- 1Occupational Medicine Unit, Bambino Gesù Children's Hospital IRCCS, Rome, Italy
- 2Alta Scuola di Economia e Management dei Sistemi Sanitari (ALTEMS), Università Cattolica del Sacro Cuore, Rome, Italy
- 3Postgraduate School of Occupational Medicine, Università Cattolica del Sacro Cuore, Rome, Italy
- 4Health Directorate, Bambino Gesù Children's Hospital IRCCS, Rome, Italy
- 5Occupational and Environmental Medicine, Epidemiology and Hygiene Department, Italian Workers’ Compensation Authority (INAIL), Rome, Italy
Introduction: Vaccination practice is a well-known individual protective measure for biological risk in healthcare. During the COVID-19 pandemic vaccine hesitancy has grown among healthcare workers (HCWs). The study aims to investigate how vaccine hesitancy influences the psychological burden experienced by healthcare workers.
Methods: This study aimed to explore attitudes of HCWs in acceptance or refusal of vaccinations related to the risk of psychological impairment (PI) and describe the associated occupational factors, during the seasonal flu/COVID-19 vaccination campaign of 2022–2023. 302 HCWs were enrolled in the study. A questionnaire was self-administered, including two scales on the risk of psychological impairment (Psychological Injury Risk Indicator, PIRI) and vaccine hesitancy (Adult Vaccine Hesitancy Scale, AVHS).
Results: PIRI scores revealed that 29.8% of participants were at risk of PI. Differences in sex, age, occupational seniority, professional category, and night shifts were found between HCWs at risk of PI and those not at risk. Females registered a four-fold higher risk than males (85.6% vs. 14.4%, χ2 = 4.450, p < 0.05). Nurses were the highest risk category, followed by physicians and technicians (54.4% vs. 30.0% vs. 12.2%, χ2 = 14.463, p < 0.001). 41.7% of participants received the flu vaccination, and 98.9% received the COVID-19 vaccine. HCWs were prone to being vaccinated to protect patients and family members. Conversely, vaccine refusal was attributed to the perception of flu vaccines as not beneficial and COVID-19 contagion at low risk. The latter was more frequently reported for HCWs at risk of PI (16.7% vs. 4.7%, χ2 = 11.882, p = 0.001). Finally, hesitant HCWs were at higher risk of psychological impairment than others.
Discussion: HCWs expressed vaccine acceptance considering their social role in the community as protectors. However, the underestimation of the risk of severity of COVID-19 was more relevant among HCWs at risk of PI than others. Psychological aspects need to be considered by healthcare providers when fighting vaccine hesitancy.
1 Introduction
Vaccination practice is a well-known individual protective measure for healthcare workers (HCWs), who are exposed to biological risk, to prevent nosocomial transmission of vaccine-preventable diseases (1–3). Since 2011 the NIOSH’s Total Worker Health® approach has aimed to integrate the occupational safety and health protection with health promotion and disease prevention activities in the workplace. In this perspective, the occupational physician takes care of the global health status of workers, helping them improve their overall well-being and thus perform better in both working and extra-work situations (4).
The term “Vaccine hesitancy,” labelled among the top 10 threats to global health by the World Health Organization (WHO) in 2019 (5), represents an emerging behavior during the process of vaccination decision-making before the vaccination uptake (6). According to Working Group on Vaccine Hesitancy, vaccine hesitancy refers to delay in acceptance or refusal of vaccination despite the availability of vaccination services (7). Moreover, from an occupational viewpoint, costs related to lack of flu vaccination are well-known to the top management, raising awareness of the economic burden of vaccine hesitancy too (8).
Since the COVID-19 outbreak, HCWs have been facing extra psychological burdens including workplace violence (9) which requires specific psychological support (10). Psychological distress has been frequently expressed by several clinical manifestations [e.g., burnout, anxiety, depression, fear of transmitting infection, feeling of incompatibility, increased substance dependence, and post-traumatic stress disorder (PTSD)], especially shown in frontline HCWs (11). The interplay between psychological stressors and biological hazards among HCWs has been reported (12). Psychological determinants of vaccine hesitancy have been investigated as one of the most significant barriers to vaccination acceptance and uptake (13). Interestingly, PTSD has been found to have a mediating role between societal adaptation and vaccine worries in HCWs (14).
In addition, the COVID-19 pandemic has left negative effects on key antecedents of general vaccination affecting people’s general attitudes towards vaccination with a general increase in vaccine hesitancy (15). Furthermore, a new level of volatility around vaccine hesitation also includes the powerful impact of digital media platforms (16). Although HCWs reported a generally high acceptance of COVID-19 vaccination, with spikes of 86.20% in China and 91.50% among nurses in Italy (17), healthcare professionals have been surprisingly touched by the vaccine hesitancy phenomenon, resulting in a global emerging behavior in this professional category (18). The perception of receiving flu vaccination due to the professional duty that HCWs have in society has exacerbated the psychological burden of this professional category (19).
The aim of the study is to explore different attitudes in acceptance/refusal of flu and COVID-19 vaccinations in HCWs at risk or not of psychological impairment (PI). Moreover, we investigated the impact of vaccine hesitancy on the risk of PI.
2 Materials and methods
2.1 Study design, setting, and eligibility
An observational cross-sectional case–control study was conducted in a pediatric hospital in Rome. The enrollment of the participants took place at the Occupational Medicine Unit between October 2022 and January 2023 during the seasonal flu/COVID-19 vaccination campaign of 2022–2023. HCWs who accepted to receive the COVID-19 and/or seasonal flu vaccines were eligible to participate to the study by completing a self-administered questionnaire.
2.2 The questionnaire
A questionnaire was administered on paper by dedicated personnel of the Unit during health surveillance visits and vaccination sessions addressed to the hospital employees. Questionnaires with missing data were excluded from the study.
Sex and age were included among demographic variables, whereas professional categories included doctors, nurses and other healthcare jobs (e.g., technicians, biologists, pharmacists, sociosanitary operators). Work seniority, night shifts and agile work were also considered among occupational variables.
Psychological factors and vaccine hesitancy were explored too.
2.2.1 Scale investigating the risk of psychological impairment
The Psychological Injury Risk Indicator (PIRI) is a standardized and validated questionnaire able to identify the tendency of psychological impairment (20). The Italian version was used (21). Given that Italian law requires HCWs to abstain from alcohol while at work, four of the five original subscales were considered, including sleep disorders (6 items), energy recovery (5 items), symptoms of post-traumatic stress syndrome (PTSD) (10 items), and chronic fatigue (5 items). Each item is scored on a seven-point Likert scale (0–6). The total score is calculated as the sum of the scores derived from each subscale; both the total and the subscale’s scores are standardized on a scale from 0 to 100. According to the original guidelines, overall scores higher than 25 indicate a potential risk of psychological injury (21). Based on the PIRI score, the population was divided into two groups, regarding HCWs at risk of psychological impairment (PI) and not at risk.
2.2.2 Questionnaire on vaccine hesitancy
A 12-item questionnaire adapted from the Adult Vaccine Hesitancy Scale (AVHS) (22) was used to assess the attitude of HCWs towards COVID-19 and seasonal flu diseases and vaccine uptake. Four areas were explored, considering vaccine administration (4 items), reasons for vaccine acceptance (3 items), reasons for vaccine refusal (3 items) and knowledge (2 items). All areas explored seasonal flu, COVID-19 and flu/COVID-19 co-administration. Questions are reported in Supplementary Table S1.
2.3 Statistical analyses
Descriptive statistical analysis was conducted on demographics and occupational variables using mean and standard deviation for continuous variables and absolute and relative frequency for categorical variables. Since the normality test was not satisfied, the comparison between the two groups was performed using non-parametric tests (Mann–Whitney for continuous variables and χ2 test and Kruskal-Wallis test for categorical variables). Moreover, acceptance and refusal factors associated with the two vaccinations were compared in the two groups using χ2 test. p values <0.05 were considered statistically significant. Effect size was reported as r based on the Z statistic from the Mann–Whitney test for continuous variables, whereas Cramer’s V was used for dichotomous categorical variables. While we have included effect sizes and confidence intervals to enhance the interpretation of our findings, the study’s findings are subject to the limitations associated with multiple testing. Considering the overall population, a logistic regression model was then set up having the risk of PI as dependent variable and the significant resulted variables by univariate analyses as independent ones. In the logistic regression model development, variables statistically significant in the univariate analyses were selected for inclusion. This approach was employed to identify the factors most strongly associated with psychological impairment. Data were analyzed using IBM Statistics Package for Social Sciences (SPSS) (version 26.0).
3 Results
Out of 400 subjects examined during the sanitary surveillance, 302 HCWs were enrolled in the study (75.5%). They were mostly females (n = 235, 77.8%). The mean age was 39.8 ± 11.1.
3.1 Risk of psychological impairment
PIRI questionnaire total score showed an overall mean value below the cut-off (19.3 ± 16.0), indicating general good psychological health. On the contrary, the subscales related to energy recovery and sleep disturbance registered higher mean values than the considered cut-offs (33.5 ± 28.9 and 27.4 ± 22.4, respectively). Overall, 29.8% of the participants (n = 90) can be considered at risk of PI. This percentage increased to 45.7% for the sleep disturbance subscale and 51.3% for the energy recovery subscale. Moreover, over 30% of participants reported problems related to chronic fatigue and PTSD (Table 1).
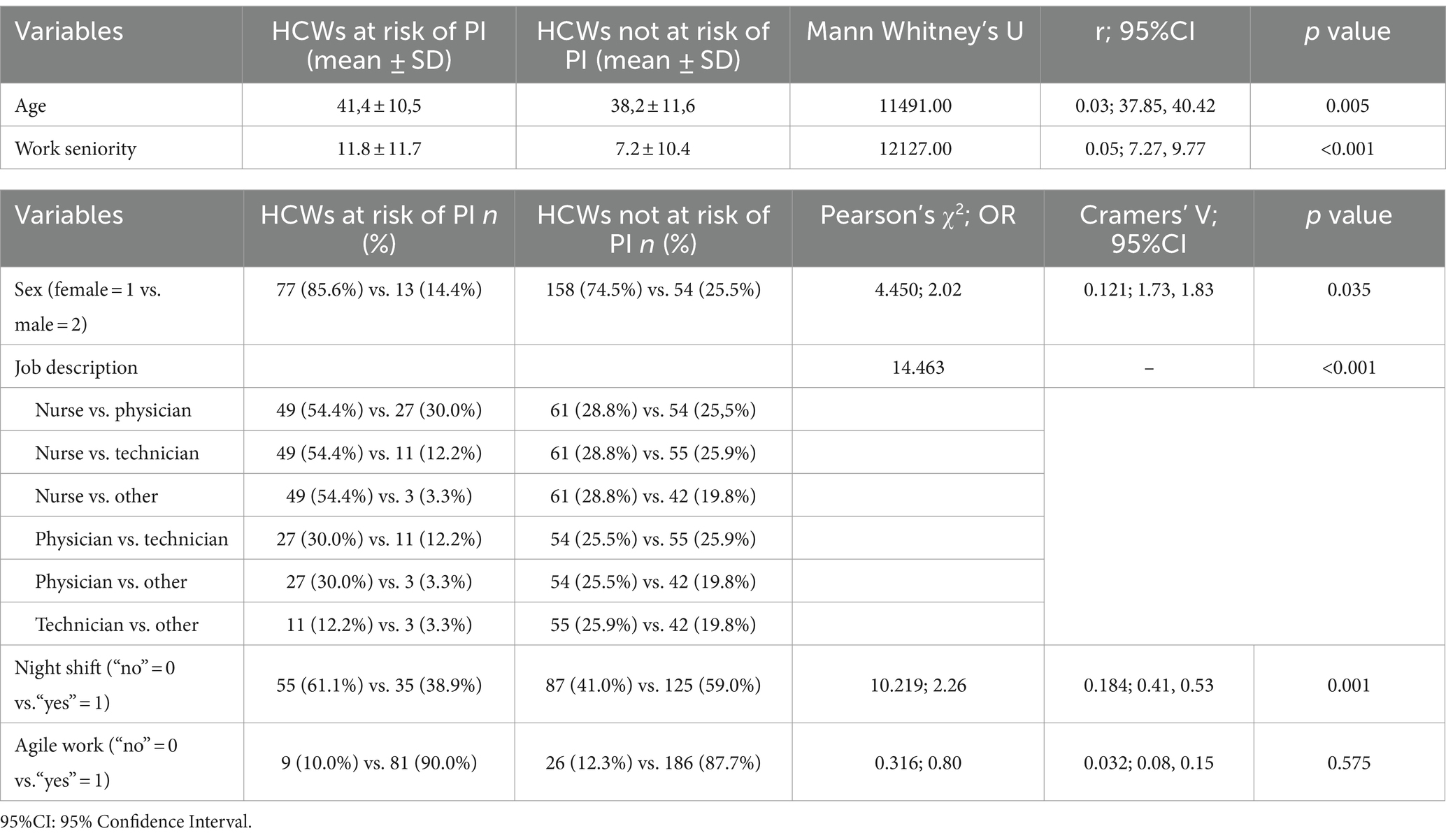
By comparing workers at risk of PI to those not at risk, differences in sex, age, occupational seniority, professional category, and night shifts were highlighted. In detail, females registered a two-fold higher risk than males (85.6% vs. 14.4%, χ2(1, 302) = 4.450, p < 0.05). In addition, workers at risk of PI had higher age and seniority than workers not at risk (41.4 ± 10.5 vs. 38.2 ± 11.6, p < 0.01; 11.8 ± 11.7 vs. 7.2 ± 10.4, Mann Whitney’s U = 11491.00 and 12127.00 respectively, p < 0.001). Nurses were the professional category at higher risk, followed by physicians and technicians (54.4% vs. 30.0% vs. 12.2%, χ2(3, 302) = 14.463, p < 0.001). Night shifts represented a significant risk factor too (61.1% vs. 41.0%, χ2(1, 302)10.219, p = 0.001). On the contrary, agile work was not significantly different between the two groups. Given the small effect size statistics, significant variables should be considered with caution (Table 2).
3.2 Vaccine administration
41.7% of participants got the flu vaccination and 31.5% had planned to get it. Most of the participants had been getting vaccinated for several years (66.8%), and 20.9% started after the COVID-19 outbreak; 12.3% had the first seasonal flu vaccination. The second COVID-19 booster dose was administered in 73.8% of subjects, followed by 16.2 and 8.9% of third and first booster doses, respectively. Co-administration was performed by half of the population, of which 20.9% had planned to get it, and 28.7% refused to get it.
Although not statistically significant, there is a trend of refusal of the flu vaccination and co-administration of flu/COVID-19 vaccines by HCWs at risk of PI. They also started to get flu vaccines since the pandemic outbreak (Table 3).
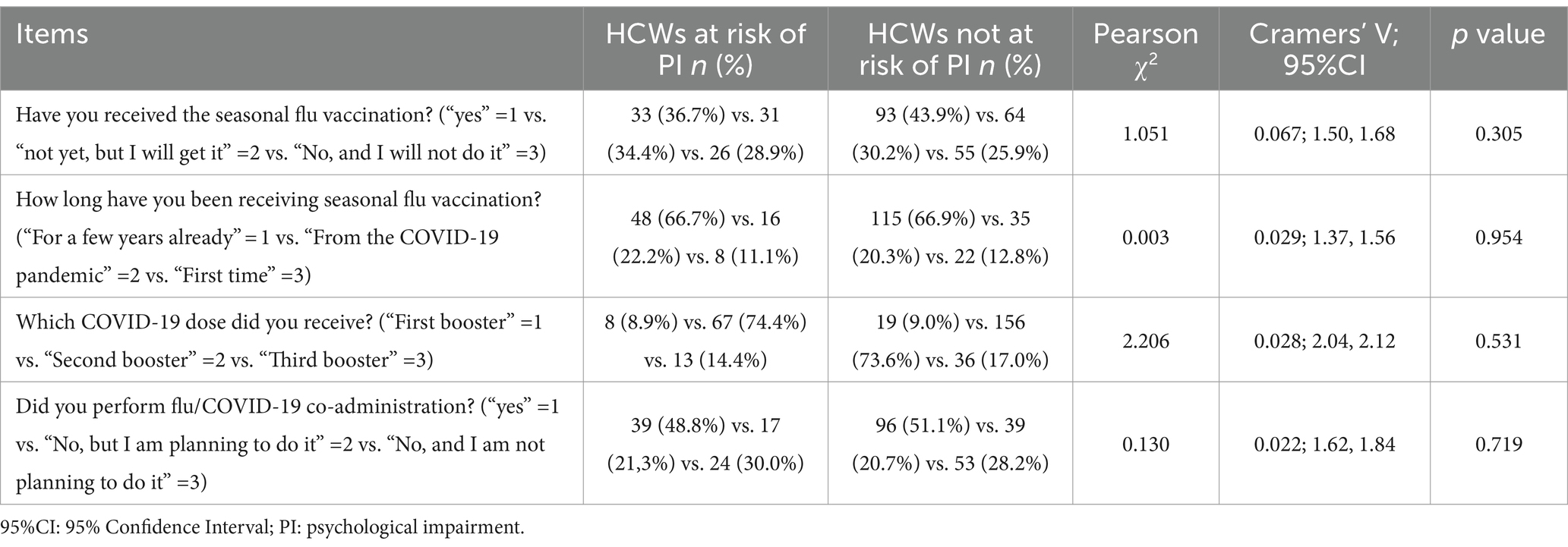
Table 3. Comparison of flu and COVID-19 vaccine administration prevalence between HCWs at risk of PI and not.
3.3 Vaccine acceptance, vaccine refusal, and knowledge
Overall, subjects referred to accept the vaccinations mostly to protect their patients and family members, and secondly to protect themselves; in addition, HCWs at risk of PI perceived a social meaning of COVID vaccination in the workplace context. Co-administration was accepted to address the severity of the diseases, according to official recommendations (Table 4A).
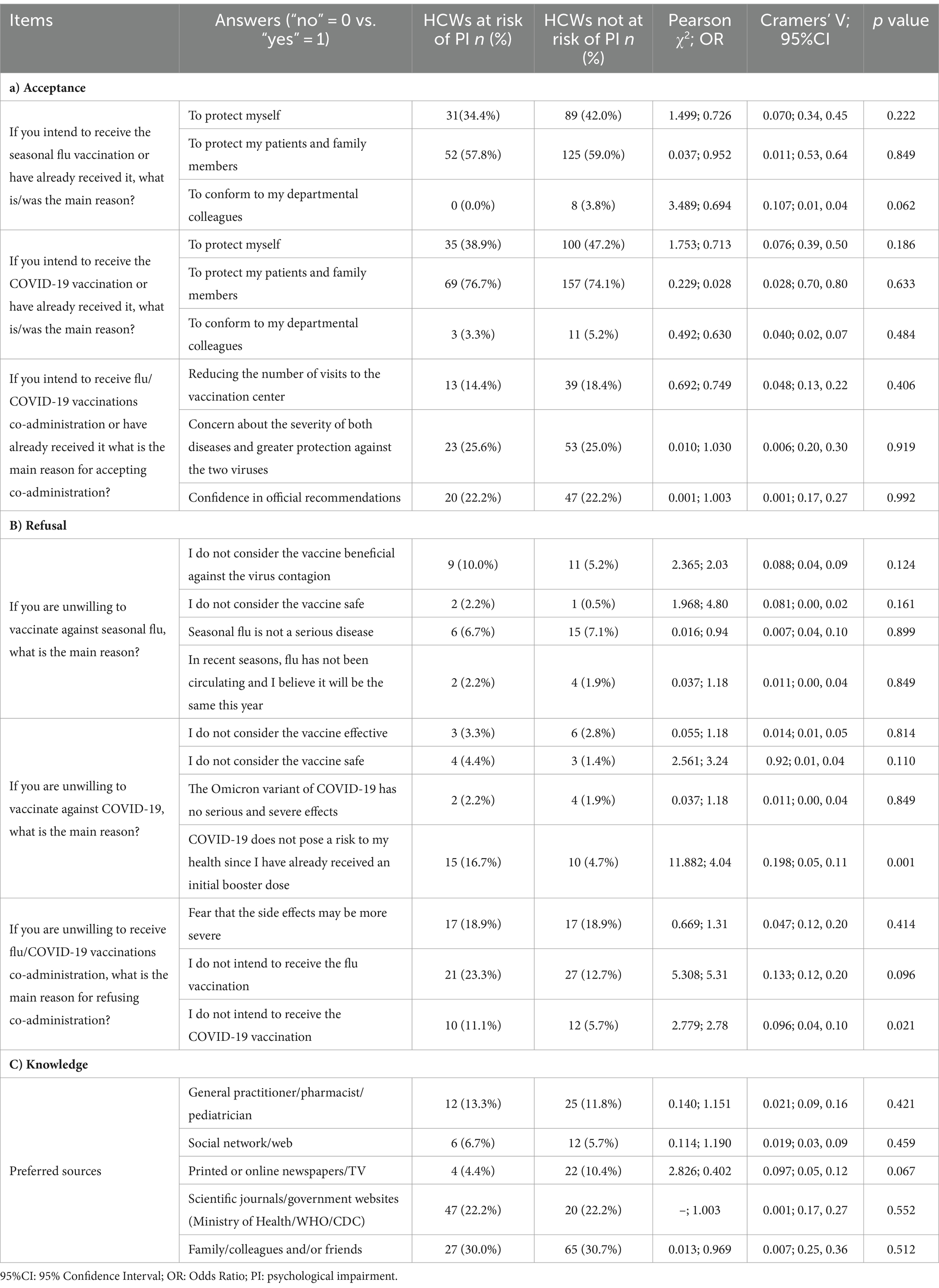
Table 4. Comparison of reasons for acceptance or refusal of vaccinations between HCWs at risk of PI and not.
The refusal of flu vaccination was attributed to the perception that it was not beneficial by HCWs at risk of PI, and because the seasonal flu was not considered a serious disease by HCWs not at risk of PI. The refusal of COVID-19 vaccination was mainly due to the perception of low risk of COVID-19 infection after having already received the full primary course plus a first booster dose; this idea was significantly more common among HCWs at risk of PI than others (Table 4B). In general, co-administration was refused because of the refusal of flu vaccination.
A range of 71.5–73.9% of participants in both groups reported that they knew about the possibility of receiving flu and COVID-19 vaccinations in the same session. The preferred sources were family/colleagues and/or friends followed by scientific journals/government websites (Ministry of Health/WHO/CDC) and General practitioner/pharmacist/pediatrician (Table 4C).
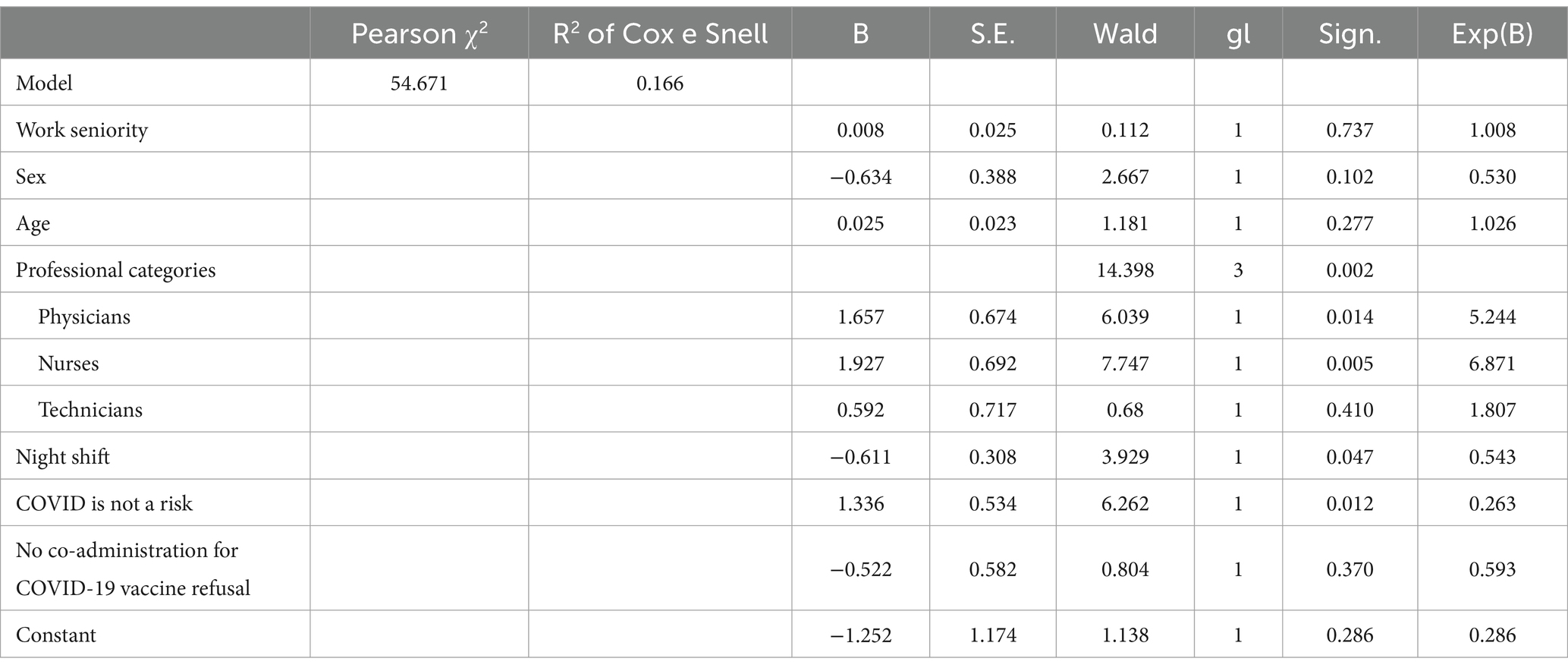
The multiple logistic regression showed that professional category, night shifts, and the underestimated risk of the severity of COVID-19 disease were determining factors of PI. Professional category, night shifts, and the belief that COVID-19 is not a severe risk were significant predictors of PI among HCWs. Specifically, being a physician or nurse increased the odds of PI, while working night shifts and underestimating the severity of COVID-19 decreased the odds of PI (Table 5).
4 Discussion
In literature, several factors influence vaccine administration, including personal factors and environmental factors. Regulations, professional duty, knowledge, individual perceptions of vulnerability, trust in the healthcare system, attitudes and past experiences are some of the identified determinants of vaccination (19, 22). Our findings showed that acceptance of flu and COVID-19 vaccinations reflected the social role of HCWs in protecting patients and family members before themselves. On the contrary, the refusal was mainly attributed to the perception of the flu vaccine as not beneficial and for COVID-19 the perceived low risk of contagion. The latter was more frequently reported for healthcare professionals at risk of psychological impairment, because the primary course plus a first booster dose should have been completed with full protection against the virus. Beyond occupational characteristics (e.g., professional category and night shift schedule), COVID-19 vaccine hesitancy impacted on the risk of PI among HCWs. According to the Total Worker Health® approach (4), exploring the HCWs’ attitudes and perceptions of the biological risk in terms of vaccine hesitancy toward two of the most relevant vaccinations in recent decades is essential to raise individual and collective awareness of the updated evidence in the field.
Firstly, regarding the social role of HCWs, the desire to protect family and patients has been already documented in literature (23). In fact, HCWs performed a key role during the COVID-19 pandemic. Beyond their critical part in the frontline battle against the virus, HCWs bridged the gap between patients and healthcare institutions in a climate of social distancing and spread essential information about virus contamination management in the general population (24). HCWs’ social role is also identified in spreading good behaviors in the community, such as building confidence in vaccination decisions, as suggested by healthcare providers (25, 26). Attitudes and perceptions of HCWs toward vaccination practices are known to influence patient vaccine acceptance (25). The COVID-19 pandemic has raised the emphasis on trust or on the more sentimental aspects of decision-making surrounding health-protective behaviors like vaccination uptake (19). Perceived susceptibility, severity, and benefit of acting have been associated with COVID-19 vaccine acceptance among HCWs (25), with the highest rate for old male physicians (27, 28). Proper communication on these themes represents a strategic role in setting up successful immunological responses (29).
Secondly, in those who refused, a general perception of the seasonal flu vaccines as non-beneficial and the COVID-19 vaccine as not safe emerged. In the literature, a renewed ethical challenge has been outlined to solve the question of flu vaccine refusal among HCWs, which includes professional duty and ethics (deontology), self-determination and conscientious objection (30). The main reasons for refusing flu vaccination were lack of time, a feeling of invulnerability, conviction of not being at risk, of being too young or in good health, and misconceptions about vaccine efficacy (31). Previous evidence showed that suboptimal vaccination toward COVID-19 among HCWs was mainly due to concerns about vaccine safety, efficacy and potential side effects, because of the absence of educational campaigns, inaccurate risk perception, unknown or uncertain vaccination status, difficulties in accessing vaccination in the workplace, and equity-rooted challenges (26, 32). Low levels of education and awareness were described for those who used mass media, social media or Internet as the main source of information (17, 18, 33, 34). Beyond renewed cross-cultural differences related to age, gender, socioeconomic status, race, and social capital (35–38), occupational factors have been associated to vaccine hesitancy (39). In this respect, COVID-19 exposure, perceived risk, mandatory vaccination, and social pressure, altruism and collective responsibility were highlighted (39). A general nurses’ attitude of wait-and-see was reported (40), especially for females (17).
Thirdly, our findings showed a general underestimation of risk. Evidence from literature indicated that the low likelihood of contracting vaccine-preventable diseases and the perceived low severity of these diseases are the foremost reasons not to take the vaccines (41). Personal beliefs and misperceptions about the risk of contracting seasonal flu are known factors influencing the flu vaccine uptake (42). A pattern of underestimating the risk associated with flu and overestimating the risk of minor adverse reactions has been highlighted too (43). A review showed that although the cumulative increase in COVID-19 caseloads of countries over time, vaccination intention did not increase (44).
Finally, we found that COVID-19 hesitant HCWs were at higher risk of psychological impairment than others. In fact, emotional, cognitive, political, religious, moral, and cultural aspects may influence vaccination uptake (5). In literature, the role of psychological aspects on vaccine hesitancy has been widely reported. Low psychological well-being (e.g., anxiety, low confidence, low collective responsibility, low reward dependence, PTSD and trait reactance) influences the perception of COVID-19 vaccination acceptance and side effects (45–47). People suffering from pre-pandemic mental conditions were not prone to take up the vaccination (48). In addition, HCWs with PTSD symptoms and anxiety symptoms were more likely to be hesitant. Psychological barriers to vaccination have been summarized in the “5Cs model” comprising five relevant psychological antecedents of vaccination: confidence, complacency (risk perceptions), constraints (barriers), calculation (extent of information search), and collective responsibility (willingness to protect the community) (49). According to this model, HCWs’ vaccine decision-making process was mainly mined by the lack of trust in the COVID-19 vaccine, anti-science sentiment, adverse side effects, and situational risk assessment (13). Conspiracy theories have been reported too (18, 25, 50).
While counterintuitive, the effect of nightshift as a protective element could be linked to the fact that healthier HCWs do nightshift. In contrast, other HCWs with other comorbidities, including mental issues, are usually exempted. Besides, not considering COVID-19 as a risk could be linked to character traits that could be protective for PI.
In conclusion, our study strengthens the role of the psychological aspect of vaccine hesitant HCWs, which surely needs to be examined during the planning of future actions. However, some limitations may be outlined, including the cross-sectional design which does not allow to identify the causality between psychological impairment and vaccine hesitancy. Future longitudinal development in the upcoming vaccination campaigns could overcome this limitation. Moreover, considering the small effect size of the statistically significant evidence, practical implications should be taken with caution. Finally, the moderate fit of the logistic regression model (as indicated by the Cox and Snell R2 value of 0.166) suggests that while the model explains a portion of the variance, a significant amount remains unexplained.
5 Conclusion
Acceptance and refusal of flu and COVID-19 vaccinations are clearly modulated by several factors. Although persistent immunological memory after vaccination has been described as functional during breakthrough COVID-19 infections, vaccine hesitancy needs to be widely faced, especially when addressing HCWs (51). Enhancing the professional and social role of HCWs may be the keystone to address vaccine hesitancy for them and in the general population as well. In this regard, multicomponent interactive and context-specific interventions are fundamental in the tailored and clear communication approach to reach all people (13, 25, 52). HCWs’ psychological aspect needs to be considered in the process of strengthening the action of Public Health. From an occupational medicine perspective, systemic approaches may play an essential role in helping raise professional responsibilities among HCWs towards the general population (53).
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The study was approved for publication by the Scientific Directorate of the IRCCS Bambino Gesù Children’s Hospital (protocol n. RAP-2024-0002, approved on 18 March 2024). All participants fulfilled a written informed consent. The survey was anonymous, and data was processed anonymously and aggregated.
Author contributions
RRDP: Conceptualization, Methodology, Writing – original draft. BC: Data curation, Investigation, Writing – original draft. GA: Writing – original draft. AD: Writing – original draft. MM: Writing – original draft. MEV: Writing – original draft. MRV: Conceptualization, Writing – review & editing. VC: Writing – review & editing. AS: Writing – review & editing. MR: Writing – review & editing. PT: Writing – review & editing. NV: Writing – review & editing. UM: Writing – review & editing. SZ: Conceptualization, Methodology, Writing – review & editing. GD: Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. Project carried out in collaboration with INAIL (CUP: E83C22006610001). This work was supported by the Italian Ministry of Health with Current Research funds.
Acknowledgments
Special thanks to Victoria d’Inzeo for the language revision.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1447334/full#supplementary-material
References
1. Fan, J, Xu, S, Liu, Y, Ma, X, Cao, J, Fan, C, et al. Influenza vaccination rates among healthcare workers: a systematic review and meta-analysis investigating influencing factors. Front Public Heal. (2023) 11:1295464. doi: 10.3389/fpubh.2023.1295464
2. Pilishvili, T, Gierke, R, Fleming-Dutra, KE, Farrar, JL, Mohr, NM, Talan, DA, et al. Effectiveness of mRNA Covid-19 vaccine among U.S. health care personnel. N Engl J Med. (2021) 385:e90. doi: 10.1056/NEJMoa2106599
3. Tavoschi, L, Quattrone, F, Agodi, A, and Lopalco, PL. Risk of transmission of vaccine-preventable diseases in healthcare settings. Future Microbiol. (2019) 14:9–14. doi: 10.2217/fmb-2018-0236
4. Schill, AL, and Chosewood, LC. The NIOSH total worker health™ program: an overview. J Occup Environ Med. (2013) 55:S8–S11. doi: 10.1097/JOM.0000000000000037
5. Dubé, È, Ward, JK, Verger, P, and Macdonald, NE. Vaccine hesitancy, acceptance, and anti-vaccination: trends and future prospects for public health. Annu Rev Public Health. (2021) 42:175–91. doi: 10.1146/annurev-publhealth-090419-102240
6. Larson, HJ, Jarrett, C, Eckersberger, E, Smith, DMD, and Paterson, P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007-2012. Vaccine. (2014) 32:2150–9. doi: 10.1016/j.vaccine.2014.01.081
7. MacDonald, NE, Eskola, J, Liang, X, Chaudhuri, M, Dube, E, Gellin, B, et al. Vaccine hesitancy: definition, scope and determinants. Vaccine. (2015) 33:4161–4. doi: 10.1016/j.vaccine.2015.04.036
8. Zaffina, S, Gilardi, F, Rizzo, C, Sannino, S, Brugaletta, R, Santoro, A, et al. Seasonal influenza vaccination and absenteeism in health-care workers in two subsequent influenza seasons (2016/17 and 2017/18) in an Italian pediatric hospital. Expert Rev Vaccines. (2019) 18:411–8. doi: 10.1080/14760584.2019.1586541
9. Di Prinzio, RR, Bondanini, G, De Falco, F, Vinci, MR, Camisa, V, Santoro, A, et al. The Management of Workplace Violence against healthcare workers: a multidisciplinary team for Total worker health® approach in a hospital. Int J Environ Res Public Health. (2022) 20:96. doi: 10.3390/ijerph20010196
10. Di Prinzio, RR, Bondanini, G, De Falco, F, Vinci, MR, Camisa, V, Santoro, A, et al. Need for psychological support and disability management programs during and after the COVID-19 pandemic in Italy: Preliminary findings from an hospital-based occupational health surveillance program. J Health Soc Sci. (2021). doi: 10.19204/2021/ndfr7
11. Dubey, S, Biswas, P, Ghosh, R, Chatterjee, S, Dubey, MJ, Chatterjee, S, et al. Psychosocial impact of COVID-19. Diabetes Metab Syndr. (2020) 14:779–88. doi: 10.1016/j.dsx.2020.05.035
12. Tomao, P, Zaffina, S, Di, PRR, Vonesch, N, Chirico, F, and Magnavita, N. The interplay between psychological stressors and biological hazards among healthcare workers during the COVID-19 pandemic. J Heal Soc Sci. (2022) 7:368–80. doi: 10.19204/2022/THNT3
13. Bendetson, J, Swann, MC, Lozano, A, West, J, Hanlon, AL, Crandell, I, et al. Deepening our understanding of COVID-19 vaccine decision-making amongst healthcare Workers in Southwest Virginia, USA using exploratory and confirmatory factor analysis. Vaccine. (2023) 11:556. doi: 10.3390/vaccines11030556
14. Hsieh, KY, Li, DJ, Chou, FHC, Hsu, ST, Wu, HC, Chou, LS, et al. Relationship of societal adaptation with vaccine worries among healthcare workers during the COVID-19 pandemic: the mediating effects of posttraumatic stress disorder. Int J Environ Res Public Health. (2022) 19:498. doi: 10.3390/ijerph19159498
15. McRee, AL, Gower, AL, Kiss, DE, and Reiter, PL. Has the COVID-19 pandemic affected general vaccination hesitancy? Findings from a national study. J Behav Med. (2023) 46:9–14. doi: 10.1007/s10865-022-00298-2
16. Larson, HJ, Gakidou, E, and Murray, CJL. The vaccine-hesitant moment. N Engl J Med. (2022) 387:58–65. doi: 10.1056/NEJMra2106441
17. Shakeel, CS, Mujeeb, AA, Mirza, MS, Chaudhry, B, and Khan, SJ. Global COVID-19 vaccine acceptance: a systematic review of associated social and behavioral factors. Vaccines. (2022) 10:110. doi: 10.3390/vaccines10010110
18. Peterson, CJ, Lee, B, and Nugent, K. COVID-19 vaccination hesitancy among healthcare workers-a review. Vaccine. (2022) 10:948. doi: 10.3390/vaccines10060948
19. Hall, CM, Northam, H, Webster, A, and Strickland, K. Determinants of seasonal influenza vaccination hesitancy among healthcare personnel: an integrative review. J Clin Nurs. (2022) 31:2112–24. doi: 10.1111/jocn.16103
20. Winwood, PC, Tuckey, MR, Peters, R, and Dollard, MF. Identification and measurement of work-related psychological injury: piloting the psychological injury risk indicator among frontline police. J Occup Environ Med. (2009) 51:1057–65. doi: 10.1097/JOM.0b013e3181b2f3d8
21. Magnavita, N, Garbarino, S, and Winwood, PC. Measuring psychological trauma in the workplace: psychometric properties of the Italian version of the psychological injury risk indicator-a cross-sectional study. ScientificWorldJournal. (2015): 720193. doi: 10.1155/2015/720193
22. Ledda, C, Costantino, C, Liberti, G, and Rapisarda, V. The Italian version of the adult vaccine hesitancy scale (aVHS) for the working-age population: cross-cultural adaptation, reliability, and validity. Vaccine. (2022) 10:224. doi: 10.3390/vaccines10020224
23. Dini, G, Toletone, A, Sticchi, L, Orsi, A, Bragazzi, NL, and Durando, P. Influenza vaccination in healthcare workers: a comprehensive critical appraisal of the literature. Hum Vaccin Immunother. (2018) 14:772–89. doi: 10.1080/21645515.2017.1348442
24. Kigongo, E, Kabunga, A, Tumwesigye, R, Musinguzi, M, Izaruku, R, and Acup, W. Prevalence and predictors of COVID-19 vaccination hesitancy among healthcare workers in sub-Saharan Africa: a systematic review and meta-analysis. PLoS One. (2023) 18:e0289295. doi: 10.1371/journal.pone.0289295
25. Desye, B . Prevalence and determinants of COVID-19 vaccine acceptance among healthcare workers: a systematic review. Front public Heal. (2022):10:941206. doi: 10.3389/fpubh.2022.941206
26. Biswas, N, Mustapha, T, Khubchandani, J, and Price, JH. The nature and extent of COVID-19 vaccination hesitancy in healthcare workers. J Community Health. (2021) 46:1244–51. doi: 10.1007/s10900-021-00984-3
27. Li, M, Luo, Y, Watson, R, Zheng, Y, Ren, J, Tang, J, et al. Healthcare workers’ (HCWs) attitudes and related factors towards COVID-19 vaccination: a rapid systematic review. Postgrad Med J. (2023) 99:520–8. doi: 10.1136/postgradmedj-2021-140195
28. Ciocca, M, Zaffina, S, Fernandez Salinas, A, Bocci, C, Palomba, P, Conti, MG, et al. Evolution of human memory B cells from childhood to old age. Front Immunol. (2021) 12:690534. doi: 10.3389/fimmu.2021.690534
29. Zaffina, S, Piano Mortari, E, Di Prinzio, RR, Cappa, M, Novelli, A, Agolini, E, et al. Case report: precision COVID-19 immunization strategy to overcome individual fragility: a case of generalized lipodystrophy type 4. Front Immunol. (2022) 13:869042. doi: 10.3389/fimmu.2022.869042
30. Van Hooste, WLC, and Bekaert, M. To be or not to be vaccinated? The ethical aspects of influenza vaccination among healthcare workers. Int J Environ Res Public Health. (2019) 16:3981. doi: 10.3390/ijerph16203981
31. Nitsch-Osuch, A, and Brydak, LB. Influenza vaccinations of health care personnel. Med Pr. (2013) 64:119–29.
32. Januszek, SM, Faryniak-Zuzak, A, Barnaś, E, Łoziński, T, Góra, T, Siwiec, N, et al. The approach of pregnant women to vaccination based on a COVID-19 systematic review. Medicina. (2021) 57:977. doi: 10.3390/medicina57090977
33. Tunç, AM, and Çevirme, A. Attitudes of healthcare workers toward the COVID-19 vaccine and related factors: a systematic review. Public Health Nurs. (2024) 41:10–21. doi: 10.1111/phn.13250
34. Bianchi, FP, Stefanizzi, P, Brescia, N, Lattanzio, S, Martinelli, A, and Tafuri, S. COVID-19 vaccination hesitancy in Italian healthcare workers: a systematic review and meta-analysis. Expert Rev Vaccines. (2022) 21:1289–300. doi: 10.1080/14760584.2022.2093723
35. Anticoli, S, Dorrucci, M, Iessi, E, Chiarotti, F, Di Prinzio, RR, Vinci, MR, et al. Association between sex hormones and anti-S/RBD antibody responses to COVID-19 vaccines in healthcare workers. Hum Vaccin Immunother. (2023) 19:697. doi: 10.1080/21645515.2023.2273697
36. Zaffina, S, Marcellini, V, Santoro, AP, Scarsella, M, Camisa, V, Vinci, MR, et al. Repeated vaccinations do not improve specific immune defenses against hepatitis B in non-responder health care workers. Vaccine. (2014) 32:6902–10. doi: 10.1016/j.vaccine.2014.10.066
37. Machida, M, Inoue, S, and Tabuchi, T. General vaccination readiness in Japan: results from the JASTIS 2023 study. Jpn J Infect Dis. (2024) 77:10.7883/yoken.JJID.2023.261:34–9. doi: 10.7883/yoken.JJID.2023.261
38. Hateftabar, F, Larson, HJ, and Hateftabar, V. Examining the effects of psychological reactance on COVID-19 vaccine acceptance: comparison of two countries. J Glob Health. (2022) 12:05057. doi: 10.7189/jogh.12-05057
39. McCready, JL, Nichol, B, Steen, M, Unsworth, J, Comparcini, D, and Tomietto, M. Understanding the barriers and facilitators of vaccine hesitancy towards the COVID-19 vaccine in healthcare workers and healthcare students worldwide: an umbrella review. PLoS One. (2023) 18:280439. doi: 10.1371/journal.pone.0280439
40. Chrdle, A, Bártlová, S, and Chloubová, I. Postoje sester a studentů ošetřovatelství k očkování proti covid-19 - přehled. Epidemiol Mikrobiol Imunol. (2023) 72:25–39.
41. Karafillakis, E, and Larson, HJ. The benefit of the doubt or doubts over benefits? A systematic literature review of perceived risks of vaccines in European populations. Vaccine. (2017) 35:4840–50. doi: 10.1016/j.vaccine.2017.07.061
42. Truong, J, Bakshi, S, Wasim, A, Ahmad, M, and Majid, U. What factors promote vaccine hesitancy or acceptance during pandemics? A systematic review and thematic analysis. Health Promot Int. (2022) 37:daab105. doi: 10.1093/heapro/daab105
43. Challenger, A, Sumner, P, Powell, E, and Bott, L. Identifying reasons for non-acceptance of influenza vaccine in healthcare workers: an observational study using declination form data. BMC Health Serv Res. (2023) 23:1167. doi: 10.1186/s12913-023-10141-2
44. Al-Amer, R, Maneze, D, Everett, B, Montayre, J, Villarosa, AR, Dwekat, E, et al. COVID-19 vaccination intention in the first year of the pandemic: a systematic review. J Clin Nurs. (2022) 31:62–86. doi: 10.1111/jocn.15951
45. Kim, E, Kim, HJ, and Han, DH. The effect of psychological factors on COVID-19 vaccination side effects: a cross-sectional survey in South Korea. Psychiatry Investig. (2023) 20:808–17. doi: 10.30773/pi.2023.0116
46. Kim, HJ, Kim, E, and Han, DH. Effect of psychological factors on COVID-19 vaccine hesitancy. J Public Health. (2023) 45:E522–31. doi: 10.1093/pubmed/fdad050
47. Soveri, A, Karlsson, LC, Mäki, KO, Holford, D, Fasce, A, Schmid, P, et al. Trait reactance as psychological motivation to reject vaccination: two longitudinal studies and one experimental study. Appl Psychol Health Well Being. (2023) 16:597–614. doi: 10.1111/aphw.12506
48. Batty, GD, Deary, IJ, and Altschul, D. Pre-pandemic mental and physical health as predictors of COVID-19 vaccine hesitancy: evidence from a UK-wide cohort study. Ann Med. (2022) 54:274–82. doi: 10.1080/07853890.2022.2027007
49. Betsch, C, Schmid, P, Korn, L, Steinmeyer, L, Heinemeier, D, Eitze, S, et al. Psychological antecedents of vaccination: definitions, measurement, and interventions. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. (2019) 62:400–9. doi: 10.1007/s00103-019-02900-6
50. Jerković, H, and Šitum, M. Vaccine hesitancy - from parental distrust to COVID-19 conspiracies. Psychiatr Danub. (2023) 35:226–31. doi: 10.24869/psyd.2023.226
51. Terreri, S, Piano Mortari, E, Vinci, MR, Russo, C, Alteri, C, Albano, C, et al. Persistent B cell memory after SARS-CoV-2 vaccination is functional during breakthrough infections. Cell Host Microbe. (2022) 30:400–408.e4. doi: 10.1016/j.chom.2022.01.003
52. Reñosa, MDC, Landicho, J, Wachinger, J, Dalglish, SL, Bärnighausen, K, Bärnighausen, T, et al. Nudging toward vaccination: a systematic review. BMJ Glob Heal. (2021) 6:237. doi: 10.1136/bmjgh-2021-006237
Keywords: COVID-19, vaccine acceptance, mental health, flu, nurse, vaccine refusal
Citation: Di Prinzio RR, Ceresi B, Arnesano G, Dosi A, Maimone M, Vacca ME, Vinci MR, Camisa V, Santoro A, Raponi M, Tomao P, Vonesch N, Moscato U, Zaffina S and Dalmasso G (2024) The impact of vaccine hesitancy on psychological impairment among healthcare workers in a Total Worker Health© approach. Front. Public Health. 12:1447334. doi: 10.3389/fpubh.2024.1447334
Edited by:
Andrea Trevisan, University of Padua, ItalyReviewed by:
Agnieszka Paulina Kijewska, Gdański Uniwersytet Medyczny, PolandFilippo Quattrone, Sant’Anna School of Advanced Studies, Italy
Copyright © 2024 Di Prinzio, Ceresi, Arnesano, Dosi, Maimone, Vacca, Vinci, Camisa, Santoro, Raponi, Tomao, Vonesch, Moscato, Zaffina and Dalmasso. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gabriele Arnesano, Z2FicmllbGVhcm5lc2FubzkzQGdtYWlsLmNvbQ==
†These authors share first authorship
‡These authors share last authorship
 Reparata Rosa Di Prinzio
Reparata Rosa Di Prinzio Bianca Ceresi1†
Bianca Ceresi1† Gabriele Arnesano
Gabriele Arnesano Vincenzo Camisa
Vincenzo Camisa Annapaola Santoro
Annapaola Santoro Paola Tomao
Paola Tomao Umberto Moscato
Umberto Moscato Salvatore Zaffina
Salvatore Zaffina Guendalina Dalmasso
Guendalina Dalmasso