- 1Department of Respiratory, Shandong Qianfoshan Hospital, Cheeloo College of Medicine, Shandong University, Jinan, China
- 2Department of Respiratory and Critical Care Medicine, Research Center for Chronic Airway Diseases, Peking University Health Science Center, Peking University Third Hospital, Beijing, China
- 3Department of Respiratory, Shandong Provincial Qianfoshan Hospital, The First Affiliated Hospital of Shandong First Medical University, Shandong Institute of Respiratory Diseases, Shandong University, Jinan, China
Objective: Despite smoking being a significant risk factor in the occurrence and progression of chronic obstructive pulmonary disease (COPD), no comprehensive analysis has been conducted to determine the potential benefits of smoking cessation for patients with established COPD or identify specific indicators that may be improved. The aim of our meta-analysis was to elucidate the positive impact of smoking cessation on COPD.
Methods: We conducted a comprehensive search of PubMed, EMBASE, Web of Science, Cochrane Library, CNKI, Wan Fang and VIP databases to identify studies that met our eligibility criteria from inception up to 1, May 2024. Data were extracted independently by two authors and pooled using a random-effects model. Study quality was evaluated using the Newcastle-Ottawa Scale (NOS).
Results: Preliminary screening of publications gave a total of 13,460 documents after which the repetitive and non-compliant studies were removed. Eventually, 11 studies were included for follow-up analysis. The pooled results showed that cessation of smoking produced significant improvements in forced expiratory volume in one second (FEV1)% predicted (MD = 6.72, 95% CI, 4.55–8.89, P < 0.001; I2 = 53%), FEV1/forced vital capacity (FVC) (MD = 6.82, 95% CI, 5.09-8.54, P < 0.001; I2 = 0%), modified Medical Research Council (mMRC) (MD = −0.49, 95% CI, −0.95–−0.02, P = 0.040; I2 = 73%), 6-minute walk test (6-MWT) (MD = 64.46, 95% CI 14.60-114.32, P = 0.010; I2 = 94%), partial oxygen pressure (MD = 1.96, 95% CI, 1.03-2.89, P < 0.001; I2 = 0%), mortality (RR = 0.75, 95% CI, 0.56-1.00, P = 0.05; I2 = 44%).
Conclusion: Our meta-analysis presented suggestive evidence that smoking cessation offered significant benefits to COPD patients, notably in the improvement of specific key indicators of pulmonary function (FEV1% predicted, FEV1/FVC), alleviating symptoms, enhancing exercise tolerance, and could reduce mortality.
PROSPERO registration: https://www.crd.york.ac.uk/prospero/, identifier: CRD42022384123.
1 Introduction
Chronic obstructive pulmonary disease (COPD) is a non-communicable respiratory illness with high global incidence and mortality rates (1, 2). It has been estimated that over 3 million people worldwide die from COPD annually, resulting in significant societal and health-care burdens (3). Numerous risk factors may contribute to the onset and progression of COPD, including environmental exposures (such as tobacco smoking, biomass smoke and indoor air pollutants) (4), aging (5), and genetic predispositions (6), among others (7). However, tobacco use as a risk factor remains an actionable intervention. The Global Initiative for Chronic Obstructive Lung Disease (also known as GOLD) committee proposed quitting smoking as a necessary and evidence-based step for the prevention and treatment of COPD in 2001 (8). While the underlying molecular mechanism of smoking-related COPD is only partially understood, the exact quantitative factors associated with smoking that affect the prognosis of patients with COPD remain unknown. The previous study indicated that quitting smoking can delay the natural progression of COPD (9), with better results achieved when the cessation of smoking occurs at an early age (10). Furthermore, studies have demonstrated that quitting smoking can significantly alleviate respiratory symptoms in the short term and improve lung function, quality of life, and survival rate in the long term among patients with COPD(9, 11). However, several studies have suggested that there is persistent lung inflammation and a decline in lung function observed in mice following smoking cessation interventions (12, 13).
Above all, there exists a dearth of comprehensive systematic reviews that substantiate the tangible advantages of smoking cessation for COPD patients. In light of this, our research aims to conduct a comprehensive systematic review and meta-analysis that elucidates the multifaceted impact of smoking cessation on COPD.
2 Methods
Before conducting this meta-analysis, we registered our study on PROSPERO (https://www.crd.york.ac.uk/PROSPERO/) with the registration code CRD42022384123. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were strictly adhered to when reporting our findings (Supplementary material 1).
2.1 Search strategy
We searched for publications in PubMed, EMBASE, Web of Science, Cochrane Library, CNKI, Wan Fang, and VIP databases from their inception up to 1, May 2024. The detailed search strategy is presented in Supplementary material 2. Two investigators (W.Z.H, Q.Y.F) independently searched and screened all relevant articles, including systematic review studies, cohort studies, books, documents, etc. We evaluated the relevance of the full text of the articles and conducted independent screening according to the following criteria.
2.2 Inclusion and exclusion criteria
Studies were included if they matched the following criteria: (1) Studies related to patients with COPD and smoking cessation; (2) The research type of the study included is a prospective or retrospective study; (3) The individuals in the included studies were required to be satisfied that they had spirometrically confirmed COPD enrolled in the study (FEV1/FVC < 0.7 post-bronchodilation) or they had physician-diagnosed COPD before. (4) The under-study individuals groups quit smoking, while the control groups continued to smoke; (5) The observation time of the participants was more than 3 months; (6) The included research confirmed whether they were in smoking status through biological measures such as exhaled CO level or self-report; (7) The study was published in English or Chinese.
The exclusion criteria include: (1) The research types were in vitro studies or animal studies, reviews, case reports, and meta-analyses. (2) The full text could not be obtained or the information used to calculate the results was insufficient; (3) The research data provided by the articles was not complete; (4) Repetitive articles; (5) The control group (continuous-smoking group) had ever tried to quit smoking.
2.3 Data extraction and quality assessment
Two authors extracted data independently and screened eligible articles according to the title, keyword, abstract, and full text of the studies. Subsequently, the articles which met the standards were included. The data extracted and analyzed included the author of the article, sample size, research types, intervention protocol, and outcome indicators of the subjects. When authors have differing opinions on data extraction, they should fully discuss the problem of disagreement and even seek the help of a third person to make a judgment. The studies with incomplete data were excluded.
The quality of the included studies was evaluated using the NOS scale by two independent reviewers (W.Z.H and Q.Y.F). The scale in question encompasses a trifold assessment of selection, comparability and outcomes, each of which comprises several dimensions. Selection, for instance, is evaluated based on four criteria, including the representativeness of the cohort, selection of the unexposed cohort (if applicable), exposure verification, and demonstration that the outcome of interest was absent at baseline. Comparability, on the other hand, takes into account the similarities between the cohorts for study design and analysis. Finally, the results dimension scrutinizes the assessment of the results, the follow-up period, and the sufficiency of the follow-up of the cohorts. The NOS scale uses a “star” rating system (ranging from 0 stars to 9 stars) to judge quality: 7–9 stars denote “high” quality, 4–6 stars denote “medium” quality and 0–3 stars represent “low” quality (14).
2.4 Statistics analysis
RevMan 5.3 (www.cochrane.org/) and STATA 15.1 (StataCorp, Cary, NC, USA) were employed for data analyses in this meta-analysis study. For dichotomous data, we estimated the summary risk ratio (RR) with a 95% confidence interval (95% CI), and for continuous data, we estimated the mean difference (MD) with a 95% CI. The pooled effect sizes (ESs) were determined using a randomized-effect model and shown in a forest plot. The I2 statistic and Q-Cochran test were used to examine heterogeneity across studies. Cochran's Q test P < 0.1 was considered significant to assume apparent heterogeneity. The I2 < 25%, 25% < I2 < 50%, and I2 > 50% were considered as low heterogeneity, moderate heterogeneity, and high heterogeneity, respectively. Subgroup analysis was based on the duration of cessation and mean age of initial cessation for COPD patients. Had we included more than 10 studies in any outcome, we would have created a funnel plot to screen for publication bias. A sensitivity analysis was conducted to assess the stability of the results by excluding one study each time. Statistical significance was set at P < 0.05.
3 Results
3.1 Search results
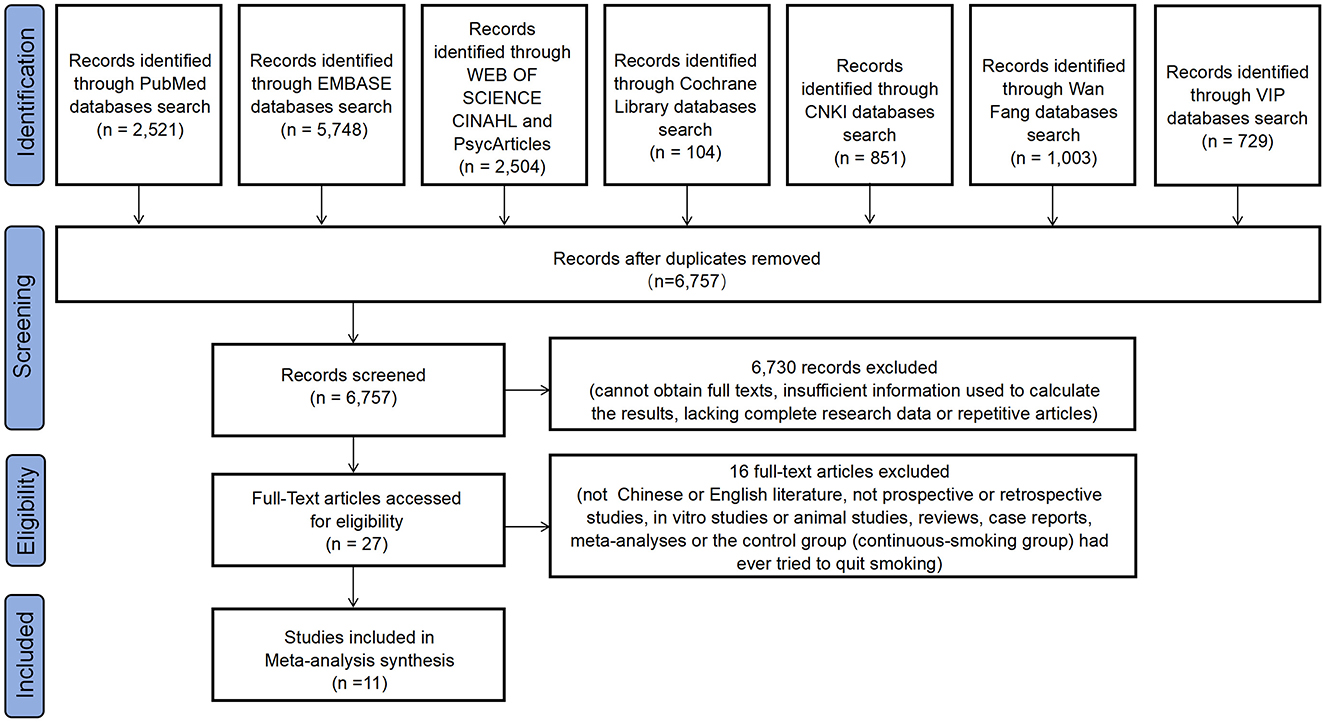
Initially, a total of 13, 460 records were retrieved from the database. After removing duplicates (n = 6,703), 6,757 studies were reviewed and 27 studies remained. Subsequently, sixteen studies were excluded based on the reasons shown in the flowchart. Finally, 11 studies were selected for inclusion in this meta-analysis. The PRISMA flowchart of the literature search and related screening process of the meta-analysis study is presented below (Figure 1).
3.2 Study characteristics
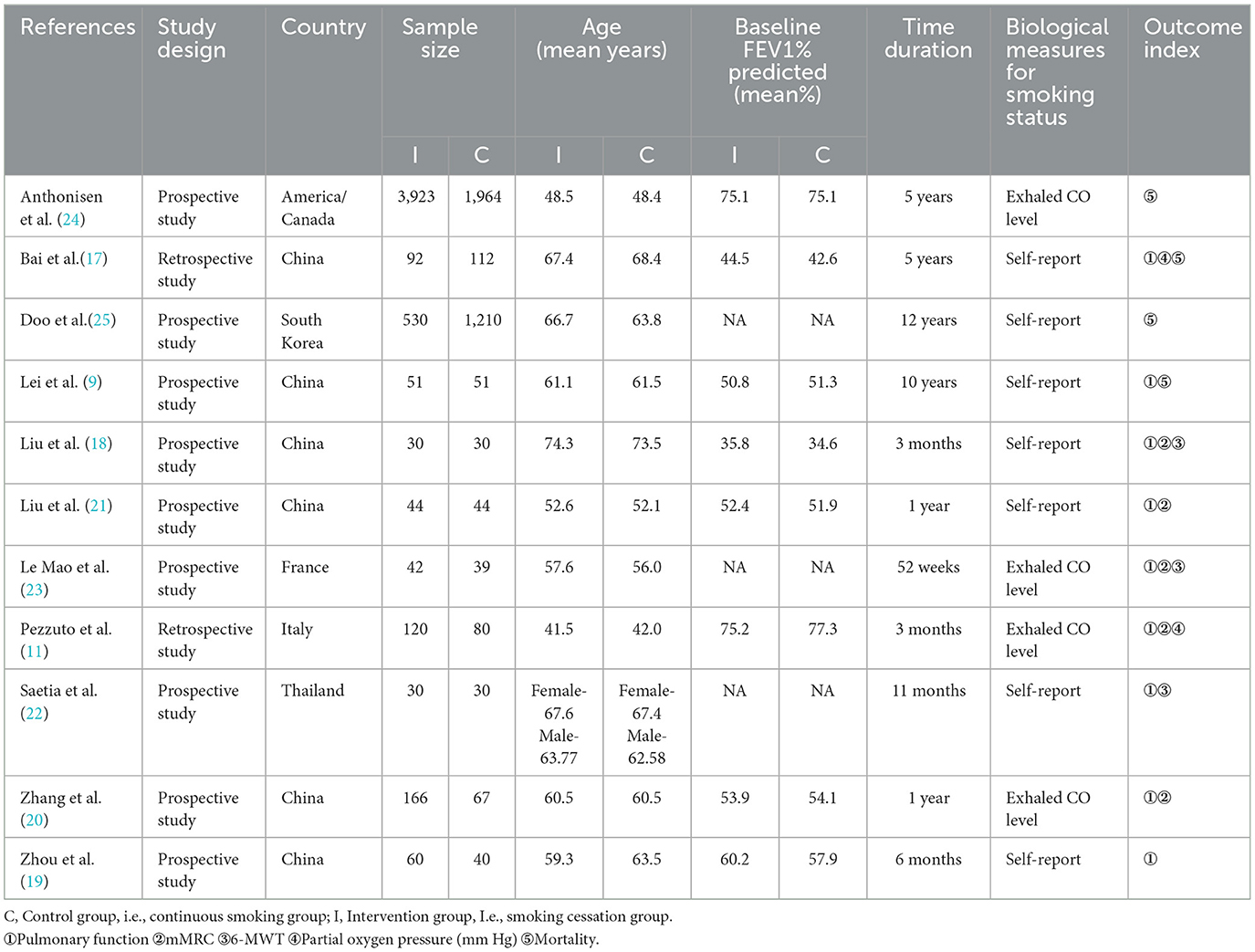
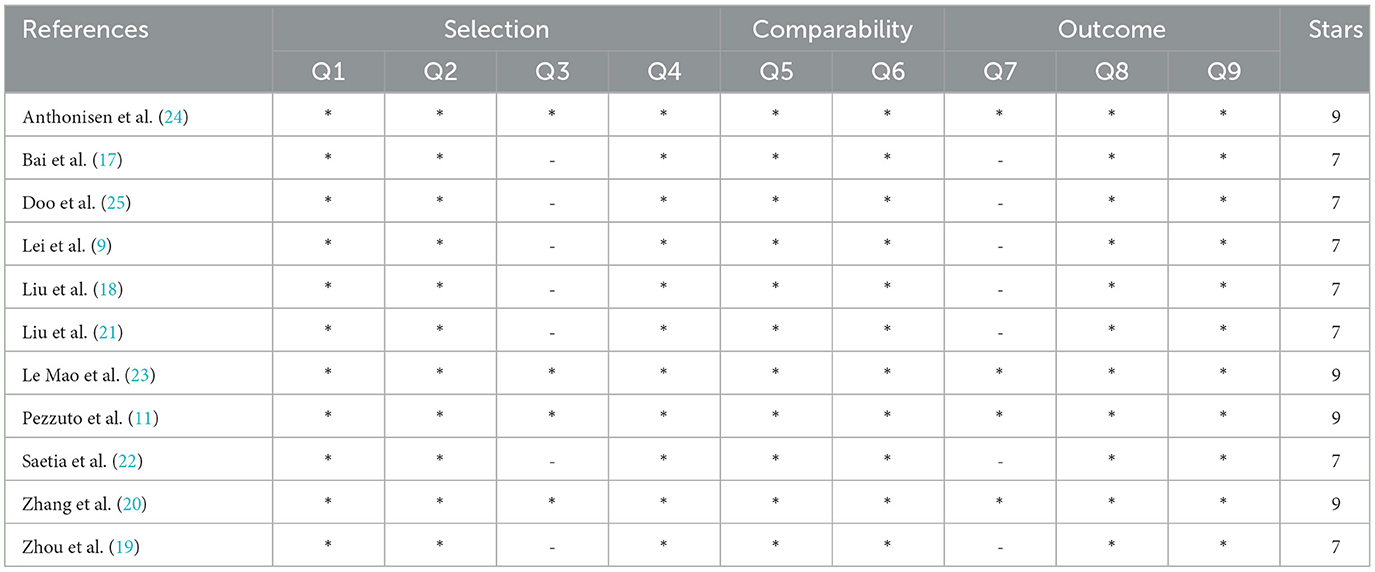
Patient and study characteristics of the 11 included studies are described in Table 1. Each of the included studies compared quitters and non-quitters for more than 3 months. Among these studies, eight conducted pulmonary function tests, while three employed dyspnea assessing indicators, including the mMRC scale (15) and 6-MWT (16). Furthermore, two studies recorded the measurement of partial pressure of oxygen in blood gas analysis, and four studies presented statistics of mortality. The NOS quality score showed that the included studies had a high-quality rating (Table 2).
3.3 Synthesized results
3.3.1 Effect of smoking cessation on pulmonary function in patients with COPD
3.3.1.1 FEV1% predicted
Seven studies (9, 11, 17–21) were pooled for meta-analysis of FEV1% predicted in patients with COPD. Compared with COPD patients who continued smoking, FEV1% predicted of COPD patients who quit smoking increased significantly (MD = 6.72, 95% CI, 4.55–8.89, P < 0.001) (Figure 2A), the between-study heterogeneity of which was I2 = 53% (P = 0.050).
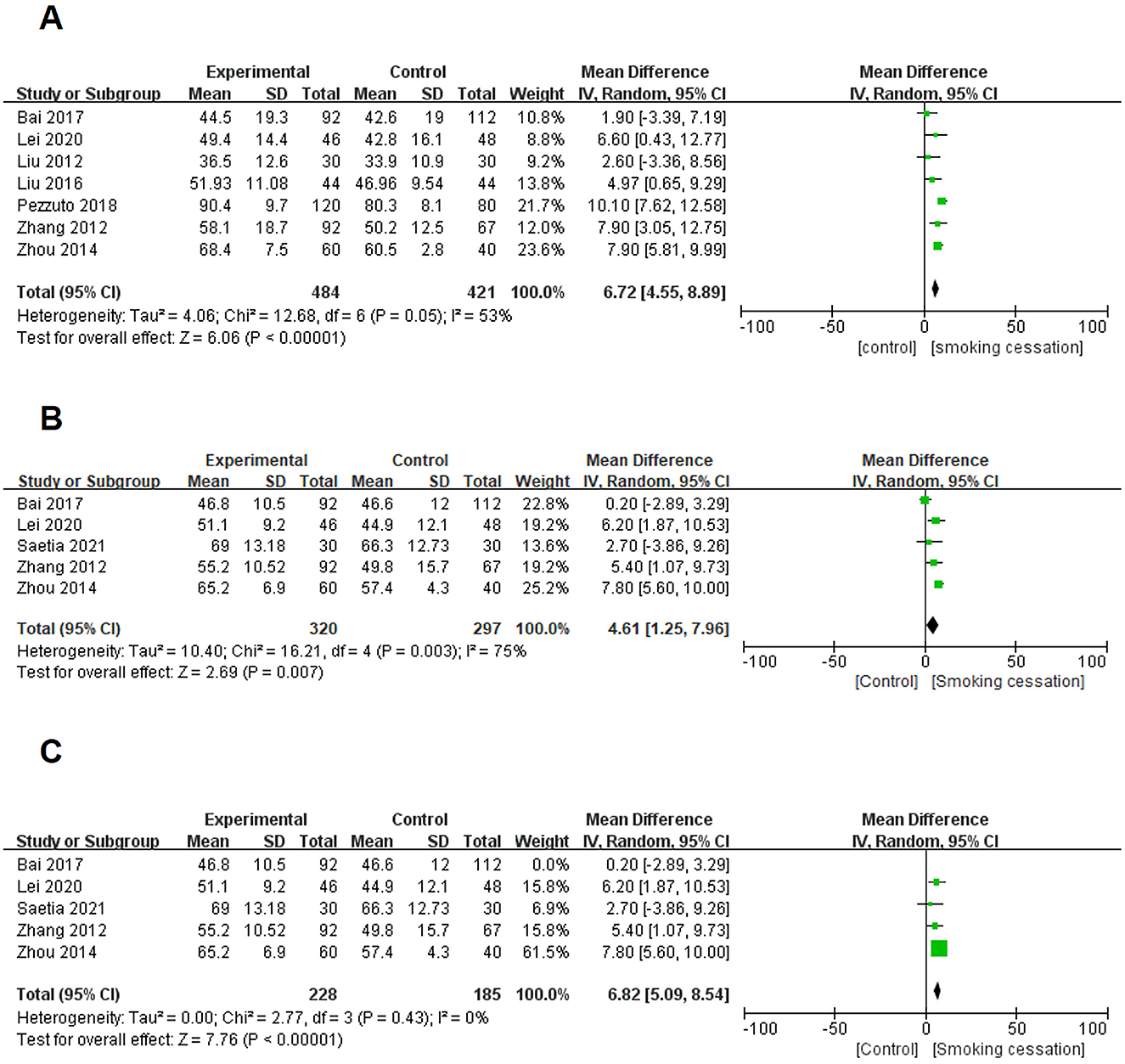
Figure 2. Forest plots for effects of smoking cessation on lung function for individuals with COPD. (A) Effects of smoking cessation on FEV1% predicted. (B) Effects of smoking cessation on FEV1/FVC were assessed before excluding studies with significant heterogeneity. (C) Effects of smoking cessation on FEV1/FVC were assessed after excluding studies with significant heterogeneity.
3.3.1.2 FEV1/FVC
Five eligible studies (9, 17, 19, 20, 22) were included to expound the impact of smoking cessation on FEV1/FVC in the lung function of COPD patients. The result revealed that the between-study heterogeneity was substantial (I2 = 75%, P = 0.003; Figure 2B). The above results showed that the heterogeneity of the research results was high. Therefore, by removing the studies one by one and conducting the analysis, we finally determined that the study, Bai 2017, was the main source of heterogeneity in this analysis. Next, the above data result was removed, and the remaining four studies were re-analyzed based on FEV1/FVC. Compared with COPD patients who continued smoking, FEV1/FVC of COPD patients who quit smoking increased significantly (MD = 6.82, 95% CI, 5.09–8.54, P < 0.001; I2 = 0%) (Figure 2C).
3.3.2 Effect of smoking cessation on dyspnea assessing indicators in patients with COPD
3.3.2.1 mMRC scale
Three studies (11, 18, 23) were included to conduct the meta-analysis of the impact of smoking cessation on the mMRC scale of COPD patients. The result revealed that the between-study heterogeneity was substantial (I2 = 73%, P = 0.030; Figure 3A). However, despite conducting sensitivity analysis, none of the studies exerted any influence on the heterogeneity observed in the final results. Thus, the analysis of the 3 existing studies showed that smoking cessation had an impact on the mMRC score of COPD patients (MD = −0.49, 95% CI, −0.95–−0.02, P = 0.040) (Figure 3A).
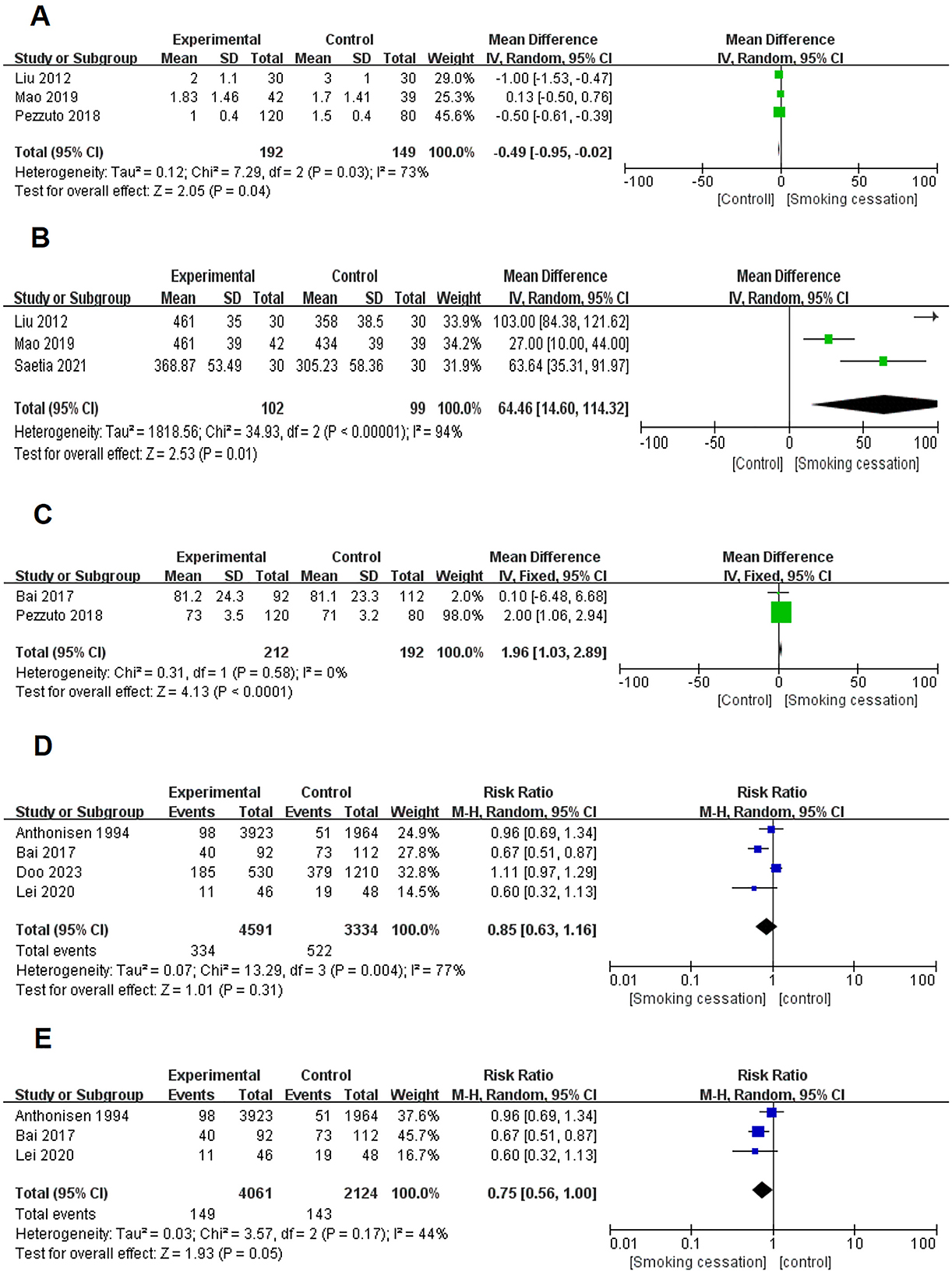
Figure 3. Forest plots for effects of smoking cessation on several objective evaluation index for individuals with COPD. (A) Effects of smoking cessation on mMRC. (B) Effects of smoking cessation on 6-MWT. (C) Effects of smoking cessation on partial oxygen pressure (mm Hg). (D) Effects of smoking cessation before excluding studies with significant heterogeneity. (E) Effects of smoking cessation on mortality were assessed after excluding studies with significant heterogeneity.
3.3.2.2 Six-minute walking test
Three studie s(18, 22, 23) were combined for the meta-analysis of 6-MWT in patients with COPD. Patients with COPD who quit smoking showed significantly better 6-MWT outcomes than those who continued to smoke. (MD = 64.46, 95% CI 14.60–114.32, P = 0.010; I2 = 94%, P < 0.001. Figure 3B). Due to the large heterogeneity, we conducted a sensitivity analysis of the one-by-one exclusion method, but there was no eligible study for removal.
3.3.3 Effect of smoking cessation on blood gas analysis in patients with COPD
Two studies (11, 17) pooled results for meta-analysis of blood gas analysis in patients with COPD and showed that the partial oxygen pressure (mm Hg) of COPD patients who quit smoking was significantly higher than that of COPD patients who continued smoking (MD = 1.96, 95% CI, 1.03–2.89, P < 0.001; I2 = 0%, P = 0.580) (Figure 3C).
3.3.4 Effect of smoking cessation on mortality of patients with COPD
Based on the preliminary meta-analysis of the four studies (9, 17, 24, 25), it was found that there was a significant heterogeneity in the results (I2 = 77%, P = 0.004) (Figure 3D). As a result, a sensitivity analysis was performed, which revealed that the Doo et al. study was the main source of heterogeneity in the results. To address this, the Doo et al. study was excluded and a meta-analysis was conducted on the remaining three studies. The analysis indicated that smoking cessation could have an impact on reducing all-cause mortality in patients with COPD (RR = 0.75, 95% CI, 0.56–1.00, P = 0.050; I2 = 44%, P = 0.170) (Figure 3E).
4 Subgroup analysis for the outcomes
To further explore the effects of duration of smoking cessation (<1 year/≥1 year) and mean age of initiation (<60-year-old/≥60-year-old) on patients with COPD, we conducted a subgroup analysis of some of the results that could be analyzed by using this method (Supplementary Figures 1A–D, 2A–D). It is noteworthy that patients with COPD who ceased smoking for less than a year manifested more significant improvements in 6-MWT compared with those who quit for over a year. Furthermore, COPD patients who quit smoking at an average age of <60 years displayed better FEV1% than those who commenced the quitting process at an average age of over 60 years. Howerver, the outcomes were inverted for 6-MWT patients.
5 Discussion
To the best of our knowledge, this is the first systematic review to investigate the impact of smoking cessation on a specific population of patients diagnosed with COPD. COPD remains a pervasive respiratory disorder that presents an enduring challenge in the 21st century, given the aging population and escalating environmental pollution. Besides, COPD frequently coexists with a range of comorbid conditions, thereby exacerbating the overall medical burden (26). While it is widely acknowledged that cigarette smoking plays a pivotal role in the onset and progression of this condition, there persists a higher prevalence of smoking among COPD patients (27, 28), highlighting the lack of awareness regarding the importance of smoking cessation or excessive tobacco dependence for those already afflicted. Our study conducted a comprehensive systematic review and meta-analysis of 11 studies to assess the impact of smoking cessation on patients with COPD, emphasizing the imperative nature of smoking cessation for individuals with COPD. The findings indicate that smoking cessation can enhance the pulmonary function of COPD patients, particularly in terms of FEV1% predicted and FEV1/FVC. Additionally, it can improve patients' endurance during physical exercise and increase the partial pressure of blood gas analysis for oxygen. From our findings, we also conclude that quitting smoking may reduce the mortality due to COPD.
The characteristic manifestations of COPD are progressive airway inflammation and incurable remodeling, primarily induced by cigarette smoke exposure (27). Chronic inhalation of cigarette smoke can activate pattern recognition receptors, such as Toll-like receptors, resulting in an innate immune response characterized by increased numbers of neutrophils and macrophages in the lungs, activation of airway epithelial cells, and mucus secretion (27). Additionally, cigarette smoke can induce excessive release of reactive oxygen species (ROS) from neutrophils and macrophages (29), thereby impairing antiprotease mechanisms and accelerating pulmonary tissue degradation, consequently facilitating the progression of emphysema (30).
Fortunately, numerous studies have demonstrated that smoking cessation not only alleviates lung dysfunction and inflammation but also delays the decline of lung function in individuals with sustained lung function injury due to COPD (31–33). In our study, we used FEV1% predicted and FEV1/FVC as indicators for evaluating lung function. Specifically, we analyzed seven studies that utilized the percentage of predicted FEV1 as an evaluation criterion and five studies that employed the FEV1/FVC. The synthesized outcomes were consistent with prior research, indicating that quitting smoking can ameliorate the pulmonary function status in individuals with COPD. During the progress of the meta-analysis, it was found that Bai et al.'s retrospective study exhibited a significant impact on the heterogeneity of the analysis outcomes, leading to its exclusion from the analysis. This disparity may be attributed to the study's retrospective nature as opposed to the prospective designs of the other four studies under scrutiny.
The assessment of breathlessness in patients with COPD is typically performed using the mMRC scale, a questionnaire that consists of five grades (34). Previous research had demonstrated that compared to continuous smokers, individuals with COPD who quit smoking had a higher likelihood of experiencing improvements in dyspnea, relief from cough symptoms, and an increase in oxygenation index. Conversely, persistent smoking results in continuous stimulation of cigarette smoke that leads to progressive exacerbation of airway inflammation and irreversible remodeling of the airway. This ultimately causes a worsening of dyspnea symptoms over time. Our meta-analysis, comprising four studies, indicates that smoking cessation positively impacts the alleviation of respiratory discomfort symptoms, particularly breathlessness, in patients with COPD. Due to the high heterogeneity of the results which cannot be eliminated, additional available studies will be included to analyze the effect of smoking cessation on improving dyspnea symptoms in patients with COPD. Additionally, the 6-MWT served as a valuable qualitative tool for assessing exercise tolerance and monitoring treatment effectiveness and disease progression in patients with COPD. Our meta-analysis of three studies revealed that smoking cessation significantly improved the 6-MWT values among COPD patients, suggesting its efficacy in enhancing exercise tolerance. Additionally, sufficient oxygen supply and efficient diffusion into tissues were indispensable for survival. The assessment of lung ventilation efficiency commonly relies on blood gas analysis, with oxygen partial pressure serving as a crucial indicator. Our meta-analysis of three cohort studies established that smoking cessation played a pivotal role in enhancing blood gas levels among patients with COPD(35). The increase in blood oxygen supply reduced the stimulation of peripheral chemoreceptors in the carotid body. As a result, the overactivation of the respiratory center was alleviated, leading to a more stable breathing pattern and improved respiratory efficiency, which further elucidated how quitting smoking could alleviate respiratory symptoms associated with COPD.
The progressive annual escalation in the mortality rate among patients with COPD is a matter of concern. Our findings indicate that quitting smoking can lead to a decrease in overall mortality among individuals with COPD, although the statistical significance is borderline, this result holds substantial clinical importance. This outcome could be attributed to the limited sample sizes in each study and the overall number of studies that were included.
Additionally, our subgroup analysis based on cessation duration and age of initial cessation revealed variations in FEV1/FVC% or 6-MWT among the groups. However, these results exhibited inconsistencies with each other, potentially attributed to the limited number of studies included in each subgroup, thereby compromising the reliability of the findings.
Our current study had several limitations. Firstly, the meta-analysis results did not reveal significant differences between male and female adults in terms of quitting smoking, which raises uncertainty about whether gender differences could impact COPD treatment outcomes. Secondly, the limited number of studies included may have resulted in publication bias and the small sample sizes in some reference studies may have led to slight deviations in outcomes. Thirdly, due to variations in intervention and observation times across studies, there was inevitable heterogeneity.
6 Conclusion
In conclusion, our meta-analysis provides compelling evidence to support the recommendation of smoking cessation as a crucial strategy in accordance with the GOLD guidelines, demonstrating significant benefits for patients with COPD. The comparative analysis between individuals who ceased smoking and those who continued revealed significant enhancements, including specific key indicators of pulmonary function (FEV1% predicted, FEV1/FVC), and exercise capacity among patients with COPD. Besides, smoking cessation also could reduce the mortality of COPD patients. Therefore, early smoking cessation among individuals diagnosed with COPD was strongly advocated to enhance their overall quality of life.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
ZW: Data curation, Formal analysis, Investigation, Methodology, Software, Writing – original draft. YQ: Data curation, Formal analysis, Investigation, Methodology, Writing – original draft. XJ: Conceptualization, Formal analysis, Supervision, Validation, Writing – review & editing. LD: Conceptualization, Funding acquisition, Methodology, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by grants from the National Natural Science Foundation of China (82270032), the Key Research and Development Program of Shandong Province (2021SFGC0504), Shandong Provincial Natural Science Foundation (ZR2021LSW015), and Jinan Clinical Medicine Research Program for Respiratory Disease (No. 202132002).
Acknowledgments
We are grateful to the researchers who studied the effects of smoking cessation on COPD.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1433269/full#supplementary-material
References
1. Christenson SA, Smith BM, Bafadhel M, Putcha N. Chronic obstructive pulmonary disease. Lancet. (2022) 399:2227–42. doi: 10.1016/S0140-6736(22)00470-6
2. Adeloye D, Song P, Zhu Y, Campbell H, Sheikh A, Rudan I. Global, regional, and national prevalence of, and risk factors for, chronic obstructive pulmonary disease (COPD) in 2019: a systematic review and modelling analysis. Lancet Respir Med. (2022) 10:447–58. doi: 10.1016/S2213-2600(21)00511-7
3. Walter K. COPD mortality, goals-of-care conversations in serious illness, and advocating for climate change science and gun violence prevention-highlights from the american thoracic society conference. JAMA. (2023) 329:2114–5. doi: 10.1001/jama.2023.4390
4. Lu Z, Coll P, Maitre B, Epaud R, Lanone S. Air pollution as an early determinant of COPD. Eur Respir Rev. (2022) 31:165. doi: 10.1183/16000617.0059-2022
5. Cho SJ, Stout-Delgado HW. Aging and lung disease. Annu Rev Physiol. (2020) 82:433–59. doi: 10.1146/annurev-physiol-021119-034610
6. Silverman EK. Genetics of COPD. Annu Rev Physiol. (2020) 82:413–31. doi: 10.1146/annurev-physiol-021317-121224
7. Wang Z, Qu J, Chang C, Sun Y. Association of the gut microbiome and different phenotypes of COPD and asthma: a bidirectional Mendelian randomization study. Microbiol Spectr. (2024) 12:e0176024. doi: 10.1128/spectrum.01760-24
8. Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO global initiative for chronic obstructive lung disease (GOLD) workshop summary. Am J Respir Crit Care Med. (2001) 163:1256–76. doi: 10.1164/ajrccm.163.5.2101039
9. Lei S, Li M, Duan W, Peng C, Chen P, Wu S. The long-term outcomes of tobacco control strategies based on the cognitive intervention for smoking cessation in COPD patients. Respir Med. (2020) 172:106155. doi: 10.1016/j.rmed.2020.106155
10. Hashimoto R, Tomioka H, Wada T, Yoshizumi Y. Outcomes and predictive factors for successful smoking cessation therapy in COPD patients with nicotine dependence. Respir Investig. (2020) 58:387–94. doi: 10.1016/j.resinv.2020.03.007
11. Pezzuto A, Stellato M, Catania G, Mazzara C, Tonini S, Caricato M, et al. Short-term benefit of smoking cessation along with glycopirronium on lung function and respiratory symptoms in mild COPD patients: a retrospective study. J Breath Res. (2018) 12:046007. doi: 10.1088/1752-7163/aad0a8
12. De Cunto G, Bartalesi B, Cavarra E, Balzano E, Lungarella G, Lucattelli M. Ongoing lung inflammation and disease progression in mice after smoking cessation: beneficial effects of formyl-peptide receptor blockade. Am J Pathol. (2018) 188:2195–206. doi: 10.1016/j.ajpath.2018.06.010
13. De Cunto G, De Meo S, Bartalesi B, Cavarra E, Lungarella G, Lucattelli M. Smoking cessation in mice does not switch off persistent lung inflammation and does not restore the expression of HDAC2 and SIRT1. Int J Mol Sci. (2022) 23:9104. doi: 10.3390/ijms23169104
14. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. (2010) 25:603–5. doi: 10.1007/s10654-010-9491-z
15. Bestall JC, Paul EA, Garrod R, Garnham R, Jones PW, Wedzicha JA. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. (1999) 54:581–6. doi: 10.1136/thx.54.7.581
16. Agarwala P, Salzman SH. Six-minute walk test: clinical role, technique, coding, and reimbursement. Chest. (2020) 157:603–11. doi: 10.1016/j.chest.2019.10.014
17. Bai JW, Chen XX, Liu S, Yu L, Xu JF. Smoking cessation affects the natural history of COPD. Int J Chron Obstruct Pulmon Dis. (2017) 12:3323–8. doi: 10.2147/COPD.S150243
18. Liu QG, Zhao SY, Zhao LL, Tian YJ, Wang XQ. Effects of smoking cessation on rehabilitation of patients with moderate or severe COPD. J Clini Pulmon Sci. (2012) 17:1008–10. doi: 10.3969/j.issn.1009-6663.2012.06.019
19. Zhou QQ, Xu XL, Xia DQ. The Smoking Cessation Effect on Pulmonary Function of Chronic Obstructive Pulmonary Disease and its Mechanism. Acta Universitatis Medicinalis Anhui. (2014) p. 1317–20.
20. Zhang B. The Effect of Smoking Cessation on Pulmonary Function and Life Quality in COPD patients. Chengde: Chengde Medical University (2012).
21. Liu PZ, Kong YH, Liu YQ. Effect of smoking cessation intervention on clinical symptoms and lung function in patients with COPD. Chin Med J Metallurg Indust. (2016) 33:450.
22. Saetia M, Puangprachang K, Semanu P, Siaosirithaworn S. Effects of 6 minute walk test and lung function test between smoking and stop smoking in chronic obstruction pulmonary disease patients at Samut Songkhram. Tobacco Induc Dis. (2021) 19:140886. doi: 10.18332/tid/140886
23. Le Mao R, Tromeur C, Paleiron N, Sanchez O, Gagnadoux F, Jouneau S, et al. Effect of early initiation of varenicline on smoking cessation in COPD patients admitted for exacerbation: the save randomized clinical trial. COPD. (2020) 17:7–14. doi: 10.1080/15412555.2019.1703928
24. Anthonisen NR, Connett JE, Kiley JP, Altose MD, Bailey WC, Buist AS, et al. Effects of smoking intervention and the use of an inhaled anticholinergic bronchodilator on the rate of decline of FEV1. The lung health study. JAMA. (1994) 272:1497–505. doi: 10.1001/jama.272.19.1497
25. Doo JH, Kim SM, Park YJ, Kim KH, Oh YH, Kim JS, et al. Smoking cessation after diagnosis of COPD is associated with lower all-cause and cause-specific mortality: a nationwide population-based cohort study of South Korean men. BMC Pulm Med. (2023) 23:237. doi: 10.1186/s12890-023-02533-1
26. Wang Z, Sun Y. Unraveling the causality between chronic obstructive pulmonary disease and its common comorbidities using bidirectional Mendelian randomization. Eur J Med Res. (2024) 29:143. doi: 10.1186/s40001-024-01686-x
27. Shahab L, Jarvis MJ, Britton J, West R. Prevalence, diagnosis and relation to tobacco dependence of chronic obstructive pulmonary disease in a nationally representative population sample. Thorax. (2006) 61:1043–7. doi: 10.1136/thx.2006.064410
28. Schauer GL, Wheaton AG, Malarcher AM, Croft JB. Health-care provider screening and advice for smoking cessation among smokers with and without COPD: 2009-2010 National Adult Tobacco Survey. Chest. (2016) 149:676–84. doi: 10.1378/chest.14-2965
29. Brusselle GG, Joos GF, Bracke KR. New insights into the immunology of chronic obstructive pulmonary disease. Lancet. (2011) 378:1015–26. doi: 10.1016/S0140-6736(11)60988-4
30. McGuinness AJ, Sapey E. Oxidative stress in COPD: sources, markers, and potential mechanisms. J Clin Med. (2017) 6:21. doi: 10.3390/jcm6020021
31. Willemse BW, Postma DS, Timens W, ten Hacken NH. The impact of smoking cessation on respiratory symptoms, lung function, airway hyperresponsiveness and inflammation. Eur Respir J. (2004) 23:464–76. doi: 10.1183/09031936.04.00012704
32. Simmons MS, Connett JE, Nides MA, Lindgren PG, Kleerup EC, Murray RP, et al. Smoking reduction and the rate of decline in FEV(1): results from the Lung Health Study. Eur Respir J. (2005) 25:1011–7. doi: 10.1183/09031936.05.00086804
33. Wiegman CH Li F, Ryffel B, Togbe D, Chung KF. Oxidative stress in ozone-induced chronic lung inflammation and emphysema: a facet of chronic obstructive pulmonary disease. Front Immunol. (2020) 11:1957. doi: 10.3389/fimmu.2020.01957
34. Young RP, Hopkins R, Eaton TE. Forced expiratory volume in one second: not just a lung function test but a marker of premature death from all causes. Eur Respir J. (2007) 30:616–22. doi: 10.1183/09031936.00021707
Keywords: smoking cessation, COPD, pulmonary function, mMRC scale, partial oxygen pressure, 6-MWT, mortality
Citation: Wang Z, Qiu Y, Ji X and Dong L (2024) Effects of smoking cessation on individuals with COPD: a systematic review and meta-analysis. Front. Public Health 12:1433269. doi: 10.3389/fpubh.2024.1433269
Received: 15 May 2024; Accepted: 21 November 2024;
Published: 11 December 2024.
Edited by:
Evangelia Fouka, Aristotle University of Thessaloniki, GreeceReviewed by:
Serafeim - Chrysovalantis Kotoulas, Hippokration General Hospital, GreeceMaria Kallieri, University General Hospital Attikon, Greece
Georgios Spyropoulos, 424 General Military Hospital, Greece
Copyright © 2024 Wang, Qiu, Ji and Dong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Liang Dong, ZGw1NTA2QDEyNi5jb20=
†These authors have contributed equally to this work
 Zihan Wang
Zihan Wang Yifan Qiu
Yifan Qiu Xiang Ji3
Xiang Ji3 Liang Dong
Liang Dong