
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Public Health , 14 August 2024
Sec. Digital Public Health
Volume 12 - 2024 | https://doi.org/10.3389/fpubh.2024.1438981
 Andrea Gentili1†
Andrea Gentili1† Leonardo Villani1†
Leonardo Villani1† Tommaso Osti1*
Tommaso Osti1* Valerio Flavio Corona1
Valerio Flavio Corona1 Angelica Val Gris1
Angelica Val Gris1 Andrea Zaino1
Andrea Zaino1 Michele Bonacquisti1
Michele Bonacquisti1 Lucia De Maio1
Lucia De Maio1 Vincenzo Solimene1
Vincenzo Solimene1 Maria Rosaria Gualano2,3
Maria Rosaria Gualano2,3 Carlo Favaretti3
Carlo Favaretti3 Walter Ricciardi1
Walter Ricciardi1 Fidelia Cascini1
Fidelia Cascini1Background: The World Health Organization defines “infodemic” as the phenomenon of an uncontrolled spread of information in digital and physical environments during a disease outbreak, causing confusion and risk-taking behaviors that can harm health. The aim of this scoping review is to examine international evidence and identify strategies and bottlenecks to tackle health-related fake news.
Methods: We performed a scoping review of the literature from 1 January 2018 to 26 January 2023 on PubMed, Web of Science, and Scopus electronic databases. We also performed a search of grey literature on institutional websites. The research question has been defined according to the PCC (population, concept, and context) mnemonic for constructing research questions in scoping reviews.
Results: The overall research in the scientific databases yielded a total of 5,516 records. After removing duplicates, and screening the titles, abstracts, and full texts, we included 21 articles from scientific literature. Moreover, 5 documents were retrieved from institutional websites. Based on their content, we decided to group recommendations and bottlenecks into five different and well-defined areas of intervention, which we called strategies: “foster proper communication through the collaboration between science and social media companies and users,” “institutional and regulatory interventions,” “check and debunking,” “increase health literacy,” and “surveillance and monitoring through new digital tools.”
Conclusion: The multidisciplinary creation of standardized toolkits that collect recommendations from the literature and institutions can provide a valid solution to limit the infodemic, increasing the health education of both citizens and health professionals, providing the knowledge to recognize fake news, as well as supporting the creation and validation of AI tools aimed at prebunking and debunking.
Health-related communication is increasingly taking place through digital technologies and social media, especially to provide information on disease etiology, prevention, and treatment, as well as for the promotion of healthy behaviors (1–3). Digital communication is widely available and allows people to access a massive quantity of information on various topics, including public health issues, contributing to the dissemination of both true and false news (4). Despite the great potential of social media to improve general knowledge on many health conditions and their outcomes (1, 2), currently, one of the main challenges with it for health professionals and institutions is related to the dissemination of false or misleading health information (4–6). This phenomenon has historically been present for vaccinations and healthcare emergencies (4, 7, 8) and had adverse effects on people (8). Recently, this situation has intensified, especially during the COVID-19 pandemic (9, 10) when a combination of traditional and new containment strategies was applied in many Countries (11, 12). The spread and accessibility of new technologies, such as social media, have allowed this phenomenon to expand rapidly and exponentially (10). Although there is a potential for positive impacts, the ability to reach many people through digital communication is associated with several potential negative factors, such as misinformation, disinformation, and mistrust (13), due to the spread of information by various sources that could be unverified or uncontrolled, generating an infodemic. The term infodemic was first used by the political scientist Rothkopf (14), during the SARS epidemic to describe the phenomenon of the uncontrolled spread of information, speculation, and rumors amplified by the media. Since then, it was used sporadically by healthcare professionals until the COVID-19 pandemic, when it was highlighted by the World Health Organization (WHO). The WHO defined infodemic as a public emergency, linking the term to the massive dissemination of information (including those considered false and misleading) during an infectious disease outbreak (15). During the COVID-19 pandemic, a tremendous increase in misinformation was observed (9, 16), which greatly impacted the world population’s ability to understand and adapt to the public health measures aimed at containing the pandemic (9, 17) and affecting vaccination campaigns (18). In this context, countering this phenomenon is a priority since it directly affects citizens health and patients’ outcomes, influences the usage of healthcare services, and it may produce an avoidable rise in the burden of certain diseases.
The purpose of this scoping review is to examine international evidence and identify gaps related to the actions taken to counteract the infodemic phenomenon. Specifically, we sought evidence on the recommendations provided and the bottlenecks encountered by the decision-makers and the general population to effectively stop this phenomenon and to limit its consequences on public health.
We performed a scoping review of the literature according to the 5-stage methodological framework described by Arksey and O’Malley (19) for scoping reviews. To define the search string and inclusion criteria, we conducted a preliminary investigation on the concepts and definition of infodemic in public health and its consequences at the population level using institutional sources and literature reviews. For the purpose of this study, we decided to use the definition of infodemic as proposed by Rothkopf (14), which defines infodemic as “a few facts, mixed with fear, speculation, and rumor, amplified and relayed swiftly worldwide by modern information technologies, have affected national and international economies, politics and even security in ways that are utterly disproportionate with the root realities” (14). The decision to use this definition is based on the fact that it appears completer and more comprehensive than others (for example, the WHO includes within its definition only those episodes of misinformation and disinformation concerning infectious diseases).
The research question has been defined according to the PCC (population, concept, and context) mnemonic for constructing research questions in scoping reviews (20, 21). A systematic search from 1 January 2018 to 26 January 2023 on PubMed, Web of Science, and Scopus electronic databases has been performed using the query reported in Supplementary Datasheet 1. We have also assessed institutional websites (such as the World Health Organization, European Commission, and European Medicines Agency) repeating the query on the Google search engine and analyzing the first 150 results. The review was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) checklist (22) and results are illustrated in the PRISMA flowchart by Moher and colleagues (Figure 1) (23).
Eligibility criteria of our study have been developed according to the PCC (population, concept, and context) mnemonic for constructing research questions in scoping reviews (Table 1). Our study included peer-reviewed articles written in English that describe structural proposals or recommendations concerning the directions and adoption of interventions or behavior aimed at tackling infodemics on health-related topics. “Health-related topics” was considered any information concerning health risk factors, specific diseases and their characteristics, and any prevention, diagnosis, or treatment topics. We included all types of interventions aimed at supervising, monitoring, preventing, and countering infodemic. In consideration of the research question, opinion pieces, commentaries, and editorials were also considered detectable, so no restrictions have been made based on article type or study design. Instead, research articles and content analyses aimed at estimating the prevalence of mis- or disinformation on health topics without recommendation have been excluded. After the scientific literature search, the identified articles were uploaded on Rayyan software (24), which allowed the removal of all duplicates. Then, each record was screened for title and abstract by at least two researchers independently (LV, AG, AVZ, TO, VFC, AZ, LDM, MB, VS). Then, any disagreement was finally discussed with and resolved by two researchers (LV, AG), when necessary. The pertinent articles with full texts available were then reviewed independently by at least two authors and the articles satisfying the eligibility criteria were included in the scoping review.
The data from the eligible studies has been extracted in a pre-defined Excel sheet and tested independently on five articles by all the researchers involved in the extraction phase. Nine researchers (LV, AG, AVZ, TO, VFC, AZ, LDM, MB, VS), then extracted data from the papers, ensuring that each article was blindly extracted by two researchers. From each eligible article, we extracted the following information:
1. General information (first author, title, year of publication, country);
2. Health-related topics (vaccinations, COVID-19, etc.);
3. Any specific recommendations aimed at countering the infodemic process in a health-related context;
4. Bottlenecks and gaps experienced: defined, for the porpoise of this work, as any type of structural, technical, social, or political challenge hindering the implementation of an intervention to contrast infodemia;
5. Validation process adopted.
The data synthesis process was conducted by four researchers (TO, AVG, LV, AG), employing an iterative process rooted in grounded theory to compare and develop emergent themes (25). Initially, the researchers analyzed the data to identify recommendations aimed at countering infodemic phenomena. These recommendations were then clustered into 24 fundamental statements. This clustering process facilitated the organization of the recommendations into five key strategies, summarized as follows: “foster proper communication through the collaboration between science and social media companies and users.”; “institutional and regulatory interventions”; “check and debunking”; “increase health literacy”; “surveillance and monitoring through new digital tools.”
In addition to recommendations, the bottlenecks identified in each article were also analyzed and clustered. This process resulted in the formulation of 11 fundamental statements, which were then mapped to the corresponding strategies, similar to the recommendations.
The thematic analysis was performed in a double-blind process by the involved researchers.
The overall research in the scientific databases yielded a total of 5,516 records. After removing duplicates, 2,142 articles were screened based on the title and abstract, and 214 based on full text. Following the inclusion and exclusion criteria, we included 21 articles from scientific literature. Moreover, 5 documents were retrieved from institutional websites. All 26 documents selected during the screening contained a clear and recognizable intervention or directive adopted to limit the spread of health-related infodemic. Considering the health topic, the majority of the included articles were related to COVID-19 (n = 15, 57.7%) (26–40), while the others dealt with fake news (41, 42), non-COVID vaccination (43, 44), the control of disinformation in schools (45), risk communication for public health emergencies (46), or with a generic and unclassifiable area of health information (47–51) (Table 2). Data was gathered from a variety of countries, although about 54% of the articles are not placed in any specific geographical setting but produce general considerations (defined as global). The characteristics of the included studies are shown in Table 2.
We identified 23 useful recommendations to counter the spread of the infodemic phenomenon. Based on their content, we decided to group those recommendations and bottlenecks into five different and well-defined areas of intervention, which we called “Strategies” (Figure 2). For each of these areas, key actors involved in that specific action, institutions, scientific community, social network services, online services, and platforms were identified and listed. Table 3 summarizes the recommendations, bottlenecks, and actors related to the five different strategies.
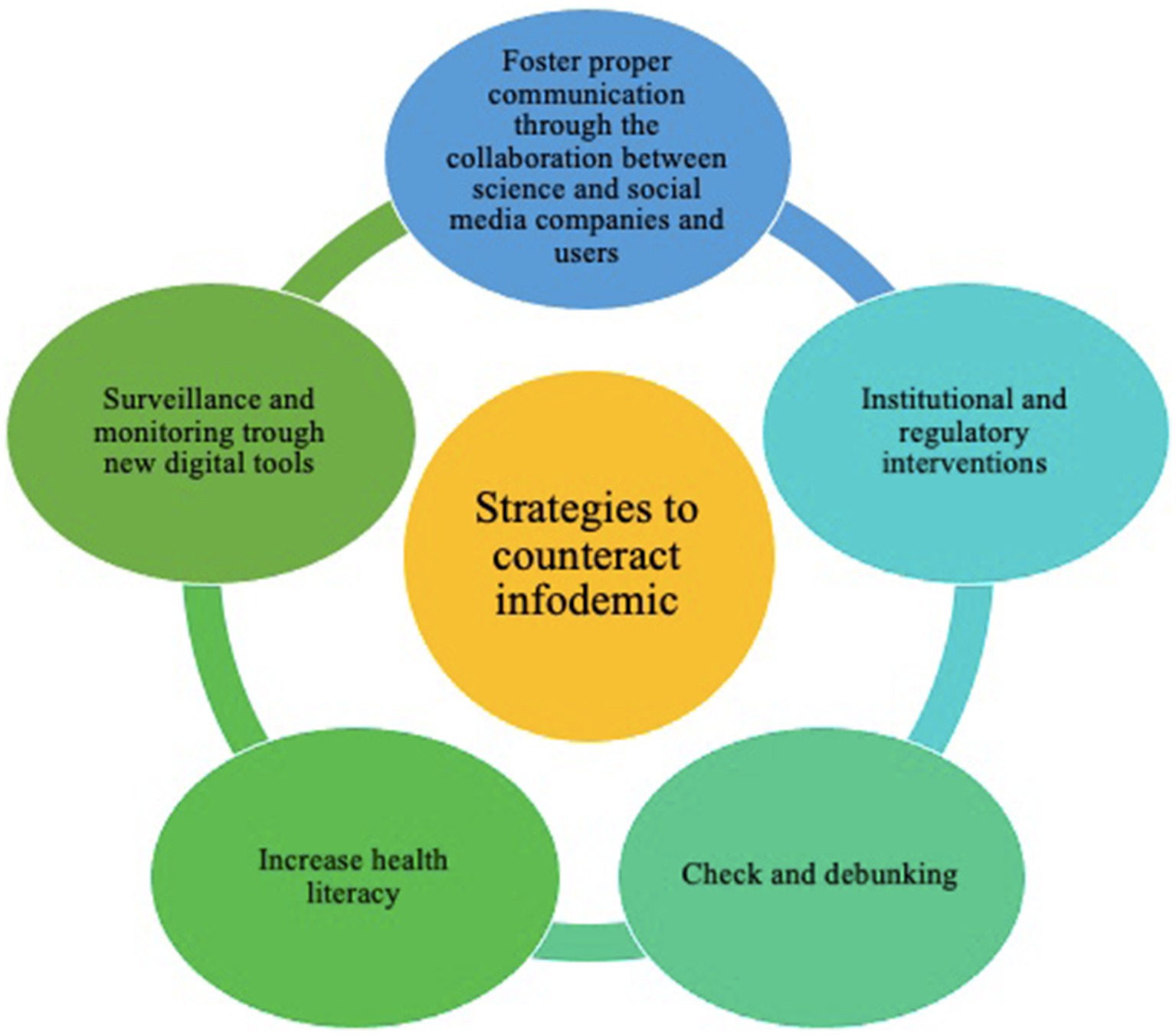
Figure 2. Representation and connections among the different identified strategies to tackle infodemic in public health.
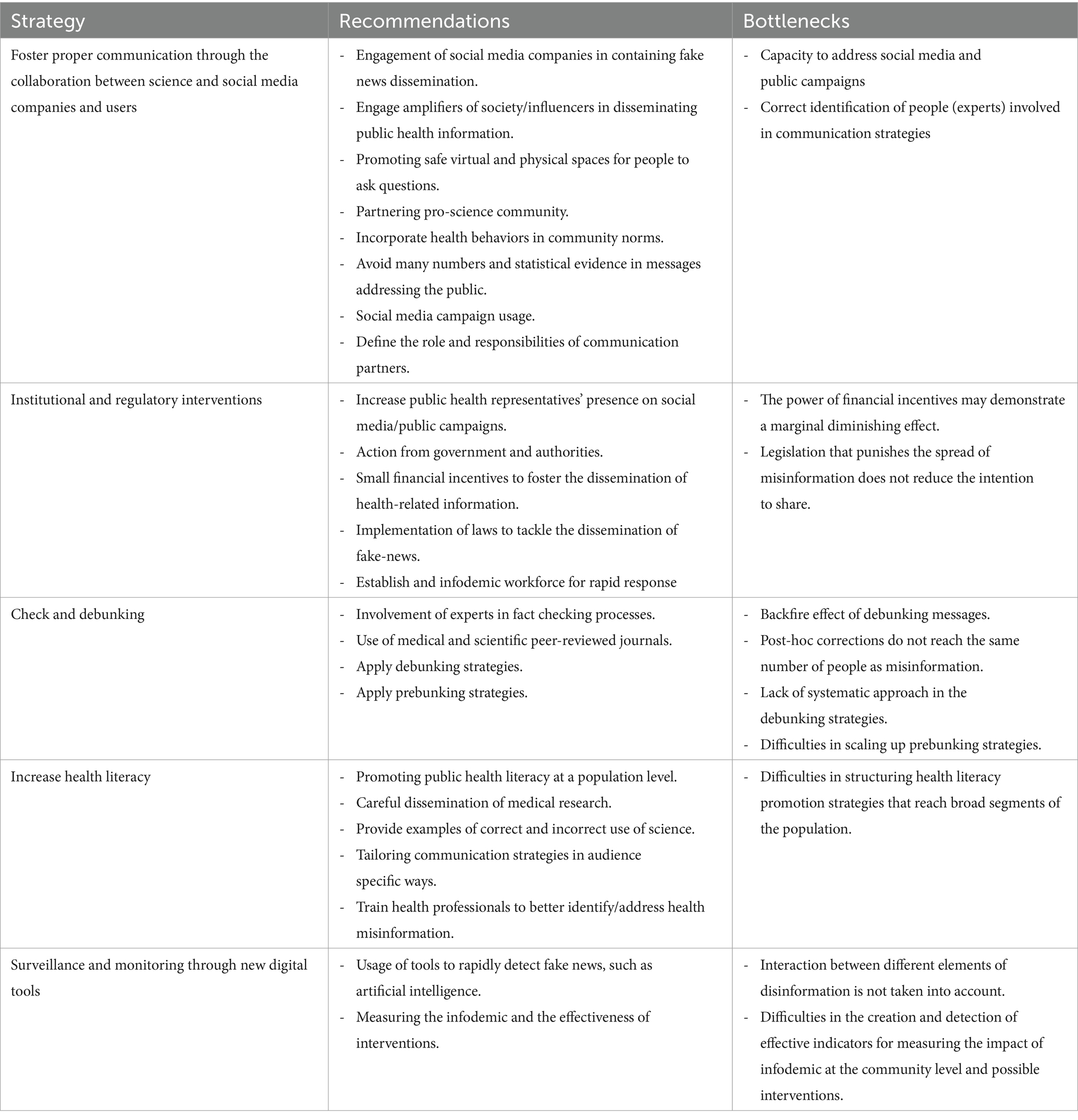
Table 3. Recommendations, bottlenecks and involved actors per strategy that tackles public health infodemic.
Many articles presented one or more recommendations on how to properly communicate and disseminate evidence-based information in the public health sector to avoid the spread of disinformation and misinformation. The most common recommendation was directed at social media companies and the influencers on them (26, 36, 38, 45). Generally, guidance involved requiring stronger actions to contain the dissemination of fake news, and creating a safe, scientifically reliable, and accessible space for people to ask questions and gather public health information through the engagement of experts and influencers in disseminating health-related information (43, 51). In this context, we found that governments and institutions should be strongly involved in countering the dissemination of misinformation through the identification of safe websites, platforms, and communities to respond to the doubts of the citizens as well as defining the role and responsibilities of social media companies and communication partners and require the incorporation of health behaviors in community norms (29, 33, 34, 41, 46). The role of social media, supported by public health experts, relates to the containment of social campaigns that report explicitly erroneous health information, and the engagement of relevant, knowledgeable personalities to communicate proven health information (34, 37, 38, 50). Lastly, the role of the scientific community can be traced back to supporting “pro-science” movements, taking care in building effective science dissemination (43), and avoiding reporting overly technical information to the “lay” public in statistical and scientific terms (31).
The recommendations for regulatory interventions are strictly connected to the dissemination of health-related information. We found that governments and other institutional bodies should aim at increasing public health representatives’ presence on social media/public campaigns (26, 36, 50), promoting financial incentives to foster the dissemination of health-related information (47), fostering the adoption of laws to tackle the dissemination of fake news (26, 40), and establishing a specific workforce for rapid response to infodemics (39). We found bottlenecks related to the marginal effect of financial incentives and the possibility that the legislation that punishes the spread of misinformation would not reduce the intention to share this kind of information (47).
The ability to rapidly identify fake news requires both technical and public health expertise (26, 32, 48, 49), in accordance with institutional plans to effectively curb the spread of fake news. In this context, the central role of the scientific community emerges. The scientific community needs to be involved in fact-checking activities (26, 48) because it has the important responsibility to work on the obstacles to the implementation of these strategies. For example, by supporting the strategies with systematic methodologies for the dissemination of prebunking (provide citizens with the tools to recognize fake news) and debunking (denying the supposed authenticity of a fake news) strategies. However, we found many bottlenecks related to the implementation of these interventions, such as the backfire effect of debunking messages (30, 49) the lack of an existing systematic approach (33, 34), the capacity to reach people for post-hoc corrections (49), and the difficulties in scaling up prebunking strategies (49).
Most of the articles suggested several recommendations to help the target population to discriminate between true and false or misleading health information. To do this, increasing health literacy for both healthcare professionals and citizens, answering questions in a primary care setting, disseminating evidence-based medical research, providing example of correct and incorrect uses of science, and tailoring communication strategies in audience specific ways were recommended (26–28, 30, 32, 37, 40–46, 48–51). Specific training for healthcare professionals is also proposed (39). For example, some articles (22, 26, 33, 38, 47) recommended improving people’s awareness by promoting long-term public health literacy and encouraging citizens to get vaccinated through evidence-based and trustworthy information. Several studies (24, 28, 39, 40, 45) suggested to strengthen the engagement of communities by supporting them with informational materials and promoting the creation of specific courses to detect health misinformation.
Finally, the importance of protecting expression, disseminating factual information, and ensuring strong protections for whistleblowers was highlighted (23, 42, 44). Some articles (26, 39) identified also bottlenecks related to the distrust of the general population towards political and public health institutions and to the difficulty of influencing personal behaviors.
Many articles recommended the development and use of new digital and artificial intelligence technologies to quickly detect the dissemination of fake news (26, 28, 30, 35, 36, 38, 46, 51), as well as the effectiveness of mitigation measures (37, 40). In particular, the interventions were oriented at:
• Using algorithms and manual methods to effectively and quickly identify misinformation and accurately push the content of rumors through algorithms to minimize their impact is an effective methodology (26, 31);
• Using artificial intelligence approaches, such as a deep convolutional neural network (FNDNet), for the automatic detection of fake news (22, 32, 48); and
• Implementing online tools for fact-checking information (24, 41, 47).
Bottlenecks for this strategy were related to the difficulties of distinguishing and categorizing the certainty of source, as well as the difficulties in the creation and detection of effective indicators for measuring the impact of interventions aimed at reducing infodemic at the community level (26, 32).
In this scoping review, we summarized recommendations and bottlenecks aimed to tackle health-related fake news, misinformation, and disinformation. We identified five main strategies: foster proper communication through the collaboration between science and social media companies and users; institutional and regulatory interventions; check and debunking; increase health literacy; and surveillance and monitoring through new digital tools. The infodemic, defined as the dissemination of an enormous amount of information, often false and misleading (14, 15), currently represents a serious threat to public health, with direct effects on the health both of individuals and the community (8). This phenomenon was particularly evident during the COVID-19 pandemic, in which misinformation and disinformation increased doubts and fear among the population, with reduced adherence to containment measures, vaccination, and treatment while simultaneously promoting the spread of the virus (10, 13, 18). Gathering evidence about possible strategies to mitigate and respond to the infodemic is therefore a public health priority, not only for countering infectious diseases epidemics but for numerous public health issues (52). As a striking example, COVID-19 vaccination reluctance was substantially connected with the frequency, diversity, and usage of social media, as well as with media trust and health information literacy (49). Another example can be found in the news: there was a widespread misconception that drinking high-grade alcohol could both clean the body and eradicate SARS-CoV-2. Following this false information, around 800 individuals have tragically passed, 5,876 have been admitted to hospitals, and 60 have become completely blind after using methanol as a coronavirus remedy (38, 49–52).
The dissemination of rumours, stigmas, and conspiracy theories can have an impact on society as a whole, including the healthcare systems (9). Therefore, it is evident that fake news producers have the power to weaken public confidence in authorities and global health organizations (9), and they have been identified by international health organizations, like the WHO, as new dangers to pandemic preparedness and management. As a result, these organizations have advocated for rigorous surveillance and control measures (53).
The infodemic phenomenon primarily stems from the lack of the general public’s ability, inclination, or time to critically examine most of the content they encounter online, communication management and information dissemination techniques are extremely vital in the field of public health (54). Even when the desire to learn more about a subject related to our own medical condition or symptoms is enhanced, determining the reliability of sources and the accuracy of information is a very challenging task (55). In our review, we identified social media and influencers as vectors that can impact and direct information, both positively and negatively (22, 32). For this reason, it is necessary for institutions to promote collaboration between themselves and social media companies, so that they can convey accurate and reliable information, with the certainty that these derive from established and reliable sources (for example, international organizations). Combining the scientific skills of healthcare professionals with the outreach capabilities of influencers is an indispensable starting point for conveying correct and understandable information to the population. During the COVID-19 pandemic, for example, several countries created a partnership with social influencers to promote vaccination campaigns, with encouraging results (53–57).
Promoting the enactment of laws that contrast the spread of fake news is another way to accomplish this goal (34, 42), even if there is still a very limited international experience on this topic. The production of laws and regulations aimed at countering the dissemination of fake news, as well as the creation of task forces aimed at surveillance and control of this phenomenon could represent valid tools.
The review also emphasized the importance of increasing the health literacy, supporting healthy lifestyles and the dissemination of scientific knowledge. It is known that health literacy relates to a person’s capacity to handle the complex demands of health in contemporary society (56), and it is related to social determinants of health (57). Different studies, for example, have shown that the dissemination of health-related information on social media increased many health outcomes (e.g., quality of life) (58, 59). However, while the dissemination of information through the web is a generally positive factor (allowing, in most cases, the consultation of trusted and surveilled information), the risk of spreading misinformation and disinformation (for example, through Google or other search engines) is high. In this context, a strong government action is needed (60). Given this, it is obvious that health literacy does not serve as a magic bullet to eliminate health inequities, which are primarily caused by the unequal distribution of opportunity, resources, and power (57). However, it is possible to maximize the contribution that health literacy makes to addressing the causes and effects of disparities and enabling individuals to have more control over the factors that affect their health (57).
Certainly, close collaboration between the scientific community, social media companies and influencers (as the main internet actors identified by our review), and governments and institutions can enable the creation of tools aimed at countering infodemic by acting on the five strategies we identified. Similar to other health emergencies (61–63), the multidisciplinary creation of standardized toolkits that collect recommendations from the literature and institutions can provide a valid solution to limit the impact of infodemics, increasing the health education of both citizens and health professionals, providing the knowledge to recognize fake news, as well as supporting the creation and validation of AI tools aimed at prebunking and debunking. It is important to remember that monitoring and correcting the spread of false and misleading news is a priority not only for public health, but for all productive sectors that are negatively influenced by this phenomenon financially.
Our study has several limitations. The adoption of Rothkopf’s (14) definition of “infodemic” may not fully capture modern aspects of the phenomenon, particularly those related to infectious diseases. Moreover, the search strategy was limited to English articles in PubMed, Web of Science, and Scopus, potentially excluding relevant studies in other languages or databases. Additionally, only the first 150 Google results for grey literature were reviewed, possibly missing other important sources. Furthermore, the study did not evaluate the effectiveness of the proposed interventions, which limits the practical implications of the findings. Finally, categorizing data into predefined themes might have constrained the analysis, overlooking nuanced aspects of infodemic.
Of course, the implementation of these toolkits can lead to legal and ethical issues (regarding privacy of patients, the control and management of sensitive information, etc.) (64). Nonetheless, ensuring the health of the population is a priority of governments, and ethical and legal issues can be overcome through the transparent and shared creation of tools aimed at fostering proper communication, increasing health literacy, encouraging recognition and reducing the spread of fake news.
AnG: Writing – original draft, Writing – review & editing. LV: Writing – original draft, Writing – review & editing. TO: Writing – original draft, Writing – review & editing. VC: Writing – original draft, Writing – review & editing. AVG: Writing – original draft, Writing – review & editing. AZ: Writing – original draft, Writing – review & editing. MB: Writing – original draft, Writing – review & editing. LM: Writing – original draft, Writing – review & editing. VS: Writing – original draft, Writing – review & editing. MG: Writing – review & editing, Writing – original draft. CF: Writing – review & editing, Writing – original draft. WR: Writing – review & editing, Writing – original draft. FC: Writing – original draft, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Università Cattolica del Sacro Cuore (UCSC) PRIN project “Artificial Intelligence algorithms to track and detect Covid-19 vaccine-related infodemic on social media” (Prot. 2022REWNTE, Cup: J53D23012380008).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1438981/full#supplementary-material
1. Smailhodzic, E, Hooijsma, W, Boonstra, A, and Langley, DJ. Social media use in healthcare: a systematic review of effects on patients and on their relationship with healthcare professionals. BMC Health Serv Res. (2016) 16:442. doi: 10.1186/s12913-016-1691-0
2. Laranjo, L, Arguel, A, Neves, AL, Gallagher, AM, Kaplan, R, Mortimer, N, et al. The influence of social networking sites on health behavior change: a systematic review and meta-analysis. J Am Med Inform Assoc. (2014) 22, 22:243–56. doi: 10.1136/amiajnl-2014-002841
3. Lupton, D . Health promotion in the digital era: a critical commentary. Health Promotion International. (2015). Oxford University Press, 30:174–83.
4. Vosoughi, S, Roy, D, and Aral, S. The spread of true and false news online. Science. (2018) 359:1146–51. doi: 10.1126/science.aap9559
5. Oyeyemi, SO, Gabarron, E, and Wynn, R. Ebola, twitter, and misinformation: a dangerous combination? BMJ 349:g6178 (2014). doi: 10.1136/bmj.g6178
6. Bin, NS, Bhatti, R, and Khan, A. An exploration of how fake news is taking over social media and putting public health at risk. Health Inf Libr J. (2021) 38:143–9. doi: 10.1111/hir.12320
7. Waszak, PM, Kasprzycka-Waszak, W, and Kubanek, A. The spread of medical fake news in social media – the pilot quantitative study. Health Policy Technol. (2018) 7:115–8. doi: 10.1016/j.hlpt.2018.03.002
8. Do Nascimento, IJB, Pizarro, AB, Almeida, JM, Azzopardi-Muscat, N, Gonçalves, MA, Björklund, M, et al. Infodemics and health misinformation: a systematic review of reviews. Bull World Health Organ. (2022) 100:544–61. doi: 10.2471/BLT.21.287654
9. Islam, MS, Sarkar, T, Khan, SH, Kamal, AHM, Murshid Hasan, SM, Kabir, A, et al. COVID-19-related infodemic and its impact on public health: a global social media analysis. Am J Trop Med Hyg. (2020) 103:1621–9. doi: 10.4269/ajtmh.20-0812
10. Kouzy, R, Abi Jaoude, J, Kraitem, A, El Alam, MB, Karam, B, Adib, E, et al. Coronavirus Goes viral: quantifying the COVID-19 misinformation epidemic on twitter. Cureus. (2020) 12:e7255. doi: 10.7759/cureus.7255
11. Cascini, F, Failla, G, Gobbi, C, Pallini, E, Hui, J, Luxi, W, et al. A cross-country comparison of Covid-19 containment measures and their effects on the epidemic curves. BMC Public Health. (2022) 22:1765. doi: 10.1186/s12889-022-14088-7
12. Cascini, F, Causio, FA, Failla, G, Melnyk, A, Puleo, V, Regazzi, L, et al. Emerging issues from a global overview of digital Covid-19 certificate initiatives. Front Public Health. (2021) 9:9. doi: 10.3389/fpubh.2021.744356
13. Jaiswal, J, LoSchiavo, C, and Perlman, DC. Disinformation, Misinformation and inequality-driven mistrust in the time of COVID-19: lessons unlearned from AIDS denialism. AIDS Behav. (2020) 24:2776–80. doi: 10.1007/s10461-020-02925-y
14. Rothkopf, DJ . When the buzz bites Back. The Washington post 11. (2003) (Accessed 2023 Jul 18); B1–B5. Available at: https://moodle2.units.it/pluginfile.php/334512/mod_resource/content/1/Rothkopf%20-%20When%20the%20Buzz%20Bites%20Back.pdf
15. World Health Organization (WHO). Infodemic. (Accessed July 18, 2023). Available at: https://www.who.int/health-topics/infodemic#tab=tab_1
16. Pian, W, Chi, J, and Ma, F. The causes, impacts and countermeasures of COVID-19 “Infodemic”: a systematic review using narrative synthesis. Inf Process Manag. (2021) 58:102713. doi: 10.1016/j.ipm.2021.102713
17. Barua, Z, Barua, S, Aktar, S, Kabir, N, and Li, M. Effects of misinformation on COVID-19 individual responses and recommendations for resilience of disastrous consequences of misinformation. Prog Dis Sci. (2020) 8:100119. doi: 10.1016/j.pdisas.2020.100119
18. Cascini, F, Pantovic, A, Al-Ajlouni, YA, Failla, G, Puleo, V, Melnyk, A, et al. Social media and attitudes towards a COVID-19 vaccination: a systematic review of the literature. EClinicalMedicine. (2022) 48:101454. doi: 10.1016/j.eclinm.2022.101454
19. Arksey, H, and O’Malley, L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. (2005) 8:19–32. doi: 10.1080/1364557032000119616
20. Pollock, D, Peters, MDJ, Khalil, H, McInerney, P, Alexander, L, Tricco, AC, et al. Recommendations for the extraction, analysis, and presentation of results in scoping reviews. JBI Evid Synth. (2023) 21:520–32. doi: 10.11124/JBIES-22-00123
21. Peters, MDJ, Marnie, C, Tricco, AC, Pollock, D, Munn, Z, Alexander, L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. (2020) 18:2119–26. doi: 10.11124/JBIES-20-00167
22. Tricco, AC, Lillie, E, Zarin, W, O’Brien, KK, Colquhoun, H, Levac, D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann. Int. Med. (2018) 169:467–73. doi: 10.7326/M18-0850
23. Moher, D, Liberati, A, Tetzlaff, J, and Altman, DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. (2009) 339:b2535. doi: 10.1136/bmj.b2535
24. Ouzzani, M, Hammady, H, Fedorowicz, Z, and Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. (2016) 5:210. doi: 10.1186/s13643-016-0384-4
25. Strauss, A, and Corbin, J. Grounded theory in practice. Thousand Oaks, CA: SAGE Publications (1997).
26. Aslani, N, Behmanesh, A, Davoodi, F, Garavand, A, and Shams, R. Infodemic challenges during COVID-19 pandemic and the strategies to Deal with them: A review article, vol. 17. Brieflands: Archives of Clinical Infectious Diseases (2022).
27. Pomeranz, JL, and Schwid, AR. Governmental actions to address COVID-19 misinformation. J Public Health Policy. (2021) 42:201–10. doi: 10.1057/s41271-020-00270-x
28. Jafarzadeh Ghoushchi, S, Bonab, SR, and Ghiaci, AM. A decision-making framework for COVID-19 infodemic management strategies evaluation in spherical fuzzy environment. Stoch Env Res Risk A. (2023) 37:1635–48. doi: 10.1007/s00477-022-02355-3
29. Scales, D, Gorman, JM, DiCaprio, P, Hurth, L, Radhakrishnan, M, Windham, S, et al. Community-oriented motivational interviewing (MI): a novel framework extending MI to address COVID-19 vaccine misinformation in online social media platforms. Comput Hum Behav. (2023) 141:107609. doi: 10.1016/j.chb.2022.107609
30. Zhao, S, Hu, S, Zhou, X, Song, S, Wang, Q, Zheng, H, et al. The prevalence, features, influencing factors, and solutions for COVID-19 vaccine misinformation: systematic review. JMIR Public Health Surveill. (2023) 9. doi: 10.2196/40201
31. Song, Y, Wang, S, and Xu, Q. Fighting misinformation on social media: effects of evidence type and presentation mode. Health Educ Res. (2022) 37:185–98. doi: 10.1093/her/cyac011
32. Dash, S, Parray, AA, De Freitas, L, Mithu, MIH, Rahman, MM, Ramasamy, A, et al. Combating the COVID-19 infodemic: a three-level approach for low and middle-income countries. BMJ Glob Health. (2021) 6:4671. doi: 10.1136/bmjgh-2020-004671
33. Scott, J . Managing the infodemic about COVID-19: strategies for clinicians and researchers. Acta Psychiatrica Scandinavica. (2021) 143:377–9. doi: 10.1111/acps.13290
34. Young, LE, Sidnam-Mauch, E, Twyman, M, Wang, L, Xu, JJ, Sargent, M, et al. Disrupting the COVID-19 misinfodemic with network interventions: network solutions for network problems. Am J Public Health. (2021) 111:514–9. doi: 10.2105/AJPH.2020.306063
35. Wang, Z, and Xu, J. An empirical research on how to tackle Infodemic in China: stakeholders and algorithms. Front Polit Sci. (2022) 4:4. doi: 10.3389/fpos.2022.858093
36. Alvarez-Risco, A, Mejia, CR, Delgado-Zegarra, J, Del-Aguila-Arcentales, S, Arce-Esquivel, AA, Valladares-Garrido, MJ, et al. The Peru approach against the COVID-19 infodemic: insights and strategies. Am J Trop Med Hygiene Am Soc Trop Med Hygiene. (2020) 103:583–6. doi: 10.4269/ajtmh.20-0536
37. Tangcharoensathien, V, Calleja, N, Nguyen, T, Purnat, T, D’Agostino, M, Garcia-Saiso, S, et al. Framework for managing the COVID-19 infodemic: methods and results of an online, crowdsourced who technical consultation. J Med Internet Res. (2020) 22:e19659. doi: 10.2196/19659
38. Hernandez, RG, Hagen, L, Walker, KOH, and Lengacher, C. The COVID-19 vaccine social media infodemic: healthcare providers’ missed dose in addressing misinformation and vaccine hesitancy. Hum Vaccin Immunother. (2021) 17:2962–4. doi: 10.1080/21645515.2021.1912551
39. World Health Organization (WHO). WHO policy brief: COVID-19 infodemic management [Internet]. 2022 (Accessed 2023 Jul 18). Available at: https://www.who.int/publications/i/item/WHO-2019-nCoV-Policy_Brief-Infodemic-2022.1
40. World Health Organization (WHO). Managing the COVID-19 infodemic—a call for action. 2020 (Accessed 2023 Jul 18). Available at: https://www.who.int/publications/i/item/9789240010314
41. Goindani, M, and Neville, J. Social reinforcement learning to combat fake news spread. Proceedings of The 35th Uncertainty in Artificial Intelligence Conference, PMLR. (2020) 115:1006–1016.
42. United Nations Development Programme (UNDP). iVerify—AI powered information platform to combat misinformation and hate speech. (2022) (Accessed 2023 Jul 18). Available at: https://www.undp.org/press-releases/undp-tool-fight-misinformation-scales-globally-digital-public-good
43. Steffens, MS, Dunn, AG, Wiley, KE, and Leask, J. How organisations promoting vaccination respond to misinformation on social media: a qualitative investigation. BMC Public Health. (2019) 19:1348. doi: 10.1186/s12889-019-7659-3
44. Whitehead, HS, French, CE, Caldwell, DM, Letley, L, and Mounier-Jack, S. A systematic review of communication interventions for countering vaccine misinformation. Vaccine. (2023) 41:1018–34. doi: 10.1016/j.vaccine.2022.12.059
45. Council of Europe. “Free to speak—safe to learn” democratic schools for all—dealing with propaganda, misinformation and fake news. (2023). (Accessed 2023 Jul 18). Available at: https://www.coe.int/en/web/campaign-free-to-speak-safe-to-learn/dealing-with-propaganda-misinformation-and-fake-news
46. Ofrin, RH, Buddha, N, Htike, M, Bhola, AK, and Bezbaruah, S. Turning commitments into actions: perspectives on emergency preparedness in South-East Asia. WHO South-East Asia J Public Health. (2020) 9:5. doi: 10.4103/2224-3151.282989
47. Au, CH, Ho, KKW, and Chiu, DKW. Stopping healthcare misinformation: the effect of financial incentives and legislation. Health Policy. (2021) 125:627–33. doi: 10.1016/j.healthpol.2021.02.010
48. Benjamin, KA, and McLean, S. Change the medium, change the message: creativity is key to battle misinformation. Adv Physiol Educ. (2022) 46:259–67. doi: 10.1152/advan.00021.2021
49. Roozenbeek, J, and van der Linden, S. How to combat health misinformation: a psychological approach. Am J Health Promot. (2022) 36:569–75. doi: 10.1177/08901171211070958
50. Trethewey, SP . Strategies to combat medical misinformation on social media. Postgrad Med J. (2020) 96:4–6. doi: 10.1136/postgradmedj-2019-137201
51. The Office of the Surgeon General. A community toolkit for addressing health misinformation. (2021) [cited 2023 Jul 18]. Available at: https://www.hhs.gov/sites/default/files/health-misinformation-toolkit-english.pdf
52. Krech, R, Cascini, F, Nagyova, I, and Sweet, M. Dealing with infodemic and health mis/dis-information: new public health organizations’ proposals. Popul Med. (2023) 5:5. doi: 10.18332/popmed/165313
53. Organisation for Economic Co-operation and Development (OECD). Enhancing public trust in COVID-19 vaccination. The role of governments. (2021) (Accessed 2023 Jul 21). Available at: https://www.oecd.org/coronavirus/policy-responses/enhancing-public-trust-in-covid-19-vaccination-the-role-of-governments-eae0ec5a/
54. Buvár, Á, Szilágyi, SF, Balogh, E, and Zsila, Á. COVID-19 messages in sponsored social media posts: the positive impact of influencer-brand fit and prior parasocial interaction. PLoS One. (2022) 17:e0276143. doi: 10.1371/journal.pone.0276143
55. World Health Organization (WHO). Risk communication and community engagement for COVID-19 vaccination implementation tool. (2022). Available at: http://apps.who.int/bookorders.
56. Pöyry, E, Reinikainen, H, and Luoma-Aho, V. The role of social media influencers in public health communication: case COVID-19 pandemic. Int J Strateg Commun. (2022) 16:469–84. doi: 10.1080/1553118X.2022.2042694
57. World Health Organization (WHO). 5000 micro-influencers in Portugal build confidence in COVID-19 vaccination [internet]. (2022) (Accessed 2023 Jul 21). Available at: https://www.who.int/europe/news-room/photo-stories/item/5000-micro-influencers-in-portugal-build-confidence-in-covid-19-vaccination
58. Bonnevie, E, Rosenberg, SD, Kummeth, C, Goldbarg, J, Wartella, E, and Smyser, J. Using social media influencers to increase knowledge and positive attitudes toward the flu vaccine. PLoS One. (2020) 15:e0240828. doi: 10.1371/journal.pone.0240828
59. Hunter, RF, De La Haye, K, Murray, JM, Badham, J, Valente, TW, Clarke, M, et al. Social network interventions for health behaviours and outcomes: A systematic review and meta-analysis. PLoS Med. (2019) 16:2890. doi: 10.1371/journal.pmed.1002890
60. Hyland-Wood, B, Gardner, J, Leask, J, and Ecker, UKH. Toward effective government communication strategies in the era of COVID-19. Humanit Soc Sci Commun. (2021) 8. doi: 10.1057/s41599-020-00701-w
61. World Health Organization (WHO). A risk communication, community engagement and infodemic management toolkit for mpox elimination. (2023). Available at: http://apps.who.int/bookorders
62. Framework and toolkit for infection prevention and control in outbreak preparedness, readiness and response at the health care facility level. Geneva: World Health Organization (2022).
63. Jesudason, T . A new toolkit for WASH programmes. Lancet Infect Dis. (2023) 23:e280. doi: 10.1016/S1473-3099(23)00419-X
Keywords: infodemic, disinformation, communication, misinformation, recommendations, bottlenecks, public health
Citation: Gentili A, Villani L, Osti T, Corona VF, Gris AV, Zaino A, Bonacquisti M, De Maio L, Solimene V, Gualano MR, Favaretti C, Ricciardi W and Cascini F (2024) Strategies and bottlenecks to tackle infodemic in public health: a scoping review. Front. Public Health. 12:1438981. doi: 10.3389/fpubh.2024.1438981
Received: 27 May 2024; Accepted: 05 August 2024;
Published: 14 August 2024.
Edited by:
Katie MacLure, National Health Service Scotland, United KingdomReviewed by:
Michael Wiblishauser, University of Houston Victoria, United StatesCopyright © 2024 Gentili, Villani, Osti, Corona, Gris, Zaino, Bonacquisti, De Maio, Solimene, Gualano, Favaretti, Ricciardi and Cascini. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tommaso Osti, dG9tbWFzby5vc3RpMDFAaWNhdHQuaXQ=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.