- 1Department of Endocrinology, Heilongjiang Provincial Hospital, Harbin, China
- 2The First Clinical College of Medicine, Mudanjiang Medical University, Mudanjiang, China
Background: This study aimed to assess the knowledge, attitudes and practices (KAP) among patients with diabetes mellitus and hyperuricemia toward disease self-management.
Methods: This web-based cross-sectional study was conducted between June 2023 and January 2024 at Heilongjiang Provincial Hospital. A self-designed questionnaire was developed to collect demographic information of patients with diabetes mellitus and hyperuricemia, and assess their knowledge, attitudes and practices toward disease self-management.
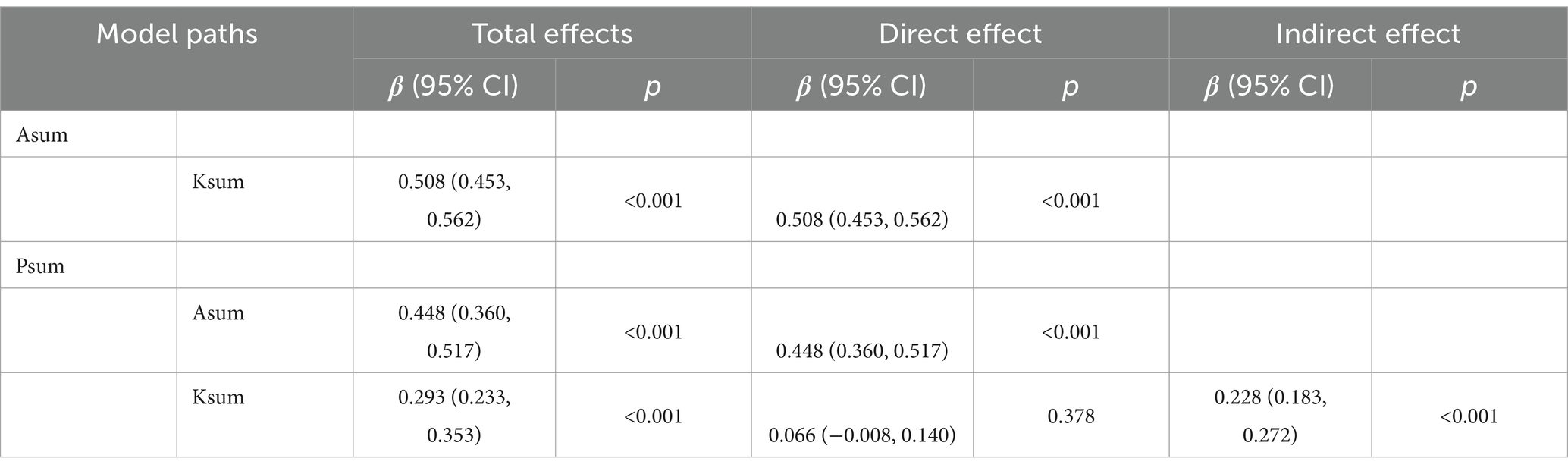
Results: A total of 482 participants were enrolled in this study, among them, 364 (75.52%) were male, 235 (48.76%) were aged between 40 and 59 years, 226 (46.89%) had a body mass index (BMI) ranging from 24 to 28 kg/m2, 337 (69.92%) had received a diagnosis of diabetes for a duration of 2 years or more, while 245 (50.83%) had been diagnosed with hyperuricemia for a similar duration. Their median (range) knowledge, attitude and practice scores were 10.00 (9.00, 11.00) (possible range: 0–12), 38.00 (36.00, 40.00) (possible range: 9–45), and 30.00 (26.00, 34.75) (possible range: 10–50), respectively. The path analysis demonstrated that knowledge had direct effects on attitude (β = 0.508, p < 0.001), and attitude had direct effects on practice (β = 0.448, p < 0.001). Additionally, there was an indirect effect of knowledge on practice mediated through attitude, with a path coefficient of 0.228 (p < 0.001).
Conclusion: This study demonstrates that patients with diabetes mellitus and hyperuricemia exhibit relatively proficient responses to certain items within the KAP dimensions. However, it also exposes a certain degree of inadequacy in the KAP level toward disease management. Interventions should focus on improving patients’ understanding of their conditions while fostering positive attitudes, ultimately translating into better self-management practices.
Introduction
The increasing prevalence of metabolic diseases, such as diabetes mellitus and hyperuricemia, has become a significant public health issue worldwide, underscoring the importance of addressing these conditions to improve global health outcomes (1). Hyperuricemia, characterized by elevated serum uric acid levels, is closely linked with metabolic disorders, including type 2 diabetes and metabolic syndrome, highlighting a complex interrelationship that contributes to the burden of metabolic diseases (2). Moreover, approximately 25% of individuals with diabetes are affected by hyperuricemia, indicating a substantial overlap between these conditions and emphasizing the need for integrated management strategies (3).
Management of diabetes mellitus and hyperuricemia requires a comprehensive approach, emphasizing the role of self-management in controlling these conditions. Dietary factors, such as the intake of alcohol, red meat, and seafood, are established risk factors for hyperuricemia and gout flares, suggesting that dietary modifications can significantly reduce the risk of these complications (4). Additionally, physical activity, weight loss, and a healthy diet are crucial for preventing diabetes and its complications, underscoring the importance of lifestyle interventions in managing these metabolic diseases and improving patient outcomes (5). Effective self-management strategies, including lifestyle and dietary modifications, are essential for mitigating the impact of these conditions and enhancing the quality of life for affected individuals.
The Knowledge-Attitude-Practice (KAP) model plays a crucial role in understanding and influencing health behaviors, serving as a fundamental framework within health literacy research. This model posits that knowledge positively affects attitudes, which in turn, guide individual practices (6). Employing the KAP theory is particularly relevant for populations dealing with complex, interrelated health issues such as diabetes mellitus and hyperuricemia. Despite the existence of KAP studies on diabetes and hyperuricemia conducted separately, there is a deficiency in research investigating the KAP pertaining to self-management among patients with both conditions (7–9). This gap highlights the need to assess the KAP among patients with diabetes mellitus and hyperuricemia toward disease self-management.
Materials and methods
Study design and participants
This cross-sectional study was conducted between June 2023 and January 2024 at Heilongjiang Provincial Hospital. The study was ethically approved by the Ethics Committee of Heilongjiang Provincial Hospital (Approval No. (2023)075). This study used convenience sampling to recruit the patients with diabetes mellitus and hyperuricemia and the inclusion criteria and exclusion criteria were as follows:
The inclusion criteria for this study were as follows: (1) aged 18 years and older, (2) diagnosed with both diabetes mellitus and hyperuricemia, supported by relevant diagnostic reports or medical records, (3) confirmation of informed consent on the first page of the questionnaire.
The exclusion criteria were as follows: (1) those who self-reported their participation in a similar study, and (2) those who did not pass the validation of the trap questions (K7 & K14, refer to the Questionnaire section).
Questionnaire
The questionnaire was developed in accordance with China multi-disciplinary expert consensus on diagnosis and treatment of hyperuricemia and related diseases (10), Comprehensive Medical Evaluation and Assessment of Comorbidities: Standards of Care in Diabetes-2023 (11) and relevant literature on disease management (12–14). The initial draft underwent refinement based on feedback from three senior experts, comprising two endocrinologists and one rheumatologist. Following this, a pilot study was conducted on a limited scale (n = 24), resulting in a Cronbach’s alpha coefficient value of 0.788, indicating good internal consistency.
The final questionnaire was in Chinese and encompassed four dimensions: demographic information, knowledge, attitudes, and practices. The demographic section consisted of 15 items, while the knowledge, attitude, and practice dimensions included 14, 9, and 10 items, respectively.
Certain questions were designed as “trap questions” to maintain the questionnaire’s quality within the study: Question 11 in the demographic section, Questions K7 and K14 in the knowledge dimension. For instance, selecting option “e” alongside any other option for Question 11 led to the exclusion of the corresponding questionnaire from analysis. Likewise, responses to K7 and K14, which conveyed contrasting meanings, were scrutinized. Patients who selected both “correct” and “incorrect” for these questions were recognized as encountering logical conflicts and thus, were omitted from the survey. Consequently, knowledge items were scored 1 point for correct answers and 0 points for incorrect ones, yielding a possible score range of 0–12. Attitude and practice items were rated on a five-point Likert scale, ranging from very positive (5 points) to very negative (1 point) for attitude, and very consistent (5 points) to very inconsistent (1 point) for practice, with respective score ranges of 9–45 and 10–50.
The sample size calculation was based on the guideline that it should be 5 to 10 times the number of items (15). With 28 items in the KAP questionnaire, the required sample size was calculated to be at least 280 participants. Accounting for an anticipated 20% of invalid responses, the adjusted minimum required sample size was 336 participants. This ensures that the study has sufficient statistical power and reliability for analysis.
Data collection was facilitated through an online questionnaire hosted on Sojump.1 Participants were prompted to begin the electronic questionnaire by selecting the option “I agree to participate in this study” prior to responding to the questions. All data collection procedures were conducted anonymously. To prevent duplicate submissions, IP restrictions were enforced, restricting completion of the survey to a single instance per IP address.
Statistical analysis
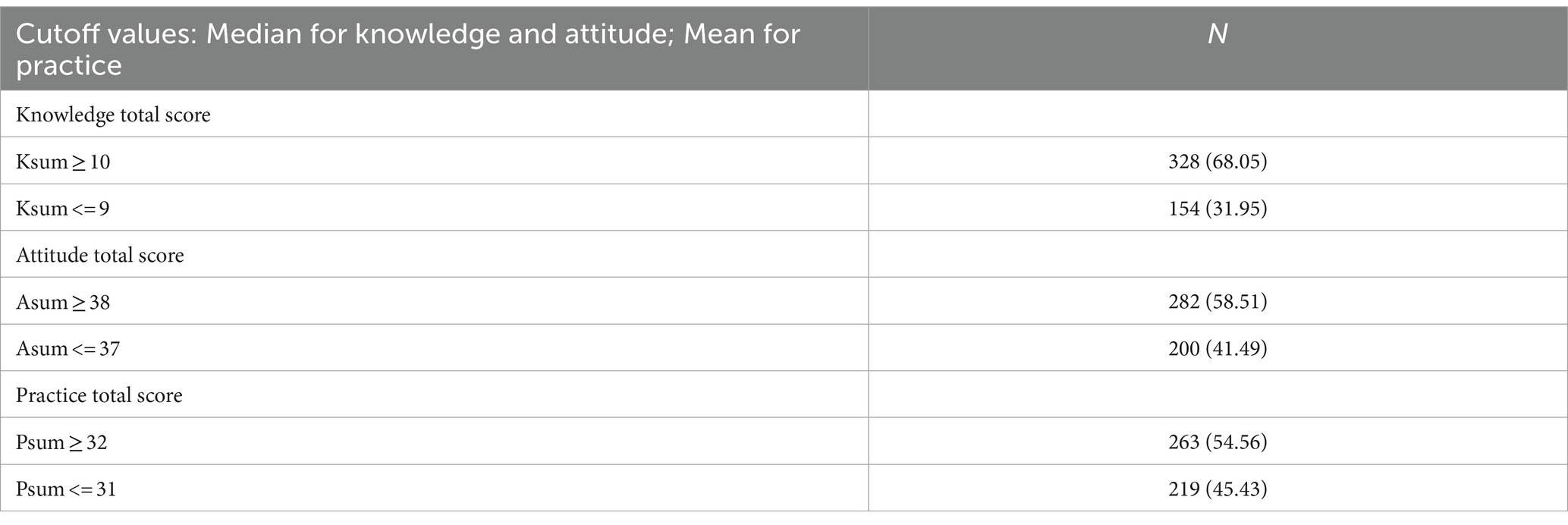
Statistical analyses were conducted using STATA 17.0 (Stata Corporation, College Station, TX, USA). Continuous variables were described as medians (25th percentile, 75th percentile) or means (SD) depending on the normality of the data, which was assessed using the Shapiro–Wilk test. Between-group comparisons were performed using the Wilcoxon rank-sum test or the Kruskal-Wallis analysis of variance, as appropriate. Categorical variables were presented as N (%). Spearman correlation analysis was employed to assess the relationships between knowledge, attitude, and practice scores. In the multivariate analysis, the median score (for non-normally distributed scores, such as knowledge and attitude scores) or the mean score (for normally distributed scores, such as practice scores) was used as the cut-off value. Thresholds for knowledge, attitudes, and practices were set at 10, 38, and 30 points, respectively. Variables with p < 0.05 in univariate analysis were included in the multivariate regression. Path analysis of the relationships among knowledge, attitudes, and practices in patients with diabetes mellitus and hyperuricemia regarding disease management was conducted using AMOS 24.0 (IBM, NY, USA). The path analysis tested the following primary hypotheses: (1) Knowledge has direct effects on attitudes; (2) Knowledge has direct effects on practices; and (3) Attitudes have direct effects on practices. A two-sided p-value <0.05 was considered statistically significant in this study.
Results
Initially, 531 questionnaires were collected. Of these, 49 questionnaires were excluded due to incorrect answers to the trap questions. Consequently, a total of 482 questionnaires were ultimately included in the study. The overall validity rate of the questionnaires was 90.77%.
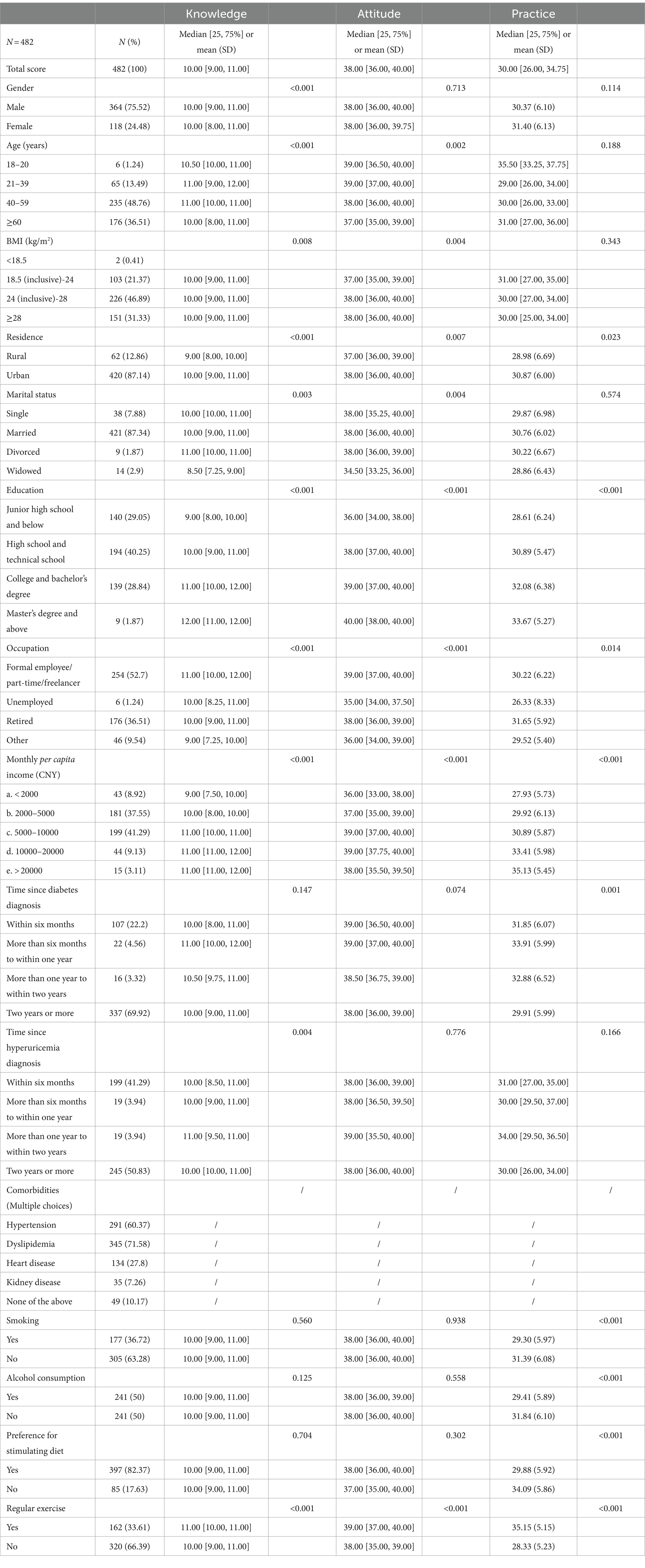
A total of 482 participants were included in this study. Among them, 364 (75.52%) were male, 235 (48.76%) were aged between 40 and 59 years, 226 (46.89%) had a body mass index (BMI) ranging from 24 to 28 kg/m2, and 194 (40.25%) had attained education up to high school or technical school level. Moreover, 337 (69.92%) had received a diagnosis of diabetes for a duration of 2 years or more, while 245 (50.83%) had been diagnosed with hyperuricemia for a similar duration. Furthermore, 177 (36.72%) were smokers, 241 (50%) were consumers of alcohol, and 397 (82.37%) exhibited a preference for diets rich in heavy oils, salt, or other stimulating ingredients. Additionally, 320 (66.39%) did not engage in regular exercise (Table 1).
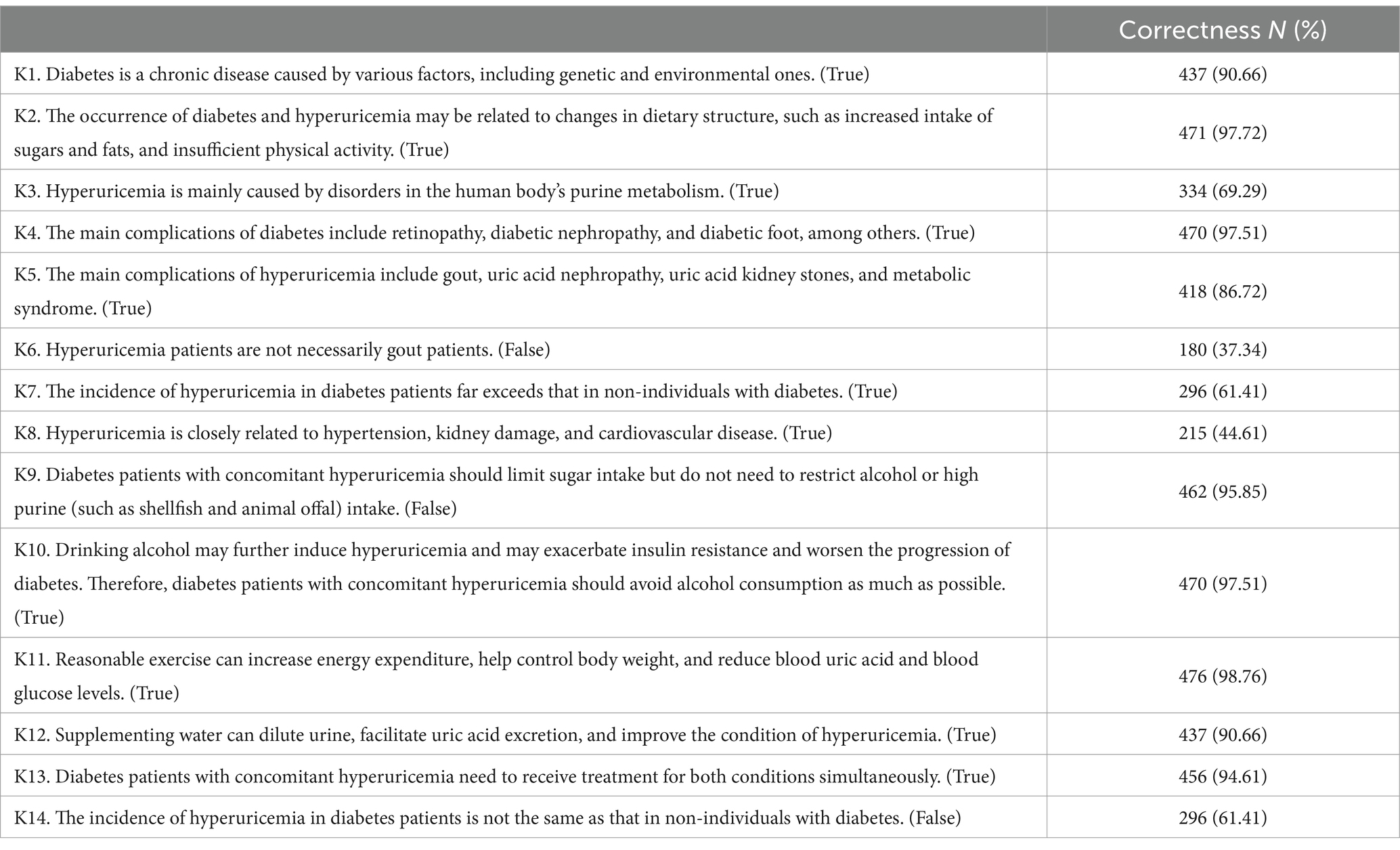
The three knowledge items with the highest correctness rates were as follows: “Reasonable exercise can increase energy expenditure, help control body weight, and reduce blood uric acid and blood glucose levels.” (K11) with a correctness rate of 98.76%, “The occurrence of diabetes and hyperuricemia may be related to changes in dietary structure, such as increased intake of sugars and fats, and insufficient physical activity.” (K2) with a correctness rate of 97.72%, “The main complications of diabetes include retinopathy, diabetic nephropathy, and diabetic foot, among others.” (K4) with a correctness rate of 97.51%. The three items with the lowest correctness rates were as follows: “Hyperuricemia patients are not necessarily gout patients.” (K6) with a correctness rate of 37.34%, “Hyperuricemia is closely related to hypertension, kidney damage, and cardiovascular disease.” (K8) with a correctness rate of 44.61%, “The incidence of hyperuricemia in diabetes patients far exceeds that in non-individuals with diabetes.” (K7) with a correctness rate of 61.41% (Table 2).
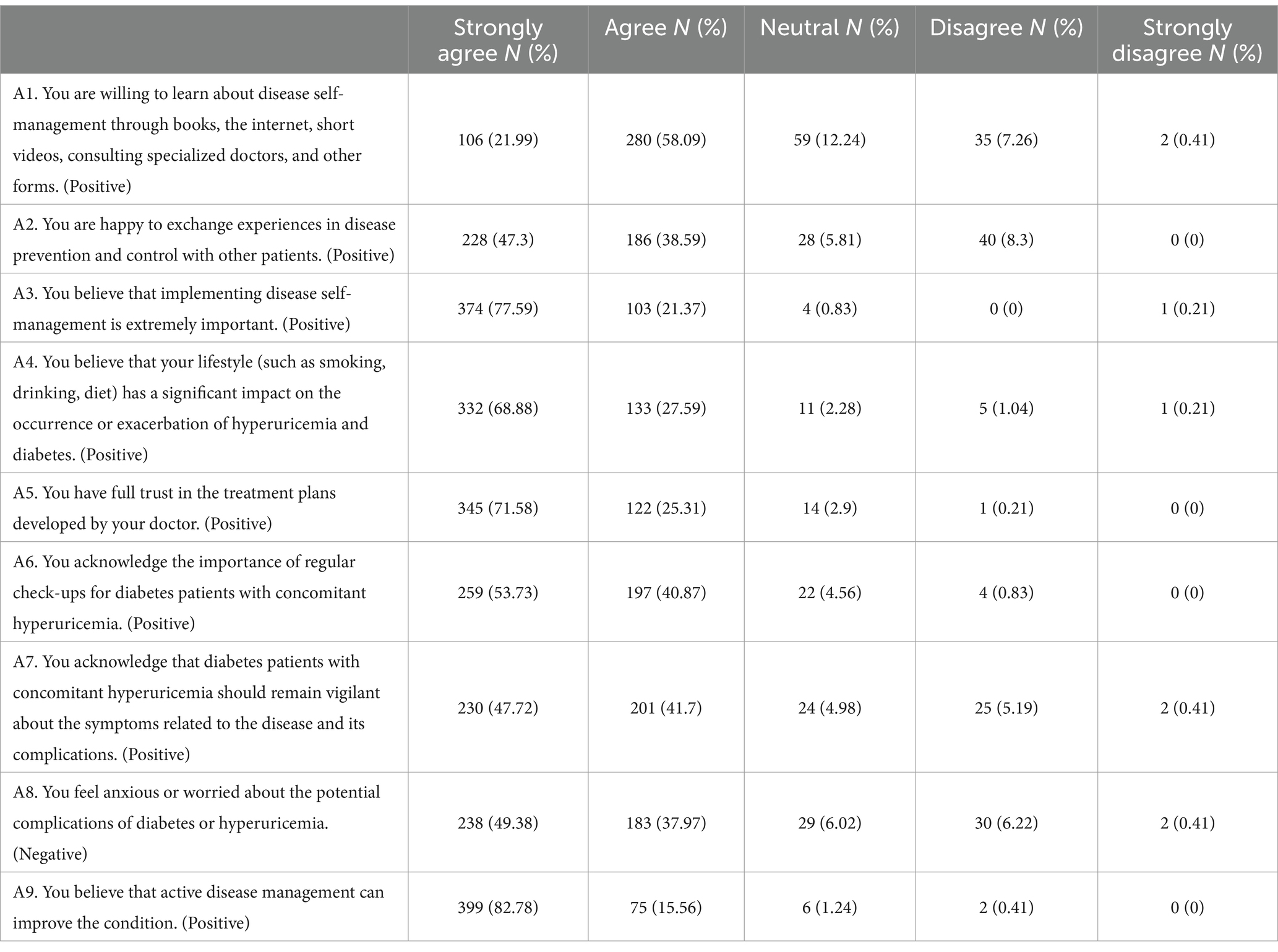
Among the participants, 82.78% strongly agreed that their condition could be improved through active disease management (A9), 77.59% strongly agreed that it was very important to implement disease self-management (A3), and 71.58% had very full trust in the treatment plan that the doctor had developed for them (A5). Concurrently, 58.09% were willing to learn about disease self-management through various forms (A1). However, nearly half of the participants (49.38%) reported experiencing anxiety or concern regarding potential complications linked to diabetes or hyperuricemia. These emotional states possess the potential to influence their quality of life and adherence to treatment protocols (A8) (Table 3).
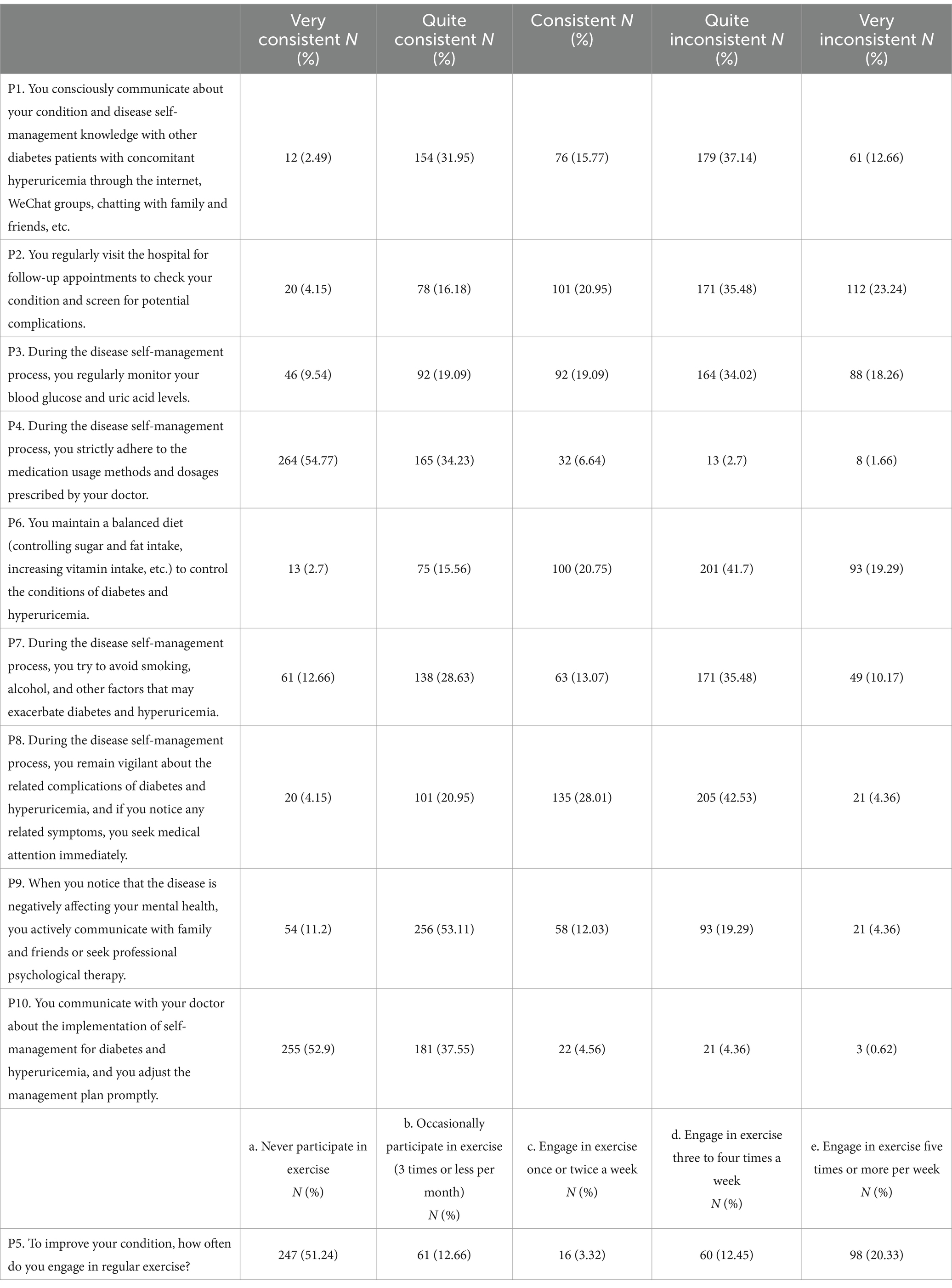
Patients’ activity or frequency of performing these practices items varied greatly, with 54.77% strictly adhering to the prescribed medication and dosage for disease self-management (P4), and 52.9% communicating closely with their physicians to make timely adjustments to their self-management plan (P10). Strikingly, 51.24% never participated in exercise to improve their condition (P5). Intriguingly, 31.95% often consciously communicate with other patients about their condition and disease self-management in various ways in their lives (P1), while a similar proportion (37.14%) rarely do so (Table 4).
Spearman’s analysis was performed to assess the relationship between knowledge, attitudes, and practices. It was shown that the knowledge and the attitudes were positively correlated (r = 0.330, p < 0.001), and knowledge and practices were also positively correlated (r = 0.266, p < 0.001). Additionally, there was a positive correlation between attitude and practice scores (r = 0.345, p < 0.001) (Table 5).
Using the median or means scores for each dimension as a cut-off value, the proportions of participants who scored above the cut-off value for knowledge, attitude and practice was 328 (68.05%), 282 (58.51%), and 263 (54.56%) (Table 6).
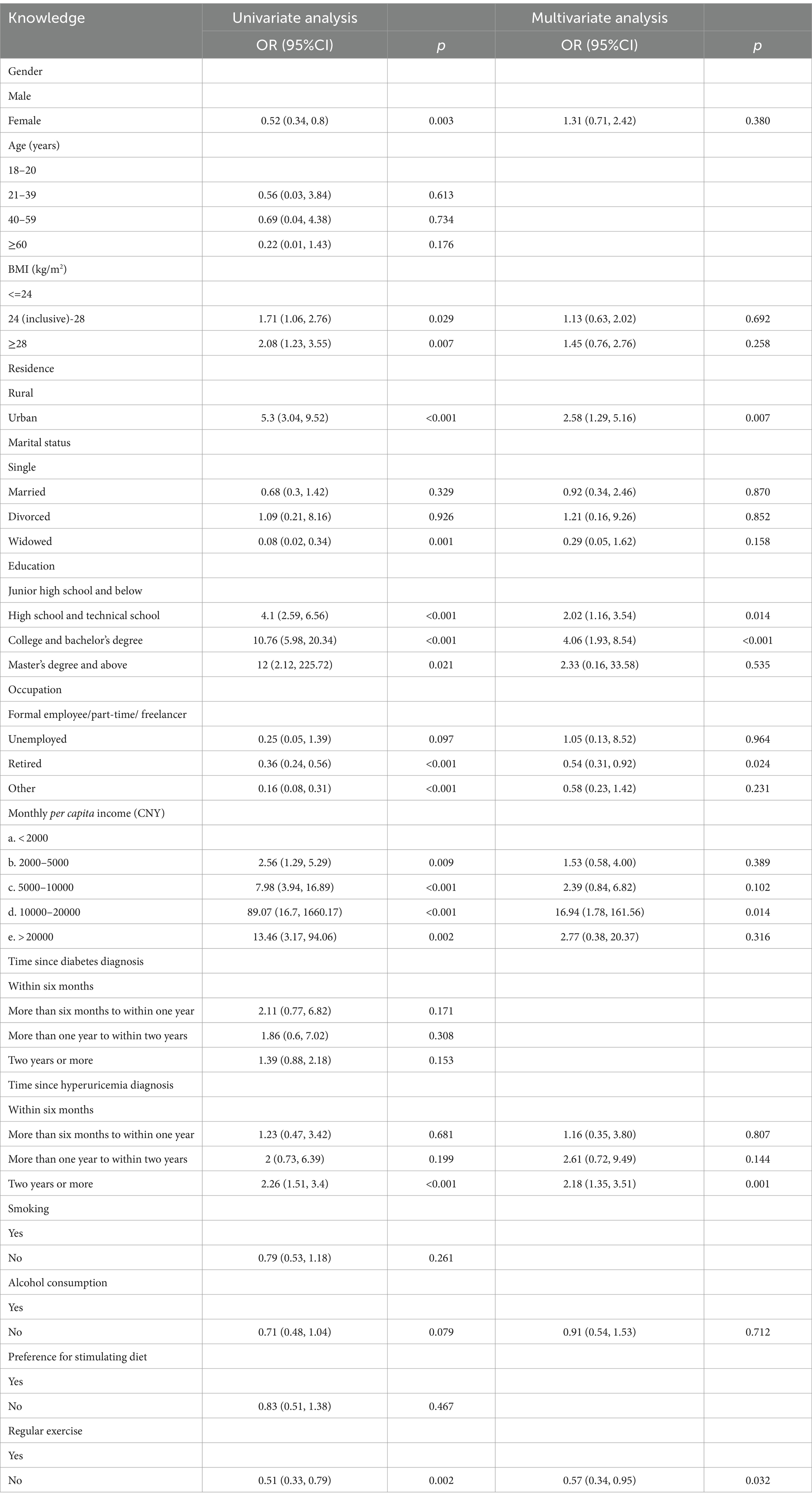
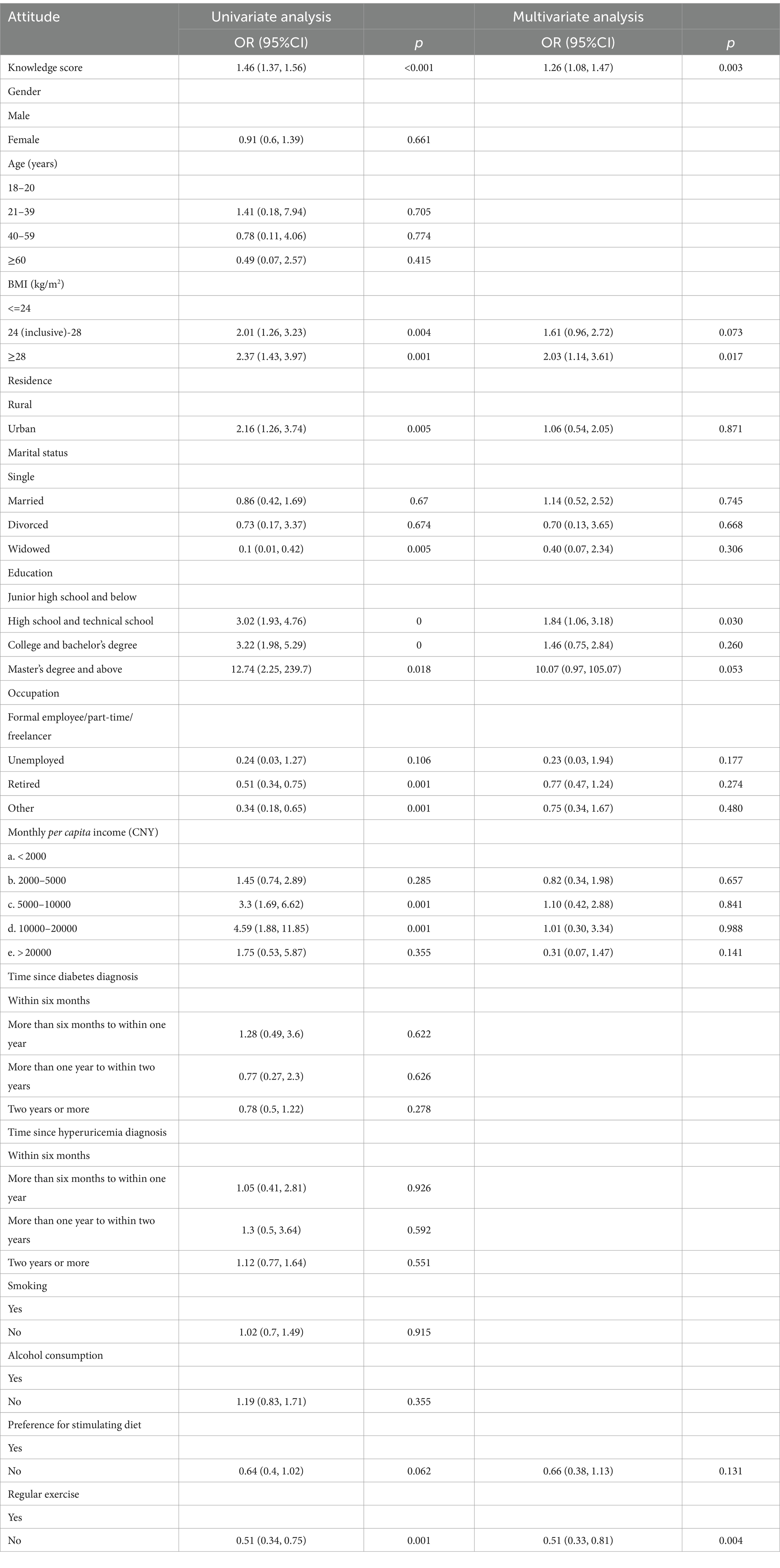
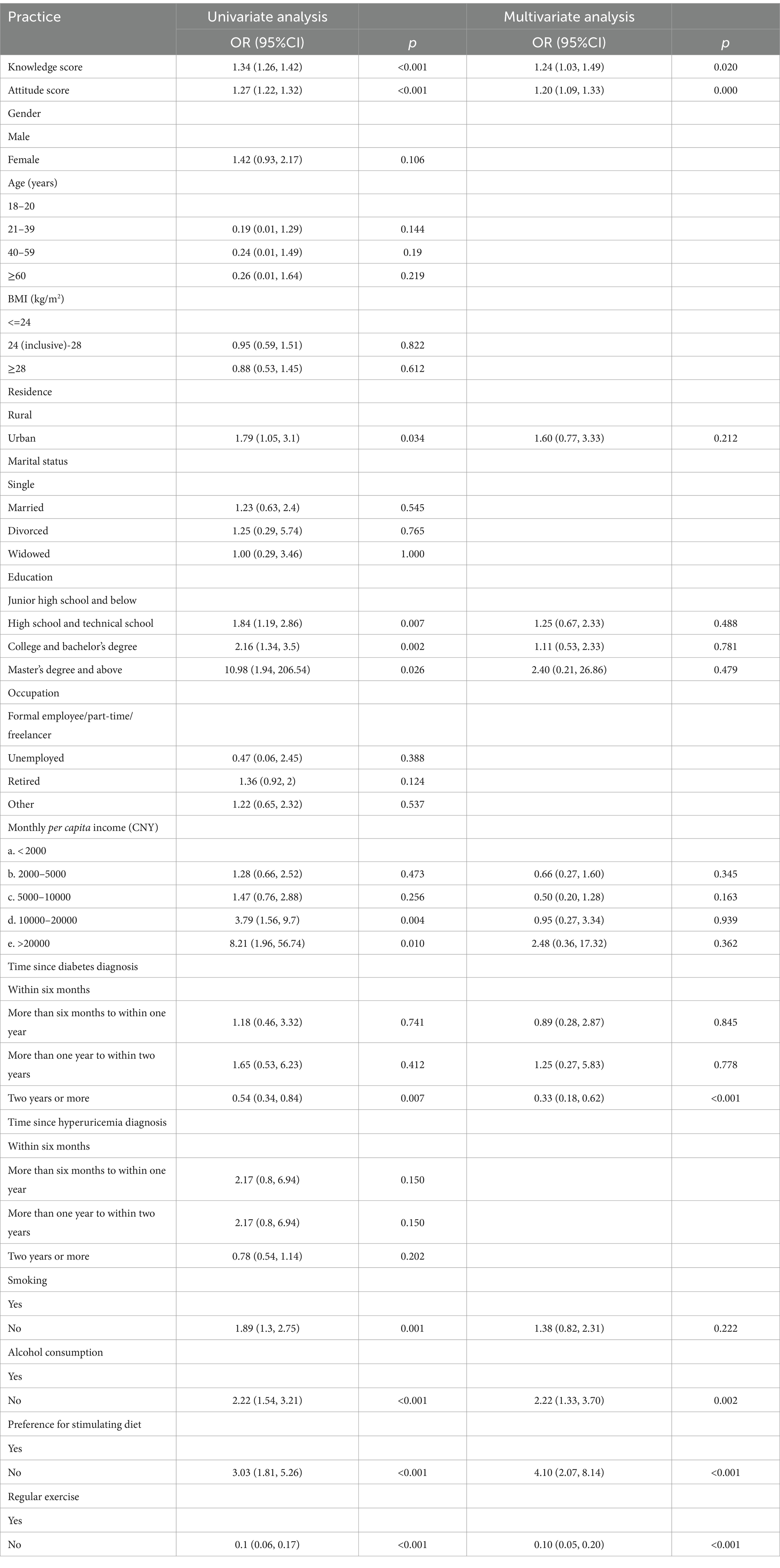
Multivariate analysis revealed that living in urban areas (OR = 2.58, 95% CI: 1.81–3.68, p = 0.007), having a high school or technical school education (OR = 2.02, 95% CI: 1.52–2.69, p = 0.014), holding a college or bachelor’s degree (OR = 4.06, 95% CI: 2.78–5.93, p < 0.001), being retired (OR = 0.54, 95% CI: 0.41–0.71, p = 0.024), having a monthly per capita income of 10000–20000 Yuan (OR = 16.94, 95% CI: 5.36–53.53, p = 0.014), being diagnosed with hyperuricemia for 2 years or more (OR = 2.18, 95% CI: 1.7–2.78, p = 0.001), and not having regular exercise habits (OR = 0.57, 95% CI: 0.44–0.74, p = 0.032) were independently associated with knowledge (Table 7). Additionally, knowledge score (OR = 1.26, 95% CI: 1.17–1.36, p = 0.003), having a BMI not less than 28 kg/m2 (OR = 2.03, 95% CI: 1.51–2.72, p = 0.017), high school or technical school education (OR = 1.84, 95% CI: 1.39–2.43, p = 0.030), and not having regular exercise habits (OR = 0.51, 95% CI: 0.41–0.65, p = 0.004) were independently associated with attitude (Table 8). Furthermore, knowledge score (OR = 1.24, 95% CI: 1.13–1.36, p = 0.020), attitude score (OR = 1.20, 95% CI: 1.14–1.26, p = 0.000), being diagnosed with diabetes for 2 years or more (OR = 0.33, 95% CI: 0.24–0.44, p < 0.001), not drinking alcohol (OR = 2.22, 95% CI: 1.71–2.9, p = 0.002), having no preference for heavy oils, salty, or other stimulating foods (OR = 4.1, 95% CI: 2.89–5.82, p < 0.001), and not having regular exercise habits (OR = 0.1, 95% CI: 0.07–0.13, p < 0.001) were independently associated with practice (Table 9).
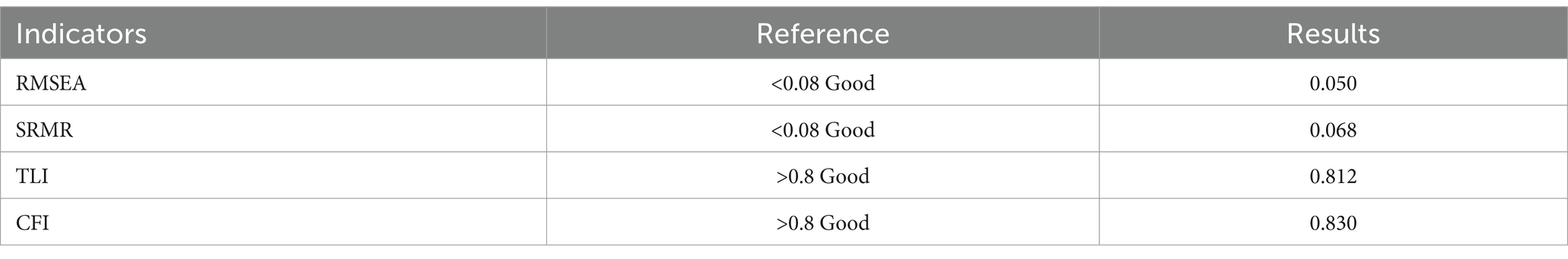
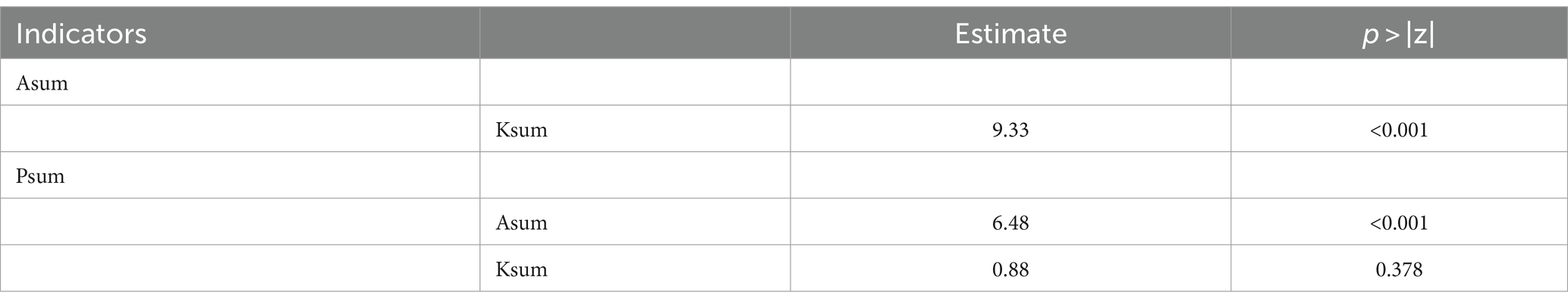
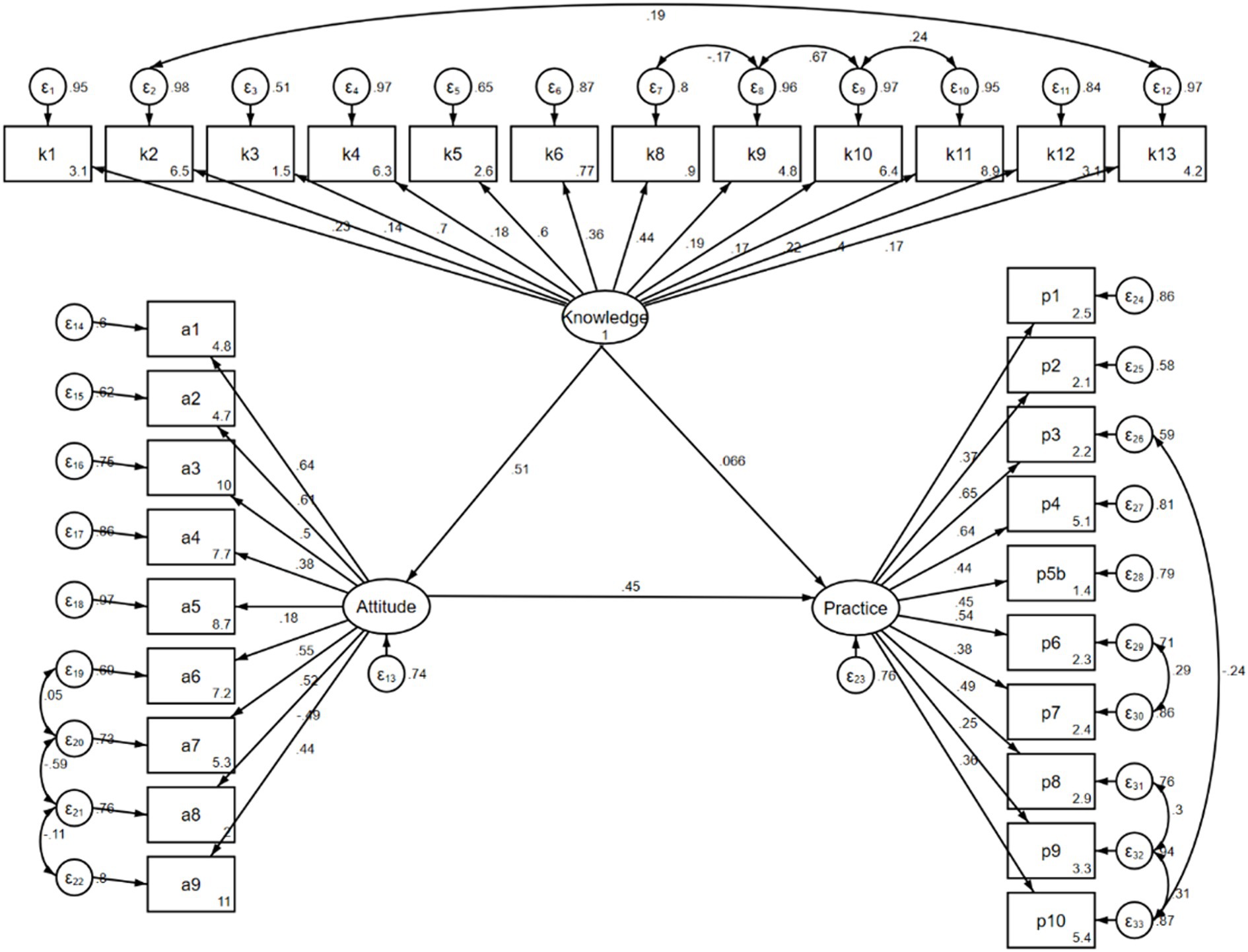
The path analysis was established to further investigate whether patients’ knowledge and attitude toward disease self-management affect their practice, whether attitude plays an intermediary role between knowledge and practice, and whether knowledge can directly affect their practice according to the KAP theory. Model fitness indices showed a good model fit (Table 10) and the results demonstrated that knowledge had direct effects on attitude (β = 0.508, p < 0.001), and attitude had direct effects on practice (β = 0.448, p < 0.001). Additionally, there was an indirect effect of knowledge on practice mediated through attitude, with a path coefficient of 0.228 (p < 0.001) (Tables 11, 12 and Figure 1).
Discussion
This study demonstrates that patients with diabetes mellitus and hyperuricemia exhibit relatively proficient responses to certain items within the KAP dimensions. However, it also exposes a certain degree of inadequacy in the KAP level toward disease management. Interventions should focus on improving patients’ understanding of their conditions while fostering positive attitudes, ultimately translating into better self-management practices.
The findings from the study revealed important insights into the KAP of patients with diabetes mellitus and hyperuricemia toward disease self-management. Overall, the results indicate that while patients generally possess positive attitudes, their knowledge levels are inadequate, and their practices are suboptimal. Previous research has identified medication management and the conflict between disease and daily life as the primary needs among the people with diabetes in China (16). Given the positive attitudes observed in this study, addressing these needs may contribute to an improvement in knowledge levels and ultimately enhance clinical outcomes for individuals with diabetes with complications.
Several demographic, lifestyle, and health-related characteristics were found to significantly influence KAP scores. For instance, education level, as evidenced by both inter-group comparisons and multivariate analysis, emerges as a significant determinant. In inter-group comparisons, individuals with higher education levels consistently scored higher across domains of health knowledge, attitudes, and practices. This finding aligns with prior research emphasizing the positive impact of education on health literacy and behaviors (17, 18). Moreover, multivariate analysis corroborates the significance of education level as an independent predictor of health knowledge, attitudes, and practices. Another notable factor is the residential area. In inter-group comparisons, urban residents demonstrated higher scores across all domains compared to their rural counterparts, reflecting potential disparities in health literacy and behaviors between urban and rural populations. Multivariate analysis identified residential area as an independent predictor of knowledge scores, indicating its continued relevance even when considering other factors. This may reflect differences in access to health information, lifestyle factors, and healthcare resources between urban and rural settings (19–21). Thus, targeted community education and health promotion initiatives may be instrumental in bridging the urban–rural health gap and improving health knowledge among rural residents.
Moreover, Spearman’s analysis revealed significant positive correlations between knowledge, attitudes, and practices, suggesting that enhancing knowledge may positively influence attitudes and subsequently lead to improved practices. The path analysis further supported these findings, demonstrating direct and indirect effects of knowledge and attitude on practices. These results are consistent with the KAP theory, which posits that enhancing knowledge and fostering positive attitudes are crucial steps toward behavior change (22, 23).
The assessment of participants’ knowledge toward diabetes and hyperuricemia unveiled both strengths and areas for improvement. While participants demonstrated a solid grasp of the relationship between lifestyle factors and disease onset, particularly acknowledging the impact of dietary habits and physical activity, there were notable misconceptions toward the association between hyperuricemia and gout. To address this, healthcare providers could implement targeted educational workshops or seminars focusing on clarifying common misconceptions about hyperuricemia and its potential complications. Additionally, integrating visual aids, such as infographics or educational videos, into patient education materials can enhance understanding and retention of key concepts. By empowering patients with accurate knowledge, healthcare providers can equip them with the necessary tools to make informed decisions about their health and engage effectively in disease self-management practices (24, 25).
Participants exhibited generally positive attitudes toward disease self-management, demonstrating a willingness to engage in proactive health behaviors. However, there was a concerning lack of awareness or denial toward the potential complications of diabetes and hyperuricemia. To address this, healthcare providers could implement targeted psychoeducational interventions aimed at raising awareness about potential complications and providing strategies for coping with anxiety or worry related to disease management (26). Peer support groups or counseling sessions facilitated by trained healthcare professionals can provide opportunities for patients to share experiences, receive support, and learn effective coping strategies. Additionally, incorporating regular discussions about potential complications and coping mechanisms into routine clinic visits can help normalize these conversations and encourage proactive engagement in disease self-management practices.
Analysis of participants’ practices revealed varying levels of consistency in disease management behaviors. While there was a strong adherence to prescribed medication regimens, challenges were observed in maintaining regular exercise habits. Regular physical activity plays a crucial role in disease management and prevention, highlighting the need for tailored interventions to promote exercise adherence. Additionally, participants demonstrated varying degrees of engagement in disease self-management activities such as monitoring blood glucose and uric acid levels and seeking medical attention promptly when necessary. To address this, healthcare providers could work collaboratively with patients to develop personalized exercise plans tailored to their preferences, abilities, and lifestyle constraints. Incorporating enjoyable and accessible physical activities, such as walking groups or chair exercises, can enhance adherence and promote long-term sustainability (27, 28). Furthermore, leveraging technology, such as smartphone apps or wearable activity trackers, can provide real-time feedback and motivation to support exercise adherence. Additionally, implementing regular follow-up appointments with healthcare providers to monitor progress, address challenges, and adjust management plans as needed can provide ongoing support and encouragement for patients to maintain consistent engagement in disease self-management practices (29, 30).
Despite the valuable insights gained from this study, several limitations must be acknowledged. Firstly, the reliance on a web-based survey may introduce selection bias, as it excludes individuals without internet access or those who are less technologically savvy. Additionally, the cross-sectional design of the study limits the ability to establish causality between variables and only provides a snapshot of participants’ KAP at a single point in time. Moreover, the study’s reliance on self-reported data introduces the possibility of recall bias and social desirability bias, potentially affecting the accuracy of responses toward participants’ knowledge, attitudes, and practices toward disease self-management.
Conclusion
In conclusion, patients with diabetes mellitus and hyperuricemia exhibit insufficient knowledge, active attitudes, and poor practices toward disease management. Healthcare providers should prioritize educational interventions targeting these patients, emphasizing the importance of comprehensive disease self-management strategies to improve outcomes.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The study was carried out after the protocol was approved by the Institutional Review Board of Heilongjiang Provincial Hospital (2023(75)). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
DW: Writing – original draft, Conceptualization. ZL: Investigation, Writing – original draft. YL: Writing – review & editing. LZ: Investigation, Writing – original draft. LX: Project administration, Writing – original draft. SH: Investigation, Writing – original draft. BD: Supervision, Writing – original draft.
Funding
The author(s) declare no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
1. Moore, JX, Chaudhary, N, and Akinyemiju, T. Metabolic syndrome prevalence by race/ethnicity and sex in the United States, National Health and nutrition examination survey, 1988-2012. Prev Chronic Dis. (2017) 14:E24. doi: 10.5888/pcd14.160287
2. Mu, L, Pan, J, Yang, L, Chen, Q, Chen, Y, Teng, Y, et al. Association between the prevalence of hyperuricemia and reproductive hormones in polycystic ovary syndrome. Reprod Biol Endocrinol. (2018) 16:104. doi: 10.1186/s12958-018-0419-x
3. Ogbera, AO, and Azenabor, AO. Hyperuricaemia and the metabolic syndrome in type 2 DM. Diabetol Metab Syndr. (2010) 2:24. doi: 10.1186/1758-5996-2-24
4. Li, QH, Zou, YW, Lian, SY, Liang, JJ, Bi, YF, Deng, C, et al. Sugar-sweeten beverage consumption is associated with more obesity and higher serum uric acid in Chinese male gout patients with early onset. Front Nutr. (2022) 9:916811. doi: 10.3389/fnut.2022.916811
5. Rostami, A, Khalili, M, Haghighat, N, Eghtesadi, S, Shidfar, F, Heidari, I, et al. High-cocoa polyphenol-rich chocolate improves blood pressure in patients with diabetes and hypertension. ARYA Atheroscler. (2015) 11:21–9.
6. Khalid, A, Haque, S, Alvi, S, Ferdous, M, Genereux, O, Chowdhury, N, et al. Promoting health literacy about cancer screening among Muslim immigrants in Canada: perspectives of imams on the role they can play in community. J Prim Care Community Health. (2022) 13:215013192110630. doi: 10.1177/21501319211063051
7. Gautam, SK, and Gupta, V. Impact of knowledge, attitude and practice on the Management of Type 2 diabetes mellitus in developing countries: a review. Curr Diabetes Rev. (2022) 18:e010521189965. doi: 10.2174/1573399817666210106104230
8. Mansy, W, Wajid, S, Alwhaibi, A, Alghadeer, SM, Alhossan, A, Babelghaith, S, et al. Assessing outpatients’ knowledge, attitude, and practice toward managing diabetes in Saudi Arabia. Inquiry. (2022) 59:469580221082781. doi: 10.1177/00469580221082781
9. Tiwaskar, M, and Vora, A. An assessment of knowledge, attitude, and practices of physicians in the Management of Hyperuricemia in India: a questionnaire-based study. J Assoc Physicians India. (2021) 69:11–2.
10. Shen, H, Wu, N, Wang, Y, Zhao, H, Zhang, L, Li, T, et al. Chloroquine attenuates paraquat-induced lung injury in mice by altering inflammation, oxidative stress and fibrosis. Int Immunopharmacol. (2017) 46:16–22. doi: 10.1016/j.intimp.2017.02.020
11. ElSayed, NA, Aleppo, G, Aroda, VR, Bannuru, RR, Brown, FM, Bruemmer, D, et al. 4. Comprehensive medical evaluation and assessment of comorbidities: standards of Care in Diabetes-2023. Diabetes Care. (2023) 46:S49–s67.2. doi: 10.2337/dc23-S004
12. Jiang, J, Zhang, T, Liu, Y, Chang, Q, Zhao, Y, Guo, C, et al. Prevalence of diabetes in patients with hyperuricemia and gout: a systematic review and Meta-analysis. Curr Diab Rep. (2023) 23:103–17. doi: 10.1007/s11892-023-01506-2
13. Bae, J, Park, KY, Son, S, Huh, Y, and Nam, GE. Associations between obesity parameters and hyperuricemia by sex, age, and diabetes mellitus: a nationwide study in Korea. Obes Res Clin Pract. (2023) 17:405–10. doi: 10.1016/j.orcp.2023.09.007
14. Liu, H, Peng, S, Yuan, H, He, Y, Tang, J, and Zhang, X. Chinese herbal medicine combined with western medicine for the treatment of type 2 diabetes mellitus with hyperuricemia: a systematic review and meta-analysis. Front Pharmacol. (2023) 14:1102513. doi: 10.3389/fphar.2023.1102513
15. Chen, C, Lai, X, Xu, A, Yang, S, Jin, J, and Yang, H. The decision for hospice care in patients with terminal illness in Shanghai: a mixed-method study. Int J Nurs Sci. (2022) 9:71–8. doi: 10.1016/j.ijnss.2021.12.002
16. Hu, L, Jin, X, Li, Y, Yang, D, Zhang, Z, He, X, et al. A mixed methods assessment of self- management needs and preferences of people with type 2 diabetes mellitus in China. Patient Prefer Adherence. (2023) 17:653–66. doi: 10.2147/ppa.S394003
17. Marciano, L, Camerini, AL, and Schulz, PJ. The role of health literacy in diabetes knowledge, self-care, and glycemic control: a Meta-analysis. J Gen Intern Med. (2019) 34:1007–17. doi: 10.1007/s11606-019-04832-y
18. Zeidi, IM, Morshedi, H, and Alizadeh Otaghvar, H. A theory of planned behavior-enhanced intervention to promote health literacy and self-care behaviors of type 2 diabetic patients. J Prev Med Hyg. (2020) 61:E601–e613. doi: 10.15167/2421-4248/jpmh2020.61.4.1504
19. Peng, W, Li, K, Yan, AF, Shi, Z, Zhang, J, Cheskin, LJ, et al. Prevalence, management, and associated factors of obesity, hypertension, and diabetes in Tibetan population compared with China overall. Int J Environ Res Public Health. (2022) 19:8787. doi: 10.3390/ijerph19148787
20. Su, B, Wang, Y, Dong, Y, Hu, G, Xu, Y, Peng, X, et al. Trends in diabetes mortality in urban and rural China, 1987-2019: a Joinpoint regression analysis. Front Endocrinol. (2021) 12:777654. doi: 10.3389/fendo.2021.777654
21. Yu, W, Li, X, Zhong, W, Dong, S, Feng, C, Yu, B, et al. Rural-urban disparities in the associations of residential greenness with diabetes and prediabetes among adults in southeastern China. Sci Total Environ. (2023) 860:160492. doi: 10.1016/j.scitotenv.2022.160492
22. Leong, CM, Lee, TI, Chien, YM, Kuo, LN, Kuo, YF, and Chen, HY. Social media-delivered patient education to enhance self-management and attitudes of patients with type 2 diabetes during the COVID-19 pandemic: randomized controlled trial. J Med Internet Res. (2022) 24:e31449. doi: 10.2196/31449
23. Parra, DI, Romero Guevara, SL, and Rojas, LZ. Influential factors in adherence to the therapeutic regime in hypertension and diabetes. Invest Educ Enferm. (2019) 37:37. doi: 10.17533/udea.iee.v37n3e02
24. Borghi, C, Agabiti-Rosei, E, Johnson, RJ, Kielstein, JT, Lurbe, E, Mancia, G, et al. Hyperuricaemia and gout in cardiovascular, metabolic and kidney disease. Eur J Intern Med. (2020) 80:1–11. doi: 10.1016/j.ejim.2020.07.006
25. Zhang, M, Zhu, X, Wu, J, Huang, Z, Zhao, Z, Zhang, X, et al. Prevalence of hyperuricemia among Chinese adults: findings from two nationally representative cross-sectional surveys in 2015-16 and 2018-19. Front Immunol. (2021) 12:791983. doi: 10.3389/fimmu.2021.791983
26. Wang, CP, Lu, YC, Hung, WC, Tsai, IT, Chang, YH, Hu, DW, et al. Inter-relationship of risk factors and pathways associated with chronic kidney disease in patients with type 2 diabetes mellitus: a structural equation modelling analysis. Public Health. (2021) 190:135–44. doi: 10.1016/j.puhe.2020.02.007
27. Huang, YF, Yang, KH, Chen, SH, Xie, Y, Huang, CB, Qing, YF, et al. Practice guideline for patients with hyperuricemia/gout. Zhonghua Nei Ke Za Zhi. (2020) 59:519–27. doi: 10.3760/cma.j.cn112138-20200505-00449
28. Liang, J, Jiang, Y, Huang, Y, Song, W, Li, X, Huang, Y, et al. The comparison of dyslipidemia and serum uric acid in patients with gout and asymptomatic hyperuricemia: a cross-sectional study. Lipids Health Dis. (2020) 19:31. doi: 10.1186/s12944-020-1197-y
29. Lou, Y, Qin, P, Wang, C, Ma, J, Peng, X, Xu, S, et al. Sex-specific Association of Serum Uric Acid Level and Change in hyperuricemia status with risk of type 2 diabetes mellitus: a large cohort study in China. J Diabetes Res. (2020) 2020:9637365:1–9. doi: 10.1155/2020/9637365
Keywords: knowledge, attitudes, practices, diabetes mellitus, hyperuricemia, disease management, cross-sectional study
Citation: Wang D, Liu Z, Liu Y, Zhao L, Xu L, He S and Duan B (2024) Knowledge, attitudes, and practices among patients with diabetes mellitus and hyperuricemia toward disease self-management. Front. Public Health. 12:1426259. doi: 10.3389/fpubh.2024.1426259
Edited by:
Michael Harris, Oregon Health and Science University, United StatesReviewed by:
Abril Violeta Muñoz Torres, National Autonomous University of Mexico, MexicoHarish Rangareddy, Haveri Institute of Medical Sciences, India
Copyright © 2024 Wang, Liu, Liu, Zhao, Xu, He and Duan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Binhong Duan, ZHVhbmJoQDE2My5jb20=
 Dan Wang
Dan Wang Zhixin Liu2
Zhixin Liu2 Binhong Duan
Binhong Duan