- 1School of Health Services Management, Xi’an Medical University, Xi'an, China
- 2School of Public Health, Xi’an Medical University, Xi’an, China
- 3Department of Respiratory and Critical Care Medicine, Tangdu Hospital, Air Force Military Medical University, Xian, China
Objective: Research on the inequality of chronic respiratory disease (CRD) is limited, and the association between CRD and all-cause mortality is not well-established. Investigating the distribution of CRD and its associated mortality risks is essential for improving CRD conditions and developing targeted intervention measures. This study aimed to explore the relationship between inequalities in CRD and all-cause mortality in China.
Methods: This study utilized nationally representative baseline data from the China Health and Retirement Longitudinal Study (CHARLS, 2011–2020, wave 1–wave 5), including a total of 14,743 subjects. The concentration index was employed to measure socioeconomic-related inequality in CRD, and the concentration index decomposition method was used to describe its influencing factors. Cox proportional hazards regression model was employed to examine the association between CRD and all-cause mortality.
Results: The prevalence of CRD was 11.79% (95% CI: 10.98, 12.66) in China. The concentration index for CRD was −0.050 (95% CI: −0.075, −0.026), indicating a certain degree of inequality in its prevalence. Chronic lung disease (concentration index = −0.046, 95% CI: −0.073, −0.019), asthma (concentration index = −0.102, 95% CI: −0.148, −0.056), and asthma-chronic obstructive pulmonary disease overlap syndrome (concentration index = −0.114, 95% CI: −0.173, −0.055) also exhibited a pro-poor distribution. The decomposition analysis of the concentration index for CRD revealed that age, education level, and economic status played substantial roles in contributing to the observed inequality. Additionally, Cox regression analysis showed that participants with CRD had an increased risk of all-cause mortality (HR = 1.49, 95% CI: 1.34, 1.65).
Conclusion: Inequalities exists in CRDs in China, with the prevalence of these diseases primarily concentrated among economically disadvantaged groups. Additionally, CRD increases the risk of all-cause mortality. Addressing the root causes of economic inequalities and enhancing the educational attainment of individuals with low socioeconomic status can help improve the situation.
Introduction
Chronic respiratory disease (CRD), primarily chronic lung diseases, are a significant category of non-communicable diseases that pose a serious threat to health (1). Globally, the prevalence of CRD stands at 7.1%, affecting an estimated 545 million people. Ranked as the third leading cause of death worldwide, following cardiovascular disease and cancer, this group of diseases is responsible for approximately 4 million deaths (2, 3). In China, CRD are also widespread, securing the fourth position among causes of death in 2019 and accounting for 10.6% of total deaths in the country (4). Beyond the threat to life, CRD can result in diminished physical function, leading to disability and increased medical costs, imposing a substantial burden on families and society (5, 6).
Asthma and chronic obstructive pulmonary disease (COPD) are prevalent CRD (7). Asthma is characterized by chronic airway inflammation, leading to recurrent wheezing, shortness of breath, coughing, and chest tightness (8). Chronic obstructive pulmonary disease, encompassing chronic bronchitis and emphysema, is characterized by persistent airflow restriction and corresponding respiratory symptoms (9). Global prevalence data indicate that asthma affects approximately 334 million people (10), while COPD affects over 200 million people, with about 65 million experiencing moderate or severe disease, making it the third leading cause of death worldwide. Notably, more than three-quarters of individuals with COPD reside in low- and middle-income countries (11, 12). Asthma and COPD also impose a significant health burden in China. Data from the China Lung Health Study reveal that the prevalence of asthma in individuals aged 20 and above in China is 4.2%, with approximately 45.7 million patients (13). As for COPD, the prevalence is 13.7% in individuals over 40 years of age, affecting nearly 100 million people nationwide (14). Studies have demonstrated the existence of asthma-chronic obstructive pulmonary disease overlap syndrome (ACOS), although there is no consistent agreement on the diagnostic criteria for this condition (15). Moreover, the clinical characteristics of this syndrome are complex, resulting in worse health status, increased treatment difficulty, and a significantly elevated risk of poor patient prognosis (16). Therefore, in-depth research and more effective management strategies for CRD are essential to reduce their burden.
Socioeconomic status serves as a comprehensive indicator of an individual’s economic and social standing, used to gauge their social status. Generally, a higher socioeconomic status tends to be positively correlated with better health. Numerous studies have identified an association between socioeconomic status and the prevalence of chronic diseases (17). One study highlighted socioeconomic inequalities among patients with various fatal chronic diseases (18). Moreover, studies conducted on the Slovenian population with chronic diseases have revealed a significantly higher incidence of chronic conditions among individuals with lower socioeconomic and employment status (19). In measuring health inequities resulting from socioeconomic factors, the concentration index is widely employed to assess health equity, and its reliability has been well validated in previous studies (20). Additionally, previous studies have shown that CRD may affect all-cause mortality, and a meta-analysis of cohort studies indicated that patients with asthma had an increased risk of all-cause mortality (21). A large national cohort study also found that patients with COPD had a significantly higher risk of all-cause death compared to those without COPD (22).
Numerous studies have highlighted a robust association between socioeconomic status and CRD. However, different studies have presented conflicting results (18, 23). Additionally, despite previous research analyzing the relationship between CRD and all-cause mortality, the literature on the relationship between CRD inequality and all-cause mortality in low- and middle-income countries, especially in China, remains limited. Furthermore, even within large cohorts, results are not entirely consistent, indicating the need for further research. To fill this gap, we used data from the China Health and Retirement Longitudinal Study (CHARLS) to analyze the relationship between CRD and all-cause mortality among Chinese adults and explore the inequitable status of CRD.
Materials and methods
Data sources and study population
The study utilized 2011–2012 baseline data (wave 1) and follow-up data (wave2-wave5) from the CHARLS. Initiated by the National School of Development at Peking University, CHARLS conducted a national baseline survey in 2011, followed by four subsequent visits in 2013, 2015, 2018, and 2020. This study adopted a multi-stage stratified probability proportional scale sampling method to sample residents over 45 years old in 150 counties and 450 communities/villages across 28 provinces (autonomous regions and municipalities directly under the Central Government) in China. The survey encompassed two main components: a household questionnaire and a physical examination survey designed to collect detailed information from the respondents. The purpose of data collection was to provide fundamental insights into China’s aging population, supporting the formulation of more effective policy programs aimed at improving the living conditions of the older adult population. A scientific sampling method was employed to ensure that the large sample of older adult people was nationally representative. The information on chronic lung diseases and asthma was obtained through a questionnaire survey, and any missing samples were deleted to ensure the data’s integrity and accuracy. The CHARLS project received ethics approval from the Peking University Ethical Review Committee (IRB00001052-11015), and subjects provided written informed consent before the investigation commenced, ensuring the ethical compliance of the study. Moreover, the present analysis received approval from Xi’an Medical University Medical Ethics Review Committee (XYLS2023077).
In this study, individuals with missing CRD information (n = 278), missing economic status information (n = 293), those under 45 years of age (n = 489), and those lost to follow-up (n = 1,905) were excluded. Finally, 14,743 participants were included in the analysis.
Study variables
Chronic respiratory diseases were the main variable in this study, encompassing chronic lung disease and asthma, as obtained from CHALRS questionnaires. The assessment of chronic lung disease involved the question, ‘Have you been diagnosed with chronic lung diseases, such as chronic bronchitis, emphysema (excluding tumors, or cancer) by a doctor?’ Asthma was determined through the question, ‘Have you been diagnosed with asthma by a doctor?’ ACOS (asthma-chronic obstructive pulmonary disease overlap syndrome) was not specifically investigated in this study. Since COPD is a significant component of chronic lung disease (24), and there is no uniform definition for ACOS, the comorbidities of chronic lung disease and asthma investigated in this study were considered as ACOS.
The primary outcome of the study was all-cause mortality. Mortality information was collected from the wave 2 to wave 5, with only wave 2 providing an exact date of death. If participants survived during the follow-up period, their survival time was the interval between the two surveys. If they died, the survival time was the interval from the date of wave 1 to the date of death of the participant, or from the date of wave 1 to the median time of the wave with recorded death.
Covariance
The covariates included in this study encompassed basic information such as age (45–59, 60–74, ≥75), gender (male, female), educational level (illiterate, primary school, secondary/high school, university or above), and marriage status (never married, married, others). Lifestyle factors, including smoking (no, yes), drinking (never, occasionally, regularly), BMI (0–23.9, 24–27.9, ≥28), basic health insurance (no, yes), and preventative health service utilization (no, yes), were also considered. BMI was calculated using the weight/height squared formula, and alcohol consumption was categorized as never, occasionally (defined as less than one drink per month), and regularly (defined as more than one drink per month).
Statistical analysis
First, the concentration index was utilized to assess the inequality of CRD, chronic lung disease, asthma, and the ACOS. The economic status indicator employed was the IM_PCE from the “Constructed Expenditure, Income, and Wealth Database” released by CHARLS in 2017. Economic status was categorized into five groups based on quartiles. To further validate the results, we conducted a stratified analysis of the inequality of the CRD based on age and sex. Data were extrapolated by applying the CHARLS sampling weight (ind_weight_ad2) to estimate the prevalence of CRD among Chinese adults aged 45 years and older. Secondly, we described the basic characteristics of the study population. Continuous data conforming to normal distribution were presented as means and standard deviations, while frequencies and percentages were used for categorical data. Thirdly, Concentration index decomposition was employed to describe the contribution of each influencing factor to the inequity. Finally, a Cox proportional hazards regression model was employed to examine the association between CRD and all-cause mortality. Additionally, a stratified analysis was performed according to sociodemographic characteristics. Stata 16.0 was used for data collation and analysis, with p < 0.05 considered statistically significant.
Results
Concentration index
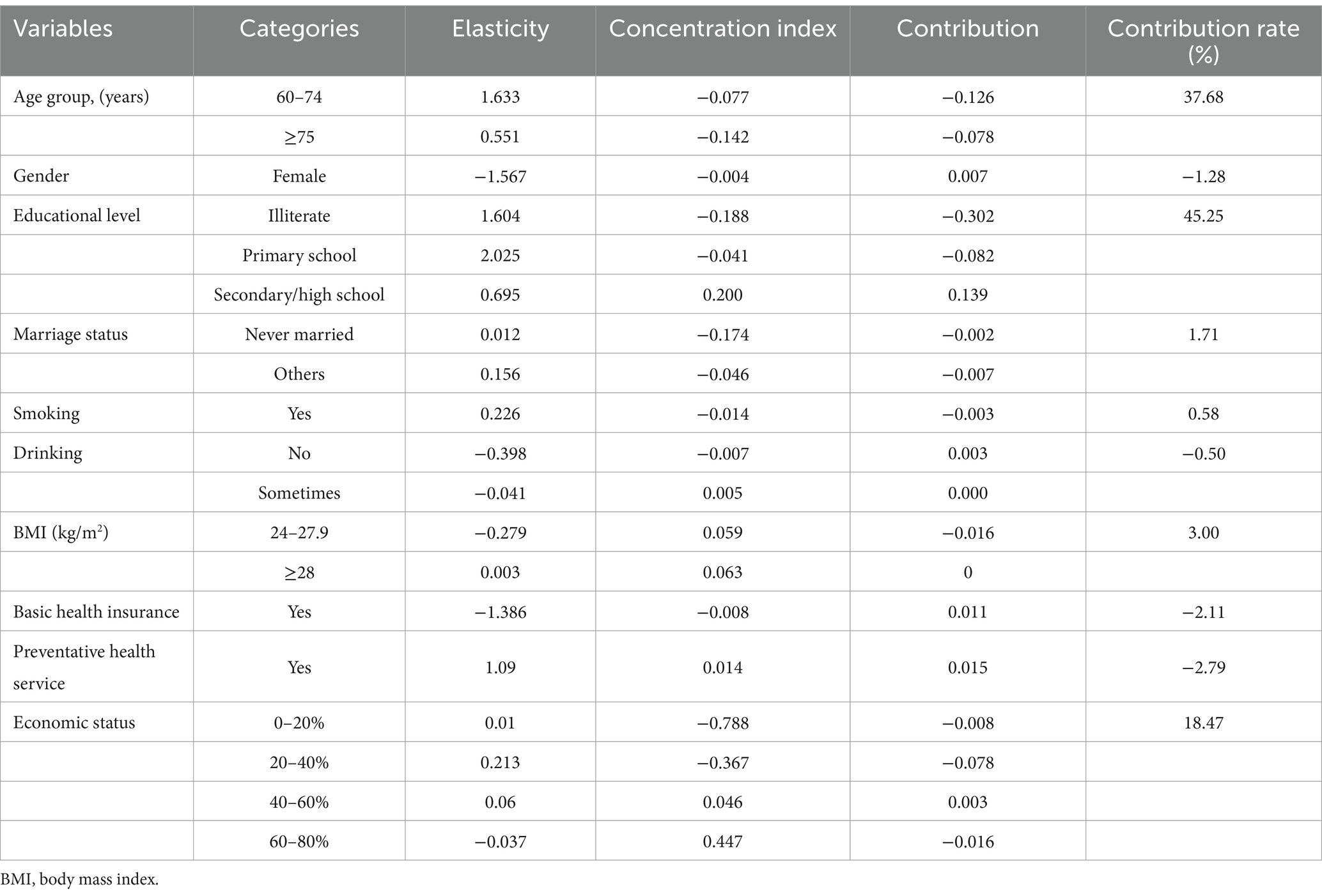
The prevalence of CRD, chronic lung disease, asthma, and ACOS were 11.79% (95% CI: 10.98, 12.66), 10.42% (95% CI: 9.65, 11.24), 3.72% (95% CI: 3.29, 4.20), and 2.34% (95% CI: 2.03, 2.71), respectively. The concentration indexes for CRD, chronic lung disease, asthma, and ACOS were −0.050 (95% CI: −0.075, −0.026), −0.046 (95% CI: −0.073, −0.019), −0.102 (95% CI: −0.148, −0.056), and −0.114 (95% CI: −0.173, −0.055) (Figure 1; Supplementary Table S1). The results indicated a certain degree of inequality in the prevalence of CRD, chronic lung disease, asthma, and ACOS, with the prevalence of these diseases mainly concentrated in the population with poor economic status.
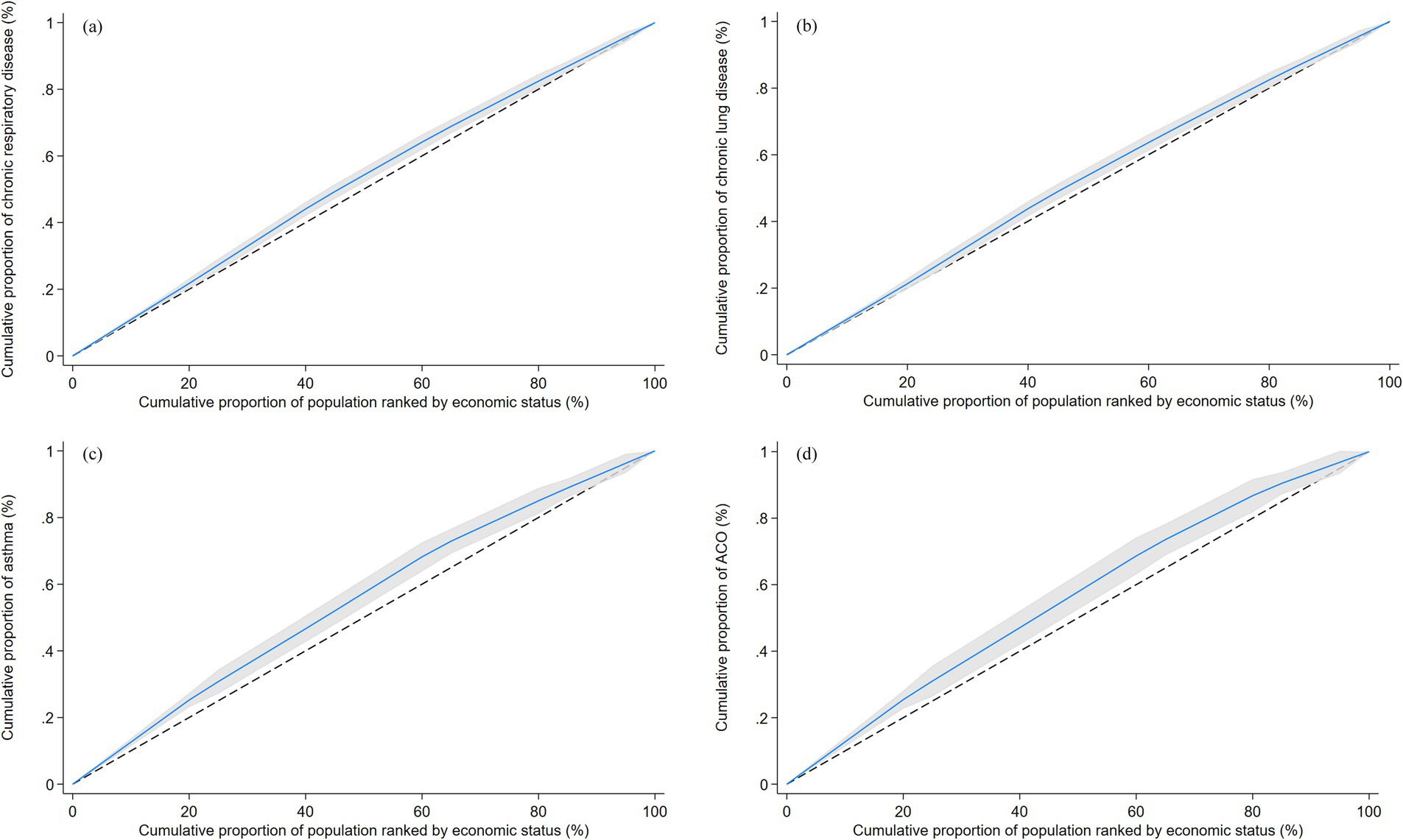
Figure 1. Concentration curves for chronic respiratory disease (A), chronic lung disease (B), asthma (C) and ACOS (D). The dotted line surrounding the curve represents the 95% CI. ACOS, asthma-chronic obstructive pulmonary disease overlap syndrome.
Stratified analysis
To further demonstrate the inequity in the prevalence of CRD in different populations, we conducted a subgroup analysis. We found that several diseases were more prevalent among individuals with lower socioeconomic status in both men and participants aged <60, consistent with the results of the main study. However, ACOS did not show significant inequities in women. No inequities were observed in several diseases among participants older than 60 years (Table 1).
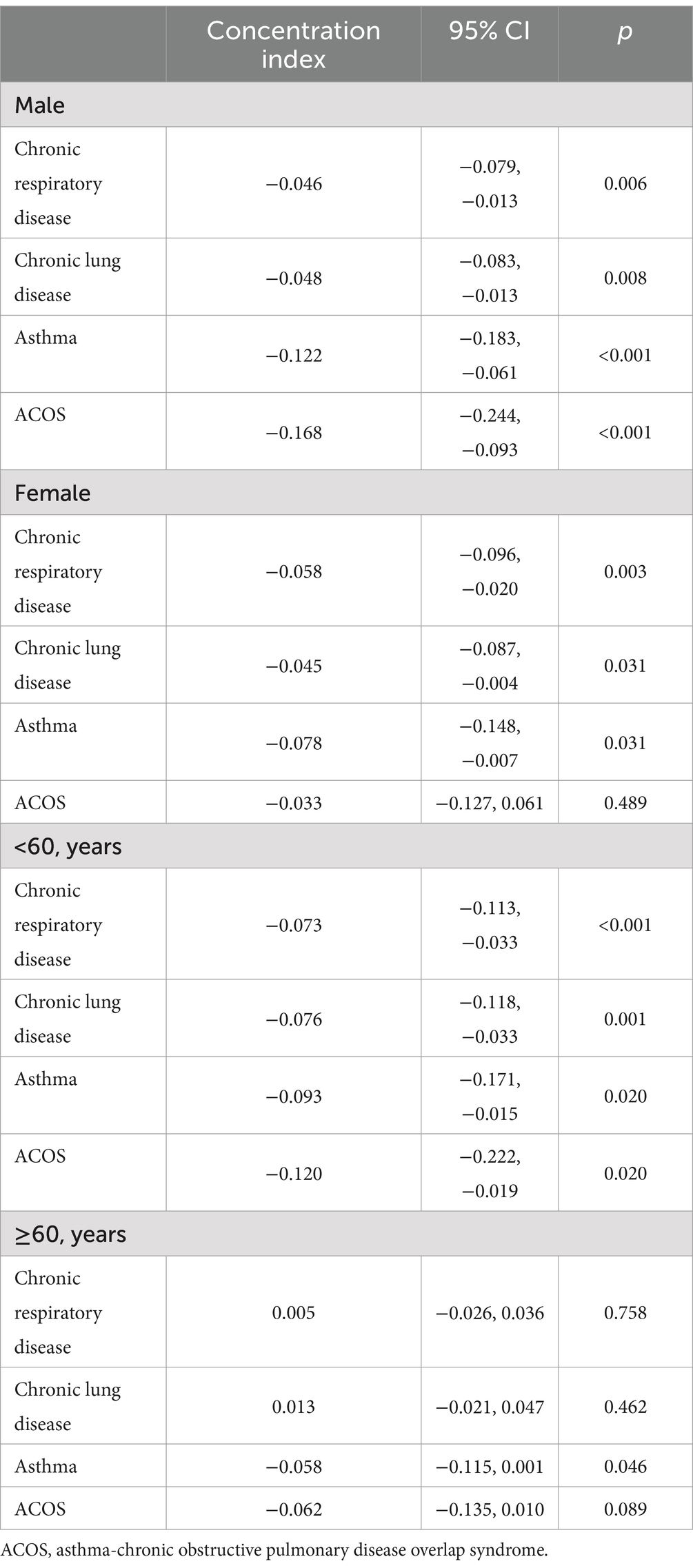
Table 1. Concentration index for chronic respiratory disease, chronic lung disease, asthma and ACOS by gender and age.
Sociodemographic characteristics of the subjects
A total of 14,743 subjects were enrolled in this study, with an average age of 59.72 ± 9.83, comprising 7,232 males (49.05%). The majority of participants had an education level of high school and below (98.22%), and 86.96% were married. Additionally, 32.33% were smokers, 41.96% were drinkers, and 31.68% were overweight or obese. Moreover, 91.06% had basic medical insurance, and 19.85% had utilized basic public health services in the previous month (Table 2).
Concentration index decomposition
The decomposition analysis of the concentration index for CRD revealed that age, education level, and economic status played substantial roles in contributing to the inequality observed in these diseases. Older age, lower educational attainment, and poorer economic status were identified as factors that elevate the inequality associated with CRD. Additionally, the study found that other factors such as marital status, smoking, and higher BMI also contributed to an increase in inequality related to CRD (Table 3).
Association of chronic respiratory disease with risks of all-cause mortality
Over the approximately 10-years follow-up period, 2,368 deaths were reported, resulting in a mortality rate of 15.76% (95% CI: 15.14, 16.41). Subjects with CRD had a higher all-cause mortality rate than those without CRD (Log-rank test, p < 0.05) (Figure 2). After adjusting for all covariates, Cox regression analysis revealed that participants with CRD had an increased risk of all-cause mortality (HR = 1.49, 95% CI: 1.34, 1.65) (Supplementary Table S2). The analysis of specific types of CRD revealed that chronic lung disease, asthma and ACOS were significantly associated with an increased risk of all-cause mortality (Supplementary Table S2). Additionally, stratified analyses based on sociodemographic characteristics showed that while the results for each subgroup varied slightly from the overall findings, there was a consistent trend indicating that CRD was associated with a higher risk of all-cause mortality across different groups (Supplementary Figure S1).
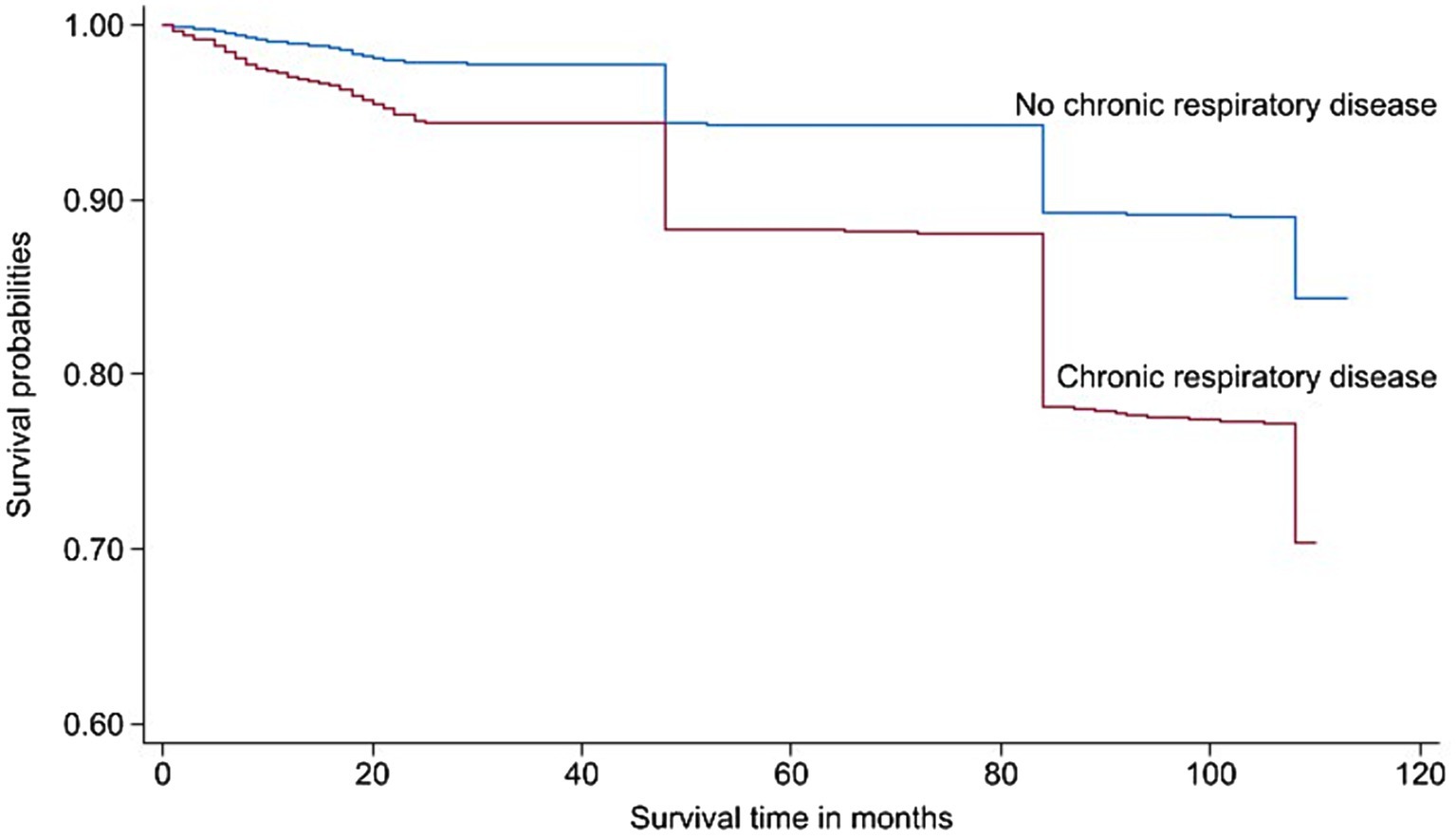
Figure 2. Kaplan–Meier curve showing the cumulative risk of all-cause mortality by chronic respiratory disease status.
Discussion
We used nationally representative data from the CHARLS baseline survey to examine the socioeconomic inequalities associated with CRD. Our study identified inequalities in CRD and its specific types (chronic lung disease, asthma, ACOS), predominantly favoring individuals of lower economic status. Age, education level and economic status were identified as significant factors contributing to these inequalities. Additionally, our findings indicated that CRD was associated with an increased risk of all-cause mortality. These results highlight the current inequitable burden of CRD and its potential implications for mortality in China.
Previous studies had revealed the inequity present in common chronic diseases, such as hypertension and diabetes (25). This study aligned with those findings, indicating a similar inequality in CRD. Adam et al., utilizing multiple rounds of cross-sectional data from the United States, demonstrated the existence and worsening of socioeconomic inequality in lung health over time (26). Furthermore, socioeconomic status emerged as a potential independent determinant of lung health. On a global scale, inequalities in CRD were also apparent. Haifeng Li et al., drawing on data from the global disease burden, identified a concentration of disability-adjusted life years associated with COPD in less developed countries (27). The socioeconomic status-driven inequality in CRD may be linked to insufficient healthcare programs and inadequate tobacco consumption control (27, 28). These findings underscored the importance of health system reform, emphasizing the need to direct more attention to vulnerable groups based on economic and social status. Additionally, CRD served as predictors of all-cause mortality (29, 30), suggesting that the income-based gap in CRD identified in our study may contribute to life expectancy inequality in China.
This study highlighted the significant impact of age, education, and economic status on chronic respiratory inequality. It was widely recognized that older adults often encounter challenges such as physical decline and a weakened immune system, increasing their susceptibility to CRD (31). A potential remedy could involve providing increased access to free basic public health services and allocating more resources to medicare drugs related to respiratory health (32). In terms of age and education, economic status emerged as a key modifiable risk factor. Previous research had identified low economic status as a risk factor for CRD (27, 28), exposing individuals to additional risk factors like poor dietary habits and increased occupational dust exposure (33). Conversely, individuals with higher economic status were more likely to leverage medical technology for health maintenance, receive health advice, actively engage in disease screenings (25, 26), and ultimately reduce the risk of CRD.
Respiratory diseases are a major cause of death worldwide and rank as the third leading cause of death globally (29). In 2017, CRDs were responsible for nearly 4 million deaths, marking an 18 percent increase since 1990 (2). Population-based studies have also reported that CRD increases the risk of all-cause mortality. Bin Zhang et al. summarized the findings of 30 cohort studies, revealing that patients with asthma had a higher all-cause mortality rate (RR = 1.38, 95% CI: 1.07, 1.77) (21). A meta-analysis pooling the results of 12 studies found that even mild COPD was associated with increased all-cause mortality (34). Additionally, a study using data from the National Health and Nutrition Examination Survey found that patients with ACO had a higher risk of all-cause death compared to individuals with asthma only, COPD only, non-asthma/COPD, or non-ACO (35). These findings are consistent with our study. The increased risk of all-cause mortality in patients with CRD not only from the disease itself but also from chronic inflammation, airway limitation, and comorbidities due to medication (e.g., osteoporosis, pneumonia, depression) (36, 37). Implementing appropriate management strategies and interventions is crucial to reducing this risk.
This study analyzed the inequality of CRD and its risk of all-cause mortality using nationally representative data, providing a crucial foundation for the control of such diseases. However, the article has several limitations. Firstly, the study did not categorize the collection of chronic lung diseases, making it challenging to determine the percentage of COPD. Consequently, chronic lung diseases were used to represent COPD, introducing a certain degree of bias. Nevertheless, considering that COPD is the primary chronic lung disease, this bias is likely minimal. Secondly, the prevalence of CRD relies on self-reporting, which may introduce bias, given the low awareness rates of diseases such as asthma and COPD in China (38, 39). Additionally, due to age limitations in the survey, we were unable to estimate the inequality of CRD in individuals over 75 years of age. Finally, this study employs data from 2011, potentially introducing bias compared to the current reality of CRD inequality.
Conclusion
There is inequality in CRD in China, primarily affecting economically disadvantaged groups, and CRD increased the risk of all-cause death. Age, education level, and economic factors significantly contribute to this inequality. Policymakers and researchers should prioritize the needs of individuals with low socioeconomic status when developing strategies to prevent CRD. Addressing the root causes of income inequality and improving educational attainment among these individuals can help mitigate the issue.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found at: http://charls.pku.edu.cn/.
Ethics statement
The studies involving humans were approved by The CHARLS project received ethics approval from the Peking University Ethical Review Committee (IRB00001052-11015), and the present analysis received approval from Xi’an Medical University Medical Ethics Review Committee (XYLS2023077). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
ZZ: Data curation, Formal analysis, Funding acquisition, Methodology, Visualization, Writing – original draft. GS: Data curation, Visualization, Writing – original draft, Writing – review & editing. FJ: Methodology, Writing – review & editing. YZ: Conceptualization, Project administration, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the fifth batch of school-level key discipline construction project of Xi’an Medical University (12202310), three Undergraduate Training Programs for Innovation and Entrepreneurship (S202311840072S, S202411840057S and 121524141) and two school-level scientific research fund from Xi’an Medical University (2023BS21 and 2023BS27), the Key Research and Development Projects of Shaanxi Province, Key Industrial Innovation Chain (Group)-Social Development Field (2022ZDLSF01-10).
Acknowledgments
We extend our sincere appreciation to all CHARLS study participants and trial investigators. This article was developed using research materials obtained from the Peking University Open Research Data Platform.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1472074/full#supplementary-material
References
1. Laxmi, V. Clarification of non communicable diseases their types and risk factor and some preventive action to reduce the chronic diseases. Pharma Innov J. (2022) 11:1896–907.
2. Soriano, JB, Kendrick, PJ, Paulson, KR, Gupta, V, Abrams, EM, Adedoyin, RA, et al. Prevalence and attributable health burden of chronic respiratory diseases, 1990–2017: A systematic analysis for the global burden of disease study 2017. Lancet Respir Med. (2020) 8:585–96. doi: 10.1016/S2213-2600(20)30105-3
3. Vos, T, Lim, SS, Abbafati, C, Abbas, KM, Abbasi, M, Abbasifard, M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the global burden of disease study 2019. Lancet. (2020) 396:1204–22. doi: 10.1016/S0140-6736(20)30925-9
4. Long, Z, Liu, W, Qi, J-L, Liu, Y-N, Liu, J-M, You, J-L, et al. Mortality trend of chronic respiratory diseases in China, 1990-2019. Zhonghua Liu Xing Bing Xue Za Zhi. (2022) 43:14–21. doi: 10.3760/cma.j.cn112338-20210601-00443
5. Booth, S, and Johnson, MJ. Improving the quality of life of people with advanced respiratory disease and severe breathlessness. Breathe. (2019) 15:198–215. doi: 10.1183/20734735.0200-2019
6. Beran, D, Zar, HJ, Perrin, C, Menezes, AM, and Burney, P. Burden of asthma and chronic obstructive pulmonary disease and access to essential medicines in low-income and middle-income countries. Lancet Respir Med. (2015) 3:159–70. doi: 10.1016/S2213-2600(15)00004-1
7. Labaki, WW, and Han, MK. Chronic respiratory diseases: A global view. Lancet Respir Med. (2020) 8:531–3. doi: 10.1016/S2213-2600(20)30157-0
8. Cevhertas, L, Ogulur, I, Maurer, DJ, Burla, D, Ding, M, Jansen, K, et al. Advances and recent developments in asthma in 2020. Allergy. (2020) 75:3124–46. doi: 10.1111/all.14607
9. Martinez, FJ, Han, MK, Allinson, JP, Barr, RG, Boucher, RC, Calverley, PM, et al. At the root: defining and halting progression of early chronic obstructive pulmonary disease. Am J Respir Crit Care Med. (2018) 197:1540–51. doi: 10.1164/rccm.201710-2028PP
10. Enilari, O, and Sinha, S. The global impact of asthma in adult populations. Ann Glob Health. (2019) 85:1–7. doi: 10.5334/aogh.2412
11. Ruvuna, L, and Sood, A. Epidemiology of chronic obstructive pulmonary disease. Clin Chest Med. (2020) 41:315–27. doi: 10.1016/j.ccm.2020.05.002
12. Adeloye, D, Song, P, Zhu, Y, Campbell, H, Sheikh, A, and Rudan, I. Global, regional, and national prevalence of, and risk factors for, chronic obstructive pulmonary disease (Copd) in 2019: A systematic review and modelling analysis. Lancet Respir Med. (2022) 10:447–58. doi: 10.1016/S2213-2600(21)00511-7
13. Huang, K, Yang, T, Xu, J, Yang, L, Zhao, J, Zhang, X, et al. Prevalence, risk factors, and management of asthma in China: A National Cross-Sectional Study. Lancet. (2019) 394:407–18. doi: 10.1016/S0140-6736(19)31147-X
14. Wang, C, Xu, J, Yang, L, Xu, Y, Zhang, X, Bai, C, et al. Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China pulmonary health [Cph] study): A National Cross-Sectional Study. Lancet. (2018) 391:1706–17. doi: 10.1016/S0140-6736(18)30841-9
15. Postma, DS, and Rabe, KF. The asthma–COPD overlap syndrome. N Engl J Med. (2015) 373:1241–9. doi: 10.1056/NEJMra1411863
16. Maselli, DJ, and Hanania, NA. Management of Asthma Copd Overlap. Ann Allergy Asthma Immunol. (2019) 123:335–44. doi: 10.1016/j.anai.2019.07.021
17. Mair, FS, and Jani, BD. Emerging trends and future research on the role of socioeconomic status in chronic illness and multimorbidity. Lancet Public Health. (2020) 5:e128–9. doi: 10.1016/S2468-2667(20)30001-3
18. Sommer, I, Griebler, U, Mahlknecht, P, Thaler, K, Bouskill, K, Gartlehner, G, et al. Socioeconomic inequalities in non-communicable diseases and their risk factors: An overview of systematic reviews. BMC Public Health. (2015) 15:1–12. doi: 10.1186/s12889-015-2227-y
19. Softič, N, Smogavec, M, Klemenc-Ketiš, Z, and Kersnik, J. Prevalence of chronic diseases among adult Slovene population. Slovenian J Public Health. (2011) 50:185–90. doi: 10.2478/v10152-010-0043-4
20. Kakwani, N, Wagstaff, A, and Van Doorslaer, E. Socioeconomic inequalities in health: measurement, computation, and statistical inference. J Econ. (1997) 77:87–103. doi: 10.1016/S0304-4076(96)01807-6
21. Zhang, B, Li, Z-F, An, Z-Y, Zhang, L, Wang, J-Y, Hao, M-D, et al. Association between asthma and all-cause mortality and cardiovascular disease morbidity and mortality: A Meta-analysis of cohort studies. Front Cardiovasc Med. (2022) 9:861798. doi: 10.3389/fcvm.2022.861798
22. Park, HY, Kang, D, Lee, H, Shin, SH, Kang, M, Kong, S, et al. Impact of chronic obstructive pulmonary disease on mortality: A large National Cohort Study. Respirology. (2020) 25:726–34. doi: 10.1111/resp.13678
23. Williams, DR, Mohammed, SA, Leavell, J, and Collins, C. Race, socioeconomic status, and health: complexities, ongoing challenges, and research opportunities. Ann N Y Acad Sci. (2010) 1186:69–101. doi: 10.1111/j.1749-6632.2009.05339.x
24. Song, P, Zha, M, Xia, W, Zeng, C, and Zhu, Y. Asthma–chronic obstructive pulmonary disease overlap in China: prevalence, associated factors and comorbidities in middle-aged and older adults. Curr Med Res Opin. (2020) 36:667–75. doi: 10.1080/03007995.2020.1722082
25. Mira, R, Newton, T, and Sabbah, W. Inequalities in the Progress of multiple chronic conditions: A systematic review of longitudinal studies. PLoS One. (2022) 17:e0263357. doi: 10.1371/journal.pone.0263357
26. Gaffney, AW, Himmelstein, DU, Christiani, DC, and Woolhandler, S. Socioeconomic inequality in respiratory health in the US from 1959 to 2018. JAMA Intern Med. (2021) 181:968–76. doi: 10.1001/jamainternmed.2021.2441
27. Li, H, Liang, H, Wei, L, Shi, D, Su, X, Li, F, et al. Health inequality in the global burden of chronic obstructive pulmonary disease: findings from the global burden of disease study 2019. Int J Chron Obstruct Pulmon Dis. (2022) 17:1695–702. doi: 10.2147/COPD.S369120
28. Sahni, S, Talwar, A, Khanijo, S, and Talwar, A. Socioeconomic status and its relationship to chronic respiratory disease. Adv Respir Med. (2017) 85:97–108. doi: 10.5603/ARM.2017.0016
29. Li, X, Cao, X, Guo, M, Xie, M, and Liu, X. Trends and risk factors of mortality and disability adjusted life years for chronic respiratory diseases from 1990 to 2017: systematic analysis for the global burden of disease study 2017. BMJ. (2020):368. doi: 10.1136/bmj.m234
30. Salciccioli, JD, Marshall, DC, Shalhoub, J, Maruthappu, M, De Carlo, G, and Chung, KF. Respiratory disease mortality in the United Kingdom compared with Eu15+ countries in 1985-2015: observational study. BMJ. (2018):k4680. doi: 10.1136/bmj.k4680
31. Cho, SJ, and Stout-Delgado, HW. Aging and lung disease. Annu Rev Physiol. (2020) 82:433–59. doi: 10.1146/annurev-physiol-021119-034610
32. Adler, NE, Glymour, MM, and Fielding, J. Addressing social determinants of health and health inequalities. JAMA. (2016) 316:1641–2. doi: 10.1001/jama.2016.14058
33. Yin, P, Zhang, M, Li, Y, Jiang, Y, and Zhao, W. Prevalence of Copd and its association with socioeconomic status in China: findings from China chronic disease risk factor surveillance 2007. BMC Public Health. (2011) 11:1–8. doi: 10.1186/1471-2458-11-586
34. Weifeng, Z, Jie, O, Fan, W, Huanuan, F, Yuyan, H, Haiqing, L, et al. Association of mild chronic obstructive pulmonary disease with all-cause mortality: A systematic review and meta-analysis. Pulmonology. (2023):S2531-0437(23)00165-4. doi: 10.1016/j.pulmoe.2023.09.002
35. Meng, Z, and An, C. Epidemiological characteristics of asthma-Copd overlap, its association with all-cause mortality, and the mediating role of depressive symptoms: evidence from Nhanes 2005-2018. BMC Public Health. (2024) 24. doi: 10.1186/s12889-024-18911-1
36. Gershon, AS, Wang, C, Guan, J, and To, T. Burden of comorbidity in individuals with asthma. Thorax. (2010) 65:612–8. doi: 10.1136/thx.2009.131078
37. Odegaard, AO, Jacobs, DR, Sanchez, OA, Goff, DC, Reiner, AP, and Gross, MD. Oxidative stress, inflammation, endothelial dysfunction and incidence of type 2 diabetes. Cardiovasc Diabetol. (2016) 15:1–12. doi: 10.1186/s12933-016-0369-6
38. Quan, Z, Yan, G, Wang, Z, Li, Y, Zhang, J, Yang, T, et al. Current status and preventive strategies of chronic obstructive pulmonary disease in China: A literature review. J Thorac Dis. (2021) 13:3865–77. doi: 10.21037/jtd-20-2051
39. Cong, S, Yao, J, Fan, J, Wang, N, Wang, B, Bao, H, et al. Analysis on awareness of chronic obstructive pulmonary disease (Copd) status and related knowledge in patients with Copd in China, 2014-2015. Zhonghua Liu Xing Bing Xue Za Zhi. (2020) 41:1034–40. doi: 10.3760/cma.j.cn112338-20200206-00074
Keywords: inequality, chronic respiratory disease, asthma, chronic obstructive pulmonary disease, all-cause mortality
Citation: Zhang Z, Shi G, Jin F and Zhang Y (2025) Exploring the association between socioeconomic inequalities in chronic respiratory disease and all-cause mortality in China: findings from the China Health and Retirement Longitudinal Study. Front. Public Health. 12:1472074. doi: 10.3389/fpubh.2024.1472074
Edited by:
Hubert Amu, University of Health and Allied Sciences, GhanaReviewed by:
Patricia M. Alt, Towson University, United StatesXinpei Wang, The University of Chicago, United States
Copyright © 2025 Zhang, Shi, Jin and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yan Zhang, eWFuemhhbmd0YW5nZHVAMTYzLmNvbQ==
 Zhuo Zhang
Zhuo Zhang Guoshuai Shi2
Guoshuai Shi2