
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 15 January 2025
Sec. Aging and Public Health
Volume 12 - 2024 | https://doi.org/10.3389/fpubh.2024.1480576
 Junfeng Zhang1†
Junfeng Zhang1† Huijie Huang1†
Huijie Huang1† Zhan Lin1
Zhan Lin1 Jingran Dong1
Jingran Dong1 Xiaoyan Zhang1
Xiaoyan Zhang1 Jing Gao2,3
Jing Gao2,3 Yin Liu2,4
Yin Liu2,4 Changping Li1*
Changping Li1* Zhuang Cui1
Zhuang Cui1Background: Activities in daily living (ADLs) disability triggered by aging population and chronic diseases in the middle-aged and older adults has become a major public health challenge. Cardiovascular-kidney-metabolic (CKM) syndrome, as a combination of several chronic conditions, has not yet been studied to explore its association with ADLs disability. We examined the association between CKM syndrome and ADLs disability among middle-aged and older adults in China and whether it varied by age and socioeconomic status.
Methods: Participants were from China Health and Retirement Longitudinal Study (CHARLS), which conducted four waves of surveys from 2011 to 2018. CKM stage was calculated through disease and physical examination data from CHARLS database. Meanwhile, the degree of disability was assessed through the ADL scale. Generalized linear mixed model was used to perform multivariate analysis to explore the association between CKM syndrome and the risk of ADLs disability.
Results: The proportion of CKM stage 0, 1, 2, and 3 among the 5,898 eligible participants (median age 60 years, 60.27% women) in 2011 were 14.70, 30.23, 41.39, and 13.68%. The risk of ADL disability was increased by 16% (odds ratio [95% confidence interval]; 1.16 [1.00–1.33]) and 33% (1.33 [1.12–1.58]) in CKM stages 2 and 3 compared with stage 0. In addition, there was a greater risk of BADL disability in 75+ age group compared to other age groups, but no significant association with IADL disability. In the subgroup aged 75+, the risk of BADL disability was increased for CKM stage 2/3 (1.48 [1.01–2.18]/1.67 [1.06–2.64]) compared with stage 0. Only in the lowest quartile of socioeconomic status group CKM stage rise was strongly associated with the risk of disability. The risk of ADL disability was greater for CKM stage 2/3 (1.45 [1.15–1.83]/1.48 [1.11–1.98]) compared to CKM stage 0 in the lowest economic status quartile.
Conclusion: For middle-aged and older adults in China, CKM syndrome is a key risk factor for ADLs disability. Therefore, effective measures should be taken to manage CKM stage at the lowest possible level, especially in older and economically disadvantaged populations.
Diabetes, chronic kidney disease (CKD) and cardiovascular disease (CVD) are three major challenges in global health, and their high and increasing prevalence in middle-aged and older adults not only affects the quality of life of individuals, but also poses a significant burden on global health and the economy (1–3). Diabetes affects approximately 9.3% of the global population and more than 460 million people. In China, the number of diabetes cases has surged and is expected to reach 140 million by 2030 (4). CKD affects about 5–7% of the global population, especially in developing countries and among vulnerable groups (5), a trend mirrored in China, where cases of CKD are on the rise, especially among people with diabetes and hypertension (6). CVD remains the leading cause of death globally, claiming 17.7 million lives annually and accounting for 31% of global deaths, with China bearing a heavy burden, especially among the older adults (5). In view of this, the Chinese Government has proposed a series of measures to curb the high prevalence of these chronic conditions. For example, the Healthy China Initiative (7) has developed programs to prevent and treat CVD and diabetes, and the Healthy Poverty Alleviation Project (8) provides chronic disease screening and treatment services targeting impoverished areas. However, due to population aging and the prevalence of risk factors for chronic conditions, the burden of chronic conditions in China continues to increase and is likely to continue to grow (9). It is considered that these conditions frequently coexist (10). To better understand the complex interactions between metabolic risk factors (e.g., obesity and diabetes mellitus), CKD, and the cardiovascular system, the American Heart Association introduced the concept of CKM syndrome in a 2023 presidential advisory note (11). CKM syndrome is defined as a spectrum of disease states associated with dysfunction or excessive obesity. CKM health is the clinical manifestation of pathophysiologic interactions between metabolic risk factors, CKD, and cardiovascular system. Adverse CKM health leads to serious clinical consequences, including premature mortality, excess morbidity, and multiorgan diseases (11).
Disability is generally recognized as difficulties in performing activities necessary for daily living (12). The most common problem affecting the health and quality of life of older adults is functional disability. Functional disability in older adults is defined as acquired difficulties in accomplishing basic daily tasks or more complex tasks required for independent living (13). The most widely used measures of functional disability are basic activities of daily living (BADL), which are daily activities that people perform without assistance such as personal care, hygiene, mobility, and eating, and instrumental activities of daily living (IADL), which are higher level activities associated with independent living in the community such as cooking, shopping, housekeeping, and money management (14, 15). According to the World Health Survey across 59 countries, the average prevalence of severe ADLs disability among adults aged 60 and above is 38.1%, varying from 29.5% in high-income countries to 43.4% in low-income countries (16). ADLs disability poses significant challenges to global health and social care systems, increasing the burden on healthcare services and family caregivers (17). It is associated with poorer quality of life (18) and higher mortality rates (19).
Both CKM syndrome and ADLs disability are common in the older adults population (16, 20), and there is no research evidence to support an association between them. CKM syndrome is a multi-system chronic condition involving the heart, kidneys, and metabolic system. In previous studies, chronic conditions affect patients’ physical, psychological, and social functioning, not just their physical health (21). Established theories such as the biopsychosocial model suggest that the functional disability of patients with chronic diseases does not only originate from the physical disease, but is also influenced by the psychological state and social environment (22). This gives us a new clue that CKM syndrome may trigger functional disability by affecting patients’ physical health, psychological state and social functioning. For patients with CKM syndrome, the multiple physical impairments of CKM syndrome, such as CVD (23, 24), CKD (25), metabolic syndrome, and obesity (26), may lead to a decrease in the patient’s ability to perform daily activities by directly affecting physical function. In addition, diabetes (27) and CVD (28) are often accompanied by mental health problems such as depression and anxiety, and these physical and psychological factors can further limit the patient’s social activities and ability to work (29–31), increasing functional disability in life. However, few prospective studies have explored the mutual relationship between CKM syndrome and ADLs disability and how this relationship varies across age and economic status groups.
To enhance our understanding of this relationship, our study utilized data from the CHARLS to estimate the association between CKM syndrome and ADLs disability from 2011 to 2018, and explored differences by age group and socioeconomic status.
This study is based on the CHARLS, a national longitudinal survey of individuals aged 45 years and older. CHARLS has conducted five waves of surveys to date, with the baseline beginning in 2011 (Wave 1). A total of 17,705 participants from 450 villages or communities across 28 provinces were recruited using the probability proportionate to size (PPS) Sampling technique. These participants were then followed up in 2013, 2015, 2018, and 2020. Information on participants’ sociodemographics, health status, physical functioning, family characteristics, and lifestyle was collected through one-on-one interviews and structured questionnaires. The overall response rate for the first wave of CHARLS was 80.5% (32). The data included individual weighting variables to ensure that the survey sample was nationally representative. CHARLS received ethical approval from the Ethics Review Committee of Peking University under the approval number IRB00001052-11015, and each participant signed a written informed consent form.
In our population-based panel data analysis, we utilized data from four waves of CHARLS in 2011, 2013, 2015, and 2018. In this study, we included observations from participants with no missing CKM and ADLs disability data for each wave. We excluded participants with missing age-sex information, missing individual weights, and those without baseline observations. Figure 1 illustrates our study population screening process.
According to the presidential advisory note issued by the American Heart Association (AHA) in early October 2023 (11), CKM syndrome is categorized into four different stages, ranging from stage 0 to stage 4 (Figure 2). We adapted the evaluation criteria for CKM to the Chinese population, and the following definitions of each CKM stage were presented:
Stage 0: No CKM health risk factors. Individuals without overweight/obesity, metabolic risk factors (hypertension, hypertriglyceridemia, metabolic syndrome, diabetes), CKD, or subclinical/clinical CVD.
Stage 1: Excess and/or dysfunctional adiposity. Individuals with overweight/obesity, abdominal obesity, or dysfunctional adipose tissue without the presence of other metabolic risk factors or CKD. BMI ≥ 23 kg/m2 waist circumference ≥ 80 cm in women and ≥ 90 cm in men. Fasting blood glucose ≥100–124 mg/dL or HbA1c between 5.7 and 6.4%.
Stage 2: Metabolic risk factors and CKD. Individuals with metabolic risk factors (hypertriglyceridemia, hypertension, diabetes mellitus, metabolic syndrome) or CKD.
Stage 3: Subclinical CVD in CKM: Subclinical Atherosclerotic cardiovascular disease or subclinical heart failure among individuals with excess/dysfunctional adiposity, other metabolic risk factors, or CKD. Or at equivalent risk (predicted high-risk cardiovascular disease or very high-risk chronic kidney disease).
Stage 4: Clinical CVD in CKM: Clinical CVD (coronary heart disease, heart failure, stroke, peripheral artery disease, Atrial fibrillation) among individuals with excess/dysfunctional adiposity, other metabolic risk factors, or CKD. Of these, stage 4a without renal failure and stage 4b with renal failure.
It was difficult to obtain the prevalence of subclinical CVD in participants from the CHARLS database. Therefore, to more accurately characterize CKM stages with physical examination data from the database, we combined stages 3 and 4 and referred to them as CKM stage 3 in this study.
The ADLs disability was measured using the BADL and IADL scales. BADL reflected six items measuring dressing, bathing, eating, getting up, toileting, and continence. IADL consisted of five items that measure housework, cooking, shopping, taking medications, and handling finances. Each item consisted of four response options (1. Have no difficulty; 2. Have difficulty but can still do it; 3. Have difficulty and need help; 4. Cannot do it). Based on previous studies, the outcomes were dichotomous, with respondents assigned a value of 1 if they had difficulty with any of the activities or were unable to perform the activity (options 2, 3, or 4), and a value of 0 if they reported no difficulty (option 1) in completing the activity (17, 33).
The covariates of interest covered social demographic characteristics, economic status, lifestyle and health conditions. Social demographic characteristics included age, sex (male, female), educational level (primary school and below, middle school, high school and above), and marital status (married or partnered, other). We categorized the economic status of the population into four levels based on annual consumption quartiles. Lifestyle features included self-reported current smoking status (yes or no) and current alcohol consumption status (yes or no). For health status, participants’ chronic disease status was assessed by self-report and classified according to the number of chronic diseases other than CKM (0, 1, 2, ≥3). Participants’ self-assessed health status was divided into three categories (good/very good, fair, and poor/very poor).
In this study, all descriptive analyses were weighted to account for the complexity, the multistage design of the study, and non-response in the CHARLS data. The distribution of categorical variables was described by n (%), and the chi-square test was employed on the weighted data to analyze whether there existed a statistical correlation between exposure factors and CKM risk.
We used generalized linear mixed model to estimate the association between CKM stages and ADLs disability. The link function was set to logit. We considered the baseline CKM stage as the stage for all follow-up time points. Adjusted odds ratios (ORs) were reported based on age, sex, marital status, education level, economic status, presence of other chronic diseases, self-assessed health, smoking, and alcohol consumption, with a 95% confidence interval. We also assessed variable covariance using the variance inflation factor (VIF). Generally, VIF values <10 is considered acceptable. Generalized linear mixed model was used to evaluate the association between CKM stages and ADLs disability in 2011 and 2015. In the generalized linear mixed model for 2011 and 2015, CKM stage and functional disability status for the respective years were used. Detailed health examination data for both years allowed us to calculate CKM stage for the respective time periods. To explore differential effects in the population, we conducted stratified analyses by age and socioeconomic status.
We conducted the following sensitivity analyses: (1) We transformed BADL, IADL, and ADL disabilities from dichotomous categories into scores and explored the association between CKM stage and scores for ADL, BADL, and ADL with linear mixed-effects model. For all questions in the BADL and IADL scales, the 4 options (1. Have no difficulty; 2. Have difficulty but can still do it; 3. Have difficulty and need help; 4. Cannot do it) were assigned values of 0, 0.33, 0.66, and 1, respectively. (2) The multiple imputation by chained equations method was applied to impute missing covariates in our study, generating five imputed datasets. We combined the estimated values from the generalized linear mixed models for each dataset from the five imputed datasets.
All analyses were conducted using statistical software R 4.4.0, and two-tailed p-values less than 0.05 were considered statistically significant.
Of the 17,705 participants in charls2011, 5,898 were eligible for inclusion in our analyses. The sociodemographic characteristics of qualified participants are shown in Table 1. Median age of the participants in 2011 was 60 years (IQR 54–68). Among the participants, 2,343 (39.73%) were male, and 3,555 (60.27%) were female. 4,545 participants (77.06%) had an educational level of primary school or below. 5,061 participants (85.81%) were married or partnered. 3,604 (61.11%) had at least 1 chronic disease. 3,699 (62.72%) perceived their health as poor or very poor.1552 (26.31%) were current smokers and 1,642 (27.84%) currently drank alcohol. The percentage of CKM stages 0, 1, 2, and 3 among eligible participants in 2011 was 14.70, 30.23, 41.39, and 13.68%, respectively. The distribution of CKM stages varied across different sex, age, marital status, number of other chronic diseases, and smoking and alcohol consumption groups (all with p < 0.001). The females, those aged 65–74, unmarried, having three or more chronic diseases and with poorer self-rated health were more likely than their counterparts to have more severe CKM syndrome. The overall prevalence of ADL, BADL, and IADL disabilities were 38.10, 24.13, and 27.96%, respectively. In addition, the more severe CKM syndrome had greater rates of ADLs disability.
Tables 2–4 demonstrate the distribution of different types of ADLs disability in the population. Different BADL, IADL, and ADL disabilities were distributed differently across CKM stages, age, education level, marital status, number of chronic diseases, and self-rated health populations. BADL, IADL, and ADL disabilities were associated with higher CKM stages, older age groups, lower education levels, being unmarried, more comorbid chronic diseases, and poorer self-rated health (all with p < 0.001).
In the overall sample, participants in CKM stages 2 and 3 had 22% (aOR = 1.22, 95% CI: 1.03–1.45) and 42% (aOR = 1.42, 95CI: 1.16–1.74) greater risks of BADL disability than those in CKM stage 0, respectively. CKM stage 3 was associated with a greater risk of IADL disability compared to CKM stage 0 (aOR = 1.31, 95% CI: 1.09–1.57). The risk of ADL disability was 16% greater for CKM stage 2 (aOR = 1.16, 95% CI: 1.00–1.33) and 33% greater for CKM stage 3 (aOR = 1.33, 95% CI: 1.12–1.58) compared to CKM stage 0 (Table 5). The VIF values of all variables in the models were <2, indicating that there was no multicollinearity between the variables. The association between CKM stage and ADLs disability in the 2011 and 2015 waves was generally consistent with our main findings (Table 6).
Age-stratified analyses showed that, overall, differences in associations between CKM stage and BADL, IADL, and ADL disabilities were similar across age subgroups. Across age subgroups, rising CKM stage was associated with an increased risk of disability in BADL, particularly evident in the 75 years and older subgroup. In the 75 years and older age subgroup, the risk of CKM stage 2 and stage 3 BADL was increased by 48% (aOR = 1.48, 95% CI: 1.01–2.18) and 67% (aOR = 1.67, 95% CI: 1.06–2.64), respectively, compared with stage 0. Within each age subgroup for IADL and ADL disabilities, higher CKM stage is associated with a greater risk of disability compared to stage 0, except in the 75 years and older subgroup (Figure 3).
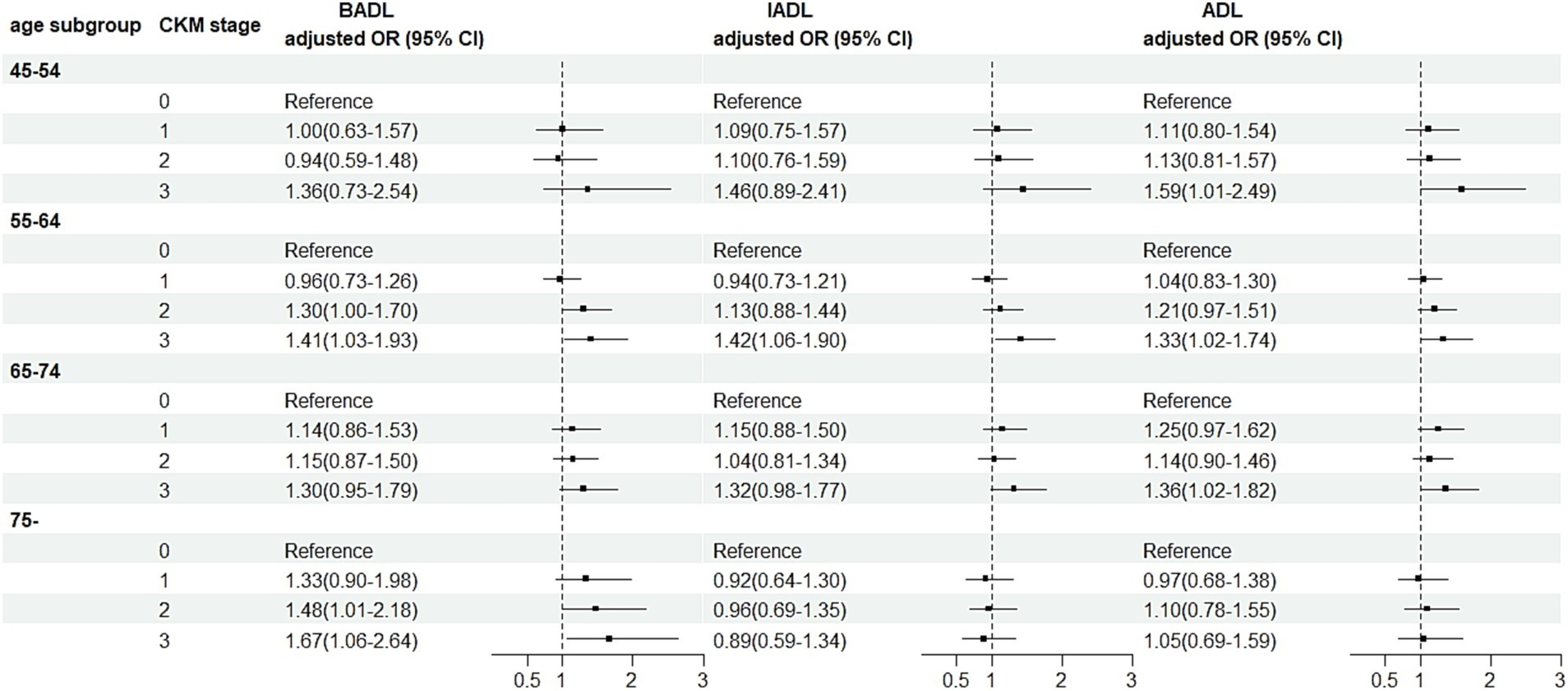
Figure 3. Association between CKM and ADLs disability by age groups. OR, odds ratio; BADL, basic activities of daily living; IADL, instrumental activities of daily living; ADL, activities of daily living; CKM, cardiovascular-kidney-metabolic syndrome. All estimates were adjusted for age, sex, marital status, education, number of other non-communicable diseases, self-reported health, smoking, drinking and socioeconomic status.
Stratified analyses by socioeconomic status showed that, overall, rising CKM stage was associated with increased risk of ADLs disability across economic status quartiles. This risk was highest in the lowest economic status quartile and lowest in the highest economic status quartile (Figure 4).
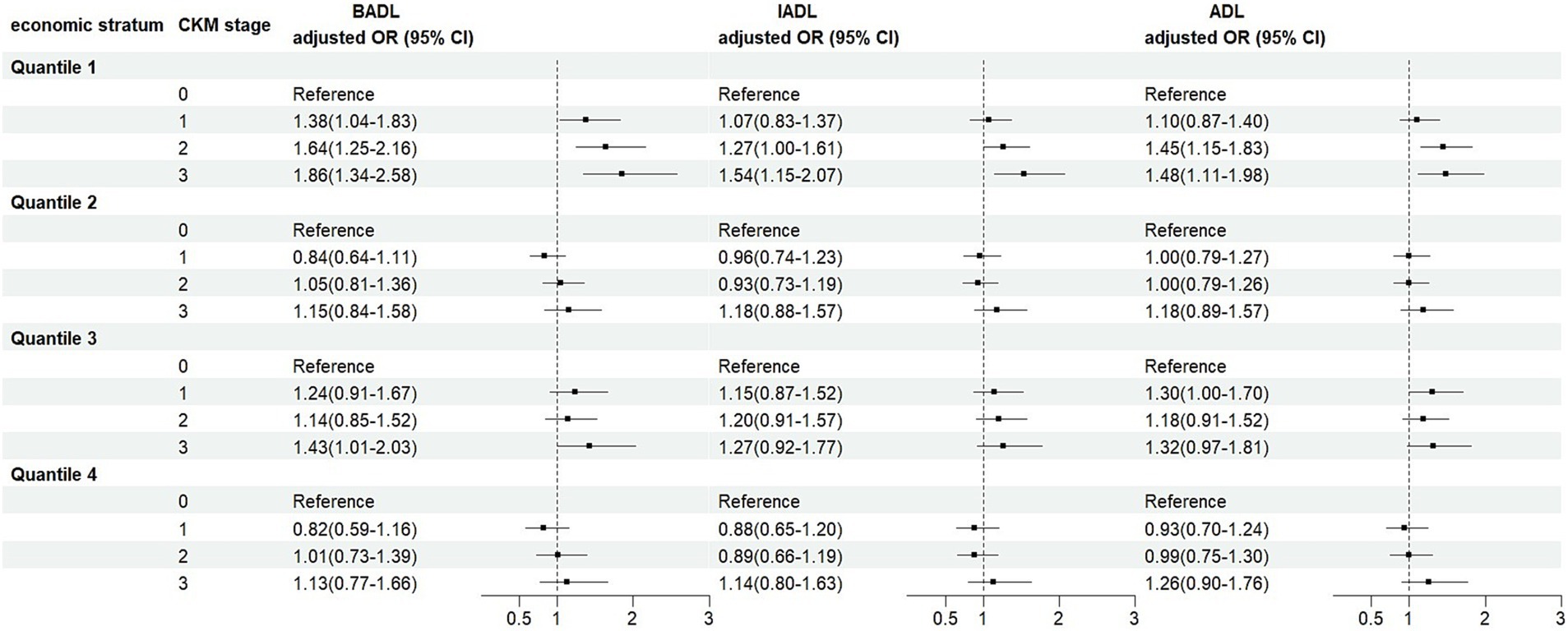
Figure 4. Association between CKM and ADLs disability by socioeconomic strata. OR, odds ratio; BADL, basic activities of daily living; IADL, instrumental activities of daily living; ADL, activities of daily living; CKM, cardiovascular-kidney-metabolic syndrome. All estimates were adjusted for age, sex, marital status, education, number of other non-communicable diseases, self-reported health, smoking, drinking and socioeconomic status.
Our sensitivity analysis modified the calculation method for ADLs disabilities from binary classification to scoring, which was consistent with our main finding that the risk of ADLs disability increased as CKM stage progressed (Table 7). The analysis after multiple imputations also yielded similar results (Table 8).
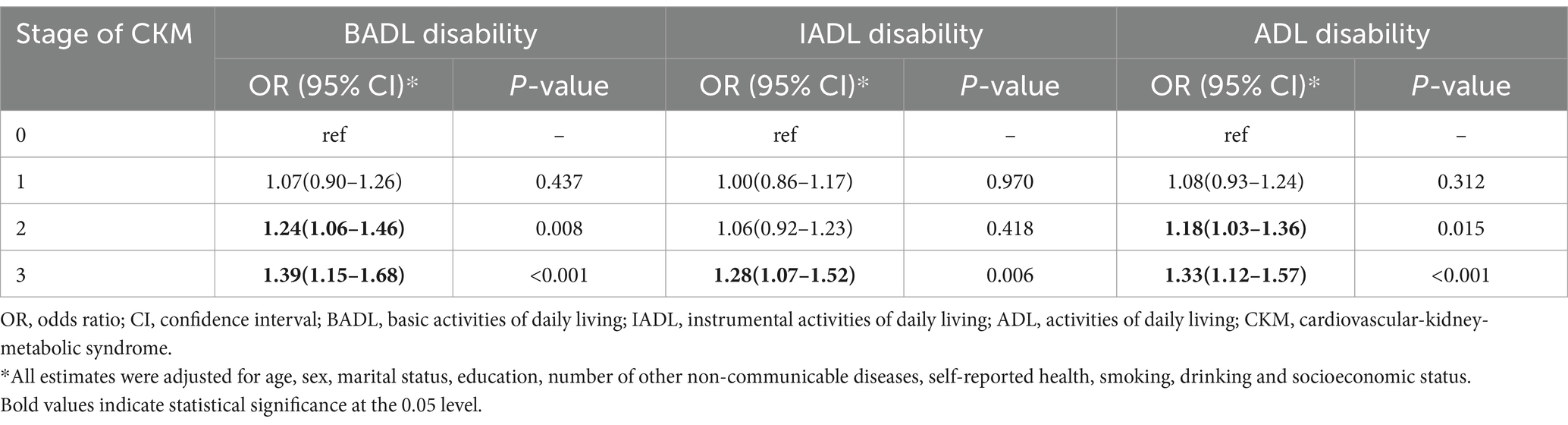
Table 8. Association between the stage of CKM and ADLs disability in China after multiple imputation, 2011–2018.
To the best of our knowledge, this study is the first to investigate the impact of CKM syndrome on ADLs disability among Chinese middle-aged and older adults. Although earlier studies have examined the impact of CVD, CKD, diabetes, and multimorbidity on ADLs disability, the impact of metabolic risk factors, CKD, and the cardiovascular system as a combined disease state on ADLs disability has not been explicitly discussed.
According to our study, there was a statistically significant association between CKM syndrome and increased risk of ADLs disability. This association persisted after adjustment for other factors in the model. In the present study, the association between rising CKM stage and ADLs disability was similar in every age group; that is, as CKM stages increased, so did the risk of ADLs disability. Besides, there was a greater risk of BADL disability in the 75- and -over age group compared with the other age groups, but there was no similar association with IADL disability. This indicated that the decline in BADL ability is more pronounced in the older population, while the decline in IADL ability may be influenced by other factors; age masked the impact of CKM stage progression on IADL impairment, which may suggest a cohort effect, indicating that people aged 75 and above have a greater lack of community-based independent living capacity than younger people. Among different socioeconomic statuses, only the group in the lowest quartile of socioeconomic status showed a strong association between rising CKM stage and risk of ADLs disability, suggesting that socioeconomic status may be an important factor influencing disability risk. This may be due to low-income groups facing limitations in accessing healthcare, health information, and living conditions.
In previous studies, the adverse effects of CKD, CVD, diabetes, and multiple diseases on ADLs disability have been widely reported. Plantinga et al. (34) found that the prevalence of disability was 2–3 times higher in people with CKD compared to non-CKD participants, and that older individuals reported higher levels of disability. A study based on the large-scale survey in Shanghai, China (35), indicated that the number of chronic diseases was strongly correlated with BADL and IADL disabilities, with older age, lower income, and female sex being key focus groups, which aligns with our predictions for vulnerable populations. Another CHARLS-based study (36) reached similar conclusions. Regarding cardiovascular system and metabolic risk factors, it was reported that in a study exploring the association between cardiometabolic multimorbidity (CM) and risk of disability (37), participants with CM at baseline had a faster progression of disability compared with those without CM. A study in Taiwan (38) identified cardiovascular disease as an independent factor contributing to elevated disability in people with diabetes. In our study, we did not just focus on single-system diseases, but covered the combined effects between cardiovascular, kidney, and metabolic risk factors. This integrated perspective allows us to gain a deeper understanding of how these systems work together to elevate the risk of ADLs disability.
Most studies of economic factors and ADLs disability are consistent with our conclusion that the risk of ADLs disability is greater in groups with lower economic status. A study exploring the association between multimorbidity and ADLs disability revealed that low-income groups were more likely to have IADL disability (35). Many studies of the association between personal income and ADLs disability have shown a significant association between low income and ADLs disability (39–41). In our study, after including economic status as a covariate in the regression model, there was no significant association with ADLs disability (p > 0.05). However, in the study by Fuller-Thomson and Gadalla (42), individual income level was a significant predictor of ADLs disability.
Our research findings provide new leads for the development of targeted policies and interventions to address the increasing burden of CKM syndrome and ADLs disability in China. We suggest that Chinese health authorities take proactive measures to alleviate the staging progression of CKM syndrome to minimize the incidence of ADLs disability. Establish a national surveillance system for CKM syndrome in order to track and assess the staging progression of CKM in real time. Utilize big data and artificial intelligence technologies to identify high-risk populations and implement early interventions. Keep CKM stage at the lowest possible level. Focus should also be placed on strengthening health education and widely promoting knowledge dissemination activities on the prevention and management of CKM syndrome and ADLs disability in the community and schools, so as to enhance the public’s health awareness and self-management ability. A cooperative mechanism involving multiple parties, including community support, health insurance policy makers, medical service providers and pharmaceutical manufacturers, should be established to ensure the accessibility and continuity of comprehensive medical services. Promote a multidisciplinary care model that provides support in various aspects, including nutrition, rehabilitation and psychology. Increase investment in disability research on CKM syndrome and ADLs, provide financial and policy support, and encourage medical institutions and scientific research institutes to carry out relevant research and innovative projects. In this process, special attention should be paid to those who may be seriously affected by CKM Syndrome, including women, the older adults, those with a history of chronic diseases, and those in poorer economic conditions, by designing and implementing special health management programs. This includes regular health checkups, personalized treatment plans, and psychological support services, and improving the distribution of healthcare resources in remote and impoverished areas to ensure that patients in these areas also have access to timely and high-quality healthcare services. In addition, social determinants of health should be taken into account (43), such as social support networks, employment, education, the natural environment and public health, to work toward the realization of health equity.
The study’s strengths include the use of a large nationally representative sample and a longitudinal study design. However, our study has several limitations. First, in order to more accurately characterize CKM stages with data from CHARLS, we had to combine stages 3 and 4 of the original CKM stages, and this combination may have made it difficult to capture subtle differences between the two stages. Besides, information about chronic conditions and ADLs disability was obtained through self-report, introducing the potential for recall bias. In the future, we hope to obtain more suitable data for calculating CKM stages and more scientific methods for characterizing the distribution of CKM syndrome in the Chinese population, to more accurately explore the association between CKM syndrome and ADLs disability.
This study provided evidence that CKM syndrome is a risk factor for ADLs disability. We also found that older age and poorer socioeconomic status increase the risk of ADLs damage. Therefore, it is of significant public health importance for Chinese health authorities to monitor and control the progression of CKM staging in the population, especially among key groups, to reduce the risk of ADLs disability in middle-aged and older adults individuals.
Publicly available datasets were analyzed in this study. This data can be found here: https://charls.charlsdata.com/users/sign_in/en.html.
This study was based on publicly available datasets (CHARLS). Ethical review and approval was not required for the study, in accordance with the local legislation and institutional requirements. The CHARLS study was reviewed and approved by Ethics Review Committee of Peking University; and tehe participants provided their written informed consent to participate in this study.
JZ: Conceptualization, Data curation, Formal analysis, Writing – original draft, Writing – review & editing. HH: Investigation, Methodology, Writing – review & editing. ZL: Data curation, Software, Writing – original draft. JD: Data curation, Writing – original draft. XZ: Data curation, Writing – original draft. JG: Formal analysis, Writing – review & editing. YL: Formal analysis, Writing – review & editing. CL: Methodology, Writing – review & editing. ZC: Methodology, Writing – review & editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by The Humanities and Social Science Fund of the Ministry of Education, China (Grant no. 17YJAZH048); National Natural Science Foundation of China (Grant no. 72374153); the Key Projects of Tianjin Natural Science Foundation (Grant no. 22JCZDJC00130); and the Key Project of Scientific and Technological Support Plan of Tianjin in 2020 (Grant no. 20YFZCSY00820).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
CKM, Cardiovascular-kidney-metabolic; ADL, Activities in daily living; BADL, Basic activities in daily living; IADL, Instrumental activities in daily living; CKD, Chronic kidney disease; CVD, Cardiovascular disease; CHARLS, The China Health and Retirement Longitudinal Study; VIF, Variance inflation factor; CM, cardiometabolic multimorbidity.
1. Bikbov, B, Purcell, SA, Levey, AS, Smith, M, Abdoli, A, Abebe, M, et al. Global, regional, and national burden of chronic kidney disease, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2020) 395:709–33. doi: 10.1016/S0140-6736(20)30045-3
2. Sun, H, Saeedi, P, Karuranga, S, Pinkepank, M, Ogurtsova, K, Duncan, BB, et al. IDF diabetes atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. (2022) 183:109119. doi: 10.1016/j.diabres.2021.109119
3. Tsao, CW, Aday, AW, Almarzooq, ZI, Anderson, CAM, Arora, P, Avery, CL, et al. Heart disease and stroke Statistics-2023 update: a report from the American Heart Association. Circulation. (2023) 147:e93–e621. doi: 10.1161/CIR.0000000000001123
4. Hsu, RK, and Powe, NR. Recent trends in the prevalence of chronic kidney disease: not the same old song. Curr Opin Nephrol Hypertens. (2017) 26:187–96. doi: 10.1097/MNH.0000000000000315
5. Couser, WG, Remuzzi, G, Mendis, S, and Tonelli, M. The contribution of chronic kidney disease to the global burden of major non-communicable diseases. Kidney Int. (2011) 80:1258–70. doi: 10.1038/ki.2011.368
6. Bermúdez-López, M, Arroyo, D, Betriu, À, Masana, L, Fernández, E, and Valdivielso, JM. New perspectives on CKD-induced dyslipidemia. Expert opinion on therapeutic. Targets. (2017) 21:967–76. doi: 10.1080/14728222.2017.1369961
7. National Health Commission of the People's Republic of China. Health China Initiative. (2019). Available at: http://www.nhc.gov.cn/guihuaxxs/s3585u/201907/e9275fb95d5b4295be8308415d4cd1b2.shtml (Accessed January 6, 2025).
8. National Health Commission of the People’s Republic of China. Health poverty alleviation project. (2017). Available at: http://www.nhc.gov.cn/cms-search/xxgk/getManuscriptXxgk.htm?id=4eed42903abd44f99380969824a07923 (Accessed January 6, 2025).
9. Peng, W, Chen, S, Chen, X, Ma, Y, Wang, T, Sun, X, et al. Trends in major non-communicable diseases and related risk factors in China 2002–2019: An analysis of nationally representative survey data. Lancet Reg Health - Western Pacific. (2023). 43:100809.
10. Marassi, M, and Fadini, GP. The cardio-renal-metabolic connection: a review of the evidence. Cardiovasc Diabetol. (2023) 22:195. doi: 10.1186/s12933-023-01937-x
11. Ndumele, CE, Rangaswami, J, Chow, SL, Neeland, IJ, Tuttle, KR, Khan, SS, et al. Cardiovascular-kidney-metabolic health: a presidential advisory from the American Heart Association. Circulation. (2023) 148:1606–35. doi: 10.1161/CIR.0000000000001184
12. Tas, U, Verhagen, AP, Bierma-Zeinstra, SM, Odding, E, and Koes, BW. Prognostic factors of disability in older people: a systematic review. Br J Gen Pract. (2007) 57:319–23.
13. Rodrigues, MA, Facchini, LA, Thumé, E, and Maia, F. Gender and incidence of functional disability in the elderly: a systematic review. Cad Saude Publica. (2009) 25:S464–76. doi: 10.1590/S0102-311X2009001500011
14. Dai, S, Wang, S, Jiang, S, Wang, D, and Dai, C. Bidirectional association between handgrip strength and ADLs disability: a prospective cohort study. Front Public Health. (2023) 11:1200821. doi: 10.3389/fpubh.2023.1200821
15. Jin, X, He, J, Liang, Y, Sun, X, Yan, S, Wu, Y, et al. Associations between household solid fuel use and activities of daily living trajectories: a nationwide longitudinal study of middle and older adults in China. Environ Int. (2022) 170:107605. doi: 10.1016/j.envint.2022.107605
16. World report on disability. World report on disability. Lancet. (2011) 377:1977. doi: 10.1016/S0140-6736(11)60844-1
17. Qiao, Y, Liu, S, Li, G, Lu, Y, Wu, Y, Shen, Y, et al. Longitudinal follow-up studies on the bidirectional association between ADL/IADL disability and multimorbidity: results from two National Sample Cohorts of middle-aged and elderly adults. Gerontology. (2021) 67:563–71. doi: 10.1159/000513930
18. Medhi, GK, Sarma, J, Pala, S, Bhattacharya, H, Bora, PJ, and Visi, V. Association between health related quality of life (HRQOL) and activity of daily living (ADL) among elderly in an urban setting of Assam. India J Family Med Prim Care. (2019) 8:1760–4. doi: 10.4103/jfmpc.jfmpc_270_19
19. Naseer, M, Forssell, H, and Fagerström, C. Malnutrition, functional ability and mortality among older people aged ⩾ 60 years: a 7-year longitudinal study. Eur J Clin Nutr. (2016) 70:399–404. doi: 10.1038/ejcn.2015.196
20. Minhas, AMK, Mathew, RO, Sperling, LS, Nambi, V, Virani, SS, Navaneethan, SD, et al. Prevalence of the cardiovascular-kidney-metabolic syndrome in the United States. J Am Coll Cardiol. (2024) 83:1824–6. doi: 10.1016/j.jacc.2024.03.368
21. Hwu, YJ. The impact of chronic illness on patients. Rehabil Nurs. (2020) 20:221–5. doi: 10.1002/j.2048-7940.1995.tb01632.x
22. Waddell, G, Burton, AK, and Aylward, M. A biopsychosocial model of sickness and disability. Guides Newsletter. (2008) 3:1–13. doi: 10.1001/amaguidesnewsletters.2008.MayJun01
23. Ettinger, WH, Fried, LP, Harris, T, Shemanski, L, Schulz, R, Robbins, J, et al. Self-reported causes of physical disability in older people: the cardiovascular health study. J Am Geriatr Soc. (1994) 42:1035–44. doi: 10.1111/j.1532-5415.1994.tb06206.x
24. Mansfield, A, Inness, EL, and Mcilroy, WE. Stroke. Handb Clin Neurol. (2018) 159:205–28. doi: 10.1016/B978-0-444-63916-5.00013-6
25. Painter, PL, Padilla, J, Krasnoff, JB, DaSilva, M, Johansen, K, Frassetto, L, et al. Physical functioning in patients with chronic kidney disease. Med Sci Sports Exerc. (2005) 37:S235–5. doi: 10.1249/00005768-200505001-01225
26. Gerber, L. 2020 Sidney Licht lecture: metabolic syndrome and obesity negatively impact function. J Int Soc Phys Rehabilit Med. (2021) 4:58–62. doi: 10.4103/jisprm.jisprm_28_20
27. Néss, S, Midthjell, K, Moum, T, Sørensen, T, and Tambs, K. Diabetes mellitus and psychological well-being. Results of the Nord-Trøndelag health survey. Scand J Soc Med. (1995) 23:179–88. doi: 10.1177/140349489502300308
28. Peck, MD, and Ai, AL. Chapter 2; cardiac conditions. J Gerontol Soc Work. (2008) 50:11–44. doi: 10.1080/01634370802137777
29. Sayeed, MSB, Joshy, G, Banks, E, and Korda, R. 1025Social interaction of middle-aged and older people with and without cardiovascular disease in Australia. Int J Epidemiol. (2021) 50:80. doi: 10.1093/ije/dyab168.080
30. Loerbroks, A, Herr, RM, Icks, A, and Bosch, JA. The association of self-reported diabetes with impaired social functioning in low-, middle- and high-income countries: findings from the world health survey. Diabet Med. (2018) 35:332–8. doi: 10.1111/dme.13578
31. Jansen, DL, Rijken, M, Monique, H, Kaptein, AA, and Groenewegen, PP. Psychological and social aspects of living with chronic kidney disease. Chronic Kidney Disease and Renal Transplantation [Internet]. InTech. (2012). Available at: http://www.intechopen.com/books/chronic-kidney-disease-and-renal-transplantation/psychological-and-social-aspects-of-living-with-chronic-kidney-disease (Accessed January 6, 2025)
32. Zhao, Y, Hu, Y, Smith, JP, Strauss, J, and Yang, G. Cohort profile: the China health and retirement longitudinal study (CHARLS). Int J Epidemiol. (2014) 43:61–8. doi: 10.1093/ije/dys203
33. Zhong, Y, Wang, J, and Nicholas, S. Gender, childhood and adult socioeconomic inequalities in functional disability among Chinese older adults. Int J Equity Health. (2017) 16:165. doi: 10.1186/s12939-017-0662-3
34. Plantinga, LC, Johansen, K, Crews, DC, Shahinian, VB, Robinson, BM, Saran, R, et al. Association of CKD with disability in the United States. Am J Kidney Dis. (2011) 57:212–27. doi: 10.1053/j.ajkd.2010.08.016
35. Su, P, Ding, H, Zhang, W, Duan, G, Yang, Y, Chen, R, et al. The association of multimorbidity and disability in a community-based sample of elderly aged 80 or older in Shanghai, China. BMC Geriatr. (2016) 16:178. doi: 10.1186/s12877-016-0352-9
36. Peng, S, Wang, S, and Feng, XL. Multimorbidity, depressive symptoms and disability in activities of daily living amongst middle-aged and older Chinese: evidence from the China health and retirement longitudinal study. J Affect Disord. (2021) 295:703–10. doi: 10.1016/j.jad.2021.08.072
37. He, H, Tu, R, Chen, H, Wang, C, Wu, S, and Wang, S. Longitudinal trajectories of disability among Chinese adults: the role of cardiometabolic multimorbidity. Aging Clin Exp Res. (2024) 36:79. doi: 10.1007/s40520-024-02732-8
38. Li, CL, Chiu, YC, Chang, HY, Hsu, KH, Bai, YB, and Wang, HH. Association of geriatric conditions and cardiovascular diseases with disability in older adults with diabetes: findings from a nationally representative survey. Geriatr Gerontol Int. (2013) 13:563–70. doi: 10.1111/j.1447-0594.2012.00935.x
39. Liu, H, and Wang, M. Socioeconomic status and ADL disability of the older adults: cumulative health effects, social outcomes and impact mechanisms. PLoS One. (2022) 17:e0262808. doi: 10.1371/journal.pone.0262808
40. Nóbrega, JCL, Medeiros, JB, Santos, TTM, Alves, SAV, Freitas, J, Silva, JMM, et al. Socioeconomic factors and health status disparities associated with difficulty in ADLs and IADLs among Long-lived populations in Brazil: a cross-sectional study. Inquiry. (2021) 58:469580211007264. doi: 10.1177/00469580211007264
41. Xu, X, Yang, L, Miao, X, and Hu, X. An investigation and analysis of the activities of daily living of older adults living at home in Ningxia Hui autonomous region of China: a cross-sectional study. BMC Geriatr. (2020) 20:369. doi: 10.1186/s12877-020-01765-8
42. Fuller-Thomson, E, and Gadalla, T. Income inequality and limitations in activities of daily living: a multilevel analysis of the 2003 American community survey. Public Health. (2008) 122:221–8. doi: 10.1016/j.puhe.2007.06.008
Keywords: cardiovascular-kidney-metabolic syndrome, disability, activities of daily living, diabetes, metabolic risk factors, chronic kidney diseases, cardiovascular diseases, CHARLS
Citation: Zhang J, Huang H, Lin Z, Dong J, Zhang X, Gao J, Liu Y, Li C and Cui Z (2025) Associations between cardiovascular-kidney-metabolic syndrome and disability in activities of daily living: a nationwide longitudinal study among the middle-aged and older adults in China. Front. Public Health. 12:1480576. doi: 10.3389/fpubh.2024.1480576
Received: 14 August 2024; Accepted: 30 December 2024;
Published: 15 January 2025.
Edited by:
Nai Peng Tey, University of Malaya, MalaysiaReviewed by:
Yuke Tien Fong, Singapore General Hospital, SingaporeCopyright © 2025 Zhang, Huang, Lin, Dong, Zhang, Gao, Liu, Li and Cui. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Changping Li, bGljaGFuZ3BpbmdAdG11LmVkdS5jbg==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.