- 1St George’s School of Health and Medical Sciences, City St George’s, University of London, London, United Kingdom
- 2Institute of Psychiatry, Psychology & Neuroscience, King’s College London, London, United Kingdom
Introduction: The aims of this synthesis were to investigate the relationship between IPV severity and mental health outcomes and shed light to gaps and limitations in existing methodologies used to assess IPV severity and its association with mental health outcomes.
Methods: We conducted a two-stage narrative synthesis of 76 studies. First, we identified IPV measures used in at least five studies, focusing on their variations and severity score calculation. Then, we analyzed findings of studies correlating IPV severity with mental health outcomes, identifying features of measures and statistical methods influencing result consistency.
Results: Measures of intimate partner violence were often modified from their original, potentially impact on the reliability and validity of these measures. The operationalization of violence severity varied across studies, leading to inconsistencies in scoring whereby compromising the consistency of severity levels across studies. We found lack of consistency in applying validated methods for scoring instruments to determine abuse severity. In this review, we consistently found that the severity of IPV and its various subtypes were linked to different mental health outcomes across multiple studies. We discovered evidence suggesting that experiencing more types of IPV was associated with worse mental health outcomes. Generally, higher levels of overall IPV severity and its specific subtypes were correlated with poorer mental health outcomes. However, our analyses did not reveal consistent patterns that would allow for a definitive determination of how individual IPV subtypes differently affect mental health outcomes. Nevertheless, we observed that increasing severity of physical IPV tended to have a notable impact on post-traumatic stress disorder (PTSD). Conversely, increasing severity of psychological IPV was consistently associated with depression. While sexual IPV severity was explored in fewer studies, the evidence regarding its impact on various mental health outcomes was less conclusive.
Discussion: To achieve a comprehensive understanding of the mechanism by which IPV severity is related to mental health it may be time to take an alternative approach to measuring IPV severity. No IPV measures assessed the acceptability of the content to people who have experienced IPV. This is an important omission with significant consequences for the validity of the evidence base.
1 Introduction
Intimate partner violence (IPV) is a pervasive criminal justice, social and public health problem. It attracts attention in social and medical sciences, but accurate measurement is problematic and there is no comprehensive review of the ways in which IPV severity is measured. Without accurate, meaningful, and robust measurement of the severity of IPV, its deleterious impact on the mental health of survivors cannot be adequately examined. This study examined commonly utilized measures to assess the severity of IPV included in a recently published systematic review by White et al. (1). The examination focused on the scoring methods employed, the adaptation and calculation of severity scores, and explored how they impact the analysis of the relationship between the severity of IPV and mental health outcomes.
Intimate partner violence refers to behavior within a relationship that has physical, sexual and/or psychological impacts, and includes acts of physical aggression, sexual coercion, psychological abuse and controlling behaviors. This definition covers violence by both current and former spouses and partners (2). It is a multifaceted phenomenon that can manifest in a myriad of often co-occurring forms and is a gendered problem with women disproportionately impacted. Globally, an estimated 37% of women and girls aged 16 years or older have experienced lifetime physical, psychological, or sexual IPV, and an estimated 24% of women and girls aged 16 years or older have experienced IPV in the past year (1).
The experience of IPV is associated with a wide range of short-term and long-term physical and mental health sequelae, sexual and reproductive health problems, and death due to homicide and suicide (3–8). Although accurate screening for IPV should be a priority, currently screening for IPV is not integrated into any of the mental health risk assessment and management tools used in mental health services the UK (9). Additionally, IPV is rarely included as an exposure or an outcome in mental health research (2). Measuring IPV is a challenge as there is a lack of consensus on how types of IPV, which can vary by severity and frequency, combine into a pattern of behavior to represent an individual’s experience (2). In addition, the effect of abuse is cumulative with combined abuse, particularly abuse involving sexual IPV, being associated with the highest levels of harm, including risk of suicidal ideation and attempting suicide (10). Given the health, social, and economic costs of IPV, United Nations’ bodies, treaties, and declarations have called for better statistics on the nature, prevalence, causes, and consequences of violence against women as a basis for its elimination (11).
The assessment and measurement of IPV is controversial (12–16). Issues include the definition of violence, the boundary between violence and non-violent coercion (17). The assessment of repeated acts of IPV is contentious due to a lack of consensus on the measurement of IPV severity. The Conflict Tactics Scale (18), an early measure developed to study the prevalence and patterns of conflict within families, differentiates between minor and severe IPV, associating severe IPV with a higher likelihood of injury. However, this binary classification oversimplifies the complexity of IPV, as similar acts can have different consequences for male and female victims. Additional indicators of IPV severity include the frequency of incidents, the emotional impact, and resulting injuries (19–21). The problem with current severity operationalization is that it often overlooks these aspects simultaneously. Researchers have identified distinct types of IPV based on controlling behavior and employed cluster (22) or latent class analysis (23, 24) to identify severity classes, aiming to create mutually exclusive subgroups based on patterns of responses to observed categorical variables (24).
Walby et al. (15) suggest an IPV measurement framework that incorporates graded distinctions in the severity and frequency of violence and coercion and considers the consequences for victims. They acknowledge the temporal misalignment between perpetrator and victim in existing frameworks, where temporality is viewed as both episodic and continuous. Their proposal recognizes the duration of the action as repeated discrete incidents of violence, while the harm may manifest as a continuous state of fear. This challenges the assumption of alignment between one perpetrator, one victim, and one event, highlighting the accumulation of harm in high-frequency victims, particularly women (15, 16, 25).
Consensus is also lacking on the most accurate and psychometrically robust method for scoring behaviors in survey measures that assess abuse and violence. The legitimacy of using dichotomous splits to compare those experiencing abuse has been questioned, as it combines individuals with one incident with those experiencing frequent and severe abuse. Researchers emphasize the impact of decisions on scoring and classifying participants on their research results (13, 26, 27). Methodological questions have been raised about using unequal interval frequency categories, weighting items to improve sensitivity, and resolving identical scores produced through weighting, stemming from either a high frequency of mild incidents or a low frequency of severe incidents (28).
To adequately address the varied needs of those impacted by IPV, it is crucial to deepen our understanding of how the severity of such violence impacts mental health outcomes. While existing research indicates that women often endure more frequent and severe instances of IPV compared to men (17), precise measurement remains deficient. Yet, the measurement and analysis of IPV severity is complex, requiring careful consideration of population characteristics, methodological challenges and survivor involvement. Using data from studies investigating the association between severity of IPV and mental health outcomes included in the recently published systematic review, we addressed the research question: ‘With specific reference to the measurement of severity of violence what are the methodological challenges in examining the relationship between severity of IPV and mental health outcomes?’ The study objectives are:
1. To examine the commonly used measures of IPV severity and assess the different ways in which these were applied in practice.
2. To narratively review the evidence regarding the association between severity of IPV and mental health outcomes.
3. To provide recommendations on the development of new measures or amending old measures/approaches.
2 Materials and methods
2.1 Study design
This study adopted a narrative synthesis approach to explore a question that was not the primary focus of the initial research (1). In this context, we scrutinized the analysis of IPV severity across the studies we included and sought to understand how the severity of distinct forms of IPV related to various mental health outcomes.
The full details regarding the review search strategy, data sources and selection of the published review can be found in the aforementioned paper. To summarize, in the original review, full-text articles were evaluated against the following criteria: (a) those that included non-military women who were 16 years or older and were assessed for IPV experiences (overall, physical, psychological/emotional, and sexual) during their lifetime (lifetime IPV) or during the past year (i.e., 12 months prior to interview) using a validated IPV measure; (b) those which presented the results of peer-reviewed research based on quantitative methodology that provided mental health outcome data for at least one time point. The systematic review was registered on Prospero with the registration number CRD42020177744 (29).
All the 201 peer-reviewed studies that were included in the initial systematic review were searched to identify studies that used a tool to measure the severity of IPV either on a continuum or using an ordinal categorical format. This subset of studies was in the English language and published between 2012 and November 2020. The authors’ initial systematic review and meta-analysis expanded on an existing review by Trevillion, Oram, Feder, and Howard (30) that identified the prevalence of intimate partner violence in individuals diagnosed with a mental disorder. Hence, our initial review included a broader range of symptoms, issues, and needs related to mental illness diagnosis, which are well-documented as outcomes of exposure to IPV. As a result, we included more eligible studies compared to the aforementioned 2012 systematic review.
Downloaded full texts were evaluated against the following criteria: (a) those that included women and men who were 16 years or older and were assessed for severity of IPV (overall, physical, psychological/emotional, and sexual) during their lifetime or during the past year using a validated IPV measure; and/or (b) those which presented data on the association between severity of IPV and mental health outcomes for at least one time point.
2.2 Data extraction
Using a template designed and tested a priori, data extracted included: the settings, population sample, country, study design, IPV measure, type and timing of assessments, detail on how severity of IPV was measured (e.g., whether in a continuous form, categorical form, cumulative scores, or any other means to measure severity of IPV), and relevant findings regarding the association between IPV severity and MH outcomes. The range of statistics pertaining to the association between IPV severity and MH outcomes such as correlation coefficients (r), regression coefficients (b), odds ratios (OR) and adjusted odds ratios (AOR) were also extracted. When available 95% confidence intervals and p-values were also extracted. Where results were not tabulated or reported with appropriate statistics, verbatim text describing the findings of relevant analysis was extracted onto a bespoke data extraction tool.
2.3 Analysis
We conducted narrative analysis to synthesize our findings (31). In our initial synthesis, we focused on measures used in at least five studies, exploring how researchers employed IPV measures to calculate the severity of IPV. Specifically, we examined variations in their usage and severity score calculation, contrasting these practices with what was outlined in the measures’ development and validation papers. During this phase, we organized summaries of the studies, emphasizing the different types of severity scores used, laying the groundwork for the subsequent analysis.
In the next stage of our synthesis, we examined studies that reported the association between IPV severity and mental health outcomes. We systematically organized and tabulated these findings based on IPV severity type, mental health outcome, IPV measure, population under study, and the main results reported. The findings column in each Tables 2–5, details the extracted statistics from the analysis of the association. Adjusted results were tabulated whenever both adjusted and unadjusted analyses were reported. The synthesis aimed to identify where consistent evidence is present, assessing if type and severity of IPV is associated more or less with a specific mental health outcome and compare how findings are consistent across statistical methods.
3 Results
3.1 Description of the sample
From the original pool of 201 studies, 76 were included in this synthesis as theses measured the severity of IPV. Of these 76 the majority were conducted in the United States (n = 38) followed by Bangladesh (n = 3), Canada (n = 3), South Africa (n = 3), China (n = 3), Thailand (n = 3), Turkey (n = 3), Belgium (n = 2), Spain (n = 2), Brazil (n = 2), Vietnam (n = 2), Japan (n = 2), Australia (n = 1), Italy (n = 1), Cameroon (n = 1), Sweden (n = 1), United Kingdom (n = 1), Tanzania (n = 1), Lebanon (n = 1), Portugal (n = 1), and Greece (n = 1). One study was multi-site across different states: one in Baltimore, MD, USA, St. Croix and St. Thomas, U.S. Virgin Islands. Fifty-eight studies were located in high income countries, 11 in upper-middle countries, six in lower-middle countries, and one in low-income countries.
Twentynine studies recruited participants from the community (25 of which recruited women only) while 21 recruited IPV-exposed populations. Sixteen studies were with women in the perinatal period, while 10 recruited clinical-based samples (patients receiving healthcare at inpatient or outpatient or prison clinics unconnected to their experience of IPV.
3.2 Participants
Study sizes ranged from 14 to 14,575 participants, with a median of 303.5. Together, the studies included 54,131 participants (44,773 women; 9,349 men; 9 transgender).
3.3 Measurement of severity of IPV
Out of the original 201 studies, 76 (38%) measured the severity of intimate partner violence (IPV). Table 1 outlines the eight measures used in at least five studies, demonstrating the various ways that 62 (82%) of the included studies applied the measures and calculated IPV severity. Twenty-four studies (32%) calculated an overall IPV severity measure, 17 of these studies (22%) used a continuous scale, while six (8%) used a categorical variable. Forty-nine of these studies (64%) reported a measure of physical IPV severity, with 14 studies (18%) using a categorical variable, and 35 studies (46%) using a continuous scale. Psychological IPV severity was measured in 39 studies (51%), with 30 studies (39%) using a continuous scale and 9 (12%) using a categorical variable. Sexual IPV severity was reported by 27 studies (36%), with 20 studies (26%) using a continuous variable and 7 (9%) using a categorical one. One study (32) reported using an IPV measure, but no details were provided about how it was calculated.
Table 1. Scales used to measure severity of IPV, frequency of use, scoring methods, adaptation and type of variable.
4 Findings
4.1 Measures of intimate partner violence
Twenty-two different measures of IPV were used across the 76 studies in our sample. Thirteen studies (17%) utilized two IPV measures, and nine studies (12%) used three IPV measures. The Revised Conflict Tactics Scale (CTS2) (18, 33, 34) was the most frequently used measure, with 35 studies (45%) employing it to measure at least one type of IPV. Ten studies (13%) used the WHO standardized questionnaire (35, 36). Eight studies (10%) employed the Danger Assessment scale (DA) (37–39), the Psychological Maltreatment of Women Inventory (PMWI) (40, 41), the Sexual Experiences Survey (SES) (42–45), and the Severity of Violence Against Women Scale (SVAW) (46). The Composite Abuse Scale (CAS) by Hegarty et al. (47) and the Index of Spousal Abuse by Hudson and McIntosh (48) were used in five studies (6%). Of the remaining 14 scales that were utilized, two were used three times (Abuse Assessment Screen; Abuse Behavior Inventory), three were used twice (Domestic Violence Scale; Woman abuse screening measure; Women’s Experiences of Battering) and the remaining nine used just once (Cumulative trauma experiences; CVES Research Version; Measure of Psychologically Abusive Behaviors; Multidimensional measure of emotional abuse; Potentially Harmful Behavior Scale; Pregnancy Risk Assessment Monitoring System; Trauma History Questionnaire; NorVold Abuse Questionnaire; Behavioral Risk Factor Surveillance System). In six studies, the PMWI was used to measure psychological IPV alongside the CTS2 which measured physical IPV, and the SES which measured sexual IPV (Table 1).
Eight measures (CTS2, WHO, PMWI, DA, SVAW, SES, CAS, ISA) were employed by at least five of the included studies (see Table 1). None of the measures that were modified by the researchers were revalidated prior to their use.
4.1.1 Revised conflict tactics scale
Data collected using the CTS2 can be reported as prevalence, chronicity and severity of IPV [for descriptions (see 18, 34)]. Chronicity for individuals with at least one experience of violence in a subscale is scored based on the frequency. Scores are summed for a continuous chronicity/severity score. In contrast severity, excluding negotiation, categorizes acts into minor or severe, with respondents classified by severity: severe (at least one severe act), minor (at least one minor act but no severe act), and none (no reported acts).
Studies measured IPV severity on a continuum and/or using a categorical variable. Of the 34 studies using the CTS2, 23 reported either descriptive and/or analytical statistics with a continuous variable of IPV chronicity, intensity, or severity (Table 1). Researchers did not consistently adhere to a validated structure and scoring scheme: seventeen studies had variations in how scales were truncated or extended, response formats altered, or scores calculated. Some studies did not use the highest frequency category (49–51) but retained the weighted scores. In contrast, two studies scored all items using 0 = no, 1 = yes, summing the items so that the subscale scores were the number of positively endorsed items within each subscale (52, 53). Two studies did not sum all items within subscales. Tsai, Tomlinson, Comulada, and Rotheram-Borus (54) used four items from the physical assault subscale (CTS2) scoring responses on a four-point scale ranging from 1 (never) to 4 (many). Each item was standardized and the summary IPV index defined as the equally weighted average of the four z-scores. Sezgin and Punamäki (55) adopted principal component analysis to derive IPV severity subscales. In five studies, severity scores were calculated for respondents who had not experienced at least one act of IPV, contradicting guidance (56–60).
Eleven studies reported IPV severity using a categorical form (24, 61–70), with eight studies using the recommended labels of minor and severe (33). Three studies used different approaches to create a categorical severity score. Esie et al. (61) developed three composite scores of IPV severity by combining items from the CTS2 and the WHO questionnaire. The frequency of psychological, physical, and sexual IPV was recorded as never (scored 0) as 1–2 times (scored 1), 3–5 times (scored 2), 6–10 times (scored 3), greater than 10 times (scored 4). Item scores were then summed to create a severity score. Each of these three scores was categorized as “none” “low” “medium” or “high” based on tertiles of the non-zero values for each IPV severity score. Lobato et al. (65) applied a three-level categorization to the composite score to use in analysis: no event, a single event, and two or more events. Ziaei et al. (70) used a 0–4 labeled categorical variable to calculate the severity of IPV by summing the different forms of IPV (physical, sexual, emotional, and controlling behavior) that an individual experienced.
4.1.2 WHO multi-country study on women’s health and domestic violence against women
Data collected using this measure can be reported as prevalence of physical and sexual IPV against women and its correlation with health outcomes in culturally diverse countries. The severity of a physically violent act is ranked according to its likelihood of causing physical injuries and defined dichotomously (moderate or severe) [(see 35)].
Of the 10 studies using this measure, seven studies created categorical ratings of IPV severity (61, 71–76), with four studies employing the minor and severe category ratings to do so. Esie et al. (61) combined items from the WHO and CTS2 as described above to produce a four-level variable. Tran et al. (76) calculated a binary variable indicating whether someone had experienced all types of IPV (controlling, emotional, physical, and sexual). Tho Tran et al. (75) scored emotional violence (EV) as 0, 1, 2, 3+ types of EV, and 0, 1, 2–5, 5+ acts of EV. The remaining two studies (77, 78) created a continuous psychological IPV severity variable by applying a 5-point Likert-type scale (0 = never to 4 = very often) on seven modified items, the severity score computed by summing the scores, range 0–28. Xu et al. (79) calculated three continuous index scores of IPV severity.
4.1.3 Psychological maltreatment of women inventory
This measure assesses nonphysical abusive behavior in male IPV perpetrators with responses being rated on a Likert-style scale (1 = never to 5 = very frequently). Scores are calculated by summing items within each subscale. A shorter 14-item version, PMWI-S, maintains these subscales (41).
Eight studies used this measure and produced continuous measures of the severity of psychological IPV by summing the item scores (49–51, 80–84). Only one study used the original 58-item measure (84), while the remaining studies either used the PMWI-S and adopted the intended response format, or added to the PMWI-S six items from CTS2 and used the CTS2 response format.
4.1.4 Danger assessment scale
This measure assesses the likelihood of lethality or near lethality in cases of IPV. The revised version (38) defined danger levels such as variable danger (0–7), increased danger (9–13), severe danger (14–17), and extreme danger (18 and above). This measure was adopted in eight studies, of which six produced continuous measures of the severity of IPV (risk of lethality) by summing the item scores (85–90) and two reported IPV severity using a categorical form (32, 91). Six studies used the newer version 20 item scale although one study dropped an item (88). Kulwicki et al. (86) and Peltzer and Pengpid (91) created categorical ratings of IPV severity. While the former did not use the weighting to calculate the total score but summed up the number of affirmative responses, the latter removed one item dealing with sexual violence from the original 15-item DA scale and summed up the number of affirmative responses to produce a total score between 0 and 14. A low, medium, high categorization was used in the analysis but was not defined.
4.1.5 Severity of violence against women scale
The SVAW assesses the frequency and severity of physical aggression, allowing researchers to explore different severity levels and analyze the distinct effects of various violence types. It is comprised of nine subscales measuring two major dimensions (threats and actual violence).
This measure was adopted in eight studies all of which produced continuous measures of the severity of IPV by summing the item scores (7, 81, 87, 88, 90–93). There were variations in the number of subscales used, for example, DeCou et al. (92), summed participants’ responses to yield a total IPV severity score, which was included in their subsequent analyses. The remaining studies reported the subscales. Saito et al. (81) used the full SVAWS but only reported prevalence of varying severity of IPV and divided their sample into abused and non-abused groups.
4.1.6 Sexual experiences survey
The SES assesses various sexual victimization experiences through 10 behaviorally specific items, covering unwanted and non-consensual encounters, including sexual coercion, attempted rape, and rape. The SES is scored on an objective severity continuum, with rape assigned a score of 4, attempted rape a score of 3, coercion a score of 2, contact a score of 1, and no victimization a score of 0. The SES was later revised to create the Short Form Victimization (SES-SFV) (42).
Eight studies used the SES, of which seven created continuous IPV severity variables (50–52, 80, 82, 83, 94), and one created categorical ratings of IPV severity (49). None of the studies used the objective severity outcome as defined by the authors. Williams et al. (94) used the SES-SFV version but summed up the items to calculate a sexual IPV severity score. The remaining studies all replaced the yes/no response format of the SES with the CTS2 response form. Four studies (50, 80, 82, 83) summed up the items to calculate a total sexual IPV severity score. To overcome the excessive skew after summing the items as intended, Flanagan et al. (49) recoded sexual IPV into an ordinal variable (0 = no victimization, 1 = moderate sexual victimization, and 2 = sexual victimization with penetration).
4.1.7 Composite abuse scale
The CAS is a comprehensive abuse measure with four dimensions: severe combined abuse, emotional abuse, physical abuse, and harassment. A 15-item version (CAS Short Form, CASR-SF) was later created, covering physical, sexual, and psychological abuse, with scores ranging from 0 to 75. The total score, calculated as the mean of responses multiplied by 15, is recommended over subscale scores (95).
Five studies used CAS and reported severity on a continuous IPV severity variable. Daugherty et al. (6), however, used the CAS-SF, and Khadra et al. (96) used only the Physical Abuse subscale. The remaining studies used the original CAS, and scored and analyzed this measure as described by the original authors.
4.1.8 Index of spousal abuse
The ISA measures the severity of physical and non-physical aggression (referred to in this paper as psychological for consistency) by an intimate partner, derived from the CTS. Each item is rated from 1 (never) to 5 (very frequently). Subscale scores, ranging from 0 to 100, are calculated with weighted items, giving greater importance to more serious forms of abuse. Clinical cut-offs are set at 10 for ISA-P (physical) and/or 25 for ISA-NP (non-physical), identifying individuals likely experiencing spousal abuse.
Five studies used this measure as intended, creating continuous IPV severity variables (32, 89, 97–99). The study by Kelly and Pich (32) used its clinical cut-offs as an inclusion criterion rather than a variable for statistical analysis.
4.2 Analyzing the association between severity of IPV and mental health outcomes
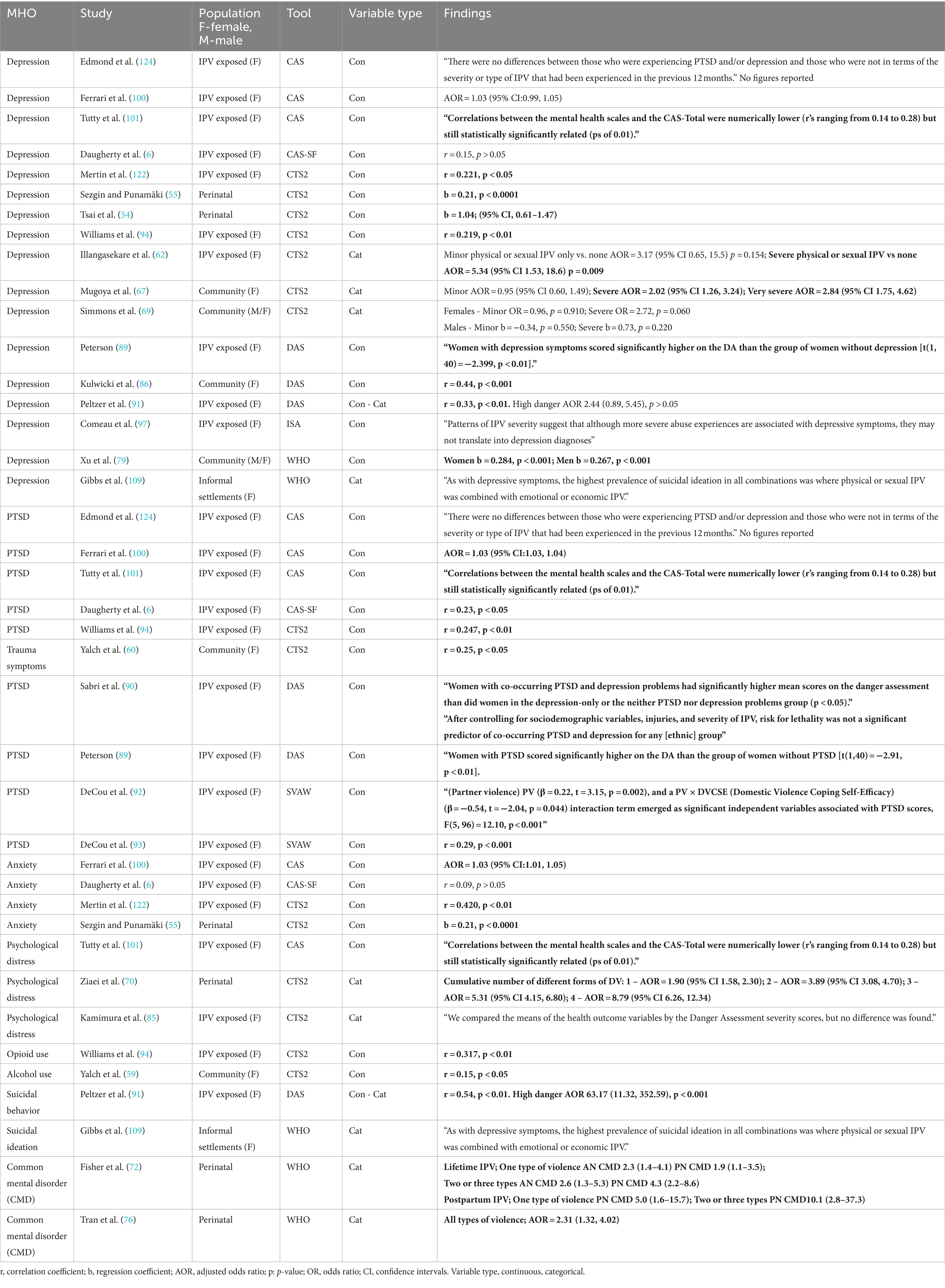
Tables 2–5, highlight the studies that explored the association between severity of IPV, either overall or by subtype, and mental health outcomes. In each table significant associations have been highlighted in bold.
Different statistics were calculated by the statistical analyses, such as correlation coefficients (r) to measure the association between two variables measured on a continuous/discrete scale; regression coefficients (b) used in multiple regression, where the mental health outcome is treated as a continuous variable, and multiple covariates (to account for confounding) are included in the model in addition to IPV variables; and crude odds ratios (OR’s) or adjusted odds ratios (AOR’s) (produced when covariates are included in the model) which were adopted when the mental health outcome was treated as binary, presence of disorder or not, to assess the association between severity of IPV and mental health outcomes.
Twenty-six studies used a measure of severity of overall IPV to explore its association with mental health outcomes (Table 2). Depression was the outcome in 17 studies, PTSD/trauma symptoms in 10, anxiety in four, psychological distress in three, and common mental disorder studies, alcohol/opioid abuse, and suicidal ideation/behavior each in two studies.
A small but statistically significant association between the severity of overall IPV and depression was reported in 11 of the 17 studies. However, in the study where they controlled for confounding variables (91), no significant association was found between risk of lethality and depression. In the two studies employing a categorical form of IPV, the OR or AOR are all greater for severe IPV than minor IPV and “very severe” in Mugoya et al. (67). Seven out of the 11 studies reporting a significant association were based on samples of women who had all experienced IPV.
In relation to the association between the severity of combined forms of IPV and PTSD (or trauma symptoms), nine out of 10 studies examining PTSD reported a significant association. Three of the nine studies adjusted for covariates (90, 93, 100) with the latter study reporting a non-significant association after adjustment. These studies mostly were based on samples of women who had all experienced IPV.
Three of the four studies that analyzed anxiety as an outcome found statistically significant associations between overall IPV severity, one of which adjusted for confounding variables (100).
With regards to psychological distress, Tutty et al. (101) reported a small but statistically significant correlation using the CAS total score, while Kamimura et al. (85) found that mean scores of psychological distress did not differ significantly between categories of risk of lethality (as measured by DA). However, in a perinatal study (70) the odds of psychological distress increased in relation to increasing number of different types of IPV.
The two studies examining the use of opioid, and alcohol reported a positive correlation with overall severity of IPV as measured by CTS2. The study by Gibbs et al. (73) examining suicidal ideation found it was more prevalent in women who experienced emotional IPV in combination with physical and sexual IPV, than those with did not report emotional IPV. Whereas Peltzer and Pengpid (91) reported that suicidal behavior was significantly correlated with risk of lethality showing that women in the highest danger category were significantly more likely to exhibit suicidal behavior. Both studies examining common mental health disorders (CMD) reported significant association, with Tran et al. (76) showing that women who had experienced all types of IPV had increased odds of having a CMD, whereas Fisher et al. (72) demonstrated that whether examining lifetime or postpartum IPV the AOR for wo-three types of IPV was greater than that for one type of IPV.
4.2.1 Association between severity of physical IPV and mental health outcomes
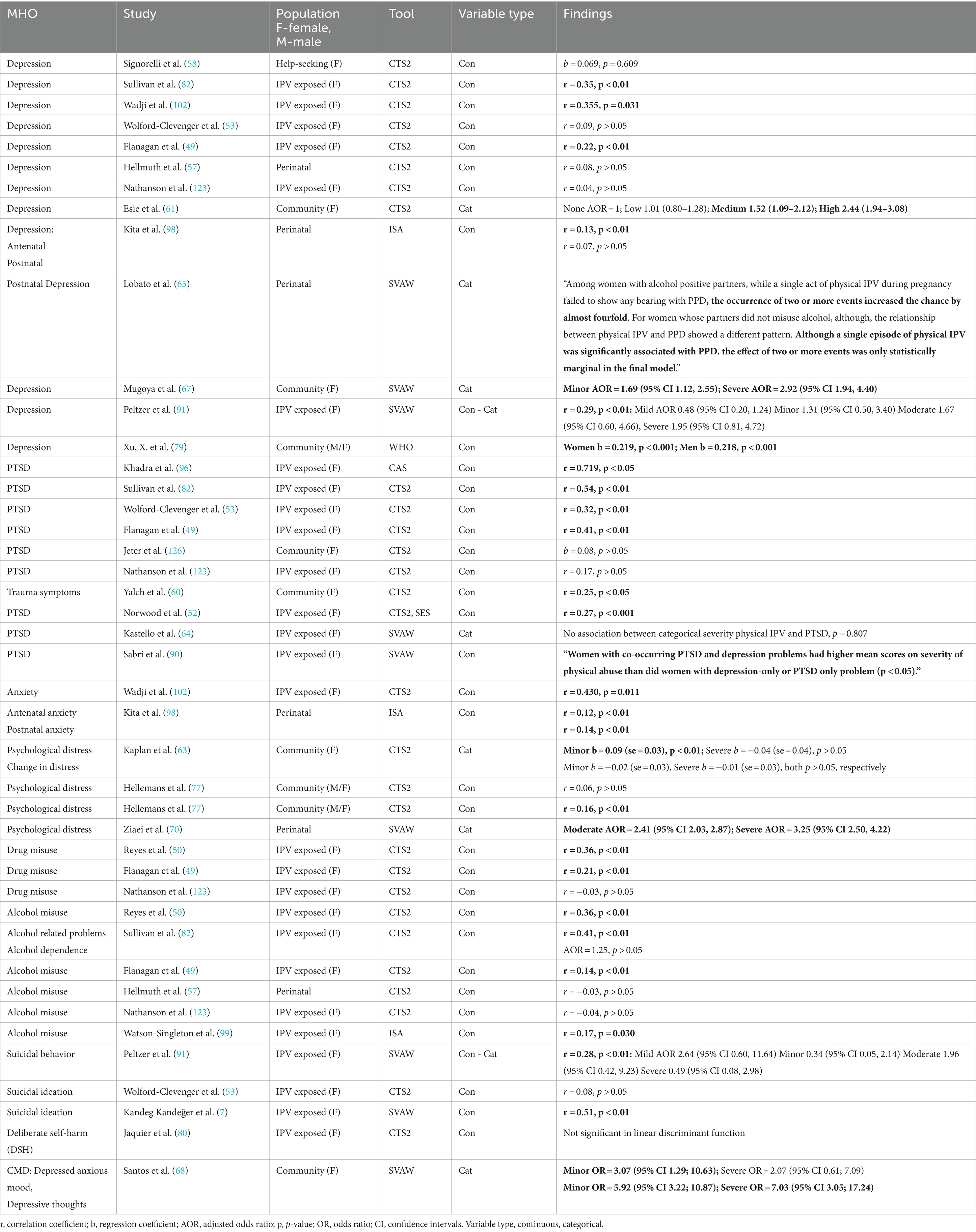
Twenty-eight studies adopted a measure of severity of physical IPV to analyze its association with a range of mental health outcomes. Depression was measured in 13 studies, PTSD/trauma symptoms in 10, alcohol/drug abuse in 10, psychological distress in three studies, suicidal ideation/behavior in three, anxiety in two, deliberate self-harm in one, and finally common mental disorders in one study (Table 3).
Eight of the 13 studies measuring depression used the CTS2 to measure severity of physical IPV. Depression was significantly associated with the severity of physical IPV in nine studies. Four of the five studies reporting statistically significant correlations presented coefficients from 0.22 to 0.355. However, in one study (91) when the categorical forms of IPV severity and depression were used and covariates were adjusted for, the AOR’s were not significant. Further, the study by Esie et al. (61) using a categorical form of severity indicated that women experiencing medium or high severity of physical IPV had increased odds of being depressed. In Lobato et al. (65) a significant association between severity of physical IPV and post-natal depression was highlighted, which appeared to be dependent on whether the partner misused alcohol or not. A study set in the community using a categorical form of SVAW (67) showed that while both minor and severe physical IPV were associated with greater odds of depression the AOR for severe was greater than for minor. In the study by Xu et al. (79) regression analysis indicated a significant association between severity of physical IPV and depression for both men and women.
Most of the studies examining the severity of physical IPV and its association with PTSD/trauma symptoms used the CTS2. Five of these seven studies reported a significant association with correlation coefficients ranging from 0.25 to 0.54. A high, statistically significant correlation (r = 0.719) between severity of physical IPV as measured by CAS and PTSD was highlighted in a sample of women who had all experienced IPV (96). The study by Sabri et al. (90) used a composite outcome of PTSD and depression and reported greater severity of physical IPV in women with both PTSD and depression than those with depression alone.
Both studies examining anxiety indicated that the severity of physical IPV was significantly associated with anxiety. In Kita et al. (98) they adopted the ISA to assess anxiety in the antenatal and postnatal periods, respectively r = 0.12 and 0.14, whereas Wadji et al. (102) found a statistically significant correlation (r = 0.43.) between severity of physical IPV and anxiety using CTS2.
With regards to psychological distress, the two papers by Hellemans et al. (77, 78) reported small correlations between physical IPV severity and psychological distress, though only Hellemans et al. (78) achieved statistical significance with r = 0.17. In Kaplan et al. (63) the authors reported two analyses, the first of baseline psychological distress, the second of change in psychological distress over 2 years. They used a categorical form of CTS2 with minor and severe physical IPV variables entered into multiple regression models alongside covariates. Regression coefficients were small with only the minor severity of physical IPV being associated with baseline psychological distress. In a perinatal study (70) using SVAW, the authors reported statistically significant associations between moderate and severe physical IPV and psychological distress, AOR’s of 2.41 and 3.25, respectively.
Most of the studies examining alcohol or drug misuse as the outcome used the CTS2 to measure severity of physical IPV. Table 2 shows statistically significant correlation coefficients being reported in six studies ranging in magnitude from 0.14 to 0.41. Moreover, of the four studies examining suicidal behavior/self-harm two studies found statistically significant correlations (7, 91), though in the latter further analysis incorporating covariates showed non-significant associations between increasing severity categories of physical IPV and outcome. Finally, Santos and Monteiro (68) examined common mental disorders and were able to show that while minor physical IPV was significantly associated with increased odds of having a depressed anxious mood, severe physical IPV was not. They also showed that while both minor and severe physical IPV was associated with greater odds of depressive thoughts, the AOR for severe was greater than for minor.
4.2.2 Association between severity of psychological IPV and mental health outcomes
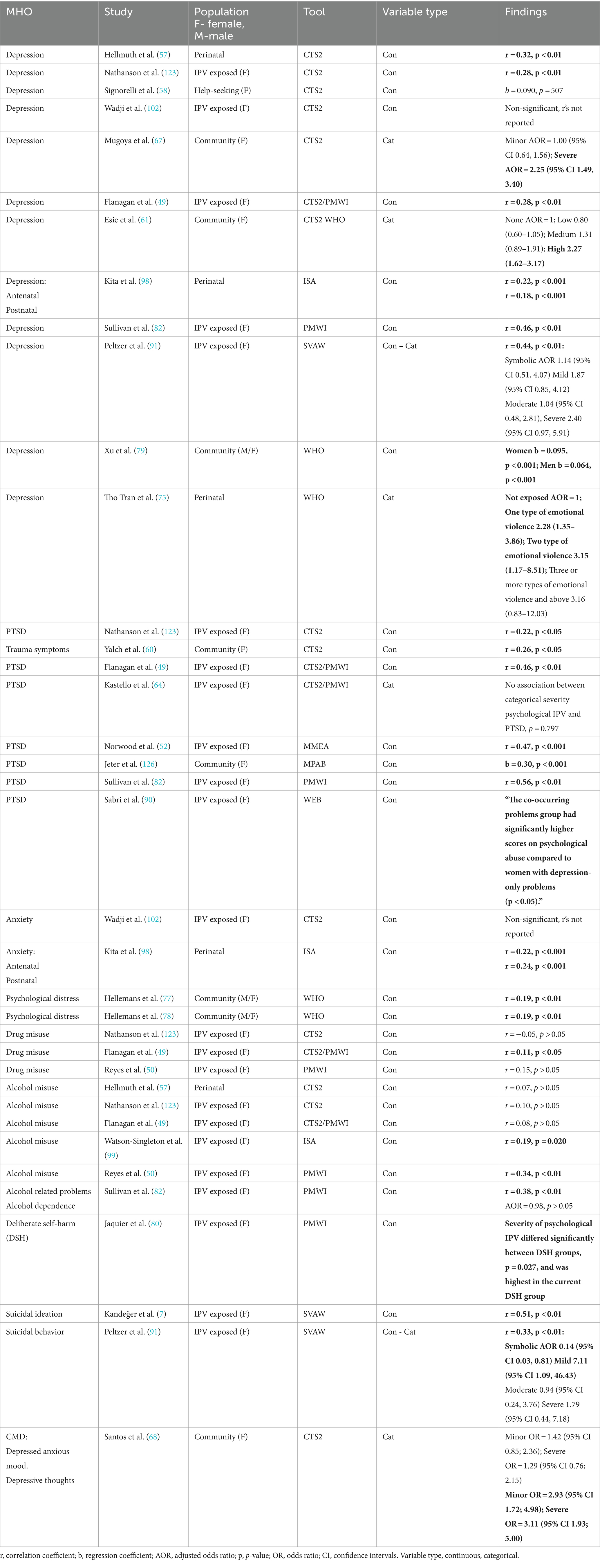
Illustrated in Table 4 are the 24 studies that conducted 42 analyses examining the association between severity of psychological IPV and a range of mental health outcomes: depression (12 studies), alcohol/drug abuse (nine), PTSD/trauma symptoms (eight), anxiety (two), psychological distress (two), suicidal ideation/behavior (two), and deliberate self-harm and common mental disorders (CMD) (one study each).
Overall, severity of psychological IPV was significantly associated with depression in 10 studies (11 analyses, highlighted in bold in Table 4). Seven of these analyses reported correlation coefficients from 0.18 to 0.46, all p < 0.01. The studies by Mugoya et al. (67) and Esie et al. (61) showed significant associations between severity of psychological IPV and depression but only at the “severe” rating of IPV. By contrast the study by Peltzer and Pengpid (91) that used the categorical form of the SVAW measure in subsequent regression analysis, did not find a statistically significant association. In Tho Tran et al. (75) they found increasing AOR’s with increasing number of types of emotional violence (expressed categorically). The lower confidence intervals around these AOR’s are above one except for the highest number of types of emotional violence category which encompasses one. The study by Xu et al. (79) reported significant associations between severity of psychological IPV and depression in both male and female participants.
Table 4 indicates that the severity of psychological IPV and PTSD are significantly associated in seven studies, with statistically significant correlation coefficients being reported in five studies ranging from 0.22 to 0.56. In the two studies examining anxiety as the outcome, only Kita et al. (98) found statistically significant correlation coefficients between severity of psychological IPV, as measured by ISA, and anxiety in both the ante and postnatal periods, r = 0.22 and 0.24, respectively. Moreover, both studies by Hellemans et al. (77, 78) which examined the association between psychological distress and severity of psychological IPV, reported statistically significant correlations of 0.19. However, the sample of adults of Turkish origin in Hellemans et al. (77) is a subsample (n = 392) of the general population sample in the other study by the same author (n = 1,445).
In the 10 analyses examining the association between severity of psychological IPV and alcohol/drug abuse, four showed a statistically significant correlation of severity of psychological IPV and use of substances. In Flanagan et al. (49) severity of psychological IPV was statistically significantly correlated (r = 0.11) to drug use, while correlations ranged from 0.19 to 0.38 in three studies (50, 82, 99) examining the association between the severity of psychological IPV and alcohol use. However, Sullivan et al. (82) also found that severity of psychological IPV was not a predictor of alcohol dependence in a regression analysis controlling for covariates.
The three studies exploring the association between severity of psychological IPV and suicide reported statistically significant positive correlations. However, Peltzer and Pengpid (91) conducted a regression analysis which did not provide evidence of a significant relationship between moderate and more severe IPV and greater odds of suicidal ideation/behavior. Finally, Jaquier et al. (80) indicated that severity of psychological IPV differed between three groups of women: those who currently self-harm, those who had in the past, and those who had never done so. Women who currently self-harm had the highest mean score of severity of psychological IPV. In the study by Santos and Monteiro (68) examining common mental health disorders, they reported significant associations between severity of psychological IPV and depressive thoughts at both minor and severe ratings of IPV. In this same study, depressed anxious mood was not associated with either minor or severe IPV.
4.2.3 Association between severity of sexual IPV and mental health outcomes
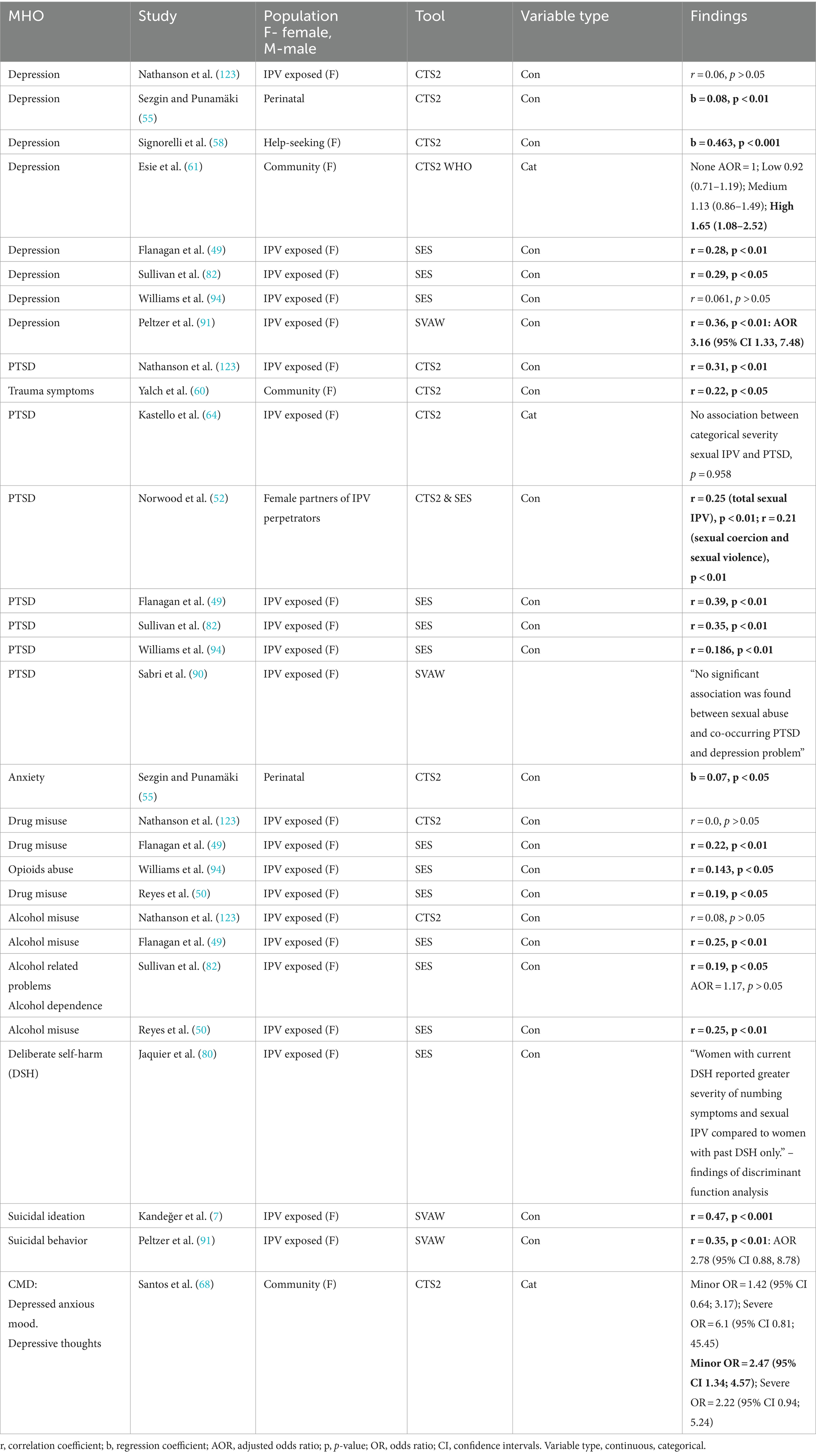
In Table 5 we highlight the 17 studies that explored the association between severity of sexual IPV and mental health outcomes: alcohol/drug use (nine studies), PTSD/trauma symptoms (eight studies), depression (eight studies), suicidal ideation/behavior (two studies), anxiety (one study), deliberate self-harm (one study) and common mental health disorders (one study).
Of the eight analyses of depression, six had significant associations between the severity of sexual violence and depression, three of which found correlation coefficients ranging from 0.29 to 0.36. Moreover, Esie et al. (61), where they used a four-level categorical rating of severity of sexual IPV, they found that just the highest severity of sexual IPV was statistically significantly associated with depression with AOR equal to 1.65. In studies using regression analyses (55, 58) significant associations between severity of sexual IPV and depression remained after multiple regression. The study by Peltzer and Pengpid (91) reported statistically significant associations between severity of sexual IPV and depression when depression was analyzed as both continuous (with correlation) and dichotomous (with logistic regression).
Of the eight studies examining the association between the severity of sexual IPV and PTSD, six reported statistically significant correlation coefficients ranging from 0.186 to 0.39. The study by Sezgin and Punamäki (55) using multiple regression models reported a significant positive association between severity of sexual IPV and anxiety. Moreover, six of the nine studies examining use of drugs or alcohol as an outcome, reported statistically significant correlation coefficients ranging from 0.143 to 0.25.
Suicidality was analyzed as the outcome in three studies, two of which reported statistically significant correlations between severity of sexual IPV and suicidal ideation/behavior, r = 0.35 and 0.47. However, Peltzer and Pengpid (91) went on to explore the association further in a logistic regression model and reported a non-significant AOR. Jaquier et al. (80) found that severity of sexual IPV significantly discriminated between women who currently self-harm and those who have done in the past, with those who currently self-harm scoring higher on severity of sexual IPV. An unadjusted analysis by Santos and Monteiro (68) found that minor severity of IPV was statistically significantly associated with depressive thoughts, while severe IPV was not.
5 Discussion
This review, comprising 76 studies, identified 22 measures utilized to evaluate the prevalence, incidence, risk, and severity of IPV and its association with mental health outcomes. The review underscored researchers’ inclinations to modify IPV measures frequently without reassessing their validity. Additionally, the commonly used measure CTS2 was seldom applied in its initially validated form. By contrast, measures exclusively measuring a single subtype of IPV, especially those developed more recently, were rarely modified. We found inconsistent findings regarding minor and severe categorical ratings of IPV severity. The examination of evidence concerning the correlation between the severity of IPV and mental health outcomes emphasizes the need for the application of statistical methods that produce more robust and accurate estimates of effect. Particularly, these estimates should be adjusted for relevant confounding variables using regression models to reduce bias.
5.1 Measurement of IPV severity in practice
Previous research has assessed the psychometric properties of IPV measures [(see 103–105)]. In our review we found that numerous studies altered the measures of IPV severity. This raises concerns about the potential impacts on the psychometric properties of the measures and in so doing jeopardizes the credibility and applicability of research findings in this critical area. It is important that researchers scientifically demonstrate the quality of their methods of measurement by showing that they are statistically reliable (13) whereby indicating how consistently the new construct is measured (e.g., test–retest reliability, internal reliability). Undertaking appropriate validity tests (e.g., content validity, construct validity, predictive validity) is key to being confident that the data, as collected and analyzed, accurately capture the true picture of what is being measured.
The operationalization of violence severity has also varied across studies: we identified scoring inconsistencies which compromised the assurance that the severity levels assigned to various incidents held uniform meaning and implications across studies. Two types of categorical ratings for the severity of IPV were found: the severity classifications were either determined by (1) the creators of assessment tools (e.g., CTS2 and WHO tools), who categorized acts as “minor” or “severe,” or (2) by the authors of individual studies. For instance, Esie et al. (61) established categories (low, medium, high) based on cut-off points from the continuous form of IPV severity, while Mugoya et al. (67), used the number of types of IPV experienced for their categories. Lack of consistency in applying validated methods for scoring instruments to determine abuse severity may reflect the lack of consensus in defining abuse (13). When making scoring decisions researchers face real difficulties in establishing reasonable comparison groups to investigate differences that might inform interventions.
Another concern arises from the practice of categorizing incidents at a single point in time, in cross-sectional studies, which would not accurately capture changes in the severity of IPV over time. This approach could overlook the escalation or de-escalation of violence and result in underreporting. Survivors may be reluctant to report incidents, especially when a relationship has not been established with researchers, due to fear or shame. The use of categorical measures may contribute to underreporting, as survivors might only disclose incidents they perceive as “severe,” potentially neglecting less severe occurrences. This selective reporting, combined with the normalization of IPV in societies (2), can lead to an inaccurate portrayal of the prevalence and distribution of IPV. This is important because underreporting means that services and support cannot be put in place. Research shows (106) that individuals report minor physical violence on measures such as the CTS, but do not report such assaults on crime victimization scales or when asked a general question about experiencing physical violence in a relationship because they usually do not interpret such aggression as having the significance of a legally defined assault. In their study Hamby et al. (106) compared endorsement of the CTS’s physical aggression items with subjective reports of experiencing partner violence, and found that minor and infrequent moderate acts of physical aggression that were endorsed on the CTS were not reported as subjective experiences of partner aggression.
Creating categorical ratings of IPV severity from continuous scores may simplify analysis and interpretation, but it also comes with several limitations. These include: (i) loss of information which can produce less accurate and precise results and therefore a reduction in statistical power, (ii) arbitrary cut-off points meaning that results are not reproducible across studies, and (iii) misrepresented relationships between variables, where arbitrary cut-off points mean that the nuances of the original variable distribution are no longer present (107). In contrast, the practice of dichotomizing the sample by categorizing individuals into two groups for analysis—such as placing anyone who has encountered at least one instance of IPV into the abuse group and categorizing everyone else with zero occurrences in each category into the non-abused group—is misleading (13). This dichotomous classification for victimization combines individuals who have experienced a single incident with those who have undergone extensive victimization. Research studies have shown that individuals experiencing very small amounts of IPV generally appear to be much more similar to those experiencing no IPV behaviors (108). Therefore, dichotomization solely based on the experience of any IPV is prone to misinterpretation. There is a risk of overlooking effects linked to a higher threshold of abuse within a relationship when individuals surpassing that threshold are grouped together with those who have encountered minimal IPV, resulting in an averaging effect.
5.2 The association between severity of IPV and mental health outcomes
A number of studies showed that increasing severity of IPV, when measured using “minor” and “severe” categorizations of IPV, was significantly associated with poorer mental health (see Tables 2, 3) (67, 70). At the same time, other studies reported that ‘minor’ or lower severity of IPV was not linked to poorer mental health, but when the violence was more severe, mental health tended to suffer (see Tables 3, 4) (61, 67). However, our review also revealed examples of statistically significant associations between minor IPV and outcome, with severe IPV and outcome unrelated, despite higher adjusted odds ratios (AOR) in Peltzer and Pengpid (91) and Santos and Monteiro (68) studies. These apparent false negatives may occur because severe IPV is less common and therefore the parameter estimates are less precise, increasing the risk of a Type II error.
In our review, the severity of IPV and its subtypes was consistently linked to various mental health outcomes across studies. We identified evidence that experiencing more subtypes of IPV was associated with poorer mental health outcomes (70, 72, 76, 109). Generally, more severe overall IPV and its subtypes correlated with poorer mental health outcomes, as indicated by positive correlation and regression coefficients, and Odds Ratios (ORs) and AORs greater than 1. Our analyses did not reveal wholly consistent patterns that would allow for a comprehensive determination of how distinct IPV subtypes affect mental health outcomes differently, but we speculate that the mental health outcome most affected by increasing severity of physical IPV is PTSD. Increasing severity of psychological IPV appears to be most constantly associated with depression. Severity of sexual IPV was explored in less studies but the evidence of its impact varying dependent on mental health outcomes was less compelling. While ideal, conducting meta-analyses to establish robust pooled estimates of these relationships faces challenges due to significant clinical and statistical heterogeneity, especially considering variations and inconsistencies in measuring and analyzing IPV severity across studies (1). Performing meta-analyses to unpick the impact of differing severity within subtypes of IPV is unlikely to produce valid and reliable results.
The studies reviewed exhibited variation in the assessment of mental health outcomes. Some studies evaluate mental health on a spectrum, while others use a dichotomous approach. These differing methods pose distinct questions: does increased severity of IPV correlate with more pronounced mental health symptoms, or does heightened severity of IPV increase the likelihood of exceeding the threshold indicative of clinically significant mental health outcomes? This variability is influenced by the study population, as some studies recruit participants based on clinical diagnoses.
Studies in the review differed with regards to the populations being studied and we categorized them as those which focused on women with previous IPV experiences, those in the community and those in perinatal samples. Without a prerequisite of IPV exposure, any measure of IPV severity showed zero-inflation, indicating that a significant proportion of the sample had not experienced IPV. This resulted in highly skewed severity scores (59, 63, 67, 69), posing challenges to analysis and interpretation, such as violating statistical assumptions and lacking sensitivity in modeling the true relationship. To address skewness, some studies applied transformations (59), though these could not correct for zero-inflation. Others (63, 67, 69) accounted for zero-inflation by using categorical forms of IPV severity; these have their own limitations as illustrated earlier.
In evaluating the association between IPV severity and mental health outcomes, it is crucial to critically assess the statistical analyses employed in these studies. Many studies relied on correlation coefficients. However, correlation coefficients are valid only for linear relationships between two variables and may oversimplify the complex connections between IPV and mental health, potentially missing nonlinear or threshold effects. Statistically, correlation coefficients measure the strength of a linear relationship along a continuous scale, but their interpretation can be misleading (110). Significance tests may yield statistically significant results with large sample sizes, even when the correlation value is clinically irrelevant. Statistical literature emphasizes the cautious interpretation of correlation coefficients (111–113). These coefficients are inadequate for determining causality direction—whether IPV directly causes mental health outcomes, vice versa, or if other factors influence both variables. Many reported coefficients serve as a preliminary analysis, preceding more comprehensive methods like structural equation modeling. Correlation coefficients alone are insufficient to describe the relationship and do not consider potential confounding variables such as socioeconomic status, social support, trauma history, responses to disclosures, and access to mental health resources. Regression models were used by some studies [(e.g., 54, 55)] allowing the inclusion of potentially confounding variables into the model. These models can be extended for longitudinal studies which can support claims of temporal causality.
Another issue is the lack of survivor involvement in the development, scoring and weighting of IPV measures. Of the eight commonly used IPV measures, only one explicitly involved people with lived experience of IPV in their development, and none reported involving people with IPV in decisions about scoring and weighting. This was the Danger Assessment Scale which was developed with consultation and content validity support from IPV survivors, shelter workers, law enforcement officials, and other clinical experts on IPV. In addition, the WHO Multi-country Study on Women’s Health and Domestic Violence Against Women had an expert consultation group on violence against women bringing together researchers, health care providers and women’s health advocates from several countries. The lack of survivor involvement might impact the ecological validity of the measures - their ability to reflect the real world (114). This could minimize or inflate the severity and impact of IPV incidents, bearing in mind their complexity and location in dynamic and evolving circumstances. There is also a risk that where measures are self-report (n = 6), researchers assume they are hearing directly from people who have experienced IPV and are capturing issues that are important and relevant to them. However, as the measures themselves might not reflect how people with lived experience understand, experience and weight the severity of IPV incidents, the information gathered is likely to be partial, potentially only capturing researcher’s conceptualizations of IPV severity. This raises the possibility of confirmation bias.
Finally, to the best of our knowledge, none of the eight IPV measures assessed the acceptability of the content to people who have experienced IPV. Acceptability, defined as a subjective evaluation of an intervention’s content made by their recipients, is important because successful implementation depends on the acceptability of the intervention to recipients and needs to be considered in the development, evaluation and implementation phases of any healthcare interventions (115). Completion of measurement tools can be considered a healthcare intervention particularly when being used in routine clinical practice. Acceptability is a precursor to fidelity (use as intended) which is a precursor for implementation (116). In reviewing measures, we noted that questions are deeply intrusive by their nature, and potentially distressing and shaming. This, coupled with the victim-blaming that is present across societies, could result in significant under-reporting as well as minimization of the severity of incidents and a lack of acceptability to users. We must ask ourselves what it is that measures of IPV severity are able to reveal.
5.3 Limitations
Undertaking secondary data analysis research avoids study repetition and over-research of sensitive topics/populations. However, there are drawbacks of utilizing data from a previous systematic review. For instance, the last search was conducted a considerable time ago (November 2020), potentially missing out on pertinent studies related to the topic. However, recent papers are unlikely to alter the established findings on the severity of IPV and its impact on mental health outcomes. Additionally, the eligibility criteria for the systematic review may not be optimal for addressing the current research question. In addition to this the limitations in the included studies, such as the researchers’ practice of deviating from the original scoring scheme of the IPV severity measures, made it impossible for us to directly compare findings across different studies or contexts. The heterogeneity of the included studies (e.g., diverse populations, settings, measurement tools and participant characteristics) was a challenge as we could not consider pooling data for secondary analysis which could have enhanced the generalizability and interpretation of the findings. The absence of standardized reporting for results and outcomes also presented a difficulty, as inconsistent reporting standards impeded our ability to effectively synthesize findings across studies. Furthermore, another limitation is that we did not reach out to authors to obtain any missing data.
5.4 Recommendations
When assessing incidents of IPV we recommend adopting a dynamic and longitudinal approach. Rather than categorizing incidents at a single point in time, practitioners should consider implementing methods that allow for the monitoring and evaluation of changes in the severity of IPV over time. This may involve utilizing measures or assessments that capture the evolving nature of IPV experiences and patterns, providing a more accurate and comprehensive understanding of the dynamics involved. Longitudinal assessments can contribute to a more nuanced and contextually rich perspective, enabling interventions and support services to be tailored to the evolving needs of individuals experiencing IPV.
Considering the outcomes of our review, which revealed the inadequacy of existing measures in assessing IPV and its severity, we propose the development of a new measure, one that actively involves individuals with lived experiences of IPV in the development, scoring, and weighting processes. The aim would be to create a measure that is not only scientifically rigorous but also ethically and culturally appropriate, promoting a more comprehensive and empathic understanding of IPV. Ample evidence exists of methods to generate reliable and valid outcome measures from the perspectives of service users (117, 118); these could be adopted by researchers working with IPV survivors. The model involves participatory qualitative and psychometric methodology to explore survivors’ experiences and perspectives and translate these into psychometrically robust outcome measures (119).
Addressing cross-cultural considerations in the measurement of IPV is crucial because how IPV is understood within a particular culture can significantly impact its identification, risk assessment, and connection to care. Cultural norms may influence what can be measured in research or clinical settings. For instance, cultural sanctions might restrict the disclosure of sexual IPV, limiting the ability to measure its effects on mental and physical health or its inclusion as an outcome in interventions (109, 120, 121). Additionally, these norms can shape how questions are framed, affecting the translation and adaptation of assessment tools across different regions.
Moreover, enhancing coordination and collaboration across sectors in the collection of IPV data is essential, as various agencies—such as health services, specialist services, criminal justice, and welfare services—must work together to reduce and eliminate violence (15). It is also important for researchers and policymakers to collect data that aligns with their specific areas of responsibility. Definitions and interpretations of IPV vary between and within disciplines and sectors. While some of this variation reflects the differing priorities of these agencies, which is often justified, other differences are simply historical and offer little practical value. Even when complete alignment in the conceptualization and measurement of violence across fields is not possible, the frameworks should at least be compatible or translatable (2).
6 Conclusion
There is a tendency in many research studies of intimate partner violence to inadequately characterize the distribution of severity of violence in the study sample, crucially impacting on our ability to interpret results and making meaningful comparisons across studies. IPV is multifaceted, with acts and forms that can shift and overlap, creating dynamic and concurrent patterns. This complexity poses significant challenges for measurement, as it requires capturing not just individual instances but also the evolving and interacting nature of violent behaviors. Traditional measurement tools may struggle to account for these fluid dynamics, making comprehensive assessment more difficult. However, accurate measurement is essential for assessment of the relationship between severity of IPV and mental health problems, one that is developed with and acceptable to individuals with experience of IPV. Men and women exposed to a range of types and severity of IPV can experience a broad spectrum of adverse mental health outcomes. However, it is not possible to make more definitive, specific claims regarding the relative effects of IPV subtypes on mental health. Chronic exposure to IPV is associated with heightened mental health issues, although this association is influenced, at least in part, by the specific type of IPV encountered.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
SW: Conceptualization, Funding acquisition, Investigation, Writing – original draft, Data curation, Formal analysis, Methodology, Software. LB: Writing – review & editing. AS: Writing – review & editing, Conceptualization, Funding acquisition. NM: Conceptualization, Funding acquisition, Writing – review & editing, Formal analysis, Investigation, Project administration, Resources, Supervision, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This project was funded by the Violence, Abuse and Mental Health Network, which was funded by UK Research and Innovation, and their support was gratefully acknowledged. Grant reference number ES/S004424/1.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. White, SJ, Sin, J, Sweeney, A, Salisbury, T, Wahlich, C, Montesinos Guevara, CM, et al. Global prevalence and mental health outcomes of intimate partner violence among women: a systematic review and Meta-analysis. Trauma Violence Abuse. (2023) 25:494–511. doi: 10.1177/15248380231155529
2. Oram, S, Fisher, HL, Minnis, H, Seedat, S, Walby, S, Hegarty, K, et al. The lancet psychiatry commission on intimate partner violence and mental health: advancing mental health services, research, and policy. Lancet Psychiatry. (2022) 9:487–524. doi: 10.1016/S2215-0366(22)00008-6
3. Ahmadabadi, Z, Najman, JM, Williams, GM, Clavarino, AM, d'Abbs, P, and Tran, N. Intimate partner violence and subsequent depression and anxiety disorders. Soc Psychiatry Psychiatr Epidemiol. (2020) 55:611–20. doi: 10.1007/s00127-019-01828-1
4. Al-Modallal, H. Effect of intimate partner violence on health of women of Palestinian origin. Int Nurs Rev. (2016) 63:259–66. doi: 10.1111/inr.12239
5. Brown, SJ, Mensah, F, Giallo, R, Woolhouse, H, Hegarty, K, Nicholson, JM, et al. Intimate partner violence and maternal mental health ten years after a first birth: an Australian prospective cohort study of first-time mothers. J Affect Disord. (2020) 262:247–57. doi: 10.1016/j.jad.2019.11.015
6. Daugherty, JC, Pérez-García, M, Hidalgo-Ruzzante, N, and Bueso-Izquierdo, N. Perceived executive functioning among female survivors of intimate partner Violenc e. J Aggress Maltreat Trauma. (2021) 30:25–42. doi: 10.1080/10926771.2020.1783734
7. Kandeğer, A, and Naziroğlu, A. The mediating effects of self-perception and somatoform dissociation in the relationship between domestic violence and suicidal ideation. Arch Womens Ment Health. (2021) 24:251–7. doi: 10.1007/s00737-020-01064-6
8. Thomas, R, Dyer, GS, Tornetta Iii, P, Park, H, Gujrathi, R, Gosangi, B, et al. Upper extremity injuries in the victims of intimate partner violence. Eur Radiol. (2021) 31:5713–20. doi: 10.1007/s00330-020-07672-1
9. Higgins, A, Doyle, L, Downes, C, Morrissey, J, Costello, P, Brennan, M, et al. There is more to risk and safety planning than dramatic risks: mental health nurses’ risk assessment and safety-management practice. Int J Ment Health Nurs. (2016) 25:159–70. doi: 10.1111/inm.12180
10. Devries, KM, Mak, JY, Garcia-Moreno, C, Petzold, M, Child, JC, Falder, G, et al. Global health. The global prevalence of intimate partner violence against women. Science. (2013) 340:1527–8. doi: 10.1126/science.1240937
11. United Nations. (2014). Guidelines for producing statistics on violence against women. United Nations, UN.
12. Bender, AK. Ethics, methods, and measures in intimate partner violence research: the current state of the field. Violence Against Women. (2017) 23:1382–413. doi: 10.1177/1077801216658977
13. Follingstad, DR. The challenges of measuring violence against women. In: eds. CM Renzetti, JL Edleson, and RK Bergen (Eds.), (Third Edition) Sourcebook on violence against women Thousand Oaks, CA: Sage Publications, Inc. 57–78. (2017).
14. Hamby, S. Measuring gender differences in partner violence: implications from research on other forms of violent and socially undesirable behavior. Sex Roles. (2005) 52:725–42. doi: 10.1007/s11199-005-4195-7
15. Walby, S, Towers, J, Balderston, S, Corradi, C, Francis, B, Heiskanen, M, et al. The concept and measurement of violence against women and men, Bristol: Policy Press (2017).
16. Walby, S, and Towers, JS. Measuring violence to end violence: mainstreaming gender. J Gender Based Viol. (2017) 1:11–31. doi: 10.1332/239868017X14913081639155
17. Walby, S, and Towers, J. Untangling the concept of coercive control: theorizing domestic violent crime. Criminol Crim Just. (2018) 18:7–28. doi: 10.1177/1748895817743541
18. Straus, M, Hamby, SL, Boney-McCoy, S, and Sugarman, DB. The revised conflict tactics scales (CTS2) development and preliminary psychometric data. J Fam Issues. (1996) 17:283–316. doi: 10.1177/019251396017003001
19. Barrett, BJ, and Pierre, MS. Variations in women’s help seeking in response to intimate partner violence: findings from a Canadian population-based study. Violence Against Women. (2011) 17:47–70. doi: 10.1177/1077801210394273
20. Cho, H, and Wilke, DJ. Gender differences in the nature of the intimate partner violence and effects of perpetrator arrest on revictimization. J Fam Violence. (2010) 25:393–400. doi: 10.1007/s10896-009-9300-1
21. Coker, AL, Smith, PH, McKeown, RE, and King, MJ. Frequency and correlates of intimate partner violence by type: physical, sexual, and psychological battering. Am J Public Health. (2000) 90:553–9. doi: 10.2105/AJPH.90.4.553
22. Johnson, MP. Conflict and control: gender symmetry and asymmetry in domestic violence. Violence Against Women. (2006) 12:1003–18. doi: 10.1177/1077801206293328
23. Ansara, DL, and Hindin, MJ. Exploring gender differences in the patterns of intimate partner violence in Canada: a latent class approach. J Epidemiol Community Health. (2010) 64:849–54. doi: 10.1136/jech.2009.095208
24. Lysova, A, and Dim, EE. Severity of victimization and formal help seeking among men who experienced intimate partner violence in their ongoing relationships. J Interpers Violence. (2022) 37:1404–29. doi: 10.1177/0886260520922352
25. Walby, S, Towers, J, and Francis, B. Is violent crime increasing or decreasing? A new methodology to measure repeat attacks making visible the significance of gender and domestic relations. Br J Criminol. (2016) 56:1203–34. doi: 10.1093/bjc/azv131
26. Follingstad, D. Rethinking current approaches to psychological abuse: conceptual and methodological issues. Aggress Violent Behav. (2007) 12:439–58. doi: 10.1016/j.avb.2006.07.004
27. Ryan, KM. Issues of reliability in measuring intimate partner violence during courtship. Sex Roles. (2013) 69:131–48. doi: 10.1007/s11199-012-0233-4
28. Follingstad, D, and Bush, H. Measurement of intimate partner violence: a model for developing the gold standard. Psychol Violence. (2014) 4:369–83. doi: 10.1037/a0037515
29. Mantovani, N, Sweeney, A, Sin, J, White, S, du Mello Kenyon, G, Iqbal, N, et al. A systematic review and meta-analysis to measure mental health harms in women and men associated with different thresholds of violence and abuse (VA). PROSPERO Int Prospect Reg Syst Rev. (2020). Available at: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020177744
30. Trevillion, K, Oram, S, Feder, G, and Howard, LM. Experiences of domestic violence and mental disorders: a systematic review and meta-analysis. PLoS One. (2012) 7:e51740. doi: 10.1371/journal.pone.0051740
31. Popay, J, Roberts, H, Sowden, A, Petticrew, M, Arai, L, Rodgers, M, et al. Guidance on the conduct of narrative synthesis in systematic reviews. Prod ESRC Methods Prog Vers. (2006) 1:b92. doi: 10.13140/2.1.1018.4643
32. Kelly, U, and Pich, K. Community-based PTSD treatment for ethnically diverse women who experienced intimate partner violence: a feasibility study. Issues Ment Health Nurs. (2014) 35:906–13. doi: 10.3109/01612840.2014.931496
33. Straus, M. Measuring Intrafamily conflict and violence: the conflict tactics (CT) scales. J Marriage Fam. (1979) 41:75–88. doi: 10.2307/351733
34. Straus, M, Hamby, SL, and Warren, WL. The conflict tactics scales handbook: revised conflict tactics scales (CTS2): CTS: parent-child version (CTSPC). Los Angeles, CA: Western Psychological Services (2003).
35. García-Moreno, C, Jansen, HA, Ellsberg, M, Heise, L, and Watts, C. WHO multi-country study on women’s health and domestic violence against women. Geneva: World Health Organization (2005).
36. Garcia-Moreno, C, Jansen, HA, Ellsberg, M, Heise, L, and Watts, CH. Prevalence of intimate partner violence: findings from the WHO multi-country study on women's health and domestic violence. Lancet. (2006) 368:1260–9. doi: 10.1016/s0140-6736(06)69523-8
37. Campbell, J. Assessing dangerousness: violence by sexual offenders, batterers, and child abusers. Sage Publications, Inc (1995).
38. Campbell, J, Webster, D, Koziol-McLain, J, Block, C, Campbell, D, Curry, MA, et al. Risk factors for femicide in abusive relationships: results from a multisite case control study. Am J Public Health. (2003) 93:1089–97. doi: 10.2105/ajph.93.7.1089
39. Campbell, J, Webster, DW, and Glass, N. The danger assessment: validation of a lethality risk assessment instrument for intimate partner femicide. J Interpers Violence. (2009) 24:653–74. doi: 10.1177/0886260508317180
40. Tolman, R. The development of a measure of psychological maltreatment of women by their male partners. Violence Vict. (1989) 4:159–77. doi: 10.1891/0886-6708.4.3.159
41. Tolman, R. The validation of the psychological maltreatment of women inventory. Violence Vict. (1999) 14:25–37. doi: 10.1891/0886-6708.14.1.25
42. Koss, MP, Abbey, A, Campbell, R, Cook, S, Norris, J, Testa, M, et al. Revising the SES: a collaborative process to improve assessment of sexual aggression and victimization. Psychol Women Q. (2007) 31:357–70. doi: 10.1111/j.1471-6402.2007.00385.x
43. Koss, MP, and Gidycz, CA. Sexual experiences survey: reliability and validity. J Consult Clin Psychol. (1985) 53:422–3. doi: 10.1037/0022-006X.53.3.422
44. Koss, MP, Gidycz, CA, and Wisniewski, N. The scope of rape: incidence and prevalence of sexual aggression and victimization in a national sample of higher education students. J Consult Clin Psychol. (1987) 55:162–70. doi: 10.1037/0022-006X.55.2.162
45. Koss, MP, and Oros, CJ. Sexual experiences survey: a research instrument investigating sexual aggression and victimization. J Consult Clin Psychol. (1982) 50:455–7. doi: 10.1037/0022-006X.50.3.455
46. Marshall, LL. Development of the severity of violence against women scales. J Fam Violence. (1992) 7:103–21. doi: 10.1007/BF00978700
47. Hegarty, K, Sheehan, M, and Schonfeld, C. A multidimensional definition of partner abuse: development and preliminary validation of the composite abuse scale. J Fam Violence. (1999) 14:399–415. doi: 10.1023/A:1022834215681
48. Hudson, WW, and McIntosh, SR. The assessment of spouse abuse: two quantifiable dimensions. J Marriage Fam. (1981) 43:873–88. doi: 10.2307/351344
49. Flanagan, JC, Jaquier, V, Overstreet, N, Swan, SC, and Sullivan, TP. The mediating role of avoidance coping between intimate partner violence (IPV) victimization, mental health, and substance abuse among women experiencing bidirectional IPV. Psychiatry Res. (2014) 220:391–6. doi: 10.1016/j.psychres.2014.07.065
50. Reyes, ME, Weiss, NH, Swan, SC, and Sullivan, TP. The role of acculturation in the relation between intimate partner violence and substance misuse among IPV-victimized Hispanic women in the community. J Interpers Violence. (2022) 37:NP7057-NP7081. doi: 10.1177/0886260520967134
51. Young-Wolff, KC, Hellmuth, J, Jaquier, V, Swan, SC, Connell, C, and Sullivan, TP. Patterns of resource utilization and mental health symptoms among women exposed to multiple types of victimization: a latent class analysis. J Interpers Violence. (2013) 28:3059–83. doi: 10.1177/0886260513488692
52. Norwood, A, and Murphy, C. What forms of abuse correlate with PTSD symptoms in partners of men being treated for intimate partner violence? Psychol Trauma Theory Res Pract Policy. (2012) 4:596–604. doi: 10.1037/a0025232
53. Wolford-Clevenger, C, and Smith, PN. The conditional indirect effects of suicide attempt history and psychiatric symptoms on the association between intimate partner violence and suicide ideation. Personal Individ Differ. (2017) 106:46–51. doi: 10.1016/j.paid.2016.10.042
54. Tsai, AC, Tomlinson, M, Comulada, WS, and Rotheram-Borus, MJ. Intimate partner violence and depression symptom severity among south African women during pregnancy and postpartum: population-based prospective cohort study. PLoS Med. (2016) 13:e1001943. doi: 10.1371/journal.pmed.1001943
55. Sezgin, AU, and Punamäki, R-L. Impacts of early marriage and adolescent pregnancy on mental and somatic health: the role of partner violence. Arch Womens Ment Health. (2020) 23:155–66. doi: 10.1007/s00737-019-00960-w
56. Fleming, KN, Newton, TL, Fernandez-Botran, R, Miller, JJ, and Burns, VE. Intimate partner stalking victimization and posttraumatic stress symptoms in post-abuse women. Violence Against Women. (2012) 18:1368–89. doi: 10.1177/1077801212474447
57. Hellmuth, JC, Gordon, KC, Moore, TM, and Stuart, GL. The moderating effect of women’s alcohol misuse on the relationship between intimate partner violence victimization and postpartum depression. Am J Addict. (2014) 23:613–5. doi: 10.1111/j.1521-0391.2014.12137.x
58. Signorelli, MS, Fusar-Poli, L, Arcidiacono, E, Caponnetto, P, and Aguglia, E. Depression, PTSD and alexithymia in victims of intimate partner violence: a case-control study. Arch Clin Psychiatr. (2020) 47:45–50. doi: 10.1590/0101-60830000000230
59. Yalch, MM, and Levendosky, AA. Main and moderating effects of temperament traits on the association between intimate partner violence and hazardous alcohol use in a sample of young adult women. Psychol Trauma Theory Res Pract Policy. (2018) 10:611–8. doi: 10.1037/tra0000311
60. Yalch, MM, Levendosky, AA, Bernard, NK, and Bogat, GA. Main and moderating influence of temperament traits on the association between intimate partner violence and trauma symptoms. J Interpers Violence. (2017) 32:3131–48. doi: 10.1177/0886260515596978
61. Esie, P, Osypuk, TL, Schuler, SR, and Bates, LM. Intimate partner violence and depression in rural Bangladesh: accounting for violence severity in a high prevalence setting. SSM Popul Health. (2019) 7:100368. doi: 10.1016/j.ssmph.2019.100368
62. Illangasekare, SL, Burke, JG, McDonnell, KA, and Gielen, AC. The impact of intimate partner violence, substance use, and HIV on depressive symptoms among abused low-income urban women. J Interpers Violence. (2013) 28:2831–48. doi: 10.1177/0886260513488682
63. Kaplan, LM, Hill, TD, and Mann-Deibert, GR. Does alcohol consumption exacerbate the mental health consequences of interpersonal violence? Violence Against Women. (2012) 18:289–308. doi: 10.1177/1077801212442623
64. Kastello, JC, Jacobsen, KH, Gaffney, KF, Kodadek, MP, Bullock, LC, and Sharps, PW. Posttraumatic stress disorder among low-income women exposed to perinatal intimate partner violence: posttraumatic stress disorder among women exposed to partner violence. Arch Womens Ment Health. (2016) 19:521–8. doi: 10.1007/s00737-015-0594-0
65. Lobato, G, Moraes, CL, Dias, AS, and Reichenheim, ME. Alcohol misuse among partners: a potential effect modifier in the relationship between physical intimate partner violence and postpartum depression. Soc Psychiatry Psychiatr Epidemiol. (2012) 47:427–38. doi: 10.1007/s00127-011-0346-z
66. Matseke, G, Peltzer, K, and Mlambo, G. Partner violence and associated factors among pregnant women in Nkangala district, Mpumalanga. South Afr J Obstetr Gynaecol. (2012) 18:77–81. doi: 10.7196/SAJOG.469
67. Mugoya, GC, Witte, T, Bolland, A, Tomek, S, Hooper, LM, Bolland, J, et al. Depression and intimate partner violence among African American women living in impoverished inner-city neighborhoods. J Interpers Violence. (2020) 35:899–923. doi: 10.1177/0886260517691519
68. Santos, AGD, and Monteiro, CFDS. Domains of common mental disorders in women reporting intimate partner violence. Rev Lat Am Enfermagem. (2018) 26:e3099. doi: 10.1590/1518-8345.2740.3099
69. Simmons, SB, Knight, KE, and Menard, S. Long-term consequences of intimate partner abuse on physical health, emotional well-being, and problem behaviors. J Interpers Violence. (2018) 33:539–70. doi: 10.1177/0886260515609582
70. Ziaei, S, Frith, AL, Ekström, EC, and Naved, RT. Experiencing lifetime domestic violence: associations with mental health and stress among pregnant women in rural Bangladesh: the MINIM at randomized trial. PLoS One. (2016) 11:e0168103. doi: 10.1371/journal.pone.0168103
71. Bernstein, M, Phillips, T, Zerbe, A, McIntyre, JA, Brittain, K, Petro, G, et al. Intimate partner violence experienced by HIV-infected pregnant women in South Africa: a cross-sectional study. BMJ Open. (2016) 6:e011999. doi: 10.1136/bmjopen-2016-011999
72. Fisher, J, Tran, TD, Biggs, B, Dang, TH, Nguyen, TT, and Tran, T. Intimate partner violence and perinatal common mental disorders among women in rural Vietnam. Int Health. (2013) 5:29–37. doi: 10.1093/inthealth/ihs012
73. Gibbs, A, Jewkes, R, Willan, S, and Washington, L. Associations between poverty, mental health and substance use, gender power, and intimate partner violence amongst young (18-30) women and men in urban informal settlements in South Africa: a cross-sectional study and structural equation model. PLoS One. (2018) 13:e0204956. doi: 10.1371/journal.pone.0204956
74. Kapiga, S, Harvey, S, Muhammad, AK, Stöckl, H, Mshana, G, Hashim, R, et al. Prevalence of intimate partner violence and abuse and associated factors among women enrolled into a cluster randomised trial in northwestern Tanzania. BMC Public Health. (2017) 17:190. doi: 10.1186/s12889-017-4119-9
75. Tho Tran, N, Nguyen, HTT, Nguyen, HD, Ngo, TV, Gammeltoft, T, Rasch, V, et al. Emotional violence exerted by intimate partners and postnatal depressive symptoms among women in Vietnam: a prospective cohort study. PLoS One. (2018) 13:e0207108. doi: 10.1371/journal.pone.0207108
76. Tran, LM, Nguyen, PH, Naved, RT, and Menon, P. Intimate partner violence is associated with poorer maternal mental health and breastfeeding practices in Bangladesh. Health Policy Plan. (2020) 35:i19–29. doi: 10.1093/heapol/czaa106
77. Hellemans, S, Loeys, T, Buysse, A, and De Smet, O. Prevalence and impact of intimate partner violence (IPV) among an ethnic minority population. J Interpers Violence. (2015) 30:3389–418. doi: 10.1177/0886260514563830
78. Hellemans, S, Loeys, T, Dewitte, M, De Smet, O, and Buysse, A. Prevalence of intimate partner violence victimization and victims’ relational and sexual well-being. J Fam Violence. (2015) 30:685–98. doi: 10.1007/s10896-015-9712-z
79. Xu, X, Zheng, L, Xu, T, and He, M. Intimate partner violence victimization and depressive symptoms in Sichuan, China: are there gender variations? J Interpers Violence. (2022) 37:Np2538–np2564. doi: 10.1177/0886260520944564
80. Jaquier, V, Hellmuth, JC, and Sullivan, TP. Posttraumatic stress and depression symptoms as correlates of deliberate self-harm among community women experiencing intimate partnerviolence. Psychiatry Res. (2013) 206:37–42. doi: 10.1016/j.psychres.2012.09.020
81. Saito, A, Creedy, D, Cooke, M, and Chaboyer, W. Effect of intimate partner violence on postpartum women's health in northeastern Thailand. Nurs Health Sci. (2012) 14:345–51. doi: 10.1111/j.1442-2018.2012.00735.x
82. Sullivan, TP, Ashare, RL, Jaquier, V, and Tennen, H. Risk factors for alcohol-related problems among victims of partner violence. Subst Use Misuse. (2012) 47:673–85. doi: 10.3109/10826084.2012.658132
83. Sullivan, TP, Weiss, NH, Woerner, J, Wyatt, J, and Carey, C. Criminal orders of protection for domestic violence: associated revictimization, mental health, and well-being among victims. J Interpers Violence. (2021) 36:10198–219. doi: 10.1177/0886260519883865
84. Tirado-Muñoz, J, Gilchrist, G, Lligoña, E, Gilbert, L, and Torrens, M. A group intervention to reduce intimate partner violence among female drug users. Results from a randomized controlled pilot trial in a community substance-abuse center. Adicciones. (2015) 27:168–78. doi: 10.20882/adicciones.703
85. Kamimura, A, Parekh, A, and Olson, LM. Health indicators, social support, and intimate partner violence among women utilizing services at a community organization. Womens Health Issues. (2013) 23:e179–85. doi: 10.1016/j.whi.2013.02.003
86. Kulwicki, A, Ballout, S, Kilgore, C, Hammad, A, and Dervartanian, H. Intimate partner violence, depression, and barriers to service utilization in Arab American women. J Transcult Nurs. (2015) 26:24–30. doi: 10.1177/1043659614524000
87. Lucea, MB, Francis, L, Sabri, B, Campbell, JC, and Campbell, DW. Disordered eating among African American and African Caribbean women: the influence of intimate partner violence, depression, and PTSD. Issues Ment Health Nurs. (2012) 33:513–21. doi: 10.3109/01612840.2012.687037
88. McFarlane, J, Maddoux, J, Cesario, S, Koci, A, Liu, F, Gilroy, H, et al. Effect of abuse during pregnancy on maternal and child safety and functioning for 24 months after delivery. Obstet Gynecol. (2014) 123:839–47. doi: 10.1097/AOG.0000000000000183
89. Peterson, K. Learned resourcefulness, danger in intimate partner relationships, and mental health symptoms of depression and PTSD in abused women. Issues Ment Health Nurs. (2013) 34:386–94. doi: 10.3109/01612840.2013.771233
90. Sabri, B, Bolyard, R, McFadgion, AL, Stockman, JK, Lucea, MB, Callwood, GB, et al. Intimate partner violence, depression, PTSD, and use of mental health resources among ethnically diverse black women. Soc Work Health Care. (2013) 52:351–69. doi: 10.1080/00981389.2012.745461
91. Peltzer, K, and Pengpid, S. Associations between intimate partner violence, depression, and suicidal behavior among women attending antenatal and general outpatients hospital services in Thailand. Niger J Clin Pract. (2017) 20:892–9. doi: 10.4103/njcp.njcp_453_15
92. DeCou, CR, Lynch, SM, Cole, TT, and Kaplan, SP. Coping self-efficacy moderates the association between severity of partner violence and PTSD symptoms among incarcerated women. J Trauma Stress. (2015) 28:465–8. doi: 10.1002/jts.22034
93. DeCou, CR, Lynch, SM, Cole, TT, and Kaplan, SP. Dissociation mediates the association between intimate partner violence and posttraumatic stress among treatment-seeking incarcerated women. J Trauma Dissociation. (2016) 17:480–93. doi: 10.1080/15299732.2016.1141148
94. Williams, JR, Cole, V, Girdler, S, and Cromeens, MG. Exploring stress, cognitive, and affective mechanisms of the relationship between interpersonal trauma and opioid misuse. PLoS One. (2020) 15:e0233185. doi: 10.1371/journal.pone.0233185
95. Ford-Gilboe, M, Wathen, CN, Varcoe, C, MacMillan, HL, Scott-Storey, K, Mantler, T, et al. Development of a brief measure of intimate partner violence experiences: the composite abuse scale (revised)—short form (CASR-SF). BMJ Open. (2016) 6:e012824. doi: 10.1136/bmjopen-2016-012824
96. Khadra, C, Wehbe, N, Lachance Fiola, J, Skaff, W, and Nehmé, M. Symptoms of post-traumatic stress disorder among battered women in Lebanon: an exploratory study. J Interpers Violence. (2015) 30:295–313. doi: 10.1177/0886260514534774
97. Comeau, J, and Davies, L. Patterns of depressive symptoms and antidepressant use among women survivors of intimate partner violence. Soc Psychiatry Psychiatr Epidemiol. (2012) 47:1527–37. doi: 10.1007/s00127-011-0459-4
98. Kita, S, Haruna, M, Matsuzaki, M, and Kamibeppu, K. Does antenatal social support affect the relationships between intimate partner violence during pregnancy and perinatal mental health? Violence Against Women. (2020) 26:573–89. doi: 10.1177/1077801219835052
99. Watson-Singleton, NN, Florez, IA, Clunie, AM, Silverman, AL, Dunn, SE, and Kaslow, NJ. Psychosocial mediators between intimate partner violence and alcohol abuse in low-income African American women. Violence Against Women. (2020) 26:915–34. doi: 10.1177/1077801219850331
100. Ferrari, G, Agnew-Davies, R, Bailey, J, Howard, L, Howarth, E, Peters, TJ, et al. Domestic violence and mental health: a cross-sectional survey of women seeking help from domestic violence support services. Glob Health Action. (2016) 9:29890. doi: 10.3402/gha.v9.29890
101. Tutty, LM, Radtke, HL, Thurston, WE, Nixon, KL, Ursel, EJ, Ateah, CA, et al. The mental health and well-being of Canadian indigenous and non-indigenous women abused by intimate partners. Violence Against Women. (2020) 26:1574–97. doi: 10.1177/1077801219884123
102. Wadji, DL, Ketcha Wanda, GJM, Wicky, C, Morina, N, and Martin-Soelch, C. From the mother to the child: the intergenerational transmission of experiences of violence in mother–child dyads exposed to intimate partner violence in Cameroon. J Interpers Violence. (2022) 37:NP3346-NP3376. doi: 10.1177/0886260520948148
103. Alexander, EF, Backes, BL, and Johnson, MD. Evaluating measures of intimate partner violence using consensus-based standards of validity. Trauma Violence Abuse. (2022) 23:1549–67. doi: 10.1177/15248380211013413
104. Arkins, B, Begley, C, and Higgins, A. Measures for screening for intimate partner violence: a systematic review. J Psychiatr Ment Health Nurs. (2016) 23:217–35. doi: 10.1111/jpm.12289
105. Rabin, R. F., Jennings, J. M., Campbell, J. C., and Bair-Merritt, M. H. (2009). Intimate partner violence screening tools: a systematic review. Am J Prev Med, 36, 439–445. e434, doi: 10.1016/j.amepre.2009.01.024
106. Hamby, L, Poindexter, V, and Gray-Little, B. Four measures of partner violence: construct similarity and classification differences. J Marriage Fam. (1996) 58:127–39. doi: 10.2307/353382
107. Altman, DG, and Royston, P. The cost of dichotomising continuous variables. BMJ. (2006) 332:1080. doi: 10.1136/bmj.332.7549.1080
108. Follingstad, D, Bradley, RG, Laughlin, JE, and Burke, L. Risk factors and correlates of dating violence: the relevance of examining frequency and severity levels in a college sample. Violence Vict. (1999) 14:365–80. doi: 10.1891/0886-6708.14.4.365
109. Gibbs, A, Corboz, J, Shafiq, M, Marofi, F, Mecagni, A, Mann, C, et al. An individually randomized controlled trial to determine the effectiveness of the women for women international programme in reducing intimate partner violence and strengthening livelihoods amongst women in Afghanistan: trial design, methods and baseline findings. BMC Public Health. (2018) 18:1–13. doi: 10.1186/s12889-018-5029-1
110. Asuero, AG, Sayago, A, and González, A. The correlation coefficient: an overview. Crit Rev Anal Chem. (2006) 36:41–59. doi: 10.1080/10408340500526766
111. Armstrong, RA. Should Pearson's correlation coefficient be avoided? Ophthalmic Physiol Opt. (2019) 39:316–27. doi: 10.1111/opo.12636
112. Hemphill, JF. Interpreting the magnitudes of correlation coefficients. Am Psychol. (2003) 58:78–9. doi: 10.1037/0003-066X.58.1.78
113. Schober, P, Boer, C, and Schwarte, LA. Correlation coefficients: appropriate use and interpretation. Anesth Analg. (2018) 126:1763–8. doi: 10.1213/ANE.0000000000002864
114. Faulkner, A, and Thomas, P. User-led research and evidence-based medicine. Br J Psychiatry. (2002) 180:1–3. doi: 10.1192/bjp.180.1.1
115. Sekhon, M, Cartwright, M, and Francis, JJ. Acceptability of healthcare interventions: an overview of reviews and development of a theoretical framework. BMC Health Serv Res. (2017) 17:88. doi: 10.1186/s12913-017-2031-8
116. Paynter, C, McDonald, C, Story, D, and Francis, JJ. Application of the theoretical framework of acceptability in a surgical setting: theoretical and methodological insights. Br J Health Psychol. (2023) 28:1153–68. doi: 10.1111/bjhp.12677
117. Evans, M, Gregory, A, Feder, G, Howarth, E, and Hegarty, K. “Even ‘daily’is not enough”: how well do we measure domestic violence and abuse?—a think-aloud study of a commonly used self-report scale. Violence Vict. (2016) 31:3–26. doi: 10.1891/0886-6708.VV-D-15-00024
118. Rose, D, Evans, J, Sweeney, A, and Wykes, T. A model for developing outcome measures from the perspectives of mental health service users. Int Rev Psychiatry. (2011) 23:41–6. doi: 10.3109/09540261.2010.545990
119. Rose, D, Sweeney, A, Leese, M, Clement, S, Jones, IR, Burns, T, et al. Developing a user-generated measure of continuity of care: brief report. Acta Psychiatr Scand. (2009) 119:320–4. doi: 10.1111/j.1600-0447.2008.01296.x
120. Alhalal, E, Ford-Gilboe, M, Wong, C, and Albuhairan, F. The reliability and validity of the Arabic version of the composite abuse scale. Violence Vict. (2019) 34:3–27. doi: 10.1891/0886-6708.VV-D-17-00111
121. Elghossain, T, Bott, S, Akik, C, and Obermeyer, CM. Prevalence of intimate partner violence against women in the Arab world: a systematic review. BMC Int Health Hum Rights. (2019) 19:1–16. doi: 10.1186/s12914-019-0215-5
122. Mertin, P, Moyle, S, and Veremeenko, K. Intimate partner violence and women's presentations in general practice settings: barriers to disclosure and implications for therapeutic interventions. Clin Psychol. (2015) 19:140–6. doi: 10.1111/cp.12039
123. Nathanson, AM, Shorey, RC, Tirone, V, and Rhatigan, DL. The prevalence of mental health disorders in a community sample of female victims of intimate partner violence. Partn Abus. (2012) 3:59–75. doi: 10.1891/1946-6560.3.1.59
124. Edmond, T, Bowland, S, and Yu, M. Use of mental health services by survivors of intimate partner violence. Soc Work Ment Health. (2013) 11:34–54. doi: 10.1080/15332985.2012.734180
125. Wong, JY, Tiwari, A, Fong, DY, Yuen, KH, Humphreys, J, and Bullock, L. Intimate partner violence, depressive symptoms, and immigration status: Does existing advocacy intervention work on abused immigrant women in the Chinese community?. J. Interpers. Violence. (2013) 28:2181–202.
126. Jeter, WK, and Brannon, LA. Moving beyond “sticks and stones”: chronic psychological trauma predicts posttraumatic stress symptoms. Journal of Trauma & Dissociation. (2014) 15:548–56.
127. Mertin, PG. An adaptation of the Conflict Tactics Scales. Australian Journal of Marriage & Family. (1992).
Keywords: intimate partner violence (IPV), severity of IPV, measurement, mental health outcomes (MHO), narrative synthesis review
Citation: White S, Bearne L, Sweeney A and Mantovani N (2024) Examining the measurement of severity of intimate partner violence and its association to mental health outcomes: a narrative synthesis. Front. Public Health. 12:1450680. doi: 10.3389/fpubh.2024.1450680
Edited by:
Ivana Maurović, University of Zagreb, CroatiaReviewed by:
Dean Ajdukovic, University of Zagreb, CroatiaSaranraj Loganathan, Mepco Schlenk Engineering College, India
Roberto Ariel Abeldaño Zuñiga, University of Helsinki, Finland
Copyright © 2024 White, Bearne, Sweeney and Mantovani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nadia Mantovani, bm1hbnRvdmFAc2d1bC5hYy51aw==; Sarah White, c3doaXRlQHNndWwuYWMudWs=
 Sarah White
Sarah White Lindsay Bearne1
Lindsay Bearne1 Nadia Mantovani
Nadia Mantovani