- 1MAP Centre for Urban Health Solutions, Unity Health Toronto, Toronto, ON, Canada
- 2Department of Family and Community Medicine, University of Toronto, Toronto, ON, Canada
- 3ICES, Toronto, ON, Canada
- 4Department of Medicine, University of Toronto, Toronto, ON, Canada
Introduction: Patients with major mental illness (MMI) and substance use disorders (SUD) face barriers in accessing healthcare. In this population-based retrospective cohort study, we investigated the uptake of COVID-19 vaccination in Ontario, Canada among community-dwelling individuals receiving healthcare for major mental illness (MMI) and/or substance use disorders (SUD), comparing them to matched general population controls.
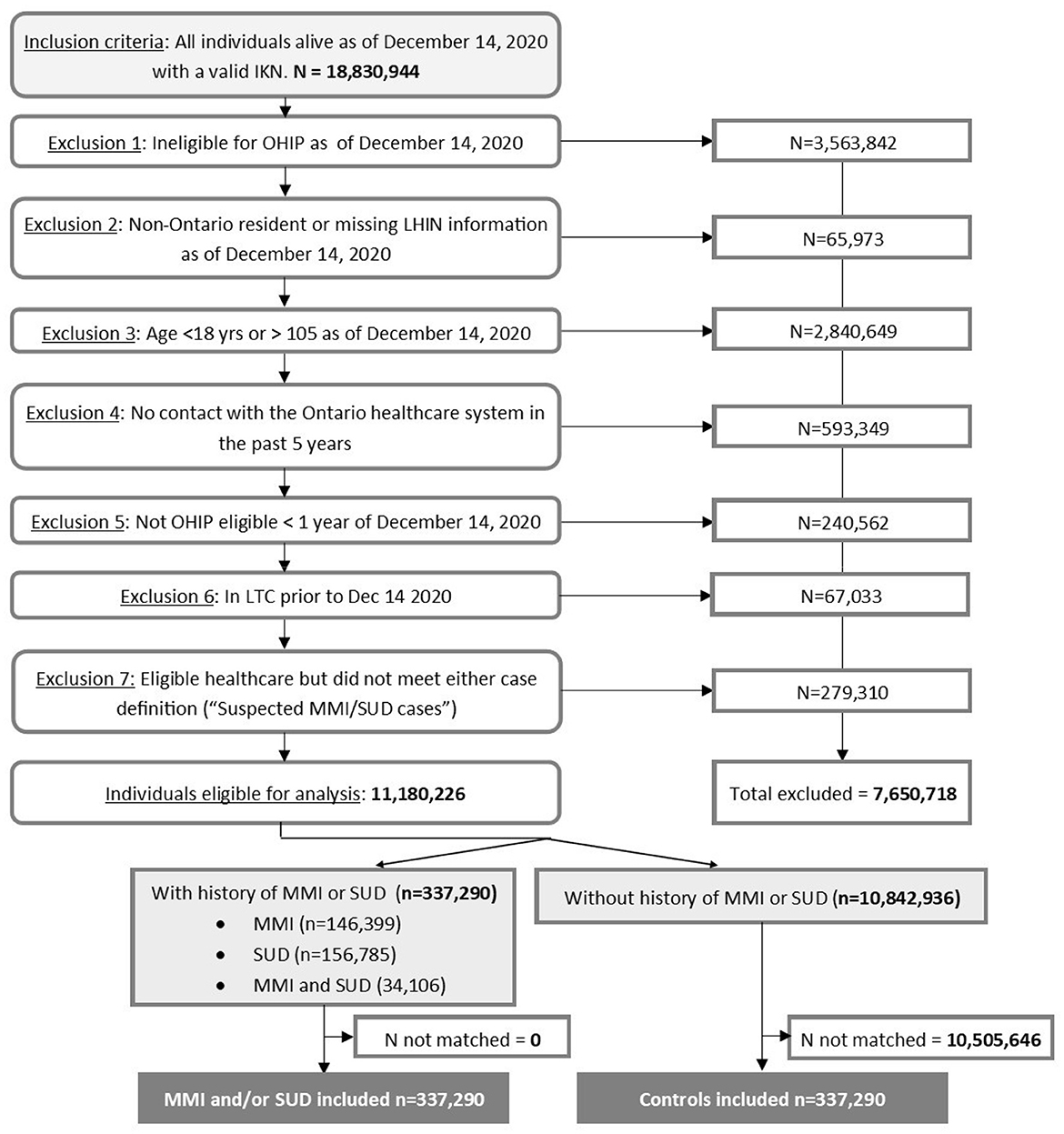
Methods: Using linked health administrative data, we identified 337,290 individuals receiving healthcare for MMI and/or SUD as of 14 December 2020, matched by age, sex, and residential geography to controls without such healthcare. Follow-up extended until 31 December 2022 to document vaccination events.
Results: Overall, individuals receiving healthcare for MMI and/or SUD (N = 337,290) had a slightly lower uptake of first (cumulative incidence 82.45% vs. 86.44%; hazard ratio [HR] 0.83 [95% CI 0.82–0.83]) and second dose (78.82% vs. 84.93%; HR 0.77 [95% CI 0.77–0.78]) compared to matched controls. Individuals receiving healthcare for MMI only (n = 146,399) had a similar uptake of first (87.96% vs. 87.59%; HR 0.97 [95% CI 0.96–0.98]) and second dose (86.09% vs. 86.05%, HR 0.94 [95% CI 0.93–0.95]). By contrast, individuals receiving healthcare for SUD only (n = 156,785) or MMI and SUD (n = 34,106) had significantly lower uptake of the first (SUD 78.14% vs. 85.74%; HR 0.73 [95% CI 0.72–0.73]; MMI & SUD 78.43% vs. 84.74%; HR 0.76 [95% CI 0.75–0.77]) and second doses (SUD 73.12% vs. 84.17%; HR 0.66 [95% CI 0.65–0.66]; MMI & SUD 73.48% vs. 82.93%; HR 0.68 [95% CI 0.67–0.69]).
Discussion: These findings suggest that effective strategies to increase vaccination uptake for future COVID-19 and other emerging infectious diseases among community-dwelling people with SUD are needed.
1 Introduction
Access to healthcare facilities is a persistent challenge for patients with substance use disorders (SUD) and major mental illness (MMI), an umbrella term referring to specific mental health disorders (such as psychotic disorder, schizophrenia, or bipolar disorder), which interfere with daily living (1–3). Public health measures that reduced the transmission of SARS-CoV-2 during the COVID-19 pandemic had the unintended side effect of limiting supports and access to care for these individuals (4). Moreover, individuals with MMI and/or SUD also faced a higher burden of SARS-CoV-2 infection and adverse sequelae of infection compared to the general population (5–7). As a result, increasing the uptake of COVID-19 vaccination is key to reducing inequitable outcomes in this group.
In Ontario, Canada, COVID-19 vaccines were accessible from December 14, 2020, but for several months, the stock was very limited, forcing the provincial government to determine how to prioritize access. At the advice of Ontario's Vaccine Distribution Taskforce (8), Ontario decided to prioritize individuals based on risk factors for negative health outcomes following infection (for example, age and comorbidities) (8, 9), by likelihood of infection (for example, healthcare or essential worker status), and eventually by geography, as determined by early infection surveillance reports (8, 10, 11). People with MMI and/or SUD were included in Phase 2 of Ontario's vaccination strategy, becoming eligible for vaccination on the basis of having these conditions as of April 2021 (12). Vaccine administration, the responsibility of regional health units and municipalities, occurred primarily through specialized mass vaccination clinics, local pharmacies, and certain local primary care providers (13). In many areas, mobile clinics were also used to help vaccinate groups with anticipated barriers to access (13, 14). However, despite efforts to improve access through eligibility prioritization, other well-known barriers to uptake may have prevented individuals with MMI and/or SUD from benefiting with regards their eligibility prioritization. These barriers include low vaccine awareness and education (including tackling misinformation and pre-existing mistrust) (15, 16), lack of transportation to vaccination centers (15), inadequate internet access or technological literacy levels (17) needed to book appointments, or the numerous competing priorities with higher short-term urgency, such as securing basic needs such as shelter (18) and food (19).
In the present study, we assessed COVID-19 vaccination rates among community-dwelling individuals receiving healthcare facilities for MMI and/or SUD in Ontario as compared to matched controls, to better understand whether this population may have faced continued barriers to vaccine uptake.
2 Methods
2.1 Study design and setting
We conducted a retrospective population-based cohort study in Ontario, Canada (population = 14.2 million) (20), from 14 December 2020 to 31 December 2022. As in most parts of Canada, the majority of Ontarians (80%) reside in large urban centers, but there are also substantial populations in rural regions with varying levels of remote dwelling (21). In Ontario, COVID-19 vaccine products were obtained and supplied free of cost through the public healthcare system and received through mass vaccination clinics, pharmacies, and eventually through mobile vaccination units (13).
We used health administrative databases associated using unique encoded identifiers and analyzed at the ICES (formerly known as the Institute for Clinical Evaluative Sciences) (22). The ICES is a prescribed entity under Section 45 of Ontario's Personal Health Information Protection Act. This Act authorizes the ICES to collect personal health information, without consent, for the purpose of analysis or compiling statistical information with respect to the management of, evaluation or monitoring of, the allocation of resources to or planning for all or part of the healthcare system. In Ontario, healthcare is administered through a single-payer model, with universal coverage of medical services provided through the Ontario Health Insurance Plan (OHIP) (23). Thus, administrative databases for health services provided cover the vast majority (>99%) of the population. This study follows the Reporting of Studies Conducted Using Observational Routinely Collected Data (RECORD) reporting guidelines (see Supplementary material A) (24).
2.2 Data sources
We identified participants using a combination of the ICES Registered Persons Database, the Canadian Institute for Health Information Discharge Abstract Database, the National Ambulatory Care Reporting System, the Ontario Mental Health Reporting System, and the Ontario Health Insurance Plan claims database. We identified vaccination outcomes through the Ontario COVAXON database, which includes all vaccine doses administered in Ontario, as well as doses administered outside Ontario, for which the individual provided proof of vaccination and consent for inclusion into the database. Other covariates were drawn from a variety of databases, including the aforementioned sources, and also certain ICES-derived datasets that apply validated case definitions, such as the Ontario Asthma dataset (25); the Ontario Chronic Obstructive Pulmonary Disease cohort (26); the Ontario Diabetes dataset (27); the Ontario Hypertension dataset (28); the Ontario Congestive Heart Failure dataset (29); and the Ontario Dementia dataset (30). All data sources are further described in Supplementary material B.
2.3 Participants
We followed-up participants from 14 December 2020, the date of the first COVID-19 vaccination in Ontario (31), until 31 December 2022, the latest date for which complete data were available at the time of analysis. Potential participants in both groups were excluded if they were ineligible for OHIP coverage (for example, recent migrants to Ontario such as interprovincial migrants, refugees whose claims have not yet been accepted, or international migrants with short-term work permits, representing fewer than 1% of the population) (23), were not Ontario residents, or were potentially not in Ontario for the period of study (i.e., if they had no contact with the Ontario healthcare system within the past 5 years). Individuals were also excluded where geographic information on the postal code was unknown, as matching on geography was required to account for vaccine prioritization by area of residence (8, 10, 11) or where the individual resided in a long-term care facility within 120 days of start of follow-up, as such individuals had different prioritization and access to COVID-19 vaccination than community-dwelling individuals, our population of interest.
Participants comprised two groups. Our first group consisted of adults aged 18 to 105 who met the case definition of MMI and/or SUD within the 3 years prior to 14 December 2020. Individuals met the case definition for MMI if they were hospitalized in an acute or psychiatric inpatient facility or had at least three emergency department visits or physician service claims with a diagnosis of any psychotic disorder or bipolar disorder. We did not include depression in our definition of MMI due to the inability of administrative data to distinguish between depression and other conditions in outpatient data. Individuals met the case definition for SUD if they were hospitalized in acute or psychiatric inpatient facilities or had at least three emergency department visits or physician service claims with a diagnosis of substance use disorder. If individuals met case definitions for both MMI and SUD, they were flagged as having both conditions. Our case definitions were adapted from validated definitions for chronic psychotic illness (32). Full case definitions including eligible codes are available in Supplementary material C. Our second control group consisted of individuals alive as of 14 December 2020 without any healthcare contact for MMI or SUD in the past 3 years. Individuals with some eligible healthcare contact for MMI and/or SUD, but not enough to meet either case definition, were excluded from both study groups.
We matched potential participants without healthcare for MMI or SUD to participants with MMI and/or SUD at a 1:1 ratio, without replacement, by age (exact), sex-at-birth (exact), and geography (forward sortation area code or FSA, which are postal districts based on residential postal codes). We matched on age since age was a key eligibility criterion for vaccination prioritization, and we matched on sex-at-birth due to expected differences in prevalence as well as vaccination uptake (33). We matched on geography because vaccination was prioritized for certain forward sortation areas that were associated with excess infection transmission in Ontario (8, 10, 11). We did not match on comorbidities or other factors that significantly differed between groups in order to avoid potentially increasing the risk of including individuals with MMI and/or SUD who do not receive healthcare facilities for their condition(s) among the controls. Individuals were censored at entry into long-term care or death.
2.4 Outcomes
Our outcome of interest was time to receipt of any COVID-19 vaccine product, as recorded in the Ontario COVID-19 vaccine database (COVAXON). We considered time to first and second doses primarily, as in Ontario, the vast majority (>99%) of vaccine products were two-dose ones. Therefore, the receipt of two doses indicates a full primary course of vaccination.
2.5 Covariates
We obtained participants' demographic characteristics as of 14 December 2020, including age, sex-assigned-at-birth, rurality, and geography of the participant's residence (Local Health Integration Network), neighborhood-level income quintile, and neighborhood-level of racialized and newcomer populations. We further identified the presence of asthma (25), chronic obstructive pulmonary disorder (26), diabetes (27), congestive heart failure (28), hypertension (29), and dementia (30) using validated case definitions. Finally, we measured the participant's Charlson comorbidity index, used to predict mortality based on the presence and severity of comorbidities, by using a methodology (34) adapted for International Classification of Diseases, 10th revision (35) using patient hospitalizations from the past 5 years. The complete variable and validated case definitions are available in Supplementary material C.
2.6 Statistical analysis
We compared baseline characteristics between groups before and after matching. Due to the size of the cohorts, we used standardized differences (36), which assess differences between group means as a percentage of the pooled standard deviation to assess the significance of differences between groups. A difference of 10% or more was considered meaningful. We calculated the cumulative incidence of receiving first and second doses of COVID-19 vaccines by group membership, overall, and stratifying by type of exposure (MMI and/or SUD; MMI only; SUD only; or MMI and SUD). Finally, we used survival modeling to estimate the hazard ratio (HR) of receiving a first or second dose of COVID-19 vaccine in the MMI and/or SUD group over the observation period, compared to their matched control; again, these were repeated by the type of exposure. Models reported were Cox proportional hazards models rather than subdistributional hazard models, taking into account the competing risk of death, as the latter did not meaningfully change results.
We ran a number of sensitivity analyses to ensure robustness of results. First, we ran adjusted survival models adjusting for a neighborhood level income, Charlson Comorbidity Index, and both neighborhood level income and Charlson Comorbidity Index. Second, we repeated our entire analysis with a more sensitive case definition (requiring only one eligible hospitalization, ED or outpatient visit to be considered part of the MMI and/or SUD cohort). Results of sensitivity analyses are presented in the Supplementary material.
In all outputs, small cells (less than or equal to five) were suppressed to protect patient privacy. All statistical tests were two-tailed with p < 0.05 set as the level of significance; analyses were conducted using SAS Enterprise Guide v 7.1.
2.7 Ethical review
This study received ethics approval from the Health Sciences Research Ethics Board at the University of Toronto (RIS Protocol # 41528).
3 Results
We identified 337,290 eligible community-dwelling people receiving healthcare facilities for MMI and/or SUD and 10,842,936 eligible community-dwelling people without healthcare facilities for MMI or SUD (Figure 1). Supplementary material D, Table 1 describes the unmatched cohorts. Briefly, individuals receiving healthcare facilities for MMI and/or SUD were younger, more likely to be male, reside in neighborhoods with the lowest income quintile, and have substantially higher rates of asthma, COPD, and dementia compared to controls. They were also more likely to have a higher Charlson score. After matching, we included 337,290 community-dwelling individuals in each group (Figure 1). Of these, a total of 146,399 participants had MMI only; 156,785 participants had SUD only; and 34,106 participants had both MMI and SUD.
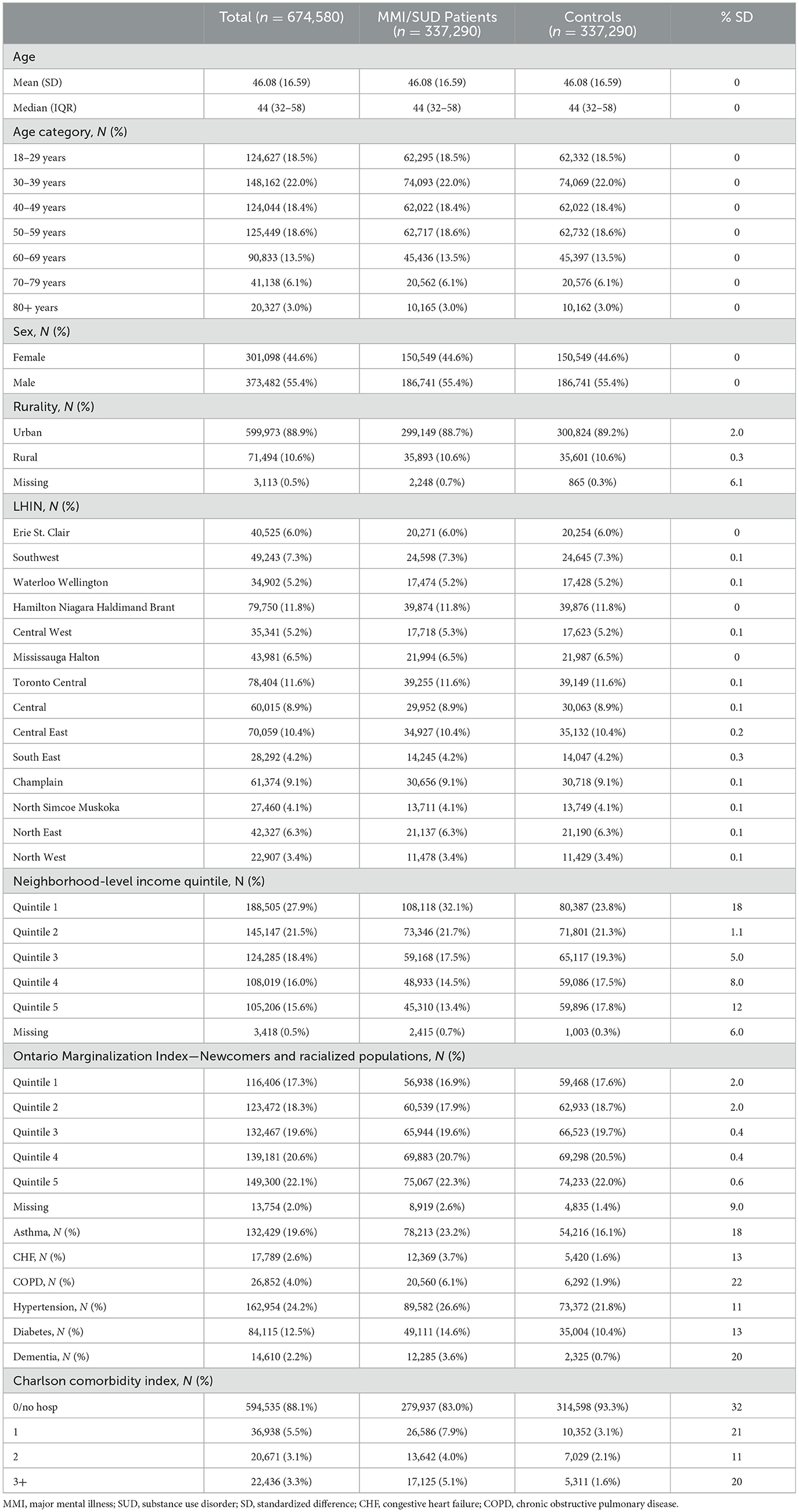
Characteristics of matched participants are provided in Table 1. After matching, few demographic characteristics between groups remained significantly different; however, individuals receiving healthcare facilities for MMI and/or SUD remained significantly more likely to reside in neighborhoods with the lowest income quintile (32.1% vs. 23.8%). They were also more likely to have a higher Charlson Comorbidity Index, as well as asthma (23.2% vs. 16.1%), COPD (6.1% vs. 1.9%), congestive heart failure (3.7% vs. 1.6%), diabetes (14.6% vs. 10.4%), hypertension (26.6% vs. 21.8%), and dementia (3.6% vs. 0.7%).
Figures 2A, B show the cumulative incidence of receiving a first and second dose of vaccine by exposure status and subgroup. By 31 December 2022, individuals with MMI and/or SUD had a cumulative incidence of first and second dose of 82.45% and 78.82%, respectively, compared to 86.44% and 84.93% among controls, respectively. However, much of the difference appears to be driven by the uptake among individuals with SUD (with or without MMI). Individuals with only MMI had a cumulative incidence of first and second dose of 87.96% and 86.09%, respectively, very similar to 87.59% and 86.05% among controls. By contrast, individuals with only SUD had a cumulative incidence of first and second dose of 78.14% and 73.12%, respectively, compared to 85.74% and 84.17% among controls, and individuals with both MMI & SUD had a cumulative incidence of cumulative incidence of first and second dose of 78.43% and 73.48%, respectively, compared to 84.74% and 82.93% among controls. In both SUD subgroups, uptake for both first and second doses began to diverge when uptake was approximately 20%, in May (first dose) and July (second dose) 2021.
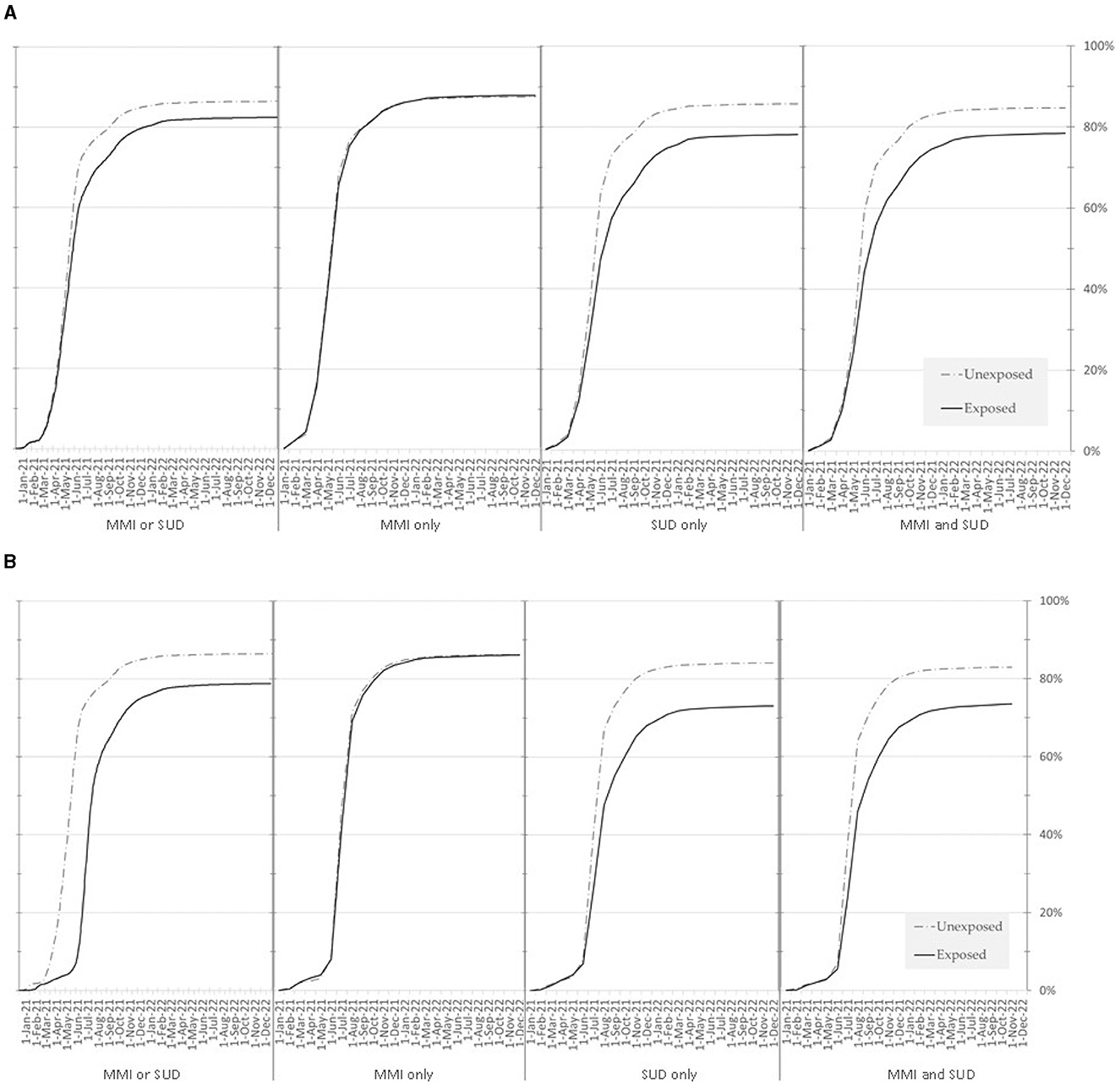
Figure 2. (A) Cumulative incidence of the first COVID-19 vaccine dose among patients with MMI and/or SUD and matched controls, between 14 December 2020 and 31 December 2022. MMI, major mental illness; SUD, substance use disorder. (B) Cumulative incidence of the second COVID-19 vaccine dose among patients with MMI and/or SUD and matched controls, between 14 December 2020 and 31 December 2022. MMI, major mental illness; SUD, substance use disorder.
Table 2 shows the results of Cox proportional hazard models assessing the association between group membership and vaccine uptake, by dose and subgroup. All subgroups had statistically significant lower first- and second-dose uptake compared to their matched controls, but the difference between MMI patients and their controls was relatively small (first dose HR 0.971 [95% CI 0.964–0.979]; second dose HR 0.940 [95% CI 0.933–0.947]); while a larger difference was observed in patients with SUD only (first dose HR 0.728 [95% CI 0.723–0.734]; second dose HR 0.657 [95% CI 0.652–0.662]) or patients with both MMI and SUD (first dose HR 0.758 [95% CI 0.746–0.770]; second dose HR 0.682 [95% CI 0.671–0.694]), compared to their corresponding controls.
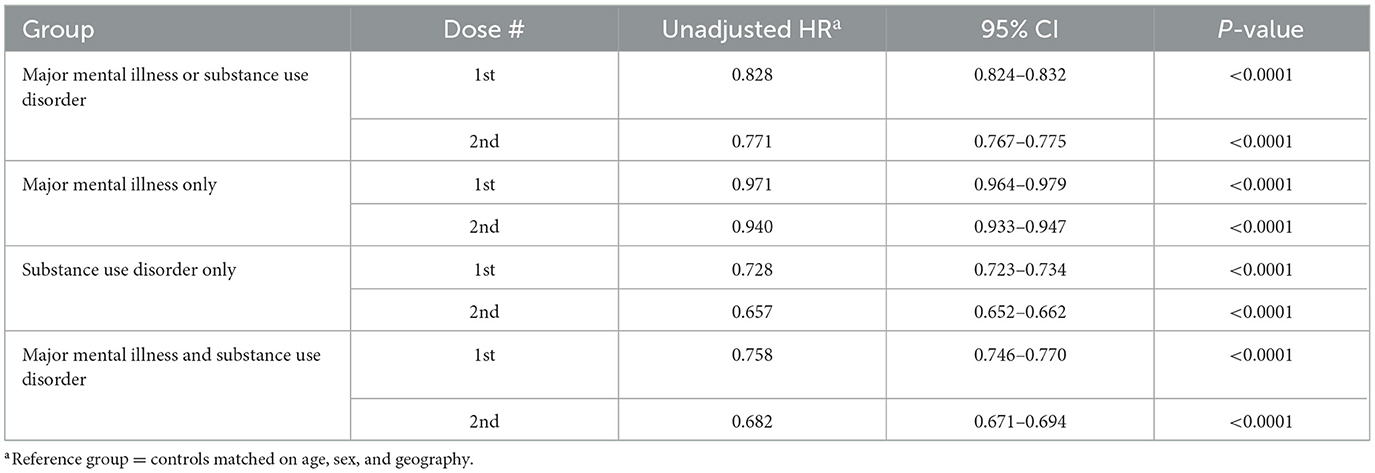
Table 2. Unadjusted Cox proportional hazards model assessing the association between major mental illness and/or substance use disorder and receipt of a first or second dose of any COVID-19 vaccine before the end of the observation period (31 December 2022).
Supplementary Table 2 presents a sensitivity analysis adjusting the MMI/SUD models for neighborhood income, Charlson Comorbidity Index, and both neighborhood income and Charlson Comorbidity Index, showing a relatively less impact of these variables on first or second dose vaccine uptake. Supplementary Table 3, Supplementary Figures 1, 2 present results when using a case definition of MMI and/or SUD that required only one eligible healthcare encounter. This less stringent case definition approximately increased the cohort size by twofold; otherwise, the cumulative incidence figures (Supplementary Figure 1, 2) and model outputs (Supplementary Table 3) were similar to those presented in the main analysis.
4 Discussion
We found that community-dwelling individuals receiving healthcare facilities for major mental illness had only slightly lower COVID-19 vaccination uptake as compared to matched controls, but that community-dwelling individuals receiving healthcare facilities for either substance use disorder or combined MMI and SUD were less likely to be vaccinated by the study end date. Results were robust, irrespective of the case definition used or by adjustment for neighborhood income or level of comorbidity. Through most of the follow-up [April 2021 onward, when Phase 2 of Ontario's vaccination plan began (12)], individuals with any mental health diagnosis or substance use disorder were eligible to receive COVID-19 vaccination on a priority basis in Ontario (9, 12). Furthermore, as this group had substantially higher comorbidity rates than matched controls, many would have been also prioritized for vaccination due to physical comorbidity risk factors, which were also prioritized in Ontario's vaccination strategy (9). Despite this, vaccination rates for the SUD and MMI & SUD groups lagged substantially behind that of matched controls, with uptake for both doses diverging once groups had a cumulative incidence of about 20%.
Previous reports concur with our findings, showing a lack of disparity in COVID-19 vaccination among people with MMI and disparities for people with SUD. People with major mental illness in other studies had vaccination rates ranging from only slightly lower (37), approximately similar (38, 39), or somewhat higher (40) than comparators in numerous settings. By contrast, most studies about individuals who use drugs report substantial COVID-19 vaccine hesitancy (41–43) and lower vaccine uptake than direct or indirect comparisons with general population comparators (44–48).
Despite both groups experiencing substantial stigma, perceptions of individuals with mental illness have changed substantially in the past decades, as understandings of the medical underpinnings of their condition have evolved (49). Moreover, individuals with substance use disorder continue to be frequently viewed through a moralistic lens, with their condition seen as a result of personal choice or moral failing rather than the complex interplay of genetic, environmental, and psychological factors (49). As a result, health professionals have been found to often hold stigmatizing views toward people with substance use disorders, which can affect the quality of care provided and feelings of patients toward healthcare (49, 50). This provides an important context to the literature about COVID-19 vaccine hesitancy and barriers to uptake, specific to people who use drugs. A recent national study (51) in Canada suggests that barriers to COVID-19 vaccination among people who use drugs include a lack of knowledge about the benefits and risks associated with the vaccine but also significant distrust toward government and healthcare agencies, and skepticism about the effectiveness of a vaccine so rapidly developed. Crucially, in this study and in other related work, people who use drugs trust information most when it is shared by peers (52), community leaders (53, 54), individuals with lived experience, harm reduction workers (55), and trusted healthcare providers (51), rather than by government or health authorities.
By contrast, Ontario took a top–down approach to its COVID-19 vaccination strategy, with the provincial government and local public health authorities organizing most of the official communication pertaining to vaccination. This was, unfortunately, judged to be disorganized and inconsistent by the Office of the Auditor General of Ontario, leading to public confusion and misunderstandings about the risks and benefits of COVID-19 vaccination (56). In combination with widespread misinformation around COVID-19 vaccine products and substantial distrust of government or healthcare officials generally, confidence in vaccination among individuals with substance use disorder was likely undermined (56). Additionally, although Public Health Ontario (a provincial agency) recommended communities adopt an individualized, culturally safe and trauma-informed approach to COVID-19 vaccination (57) and the province eventually promoted targeted strategies emphasizing accessibility (14), vaccination administration was organized by local public health units, (13) with the result that each local area in practice engaged with marginalized communities only to the extent possible by local resources and planning. Toronto, for example, invested significantly to enhance outreach through their Vaccine Engagement Team (VET) (58), which resulted in excellent local vaccination rates (59) as well as significantly reduced gaps in vaccination among groups with higher rates of substance use disorder, such as homeless people (60). Such approaches have also been used elsewhere with success (52–54), but were not very common across Canada (51, 56).
4.1 Strengths and limitations
Our study benefits from leveraging linked health administrative data which follow the vast majority of the Ontario population (that is, those eligible for OHIP coverage, representing over 99% of Ontario residents), giving us a quasi-population-level assessment of vaccination uptake among community-dwelling people receiving healthcare facilities for MMI and/or SUD. However, OHIP eligibility does not include recent migrants to Ontario such as interprovincial migrants, refugees whose claims have not yet been accepted, or international migrants with short-term work permits (23). The prevalence of major mental illness and substance use disorder may differ in some of these groups compared to the general population (61); therefore, results should only be extended to Ontarians with OHIP coverage.
Furthermore, our case definition of major mental illness and substance use disorder relies on the interaction with the healthcare system. Previous work has shown that a significant number of individuals with major mental illness or who use drugs experience stigma during healthcare interactions (62), which can result in healthcare avoidance; healthcare-avoidant individuals with MMI and/or SUD might be more likely to be distrustful of healthcare deemed non-essential like COVID-19 vaccination. Thus, our results may understate the true disparity in vaccine uptake in these groups. Combined with a lack of validation work to verify the case definition performance of our MMI and SUD constructs, our results should only be generalized to community-dwelling people with MMI and/or SUD who use healthcare.
Finally, our definition of MMI did not include codes for major depressive disorder, largely due to the inability of outpatient administrative databases in cleanly separating out this condition from other conditions not part of MMI (such as anxiety). As a result, findings may not be representative of results for individuals with major depressive disorder.
5 Conclusions
Community-dwelling people in Ontario receiving healthcare for SUD or combined MMI and SUD have lower COVID-19 vaccine uptake than controls matched by age, sex-at-birth, and geography. Our results suggest that efforts to improve vaccination uptake need to target the specific concerns and barriers faced by people who use drugs. Future work should determine the specific concerns and barriers to vaccination faced by people who use drugs in Ontario and assess the impact of strategies targeting such barriers and concerns, such as community-led outreach by trusted individuals.
Data availability statement
The datasets presented in this article are not readily available because the dataset from this study is held securely in coded form at ICES. While legal data sharing agreements between ICES and data providers (e.g., healthcare organizations and government) prohibit ICES from making the dataset publicly available, access may be granted to those who meet pre-specified criteria for confidential access, available at www.ices.on.ca/DAS (email: ZGFzQGljZXMub24uY2E=). The full dataset creation plan and underlying analytic code are available from the authors upon request, understanding that the computer programs may rely upon coding templates or macros that are unique to ICES and are therefore either inaccessible or may require modification. Requests to access data, the dataset creation plan or underlying analytic code may be sent to the corresponding author. Requests to access the datasets should be directed to ZGFzQGljZXMub24uY2E=.
Ethics statement
The studies involving humans were approved by Health Sciences Research Ethics Board at the University of Toronto. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
LR: Validation, Visualization, Writing – original draft, Writing – review & editing. AH: Conceptualization, Methodology, Writing – review & editing. VA: Data curation, Formal analysis, Methodology, Software, Validation, Writing – review & editing. MC: Methodology, Project administration, Validation, Writing – review & editing. SH: Conceptualization, Methodology, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by ICES, which was funded by an annual grant from the Ontario Ministry of Health (MOH) and the Ministry of Long-Term Care (MLTC). This study also received funding and support from the St Joseph's Health Centre Seed Grant and the Ontario Health Data Platform, a Province of Ontario initiative to support Ontario's ongoing response to COVID-19 and its related impacts. The opinions, results and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by the OHDP, its partners, or the Province of Ontario is intended or inferred.
Acknowledgments
The authors wish to thank Dr. Ning Liu for her contributions to this study. This study used data adapted from the Statistics Canada Postal Code Conversion File, which is based on data licensed from Canada Post Corporation and/or data adapted from the Ontario Ministry of Health Postal Code Conversion File, which contains data copied under license from ©Canada Post Corporation and Statistics Canada. Parts of this material are based on data and/or information compiled and provided by CIHI and the Ontario Ministry of Health. We also thank the Toronto Community Health Profiles Partnership for providing access to the Ontario Marginalization Index.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
The analyses, conclusions, opinions, and statements expressed herein are solely those of the authors and do not reflect those of the funders or data sources; no endorsement by any of the funders or data sources is intended or should be inferred.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1426152/full#supplementary-material
References
1. Chadwick A, Street C, McAndrew S, Deacon M. Minding our own bodies: Reviewing the literature regarding the perceptions of service users diagnosed with serious mental illness on barriers to accessing physical health care. Int J Mental Health Nursing. (2012) 21:211–9. doi: 10.1111/j.1447-0349.2011.00807.x
2. Knaak S, Mantler E, Szeto A. Mental illness-related stigma in healthcare: Barriers to access and care and evidence-based solutions. in Healthcare Management Forum 2017. Los Angeles, CA: SAGE Publications. (2017). p. 111–116. doi: 10.1177/0840470416679413
3. Livingston JD. Structural Stigma in Health-Care Contexts for People With Mental Health and Substance Use Issues. Ottawa, Canada: Mental Health Commission of Canada. (2020).
4. Melamed OC, Hahn MK, Agarwal SM, Taylor VH, Mulsant BH, Selby P. Physical health among people with serious mental illness in the face of COVID-19: concerns and mitigation strategies. Gen Hosp Psychiatry. (2020) 66:30–3. doi: 10.1016/j.genhosppsych.2020.06.013
5. Bertolini F, Witteveen AB, Young S, Cuijpers P, Ayuso-Mateos JL, Barbui C, et al. Risk of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 mortality in people with pre-existing mental disorders: an umbrella review. BMC Psychiatry. (2023) 23:1–2. doi: 10.1186/s12888-023-04641-y
6. De Hert M, Mazereel V, Stroobants M, De Picker L, Van Assche K, Detraux J. COVID-19-related mortality risk in people with severe mental illness: a systematic and critical review. Front Psychiatry. (2022) 12:798554. doi: 10.3389/fpsyt.2021.798554
7. Yang H, Chen W, Hu Y, Chen Y, Zeng Y, Sun Y, et al. Pre-pandemic psychiatric disorders and risk of COVID-19: a UK Biobank cohort analysis. Lancet Healthy Long. (2020) 1:e69–79. doi: 10.1016/S2666-7568(20)30013-1
8. Bogoch II, Halani S. COVID-19 vaccines: a geographic, social and policy view of vaccination efforts in Ontario, Canada. Camb J Regions, Econ Soc. (2022) 15:757–70. doi: 10.1093/cjres/rsac043
9. Government of Ontario. Ontario's Vaccine Distribution Implementation Plan. Available online at: https://www.ontario.ca/page/ontarios-vaccine-distribution-implementation-plan (accessed July 10, 2023).
10. Mishra S, Stall NM, Ma H, Odutayo A, Kwong JC, Allen U, et al. A vaccination strategy for Ontario COVID-19 hotspots and essential workers. Sci Briefs. (2021) 2:26. doi: 10.47326/ocsat.2021.02.26.1.0
11. Brown KA, Stall NM, Joh E, Allen U, Bogoch II, Buchan SA, et al. A Strategy for the Mass Distribution of COVID19 Vaccines in Ontario Based on Age and Neighbourhood. In: Science Briefs of the Ontario COVID-19 Science Advisory Table. Toronto, ON: Ontario COVID-19 Science Advisory Table (2021).
12. Government of Ontario. Populations Eligible for Phase Two COVID-19 Vaccination: Phase Two to Vaccinate Groups Based on Age and Risk. (2023). Available online at: https://news.ontario.ca/en/backgrounder/60570/populations-eligible-for-phase-two-covid-19-vaccination (accessed July 10, 2023).
13. Fitzpatrick T, Allin S, Camillo CA, Habbick M, Mauer-Vakil D, Muhajarine N, et al. COVID-19 Vaccination Rollout: Ontario. (2022). Available online at: https://covarrnet.ca/wp-content/uploads/2022/02/covid-19-vaccination-rollout-ontario-2022-01-21.pdf (accessed July 10, 2023).
14. Government of Ontario. Ontario Deploying Last Mile Strategy to Further Increase Vaccination Rates. (2023). Available online at: https://news.ontario.ca/en/release/1000762/ontario-deploying-last-mile-strategy-to-further-increase-vaccination-rates (accessed August 11, 2023).
15. Warren N, Kisely S, Siskind D. Maximizing the uptake of a COVID-19 vaccine in people with severe mental illness: a public health priority. JAMA Psychiat. (2021) 78:589–90. doi: 10.1001/jamapsychiatry.2020.4396
16. Eyllon M, Dang AP, Barnes JB, Buresh J, Peloquin GD, Hogan AC, et al. Associations between psychiatric morbidity and COVID-19 vaccine hesitancy: an analysis of electronic health records and patient survey. Psychiatry Res. (2022) 307:114329. doi: 10.1016/j.psychres.2021.114329
17. Spanakis P, Wadman R, Walker L, Heron P, Mathers A, Baker J, et al. Measuring the digital divide among people with severe mental ill health using the essential digital skills framework. Perspect Public Health. (2022) 5:17579139221106399. doi: 10.1177/17579139221106399
18. Smartt C, Prince M, Frissa S, Eaton J, Fekadu A, Hanlon C. Homelessness and severe mental illness in low-and middle-income countries: scoping review. BJPsych Open. (2019) 5:e57. doi: 10.1192/bjo.2019.32
19. Rodgers IT, Samaranayake D, Anderson A, Capobianco L, Cohen DE, Ehntholt A, et al. The impacts of COVID-19 on a statewide population with mental illness. Psychiatric Serv. (2022) 73:674–8. doi: 10.1176/appi.ps.202100328
20. Statistics Canada. Census Profile. (2021). Available online at: https://www12.statcan.gc.ca/census-recensement/2021/dp-pd/prof/details/page.cfm?Lang=E&SearchText=Ontario&DGUIDlist=2021A000235&GENDERlist=1,2,3&STATISTIClist=1,4&HEADERlist=0 (accessed January 28, 2024).
21. Statistics Canada. Population Growth in Canada's Rural Areas, 2016 to 2021. Available online at: https://www12.statcan.gc.ca/census-recensement/2021/as-sa/98-200-x/2021002/98-200-x2021002-eng.cfm (accessed January 28, 2024).
22. Schull MJ, Azimaee M, Marra M, Cartagena RG, Vermeulen MJ, Ho M, Guttmann A. ICES: data, discovery, better health. Int J Populat Data Sci. (2019) 4:1135. doi: 10.23889/ijpds.v4i2.1135
23. Government of Ontario. OHIP Eligibility. (2023). Available online at: https://www.health.gov.on.ca/en/public/publications/ohip/docs/ohip_eligibility_fs_en.pdf (accessed January 28, 2024).
24. Benchimol EI, Smeeth L, Guttmann A, Harron K, Moher D, Petersen I, et al. RECORD Working Committee. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS medicine. (2015) 12:e1001885. doi: 10.1371/journal.pmed.1001885
25. Gershon AS, Wang C, Guan J, Vasilevska-Ristovska J, Cicutto L, To T. Identifying patients with physician-diagnosed asthma in health administrative databases. Can Resp J. (2009) 16:183–8. doi: 10.1155/2009/963098
26. Gershon AS, Wang C, Guan J, Vasilevska-Ristovska J, Cicutto L, To T. Identifying individuals with physcian diagnosed COPD in health administrative databases. COPD. (2009) 6:388–94. doi: 10.1080/15412550903140865
27. Hux JE, Ivis F, Flintoft V, Bica A. Diabetes in Ontario: determination of prevalence and incidence using a validated administrative data algorithm. Diabetes Care. (2002) 25:512–6. doi: 10.2337/diacare.25.3.512
28. Tu K, Campbell NR, Chen ZL, Cauch-Dudek KJ, McAlister FA. Accuracy of administrative databases in identifying patients with hypertension. Open Med. (2007) 1:e18.
29. Schultz SE, Rothwell DM, Chen Z, Tu K. Identifying cases of congestive heart failure from administrative data: a validation study using primary care patient records. Chronic Dis Injur Can. (2013) 33:3. doi: 10.24095/hpcdp.33.3.06
30. Jaakkimainen RL, Bronskill SE, Tierney MC, Herrmann N, Green D, Young J, et al. Identification of physician-diagnosed Alzheimer's disease and related dementias in population-based administrative data: a validation study using family physicians' electronic medical records. J Alzheimer's Dis. (2016) 54:337–49. doi: 10.3233/JAD-160105
31. Government of Ontario. Ontario Delivers First COVID-19 Vaccine in the Country. (2023). Available online at: https://news.ontario.ca/en/statement/59635/ontario-delivers-first-covid-19-vaccine-in-the-country (accessed July 10, 2023).
32. Kurdyak P, Lin E, Green D, Vigod S. Validation of a population-based algorithm to detect chronic psychotic illness. Can J Psychiat. (2015) 60:362–8. doi: 10.1177/070674371506000805
33. Government of Canada. COVID-19 Vaccination: Vaccination Coverage. Available online at: Available online at: https://health-infobase.canada.ca/covid-19/vaccination-coverage/ (accessed July 10, 2023).
34. Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. (1992) 45:613–9. doi: 10.1016/0895-4356(92)90133-8
35. Sundararajan V, Henderson T, Perry C, et al. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol. (2004) 57:1288–94. doi: 10.1016/j.jclinepi.2004.03.012
36. Austin PC. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat Simul Comput. (2009) 38:1228–34. doi: 10.1080/03610910902859574
37. Gibbon S, McPhail E, Mills G, McBride M, Storer R, Taylor N, et al. Uptake of COVID-19 vaccination in a medium secure psychiatric hospital population. BJPsych open. (2021) 7:e108. doi: 10.1192/bjo.2021.924
38. Peritogiannis V, Drakatos I, Gioti P, Garbi A. Vaccination rates against COVID-19 in patients with severe mental illness attending community mental health services in rural Greece. Int J Soc Psychiat. (2023) 69:208–15. doi: 10.1177/00207640221081801
39. Haderlein TP, Steers WN, Dobalian A. Serious mental illness diagnosis and COVID-19 vaccine uptake in the veterans health administration. Psychiat Serv. (2022) 73:918–21. doi: 10.1176/appi.ps.202100499
40. Chen A, Beste LA, Strack K, Geyer J, Wheat C, Nelson K, et al. COVID-19 Vaccinations among US veterans with mental illness: a retrospective cohort study. J Gen Intern Med. (2022) 37:3775–7. doi: 10.1007/s11606-022-07763-3
41. Masson CL, McCuistian C, Straus E, Elahi S, Chen M, Gruber VA, et al. COVID-19 vaccine trust among clients in a sample of California residential substance use treatment programs. Drug Alcohol Depend. (2021) 225:108812. doi: 10.1016/j.drugalcdep.2021.108812
42. Powell N, Taylor B, Hotton A, Lamuda P, Flanagan E, Pyra M, et al. The relationship between substance use stigma and COVID-19 vaccine hesitancy. Vaccines. (2023) 11:1194. doi: 10.3390/vaccines11071194
43. Mellis AM, Kelly BC, Potenza MN, Hulsey JN. Trust in a COVID-19 vaccine among people with substance use disorders. Drug Alcohol Depend. (2021) 220:108519. doi: 10.1016/j.drugalcdep.2021.108519
44. Cepeda JA, Feder KA, Astemborski J, Schluth C, Kirk GD, Mehta SH, et al. COVID-19 vaccine hesitancy and vaccination status in a community-based cohort of people who inject drugs in Baltimore, Maryland, March–June 2021. Public Health Rep. (2022) 137:1031–40. doi: 10.1177/00333549221110299
45. Javanbakht M, Khan L, Mustanski B, Shoptaw S, Baum MK, Mehta SH, et al. Substance use and other factors associated with COVID-19 vaccine uptake among people at risk for or living with HIV: findings from the C3PNO consortium. Preventive Medicine Reports. (2023) 24:102300. doi: 10.1016/j.pmedr.2023.102300
46. Strathdee SA, Abramovitz D, Vera CF, Artamonova I, Patterson TL, Smith DM, et al. Predictors of COVID-19 vaccine uptake among people who inject drugs. Vaccine. (2023) 41:1916–24. doi: 10.1016/j.vaccine.2023.01.042
47. Iversen J, Wand H, Kemp R, Bevan J, Briggs M, Patten K, et al. Uptake of COVID-19 vaccination among people who inject drugs. Harm Reduct J. (2022) 19:59. doi: 10.1186/s12954-022-00643-3
48. Lower vaccination rates among people who use drugs could lead to serious outcomes from COVID-19. Vancouver (CA): UBC Faculty of Medicine (2022) Available online at: https://www.med.ubc.ca/news/lower-vaccination-rates-among-people-who-use-drugs-could-lead-to-serious-outcomes-from-covid-19/ (accessed August 11, 2023).
49. National National Academies of Sciences Division Division of Behavioral Board Board on Behavioral Sensory Sciences Committee Committee on the Science of Changing Behavioral Health Social Norms. Ending Discrimination Against People With Mental and Substance use Disorders: The Evidence for Stigma Change. Washington, D.C.: National Academies Press (2016).
50. Van Boekel LC, Brouwers EP, Van Weeghel J, Garretsen HF. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend. (2013) 131:23–35. doi: 10.1016/j.drugalcdep.2013.02.018
51. Ali F, Kaura A, Russell C, Bonn M, Bruneau J, Dasgupta N, et al. Identifying barriers and facilitators to COVID-19 vaccination uptake among People Who Use Drugs in Canada: a National Qualitative study. Harm Reduct J. (2023) 20:1–5. doi: 10.1186/s12954-023-00826-6
52. Karras J, Harrison M, Seale H. ‘Getting the vaccine makes me a champion of it': Exploring perceptions towards peer-to-peer communication about the COVID-19 vaccines amongst Australian adults. Health Expect. (2023) 26:1505–13. doi: 10.1111/hex.13751
53. Kaufman J, Overmars I, Leask J, Seale H, Chisholm M, Hart J, et al. Vaccine champions training program: empowering community leaders to advocate for COVID-19 vaccines. Vaccines. (2022) 10:1893. doi: 10.3390/vaccines10111893
54. Vanderslott S, Joynes-Burgess K, Kadambari S, O'Dwyer E, Alidu L. Examining the role of community champions to promote vaccine uptake in under-served communities in the United Kingdom: Lessons from the COVID-19 pandemic. SSM-Qual Res Health. (2024) 5:100436. doi: 10.1016/j.ssmqr.2024.100436
55. Treloar C, Rance J, Yates K, Mao L. Trust and people who inject drugs: the perspectives of clients and staff of Needle Syringe Programs. Int J Drug Policy. (2016) 27:138–45. doi: 10.1016/j.drugpo.2015.08.018
56. Office of the Auditor General of Ontario. Value-for-Money Audit: COVID-19 Vaccination Program. Available online at: https://www.auditor.on.ca/en/content/annualreports/arreports/en22/AR_COVIDVaccination_en22.pdf (accessed August 11, 2023).
57. Public Health Ontario. Building Confidence in Vaccines. Available online at: https://www.publichealthontario.ca/-/media/documents/ncov/vaccines/2021/04/covid-19-building-confidence-in-vaccines.pdf?la=en (accessed August 11, 2023).
58. City of Toronto. COVID-19: Vaccine Engagement Teams Updates. Available online at: https://www.toronto.ca/community-people/health-wellness-care/health-programs-advice/respiratory-viruses/covid-19/covid-19-vaccines/covid-19-city-immunization-program/vaccine-engagement-teams-updates/ (accessed August 11, 2023).
59. City of Toronto. Toronto is a Global Leader in COVID-19 Vaccination Coverage. Available online at: https://www.toronto.ca/news/toronto-is-a-global-leader-in-covid-19-vaccination-coverage/#:~:text=Overall%2C%20Toronto's%20vaccination%20coverage%20is,than%20the%20other%20cities%20reviewed.&text=As%20of%20March%2017%2C%20approximately,of%20the%20COVID%2D19%20vaccine (accessed August 11, 2023).
60. Richard L, Liu M, Jenkinson JI, Nisenbaum R, Brown M, Pedersen C, et al. COVID-19 vaccine coverage and sociodemographic, behavioural and housing factors associated with vaccination among people experiencing homelessness in Toronto, Canada: a Cross-Sectional Study. Vaccines. (2022) 10:1245. doi: 10.3390/vaccines10081245
61. Blackmore R, Boyle JA, Fazel M, Ranasinha S, Gray KM, Fitzgerald G, et al. The prevalence of mental illness in refugees and asylum seekers: a systematic review and meta-analysis. PLoS Med. (2020) 17:e1003337. doi: 10.1371/journal.pmed.1003337
62. O'Reilly CL, Paul D, McCahon R, Shankar S, Rosen A, Ramzy T. Stigma and discrimination in individuals with severe and persistent mental illness in an assertive community treatment team: Perceptions of families and healthcare professionals. Int J Soc Psychiat. (2019) 65:570–9. doi: 10.1177/0020764019867358
Keywords: COVID-19 vaccination, major mental illness, substance use disorder, Ontario (Canada), disparities (health)
Citation: Richard L, Holland A, Aghanya V, Campitelli MA and Hwang SW (2024) Uptake of COVID-19 vaccination among community-dwelling individuals receiving healthcare for substance use disorder and major mental illness: a matched retrospective cohort study. Front. Public Health 12:1426152. doi: 10.3389/fpubh.2024.1426152
Received: 30 April 2024; Accepted: 24 June 2024;
Published: 05 July 2024.
Edited by:
MinJae Lee, University of Texas Southwestern Medical Center, United StatesReviewed by:
Michele Andrasik, Fred Hutchinson Cancer Center, United StatesDonald K. McInnes, United States Department of Veterans Affairs, United States
Alysse Wurcel, Tufts Medical Center, United States
Copyright © 2024 Richard, Holland, Aghanya, Campitelli and Hwang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lucie Richard, bHVjaWUucmljaGFyZEB1bml0eWhlYWx0aC50bw==
 Lucie Richard
Lucie Richard Anna Holland2
Anna Holland2 Stephen W. Hwang
Stephen W. Hwang