
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 27 November 2024
Sec. Public Health Education and Promotion
Volume 12 - 2024 | https://doi.org/10.3389/fpubh.2024.1478592
 Kyaw Soe Thant1
Kyaw Soe Thant1 Aksara Thongprachum1*
Aksara Thongprachum1* Sineenart Chautrakarn1
Sineenart Chautrakarn1 Pannawich Chantaklang2
Pannawich Chantaklang2 Suwat Chariyalertsak1
Suwat Chariyalertsak1Introduction: Despite progress in controlling HIV/AIDS and STIs, these health challenges persist, with 39.9 million people living with HIV in 2023 and more than 350 million affected by STIs annually. Thailand is a major migrant hub in Southeast Asia. This study investigated the factors influencing preventive behaviors related to HIV/AIDS and STIs among Myanmar migrants in Chiang Mai province, Thailand.
Methods: A cross-sectional study was conducted in 2023 among 424 Myanmar migrants aged 18–45 years. Participants were selected through convenience sampling from a local hospital and community gathering locations in Chiang Mai province. Multiple logistic regression analysis was used to identify factors influencing preventive behaviors.
Results: The participants’ average age was 29.92 years; 56.8% were married, and 67.5% had completed primary or lower education. The average monthly income was <10,000 THB (47.6%). Most participants had a good knowledge level of HIV (63.2%), while 80% had poor knowledge of STIs. Among the sexually active participants (n = 274), 91.2% had good preventive behavior. The multivariate analysis indicated that migrants working in non-construction or day labor roles were less likely to practice preventive behaviors (aOR = 0.210, 95% CI: 0.046–0.972, p = 0.046). Additionally, migrants who had lived in Chiang Mai for more than 10 years were less likely to engage in preventive behaviors (aOR = 0.067, 95% CI: 0.010–0.465, p = 0.006). There was a statistically significant association between preventive behaviors and a positive attitude, with an aOR of 4.575 (95% CI: 1.226–17.073, p = 0.024).
Conclusion: Low STI knowledge and negative attitudes toward condom use were found in this study. Culturally relevant and sensitive interventions and effective sexual health education are needed.
Despite three decades of progress in managing human immunodeficiency virus (HIV), it remains a major global health challenge. By 2023, 39.9 million people were living with HIV (PLWHA) worldwide, approximately 630,000 deaths due to HIV-related causes and only 77% of PLWHA received antiretroviral therapy (1). Globally, the burden of sexually transmitted infections (STIs) is significant, with approximately 1 million infections daily from four curable STIs including syphilis (2). In Thailand, an estimated 560,000 people were living with HIV in 2023, with an incidence rate of 0.13 per 1,000 uninfected population (3). In addition, syphilis accounted for the highest number of STI cases by 2021 (4). In Chiang Mai province, the case rate of five common STI infections (Syphilis, Gonorrhea, Chlamydia, Chancroid, and Lymphogranuloma Venereum) was 69.6 per 100,000 population in 2021 (5).
World Health Organization (WHO) aims to end AIDS, viral hepatitis, and STIs by 2030 through coordinated strategies (2). Thailand’s National Strategy to End AIDS: 2017–2030 targets reducing new HIV cases to <1,000 annually, AIDS-related deaths to <4,000 annually, and decreasing discrimination based on HIV or gender by 90% (6). Key populations for the strategy include men who have sex with men, sex workers, people who inject drugs, prisoners, and migrant workers.
Thailand, a major migrant hub in South-East Asia (7), hosts 2,167,937 documented migrant workers as of 2022, primarily from Myanmar, Cambodia, and Laos People’s Democratic Republic (Laos PDR) where 60.9% from Myanmar (7). In Chiang Mai Province, there were 101,377 migrant workers in December 2022, with 99% from Myanmar (8). Migrants, though not categorized as a key population by WHO, are considered as vulnerable group for HIV/AIDS and STI infections (9). The increasing trend of transborder migration heightens the risk of spreading infectious diseases, with an observed increasing rate of HIV transmission in migrant populations worldwide (10). The prevalence rate of HIV among migrant workers in Thailand was 0.2% in 2020 (4). Among the 12 provinces in Thailand with higher migrant populations (4), Chiang Mai had the highest prevalence rate at 1.3%.
Risk factors for HIV/AIDS and syphilis among migrants include limited condom use, having multiple partners, lack of HIV/AIDS knowledge (9, 11–13), and having a sexual partner with an STI (14). Studies highlight reasons for inconsistent condom usage as limited knowledge and poor attitudes toward condoms among migrants (15–18). External migrants face unprotected sex risks due to low-income status, debt, homelessness, and limited access to medical care (19). Mobility increases their vulnerability to STIs (10) and health risks for migrants in terms of susceptibility to and dissemination, which are not unidirectional (20). Challenges in HIV/AIDS care for cross-country migrants include low levels of knowledge on condom use, limited access to testing and counseling services, stigma, and discrimination (21).
A 2011 nationwide hospital-based survey in Thailand revealed that migrant workers faced substantially higher relative risks for sexually transmitted infections, tuberculosis, and malaria compared to Thai workers (22). Existing studies on HIV/AIDS among migrants in Chiang Mai have predominantly focused on sub-populations such as sex workers, people living with HIV/AIDS, and cross-border youths, with limited studies on the general migrant population (17, 18). This study aims to address this gap by investigating knowledge, attitudes, and preventive behaviors related to HIV/AIDS and STI infections among general migrants in Chiang Mai province. This study’s findings could provide insights for public health professionals and policymakers in the region, informing targeted preventive activities against HIV/AIDS and STIs among migrants.
This cross-sectional study was conducted among Myanmar migrant workers in Chiang Mai province, Thailand from October to December 2023. The sample size was calculated for a single proportion of binomial outcomes in an infinite population, using a population proportion of 50%, a 5% level of estimation, and a 95% confidence interval, resulting a minimal sample size of 385. After adding a 10% incomplete data rate, a total of 424 participants were included in the study (23). Adult migrants aged 18 to 45 years, were recruited using convenience sampling from Nakornping Hospital and community gathering settings. The recruitment occurred at the migrant health screening site of Nakornping Hospital, where four trained research assistants, fluent in Tai-Yai and Myanmar, approached individuals seeking health services. To identify migrants, the research assistants conversed with attendees and used a brief screening process to confirm their migrant status. The inclusion criteria were as follows: participants had to be (1) adults aged 18 to 45 years, (2) currently residing in Chiang Mai for over 1 month, (3) fluent in Tai-Yai or Myanmar, and (4) willing to provide informed consent for participation in the survey. Data was collected in a gender-matched approach with participants who consented to the survey. After 6 weeks of recruitment at Nakornping Hospital, administrative changes reduced migrant visits and health screening days. Consequently, data collection was extended to community gathering places, such as monasteries, where Myanmar migrants frequently gather for social gatherings, ensuring that the recruitment remained focused on the target population. The study was approved by the research ethics committees of the Faculty of Public Health, Chiang Mai University (ET041/2023) and Nakornping Hospital (NKP no. 148/66).
The survey questionnaire used in the Prevention of HIV/AIDS among Migrant Workers in Thailand 2 program (PHAMIT-2) (24) was adjusted and developed in English. It was validated by three experts with extensive experience in the HIV/AIDS field and translated into Tai-Yai and Myanmar by native speakers. The overall index of item-objective congruence (IOC) was 0.86, indicating strong relevance of the items to the study objectives, as experts provided scores of 1, 0, and − 1 based on their opinions of relevance, neutrality, and irrelevance, respectively. The questionnaire consisted of six parts: (1) socio-demographic data; (2) HIV/AIDS knowledge questions, comprising seven items with responses of “Yes,” “No,” and “Do not Know.” A score of 1 was assigned for correct answers and 0 for incorrect or “Do not Know.” Knowledge levels were categorized as “Good” if the score was ≥4.82 (mean score), otherwise “Poor”; (3) STI knowledge was classified as “Good” if the score was ≥0.76 (mean score) out of 5, otherwise “Poor”; (4) six items on a Likert scale assessed attitudes toward HIV, while four items each assessed attitudes toward condom use and STIs. A total of 14 items on a Likert scale evaluated overall attitudes toward HIV/AIDS, condom use, and preventive behaviors, ranging from 5 (Strongly Agree) to 1 (Strongly Disagree), with negative items reverse-scored. Attitudes were categorized as “Good” if the score exceeded the mean in each domain. For the overall attitude assessment, a score above 51.28 out of 70 (mean score) was categorized as “Good,” otherwise as “Poor”; and (5) questions on sexual behaviors.
In this study, preventive behavior was measured by three criteria among participants who had sexual intercourse: not engaging with a non-regular partner, always using condoms with non-regular partners in the past 12 months, and consistently using condoms with sex workers in the past 6 months. Participants received a score of 1 for each criterion they met. Those with a score of 1 or higher were classified as “Preventive,” while those with a score below 1 were classified as “Un-preventive.” Data were collected through face-to-face interviews and recorded using the Kobo Collect application on smartphones/tablets. It was further tested among 30 Myanmar migrant workers in Chiang Mai Province, showing internal consistency with KR-20 of 0.777 for knowledge scores and Cronbach’s alpha of 0.713 for attitude scores.
Data analysis utilized SPSS version 26.0 (SPSS Inc., Chicago, IL, USA). Descriptive statistics (frequency, mean, median, and standard deviation) summarized sociodemographic factors, knowledge, attitudes, and preventive behaviors. Multiple logistic regression identified associations between these factors and preventive behaviors related to HIV/AIDS and STIs.
Table 1 shows the socio-demographic characteristics of 424 participants, 50% female and 50% male, with a mean age of 29.92 ± 7.9 years. In terms of marital status, 56.4% being married and 25.7% being single. A total of 38.7% had no formal education and 28.8% had primary education. Nearly 32% have been living in Chiang Mai for more than 10 years. More than 63% were construction workers or daily laborers. Nearly half of the participants (47.6%) had an average monthly income of <10,000 THB. The majority (85.8%) had personal identification (ID) status, such as a passport or work permit, allowing them to live and work legally in Chiang Mai Province and 69.8% had health insurance. Only 35.6% had a history of drinking alcohol in the last 3 months.
Table 2 presents participant’s knowledge, with 63.2% having “Good” HIV knowledge. The average score was 4.82 (SD = 1.63). Participants had a good level of transmission knowledge and more than 90% of participants correctly responded that HIV can be transmitted through blood transfusion. Regarding HIV prevention knowledge, only 64.2% of participants were aware that HIV can be prevented by condom use.
Only 20% of the participants had good STI knowledge with an average score of 0.76 (SD = 1.62). Twenty-three percent of the participants had ever heard of STI infections. Among them, 74.5% could name at least one type of STI and only 56.1% knew any STI symptoms.
Table 3 shows migrants’ attitudes toward HIV/AIDS, condom usage and STI infections. The overall mean attitude score was 51.28 (SD = 5.32) with 53.5% of the participants having an overall “Good” attitude. Attitude toward HIV/AIDS was good among participants as 66.5% had an above mean score of 24.25 (SD = 3.66). In contrast, 62.7% had poor attitudes toward condom usage, scoring below the mean of 12.41 (SD = 2.08). Regarding attitude toward STIs, 59.7% had a good attitude with a mean score of 14.61 (SD = 2.10).
The majority of the participants (64.6%) reported having had prior sexual experience, with males (75.5%) and females (53.8%). A total of 17.9% did not respond to this question, possibly due to its sensitive nature. Among those with prior sexual experience, 78.4% (n = 215) reported having a regular partner, and of these, 77.2% never used condoms with their regular partner.
Of the participants who had prior sexual exposure, 5.8% (n = 16) reported having a non-regular partner, with 50% of those having more than one non-regular partner in the last 12 months. Among those with non-regular partners, 43.8% (n = 7) reported always using condoms.
Additionally, only 1.5% (n = 4) of participants with prior sexual experience reported visiting sex workers in the last 6 months, and of these 75% (n = 3) always used condoms (see Supplementary Table 1 for detailed sexual behaviors).
From the total of 424 participants, 274 (64.4%) reported prior sexual experience. Among these, 91.2% reported preventive behaviors, scoring 1 or higher based on the criteria of: not engaging with a non-regular partner, consistently using condoms with non-regular partners in the past 12 months, and always using condoms with sex workers in the past 6 months. After excluding participants who did not respond to questions regarding health insurance status and monthly income, 262 participants were included in the final logistic regression model. Table 4 presents the findings from the multivariate analysis, indicating that migrants in non-construction or day labor roles were less likely to practice preventive behaviors compared to construction workers (aOR = 0.210, 95% CI: 0.046–0.972, p = 0.046). Additionally, migrants who had lived in Chiang Mai for more than 10 years were less likely to engage in preventive behaviors (aOR = 0.067, 95% CI: 0.010–0.465, p = 0.006). Furthermore, participants with a positive attitude toward HIV/AIDS were 4.5 times more likely to engage in preventive behaviors than those with a negative attitude (aOR = 4.575, 95% CI: 1.226–17.073, p = 0.024).
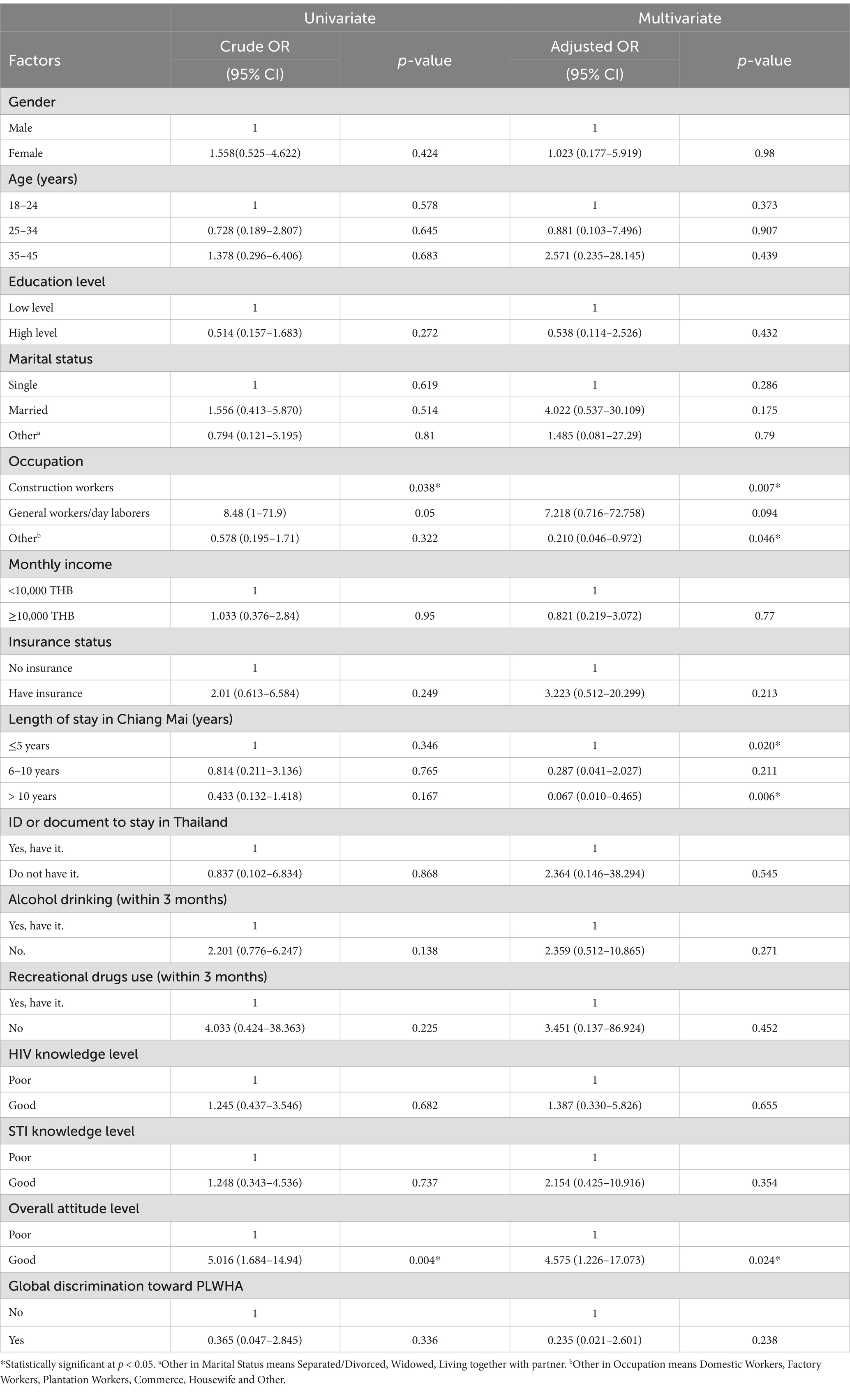
Table 4. Univariable and multivariable analysis of factors associated with the preventive behaviors (n = 262).
The cross-sectional study aimed to examine the factors influencing preventive behaviors related to HIV/AIDS and STIs among Myanmar migrants in Chiang Mai province. Despite a good level of HIV knowledge among participants, most migrants showed a poor level of STI knowledge and a negative attitude toward condom usage.
Participants demonstrated a good level of HIV knowledge (63.2%), particularly about transmission methods over prevention. Misunderstandings included that HIV/AIDS could be transmitted through sharing meals (58.7%) and unawareness that antiretroviral drugs prevent transmission during pregnancy (51.2%). These misconceptions can increase stigma and delay HIV care. Similar findings in prior studies among Myanmar migrants (12, 25, 26) revealed the ongoing need for accessible health education using simple language and visual aids. Despite good HIV knowledge, its correlation with preventive behaviors was weak, consistent with previous studies (12, 26), indicating the influence of social, cultural, and environmental factors on behaviors. This can be addressed by implementing community-based interventions that promote safe practices, reduce stigma, and create supportive environments for at-risk populations.
The majority (77%) reported limited awareness regarding STIs. This aligns with previous findings from a 2010 nationwide survey (24) and recent studies (12), indicating persistent gaps in STI knowledge. HIV/AIDS and other STI infections share a common mode of transmission and having a STI is the risk of getting HIV exposure (27). The observed discrepancy might be attributed to the disproportionate focus of public health campaigns on HIV, highlighting the need for comprehensive sexual health education that encompasses all aspects of STIs, not only HIV/AIDS. This can be addressed with community outreach programs that provide immediate access to comprehensive sexual health information and resources. Collaborating with local organizations, healthcare providers, and community leaders will help effectively reach at-risk populations. Long-term strategies should include integrating sexual health education into school curricula and providing age-appropriate information about STIs and safe practices to enhance awareness. Additionally, partnerships with NGOs and the use of digital platforms can promote the reach and impact of these initiatives.
Overall, 53.5% had a good attitude toward HIV/AIDS, STI infections, and condom usage, with better attitudes toward HIV/AIDS and STI infections than condom use. Nearly half of the participants felt embarrassed to buy condoms and believed that wearing condoms reduced sexual feelings. This is supported by the findings of poor attitudes toward condom use among Myanmar migrants in Surat Thani (15) and cross-border youth in Chiang Mai (18). In addition, only 64.2% correctly identified condom use as effective in HIV prevention, reflecting the variation in social and cultural norms, personal preferences, influence of peer and partner perceptions, and access to information. Those who had less access to information regarding the effectiveness of condoms, personal preference from partners, and social norms of carrying condoms seen as promiscuity would make them less likely to view condoms favorably. The discrepancy in attitudes toward HIV/AIDS, STI infections and condom usage shows the need for tailored education and awareness campaigns that address misconceptions about condom use.
Among 424 migrants, 64.6% reported sexual experience, with more males (75.5%) than females (53.8%). Condom use with regular partners was notably low (77.2% never used condoms), consistent with findings from previous studies showing 7% condom usage in Chiang Rai province (28) and 17% condom usage among migrant sex workers in Chiang Mai province (17). This could be explained by the perception of trust and intimacy leading individuals to be less likely to use condoms in emotionally close or long-term relationships. This lack of condoms used in presumed safe relationships might increase the risk of HIV/AIDS and STI infections especially when partners are unaware of each other’s HIV status or risk factors. To address this, promoting consistent condom use along with regular HIV testing should be emphasized among the sexually active community.
A total of 16 participants (5.8%) reported having non-regular partners in the past year, with 43.8% consistently using condoms. Additionally, 75% used condoms during their most recent encounter, and 50% reported having more than one non-regular partner in the last year. Compared to migrants in Ranong Province (66.7%) (29), condom usage was lower, while non-usage with non-regular partners was higher in Samut Sakhon Province (39.3%) and Patumthani Province (40.56%) (12, 25). This risky behavior favors the high risk of exposure to HIV and STI infections through associated occasional sexual partners. Targeted interventions for promoting condom use and enhancing condom accessibility are critical.
91.2% of participants engaged in preventive behaviors by not having non-regular partners and always using condoms with non-regular partners or sex workers. This finding reflects a study among Myanmar migrants in Samut Sakhon province, where 85.3% engaged in protective sexual behaviors (12). Multi-structural determinants such as policies, sociocultural challenges, health factors, and risky sexual behaviors influence HIV risk (9). Factors such as age, income, HIV/AIDS awareness, lifestyle, and sexual activities are significant, highlighting the complex environment for migrants (30).
A significant association was found between the duration of stay in Chiang Mai and migrants’ preventive behaviors. Migrants staying more than 10 years showed poorer preventive behavior compared to those staying for <5 years. Longer-term migrants might become desensitized to HIV/AIDS and STI risks or face barriers in accessing ongoing prevention and education services. This could be due to factors such as socio-economic integration and cultural assimilation. Prolonged stays in other countries correlate with poor preventive behavior, especially low condom usage (30, 31). This suggests the necessity for targeted interventions for long-term migrants.
The analysis revealed that migrants in the “other” occupational category, excluding construction workers and daily workers, were significantly less likely to engage in preventive behaviors compared to “construction workers,” with an adjusted OR of 0.210 (95%Cl: 0.046–0.972). Construction sites often function as closed communities that foster peer communication and experience sharing among workers, providing a platform to promote preventive behaviors. A study among Myanmar migrant workers in Ranong province (29) found that factory workers had safer sex behaviors compared to workers in other types of jobs. Occupational differences suggest that certain types of working environments or conditions may either facilitate or hinder the adoption of prevention measures. For instance, female migrant workers in China working at entertainment venues were more likely to engage in preventive behaviors than those working in factories and restaurants (11). These differences suggest the need for targeted HIV preventive interventions. These might include workplace education programs, improved access to condoms, HIV testing and initiatives addressing specific barriers to prevention in different occupation settings. Understanding factors related to lower engagement in preventive behaviors among migrant workers in specific occupations can inform the development of more effective and context-sensitive HIV/AIDS prevention activities.
Another influencing factor affecting preventive behaviors was their attitude. Participants with a good attitude were 4.5 times more likely to engage in preventive behaviors compared to those with a poor attitude. Belief in the effectiveness of prevention methods and confidence in one’s ability to use them are crucial for behavior change (32). Additionally, activities that increase migrants’ confidence, such as practical demonstrations on proper condom use and easy access to HIV testing, and counseling, will further encourage preventive behaviors.
The study findings show that migrants have low STI knowledge and poor attitudes toward condom use, with preventive behavior being particularly rare among those who have lived for over 10 years and work in non-construction jobs. To support the Sustainable Development Goals of eliminating HIV and STIs by 2030 (33), it is recommended to expand culturally sensitive, tailored health education programs, provide accessible HIV early testing services, and strengthen collaboration between governmental and non-governmental organizations to improve service delivery and reduce risk factors among migrants.
While previous research had identified socio-demographic factors such as gender and marital status (29, 31, 34), education level (17), and income-expense balance (12) as influencing factors on preventive behaviors among migrants, this study found no such association. This is consistent with findings from studies in Bangkok and the 2010 migrant survey, where gender, marital status (35, 36) and education level (36) were also not related to HIV preventive behaviors among migrant workers. Those could be explained by differences in demographic composition and socio-economic context of the study populations which might vary in behaviors and attitudes subsequently. Moreover, preventive behaviors might vary significantly across the different sub-populations of migrants, such as sex workers and migrants living with HIV, where the study population in this study was the general migrant population. The diversity within the migrant population likely contributes to the complexity of behaviors and determinants, and indicating the targeted interventions could be more effective.
Bias might arise from hospital-based data collection and self-reported information, potentially influenced by social desirability bias or recall issues. The convenience sampling method and the focus on Chiang Mai province limit generalizability to broader migrant populations and other regions. The cross-sectional study design could not draw causality conclusions from the analysis. A 17.9% non-response rate on sensitive behavior questions, particularly among certain demographics, introduces potential bias, possibly affecting the interpretation of preventive behaviors.
The study highlighted significant gaps in STI knowledge and attitudes toward condom usage among Myanmar migrants in Chiang Mai province, Thailand. Despite a reasonable level of HIV/AIDS knowledge, misconceptions about transmission and prevention persist, particularly regarding condom use and attitudes toward people living with HIV/AIDS.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The study was approved by the research Ethics Committees of the Faculty of Public Health, Chiang Mai University (ET041/2023) and Nakornping Hospital (NKP no. 148/66).
KT: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Visualization, Writing – original draft, Writing – review & editing. AT: Conceptualization, Formal analysis, Methodology, Resources, Supervision, Writing – review & editing. SiC: Conceptualization, Formal analysis, Methodology, Supervision, Writing – review & editing. PC: Project administration, Supervision, Validation, Writing – review & editing. SuC: Conceptualization, Methodology, Supervision, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
We are grateful to the Presidential Scholarship program, the directors of the Nakornping Hospital, and we thank all the migrants who participated in the study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1478592/full#supplementary-material
1. WHO. (2023). HIV and AIDS: World Health Organization. Available at: https://www.who.int/news-room/fact-sheets/detail/hiv-aids (Accessed September 14, 2024).
2. WHO. Global Health sector strategies on, respectively, HIV, viral hepatitis and sexually transmitted infections for the period 2022–2030: World Helath organization. Geneva: WHO (2022).
3. WHO. HIV country profile: Thailand: World Helath organization (2023). Available at: https://cfs.hivci.org/index.html (Accessed September 18, 2024).
4. Department of Disease Control MoPH. Annual Report of Division of AIDS and STIs. Nonthaburi: Department of Disease Control MoPH (2021).
5. HIV Info Hub. Rates of 5 major STIs by province: Division of AIDS and sexually transmitted diseases, department of disease control (2021) Available at: https://hivhub.ddc.moph.go.th/epidemic.php (Accessed May 5, 2024).
6. National AIDS Committee. Thailand National Strategy to end Aids 2017–2030. New Delhi: National AIDS Committee (2017).
7. ILO. Triangle in ASEAN quarterly briefing note: Thailand (July–September 2022). Geneva: ILO (2022).
8. Office of Foreign Workers Administration. Statistics on the number of foreign workers authorized work balance through out the kingdom for the month of December 2022. Washington, DC: Office of Foreign Workers Administration (2022).
9. Weine, SM, and Kashuba, AB. Labor migration and HIV risk: a systematic review of the literature. AIDS Behav. (2012) 16:1605–21. doi: 10.1007/s10461-012-0183-4
10. WHO. World report on the health of refugees and migrants. Geneva: World Health Organization (2022).
11. Huang, W, Dong, Y, Chen, L, Song, D, Wang, J, Tao, H, et al. HIV risk and sexual health among female migrants in China. Health Promot Int. (2016) 31:595–605. doi: 10.1093/heapro/dav049
12. Paloga, A, Arthan, D, Maneekan, P, Kitcharoen, P, Wattanapisit, A, Paratthakonkun, C, et al. HIV and syphilis knowledge, perceptions, and practices among Myanmar migrant Workers in Samut Sakhon Province, Thailand. BMC Public Health. (2022) 22:2206. doi: 10.1186/s12889-022-14674-9
13. Abdulkader, RS, Kant, S, Rai, SK, Goswami, K, and Misra, P. Prevalence and determinants of sexually transmitted infections (STIs) among male migrant factory Workers in Haryana, North India. Indian J Public Health. (2015) 59:30–6. doi: 10.4103/0019-557x.152854
14. Rasmi, A, Ratanalertnavee, J, and Reawrang, S. Prevalence and risk factors of HIV and syphilis infection among migrant Workers in Takuapa District, Phangnga Province. Dis Control J. (2019) 45:75–84.
15. Hounnaklang, N, Sarnkhaowkhom, C, and Bannatham, R. The beliefs and practices on sexual health and sexual transmitted infection prevention of Myanmar migrant Workers in Thailand. Open Public Health J. (2021) 14:294–9. doi: 10.2174/1874944502114010294
16. Baltazar, CS, Horth, R, Inguane, C, Sathane, I, César, F, Ricardo, H, et al. HIV prevalence and risk behaviors among Mozambicans working in south African mines. AIDS Behav. (2015) 19:S59–67. doi: 10.1007/s10461-014-0941-6
17. O’Connor, SY, Tangmunkongvorakul, A, Srithanaviboonchai, K, Sripan, P, Banwell, C, and Kelly, M. Association between sociodemographic factors and condom use among migrant sex Workers in Chiang Mai, northern Thailand. Int J Environ Res Public Health. (2022) 16:9830. doi: 10.3390/ijerph19169830
18. Manoyos, V, Tangmunkongvorakul, A, Srithanaviboonchai, K, Yangyuenkul, S, and Grimes, RM. Sexual risk behaviors for HIV infections among Young cross-border migrant workers living in urban Chiang Mai, Thailand. J. Health Res. (2016) 30:47. doi: 10.14456/jhr.2016.47
19. El-Bassel, N, Gilbert, L, Shaw, SA, Mergenova, G, Terlikbayeva, A, Primbetova, S, et al. The silk road project: how mobility and migration status influence HIV risks among male migrant Workers in Central Asia. PLoS One. (2016) 11:e0151278. doi: 10.1371/journal.pone.0151278
20. Abbas, M, Aloudat, T, Bartolomei, J, Carballo, M, Durieux-Paillard, S, Gabus, L, et al. Migrant and refugee populations: a public health and policy perspective on a continuing global crisis. Antimicrob Resist Infect Control. (2018) 7:1–11. doi: 10.1186/s13756-018-0403-4
21. Suphanchaimat, R, Sommanustweechai, A, Khitdee, C, Thaichinda, C, Kantamaturapoj, K, Leelahavarong, P, et al. HIV/AIDS health care challenges for cross-country migrants in low- and middle-income countries: a scoping review. HIV/AIDS Res. Palliative Care. (2014) 6:19–38. doi: 10.2147/HIV.S56277
22. Rakprasit, J, Nakamura, K, and Seino, K. Morita a. healthcare use for communicable diseases among migrant workers in comparison with Thai workers. Ind Health. (2017) 55:67–75. doi: 10.2486/indhealth.2016-0107
23. Dhand, N, and Khatkar, M. (2014). Statulator: An Online Statistical Calculator. Available at: https://statulator.com/SampleSize/ss1P.html (Accessed June 1, 2023).
24. Chamratrithirong, A. Prevention of HIV/AIDS among migrant Workers in Thailand 2 [PHAMIT 2]: The baseline survey 2010: Institute for Population and Social Research, under Mahidol University. Salaya: Mahidol University (2012).
25. Rakkapao, N, Kiattisaksiri, P, and Samakkekarom, R. Knowledge, attitudes, and HIV/AIDS risk behaviors of Myanmar migrant Workers in Thailand. Global Health Manage J. (2019) 3:84–94. doi: 10.35898/ghmj-33452
26. Aung, HP, and Panza, A. Factors influencing sexual behaviors among Young Myanmar migrant Workers in Samut Sakhon, Thailand. J Health Res. (2016) 30:66. doi: 10.14456/jhr.2016.66
27. WHO. Consolidated guidelines on HIV, viral hepatitis and STI prevention, diagnosis, treatment and Care for key Populations: World Health Organization. Geneva: WHO (2022).
28. Aung, H, and Perngparn, U. Substance use and HIV-related sexual risk behaviors among Myanmar migrant Workers in Mae Sai, Chiang Rai Province, Thailand. J Health Res. (2014) 28:1–12.
29. Aung, YN, and Pongpanich, S. Living and working environment, and factors associated with the safe sex behavior and Sexuallly transmitted infection of Myanmar migrant Workers in Muang District, Ranong Province, Thailand. Bangkok: Chulalongkorn University (2010).
30. Behera, MR, and Intarak, R. HIV risk among labor migrants: an in-depth study of the literature. Indian J Pub Health Res Dev. (2018) 9:107–15. doi: 10.5958/0976-5506.2018.01816.8
31. Ford, K, and Chamrathrithirong, A. Sexual partners and condom use of migrant Workers in Thailand. AIDS Behav. (2007) 11:905–14. doi: 10.1007/s10461-007-9207-x
32. Rosenstock, IM. The health belief model and preventive health behavior. Health Educ Monogr. (1974) 2:354–86. doi: 10.1177/109019817400200405
33. WHO. (2023). SDG target 3.3 communicable diseases: WHO. Available at: https://www.who.int/data/gho/data/themes/topics/sdg-target-3_3-communicable-diseases (Accessed September 16, 2023).
34. Pan, X, Zhu, Y, Wang, Q, Zheng, H, Chen, X, Su, J, et al. Prevalence of HIV, syphilis, HCV and their high risk behaviors among migrant Workers in Eastern China. PLoS One. (2013) 8:e57258. doi: 10.1371/journal.pone.0057258
35. Ford, K, Chamratrithirong, A, Apipornchaisakul, K, Panichapak, P, and Pinyosinwat, T. Social integration, AIDS knowledge and factors related to HIV prevention among migrant Workers in Thailand. AIDS Behav. (2014) 18:390–7. doi: 10.1007/s10461-013-0410-7
Keywords: Myanmar migrant, HIV/AIDS, preventive behaviors, STI, Thailand
Citation: Thant KS, Thongprachum A, Chautrakarn S, Chantaklang P and Chariyalertsak S (2024) Knowledge, attitude, and preventive behaviors related to HIV/AIDS and sexually transmitted infections among Myanmar migrants in Chiang Mai province, Thailand. Front. Public Health. 12:1478592. doi: 10.3389/fpubh.2024.1478592
Received: 10 August 2024; Accepted: 13 November 2024;
Published: 27 November 2024.
Edited by:
Nyi Nyi Naing, Sultan Zainal Abidin University, MalaysiaReviewed by:
Alexandra M. Bitty-Anderson, African Research Center in Epidemiology and Public Health (CARESP), TogoCopyright © 2024 Thant, Thongprachum, Chautrakarn, Chantaklang and Chariyalertsak. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Aksara Thongprachum, YWtzYXJhLnRAY211LmFjLnRo
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.