- 1School of Kinesiology, Faculty of Health Sciences, Western University, London, ON, Canada
- 2Department of Epidemiology and Biostatistics, Schulich School of Medicine and Dentistry, Western University, London, ON, Canada
- 3Department of Anesthesia & Perioperative Medicine, Schulich School of Medicine and Dentistry, Western University, London, ON, Canada
- 4Schulich Interfaculty Program in Public Health, Western University, London, ON, Canada
Introduction: Comprising approximately 13.6% of the United States population, Black/African American individuals are overrepresented in sports associated with a high risk of concussion. However, there has been a notable absence of systematic reviews examining whether concussion literature accurately reflects the participation and experiences of Black/African American individuals. Therefore, this study aims to systematically review the prevalence of Black/African American individuals compared to White individuals diagnosed with concussions in the literature.
Methods: A systematic search was performed across four electronic databases: PubMed, MEDLINE (Ovid), Scopus and Web of Science. Articles were searched from inception to January 5, 2022. Prevalence data were extracted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. A meta-analysis of proportions was conducted within hospital records and national survey data.
Results: Among 447 identified studies, 11 were included, representing 1,839,901 individuals diagnosed with a concussion, with 73.6% identifying as White and 12.5% identifying as Black/African American. The mean proportion of Black/African American diagnosed with a concussion in hospital records (13.9%; 95% CI [12.8, 15.1]) exceeded that in national surveys (6.4%; 95% CI [3.5, 11.3]) but lower than sports-centered studies (16%).
Discussion: These findings underscore the need to address racial disparities in healthcare within the broader context of social determinants of health and systemic inequities. By identifying gaps in the current research, this study lays the foundation for future investigation aimed at elucidating and addressing healthcare disparities.
1 Introduction
The exploration of social determinants of health’s influence on concussion identification, diagnosis, and rehabilitation is a growing focus in concussion literature (1). Notably, race has emerged as a significant determinant of health (2), particularly for individuals identifying as Black/African American, exerting substantial influence on these processes.
Historically, Black/African American individuals have been overlooked and excluded from medical literature (3). A recent systematic review demonstrated that only 15% of concussion literature within athletic populations over the past decade included the racial identification of participants, underscoring the deficiency in addressing race as a demographic variable within concussion literature (3). This deficiency is particularly problematic given reported racial disparities in both concussion incidence (4, 5), and outcomes (6).
Despite comprising approximately 13.6% of the United States population Black/African American individuals are disproportionately overrepresented in contact and collision sports, elevating their concussion risk (7, 8). Paradoxically, recent studies have revealed disparities in concussion diagnosis rates, with Black/African American individuals being diagnosed less frequently compared to their White counterparts (6, 9). Social inequities, including lower concussion symptom knowledge (10), and barriers to healthcare access (6, 9), are believed to contribute to these discrepancies.
Previously, a systematic review addressed the reporting of race and ethnicity in sports-related concussion (SRC) studies (3). However, SRC is only one mechanism of injury. In the pediatric population, motor vehicle collisions, and falls account for the majority of concussion injuries, followed by nonaccidental trauma and SRC (11). In older adults, fall-related head-injuries are cited as the most common concussion mechanisms (12). Broadening the scope to address the reporting of race in all concussion literature is imperative to ensure accurate understanding of the issue. Therefore, this study aims to systematically review the prevalence of Black/African American individuals compared to White individuals diagnosed with concussions in the literature. Such findings hold the potential to shed light on a demographic currently overlooked in concussion literature.
2 Methods
A systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines (13). This review protocol was not registered in an online database. This systematic review and meta-analysis were exempt from the institutional Research Ethics Board (WesternREM) as it involved data that is publicly available.
A literature review was conducted using the following databases: PubMed, Ovid Medical Literature Analysis and Retrieval System Online (MEDLINE), Scopus and Web of Science. The following search logic was used to extract articles from the database: (Black OR “African American”) AND (concussion OR “brain concussion” OR “mild traumatic brain injury” OR mTBI) and the following MeSH terms: (“blackness”[All Fields] OR “blacks”[MeSH Terms] OR “blacks”[All Fields] OR “black”[All Fields] OR “African American”[All Fields]) AND (“brain concussion”[MeSH Terms] OR (“brain”[All Fields] AND “concussion”[All Fields]) OR “brain concussion”[All Fields] OR “concussion”[All Fields] OR “concussions”[All Fields] OR “concussed”[All Fields] OR “concussive”[All Fields] OR “brain concussion”[All Fields] OR “mild traumatic brain injury”[All Fields] OR “mTBI”[All Fields]). Filters within the database were set to peer-reviewed journal articles published from the databases inception up to and including articles published January 5, 2022.
2.1 Literature search and study selection criteria
Inclusion criteria for this review were (i) original research (including randomized clinical trials (RCT), quasi-experimental designs, case studies and series, prospective and retrospective studies, cohort studies, and pilot studies), (ii) include human participants who have sustained a concussion or mild traumatic brain injury (mTBI), (iii) include results that compare study outcomes between Black/African American and Caucasian/White/ (iv) completed in the United States of America. Articles published in English, with any sample size were included. There were no limitations to the age of participants or mechanism of injury. Diagnosis of a concussion could have been rendered at any time. Review articles and articles published in only abstract form were excluded.
The screening, full-text review and data extraction were performed by two authors (TM and AC) using Covidence Systematic Review software (Veritas Health Innovation). TM and AC met frequently to discuss coding within the review. When a disagreement occurred, discussions continued until the two authors reached a consensus. Phase I applied the search terms to extract the first round of articles from PubMed (n = 131), MEDLINE (n = 66), Scopus (n = 107) and Web of Science (n = 133). Phase II involved preliminary distillations of the identified articles through title and abstract screening by removing studies irrelevant to the research question (n = 164), studies containing the wrong patient population (n = 19), studies containing the wrong outcome due to not comparing Black/African and White individuals (n = 15), focused on other areas of health (n = 2) and not completed in the United States (n = 1). Consequently, these articles were not considered for this review. During phase III, the refined list of articles (n = 11) was reviewed, and the following data was extracted: type of study, location, duration, funding sources, population characteristics (population type, sample size, race, age, sex), definition of concussion, number of individuals with a concussion based on racial categories, concussion assessment(s) and key findings on outcome measures related to neurocognitive assessments, and/or symptom scales. Studies reporting the prevalence or incidence of concussion in Black/African American individuals, or provided sufficient data to permit calculation, were included.
2.2 Statistical analysis
The proportion of Black/African American vs. White individuals with a concussion were compared using a meta-analysis of proportions. A separate random effects meta-analysis was performed for prevalence estimates derived from hospital records (5, 14–21), those derived from national survey data (22), and those generated from the medical records of athletes attending a sport concussion center (6). For the national survey data the authors were contacted and provided values for the unweighted number of individuals who reported a concussion, which were used in the meta-analysis (22). In each meta-analysis, the mean proportion of Black/African American individuals with a concussion, weighted by variance, was computed, in addition to the 95% confidence interval [CI].
2.3 Quality assessment and risk of bias
To assess the risk of bias in studies, the JBI Critical Appraisal Checklist tools created by International Joanna Briggs Institute were used. The JBI critical appraisal checklist was designed to determine the extent to which a study has addressed the possibility of bias in its design, conduct, and analysis, and to assess the methodological quality of a study (21). There were 10 questions to guide the evaluation of case series studies, eight for the evaluation of analytic cross-sectional studies and nine for the evaluation of prevalence studies. The questions were quantified using scores from 0 to 1. One point is given if the answer is “YES” and zero points if the answer is “NO,” “not clear” or “not applicable.”
3 Results
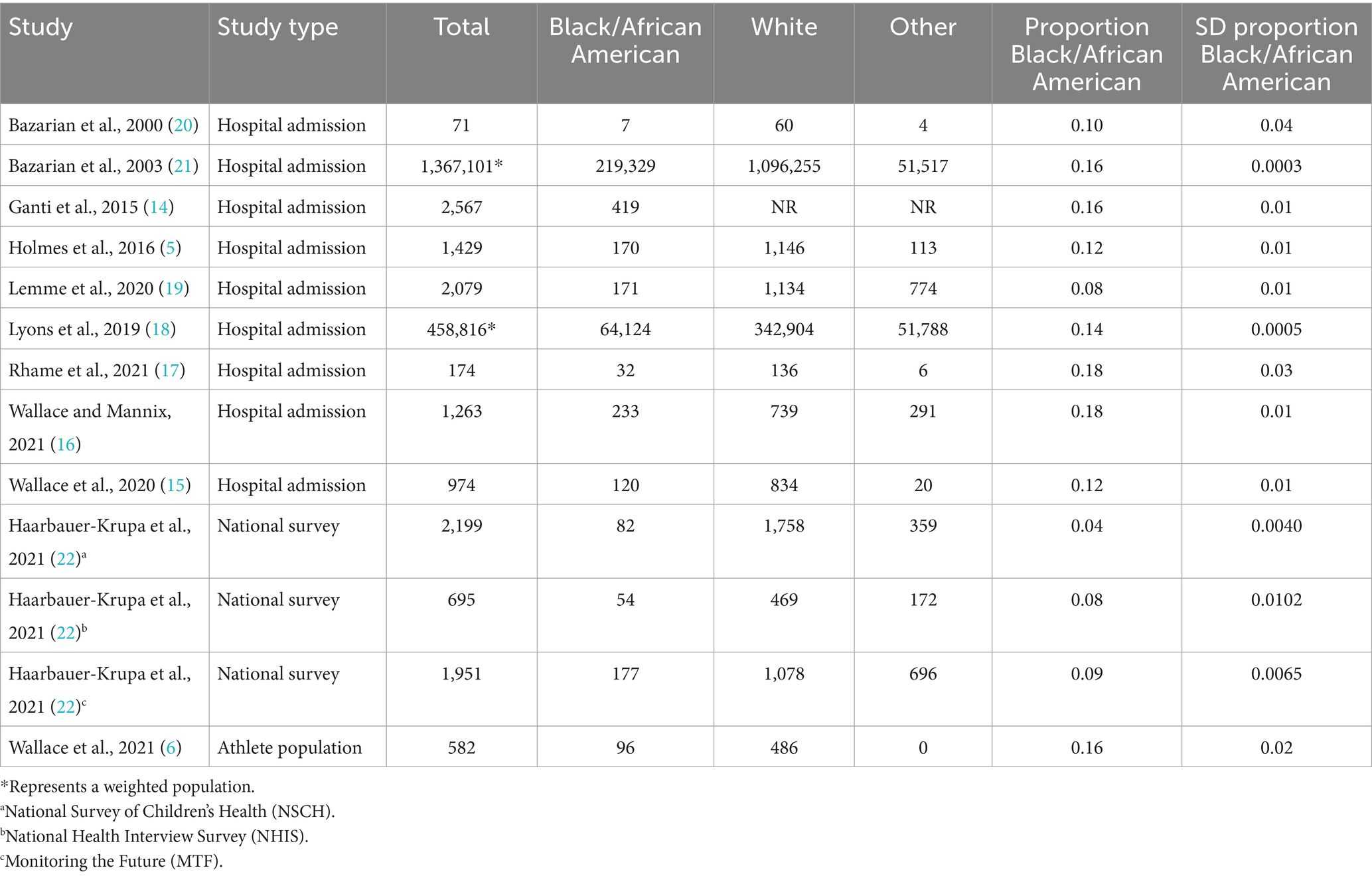
The data extraction process resulted in 11 distinct studies (5, 6, 14–22), that satisfied the predefined inclusion and exclusion criteria (Figure 1). In total, these studies encompassed 1,839,901 participants diagnosed with concussions. Among these participants, 285,014 identified as Black/African American, 1,446,999 as White and 105,740 as belonging to other racial groups (Table 1).
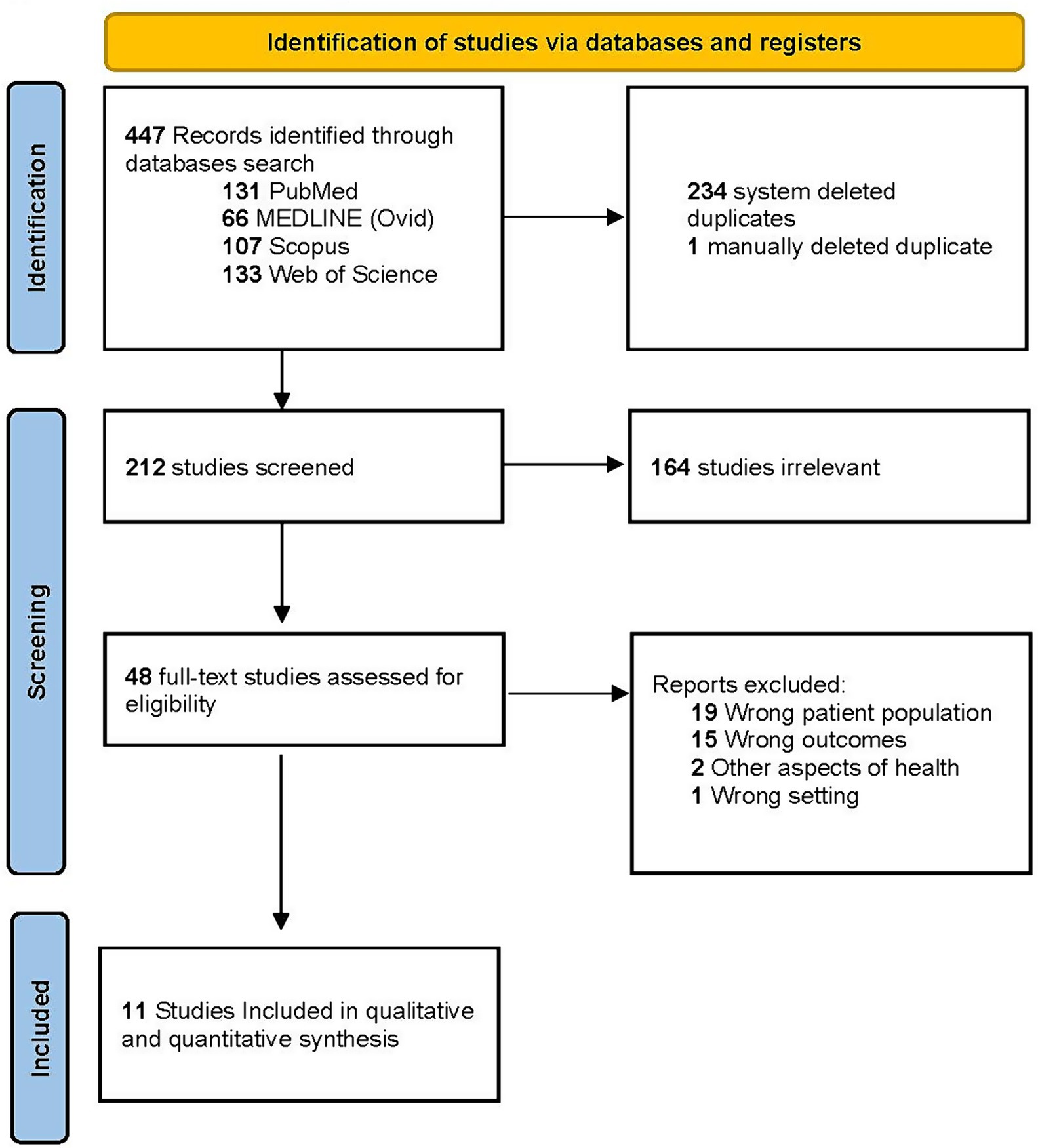
Figure 1. PRISMA flow diagram of study selection. Flow diagram of search results and review of studies for inclusion.
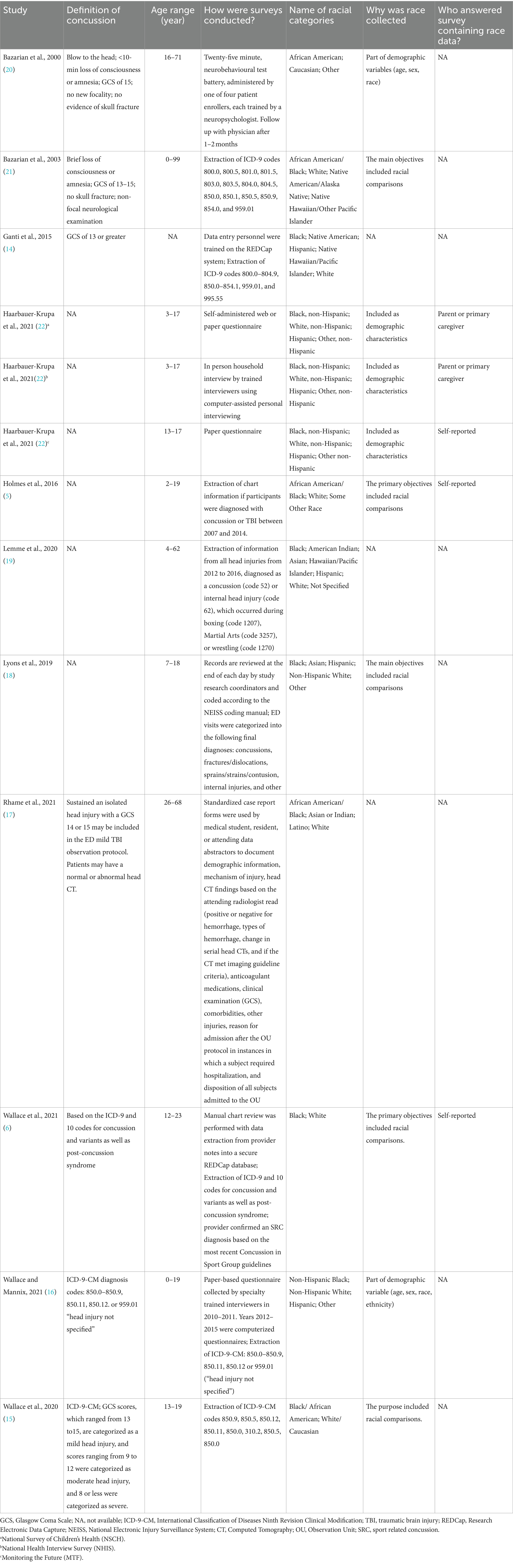
The age distribution varied across the 11 articles. Two studies focused solely on children and adolescents (≤18 years) (18, 22), while one study exclusively involved adults (>18 years) (17). The remaining seven studies included both child and adult participants (Table 2) (5, 6, 15, 16, 19–21). Notably, one study did not specify the age range of its participants (14).
Racial demographics were captured through various means. Some studies included racial categories as part of their demographic variables (15, 16, 20, 22), while others focused on race as a primary variable of interest (5, 6, 18, 21). However, in three studies, the rationale for collecting racial data was not explicitly states (14, 17, 19). Participants or their parent/caregiver provided information on race (5, 6, 22), though in several instances it was not stated who reported this data (Table 2) (14–21).
3.1 Quality assessment and risk of bias
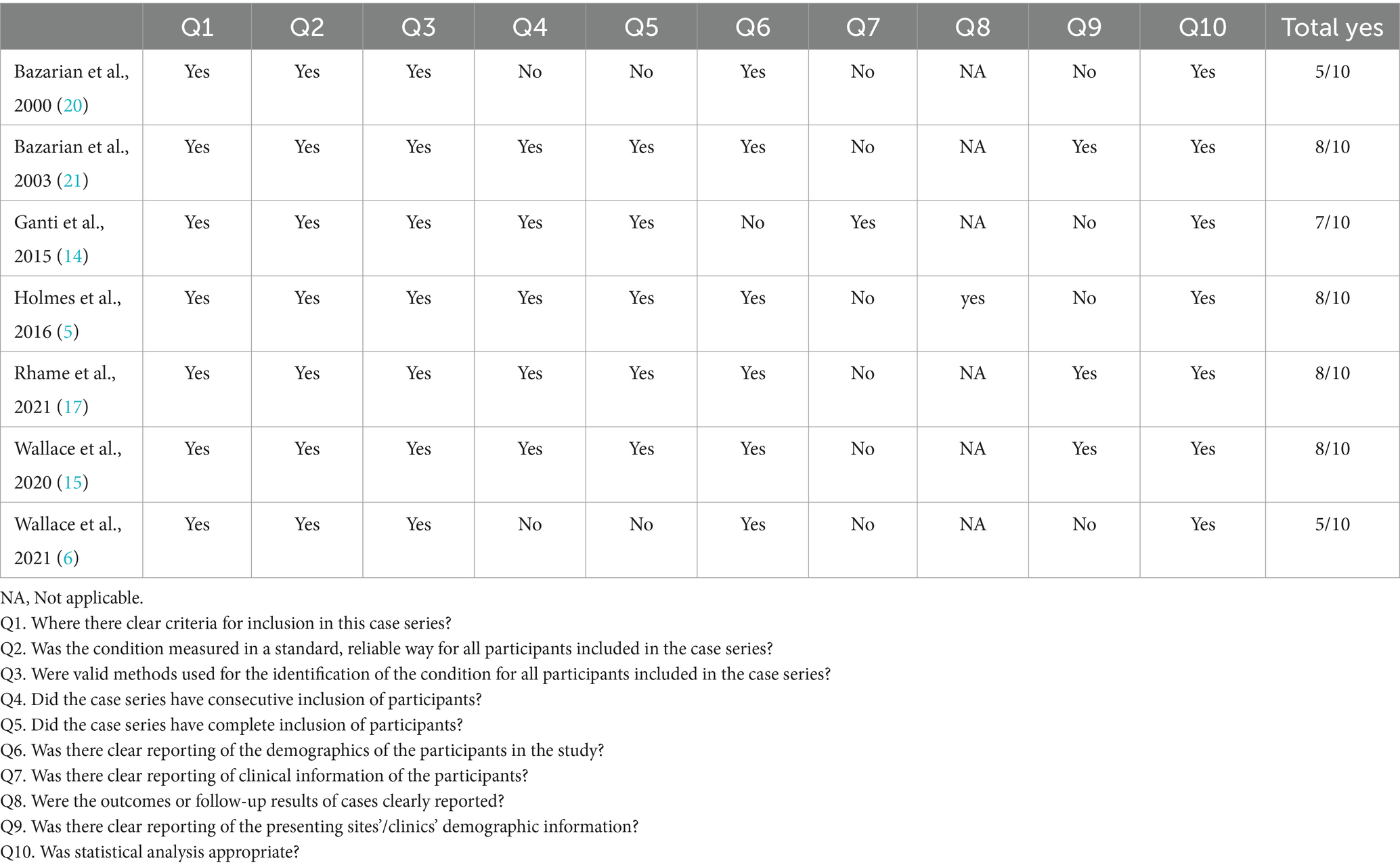
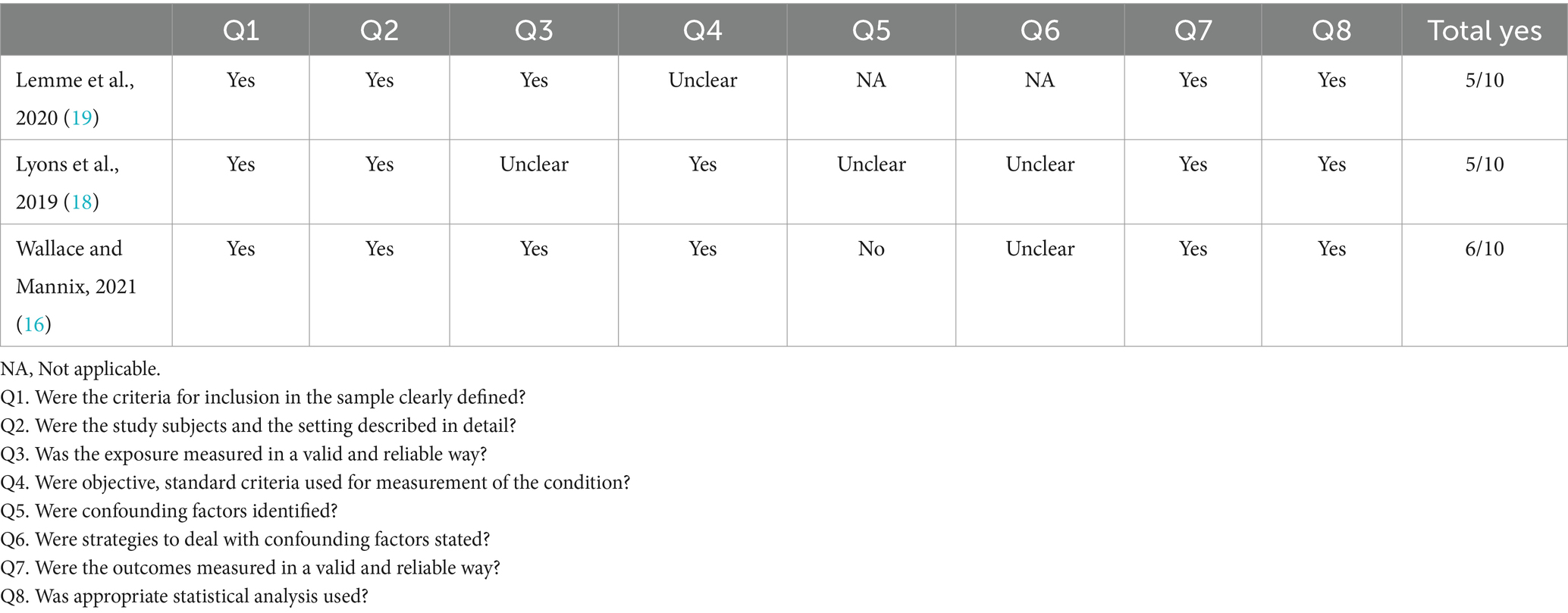
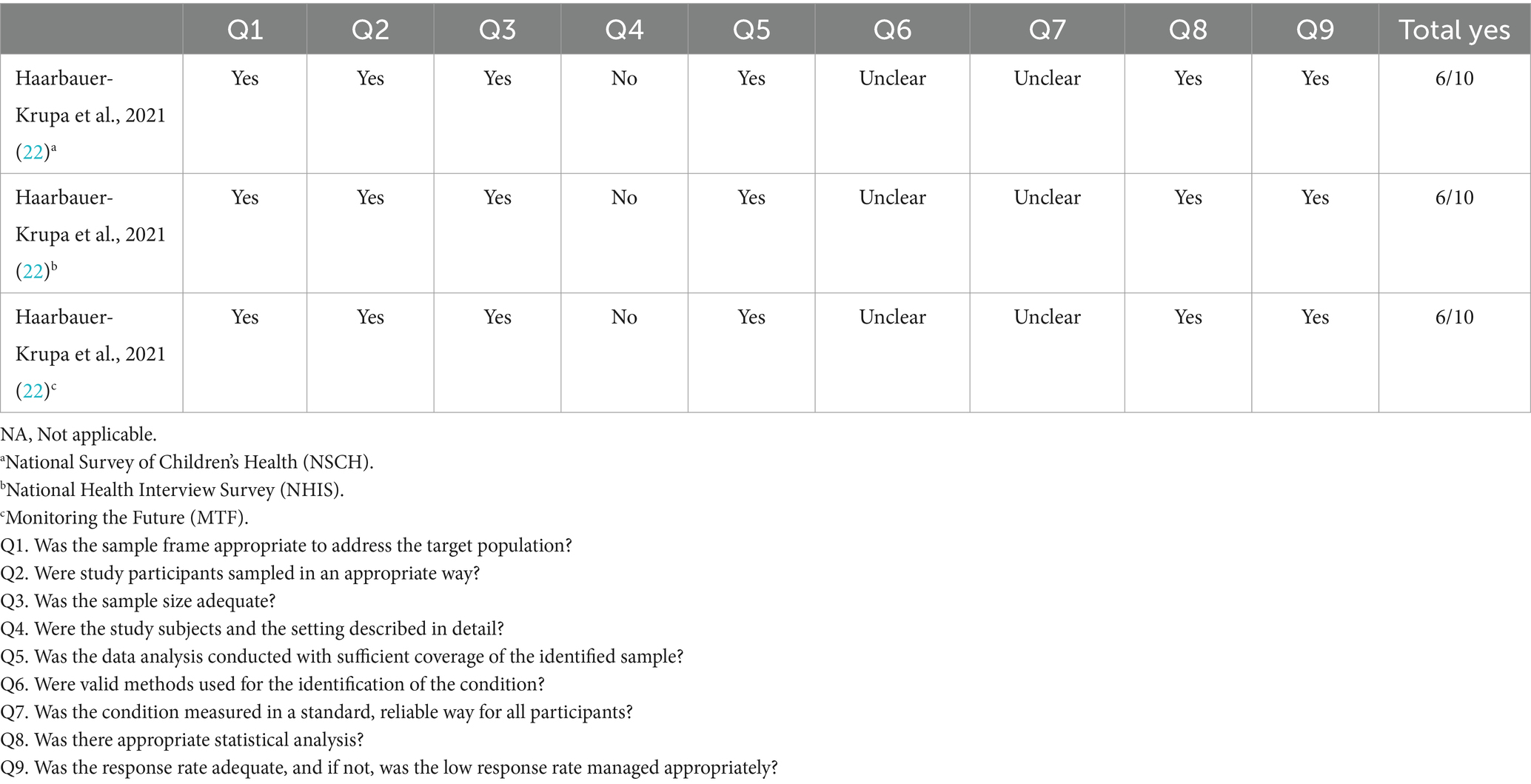
The methodological quality was assessed using various versions of the JBI checklist. The JBI checklist for case series was used for seven studies (Table 3) (5, 6, 12, 13, 15, 18, 19), the JBI checklist for analytic cross-sectional studies was used for three studies (Table 4) (14, 16, 17), and the JBI checklist for prevalence studies was used for one study (Table 5) (20).
Applying the JBI checklist for case series scores ranged from 5 to 8 out of 10 with a majority of articles scoring 8/10 (57%). Within this quality assessment only one study included follow-up results, meeting criteria for question 8, making it not applicable in all other studies. However, all studies included clear criteria (question 1), the condition to be measured in a standard, reliable way (question 2), with valid methods (question 3), and appropriate statistical analysis (question 10).
Within the three studies analyzed using the JBI analytic cross-sectional studies checklist the scores two studies (18, 19), scored 5/10 while one study (16), scored 6/10. The one study (22), that was analyzed using the JBI prevalence checklist scored a 6/10.
3.2 Prevalence
Where a single study encompassed multiple populations, separate proportion were calculated for each population (22). Within the meta-analysis, conducted using weighted proportions across all studies, the predominant racial identification was White, comprising 73.6% of the sample population, while Black/African American individuals constituted a smaller percentage at 12.5% among those diagnosed with a concussion.
The majority of the studies (n = 9) included data from individuals diagnosed with a concussion in either a hospital setting or an emergency department (ED) (5, 14–21). Across these studies, the mean proportion of Black/African American individuals (13.9, 95% CI [12.8, 15.1]; Figure 2) was lower compared to those who identified as White. One study analyzed data from three distinct national survey datasets (22). Across these three datasets, a similar trend was observed, with a lower proportion of Black/African American individuals (6.4, 95% CI [3.5, 11.3]; Figure 3) compared to those identifying as White among those diagnosed with concussions. Additionally, one study focused on athletes, accessing medical records from a sport concussion center, where 16% of the concussed group identified as Black/African American (Table 1) (6).
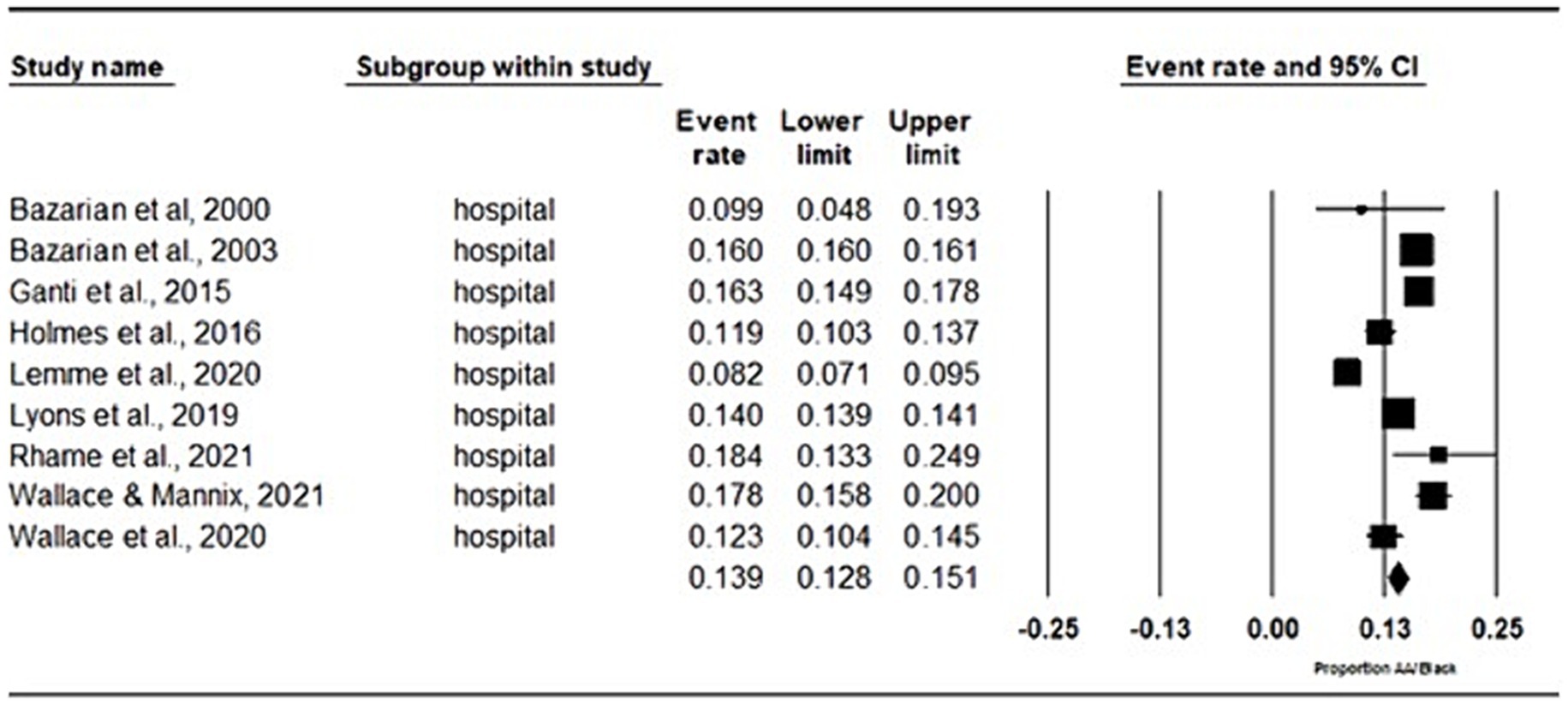
Figure 2. Meta-analysis of proportions of hospital/emergency department records. Proportion of AA/Black individuals included in studies that took place in a hospital and emergency department setting.
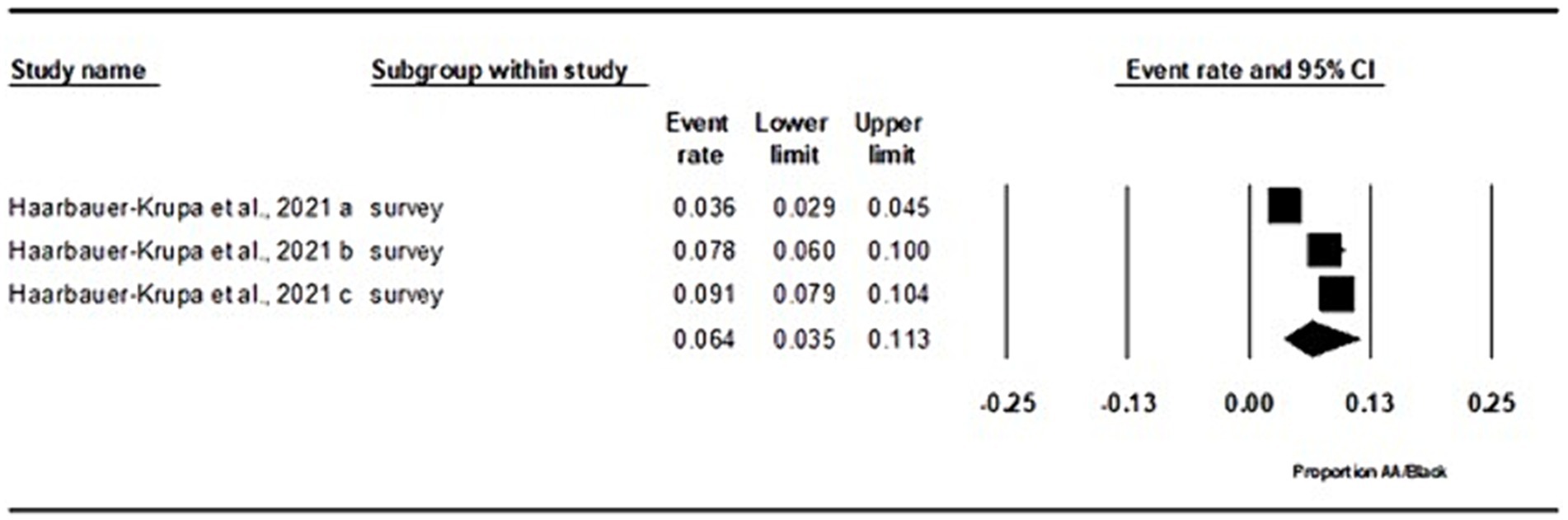
Figure 3. Meta-analysis of proportions of national survey data. Proportion of AA/Black individuals included in studies that collected data from a National Survey Data.
4 Discussion
The influence of social determinants of health, such as race, on the identification, diagnosis, and rehabilitations of concussion is increasingly gaining attention in concussion research. In this study, the aim was to systematically review the prevalence of concussions among Black/African American individuals compared to White individuals in the existing literature. Our findings revealed variability in the representation of Black/African American individuals depending on the method of data collection. When examining hospital records, the prevalence of concussions among Black/African American individuals (13.9%) closely mirrored their representation in the general population (13.6%) (7). However, disparities emerged when comparing to national survey data, where Black/African American individuals were underrepresented at 6.4%. Conversely, in sport-related contexts, they were overrepresented, comprising 16% of diagnosed cases.
According to the 2021 census data, the racial distribution in the United States shows Black/African American individuals constitute 13.6% of the population, while White individuals make up 75.8% (7). If Black/African American individuals face similar likelihoods of sustaining concussion and have equitable access to appropriate medical care, we would anticipate their representation among concussion cases to align with their population percentage, as observed in hospital-based studies.
This alignment with population demographics may be influenced by the structure of the healthcare system in the United States. Data from 2020 indicated that 19.5% of Black individuals in the United States live below the poverty line, a rate significantly higher than the national average of 11.4% and more than double that of White individuals at 8.2% (23). Arbogast et al., (24) indicated that non-Hispanic Black patients and those with Medicaid coverage are more likely to utilize the emergency department (ED) setting as an initial point of entry into the healthcare system. However, accurate clinical identification of a concussion can be difficult due to varying definitions and criteria (25). Variations in concussion symptom presentation and lack of structural abnormalities on neuroimaging often lead concussions to be misdiagnosed in the ED (26, 27). It has previously been reported that 45% of children (26) and 56% of adults (28) that present to the ED met diagnosis criteria for a concussion, yet did not receive a diagnosis. The prevalence of misdiagnosis in the ED makes it possible that concussion clinics may be a more appropriate place to receive an accurate concussion diagnosis. However, concussion clinics are not utilized by all parts of the general population, specifically it has been found that non-Hispanic White individuals are more likely to utilize a concussion clinic and those not on Medicaid or state Child Health insurance plans were less likely to present in a specialized clinic (29, 30).
In additional to misdiagnosis, ED usage may be affected by factors such as accessibility, individual interpretation of injury severity and perception of primary care’s ability to handle acute injury and illness (31), all which have been shown to be associated with race, leading to a lower likelihood of Black/African American individuals seeking care (32–35). Additionally, previous studies have indicated disparities in concussion diagnosis rates between Black/African American individuals and White/non-Hispanic individuals within ED settings (15). Systemic factors, including implicit bias among healthcare practitioners, have been extensively studied (34, 36–38). Research has demonstrated that clinicians often exhibit moderate to strong implicit bias against Black patients (34), which can directly influence treatment recommendations and care decisions (38). Therefore, while our finding of Black/African American individuals accounting for 13.9% of concussions diagnosed in hospitals align with the distribution of the general population, it may not fully capture the concussion prevalence of Black/African individuals due to potential biases and disparities in healthcare delivery.
In the national survey data, Black/African American individuals were found to be underrepresented compared to their distribution in the population (7). These surveys primarily focused on children and adolescents, addressing lifetime prevalence, which could potentially explain the lower observed prevalence rate among Black/African American individuals. As a concussion diagnosis is based on symptom presentation, it is crucial for individuals or caregivers to possess a comprehensive understanding of concussion symptoms and seek appropriate medical attention. Previous studies have indicated a disparity in concussion symptom knowledge between Black/African American and White athletes (10, 33), as well as among parents/guardians (32).
The non-specific nature of concussion symptoms poses a risk of misdiagnosis, as many symptoms can overlap with those of other health conditions (39). Additionally, limitations related to health literacy may contribute to this underrepresentation, as medical terminology used in symptom checklists might hinder individuals from accurately identifying symptoms. Previous research has highlighted that Black/African American individuals may have lower health literacy compared to their White counterparts (40, 41). Symptoms such as “fatigue” and “nausea” for instance, may pose challenges for those less familiar with medical terminology (33). Systemic institutional factors, such as chronic underfunding of schools in Black/African American communities, may further exacerbate disparities in health literacy (42). This lower health literacy has been associated with adverse health outcomes, poorer health status and decreased satisfaction with healthcare services (40, 41).
The proportion of Black/African American individuals diagnosed with a concussion in athletic literature exceeded their representation in the general population. This observation can be attributed, in part, to the demographic composition of contact and collision sports. In a nationally representative sample, it has been reported that African American youth make up approximately 27% of participants in tackle football, while White youth make up only approximately 10% (43). Black/African American individuals comprise approximately 50% of collegiate athletes in the National Collegiate Athletic Association (NCAA) participating in high-concussion risk, revenue-producing sports such as football, men’s basketball and women’s basketball (4). This overrepresentation of Black/African American players is also seen in the NFL, with Black/African American players comprising over 70% (44). Given this significant overrepresentation in sports associated with elevated concussion risk, and the potential for athletes to have immediate access to healthcare professionals such as Athletic Trainers and Sport Medicine Physicians, that may be more familiar with concussion injuries, it is expected that the proportion of Black/African diagnosed with concussions within athlete populations would surpass that of the general population.
While variations in concussion diagnosis were evident across different forms of data collection, it is plausible that none of the findings in the concussion literature accurately reflect the Black/African American experience with concussions. Out of the 11 articles in this study, 10 relied on medical chart reviews based on a concussion diagnosis made by a healthcare professional. However, the lack of concise definitions of concussion led to nearly every study utilizing a different definition (25). Often, it was not clarified whether clinicians distinguished between a diagnosis of concussion, traumatic brain injury, sport-related concussion, or other head injuries, as the interpretation of the concussion definition was left to individual clinicians. This ambiguity, coupled with disparities in the quality and standard of care received by Black communities (35, 36, 38), may contribute to underdiagnosis within minority communities.
This notion is supported by literature contradicting the findings of this systematic review, which indicates that Black/African American individuals are underrepresented in the ED for head injuries and are less likely to be diagnosed with a concussion compared to their white counterparts (15, 18). Furthermore, feelings of distrust towards healthcare practitioners, along with discomfort and fear of discrimination experienced by Black/African American individuals, have been found to lead to delays in seeking medical care (34, 35). Given the nature of concussion diagnosis, such a delay may contribute to an under-reporting and underdiagnosis of concussions in Black/African American individuals.
4.1 Limitations
This review is subject to several limitations that warrant consideration. While the authors aimed to comprehensively identify and extract all articles meeting the inclusion criteria, the search was limited to four databases: PubMed, MEDLINE (Ovid), Scopus and Web of Science. These restrictions may have inadvertently resulted in the oversight of additional concussion studies.
Furthermore, the absence of a universally accepted definition of concussion poses a challenge (35). In the United States, the American Medical Society for Sport Medicine (AMSSM) released a definition of concussion in 2013 (36), updated in 2019 (37). Globally, the International Conference on Concussion in Sport revises their definition every 4 years, with updates occurring between 2001 and 2016 (38, 39). Given that the papers included in this review spanned from 2000 to 2021, changes in concussion definitions during this 21-year period may have influenced concussion recognition and diagnosis across studies. The authors acknowledge this discrepancy, however, while some agreement exists among various concussion definitions, individual diagnosis and management decisions remain within the realm of clinical judgment and therefore limiting the timeline of which this review covered had the potential to influence the results of the review based on the authors personal interpretation on the appropriate definition and diagnosis of concussion. Additional limitations stem from variable sample compositions, including variations in age demographics, and the retrospective nature of some studies. Moreover, many studies failed to provide information on potentially confounding variables such as socioeconomic status, prior concussion history, presence of ADHD, and sex, all of which have been shown to influence concussion reporting behavior and diagnosis (40–45).
5 Conclusion
The findings of this systematic review and meta-analysis provide valuable insight into the intricate interplay between race and healthcare, emphasizing the complexities involved in diagnosing concussions and accurately representing them in the literature. Contrary to prior assumptions, the observed findings challenge the notion of overrepresentation of Black/African American individuals in all concussion studies. These findings may be attributed to various factors stemming from social determinants of health, perpetuated by racial disparities in healthcare. However, it is essential to contextualize these healthcare disparities within the broader context of racial inequities embedded within laws, regulations, and social institutions (45).
Achieving an accurate representation of concussion is paramount. Addressing healthcare disparities requires a comprehensive understanding of the issue, and the findings of this systematic review underscore an underexplored area within healthcare research. Future research endeavors should focus on identifying health disparities associated with race that hinder Black/African American individuals from accessing appropriate care. By pinpointing gaps in the current literature, this study lays the foundation for further research aimed at elucidating and ultimately mitigating racial disparities in concussion diagnosis and care. Through efforts aimed at addressing these disparities, we can work towards ensuring equitable healthcare access and outcomes for all individuals, regardless of race or ethnicity.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
TM: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. AJ-B: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. AC: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Natural Sciences and Engineering Research Council of Canada RGPIN/0512701 (AC). TM was supported by an Ontario Graduate Scholarship (OGS). The funding organizations were not directly involved in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Acknowledgments
Part of this manuscript has previously appeared online as part of graduate thesis completed by TM. The entire thesis can be found at: TM, “Implications of Race on Post-Concussion Neurocognitive Performance and Symptom Presentation” (2022). Electronic Thesis and Dissertation Repository. 8607. https://ir.lib.uwo.ca/etd/8607. GPT-3.5 language model developed by OpenAI (ChatGPT) was used for editing assistance specifically with the usage of prompts relating to clarity, grammar, and spelling. All ideas are original to the authors and all work has been adequately reviewed and edited.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Wallace, J, Covassin, T, Moran, R, and Deitrick, JM. Factors contributing to disparities in baseline neurocognitive performance and concussion symptom scores between Black and white collegiate athletes. J Racial Ethn Health Disparities. (2018) 5:894–900. doi: 10.1007/s40615-017-0437-y
2. Health People 2030. (2024) Social determinants of health. Available at: https://health.gov/healthypeople/priority-areas/social-determinants-health
3. Jo, J, Williams, KL, Wallace, J, Anand, M, Anesi, TJ, Brewer, C, et al. Systematic review examining the reporting of race and ethnicity in sport-related concussion studies. J Athl Train. (2023) 59:354–62. doi: 10.4085/1062-6050-0072.23
4. Wallace, J, Bretzin, A, Beidler, E, Hibbler, T, Delfin, D, Gray, H, et al. The underreporting of concussion: differences between Black and white high school athletes likely stemming from inequities. J Racial Ethn Health Disparities. (2021) 8:1079–88. doi: 10.1007/s40615-020-00864-x
5. Holmes, L, Tworig, J, Casini, J, Morgan, I, O’Brien, K, Oceanic, P, et al. Implication of socio-demographics on cognitive-related symptoms in sports concussion among children. Sports Med-Open. (2016) 2:38. doi: 10.1186/s40798-016-0058-8
6. Wallace, J, Hou, BQ, Hajdu, K, Tang, AR, Grusky, AZ, Lee, T, et al. Healthcare navigation of Black and white adolescents following sport-related concussion: a path towards achieving health equity. J Athl Train. (2021) 57:352–9. doi: 10.4085/1062-6050-0330.21
7. U.S. Census Bureau. Quick facts: United States. (2021). Available at: https://www.census.gov/quickfacts/fact/table/US/PST045221
8. Wallace, J, Moran, R, Beidler, E, McAllister Deitrick, J, Shina, J, and Covassin, T. Disparities on baseline performance using neurocognitive and oculomotor clinical measures of concussion. Am J Sports Med. (2020) 48:2774–82. doi: 10.1177/0363546520946753
9. National Collegiate Athletic Association. (2022). NCAA Demographics Database [Data visualization dashboard]. Available at: https://www.ncaa.org/sports/2018/12/13/ncaa-demographics-database.aspx
10. Wallace, J, Covassin, T, and Moran, R. Racial disparities in concussion knowledge and symptom recognition in American adolescent athletes. J Racial Ethn Health Disparities. (2018) 5:221–8. doi: 10.1007/s40615-017-0361-1
11. Dewan, MC, Mummareddy, N, Wellons, JC, and Bonfield, CM. Epidemiology of global pediatric traumatic brain injury: qualitative review. World Neurosurg. (2016) 91:497–509.e1. doi: 10.1016/j.wneu.2016.03.045
12. Reid, DBC, Shah, KN, Baum, EJ, and Daniels, AH. Concussion: mechanisms of injury and trends from 1997 to 2019. R I Med J. (2013) 103:71–5.
13. Moher, D, Liberati, A, Tetzlaff, J, and Altman, DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. (2009) 339:b2535. doi: 10.1136/bmj.b2535
14. Ganti, L, Conroy, LM, Bodhit, A, Daneshvar, Y, Patel, PS, Ayala, S, et al. Understanding why patients return to the emergency department after mild traumatic brain injury within 72 hours. West J Emerg Med. (2015) 16:481–5. doi: 10.5811/westjem.2015.2.23546
15. Wallace, J, Moran, R, Bretzin, A, Hileman, B, and Huang, GS. Examination of racial disparities in adolescents seen in the emergency Department for Head, neck, or brain injury. J Emerg Med. (2020) 59:783–94. doi: 10.1016/j.jemermed.2020.07.002
16. Wallace, JS, and Mannix, RC. Racial disparities in diagnosis of concussion and minor head trauma and mechanism of injury in pediatric patients visiting the emergency department. J Pediatr. (2021) 233:249–254.e1. doi: 10.1016/j.jpeds.2021.01.057
17. Rhame, K, Le, D, Ventura, A, Horner, A, Andaluz, N, Miller, C, et al. Management of the mild traumatic brain injured patient using a multidisciplinary observation unit protocol. Am J Emerg Med. (2021) 46:176–82. doi: 10.1016/j.ajem.2020.06.088
18. Lyons, TW, Miller, KA, Miller, AF, and Mannix, R. Racial and ethnic differences in emergency department utilization and diagnosis for sports-related head injuries. Front Neurol. (2019) 10:690. doi: 10.3389/fneur.2019.00690
19. Lemme, NJ, Johnston, B, DeFroda, SF, Owens, BD, and Kriz, PK. Incidence of combat sport-related mild traumatic brain injuries presenting to the emergency department from 2012 to 2016. Clin J Sport Med Off J Can Acad Sport Med. (2020) 30:585–90. doi: 10.1097/JSM.0000000000000633
20. Bazarian, J, Hartman, M, and Delahunta, E. Minor head injury: predicting follow-up after discharge from the emergency department. Brain Inj. (2000) 14:285–94. doi: 10.1080/026990500120754
21. Bazarian, JJ, Pope, C, McClung, J, Cheng, YT, and Flesher, W. Ethnic and racial disparities in emergency department care for mild traumatic brain injury. Acad Emerg Med Off J Soc Acad Emerg Med. (2003) 10:1209–17. doi: 10.1197/S1069-6563(03)00491-3
22. Haarbauer-Krupa, J, Lebrun-Harris, LA, Black, LI, Veliz, P, Daugherty, J, Desrocher, R, et al. Comparing prevalence estimates of concussion/head injury in U.S. children and adolescents in national surveys. Ann Epidemiol. (2021) 54:11–20. doi: 10.1016/j.annepidem.2020.11.006
23. Shrider, EA, Kollar, M, Chen, F, and Semega, J. U.S Census Bureau, Current Population Reports. Income and Poverty in the United States: 2020. Washington, DC: U.S. Government Publishing Office. (2021). 60–273
24. Arbogast, KB, Curry, AE, Pfeiffer, MR, Zonfrillo, MR, Haarbauer-Krupa, J, Breiding, MJ, et al. Point of health care entry for youth with concussion within a large pediatric care network. JAMA Pediatr. (2016) 170:e160294. doi: 10.1001/jamapediatrics.2016.0294
25. Kazl, C, and Torres, A. Definition, classification, and epidemiology of concussion. Semin Pediatr Neurol. (2019) 30:9–13. doi: 10.1016/j.spen.2019.03.003
26. Boutis, K, Weerdenburg, K, Koo, E, Schneeweiss, S, and Zemek, R. The diagnosis of concussion in a pediatric emergency department. J Pediatr. (2015) 166:1214–1220.e1. doi: 10.1016/j.jpeds.2015.02.013
27. Rowe, BH, Eliyahu, L, Lowes, J, Gaudet, LA, Beach, J, Mrazik, M, et al. Concussion diagnoses among adults presenting to three Canadian emergency departments: missed opportunities. Am J Emerg Med. (2018) 36:2144–51. doi: 10.1016/j.ajem.2018.03.040
28. Powell, JM, Ferraro, JV, Dikmen, SS, Temkin, NR, and Bell, KR. Accuracy of mild traumatic brain injury diagnosis. Arch Phys Med Rehabil. (2008) 89:1550–5. doi: 10.1016/j.apmr.2007.12.035
29. Rosenbaum, AM, and Arnett, PA. The development of a survey to examine knowledge about and attitudes toward concussion in high-school students. J Clin Exp Neuropsychol. (2010) 32:44–55. doi: 10.1080/13803390902806535
30. Thomas, DJ, Coxe, K, Li, H, Pommering, TL, Young, JA, Smith, GA, et al. Length of recovery from sports-related concussions in pediatric patients treated at concussion clinics. Clin J Sport Med. (2018) 28:56–63. doi: 10.1097/JSM.0000000000000413
31. Fieldston, ES, Alpern, ER, Nadel, FM, Shea, JA, and Alessandrini, EA. A qualitative assessment of reasons for nonurgent visits to the emergency department: parent and health professional opinions. Pediatr Emerg Care. (2012) 28:220–5. doi: 10.1097/PEC.0b013e318248b431
32. Wallace, J, Affagato, R, Brooke, M, McAllister-Deitrick, J, Moran, RN, and Covassin, T. Racial disparities in parent knowledge of concussion and recognition of signs and symptoms. J Saf Res. (2020) 75:166–72. doi: 10.1016/j.jsr.2020.09.007
33. Wallace, J, Beidler, E, Kerr, ZY, Hibbler, T, Anderson, M, and Register-Mihalik, JK. Assessing differences in concussion symptom knowledge and sources of information among Black and white collegiate-athletes. J Head Trauma Rehabil. (2021) 36:139–48. doi: 10.1097/HTR.0000000000000672
34. Blair, IV, Steiner, JF, Fairclough, DL, Hanratty, R, Price, DW, Hirsh, HK, et al. Clinicians’ implicit ethnic/racial Bias and perceptions of care among Black and Latino patients. Ann Fam Med. (2013) 11:43–52. doi: 10.1370/afm.1442
35. Feagin, J, and Bennefield, Z. Systemic racism and U.S. health care. Soc Sci Med. (1982) 2014:7–14.
36. FitzGerald, C, and Hurst, S. Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics. (2017) 18:19. doi: 10.1186/s12910-017-0179-8
37. Fyffe, DC, Mukherjee, S, Barnes, LL, Manly, JJ, Bennett, DA, and Crane, PK. Explaining differences in episodic memory performance among older African Americans and whites: the roles of factors related to cognitive reserve and test Bias. J Int Neuropsychol Soc JINS. (2011) 17:625–38. doi: 10.1017/S1355617711000476
38. Williams, DR, and Wyatt, R. Racial Bias in health care and health: challenges and opportunities. JAMA. (2015) 314:555–6. doi: 10.1001/jama.2015.9260
39. Currie, DW, Kraeutler, MJ, Schrock, JB, McCarty, EC, and Comstock, RD. Time trends in concussion symptom presentation and assessment methods in high school athletes. Am J Sports Med. (2017) 45:3368–73. doi: 10.1177/0363546517725068
40. Kelly, PA, and Haidet, P. Physician overestimation of patient literacy: a potential source of health care disparities. Patient Educ Couns. (2007) 66:119–22. doi: 10.1016/j.pec.2006.10.007
41. Shea, JA, Beers, BB, McDonald, VJ, Quistberg, DA, Ravenell, KL, and Asch, DA. Assessing health literacy in African American and Caucasian adults: disparities in rapid estimate of adult literacy in medicine (REALM) scores. Fam Med. (2004) 36:575–81.
42. Baker, B, and Cotto, R. The under-funding of Latinx-serving school districts. Phi Delta Kappan. (2020) 101:40–46. doi: 10.1177/0031721720909593
43. Jon Solomon. Project Play Aspen Institute. (2020). Survey: African-American youth more often play sports to chase college, pro dreams. Available at: https://projectplay.org/news/african-american-youth-more-often-play-sports-to-chase-college-pro-dreams#:~:text=Only%2010%25%20of%20White%20children,%25)%20and%20flag%20(8%25)
44. Marquez-Velarde, G, Grashow, R, Glass, C, Blaschke, AM, Gillette, G, Taylor, HA, et al. The paradox of integration: racial composition of NFL positions from 1960 to 2020. Sociol Race Ethn. (2023) 9:451–69. doi: 10.1177/23326492231182597
Keywords: concussion, mTBIs, prevalence, health equity, social determinants of health, disparities, Black/African American
Citation: MacEachern T, John-Baptiste A and Christie A (2024) The prevalence of Black/African American individuals in concussion literature: a systematic review and meta-analysis. Front. Public Health. 12:1430428. doi: 10.3389/fpubh.2024.1430428
Edited by:
Sivaniya Subramaniapillai, Université de Lausanne, SwitzerlandReviewed by:
Karie Zach, Medical College of Wisconsin, United StatesMegan Loftin, State of Michigan, United States
Copyright © 2024 MacEachern, John-Baptiste and Christie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Taia MacEachern, dGJtYWNlYWNoZXJuQGNyaW1zb24udWEuZWR1
†These authors have contributed equally to this work
 Taia MacEachern
Taia MacEachern Ava John-Baptiste2,3,4†
Ava John-Baptiste2,3,4† Anita Christie
Anita Christie