- 1Section of Infectious Diseases, Department of Internal Medicine, Yale School of Medicine, New Haven, CT, United States
- 2Division of Social and Administrative Sciences, School of Pharmacy, University of Wisconsin-Madison, Madison, WI, United States
- 3Division of Infectious Diseases, Johns Hopkins University School of Medicine, Baltimore, MD, United States
- 4School of Communication, Illinois State University, Normal, IL, United States
- 5Department of Medicine, School of Medicine and Public Health, University of Wisconsin-Madison, Madison, WI, United States
- 6School of Medicine and Public Health, University of Wisconsin, Madison, WI, United States
Introduction: Medication adherence contributes to poor HIV outcomes, especially among people with HIV and Substance use disorder (SUD). Mobile health applications have been leveraged to improve behavioral health outcomes among this population. Our cross-sectional study examined the relationship between medication adherence with factors such as treatment self-regulation, isolation, and internalized stigma, among people with HIV and SUD using the Addiction Comprehensive Health Enhancement Support System (A-CHESS) mobile app.
Methods: A sample of 208 participants using A-CHESS to improve treatment adherence completed a survey. Adherence was measured using the Four-item Morisky Medication Adherence Scale and dichotomized (maximum score of 20 points considered as adherent). Positive and negative affect was measured separately using Positive Affect Negative Affect Schedule and loneliness was measured using UCLA three-item Loneliness Scale. Internalized stigma was measured using Internalized AIDS-Related Stigma Scale. Competence/Treatment self-regulation was measured using Treatment Self-regulation Questionnaire. Multivariable logistic regression was used to assess the associations of affect, treatment self-regulation, isolation, and internalized stigma, with adherence to antiretroviral therapy adjusting for age, education, and gender.
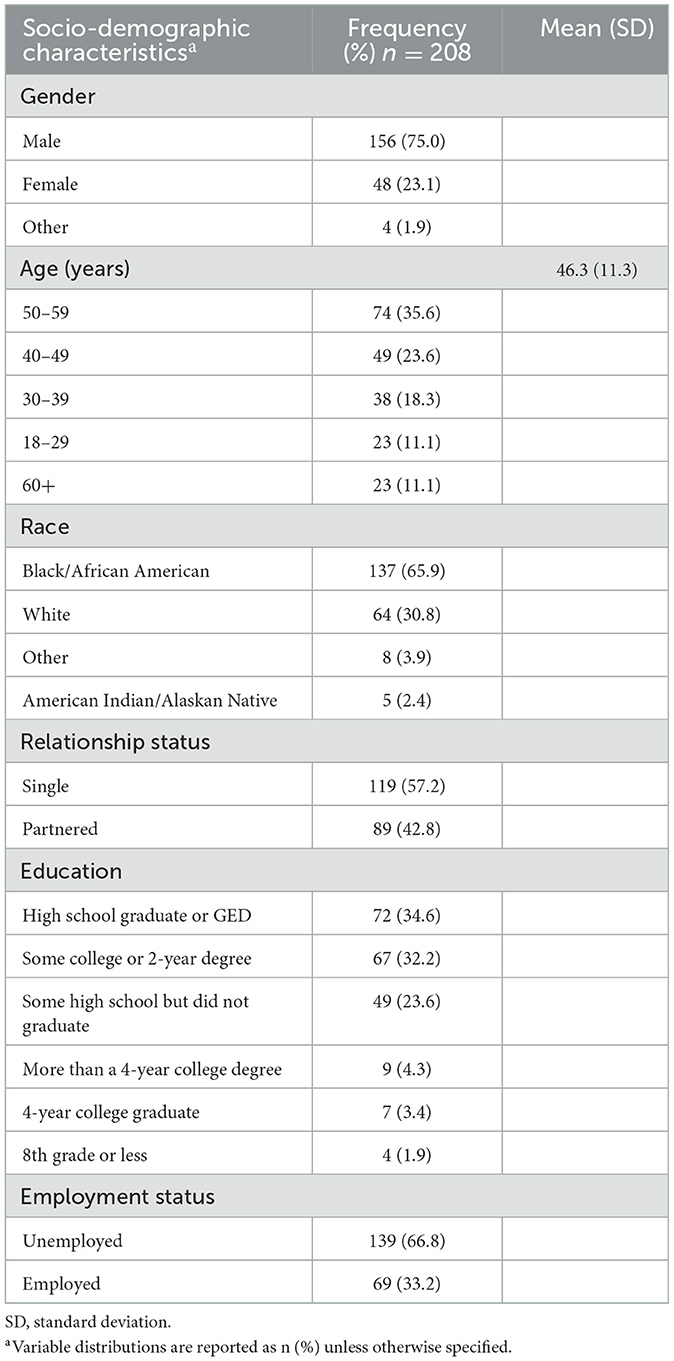
Results: Among 208 participants in this study, most were Black (n = 137; 66%), male (n = 156; 75%) and had a mean age of 46 (standard deviation = 11.3). The most reported substances associated with missing HIV medication were alcohol (27%) and cocaine/crack (20%). Logistic regression analysis revealed that internalized stigma was significantly associated with HIV medication adherence (OR = 0.82; 95% CI: 0.70–0.99; p = 0.034).
Conclusion: Internalized stigma was significantly associated with HIV medication adherence. Further research is needed to better understand this relationship and develop interventions addressing stigma in people with HIV and SUD.
1 Introduction
Antiretroviral therapy (ART) has transformed the health and quality of life of people living with HIV (PWH), enabling them to achieve life expectancies comparable to those without the virus (1). However, the effectiveness of ART depends on appropriate medication adherence (2), which entails following the prescribed timing, dosage, and frequency over the recommended treatment duration (3). Optimal adherence to ART decreases viral load (4), improves immune function (5), reduces mortality rates (6), and enhances the overall quality of life in PWH (7–9).
According to HIV surveillance data from the Centers for Disease Control and Prevention (CDC), only 62.7% of PWH achieve viral suppression (10), indicating suboptimal medication adherence. Prior research indicates that ART adherence is impacted by several complex psychosocial factors, including substance use disorder (SUD) (11, 12). The syndemic theory suggests that multiple co-occurring psychosocial comorbidities interact synergistically to contribute to poor health outcomes for PWH (13). Substance use has been identified as an independent risk factor for poor HIV outcomes within the syndemic context (14, 15). For instance, a prospective study found that individuals using drugs, regardless of their usage pattern (e.g., intermittent use, persistent use), had higher odds of having an unsuppressed viral load than non-users (16). Moreover, increased alcohol consumption has been linked to lower odds of improving ART adherence (17, 18). Therefore, it is imperative to investigate medication adherence within this subpopulation to understand the factors influencing adherence and develop targeted interventions.
Factors impacting care among PWH and SUD operate on multiple levels, including intrapersonal, interpersonal, community, societal, and structural (19). Multiple behavioral change theories explore the factors influencing adherence in chronic disease management (20, 21). Specifically, psychological theories such as the Health Belief Model (22), Social-Cognitive Theory (23), and Theory of Reasoned Action (24) have challenged the passive role of patients in healthcare, emphasizing that adherence depends on individuals being informed, motivated, and convinced of treatment benefits (25, 26). Despite the promises of these theories in understanding medication adherence, they do not account for external factors, such as social relationships, and ones' perception of their relationship which impacts the individual's engagement in a behavior (26).
Additionally, there are still limitations in applying theory-driven evidence-based models to develop effective interventions to understand and address medication adherence (27). A recent scoping review of qualitative studies exploring the complexity of medication adherence in patients with chronic disease found that only 17 studies had a behavior theory-based approach to understanding medication adherence (28). A review of the utility of health behavior theories for developing interventions to promote long-term medication adherence identified that only one study employed an explicit theoretical framework (29). Specifically, in HIV research, many ART adherence interventions have limited or no explicit theoretical basis (30).
Self-determination theory (SDT) is one prominent theory used extensively to promote health behavior change (31, 32). Findings from a recent meta-analysis support the efficacy of SDT interventions in promoting health behavior change (33). SDT suggests that individuals achieve greater self-regulation by internalizing their behaviors, moving from external control to autonomous regulation, with motivation types and environmental factors playing a role in this process (34). A qualitative study of PWH in New York integrated Critical Race Theory, Harm Reduction, and SDT to identify and understand the complex and multi-level factors that drive poor engagement in HIV care focused on the positive impact of the SDT construct of social-relatedness and engagement in care (35). Similarly, SDT was applied to address drug-related harm among PWH who use drugs (36). SDT provides valuable insights into the impact of social environments on addiction among individuals with unmet psychosocial needs, such as relatedness (37).
Psychological theories and approaches are valuable in identifying modifiable factors associated with behaviors like medication adherence (38), and they hold particular promise for individuals with SUD who face unique challenges with adherence. Theory-based interventions can significantly improve health outcomes for people with SUD. The proven efficacy of SDT in diverse health behaviors suggests its potential to effectively identify the complex factors that impact treatment adherence among PWH and SUD. Our study aims to apply Self Determination Theory to examine the association between SDT and ART adherence among individuals with SUD, utilizing a secondary analysis of a larger mobile health study focused on identifying risky behaviors impacting treatment adherence in PWH and SUD.
2 Materials and methods
2.1 Study design
This cross-sectional study assessed associations between medication adherence among PWH and SUD using survey data collected from March 2019 to June 2019. This study is part of a larger project implementing the Addiction-Comprehensive Health Enhancement Support System (A-CHESS) from March 2019 to March 2020 to enhance support and engagement in care for individuals with HIV and SUD. A-CHESS, developed by the Center for Health Enhancement System Studies at the University of Wisconsin-Madison, offers a comprehensive range of services to address the multifaceted challenges faced by individuals seeking addiction treatment and prevention (39). These services include discussion forums, cognitive behavioral therapy boosters, games, relaxation activities, and educational resources on hepatitis C, HIV, and SUD. Aligned with the components of self-determination theory, A-CHESS aims to enhance self-motivation and wellbeing by catering to the psychological needs of competence, autonomy, and relatedness (40). Our study uses a baseline survey completed by A-CHESS participants.
2.2 Participant recruitment
PWH and SUD were identified by research coordinators at HIV clinics in Wisconsin through provider referrals. To be eligible for participation, individuals had to be 18 years or older, have clinical documentation of HIV infection, and have a history of substance use disorder. SUD history was defined by meeting one or more of the following criteria: a positive result on substance-use screening tests, evidence of substance use within the past year, current involvement in a substance-use treatment program, regular participation in a substance-use disorder-oriented support group (at least monthly), or a lifetime history of problematic drug or alcohol use with recent incarceration.
Patient Consent Statement: All participants provided written informed consent before enrollment in the study. The University of Wisconsin-Madison Health Sciences Institutional Review Board (IRB) provided approval for the study.
2.3 Data collection and measures
The baseline survey for A-CHESS study participants was administered by trained research staff, who conducted the surveys over the phone or in person. The estimated completion time for the survey was 20–30 min, and all data collected by the research staff were securely stored in a Research Electronic Data Capture (REDCap) database (41). Participants received $50 for completing the baseline survey.
The baseline survey administered to the A-CHESS study participants assessed diverse items related to HIV and substance use such as health service utilization, withdrawal symptoms, and risky sexual behaviors. However, only theory-informed relevant measures were utilized for this study. The selection of specific baseline survey measures was guided by the principles of SDT as outlined in the existing literature.
According to SDT, intrinsic motivation is the satisfaction of the three innate basic psychological needs of autonomy, competence, and relatedness (32). When these needs are satisfied, it is assumed that self-determined forms of motivational regulation guide behavior such as medication adherence (32). Autonomy involves having a sense of volition in determining one's behavior (42). Competence consists of the experience of feeling capable and effective when interacting with one's environment (42, 43). Relatedness involves feeling a sense of support and connection with others (42). Guided by these constructs, we selected positive/negative affect, loneliness scale, internalized AIDS-related stigma, and treatment self-regulation as independent measures.
2.3.1 Dependent variable
Our dependent variable of interest is ART adherence, measured using the Four-item Morisky Medication Adherence Scale (MMAS-4) (44). The MMAS-4 is widely used to capture self-reported medication-taking behavior (45). It consists of four items, including questions such as “How often do you forget to take your HIV medications?” and “If you feel worse from taking your HIV medications, how likely are you to stop taking it?” with response options ranging from 1 (indicating a higher frequency or likelihood) to 5 (indicating a lower frequency or likelihood). Each question was assigned one point, resulting in a total score of 20. Adherence was defined as achieving the maximum score of 20 points, while nonadherence scored as any total points below 20 (46). Previous research has shown that the MMAS-4 effectively evaluates ART adherence (47). MMAS-4 has also demonstrated a moderate to high concordance with electronic medication monitoring devices (48). The sensitivity and specificity of the MMAS were reported as 81% and 44%, respectively. We calculated a Cronbach's alpha of 0.9878 for the medication adherence scale.
2.3.2 Independent variables
2.3.2.1 Positive Affect Negative Affect Schedule (PANAS)
To measure individuals' feelings of self and engagement in personally meaningful activities and their sense of constraint and frustration, we utilized the Positive and Negative Affect Schedule (PANAS) (49). The PANAS has strong reported validity with such measures as general distress and dysfunction, identified as feelings that undermine autonomy (50). Negative affect, on the other hand, involves experiencing the world more negatively (51). Participants were asked to respond to the 20 items of the PANAS, where individuals indicate to what extent they feel 20 emotions, including Interested, Distressed, Excited, Upset, Strong, Guilty, or Scared. The emotions are scored using a 5-point Likert scale from 1 point for “Very slightly or not at all” to 5 points for “Extremely.” The final score is derived from the sum of the 10 items on both the positive and negative sides. The reliability and validity of the PANAS scale are moderately good (49, 50). The Cronbach alpha coefficient for the Positive Affect Scale is 0.87; for the Negative Affect Scale is 0.89. We measured negative and positive affect as two distinct continuous measures ranging from 10 to 50 (52).
2.3.2.2 Internalized AIDS-Related Stigma Scale
Internalized stigma refers to the process whereby individuals living with HIV internalize negative societal attitudes and develop self-deprecating beliefs about themselves. We utilized the Internalized AIDS-Related Stigma Scale to measure internalized AIDS-related stigma on a six-item scale, which asks the following questions: (1) It is difficult to tell people about my HIV infection. (2) Being HIV-positive makes me feel dirty. (3) I feel guilty that I am HIV positive. (4) I am ashamed that I am HIV positive. (5) I sometimes feels worthless because I am HIV positive. (6) I hide my HIV status from others (53). Each item offers a binary (yes/no) response, and the total scale score is computed as the sum of the items.
2.3.2.3 The University of California-Los Angeles 3-item Loneliness Scale
We utilized the three-item Loneliness Scale developed by the University of California-Los Angeles (UCLA) to measure social relatedness (54). Loneliness encompasses isolation, disconnection, and a lack of belongingness (55). The scale assesses three aspects of loneliness: feeling left out, isolated, and lacking companionship. Ranging from hardly ever (or never) to some of the time or often, participants are asked to indicate the frequency with which they experience the following: lack of compassion, feeling left out and feeling isolated from others. We calculated a continuous scale score for the loneliness measure, with scores falling within the range of 3–12 (56). Cronbach's alpha reliability coefficient is 0.79.
2.3.2.4 Treatment Self-regulation Questionnaire (TSRQ)
Competence refers to an individual's experience of feeling capable and effective when interacting with their environment. In the context of SDT, competence is one of the three basic psychological needs that, when satisfied, contribute to intrinsic motivation and wellbeing.
We assessed competence using the Treatment Self-regulation Questionnaire (TSRQ) (57). Treatment self-regulation involves regulating and managing one's own behaviors, thoughts, and emotions related to adhering to a treatment regimen (58). It reflects an individual's perceived competence in effectively engaging in self-directed actions to adhere to a behavior. The scale includes six questions about self-regulation related to substance use, such as: “I want to reduce my use because...” with response options like, “I want to take responsibility for my own health,” “I believe this is the best choice for my health,” and “It aligns with my life goals.” By assessing treatment self-regulation, researchers can gain insights into an individual's perceived competence in managing their health-related behaviors and the extent to which they feel capable of adhering to the treatment requirements. On a 5-point Likert scale, participants were asked to rate the self-regulation questions from “Not True” to “Very True.” Each score on the scale is worth one point, and the total points are 30. We calculated a Cronbach alpha of 0.85, indicating good internal consistency.
2.3.2.5 Sociodemographic information
We asked participants to provide information regarding their gender. We collected age as a continuous variable, allowing participants to enter their exact age. We inquired about the highest level of education completed by each participant and categorized it as either having completed college or not. For participant race, we presented options including White, Black or African American, Asian, Native Hawaiian or other Pacific Islander, and American Indian or Alaskan Native. We also allowed participants to enter a different race through an open text field.
2.4 Statistical analysis
Frequency distributions and descriptive statistics were used to summarize the characteristics of A-CHESS participants. All categorical variables are described as numbers and percentages.
Multivariable logistic regression was used to examine the association between the dependent variable, medication adherence, and the primary independent variables of interest (AIDS-related stigma, loneliness, positive/negative affect, treatment self-regulation). Other covariates were selected based on their hypothesized association with the primary covariates of interest and medication adherence. These variables are self-reported and include participants' sociodemographic characteristics. Demographic characteristics reported included age, gender (“male,” “female,” and “transgender”), educational level, and employment status. Odds ratios (OR) and 95% confidence intervals were estimated. A two-sided p < 0.05 was considered statistically significant. All the statistical analyses will be carried out using IBM SPSS Statistics (Version 28.0).
3 Results
3.1 Participant characteristics
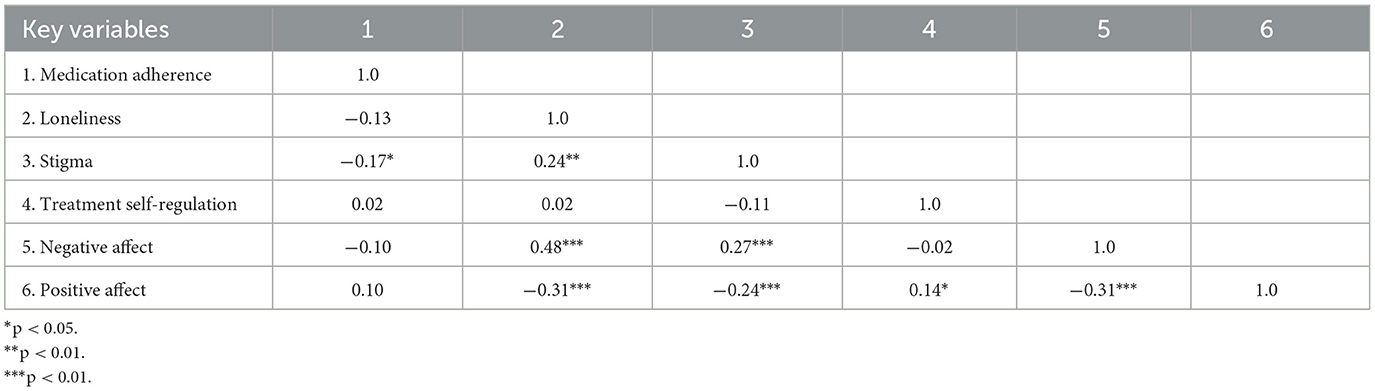
A total of 208 individuals with HIV and SUD were enrolled in the study and completed the baseline survey. Most participants were male (75%) with a mean age of 46.34 (standard deviation 11.26). Among the participants, 65.9% identified as Black/African American. Additionally, 57.2% reported being single, and ~66.8% were unemployed (Table 1). Table 2 shows the correlation between key variables. Several key variables were significantly correlated. Stigma was negatively correlated with medication adherence (r = −0.17, p < 0.05). Additionally, loneliness was positively correlated with negative affect (r = 0.48, p < 0.001) and negatively correlated with positive affect (r = −0.31, p < 0.001).
3.2 Associations of positive and negative affect, treatment self-regulation, stigma, loneliness with medication adherence
Unadjusted and adjusted logistic regression examined the associations between SDT constructs and medication adherence among individuals with HIV and SUD. Adjusted multivariable logistic regression revealed that stigma was significantly associated with medication adherence (adjusted odds ratio = 0.83, 95% CI (0.70, 0.99), p = 0.04]. Higher levels of stigma were associated with reduced odds of medication adherence. However, the analysis did not reveal significant associations between medication adherence and other SDT constructs, including loneliness, negative affect, Treatment Self-Regulation (TSR), and positive affect (Table 3).

Table 3. Associations of positive and negative affect, treatment self-regulation, stigma, loneliness with medication adherence.
The overall model, including all variables, was statistically significant [χ2 (df = 8, N = 208) = 17.19, p = 0.03], indicating that the model can distinguish between adherent respondents and those not adherent to ART. The model explained between 8.2% (Cox and Snell R square) and 10.9% (Nagelkerke R squared) of the variance in adherence and correctly classified 62.9% of cases.
4 Discussion
In this study, we assessed the associations of SDT constructs including stigma, positive affect, negative affect, treatment self-regulation, and loneliness with medication adherence among individuals with HIV and SUD. While affect, treatment self-regulation, and loneliness were not significantly associated with medication adherence, stigma was found to be significantly associated with medication adherence. This finding highlights that stigma may contribute to HIV and substance use on treatment adherence, suggesting the need for targeted interventions to address and reduce stigma-related barriers.
The differential findings between stigma and loneliness suggest that it may be important to consider the unique contributions of different factors related to self-determination theory in understanding medication adherence. While both stigma and loneliness are measures of social relatedness, only stigma showed a significant association with medication adherence. These findings suggest that stigma may have a more noticeable impact on medication adherence than feelings of loneliness or lack of social connectedness. Addressing and reducing stigma could potentially play a role in improving medication adherence among individuals with HIV and substance use disorders, and may be considered as a potential factor when designing interventions.
The results of our study align with the existing literature that has consistently associated stigma to poor adherence to ART among individuals with HIV (59–61). However, it is worth noting that few studies have reported the psychosocial mechanisms through which stigma operates, including factors associated with the development of stigma. One study of PWH shows that internalized stigma creates negative appraisal, leading to anxiety and expectations of negative judgment from others, which likely leads to suboptimal medication adherence (62). Another study showed that a person's perceived severity of stigmatizing attitudes that exist in their community leads to internalized stigma, which lowers medication adherence (63). A review of 38 studies reporting either cross-sectional or prospective analyses of the association of HIV-related stigma to medication adherence found substantial empirical evidence linking stigma to adherence. However, these studies and ours did not explore the multiple domains of stigma (64). These findings call for further research to explore the underlying processes through which stigma influences medication adherence, allowing for more targeted interventions to address stigma-related barriers.
Our study focused solely on internalized AIDS-related stigma and did not investigate the impact of intersectional stigmas. Individuals with HIV and substance use disorders may face multiple stigmatized identities (related to their HIV and SUD diagnosis) that can impact their health-seeking behaviors (65). Future studies should examine the effects of various stigmas, such as HIV-related stigma and substance use disorder-related stigma, to understand their influence on medication adherence.
Our findings shed light on the potential role of autonomy in medication adherence. Although autonomy measures, such as affect, were included in our study, they did not show a significant association with medication adherence. Our findings contrast with previous studies that have reported associations between negative affect and medication adherence (66–68). It is vital to differentiate negative affect from depression and consider the conceptual and theoretical differences between these constructs (69). Our findings differ from studies showing unique positive associations between positive affect and health-related outcomes, including viral load suppression in those living with HIV (70). One study showed that increased positive states of mind mediated the association between perceived social support and improved ART adherence (71). In a study of PWH who use methamphetamine, positive affect was independently associated with ART adherence (15).
Studies examining competence as a contributing factor in medication adherence within the framework of self-determination have been relatively limited. Our study aimed to address this gap by investigating competence in the context of treatment self-regulation related to substance use. While previous research has highlighted the importance of perceived competence as a strong predictor of adherence, these studies have primarily focused on competence in general without explicitly considering its relationship with substance use (72). Our study did not find clear evidence that competence in managing SUD is associated with ART adherence.
Although theoretical frameworks, such as self-determination theory, provide a systematic approach to organizing psychosocial factors and developing tailored intervention messages and strategies for promoting behavioral changes (73), it is important to acknowledge that medication adherence is a complex behavior influenced by various factors beyond a single theory. External factors can significantly impact medication adherence, as such, there may be a need to consider multiple behavioral theories in understanding this phenomenon (29).
While our study focused on self-determination theory as a framework for examining autonomy, competence, and relatedness in relation to medication adherence, other behavioral theories may offer additional insights. Exploring the contributions of alternative theories that account for HIV and SUD, such as Capability, Opportunity, and Motivation–Behavior (74), could provide a more comprehensive understanding of medication adherence in individuals with HIV and substance use disorders. However, to facilitate meaningful comparisons and enhance the overall evidence base, it is crucial to ensure consistency in the operationalization of theories across studies (75).
Our study has certain limitations that need to be acknowledged. First, the cross-sectional nature of the survey prevents us from establishing causality between socio-behavioral factors and medication adherence. While the Morisky Four-item medication adherence scale provides reasonable estimates of medication-taking behavior, it may not serve as an adequate explanatory tool for understanding why patients are not adherent, potentially leading to a weak relationship between the Morisky scale and objective clinical outcome measures (76). The loneliness scale was used as a proxy for social relatedness. Still, it may not fully capture the extent of one's relationship with others and only accounts for one's perception of their relationships. Therefore, this study does not include measurements related to social interaction, including the frequency and intensity of the interactions, which can be beneficial for understanding medication-taking behaviors. Additionally, reliance on self-report recall for measuring adherence, while validated in previous research (77), is susceptible to recall bias. Although patient self-report is one of the critical indirect methods of measuring medication adherence (76), our study could benefit from improved data collection methods, such as integrating innovative technologies like smart pill bottles or medication event monitoring systems, to gather more frequent and objective data on medication adherence.
5 Conclusion
Our study highlights the association between internalized stigma and medication adherence among individuals with HIV and SUD. The findings suggest that interventions focused on medication adherence may benefit from considering the role of stigma when examining medication-taking behaviors. Future research should explore how stigma influences medication adherence and explore the impact of intersectional stigmas for both HIV and substance use. Addressing medication adherence challenges may require a multifaceted and interdisciplinary approach that considers the complex interplay of individual, social, and systemic factors.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by University of Wisconsin-Madison Minimal Risk IRB (Health Sciences). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
AT: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. TV: Writing – review & editing. FY: Formal analysis, Writing – review & editing. OS: Conceptualization, Resources, Supervision, Writing – review & editing. CL: Data curation, Project administration, Writing – review & editing. SD: Data curation, Project administration, Writing – review & editing. RM: Data curation, Project administration, Writing – review & editing. RW: Funding acquisition, Resources, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The research presented in this paper was made possible through grants from the National Institutes of Health (NIH): National Institute of Drug Abuse—1DP2DA042424-01. The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Acknowledgments
The authors wish to acknowledge the participation of all the study participants who contributed to this work. The authors have attained written permission from Dr. Morisky MMAR, LLC, for the use of MMAS-4.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Dunne EM, Cook RL, Ennis N. Non-planning impulsivity but not behavioral impulsivity is associated with HIV medication non-adherence. AIDS Behav. (2019) 23:1297–305. doi: 10.1007/s10461-018-2278-z
2. Byrd KK, Hou JG, Hazen R, Kirkham H, Suzuki S, Clay PG, et al. Antiretroviral adherence level necessary for HIV viral suppression using real-world data. J Acquir Immune Defic Syndr. (2019) 82:245. doi: 10.1097/QAI.0000000000002142
3. Huang Y-M, Pecanac KE, Shiyanbola OO. “Why am i not taking medications?” barriers and facilitators of diabetes medication adherence across different health literacy levels. Qual Health Res. (2020) 30:2331–42. doi: 10.1177/1049732320945296
4. Gross R, Bilker WB, Friedman HM, Strom BL. Effect of adherence to newly initiated antiretroviral therapy on plasma viral load. AIDS. (2001) 15:2109–17. doi: 10.1097/00002030-200111090-00006
5. Barnes E, Zhao J, Giumenta A, Johnson M. The effect of an integrated health system specialty pharmacy on HIV antiretroviral therapy adherence, viral suppression, and CD4 count in an outpatient infectious disease clinic. J Manag Care Spec Pharm. (2020) 26:95–102. doi: 10.18553/jmcp.2020.26.2.95
6. Boussari O, Subtil F, Genolini C, Bastard M, Iwaz J, Fonton N, et al. Impact of variability in adherence to HIV antiretroviral therapy on the immunovirological response and mortality. BMC Med Res Methodol. (2015) 15:10. doi: 10.1186/1471-2288-15-10
7. Mannheimer SB, Matts J, Telzak E, Chesney M, Child C, Wu AW, et al. Quality of life in HIV-infected individuals receiving antiretroviral therapy is related to adherence. AIDS Care. (2005) 17:10–22. doi: 10.1080/09540120412331305098
8. Fumaz CR, Tuldrà A, Ferrer MJ, Paredes R, Bonjoch A, Jou T, et al. Quality of life, emotional status, and adherence of HIV-1-infected patients treated with efavirenz versus protease inhibitor-containing regimens. J Acquir Immune Defic Syndr. (2002) 29:244–53. doi: 10.1097/00126334-200203010-00004
9. Oguntibeju OO. Quality of life of people living with HIV and AIDS and antiretroviral therapy. HIV/AIDS. (2012) 4:117–24. doi: 10.2147/HIV.S32321
10. Harris NS, Johnson AS, Huang Y-LA, Kern D, Fulton P, Smith DK, et al. Vital signs: status of human immunodeficiency virus testing, viral suppression, and HIV preexposure prophylaxis - United States, 2013-2018. MMWR Morb Mortal Wkly Rep. (2019) 68:1117–23. doi: 10.15585/mmwr.mm6848e1
11. Cherenack EM, Enders K, Rupp BM, Seña AC, Psioda M. Daily predictors of art adherence among young men living with HIV who have sex with men: a longitudinal daily diary study. AIDS Behav. (2022) 26:1727–38. doi: 10.1007/s10461-021-03523-2
12. Hendershot CS, Stoner SA, Pantalone DW, Simoni JM. Alcohol use and antiretroviral adherence: review and meta-analysis. J Acquir Immune Defic Syndr. (2009) 52:180–202. doi: 10.1097/QAI.0b013e3181b18b6e
13. Singer M, Bulled N, Ostrach B, Mendenhall E. Syndemics and the biosocial conception of health. Lancet. (2017) 389:941–50. doi: 10.1016/S0140-6736(17)30003-X
14. Meyer JP, Althoff AL, Altice FL. Optimizing care for HIV-infected people who use drugs: evidence-based approaches to overcoming healthcare disparities. Clin Infect Dis. (2013) 57:1309–17. doi: 10.1093/cid/cit427
15. Carrico AW. Substance use and HIV disease progression in the Haart Era: implications for the primary prevention of HIV. Life Sci. (2011) 88:940–7. doi: 10.1016/j.lfs.2010.10.002
16. Feldman MB, Kepler KL, Irvine MK, Thomas JA. Associations between drug use patterns and viral load suppression among HIV-positive individuals who use support services in New York City. Drug Alcohol Depend. (2019) 197:15–21. doi: 10.1016/j.drugalcdep.2018.12.015
17. Barai N, Monroe A, Lesko C, Lau B, Hutton H, Yang C, et al. The association between changes in alcohol use and changes in antiretroviral therapy adherence and viral suppression among women living with HIV. AIDS Behav. (2017) 21:1836–45. doi: 10.1007/s10461-016-1580-x
18. Azar MM, Springer SA, Meyer JP, Altice FL. A systematic review of the impact of alcohol use disorders on HIV treatment outcomes, adherence to antiretroviral therapy and health care utilization. Drug Alcohol Depend. (2010) 112:178–93. doi: 10.1016/j.drugalcdep.2010.06.014
19. Glynn TR, Safren SA, Carrico AW, Mendez NA, Duthely LM, Dale SK, et al. High levels of syndemics and their association with adherence, viral non-suppression, and biobehavioral transmission risk in Miami, a US city with an HIV/AIDS Epidemic. AIDS Behav. (2019) 23:2956–65. doi: 10.1007/s10461-019-02619-0
20. Liddelow C, Mullan B, Novoradovskaya E. Exploring medication adherence amongst australian adults using an extended theory of planned behaviour. Int J Behav Med. (2020) 27:389–99. doi: 10.1007/s12529-020-09862-z
21. Lu J, Zhang N, Mao D, Wang Y, Wang X. How social isolation and loneliness effect medication adherence among elderly with chronic diseases: an integrated theory and validated cross-sectional study. Arch Gerontol Geriatr. (2020) 90:104154. doi: 10.1016/j.archger.2020.104154
22. Rosenstock IM. Historical origins of the health belief model. Health Educ Monogr. (1974) 2:328–35. doi: 10.1177/109019817400200403
23. Bandura A. Social cognitive theory of self-regulation. Organ Behav Hum Decis Process. (1991) 50:248–87. doi: 10.1016/0749-5978(91)90022-L
24. Fishbein M. A theory of reasoned action: some applications and implications. Nebr Symp Motiv. (1980) 27:65–116.
25. Al-Noumani H, Al Omari O, Al-Naamani Z. Role of health literacy, social support, patient-physician relationship, and health-related quality of life in predicting medication adherence in cardiovascular diseases in Oman. Patient Prefer Adherence. (2023) 17:643–52. doi: 10.2147/PPA.S401666
26. Abbas S, Kermode M, Khan MD, Denholm J, Adetunji H, Kane S. What makes people with chronic illnesses discontinue treatment? A practice theory informed analysis of adherence to treatment among patients with drug-resistant tuberculosis in Pakistan. Int J Health Policy Manag. (2023) 12:1–11. doi: 10.34172/ijhpm.2022.6576
27. Xu H-Y, Yu Y-J, Zhang Q-H, Hu H-Y, Li M. Tailored interventions to improve medication adherence for cardiovascular diseases. Front Pharmacol. (2020) 11:510339. doi: 10.3389/fphar.2020.510339
28. Kvarnström K, Westerholm A, Airaksinen M, Liira H. Factors contributing to medication adherence in patients with a chronic condition: a scoping review of qualitative research. Pharmaceutics. (2021) 13:1100. doi: 10.3390/pharmaceutics13071100
29. Munro S, Lewin S, Swart T, Volmink J. A review of health behaviour theories: how useful are these for developing interventions to promote long-term medication adherence for Tb and HIV/AIDS? BMC Public Health. (2007) 7:104. doi: 10.1186/1471-2458-7-104
30. Galárraga O, Genberg BL, Martin RA, Barton Laws M, Wilson IB. Conditional economic incentives to improve HIV treatment adherence: literature review and theoretical considerations. AIDS Behav. (2013) 17:2283–92. doi: 10.1007/s10461-013-0415-2
31. Patrick H, Williams GC. Self-determination theory: its application to health behavior and complementarity with motivational interviewing. Int J Behav Nutr Phys Activity. (2012) 9:18. doi: 10.1186/1479-5868-9-18
32. Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. (2000) 55:68. doi: 10.1037//0003-066X.55.1.68
33. Sheeran P, Wright CE, Avishai A, Villegas ME, Lindemans JW, Klein WMP, et al. Self-determination theory interventions for health behavior change: meta-analysis and meta-analytic structural equation modeling of randomized controlled trials. J Consult Clin Psychol. (2020) 88:726. doi: 10.1037/ccp0000501
34. Caruso A, Grolnick W, Rabner J, Lebel A. Parenting, self-regulation, and treatment adherence in pediatric chronic headache: a self-determination theory perspective. J Health Psychol. (2021) 26:1637–50. doi: 10.1177/1359105319884596
35. Cluesman SR, Gwadz M, Freeman R, Collins LM, Cleland CM, Wilton L, et al. Exploring behavioral intervention components for African American/Black and Latino persons living with HIV with non-suppressed HIV viral load in the United States: a qualitative study. Int J Equity Health. (2023) 22:1–29. doi: 10.1186/s12939-023-01836-3
36. Gwadz M, Cluesman SR, Freeman R, Collins LM, Dorsen C, Hawkins RL, et al. Advancing behavioral interventions for African American/Black and Latino Persons living with HIV using a new conceptual model that integrates critical race theory, harm reduction, and self-determination theory: a qualitative exploratory study. Int J Equity Health. (2022) 21:97. doi: 10.1186/s12939-022-01699-0
37. Sun Y, Zhang Y. A review of theories and models applied in studies of social media addiction and implications for future research. Addict Behav. (2021) 114:106699. doi: 10.1016/j.addbeh.2020.106699
38. Conn VS, Enriquez M, Ruppar TM, Chan KC. Meta-analyses of theory use in medication adherence intervention research. Am J Health Behav. (2016) 40:155–71. doi: 10.5993/AJHB.40.2.1
39. Gustafson DH Sr., Landucci G, McTavish F, Kornfield R, Johnson RA, Mares ML, et al. The effect of bundling medication-assisted treatment for opioid addiction with mhealth: study protocol for a randomized clinical trial. Trials. (2016) 17:592. doi: 10.1186/s13063-016-1726-1
40. Hochstatter KR, Akhtar WZ, Dietz S, Pe-Romashko K, Gustafson DH, Shah DV, et al. Potential influences of the COVID-19 pandemic on drug use and HIV care among people living with HIV and substance use disorders: experience from a pilot mhealth intervention. AIDS Behav. (2021) 25:354–9. doi: 10.1007/s10461-020-02976-1
41. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (redcap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. (2009) 42:377–81. doi: 10.1016/j.jbi.2008.08.010
42. Deci EL, Ryan RM. Self-determination theory: a macrotheory of human motivation, development, and health. Can Psychol. (2008) 49:182. doi: 10.1037/a0012801
43. Church AT, Katigbak MS, Locke KD, Zhang H, Shen J, de Jesús Vargas-Flores J, et al. Need satisfaction and well-being: testing self-determination theory in eight cultures. J Cross Cult Psychol. (2013) 44:507–34. doi: 10.1177/0022022112466590
44. Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. (1986) 24:67–74. doi: 10.1097/00005650-198601000-00007
45. Fayet F, Fan A, Rodere M, Savel C, Pereira B, Soubrier M. Adherence to subcutaneous anti-TNF treatment in chronic inflammatory rheumatism and therapeutic patient education. Patient Prefer Adherence. (2020) 14:363–9. doi: 10.2147/PPA.S240179
46. Guerra C, Conte E, Del Rio AI, Motta J, Moreno Velásquez I, Quintana HK. Medication adherence in hypertensive individuals in PANAMA 2019: a National Cross-Sectional Study. Healthcare. (2022) 10:2244. doi: 10.3390/healthcare10112244
47. Walsh JC, Mandalia S, Gazzard BG. Responses to a 1 month self-report on adherence to antiretroviral therapy are consistent with electronic data and virological treatment outcome. Aids. (2002) 16:269–77. doi: 10.1097/00002030-200201250-00017
48. Shi L, Liu J, Fonseca V, Walker P, Kalsekar A, Pawaskar M. Correlation between adherence rates measured by mems and self-reported questionnaires: a meta-analysis. Health Qual Life Outcomes. (2010) 8:1–7. doi: 10.1186/1477-7525-8-99
49. Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. (1988) 54:1063. doi: 10.1037//0022-3514.54.6.1063
50. Crawford JR, Henry JD. The Positive and Negative Affect Schedule (PANAS): construct validity, measurement properties and normative data in a large non-clinical sample. Br J Clin Psychol. (2004) 43(Pt 3):245–65. doi: 10.1348/0144665031752934
51. Merz EL, Malcarne VL, Roesch SC, Ko CM, Emerson M, Roma VG, et al. Psychometric Properties of Positive and Negative Affect Schedule (PANAS) original and short forms in an african american community sample. J Affect Disord. (2013) 151:942–9. doi: 10.1016/j.jad.2013.08.011
52. Magyar-Moe JL. Worksheet 3.1: the Positive and Negative Affect Schedule (PANAS; Watson Et Al., 1988). In:Magyar-Moe JL, , editor. Therapist's Guide to Positive Psychological Interventions. Amsterdam: Elsevier (2009). doi: 10.1016/B978-0-12-374517-0.00004-8
53. Kalichman SC, Simbayi LC, Cloete A, Mthembu PP, Mkhonta RN, Ginindza T. Measuring aids stigmas in people living with HIV/AIDS: the internalized aids-related stigma scale. AIDS Care. (2009) 21:87–93. doi: 10.1080/09540120802032627
54. Perissinotto CM, Stijacic Cenzer I, Covinsky KE. Loneliness in older persons: a predictor of functional decline and death. Arch Intern Med. (2012) 172:1078–83. doi: 10.1001/archinternmed.2012.1993
55. Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res Aging. (2004) 26:655–72. doi: 10.1177/0164027504268574
56. Rosenberg M, Luetke M, Hensel D, Kianersi S, Fu T-c, Herbenick D. Depression and loneliness during COVID-19 restrictions in the United States, and their associations with frequency of social and sexual connections. medRxiv. (2020) 2020.05.18.20101840. doi: 10.1101/2020.05.18.20101840
57. Brown JM, Miller WR, Lawendowski LA. The self-regulation questionnaire. In:VandeCreek L, Jackson TL, , editors. Innovations in Clinical Practice: A Sourcebook. Sarasota, FL: Professional Resource Press/Professional Resource Exchange (1999). p. 281–92.
58. Hagger MS. Self-Regulation: An Important Construct in Health Psychology Research and Practice. New York, NY: Taylor & Francis (2010). p. 57–65. doi: 10.1080/17437199.2010.503594
59. Vanable PA, Carey MP, Blair DC, Littlewood RA. Impact of HIV-related stigma on health behaviors and psychological adjustment among HIV-positive men and women. AIDS Behav. (2006) 10:473–82. doi: 10.1007/s10461-006-9099-1
60. Green TC, Kershaw T, Lin H, Heimer R, Goulet JL, Kraemer KL, et al. Patterns of drug use and abuse among aging adults with and without HIV: a latent class analysis of a US veteran cohort. Drug Alcohol Depend. (2010) 110:208–20. doi: 10.1016/j.drugalcdep.2010.02.020
61. Zeng C, Li X, Qiao S, Yang X, Shen Z, Zhou Y. Anticipated stigma and medication adherence among people living with HIV: the mechanistic roles of medication support and art self-efficacy. AIDS Care. (2020) 32:1014–22. doi: 10.1080/09540121.2020.1728213
62. Blake Helms C, Turan JM, Atkins G, Kempf M-C, Clay OJ, Raper JL, et al. Interpersonal mechanisms contributing to the association between HIV-related internalized stigma and medication adherence. AIDS Behav. (2017) 21:238–47. doi: 10.1007/s10461-016-1320-2
63. Turan B, Budhwani H, Fazeli PL, Browning WR, Raper JL, Mugavero MJ, et al. How Does stigma affect people living with HIV? The mediating roles of internalized and anticipated HIV stigma in the effects of perceived community stigma on health and psychosocial outcomes. AIDS Behav. (2017) 21:283–91. doi: 10.1007/s10461-016-1451-5
64. Sweeney SM, Vanable PA. The association of HIV-related stigma to HIV medication adherence: a systematic review and synthesis of the literature. AIDS Behav. (2016) 20:29–50. doi: 10.1007/s10461-015-1164-1
65. Yang F, Shah DV, Tahk A, Vjorn O, Dietz S, Pe-Romashko K, et al. Mhealth and social mediation: mobile support among stigmatized people living with HIV and substance use disorder. New Media Soc. (2023) 25:702–31. doi: 10.1177/14614448231158653
66. Kardas P, Lewek P, Matyjaszczyk M. Determinants of patient adherence: a review of systematic reviews. Front Pharmacol. (2013) 4:91. doi: 10.3389/fphar.2013.00091
67. Grenard JL, Munjas BA, Adams JL, Suttorp M, Maglione M, McGlynn EA, et al. Depression and medication adherence in the treatment of chronic diseases in the united states: a meta-analysis. J Gen Intern Med. (2011) 26:1175–82. doi: 10.1007/s11606-011-1704-y
68. Sin NL, DiMatteo MR. Depression treatment enhances adherence to antiretroviral therapy: a meta-analysis. Ann Behav Med. (2014) 47:259–69. doi: 10.1007/s12160-013-9559-6
69. Geisser ME, Roth RS, Theisen ME, Robinson ME, Riley Iii JL. Negative affect, self-report of depressive symptoms, and clinical depression: relation to the experience of chronic pain. Clin J Pain. (2000) 16:110–20. doi: 10.1097/00002508-200006000-00004
70. Wilson TE, Weedon J, Cohen MH, Golub ET, Milam J, Young MA, et al. Positive affect and its association with viral control among women with HIV infection. Health Psychol. (2017) 36:91. doi: 10.1037/hea0000382
71. Gonzalez JS, Penedo FJ, Antoni MH, Durán RE, McPherson-Baker S, Ironson G, et al. Social support, positive states of mind, and hiv treatment adherence in men and women living with HIV/Aids. Health Psychol. (2004) 23:413. doi: 10.1037/0278-6133.23.4.413
72. Kennedy S, Goggin K, Nollen N. Adherence to HIV medications: utility of the theory of self-determination. Cognit Ther Res. (2004) 28:611–28. doi: 10.1023/B:COTR.0000045568.95219.e2
73. Dai M, Calabrese C. Socio-behavioral factors related to prep non-adherence among gay male prep users living in California and New York: a behavioral theory informed approach. J Behav Med. (2022) 45:240–51. doi: 10.1007/s10865-021-00275-1
74. Easthall C, Barnett N. Using theory to explore the determinants of medication adherence; moving away from a one-size-fits-all approach. Pharmacy. (2017) 5:50. doi: 10.3390/pharmacy5030050
75. Moore GF, Evans RE. What theory, for whom and in which context? Reflections on the application of theory in the development and evaluation of complex population health interventions. SSM Popul Health. (2017) 3:132–5. doi: 10.1016/j.ssmph.2016.12.005
76. Tan XI, Patel I, Chang J. Review of the four item morisky medication adherence scale (Mmas-4) and eight item morisky medication adherence scale (MMAS-8). Inov Pharm. (2014) 5:5. doi: 10.24926/iip.v5i3.347
Keywords: HIV, stigma, social isolation, substance use disorder, adherence, mobile health, digital health, antiretroviral therapy
Citation: Tarfa A, Verinumbe T, Yang FE, Shiyanbola OO, Liebert C, Dietz S, Miller R and Westergaard RP (2024) Associations of stigma, loneliness, and treatment self-regulation with HIV medication adherence among individuals with substance use disorder using a mobile health application. Front. Public Health 12:1440807. doi: 10.3389/fpubh.2024.1440807
Received: 30 May 2024; Accepted: 14 October 2024;
Published: 05 November 2024.
Edited by:
Hsun-Yu Chan, National Taiwan Normal University, TaiwanReviewed by:
Timothy N. Crawford, Wright State University, United StatesTingLan Ma, Uniformed Services University of the Health Sciences, United States
Copyright © 2024 Tarfa, Verinumbe, Yang, Shiyanbola, Liebert, Dietz, Miller and Westergaard. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Adati Tarfa, YWRhdGkudGFyZmFAeWFsZS5lZHU=
 Adati Tarfa
Adati Tarfa Tarfa Verinumbe
Tarfa Verinumbe Fan (Ellie) Yang4
Fan (Ellie) Yang4 Sarah Dietz
Sarah Dietz