- 1Lianyungang Maternal and Child Health Hospital, Lianyungang, China
- 2Department of Nursing, The First Affiliated Hospital of Dalian Medical University, Dalian, China
- 3Department of Nursing, The Second Affiliated Hospital of Dalian Medical University, Dalian, China
Introduction: Insomnia symptoms are prevalent among healthcare workers and represent a potential public health problem. However, there is currently insufficient evidence on insomnia symptoms among doctors and nurses under the context of high prevalence of multiple infectious diseases after the pandemic in China. The purpose of this study was to analyze the prevalence of insomnia symptoms among doctors and nurses in third-grade class-A general hospitals under the context of high prevalence of multiple infectious diseases, and to explore the influence of demographic characteristics, work-related factors, health and lifestyle-related factors on insomnia symptoms.
Methods: An institution-based cross-sectional survey was conducted among doctors and nurses in two third-grade class-A general hospitals. A structured questionnaire was used to collect information on demographic characteristics, work-related factors, health and lifestyle-related factors, and insomnia symptoms among doctors and nurses. Multivariate logistics regression analysis was applied to identify factors significantly associated with insomnia symptoms among doctors and nurses, respectively.
Results: A total of 1,004 participants were included in this study, including 503 doctors and 501 nurses. The prevalence of insomnia symptoms in doctors and nurses was 47.7 and 51.3%, respectively. Multivariate logistics regression analysis showed that workplace violence (OR: 1.631, 95% CI: 1.050–2.532), doctor-patient relationship (OR: 1.603, 95% CI: 1.049–2.450), chronic pain (OR: 4.134, 95% CI: 2.579–6.625), chronic disease (OR: 1.825, 95% CI: 1.164–2.861), and anxiety symptoms (OR: 2.273, 95% CI: 1.357–3.807) were associated factors with insomnia symptoms in doctors. Education (OR: 0.301, 95% CI: 0.106–0.851), service years (OR: 1.978, 95% CI: 1.304–3.002), weekly working hours (OR: 1.694, 95% CI: 1.061–2.705), chronic pain (OR: 5.359, 95% CI: 3.241–8.860), and anxiety symptoms (OR: 2.472, 95% CI: 1.478–4.136) were associated factors with insomnia symptoms in nurses.
Conclusion: The prevalence of insomnia symptoms among doctors and nurses was high, and affected by many factors. This information can inform tailored interventions to insomnia symptoms by doctors and nurses who play an important role in public health.
Introduction
Sleep is an irreplaceable form of rest that allows the body to function undisturbed and is an important determinant of the level of health (1). Sleep problems have negative effects on the immune system and metabolism and are also associated with diseases such as hypertension (2, 3). In addition, insomnia symptoms affect concentration and are a risk factor for excessive daytime sleepiness (4, 5). Sleep problems also have significant economic costs. The Australian study showed that the financial cost of sleep disorders was equivalent to 0.73% of gross domestic product, and the non-financial cost was 3.2% of the total burden of disease for the year (6).
Healthcare workers were at higher risk for sleep quality problems such as insomnia symptoms than other occupational groups (7, 8). The level of insomnia symptoms in nurses was significantly higher than the normal level in the general population (9). A qualitative analysis of nurses revealed that 92% of participants reported at least one sleep problem, of which 68% were insomnia-related problems (10). A systematic review and meta-analysis revealed an estimated prevalence of insomnia symptoms of healthcare workers during the COVID-19 pandemic of 38.9% (11). Given the prevalence of insomnia symptoms among healthcare workers, it is necessary to develop possible mitigation strategies. One study showed that 95% of nurses expressed interest in participating in sleep interventions (10). Improving insomnia symptoms may provide important benefits to the health of healthcare workers and healthcare system. However, the development of strategies to improve insomnia symptoms first requires the identification of risk factors for insomnia symptoms.
Previous studies among doctors and nurses identified a number of risk factors for insomnia symptoms. Studies in China found that organic diseases were independent factors for insomnia symptoms in healthcare workers (8). Studies in Bangladesh revealed a higher risk of severe insomnia symptoms among female healthcare workers (12). Studies in Greek showed that young nurses were prone to insomnia (13). Studies in Brazilian nurses showed that job strain was associated with increased odds of insomnia symptoms. The prevalence of insomnia symptoms was higher among nurses with particularly low or high body mass index (BMI), no physical activity, high-risk alcohol use, current smoking, and more than 3 cups of coffee per day (14). Studies in Australian nurses found that anxiety and depressive symptoms were significantly associated with insomnia symptoms (9). Studies among both doctors and nurses showed that exposure to workplace violence had a significant influence on sleep quality (15, 16). Although several studies have been published on factors associated with insomnia symptoms among doctors and nurses, there is a lack of studies that simultaneously focus on demographic characteristics, work-related factors, health and lifestyle-related factors, etc. In addition, studies in other populations had shown that pain was positively associated with insomnia symptoms and that family function could help with insomnia symptoms remission (17, 18). However, there is limited evidence regarding the influence of pain and family function on insomnia symptoms among doctors and nurses. We inferred that they might also have an influence on insomnia symptoms among doctors and nurses.
In general, previous evidence on insomnia symptoms has focused more on nurses or healthcare workers as a whole. There is a lack of research on the prevalence and influencing factors of insomnia symptoms among doctors. However, doctors and nurses differ in their duties, healthcare tasks, and hours of work, among others. It is necessary to pay attention to the insomnia symptoms and associated factors of doctors and nurses in the same context. In addition, most studies were conducted during the COVID-19 pandemic, and there was insufficient evidence on insomnia symptoms among doctors and nurses under the context of high prevalence of multiple infectious diseases after the pandemic. Previous study showed no significant change in insomnia symptoms among doctors and nurses 1 year after the end of quarantine (19). At the same time, there is a lack of data on this topic in northeast China. However, there is a large geographic variation in the prevalence of insomnia symptoms (20). It is worth noting that third-grade class-A general hospitals have higher requirements on the professional level, technical ability, academic research, innovation ability and service quality of doctors and nurses than other types of hospitals. However, there is also a lack of information on insomnia symptoms among doctors and nurses in third-grade class-A general hospitals.
In view of this, this study conducted a cross-sectional survey among doctors and nurses in two large third-grade class-A general hospitals in Dalian, Liaoning Province, Northeast China. It aimed to analyze the prevalence of insomnia symptoms among doctors and nurses in third-grade class-A general hospitals under the context of high prevalence of multiple infectious diseases, and to explore the influence of demographic characteristics, work-related factors, health and lifestyle-related factors on insomnia symptoms. This study aimed to assess insomnia symptoms among doctors and nurses separately as important evidence to guide the improvement of insomnia symptoms among doctors and nurses.
Methods
Study design
An institution-based cross-sectional survey was conducted from February to March 2024 in two large third-grade class-A general hospitals in Dalian, Liaoning Province, Northeast China. The two hospitals have strong technical strength and modern medical equipment, and are the university affiliated hospitals with strong comprehensive strength and reliable by the people in Liaoning region.
Participants
Doctors and nurses who met the inclusion criteria and worked in two large third-grade class-A general hospitals were recruited using random sampling. The inclusion criteria were as follows: (1) age ≥ 18 years; (2) the length of service was greater than or equal to 1 year; (3) no history of psychiatric diagnosis; (4) consent to participate in the study. Written informed consent was obtained after a brief explanation to the participants by trained research staff. Also, a self-report questionnaire was distributed to each participant, and the participants were asked to answer each question as honestly and accurately as possible. Participation in the study was anonymous and voluntary, and all questionnaires were completed independently by the participants. The minimum required sample size was obtained using the single population proportion formula. Due to the lack of previous similar studies at this study site, in order to calculate the maximum sample size, a prevalence of insomnia symptoms as 50, 95% confidence interval (CI), a margin error of 5%, and a non-response rate of 20% were used in the current study. The minimum sample size required for the calculation was 461. Considering invalid questionnaires and to obtain more reliable conclusions, we decided to recruit 510 doctors and 510 nurses each. In this study, 1,020 questionnaires were distributed and all of them were recovered, with a recovery rate of 100%. Sixteen questionnaires with missing or identical answers to each question were excluded. Finally, 503 doctors and 501 nurses were included in the statistical analysis, with participation rates of 98.6 and 98.2%, respectively.
Date collection
A structured questionnaire designed after literature review and expert consultation was used for data collection in this study. This structured questionnaire was initially pre-surveyed at the study site and was modified and adjusted. The questionnaire included demographic characteristics, work-related factors, health and lifestyle-related factors, and insomnia symptoms.
Demographic characteristics
Gender, age, marital status, education, and professional title were collected in this study. Age was divided into three ranges including “<30,” “30–40,” and “>40.” Options for marital status included “unmarried,” “married,” and “divorced or loss of spouse.” Education was categorized as “bachelor degree or below” and “master degree or above.” Options for professional title included “no or junior,” “intermediate,” and “senior.”
Work-related factors
Five work-related factors were assessed, including service years, weekly working hours, number of night shifts per month, workplace violence, and doctor-patient relationship. Service years were divided into “≤10” and “>10.” Weekly working hours were divided into “≤40” and “>40.” The number of night shifts per month was divided into “≤3” and “>3.”
Workplace violence was measured using the Workplace Violence Scale (WVS). It was used to assess the frequency of workplace violence experienced by healthcare workers in the past year and has been shown to have satisfactory reliability and validity (21). It consisted of 5 items: physical assault, emotional abuse, threats, verbal sexual harassment, and sexual abuse. The scores of the 5 items were summed to obtain a total WVS score, which ranged from 0 to 15. The higher the score, the higher the frequency of workplace violence experienced by the participant. A total score of 0 was defined as no violence, and a score of 1–5, 6–10, and 11–15 was defined as low, moderate, and high violence, respectively (22). In this study, a score greater than 0 was considered as having experienced workplace violence. In the study context, the Cronbach’s α of the WVS was 0.746.
Doctor-patient relationship was measured using the 10-item Difficult Doctor-Patient Relationship Questionnaire (DDPRQ-10). It was a widely used tool to assess the quality of the doctor-patient relationship from a doctor’s perspective (23, 24). It has already shown satisfactory reliability and validity in the Chinese healthcare setting (25). The DDPRQ-10 consisted of 10 items, each rated on a 5-point Likert scale ranging from 1 (not at all) to 5 (very much). Total scores ranged from 10 to 50, with higher scores indicated a more difficult doctor-patient relationship. In the current study, total scores greater than or equal to the mean were labeled as having a poor doctor-patient relationship (26). In the study context, the Cronbach’s α of the DDPRQ-10 was 0.815.
Health and lifestyle-related factors
Six health and lifestyle-related factors were assessed, including chronic pain, chronic disease, physical exercise, perceived stress, anxiety symptoms, and family function. Chronic pain was measured by asking “Have you had persistent pain in a certain part of your body for at least 1 month?.” Chronic diseases were obtained by asking “Do you have a chronic disease?.” Physical exercise was categorized as “never (0 times/week),” “sometimes (1–3 times/week),” and “often (>3 times/week)” according to the number of weekly exercises (at least 30 min).
Perceived stress was measured using the Perceived Stress Scale-10 (PSS-10) (27). It measured the level of perceived stress of the study subjects in the past month. It consisted of 10 items, each with a 5-point Likert scale ranging from 0 (never) to 4 (almost always). The scores of the 10 items were summed to obtain the total PSS-10 score, which ranged from 0 to 40. Higher scores indicated higher perceived stress among participants. A total score of 15 or greater was defined as perceived higher stress (28). The PSS-10 had been widely used in China and showed good internal consistency (29, 30). In the study context, the Cronbach’s α of the PSS-10 was 0.768.
Anxiety symptoms were measured using the Generalized Anxiety Disorder-7 (GAD-7) (31). It assessed the frequency of anxiety symptom distress in participants over the past 2 weeks. It contained 7 items, each with a Likert scale ranging from 0 (not at all) to 3 (almost every day). The scores of the 7 items were summed to obtain the total GAD-7 score, which ranged from 0 to 21. The higher the score, the higher the degree of anxiety symptoms present by the participant. A total score of 7 or greater was considered the presence of anxiety symptoms (32). The GAD-7 had been widely used and proved to be effective (33, 34). In the study context, the Cronbach’s α of the GAD-7 was 0.928.
Family function was measured using the Family APGAR index (APGAR) (35). The scale consisted of 5 items: adaptation, partnership, growth, affection, and resolve. Five self-reported items were rated using a 3-point Likert scale, with scores ranging from 0 (hardly never) to 2 (always). Total scores varied between 0 and 10, with higher scores reflected better family function. Total scores of 0–6 and 7–10 indicate severe or moderate family dysfunction and good family function, respectively (36). The APGAR had recognized reliability and validity (37). In the study context, the Cronbach’s α of the APGAR was 0.915.
Insomnia symptoms
Insomnia symptoms were measured using the Insomnia Severity Index (ISI) (38). This scale used a 5-point Likert scale to rate 7 self-reported items. The total score was the sum of the scores for each item, ranging from 0 to 28. Higher total scores represented more severe insomnia symptoms. The recommended cut-off value of the scale for detecting insomnia symptoms was 7 (39). Therefore, a total score higher than 7 was considered to have insomnia symptoms in this study. The ISI had already shown good reliability and validity (40, 41). In the study context, the Cronbach’s α of the ISI was 0.926.
Data analysis
Epidata version 3.1 (EpiData Association, Odense, Denmark) software was used for data entry and SPSS version 21.0 (IBM Corporation, Armonk, State of New York) software was used for statistical analysis. Continuous variables were described as means and standard deviations, and categorical variables as frequencies and percentages. Chi-square test and Fisher’s exact test were used to compare the distribution characteristics of insomnia symptoms. Variables with P less than 0.05 in the Chi-square test and Fisher’s exact test were included in the multivariate logistics regression model to identify the independent associated factors with insomnia symptoms in doctors and nurses. Odds ratio (OR) and its 95% CI were calculated. Collinearity tests were performed to test for collinearity between the variables included in the regression model. It was found that the variance inflation factor of each variable was less than 10, and the tolerance was much greater than 0.1. Thus, collinearity between variables was not present. All statistical tests in this study were two-sided, and all hypotheses were tested at the 0.05 significance level.
Results
Characteristics of the participants
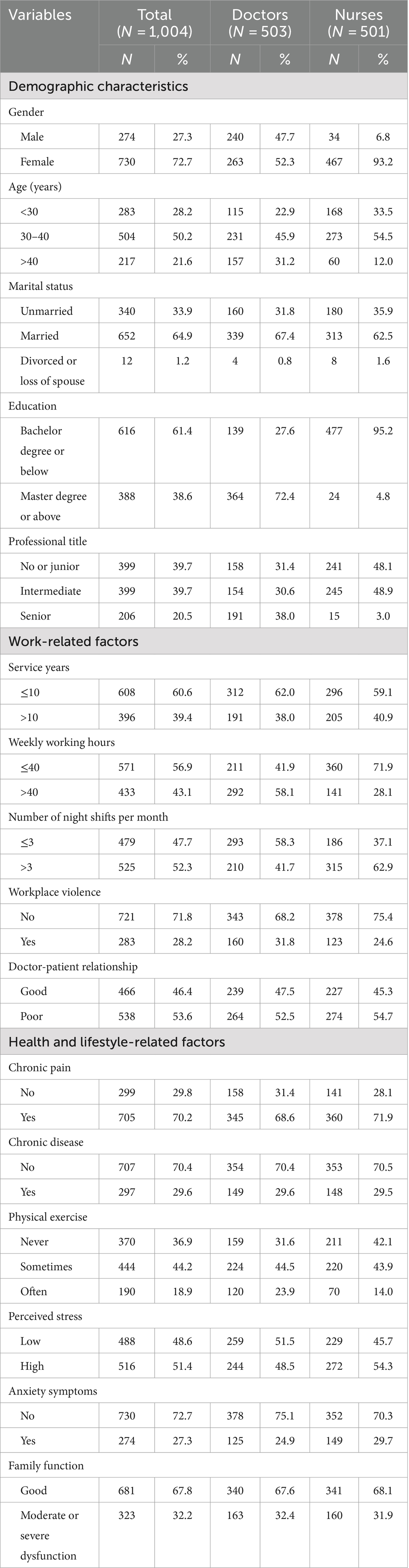
A total of 1,004 participants were included in this study, including 503 doctors and 501 nurses. In terms of demographic characteristics, the mean age of the participants was 34.96 ± 8.41 years, and more than half of the participants (50.2%) were 30 to 40 years of age. Nearly three quarters of the participants (72.7%) were female, and nearly two-thirds (64.9%) were married. The majority of participants (61.4%) had a bachelor degree or below, and almost one-fifth (20.5%) had a senior title. In terms of work-related factors, a small number of participants (39.4%) had worked for more than 10 years. More than half of the participants (56.9%) worked 40 h or less per week, and almost half (52.3%) worked more than 3 night shifts per month. More than a quarter of participants (28.2%) had experienced workplace violence in the past year, and 53.6% had a poor doctor-patient relationship. In terms of health and lifestyle-related factors, a large proportion of participants (70.2%) had pain in at least one body part for more than a month, and a minority (29.6%) had chronic disease. Only 18.9% of the participants often participated in physical exercise, and more than half (51.4%) perceived high stress. More than a quarter of participants (27.3%) had anxiety symptoms, and almost one-third (32.2%) had a moderate or severe family dysfunction (Table 1).
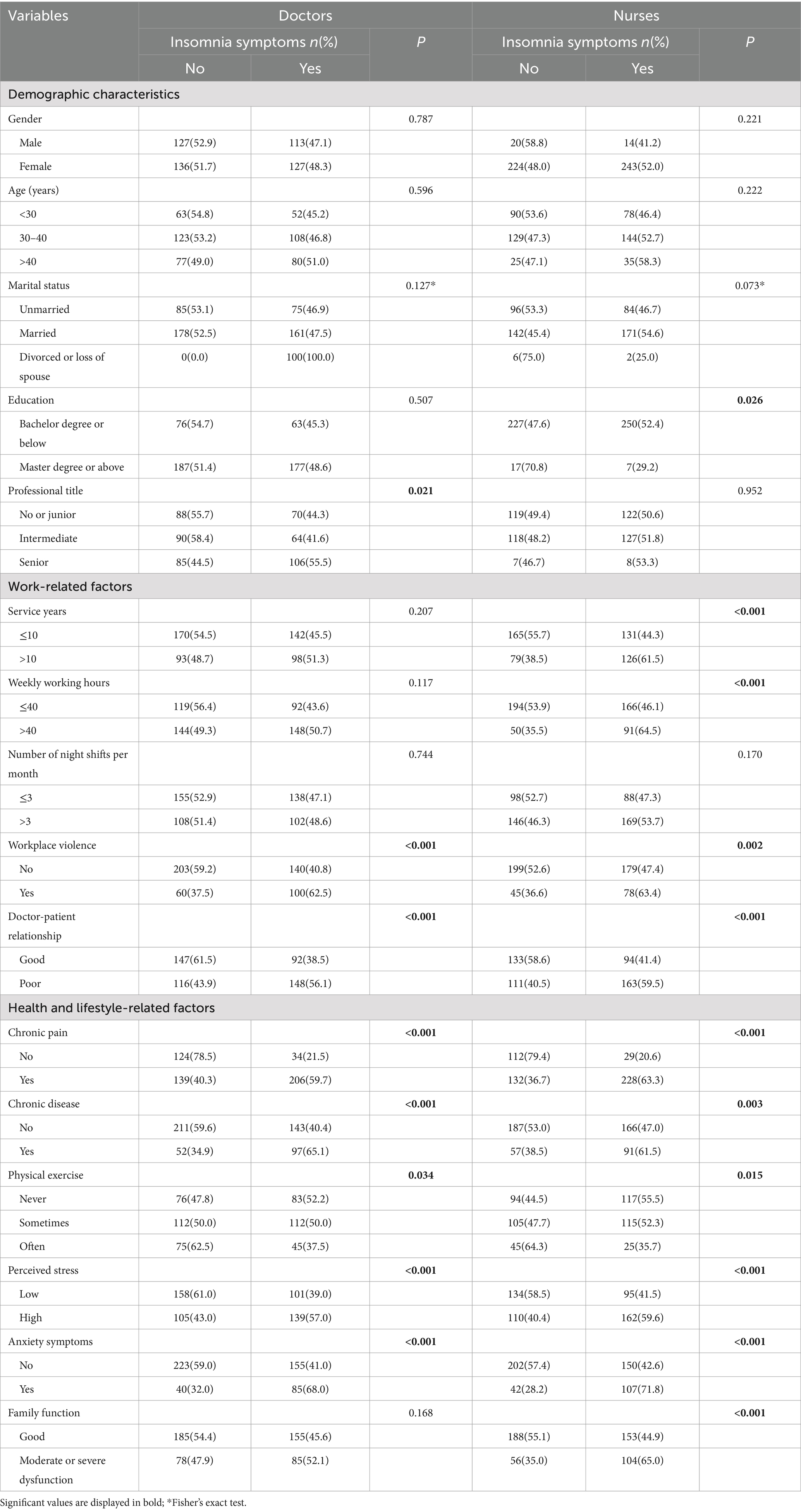
Univariate analysis of insomnia symptoms among doctors and nurses
Among 1,004 participants, the mean score of insomnia symptoms was 7.62 ± 5.68, and the prevalence of insomnia symptoms was 49.5%. The mean scores of insomnia symptoms of doctors and nurses were 7.37 ± 5.49 and 7.88 ± 5.85, respectively, and the prevalence of insomnia symptoms was 47.7 and 51.3%, respectively. Table 2 shows the associations between demographic characteristics, work-related factors, health and lifestyle-related factors and insomnia symptoms. Univariate analysis showed that professional title, workplace violence, doctor-patient relationship, chronic pain, chronic disease, physical exercise, perceived stress and anxiety symptoms were statistically significant with insomnia symptoms among doctors (p < 0.05). Education, service years, weekly working hours, workplace violence, doctor-patient relationship, chronic pain, chronic disease, physical exercise, perceived stress, anxiety symptoms, and family function were statistically significant with insomnia symptoms among nurses (p < 0.05) (Table 2).
Multivariate logistics regression analysis of insomnia symptoms among doctors
Multivariate logistics regression analysis revealed that doctors who had experienced workplace violence were almost 1.631 times more likely to report insomnia symptoms than doctors who had not experienced workplace violence (OR: 1.631, 95% CI: 1.050–2.532). Doctors with poor doctor-patient relationships were almost 1.603 times more likely to report insomnia symptoms than doctors with good doctor-patient relationships (OR: 1.603, 95% CI: 1.049–2.450). Doctors with chronic pain were almost 4.134 times more likely to report insomnia symptoms than doctors without chronic pain (OR: 4.134, 95% CI: 2.579–6.625). Doctors with chronic disease were almost 1.825 times more likely to report insomnia symptoms than doctors without chronic disease (OR: 1.825, 95% CI: 1.164–2.861). Doctors with anxiety symptoms were almost 2.273 times more likely to report insomnia symptoms than doctors without anxiety symptoms (OR: 2.273, 95% CI: 1.357–3.807). Thus, workplace violence, doctor-patient relationship, chronic pain, chronic disease, and anxiety symptoms were associated factors with insomnia symptoms in doctors (Table 3).

Table 3. Multivariate logistics regression analysis of factors associated with insomnia symptoms among doctors.
Multivariate logistics regression analysis of insomnia symptoms among nurses
Multivariate logistics regression analysis revealed that nurses with master degree or above were more likely to avoid developing insomnia symptoms (OR: 0.301, 95% CI: 0.106–0.851). Nurses with more than 10 years of service were almost 1.978 times more likely to have insomnia symptoms than nurses with less than or equal to 10 years of service (OR: 1.978, 95% CI: 1.304–3.002). Nurses who worked more than 40 h per week were almost 1.694 times more likely to have insomnia symptoms than nurses who worked 40 h per week or less (OR: 1.694, 95% CI: 1.061–2.705). Nurses with chronic pain were more likely to have insomnia symptoms (OR: 5.359, 95% CI: 3.241–8.860). Nurses with anxiety symptoms were almost 2.472 times more likely to have insomnia symptoms than nurses without anxiety symptoms (OR: 2.472, 95% CI: 1.478–4.136). Therefore, education, service years, weekly working hours, chronic pain, and anxiety symptoms were associated factors with insomnia symptoms in nurses (Table 4).
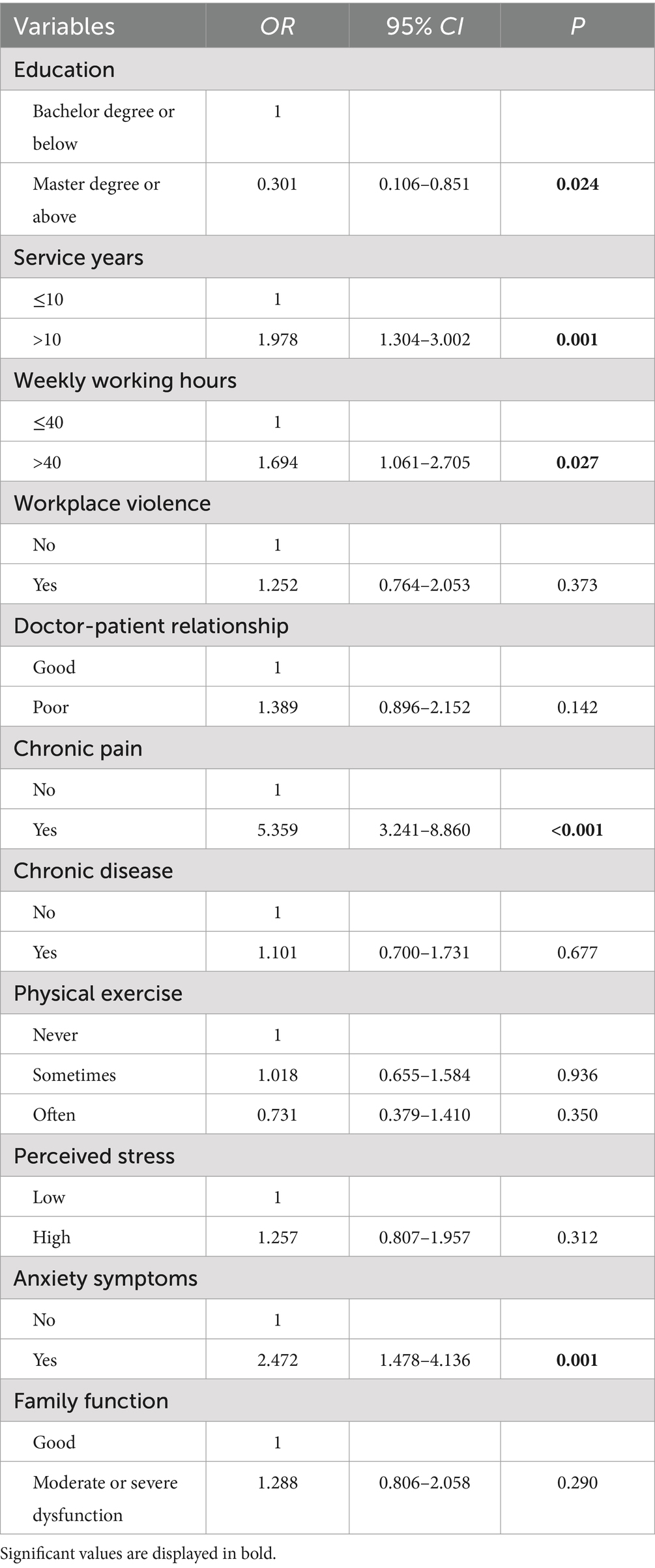
Table 4. Multivariate logistics regression analysis of factors associated with insomnia symptoms among nurses.
Discussion
This cross-sectional study included 503 doctors and 501 nurses. The results showed that the prevalence of insomnia symptoms was high among doctors and nurses in third-grade class-A general hospitals under the context of high prevalence of multiple infectious diseases. The prevalence of insomnia symptoms was 47.7% in doctors and 51.3% in nurses. The prevalence of insomnia symptoms was higher among nurses than among doctors, a finding consistent with the results of previous studies (42, 43). Furthermore, the prevalence of insomnia symptoms among doctors in this study was equivalent to that in Turkey (44.1%) (44). The prevalence of insomnia symptoms among nurses in this study was higher than that in Rio de Janeiro, Brazil (34.3%) and lower than that in Turkey (60.6%) (14, 44). The possible reasons for this were differences in study methods, samples, and contexts. Overall, doctors and nurses are experiencing the effects of insomnia symptoms. Therefore, it is necessary to screen doctors and nurses regularly for insomnia symptoms and provide them with ongoing support. Notably, this study also identified education, service years, weekly working hours, chronic pain, and anxiety symptoms were associated factors with insomnia symptoms in nurses. Workplace violence, doctor-patient relationship, chronic pain, chronic disease, and anxiety symptoms were associated factors with insomnia symptoms in doctors.
Years of education was closely related to sleep disturbances (43). In this study, more insomnia symptoms were observed among nurses with a bachelor degree or below of education. This is similar to previous findings among medical staff that were education level associated with insomnia symptoms (45). This is also consistent with previous studies in the general Chinese population, which showed that low education level was associated with high insomnia symptoms (46). The possible reason for this difference is that nurses with low education level felt inadequate in their nursing ability. Therefore, nurses with low education need more intervention support for insomnia symptoms.
Studies showed that women health workers who have worked for more than 10 years were vulnerable to stress, depression and anxiety (47). Long working years was a risk factor for insomnia in medical staff (48). The present study, similar to previous reports, found that nurses with more than 10 years of service were more likely to develop insomnia symptoms. One possibility is that nurses with longer service years may face more occupational fatigue. Therefore, more attention should be paid to nurses with longer service years in the development of insomnia interventions. Evidence suggested that work overload could predict levels of insomnia (49). This study found that nurses working more than 40 h per week were more likely to experience insomnia symptoms. This may be because nurses are often required to work shifts and longer working hours result in insufficient recovery time between shifts. Insufficient recovery time has been shown to be associated with worse sleep (50). Therefore, reasonable arrangement of nurses’ working time and improvement of nurses’ working efficiency should be paid attention to.
Systematic reviews and meta-analyses have shown a direct relationship between exposure to violence and sleep problems among workers (51). Longitudinal surveys in Swedish suggested an association between the occurrence of workplace violence and the subsequent appearance of sleep disturbances (52). Prevention of workplace violence may improve sleep quality (53). This study also demonstrated that workplace violence was associated with insomnia symptoms in doctors. In China, most doctors have experienced various kinds of violence from patients or their families (15). The current study found that the prevalence of workplace violence in doctors was 31.8%. Workplace violence against doctors has become a public health problem (54). Further research on doctor workplace violence is needed so that effective measures can be taken to prevent doctor workplace violence. This may not only reduce various harms caused by workplace violence, but also reduce the incidence of insomnia symptoms. In China, the doctor-patient relationship is fragile, and most patients do not trust doctors (54). An important reason is that most doctors focus on dealing with technical problems and ignore the humanistic aspects of care (15). In addition, the public is less satisfied with the current doctor-patient relationship (55). This study found that the doctor-patient relationship was an important influencing factor of insomnia symptoms in doctors. Therefore, it is very important to improve the doctor-patient relationship. This requires the engagement and increased effort of healthcare workers, patients and managers.
This study shed new light on a variable rarely mentioned in the previous literature, that was, chronic pain was associated factor for insomnia symptoms among doctors and nurses. This is similar to previous reports in other populations in which frequent pain was significantly associated with an increased prevalence of insomnia symptoms (56). Notably, this study found that 68.6 and 71.9% of doctors and nurses, respectively, had pain in at least one body part for more than 1 month. These findings highlight the importance of assessing and managing pain among doctors and nurses. Insomnia was highly prevalent in patients with chronic diseases (57). This study found that doctors with chronic disease were more likely to report insomnia symptoms. This result is similar to previous findings in which the occurrence of chronic diseases had a statistically significant effect on the severity of negative mental health symptoms such as insomnia (58). The underlying symptoms of chronic diseases themselves and treatment-related factors may interfere with sleep and contribute to the high prevalence of insomnia in this population (59). Therefore, more attention should be paid to doctors with chronic diseases and effective measures should be developed.
There was a bidirectional relationship between anxiety and sleep disturbances (43). The current study found that anxiety symptoms were significantly associated with insomnia symptoms among doctors and nurses. This is supported by previous findings in which anxiety level was an influencing factor for insomnia among front-line medical staff (60). Thus, early recognition of signs of insomnia symptoms is crucial.
Although this study presents some important findings, there are some limitations that need to be mentioned. First, this study was a cross-sectional survey and could not find causal relationships between variables. Therefore, longitudinal research is a direction worthy of attention in the future. Second, we conducted the survey in only one city, which is very small compared to the Chinese population of doctors and nurses. The results can only be generalized to regions with the same background. Therefore, future studies with more regions and larger samples are needed. Finally, this study only focused on third-grade class-A general hospitals and ignored specialized hospitals and primary hospitals. Future studies are recommended to be carried out in hospitals of different nature.
Conclusion
In conclusion, this study demonstrated a high prevalence of insomnia symptoms among doctors and nurses in third-grade class-A general hospitals. Close monitoring and early intervention are essential. This study also identified workplace violence, doctor-patient relationship, chronic pain, chronic disease, and anxiety symptoms were associated factors with insomnia symptoms in doctors. Education, service years, weekly working hours, chronic pain, and anxiety symptoms were associated factors with insomnia symptoms in nurses. This can help doctors and nurses to develop precise interventions for insomnia symptoms, resulting in benefits for doctor and nurse long-term health outcomes, quality of care, and the overall economy.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics Committee of the First Affiliated Hospital of Dalian Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
XC: Conceptualization, Data curation, Methodology, Software, Writing – original draft. BW: Conceptualization, Investigation, Software, Writing – review & editing. YW: Conceptualization, Investigation, Writing – review & editing, Supervision. SH: Investigation, Writing – review & editing. DL: Investigation, Writing – review & editing. DY: Conceptualization, Methodology, Writing – review & editing, Project administration, Supervision.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to thank all the doctors and nurses who took time out of their busy schedules to participate in this study. We would also like to thank those who helped us during the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Knap, M, Maciąg, D, Trzeciak-Bereza, E, Knap, B, Czop, M, and Krupa, S. Sleep disturbances and health consequences induced by the specificity of Nurses' work. Int J Environ Res Public Health. (2022) 19:19. doi: 10.3390/ijerph19169802
2. Irish, LA, Dougall, AL, Delahanty, DL, and Hall, MH. The impact of sleep complaints on physical health and immune outcomes in rescue workers: a 1-year prospective study. Psychosom Med. (2013) 75:196–201. doi: 10.1097/PSY.0b013e31827d85ab
3. Li, Y, Vgontzas, AN, Fernandez-Mendoza, J, Bixler, EO, Sun, Y, Zhou, J, et al. Insomnia with physiological hyperarousal is associated with hypertension. Hypertension. (2015) 65:644–50. doi: 10.1161/hypertensionaha.114.04604
4. Lee, S, Mu, C, Gonzalez, BD, Vinci, CE, and Small, BJ. Sleep health is associated with next-day mindful attention in healthcare workers. Sleep Health. (2021) 7:105–12. doi: 10.1016/j.sleh.2020.07.005
5. Chen, L, Luo, C, Liu, S, Chen, W, Liu, Y, Li, Y, et al. Excessive daytime sleepiness in general hospital nurses: prevalence, correlates, and its association with adverse events. Sleep Breath. (2019) 23:209–16. doi: 10.1007/s11325-018-1684-9
6. Streatfeild, J, Smith, J, Mansfield, D, Pezzullo, L, and Hillman, D. The social and economic cost of sleep disorders. Sleep. (2021) 44:44. doi: 10.1093/sleep/zsab132
7. Huang, Y, and Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. (2020) 288:112954. doi: 10.1016/j.psychres.2020.112954
8. Zhang, WR, Wang, K, Yin, L, Zhao, WF, Xue, Q, Peng, M, et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. (2020) 89:242–50. doi: 10.1159/000507639
9. Khan, WAA, Conduit, R, Kennedy, GA, and Jackson, ML. The relationship between shift-work, sleep, and mental health among paramedics in Australia. Sleep Health. (2020) 6:330–7. doi: 10.1016/j.sleh.2019.12.002
10. Lee, S, Gonzalez, BD, and Small, BJ. My job impacts my sleep: signs and symptoms of insomnia among healthcare workers. Ind Health. (2021) 59:86–98. doi: 10.2486/indhealth.2020-0191
11. Pappa, S, Ntella, V, Giannakas, T, Giannakoulis, VG, Papoutsi, E, and Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. (2020) 88:901–7. doi: 10.1016/j.bbi.2020.05.026
12. Acherjya, GK, Ali, M, Roy, GC, Rahman, MS, Nuruzzaman, M, Biswas, R, et al. Psychological assessment of health-care workers working during COVID-19 pandemic condition in Bangladesh. Mymensingh Med J. (2022) 31:466–76.
13. Kousloglou, S, Mouzas, O, Bonotis, K, Roupa, Z, Vasilopoulos, A, and Angelopoulos, N. Insomnia and burnout in Greek nurses. Hippokratia. (2014) 18:150–5.
14. Portela, LF, Kröning Luna, C, Rotenberg, L, Silva-Costa, A, Toivanen, S, Araújo, T, et al. Job strain and self-reported insomnia symptoms among nurses: what about the influence of emotional demands and social support? Biomed Res Int. (2015) 2015:820610:1–8. doi: 10.1155/2015/820610
15. Sun, T, Gao, L, Li, F, Shi, Y, Xie, F, Wang, J, et al. Workplace violence, psychological stress, sleep quality and subjective health in Chinese doctors: a large cross-sectional study. BMJ Open. (2017) 7:e017182. doi: 10.1136/bmjopen-2017-017182
16. Zhang, SE, Liu, W, Wang, J, Shi, Y, Xie, F, Cang, S, et al. Impact of workplace violence and compassionate behaviour in hospitals on stress, sleep quality and subjective health status among Chinese nurses: a cross-sectional survey. BMJ Open. (2018) 8:e019373. doi: 10.1136/bmjopen-2017-019373
17. Lynch Milder, MK, McQuillan, ME, Honaker, SM, Miller, MM, Tolley, J, Michel, MA, et al. Concurrent and longitudinal associations among insomnia symptoms, internalizing problems, and chronic pain in youth. Health Psychol. (2023) 42:15–23. doi: 10.1037/hea0001244
18. Wang, D, Zhao, J, Zhai, S, Huang, S, Yang, Z, Pan, Y, et al. Longitudinal trajectories of insomnia symptoms among college students during the COVID-19 lockdown in China. J Psychosom Res. (2022) 157:110795. doi: 10.1016/j.jpsychores.2022.110795
19. Li, XJ, Guo, TZ, Xie, Y, Bao, YP, Si, JY, Li, Z, et al. Cross-sectional survey following a longitudinal study on mental health and insomnia of people with sporadic COVID-19. World J Psychiatry. (2022) 12:1076–87. doi: 10.5498/wjp.v12.i8.1076
20. Bjornsdottir, E, Lindberg, E, Benediktsdottir, B, Gislason, T, Garcia Larsen, V, Franklin, K, et al. Are symptoms of insomnia related to respiratory symptoms? Cross-sectional results from 10 European countries and Australia. BMJ Open. (2020) 10:e032511. doi: 10.1136/bmjopen-2019-032511
21. Qiu, T, Liu, C, Huang, H, Yang, S, Gu, Z, Tian, F, et al. The mediating role of psychological capital on the association between workplace violence and professional identity among Chinese doctors: a cross-sectional study. Psychol Res Behav Manag. (2019) 12:209–17. doi: 10.2147/prbm.S198443
22. Tian, Y, Yue, Y, Wang, J, Luo, T, Li, Y, and Zhou, J. Workplace violence against hospital healthcare workers in China: a national WeChat-based survey. BMC Public Health. (2020) 20:582. doi: 10.1186/s12889-020-08708-3
23. Hahn, SR, Thompson, KS, Wills, TA, Stern, V, and Budner, NS. The difficult doctor-patient relationship: somatization, personality and psychopathology. J Clin Epidemiol. (1994) 47:647–57. doi: 10.1016/0895-4356(94)90212-7
24. Hahn, SR. Physical symptoms and physician-experienced difficulty in the physician-patient relationship. Ann Intern Med. (2001) 134:897–904. doi: 10.7326/0003-4819-134-9_part_2-200105011-00014
25. Du, J, Wang, Y, Wu, A, Jiang, Y, Duan, Y, Geng, W, et al. The validity and IRT psychometric analysis of Chinese version of difficult doctor-patient relationship questionnaire (DDPRQ-10). BMC Psychiatry. (2023) 23:900. doi: 10.1186/s12888-023-05385-5
26. Molla, A, Mekuriaw, B, and Kerebih, H. Depression and associated factors among patients with tuberculosis in Ethiopia: a cross-sectional study. Neuropsychiatr Dis Treat. (2019) 15:1887–93. doi: 10.2147/ndt.S208361
27. Cohen, S, Kamarck, T, and Mermelstein, R. A global measure of perceived stress. J Health Soc Behav. (1983) 24:385–96. doi: 10.2307/2136404
28. Liu, Y, Chen, H, Zhang, N, Wang, X, Fan, Q, Zhang, Y, et al. Anxiety and depression symptoms of medical staff under COVID-19 epidemic in China. J Affect Disord. (2021) 278:144–8. doi: 10.1016/j.jad.2020.09.004
29. Jiang, C, Jiang, W, Yue, Y, Li, L, Sun, T, Chen, G, et al. The trends of psychosomatic symptoms and perceived stress among healthcare workers during the COVID-19 pandemic in China: four cross-sectional nationwide surveys, 2020-2023. Psychiatry Res. (2023) 326:115301. doi: 10.1016/j.psychres.2023.115301
30. Xiong, J, Ma, H, Ma, R, Xu, T, and Wang, Y. The relationship between perceived stress and prolonged grief disorder among Chinese Shidu parents: effects of anxiety and social support. BMC Psychiatry. (2023) 23:714. doi: 10.1186/s12888-023-05206-9
31. Spitzer, RL, Kroenke, K, Williams, JB, and Löwe, B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
32. Wu, F, Zhou, L, Chen, C, Lin, W, Liu, P, Huang, W, et al. Association between intimate partner violence and prenatal anxiety and depression in pregnant women: a cross-sectional survey during the COVID-19 epidemic in Shenzhen, China. BMJ Open. (2022) 12:e055333. doi: 10.1136/bmjopen-2021-055333
33. Sun, L, Wang, X, Hong, Y, Li, C, Zeng, W, Liu, P, et al. COVID-19 pandemic-related depression and anxiety under lockdown: the chain mediating effect of self-efficacy and perceived stress. Front Psych. (2023) 14:1100242. doi: 10.3389/fpsyt.2023.1100242
34. Gong, Y, Zhou, H, Zhang, Y, Zhu, X, Wang, X, Shen, B, et al. Validation of the 7-item generalized anxiety disorder scale (GAD-7) as a screening tool for anxiety among pregnant Chinese women. J Affect Disord. (2021) 282:98–103. doi: 10.1016/j.jad.2020.12.129
35. Smilkstein, G. The family APGAR: a proposal for a family function test and its use by physicians. J Fam Pract. (1978) 6:1231–9.
36. Shao, R, He, P, Ling, B, Tan, L, Xu, L, Hou, Y, et al. Prevalence of depression and anxiety and correlations between depression, anxiety, family functioning, social support and coping styles among Chinese medical students. BMC Psychol. (2020) 8:38. doi: 10.1186/s40359-020-00402-8
37. Smilkstein, G, Ashworth, C, and Montano, D. Validity and reliability of the family APGAR as a test of family function. J Fam Pract. (1982) 15:303–11.
38. Morin, CM, Belleville, G, Bélanger, L, and Ivers, H. The insomnia severity index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. (2011) 34:601–8. doi: 10.1093/sleep/34.5.601
39. Lai, J, Ma, S, Wang, Y, Cai, Z, Hu, J, Wei, N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
40. Liu, Z, Liu, R, Zhang, Y, Zhang, R, Liang, L, Wang, Y, et al. Association between perceived stress and depression among medical students during the outbreak of COVID-19: the mediating role of insomnia. J Affect Disord. (2021) 292:89–94. doi: 10.1016/j.jad.2021.05.028
41. Bastien, CH, Vallières, A, and Morin, CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. (2001) 2:297–307. doi: 10.1016/s1389-9457(00)00065-4
42. Dragioti, E, Tsartsalis, D, Mentis, M, Mantzoukas, S, and Gouva, M. Impact of the COVID-19 pandemic on the mental health of hospital staff: an umbrella review of 44 meta-analyses. Int J Nurs Stud. (2022) 131:104272. doi: 10.1016/j.ijnurstu.2022.104272
43. Wang, P, Shen, X, Jiang, Y, Wu, L, Shen, J, Nie, X, et al. Psychological and sleep disturbances among first-line, second-line, and at home medical staff during the COVID-19 pandemic in Shanghai, China. Front Public Health. (2022) 10:1006610. doi: 10.3389/fpubh.2022.1006610
44. Şahin, MK, Aker, S, Şahin, G, and Karabekiroğlu, A. Prevalence of depression, anxiety, distress and insomnia and related factors in healthcare workers during COVID-19 pandemic in Turkey. J Community Health. (2020) 45:1168–77. doi: 10.1007/s10900-020-00921-w
45. Zhang, C, Yang, L, Liu, S, Ma, S, Wang, Y, Cai, Z, et al. Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Front Psych. (2020) 11:306. doi: 10.3389/fpsyt.2020.00306
46. Xiang, YT, Ma, X, Cai, ZJ, Li, SR, Xiang, YQ, Guo, HL, et al. The prevalence of insomnia, its sociodemographic and clinical correlates, and treatment in rural and urban regions of Beijing, China: a general population-based survey. Sleep. (2008) 31:1655–62. doi: 10.1093/sleep/31.12.1655
47. Li, G, Miao, J, Wang, H, Xu, S, Sun, W, Fan, Y, et al. Psychological impact on women health workers involved in COVID-19 outbreak in Wuhan: a cross-sectional study. J Neurol Neurosurg Psychiatry. (2020) 91:895–7. doi: 10.1136/jnnp-2020-323134
48. Cheng, Z, Tao, Y, Liu, T, He, S, Chen, Y, Sun, L, et al. Psychology, stress, insomnia, and resilience of medical staff in China during the COVID-19 policy opening: a cross-sectional survey. Front Public Health. (2023) 11:1249255. doi: 10.3389/fpubh.2023.1249255
49. Mennicken, B, Petit, G, Yombi, JC, Belkhir, L, Deschietere, G, Germeau, N, et al. Psychological distress among hospital caregivers during and after the first wave of COVID-19: individual factors involved in the severity of symptoms expression. Psychiatry Res Commun. (2022) 2:100037. doi: 10.1016/j.psycom.2022.100037
50. Querstret, D, O'Brien, K, Skene, DJ, and Maben, J. Improving fatigue risk management in healthcare: a scoping review of sleep-related/fatigue-management interventions for nurses and midwives (reprint). Int J Nurs Stud. (2020) 112:103745. doi: 10.1016/j.ijnurstu.2020.103745
51. Magnavita, N, Di Stasio, E, Capitanelli, I, Lops, EA, Chirico, F, and Garbarino, S. Sleep problems and workplace violence: a systematic review and Meta-analysis. Front Neurosci. (2019) 13:997. doi: 10.3389/fnins.2019.00997
52. Heming, M, Xu, T, Nyberg, A, and Magnusson Hanson, LL. The relationship between onset of workplace violence and onset of sleep disturbances in the Swedish working population. J Sleep Res. (2021) 30:e13307. doi: 10.1111/jsr.13307
53. Magnavita, N, Mele, L, Meraglia, I, Merella, M, Vacca, ME, Cerrina, A, et al. The impact of workplace violence on headache and sleep problems in nurses. Int J Environ Res Public Health. (2022) 19:19. doi: 10.3390/ijerph192013423
54. Pan, Y, Yang, X, He, JP, Gu, YH, Zhan, XL, Gu, HF, et al. To be or not to be a doctor, that is the question: a review of serious incidents of violence against doctors in China from 2003–2013. J Public Health. (2015) 23:111–6. doi: 10.1007/s10389-015-0658-7
55. Shi, J, Jiang, Y, Hu, P, Gong, Y, and Li, Y. A surveying study on social satisfaction to current doctor-patient relationship in China. J Serv Sci Manag. (2015) 8:695–702. doi: 10.4236/jssm.2015.85071
56. Liu, X, Yang, Y, Liu, ZZ, and Jia, CX. A longitudinal study of bidirectional associations between frequent pain and insomnia symptoms in adolescents. Sleep Health. (2022) 8:467–74. doi: 10.1016/j.sleh.2022.05.009
57. Hayes, D Jr, Anstead, MI, Ho, J, and Phillips, BA. Insomnia and chronic heart failure. Heart Fail Rev. (2009) 14:171–82. doi: 10.1007/s10741-008-9102-1
58. Lewko, J, Misiak, B, and Sierżantowicz, R. The relationship between mental health and the quality of life of polish nurses with many years of experience in the profession: a cross-sectional study. Int J Environ Res Public Health. (2019) 16:798. doi: 10.3390/ijerph16101798
59. Lindner, AV, Novak, M, Bohra, M, and Mucsi, I. Insomnia in patients with chronic kidney disease. Semin Nephrol. (2015) 35:359–72. doi: 10.1016/j.semnephrol.2015.06.007
Keywords: insomnia symptoms, associated factors, doctors, nurses, China
Citation: Chen X, Wang B, Wang Y, He S, Liu D and Yan D (2024) Prevalence and associated factors of insomnia symptoms among doctors and nurses under the context of high prevalence of multiple infectious diseases: a cross-sectional study. Front. Public Health. 12:1423216. doi: 10.3389/fpubh.2024.1423216
Edited by:
Tao Rui, Chaohu Hospital of Anhui Medical University, ChinaReviewed by:
Mo Daming, Hefei Fourth People’s Hospital, ChinaDaomin Zhu, Hefei Fourth People’s Hospital, China
Copyright © 2024 Chen, Wang, Wang, He, Liu and Yan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dongmei Yan, NTk2NzUxNjc1QHFxLmNvbQ==
†These authors have contributed equally to this work
 Xu Chen
Xu Chen Bin Wang
Bin Wang Yu Wang3†
Yu Wang3† Dongmei Yan
Dongmei Yan