- Department of Endocrinology, The Central Hospital of Enshi Tujia and Miao Autonomous Prefecture, Enshi, Hubei, China
Background: Effective management of diabetes mellitus (DM) involves comprehensive knowledge, attitudes, and practices (KAP) by nurses, which is essential for optimal patient care and aiding patients in their self-management of the condition.
Method: This survey evaluates nurses' self-assessed knowledge, attitudes, and practices (KAP) related to diabetes management, focusing on their perceptions of personnel expertise and care approaches. Using a stratified sampling method, the survey was disseminated across various online platforms from January 2023 to February 2024 within China, including WeChat and Sina Weibo. We employed binary logistic regression and Chi-square tests to explore the statistical correlates of KAP related to DM.
Results: A total of 4,011 nurses participated, revealing significant perceived knowledge deficiencies in specialized DM management areas, with only 34% (n = 1,360) proficient in current pharmacological treatments. Attitudinal assessments showed that 54% (n = 2,155) recognized the importance of cultural competence in dietary counseling. Practices were strong in routine glucose monitoring (96%, n = 3,851) but weaker in psychological support (68%, n = 2,736). Regression analysis indicated significant effects of experience on KAP, where nurses with 1–5 years of experience were more likely to show better knowledge (OR = 1.09; p = 0.08), and those with advanced degrees demonstrated higher competence (OR = 1.52; p = 0.028). Marital status influenced attitudes, with single nurses more likely to exhibit positive attitudes (OR = 0.49; p < 0.001), and work environment impacted knowledge, with hospital-based nurses more knowledgeable (OR = 1.15; p = 0.14). Additionally, gender differences emerged, with male nurses showing greater knowledge (OR = 1.65; p = 0.03) and better practices in diabetes care (OR = 1.47; p = 0.04).
Conclusion: The study underscores the critical need for targeted educational programs and policy interventions to enhance nursing competencies in DM management. While the study provides valuable insights into nurses' perceptions of their competencies, future research should incorporate objective knowledge assessments to ensure a comprehensive understanding of their actual capabilities. Interestingly, the data also suggests a substantial opportunity to leverage technology and inter-professional collaboration to further enhance DM management efficacy among nurses, fostering an integrated care approach.
1 Introduction
Diabetes mellitus (DM) represents a significant global public health issue, characterized by chronic hyperglycemia resulting from issues in insulin secretion, insulin action, or both (1, 2). The International Diabetes Federation (IDF) estimates that ~537 million adults were living with diabetes in 2021, and this number is expected to rise to 643 million by 2030 (3–5). In China, the prevalence of DM has notably increased in recent decades, now affecting over 114 million adults, which represents ~11% of the adult population (6, 7). This chronic metabolic disorder is characterized by either a lack of insulin production or the body's inability to effectively use insulin, presenting growing difficulties on a global scale and affecting people of all socioeconomic backgrounds (8, 9). It is considered one of the leading causes of illness and death worldwide; alarmingly, in 2015, diabetes was linked to almost 5 million fatalities in persons between the ages of 20 and 79 (10, 11). The increased death rates can be attributed to many consequences, including cerebrovascular diseases, renal failure, eyesight impairment, cardiovascular disorders, and limb amputations (12–14). These negative consequences are worsened by the worldwide trend toward increasingly inactive lifestyles and cultural changes that encourage unhealthy eating habits and reduce levels of physical activity (11). Therefore, it is crucial to prioritize the reduction of these risk factors to decrease the occurrence of DM and enhance public health results (15).
Nurses play a crucial role in the management of diabetes, as they often serve as primary caregivers and are directly involved in patient education and care (16, 17). Holistic management, which encompasses a comprehensive, multifactorial approach to care, is increasingly recognized as crucial in managing diabetes effectively (18). Assessing the KAP of nurses regarding holistic diabetes management is vital for identifying gaps in the current healthcare provision and for developing targeted educational and training programs (18). Studies have shown that enhancing nurses' competencies can lead to improved patient outcomes, direct care, and support in self-management practices in diabetes care (18–21). However, there is limited data available on the KAP among nurses in China regarding the holistic management of DM (22).
Several studies have indicated variability in KAP among nurses concerning diabetes care, often associated with differences in education levels, regional healthcare policies, and available resources (20, 21, 23–26). For instance, research in urban hospitals in Beijing showed higher levels of knowledge and more positive attitudes compared to rural areas, where resources and training opportunities tend to be more limited (27). Understanding these disparities is critical for developing targeted educational programs, funding, and policy interventions aimed at enhancing holistic diabetes care (26). Moreover, given the rapid evolution of diabetes treatment protocols and the integration of technological advances in patient care, continual professional development and training are paramount for nursing staff (22).
Nurses are essential in diabetes management, serving as primary caregivers involved in patient education and care. Holistic management, which includes a comprehensive, multifactorial approach, is crucial for effective diabetes care. In this study, “knowledge” refers to understanding diabetes pathophysiology, treatment protocols, and self-management techniques. “Attitudes” encompass nurses' beliefs and perspectives on diabetes care, including holistic and culturally competent approaches. “Practices” involve implementing diabetes care protocols, patient education, and management strategies. Effective self-management, facilitated by nurses, is vital for optimal glycemic control and complication prevention. However, the extent of nurses' knowledge and skills for holistic diabetes management, particularly in China, remains under-examined. Nurses' attitudes and practices significantly influence their ability to educate and support patients, with China's cultural, systemic, and educational frameworks providing a unique context that may differ from Western settings (22, 28, 29). Given this background, the current study aimed to evaluate nurses' self-perceived knowledge, attitudes, and practices concerning diabetes management within Chinese healthcare institutions. In addition, the perceptions influence their professional behaviors and identify areas for educational improvements.
2 Methodology
2.1 Study
To investigate the KAP of nurses in the comprehensive management of DM, we conducted a systematic evaluation via a digital, anonymized survey. This cross-sectional study harnessed a stratified sampling method to disseminate the survey hyperlink across multiple online channels, using the snowball technique, including WeChat, Sina Weibo, QQ, email, and other prominent social networks utilized predominantly within China. A total of 5,000 nurses were invited to participate via email and social media platforms. Out of these, 4,011 nurses responded, resulting in a participation rate of 80.22%. Information on those who declined to participate was not systematically recorded. Participants were mandated to respond to each query on the survey, available in both Mandarin and English. The data collection phase extended from January 2023 to February 2024. Participation was voluntary, with nurses informed about the study's aims and assured of the confidentiality and anonymity of their inputs. The study covered diverse geographical locales across China, integrating both urban and rural healthcare settings. Data anonymization was ensured by assigning unique codes to each participant and removing any identifying information before analysis.
2.2 Inclusion and exclusion criteria
Inclusion criteria were as follows: (i) registered nurses currently practicing in China, and (ii) age 18 years or older. These criteria remained consistent throughout the study. Exclusion criteria included (i) nurses with diagnosed DM, as their personal experiences might skew perceptions, (ii) non-resident nurses temporarily working in China, and (iii) those unable to provide informed consent due to any reason.
2.3 Measurements
The survey tool was meticulously crafted by modifying and integrating elements from previously validated instruments pertinent to diabetes care. The cut-off of ~50% was set following precedents in previous studies, ensuring consistency and comparability of results across similar research (20, 21, 23–26, 30–32). We assessed nurses' self-perceived knowledge through a series of 16 questions covering topics such as the pathophysiology of DM, current treatment protocols, patient education strategies, and self-management techniques. These questions were designed to gauge how confident nurses felt about their knowledge rather than objectively measuring their actual knowledge. Each correct response was awarded one point, with a total possible score of 16. A threshold of ≥50% (eight points) was set to classify respondents as knowledgeable.
Furthermore, we evaluated attitudes toward DM management using 14 questions about personal beliefs, perceived efficacy of treatment modalities, and readiness to implement holistic care approaches. Attitude scores were allocated based on responses, with “Agree” scoring one point, reflecting a positive orientation, and “Disagree” or “Uncertain” scoring zero. A cutoff of seven was used to differentiate between predominantly positive and negative attitudes.
In addition, practices were scrutinized using eight questions related to the implementation of diabetes management protocols, participation in diabetes education programs, and adherence to clinical guidelines. Practice scores were calculated by assigning one point for each affirmative response indicative of best practices. The cutoff score of five for practice behaviors was determined based on prior studies and expert consultations.
Responses of “Not Sure” were categorized as “No” for knowledge, attitudes, and practices. This conservative approach ensured that only confident affirmative responses were considered as “Yes”, maintaining the study's rigor by treating uncertainty as a lack of knowledge or negative attitude. Academic qualifications were categorized as follows: Associate Degree in Nursing (typically 2–3 years of study), Bachelor of Science in Nursing (4 years), Master of Science in Nursing (two additional years post-bachelor), and Doctor of Nursing Practice (3–4 additional years post-master). The survey further collected detailed demographic information to explore correlations between these factors and KAP results. Specific questions included years of nursing experience, gender, marital status, type of institution employed in (hospital, clinic), the highest level of educational attainment, employment status (full-time, part-time, other), and primary department of work within the healthcare facility.
2.4 Statistical analysis
In this study, the statistical analysis was rigorously conducted using both exploratory and inferential techniques to comprehensively evaluate the data gathered from the survey on DM management among nurses. The initial step involved summarizing the frequency distributions of socio-demographic variables via descriptive statistical analysis. All statistical computations were executed using R statistical software (version 4.2.2). We managed our datasets using the R environment, leveraging several packages such as dplyr for data manipulation and ggplot2 for graphical representations. Instead of using traditional reliability measures like Cronbach's alpha, we opted for Guttman's λ2, which we calculated to be 0.86, suggesting the high reliability of the survey instrument without the stringent assumptions required by Cronbach's alpha (33). Further, binary logistic regression was employed to ascertain the Odds Ratio (ORs), which provided insights into the likelihood of high knowledge, positive attitudes, and effective practices among the nurses based on predictor variables. This was complemented with the reporting of regression coefficients, their significance levels, and 95% confidence intervals (CI) to reinforce the robustness of our findings.
3 Results
3.1 Social and demographic characteristics
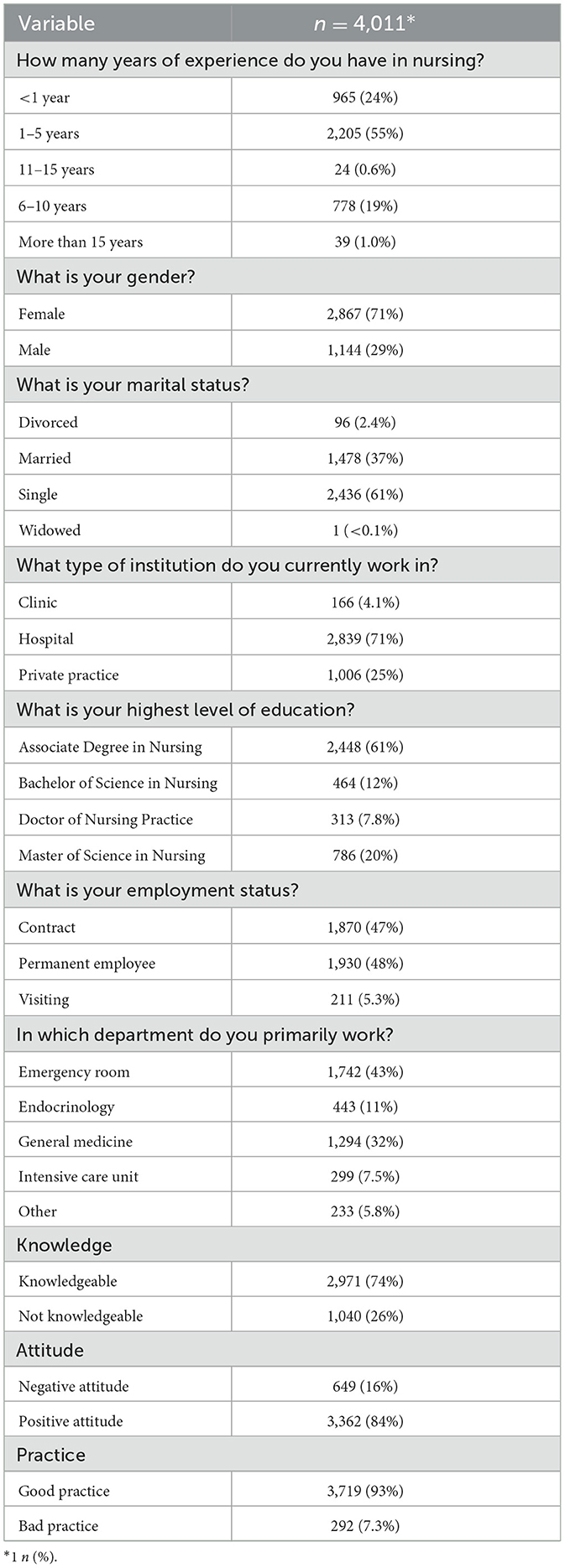
In the current study, a total of 4,011 registered nurses participated, yielding significant insights into their demographics and professional backgrounds. The distribution of experience notably concentrates in the 1–5 years category with 55% (n = 2,205), while a large majority, 71% (n = 2,867), of the cohort are female, and 61% (n = 2,436) reported being single. Work settings are heavily skewed toward hospitals at 71% (n = 2,839), with 61% (n = 2,448) holding an Associate Degree in Nursing. Employment is nearly equally divided between contract positions at 47% (n = 1,870) and permanent roles at 48% (n = 1,930). Nurses are primarily deployed in emergency rooms (43%, n = 1,742) and general medicine (32%, n = 1,294). In terms of professional competency in DM management, 74% (n = 2,971) of nurses are classified as knowledgeable. Attitudes toward their practice are positive for 84% (n = 3,362), and a substantial 93% (n = 3,719) engage in good practice. These data points underscore crucial areas for targeted educational and policy initiatives to boost the efficacy of diabetes care (Table 1).
3.2 Knowledge assessment
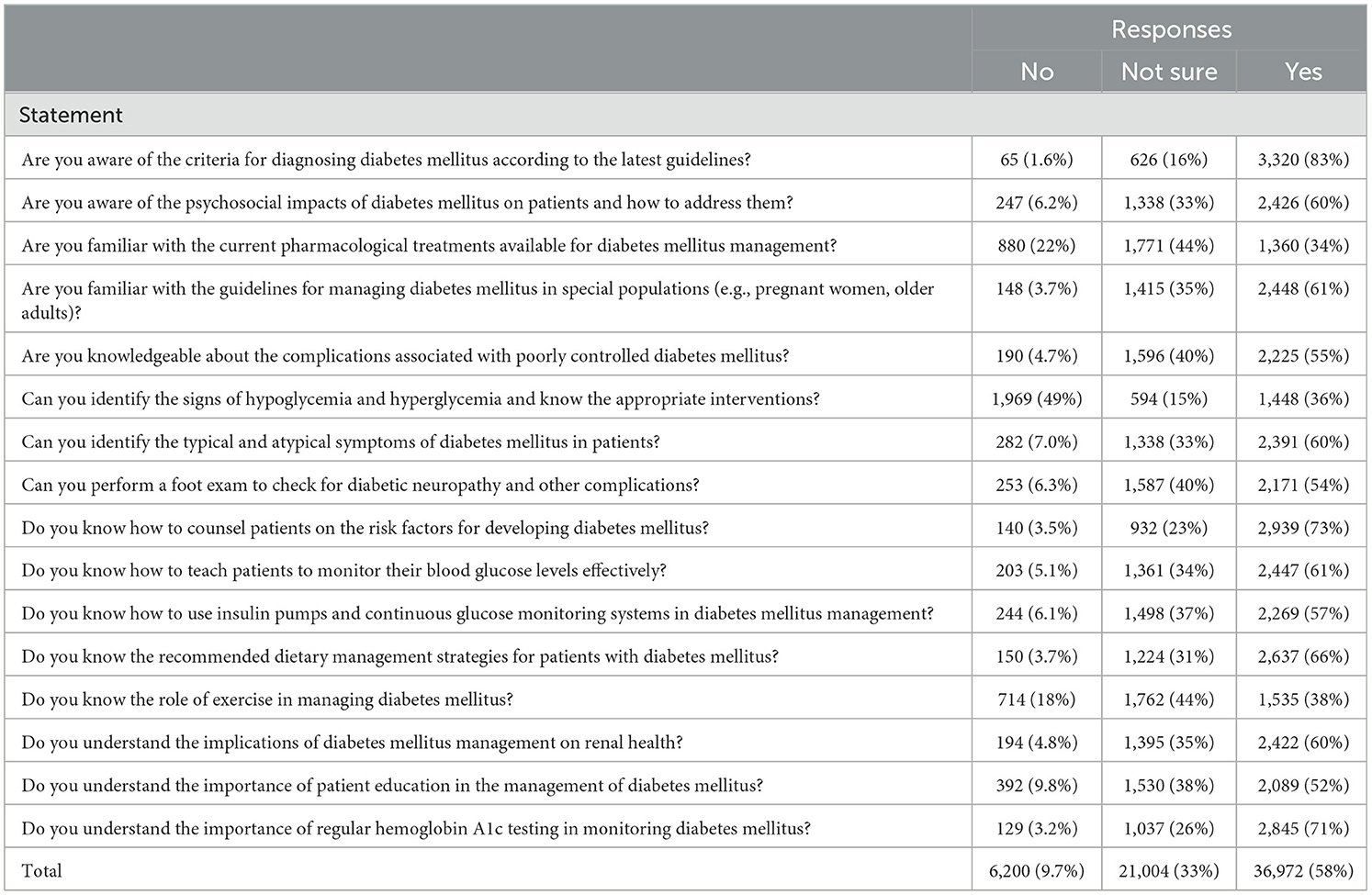
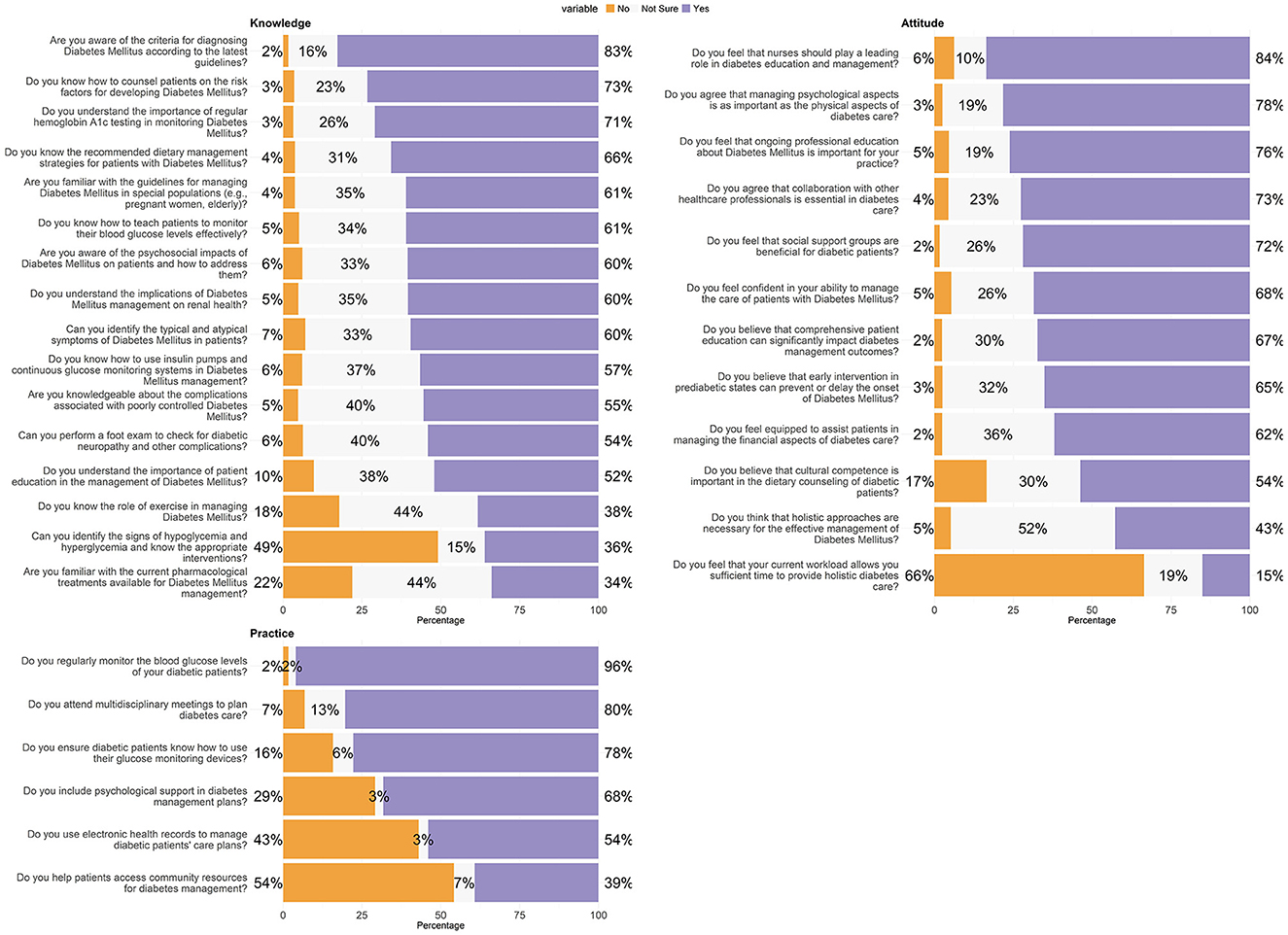
Table 2 provides a comprehensive evaluation of the knowledge level among participants regarding various aspects of DM management. The data highlights areas where knowledge is well-established and areas where improvement is needed. The vast majority of participants (83%, n = 3,320) are familiar with the criteria for diagnosing DM according to the latest guidelines, demonstrating a strong awareness of foundational diagnostic criteria. However, knowledge gaps appear in more specialized areas, such as the management of DM in special populations like pregnant women and the older adults, where only 61% (n = 2,448) feel confident. Similarly, while a majority understands the psychosocial impacts of DM (60%, n = 2,426) and complications associated with poor control (55%, n = 2,225), there is less certainty about current pharmacological treatments, with only 34% (n = 1,360) indicating familiarity. A significant concern is the high percentage of respondents who lack confidence in identifying the signs of hypoglycemia and hyperglycemia (49%, n = 1,969), which are critical skills for effective patient management. This highlights a crucial need for enhanced training and education. Responses also show that 73% (n = 2,939) of nurses are adept at counseling patients on risk factors, and a comparable majority (61%, n = 2,447) can teach patients to monitor their blood glucose levels effectively. Knowledge about the use of technology in management, like insulin pumps and continuous glucose monitoring systems, is moderately high at 57% (n = 2,269). The role of lifestyle factors in managing DM is less well-understood; only 38% (n = 1,535) are familiar with the role of exercise, indicating a potential area for educational interventions, as shown in Figure 1.
3.3 Attitude assessment
Table 3 delineates the attitudes of participants toward various facets of diabetes care, highlighting the consensus and areas of ambivalence among the nursing professionals surveyed. A significant majority of respondents, 73% (n = 2,912), recognize the essential nature of collaboration with other healthcare professionals in diabetes care, reflecting a widespread appreciation for interdisciplinary approaches.
Similarly, 78% (n = 3,139) agree that managing psychological aspects is as important as addressing the physical aspects of diabetes care, indicating a holistic understanding of patient needs. This is further supported by the 67% (n = 2,702) who believe that complete patient education can significantly influence diabetes management outcomes, emphasizing the role of education in effective diabetes care. However, attitudes vary concerning cultural competence in dietary counseling, with only 54% (n = 2,155) acknowledging its importance, suggesting a potential area for further training and awareness. Another notable insight is the strong endorsement of early intervention in prediabetic states to prevent or delay the onset of DM, supported by 65% (n = 2,612) of participants.
The confidence in managing diabetes care is affirmed by 68% (n = 2,747) of the nurses. However, only 62% (n = 2,486) feel equipped to assist patients in managing the financial aspects of their care, indicating a gap in addressing the economic challenges faced by patients. A substantial 84% (n = 3,351) feel that nurses should play a leading role in diabetes education and management, and 76% (n = 3,053) recognize the importance of ongoing professional education in their practice. This is congruent with the 72% (n = 2,884) who see social support groups as beneficial for diabetic patients, underscoring the value placed on community and continuing education. Contrastingly, a significant majority, 66% (n = 2,666), feel that their current workload does not allow them sufficient time to provide holistic diabetes care, highlighting systemic constraints that may hinder the optimal delivery of care. Moreover, the necessity of holistic approaches in diabetes management garners less consensus, with only 43% (n = 1,712) endorsing this perspective amidst a substantial 52% (n = 2,091) unsure, suggesting an area ripe for further exploration and advocacy in the professional community, as shown in Figure 1.
3.4 Practice assessment
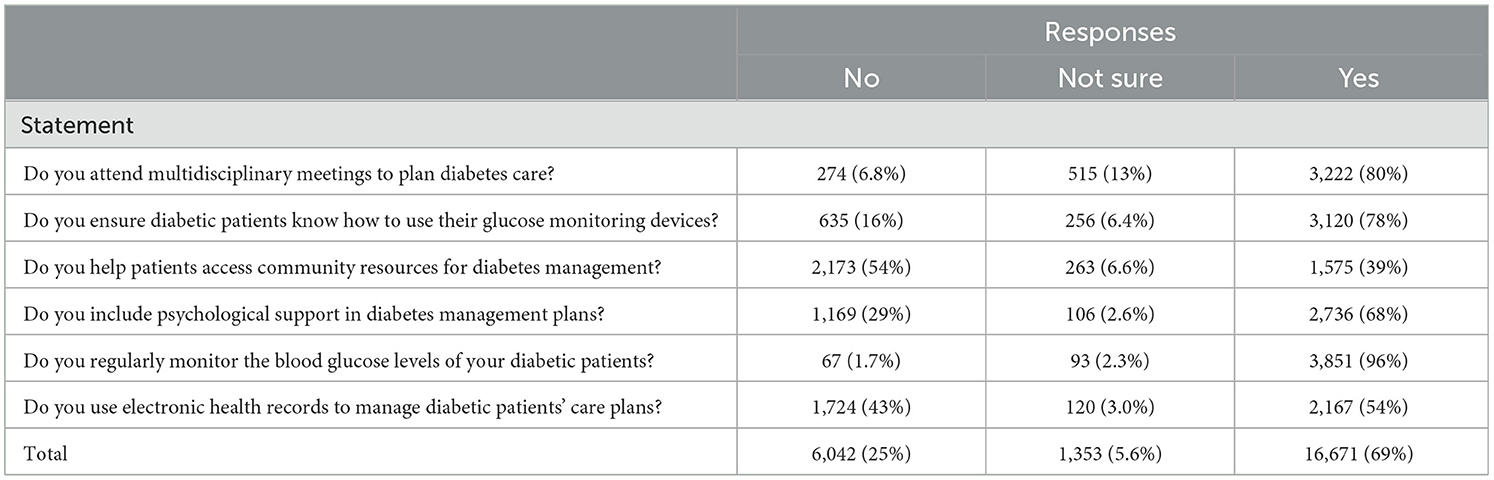
Table 4 assesses the practical engagement of participants in the management of diabetes care, revealing strong adherence to several best practices while identifying areas where improvement could be beneficial. Most nurses, 80% (n = 3,222), actively participate in multidisciplinary meetings to plan diabetes care, illustrating a robust collaborative practice among healthcare professionals.
Moreover, a significant 78% (n = 3,120) ensure that diabetic patients are proficient in using their glucose monitoring devices, which is crucial for the day-to-day management of their condition. Similarly, the monitoring of blood glucose levels is nearly universal among respondents, with 96% (n = 3,851) regularly performing this essential task, reflecting a high level of diligence in patient care. However, the responses also highlight some areas needing attention. Although 68% (n = 2,736) include psychological support in their management plans, indicating a holistic approach to patient care, there remains a significant portion of nurses who could further integrate this critical aspect into their routines. The use of electronic health records (EHRs) to manage care plans is reported by 54% (n = 2,167) of the participants, suggesting that there is room for increased adoption of this technology to enhance patient management efficiency. Additionally, helping patients access community resources for diabetes management appears to be a less frequent practice, with only 39% (n = 1,575) actively assisting in this area, indicating a potential gap in fully supporting patients beyond clinical settings, as shown in Figure 1.
3.5 Binary logistic regression
3.5.1 Statistical correlates of knowledge level in nursing professionals
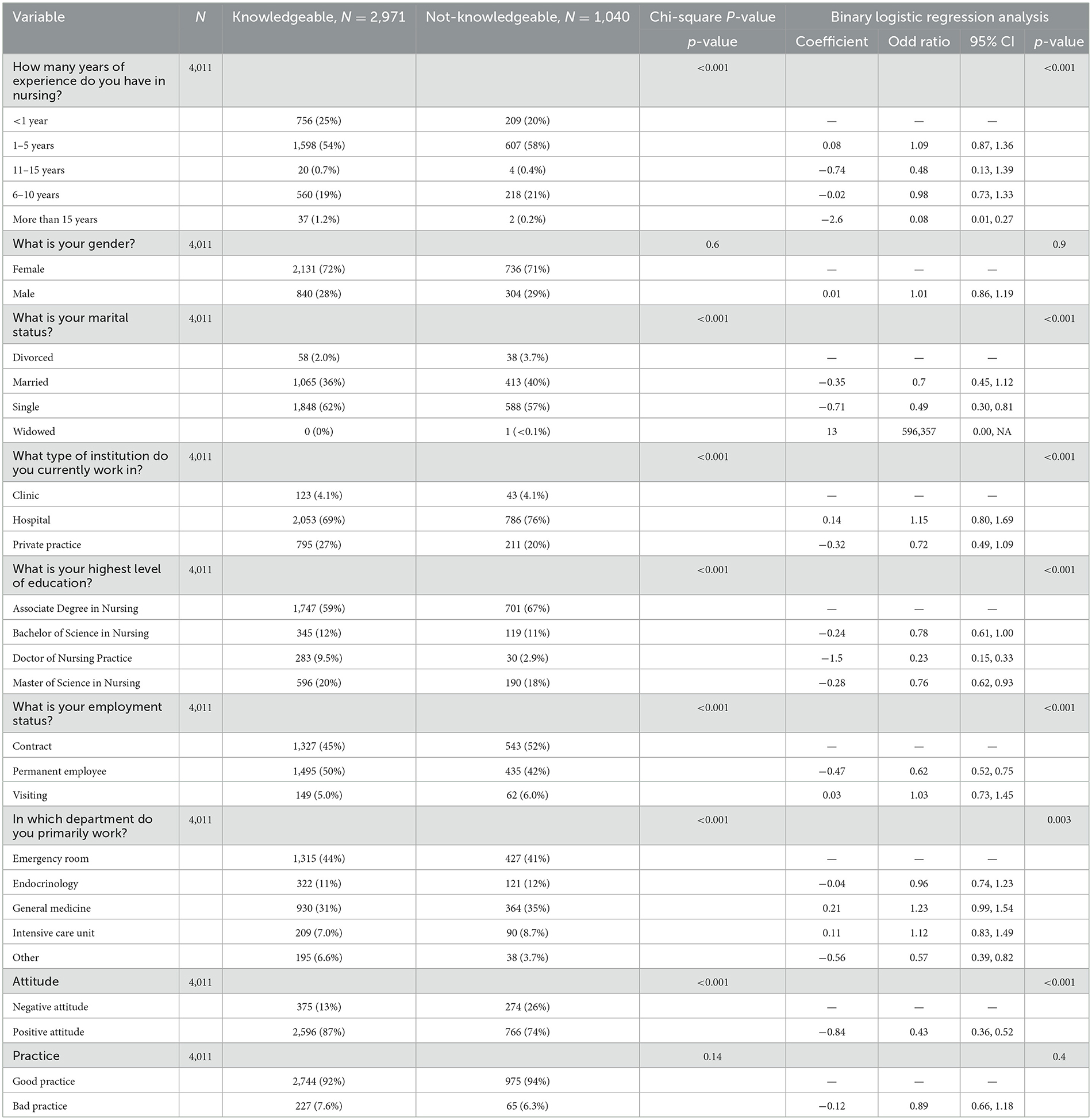
The dataset comprises 4,011 participants, categorized into “Knowledgeable” nurses (n = 2,971) and “Not Knowledgeable” (n = 1,040) nurses. Statistical analyses, including Chi-square tests and binary logistic regression, were utilized to examine the influence of various variables on knowledge levels.
In terms of years of nursing experience, significant differences in knowledge levels were observed (Chi-square p < 0.001). Notably, nurses with more than 15 years of experience showed a significantly lower likelihood of being knowledgeable OR = 0.08, 95% CI = 0.01–0.27, p < 0.001). Conversely, those with 1–5 years of experience exhibited a moderately higher knowledge level, though this was not statistically significant (OR = 1.09, 95% CI = 0.87–1.36, p = 0.08). Regarding demographic variables, marital status revealed significant effects (Chi-square p < 0.001), with single nurses being more likely to be knowledgeable compared to their married or divorced counterparts (OR = 0.49, 95% CI = 0.30–0.81, p < 0.001 for singles). The work environment also impacted knowledge levels significantly (Chi-square p < 0.001). Nurses employed in hospitals were somewhat more likely to be knowledgeable (OR = 1.15, 95% CI = 0.80–1.69, p = 0.14), whereas those in private practice were less likely to be knowledgeable (OR = 0.72, 95% CI = 0.49–1.09, p < 0.001). Educational attainment strongly correlated with knowledge, where nurses with a Doctor of Nursing Practice were significantly more likely to be knowledgeable (OR = 0.23, 95% CI = 0.15–0.33, p < 0.001). However, the attitude toward nursing practice significantly differentiated knowledge levels (Chi-square p < 0.001). Nurses with a positive attitude were twice as likely to be knowledgeable compared to those with a negative outlook (OR = 0.43, 95% CI = 0.36–0.52, p < 0.001). Overall, these results underscore the complex interplay of experience, demographic factors, work environment, educational background, and attitude in shaping knowledge levels among nurses (Table 5).
3.5.2 Statistical correlates of attitude in nursing professionals
This analysis encompasses data from 4,011 nursing professionals, stratified into “Negative Attitude” (n = 649) and “Positive Attitude” (n = 3,362) groups. The influence of various professional and demographic variables on attitudes was assessed using Chi-square tests and binary logistic regression models, yielding significant findings (Chi-square p < 0.001 across multiple variables).
Experience in nursing emerged as a significant determinant of attitude (Chi-square p < 0.001). Nurses with < 1 year of experience displayed a lower incidence of positive attitudes compared to those with more experience. In contrast, nurses with more than 15 years of experience had markedly higher odds of possessing a positive attitude (OR = 5.79, 95% CI = 2.66–12.4, p < 0.001), highlighting the potential impact of extensive professional experience on attitude formation. Gender differences were also pronounced, with males showing higher odds of having a positive attitude compared to females (OR = 2.18, 95% CI = 1.80–2.64, p < 0.001). Marital status further influenced attitudes, with single nurses more likely to exhibit a positive attitude compared to their married or divorced peers (OR for singles = 0.19, 95% CI = 0.11–0.33, p < 0.001). However, in work settings, nurses employed in hospitals and private practices had lower odds of possessing a positive attitude compared to those in clinics, though the effect was moderate (OR for hospitals = 0.6, 95% CI = 0.41–0.89, p = 0.03).
Educational attainment was a strong predictor of attitude. Nurses with a Master of Science in Nursing were significantly less likely to have a positive attitude compared to those with lower educational qualifications (OR = 0.17, 95% CI = 0.12–0.24, p < 0.001). Permanent employees and those working in general medicine had slightly lower odds of a positive attitude (OR for permanent employees = 0.94, 95% CI = 0.76–1.17, p = 0.8). Knowledge and practice were also significant, with knowledgeable and well-practicing nurses more likely to hold positive attitudes (OR for knowledgeable = 2.36, 95% CI = 1.95–2.86, p < 0.001 for knowledge; OR for good practice = 0.57, 95% CI = 0.37–0.85, p = 0.005 for practice). These results underscore the multifaceted nature of attitude formation among nurses, influenced by professional experience, demographic traits, educational background and workplace environment influence professional practices, as shown in Table 6.
3.5.3 Statistical correlates of practice variations in nursing professionals
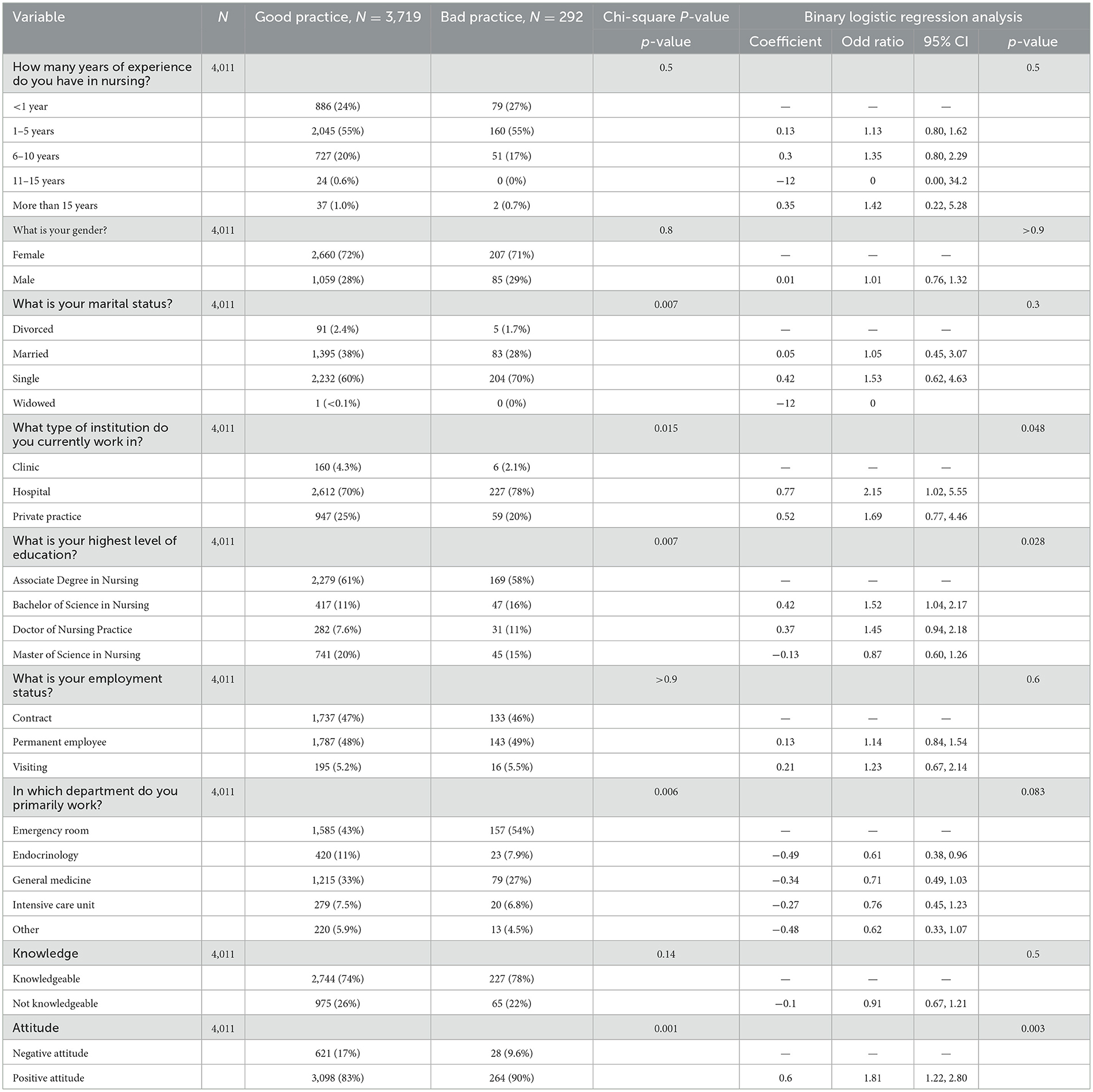
In the present investigation, we scrutinized a dataset comprising 4,011 nursing professionals to delineate the association between various professional and demographic variables and their adherence to established practice norms, categorically differentiated into “Good Practice” (n = 3,719) and “Bad Practice” (n = 292). Utilizing Chi-square tests and binary logistic regression analyses, significant statistical correlations were unearthed that elucidate the influence of these variables on nursing practices.
Professional tenure emerged as a salient variable, albeit with nuanced disparities in its influence on practice outcomes. Specifically, nurses with an intermediate level of experience (6–10 years) exhibited a marginally enhanced propensity toward adhering to good practice standards (OR = 1.35, 95% CI = 0.80–2.29, p = 0.3). However, this association did not achieve statistical significance. Marital status demonstrated a moderate correlation with practice quality, particularly among single nurses who exhibited an increased likelihood of engaging in good practice (OR = 1.53, 95% CI = 0.62–4.63, p = 0.3), though these findings lacked statistical significance. The type of healthcare institution also played a pivotal role, with nurses employed in hospitals demonstrating a higher likelihood of maintaining good practice standards compared to their counterparts in private practices or clinics (OR = 2.15, 95% CI = 1.02–5.55, p = 0.048).
Nurses holding a Bachelor of Science in Nursing degree were significantly more inclined to exhibit good practice behaviors compared to those with alternative qualifications (OR = 1.52, 95% CI = 1.04–2.17, p = 0.028), underscoring the impact of advanced educational credentials on practice quality. Conversely, employment status exhibited no discernible effect on practice quality, indicating that the contractual nature of employment—whether permanent, contractual, or visiting—did not distinctively influence practice outcomes (OR for permanent employees = 1.14, 95% CI = 0.84–1.54, p = 0.6). Departmental affiliation provided additional insights, with nurses in the Endocrinology department more likely to adhere to good practice standards compared to those in other departments (OR = 0.61, 95% CI = 0.38–0.96, p = 0.083), suggesting that specialization may exert an influence on practice behaviors. Professional attitude toward the nursing role had a definitive impact, with individuals harboring a positive attitude significantly more inclined toward good practices (OR = 1.81, 95% CI = 1.22–2.80, p = 0.003). These findings articulate a complex interplay of factors such as experience, marital status, institutional context, educational background, and professional attitude in modulating nursing practices, which are pivotal for the delivery of efficacious patient care (Table 7).
3.6 Key observations on nurses' knowledge, attitudes, and practices
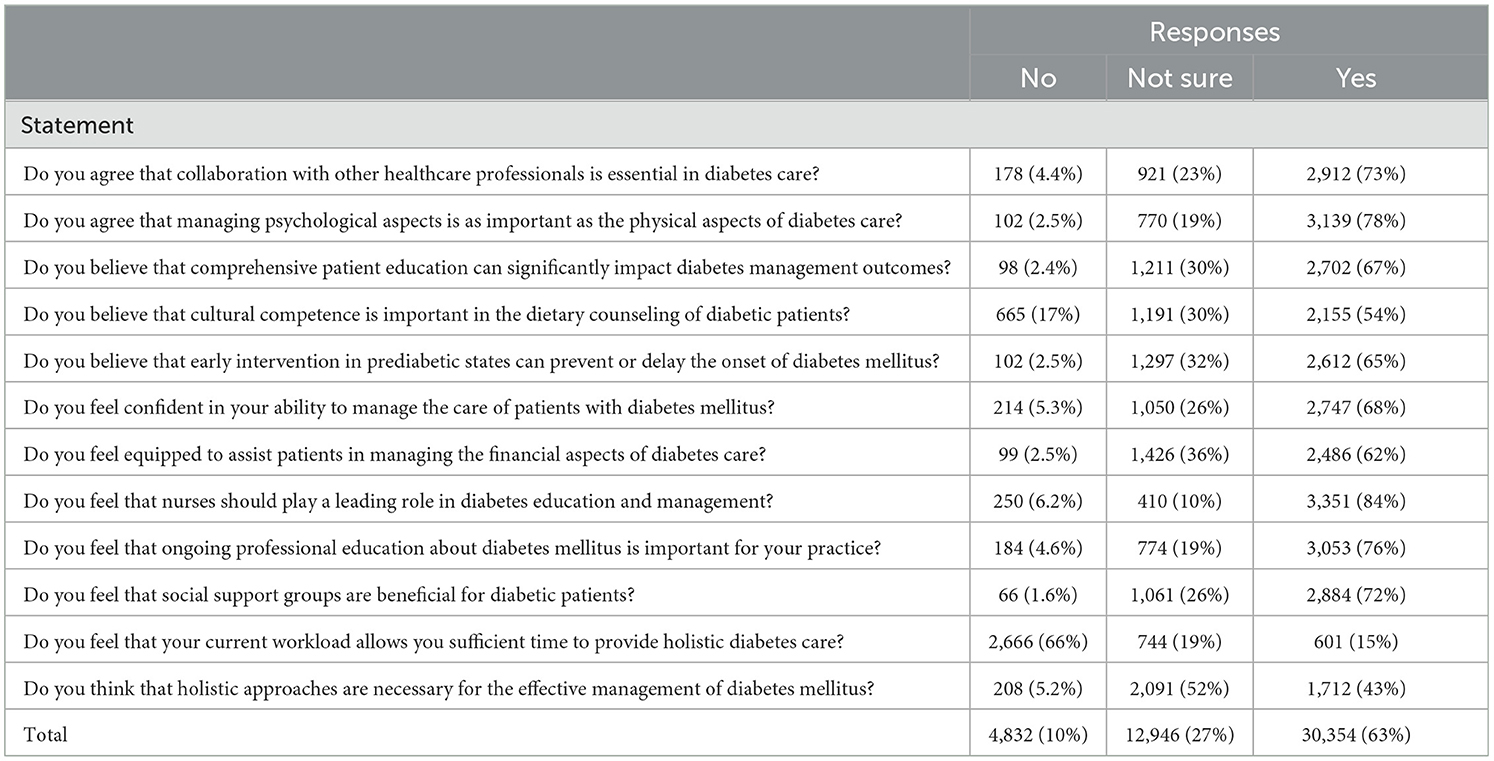
Nursing professionals with “1–5 years” of experience exhibit a significant inclination toward being “Knowledgeable”, evidenced by the substantial chords connecting these segments. Similarly, the “Female” gender segment has a robust association with a “Positive Attitude”, highlighted by the thick chords. In contrast, the “More than 15 years” experience category shows fewer individuals with a “Not-Knowledgeable” attribute, suggesting that extensive experience might correlate with a higher likelihood of possessing substantial professional knowledge. Educational levels, particularly those holding an “Associate Degree in Nursing”, demonstrate a strong connection to being “Knowledgeable”, while “Doctor of Nursing Practice” and “Master of Science in Nursing” segments are predominantly linked to “Good Practice”. This visualization suggests a correlation between advanced educational qualifications and the propensity to engage in best practice behaviors, as shown in Figure 2.
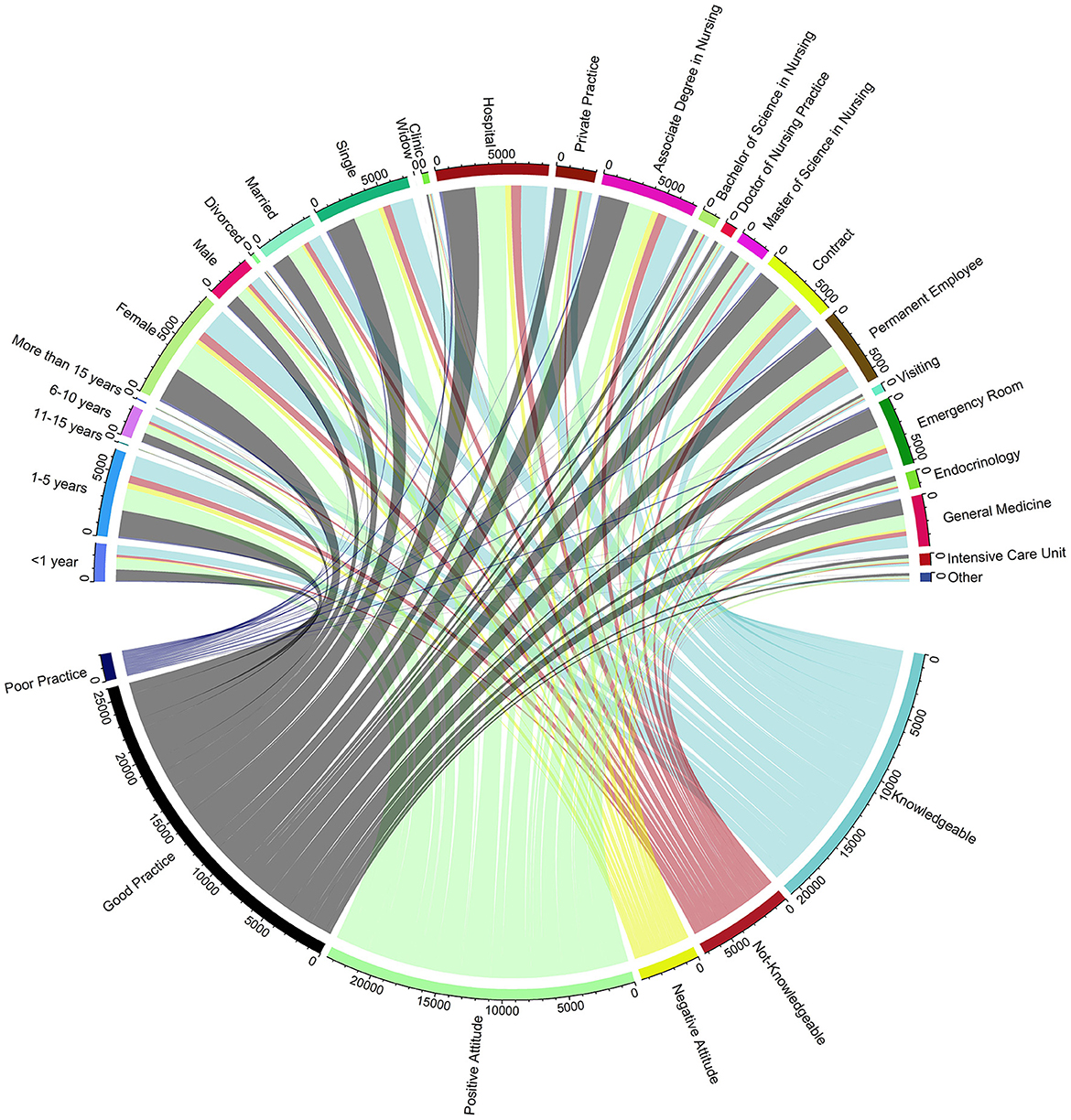
Figure 2. Correlation between demographic characteristics, educational background, work environment, and knowledge, attitudes, and practices. this chord diagram shows the relationships between demographic factors, educational background, work environment, and nurses' knowledge, attitudes, and practices (KAP) in diabetes management. Outer segments represent categories; inner chords indicate connections to KAP outcomes.
4 Discussion
The results from this study provided significant insights into the demographics, KAP, of nurses in diabetes management. A substantial majority of the participating nurses were women with a background in hospital settings, highlighting the need for targeted educational programs in these environments. While there was a commendable level of foundational knowledge regarding the diagnosis of DM, notable gaps were evident in specialized knowledge areas, particularly in managing diabetes in special populations and the use of advanced technologies. Attitudes toward interdisciplinary collaboration and the psychological aspects of diabetes care were generally positive, yet there was a disparity in recognizing the importance of cultural competence in dietary counseling. Practice assessments revealed strong adherence to best practices like regular blood glucose monitoring and participation in multidisciplinary meetings but also pointed out areas for improvement, such as the integration of psychological support and utilization of electronic health records. These findings underscored the critical areas where educational and policy initiatives could significantly enhance the efficacy and comprehensiveness of diabetes care delivered by nurses.
The study involved 4,011 registered nurses, predominantly female (71%) and with 1–5 years of experience (55%). This demographic profile aligns with findings from who reported a predominance of early-career female nurses in urban hospital settings. The high percentage of nurses holding an Associate Degree in Nursing (61%) is slightly above the national average reported by the American Association of Colleges of Nursing, which could reflect regional educational trends or specific recruitment policies of the hospitals involved in the study (34, 35). Our results demonstrated that a high proportion of participants (83%) are well-versed in the criteria for diagnosing DM, echoing findings from other studies that highlight strong foundational knowledge in healthcare professionals (36). However, our study revealed considerable knowledge gaps in managing DM, with only 61% confidence reported among participants. This discrepancy is notable when compared to the literature, where higher competence is often noted, possibly due to targeted training programs in these areas (37). The lower familiarity with pharmacological treatments in our study (34%) could be attributed to the rapid evolution of diabetes management protocols, which may outpace standard nursing curricula (38, 39).
Our analysis revealed that nurses with more than 15 years of experience were less likely to be knowledgeable, a finding that contrasts with the assumption that expertise correlates positively with knowledge. This may be due to the obsolescence of earlier training not aligned with modern guidelines (40, 41). In contrast, those with 1–5 years of experience showed a non-significantly higher knowledge level, possibly reflecting more recent and updated educational exposures. Marital status and work environment also significantly impacted knowledge levels, with single nurses and those in hospital settings displaying higher knowledge levels. This supports literature suggesting that dynamic hospital environments provide more continual learning opportunities compared to private practices (42, 43).
Notably, attitudes toward nursing practice showed a significant correlation with knowledge levels. Nurses with a positive attitude were twice as likely to be knowledgeable, a finding supported by research that links positive professional attitudes with enhanced engagement and proactive learning (44, 45). This underscores the importance of fostering supportive environments that cultivate positive attitudes among healthcare professionals (46, 47). Furthermore, this study significantly contributes to existing knowledge by highlighting the critical role of demographics and professional environment in nursing education, particularly in specialized areas of DM management.
Our study found that a significant majority (73%, n = 2,912) of nursing professionals recognize the importance of interdisciplinary collaboration in diabetes care, which is consistent with the literature that underscores the effectiveness of collaborative approaches in chronic disease management (36). Similarly, the appreciation for managing psychological aspects alongside physical health, as indicated by 78% (n = 3,139) of respondents, aligns with recommendations for holistic patient care (48, 49). However, some studies suggest potential barriers to integrating psychological care, primarily due to time constraints and lack of specific training, which might explain the lower consensus on holistic care approaches observed in our study (43% endorsement) (50–52). The strong belief in the impact of patient education on DM management outcomes, supported by 67% (n = 2,702) of our participants, echoes the findings of previous studies highlighting education as a critical component of effective diabetes management (53, 54). However, our results also reveal a gap in recognizing the importance of cultural competence in dietary counseling, with only 54% (n = 2,155) acknowledging its significance. This discrepancy could be attributed to varying levels of exposure to culturally diverse populations and suggests a need for enhanced training programs that emphasize cultural sensitivity in care provision (52, 54).
Our findings indicate a gap in nurse preparedness to assist with the financial aspects of diabetes care, as only 62% (n = 2,486) feel equipped to address these issues. Literature suggests that economic barriers significantly affect patient adherence to treatment plans, underscoring the need for comprehensive training that includes financial navigation (55, 56). Moreover, the concern about workload constraints, as expressed by 66% (n = 2,666) of the nurses, mirrors the broader issues within the healthcare system that limit the time available for holistic care (57, 58).
Our statistical analysis revealed significant determinants of nursing attitudes toward diabetes care. Experience, gender, marital status, and workplace setting were all influential, consistent with prior research indicating that these factors shape healthcare professionals' perceptions and practices (59, 60). Notably, our finding that nurses with more experience are more likely to have a positive attitude is supported by studies that link professional experience with enhanced competence and confidence in patient care (60). Our study contributes to the existing body of knowledge by providing contemporary data on nurses' attitudes toward various aspects of diabetes care, highlighting areas of consensus as well as aspects requiring further attention and development. The significant statistical correlates identified offer insights into the factors that influence healthcare attitudes and practices, thereby informing targeted interventions to enhance diabetes care quality.
The majority of nurses (80%, n = 3,222) demonstrated a robust engagement in multidisciplinary meetings for diabetes care planning. This finding is consistent with the literature, which emphasizes the importance of collaborative practices in enhancing patient outcomes (61). Additionally, 78% (n = 3,120) of nurses ensured proficiency in the use of glucose monitoring devices among patients, a practice pivotal for effective diabetes management (11, 62). However, our study also identified gaps in the integration of psychological support and the use of EHRs, with only 68% (n = 2,736) including psychological support in their management plans and 54% (n = 2,167) utilizing EHRs. These areas lag behind the optimal standards suggested by recent studies, which highlight the critical nature of comprehensive support systems and technological integration in chronic disease management (63, 64).
Our findings on professional tenure and educational background offer insights into practice variability. Intermediate-experienced nurses showed an increased, though statistically insignificant, adherence to good practices, a trend that diverges slightly from the significant positive correlation found in the literature (65). Additionally, the influence of educational background, particularly holding a Bachelor of Science in Nursing, significantly correlated with better practice standards, reinforcing the literature that links higher educational qualifications with improved care delivery (65, 66). This study highlights the complex influences on nursing practices and suggests targeted interventions and policies to improve diabetes care through education and technology use. It deepens the understanding of demographic and professional impacts on care efficiency, providing a basis for future research and policy enhancement.
Additionally, the reliance on self-reported data may introduce response bias, as participants might provide socially desirable answers rather than reflecting true behaviors or beliefs. While the stratified sampling method aimed to ensure a representative sample, the potential for selection bias exists, especially given the voluntary nature of participation. This could result in an overrepresentation of nurses who are more engaged or interested in diabetes care, skewing the results toward more favorable KAP outcomes. The exclusive use of online channels for survey dissemination might have excluded nurses with limited internet access or digital literacy, potentially biasing the sample toward those more comfortable with technology.
5 Conclusion
This comprehensive analysis of 4,011 nursing professionals provides critical insights into the factors influencing diabetes management KAP among registered nurses. Key findings highlight the significant impact of professional experience, educational attainment, and work environment on diabetes care competencies. Nurses with 1–5 years of experience tend to have higher knowledge levels, indicating that recent education aligns closely with current diabetes management standards. In contrast, those with over 15 years of experience show reduced knowledge, suggesting a gap between their training and modern clinical protocols. Educational qualifications profoundly influence outcomes; higher degrees, such as a Doctor of Nursing Practice, correlate with better knowledge and adherence to best practice guidelines, emphasizing the need for advanced education in enhancing nursing competencies. Attitudinal data reveal a strong recognition of the need for psychological support and interdisciplinary collaboration in diabetes care, yet there is variability in the acceptance of cultural competence in dietary counseling. This underscores the potential for targeted educational interventions to bridge these gaps. Overall, the study advocates for focused educational programs and systemic enhancements to optimize diabetes care and improve nurse efficacy and satisfaction in their critical roles.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical approval was obtained from the Departmental Bioethical Committee of the Department of Endocrinology, the Central Hospital of Enshi Tujia, and Miao Autonomous Prefecture. Informed consent was taken from all participants before they participated in the study.
Author contributions
LH: Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Resources, Software, Visualization, Writing – original draft. WJ: Conceptualization, Data curation, Funding acquisition, Project administration, Software, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We gratefully acknowledge the vital contributions of all nursing staff who participated in this study, sharing their insights and experiences, which have been essential to this research. We also appreciate the assistance from our colleagues, who provided critical feedback and helped in the data analysis phase.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Rachdaoui N. Insulin: the friend and the foe in the development of type 2 diabetes mellitus. Int J Mol Sci. (2020) 21:1770. doi: 10.3390/ijms21051770
2. Soomro MH, Jabbar A. Diabetes Etiopathology, Classification, Diagnosis, and Epidemiology. BIDE's Diabetes Desk Book: Elsevier (2024). p. 19–42. doi: 10.1016/B978-0-443-22106-4.00022-X
3. Kumar A, Gangwar R, Ahmad Zargar A, Kumar R, Sharma A. Prevalence of diabetes in India: a review of IDF diabetes atlas 10th edition. Curr Diabetes Rev. (2024) 20:105–14. doi: 10.2174/1573399819666230413094200
4. Hossain MJ, Al-Mamun M, Islam MR. Diabetes mellitus, the fastest growing global public health concern: early detection should be focused. Health Sci Rep. (2024) 7:e2004. doi: 10.1002/hsr2.2004
5. Salsabila Z, Sjaaf AC. The analysis of diabetes self-management implementation on type 2 diabetes mellitus patients: a protocol for systematic review and meta-analysis. Jurnal Ekonomi Kesehatan Indonesia. (2022) 7:133–48. doi: 10.7454/eki.v7i2.6100
6. Li X, Tan TE, Wong TY, Sun X. Diabetic retinopathy in China: epidemiology, screening and treatment trends—A review. Clin Exp Ophthalmol. (2023) 51:607–26. doi: 10.1111/ceo.14269
7. Meng X, Liu X, Tan J, Sheng Q, Zhang D, Li B, et al. From Xiaoke to diabetes mellitus: a review of the research progress in traditional Chinese medicine for diabetes mellitus treatment. Chin Med. (2023) 18:75. doi: 10.1186/s13020-023-00783-z
8. Arokiasamy P, Salvi S, Selvamani Y. Global Burden of Diabetes Mellitus. Handbook of Global Health. Springer International Publishing (2021). p. 1–44.
9. Butt MD, Ong SC, Rafiq A, Malik T, Sajjad A, Batool N, et al. An observational multi-center study on type 2 diabetes treatment prescribing pattern and patient adherence to treatment. Sci Rep. (2023) 13:23037. doi: 10.1038/s41598-023-50517-2
10. Ogurtsova K, da Rocha Fernandes J, Huang Y, Linnenkamp U, Guariguata L, Cho NH, et al. IDF Diabetes atlas: global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract. (2017) 128:40–50. doi: 10.1016/j.diabres.2017.03.024
11. Bommer C, Heesemann E, Sagalova V, Manne-Goehler J, Atun R, Bärnighausen T, et al. The global economic burden of diabetes in adults aged 20–79 years: a cost-of-illness study. Lancet Diabetes Endocrinol. (2017) 5:423–30. doi: 10.1016/S2213-8587(17)30097-9
12. Dal Canto E, Ceriello A, Rydén L, Ferrini M, Hansen TB, Schnell O, et al. Diabetes as a cardiovascular risk factor: an overview of global trends of macro and micro vascular complications. Eur J Prev Cardiol. (2019) 26(2_suppl):25–32. doi: 10.1177/2047487319878371
13. Lee E, Keen H, Bennett P, Fuller J, Lu M, Group WMS. Follow-up of the WHO Multinational Study of Vascular Disease in Diabetes: general description and morbidity. Diabetologia. (2001) 44:S3–S13. doi: 10.1007/PL00002936
14. Lazzarini PA, Pacella RE, Armstrong DG, van Netten JJ. Diabetes-related lower-extremity complications are a leading cause of the global burden of disability. Diabet Med. (2018) 35:1297–9. doi: 10.1111/dme.13680
15. Schulze MB, Hu FB. Primary prevention of diabetes: what can be done and how much can be prevented? Annu Rev Public Health. (2005) 26:445–67. doi: 10.1146/annurev.publhealth.26.021304.144532
16. Sørensen M, Groven KS, Gjelsvik B, Almendingen K, Garnweidner-Holme L. The roles of healthcare professionals in diabetes care: a qualitative study in Norwegian general practice. Scand J Prim Health Care. (2020) 38:12–23. doi: 10.1080/02813432.2020.1714145
17. Swiatoniowska N, Sarzyńska K, Szymańska-Chabowska A, Jankowska-Polańska B. The role of education in type 2 diabetes treatment. Diabetes Res Clin Pract. (2019) 151:237–46. doi: 10.1016/j.diabres.2019.04.004
18. McGill M, Felton A-M. New global recommendations: a multidisciplinary approach to improving outcomes in diabetes. Prim Care Diabetes. (2007) 1:49–55. doi: 10.1016/j.pcd.2006.07.004
19. Tschannen D, Aebersold M, Sauter C, Funnell MM. Improving nurses' perceptions of competency in diabetes self-management education through the use of simulation and problem-based learning. J Cont Educ Nurs. (2013) 44:257–63. doi: 10.3928/00220124-20130402-16
20. Farzaei M, Shahbazi S, Gilani N, Ostadrahimi A, Gholizadeh L. Nurses' knowledge, attitudes, and practice with regards to nutritional management of diabetes mellitus. BMC Med Educ. (2023) 23:192. doi: 10.1186/s12909-023-04178-4
21. Qasim M, Awan UA, Afzal MS, Saqib MA, Siddiqui S, Ahmed H. Dataset of knowledge, attitude, practices and psychological implications of healthcare workers in Pakistan during COVID-19 pandemic. Data Brief. (2020) 32:106234. doi: 10.1016/j.dib.2020.106234
22. Yin T, Yin D, He H, Zheng X, Li R, Yang H, et al. The awareness and attitude of contracted service among general medical practitioners in community health service centers in urban China: a cross-sectional study. Front Public Health. (2021) 9:572311. doi: 10.3389/fpubh.2021.572311
23. Elmahdy MA, Anwer MM. Assessment of nurses' knowledge, attitude and practice regarding nutritional care management of diabetic patients in Benha University Hospital. Egypt J Hosp Med. 94:379–89. doi: 10.21608/ejhm.2024.337736
24. Gharsangi K, Himral P, Bhawani R. Knowledge, attitude and practices regarding diabetes and its complications among health care workers in medical college of North India. Int J Collab Res Int Med Public Health. (2021) 13:1–7.
25. Alkubati SA, Albagawi B, Alharbi TA, Alharbi HF, Alrasheeday AM, Llego J, et al. Nursing internship students' knowledge regarding the care and management of people with diabetes: a multicenter cross-sectional study. Nurse Educ Today. (2023) 129:105902. doi: 10.1016/j.nedt.2023.105902
26. Wang M, Xu X, Huang Y, Shao S, Chen X, Li J, et al. Knowledge, attitudes and skills of dementia care in general practice: a cross-sectional study in primary health settings in Beijing, China. BMC Fam Pract. (2020) 21:1–9. doi: 10.1186/s12875-020-01164-3
27. Zhao X, Wang H, Li J, Yuan B. Training primary healthcare workers in China's township hospitals: a mixed methods study. BMC Fam Pract. (2020) 21:1–13. doi: 10.1186/s12875-020-01333-4
28. Zhao M, Zhang M, Ying J, Wang S, Shi Y, Li H, et al. Knowledge, attitudes, practices and information demand in relation to haze in China: a cross-sectional study. BMC Public Health. (2019) 19:1–11. doi: 10.1186/s12889-019-7772-3
29. Shao S, Zhang H, Chen X, Xu X, Zhao Y, Wang M, et al. Health education services utilization and its determinants among migrants: a cross-sectional study in urban-rural fringe areas of Beijing, China. BMC Fam Pract. (2021) 22:1–19. doi: 10.1186/s12875-021-01368-1
30. Niroomand M, Ghasemi SN, Karimi-Sari H, Kazempour-Ardebili S, Amiri P, Khosravi MH. Diabetes knowledge, attitude and practice (KAP) study among Iranian in-patients with type-2 diabetes: a cross-sectional study. Diab Metab Syndr. (2016) 10:S114–S9. doi: 10.1016/j.dsx.2015.10.006
31. Awan UA, Naeem W, Khattak AA, Mahmood T, Kamran S, Khan S, et al. An exploratory study of knowledge, attitudes, and practices toward HPV associated anal cancer among Pakistani population. Front Oncol. (2023) 13:1257401. doi: 10.3389/fonc.2023.1257401
32. Awan UA, Khattak AA, Ahmed N, Guo X, Akhtar S, Kamran S, et al. An updated systemic review and meta-analysis on human papillomavirus in breast carcinogenesis. Front Oncol. (2023) 13:1219161. doi: 10.3389/fonc.2023.1219161
33. Guttman L. A basis for analyzing test-retest reliability. Psychometrika. (1945) 10:255–82. doi: 10.1007/BF02288892
34. Hao P, Wu L, Liu Y. A survey on work status and competencies of Clinical Research Nurses in China. J Res Nurs. (2022) 27:82–98. doi: 10.1177/17449871211067963
35. Giddens J, Douglas JP, Conroy S. The revised AACN essentials: implications for nursing regulation. J Nurs Regul. (2022) 12:16–22. doi: 10.1016/S2155-8256(22)00009-6
36. Smith NR, Bally JM, Holtslander L, Peacock S, Spurr S, Hodgson-Viden H, et al. Supporting parental caregivers of children living with life-threatening or life-limiting illnesses: a Delphi study. J Special Pediatr Nurs. (2018) 23:e12226. doi: 10.1111/jspn.12226
37. Lebel S, Mutsaers B, Tomei C, Leclair CS, Jones G, Petricone-Westwood D, et al. Health anxiety and illness-related fears across diverse chronic illnesses: a systematic review on conceptualization, measurement, prevalence, course, and correlates. PLoS ONE. (2020) 15:e0234124. doi: 10.1371/journal.pone.0234124
38. Sharma V, Feldman M, Sharma R. Telehealth technologies in diabetes self-management and education. J Diabetes Sci Technol. (2024) 18:148–58. doi: 10.1177/19322968221093078
39. Sugandh F, Chandio M, Raveena F, Kumar L, Karishma F, Khuwaja S, et al. Advances in the management of diabetes mellitus: a focus on personalized medicine. Cureus. (2023) 15:43697. doi: 10.7759/cureus.43697
40. Dunstan DW, Daly RM, Owen N, Jolley D, Vulikh E, Shaw J, et al. Home-based resistance training is not sufficient to maintain improved glycemic control following supervised training in older individuals with type 2 diabetes. Diabetes Care. (2005) 28:3–9. doi: 10.2337/diacare.28.1.3
41. Hjelm K, Mufunda E, Nambozi G, Kemp J. Preparing nurses to face the pandemic of diabetes mellitus: a literature review. J Adv Nurs. (2003) 41:424–34. doi: 10.1046/j.1365-2648.2003.02548.x
42. Hausken M, Graue M. Developing, implementing and evaluating diabetes care training for nurses and nursing aides in nursing homes and municipal home-based services. Eur Diab Nurs. (2013) 10:19–24b. doi: 10.1002/edn.219
43. Rubin DJ, Moshang J, Jabbour SA. Diabetes knowledge: are resident physicians and nurses adequately prepared to manage diabetes? Endocr Pract. (2007) 13:17–21. doi: 10.4158/EP.13.1.17
44. AbuRuz ME, Hayeah HA, Al-Dweik G, Al-Akash HY. Knowledge, attitudes, and practice about evidence-based practice: a Jordanian study. Health Sci J. (2017) 11:1. doi: 10.21767/1791-809X.1000489
45. Ma'moun AS, Abu-Moghli FA. Perceived knowledge, attitudes, and implementation of evidence-based practice among Jordanian nurses in critical care units. Dimens Crit Care Nurs. (2020) 39:278–86. doi: 10.1097/DCC.0000000000000431
46. White-Williams C, Patrician P, Fazeli P, Degges MA, Graham S, Andison M, et al. Use, knowledge, and attitudes toward evidence-based practice among nursing staff. J Contin Educ Nurs. (2013) 44:246–54. doi: 10.3928/00220124-20130402-38
47. Zhou F, Hao Y, Guo H, Liu H. Attitude, knowledge, and practice on evidence-based nursing among registered nurses in traditional Chinese medicine hospitals: a multiple center cross-sectional survey in China. Evid Based Comp Altern Med. (2016) 2016:5478086. doi: 10.1155/2016/5478086
48. Berkowski JA, Shelgikar AV. Disorders of excessive daytime sleepiness including narcolepsy and idiopathic hypersomnia. Sleep Med Clin. (2016) 11:365–78. doi: 10.1016/j.jsmc.2016.04.005
49. Smagula SF, Biggs ML, Jacob ME, Rawlings AM, Odden MC, Arnold A, et al. Associations of modifiable behavioral risk factor combinations at 65 to 74 years old with cognitive health span for 20 years. Psychosom Med. (2022) 84:785–92. doi: 10.1097/PSY.0000000000001100
50. Alotaibi A, Gholizadeh L, Al-Ganmi AHA, Perry L. Factors influencing nurses' knowledge acquisition of diabetes care and its management: a qualitative study. J Clin Nurs. (2018) 27:4340–52. doi: 10.1111/jocn.14544
51. Hollis M, Glaister K, Anne Lapsley J. Do practice nurses have the knowledge to provide diabetes self-management education? Contemp Nurse. (2014) 46:234–41. doi: 10.5172/conu.2014.46.2.234
52. Albisser AM, Harris RI, Albisser JB, Sperlich M. The impact of initiatives in education, self-management training, and computer-assisted self-care on outcomes in diabetes disease management. Diabetes Technol Ther. (2001) 3:571–9. doi: 10.1089/15209150152811199
53. Hill-Briggs F, Lazo M, Peyrot M, Doswell A, Chang Y-T, Hill MN, et al. Effect of problem-solving-based diabetes self-management training on diabetes control in a low income patient sample. J Gen Intern Med. (2011) 26:972–8. doi: 10.1007/s11606-011-1689-6
54. Polonsky WH, Earles J, Smith S, Pease DJ, Macmillan M, Christensen R, et al. Integrating medical management with diabetes self-management training: a randomized control trial of the Diabetes Outpatient Intensive Treatment program. Diab Care. (2003) 26:3048–53. doi: 10.2337/diacare.26.11.3048
55. Bhojani U, Devedasan N, Mishra A, De Henauw S, Kolsteren P, Criel B. Health system challenges in organizing quality diabetes care for urban poor in South India. PLoS ONE. (2014) 9:e106522. doi: 10.1371/journal.pone.0106522
56. Seuring T, Archangelidi O, Suhrcke M. The economic costs of type 2 diabetes: a global systematic review. Pharmacoeconomics. (2015) 33:811–31. doi: 10.1007/s40273-015-0268-9
57. Bekele H, Asefa A, Getachew B, Belete AM. Barriers and strategies to lifestyle and dietary pattern interventions for prevention and management of type-2 diabetes in Africa, systematic review. J Diab Res. (2020) 2020:7948712. doi: 10.1155/2020/7948712
58. Hall V, Thomsen RW, Henriksen O, Lohse N. Diabetes in Sub Saharan Africa 1999-2011: epidemiology and public health implications. A systematic review. BMC Public Health. (2011) 11:1–12. doi: 10.1186/1471-2458-11-564
59. Cheng LJ, Wang W, Lim ST, Wu VX. Factors associated with glycaemic control in patients with diabetes mellitus: a systematic literature review. J Clin Nurs. (2019) 28:1433–50. doi: 10.1111/jocn.14795
60. Bosun-Arije FS, Ling J, Graham Y, Hayes C. A systematic review of factors influencing Type 2 Diabetes Mellitus management in Nigerian public hospitals. Int J Afr Nurs Sci. (2019) 11:100151. doi: 10.1016/j.ijans.2019.100151
62. American Diabetes Association. Economic costs of diabetes in the US in 2012. Diabetes Care. (2013) 36:1033–46. doi: 10.2337/dc12-2625
63. Baxter S, Johnson M, Chambers D, Sutton A, Goyder E, Booth A. The effects of integrated care: a systematic review of UK and international evidence. BMC Health Serv Res. (2018) 18:1–13. doi: 10.1186/s12913-018-3161-3
64. Saqib MA, Siddiqui S, Qasim M, Jamil MA, Rafique I, Awan UA, et al. Effect of COVID-19 lockdown on patients with chronic diseases. Diabetes Metab Syndrome Clin Res Rev. (2020) 14:1621–3. doi: 10.1016/j.dsx.2020.08.028
65. Fang M. Trends in diabetes management among US adults: 1999–2016. J Gen Intern Med. (2020) 35:1427–34. doi: 10.1007/s11606-019-05587-2
66. Gorina M, Limonero JT, Alvarez M. Effectiveness of primary healthcare educational interventions undertaken by nurses to improve chronic disease management in patients with diabetes mellitus, hypertension and hypercholesterolemia: a systematic review. Int J Nurs Stud. (2018) 86:139–50. doi: 10.1016/j.ijnurstu.2018.06.016
Keywords: nurses, healthcare workers, KAP, diabetes mellitus, diabetes management
Citation: Hu L and Jiang W (2024) Assessing perceptions of nursing knowledge, attitudes, and practices in diabetes management within Chinese healthcare settings. Front. Public Health 12:1426339. doi: 10.3389/fpubh.2024.1426339
Received: 01 May 2024; Accepted: 22 July 2024;
Published: 12 August 2024.
Edited by:
Olga Ribeiro, Escola Superior de Enfermagem do Porto, PortugalReviewed by:
Maria Rui Sousa, Escola Superior de Enfermagem do Porto, PortugalStella Bosun-Arije, Manchester Metropolitan University, United Kingdom
Copyright © 2024 Hu and Jiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wen Jiang, anc4MDYwMjg0NzEmI3gwMDA0MDsxNjMuY29t
 Lan Hu
Lan Hu Wen Jiang
Wen Jiang