- Department of Social Science, University of Siegen, Siegen, Germany
Introduction: Sleep-related complaints affect a significant proportion of the adult population in many societies. Despite the prevalence of symptoms and potential secondary and comorbid conditions, the utilization of professional help is quite low. The underlying reasons for this phenomenon have yet to be adequately investigated. To address this gap, we expand the conventional explanatory models to encompass the perceived cause as an explanatory factor. This is aimed to contribute to a better understanding of the help-seeking behavior and to create the basis for possible measures.
Materials and methods: The empirical basis of the study is a quantitative data set collected in Germany in 2015 comprising 3,000 individuals between the ages of 40 and 75. Of these individuals, 761 reported experiencing sleep-related complaints. In our logistic regression, the binary dependent variable is whether professional help has already been sought. In addition to the factors included in the behavioral model of health service use, we utilize the perceived cause as a predictor, categorizing the variable as follows: exclusively mental, partially mental, and not mental.
Results: Our analysis shows that individuals who attributed their sleep disturbances solely to their psyche were significantly less likely to seek professional help (AME: −0.158**). These differences remain significant after controlling for the severity of the complaints, their duration, and other covariates (AME: −0.117**). The data also suggest that this group is more likely to seek self-help through medication.
Discussion: The results indicate the importance of focusing healthcare systems and public health policy on sleep-related complaints and their management. The aim is not only to alleviate sleep complaints, but also to reduce the risk of secondary diseases and to identify possible comorbidities. Additionally, it is a factor in reducing safety risks for the general public. Therefore, various measures should be implemented, including destigmatizing, improving health literacy, a more comprehensive offer of cognitive-behavioral therapy (CBT-I), and a more thorough examinations by physicians.
1 Introduction
Sleep-related complaints are prevalent phenomenon in modern societies. In many countries, approximately one-third of adults reporting symptoms (1–3). Symptoms can be dissatisfaction with quality or quantity of sleep, daytime sleepiness, and problems in initiating or maintaining sleep (4). Several studies have identified negative effects of sleep deprivation, such as an increased risk of memory problems, coronary heart disease, type 2 diabetes, cognitive impairment and accidents (5–9). According to these and other studies, sleep complaints reduce individual and societal health and well-being, increase healthcare costs, and have a negative impact on productivity (10–12).
Despite the high individual and societal costs, studies show that the step of seeking professional help for sleep complaints is very rarely taken. In Canada, for instance, the use of professional help for sleep-related complaints is as low as 13% (2). One possible explanation for this behavior could be that sleep complaints often have a psychological cause (13, 14). It is argued that the rate of help-seeking in cases of mental health issues is relatively low especially for the older adults (15–17). This, in turn, could be related to the stigmatization that still surrounds mental health issues (18).
A number of studies have identified stigmatization as a major barrier to healthcare utilization (19–21). While stigmatization and healthcare utilization in general is well studied, less is known about why people with sleep-related complaints rarely seek professional help. We hypothesize that underutilization in case of sleep complaints are related to a perceived stigmatization of mental health problems (22). In alignment with the findings of Stolzenburg et al. (23), which indicate that individuals with an untreated depressive syndrome who do not have a biomedical explanation for their symptoms tend to have a lower utilization rate, we formulate the following research question in relation to sleep complaints: Are individuals experiencing sleep-related complaints less likely to seek professional help if they perceive the underlying cause to be psychological?.
To answer this question, we use a quantitative data set that includes middle-aged and older adults with sleep complaints (24). This group is distinguished by a high prevalence of sleep disorders and a notable reluctance to utilize services for mental health impairments (25, 26). The objective of this study is to enhance understanding of the low utilization of professional help for sleep complaints and to highlight potential strategies that could facilitate an increase in such utilization. This could contribute to more appropriate treatment and an enhanced quality of life for those affected, as well as increased productivity for society as a whole and a reduction in the risk of accidents.
1.1 Help-seeking theory
According to the theory of help-seeking in case of sickness (27), the use of professional help is the final stage of the help-seeking process. Whether these steps are taken and how long it takes to take the single steps depends on many different factors. Andersen’s Behavioral Model of Health Services is considered a well-established analytical basis for explaining help-seeking behavior (28–30). Basically, it distinguishes between three factors that influence the decision to seek help. These are predisposing factors, enabling resources, and need. Predisposing factors are individual characteristics that exist before or independently of the occurrence of a particular episode of illness. These indirect factors are primarily demographic and socio structural such as gender, age, education, occupation, and ethnicity. In addition, Andersen includes general (health) attitudes and health awareness. Even if there is a belief that a physician’s treatment could help, there are preconditions for seeking care in the first place. For example, there may be some costs associated with seeking care, which requires the availability of financial resources. Enabling resources include above all the financial aspects or the type of health insurance. The accessibility of healthcare providers may also play a role, for example, if the density of healthcare providers is lower in rural than in urban areas. The most direct influence on decision making is the disease itself (need). In order to have a need, the disease must first be perceived, and its extent and severity determined. Sufferers can assess this, for example, by the extent of their daily impairment. The exact description of how we operationalized the factors in our analysis is given in the Methods section. Before, we discuss in more detail what additional role stigmatization might play in the context of seeking professional help.
1.2 Stigmatization
Goffman describes stigmatization as the process of assigning negative attributes to individuals or groups, thereby discrediting them and denying them social acceptance (31). Today, stigma is used as a sociological and social psychological concept that consists of three components: stereotypes, collective prejudice, and discrimination (32). People are thus devalued and discriminated against on the basis of one or more characteristics. People who are stigmatized usually experience poorer health and quality of life, which sometimes extends to their social environment (33, 34). Health-related stigma accounts for a large part of the research in this area that shows a broad evidence of stigma toward persons with mental illnesses such as schizophrenia and depression (35, 36). A decisive aspect is so-called self-stigmatization. This is a form of stigma in which individuals identify characteristics of themselves that are stigmatized or feel that they belong to a stigmatized group (37). These individuals assume that they do not deserve the same esteem as others and are afraid of being devalued by others, which leads to passive behavior (38). Therefore, stigmatization is considered a key barrier to seeking healthcare services (19–21). It does not only lead to lower utilization but is often accompanied by an increase in health impairments (39, 40). Since sleep-related complaints often have or are associated with a psychological cause (13, 14), this could be a central explanatory factor for low utilization of professional help by certain risk groups.
1.3 Earlier studies
A large number of the factors have been empirically verified in previous studies on help-seeking behavior. Regarding socioeconomic factors, women, younger adults as well as people with higher education are more likely to use the healthcare system (41–43). A crucial factor for help-seeking is the severity of the symptoms. The more severe the symptoms, the more likely it is visiting a professional (44). In the context of attitudes, people who are more likely to agree with self-help beliefs are less likely to use professional help (45).
As already mentioned, it also seems to play a role whether the suffering is perceived as something mental or more physical. An American study revealed that less than 30% of those who met the criteria for a psychiatric diagnosis according to the DSM-IV did actually use professional help (17). Those who know mental health professionals and those who communicate their complaints more openly in turn tend to use professional help significantly more (46). It has been shown that women generally exhibit a more positive attitude toward seeking professional help in case of mental illness and have higher trust in healthcare providers than men (47). Having trust in physicians was found to be a positive factor for seeking professional help in case of mental problems (48). However, when depression is accompanied by physical pain, people are more likely to seek help (49). This, in turn, supports our thesis that help seeking is more likely if there is not solely a mental health problem. Similar to the focus of our research, a study with German respondents examined the causal beliefs of people with an untreated mental illness and help-seeking intentions (23). The results of this study demonstrate that the intention to seek professional help is highest when the perceived cause is biomedical and is significantly lower for person-related causes, childhood trauma, stress, and unhealthy behaviors (23).
There is also some scientific research in the context of sleep-related complaints. Studies show that one third of the Canadian population and over 50 percent of the Italian population suffer from sleep complaints (2, 50). There is also evidence of an increase in prevalence during the pandemic (51). In general sleep-related complaints are positively correlated with aging (52), being female, having a low household income, lower education, and physical as well as psychological problems (53). However, only one out of ten of the affected use professional help (2). People significantly seek more professional help if they have higher education (54). The severity of the impairment also plays an important role here. People who report having daytime impairment due to their sleep complaints, tend to seek professional help more often than people without daytime impairment (54).
In the rare case that people seek professional help for their sleep complaints, they are often treated with prescription drugs (50, 55). In contrast to this, the image of the best possible “natural sleep” without any aids persists (56). Another way are self-help strategies. In a Chinese study 32% of the respondents with sleep-related complaints reported self-help strategies like relaxation and reading (57). Women are more likely to try self-help methods for dealing with their sleep-related complaints whereas men are more likely to use medication (58, 59).
Despite the extensive literature on this topic, we are unaware of any studies that have examined the influence of perceived cause on help-seeking behavior for sleep-related complaints. Such research is important to understand why and in which cases people tend to prefer to not seek professional help, although there are numerous health-related consequences for untreated sleep complaints. In the field of psychiatric disorders, illnesses like attention-deficit hyperactivity disorder (ADHD), depression, and bipolar disease are known to be related or accompanied by sleeping difficulties (60, 61). There are effects in both directions. Sleep complaints also affect psychiatric disorders. The relationship between these two groups is complex and bidirectional (62). It has also been shown that people who suffer from sleep-related complaints are prone to other comorbidities. An association has been found between people with sleep complaints and a higher rate of comorbidity with conditions such as anxiety-depressive disorders, other psychiatric disorders, chronic pain, and cardiovascular diseases (50, 63). Sleep deprivation also correlates with weight gain, increased risk of diabetes type 2, dementia, cognitive impairment and car accidents (8, 9, 64–66). For example, 24 h of sleep deprivation leads to cognitive impairment similar to a blood alcohol concentration of 100 mg/dL (67).
Research results point out the massive consequences of sleep-related complaints for the individual patient, for the society, and the healthcare system. This highlights the importance of examining sleep complaints and help-seeking behavior and especially an understanding of fundamental parameters that influence the help-seeking behavior like the perceived cause. If these parameters and causes are identified, organizational and structural adjustments may lead to better access and treatment of people with sleep complaints.
2 Materials and methods
2.1 Sample
The data basis for this study is the Healthcare-seeking in Germany (HEALSEE) survey (24). This representative survey provides detailed information on the decision-making behavior in the event of illness and the use of healthcare services by people aged between 40 and 75 in Germany. The sample is composed of 3,000 individuals who were selected through a multi-stage random process utilizing a dual-frame approach, whereby synthetic telephone numbers were generated. The computer-assisted telephone interviews (CATI) of the persons took place between April and August 2015. The focus of the study was on how people respond to and make decisions in the case of back pain, digestive complaints, and sleep complaints.
All participants were first asked whether they had back pain, digestive complaints, or sleep-related complaints in the past 3 months. If none of these applied, these individuals were classified as respondents with no symptoms. The exact question for recording sleep complaints was as follows: “Have you had problems falling asleep, trouble sleeping through the night, or an excessive need to sleep at least once in the last three months?.” This was followed by a measure of the frequency of the problem(s), with the response options once, now and then, and more often/regularly. In the case of the presence of more than one of the complaints mentioned, the classification was made based on what the respondents described as their most frequent symptom. If the frequency was also equal, the complaints referred to in the following survey was chosen at random. It should be noted that the data presented in this study are based solely on self-reports and did not include prior or further diagnostic procedures, such as clinical interviews or medical examinations. Participants were then asked specific questions about the symptom, how they deal with the symptom, health attitudes, health literacy, data on general health and their social network. Furthermore, socioeconomic characteristics were surveyed as well as institutional factors such as insurance status and distance to the next general practitioner. Since it is in our interest to investigate the utilization behavior of persons with sleep-related complaints, all persons belonging to the other symptom groups or to the group without symptoms are excluded from the analysis. The result is an initial sample size of 761 respondents.
2.2 Variables
This chapter provides a comprehensive account of the operationalization of the variables employed in the study. In addition to the dependent variable of the utilization of professional help and the perceived cause as the central predictor, the other explanatory factors are derived from the Behavioral Model of Health Services, which was presented in section 1.1.
2.2.1 Utilization of healthcare services (DV)
The respondents were presented with a whole range of possible interventions and were asked which of these they had already taken in response to the complaints. In addition to low-threshold measures such as the use of a home remedy or an internet search, the surveyed interventions ranged all the way to physician visits. The last one is covered by the questions whether a family physician, a specialized physician, a hospital/emergency room, or a psychologist/psychotherapist was ever consulted due to the symptoms. The four binary variables were again combined into one dummy variable. As soon as a person has ever contacted or visited one or more of the four provider groups because of his or her sleep complaints, this is considered as seeking professional help.
2.2.2 Cause of the symptoms (central IV)
The cause of the complaints serves as the central explanatory factor. The introductory question was as follows: “To what cause(s) do you yourself attribute your sleep disturbances?.” The respondents were given several possible causes and could also add additional reasons. The open statements were taken into account in the generation of the variable. First, however, these were checked to ensure that the information did not reflect one of the predefined categories. In this case, the information was post-coded. Among other things, it was asked whether mental problems are a possible cause. The exact wording of this question was as follows: “Do you attribute your sleep complaints to poor mental health, such as stress, worries or family problems?” In order to be able to check the extent to which people who suspect a mental cause for their complaints show a different utilization behavior, we created a variable with three values. It distinguishes between people who see only mental health problems as the cause, those who see mental health problems as one of two or more causes, and those who see one or more causes other than mental health. This offers the possibility to differentiate whether the mental aspect is seen as a partial or the sole reason.
2.2.3 Need (symptom severity and duration)
As further important covariates, we consider the perceived daily impairment by the complaints and its duration. The severity of the symptoms is expressed on a five-point scale from “not at all” to “very much,” with intermediate gradations. When being asked for how long the symptoms have already persisted, it was possible to give an exact date. The dispersion of the resulting variable is highly right skewed, therefore we use the logarithm.
2.2.4 Predisposing factors
We also control for general sociodemographic characteristics and health-related networks. We use education in the form of the highest school-leaving qualification, gender, migration background, and age. For age, the regression diagnostics showed that there is a curvilinear relationship. For this reason, the quadratic term of the age variable was also included. To adequately account for the presence of networks within healthcare, people were asked how easy it is for them to find someone who could recommend a physician. Originally, the variable had four values, but due to the small number of people for whom it is “not” or “not so easy” to get a recommendation, these two categories were combined. Also, a binary variable is included, which contains the information whether there is a psychologist and or doctor in the circle of family, friends, or acquaintances. To capture how people deal with health complaints as well as general problems, we consider several attitudinal questions. For the openness of dealing with symptoms, we take the number of people they have told about the complaints as an indicator. Furthermore, the competence of general practitioners, specialists, and psychologists with regard to one’s own complaints is provided. Since the dependent variable of utilization includes all three professions, a new variable was formed corresponding to the highest competency score in each case. A high score means that at least one profession is rated as competent to alleviate one’s own symptoms. In addition, on a four-point scale from “Do not agree at all” to “Agree completely,” the general handling of problems (in the following, deliberation) was recorded on the one hand and the handling of pain and other symptoms (in the following, self-determination) on the other hand. In the first case, a high level of agreement means that one first looks at a problem in detail before making a decision on how to deal with it. In the case of the second, agreement expresses that one first tries to always immediately want to know the cause of health problems.
2.2.5 Enabling resources
To account for differences in utilization due to a lower coverage rate, the distance to the primary care physician as well as to the nearest hospital is added. Another institutional factor considered is the type of health insurance (statutory health insurance or private health insurance). For instance, patients with private health insurance have a shorter average waiting time for specialist appointments (68). A detailed overview of the descriptive statistics for the variables is provided in Table 1.
2.3 Analytical strategy
Due to the nature of the dependent variable, a logistic regression is performed as follows. A total of three models are estimated, first a simple model with utilization as the dependent variable as well as the type of cause, the severity, and the duration of the symptoms (need). The second model also takes predisposing factors such as sociodemographics, personal health network and attitudes into account. The last model also includes enabling resources. In this way, it can be ensured whether the suspected correlation is still evident when controlling for already known influencing factors. Moreover, an additional logistic regression model was calculated for all individuals who indicated that they had never sought professional help for their sleep complaints. This model included medication use as the dependent variable. The specific question posed was, “Have you ever taken or used any medication to alleviate your sleep complaints?” The same variables were used as explanatory factors as in the final model for utilization. Instead of odds ratios, Average Marginal Effects (AME) are reported as this allows easier interpretation and better comparability of the coefficients between tested models (69). In this particular context, the AMEs illustrate the average change in the probability of utilization in relation to an increase of one unit in the respective independent variable. Due to the large number of variables used, there are observations that have to be excluded due to missing values. Of the 761, a total of 618 (81%) persons have valid values for all variables. All analyses were performed using STATA 18 (StataCorp LLC).
3 Results
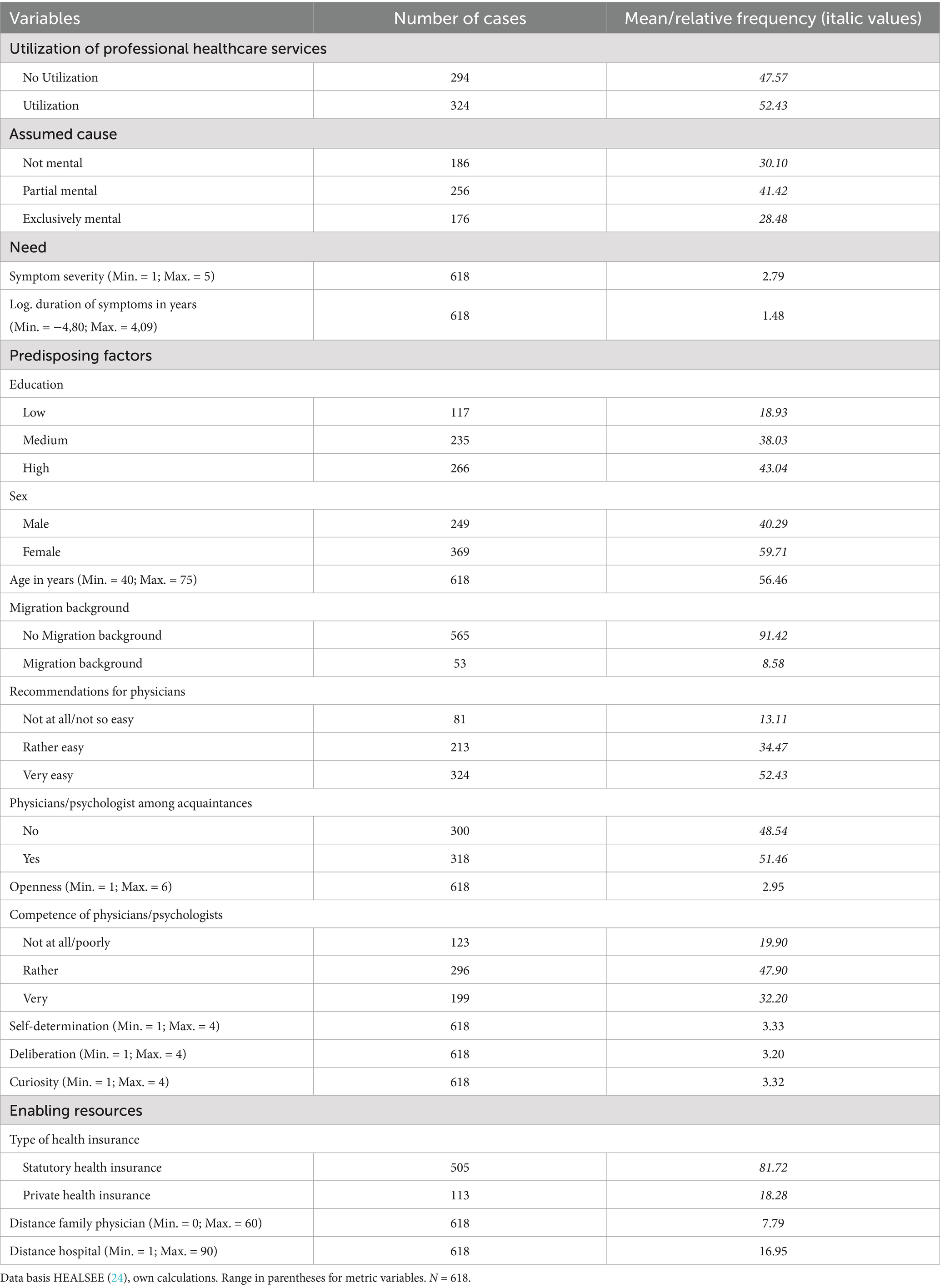
We begin with an overview of the dependent as well as the central independent variable. Figure 1 shows the level of use of professional help depending on the suspected cause. With about 52% (95% CI = 48.48 to 56.38), more than half of the respondents have consulted professional help for their sleep complaints. About 48% had not yet consulted professional help. There are considerable differences depending on the suspected cause. People who do not assume that their mental health is involved have used professional help slightly more frequently than average (53%; 95% CI = 46.02 to 60.43). The percentage is even higher (58%; 95% CI = 52.54 to 64.65) among those who assume that psychological problems play a role but that there are other causes as well. There is a large difference of 10, respectively, 16 percentage points compared with people with an exclusively mental cause (43%; 95% CI = 35.27 to 49.95). The considerable mean differences between this group and the other two groups are also statistically significant. With regard to the research question, this first simple comparison of mean values already shows clear differences depending on the suspected cause. As anticipated, the group that suspects an exclusively mental cause reported the lowest level of utilization.
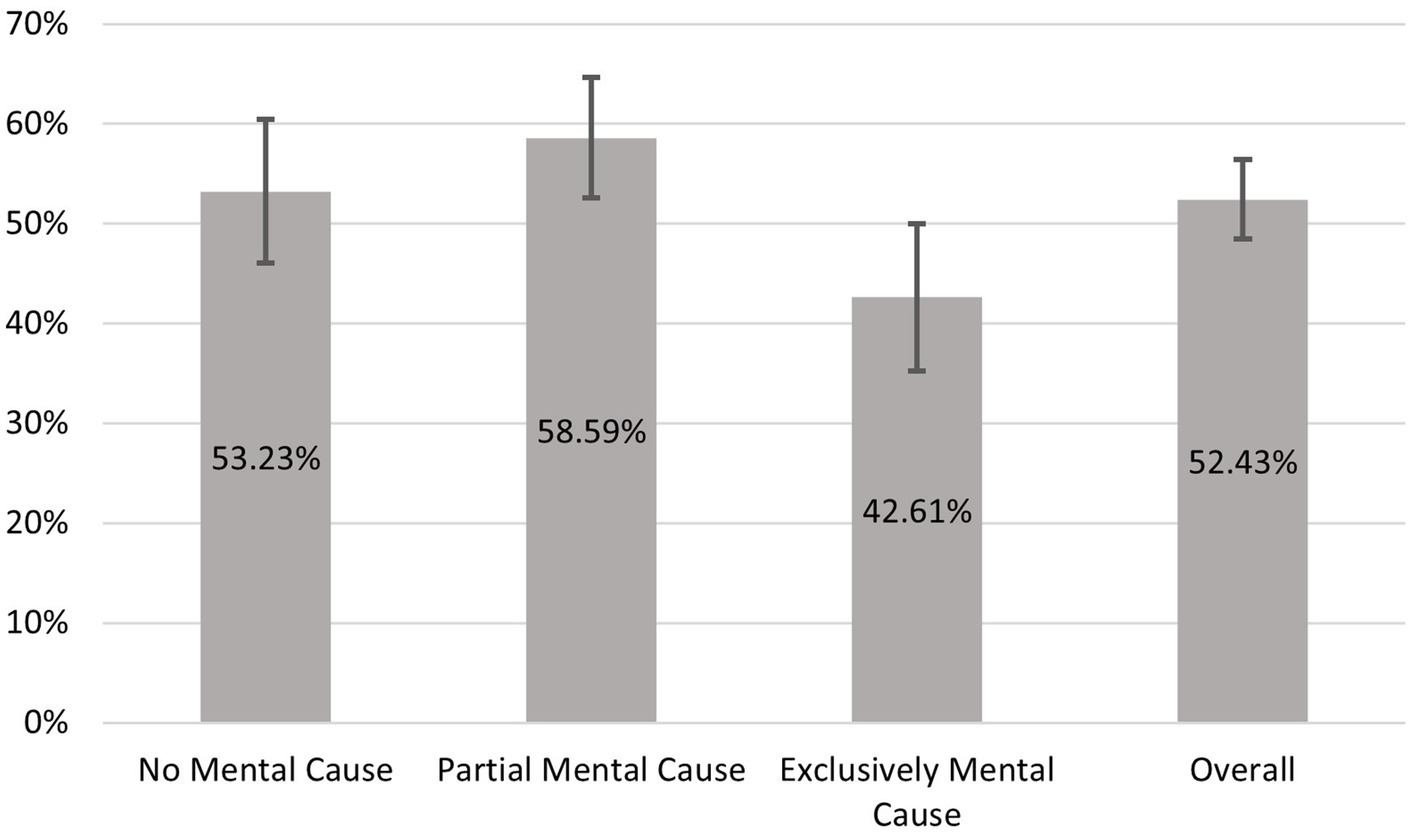
Figure 1. Utilization depending on the assumed cause of the symptoms. Data basis HEALSEE (24), own calculations. N = 618.
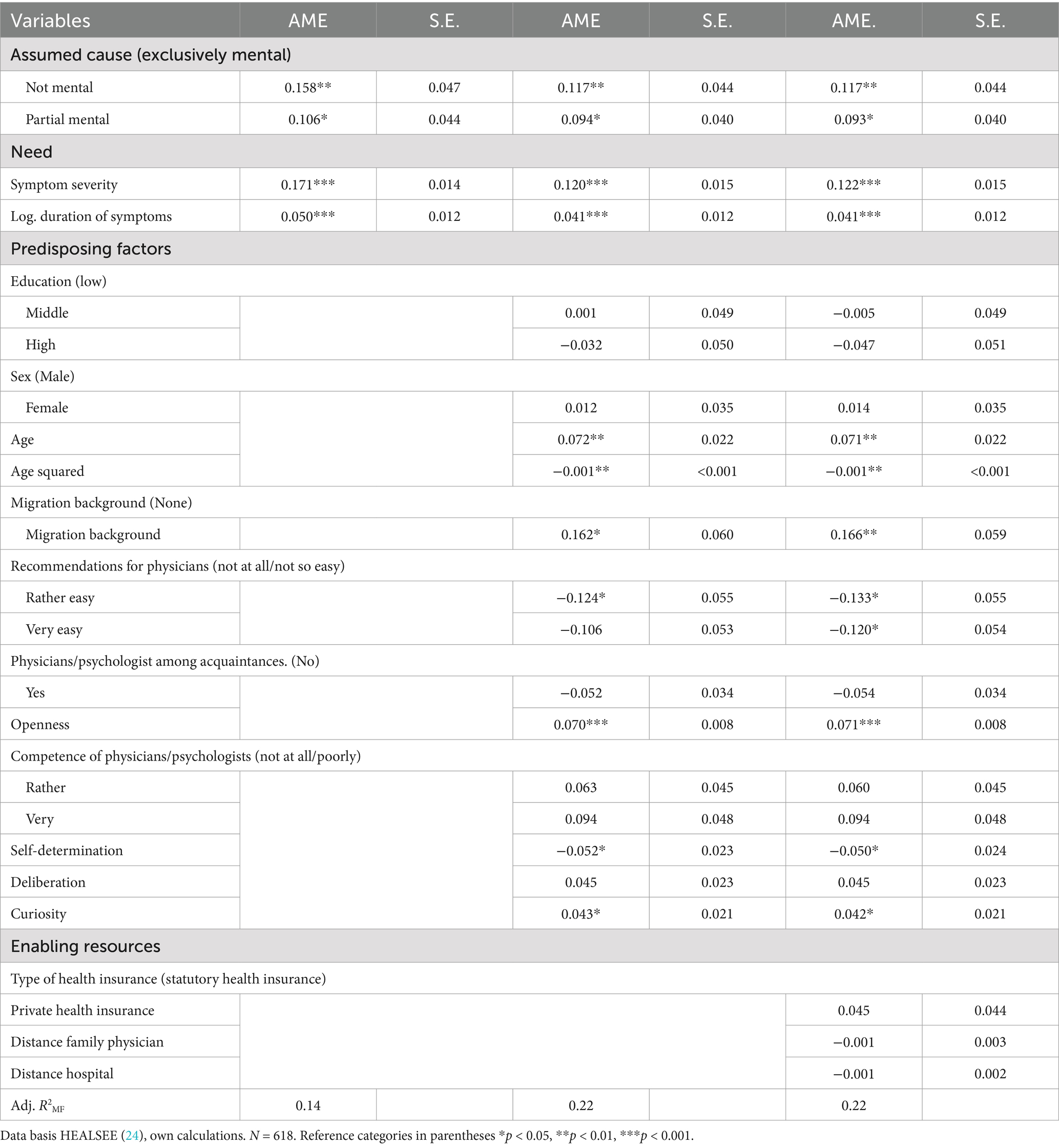
The results of the multiple logistic regression illustrate the extent to which these differences persist or change when controlling for other variables (see Table 2). The first model includes, in addition to the cause, the symptom severity and duration as covariates. Even controlling for these two additional factors, there is a significant difference between the reference category (exclusively mental) and not or partial mental. However, the largest difference from the reference category is not partial mental, as in the descriptive statistics, but not mental. More specifically, the probability of utilization is approximately 16% higher when it is assumed that no mental component is involved (AME: 0.158; p < 0.01). Furthermore, as expected, the probability of seeking help increases with increasing impairment (AME: 0.171; p < 0.001). The same applies to the duration (AME: 0.050; p < 0.001). The longer a person has complaints, the more likely it is that he or she is consulting professional help.
The second model also takes into account socio-demographic variables as well as relevant network and attitudinal variables of the individuals. The difference between an exclusively psychological cause and the other manifestations nevertheless remains stable and continues to be significant (Not mental - AME: 0.117; p < 0.01; Partial Mental - AME: 0.106; p < 0.05). The same applies for the duration and severity of the complaints. Of the sociodemographic variables, age and migration background are statistically relevant. Persons with a migration background have a significantly higher utilization level. For age, there is a curvilinear relationship. This means that with increasing age, the probability of utilization initially increases until this effect weakens and decreases again at an advanced age. Of the other predictors included in the second model, openness in dealing with sleep-related complaints in particular contributes to explaining the different utilization behavior. The more openly and with the more people one talks about it, the more likely one is to use professional help. Always wanting to know the exact cause as soon as one is confronted with health complaints also leads to an increase, whereas high self-determination seems to be an inhibitor. A network of contacts in the healthcare system is not conducive to seeking professional healthcare for sleep-related complaints, at least when other variables are taken into account. The possibility to get recommendations for doctors without problems even has a significant negative effect.
In the third model, we additionally control for the institutional characteristics of the respondents. The addition changes the previous effects only marginally. Moreover, none of them has a significant impact on the dependent variable. Thus, the institutional factors used in our analysis seem to play a minor role. In consideration of the research question, it can be stated that even when known factors are taken into account, the perceived cause also contributes significantly to the explanation of help-seeking behavior for sleep complaints.
In order to gain a more accurate understanding of the extent to which there is a genuine risk of underuse, we examine whether the discrepancy in seeking professional assistance is also evident in cases of severe complaints or whether the observed effect is largely attributable to the reluctance of individuals with only mild complaints to seek help if they suspect a psychological cause. Figure 2 displays the predicted probabilities for the three cause groups for all five degrees of impairment. For all severity levels, the probability of utilization is highest for those without any mental health involvement. For those with partial involvement, the values are only minimally lower and never significantly different. For people with an exclusively psychological cause, however, the predicted values are significantly lower. Although the magnitude of the differences decreases somewhat with increasing impairment, it does so only slowly. For example, the probability of utilization in the case of a moderate impairment of everyday life due to the complaints for people with no or only partial involvement of their mental health is still around 60% and that of those with exclusively mental health problems is 47%. In the case of very severe complaints, the differences become smaller and the difference between a partial mental involvement and an exclusively mental cause can no longer be statistically confirmed on the highest level of complaints. However, even then there is a difference of almost 10 percentage points. In addition, the other values differ significantly from each other, even if the symptoms have a strong negative effect on coping with everyday life.
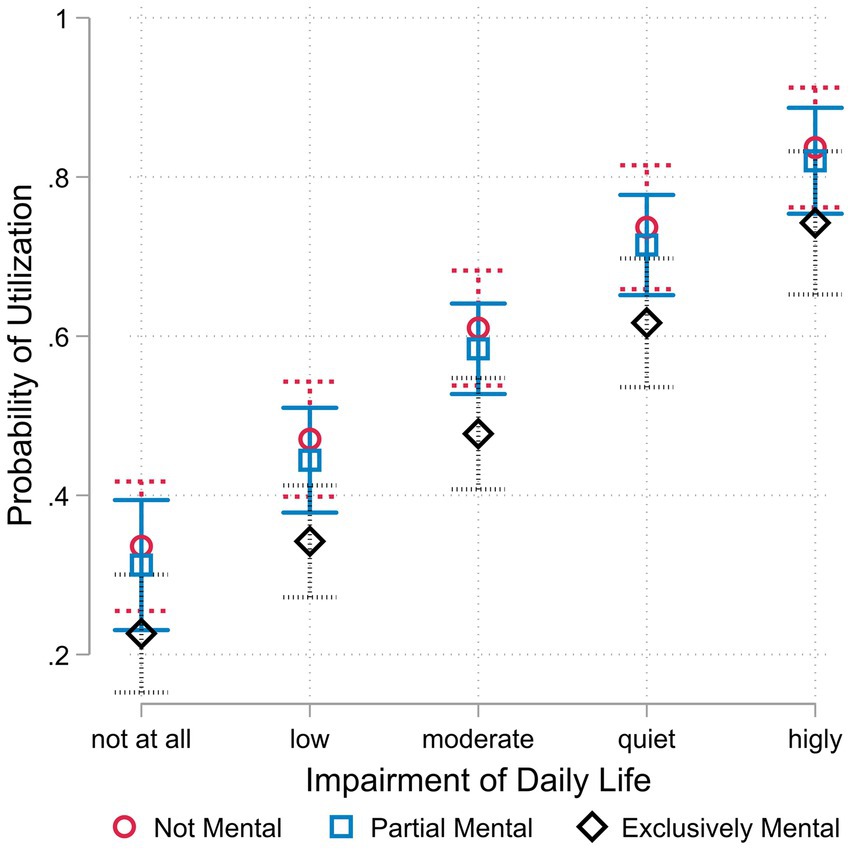
Figure 2. Predicted probability of utilization by cause and severity of symptoms. Data basis HEALSEE (24), own calculations. N = 618; 95%- Confidence intervals.
Our findings indicate a risk of undertreatment of sleep complaints in individuals who consider their mental health to be causal. The fact that the differences in utilization persist even with very severe complaints once again underlines the problem. However, it is still unclear to what extent self-medication may be occurring in addition to the risk of underuse. The results of the logistic regression, with the intake of medication as the dependent variable, are presented in Figure 3. It can be observed that individuals who hypothesize an exclusively psychological cause are the most likely, at approximately 28.5% (95% CI = 19.96 to 36.89), to have previously taken medication for their symptoms. For those without a psychological cause, the share is less than a quarter (95% CI = 15.92 to 33.93), and for those with a partial cause, it is only 22% (95% CI = 14.75 to 29.70). In addition to underuse, there also appears to be a risk of medication misuse for people with sleep problems, especially if they suspect a mental cause. It should be noted, however, that the differences are not significant and the confidence intervals are quite large. One reason for this is the small number of cases (N = 275) for this model.
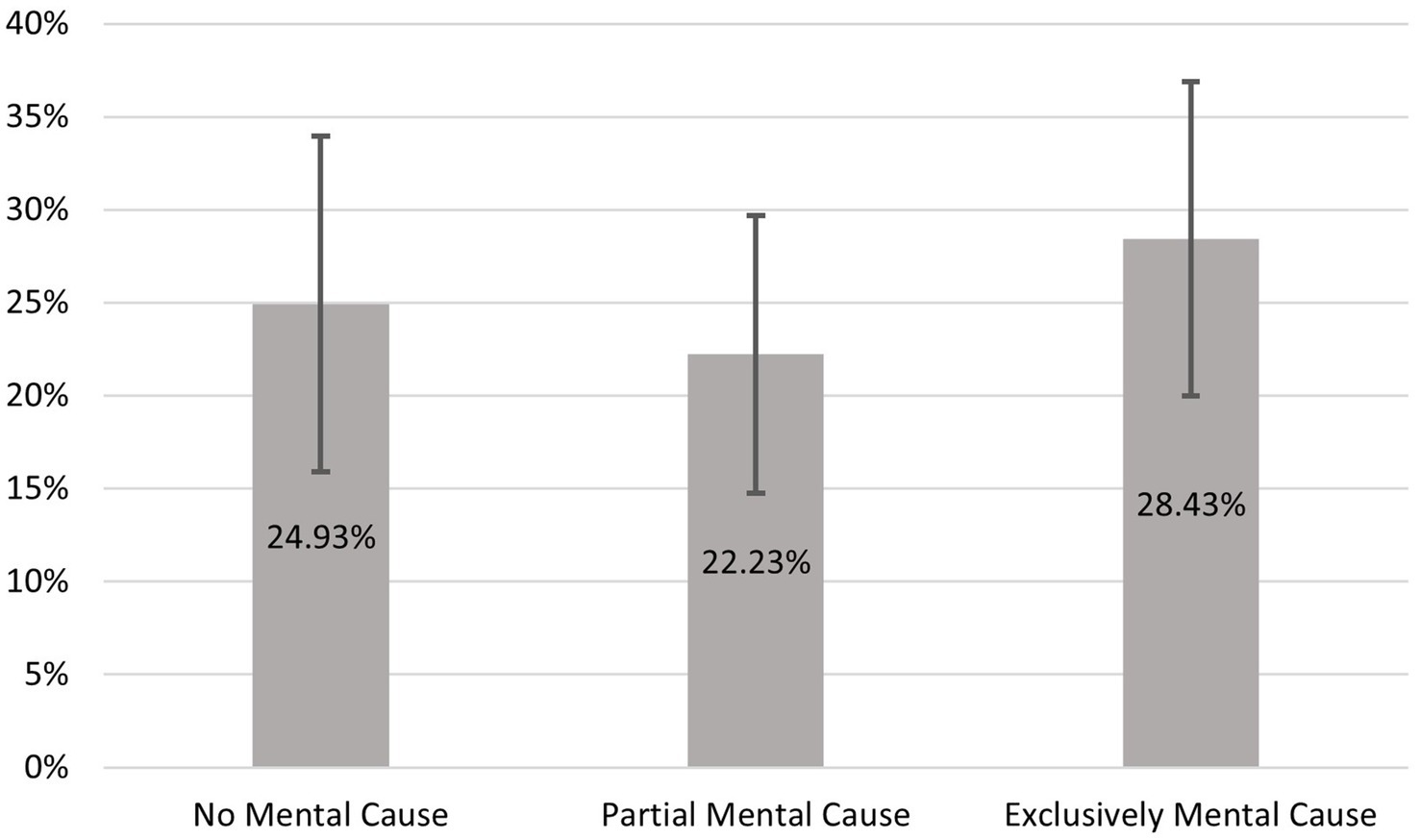
Figure 3. Predicted probability of medication use of individuals who did not seek professional help. Data basis HEALSEE (24), own calculations. N = 275; 95%- confidence intervals.
4 Discussion
The objective of this analysis was to examine whether there is a difference in help-seeking behavior for sleep-related complaints if the underlying cause is assumed to be psychological. First of all, the results show that the help-seeking behavior for sleep complaints is slightly higher than 50%, regardless of the assumed cause. This finding is consistent with previous results (54), although there are also studies that have identified significantly lower utilization rates (2). One potential explanation for this discrepancy is the use of disparate operational definitions and country-specific factors. In relation to the research question, the study provides significant results. While individuals who perceive a non-mental or only partially mental cause for their sleep complaints are more likely to engage in higher levels of help-seeking behavior, there is a significantly lower use of health services for sleep disorders due to mental reasons. This underlines the results of previous studies which have shown that the use of professional help for mental health problems is often quite low (16, 17). One crucial factor contributing to this phenomenon is the stigmatization of mental illnesses. As proven in several studies, stigmatization is a major barrier to healthcare utilization (19–21). This problem, including medical gaslighting of mental health issues, is particularly serious for certain population groups such as women and minorities (70). If patients experience stigmatization and as a consequence remain untreated, the result could be underutilization of necessary treatment (71). The findings of our study indicate that these discrepancies in help-seeking behavior were evident even in cases of severe symptoms. Furthermore, there were indications that people who perceive the cause as psychological are the individuals who increasingly take medication on their own. Self-medication might be a risky method for dealing with sleep complaints, because there is an unknown efficacy and safety of herbal and non-prescription medications (72). This leads us to conclude that there is a need for measures that encourage people to seek professional help for sleep problems. It is important to resolve this discrepancy between having sleep complaints and dealing with it professionally, especially in view of the personal impairment, health risks and possible co-morbidities (50, 63).
4.1 Policy recommendations
We suggest the implementation of measures that remove the personal barriers that are felt through the ongoing stigmatization of mental health issues within society. Stigma results in the alteration of a person’s image simply by virtue of a characteristic such as mental illness (37). Presenting a holistic picture of a person in the media can lead to destigmatization, as not just the characteristic effects of the mental health illness is drawn (73). In addition to destigmatization, improving mental health literacy is another important factor in removing personal barriers to seeking help for mental health problems. Knowing about the symptoms, the treatment and help-seeking sources can improve the possibility for help-seeking (74).
Not only is it important to find a solution to the gap in help-seeking behavior due to the perceived cause, but also to find a way to engage and collect those people who have not yet taken the next step to professional help. This is particularly important in view of the fact that longer working hours make it more difficult for women to utilize health services, which could make the situation even more problematic in the future (75). There are two levels that should be addressed in regard to resolve the discrepancy between sleep-related complaints and dealing with it professionally. The first is the help seeking behavior itself. Although there are predictors which increase the probability to seek professional help such as severity and duration, openness and age, the access to professional help needs to be made more low-threshold. Cognitive-behavioral therapy (CBT-I) and cognitive-behavioral self-help therapy (Digital CBT-I) are treatment methods, which fulfill these requirements. (d)CBTI is recommended as first-line treatment of sleep complaints by the American College of Physicians and has been adopted by European countries. The efficacy of this approach has been validated, and it can achieve relatively quick results (76, 77). Both CBT-I and dCBT-I consist of different strategies as sleep restriction, stimulus control and cognitive reappraisal (78). In contrary to CBT-I which is provided through face-to-face individual or group treatment, dCBT-I is the digital version of this program and entirely self-directed. While CBT-I has indicated superior outcomes, dCBT-I is also beneficial for sleep complaints (79). Studies illustrate that CBT-I is as effective as sedative medication during acute treatment of 4–8 weeks (80) and is more effective in the long run (81). Positive experiences with dCBT-I could lead people to a more open mindset about mental health and encourage them to seek further psychological help. We further suggest that conversations should be initiated by the physician in order to shift the burden of individual responsibility of the patient to the systematic assessments by healthcare professionals. When seeing physicians, patients often state physical pain, but as physicians become more aware of impairments like sleep complaints and their side effects, the physicians should proactively address the topic themselves (55). This additional engagement by physicians would mean an increase in time, effort and consequently costs, but in the long-term this may lead to a decrease in the high costs for the economy and society (10, 82, 83).
The second level is to address the society. As long as sleep complaints are not regarded as an important health problem, people will not take them seriously. We advocate for a common awareness of the illness and its consequences (64, 66). Placing this information in media, such as social media, news, films or series, where it can be accessed by almost everyone, can be a way of raising awareness (84). Given that general practice surgeries and treatment centers are the initial point of contact for individuals experiencing health-related issues, they can serve as a conduit for disseminating informational leaflets pertaining to specific symptoms and potential treatment options for sleep-related complaints.
After all, it is not just one thing that needs to be changed, but several measures at different levels that need to be addressed in order to increase help-seeking behavior not only for mental but also for partially mental and non-psychological causes.
4.2 Limitations
It is evident that the data set, while representative, is limited in that it refers only to individuals from Germany between the ages of 40 and 75 years. Therefore, it is not possible to transfer the results in a one-to-one manner to other countries or age groups. In addition, the analyzed data are cross-sectional, which, in contrast to panel data, precludes the possibility of inferring causal effects. Moreover, the data set exclusively contains information on individuals who had registered complaints within the three-month period preceding the survey. While this approach excludes individuals with complaints from longer ago, it mitigates the potential for recall bias. It is also crucial to highlight that no clinical interviews or other medical examinations were conducted to verify the reported symptoms. Instead, the data was based solely on self-reports made via telephone. One of the study’s key strengths is its comprehensive consideration of the numerous factors that influence help-seeking behavior, which reduces the risk of obtaining distorted results due to a lack of consideration. It must be acknowledged, however, that the model cannot be considered complete.
5 Conclusion
More and more people are affected by mental health problems (85). This is a growing societal and economic problem as indicated by the number of working days lost due to mental illness that in Germany increased by 56% between 2010 and 2020 (85). Sleep complaints and related mental health problems are a growing burden for individuals, the economy, and the society as a whole. Our study suggests that stigmatization plays a key role in utilization. Therefore, better solutions on how to identify and solve sleep complaints are highly required. Further research should therefore focus more on the possible stigmatization and expand existing explanatory models of utilization behavior to include this factor. This may, in turn, facilitate the identification and reduction of potential instances of underuse and misuse of medication. In addition, however, it should also be investigated what the treatment looks like when professional help is sought and whether the approach is adequate.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: https://search.gesis.org/research_data/ZA5248.
Ethics statement
Ethical review and approval was not required for this study in accordance with the local legislation and institutional requirements.
Author contributions
LR: Conceptualization, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. TS: Data curation, Investigation, Methodology, Writing – original draft, Writing – review & editing, Formal analysis, Software, Visualization. CW: Data curation, Investigation, Methodology, Writing – original draft, Writing – review & editing, Conceptualization, Funding acquisition, Project administration, Resources, Supervision.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. The research was funded by the German Research Association DFG with the grant number 214418620.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Roth, T, Jaeger, S, Jin, R, Kalsekar, A, Stang, PE, and Kessler, RC. Sleep problems, comorbid mental disorders, and role functioning in the national comorbidity survey replication. Biol Psychiatry. (2006) 60:1364–71. doi: 10.1016/j.biopsych.2006.05.039
2. Morin, CM, LeBlanc, ML, Daley, M, Gregoire, J-P, and Mérette, C. Epidemiology of insomnia: prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Med. (2006) 7:123–30. doi: 10.1016/j.sleep.2005.08.008
3. Dopheide, JA. Insomnia overview: epidemiology, pathophysiology, diagnosis and monitoring, and nonpharmacologic therapy. Am J Manag Care. (2020) 26:S76–84. doi: 10.37765/ajmc.2020.42769
4. American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. Arlington, VA: American Psychiatric Association (2013).
5. King, CR, Knutson, KL, Rathouz, PJ, Sidney, S, Liu, K, and Lauderdale, DS. Short sleep duration and incident coronary artery calcification. JAMA. (2008) 300:2859–66. doi: 10.1001/jama.2008.867
6. Spiegel, K, Knutson, K, Leproult, R, Tasali, E, and van Cauter, E. Sleep loss: a novel risk factor for insulin resistance and type 2 diabetes. J Appl Physiol. (2005) 99:2008–19. doi: 10.1152/japplphysiol.00660.2005
7. Alhola, P, and Polo-Kantola, P. Sleep deprivation: impact on cognitive performance. Neuropsychiatr Dis Treat. (2007) 3:553–67.
8. Gottlieb, DJ, Ellenbogen, JM, Bianchi, MT, and Czeisler, CA. Sleep deficiency and motor vehicle crash risk in the general population: a prospective cohort study. BMC Med. (2018) 16:44. doi: 10.1186/s12916-018-1025-7
9. Brachem, C, Winkler, A, Tebrügge, S, Weimar, C, Erbel, R, Jöckel, K-H, et al. Associations between self-reported sleep characteristics and incident mild cognitive impairment: the Heinz Nixdorf recall cohort study. Sci Rep. (2020) 10:6542. doi: 10.1038/s41598-020-63511-9
10. Rosekind, MR, and Gregory, KB. Insomnia risks and costs: health, safety, and quality of life. Am J Manag Care. (2010) 16:617–26.
11. Chattu, VK, Sakhamuri, SM, Kumar, R, Spence, DW, BaHammam, AS, and Pandi-Perumal, SR. Insufficient sleep syndrome: is it time to classify it as a major noncommunicable disease? Sleep Sci. (2018) 11:56–64. doi: 10.5935/1984-0063.20180013
12. Wickwire, EM, Shaya, FT, and Scharf, SM. Health economics of insomnia treatments: the return on investment for a good night's sleep. Sleep Med Rev. (2016) 30:72–82. doi: 10.1016/j.smrv.2015.11.004
13. Harvey, AG, Murray, G, Chandler, RA, and Soehner, A. Sleep disturbance as transdiagnostic: consideration of neurobiological mechanisms. Clin Psychol Rev. (2011) 31:225–35. doi: 10.1016/j.cpr.2010.04.003
14. Baglioni, C, Nanovska, S, Regen, W, Spiegelhalder, K, Feige, B, Nissen, C, et al. Sleep and mental disorders: a meta-analysis of polysomnographic research. Psychol Bull. (2016) 142:969–90. doi: 10.1037/bul0000053
15. Heinig, I, Wittchen, H-U, and Knappe, S. Help-seeking behavior and treatment barriers in anxiety disorders: results from a representative German community survey. Community Ment Health J. (2021) 57:1505–17. doi: 10.1007/s10597-020-00767-5
16. Volkert, J, Andreas, S, Härter, M, Dehoust, MC, Sehner, S, Suling, A, et al. Predisposing, enabling, and need factors of service utilization in the elderly with mental health problems. Int Psychogeriatr. (2018) 30:1027–37. doi: 10.1017/S1041610217002526
17. Byers, AL, Arean, PA, and Yaffe, K. Low use of mental health services among older Americans with mood and anxiety disorders. Psychiatr Serv. (2012) 63:66–72. doi: 10.1176/appi.ps.201100121
18. Aydin, N, and Fritsch, K. Stigma und Stigmatisierung von psychischen Krankheiten. Psychotherapeut. (2015) 60:245–57. doi: 10.1007/s00278-015-0024-9
19. Fox, AB, Smith, BN, and Vogt, D. How and when does mental illness stigma impact treatment seeking? Longitudinal examination of relationships between anticipated and internalized stigma, symptom severity, and mental health service use. Psychiatry Res. (2018) 268:15–20. doi: 10.1016/j.psychres.2018.06.036
20. Mahajan, AP, Sayles, JN, Patel, VA, Remien, RH, Sawires, SR, Ortiz, DJ, et al. Stigma in the HIV/AIDS epidemic: a review of the literature and recommendations for the way forward. AIDS. (2008) 22:S67–79. doi: 10.1097/01.aids.0000327438.13291.62
21. Nearchou, FA, Bird, N, Costello, A, Duggan, S, Gilroy, J, Long, R, et al. Personal and perceived public mental-health stigma as predictors of help-seeking intentions in adolescents. J Adolesc. (2018) 66:83–90. doi: 10.1016/j.adolescence.2018.05.003
22. Wrigley, S, Jackson, H, Judd, F, and Komiti, A. Role of stigma and attitudes toward help-seeking from a general practitioner for mental health problems in a rural town. Aust N Z J Psychiatry. (2005) 39:514–21. doi: 10.1080/j.1440-1614.2005.01612.x
23. Stolzenburg, S, Freitag, S, Evans-Lacko, S, Speerforck, S, Schmidt, S, and Schomerus, G. Individuals with currently untreated mental illness: causal beliefs and readiness to seek help. Epidemiol Psychiatr Sci. (2019) 28:446–57. doi: 10.1017/S2045796017000828
24. Wendt, C, Reibling, N, and Mischke, M, Böhr D. Healthcare-Seeking in Germany (HEALSEE) GESIS Data Archive, Germany
25. Gulia, KK, and Kumar, VM. Sleep disorders in the elderly: a growing challenge. Psychogeriatrics. (2018) 18:155–65. doi: 10.1111/psyg.12319
26. Gonçalves, DC, Coelho, CM, and Byrne, GJ. The use of healthcare services for mental health problems by middle-aged and older adults. Arch Gerontol Geriatr. (2014) 59:393–7. doi: 10.1016/j.archger.2014.04.013
27. Becker, MH, and Maiman, LA. Models of health-related behavior In: D Mechanic, editor. Handbook of health, health care, and the health professions. New York: Free Press (1983). 539–68.
28. Aday, LA, and Andersen, R. A framework for the study of access to medical care. Health Serv Res. (1974) 9:208–20.
29. Andersen, R, and Newman, JF. Societal and individual determinants of medical care utilization in the United States. Milbank Mem Fund Q Health Soc. (1973) 51:95–124. doi: 10.2307/3349613
30. Andersen, RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. (1995) 36:1–10. doi: 10.2307/2137284
31. Goffman, E. Stigma: Notes on the management of spoiled identity. Englewood Cliffs, NJ: Prentice-Hall (1963). 147 p.
32. Corrigan, PW, and Watson, AC. Understanding the impact of stigma on people with mental illness. World Psychiatry. (2002) 1:16–20.
33. Alonzo, AA, and Reynolds, NR. Stigma, HIV and AIDS: an exploration and elaboration of a stigma trajectory. Soc Sci Med. (1995) 41:303–15. doi: 10.1016/0277-9536(94)00384-6
34. Corrigan, PW, Druss, BG, and Perlick, DA. The impact of mental illness stigma on seeking and participating in mental health care. Psychol Sci Public Interest. (2014) 15:37–70. doi: 10.1177/1529100614531398
35. Angermeyer, MC, and Matschinger, H. The stigma of mental illness: effects of labelling on public attitudes towards people with mental disorder. Acta Psychiatr Scand. (2003) 108:304–9. doi: 10.1034/j.1600-0447.2003.00150.x
36. Corrigan, P, Markowitz, FE, Watson, A, Rowan, D, and Kubiak, MA. An attribution model of public discrimination towards persons with mental illness. J Health Soc Behav. (2003) 44:162–79. doi: 10.2307/1519806
37. Boyd, JE, Adler, EP, Otilingam, PG, and Peters, T. Internalized Stigma of Mental Illness (ISMI) scale: a multinational review. Compr Psychiatry. (2014) 55:221–31. doi: 10.1016/j.comppsych.2013.06.005
38. Peters, L, Burkert, S, Brenner, C, and Grüner, B. Experienced stigma and applied coping strategies during the COVID-19 pandemic in Germany: a mixed-methods study. BMJ Open. (2022) 12:e059472. doi: 10.1136/bmjopen-2021-059472
39. Link, BG, and Phelan, JC. Stigma and its public health implications. Lancet. (2006) 367:528–9. doi: 10.1016/S0140-6736(06)68184-1
40. Schubert, M, Ludwig, J, Freiberg, A, Hahne, TM, Romero Starke, K, Girbig, M, et al. Stigmatization from work-related COVID-19 exposure: a systematic review with Meta-analysis. Int J Environ Res Public Health. (2021) 18:18. doi: 10.3390/ijerph18126183
41. Boldero, J, and Fallon, B. Adolescent help-seeking: what do they get help for and from whom? J Adolesc. (1995) 18:193–209. doi: 10.1006/jado.1995.1013
42. Schomerus, G, Appel, K, Meffert, PJ, Luppa, M, Andersen, RM, Grabe, HJ, et al. Personality-related factors as predictors of help-seeking for depression: a population-based study applying the behavioral model of health services use. Soc Psychiatry Psychiatr Epidemiol. (2013) 48:1809–17. doi: 10.1007/s00127-012-0643-1
43. Harel, Z, Ehrlich, P, and Hubbard, RW. The vulnerable aged: People, services, and policies. New York: Springer Pub. Co (1990). 318 p.
44. Ingham, J, and Miller, P. Consulting with mild symptoms in general practice. Soc Psychiatry. (1982) 17:77–88. doi: 10.1007/BF00583447
45. Kuhl, J, Jarkon-Horlick, L, and Morrissey, RF. Measuring barriers to help-seeking behavior in adolescents. J Youth Adolesc. (1997) 26:637–50. doi: 10.1023/A:1022367807715
46. Tijhuis, MA, Peters, L, and Foets, M. An orientation toward help-seeking for emotional problems. Soc Sci Med. (1990) 31:989–95. doi: 10.1016/0277-9536(90)90108-5
47. Leong, F, and Zachar, P. Gender and opinions about mental illness as predictors of attitudes toward seeking professional psychological help. Brit J Guid Counsel. (1999) 27:123–32. doi: 10.1080/03069889900760101
48. Thompson, AE, Anisimowicz, Y, Miedema, B, Hogg, W, Wodchis, WP, and Aubrey-Bassler, K. The influence of gender and other patient characteristics on health care-seeking behaviour: a QUALICOPC study. BMC Fam Pract. (2016) 17:38. doi: 10.1186/s12875-016-0440-0
49. Bonnewyn, A, Katona, C, Bruffaerts, R, Haro, JM, Graaf, R d, Alonso, J, et al. Pain and depression in older people: comorbidity and patterns of help seeking. J Affect Disord. (2009) 117:193–6. doi: 10.1016/j.jad.2009.01.012
50. Proserpio, P, Biggio, G, Ferri, R, Girardi, P, Agostoni, EC, Manni, R, et al. Insomnia in primary care: a survey conducted on Italian patients older than 50 years-results from the "Sonno e salute" study. Neurol Sci. (2022) 43:6487–94. doi: 10.1007/s10072-022-06309-z
51. Wong, SY, Zhang, D, Sit, RW, Yip, BH, Chung, RY-N, Wong, CK, et al. Impact of COVID-19 on loneliness, mental health, and health service utilisation: a prospective cohort study of older adults with multimorbidity in primary care. Br J Gen Pract. (2020) 70:e817–24. doi: 10.3399/bjgp20X713021
52. Phillips, B, and Ancoli-Israel, S. Sleep disorders in the elderly. Sleep Med. (2001) 2:99–114. doi: 10.1016/S1389-9457(00)00083-6
53. Bedford, LE, Tang, EH, Dong, W, Wong, CK, Tse, ET, Ng, AP, et al. Who reports insufficient and disturbed sleep? Results from a representative population-based health survey in Hong Kong. BMJ Open. (2022) 12:e058169. doi: 10.1136/bmjopen-2021-058169
54. Aikens, JE, and Rouse, ME. Help-seeking for insomnia among adult patients in primary care. J Am Board Fam Pract. (2005) 18:257–61. doi: 10.3122/jabfm.18.4.257
55. Torrens Darder, I, Argüelles-Vázquez, R, Lorente-Montalvo, P, Del Torrens-Darder, MM, and Esteva, M. Primary care is the frontline for help-seeking insomnia patients. Eur J Gen Pract. (2021) 27:286–93. doi: 10.1080/13814788.2021.1960308
56. Nettleton, S, Meadows, R, and Neale, J. Disturbing sleep and sleepfulness during recovery from substance dependence in residential rehabilitation settings. Sociol Health Illn. (2017) 39:784–98. doi: 10.1111/1467-9566.12528
57. Chung, K-F, Kan, KK-K, and Yeung, W-F. Insomnia in adolescents: prevalence, help-seeking behaviors, and types of interventions. Child Adolesc Ment Health. (2014) 19:57–63. doi: 10.1111/camh.12009
58. Venn, S, Meadows, R, and Arber, S. Gender differences in approaches to self-management of poor sleep in later life. Soc Sci Med. (2013) 79:117–23. doi: 10.1016/j.socscimed.2012.09.037
59. van de Straat, V, Buffel, V, and Bracke, P. Medicalization of sleep problems in an aging population: a longitudinal cross-National Study of medication use for sleep problems in older European adults. J Aging Health. (2018) 30:816–38. doi: 10.1177/0898264317696775
60. Colten, HR, and Altevogt, BM eds. Sleep disorders and sleep deprivation: An unmet public health problem. Washington, DC: Institute of Medicine; National Academies Press (2006). 404 p p.
61. Lacruz, ME, Schmidt-Pokrzywniak, A, Dragano, N, Moebus, S, Deutrich, SE, Möhlenkamp, S, et al. Depressive symptoms, life satisfaction and prevalence of sleep disturbances in the general population of Germany: results from the Heinz Nixdorf recall study. BMJ Open. (2016) 6:e007919. doi: 10.1136/bmjopen-2015-007919
62. Krystal, AD. Psychiatric disorders and sleep. Neurol Clin. (2012) 30:1389–413. doi: 10.1016/j.ncl.2012.08.018
63. Vallières, A, Pappathomas, A, Araújo, T, Crawford, MR, and De, BGS. Who is seeking help for sleep? A clinical profile of patients in a sleep psychology clinic. Int J Behav Med. (2021) 28:207–13. doi: 10.1007/s12529-020-09882-9
64. Al Lawati, NM, Patel, SR, and Ayas, NT. Epidemiology, risk factors, and consequences of obstructive sleep apnea and short sleep duration. Prog Cardiovasc Dis. (2009) 51:285–93. doi: 10.1016/j.pcad.2008.08.001
65. Buxton, OM, Pavlova, M, Reid, EW, Wang, W, Simonson, DC, and Adler, GK. Sleep restriction for 1 week reduces insulin sensitivity in healthy men. Diabetes. (2010) 59:2126–33. doi: 10.2337/db09-0699
66. Robbins, R, Quan, SF, Weaver, MD, Bormes, G, Barger, LK, and Czeisler, CA. Examining sleep deficiency and disturbance and their risk for incident dementia and all-cause mortality in older adults across 5 years in the United States. Aging (Albany NY). (2021) 13:3254–68. doi: 10.18632/aging.202591
67. Dawson, D, and Reid, K. Fatigue, alcohol and performance impairment. Nature. (1997) 388:235. doi: 10.1038/40775
68. Breitenbach, A, and Heinrich, M. Diskriminierung im deutschen Krankenversicherungssystem: Werden gesetzlich Versicherte bei der Terminvergabe von Fachärzten benachteiligt? (2023). Available at:https://nbn-resolving.org/urn:nbn:de:0168-ssoar-85085-2
69. Williams, R. Using the margins command to estimate and interpret adjusted predictions and marginal effects. Stata J. (2012) 12:308–31. doi: 10.1177/1536867X1201200209
70. Sebring, JC. Towards a sociological understanding of medical gaslighting in western health care. Sociol Health Illn. (2021) 43:1951–64. doi: 10.1111/1467-9566.13367
71. Hulka, BS, and Wheat, JR. Patterns of utilization: the patient perspective. Med Care. (1985) 23:438–60. doi: 10.1097/00005650-198505000-00009
72. Bartlett, DJ, Marshall, NS, Williams, A, and Grunstein, RR. Predictors of primary medical care consultation for sleep disorders. Sleep Med. (2008) 9:857–64. doi: 10.1016/j.sleep.2007.09.002
73. Li, Y. From “whom to blame” to “nothing to fear”: documentary narratives, voices, and “dependent destigmatization” of severe mental patients (SMPs) in Hong Kong. Chin J Commun. (2016) 9:403–21. doi: 10.1080/17544750.2016.1202293
74. Xu, Z, Huang, F, Kösters, M, Staiger, T, Becker, T, Thornicroft, G, et al. Effectiveness of interventions to promote help-seeking for mental health problems: systematic review and meta-analysis. Psychol Med. (2018) 48:2658–67. doi: 10.1017/S0033291718001265
75. Christiaens, W, and Bracke, P. Work-family conflict, health services and medication use among dual-income couples in Europe. Sociol Health Illn. (2014) 36:319–37. doi: 10.1111/1467-9566.12049
76. Bjorvatn, B, Fiske, E, and Pallesen, S. A self-help book is better than sleep hygiene advice for insomnia: a randomized controlled comparative study. Scand J Psychol. (2011) 52:580–5. doi: 10.1111/j.1467-9450.2011.00902.x
77. Erten Uyumaz, B, Feijs, L, and Hu, J. A review of digital cognitive behavioral therapy for insomnia (CBT-I apps): are they designed for engagement? Int J Environ Res Public Health. (2021) 18:18. doi: 10.3390/ijerph18062929
78. Baglioni, C, Altena, E, Bjorvatn, B, Blom, K, Bothelius, K, Devoto, A, et al. The European academy for cognitive Behavioural therapy for insomnia: an initiative of the European insomnia network to promote implementation and dissemination of treatment. J Sleep Res. (2020) 29:e12967. doi: 10.1111/jsr.12967
79. Espie, CA. "stepped care": a health technology solution for delivering cognitive behavioral therapy as a first line insomnia treatment. Sleep. (2009) 32:1549–58. doi: 10.1093/sleep/32.12.1549
80. Smith, MT, Perlis, ML, Park, A, Smith, MS, Pennington, J, Giles, DE, et al. Comparative meta-analysis of pharmacotherapy and behavior therapy for persistent insomnia. Am J Psychiatry. (2002) 159:5–11. doi: 10.1176/appi.ajp.159.1.5
81. Morin, CM, Colecchi, C, Stone, J, Sood, R, and Brink, D. Behavioral and pharmacological therapies for late-life insomnia: a randomized controlled trial. JAMA. (1999) 281:991–9. doi: 10.1001/jama.281.11.991
82. Hillman, D, Mitchell, S, Streatfeild, J, Burns, C, Bruck, D, and Pezzullo, L. The economic cost of inadequate sleep. Sleep. (2018) 41:41. doi: 10.1093/sleep/zsy083
83. Penzel, T, Peter, JH, Peter, H, Becker, HF, Fietze, I, Fischer, J, et al. Themenheft 27 "Schlafstörungen. Berlin: Robert Koch-Institut (2005).
84. Rossmann, C. Die mediale Konstruktion von Gesundheit und Krankheit In: M Richter and K Hurrelmann, editors. Soziologie von Gesundheit und Krankheit. Wiesbaden: Springer Fachmedien Wiesbaden (2016)
Keywords: sleep, sleep complaints, mental health, stigmatization, self-perceived cause, CBT-I, medication
Citation: Rauch L, Schneider T and Wendt C (2024) Seeking professional help for sleep-related complaints. Front. Public Health. 12:1430574. doi: 10.3389/fpubh.2024.1430574
Edited by:
Mosad Zineldin, Linnaeus University, SwedenReviewed by:
Leisha Cuddihy, University of Rochester, United StatesAquartuti Tri Darmayanti, School of Health Sciences Mamba’ul Ulum, Indonesia
Barış Kılıç Demir, Ministry of Health, Türkiye
Copyright © 2024 Rauch, Schneider and Wendt. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Claus Wendt, d2VuZHRAc296aW9sb2dpZS51bmktc2llZ2VuLmRl
†These authors have contributed equally to this work and share first authorship
 Lisa Rauch
Lisa Rauch Torsten Schneider
Torsten Schneider Claus Wendt
Claus Wendt