- 1School of Nursing, Duke University, Durham, NC, United States
- 2School of Medicine, Duke University, Durham, NC, United States
Introduction: We examined the influence of special healthcare needs, onset of the COVID-19 pandemic, and their interaction on receiving transition services to prepare for future adult care among US adolescents, and whether social determinants of health moderated the relationship of these factors with receiving transition services.
Methods: We analyzed the National Survey of Children's Health (2019, 2020–2021) using adjusted multivariable logistic regression models. We assessed a repeated cross-sectional, nationally representative sample of adolescents aged 12–17 years old. Sampling weights were used to generalize samples to the populations of interest. The main outcome was receipt of transition services to prepare for future adult healthcare. Measures included pre vs. post COVID-19 onset, special healthcare needs, and social determinants of health (health insurance, food sufficiency, neighborhood safety, household language, race/ethnicity, and household poverty level). Sex and two-parent households were included as covariates.
Results: A total of 45,935 adolescents were included, with N=12,230 in the pre COVID-19 group and N=33,705 in the post COVID-19 group. We found statistically significant higher odds of receiving transition services among adolescents with special healthcare needs (95 CI = 1.23, 1.58), females (95 CI = 1.09, 1.39), and during pre COVID-19 (95 CI = 1.14, 1.45). Private insurance (95 CI = 1.03, 1.37), English as primary household language (95 CI = 1.19, 2.27), and race/ethnicity were significant predictors of receipt of transition services. Neighborhood safety significantly moderated (95 CI = 1.70, 6.60) the relationship between special healthcare needs and receipt of transition services.
Discussion: This population-based study identified significant disparities in receipt of transition services provided to US adolescents via the differential impact of social determinants of health, special healthcare needs, and COVID-19 onset on receipt of services.
1 Introduction
Despite national priorities to support adolescents transitioning from pediatric to adult healthcare, US-wide surveys continue to document low rates of adolescents receiving transition services that could prepare them to thrive in adult-focused environments (1). Providing all adolescents services that develop their health literacy, self-care skills, and smooth the transition process is necessary as they develop and experience changes in healthcare status, care providers, work, school, and lifestyles (2). Prior to 2020, transition programs for adolescents with or without special healthcare needs (SHCN) were not widely available outside of children's hospitals (3). The disruption of the COVID-19 pandemic onset in 2020 created additional challenges in providing transition services (4, 5). Most recently, an estimated 11.8 million US adolescents experienced missed or delayed care visits in 2022 due to COVID, indicating potential gaps in care coordination (1).
Gaps in receiving services to prepare for transition are also influenced by social determinants of health (SDOH) like household poverty level, race and ethnicity, food insufficiency, and unsafe neighborhoods (6, 7). The consequences of inadequate transition preparation include increased risk for mental health comorbidities, low medication adherence, and poor health outcomes (2, 8, 9). This may be especially detrimental to adolescents with SHCN like sickle cell disease or cystic fibrosis for whom the transition is made more challenging due to complex disease management and treatment regimens (3, 9, 10). Notably, unnecessary admissions, complications, and readmissions resulting from failed care coordination/transitional care cost the U.S. healthcare system an estimated $27.2–78.2 billion dollars annually (11).
Researchers have identified the COVID-19 pandemic and SDOH as key forces impacting the health of transition-age adolescents in the US (4–7, 12). COVID-19 has impacted socio-economic opportunities for families, worsened social determinants of health, and created delays in transitions to adult healthcare (4, 5, 12). Additionally, adolescent females and adolescents residing in two-parent households have higher rates of receiving transition services/preparation compared to their peers (13). Studies suggest adolescents without SHCN receive less transition-related information from providers than adolescents with SHCN (5). However, while researchers have investigated the associations between person- and family-centered factors and the receipt of transitional care, there is a gap in exploring associations between systemic factors (i.e., COVID-19 pandemic) and multi-level SDOH factors on receipt of transition services (6, 7, 13, 14). This gap makes it difficult to understand health inequities inherent in receipt of transitional care provided to diverse adolescents in the US (6, 7, 13, 14).
Thus, our study goal was to determine whether US adolescents with SHCN were less likely to receive transition services to prepare for future adult healthcare compared to their peers, and to evaluate the differential impact of COVID-19 onset on receipt of these services among those with special healthcare needs and those without. Additionally, we examined SDOH that modified the effect of SHCN and COVID-19 on receipt of transition services. Hence, we aimed to determine the influence of SHCN, onset of COVID-19, and their interaction on the receipt of transition services, covarying for adolescent sex and two-parent household (13). Further, we aimed to identify SDOH that moderated the impact of these two factors (SHCN and/or COVID-19) on receipt of services, covarying for adolescent sex and two-parent household.
2 Methods
2.1 Design
We used a cross-sectional 2 × 2 factorial design to explore data from the 2019 and the combined 2020 and 2021 National Survey of Children's Health (NSCH), which enrolls a repeated cross-sectional nationally representative sample of youth aged 0–17 years old in the U.S. each year (15–17). The data were collected from independent samples, with 2019 data collected prior to the COVID-19 pandemic onset and 2020–2021 data obtained after COVID-19 onset. The Duke University Institutional Review Board determined this study as exempt as data were anonymized and publicly available. Data were reported using the STROBE statement (see Supplementary Table 2) (18).
2.2 Data source
The NSCH is a publicly available, fully-deidentified database with data collected each enrollment year from caregivers via an online or paper survey about one randomly selected child in their household (15). The NSCH survey included items on healthcare, individual and family characteristics, and school and community factors (19–21). Survey data elements were collected from June 2019 to January 2020 for the 2019 dataset (weighted survey response rate: 42.4%) (19), July 2020 to January 2021 for the 2020 dataset (weighted survey response rate: 42.4%) (20), and June 2021 to January 2022 for the 2021 dataset (weighted survey response rate: 40.3%) (21).
2.3 Participants
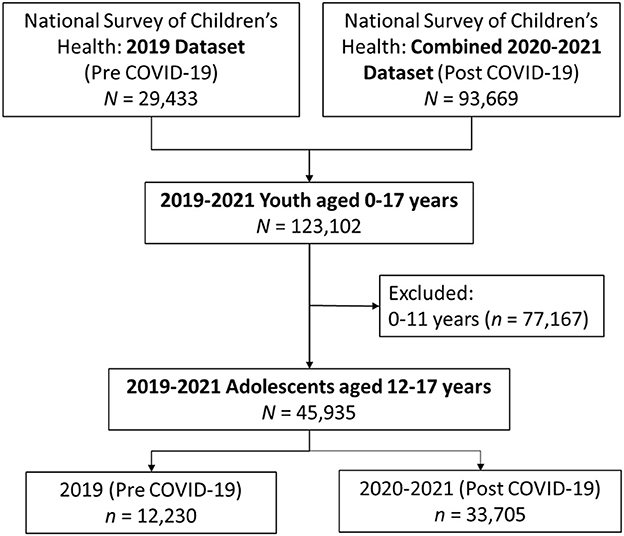
For this study, we included only data on transition-age adolescents (12–17 years) with and without special healthcare needs. The final analysis sample was 45,935 adolescents, with N = 12,230 in the pre COVID-19 group and N = 33,705 in the post COVID-19 group (see Figure 1).
2.4 Measures
Key analytic measures, definitions, and coding for the final analyses are summarized in Supplementary Table 1.
2.4.1 Main outcome
The outcome was receipt of preparation services for transition to adult healthcare, coded as no (0) or yes (1). Hereafter referred to as “transition services”, this outcome was defined as having received early development of self-care skills, one-on-one provider communication skills, and information on the transition process and changes in healthcare. This outcome was derived in the dataset from three components: (1) doctor spoke with the adolescent privately without an adult in the room during the last medical care visit, (2) a discussion about transitioning to adult care occurred, and (3) doctors actively worked with the adolescent to gain skills and understand changes in healthcare (16, 17). If there was a yes response to any of the three items, then the adolescent was coded as having received transition services.
2.4.2 Special healthcare needs
Special healthcare needs of adolescents (SHCN vs. no SHCN) was operationalized by the Maternal and Child Health Bureau's consequences-based definition of children, with SHCN defined as an adolescent experiences a medical or health condition lasting 12 months or more that requires prescription medication, or above average use of medical/mental/educational services, or has functional limitations, or requires utilization of specialized therapies, or incurs treatment for emotional or developmental problems (16, 17). We chose a binary assessment of special healthcare needs because despite complexity of care, adolescents with any special healthcare needs utilize a larger portion of healthcare and financial resources, they require services beyond what is generally required by adolescents, and they require care coordination among primary care, medical specialty, and/or nonmedical specialty providers compared to adolescents with no special healthcare needs (22).
2.4.3 COVID-19 onset group
Adolescents were divided into two groups based on whether the data were collected before (year 2019) or after (years 2020–2021) the onset of the COVID-19 pandemic (pre- vs. post-COVID).
2.4.4 Social determinants of health
Seven social determinants of health were considered including private health insurance (no, yes); public health insurance (no, yes); food sufficiency (sometimes/often not afford enough to eat, always could afford enough to eat but not always nutritious meals, always afford to eat nutritious meals); safe neighborhood (definitely agree, somewhat agree, somewhat/definitely disagree); household language (English, not English); race and ethnicity (Hispanic individuals, White non-Hispanic, Black non-Hispanic, Asian non-Hispanic, Other/multi-racial non-Hispanic); and household poverty level (no, yes—defined as 0–99% federal poverty level, FPL).
2.4.5 Covariates
Sex (male, female) and two-parent household (no, yes) were included as covariates based on prior literature (13). Two-parent household was defined as two parents (married or not) who lived in the same household. The dataset only included adolescent age groups (i.e., 0–5 years, 6–11 years, 12–17 years) and not individual ages and thus age was not included as a covariate (16, 17).
2.4.6 Design variables
The NCSH datasets provided survey design variables to obtain better parameter estimates, particularly standard error. The variables account for the complex survey design and adjust for under- or over-representation of subpopulations. Design variables applied were individual sampling weights (FWC), two strata variables (FIPSST, state of residence; STRATUM, identified households with children), and a cluster variable (HHID, unique household identifier) (16, 17).
2.5 Data analysis
Descriptive statistics were used to detail sample characteristics and key analytic variables. Non-directional statistical tests were performed with statistical significance set at 0.05. Effect sizes and their 95% confidence intervals were used to address clinical significance. Using SAS 9.4 software (Cary, NC) (23), data were analyzed with procedures designed for population-based research, thus, weighted analyses incorporated sampling weights and other design variables.
2.5.1 Sample characteristics
The sample characteristics for the two COVID-19 groups were described and compared using Rao-Scott chi-square tests. Characteristics included SDOH, covariates, SHCN, and transition services.
2.5.2 Transition services: role of COVID-19 onset and special healthcare needs
Covariate-adjusted multivariable logistic regression was used to examine the effects of COVID-19 group and SHCN and their interaction on transition services, after covarying for sex and two-parent household. The event of interest was receipt of transition services (1, yes). In the event of a significant interaction at the 0.05 level, a posteriori subgroup comparisons were planned to further delineate the interaction. Adjusted odds ratios (aORs) and 95% confidence intervals (CIs) were used to evaluate clinical significance (24).
2.5.3 Transition services: moderating effects of social determinants of health
Seven SDOH were examined to determine whether the characteristic was either a non-specific predictor or moderator of the relationship between COVID-19 group and/or SHCN with transition services, after covarying for sex and two-parent household. Each SDOH was evaluated in separate multivariable logistic regression models in which the SDOH of interest and SDOH interactions were added to the core model described above. Each model included the following explanatory variables: (a) COVID-19 group and SHCN factors and their interaction; (b) sex and two-parent household as covariates; and (c) SDOH and its two-way and three-way interaction with the factors. If the COVID-by-SHCN interaction was not statistically significant at the 0.05 level, this interaction term and COVID-by-SHCN-by-SDOH interaction were both dropped from the final pragmatic moderator model. The SDOH was determined to be a non-specific predictor of transition services if only the main effect was statistically significant. The SDOH was determined to be a moderator when a two-way SDOH interaction with COVID and/or SHCN or a three-way interaction with COVID and SHCN was statistically significant.
2.6 Statistical power
The expected sample sizes for adolescents pre vs. post COVID-19 and SHCN vs. no SHCN provided at least 80% statistical power to test for main and interaction effects on transition services in a multivariable logistic regression model, covarying for SDOH and covariate terms and assuming two-tailed tests with significance set at 0.05 and small effect sizes (when aOR > 1: small effect = 1.50 or when aOR < 1: small effect = 0.67).
3 Results
3.1 Sample characteristics
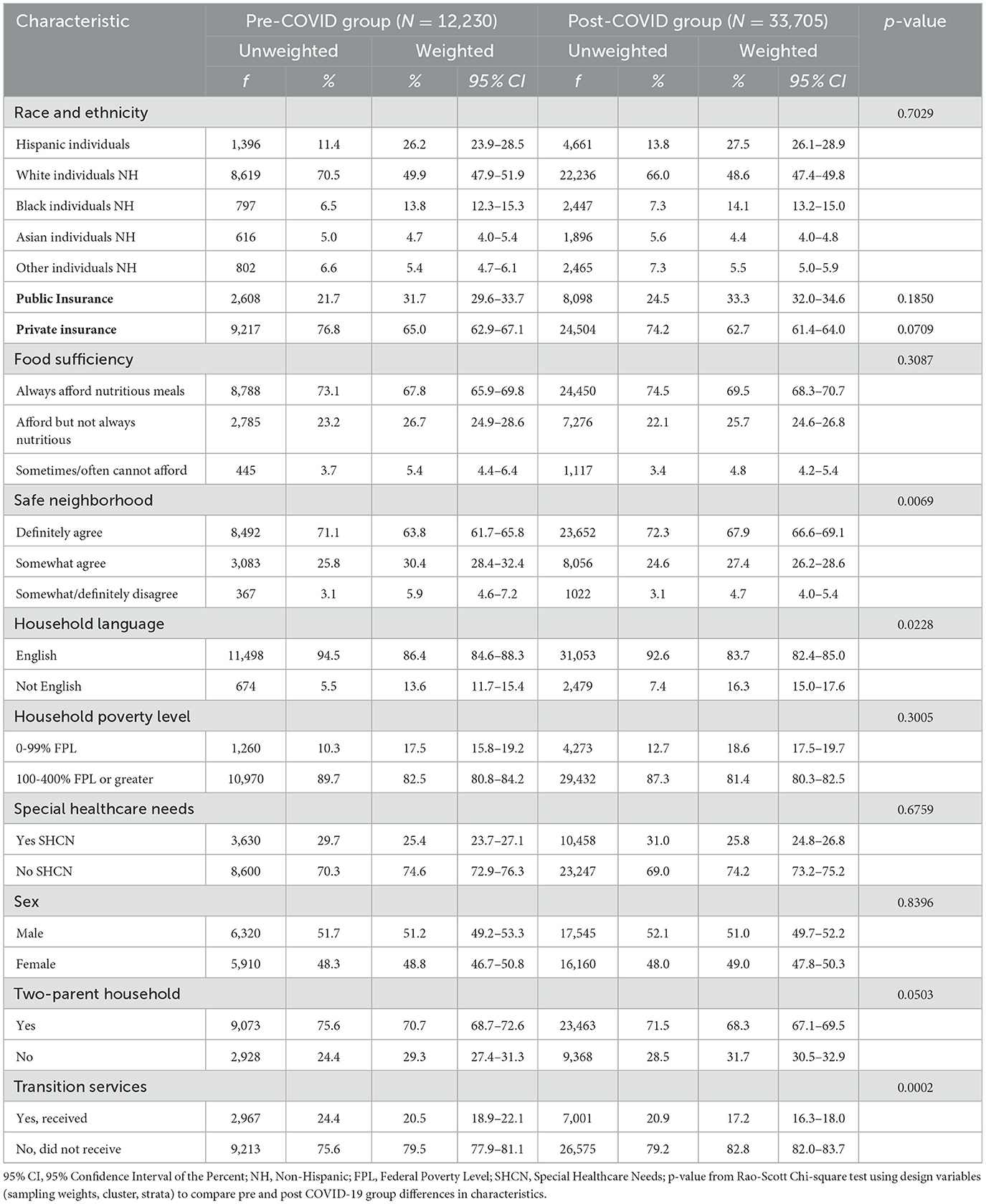
As described in Table 1, when compared to the post COVID-19 group, the pre COVID-19 group had a significantly higher proportion of adolescents whose caregiver reported English as the primary household language (86% vs. 84%, p = 0.0228), a two-parent household (71% vs. 68%, p = 0.0503), and caregivers that somewhat or definitely disagreed to living in a safe neighborhood (unsafe neighborhood, 6% vs. 5%, p = 0.0069). Although statistically significant, the effect sizes were small. The proportion of adolescents with SHCN did not differ for the pre and post COVID-19 groups (26% vs. 25%, p = 0.6759).
3.2 Transition services: role of COVID-19 onset and special healthcare needs
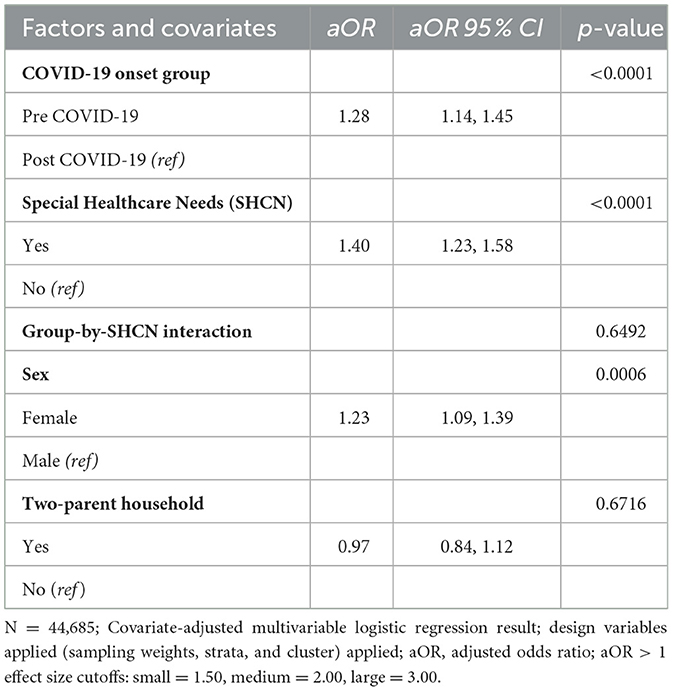
Only 21.7% (n = 9,968) of the total sample of adolescents received transition services. Further, the proportion of adolescents who had received transition services was significantly higher in the pre COVID-19 group compared to the post COVID-19 group (21% vs. 17%, p = 0.0002, Table 1). The covariate-adjusted multivariable logistic regression results in Table 2 indicated a significant main effect of COVID-19 group (p < 0.0001) and SHCN (p < 0.0001), but no interaction effect (p = 0.6492) on transition services, after covarying for sex and two-parent household. Specifically, the odds of receiving transition service were 28% higher (aOR = 1.28) among the pre COVID-19 adolescents compared to those post COVID-19, and were 40% (aOR = 1.40) higher for those with SHCN relative to those with no SHCN. Although two-parent household was not related to transition services, female adolescents had significantly higher odds of receiving transition services than male adolescents (aOR = 1.23, p = 0.0006). Estimated effect sizes for the findings in Table 2 were small.
3.3 Transition services: moderating effects of social determinants of health
The COVID-19-by-SHCN interaction was not statistically significant in the prior analysis; thus, this two-way and three-way interaction term were omitted from the moderator analyses. A separate covariate-adjusted logistic regression model was used to evaluate the moderating effect of each SDOH.
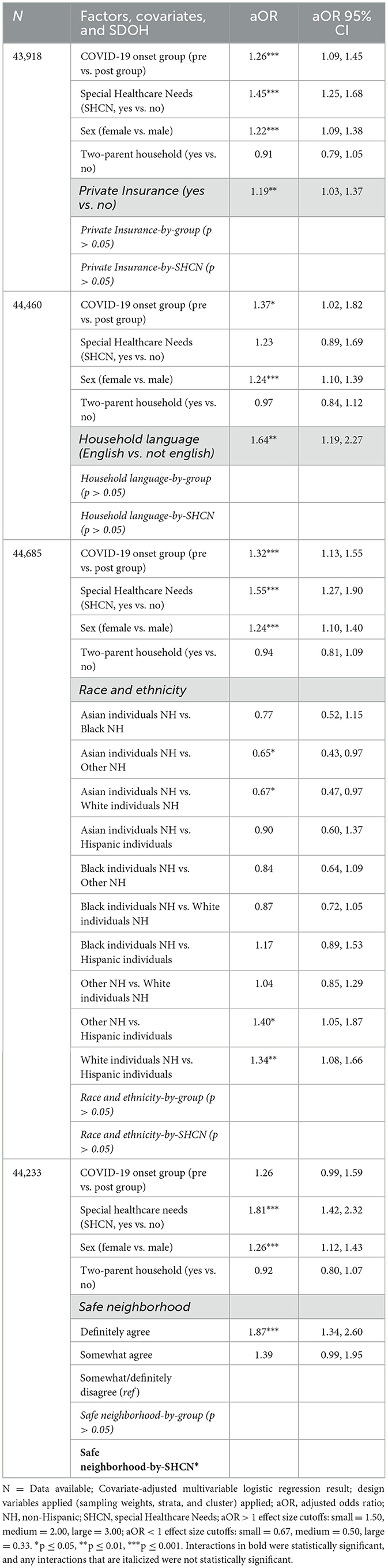
Table 3 presents the regression model and results for the significant SDOH. The odds of receiving transition services were significantly higher for those with private insurance compared to peers (main effect only, p = 0.0193), and for those in which the primary household language was English compared to another language (main effect only, p = 0.0027). English as primary household language had a medium effect size (aOR = 1.64). Race and ethnicity was also a significant predictor of transition services (main effect only, p = 0.0103), with the a posteriori pairwise contrast indicating significantly: (a) greater odds of transition services for Non-Hispanic Other/multiracial groups and Non-Hispanic Whites relative to Hispanics individuals (aOR = 1.40 and 1.34, both p < 0.03, respectively) and (b) lower odds of transition services in Non-Hispanic Asians relative to Non-Hispanic Other/multiracial groups and Non-Hispanic Whites (aOR = 0.65 and 0.67, both p < 0.044, respectively).
Safe neighborhood was a moderator of the SHCN-transition services, as indicated by the significant safe neighborhood-by-SHCN interaction (p = 0.0318, Table 3). Figure 2 shows that adolescents with no SHCN had a significantly lower probability of transition services across all three levels of neighborhood safety compared to those with SHCN (SHCN main effect, p < 0.0001). However, probability of transition services for the two SHCN groups diverged when the neighborhood was reported to be unsafe. When safe neighborhood was rated as somewhat or definitely disagree, the probability of transition services was increased among those with SHCN and decreased among those without SHCN (aOR = 3.35, 95% CI 1.70–6.60, p = 0.0005). Notably, this finding had a large effect size (aOR > 3.00).
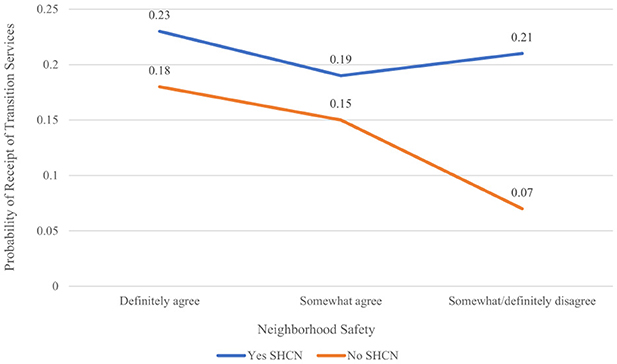
Figure 2. Safe neighborhood: moderator of SHCN and transition services relationship. SHCN, special healthcare needs.
4 Discussion
We aimed to examine the (1) impact of special healthcare needs, onset of COVID-19, and their interaction on receipt of transition services among US adolescents, and whether (2) social determinants of health moderated relationships between special healthcare needs and COVID-19 onset on receipt of transition services. We found significant disparities exist among US adolescents who receive transition services to prepare for adult-focused care.
In this nationally-representative sample of 45,935 adolescents, 78.3% did not receive transition services that could help them thrive in adult-focused care. This finding aligns with previously reported low rates of transition services provided to adolescents since 2016, however, we found an important distinction in care provided in relation to the COVID-19 pandemic (25). After the COVID-19 pandemic onset in 2020, the probability of receiving transition services was significantly lower for all adolescents compared to services provided in 2019, and significantly lower for males without SHCN compared to their peers. These results align with prior studies identifying healthcare barriers brought on by COVID-19 (e.g., fewer routine visits, delayed or altered care) which significantly disrupt the level of transitional care provided to adolescents (4, 12, 26). Our findings expand prior research by identifying that all adolescents in the post COVID-19 group suffered lower odds of receiving transition services compared to pre COVID-19, highlighting a critical need to adjust current, ineffective care practices. Notably, while all adolescents are disadvantaged from a systemic lack of adult-focused care preparation post COVID-19, adolescents living with chronic conditions like sickle cell disease and cystic fibrosis require more healthcare resources compared to their peers (22). The costs of a lack of adult-focused care preparation can be more than financial and contribute to the growing inequities that are experienced by these young adults and their families. These adolescents are at an increased risk for poor health and psychosocial outcomes if they lack preparation for self-care skills needed to manage their highly complex treatment regimens and care appointments in adulthood (10).
Private insurance (healthcare system-level factor), household language (family-level factor), and race and ethnicity (individual-level factor) were all statistically significant predictors of receiving transition services (27). Private insurance has been associated with increased transition readiness among adolescents with chronic conditions, indicating a need to enhance transitional services among adolescents with public insurance like Medicaid (13). Unlike previous literature where small samples limit analyses (13), our sample size allowed identification of the odds of receiving transition services as lower among adolescents who identified as non-Hispanic Asian, non-Hispanic Black, or Hispanic individuals and among those living in non-English speaking households. Additionally, it is important to note that English as primary household language had a medium effect size, suggesting clinical relevance and the need for more non-English resources and tools for families going through the transition process. Healthcare professionals in clinical settings must develop protocols to actively screen patients more at risk for not receiving transition services using tools like PRAPARE (28). The availability of culturally competent resources would assist in reducing health inequities that impact delivery of transitional care in these underserved populations (2). Also, the significant predictors that impact receipt of transition services do so via multiple levels (i.e., individual, family, healthcare system) (27). These results align with principles from the Healthcare Transition Research Consortium Model and SDOH frameworks (14, 27), and thus use of these frameworks in the development of transitional care interventions are more likely to target individual, family, and healthcare system-level factors that impact care delivery.
Adolescents with SHCN living in somewhat or definitely unsafe neighborhoods had a greater probability of receiving transition services compared to adolescents without SHCN. This finding had a large effect size, suggesting a high clinical relevancy and a critical need for mobile or community-based healthcare providers to assess neighborhood safety among transition-age adolescents. Families of adolescents without special healthcare needs who don't feel safe enough to venture outside of their homes may forgo healthcare services, indicating a significant subpopulation at risk for gaps in continuity of care. Adolescents in supportive neighborhoods were reported to experience positive transitional care services, like a provider describing the move to adult-focused care (7). Our results expand prior research by identifying neighborhood safety as a significant environment-level SDOH moderator that may not be actively assessed within inpatient or outpatient settings. Enhancing community-level partnerships and resources to reduce risks of harmful SDOH may help to improve transition service use outcomes among adolescents (2, 6, 7). For example, Medicaid managed care contracts could be used to evaluate for SDOH risks and pay for resources (29).
Our study was limited by the secondary analysis design, requiring use of previously specified variables. Thus, receipt of transition services may not capture the full scope of this construct (16, 17). In addition, data were caregiver-reported (i.e., missing the adolescent perspective), and asked caregivers to recall service use over the past year, increasing the risk for recall bias. The repeated cross-sectional nature of the survey design allowed for the determination of important associations, but future research using multi-level or structural equation modeling would allow testing for causal relationships. Future research could also assess complexity of healthcare needs as a subgroup of adolescents with special healthcare needs.
Recent social determinants of health frameworks suggest that strength-based factors, such as family resilience, may moderate SDOH and health inequities across the lifespan (14). Future studies using longitudinal data could assess the impact of SDOH factors on health outcomes for AYAs in young adulthood. Moreover, future health policy work should identify existing structures that could pay for community health workers and resources to reduce the impact of SDOH factors on receipt of transition services. For example, states can utilize Medicaid to address unmet needs contributed by social determinants of health, as is being done in North Carolina's Healthy Opportunities Pilots program (30). Since North Carolina has expanded Medicaid, the biggest enrollee group is young adults 19–29 years old, suggesting public health interventions via Medicaid would impact this transition-age population (31). Interventions that maximize care coordination and reduce disparities are estimated to save the US healthcare system $29.6–38.2 billion annually (11).
5 Conclusion
Inequities exist among US adolescents in the receipt of transition services to prepare for adult-focused care. Notably, post COVID-19, male adolescents without SHCN had the lowest probability of receiving transition services. Among adolescents who lived in unsafe neighborhoods, those without SHCN had lower odds of receiving transition services. These findings highlight the impact systemic issues have on transition services and the need for enhanced transitional care among these groups.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: https://www.childhealthdata.org/help/dataset.
Ethics statement
The Duke University Institutional Review Board determined this study as exempt as data were anonymized and publicly available. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
TG: Conceptualization, Formal analysis, Methodology, Visualization, Writing – original draft, Writing – review & editing. SS: Formal analysis, Methodology, Supervision, Visualization, Writing – review & editing. GM: Writing – review & editing. SD: Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. Funding support from the Duke Clinical and Translational Science Institute (CTSI) (CTSA grant UL1TR002553) and from the National Clinician Scholars Program at Duke University will be used to pay for the open access publication fees.
Acknowledgments
We would like to thank the National Clinician Scholars Program staff and faculty at Duke University for their support and guidance.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1452418/full#supplementary-material
References
1. Child and Adolescent Health Measurement Initiative. National Survey of Children's Health Interactive Data Query. In: Data Resource Center for Child and Adolescent Health supported by the U.S. Department of Health and Human Services, Health Resources and Services Administration (HRSA), Maternal and Child Health Bureau (MCHB). Bethesda, MD: Health Resources and Services Administration, Maternal and Child Health Bureau (2022). Available at: http://www.childhealthdata.org (accessed 13 December, 2023).
2. Betz CL, Coyne IT. Transition from Pediatric to Adult Healthcare Services for Adolescents and Young Adults with Long-Term Conditions: An International Perspective on Nurses' Roles and Interventions. Cham: Springer (2020).
3. Mubanga N, Baumgardner DJ, Kram JJF. Health care transitions for adolescents and young adults with special health care needs: where are we now? J Patient Cent Res Rev. (2017) 4:90–5. doi: 10.17294/2330-0698.1406
4. Mont'Alvao A, Aronson P, Mortimer J. Uncertainty and disruption in the transition to adulthood during COVID-19. In:Muschert GW, Budd KM, Lane DC, Smith JA, , editors. Social Problems in the Age of COVID-19 Vol 2: Volume 2: Global Perspectives. Paris: Bristol University Press (2020). p. 15–26. doi: 10.46692/9781447360629.004
5. Meyers MJ, Irwin CE. Health care transitions for adolescents. Pediatrics. (2023) 151:e2022057267L. doi: 10.1542/peds.2022-057267L
6. Bailey K, Avolio J, Lo L, Gajaria A, Mooney S, Greer K, et al. Social and structural drivers of health and transition to adult care. Pediatrics. (2023) 153:e2023062275. doi: 10.1542/peds.2023-062275
7. Mooney-Doyle K, Ventura Castellon E, Lindley LC. Factors associated with transitions to adult care among adolescents and young adults with medical complexity. Am J Hosp Palliat Care. (2023) 41:245–52. doi: 10.1177/10499091231177053
8. Vaks Y, Bensen R, Steidtmann D, Wang TD, Platchek TS, Zulman DM, et al. Better health, less spending: redesigning the transition from pediatric to adult healthcare for youth with chronic illness. Healthc (Amst). (2016) 4:57–68. doi: 10.1016/j.hjdsi.2015.09.001
9. White PH, Cooley WC. Transitions Clinical Report Authoring Group. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. (2018) 142:e20182587. doi: 10.1542/peds.2018-2587
10. Lanzkron S, Sawicki GS, Hassell KL, Konstan MW, Liem RI, McColley SA. Transition to adulthood and adult health care for patients with sickle cell disease or cystic fibrosis: Current practices and research priorities. J Clin Transl Sci. (2018) 2:334–42. doi: 10.1017/cts.2018.338
11. Shrank WH, Rogstad TL, Parekh N. Waste in the US health care system: estimated costs and potential for savings. JAMA. (2019) 322:1501–9. doi: 10.1001/jama.2019.13978
12. Hunt WR, Linnemann RW, Middour-Oxler B. Transition planning for chronic illnesses in the time of COVID-19. J Patient Exp. (2020) 7:848–50. doi: 10.1177/2374373520978875
13. Varty M, Popejoy LL. A systematic review of transition readiness in youth with chronic disease. West J Nurs Res. (2020) 42:554–66. doi: 10.1177/0193945919875470
14. Thimm-Kaiser M, Benzekri A, Guilamo-Ramos V. Conceptualizing the mechanisms of social determinants of health: a heuristic framework to inform future directions for mitigation. Milbank Q. (2023) 101:486–526. doi: 10.1111/1468-0009.12642
15. Child and Adolescent Health Measurement Initiative. National Survey of Children's Health Sampling and Survey Administration. Data Resource Center for Child and Adolescent Health supported by the U.S. Department of Health and Human Services, Health Resources and Services Administration (HRSA), Maternal and Child Health Bureau (MCHB). (2019). Available at: http://www.childhealthdata.org (accessed 13 December, 2023).
16. Child and Adolescent Health Measurement Initiative (CAHMI) (2023). 2020-2021 National Survey of Children's Health (2 years combined dataset). SAS codebook for data users: Child and Family Health Measures, National Performance and Outcome Measures, and Subgroups, Version 1.0. Data Resource Center for Child and Adolescent Health supported by Cooperative Agreement U59MC27866 from the U.S. Department of Health and Human Services, Health Resources and Services Administration (HRSA), Maternal and Child Health Bureau (MCHB). Available at: http://www.childhealthdata.org (accessed 13 December, 2023).
17. Child and Adolescent Health Measurement Initiative (CAHMI) (2021). “2019 National Survey of Children's Health: Child and Family Health Measures, National Performance and Outcome Measures, and Subgroups, SAS Codebook, Version 1.0”, Data Resource Center for Child and Adolescent Health supported by Cooperative Agreement U59MC27866 from the U.S. Department of Health and Human Services, Health Resources and Services Administration (HRSA), Maternal and Child Health Bureau (MCHB). Available at: from http://www.childhealthdata.org (accessed 13 December, 2023).
18. Cuschieri S. The STROBE guidelines. Saudi J Anaesth. (2019) 13:S31–4. doi: 10.4103/sja.SJA_543_18
19. Child and Adolescent Health Measurement Initiative. National Survey of Children's Health Methodology Report. Data Resource Center for Child and Adolescent Health supported by the U.S. Department of Health and Human Services, Health Resources and Services Administration (HRSA), Maternal and Child Health Bureau (MCHB). (2022). Available at: http://www.childhealthdata.org (accessed 13 December, 2023).
20. Child and Adolescent Health Measurement Initiative. National Survey of Children's Health Methodology Report. Data Resource Center for Child and Adolescent Health supported by the U.S. Department of Health and Human Services, Health Resources and Services Administration (HRSA), Maternal and Child Health Bureau (MCHB). (2022). Available at: http://www.childhealthdata.org (accessed 13 December, 2023).
21. Child and Adolescent Health Measurement Initiative. National Survey of Children's Health Methodology Report. Data Resource Center for Child and Adolescent Health supported by the U.S. Department of Health and Human Services, Health Resources and Services Administration (HRSA), Maternal and Child Health Bureau (MCHB). (2021). Available at: http://www.childhealthdata.org (accessed 13 December, 2023).
22. Goldson E, Louch G, Washington K, Scheu H. Guidelines for the care of the child with special health care needs. Adv Pediatr. (2006) 53:165–82. doi: 10.1016/j.yapd.2006.04.012
25. Child and Adolescent Health Measurement Initiative. National Survey of Children's Health Interactive Data Query [2016–2020]. Data Resource Center for Child and Adolescent Health supported by the U.S. Department of Health and Human Services, Health Resources and Services Administration (HRSA), Maternal and Child Health Bureau (MCHB). Available at: http://www.childhealthdata.org (accessed 13 December, 2023).
26. Girdwood TC, Goralski JL, Ferris ME, Lynn MR, Dellon EP, Kainz K, et al. Perceptions of caregivers and adolescents/young adults with cystic fibrosis regarding health care transition readiness during the COVID-19 pandemic: a qualitative study. Health Care Trans. 1:100011. doi: 10.1016/j.hctj.2023.100011
27. Betz CL, Ferris ME, Woodward JF, Okumura MJ, Jan S, Wood DL. The health care transition research consortium health care transition model: a framework for research and practice. J Pediatr Rehabil Med. (2014) 7:3–15. doi: 10.3233/PRM-140277
28. PRAPARE. Protocol for Responding to and Assessing Patient Assets, Risks, and Experiences: Implementation and Action Toolkit. Available at: https://prapare.org/knowledge-center/prapare-implementation-and-action-toolkit/https-prapare-org-wp-content-uploads-2021-10-full-toolkit_june-2022_final-pdf/ (accessed 13 December, 2023).
29. Addressing Social Determinants of Health via Medicaid Managed Care Contracts and Section 1115 Demonstrations. Available at: https://www.chcs.org/media/Addressing-SDOH-Medicaid-Contracts-1115-Demonstrations-121118.pdf (accessed 13 December, 2023).
30. Rapfogel N, Rosenthal J. Fact Sheet: How North Carolina is Addressing Social Determinants of Health Through Medicaid. (2022). Washington, DC: The Center for American Progress. Available at: www.americanprogressorg/article/fact-sheet-how-north-carolina-is-addressing-social-determinants-of-health-through-medicaid/
31. North Carolina Medicaid. Medicaid expansion dashboard. In: North Carolina Medicaid Division of Health Benefits. Available at: https://medicaid.ncdhhs.gov/reports/medicaid-expansion-dashboard (accessed March 14, 2024).
Keywords: adolescents, special healthcare needs, transition to adult care, health inequities, COVID-19, social determinants of health
Citation: Girdwood TC, Silva SG, Maslow GR and Docherty SL (2024) Disparities exist among US adolescents in the receipt of transition to adult healthcare services: the differential impact of social determinants of health, healthcare needs, and COVID-19. Front. Public Health 12:1452418. doi: 10.3389/fpubh.2024.1452418
Received: 20 June 2024; Accepted: 14 November 2024;
Published: 18 December 2024.
Edited by:
Joao Sollari Lopes, National Statistical Institute of Portugal, PortugalReviewed by:
Tony Kuo, University of California, Los Angeles, United StatesJohn Pascoe, Wright State University, United States
Copyright © 2024 Girdwood, Silva, Maslow and Docherty. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tyra C. Girdwood, dHlyYS5naXJkd29vZEBkdWtlLmVkdQ==
†ORCID: Tyra C. Girdwood orcid.org/0000-0002-5209-610X
 Tyra C. Girdwood
Tyra C. Girdwood Susan G. Silva1
Susan G. Silva1 Gary R. Maslow
Gary R. Maslow