore S. Social capital and depressive symptoms: the association of psychosocial and network dimensions of social capital with depressive symptoms in Montreal, Canada. Soc Sci Med. (2013) 86:96–102. doi: 10.1016/j.socscimed.2013.03.005
112. Eriksson M, Ng N. Changes in access to structural social capital and its influence on self-rated health over time for middle-aged men and women: a longitudinal study from northern Sweden. Soc Sci Med. (2015) 130:250–8. doi: 10.1016/j.socscimed.2015.02.029
113. Pénard T, Poussing N. Internet use and social capital: the strength of virtual ties. J Econ Issues. (2010) 44:569–95. doi: 10.2753/JEI0021-3624440301
114. Lim SER, Meredith SJ, Agnew S, Clift E, Ibrahim K, Roberts HC. Volunteer-led online group exercise for community-dwelling older people: a feasibility and acceptability study. BMC Geriatr. (2023) 23:461. doi: 10.1186/s12877-023-04184-7
115. Sun J, Kong X, Li H, Chen J, Yao Q, Li H, et al. Does social participation decrease the risk of frailty? Impacts of diversity in frequency and types of social participation on frailty in middle-aged and older populations. BMC Geriatr. (2022) 22:553. doi: 10.1186/s12877-022-03219-9
116. Yang Y, Zeng D, Yang F. Internet use and subjective well-being of the elderly: an analysis of the mediating effect based on social capital. Int J Environ Res Public Health. (2022) 19:12087. doi: 10.3390/ijerph191912087
Keywords: frailty, physical activity, social activity, economic activity, information activity, sleep activity, older adults
Citation: Ni Z, Zhu X, Shen Y, Zhu X, Xie S and Yang X (2024) Effects of activities participation on frailty of older adults in China. Front. Public Health 12:1483166. doi: 10.3389/fpubh.2024.1483166
Received: 19 August 2024; Accepted: 04 November 2024;
Published: 20 November 2024.
Edited by:
Emiliana Giacomello, University of Trieste, ItalyCopyright © 2024 Ni, Zhu, Shen, Zhu, Xie and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shiyu Xie, NTQwMDAxQG5qdWNtLmVkdS5jbg==; Xiaoguang Yang, eWFuZ194Z0BzanR1LmVkdS5jbg==
†These authors have contributed equally to this work and share first authorship
 Zihan Ni
Zihan Ni Xiuyuan Zhu1†
Xiuyuan Zhu1† Shiyu Xie
Shiyu Xie