- 1School of Public Administration, Hohai University, Nanjing, China
- 2School of Humanities, Southeast University, Nanjing, China
Objective: The role of informal social support in fostering active aging within the context of the “silver wave” is significant. This study investigated how such support influenced the mental health of older adults, with the goal of affirming its indispensable contribution to enhancing their psychological well-being.
Methods: Employing Principal Component Analysis (PCA) to construct the informal social support variable, this study rigorously analyzed the effects and underlying mechanisms of informal social support on mental health in older adults, utilizing data from the 2018 China Longitudinal Aging Social Survey (CLASS).
Results: Informal social support exerted a substantial positive influence on the mental health of older adults, particularly among younger, non-agricultural older adult populations who preferred cohabitation with their children. This form of support significantly enhanced mental well-being by elevating life satisfaction, improving access to medical services, and fostering active social engagement.
Conclusion: This study elucidates the role of informal social support in bolstering the mental health of older adults. Future efforts should focus on fostering a supportive environment that enhances older adult care experiences, reforming the healthcare system to better meet the needs of the aging population, and promoting avenues for social engagement, thereby achieving a balanced integration of their emotional and physical care.
1 Introduction
The 2023 United Nations “World Social Report” identified a significant demographic shift, noting that the global population aged 65 and over reached 761 million in 2021, with projections indicating a rise to 1.6 billion by 2050. This demographic transformation will have far-reaching implications for various facets of human activity and societal structure. Consequently, enhancing older adult health and well-being has emerged as a strategic priority for global policymakers. The rapid acceleration of population aging is also associated with increased mental health challenges among older adults (1). The abrupt transition in social roles post-retirement often leaves individuals struggling to adapt, potentially leading to diminished self-worth and psychological issues like loneliness. A World Health Organization report has highlighted that addressing mental health in older adults is integral to fostering active aging. Thus, examining this issue is both a practical response to these mental health challenges in society and an essential component of the broader agenda on active aging.
The mental well-being of older adults has increasingly attracted scholarly attention, emerging as a key aspect in the progression of aging-related initiatives (2). The various determinants influencing older adults’ mental health have stimulated significant public discourse. Current studies indicate a substantial positive correlation between social support and the mental health of older adults, highlighting its substantial impact (3). Social support, a concept rooted in the 1970s, encapsulates the perceived care and assistance received from others. This concept has gained significant traction across disciplines such as Sociology, Psychology, and Medicine. In the context of older adult mental health, researchers have categorized social support into formal and informal types (4). Formal support, typically provided by governmental bodies, institutions, enterprises, and communities, includes mechanisms such as social security systems, medical security frameworks, and policies that prioritize the welfare and dignity of older adults. Conversely, informal support stems primarily from familial connections, neighbors, friends, and peer groups, offering emotional, behavioral, and informational assistance (5). One report has highlighted that the demand for informal older adults support is expected to increase due to larger older cohorts and longer periods of care needs (6). Especially after COVID-19, the informal social support among the older adults is increasing rapidly due to the shortage of medical resources and the cessation or limitation of formal services for older adults (7).
Therefore, this study investigates the influence of informal social support on mental health in older adults by examining the relationship and underlying mechanisms. The research addresses two key questions: (1) To what extent does informal social support affect the mental well-being of older adults? (2) Through what pathways does this influence operate? Utilizing data from the 2018 China Longitudinal Aging Social Survey (CLASS) and applying Principal Component Analysis (PCA), this study provides a comprehensive analysis of the effects and mechanisms by which informal social support impacts the mental health of older adults.
The study makes several distinct contributions. Firstly, it introduced the concept of informal social support, offering a novel lens to assess its influence on mental health in older adults, thereby broadening the existing insights in this area. Secondly, PCA was employed to construct a multidimensional framework for informal social support variables, enhancing the precision of measurement methods and providing empirical evidence at the micro-level for the pathways through which informal social support influences mental health in older adults. Thirdly, the study not only dissected the heterogeneity of informal social support’s role in enhancing mental health in older adults but also rigorously investigated the transmission pathways, focusing on life satisfaction, access to healthcare, and social engagement, thereby extending the scope of current research.
2 Literature review
The international society faces growing concerns regarding the mental health of older adult population. Mental health, defined as a state of complete psychological well-being, encompasses positive internal experiences, strong social adaptability, and the effective use of personal potential and social functions. This state is understood as a dynamic and ongoing process of achieving balance (8). Presently, nearly one-third of older adult population experiences psychological disorders (9). When mental health is maintained, older adults tend to lead more joyful lives, which correlates with a heightened sense of subjective well-being (10). Notably, older adult women report higher levels of spiritual well-being compared to their male counterparts (11). Additionally, those who are rural, widowed, or of lower income are at a greater risk of experiencing loneliness (12).
Extensive research has been conducted on factors influencing mental health in older adults. One study emphasized the internal attributes of older adults, noting that enhanced social participation is associated with a deceleration in the progression of depression, ultimately benefiting mental well-being (13). Additionally, cultivating positive lifestyle choices and habits contributes to sustaining mental health in older adults (14). Some researchers have identified a strong correlation between sleep quality, dietary habits, physical activity, and the mental well-being of older adults (15). Further research has highlighted the influence of external factors, noting that, in the context of rapid advancements in information technology, internet usage inversely correlates with depression levels among older adults, while the digital divide poses risks to their mental health (16). Consequently, increased frequency and proficiency in internet usage, along with a broader utilization of its functions, contribute to improved psychological health in this population (17).
Current research has yet to systematically address the effects of informal social support on mental health in older adults. Existing literature, while acknowledging the role of social support, primarily emphasizes its overall impact. For instance, Krause in 2007 found that social support positively correlates with improved mental health and enhances older adults’ sense of life meaning (18). Studies also indicate that informal support networks help alleviate death-related anxiety among older adults, whereas formal interventions, such as participation in major illness insurance and cooperative medical reimbursement, are associated with heightened anxiety about death (19). In addition, informal support exerts a more profound influence on the mental well-being of older adults compared to formal support (20). Wang et al. in 2022 demonstrated that interactions with relatives and friends, facilitated by social media and active engagement, significantly alleviate loneliness among older adults, thereby bolstering their future outlook (21). Li et al. in 2022, examining the role of filial piety within the context of Chinese culture, identified the fulfillment of filial expectations as a critical determinant of life satisfaction in older adults (22). Notably, disharmony within family relationships can extend its impact on the broader aspects of older adult parents’ lives, contributing to reduced overall life satisfaction (23). While some researchers suggest that care from grandchildren can elevate the happiness of older adults, excessive attention may have the opposite effect (24).
The current body of literature offers a substantial basis for this study, yet certain aspects warrant deeper investigation. First, although extensive research has examined mental health in older adults through the lens of social support—both formal and informal—the multitude of indicators complicates the imprecise analysis of their specific impacts on mental well-being. Second, prior studies on informal social support have predominantly employed limited measurement approaches, often focusing solely on interactions with children or relatives. This narrow scope fails to capture a comprehensive, multidimensional framework for understanding the pathways through which informal social support influences mental health.
This study seeks to bridge existing research gaps by first examining the influence of informal social support on mental health in older adults, thereby broadening the scope of inquiry within this field. The analysis specifically incorporated nine indicators drawn from three distinct categories—children, relatives/family members, and friends—to offer a more nuanced and comprehensive understanding of the mechanisms through which informal social support impacts the mental well-being of older adults, supported by robust literature.
3 Research design
3.1 Data source
The data utilized in this study were sourced from CLASS, a survey primarily designed and implemented through a collaboration between the Development Research Center and the Institute of Gerontology at Renmin University of China, employing Probability Proportional to Size Stratified Sampling (PPS). Initiated in 2014 as a baseline, the survey follows a biennial cycle to systematically capture social and economic background data on China’s older adult population. This longitudinal approach aimed to illuminate the various challenges encountered during the aging process, thereby providing both theoretical and empirical foundations for addressing the implications of China’s aging demographic. In 2018, CLASS expanded its scope to include 28 provinces, municipalities, and autonomous regions, targeting older adult individuals aged 60 and above, with an initial sample size of 11,419. Following data cleaning and the exclusion of missing values, 7,063 valid samples were retained.
3.2 Variable selection and processing
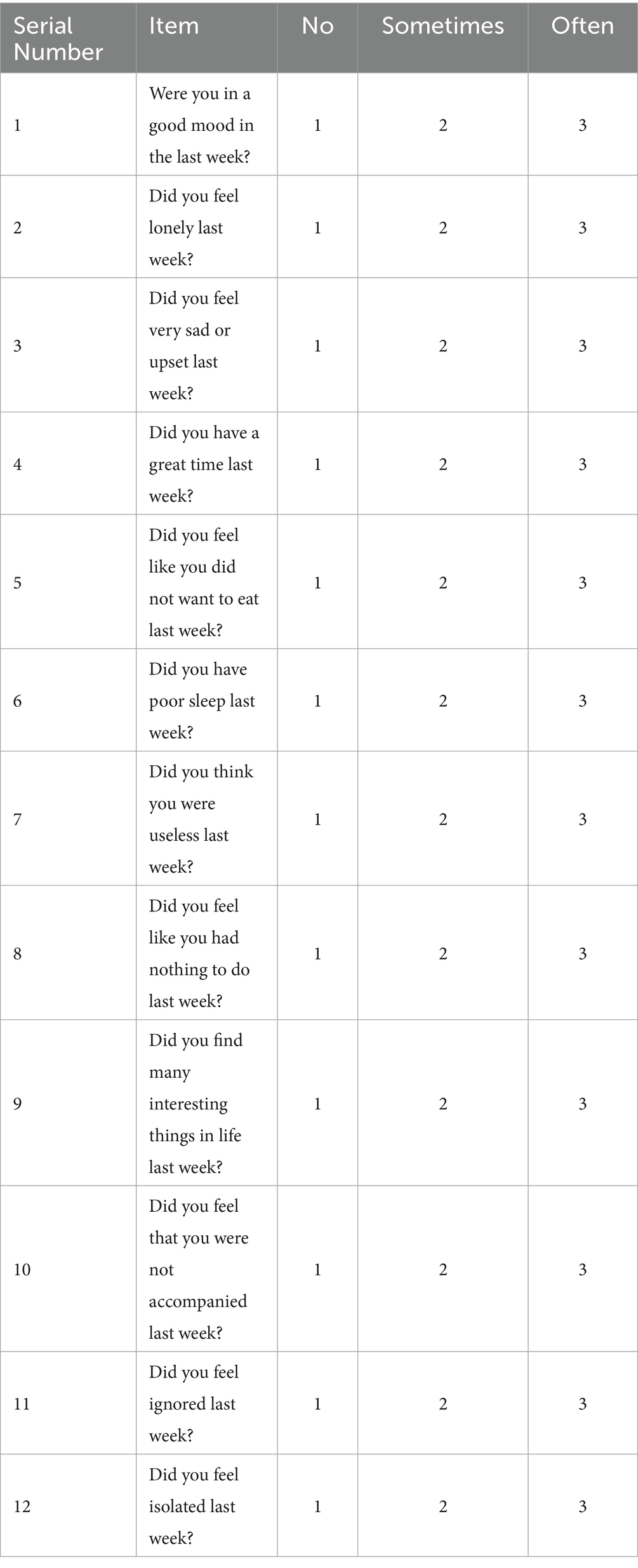
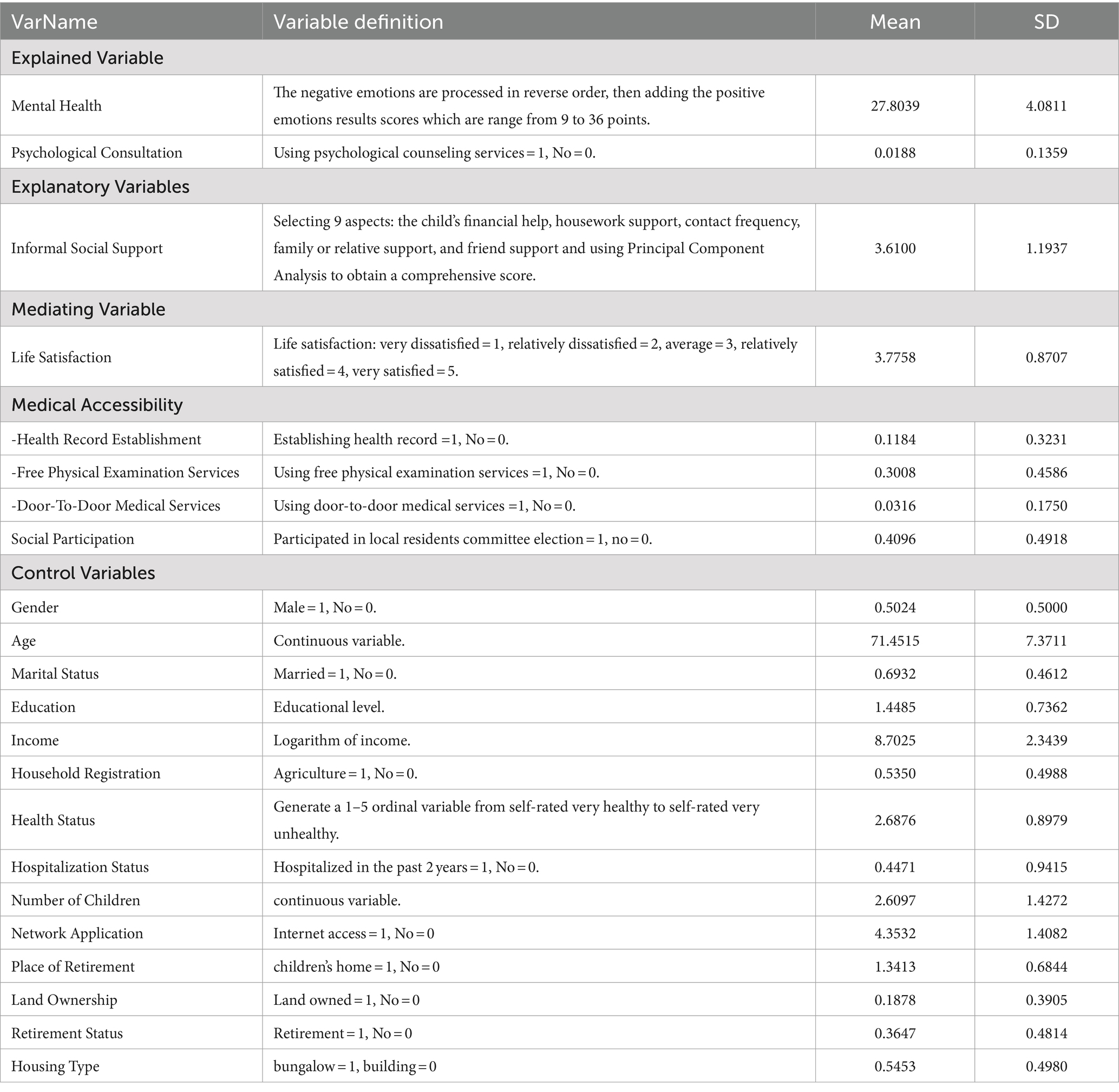
The dependent variable in this study was the mental health level of older adults, measured using indicators derived from the CLASS 2018 database. A total of 12 items constituted the relevant indicators (Table 1). Items 1, 4, and 9 corresponded to positive mental health indicators, while the remaining items reflect negative aspects. Responses were scored on a scale of 1 to 3 for “no,” “sometimes,” and “often,” respectively. Negative indicators were reverse-coded to accurately represent the overall mental health level. This variable was continuous, with scores ranging from 9 to 36 points, where a higher score indicated a higher level of mental health.
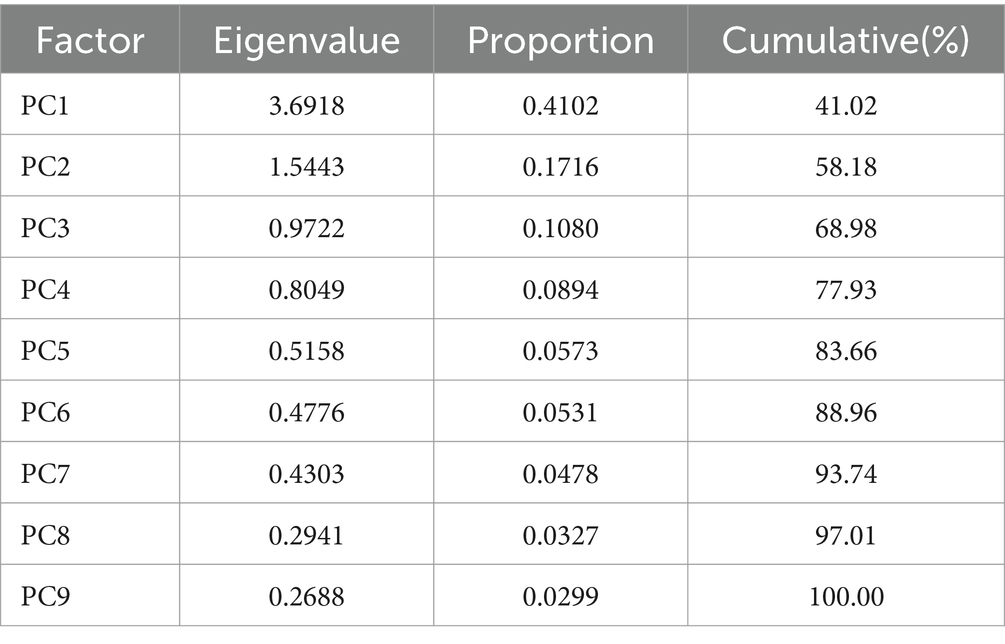
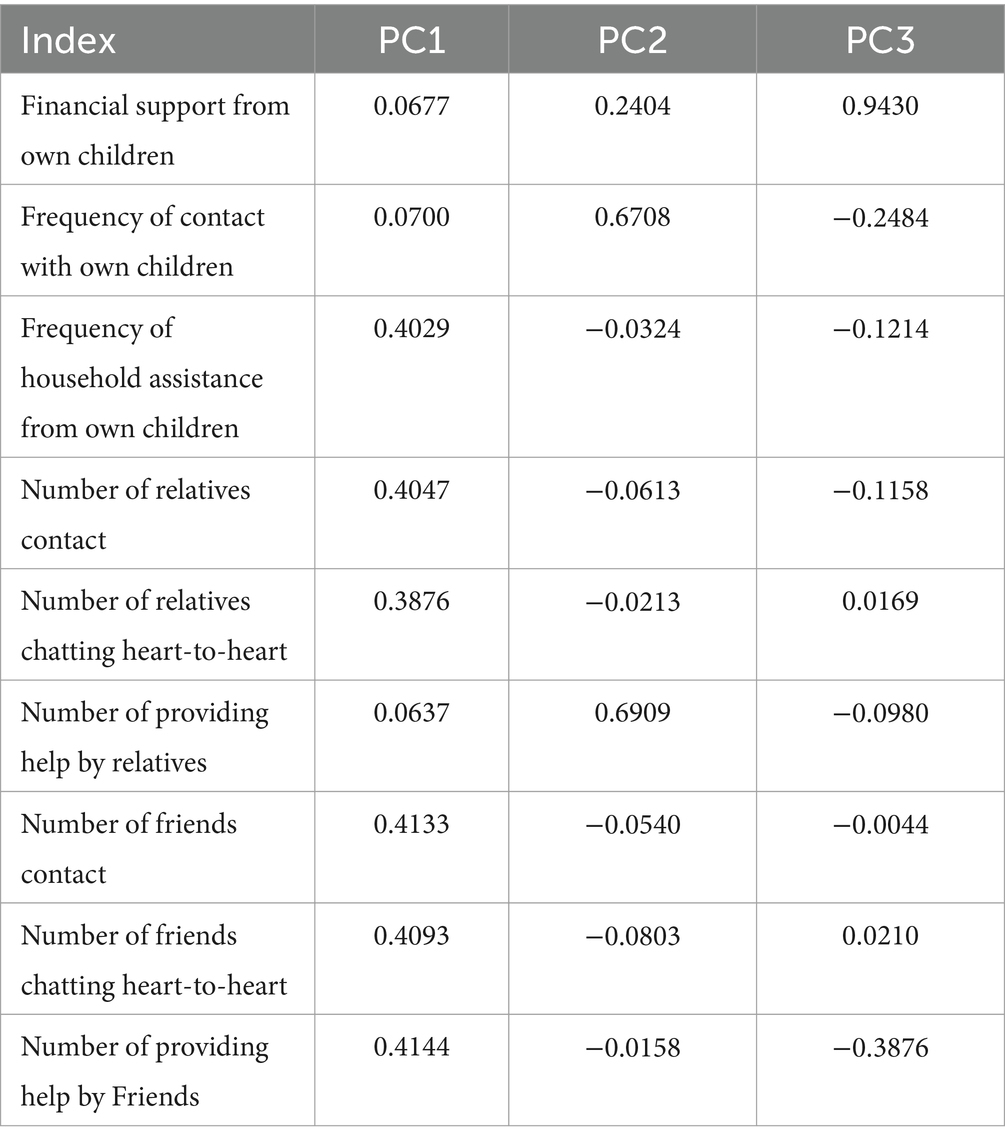
This study focused on informal social support as the independent variable. PCA was employed to condense indicators such as financial support from children, frequency of contact, household assistance, and communication with family, relatives, and friends, including heart-to-heart conversations and the extent of provided help. Initially, indicators were standardized, and then the reliability of the PCA method is assessed using the Kaiser-Meyer-Olkin (KMO) measure and Bartlett’s test of sphericity. After conducting the analysis in Stata 17, the KMO value was found to be 0.798, and Bartlett’s test of sphericity was significant at p = 0, indicating that the PCA results are reliable. Then, the factor matrix was subjected to an orthogonal rotation using the varimax method, yielding the factor loadings and eigenvalues of the principal components. The results are presented in Tables 2, 3.
Initially, based on the principle of retaining principal components with eigenvalues greater than 1, two principal components were selected. However, as shown in Table 1, the cumulative contribution rate of these two components is only 58.18%. To retain more information from the original data, the cumulative contribution rate was increased to nearly 70%, leading to the retention of three principal components with eigenvalues of 3.6918, 1.5543, and 0.9722. These components contribute 41.02, 17.16, and 10.80% of the total variance, respectively. To obtain the factor loadings of the principal components, a varimax rotation was applied using the varimax method. Table 3 presents the scoring coefficients for the principal components by Stata 17. The expressions for calculating the principal component scores are [as shown in (Equations 1–3)]:
Based on the above expressions, using the variance contribution rates of each component as weights, an evaluation formula for Informal Social Support (ISS) is established [as shown in Equation (4)], which measures the core explanatory variable of informal social support in this study.
Life satisfaction, medical accessibility, and social participation serve as mediating variables in this study. To assess life satisfaction among older adults, the study employed the “satisfaction with current life” item from the CLASS 2018 questionnaire as the primary indicator. Responses were quantified on a five-point ordinal scale, with values ranging from 1 (“very dissatisfied”) to 5 (“very satisfied”). This study operationalized the mediating variable of medical accessibility through three dimensions: health record establishment, free physical examination services, and door-to-door medical services. For health record establishment, the variable was constructed by selecting the database item “whether a health record was established in the past 12 months” and assigning a binary value (1 for “yes” and 0 for “no”). Similarly, the variable for free physical examination services was based on “whether free physical examination services were utilized in the past 12 months,” also coded as 1 for “yes” and 0 for “no.” The door-to-door medical services variable followed the same method, using the item “whether door-to-door medical services were used in the past 12 months” with identical binary coding. Additionally, the variable for older adults social participation was derived from the CLASS2018 database by selecting “whether the individual participated in voting for the local resident committee/village committee in the past 3 years” and assigning a binary value (1 for “yes” and 0 for “no”) to quantify social participation.
This study controlled for variables influencing the mental health of older adults across multiple dimensions, including personal attributes, family characteristics, and socioeconomic status. Specifically, age, gender, marital status, household registration, and health status were accounted for under personal attributes. Family characteristics considered included the number of children, housing type, and land ownership. Socioeconomic status variables included educational level, income, retirement status, and pension location. Internet usage was also controlled, representing the frequency and proficiency of internet engagement among older adults. Additionally, regional variations were addressed through the use of dummy variables. Detailed descriptive statistics were provided in Table 4.
4 Empirical results and analysis
4.1 Empirical test of the impact of informal social support on the mental health of older adults
The baseline regression results, derived using Ordinary Least Squares (OLS), were presented in Table 5. The findings consistently demonstrate that informal support exerted a statistically significant positive effect on the mental health of older adults, maintaining robustness across models with only core explanatory variables and those with all control variables included. For instance, in Model (3), even after incorporating all control variables, informal social support continued to positively influence the mental health of older adults. This suggests that informal support, typically provided by children, relatives, and friends, plays a vital role in enhancing the mental well-being of older adults. Emotional, financial, and caregiving support from core family members significantly influence the mental health of older adults, enhancing their quality of life in later years. Conversely, support from non-core family members, such as friends and neighbors, alleviates the pressures of dependency on children, contributing to improved mental health through role redefinition and identity reinforcement. In the context of an aging society, each incremental increase in informal social support correlates with a 0.402-unit improvement in mental health in older adults. From a human capital perspective, this dynamic holds substantial implications for bolstering national health capital, individual well-being, and overall human capital quality.
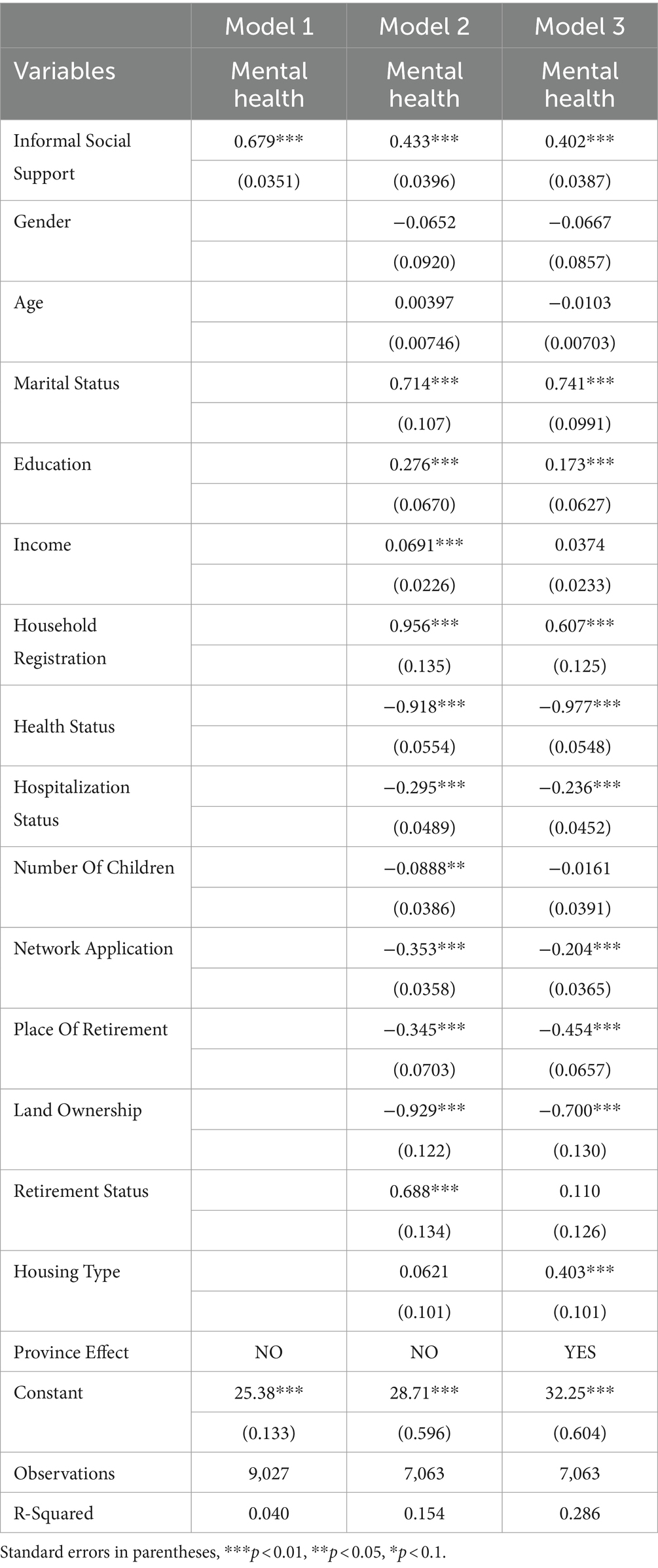
Table 5. Regression analysis of the influence of informal social support on mental health of older adults.
The regression analysis of control variables in Model (3) revealed several key insights. Although age correlated with a gradual decline in mental health among older adults, this relationship lacked statistical significance. Conversely, married older adult individuals exhibited significantly better mental health compared to their unmarried counterparts. Furthermore, the significantly negative coefficients for self-rated health and hospitalization status suggested a direct link between physical and mental well-being, with better physical health corresponding to improved mental health in older adults. Regarding family characteristics, the presence of more children appeared to correlate with a decline in the mental health of older adults, though this relationship did not reach statistical significance. In contrast, socioeconomic status indicators such as income and educational attainment showed significantly positive coefficients, affirming their beneficial effects on mental health in older adults. Moreover, engagement in internet use by older adults was associated with a modest inhibitory effect on their mental well-being.
4.2 Robustness test
4.2.1 Instrumental variable method
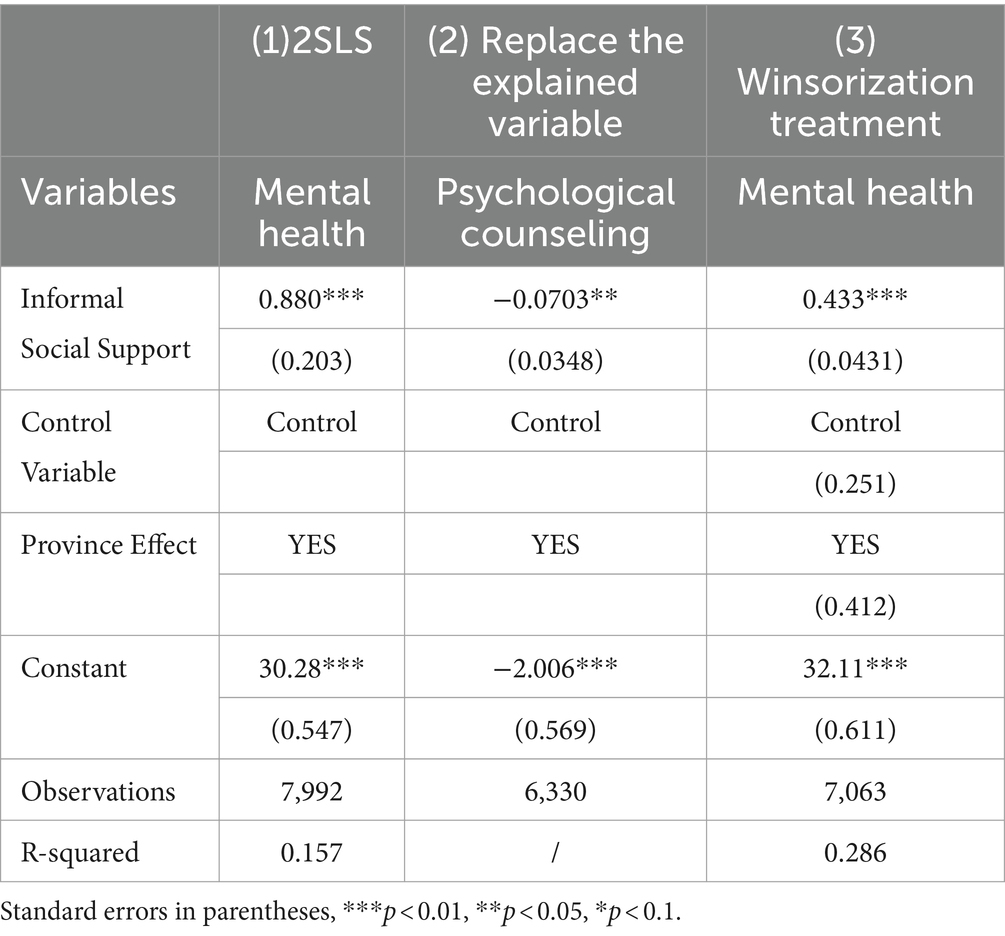
Previous regression analysis indicated a significant positive impact of informal social support on the mental health of older adults. However, the potential for reverse causality between informal social support and mental health presents a serious endogeneity issue. Emotional or financial assistance from children, family members, and friends can alleviate older adults’ living pressures, mitigate feelings of loneliness and alienation, and enhance mental health levels (25). Conversely, older adult individuals who are ill or widowed, driven by the traditional notion of “raising children to care for oneself in old age,” may place greater demands on their children for financial and emotional support. To mitigate endogeneity issues, including self-selection and omitted variables, this study adopted the approach of Zheng and Zheng in 2017 by selecting the provincial average wage level as an instrumental variable (26). A higher average local salary tends to increase the likelihood that older adult individuals will opt for self-reliance, declining financial or emotional support from children, friends, and others. Additionally, elevated socioeconomic status among older adults correlates with reduced dependence on informal social support (27), thereby meeting the requirements for a valid instrumental variable. However, the correlation between the provincial average wage level and the mental health of older adult individuals proved to be relatively weak, thereby supporting the exogeneity assumption of the instrumental variable. Column (1) of Table 6 presented the results from the Two-Stage Least Squares (2SLS) regression. The analysis confirmed that informal social support continued to exert a significantly positive impact on the mental health of older adults at the 1% significance level, reinforcing the robustness of the findings.
4.2.2 Replacing the explained variable
The main regression employed a composite measure of various psychological emotions to effectively represent the mental health status of older adults. An alternative approach to assess mental health was through the utilization of psychological counseling services, as individuals who opted for these services may exhibited poorer mental health. To ensure robustness, this study incorporated the question “Do you use psychological counseling?” from the CLASS 2018 questionnaire as the dependent variable to further analyze the impact of informal social support on mental health in older adults. As shown in Column (2) of Table 6, even after substituting the dependent variable, the coefficient for informal social support remained significantly positive at the 1% level, confirming that informal social support continued to have a substantial positive effect on the mental health of older adult individuals, and the regression results maintained robustness following this adjustment.
4.2.3 Winsorization treatment
Outlier values in the data could potentially bias the analysis results. To mitigate this, a 5% winsorization was applied to both ends of the distribution of the explanatory variable, reducing the impact of extreme values, followed by a regression analysis. The regression results, presented in Column (3) of Table 6, demonstrated that even after the winsorization treatment, the coefficient for informal social support on mental health in older adults remained significant at the 1% level. This result suggests a robust positive correlation between higher levels of informal social support and improved mental health outcomes in older adults.
5 Further analysis
5.1 Heterogeneity analysis
The analysis determined that while informal social support generally enhanced the mental health of older adults, this conclusion only reflected the average effect and does not account for the heterogeneous impact across different groups. To derive more nuanced insights, group regressions were conducted based on age, household registration, and retirement location. The detailed results were presented in Table 7.
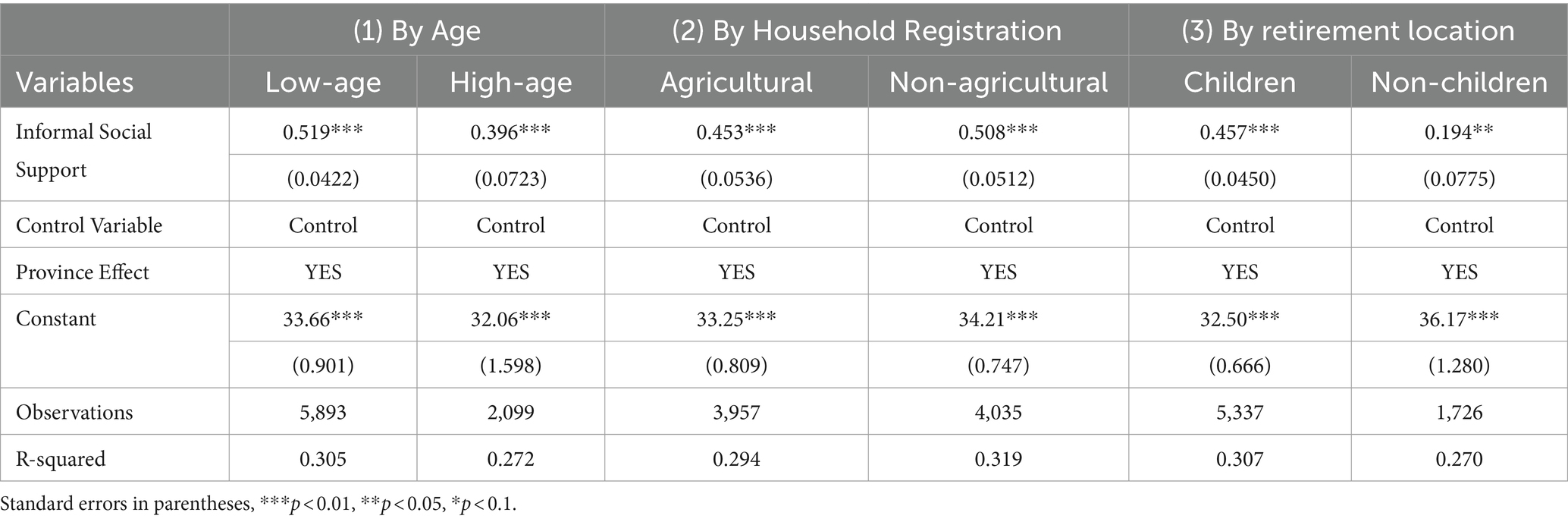
Table 7. Heterogeneity analysis of the impact of informal social support on the mental health of older adults.
5.1.1 Age difference
This study categorized older adults population into two groups—low-age and high-age—based on whether respondents were born before 1943. The regression results in Column (1) of Table 7 revealed that informal social support exerted a more substantial positive effect on the mental health of the low-age older adults compared to their high-age counterparts. A plausible explanation lies in the strong positive correlation between advancing age and the prevalence of physical and mental health challenges. As age increased, support from children, friends, and relatives may have diminishing returns on the health of older adults. High-age individuals are more susceptible to severe life challenges such as disability, cognitive decline, and illness, which can erode their will to live. Consequently, for those with better physical health, informal social support plays a more significant role in enhancing mental well-being, while its impact is less pronounced among those in the high-age category.
5.1.2 Household registration differences
This study investigated the differential impact of informal social support on mental health in older adults based on household registration status, categorizing respondents into agricultural and non-agricultural groups. The regression results presented in Column (2) of Table 7 indicated a stronger positive correlation between informal social support and mental health in the non-agricultural older adult population. In contrast, this effect was comparatively weaker among those with agricultural household registration. Consequently, it is essential for relevant authorities to prioritize the mental health of older adults in agricultural households and improve the effectiveness of informal social support in rural areas.
5.1.3 Place of retirement differences
To examine the influence of retirement location on the effect of informal social support on mental health in older adults, this study utilized the CLASS 2018 survey item, “Where do you plan to retire in the future?” Respondents were categorized into two groups: those planning to retire in their children’s households and those opting for non-children’s households (nursing homes, their own homes, etc.). A group regression analysis was then conducted. The results, presented in Column (3) of Table 7, indicated that informal social support exerted a stronger positive effect on the mental health of older adult individuals planning to retire in their children’s households compared to those choosing other retirement settings. This effect may be attributed to the higher availability of financial and emotional support from children, which enhanced the efficacy of informal social support. Consequently, it is imperative for core family members to consider retirement location choices carefully and prioritize the mental health of older adults.
5.2 Analysis of the mechanism of influence
To examine the indirect influence of the mediating variable, this paper draws on the mediation effect model proposed by Wen and Ye (28). Firstly, the impact of informal social support on the mediating variable is tested. Secondly, the influence of the mediating variable on the mental health of the older adults is assessed. Lastly, the combined effect of informal social support and the mediating variable on the mental health of the older adults is examined. The formulas are as follows:
In the above equations, _irepresents the mediating variable, _idenotes informal social support, and indicates the level of mental health in older adults, represents the control variables. While and represent random error terms. If, in Equation 5, remains significant or decreases slightly, and both and are significant in Equation 6, it suggests a partial mediation effect, indicating that the influence of the independent variable on the dependent variable is partly transmitted through the mediating variable. If becomes insignificant in Equation 5 and both and remain significant in Equation 6, this indicates a full mediation effect, meaning the impact of the independent variable on the dependent variable is entirely realized through the mediating variable. If neither nor are significant in Equation 6, it implies that no mediation effect exists. The analysis was conducted through three pathways: life satisfaction, medical accessibility, and social participation. The results were presented in Table 8.
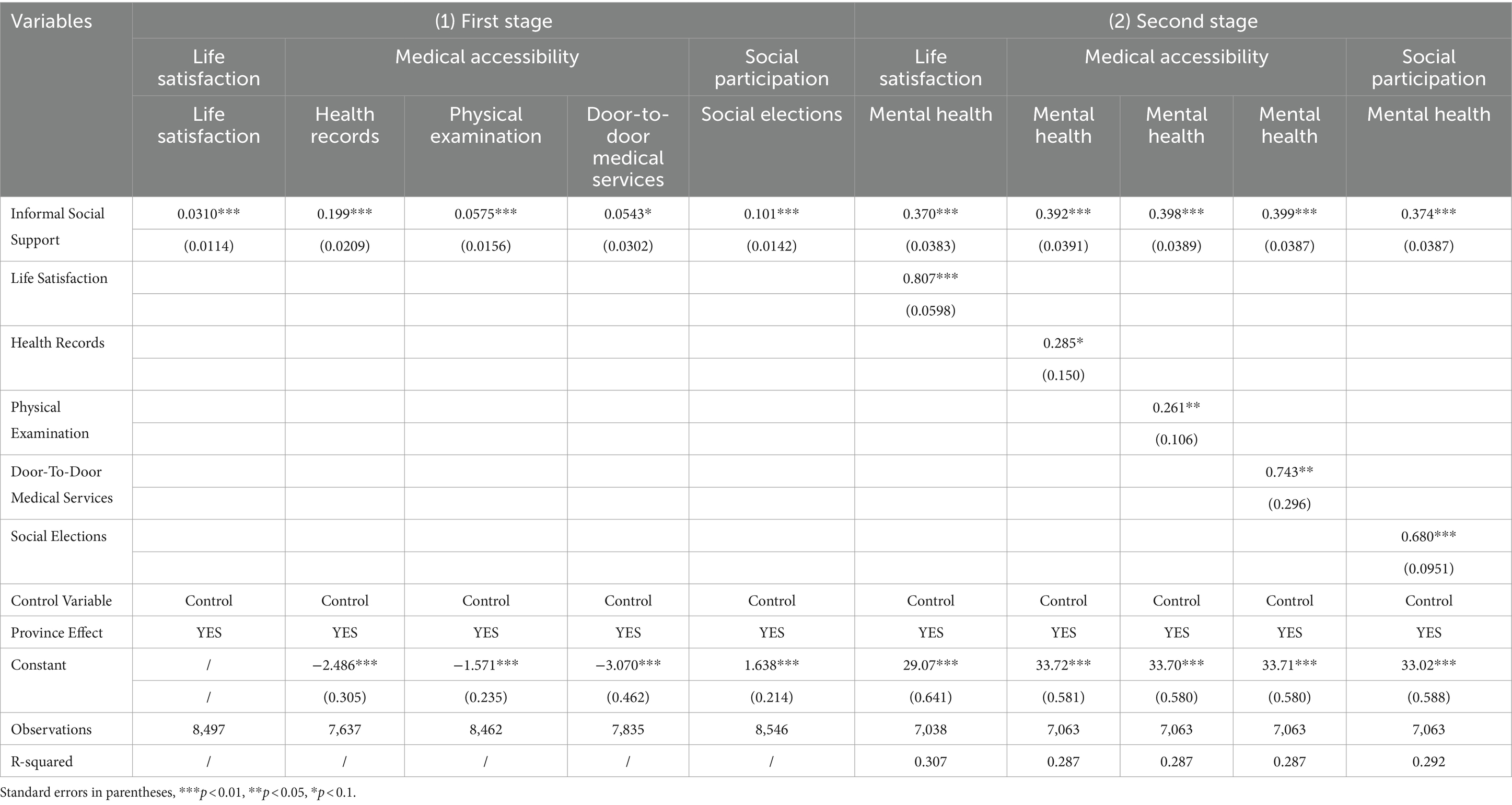
Table 8. Analysis of the impact mechanism of informal social support on the mental health of older adults.
Table 8, Column (1) presented the first stage of the mediating effect analysis, examining the influence of informal social support on mediating variables. Informal social support markedly enhanced life satisfaction among older adults and exerted a significant positive impact on establishing health records, participating in physical examinations, and utilizing door-to-door medical services, thereby improving medical accessibility for this demographic. Furthermore, it significantly increased their likelihood of engaging in social elections, thereby strengthening their capacity for social participation. The regression results thus suggest that informal social support effectively boosts life satisfaction, medical accessibility, and social engagement among older adults.
Table 8, Column (2), presented the second stage of the mediating effect, analyzing the influence of informal social support and mediating variables on the mental health of older adults. The results indicated that the coefficients for informal social support were significantly positive at the 1% level, as were the coefficients for each mediating variable. Enhancing life satisfaction among older adults contributed to fostering a healthy psychological state. Regarding medical accessibility, measures such as establishing health records, participating in free physical examinations, and utilizing door-to-door medical services significantly elevated the mental health levels of older adults. Additionally, engagement in social elections markedly improved their mental health. Thus, informal social support indirectly enhanced mental health by improving life satisfaction, medical accessibility, and social participation among older adults.
6 Discussion
Many older adult individuals are likely to encounter the challenge of shifting social roles following retirement, making attention to their mental health imperative. The decline in cognitive function, coupled with the abrupt lifestyle changes associated with retirement, can lead to psychological difficulties in approximately 85% of older adult population (29). Disengagement Theory posits that societal balance is maintained through a reciprocal interaction between society and the withdrawal of older adults, governed by established rules that remain unaffected by individual desires (30). Consequently, disengagement from social roles and interactions is an inherent aspect of aging, often accompanied by negative emotions. Addressing this requires enhanced psychological support and emotional care from children, relatives, and friends. China’s deep-rooted cultural tradition of respecting, honoring, and caring for older adults has been perpetuated for thousands of years, forming the ethical foundation of the country’s older adults care practices (31). In rural society, cultural norms and beliefs such as “filial piety” and “raising children for old age” play a central role in guiding social behavior. Social expectations further reinforce the obligation for children to provide financial and emotional support to their parents. Consequently, the family-based and home-based pension models have remained predominant due to the historical continuity of these cultural traditions. Additionally, research indicates that older adult individuals with a larger network of relatives and friends are more likely to maintain a positive outlook during the aging process (32). Social support from friends mitigates the risk of chronic diseases that contribute to anxiety in older adults and alleviates symptoms of depression (33). Consequently, informal social support—primarily from children, family, relatives, and friends—emerges as a significant factor positively influencing the mental health of older adults, a key conclusion of this study.
An in-depth analysis was conducted on how informal social support influenced the mental health of older adults. Older adults care extends beyond merely providing basic needs such as support and dependence; it should prioritize enhancing quality of life and overall satisfaction. The predominant Chinese older adults care model, which emphasizes home-based care, effectively improves the quality of life for older adult individuals residing with their children (34). In contrast, those living in older adults care institutions often report lower levels of life satisfaction (35). This correlation between informal social support and life satisfaction has been validated by various studies. Further research indicates that living arrangements play a critical role in determining the life satisfaction levels of older adults (36). Thus, informal social support plays a significant role in enhancing the life satisfaction of older adults, which is a critical indicator of their overall quality of life and mental health (37). Previous studies have identified a negative correlation between poor psychological well-being and life satisfaction among older adults (38), with this relationship being particularly pronounced in cases of depression (39). Additionally, research suggests that self-esteem and family functioning are key factors in boosting life satisfaction among middle-aged and older adult individuals in rural areas (40). This study empirically supported the notion that enhancing life satisfaction was a primary mechanism by which informal social support influences the mental health of older adults.
Beyond life satisfaction, medical accessibility plays a significant role in the mental health of older adults. This study posited that informal social support enhanced access to medical services, thereby influencing mental health in older adults. The financial status of older adults or their families often acts as a key barrier to obtaining social care and professional medical services (41). Scholars have argued that better economic conditions increase the likelihood of choosing social care and professional medical services (42). Consequently, older adult individuals with limited financial resources or low pension incomes who require medical treatment due to illness are more dependent on their children for assistance. Regarding the influence of medical services on mental health, regular physical examinations and effective doctor-patient interactions enhance older adults’ understanding of their health and improve their physical and mental management abilities. In response, some researchers have proposed the “Door-to-door Medical Services” model, which enables older adults to receive follow-up visits, chronic disease management, physical examinations, and other medical services at home. This model fosters a harmonious doctor-patient relationship, as it is rooted in the familiarity of older adults with their local communities, thereby enhancing their sense of identity and comfort (43). Consequently, increased access to medical services, caregiving, and daily companionship are important factors in improving the mental health of older adults.
The study demonstrated that informal social support enhanced the mental health of older adults by encouraging greater social participation. Family support serves as a fundamental catalyst for this participation, making a positive and nurturing family environment essential for bolstering their emotional inclination to engage in social activities. Within the Chinese cultural context, kinship ties, which are central to the Differential Mode of Association, resemble a series of concentric circles. From the kinship networks established through birth and marriage, broader social networks emerge; this pattern extends to geographical relationships as well (44). For older adults in China, the family remains the primary source of support resources (45). Family-based social networks exert a more pronounced influence on the mental health of older adults in China. Women, compared to men, demonstrate a greater willingness and aptitude for cultivating social relationships outside the family, a tendency that becomes increasingly evident with age (46). Consequently, older adult women tend to have broader friendship networks and more extensive overall social connections than their male counterparts (47). Additionally, researchers have highlighted the strong correlation between the health of older adults and their living environment, emphasizing that social integration and interpersonal relationships provide essential meaning to their lives (48). Thus, social participation plays a vital role in enhancing the mental health of older adults.
The findings of this study hold significant policy implications. Addressing the mental health challenges faced by older adults necessitates the cultivation of a supportive environment to improve their care experience, the reform of the medical system to better meet their needs, and the encouragement of social participation to facilitate their continued contributions.
First, to enhance the care experience of older adults, fostering a supportive and harmonious atmosphere is essential. Promoting cultural values such as “filial piety” and “harmony in the family brings prosperity” tailored to local contexts can help establish a peaceful and cohesive family environment. Additionally, influenced by family ties and blood relations, older adults often anticipate spending their later years surrounded by their children and family members. Thus, family-based older adults care models require redefinition, moving beyond rigid adherence to tradition toward fostering relationships grounded in mutual respect and open communication among family members. It is essential to ensure older adults receive full understanding and care while enhancing family cohesion to elevate their life satisfaction and overall happiness.
Second, addressing the needs of older adults requires strengthening the medical system. This involves advancing the reform of medical services, with a focus on enhancing the supply infrastructure and creating an integrated coordination mechanism between comprehensive hospitals and community health organizations. Tailored care services should be provided based on the diverse medical needs of older adults, aiming to establish a comprehensive and effective healthcare system for this population. Moreover, equitable distribution of medical resources is critical, particularly in enhancing policy support for rural and remote regions. Regular physical examinations and psychological care should be provided through government initiatives, ensuring that older adults have consistent access to medical services.
Third, promoting social participation among older adults enables them to remain active contributors to society. Older adult individuals in good health can be encouraged by some public policies to engage in community volunteer services or simple employment within their capabilities. These activities allow them to realize their value and expand their social networks through meaningful societal interaction (49). Additionally, as information technology continues to evolve with older adults-oriented reforms, online participation has emerged as a new avenue for social integration. For those with limited mobility, enhancing digital literacy and bridging the digital divide can expand their opportunities for online social engagement.
7 Conclusion
Utilizing data from the 2018 China Longitudinal Aging Social Survey (CLASS), this study employs Principal Component Analysis (PCA) to systematically assess the impact of informal social support on mental health in older adults and its underlying mechanisms. The analysis reveals that informal social support exerts a significant positive effect on mental health, particularly among younger, non-agricultural older adult individuals who prefer cohabitation with their children. Among various forms of informal social support, assistance from family and relatives emerges as the most influential factor in enhancing older adult mental well-being. The mechanisms driving this effect include increased life satisfaction, improved medical accessibility, and greater social participation. This study elucidates the impact of informal social support on enhancing the mental health of older adults. Moving forward, efforts should focus on fostering a supportive environment that enriches the care experience for older adults, reforming the medical system to better address their needs, and encouraging social participation to enable their continued contributions. These measures will help achieve a balanced integration of “spiritual care” and “physical care.”
While this study robustly argues for the relationship between informal social support and mental health in older adults, it still has some limitations as follow. First, this study uses cross-sectional survey data, which has certain limitations in the vertical dimension. Second, this study explored the role of life satisfaction, medical accessibility and social participation as the mediating variables, but there may be multiple mediating pathways from other perspectives. By combining all the analysis, future research could utilize panel data to track individual changes for a better understanding. Additionally, the potential mediating variables within digital and intelligent elements could be further considered to expand the depth and scope of future research in the coming era of artificial intelligence.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found at: http://www.isss.pku.edu.cn/cfps/sjzx/gksj/index.htm.
Ethics statement
The studies involving humans were approved by School of Public Administration, Hohai University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
YD: Conceptualization, Formal analysis, Supervision, Validation, Writing – original draft, Writing – review & editing, Funding acquisition, Project administration, Resources, Visualization. LC: Data curation, Methodology, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. HC: Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Postgraduate Research & Practice Innovation Program of Jiangsu Province (Project No. KYCX22_0696).
Acknowledgments
The authors would like to acknowledge the contributions of specific colleagues, institutions, and agencies that supported this work.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Zhai, S, Zhuang, Q, and Wang, Z. Study on the relationship between social support and mental health of the elderly in China: a case study of Xi’an city, Shaanxi province. J Ment Health. (2019) 28:119–24. doi: 10.1080/09638237.2017.1340626
2. Zhou, D, Zhan, Q, and Li, L. The impact of self-employment on mental health of the younger elderly in China. BMC Geriatr. (2023) 23:1–14. doi: 10.1186/s12877-023-03948-5
3. Zhang, C, and Dong, C. The influence of social support on the mental health of elderly individuals in healthy communities with the framework of mental toughness. Psychol Res Behav Manag. (2023) 16:2977–88. doi: 10.2147/PRBM.S413901
4. Gallardo-Peralta, LP, de Roda, ABL, Ángeles Molina-Martínez, M, and Schettini del Moral, R. Family and community support among older Chilean adults: the importance of heterogeneous social support sources for quality of life. J Gerontol Soc Work. (2018) 61:584–604. doi: 10.1080/01634372.2018.1489928
5. Hutchison, C . Social support: factors to consider when designing studies that measure social support. J Adv Nurs. (1999) 29:1520–6. doi: 10.1046/j.1365-2648.1999.01041.x
6. The World Bank Group . Why should we care about care? The role of informal childcare and eldercare in aging societies. (2010). Available at: https://documents1.worldbank.org/curated/en/687741468257352228/pdf/ACS13024-REVISED-WP-PUBLIC-Box393205B.pdf [Accessed on August 22, 2024].
7. Kim, Hongsoo . Older People’s health and long-term care during COVID-19: Impacts and policy responses. (2023). Available at: https://thedocs.worldbank.org/en/doc/cb06300a736bfc104914e21c0370c0e1-0070012023/original/PN3-older-people.pdf [Accessed on August 25, 2024].
8. Galderisi, S, Heinz, A, Kastrup, M, Beezhold, J, and Sartorius, N. Toward a new definition of mental health. World Psychiatry. (2015) 14:231–3. doi: 10.1002/wps.20231
9. Tao, T, Yuhuai, C, and Jing, ZHU. Effect of air pollution and rural-urban difference on mental health of the elderly in China. Iran J Public Health. (2015) 44:1084–94. doi: 10.1046/j.1365-2443.1996.d01-231.x
10. Elliot, D . Defining the relationship between health and well-being in bioethics. New Bioethics. (2016) 22:4–17. doi: 10.1080/20502877.2016.1155267
11. Bailly, N, Martinent, G, Ferrand, C, Agli, O, Giraudeau, C, Gana, K, et al. Spirituality, social support, and flexibility among older adults: a five-year longitudinal study. Int Psychogeriatr. (2018) 30:1745–52. doi: 10.1017/S1041610218000029
12. Drennan, J, Treacy, M, and Butler, M. The experience of social and emotional loneliness among older people in Ireland. Ageing Soc. (2008) 28:1113–32. doi: 10.1017/S0144686X08007526
13. Wang, X, Guo, J, Liu, H, Zhao, T, Li, H, and Wang, T. Impact of social participation types on depression in the elderly in China: an analysis based on counterfactual causal inference. Front Public Health. (2022) 10:792765. doi: 10.3389/fpubh.2022.792765
14. Tian, H, and Chen, J. Impact of lifestyle and diets behaviors on elderly health: questionnaire based cross-sectional study. Prog Nutr. (2022) 24:e2022088. doi: 10.23751/pn.v24i2.12532
15. Zhao, Y, Song, J, and Brytek-Matera, A. The relationships between sleep and mental and physical health of Chinese elderly: exploring the mediating roles of diet and physical activity. Nutrients. (2021) 13:1316. doi: 10.3390/NU13041316
16. Guo, H, Feng, S, and Liu, Z. The temperature of internet: internet use and depression of the elderly in China. Front Public Health. (2022) 10:1076007. doi: 10.3389/fpubh.2022.1076007
17. Fan, S, and Yang, Y. How does internet use improve mental health among middle-aged and elderly people in rural areas in China? A quasi-natural experiment based on the China health and retirement longitudinal study (CHARLS). Int J Environ Res Public Health. (2022) 19:13332. doi: 10.3390/ijerph192013332
18. Krause, N . Longitudinal study of social support and meaning in life. Psychol Aging. (2007) 22:456–69. doi: 10.1037/0882-7974.22.3.456
19. Wang, P, Shang, J, and He, J. Impact of social support on death anxiety of older adults in rural China. Northwest Population J. (2021) 42:85–96. doi: 10.15884/j.cnki.issn.1007-0672.2021.01.007
20. Muramatsu, N, Yin, H, and Hedeker, D. Functional declines, social support, and mental health in the elderly: does living in a state supportive of home and community-based services make a difference? Soc Sci Med. (2010) 70:1050–8. doi: 10.1016/j.socscimed.2009.12.005
21. Wang, H, Sun, X, Wang, R, Yang, Y, and Wang, Y. The impact of media use on disparities in physical and mental health among the older people: an empirical analysis from China. Front Public Health. (2022) 10:949062. doi: 10.3389/fpubh.2022.949062
22. Li, X, Jin, Y, and Liu, J. Is older adult happier with more filial piety children? The role of filial responsibility expectation of older adult. Acta Psychol Sin. (2022) 54:1381–90. doi: 10.3724/SP.J.1041.2022.01381
23. Huang, V, and Fiocco, AJ. Measuring perceived receipt of filial piety among Chinese middle-aged and older adults. J Cross Cult Gerontol. (2020) 35:195–208. doi: 10.1007/s10823-019-09391-7
24. Chyi, H, and Mao, S. The determinants of happiness of China’s elderly population. J Happiness Stud. (2012) 13:167–85. doi: 10.1007/s10902-011-9256-8
25. Sun, W, and Shi, D. The effect mechanism of social support and mental health of rural elderly. Sociolog Rev China. (2020) 8:77–87.
26. Zheng, Z, and Zheng, Y. The influence of social support on the health and life satisfaction of the elderly: re-examine based on the endogenous of intergenerational economic support. Population Econ. (2017):63–76.
27. Chen, YJ, and Chen, CY. Living arrangement preferences of elderly people in Taiwan as affected by family resources and social participation. J Fam Hist. (2012) 37:381–94. doi: 10.1177/0363199012440948
28. Wen, Z, and Ye, B. Analyses of mediating effects: the development of methods and models. Adv Psychol Sci. (2014) 22:731–45. doi: 10.3724/SP.J.1042.2014.00731
29. Luan, W, Yang, F, and Chuan, H. The study on the psychological health status of old people in China and its influencing factors. J Northwest University (Philos Soc Sci Edition). (2012) 42:75–83. doi: 10.16152/j.cnki.xdxbsk.2012.03.018
30. Yen, CH, Liao, WC, Chen, YR, Kao, MC, Lee, MC, and Wang, CC. A Chinese version of Kogan's attitude toward older people scale: reliability and validity assessment. Int J Nurs Stud. (2009) 46:37–43. doi: 10.1016/j.ijnurstu.2008.05.004
31. Hu, Z, Peng, X, and Li, G. Strategic changes and policy choices in the governance of China's aging society. Soc Sci China. (2020) 41:185–208. doi: 10.1080/02529203.2020.1844451
32. Kim, G, Jang, Y, and Chiriboga, DA. Personal views about aging among Korean American older adults: the role of physical health, social network, and acculturation. J Cross Cult Gerontol. (2012) 27:139–48. doi: 10.1007/s10823-012-9165-2
33. Mchugh, JE, and Lawlor, BA. Exercise and social support are associated with psychological distress outcomes in a population of community-dwelling older adults. J Health Psychol. (2012) 17:833–44. doi: 10.1177/1359105311423861
34. Xu, Q, Wang, J, and Qi, J. Intergenerational coresidence and the subjective well-being of older adults in China. Demogr Res. (2019) 41:1347–72. doi: 10.4054/DemRes.2019.41.48
35. Liu, T, Hao, X, and Zhang, Z. Identifying community healthcare supports for the elderly and the factors affecting their aging care model preference: evidence from three districts of Beijing. BMC Health Serv Res. (2016) 16:83–92. doi: 10.1186/s12913-016-1863-y
36. Chen, F, and Short, SE. Household context and subjective well-being among the oldest old in China. J Fam Issues. (2008) 29:1379–403. doi: 10.1177/0192513X07313602
37. Requena, C, Martínez, AM, and Ortiz, T. Vital satisfaction as a health indicator in elderly women. J Women Aging. (2010) 22:15–21. doi: 10.1080/08952840903488872
38. Adams, TR, Rabin, LA, and Da Silva, VG. Social support buffers the impact of depressive symptoms on life satisfaction in old age. Clin Gerontol. (2016) 39:139–57. doi: 10.1080/07317115.2015.1073823
39. Shao, L, Yu, G, and Zhang, D. The mechanisms underlying the negative effect of depression on life satisfaction among the elderly: the roles of ostracism and economic income. Int Psychogeriatr. (2022) 34:715–24. doi: 10.1017/S1041610221001162
40. Gao, J, Ma, X, and Yang, T. Analysis of effect of self-esteem and family function on the relationship between depressive symptoms and life satisfaction of middle-aged and elderly people in rural areas in Guangdong Province. Med Society. (2023) 36:133–8. doi: 10.13723/j.yxysh.2023.07.024
41. Yang, S, Wang, D, and Li, C. Medical treatment behaviour of the elderly population in shanghai: group features and influencing factor analysis. Int J Environ Res Public Health. (2021) 18:4108. doi: 10.3390/ijerph18084108
42. Zhan, HJ, Liu, G, and Guan, X. Willingness and availability: explaining new attitudes toward institutional elder care among Chinese elderly parents and their adult children. J Aging Stud. (2006) 20:279–90. doi: 10.1016/j.jaging.2005.09.006
43. Zheng, Y, and Hao, X. The influence of medical care services accessibility on the choice of Care Services of the Elderly:an empirical study based on Beijing. Population Develop. (2021) 27:117–23.
45. Tang, D, Lin, Z, and Chen, F. Moving beyond living arrangements: the role of family and friendship ties in promoting mental health for urban and rural older adults in China. Aging Ment Health. (2020) 24:1523–32. doi: 10.1080/13607863.2019.1602589
46. Schwartz, E, and Litwin, H. Social network changes among older Europeans: the role of gender. Eur J Ageing. (2018) 15:359–67. doi: 10.1007/s10433-017-0454-z
47. Santini, ZI, Fiori, KL, Feeney, J, Tyrovolas, S, Haro, JM, and Koyanagi, A. Social relationships, loneliness, and mental health among older men and women in Ireland: a prospective community-based study. J Affect Disord. (2016) 204:59–69. doi: 10.1016/j.jad.2016.06.032
48. Hupkens, S, Machielse, A, Goumans, M, and Derkx, P. Meaning in life of older persons: an integrative literature review. Nurs Ethics. (2018) 25:973–91. doi: 10.1177/0969733016680122
49. The World Bank Group . World Bank support to aging countries-an independent evaluation. (2021). Available at: https://ieg.worldbankgroup.org/sites/default/files/Data/Evaluation/files/Aging Countries.pdf [Accessed on August 30, 2024].
Keywords: mental health of older adults, informal social support, life satisfaction, medical accessibility, social participation
Citation: Dong Y, Cheng L and Cao H (2024) Impact of informal social support on the mental health of older adults. Front. Public Health. 12:1446246. doi: 10.3389/fpubh.2024.1446246
Edited by:
I-Shiang Tzeng, National Taipei University, TaiwanReviewed by:
Carlos Madeira, Central Bank of Chile, ChileEvelyn Acoba, Central Luzon State University, Philippines
Copyright © 2024 Dong, Cheng and Cao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lanyan Cheng, bGFueWFuLmNoZW5nQG91dGxvb2suY29t
 Yi Dong1
Yi Dong1 Lanyan Cheng
Lanyan Cheng