- Center for Healthcare Data Modeling, Department of Biostatistics and Epidemiology, School of Public Health, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
Introduction: We analyzed the changes in the top 10 non-communicable diseases (NCDs) over the past century across the World Health Organization (WHO) regions.
Materials and methods: The data were extracted from the Global Burden of Disease (GBD) studies. After we accessed this source, all NCDs were sorted according to their prevalence in 2019, and the 10 most common NCDs were selected. Then, the incidence, prevalence, and mortality rates of these 10 NCDs were compared to the rates in 2000.
Results: Diabetes and kidney disease had the highest increase in incidence (49.4%) and prevalence (28%) in the Eastern Mediterranean region. Substance use disorders had a huge increase (138%) in the mortality rates among women in the Americas region. On the other hand, women in Southeast Asia experienced the greatest decrease in incidence (−19.8%), prevalence (−15.8%), and mortality rates (−66%).
Conclusion: In recent years, nearly all NCDs have shown an increase, yet mortality rates have declined across all regions. Lifestyle can be a major cause of this increase, but advancements in health and medical services, such as screening and treatment, have played a crucial role in improving survival rates.
Introduction
Non-communicable diseases (NCDs) are one of the biggest global health challenges. Before the COVID-19 pandemic, most studies focused on NCDs; incidence, prevalence, and mortality rates were the topics researchers were interested in when discussing these diseases.
Globally, NCDs are increasing each year, accounting for approximately 60% of all causes of death annually. Notably, approximately 25% of these deaths occur before the age of 60 years. Some studies estimate that approximately 52 million deaths occur around the world each year, with significant variations observed from region to region (1–3).
Lifestyle-related, environmental, and genetic factors are the major risk factors associated with NCDs. Additionally, changes in the population pyramid and globalization contribute to an increased prevalence of these risk factors across all regions (2, 4).
Cardiovascular diseases (CVDs), cancers, respiratory diseases, and diabetes are the most important NCDs, accounting for more than 60% of all deaths (2). Approximately a 30% increase in mortality rates was reported for CVDs as NCDs from 1990 to 2016, and the prevalence of this disease increased by approximately 15% in this same period (5). Chronic respiratory diseases, another group of NCDs, have also seen significant increases, with deaths rising by approximately 18% and prevalence by approximately 40% from 1990 to 2017 (6). Neoplasms are a major type of NCDs; it has been estimated that a 100% increase in new cases has occurred from 2008 to 2022 (12.7 to 22.2 million) (7).
During the COVID-19 pandemic, the WHO focused on COVID-19 to control and manage this challenging situation. However, comorbidities such as hypertension, CADs, chronic kidney disease, malignancies, chronic respiratory disease, and diabetes were the leading causes of COVID-19 deaths and significantly contributed to the increase in mortality rates worldwide (8, 9).
The Sustainable Development Goals (SDGs) have been used by the WHO to transform the world. One of these goals is to promote good health and wellbeing, with a reduction in mortality due to major NCDs as its main target. To achieve this target, we need to have an understanding of major NCDs and examine the changes in incidence, prevalence, and mortality rates in recent years. In this study, we analyzed the changes in the top 10 NCDs over the past century across the WHO regions.
Materials and methods
Data source and processing
This study used secondary data from the Institute for Health Metrics and Evaluation. The Global Burden of Diseases (GBD) was a metric that collected and analyzed 87 risk factors and 369 diseases from 204 countries. NCDs were part of this dataset for which incidence, prevalence, and mortality rates were calculated. After access to this source, all the NCDs were sorted according to their prevalence in 2019, and the 10 most common NCDs were selected. These diseases were neurological disorders (Alzheimer’s, Parkinson’s, and multiple sclerosis), musculoskeletal disorders (rheumatoid arthritis), psychological disorders (eating disorder, anorexia nervosa, and bulimia), diabetes and kidney diseases, neoplasms (all cancers), CADs (rheumatic heart disease, ischemic heart disease, stroke, and cardiomyopathy), chronic respiratory diseases (pneumoconiosis, asthma, silicosis, and asbestosis), substance use disorders (alcohol and drug use), skin and subcutaneous diseases (bacterial skin disease and cellulitis), and digestive diseases [chronic liver disease due to viral hepatic or alcohol, peptic ulcer, appendicitis, pancreatic, non-alcoholic fatty liver disease (NAFLD), and non-alcoholic steatohepatitis (NASH)]. The next step was the eradication of these diseases in 2000.
Data analysis
Description of NCDs in 2019
Incidence, prevalence, and mortality rates were the indices used to describe the 10 most common NCDs around the world in 2019. These indices were reported as age-standardized rates per 100,000 populations (95% UI) by sex.
Changes in the 10 most common NCDs from 2000 to 2019
To show the changes in the 10 most common NCDs from 2000 to 2019 by sex and WHO regions, Formula 1 was generated and applied to incidence, prevalence, and mortality rates.
where T0 is the incidence, prevalence, or mortality rates in 2000, and T1 is the incidence, prevalence, or mortality rates in 2019.
Changes in NCDs across the WHO regions
The changes in NCDs (overall) were calculated according to Formula 1. ArcMap GIS 10.1 was used to illustrate the geographical distribution of changes in incidence, prevalence, and mortality rates of NCDs across different WHO regions, based on quartiles (Q1–Q4).
Results
Description of NCDs in 2019
Results among men
The results showed that skin and subcutaneous diseases (63624.2, 95% UI: 61120.3–63624.2), neurological disorders (9737.5, 95% UI: 8714.8–10772.6), and digestive diseases (5174.1, 95% UI: 4728.2–5,654) had the highest incidence among NCDs, but the most prevalence was reported for neurological disorders (30489.4, 95% UI: 28013.6–32984.1), digestive diseases (29095.9, 95% UI: 27493.5–30652.7), and skin and subcutaneous diseases (25356.9, 95% UI: 24612.5–2649.4). CVDs (280.8, 95% UI: 259.2–299.8), neoplasms (157.1, 95% UI: 144.8–168.3), and chronic respiratory diseases (66.7, 95% UI: 60.5–73.1) had the highest mortality rates.
Results among women
The results among women were like those among men. Skin and subcutaneous diseases (61816.9, 95% UI: 59497.7–64330.2), neurological disorders (10784.6, 95% UI: 9731.9–11861.2), and digestive diseases (5733.7, 95% UI: 5237.4–6253.3) had the highest incidence among NCDs. The prevalence of NCDs among women showed that neurological disorders (36401.1, 95% UI: 33706.3–39072.6), skin and subcutaneous diseases (26959.3, 95% UI: 26266.2–27732.4), and digestive diseases (26735.4, 95% UI: 25282.1–28176.7) had the highest prevalence among NCDs.
Like men, CVDs (204, 95% UI: 180.9–221.5), neoplasms (100.5, 95% UI: 92–107.9), and chronic respiratory diseases (39.7, 95% UI: 33.2–44.7) had the highest mortality rates.
Table 1 presents more details.
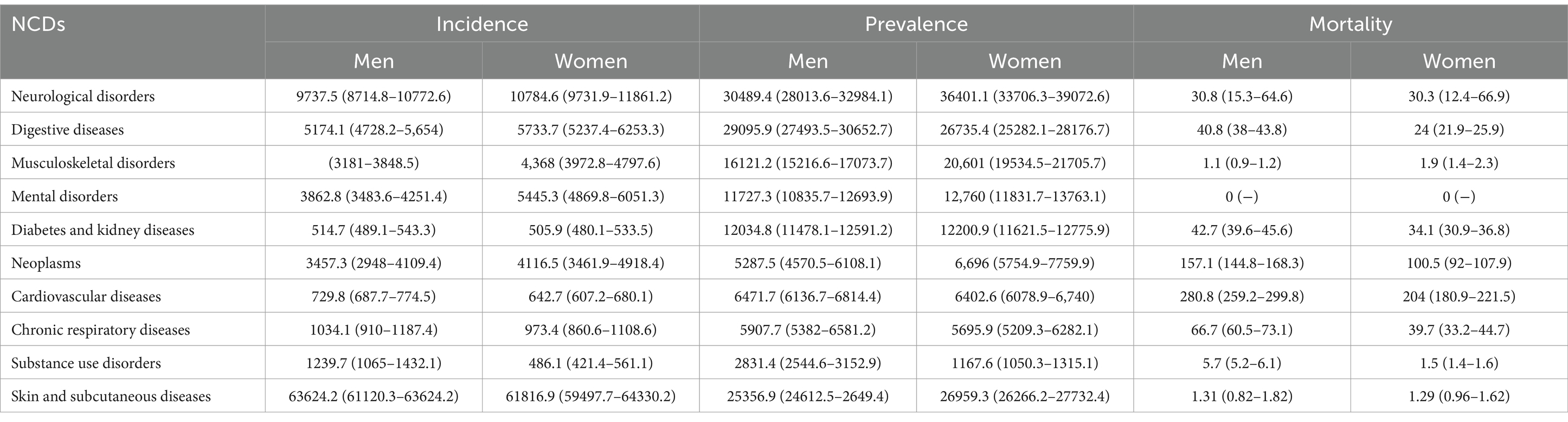
Table 1. Age-standardized rates (ASRs) of incidence, prevalence, and mortality rates of NCDs in the world in 2019.
Changes in the top 10 NCDs from 2000 to 2019
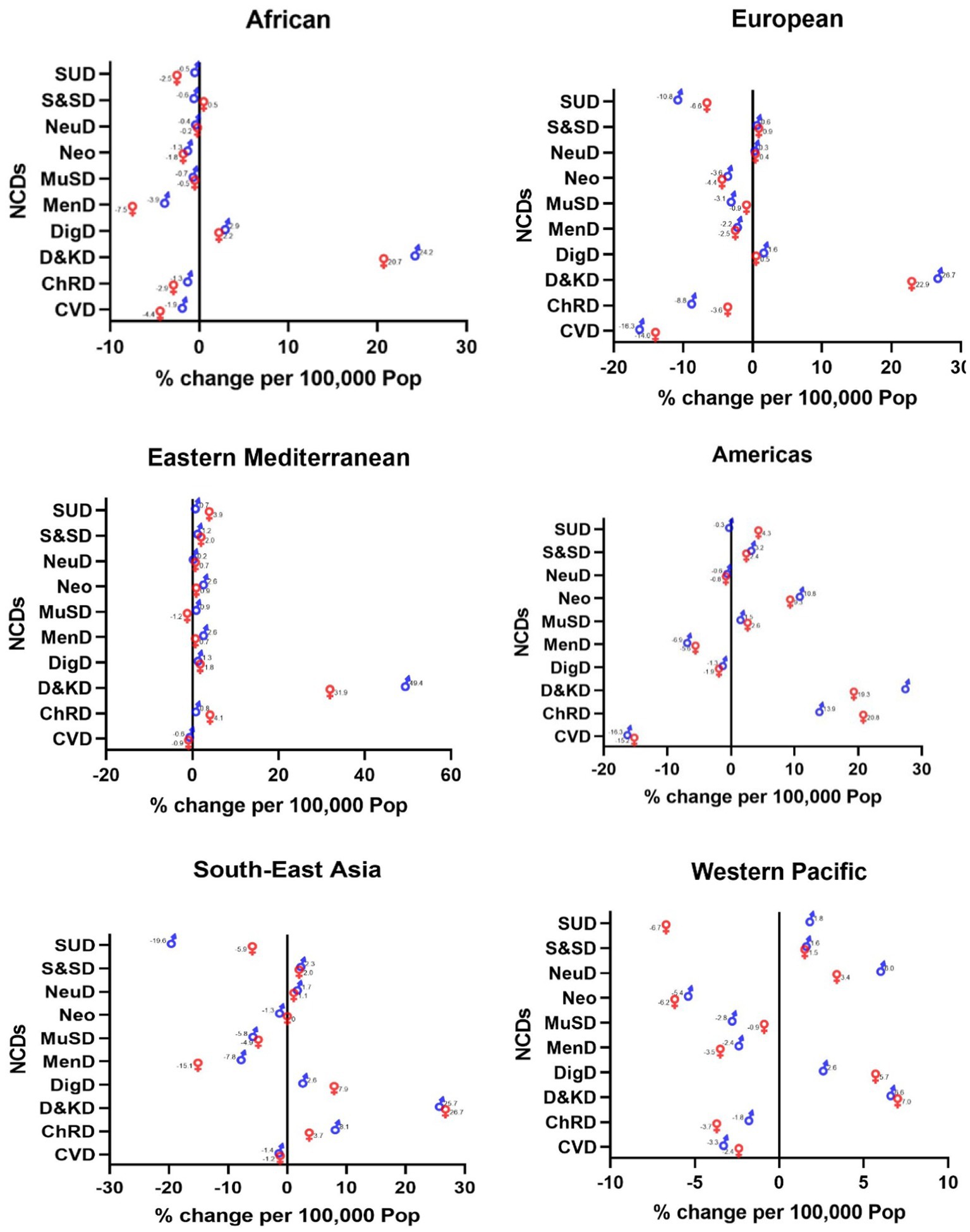
Changes in incidence
Diabetes and kidney diseases are two NCDs that have had the highest increase in recent years. The rise occurred across all WHO regions, and it was the highest among Eastern Mediterranean men (49.4%), American women (28%), European men (26.7%), Southeast Asian women (26.7%), African men (24.2%), and Western Pacific women (7%) (Figure 1).
Substance use disorders among Southeast Asian men (−19.6%), CADs among European men (−16.3%) and American women (−16.3%), mental disorders among African women (−7.5%), substance use disorders among Western Pacific women (−6.7%), and musculoskeletal disorders among Eastern Mediterranean women (−1.2%) had the highest decrease (Figure 1).
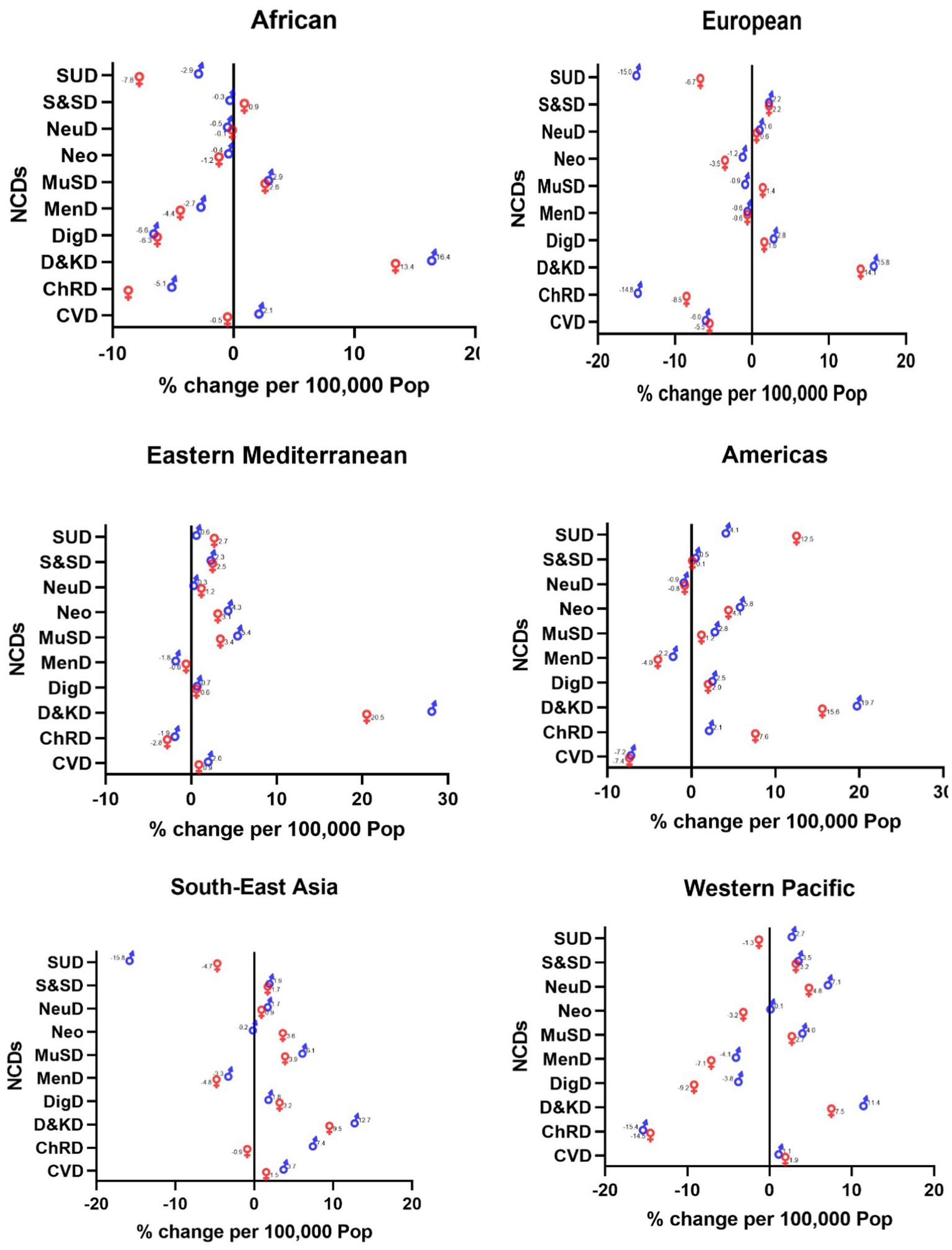
Changes in prevalence
Likewise, the incidence of diabetes and kidney diseases was on the rise among NCDs. Eastern Mediterranean men (28%), American men (19.7%), African men (16.4%), European men (15.8%), Southeast Asian men (12.7%), and Western Pacific men (11.4%) showed the most increase (Figure 2).
Substance use disorders among Southeast Asian women (−15.8%), chronic respiratory diseases among Western Pacific men (−15.4%), substance use disorders among European men (−15%), substance use disorders among African men (−7.8%), CVDs among American women (−7.4%), and chronic respiratory diseases among Eastern Mediterranean men (−2.8%) had the highest decrease (Figure 2).
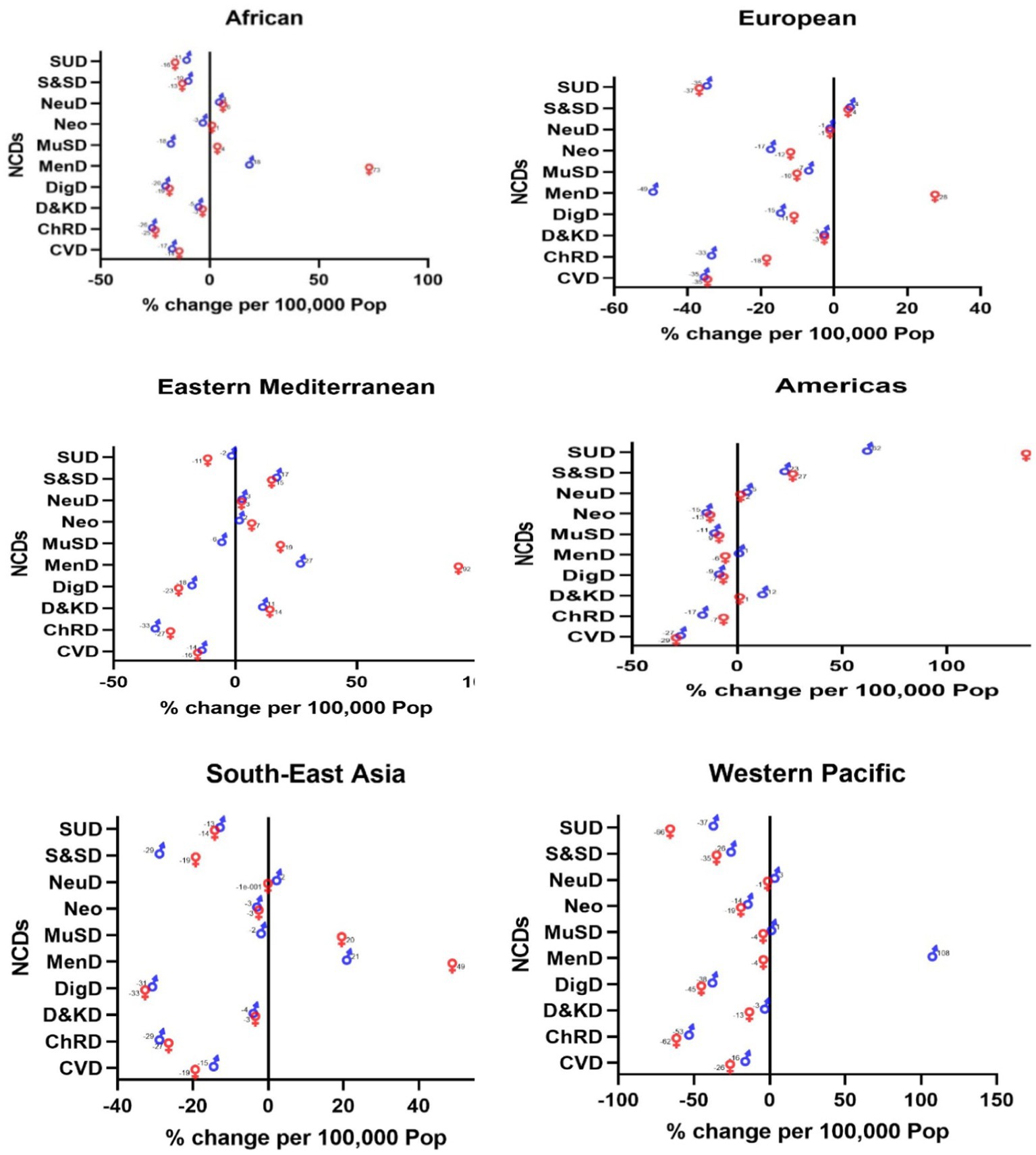
Changes in death
Substance use disorders among American women saw a huge increase of 138%. Mental disorders were the second most significant NCD to increase in recent years; with the following increases reported: Western Pacific women (108%), Eastern Mediterranean women (92%), African women (73%), Southeast Asian women (49%), and European women (28%), (Figure 3).
Contrary to other regions, substance use disorders had the greatest reduction among Southeast Asian women (−66%), and mental disorders had the highest decrease among women in the European region (−49%). Chronic respiratory diseases were another NCD that saw a decrease among Eastern Mediterranean men (−33%). Digestive disease among Southeast Asian women (−33), CVDs among American women (−29%), and chronic respiratory diseases among African men (−26%) decreased as well (Figure 3).
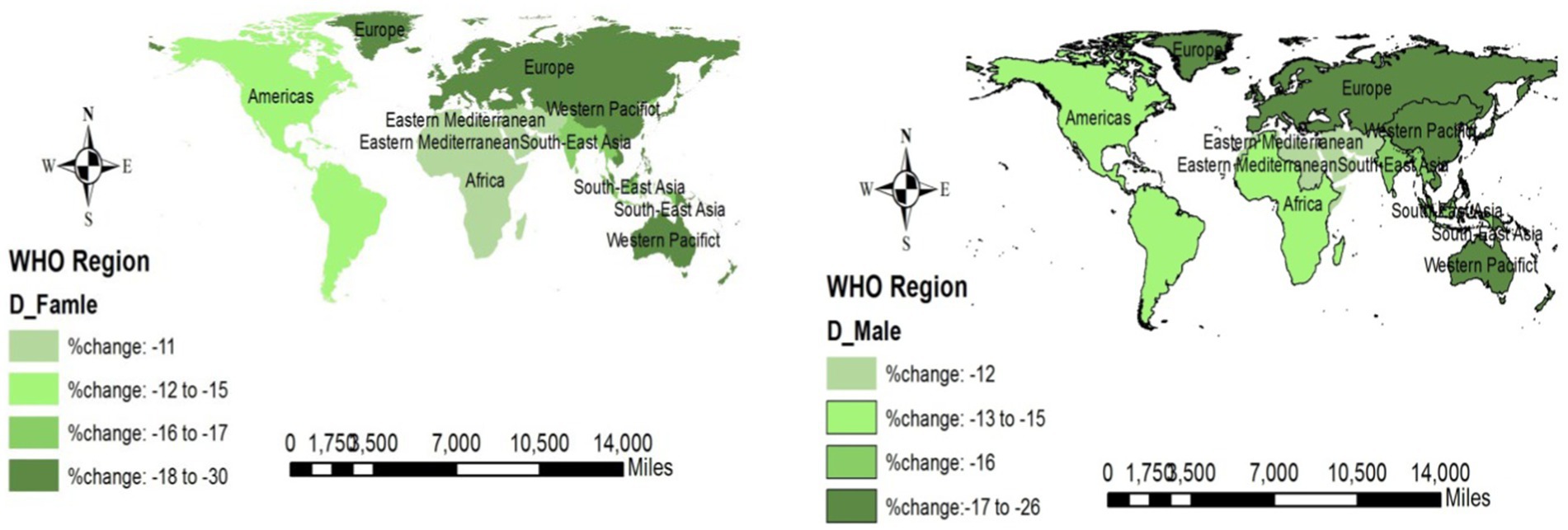
Changes in NCDs across the WHO regions
Changes in incidence
Western Pacific women reported a decreasing change in all NCDs (−0.4%), but this factor increased in American women (1.1–1.2%). Like women, men in the Western Pacific region showed a decreasing change (−0.2%), but this value in the Americas region was on the rise (1.4–1.5%). Figure 4 shows the overall changes in NCDs across the WHO regions.
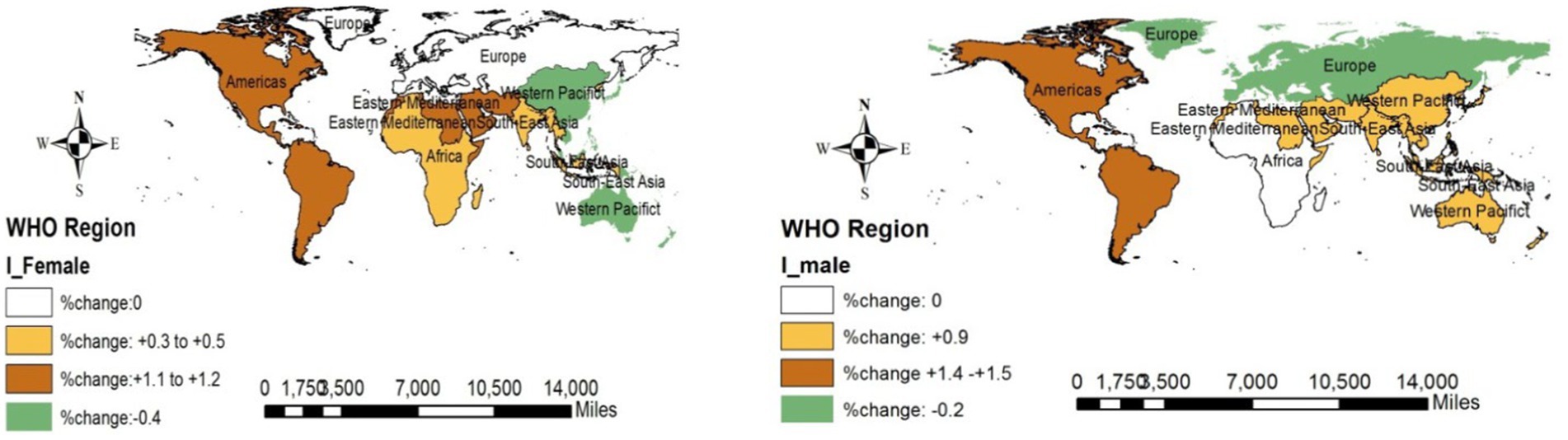
Figure 4. Changes in the incidence of NCDs (overall) across the WHO regions (2019 compared to 2000).
Changes in prevalence
The prevalence of NCDs in all WHO regions was decreasing among men, but across the Americas region, it was increasing (0.5%). Figure 5 depicts the overall NCD changes across the WHO regions.
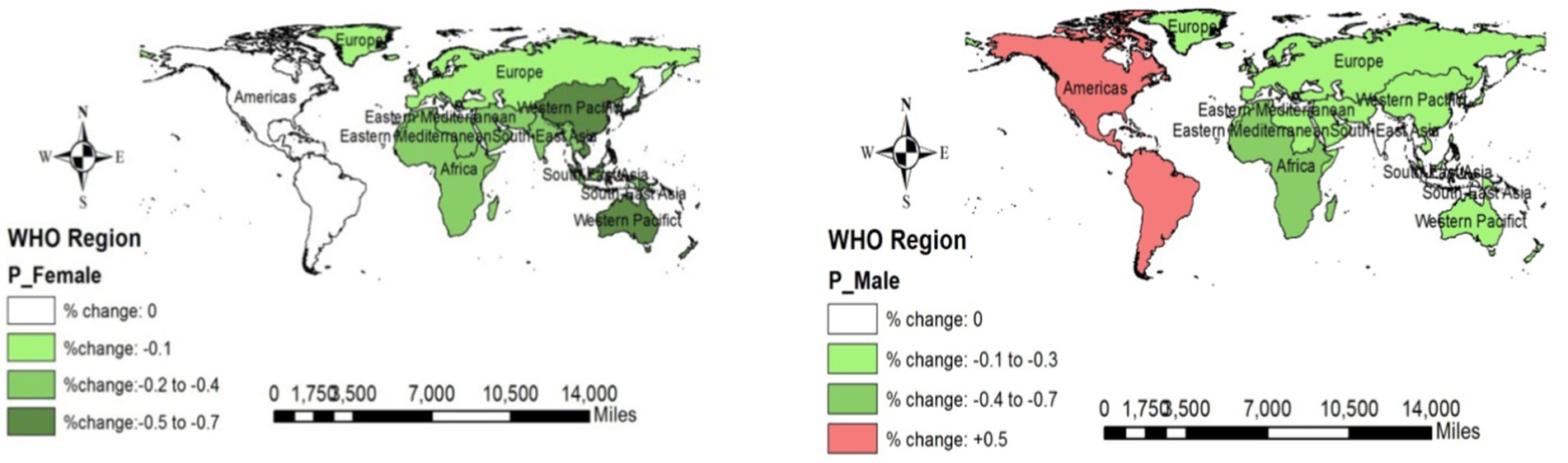
Figure 5. Changes in the prevalence of NCDs (overall) across the WHO regions (2019 compared to 2000).
Changes in mortality rates
Fortunately, the mortality rates of NCDs across all regions and both sexes were decreasing. European and Western Pacific regions reported the highest decrease (−18% to −30% among men and −17 to 26% among women) across the WHO regions. More details are displayed in Figure 6.
Discussion
An overview of the results shows that the incidence of substance use disorders and diabetes and kidney diseases has increased across all WHO regions; the prevalence of mental disorders, diabetes and kidney diseases, and substance use disorders has increased across all WHO regions as well. On the other hand, the mortality rates due to digestive diseases, chronic respiratory diseases, CVDs, and neurological disorders have decreased across all WHO regions. We will clarify the probable causes of the changes in incidence, prevalence, and mortality rates associated with NCDs.
Neurological disorders
The incidence and prevalence of this disease have increased in Europe, Southeast Asia, and the Western Pacific region; this increase was observed in the mortality rates in Africa, the Eastern Mediterranean, and the American region. Aging and the quality of rehabilitation and treatment services could be major causes of this difference among regions. Furthermore, measurement bias because of self-reporting and variations in the definitions of certain neurological disorders, such as dementia, multiple sclerosis, and Parkinson’s disease, could have led to differences in the rates of these diseases across different regions (10, 11).
Digestive diseases
Except for the Americas, the rest of the regions showed an increased incidence of digestive diseases. Contrary to this result, the prevalence of digestive diseases has decreased in the Americas and Eastern Mediterranean region. The mortality rates from digestive diseases in all the regions have declined. A wide range of digestive diseases, including chronic liver disease due to viral hepatitis or alcohol, peptic ulcer, appendicitis, NAFLD, and NASH, are influenced by several risk factors such as lifestyle choices and psychological attributes. One of the reasons for the high prevalence of digestive diseases in the Americas could be lifetime chronic digestive diseases in this region (12, 13).
Musculoskeletal disorders
The incidence and prevalence of this disorder have been growing in recent years. In contrast, the mortality rates have decreased. Aging and a sedentary lifestyle are two major risk factors for these disorders. Additionally, changes in the workforce and the increasing number of workers over 65 years old have played a role in the rise of these conditions during the specified period (14–16). Long-term stress, lack of social support, depression, and sleep problems are the other major risk factors (17).
Mental disorders
The incidence and prevalence of mental disorders have dropped in almost all regions, but mortality rates have risen in almost all regions. Since these results focused on eating disorders while major psychological disorders such as depression, anxiety, autism, and schizophrenia were missed, the major causes of this outcome could be eating disorders, obesity, weight stigma, dieting, and starvation (18, 19).
Diabetes and kidney diseases
The prevalence and incidence of diabetes and kidney diseases have been increasing in recent years worldwide; the Eastern Mediterranean is a region that has witnessed the biggest change. This trend could be expected due to an increase in sedentary lifestyles, food habits, and smoking in almost all countries; on the other hand, since diabetes and kidney diseases are chronic conditions, their prevalence tends to increase every year (20–22).
Neoplasms
The prevalence, incidence, and mortality rates have dropped in almost all regions. This improvement can be attributed to factors such as screening programs, early detection, high education levels, and better health service promotion. However, it is important to note that the situation varies by country; while some cancers are decreasing, others are increasing in different regions. For example, breast cancer is one of the most prevalent neoplasms in many countries, but screening programs have helped in the early detection and contributed to a reduction in mortality rates of this cancer (7, 23–25). Moreover, many countries within a region have varying levels of income, and these differences can affect the prevalence, incidence, and mortality rates of neoplasms in the region (23).
Cardiovascular diseases
The incidence of CVDs has decreased, while the prevalence is still high; mortality rates have decreased in all regions as well. Overall, CVDs have a high prevalence around the world because of lifestyle changes. Nevertheless, CVDs are increasing in developing countries and declining in developed countries. It seems that some countries have achieved the SDGs by reducing CVD deaths, which is a main goal of NCDs (5, 26).
Chronic respiratory diseases
The prevalence and incidence across the Americas, Southeast Asia, and Eastern Mediterranean regions have increased; in contrast, mortality rates have recently decreased. Smoking, household pollution due to solid fuel, occupational and biomass exposures, and urbanization could be causes of these results. In addition, an increase in non-fatal respiratory diseases and health service promotion could have reduced the global mortality rates (27–30).
Substance use disorders
Except for the Americas, in the rest of the regions, incidence, prevalence, and mortality rates have declined. It is difficult to find reasons for the increasing substance use in America, but the legalization of some substances such as cannabis in many states and their normalization may justify these results (31).
Skin and subcutaneous diseases
Cellulitis has increased in the specified years in almost all regions. Several studies showed that the high prevalence of injury, smoking, overweight, and diabetes mellitus could increase cellulitis. These risk factors have risen across all communities, contributing to the rising prevalence of these diseases (27, 28, 32–34).
Conclusion
Almost all NCDs have increased in recent years; despite this, the mortality rates have declined in all. Lifestyle choices can be a major cause of the increase, but health and medical services such as screening and treatment help people survive. On the other hand, according to prevalence, incidence, and disease duration (P = I*D), even if the incidence does not change, the prevalence will remain high for many years. Although survival is preferred, living with a disease for a lifetime may not be the best choice. Prevention is better than cure is a slogan that we should strive toward.
Strengths and limitations
This was a comprehensive study in which the most common NCDs across the WHO regions were assessed. These results have been reported by regions and NCDs and discussed point by point. Additionally, this was an ecological study with the potential for ecological fallacy; thus, we could not attribute the results of a region to every country in that region. In addition, this is just a descriptive study that has not used analytical statistics.
Summary
What is already known on this topic?
It is widely recognized that NCDs are a significant global health concern, responsible for many deaths each year.
What is added by this report?
This research shows the changes in incidence, prevalence, and mortality rates for every NCD across the WHO regions.
What are the implications for public health practice?
Updated information about NCDs could help health policymakers design an appropriate intervention to prevent NCDs by region.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found at: https://vizhub.healthdata.org/gbd-results/.
Ethics statement
This work was conducted on non-human subjects and only used the available aggregated data.
Author contributions
MT: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
I would like to thank the Institute for Health Metrics and Evaluation (IHME) for providing the data for the research.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Jan, S, Laba, T-L, Essue, BM, Gheorghe, A, Muhunthan, J, Engelgau, M, et al. Action to address the household economic burden of non-communicable diseases. Lancet. (2018) 391:2047–58. doi: 10.1016/S0140-6736(18)30323-4
2. Bhandari, GP, Angdembe, MR, Dhimal, M, Neupane, S, and Bhusal, C. State of non-communicable diseases in Nepal. BMC Public Health. (2014) 14:1–9. doi: 10.1186/1471-2458-14-23
3. Boutayeb, A, Boutayeb, S, and Boutayeb, W. Multi-morbidity of non-communicable diseases and equity in WHO eastern Mediterranean countries. Int J Equity Health. (2013) 12:1–13. doi: 10.1186/1475-9276-12-60
4. Maiyaki, MB, and Garbati, MA. The burden of non-communicable diseases in Nigeria; in the context of globalization. Ann Afr Med. (2014) 13:1–10. doi: 10.4103/1596-3519.126933
5. Liu, S, Li, Y, Zeng, X, Wang, H, Yin, P, Wang, L, et al. Burden of cardiovascular diseases in China, 1990-2016: findings from the 2016 global burden of disease study. JAMA Cardiol. (2019) 4:342–52. doi: 10.1001/jamacardio.2019.0295
6. Soriano, JB, Kendrick, PJ, Paulson, KR, Gupta, V, Abrams, EM, Adedoyin, RA, et al. Prevalence and attributable health burden of chronic respiratory diseases, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet Respir Med. (2020) 8:585–96. doi: 10.1016/S2213-2600(20)30105-3
7. Bray, F, Jemal, A, Grey, N, Ferlay, J, and Forman, D. Global cancer transitions according to the human development index (2008–2030): a population-based study. Lancet Oncol. (2012) 13:790–801. doi: 10.1016/S1470-2045(12)70211-5
8. Djaharuddin, I, Munawwarah, S, Nurulita, A, Ilyas, M, Tabri, NA, and Lihawa, N. Comorbidities and mortality in COVID-19 patients. Gac Sanit. (2021) 35:S530–2. doi: 10.1016/j.gaceta.2021.10.085
9. Sanyaolu, A, Okorie, C, Marinkovic, A, Patidar, R, Younis, K, Desai, P, et al. Comorbidity and its impact on patients with COVID-19. SN Compr Clin Med. (2020) 2:1069–76. doi: 10.1007/s42399-020-00363-4
10. Feigin, VL, Nichols, E, Alam, T, Bannick, MS, Beghi, E, Blake, N, et al. Global, regional, and national burden of neurological disorders, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol. (2019) 18:459–80. doi: 10.1016/S1474-4422(18)30499-X
11. Leonardi, M, Steiner, TJ, Scher, AT, and Lipton, RB. The global burden of migraine: measuring disability in headache disorders with WHO's classification of functioning, disability and health (ICF). J Headache Pain. (2005) 6:429–40. doi: 10.1007/s10194-005-0252-4
12. Stanghellini, V, Chan, FK, Hasler, WL, Malagelada, JR, Suzuki, H, Tack, J, et al. Gastroduodenal disorders. Gastroenterology. (2016) 150:1380–92. doi: 10.1053/j.gastro.2016.02.011
13. Lewis, JR, and Mohanty, SR. Non-alcoholic fatty liver disease: a review and update. Dig Dis Sci. (2010) 55:560–78. doi: 10.1007/s10620-009-1081-0
14. Vos, T, Barber, RM, Bell, B, Bertozzi-Villa, A, Biryukov, S, Bolliger, I, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the global burden of disease study 2013. Lancet. (2015) 386:743–800. doi: 10.1016/S0140-6736(15)60692-4
15. Davis, K, Dunning, K, Jewell, G, and Lockey, J. Cost and disability trends of work-related musculoskeletal disorders in Ohio. Occup Med. (2014) 64:608–15. doi: 10.1093/occmed/kqu126
16. Wang, K, Xing, D, Dong, S, and Lin, J. The global state of research in non-surgical treatment of knee osteoarthritis: a bibliometric and visualized study. BMC Musculoskelet Disord. (2019) 20:1–10. doi: 10.1186/s12891-019-2804-9
17. Kazeminasab, S, Nejadghaderi, SA, Amiri, P, Pourfathi, H, Araj-Khodaei, M, Sullman, MJ, et al. Neck pain: global epidemiology, trends and risk factors. BMC Musculoskelet Disord. (2022) 23:1–13. doi: 10.1186/s12891-021-04957-4
18. Hilbert, A, Pike, KM, Goldschmidt, AB, Wilfley, DE, Fairburn, CG, Dohm, F-A, et al. Risk factors across the eating disorders. Psychiatry Res. (2014) 220:500–6. doi: 10.1016/j.psychres.2014.05.054
19. Striegel-Moore, RH, and Bulik, CM. Risk factors for eating disorders. Am Psychol. (2007) 62:181. doi: 10.1037/0003-066X.62.3.181
20. Koye, DN, Magliano, DJ, Nelson, RG, and Pavkov, ME. The global epidemiology of diabetes and kidney disease. Adv Chronic Kidney Dis. (2018) 25:121–32. doi: 10.1053/j.ackd.2017.10.011
21. Gheith, O, Farouk, N, Nampoory, N, Halim, MA, and Al-Otaibi, T. Diabetic kidney disease: world wide difference of prevalence and risk factors. J Nephropharmacol. (2016) 5:49.
22. Harding, JL, Pavkov, ME, Magliano, DJ, Shaw, JE, and Gregg, EW. Global trends in diabetes complications: a review of current evidence. Diabetologia. (2019) 62:3–16. doi: 10.1007/s00125-018-4711-2
23. Malvezzi, M, Carioli, G, Bertuccio, P, Boffetta, P, Levi, F, La Vecchia, C, et al. European cancer mortality predictions for the year 2019 with focus on breast cancer. Ann Oncol. (2019) 30:781–7. doi: 10.1093/annonc/mdz051
24. Chatenoud, L, Bertuccio, P, Bosetti, C, Malvezzi, M, Levi, F, Negri, E, et al. Trends in mortality from major cancers in the Americas: 1980–2010. Ann Oncol. (2014) 25:1843–53. doi: 10.1093/annonc/mdu206
25. Fitzmaurice, C, Dicker, D, Pain, A, Hamavid, H, Moradi-Lakeh, M, Mac Intyre, MF, et al. The global burden of cancer 2013. JAMA Oncol. (2015) 1:505–27. doi: 10.1001/jamaoncol.2015.0735
26. Gupta, R, Mohan, I, and Narula, J. Trends in coronary heart disease epidemiology in India. Ann Glob Health. (2016) 82:307–15. doi: 10.1016/j.aogh.2016.04.002
27. Chlebicki, MP, and Oh, CC. Recurrent cellulitis: risk factors, etiology, pathogenesis and treatment. Curr Infect Dis Rep. (2014) 16:1–8. doi: 10.1007/s11908-014-0422-0
28. Cannon, J, Dyer, J, Carapetis, J, and Manning, L. Epidemiology and risk factors for recurrent severe lower limb cellulitis: a longitudinal cohort study. Clin Microbiol Infect. (2018) 24:1084–8. doi: 10.1016/j.cmi.2018.01.023
29. Simonsen, SE, Van Orman, E, Hatch, B, Jones, S, Gren, L, Hegmann, K, et al. Cellulitis incidence in a defined population. Epidemiol Infect. (2006) 134:293–9. doi: 10.1017/S095026880500484X
30. Andersen, PK, Geskus, RB, de Witte, T, and Putter, H. Competing risks in epidemiology: possibilities and pitfalls. Int J Epidemiol. (2012) 41:861–70. doi: 10.1093/ije/dyr213
31. Pathak, S, Deruiter, J, Ramesh, S, Govindarajulu, M, Almaghrabi, M, Nadar, R, et al. The legality of use and consumption of cannabis (marijuana) in the United States of America. Singapore: Cannabis/Marijuana for Healthcare, Springer; (2022). 113–130.
32. Vignes, S, Poizeau, F, and Dupuy, A. Cellulitis risk factors for patients with primary or secondary lymphedema. J Vasc Surg Venous Lymphat Disord. (2022) 10:179–85. e1. doi: 10.1016/j.jvsv.2021.04.009
33. Halilovic, J, Heintz, BH, and Brown, J. Risk factors for clinical failure in patients hospitalized with cellulitis and cutaneous abscess. J Infect. (2012) 65:128–34. doi: 10.1016/j.jinf.2012.03.013
Keywords: neurologic disorder, cancer, cardiovascular disease, diabetes mellitus, substance-related disorder, musculoskeletal diseases, global health
Citation: Taheri Soodejani M (2024) Non-communicable diseases in the world over the past century: a secondary data analysis. Front. Public Health. 12:1436236. doi: 10.3389/fpubh.2024.1436236
Edited by:
Philimon N. Gona, University of Massachusetts Boston, United StatesReviewed by:
Nilesh Chandrakant Gawde, Tata Institute of Social Sciences, IndiaSatabdi Mitra, KPC Medical College and Hospital, India
Copyright © 2024 Taheri Soodejani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Moslem Taheri Soodejani, bW9zbGVtLnRhaGVyaTIwMDlAeWFob28uY29t
 Moslem Taheri Soodejani
Moslem Taheri Soodejani