- 1Faculty of Public Health, Al Quds University, Jerusalem, Palestine
- 2Faculty of Health Professions, Al Quds University, Jerusalem, Palestine
- 3Faculty of Medicine, Al Quds University, Jerusalem, Palestine
Introduction: During times of conflict, healthcare personnel face a heightened vulnerability to experiencing psychological problems such as burnout. The impact of conflict or wars on mental health professionals in Palestine and their strategies for managing these problems are currently not recognized. This study sought to assess the prevalence of burnout symptoms and coping strategies among healthcare workers in Palestine, in the context of the ongoing conflict and political violence.
Methods: The study utilized a cross-sectional research design. Self-reported questionnaires, including the shortened version (9 items) of The Maslach Burnout Questionnaire and Brief COPE scales, were used to gather data. The relationship between the research variables and burn symptoms was investigated using Chi-squared test, Student’s t-test, Mann–Whitney, and Analysis of variance and multi-regression.
Results: A total of 713 participants were recruited. The prevalence rates were as follows: burnout—(72.9%), emotional exhaustion (44.2%), depersonalization (9.8%), and low personal accomplishment (72.2%). The multivariate analysis found that those who worked more than 16 h per day and those who had 1–15 years of job experience were more likely to had emotional exhaustion. Active coping, substance use, informational support, and emotional support all reduced the likelihood of burnout while behavioral disengagement and self-blame increased the possibility of experiencing burnout. Finally, substance use decreased emotional exhaustion, increased depersonalization and enhanced personal accomplishment.
Conclusion: The findings revealed a high prevalence of burnout among health professionals during wartime and political violence. As a result, health professionals are vulnerable to mental problems during political violence and they need immediate assistance in enhancing their mental wellbeing through psychological support, and comprehensive training in stress management.
Introduction
War is a condition of armed enmity and violence between or within countries (1). The occurrence causes widespread destruction, massive human fatalities, and population displacement (2). Also, war has a significant impact on health, damaging the physical and mental well-being of persons living in war zones (3). Health services are frequently disrupted, resulting in a scarcity of medical supplies and healthcare personnel. Healthcare personnel, including physicians, nurses, pharmacists, and anesthetists, confront substantial challenges such as working in dangerous conditions, managing a large number of patients, and dealing with personal bereavement and emotional distress (4). Additionally, the destruction of healthcare infrastructure, such as hospitals and clinics, impairs the ability to provide adequate medical care (5). Furthermore, healthcare professionals frequently experience significant levels of stress and burnout, which are exacerbated by the ongoing threat to their safety and the excessive demand for medical services (6, 7).
Burnout is particularly prevalent in demanding professions like healthcare (8). Burnout is characterized by three distinct aspects: emotional exhaustion (EE), depersonalization (DP), and a decreased sense of personal accomplishment (PA) (9). It can arise from factors such as an overwhelming workload, a lack of control, inadequate incentives, a sense of isolation, a lack of justice, or conflicting values (10). Wars exacerbate these characteristics by causing extreme working conditions, prolonged stress, and traumatic events, all of which lead to occupational burnout among healthcare professionals (7, 11). Research has found that burnout rates among healthcare staff have reached critical levels, especially in areas experiencing ongoing violence (12, 13). Healthcare staff in Syria, Ukraine, and Libya experience significant emotional exhaustion and depersonalization due to the high number of victims and constant threats to their lives (12, 14). For example, a cross-sectional study done during the war in Ukraine indicated that emotional exhaustion (EE) and depersonalization (DP) were present in 31.6 and 33.4% of physicians, respectively, and in 17.9 and 18.2% of nurses (15).
The strategies employed by healthcare workers to manage stress might influence their vulnerability to burnout (16). Coping strategies are typically classified as problem-focused, emotion-focused, and avoidance-focused techniques (17). Problem-focused coping entails addressing the issue directly to minimize stress. Emotion-focused coping is the process of controlling emotions that develop as a result of a stressful circumstance (18). Avoidance-focused coping involves avoiding or distancing oneself from the situation (19). Research shows that problem-focused and emotion-focused coping are more successful in reducing burnout than avoidance-focused coping. For example, healthcare personnel who engage in regular physical exercise and seek social support had reduced rates of burnout (20).
In Palestine, the Israeli military has occupied the West Bank and Gaza Strip since 1967. Israel unilaterally withdrew all of its armed forces and settlers from the Gaza Strip in 2005. The Palestinian Ministry of Health (MOH), UNRWA, NGOs, and the private sector are all involved in the administration of healthcare services in Palestine, which also include primary, secondary, and tertiary levels (21). There are a total of 743 primary healthcare centers in Palestine, with 583 located in the West Bank and 160 in Gaza. The Palestinian National Institute of Public Health manages 81 hospitals, with 51 in the West Bank (including East Jerusalem) and 30 in Gaza (22). The continuous political violence in Palestine, especially after October 7, 2023, has had a significant impact on the health status in Palestine (23). The healthcare system encounters several obstacles, such as scarcity of medical resources, impaired infrastructure, and restricted availability of healthcare services (23). Healthcare professionals work under persistent danger, intensifying their stress levels and increasing the likelihood of experiencing burnout (24). For example, in the West Bank, 286 assaults on healthcare have impeded the delivery of care, including the distribution of vital pharmaceuticals and equipment, hospital closures, and denial of ambulance access (25).
This prevailing political instability and recurrent episodes of violence have engendered a dangerous environment for both patients and healthcare professionals. The difficulties in delivering and accessing healthcare services are made even more complex by restricted mobility, limited resources, and persistent security concerns (26). Nevertheless, there is a lack of research that explicitly focuses on work burnout in the Palestinian healthcare system during periods of political conflict (27). Only a few studies have been conducted among health professionals, and none have specifically focused on the current war period or examined coping strategies (28, 29). This research aimed to examine burnout and coping strategies among healthcare workers in the West Bank who provided medical care to Palestinians during the political crisis that started on October 7, 2023. Also, the study aimed to assess the relationship between burnout, coping strategies, and sociodemographic factors. Finally, the study looked at the factors that might predict the development of burnout symptoms among healthcare professionals.
Methods
Study design and sampling
The study was a descriptive cross-sectional survey that ran from 15 January 2024 to 1 February 2024. An online sample size calculator1 determined a sample size of 587, with a 5% margin of error and a 95% confidence interval, supposing that 50% of healthcare teams experience burnout. The study targeted all Palestinian health professionals currently working in the West Bank and Jerusalem during the ongoing Gaza war and political violence, including doctors, nurses, pharmacists, and allied professionals (e.g., anesthetics technicians, X-ray technicians, and medical laboratory). Health professionals in Gaza were unable to fill out the questionnaire because of the catastrophic war conditions, ongoing displacement, and restricted Internet access. Participants were chosen using convenience and snowball sampling methods. Data were gathered using an anonymous online self-administered survey. In response to Israeli military restrictions on mobility and closures in the West Bank and Jerusalem, participants were asked to complete an electronic version of the questionnaire, designed using Google Forms. The study link was distributed to participants via a variety of channels, including social media, WhatsApp, emails, and work-related organization websites. Furthermore, participants were asked to share the link with mental health practitioners throughout the country, and 713 from Jerusalem and the West Bank responded.
Tools and measures
The study used a self-reported questionnaire, which had the following three sections:
Section one included a socio-demographic sheet to collect information related to the participants’ age, gender, living place, marital status, occupation, work place, education level, monthly income, governorate (north governorate included Nablus, Jenin, Qalqilia, Tulkarim, Tubas, and Salfeet, middle governorate included Ramallah, East Jerusalem, and Jericho, and south governorate included Hebron and Bethlehem), years of experience and working hours per day.
The second section had the shortened version of the Maslach Burnout Questionnaire (9) which comprises 9 items that evaluate three subscales: personal accomplishment (PA) (3 items), depersonalization (DP) (3 items), and emotional exhaustion (EE) (3 items). The score of each subscale could range from minimum 0 to maximum 18. High score of EE and DP and a lower score of PA indicates a higher level of burnout. For EE and DP, subscale score of 0–9 was categorized as “no to low burnout” and subscale score of 10–18 was regarded as “moderate to severe burnout.” It was the opposite for PA because higher PA scores indicate lesser burnout. A seven-point Likert scale, with 0 representing “Never” and 6 representing “Every day,” can be used to answer questions.
Validated burnout thresholds for the a-MBI were employed (>6 for depersonalization, >9 for emotional exhaustion, and < 9 for personal achievement). In accordance with prior research, participants were classified as experiencing burnout if they exceeded the established threshold scores in either the depersonalization or emotional exhaustion domains (30, 31). Depersonalization and emotional exhaustion subscales had respective Cronbach’s alphas of 0.82 and 0.77 and Personal accomplishment 0.71.
The third section had the Brief COPE scale which was developed by Carver (32) and consisted of 28 questions. Both cognitive and behavioral strategies of coping are included and for each category, respondents indicate whether they have used a coping response on a four-point Likert scale (1 = I have not been doing this at all, 2 = I have been doing this a little bit; 3 = I have been doing this an average amount; 4 = I have been doing this a lot) and the higher score represents greater coping strategies used by the respondents. The Brief COPE scale assesses the following coping mechanisms: self-distraction, active coping, denial, substance use, emotional support, instrumental support, behavioral disengagement, venting, positive reframing, planning, humor, acceptance, religion, and self-blame. The internal consistency coefficient (Cronbach’s α) was 0.850.
The survey was translated into Arabic and back into English. The Arabic terminology was piloted by 20 health professionals and reviewed by five experts to verify accuracy and understandability.
Data analysis
The data were analyzed using SPSS version 25 (IBM Corp., Chicago, Illinois, USA). A descriptive analysis was performed using the means and the standard deviations for the quantitative variables, and frequencies and percentages for the categorical variables. Chi-squared test, Student’s t-test, Mann–Whitney, and Analysis of variance were used to analyze the relationships between the sociodemographic, occupational, work condition, coping strategies, and MBI dimensions. Statistically significant variables were further analyzed with multivariate logistic regression. A p < 0.05 was considered sufficient for statistical significance. Adjusted odds ratio and 95% confidence interval were also reported.
Ethical approval and consent to participate
The Declaration of Helsinki was followed in the implementation of all study methods. Al Quds University Research Ethical Committee approval was obtained (Ref No: 347/REC/2023). There was anonymity in this online survey. At the outset of the survey, written information was given regarding its goal and the intended use of the data. By completing the questionnaire, the participants gave their informed consent to take part in the research.
Results
Study participant’s socio-demographic characteristics
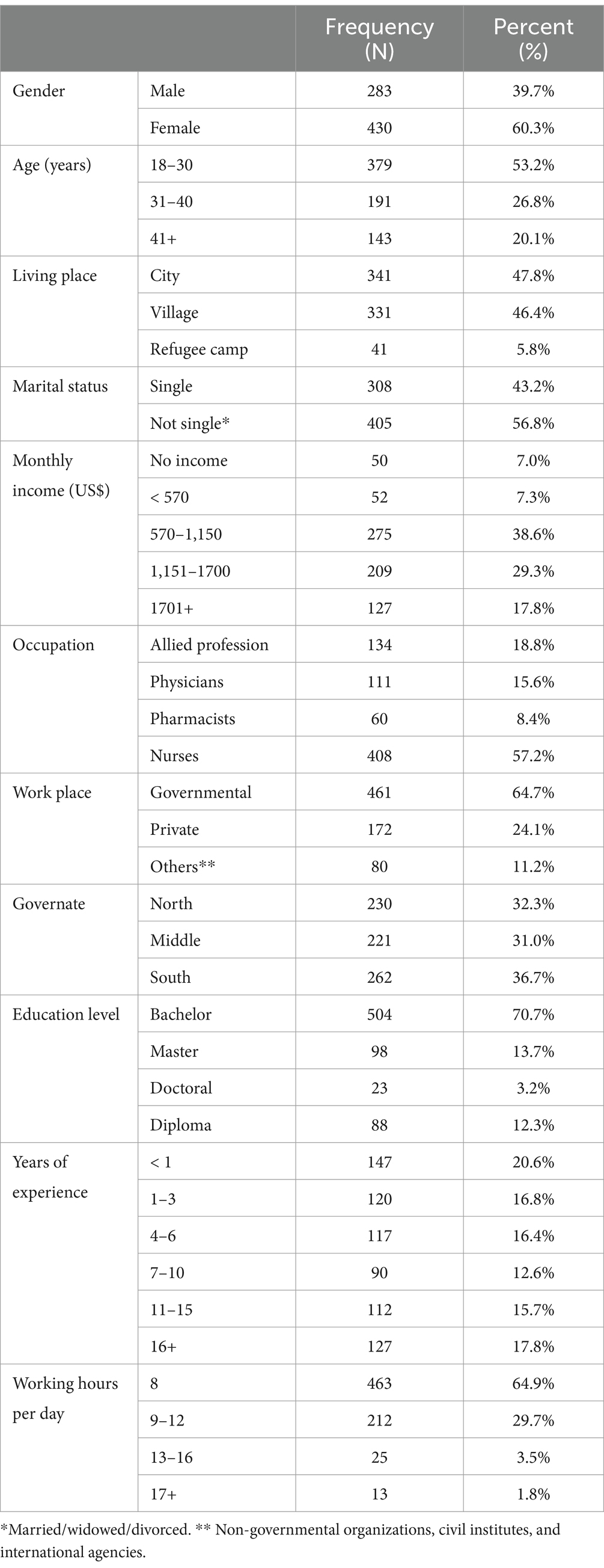
The sample included 713 healthcare professionals, 60.3% of whom were female. 53.2% were aged 18–30, 43% were unmarried, and 47.3% earned more than $1,150 every month. Nursing accounted for 57.2% of participants, with 64.7% working in government hospitals and primary care centers. Additionally, 70% had a bachelor’s degree, 46.1% had been working in their present position for more than 6 years, and 64.9% worked an eight-hour shift daily as seen in Table 1.
Prevalence of burnout
The overall burnout mean was 22.47 (SD 8.65), with a median of 22 (25th percentile = 17, 75th percentile = 28). Thus, 24% had a score less than 17 (n = 171), 3.1% had a score between 18 and 28 (n = 22), and 72.9% had a high score more than 28 (n = 713). According to the burnout subscale analysis, the prevalence of emotional exhaustion in the sample was 44.2% (n = 315), 9.8% (n = 70) for depersonalization, and 72.2% (n = 515) had poor personal accomplishment. For nurses, 40.9% had emotional exhaustion, 9.8% had depersonalization and 71.8% had poor personal accomplishment. For physicians, 56.8% had emotional exhaustion, 10.8% had depersonalization and 78.4% % had poor personal accomplishment.
Coping strategies subscale
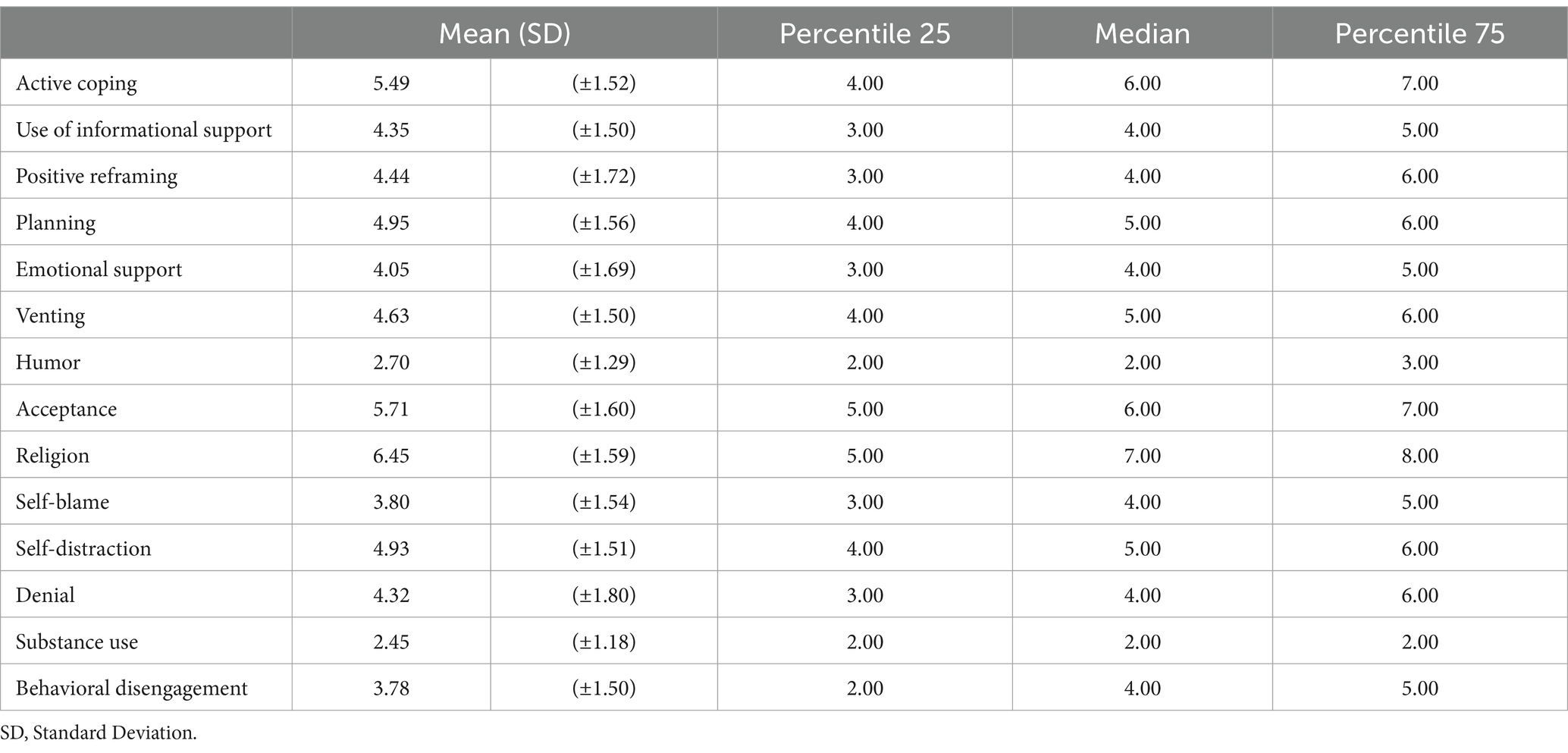
Table 2 shows the description of the coping strategies subscale. Religion showed the highest mean 6.45 (SD ± 1.59) and the highest 75th percentile (8) and substance abuse showed the lowest mean 2.45 (SD ±1.18) and the lowest 75th percentile (2).
Association between burnout subscale and participant’s socio-demographic characteristics
Subgroup analysis was conducted to explore the burnout level in different socio-demographics (Table 3). The findings showed that emotional exhaustion subscale was significantly associated with participants’ age (p = 0.005), monthly income (p = 0.023), education level (p = 0.002), occupation (p = 0.004), years of experience (p < 0.001), and the number of daily working hours (p = 0.002). Also, depersonalization subscale was associated with participants’ gender (p = 0.009), age (p < 0.001), marital status (p = 0.003), monthly income (p = 0.035), place of work (p = 0.048), the number of years of experience (p = 0.001), and the number of daily working hours (p = 0.009). In addition, personal accomplishment subscale was associated with participants’ gender (p = 0.022), education level (p = 0.003), monthly income (p = 0.030), marital status (p = 0.015), place of work (p = 0.026), and the number of years of experience (p < 0.001).
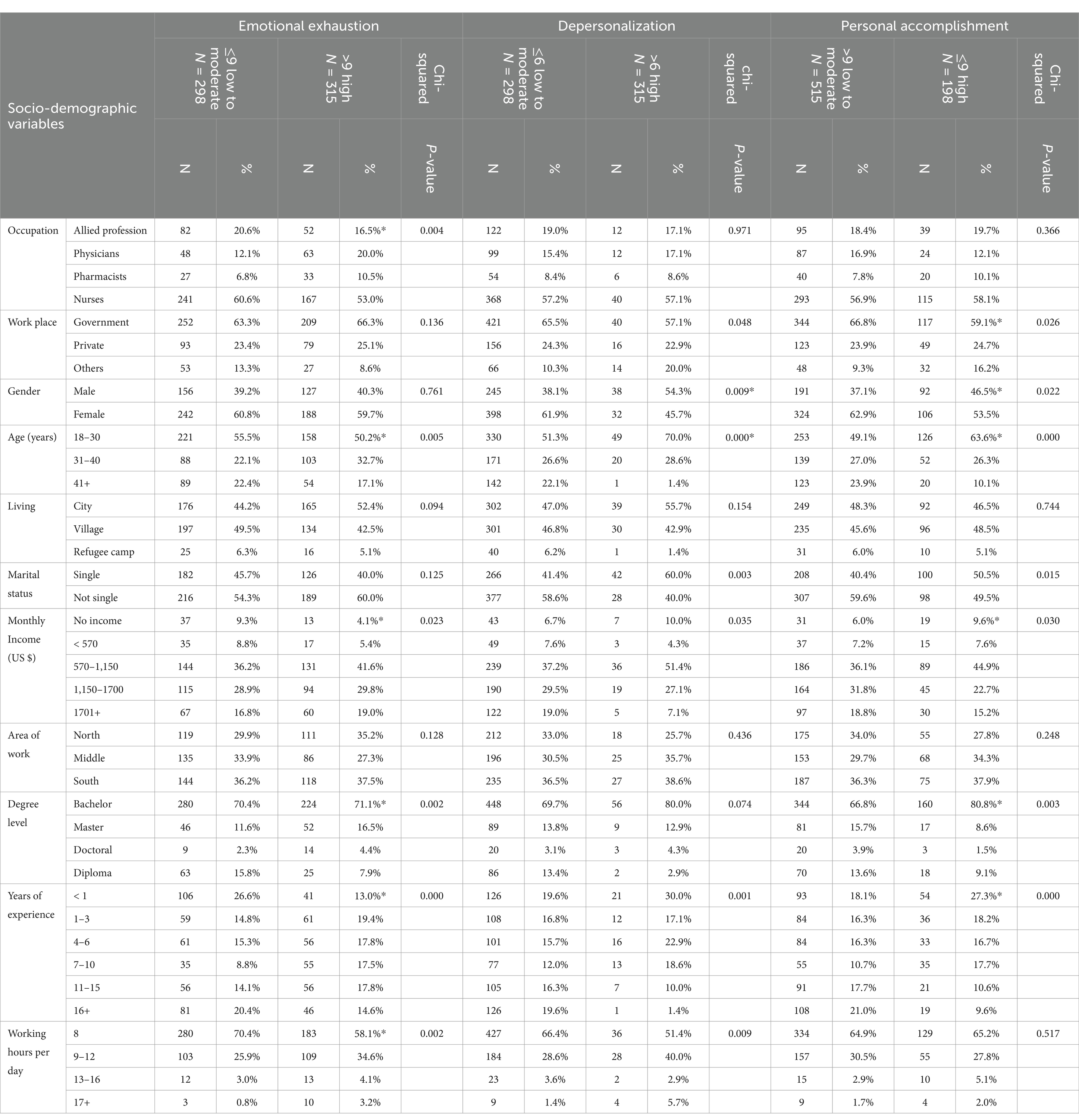
Table 3. Associations between socio-demographic, occupation, and work condition variables and Burnout symptom level (N = 715).
Burnout and coping strategies
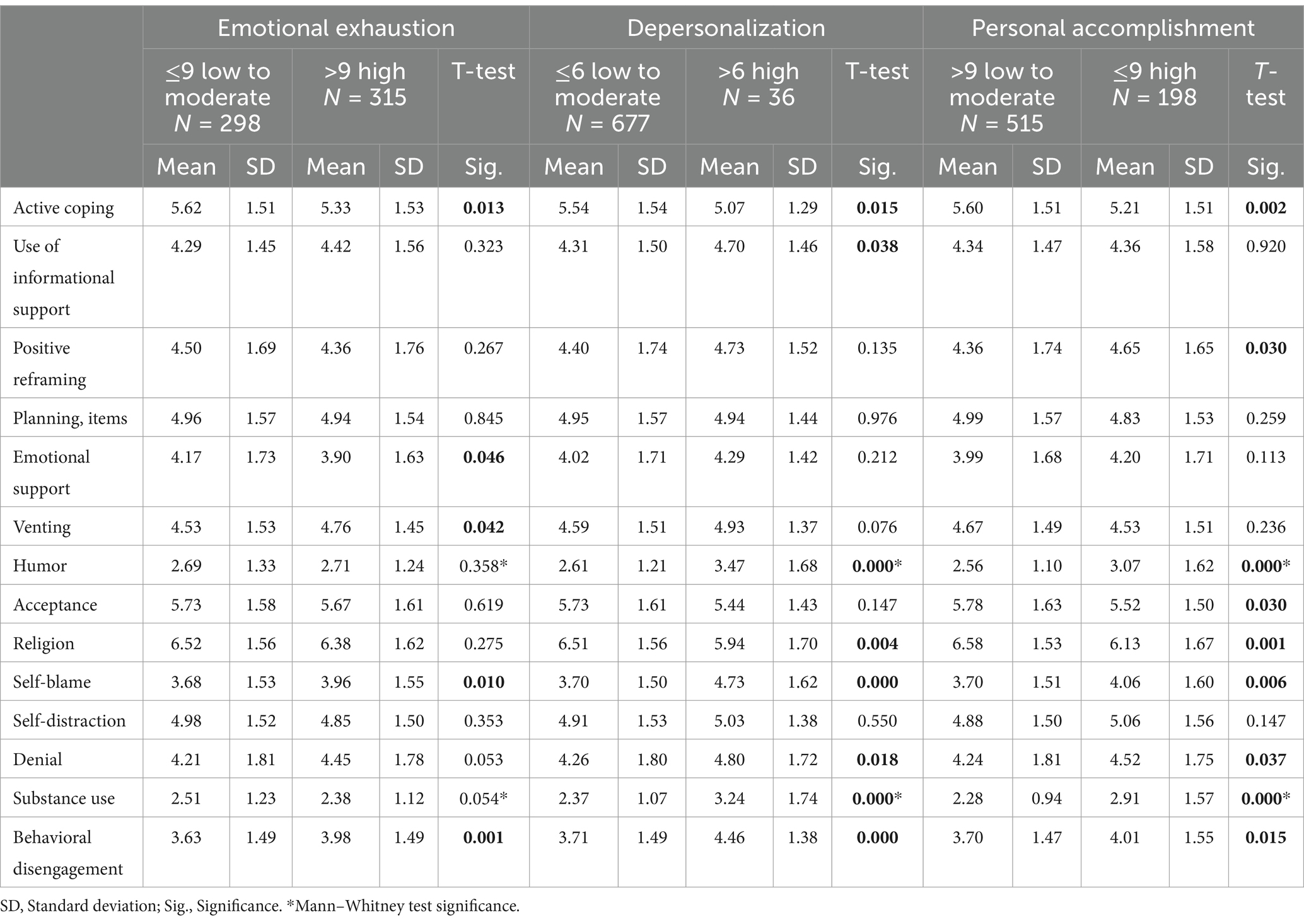
Subgroup analysis was conducted to explore the burnout level in different coping strategies (Table 4). Emotional Exhaustion subscale was significantly associated with active coping (p = 0.013), emotional support (p = 0.046), venting (p = 0.042), self-blame (p = 0.10), and behavioral disengagement (p = 0.001). Also, depersonalization subscale was significantly associated with active coping (p = 0.015), humor (p = <0.001), religion (p = 0.004), self-blame (p = 0.001), denial (p = 0.018), substance use (p = <0.001), and behavioral disengagement (p = <0.001). In addition, the personal accomplishment subscale was significantly associated with active coping (p = 0.002), positive reframing (0.03), humor (<0.001), self-blame (0.006), acceptance (0.03), religion (0.001), denial (0.037), substance use (<0.001), and behavioral disengagement (0.015).
Multivariate logistic regression model
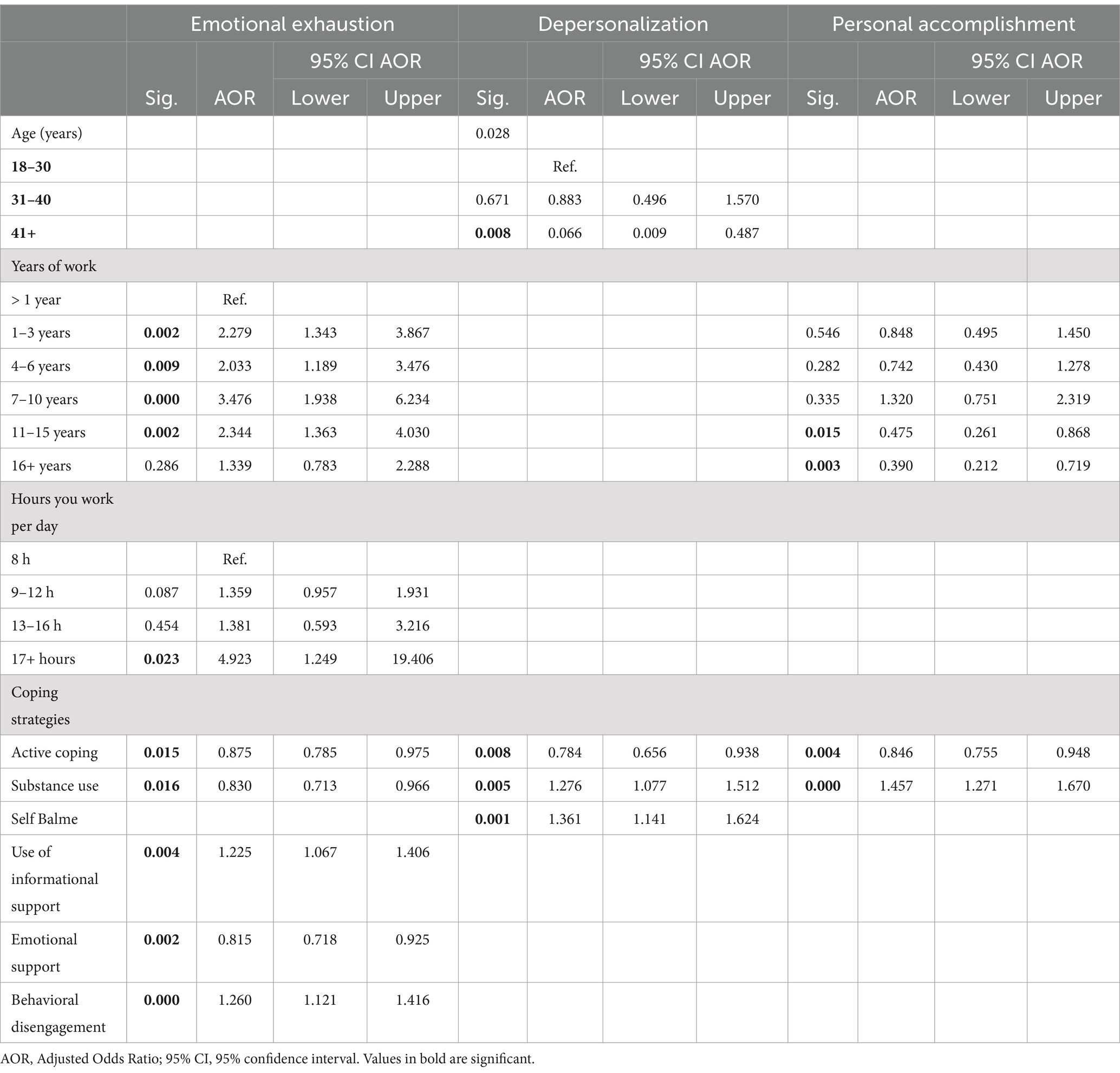
Multivariate analysis supported some of the previously stated findings. The results revealed that increasing participants’ years of experience, working hours per day, and usage of behavioral disengagement increased the likelihood of emotional exhaustion (AOR = 1.26, 95% CI = 1.21–1.461). Additionally, active coping, substance use, informational support, and emotional support reduced the likelihood of experiencing emotional exhaustion. Furthermore, active coping reduced the probability of experiencing depersonalization (AOR = 0.745, 95% CI = 0.656–0.938), but substance use and self-blame increased the likelihood of having it. Furthermore, increasing the number of experience years and using active coping reduced the likelihood of having personal accomplishment (AOR = 0.846, 95%CI = 0.755–0.948), whereas substance use increased the odds of having it (AOR = 1.457, 95%CI = 1.271–1.670) (Table 5).
Discussion
The mental health of health professionals is a critical problem because they are in charge of delivering long-term care to the people. The current study found that more than two-thirds of Palestinian health professionals (72.9%) experienced burnout, 44.2% had emotional exhaustion, 9.8% had depersonalization, and 72.2% experienced low personal accomplishment. Burnout findings are considered high when compared to other research in the literature review. Hamdan and Hamra (28) conducted study in the West Bank and Gaza to assess burnout levels among healthcare professionals (nurses, physicians, and administrative staff) in hospital emergency rooms during non-war periods, it was found that among emergency department staff, 64.0% experienced significant emotional exhaustion, 38.1% experienced depersonalization, and 34.6% had poor personal achievement (28). In Uganda, Kabunga et al. reported that 39.8% of respondents had significant levels of burnout in none war-times (33). In Indonesia, one research in none war-times revealed that 15.5% had emotional exhaustion (EE), 5.2% had depersonalization (DP), and 39.2% had personal accomplishment (34). In a cross-sectional research in Ukraine in war-times, EE and DP were found in 31.6 and 33.4% of physicians, respectively, as well as 17.9 and 18.2% of nurses (15). Another study found that 67% of Polish physicians suffered from burnout in non-war times (35).
Other research, on the other hand, found high level of burnout similar to the current study. According to one systematic review, the prevalence of high burnout varied from 0.9 to 40%, high emotional exhaustion from 0 to 49.7%, depersonalization from 0 to 59.6%, and low personal accomplishment from 0 to 60% (36). According to Alhaffar et al.’s study, during the Syrian conflict, 77.9 and 54.6% of physicians reported significant levels of EE and DP (14) and Elhadi et al. found that 67.1% of Libyan physicians had high EE and 47.4% had high DP after civil war (12). These findings may indicate that political conflict and wars raise burnout level among health professionals. Therefore, paying attention to their needs and their psychological status is very crucial in wartime.
The findings of the current study revealed several factors that may lead to an increase in burnout among Palestinian health professionals. The study found that those who worked more than 16 h per day and health professionals with 7–10 years of work experience were at the greatest risk of developing emotional exhaustion, followed by those with 1–3 years of experience. Also, those with 4–6 years of experience were at a higher risk of emotional exhaustion than health professionals with less than 1 year of experience.
These findings are supported by other studies in the literature review (37–39). Long years of employment can be related to people gradually taking on increasingly major responsibilities, which causes increased stress. Furthermore, professionals may use fewer coping strategies at work and experience chronic fatigue as a result of repeatedly experiencing the same issues day after day for a long period (40). In Palestine, with the start of the continuing battle in Gaza on October 7th, the majority of Palestinian hospital facilities declared an emergency. They directed all healthcare staff to postpone their holidays and return to work to meet the urgent situation. Also, due to the Israeli military’s blockade of Palestinian cities and implementation of mobility restrictions in the West Bank, a large number of these healthcare professionals were asked to remain at their jobs to solve the staffing shortage. As a result, health professionals who work long hours and have prolonged careers are more prone to develop emotional exhaustion in conflict situations. Long working hours are an indication of concern since they can lead to the onset of medical problems. A high level of burnout can lead to stress-related diseases and mental problems such as depression, anxiety, and low self-esteem. It can also lead to an increase in the occurrence of physical health issues such as sleep disruptions, migraines, cardiovascular disease, and other diseases (41).
On the other hand, our study found that professionals with more than a decade of work experience were more likely to have personal accomplishments and less likely to experience burnout than those with less than a year of experience. Work experience can be linked to workers’ capacity and autonomy in shaping their responsibilities positively. Employees who deliberately created a productive and stimulating work environment for themselves reported an increase in psychological resources such as hope, resilience, self-efficacy, and optimism, as well as improved job satisfaction (42). Habibisaravi et al. found that working professionals with extensive work experience showed stronger resilience and were capable of efficiently balancing their personal lives with their professional obligations lowering their burnout levels (43). Thus, our findings highlight the need for early screening for mental and physical health problems, such as cardiovascular disease, among healthcare professionals. Additionally, it emphasizes the need to limit working hours to a maximum of 40 per week.
Furthermore, the current study found that Palestinian health professionals used several coping strategies to minimize burnout. Active coping, substance use, informational support, and emotional support all decreased the probability of experiencing emotional exhaustion. Furthermore, active coping decreased the likelihood of developing depersonalization, but substance use increased personal accomplishment. Other research revealed similar findings. Menaldi et al. found that active coping, instrumental support, and substance use reduced the likelihood of experiencing EE (34). Doolittle and Windish showed that active coping was highly related to decreased emotional exhaustion and depersonalization. Problem-focused coping strategies, such as active coping and informational support, are active attempts to deal with a stressful situation by engaging in problem-solving activities to modify the situation or explore alternatives (44). Positive emotional coping strategies, such as emotional support, involve demonstrating compassion and understanding to oneself while attempting to address a problem independently, regardless of the outcome. These strategies also include making cognitive modifications that help produce positive feelings and enhance a sense of calmness in difficult circumstances, hence reducing EE and depersonalization (45). Furthermore, our data indicated that active coping had a negative relationship with personal accomplishment. According to Doolittle and Windish et al., personal accomplishment refers to the things that support and add value to the everyday tasks of patient care, therefore influencing one’s achievement. However, using active coping strategies alone may not be enough to alleviate the severe physical demands and reflexive dehumanization that come with all of the complicated aspects of patient care in challenging circumstances in areas of conflict (44).
Interestingly, our research indicated that substance use decreased EE and enhanced personal accomplishment. Avoidant coping strategies, such as substance use, are not necessarily maladaptive and can have different impacts depending on the level of stress (46, 47). Cecil et al. revealed a substantial negative relationship between burnout syndrome and alcohol use. They proposed that the frequency of alcohol intake in individuals might be more strongly related to the joy of drinking and socializing, lowering their level of burnout and EE and improving their relationships with others and their patients (48). Thus, substance use may boost professionals’ confidence and belief in their capacity to manage difficult situations, resulting in a more favorable appraisal of their accomplishments and personal fulfillment. However, the current study found that substance use increased the likelihood of depersonalization. Depersonalization (DP) is characterized by a lack of empathy and a cold, detached manner (49). Elkardi et al. showed that burnout can lead to substance use among healthcare professionals (50). Individuals who are undergoing burnout may use drugs as a coping strategy. The use of these substances constitutes an emotional confrontation since they aim to interfere with the individual’s ability to understand challenging situations through an escape strategy, which may result in depersonalization (48). Some studies indicate that the use of substances might provide a rapid but temporary relief response (51, 52). Therefore, this coping method may provide temporary relief from burnout symptoms, but it has the potential to lead to serious problems such as drug addiction. A study revealed that physicians who used alcohol four or more times weekly had a 3.3-fold greater chance of acquiring burnout syndrome (53). Other research, however, found no significant association between substance use and burnout (54). It is worth noting that the Brief Cope Scale does not indicate the sort of substance used, such as smoking, alcohol, or narcotics. As a result, more research is needed to determine what substances Palestinian health professionals take to cope with the stress of political violence.
Furthermore, the current study’s findings revealed that behavioral disengagement increased the probability of experiencing emotional exhaustion, whereas self-blame raised the likelihood of depersonalization. Other research found similar findings (44, 55). According to Leo et al., some escapist-avoidance strategies, such as disengagement, that lack a problem-solving approach may impede one’s ability to cope with a situation using their own or external resources, resulting in emotional exhaustion (13). Furthermore, persons who engage in self-blame are often seen to be competent in their domains of expertise. Individuals with a high sense of diligence may accept responsibility for work that others may not see as their own. This behavior makes them more likely to develop stress-related disorders and burnout (56).
This research has limitations. Convenience sampling and cross-sectional designs reduce the ability to demonstrate causal relationships and affect the representativeness of the sample and the generalizability of the findings. Furthermore, there is a possibility of reporting bias due to the use of a self-reported questionnaire. Given that recruiting took place using platforms such as Google Docs and WhatsApp, it is probable that health professionals already employed in the impacted areas, including the Gaza Strip, do not have access to or the chance to use this technology. As a result, this situation may have an impact on the sample’s representativeness. Additionally, few studies examine burnout among healthcare professionals during wartime. As a result, comparing our findings to other studies is limited. Also, in this study we were not able to calculate the response rate due to the use of anonymous online questionnaire. Despite these limitations, the findings of the current study provide light on the psychological well-being of health workers living in conflict-affected countries. This study provides a major contribution to the current literature since it is the first to analyze burnout and coping methods among Palestinian healthcare professionals throughout periods of armed conflict and political violence.
Implication for practice
As a result, professionals must develop effective coping strategies early in their careers to reduce the risk of developing burn out. Training sessions or seminars can help health practitioners understand their typical defense style and how it affects them and their ability to provide treatment during political violence. Furthermore, excessive workloads, prolonged working hours, a stressful work environment, and substandard workplace conditions have been identified as risk factors for stress, maladaptation, and burnout among health professionals. Consequently, health policymakers and managers can enhance stress adaptation among these health professionals during wartime by improving sleep quality and hours, offering a nutritious diet, reducing excessive workloads, promoting regular physical exercise and relaxation techniques, facilitating social engagement, ensuring a suitable work-life balance, and guaranteeing the physical safety of their employees (57). Further, health professionals should receive psychological support, treatment, and psychotherapy at the workplace to overcome their negative emotions to improve their well-being and a sense of efficacy and competence. Additionally, the study findings may underscore the necessity of implementing regulations and policies that safeguard and assist healthcare professionals during conflict and war. Thus, our research suggests the need for early screening for medical and mental problems, such as cardiovascular disease, among healthcare workers. Additionally, it highlights the need to limit working hours to a maximum of 40 per week.
More qualitative and quantitative research is required to fully understand the factors that increase burn out among health professionals and coping strategies for dealing with patients during political violence. Additional study is required to examine which drugs Palestinian health professionals use to deal with the stress of political violence. Finally, further research is needed to assess burnout levels in certain health professions in order to investigate burnout levels and related causes during wars and political violence.
Conclusion
The study found that burnout symptoms are common among Palestinian health professionals, particularly in less experienced professionals and those who work for long ours. In addition, using self-blame, and behavioral disengagement as coping mechanisms increases the likelihood of developing burnout symptoms. The study highlights the significance of identifying stressors faced by health professionals during wartime and implementing measures to prevent occupational burnout. Consequently, health professionals need immediate assistance in enhancing their mental wellbeing through psychological intervention and, and comprehensive training in stress management.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Al Quds University Research Ethical Committee (Ref No: 347/REC/2023). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. The social media data was accessed and analyzed in accordance with the platform’s terms of use and all relevant institutional/national regulations.
Author contributions
MA: Conceptualization, Data curation, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing. NE: Data curation, Formal analysis, Writing – original draft, Writing – review & editing. AA: Data curation, Validation, Writing – original draft, Writing – review & editing. AH: Data curation, Validation, Writing – review & editing. MZ: Data curation, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors would like to thank all participants for their participation in the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
1. Solis, G. (2016). The law of armed conflict: international humanitarian law in war. Cambridge University Press.
2. Garry, S, and Checchi, F. Armed conflict and public health: into the 21st century 2020; 42(3): e287-e298. doi: 10.1093/pubmed/fdz095. Erratum in. J Public Health. (2021) 43:e110. doi: 10.1093/pubmed/fdaa036
3. Rizzi, D, Ciuffo, G, Sandoli, G, Mangiagalli, M, de Angelis, P, Scavuzzo, G, et al. Running away from the war in Ukraine: the impact on mental health of internally displaced persons (IDPs) and refugees in transit in Poland. Int J Environ Res Public Health. (2022) 19:16439. doi: 10.3390/ijerph192416439
4. AlKhaldi, M, Kaloti, R, Shella, D, Al Basuoni, A, and Meghari, H. Health system's response to the COVID-19 pandemic in conflict settings: policy reflections from Palestine. Glob Public Health. (2020) 15:1244–56. doi: 10.1080/17441692.2020.1781914
5. Narwal, S, and Jain, S. Building resilient health systems: patient safety during COVID-19 and lessons for the future. J Health Manag. (2021) 23:166–81. doi: 10.1177/0972063421994935
6. Abed Alah, M. Echoes of conflict: the enduring mental health struggle of Gaza’s healthcare workers. Confl Heal. (2024) 18:21. doi: 10.1186/s13031-024-00577-6
7. Dominic, C, Gopal, D, and Sidhu, A. ‘It’s like juggling fire daily’: well-being, workload and burnout in the British NHS - a survey of 721 physicians. Work. (2021) 70:395–403. doi: 10.3233/WOR-205337
8. De Hert, S. Burnout in healthcare workers: prevalence, impact and preventative strategies. Local Reg Anesth. (2020) 13:171–83. doi: 10.2147/LRA.S240564
9. Maslach, C, Jackson, SE, and Leiter, MP. Maslach burnout inventory. Palo Alto, CA: Consulting Psychologists Press (1996).
10. Nápoles, J. Burnout: a review of the literature. Update: applications of research in music. Education. (2021) 40:875512332110376. doi: 10.1177/87551233211037669
11. Harrell, M, Selvaraj, SA, and Edgar, M. DANGER! Crisis health Workers at Risk. Int J Environ Res Public Health. (2020) 17:5270. doi: 10.3390/ijerph17155270
12. Elhadi, M, Khaled, A, Malek, AB, El-Azhari, AE, Gwea, AZ, Zaid, A, et al. Prevalence of anxiety and depressive symptoms among emergency physicians in Libya after civil war: a cross-sectional study. BMJ Open. (2020) 10:e039382. doi: 10.1136/bmjopen-2020-039382
13. Leo, CG, Sabina, S, Tumolo, MR, Bodini, A, Ponzini, G, Sabato, E, et al. Burnout among healthcare workers in the COVID 19 era: a review of the existing literature. Front Public Health. (2021) 9:750529. doi: 10.3389/fpubh.2021.750529
14. Alhaffar, BA, Abbas, G, and Alhaffar, AA. The prevalence of burnout syndrome among resident physicians in Syria. J Occup Med Toxicol. (2019) 14:31. doi: 10.1186/s12995-019-0250-0
15. Owoc, J, Mańczak, M, Olszewski, R, Shevchuk, O, Zaporozhan, S, and Korda, M. (2023). Can war help in better understanding of burnout phenomenon? A cross sectional study of burnout in Ukrainian medical staff. Available at: https://ssrn.com/abstract=4757684 (Accessed June, 12, 2024).
16. Lazarus, RS. From psychological stress to the emotions: a history of changing outlooks. Annu Rev Psychol. (1993) 44:1–22. doi: 10.1146/annurev.ps.44.020193.000245
17. Fitzgibbon, K, and Murphy, KD. Coping strategies of healthcare professional students for stress incurred during their studies: a literature review. J Ment Health. (2023) 32:492–503. doi: 10.1080/09638237.2021.2022616
18. Theodoratou, M, Farmakopoulou, I, Kougioumtzis, G, Kaltsouda, A, Siouti, Z, Sofologi, M, et al. Emotion-focused coping, social support and active coping among university students: gender differences. J Psychol Clin Psychiatry. (2023) 14:5–9. doi: 10.15406/jpcpy.2023.14.00720
19. Ding, Y, Fu, X, Liu, R, Hwang, J, Hong, W, and Wang, J. The impact of different coping styles on psychological distress during the COVID-19: the mediating role of perceived stress. Int J Environ Res Public Health. (2021) 18:10947. doi: 10.3390/ijerph182010947
20. Kua, Z, Hamzah, F, Tan, PT, Ong, LJ, Tan, B, and Huang, Z. Physical activity levels and mental health burden of healthcare workers during COVID-19 lockdown. Stress Health. (2022) 38:171–9. doi: 10.1002/smi.3078
21. Alameddine, M, Fouad, FM, Diaconu, K, Jamal, Z, Lough, G, Witter, S, et al. Resilience capacities of health systems: accommodating the needs of Palestinian refugees from Syria. Soc Sci Med. (2019) 220:22–30. doi: 10.1016/j.socscimed.2018.10.018
22. PNIPH. (2018). Overview of public health in Palestine. Available at: https://www.pniph.org/en/about/overview-of-public-health-in-palestine (Accessed November, 2024).
23. Ben Saad, H, and Dergaa, I. Public health in peril: assessing the impact of ongoing conflict in Gaza strip (Palestine) and advocating immediate action to halt atrocities. New Asian. J Med. (2023) 1:1–6. doi: 10.61838/kman.najm.1.2.1
24. Søvold, LE, Naslund, JA, Kousoulis, AA, Saxena, S, Qoronfleh, MW, Grobler, C, et al. Prioritizing the mental health and well-being of healthcare workers: an urgent global public health priority. Front Public Health. (2021) 9:679397. doi: 10.3389/fpubh.2021.679397
25. Palestinian Central Bureau of Statistics (2024). The Palestinian central Bureau of Statistics “PCBS” issues a press release on world health day. Available at: https://www.pcbs.gov.ps/portals/_pcbs/PressRelease/Press_En_WorldHealthDay2024E.pdf (Accessed November, 2024).
26. Jabali, O, Ayyoub, AA, and Jabali, S. Navigating health challenges: the interplay between occupation-imposed movement restrictions, healthcare access, and community resilience. BMC Public Health. (2024) 24:1297. doi: 10.1186/s12889-024-18817-y
27. Shawahna, R, Maqboul, I, Ahmad, O, Al-Issawy, A, and Abed, B. Prevalence of burnout syndrome among unmatched trainees and residents in surgical and nonsurgical specialties: a cross-sectional study from different training centers in Palestine. BMC Med Educ. (2022) 22:322. doi: 10.1186/s12909-022-03386-8
28. Hamdan, M, and Hamra, AA. Burnout among workers in emergency Departments in Palestinian hospitals: prevalence and associated factors. BMC Health Serv Res. (2017) 17:407. doi: 10.1186/s12913-017-2356-3
29. Veronese, G, and Pepe, A. Psychological distress, professional burnout, and trauma in Palestinian health care helpers: a two-wave quantitative longitudinal study. Psychol Trauma. (2022) 14:523–34. doi: 10.1037/tra0000941
30. Mcloughlin, C, Abdalla, A, O'Callaghan, AK, Casey, S, and Barrett, E. The impact of COVID-19 on burnout, psychological well-being, and Work satisfaction in psychiatry trainees in Ireland. Acad Psychiatry. (2022) 46:701–9. doi: 10.1007/s40596-022-01633-0
31. Riley, MR, Mohr, DC, and Waddimba, AC. The reliability and validity of three-item screening measures for burnout: evidence from group-employed health care practitioners in upstate New York. Stress Health. (2018) 34:187–93. doi: 10.1002/smi.2762
32. Carver, CS. You want to measure coping but your protocol’s too long: consider the brief COPE. Int J Behav Med. (1997) 4:92–100. doi: 10.1207/s15327558ijbm0401_6
33. Kabunga, A, Kigongo, E, Okalo, P, Udho, S, Grace, AA, Tumwesigye, R, et al. Burnout and coping mechanisms among healthcare professionals in Central Uganda. Front Psych. (2024) 15:1373743. doi: 10.3389/fpsyt.2024.1373743
34. Menaldi, SL, Raharjanti, NW, Wahid, M, Ramadianto, AS, Nugrahadi, NR, Adhiguna, GMYP, et al. Burnout and coping strategies among resident physicians at an Indonesian tertiary referral hospital during COVID-19 pandemic. PLoS One. (2023) 18:e0280313. doi: 10.1371/journal.pone.0280313
35. Hagihara, A, and Murata, S. Burnout among physicians in Poland. Pol Arch Intern Med. (2021) 131:612–4. doi: 10.20452/pamw.16068
36. Hosseini, SM, Hesam, S, and Hosseini, SA. Burnout among military personnel: a systematic review. Iran J Psychiatry. (2023) 18:213–36. doi: 10.18502/ijps.v18i2.12371
37. Wang, Z, Xie, Z, Dai, J, Zhang, L, Huang, Y, and Chen, B. Physician burnout and its associated factors: a cross-sectional study in Shanghai. J Occup Health. (2014) 56:73–83. doi: 10.1539/joh.13-0108-OA
38. Hu, NC, Chen, JD, and Cheng, TJ. The associations between long working hours, physical inactivity, and burnout. J Occup Environ Med. (2016) 58:514–8. doi: 10.1097/JOM.0000000000000715
39. Wang, J, Wang, W, Laureys, S, and Di, H. Burnout syndrome in healthcare professionals who care for patients with prolonged disorders of consciousness: a cross-sectional survey. BMC Health Serv Res. (2020) 20:841. doi: 10.1186/s12913-020-05694-5
40. Duli, S. Proactive coping and professional burnout in special education. AJIS. (2015) 4:18. doi: 10.5901/ajis.2015.v4n3s1p18
41. Oser, CB, Biebel, EP, Pullen, E, and Harp, KL. Causes, consequences, and prevention of burnout among substance abuse treatment counselors: a rural versus urban comparison. J Psychoactive Drugs. (2013) 45:17–27. doi: 10.1080/02791072.2013.763558
42. Bakker, AB, and Demerouti, E. Job demands–resources theory: taking stock and looking forward. J Occup Health Psychol. (2017) 22:273–85. doi: 10.1037/ocp0000056
43. Habibisaravi, R, Ghasemihamedani, F, Oveis, G, Azizi, S, and Assadi, T. Assessing job burnout status in front-line healthcare providers at Mazandaran University of Medical Sciences during the COVID-19 epidemic in 2022. Health Emerg Disast Q. (2023) 8:149–58. doi: 10.32598/hdq.8.3.34.5
44. Doolittle, BR, and Windish, DM. Correlation of burnout syndrome with specific coping strategies, behaviors, and spiritual attitudes among interns at Yale University, New Haven, USA. J Educ Eval Health Prof. (2015) 12:41. doi: 10.3352/jeehp.2015.12.41
45. Seguin, M, and Roberts, B. Coping strategies among conflict-affected adults in low- and middle-income countries: a systematic literature review. Glob Public Health. (2017) 12:811–29. doi: 10.1080/17441692.2015.1107117
46. Ahmead, M, Shehadah, F, and Abuiram, I. Correlation of death anxiety with coping strategies among Palestinian women with breast cancer: a cross-sectional study. Front Public Health. (2024) 12:1420306. doi: 10.3389/fpubh.2024.1420306
47. Hofmann, SG, and Hay, AC. Rethinking avoidance: toward a balanced approach to avoidance in treating anxiety disorders. J Anxiety Disord. (2018) 55:14–21. doi: 10.1016/j.janxdis.2018.03.004
48. Cecil, J, McHale, C, Hart, J, and Laidlaw, A. Behaviour and burnout in medical students. Med Educ Online. (2014) 19:25209. doi: 10.3402/meo.v19.25209
49. Andrade, GF, da Silva Menolli, PV, Clemente, PA, Mesas, AE, Silva, DC, and Girotto, E. Burnout syndrome and consumption of alcohol and illicit substances in university students. Paidéia. (2021) 31. doi: 10.1590/1982-4327e3134
50. Elkardi, S, Choujaa, H, and Agoub, M. Burn out of health care professionnels leads to addiction. Eur Psychiatry. (2023) 66:S466–7. doi: 10.1192/j.eurpsy.2023.1000
51. Carlotto, RC, Teixeira, MAP, and Dias, ACG. Adaptação acadêmica e coping em estudantes universitários [Academic adaptation and coping in university students]. Psico USF. (2015) 20:421–32. doi: 10.1590/1413-82712015200305
52. Pietrowski, DL, Cardoso, NO, and Bernardi, CCN. Estratégias de coping frente à síndrome de burnout entre os professores: uma revisão integrativa da literatura nacional. Cont Clín. (2018) 11:397–409. doi: 10.4013/ctc.2018.113.10
53. Winkel, AF, Woodland, MB, Nguyen, AT, and Morgan, HK. Associations between residents’ personal behaviors and wellness: a national survey of obstetrics and gynecology residents. J Surg Educ. (2020) 77:40–4. doi: 10.1016/j.jsurg.2019.08.014
54. Allen, HK, Lilly, F, Green, KM, Zanjani, F, Vincent, KB, and Arria, AM. Graduate student burnout: substance use, mental health, and the moderating role of advisor satisfaction. Int J Ment Health Addict. (2022) 20:1130–46. doi: 10.1007/s11469-020-00431-9
55. Kusalaruk, P, and Saravithi, J. Coping strategies and relationship with burnout among residents in Thailand. Eur Psychiatry. (2023) 66:S321–2. doi: 10.1192/j.eurpsy.2023.711
56. Gibbons, C. Stress, coping, burnout and mental health in the Irish police force. J Police Crim Psych. (2024) 39:348–57. doi: 10.1007/s11896-023-09638-7
Keywords: professional burnout, coping strategies, nurses, health professionals, Palestine, physicians
Citation: Ahmead M, El Sharif N, Alwawi A, Hemeid A and Ziqan M (2024) The prevalence of burnout and coping strategies among Palestinian health professionals: a cross sectional study. Front. Public Health. 12:1477812. doi: 10.3389/fpubh.2024.1477812
Edited by:
Shan Jiang, Zhejiang University, ChinaReviewed by:
Mansoor Malik, Johns Hopkins Medicine, United StatesJordi Fernandez-Castro, Autonomous University of Barcelona, Spain
Jonathan Ripp, Mount Sinai Hospital, United States
Copyright © 2024 Ahmead, El Sharif, Alwawi, Hemeid and Ziqan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Muna Ahmead, bXVuYWFobWVhZEB5YWhvby5jb20=
 Muna Ahmead
Muna Ahmead Nuha El Sharif
Nuha El Sharif Abdallah Alwawi
Abdallah Alwawi Asma Hemeid3
Asma Hemeid3