- 1Department of Orthopedics, Bao’an Clinical Institute of Shantou University Medical College, Shantou, Guangdong, China
- 2Department of Orthopedics, Shenzhen Bao’an Shiyan People’s Hospital, Shenzhen, Guangdong, China
Background: The cardiometabolic index (CMI) is a novel metabolic biomarker, but research on its association with osteporosis (OP) is limited. The objective of this research was to clarify the relationship between CMI and OP in the older adult population of the United States.
Methods: This study conducted a cross-sectional analysis using NHANES data 2007–2018 with exclusion of 2011–2012 and 2015–2016 cycles. Logistic regression was used to investigate the relationship between CMI and OP prevalence. Restricted cubic spline curve (RCS) and threshold saturation analyses were performed to explore the nonlinear association between CMI and OP prevalence. Subgroup analyses, sensitivity analyses, and additional analyses were conducted to ensure the robustness and reliability of the findings.
Results: The study included 4,191 participants, revealing that those with OP had significantly lower CMI levels. Logistic regression revealed a strong inverse correlation between Log CMI and OP (OR = 0.72, 95% CI = 0.59–0.88), which persisted after adjusting for covariates. RCS analysis revealed a nonlinear inverse relationship with the critical threshold at CMI = 0.93. Below this threshold, each unit increase in CMI was associated with a 37% reduction in OP prevalence, but changes above this threshold were not significant. Subgroup and sensitivity analyses confirmed the robustness of the findings.
Conclusion: Elevated CMI exhibited a robust inverse correlation with the prevalence of OP in the older adult U.S. population. Maintaining a moderate CMI significantly diminishes the risk of developing OP.
1 Introduction
The deterioration of bone microstructure and significant reductions in bone mineral density (BMD) are the hallmarks of osteoporosis (OP), a systemic skeletal disease that leads to a substantially increased risk of fractures and increased bone fragility (1, 2). On a global scale, more than 19.7% of individuals are affected by OP, and the percentages are significantly greater among the older adult population (3). As the global population continues to get older, the occurrence of OP is expected to increase, posing a substantial challenge to public health systems (4). OP substantially elevates the risk of fragility fractures, leading to severe health issues, long-term disability, and a dramatic increase in medical costs and care needs (5, 6). Since OP often progresses without noticeable symptoms in its early stages, it is typically not detected until fractures occur. Hence, early identification and evaluation of risk factors linked to OP are essential for effective clinical interventions and treatment strategies.
Recent studies have established a strong connection between metabolic disorders and OP. Metabolic disorders not only are major risk factors for cardiovascular diseases and diabetes but also negatively impact bone health, contributing to the development and progression of OP (7–9). The cardiometabolic index (CMI) is a newly metabolic indicator that combines the waist-to-height ratio (WHtR) to measure obesity and the levels of triglycerides (TG) and high-density lipoprotein cholesterol (HDL-C) to evaluate lipid health (10). Research indicates that the CMI is a valuable tool for assessing the risk of diabetes-related conditions and is a reliable predictor of diabetes (11). Additionally, CMI has received considerable attention in the evaluation of various disease states (12–14). An observational study revealed a correlation between high CMI and a greater likelihood of experiencing depression (15). This suggests that by effectively controlling dyslipidemia and improving lipid profiles, the risk of developing depression might be reduced. Similarly, another study revealed a direct correlation between CMI and nonalcoholic fatty liver disease (NAFLD) and fibrosis, highlighting the potential of CMI as a reliable indicator of NAFLD and fibrosis (16). Current research has focused on the components of the cardiometabolic syndrome and their impact on bone health, but has often overlooked how composite metrics such as the CMI can provide a more comprehensive risk assessment (17–19). Previous research elucidating an integrated approach to nutritional and physiological assessment has been shown to be effective in predicting health outcomes (20). Based on these findings, the present study aims to fill this research gap by systematically exploring the relationship between CMI as a comprehensive metric and OP prevalence in the older adult population in the U.S. The aim is to provide strong theoretical support and practical guidance for early prevention and intervention strategies for OP.
2 Methods
2.1 Survey description
The National Health and Nutrition Examination Survey (NHANES) is a study using complex sampling methods representative of the U.S. population to assess nutrition and health. The National Center for Health Statistics (NCHS) Research Ethics Review Board reviews and authorizes research involving human subjects. Participants submitted written informed consent.
2.2 Study population
The following were the requirements for this study to be included: (1) were at least 50 years old; (2) had a proximal femur DXA scan and full data available for this scan; and (3) had complete data for waist circumference (WC), body height (BH), TG levels, and HDL-C levels.
2.3 Calculation of CMI
Based on anthropometric and laboratory data, the CMI was calculated using a formula that has been established in prior research. The initial calculation of the WHtR involved the use of WC (cm) and BH (cm). The CMI was subsequently calculated by integrating the levels of HDL-C and TG. The formula is as follows:
2.4 Definition of osteoporosis
Dual-energy X-ray absorptiometry (DXA) is widely acknowledged as the most reliable method for assessing BMD because of its quickness, ease of use, and low level of radiation exposure. NHANES conducted DXA scans of the proximal femur, which included the entire femur, femoral neck, trochanter, and intertrochanter, at mobile examination centers over the time periods of 2005–2010, 2013–2014, and 2017–2018. The T scores were computed using a comparison group consisting of non-Hispanic white women between the ages of 20 and 29, as recommended by the World Health Organization’s standards (Supplementary Table 1). Individuals whose T scores for total femur BMD, femoral neck BMD, trochanter BMD, or intertrochanter BMD were below −2.5 standard deviations were categorized as having OP (3, 21).
2.5 Covariates
This study accounted for multiple covariates, including demographic characteristics, lifestyle factors, health status, and laboratory examination data. The demographic factors included age, sex, race, poverty index ratio (PIR), and education level. Lifestyle variables included smoking status and levels of physical activity. Smoking status was determined by whether an individual had smoked over more than 100 cigarettes in their lifetime. Physical activity was assessed using the Global Physical Activity Questionnaire and quantified in metabolic equivalent (MET) minutes, with levels below less than 600 min per week categorized as inactive. Health status variables included chronic kidney disease, diabetes, and hypertension, as determined by physician diagnosis or self-reports. The laboratory data included the serum calcium, and serum phosphorus concentrations, and levels of the AST, ALT, SCR, and SUA levels.
2.6 Statistical analysis
Data from 2007 to 2018 were sourced from the NHANES, excluding the 2011–2012 and 2015–2016 cycles due to missing proximal femur DXA scan data, covering four survey cycles. Participants met the inclusion criteria, and descriptive analyses were performed by OP status. The association between CMI and OP prevalence was analyzed using univariate and multivariate logistic regression models, with CMI dichotomized to strengthen the robustness of the results. RCS and threshold saturation analyses revealed the nonlinear relationship and critical point between CMI and OP. Subgroup analyses considered factors such as age, sex, race, chronic kidney disease, diabetes, and hypertension. Sensitivity analyses confirmed the reliability and stability of the results. Additional studies have explored the correlation between CMI and BMD in various femur locations, supporting the validity of these findings. R software (version 4.2.3) was used for analyses, with a significance level of p < 0.05.
3 Results
3.1 Characteristics of study population
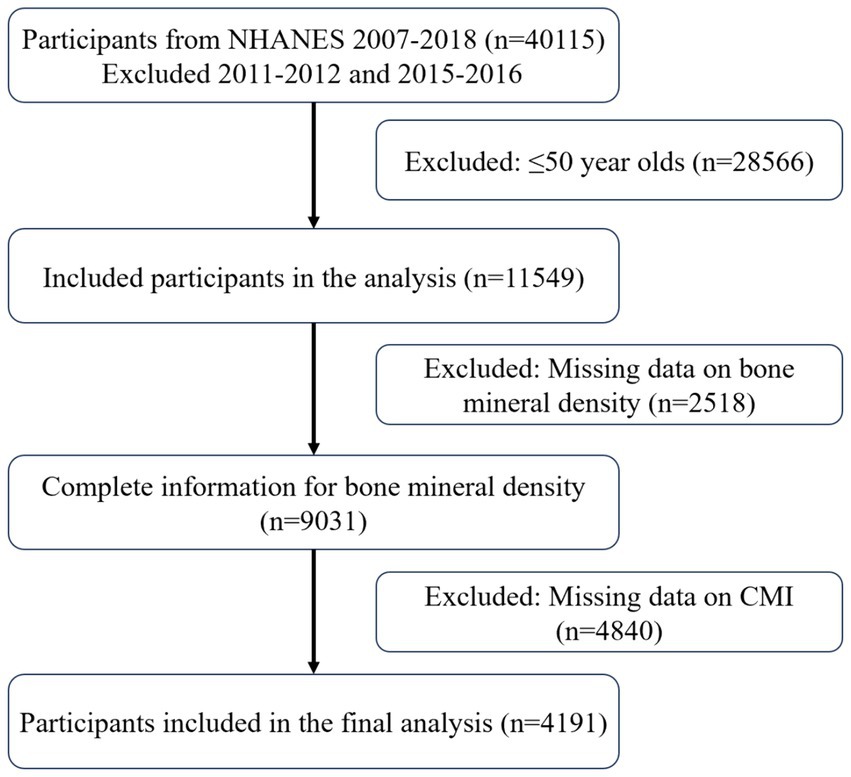
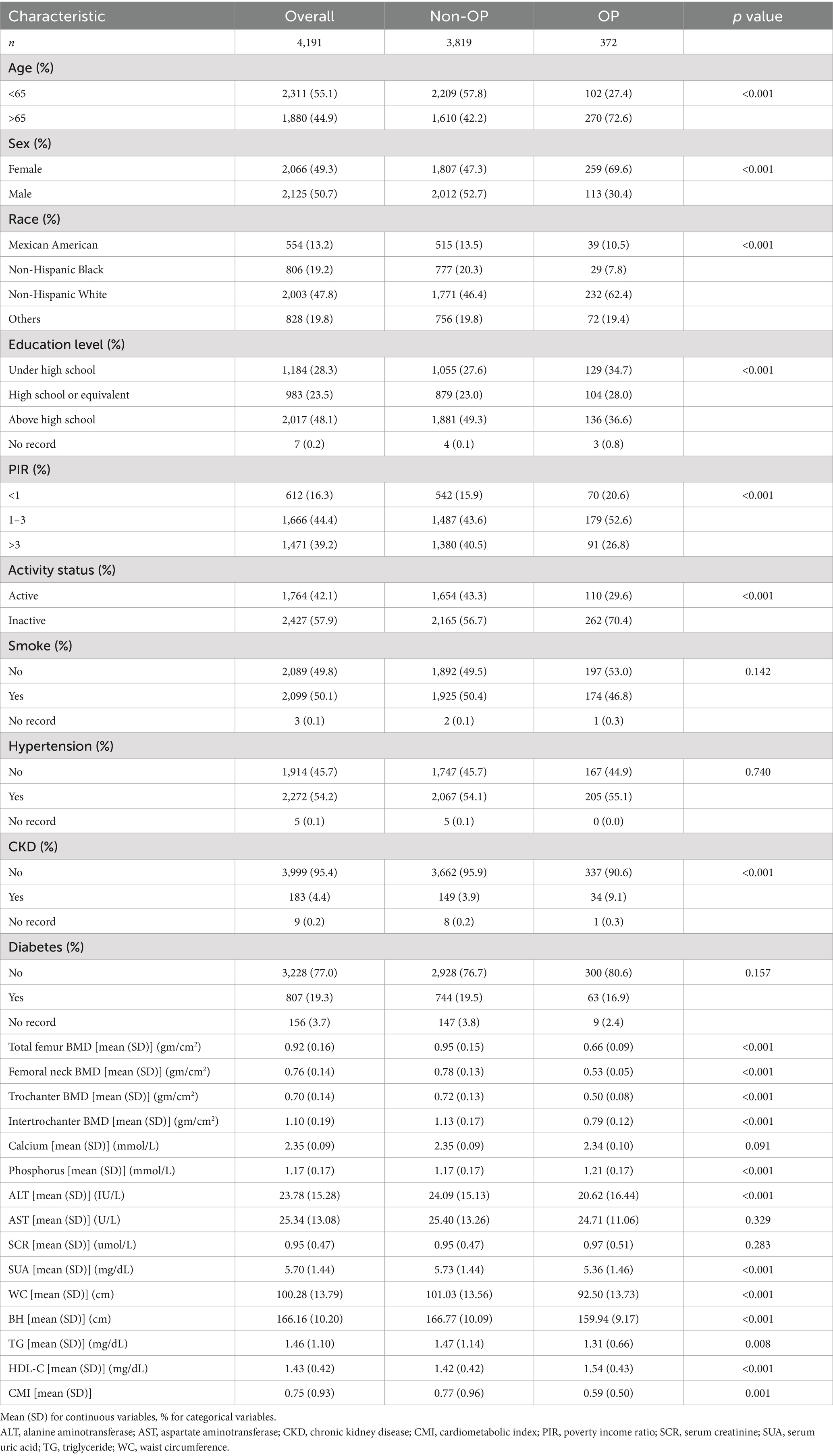
Figure 1 illustrates the selection process, which included 4,191 participants in the cross-sectional analysis. These participants consisted of 3,819 non-OP and 372 OP individuals. The baseline characteristics by OP status are detailed in Table 1. OP patients were typically older adult, had a greater proportion of females, were more likely to be non-Hispanic white, had lower education levels and moderate income levels, and participated in less physical activity. It is important to note that their CMI levels were lower.
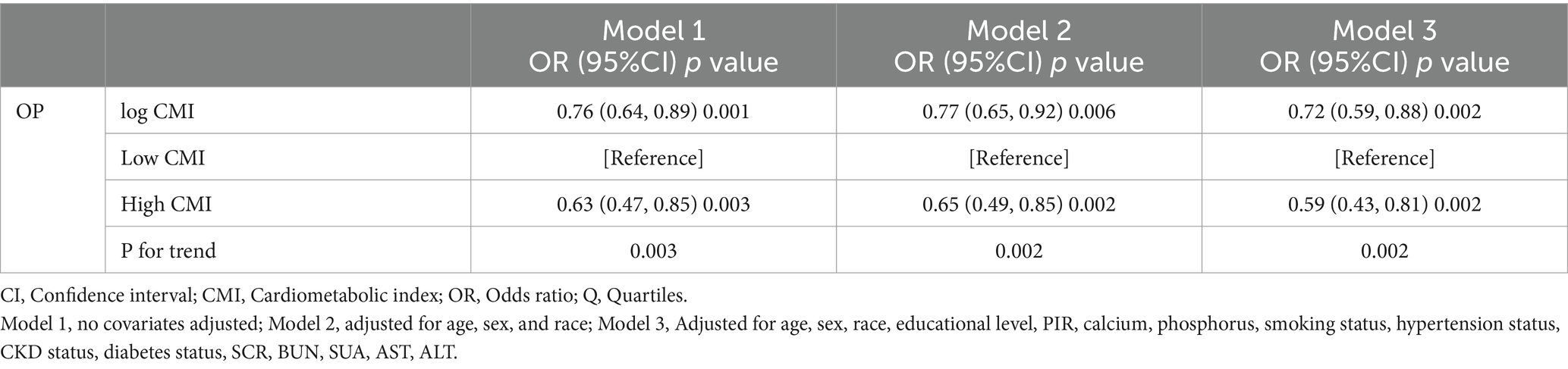
3.2 Association between CMI and proximal femur BMD
To address the left-skewed distribution of CMI, a logarithmic transformation was applied. The results of the logistic regression analysis that examined the relationship between CMI and OP are summarized in Table 2. Model 1 revealed a negative correlation between Log CMI and OP (OR = 0.76, 95% CI = 0.64–0.89). Model 3, which was adjusted for a variety of covariates, demonstrated that a 28% decrease in the prevalence of OP was associated with each unit increase in Log CMI (OR = 0.72, 95% CI = 0.59–0.88). When CMI was dichotomized, a high CMI was significantly negatively associated with OP compared to a low CMI (OR = 0.59, 95% CI = 0.43–0.81). These results indicate a consistent negative association between CMI and OP.
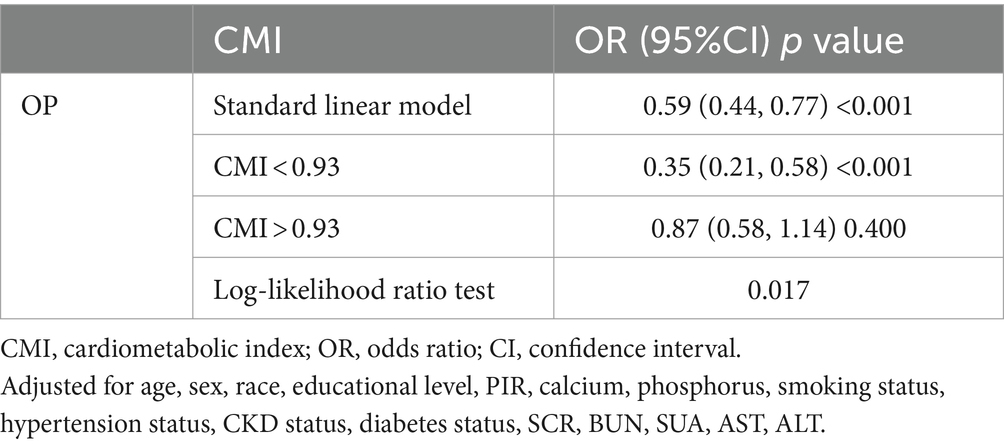
3.3 Nonlinear relationship and threshold effect analysis
Figure 2 depicts the link between the CMI dosage and the occurrence of OP, as determined by the RCS analysis. The graph shows a nonlinear negative association (P-nonlinear = 0.0368). Threshold effect analysis identified a critical point between CMI and the prevalence of OP at CMI = 0.92. Table 3 shows the relationship between CMI and the prevalence of OP on either side of the critical point. On the left side of the critical point, the prevalence of OP decreases with increasing CMI; on the right side, changes in CMI have no statistically significant impact on the prevalence of OP.
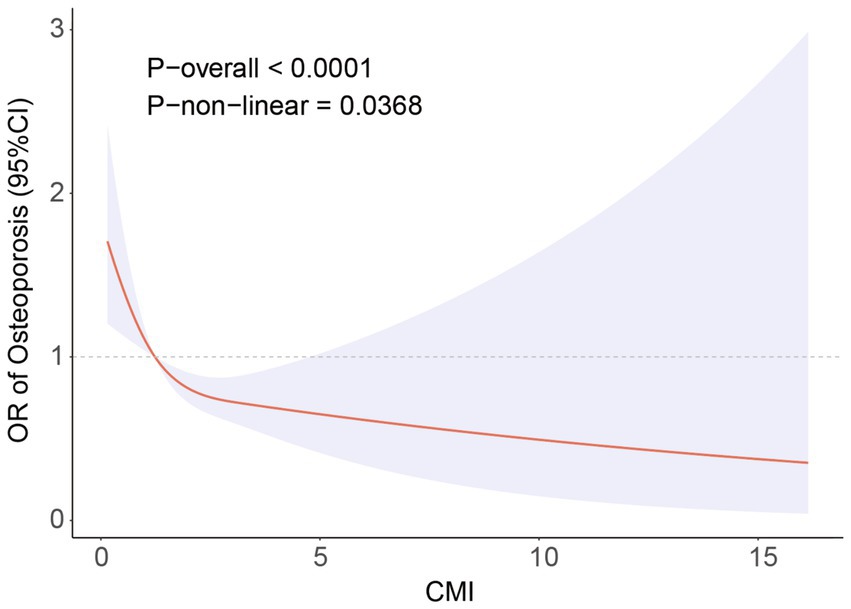
Figure 2. RCS analysis showing the relationship between CMI and OP. Adjusted for age, sex, race, educational level, PIR, calcium, phosphorus, smoking status, hypertension status, CKD status, diabetes status, SCR, BUN, SUA, AST, ALT.
3.4 Subgroup analysis
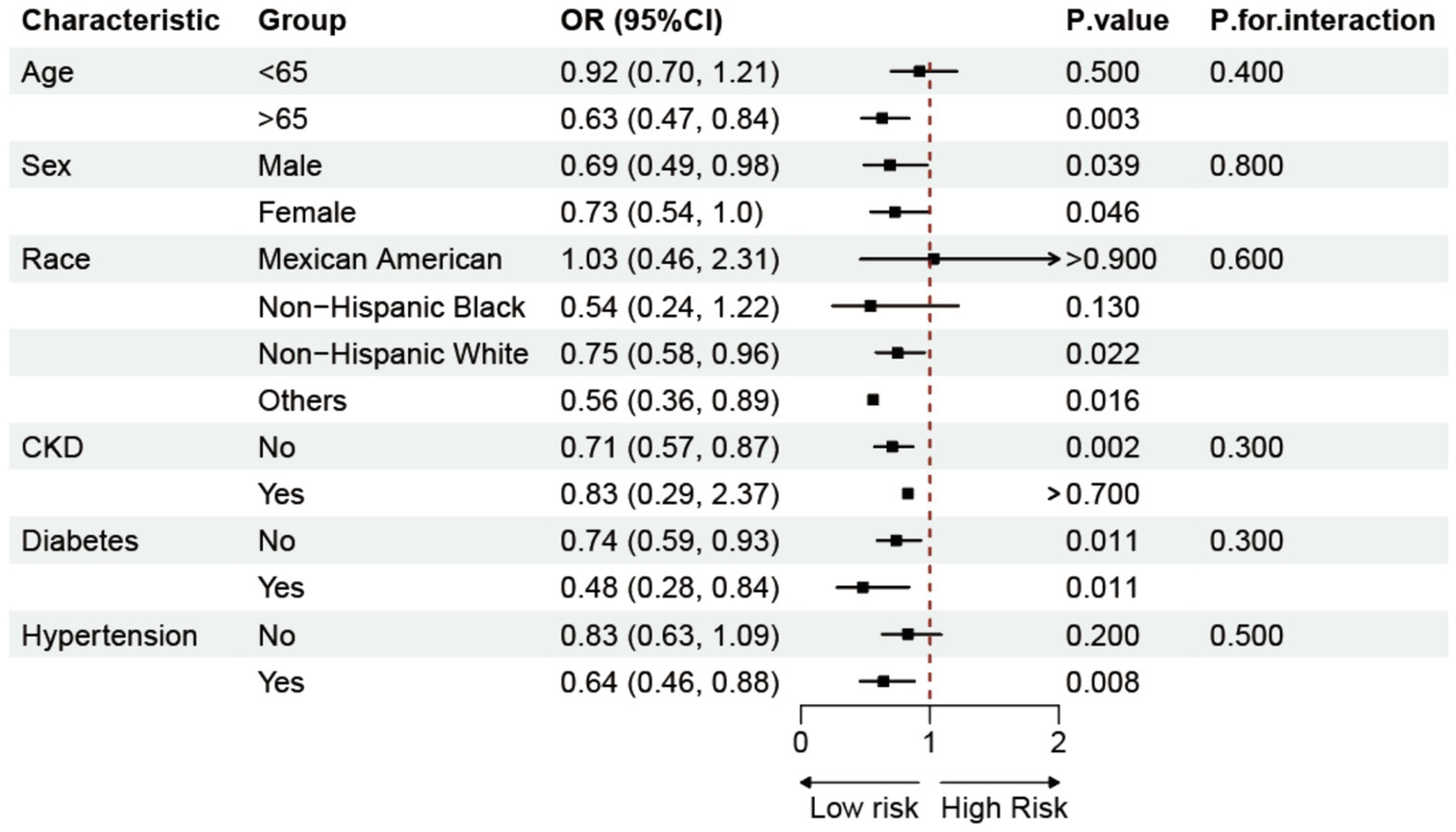
To explore the potential influencing factors between CMI and the prevalence of OP, we conducted a subgroup study, combining characteristics such as age, gender, race, chronic kidney disease, diabetes, and hypertension (Figure 3). The results of the analyses showed that the negative association between CMI and OP was more pronounced in people over 65 years of age, whereas the association was not significant in people under 65 years of age. However, the interaction analysis did not find a significant interaction between these factors and the relationship between CMI and OP.
3.5 Sensitivity and additional analysis
Sensitivity analyses were implemented to confirm the consistency and robustness of the studies (Supplementary Table 2). After excluding participants with a CMI ± 3 SDs, 4,140 participants remained. After fully adjusting for covariates, the negative association between CMI and the prevalence of OP remained stable. This relationship was also validated when the CMI was dichotomized. Finally, additional analyses were performed. Linear regression analysis demonstrated a consistent positive correlation between CMI and BMD in various regions of the femur, as illustrated in Supplementary Table 3. Supplementary Figures 1–4 demonstrate that the RCS analysis revealed a nonlinear positive relationship between CMI and BMD in several areas of the femur, with the BMD progressively increasing as the CMI increased.
4 Discussion
This research analyzed data from 4,191 individuals to explore the relationship between CMI and OP in the older population of the United States. After accounting for several factors, the results confirmed that the inverse association between CMI and OP occurrence persisted. Notably, RCS analysis revealed a nonlinear negative correlation between CMI and OP prevalence, identifying a critical point at CMI = 0.93 through a threshold saturation effect. An increase in CMI within a certain range was linked to a decrease in the occurrence of OP. Subgroup analysis further showed that this negative correlation remained stable across various populations. Finally, sensitivity and supplementary analyses reinforced the robustness and consistency of the findings. These results suggest that within a specific range, CMI may be a protective factor against OP, and further research on CMI could aid in the prevention and delay of OP progression.
In recent years, obesity has grown to be a significant global public health concern. It is associated with higher death rates and an increase in the prevalence of chronic illnesses such diabetes, hypertension, and dyslipidemia (22–24). The connection between obesity and bone metabolism has garnered increasing attention (25). Research has suggested that central obesity, with WC serving as a significant measure, may offer protection against OP. Current research indicates that WC contributes to BMD maintenance as well (18). Another study confirmed that the obesity index (WC, WHtR, BMI) was negatively associated with the risk of OP in older adults (17). People with obesity often have lipid metabolism issues, which are strongly connected to bone health. A study conducted on individuals between the ages of 20 and 59 years revealed a positive correlation between HDL-C levels and BMD in the lumbar spine (26). Subgroup analyses showed that the negative association between CMI and OP was more pronounced in specific populations. This may be due to the fact that older adults are more susceptible to the adverse effects of metabolic abnormalities on bone health, especially when bone loss is more pronounced, potentially making CMI a stronger predictor of OP in these patients (27). However, interaction analyses showed that although CMI was more strongly associated with OP in specific populations, these characteristics did not significantly alter the overall negative correlation between the two, suggesting that CMI, as a composite metabolic index, is generalizable to OP across populations. In summary, CMI as a comprehensive indicator can integrate the roles of multiple metabolic components and simplify the complex process of assessing metabolic syndrome, thus providing a wide range of applications in clinical practice.
Although the precise mechanisms underlying the connection between CMI and OP remain unclear, several hypotheses may explain this link. CMI is a comprehensive indicator to assess obesity and lipid metabolism, which may further respond to OP through adipose tissue and metabolic pathways response pathways. The interplay between obesity and OP is complex and multifaceted, encompassing both protective and risk factors (28, 29). Humans experience the production of cytokines, such as IL-1β, TNF-α, and IL-6, from their adipose tissue. These cytokines can activate intracellular signaling pathways, which may result in the loss of bone mass (30). Moreover, disturbances in lipid metabolism play a crucial role in influencing bone health. Obesity-induced dyslipidemia is characterized by elevated levels of lipoproteins rich in TG and reduced levels of HDL-C (24). Oxidized lipids stimulate the transformation of mesenchymal stem cells (MSCs) into adipocytes, but increased levels of cholesterol in the bloodstream suppress the Wnt signaling pathway, which impacts the differentiation of MSCs into osteoblasts (31, 32). Oxidized lipids and cholesterol disrupt the balance between osteoblasts and osteoclasts, affecting bone microenvironment homeostasis and potentially leading to OP (33–35). Moreover, a high TG/HDL-C ratio is a significant marker of insulin resistance and metabolic syndrome and can worsen lipid metabolism disorders, impair osteoblast function, and reduce BMD (36, 37). Our study suggested that CMI is a protective factor against OP, exhibiting a saturation threshold effect. When the CMI falls below the designated threshold, the combined effects of mechanical stress and hormone production have a favorable impact on bones, leading to an increase in BMD. In contrast, the initial positive effects on bone health might be offset by factors like the accumulation of abdominal fat, shifts in body composition, proinflammatory conditions, and insulin resistance once the CMI surpasses this limit. Thus, the relationship between CMI and OP arises from multifactorial and multipathway interactions, necessitating further research to fully understand the biological mechanisms involved in the connection between CMI and bone metabolism.
Our study has several strengths. First, OP is prevalent among older adult individuals, and a national sample of people over 50 years old was selected to address this concern. Second, various covariates were included to control for potential confounding factors. Ultimately, sensitivity and supplemental studies were conducted to verify the strength and reliability of the results. Nevertheless, this research has several limitations. The cross-sectional design restricts the capacity to establish a causal relationship between CMI and OP. In addition, certain variables in this study were collected through self-reported methods, which may have introduced biases such as recall inaccuracies and reporting errors, and these data relied on the memory and honesty of the participants. Despite the sophisticated sampling techniques utilized in this study, the results may not reflect the true situation with complete accuracy. The population analyzed in this study was the older American population, and these results still need to be validated in the future with more extensive surveys of other ethnic populations and age groups. Numerous prospective studies are still needed in the future to further validate the causal association between CMI and OP.
5 Conclusion
According to the results of this study, higher CMI is strongly associated with a lower prevalence of OP in the older U.S. population, and maintaining a certain level of CMI may help to reduce the prevalence of OP. This result suggests that accurate management and optimization of CMI may be a key strategy for preventing and reducing the risk of OP.
Data availability statement
The National Health and Nutrition Examination Survey (NHANES) data is a publicly available database for use by personnel worldwide, and all data are available at https://www.cdc.gov/nchs/nhanes/nhanes_products.htm.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the patients/participants or the patients’/participants’ legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
DL: Data curation, Formal analysis, Methodology, Writing – original draft. JL: Data curation, Software, Writing – original draft. YL: Project administration, Validation, Writing – review & editing. WD: Resources, Validation, Writing – review & editing. ZL: Conceptualization, Methodology, Writing – review & editing.
Funding
The author(s) declare no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We are appreciative that the National Center for Medical Research at the Institute of Prevention and Control of Disorders has made the National Health and Nutritional Evaluation Survey available to all citizens of the country.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1462169/full#supplementary-material
Abbreviations
ASM, appendicular skeletal muscle mass; BH, body height; BMD, bone mineral density; BMI, body mass index; CI, confidence interval; CMI, cardiometabolic index; DXA, dual-energy X-ray absorptiometry; HDL-C, high-density lipoprotein cholesterol; MET, metabolic equivalent; NHANES, National Health and Nutrition Examination Survey; OP, osteoporosis; OR, odds ratio; PIR, poverty income ratio; SMI, skeletal muscle index; TG, triglyceride; WC, waist circumference; WHtR, waist-to-height ratio.
References
1. Johnston, CB, and Dagar, M. Osteoporosis in older adults. Med Clin North Am. (2020) 104:873–84. doi: 10.1016/j.mcna.2020.06.004
2. Walker, MD, and Shane, E. Postmenopausal osteoporosis. N Engl J Med. (2023) 389:1979–91. doi: 10.1056/NEJMcp2307353
3. Xiao, PL, Cui, AY, Hsu, CJ, Peng, R, Jiang, N, Xu, XH, et al. Global, regional prevalence, and risk factors of osteoporosis according to the World Health Organization diagnostic criteria: a systematic review and meta-analysis. Osteoporosis Int. (2022) 33:2137–53. doi: 10.1007/s00198-022-06454-3
4. Bouvard, B, Annweiler, C, and Legrand, E. Osteoporosis in older adults. Joint Bone Spine. (2021) 88:105135. doi: 10.1016/j.jbspin.2021.105135
5. Lo, JC, Yang, W, Park-Sigal, JJ, and Ott, SM. Osteoporosis and fracture risk among older US Asian adults. Curr Osteoporos Rep. (2023) 21:592–608. doi: 10.1007/s11914-023-00805-7
6. Barron, RL, Oster, G, Grauer, A, Crittenden, DB, and Weycker, D. Determinants of imminent fracture risk in postmenopausal women with osteoporosis. Osteoporosis Int. (2020) 31:2103–11. doi: 10.1007/s00198-020-05294-3
7. Ali, D, Tencerova, M, Figeac, F, Kassem, M, and Jafari, A. The pathophysiology of osteoporosis in obesity and type 2 diabetes in aging women and men: the mechanisms and roles of increased bone marrow adiposity. Front Endocrinol. (2022) 13:981487. doi: 10.3389/fendo.2022.981487
8. Shi, W, and Zhang, Q. Association between metabolic syndrome and the musculoskeletal system. Nutrients. (2023) 15:4475. doi: 10.3390/nu15204475
9. Sheu, A, Greenfield, JR, White, CP, and Center, JR. Assessment and treatment of osteoporosis and fractures in type 2 diabetes. Trends Endocrinol Metab. (2022) 33:333–44. doi: 10.1016/j.tem.2022.02.006
10. Xi, WF, and Yang, AM. Association between cardiometabolic index and controlled attenuation parameter in U.S. adults with NAFLD: findings from NHANES (2017-2020). Lipids Health Dis. (2024) 23:40. doi: 10.1186/s12944-024-02027-x
11. Wakabayashi, I, and Daimon, T. The "cardiometabolic index" as a new marker determined by adiposity and blood lipids for discrimination of diabetes mellitus. Clin Chim Acta. (2015) 438:274–8. doi: 10.1016/j.cca.2014.08.042
12. He, L, Lin, C, Tu, Y, Yang, Y, Lin, M, Tu, H, et al. Correlation of cardiometabolic index and sarcopenia with cardiometabolic multimorbidity in middle-aged and older adult: a prospective study. Front Endocrinol. (2024) 15:1387374. doi: 10.3389/fendo.2024.1387374
13. Liu, X, Wu, Q, Yan, G, Duan, J, Chen, Z, Yang, P, et al. Cardiometabolic index: a new tool for screening the metabolically obese normal weight phenotype. J Endocrinol Investig. (2021) 44:1253–61. doi: 10.1007/s40618-020-01417-z
14. Sun, Q, Ren, Q, Du, L, Chen, S, Wu, S, Zhang, B, et al. Cardiometabolic index (CMI), lipid accumulation products (LAP), waist triglyceride index (WTI) and the risk of acute pancreatitis: a prospective study in adults of North China. Lipids Health Dis. (2023) 22:190. doi: 10.1186/s12944-023-01948-3
15. Zhou, X, Tao, XL, Zhang, L, Yang, QK, Li, ZJ, Dai, L, et al. Association between cardiometabolic index and depression: National Health and nutrition examination survey (NHANES) 2011-2014. J Affect Disord. (2024) 351:939–47. doi: 10.1016/j.jad.2024.02.024
16. Yan, L, Hu, X, Wu, S, Cui, C, and Zhao, S. Association between the cardiometabolic index and NAFLD and fibrosis. Sci Rep. (2024) 14:13194. doi: 10.1038/s41598-024-64034-3
17. Tian, H, Pan, J, Qiao, D, Dong, X, Li, R, Wang, Y, et al. Adiposity reduces the risk of osteoporosis in Chinese rural population: the Henan rural cohort study. BMC Public Health. (2020) 20:285. doi: 10.1186/s12889-020-8379-4
18. Pan, R, Wang, R, Zhang, Y, Ji, H, Liang, X, and Zhao, Y. The association of waist circumference with bone mineral density and risk of osteoporosis in US adult: national health and nutrition examination survey. Bone. (2024) 185:117134. doi: 10.1016/j.bone.2024.117134
19. Kan, B, Zhao, Q, Wang, L, Xue, S, Cai, H, and Yang, S. Association between lipid biomarkers and osteoporosis: a cross-sectional study. BMC Musculoskelet Disord. (2021) 22:759. doi: 10.1186/s12891-021-04643-5
20. Irandoust, KJHN . The interplay of nutrition, physiology, and performance in sports: a comprehensive review. Health Nexus. 1 (2023) 21–30. doi: 10.61838/kman.hn.1.3.3
21. Siris, ES, Adler, R, Bilezikian, J, Bolognese, M, Dawson-Hughes, B, Favus, MJ, et al. The clinical diagnosis of osteoporosis: a position statement from the National Bone Health Alliance Working Group. Osteoporosis Int. (2014) 25:1439–43. doi: 10.1007/s00198-014-2655-z
22. Golden, A . Obesity’s impact. Nurs Clin North Am. (2021) 56:XIII–XIV. doi: 10.1016/j.cnur.2021.08.004
23. Piché, ME, Tchernof, A, and Després, JP. Obesity phenotypes, diabetes, and cardiovascular diseases. Circ Res. (2020) 126:1477–500. doi: 10.1161/CIRCRESAHA.120.316101
24. Stadler, JT, and Marsche, G. Obesity-related changes in high-density lipoprotein metabolism and function. Int J Mol Sci. (2020) 21:8985. doi: 10.3390/ijms21238985
25. Rinonapoli, G, Pace, V, Ruggiero, C, Ceccarini, P, Bisaccia, M, Meccariello, L, et al. Obesity and bone: a complex relationship. Int J Mol Sci. (2021) 22:13662. doi: 10.3390/ijms222413662
26. Xie, R, Huang, X, Liu, Q, and Liu, M. Positive association between high-density lipoprotein cholesterol and bone mineral density in U.S. adults: the NHANES 2011-2018. J Orthop Surg Res. (2022) 17:92. doi: 10.1186/s13018-022-02986-w
27. Pignolo, RJ . Aging and bone metabolism. Compr Physiol. (2023) 13:4355–86. doi: 10.1002/cphy.c220012
28. Liu, Y, Liu, Y, Huang, Y, Le, S, Jiang, H, Ruan, B, et al. The effect of overweight or obesity on osteoporosis: a systematic review and meta-analysis. Clin Nutr. (2023) 42:2457–67. doi: 10.1016/j.clnu.2023.10.013
29. Piñar-Gutierrez, A, García-Fontana, C, García-Fontana, B, and Muñoz-Torres, M. Obesity and bone health: a complex relationship. Int J Mol Sci. (2022) 23:8303. doi: 10.3390/ijms23158303
30. Wang, X, Zhang, C, Zhao, G, Yang, K, and Tao, L. Obesity and lipid metabolism in the development of osteoporosis (review). Int J Mol Med. (2024) 54:61. doi: 10.3892/ijmm.2024.5385
31. Maeda, K, Kobayashi, Y, Koide, M, Uehara, S, Okamoto, M, Ishihara, A, et al. The regulation of bone metabolism and disorders by Wnt signaling. Int J Mol Sci. (2019) 20:5525. doi: 10.3390/ijms20225525
32. Hu, L, Yin, C, Zhao, F, Ali, A, Ma, J, and Qian, AJIJOMS. Mesenchymal stem cells: cell fate decision to osteoblast or adipocyte and application in osteoporosis treatment. Int J Mol Sci. (2018) 19:360. doi: 10.3390/ijms19020360
33. Che, Y, Yang, J, Tang, F, Wei, Z, Chao, Y, Li, N, et al. New function of cholesterol oxidation products involved in osteoporosis pathogenesis. Int J Mol Sci. (2022) 23:2020. doi: 10.3390/ijms23042020
34. Park-Min, KH . Metabolic reprogramming in osteoclasts. Semin Immunopathol. (2019) 41:565–72. doi: 10.1007/s00281-019-00757-0
35. Kong, X, Tao, S, Ji, Z, Li, J, Li, H, Jin, J, et al. FATP2 regulates Osteoclastogenesis by increasing lipid metabolism and ROS production. J Bone Miner Res Off J Am Soc Bone Miner Res. (2024) 39:737–52. doi: 10.1093/jbmr/zjae034
36. Oliveri, A, Rebernick, RJ, Kuppa, A, Pant, A, Chen, Y, Du, X, et al. Comprehensive genetic study of the insulin resistance marker TG:HDL-C in the UK biobank. Nat Genet. (2024) 56:212–21. doi: 10.1038/s41588-023-01625-2
Keywords: cardiometabolic index, osteoporosis, bone density, cross-sectional study, NHANES
Citation: Li D, Li J, Li Y, Dong W and Lin Z (2024) Association between the cardiometabolic index and osteoporosis: a cross-sectional study of the NHANES. Front. Public Health. 12:1462169. doi: 10.3389/fpubh.2024.1462169
Edited by:
Morteza Taheri, University of Tehran, IranReviewed by:
Khadijeh Irandoust, Imam Khomeini International University, IranElahe Arab Ameri, University of Tehran, Iran
Copyright © 2024 Li, Li, Li, Dong and Lin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhuofeng Lin, NTQyNzkxNDY0QHFxLmNvbQ==
†These authors have contributed equally to this work
 Deyan Li
Deyan Li Jinli Li1,2†
Jinli Li1,2†