
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Public Health , 30 January 2025
Sec. Environmental Health and Exposome
Volume 12 - 2024 | https://doi.org/10.3389/fpubh.2024.1434611
Purpose: This study comprehensively examined the correlation between unclean cooking fuels (UCF) and ocular health, covering diverse eye conditions such as cataracts, visual impairments, and ocular discomfort.
Methods: According to MOOSE and PRISMA guidelines, a meta-analysis and systematic review was conducted on 28 studies from 3 databases. Literature quality was assessed using the Newcastle-Ottawa Scale. Heterogeneity among articles was gaged with the I2 statistic, sensitivity analysis used ‘leave-one-out test’, and publication bias was evaluated using Egger, Begg tests, and funnel plot analysis.
Results: The study evidenced a significant association between UCF exposure and cataracts [OR 2.29, 95% CI (1.24, 4.23)], visual impairments [OR 1.70, 95% CI (1.45, 2.00)], and eye diseases/symptoms [OR 2.03, 95% CI (1.25, 3.29)]. However, no correlation was found between UCF exposure and glaucoma or elevated intraocular pressure [OR 0.96, 95% CI (0.84, 1.10), n = 2]. Subgroup analysis revealed that UCF cooking had an impact on nuclear cataracts [OR 1.98, 95% CI (1.67, 2.33), n = 4]. But not on cortical cataracts [OR 1.25, 95% CI (0.98, 1.60), n = 3]. Additionally, UCF exposure was linked to severe visual impairments like night blindness [OR 2.03, 95% CI (1.00, 4.96)], blindness [OR 1.43, 95% CI (1.32, 1.55)], and specific ocular symptoms such as tearing while cooking (OR = 3.20), eye irritation (OR = 2.58), and red eyes (OR = 2.03).
Conclusion: UCF cooking had significant impact on ocular health, notably on eye symptoms, cataracts, and visual impairments. UCF exposure presented demographic inequalities in cataract prevalence, while eye symptoms can serve as a reliable self-assessment of UCF exposure.
Visual impairment was one of the major barriers to unleashing human potential, significantly reducing productivity and educational attainment (1). In 2020, the prevalence of visual impairment reached 15,841 per 100,000 (with a range of 12,790.88 to 19,596.32) (2), resulting in a global productivity loss of up to $410.7 billion (1). Cataracts were significant components of visual impairment. According to the Global Burden of Disease (GBD) study, cataracts caused by household air pollution (HAP) accounted for 29.81% of the global disease burden, increasing to 50.72% in low-income regions (2), highlighting substantial health inequalities. The primary cause of HAP was the burning of unclean fuels (UCF), with approximately 2.6 billion people worldwide using these fuels for cooking (3). In 2019, nearly 2.3 million premature deaths were attributed to HAP (4), and the use of such fuels was notably higher in low-income areas compared to other regions (2). Therefore, for low-income populations, the preventive measure of improving fuel quality and cooking appliances may be more cost-effective compared to relying on cataract surgery after its onset.
Research indicated that the UCF exposure could lead to eye symptoms (5), including eye pain, blurred vision, redness, and tear while cooking (TWC), diminishing quality of life. Although these relatively common eye symptoms had not received as much research attention as visual impairment, they played an important role in the early indication of vision problems (6), and could serve as key marker for identifying specific populations at higher health risk due to HAP, especially after changes in cooking environments. Additionally, air pollution affected various chronic diseases (7–9), and using eye health as an assessment criterion might help raise awareness about UCF exposure.
The impact of UCF exposure on eye health has often been neglected by researchers in the past (10, 11). Moreover, the existing clinical studies did not comprehensively cover the types of fuels (12, 13) and eye health burden (14, 15), resulting in a lack of thorough assessment. Additionally, the conclusions drawn from different studies were contradictory (14, 16), highlighting the urgent need for an evidence-based medicine to claim the potential hazards of UCF on eye health.
Therefore, we conducted this systematic review and meta-analysis. Our study encompassed cataracts, visual impairments, ocular discomfort, glaucoma, and conjunctival diseases, while also performing subgroup analyses on fuel types, cataract subtypes, demographic characteristics. The significance of this research was identifying gaps in the current studies, exploring evidence related to health inequalities, and establishing effective health evaluation indicators.
Although this meta-analysis was not formally registered, we diligently adhered to the Meta-analysis Of Observational Studies in Epidemiology (MOOSE) guidelines (17) and the Preferred Reporting Items for Systematic and Meta-analysis Protocols (PRISMA) guidelines (18) throughout the entire process.
We searched all literature in the PubMed, Embase and Web of Science databases from their inception until November 10, 2023. Supplementary Table S1 provided an extensive list of detailed search terms and comprehensive information on the search strategy used in this study. No requirements were set for journal type. Studies must be published as original articles in English, encompassing clinical research types such as case–control studies, cross-sectional studies, cohort studies, case series studies, and randomized controlled trials. Conference abstracts, letters, books, review will be excluded. Additionally, studies lacking full-text access or available data will be excluded. All documents were imported into Endnote 20.
UCF encompassed biomass fuels, solid fuels, wood, crop residue, coal, animal dung, kerosene, straw and charcoal. Clean fuel consisted of natural gas, biogas, liquefied petroleum gas (LPG), electricity, and propane. Ocular outcomes under study included cataracts, visual impairments, myopia, hyperopia, blindness, night blindness, eye discomfort, tearing while cooking (TWC), eye irritation and red eyes.
Using Endnote X20 software, duplicate and unqualified research types of articles were removed. Two reviewers (S.C and Y.T) independently reviewed the remaining articles and excluded some articles that were obviously irrelevant to the research subject or animal experiment articles by title and abstract. For potentially relevant articles, the reviewers confirmed the articles that could be included in the study by intensively reading the full text. Finally, according to whether the research data could be converted into Odds ratio (OR), the literature was divided into included group or excluded group. Specific steps were shown in Figure 1. For ambiguous articles, the decision of whether to include the article was made after discussion with a third person (S.X). The original data of the pictures in the article through WebPlotDigitizer 4.5 software (19). The data extracted by this software will be specifically labeled in the figures.
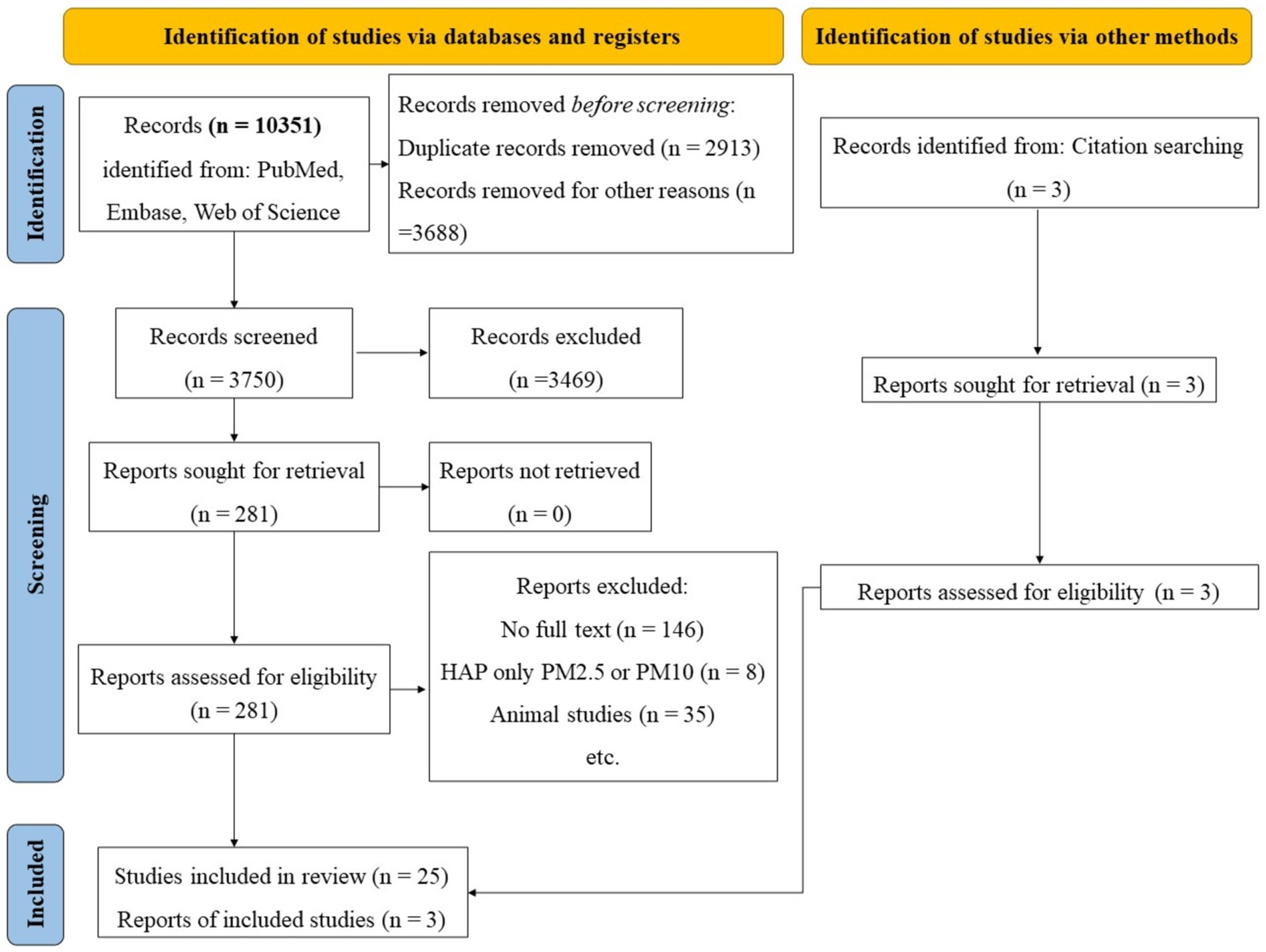
Figure 1. Flowchart of literature inclusion in the meta-analysis. HAP, Household air pollutants; PM2.5, Particulate matter 2.5.
We conducted a search in the PubMed, Embase, and Web of Science databases, yielding a total of 10,351 articles. Among these, 2,913 articles were duplicate records, and 3,688 articles were excluded due to the absence of abstracts or inapposite article types. Ultimately, 3,750 articles underwent preliminary analysis. After carefully reviewing the titles and abstracts, we excluded 3,469 articles that were clearly unrelated to our study, leaving 281 articles for full-text review. Due to a lack of available original data or animal studies, we subsequently excluded 256 articles. In the end, a total of 25 articles were included in this study. Additionally, while reviewing the references of these 25 articles, we identified another three relevant articles that had not been previously included, and we added them to the analysis (Figure 2).
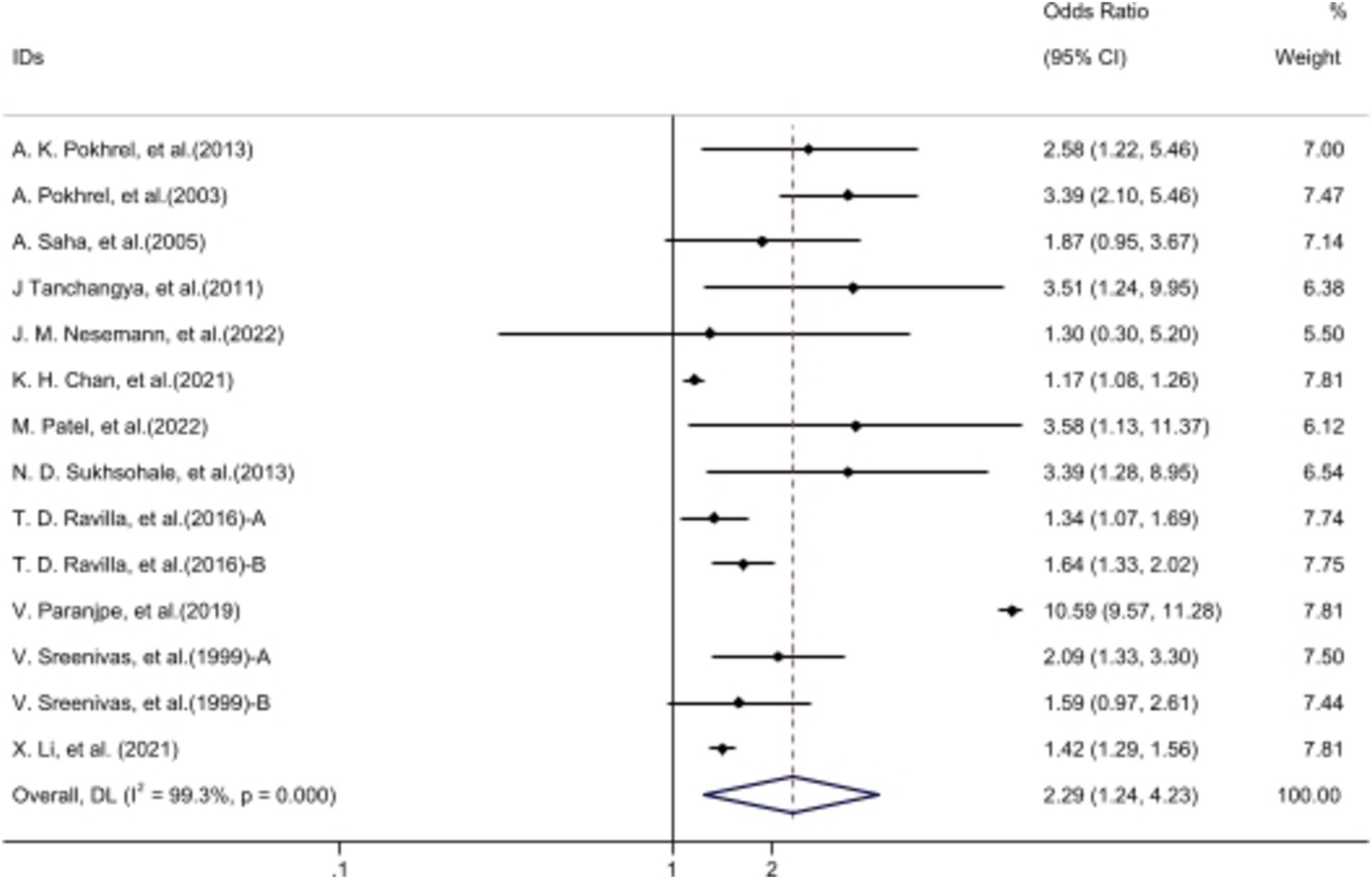
Figure 2. The forest plot: Comparison of cataracts in individuals using UCF vs. clean fuels. Ravilla et al. (15): A, male exposed to UCF/CF; B, female exposed to UCF/CF. Sreenivas et al. (14): A, data from Angamally, India; B, data from Calcutta, India. The data of ‘Patel et al. (5)’ from WebPlotDigitizer 4.5 software. Volunteers cooking with UCF exhibited a higher incidence of cataracts compared to those using clean fuels.
We conducted a comprehensive systematic review on UCF exposure and eye health, and performed a meta-analysis on studies with two or more articles. All analyses were performed using Excel 2017, Stata/MP (version 17), and Adobe Illustrator 2018 for data processing, statistical computations, and image generation, respectively. Forest plots were utilized to depict the adverse effects of UCF on ocular health. Data were aggregated to calculate OR values alongside 95% confidence intervals (CI). Outcomes from the included studies were assessed using either random or fixed effects models, chosen based on the degree of heterogeneity determined by the I-squared (I2) statistic. If I2 > 50%, a random effects model was utilized for meta-analysis; otherwise, a fixed effects model was applied (20). Sensitivity analysis involved a systematic investigation of each article’s impact on the outcomes (21). Publication bias was evaluated using both Egger’s test and Begg’s suggestion (22). A significance threshold of p-value (p) < 0.05 was set for all analytical outcomes (Figure 3; Table 1).
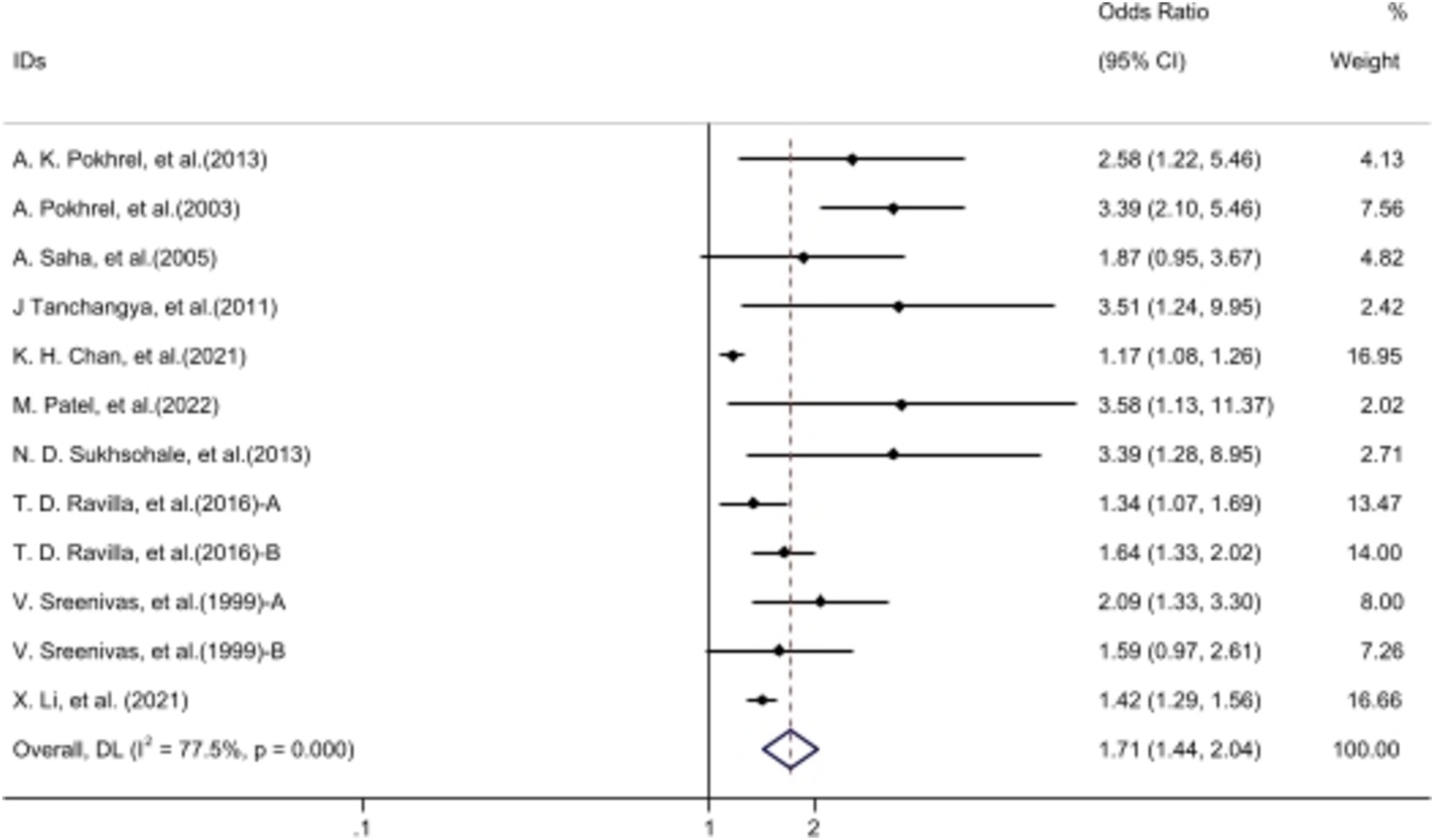
Figure 3. The forest plot: comparison of cataracts in individuals using UCF vs. clean fuels after revision. Ravilla et al. (15): A, male exposed to UCF/CF; B, female exposed to UCF/CF. Sreenivas et al. (14): A, data from Angamally, India; B, data from Calcutta, India. The data of ‘Patel et al. (5)’ from WebPlotDigitizer 4.5 software. Nesemann et al. (52), Paranjpe et al. (12) were excluded. Volunteers cooking with UCF exhibited a higher incidence of cataracts compared to those using clean fuels after revision.
All 28 studies were conducted in developing countries, with 14 taking place in India, with a few carried out in Latin America and Africa. As for the study types, 11 cross-sectional studies, 8 cohort studies, 8 case–control studies, and 1 multicenter study were included. The literature was evaluated using the NOS (23), with scores ranging between 3 to 7 across all articles (Table 2). In terms of subject matter, 14 articles focused on cataracts, 8 studies addressed visual impairments, and 10 articles discussed ocular symptoms. In contrast, there was only one article that explored topics such as glaucoma, conjunctivitis, and night blindness. Supplementary Figure S1 presented a summary of the forest plots in this meta-analysis; Supplementary Figure S2 provided an overview of the funnel plots in this meta-analysis; Supplementary material S1 outlined the sensitivity analysis results of this meta-analysis.
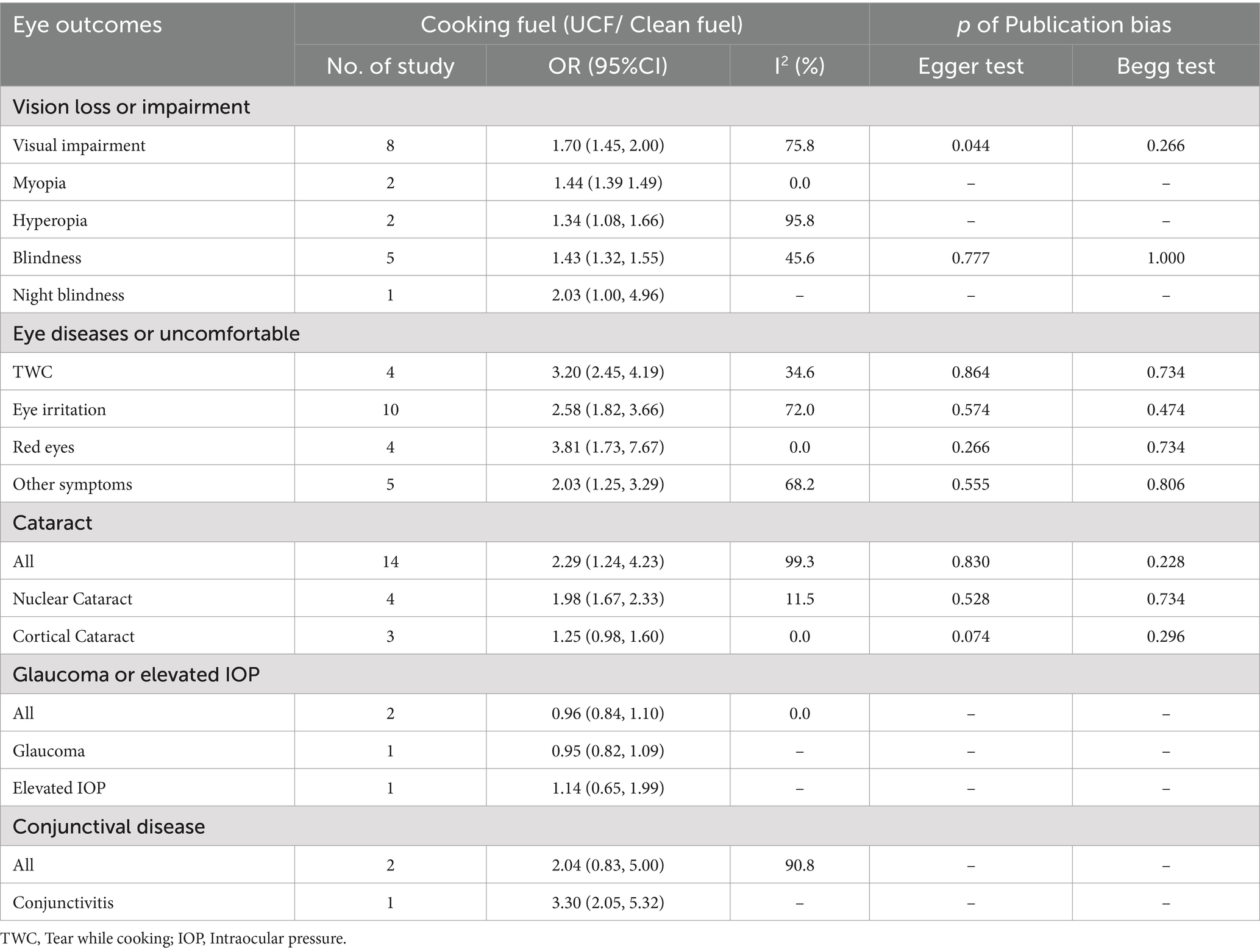
Table 2. The meta-analysis outcomes: comparison of eye healthy problems in individuals using UCF vs. clean fuels.
Fourteen articles demonstrated a significant association between UCF and cataracts [OR 2.29, 95% CI (1.24, 4.23)]. Despite considerable heterogeneity among studies (I2 = 99.1%), sensitivity analysis indicated relatively stable outcomes (Supplementary material S1). Funnel plot analysis showed an even distribution of articles on both sides (Supplementary Figure S2), with p > 0.05 from publication bias tests (Table 2), indicating no such bias. After excluding two articles out of the 95% CI of funnel plot, exposure to biomass fuels still had a negative impact on the incidence of cataracts [OR 1.71 95% CI (1.44, 2.03)] and the heterogeneity dropped to 77.5%.
Among the five articles discussing the relationship between kerosene exposure and cataracts, there was low heterogeneity among them (I2 = 14.4%). Meta-analysis outcomes suggested a potential link between kerosene cooking and cataract development [OR 1.48, 95% CI (1.11, 1.97)] (Supplementary Figure S1), yet Egger’s analysis indicated potential publication bias (p = 0.03). The results of the subgroup analysis showed a significant association between UCF exposure and nuclear cataracts, while no significant correlation was found with cortical cataracts. Additionally, the impact of UCF exposure on females (OR 1.28) was greater than that on males (OR 1.23). For more results from the subgroup analysis, please refer to Table 2.
Meta-analysis revealed a positive association between UCF-based cooking and visual impairments [OR 1.70, 95% CI (1.45, 2.00)] (Supplementary Figure S1), with substantial heterogeneity among these studies (I2 = 75.8%). Sensitivity analysis showed that the meta-analysis results were stable, with the lowest 95% CI being 1.37 (Supplementary material S1). While the funnel plot exhibited symmetry, Egger’s analysis suggested potential publication bias (p = 0.04). Among other vision loss catalogs, five touch upon blindness [OR 1.43, 95% CI (1.32, 1.55)], two upon myopia [OR 1.44, 95% CI (1.39, 1.49)], two upon hyperopia [OR 1.34, 95% CI (1.08, 1.66)], and one specifically examined night blindness [OR 2.03 95% CI (1.00, 4.96)]. Following a comprehensive review, the findings were considered credible.
Eye symptoms were mostly self-assessed by patients and obtained through questionnaires. Therefore, we selected three most commonly used eye symptoms: (TWC, eye irritation, red eyes). Meta-analysis suggested that exposure to UCF wound promoted the development of these symptom (Table 2). The sensitivity analysis showed that the results were stable and there was no publication bias (Table 2). Only articles related to eye irritation symptoms had high heterogeneity (I2 = 72.0%). Five articles did not cite specific types of eye disease or symptom, so we combined them as a broad concept as other eye disease or symptom, and we found that exposure to UCF cooking increased the occurrence of this catalog [OR 2.03, 95% CI (1.25, 3.29)], but the heterogeneity between articles was high (I2 = 68.2). The sensitivity analysis indicated that the meta-analysis results were stable. Both Egger test and Begg test believed that the relevant studies had no publication bias (Table 2).
Our research indicated that UCF exposure was closely related to eye health. This association was supported by foundational studies, showing that the combustion of UCF had low efficiency (24, 25), generating a significant amount of particulate matter and gaseous pollutants (26), including carbon monoxide and nitrogen oxides (27, 28). These pollutants could directly cause eye inflammation (15) or indirectly affect eye health by increasing reactive oxygen species release (29, 30) and decreasing dopamine release (31).
Our study demonstrated that the health burden of cataracts associated with UCF exposure varied based on fuel type, country, cataract type, exposure duration, gender, fuel conversion, and urban–rural status. For instance, patients with over 40 years of cooking time had a higher incidence of cataracts (OR 1.16) compared to those with 1–19 years of cooking time (OR 1.09). Additionally, the impact of UCF cooking on women (OR 1.28) was greater than on men (OR 1.23) (32), likely because women were typically the primary cooks and had longer cooking durations. Patients transitioning from biomass fuels to clean fuels had lower odds ratios than those who continued using biomass fuels (33) (Table 3), suggesting that early switching to cleaner cooking fuels might help mitigate health risks.
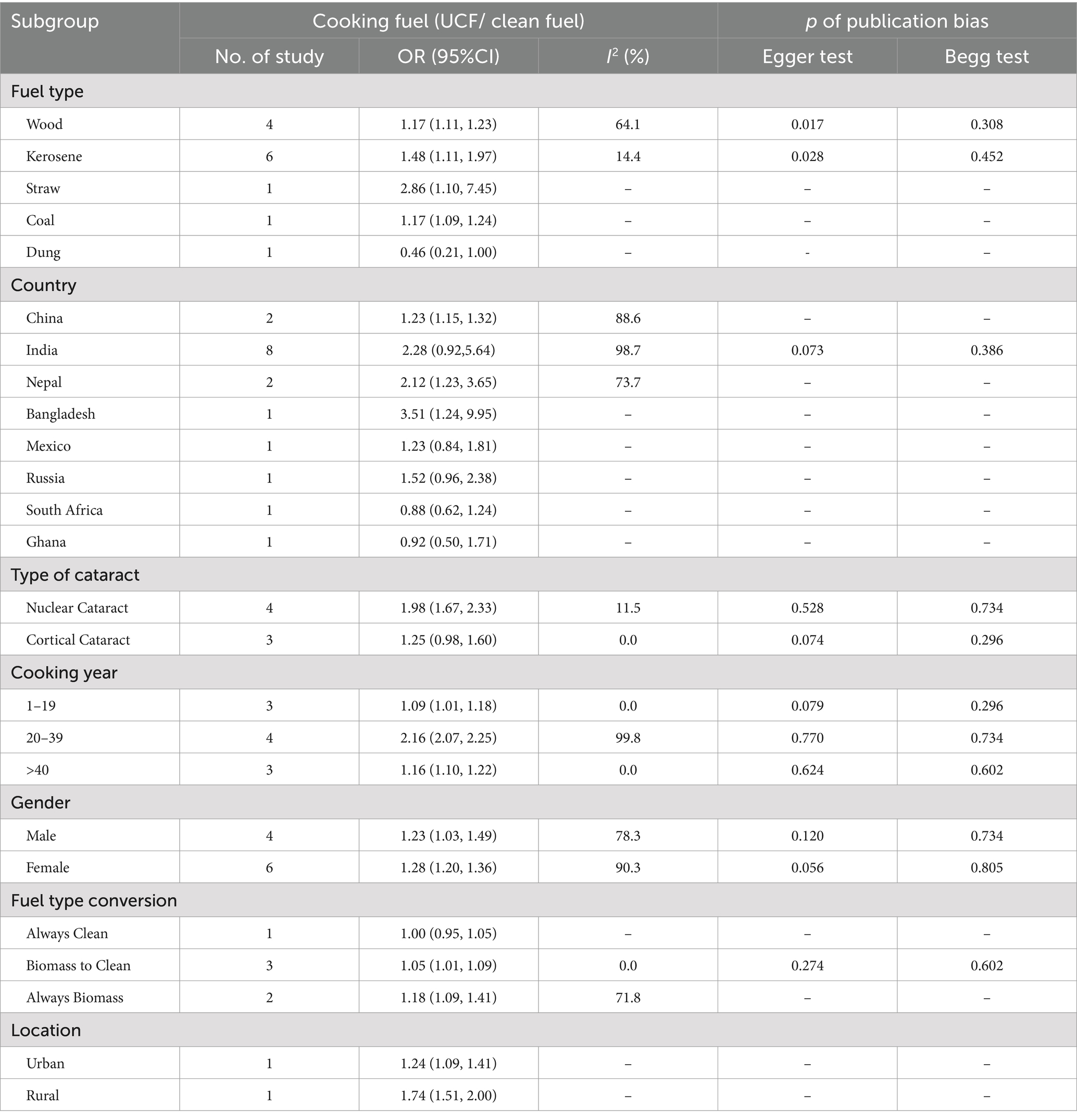
Table 3. The meta-analysis and subgroup analysis outcomes: comparison of cataract in individuals using UCF vs. clean fuels.
Furthermore, based on a larger data source, our research confirmed that UCF exposure was significantly associated only with nuclear cataracts [OR 1.98, 95% CI (1.67, 2.33)], not with cortical cataracts [OR 1.25, 95% CI (0.98, 1.60)]. Sensitivity analyses yielded stable results (Supplementary material S1), with no evidence of heterogeneity (Table 3) or publication bias. It remains unclear whether nuclear cataracts are more sensitive to air pollution or the limited number of studies on cortical cataracts led to false negatives, indicating a need for further research to clarify this issue.
In low-income countries, the burden of cataracts was relatively high, and studies showed that cataract surgery was cost-effective (34). However, due to limited access to medical services, poor quality of care, and cultural beliefs, it was often challenging to reach those in need, even when financial resources were sufficient (35, 36). Therefore, we suggested that preventing exposure to UCF, enhancing health education, and providing targeted cataract surgeries could be more effective and economical strategies.
The limited number of studies examining the link between UCF exposure and some other eye conditions necessitates descriptive analysis only. Articles explored glaucoma (37) or increased intraocular pressure (IOP) (38), both indicating no significant relationship between UCF exposure and them [OR 0.96, 95% CI (0.84, 1.10)]. A study by the China Kadoorie Biobank (37), encompassing 512,715 adults aged 30 to 79 across 10 areas in China from 2004 to 2008, found that exposure to solid fuels positively correlated with an increased prevalence of Conjunctiva disorder [OR 1.32, 95% CI (1.25, 1.39), n = 4,877] and disorders affecting the sclera, cornea, iris, and ciliary body [OR1.37, 95% CI (1.22, 1.48), n = 1,583]. Similarly, a research observed higher biomass fuel exposure levels among patients with conjunctivitis (39). However, in order to gain a comprehensive understanding and confirm the reliability of these results, additional detailed studies were needed in the future.
Previous studies indicated that visual impairment exhibited significant health inequalities between different income countries (2). Specifically, the incidence of visual impairment in low-income countries was eight times higher than in high-income countries, while in middle-income countries, it was four times higher (1). This disparity might be linked to high exposure to UCF in low-income regions. As the cost of clean fuels (such as LPG) was significantly higher than that of UCF (40), local residents often found it unaffordable, resulting in unequal access to fuel (40). To bridge this gap, reducing income inequality was crucial. Policy improvements, such as promoting remittance inflows or providing subsidies for fossil fuels, could enhance the availability of clean cooking fuels (40, 41).
Our research showed that eye symptoms effectively reflected individuals’ exposure levels to UCF, supporting the scientific validity of UCF-related questionnaire designs. Therefore, it was essential to prioritize measures to reduce UCF exposure for patients exhibiting eye symptoms. For low-income groups with limited financial means who could not access to clean fuels, it was recommended to utilize open or well-ventilated cooking environments, or to wear protective eyewear to minimize direct contact between the eyes and smoke. For women with long-term UCF exposure and users with better economic conditions, we advised transitioning to clean fuels as soon as possible. Additionally, we recommended that patients experiencing significant eye symptoms during cooking undergo chronic disease screenings to identify potential health issues promptly (42).
This study was unable to access individual-level data, limiting analysis and summarization to the population level. Most studies included were retrospective, with few prospective studies, affecting the reliability of results. Self-assessment of eye symptoms by patients without medical examinations might introduce bias.
UCF usage was significantly linked to eye health issues, notably eye symptoms, cataracts, and visual impairments. Further prospective and foundational research was crucial to authenticate potential impacts and underlying mechanisms, addressing data limitations and mitigating biases arising from self-assessment.
S-HC: Conceptualization, Formal analysis, Software, Supervision, Visualization, Writing – original draft, Writing – review & editing. YT: Data curation, Formal analysis, Methodology, Project administration, Resources, Software, Supervision, Validation, Writing – review & editing. SX: Data curation, Formal analysis, Resources, Supervision, Validation, Writing – review & editing, Investigation, Visualization.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by grants from National Natural Science Foundation of China Regional Science Fund Project (no. 82460913); Jiangxi Provincial Department of Education Technology Research Project (no. GJJ2200936).
We used GPT-4.0 for language refinement in the manuscript. After applying the generative AI tool, the revised text was thoroughly reviewed by a native English-speaking author (Yuan Tang) to ensure linguistic accuracy and fluency.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1434611/full#supplementary-material
1. Tan, TF, Thirunavukarasu, AJ, Jin, L, Lim, J, Poh, S, Teo, ZL, et al. Artificial intelligence and digital health in global eye health: opportunities and challenges. Lancet Glob Health. (2023) 11:e1432–43. doi: 10.1016/S2214-109X(23)00323-6
2. Murray, CJL. Findings from the global burden of disease study 2021. Lancet. (2024) 403:2259–62. doi: 10.1016/s0140-6736(24)00769-4
4. Zhao, S, Wang, H, Chen, H, Wang, S, Ma, J, Zhang, D, et al. Global magnitude and long-term trend of ischemic heart disease burden attributed to household air pollution from solid fuels in 204 countries and territories, 1990–2019. Indoor Air. (2022) 32:e12981. doi: 10.1111/ina.12981
5. Patel, M, Shrestha, MK, Manandhar, A, Gurung, R, Sadhra, S, Cusack, R, et al. Effect of exposure to biomass smoke from cooking fuel types and eye disorders in women from hilly and plain regions of Nepal. Br J Ophthalmol. (2022) 106:141–8. doi: 10.1136/bjophthalmol-2020-316766
6. Coles-Brennan, C, Sulley, A, and Young, G. Management of digital eye strain. Clin Exp Optom. (2019) 102:18–29. doi: 10.1111/cxo.12798
7. Ayebeng, C, Okyere, J, and Dickson, KS. Influence of type of cooking fuel on risk of hypertension among reproductive-age women in sub-Saharan Africa: insights from nationally representative cross-sectional surveys. Int Health. (2023) 16:325–33. doi: 10.1093/inthealth/ihad060
8. Li, L, Yang, A, He, X, Liu, J, Ma, Y, Niu, J, et al. Indoor air pollution from solid fuels and hypertension: a systematic review and meta-analysis. Environ Pollut. (2020) 259:113914. doi: 10.1016/j.envpol.2020.113914
9. Kurmi, OP, Arya, PH, Lam, K-BH, Sorahan, T, and Ayres, JG. Lung cancer risk and solid fuel smoke exposure: a systematic review and meta-analysis. Eur Respir J. (2012) 40:1228–37. doi: 10.1183/09031936.00099511
10. Chavan, RG, Kaur, J, and Charan, GS. Unseen crisis: revealing the hidden health impact of indoor air pollution—a scoping review. J Educ Health Promot. (2024) 13:410. doi: 10.4103/jehp.jehp_412_24
11. Pillarisetti, A, Ye, W, and Chowdhury, S. Indoor air pollution and health: bridging perspectives from developing and developed countries. Annu Rev Environ Resour. (2022) 47:197–229. doi: 10.1146/annurev-environ-012220-010602
12. Paranjpe, V, Rabinovich, EP, Sharma, N, Srivastava, A, Galor, A, Hackam, A, et al. Solid fuel exposure and the development of cataracts. Invest Ophthalmol Vis Sci. (2019) 60:4254–4.
13. Pokhrel, AK, Bates, MN, Shrestha, SP, Bailey, IL, DiMartino, RB, and Smith, KR. Biomass stoves and lens opacity and cataract in Nepalese women. Optom Vis Sci. (2013) 90:257–68. doi: 10.1097/OPX.0b013e3182820d60
14. Sreenivas, V, Prabhakar, AK, Badrinath, SS, Fernandez, T, Roy, IS, Sharma, T, et al. A rural population based case-control study of senile cataract in India. J Epidemiol. (1999) 9:327–36. doi: 10.2188/jea.9.327
15. Ravilla, TD, Gupta, S, Ravindran, RD, Vashist, P, Krishnan, T, Maraini, G, et al. Use of cooking fuels and cataract in a population-based study: the India eye disease study. Environ Health Perspect. (2016) 124:1857–62. doi: 10.1289/EHP193
16. Tanchangya, J, and Geater, AF. Use of traditional cooking fuels and the risk of young adult cataract in rural Bangladesh: a hospital-based case-control study. BMC Ophthalmol. (2011) 11:1–13. doi: 10.1186/1471-2415-11-16
17. Stroup, DF, Berlin, JA, Morton, SC, Olkin, I, Williamson, GD, Rennie, D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. (2000) 283:2008–12. doi: 10.1001/jama.283.15.2008
18. Moher, D, Shamseer, L, Clarke, M, Ghersi, D, Liberati, A, Petticrew, M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. (2015) 4:1–9. doi: 10.1186/2046-4053-4-1
19. Drevon, D, Fursa, SR, and Malcolm, AL. Intercoder reliability and validity of web plot digitizer in extracting graphed data. Behav Modif. (2017) 41:323–39. doi: 10.1177/0145445516673998
20. Borenstein, M, Hedges, LV, Higgins, JP, and Rothstein, HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. (2010) 1:97–111. doi: 10.1002/jrsm.12
21. Mathur, MB, and Vander Weele, TJ. Sensitivity analysis for publication bias in meta-analyses. J R Stat Soc C Appl Stat. (2020) 69:1091–119. doi: 10.1111/rssc.12440
22. Peters, JL, Sutton, AJ, Jones, DR, Abrams, KR, and Rushton, L. Comparison of two methods to detect publication bias in meta-analysis. JAMA. (2006) 295:676–80. doi: 10.1001/jama.295.6.676
23. Wells, GA, Shea, B, O’Connell, D, Peterson, J, Welch, V, Losos, M, et al. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. (2000).
24. Isara, AR, and Aigbokhaode, AQ. Household cooking fuel use among residents of a sub-urban community in Nigeria: implications for indoor air pollution. Eur J Med. (2014) 46:203–8. doi: 10.5152/eajm.2014.0051
25. Demirbas, A. Combustion characteristics of different biomass fuels. Prog Energy Combust Sci. (2004) 30:219–30. doi: 10.1016/j.pecs.2003.10.004
26. Li, X, Duan, L, Wang, S, Duan, J, Guo, X, Yi, H, et al. Emission characteristics of particulate matter from rural household biofuel combustion in China. Energy Fuel. (2007) 21:845–51. doi: 10.1021/ef060150g
27. Wei, W, Zhang, W, Hu, D, Ou, L, Tong, Y, Shen, G, et al. Emissions of carbon monoxide and carbon dioxide from uncompressed and pelletized biomass fuel burning in typical household stoves in China. Atmos Environ. (2012) 56:136–42. doi: 10.1016/j.atmosenv.2012.03.060
28. Balmes, JR. Household air pollution from domestic combustion of solid fuels and health. J Allergy Clin Immunol. (2019) 143:1979–87. doi: 10.1016/j.jaci.2019.04.016
29. Dutta, A, Ray, MR, and Banerjee, A. Systemic inflammatory changes and increased oxidative stress in rural Indian women cooking with biomass fuels. Toxicol Appl Pharmacol. (2012) 261:255–62. doi: 10.1016/j.taap.2012.04.004
30. Mondal, NK, Saha, H, Mukherjee, B, Tyagi, N, and Ray, MR. Inflammation, oxidative stress, and higher expression levels of Nrf 2 and NQO1 proteins in the airways of women chronically exposed to biomass fuel smoke. Mol Cell Biochem. (2018) 447:63–76. doi: 10.1007/s11010-018-3293-0
31. Yuan, T, and Zou, H. Effects of air pollution on myopia: an update on clinical evidence and biological mechanisms. Environ Sci Pollut Res. (2022) 29:70674–85. doi: 10.1007/s11356-022-22764-9
32. Albalak, R, Frisancho, AR, and Keeler, GJ. Domestic biomass fuel combustion and chronic bronchitis in two rural Bolivian villages. Thorax. (1999) 54:1004–8. doi: 10.1136/thx.54.11.1004
33. Malla, S, and Timilsina, GR. Household cooking fuel choice and adoption of improved cookstoves in developing countries: a review. World Bank Policy Research Working Paper 2014, p. 6903.
34. Flessa, S. Cataract surgery in low-income countries: a good deal! Healthcare. (2022) 10:2580. doi: 10.3390/healthcare10122580
35. Grimes, CE, Bowman, KG, Dodgion, CM, and Lavy, CB. Systematic review of barriers to surgical care in low-income and middle-income countries. World J Surg. (2011) 35:941–50. doi: 10.1007/s00268-011-1010-1
36. Lindfield, R, Vishwanath, K, Ngounou, F, and Khanna, RC. The challenges in improving outcome of cataract surgery in low and middle income countries. Indian J Ophthalmol. (2012) 60:464–9. doi: 10.4103/0301-4738.100552
37. Chan, KH, Yan, M, Bennett, DA, Guo, Y, Chen, Y, Yang, L, et al. Long-term solid fuel use and risks of major eye diseases in China: a population-based cohort study of 486, 532 adults. PLoS Med. (2021) 18:e1003716. doi: 10.1371/journal.pmed.1003716
38. Ahmed, MS, Ullah, AY, Barman, N, Ratan, ZA, Mostafa, S, Khaleque, A, et al. Risk factors associated with elevated intraocular pressure: a population-based study in a rural community of Bangladesh. BMJ Open Ophthalmol. (2023) 8:e001386. doi: 10.1136/bmjophth-2023-001386
39. Del Risco, J, Sócola, FA, Noda, JR, Bravo, YA, López, LM, Lazo, MA, et al. Conjunctivitis symptoms between people exposed to biomass fuel combustion. A106. Biomass smoke: Organic does not mean less harmful! New York: American Thoracic Society (2010). A2429 p.
40. Murshed, M. The relevance of reducing income inequality for eliminating urban-rural divide in clean cooking fuel accessibility: evidence from Latin America and the Caribbean. Energy. (2023) 278:127718. doi: 10.1016/j.energy.2023.127718
41. Murshed, M. Can income inequality reduction policies limit the disparity between urban and rural clean cooking fuel access rates? Sustain Dev. (2024) 2024:3169. doi: 10.1002/sd.3169
42. Smith, L, López Sánchez, GF, Soysal, P, Tully, MA, and Koyanagi, A. Unclean cooking fuel use and health outcomes in older adults: potential mechanisms, public health implications, and future directions. J Gerontol A. (2023) 78:2342–7. doi: 10.1093/gerona/glad183
43. Ellegård, A. Tears while cooking: an indicator of indoor air pollution and related health effects in developing countries. Environ Res. (1997) 75:12–22. doi: 10.1006/enrs.1997.3771
44. Pokhrel, AK, Smith, KR, Khalakdina, A, Deuja, A, and Bates, MN. Case–control study of indoor cooking smoke exposure and cataract in Nepal and India. Int J Epidemiol. (2005) 34:702–8. doi: 10.1093/ije/dyi015
45. Saha, A, Kulkarni, P, Shah, A, Patel, M, and Saiyed, H. Ocular morbidity and fuel use: an experience from India. Occup Environ Med. (2005) 62:66–9. doi: 10.1136/oem.2004.015636
46. James, BS, Shetty, RS, Kamath, A, and Shetty, A. Household cooking fuel use and its health effects among rural women in southern India—a cross-sectional study. PLoS One. (2020) 15:e0231757. doi: 10.1371/journal.pone.0231757
47. Norbäck, D, Zhang, X, Fan, Q, Zhang, Z, Zhang, Y, Li, B, et al. Home environment and health: domestic risk factors for rhinitis, throat symptoms and non-respiratory symptoms among adults across China. Sci Total Environ. (2019) 681:320–30. doi: 10.1016/j.scitotenv.2019.05.084
48. Walker, ES, Clark, ML, Young, BN, Rajkumar, S, Benka-Coker, ML, Bachand, AM, et al. Exposure to household air pollution from biomass cookstoves and self-reported symptoms among women in rural Honduras. Int J Environ Health Res. (2020) 30:160–73. doi: 10.1080/09603123.2019.1579304
49. Diaz, E, Smith-Sivertsen, T, Pope, D, Lie, RT, Diaz, A, McCracken, J, et al. Eye discomfort, headache and back pain among Mayan Guatemalan women taking part in a randomised stove intervention trial. J Epidemiol Community Health. (2007) 61:74–9. doi: 10.1136/jech.2006.043133
50. Das, I, Jagger, P, and Yeatts, K. Biomass cooking fuels and health outcomes for women in Malawi. EcoHealth. (2017) 14:7–19. doi: 10.1007/s10393-016-1190-0
51. Katz, J, Tielsch, JM, Thulasiraj, RD, Coles, C, Sheeladevi, S, Yanik, EL, et al. Risk factors for maternal night blindness in rural South India. Ophthalmic Epidemiol. (2009) 16:193–7. doi: 10.1080/09286580902863080
52. Nesemann, JM, Srinivasan, M, Ravindran, RD, Edwards, T, O’brien, KS, Kim, UR, et al. Relationship between cooking fuel and lens opacities in South India: a 15-year prospective cohort study. Am J Ophthalmol. (2022) 243:66–76. doi: 10.1016/j.ajo.2022.06.021
53. Raufman, J, Blansky, D, Lounsbury, DW, Mwangi, EW, Lan, Q, Olloquequi, J, et al. Environmental health literacy and household air pollution-associated symptoms in Kenya: a cross-sectional study. Environ Health. (2020) 19:1–6. doi: 10.1186/s12940-020-00643-5
54. Sahoo, KC, Dash, GC, Panda, S, Kshatri, JS, Uddin, A, Pattnaik, M, et al. Impact of smokeless cooking fuel use on health status of women in a rural setting of eastern India. Int J Environ Health Res. (2023) 33:464–72. doi: 10.1080/09603123.2022.2035324
55. Li, Z, Commodore, A, Hartinger, S, Lewin, M, Sjödin, A, Pittman, E, et al. Biomonitoring human exposure to household air pollution and association with self-reported health symptoms–a stove intervention study in Peru. Environ Int. (2016) 97:195–203. doi: 10.1016/j.envint.2016.09.011
56. Sukhsohale, ND, Narlawar, UW, and Phatak, MS. Indoor air pollution from biomass combustion and its adverse health effects in Central India: an exposure-response study. Indian J Community Med. (2013) 38:162–7. doi: 10.4103/0970-0218.116353
57. Adhikari, S, Shrestha, U, Shrestha, MK, Paudyal, M, Thapa, B, and Shrestha, M. Environmental factors associated with ocular morbidity among children in three ecological regions of Nepal: a phase II Nepal Pediatric ocular diseases study. Int Ophthalmol. (2018) 38:2313–9. doi: 10.1007/s10792-017-0724-y
58. Islam, S, Upadhyay, AK, Mohanty, SK, Pedgaonkar, SP, Maurer, J, and O'Donnell, O. Use of unclean cooking fuels and visual impairment of older adults in India: a nationally representative population-based study. Environ Int. (2022) 165:107302. doi: 10.1016/j.envint.2022.107302
59. Aung, TW, Baumgartner, J, Jain, G, Sethuraman, K, Reynolds, C, Marshall, JD, et al. Effect on blood pressure and eye health symptoms in a climate-financed randomized cookstove intervention study in rural India. Environ Res. (2018) 166:658–67. doi: 10.1016/j.envres.2018.06.044
60. Mishra, VK, Retherford, RD, and Smith, KR. Biomass cooking fuels and prevalence of blindness in India. J Environ Med. (1999) 1:189–99. doi: 10.1002/jem.30
61. Khushk, WA, Fatmi, Z, White, F, and Kadir, MM. Health and social impacts of improved stoves on rural women: a pilot intervention in Sindh, Pakistan. Indoor Air. (2005) 15:311–6. doi: 10.1111/j.1600-0668.2005.00367.x
62. Li, X, Guo, Y, Liu, T, Xiao, J, Zeng, W, Hu, J, et al. The association of cooking fuels with cataract among adults aged 50 years and older in low-and middle-income countries: results from the WHO study on global AGEing and adult health (SAGE). Sci Total Environ. (2021) 790:148093. doi: 10.1016/j.scitotenv.2021.148093
Keywords: health inequalities, cataracts, visual impairments, ocular symptoms, unclean cooking fuel
Citation: Chen S-H, Tang Y and Xue S (2025) Eye health risks associated with unclean fuel: a meta-analysis and systematic review. Front. Public Health. 12:1434611. doi: 10.3389/fpubh.2024.1434611
Received: 18 May 2024; Accepted: 24 December 2024;
Published: 30 January 2025.
Edited by:
Xinming Wang, Chinese Academy of Sciences, ChinaReviewed by:
Chao Li, Shandong University, ChinaCopyright © 2025 Chen, Tang and Xue. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Song Xue, eHVlc29uZzIwMjJAY3N1LmVkdS5jbg==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.